User login
RSS feeds are a versatile online tool
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Recently I mentioned RSS news feeds as a useful, versatile online tool, but because it has been a while since I’ve discussed RSS feeds, an update is certainly in order.
The sheer volume of information on the web makes quick and efficient searching an indispensable skill, but once you have become quick and efficient at finding the information you need, a new problem arises: The information changes! All the good medical, news, and other information-based websites change and update their content on a regular, but unpredictable basis. And checking each one for new information can be very tedious, if you can remember to do it at all.
Many sites offer an e-mail service to notify you of new content, but multiple e-mail subscriptions clutter your inbox and often can’t select out the information you’re really interested in. RSS (which stands for “Rich Site Summary” or “Really Simple Syndication,” depending on whom you ask) is a file format, and websites use that format (or a similar one called Atom) to produce a summary file, or “feed,” of new content, along with links to full versions of that content. When you subscribe to a given website’s feed, you’ll receive a summary of new content each time the website is updated.
Thousands of websites now offer RSS feeds, including most of the large medical information services, all the major news organizations, and many web logs.
Many readers are free, but those with the most advanced features usually charge a fee of some sort. (As always, I have no financial interest in any enterprise discussed in this column.) A comprehensive and more or less up-to-date list of available readers can be found in the Wikipedia article “Comparison of feed aggregators.”
It’s not always easy to find out whether a particular website offers a feed, because there is no universally recognized method of indicating its existence. Look for a link to “RSS” or “Syndicate This,” or an orange rectangle with the letters “RSS,” or “XML” (don’t ask). These links are not always on the home page. You may need to consult the site map to find a link to a page explaining available feeds, and how to find them.
Some of the major sites have multiple feeds to choose from. For example, you can generate a feed of current stories related to the page that you are following on Google News by clicking the RSS link on any Google News page.
In addition to notifying you of important news headlines, changes to your favorite websites, and new developments in any medical (or other) field of interest to you, RSS feeds have many other uses. Some will notify you of new products in a store or catalog, new newsletter issues (including e-mail newsletters), weather and other changing-condition alerts, and the addition of new items to a database – or new members to a group.
It can work the other way as well: If you want readers of your website, blog, or podcast to receive the latest news about your practice, such as new treatments and procedures you’re offering – or if you want to know immediately anytime your name pops up in news or gossip sites – you can create your own RSS feed. Next month, I’ll explain exactly how to do that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Accounting 101: Basics you need to know
Physicians practice medicine and communicate within the world of medical language, yet there is a lack of awareness and understanding by many health care professionals of the universal language of business, which is accounting. Just as Latin provides the basic framework for medically related terminology, accounting is the standard language used to convey financial information to both internal and external stakeholders.
Accounting principles are important to physicians at any level. Whether you are starting out in private practice, running a clinical department, or working as an executive in a health care system, most decisions are based on the interpretation of financial data using accounting principles. Accounting standards in the United States are developed by the Financial Accounting Standard Board (FASB) and established as a set of principles and guidelines called Generally Accepted Accounting Principles (GAAP).1–3
Accrual- vs cash-based accounting
There are 2 approaches to recording financial transactions: accrual- and cash-based accounting methods. The main difference between them is in the timing of the recorded financial transactions (when revenue and expenses are recognized on the accounting books). Under GAAP, the matching principle, which is one of the most basic and utilized guidelines of accounting, specifies that accrual accounting be used. In the United States, most businesses (publically traded companies and moderate- to large-sized companies) use accrual accounting, while some individual and smaller businesses, including health care services such as physician practices, use the cash method.1–4
Accrual-based accounting
Accrual-based accounting specifies that revenues are recorded when they are earned, and expenses are recorded when they occur. A health care business may earn revenue for services on one day, but the cash may not be received or recorded on the accounting books for several weeks or months and at an amount less than billed.
Accrual-based accounting provides a more accurate representation of a business’ financial performance, since it uses the principle in which expenses are matched to revenues in the same time period. This enables a more precise representation of true financial performance during a given time frame.1–4
Cash-based accounting
Cash-based accounting is the easiest method to understand and implement because financial transactions are recorded in the accounting books when money is received or spent without the need for complex accounting techniques or integration of accounts receivable or payable.
Despite the ease of use and simplicity in tracking cash flow, this method can be deceiving because revenue may be received or expenses may need to be paid at times that are not consistent with when the revenue has been earned or expenses incurred. This can result in misleading information on the business’ health and the accuracy of tracking financial performance over time, since revenue and expenses for a particular transaction may occur at different times.1–4
Which accounting process to choose?
Even though accrual-based accounting may provide a more accurate financial representation of a business’ performance, many smaller businesses, including physician practices, prefer to use cash-based accounting. In addition, many health care businesses are eligible to use cash-based accounting per Internal Revenue Service (IRS) rules by qualifying for the Gross Receipts Test and being a qualified Personal Service Corporation (PSC):
- The Gross Receipts Test states that if the average annual gross receipts of the business are less than $5 million, the business can use the cash-based accounting method.
- If at least 95% of a business activity involves performing health care services, and at least 95% of the business is owned by employees performing health care services, then the business qualifies as a PSC that may use the cash-based accounting method.
Many physician practices qualify to use cash-based accounting, which reduces the complexity of following accrual-based accounting rules and simplifies overall cash-flow management.5
Read about insurance, capital equipment depreciation, more
CASE New practice opens
Practice A opens its practice on January 1. The practice borrows $20,000 from the bank to purchase hysteroscopic equipment for office-based tubal sterilizations and an additional $50,000 for an ultrasound machine. Both loans have a 5% annual interest rate amortized over 5 years. The practice leases office space and pays rent 2 months in advance at $8,000 ($4,000 per month). On January 1, the practice pays a $1,200 premium for annual property and liability insurance and $12,500 for the first quarter payment for professional liability insurance ($50,000 annually, paid quarterly). Other costs the practice pays in January include: utilities, $400; EHR licensing, $300; technical support, $200; and salaries, $10,000.
The practice purchases 4 sets of sterilization spring devices at $1,500 each ($6,000) to have in stock. One hysteroscopic sterilization procedure is performed on a patient in January using 1 device. The practice is reimbursed $2,500 for the procedure.
In January, the practice bills $150,000 in charges, but after insurance contractual adjustments, January’s revenue is $50,000. Actual cash payments from billings received are $10,000 in January, $30,000 in February, and $10,000 in March.
At first glance, there is a noticeable difference on the sales or recognition of revenues based on the type of accounting (TABLE). With the accrual method, because the billing charges are submitted in January when the services were provided (minus the insurance contractual adjustments), the $50,000 revenue is immediately counted and recognized, even though the practice only received $10,000 cash for those billings during January. While the benefit to accrual accounting is the timely recognition of the revenue when the service was provided, the downside is that much of those billings might actually be paid over 90 days, and some of those billings may go unpaid by the insurance company or the patients, which would require adjustments in later months.
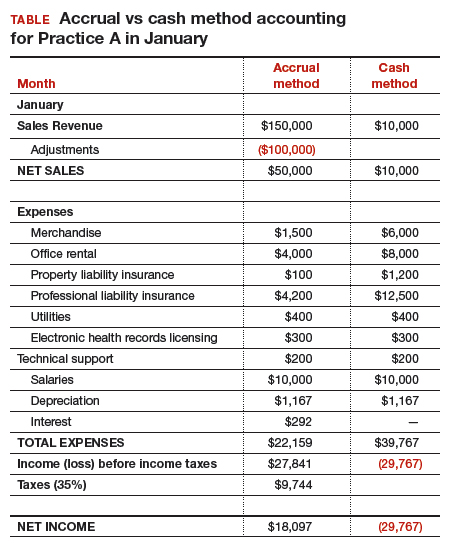
The cash-based method is simpler to understand because the cash received for the month is recognized as the revenue, regardless of the amount charged that month.
Merchandise. In the accrual method, the cost of merchandise sold (the hysteroscopic sterilization implants) is recognized as an expense when the revenue is generated from its sale. In this case, the date that the patient has the hysteroscopic in-office sterilization procedure is when the revenue and the expense of the implant are recognized.
In a cash-based accounting method, the $6,000 cost of the implants is recognized at the time of purchase in January.
Lease. In this scenario, even though 2 months of lease for the office were paid, the accrual method only recognizes the January payment; the second payment is recognized in February. In the cash method, because both months were paid in January, the total expense of $8,000 is recognized in January.
Property liability insurance. The property liability insurance payment is required at the start of the year. In accrual accounting, this expense is divided over 12 months, while in the cash method, the expense is counted at the time the payment is made.
Professional liability insurance. The professional liability insurance expense of $50,000 per year is made in quarterly payments, so for the accrual method, the annual amount would be distributed over 12 months at $4,200 per month. With the cash method, it would be paid—and recognized as an expense—quarterly at $12,500, starting in January.
Capital equipment depreciation. Capital medical equipment (hysteroscopy and ultrasound) can be depreciated using a straight-line 5-year depreciation. A total $70,000 worth of equipment divided by 5 years is $14,000 per year, depreciated over 5 years. One-twelfth of $14,000 equals $1,167, which is recorded as a January depreciation expense. Because the Internal Revenue Code requires capital assets to be depreciated, even for cash-basis taxpayers, the common practice is to record depreciation expense for both cash- and accrual-basis income accounting.6
Interest on loans. A loan’s principal payment will not be included on the income statement. The principal payment, a reduction of a liability (loans payable), is reported on the balance sheet. Only the interest portion of a loan payment is reported on the income statement (interest expense). In accrual accounting, the accrued interest on the loan payment for the year is $3,500 ($292 for January). For the cash-basis method, because the interest is paid annually at year-end, interest will not be expensed until December.
Taxes. The IRS states that, “Individuals, including sole proprietors, partners, and S corporation shareholders, generally have to make estimated tax payments if they expect to owe tax of $1,000 or more when their return is filed. Corporations generally have to make estimated tax payments if they expect to owe tax of $500 or more when their return is filed.”7
Assuming 35% tax liability, the accrual method would create a tax liability of $9,744 on a profit of $27,841. With the cash method, there would be no tax liability because there was no net profit.
Other expenses. The utilities, EHR licensing, tech support, and salaries are expensed the same way for both methods.
Net income. The resulting final net income is vastly different for the month of January depending on the accounting method utilized. The accrual method results in a net income of $18,097, while the cash-basis method results in a net loss of $29,767. Over the course of the year, these imbalances are likely to even out.
Related article:
Business law critical to your practice
Choosing an accounting method
Depending on the accounting method, a practice’s performance and profit will seem very different. The type of accounting method chosen will depend on what goals the owners want to achieve.
The accrual method provides a more accurate picture of business flow and performance and will be less subject to monthly variations due to large purchases or variations in expenses. If the practice chooses this method using an income statement, it should also employ a cash-flow statement.
The cash method of accounting will give a convenient and practical summary of the practice’s cash flow.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- About the FASB. Financial Accounting Standards Board website. http://www.fasb.org/jsp/FASB/PageSectionPage&cid=1176154526495. Accessed November 7, 2017.
- What is the difference between accrual accounting and cash accounting? Investopedia. https://www.investopedia.com/ask/answers/121514/what-difference-between-accrual-accounting-and-cash-accounting.asp. Accessed November 7, 2017.
- Accounting Basics (Explanation). Part 2: Income Statement. Accounting Coach. https://www.accountingcoach.com/accounting-basics/explanation/2. Accessed November 7, 2017.
- Stickney C, Weil R. Financial Accounting: An Introduction to Concepts, Methods, and Uses. 11th ed. Nashville, TN: Southwestern College Publishing Group; 2006:97-110.
- Internal Revenue Service. Publication 538 (12/2016), Accounting Periods and Methods. https://www.irs.gov/publications/p538#en_US_201612_publink1000270634. Revised December 2016. Accessed November 7, 2017.
- Klinefelter D, McCorkle D, Klose S. Financial Management: Cash vs. Accrual Accounting. Risk Management. AgriLife Extension. Texas A&M System. http://agrilife.org/agecoext/files/2013/10/rm5-16.pdf. Published 2013. Accessed November 7, 2017.
- Internal Revenue Service. Small Business and Self-Employed Tax Center: Estimated Taxes. https://www.irs.gov/businesses/small-businesses-self-employed/estimated-taxes. Updated November 2, 2017. Accessed November 7, 2017.
Physicians practice medicine and communicate within the world of medical language, yet there is a lack of awareness and understanding by many health care professionals of the universal language of business, which is accounting. Just as Latin provides the basic framework for medically related terminology, accounting is the standard language used to convey financial information to both internal and external stakeholders.
Accounting principles are important to physicians at any level. Whether you are starting out in private practice, running a clinical department, or working as an executive in a health care system, most decisions are based on the interpretation of financial data using accounting principles. Accounting standards in the United States are developed by the Financial Accounting Standard Board (FASB) and established as a set of principles and guidelines called Generally Accepted Accounting Principles (GAAP).1–3
Accrual- vs cash-based accounting
There are 2 approaches to recording financial transactions: accrual- and cash-based accounting methods. The main difference between them is in the timing of the recorded financial transactions (when revenue and expenses are recognized on the accounting books). Under GAAP, the matching principle, which is one of the most basic and utilized guidelines of accounting, specifies that accrual accounting be used. In the United States, most businesses (publically traded companies and moderate- to large-sized companies) use accrual accounting, while some individual and smaller businesses, including health care services such as physician practices, use the cash method.1–4
Accrual-based accounting
Accrual-based accounting specifies that revenues are recorded when they are earned, and expenses are recorded when they occur. A health care business may earn revenue for services on one day, but the cash may not be received or recorded on the accounting books for several weeks or months and at an amount less than billed.
Accrual-based accounting provides a more accurate representation of a business’ financial performance, since it uses the principle in which expenses are matched to revenues in the same time period. This enables a more precise representation of true financial performance during a given time frame.1–4
Cash-based accounting
Cash-based accounting is the easiest method to understand and implement because financial transactions are recorded in the accounting books when money is received or spent without the need for complex accounting techniques or integration of accounts receivable or payable.
Despite the ease of use and simplicity in tracking cash flow, this method can be deceiving because revenue may be received or expenses may need to be paid at times that are not consistent with when the revenue has been earned or expenses incurred. This can result in misleading information on the business’ health and the accuracy of tracking financial performance over time, since revenue and expenses for a particular transaction may occur at different times.1–4
Which accounting process to choose?
Even though accrual-based accounting may provide a more accurate financial representation of a business’ performance, many smaller businesses, including physician practices, prefer to use cash-based accounting. In addition, many health care businesses are eligible to use cash-based accounting per Internal Revenue Service (IRS) rules by qualifying for the Gross Receipts Test and being a qualified Personal Service Corporation (PSC):
- The Gross Receipts Test states that if the average annual gross receipts of the business are less than $5 million, the business can use the cash-based accounting method.
- If at least 95% of a business activity involves performing health care services, and at least 95% of the business is owned by employees performing health care services, then the business qualifies as a PSC that may use the cash-based accounting method.
Many physician practices qualify to use cash-based accounting, which reduces the complexity of following accrual-based accounting rules and simplifies overall cash-flow management.5
Read about insurance, capital equipment depreciation, more
CASE New practice opens
Practice A opens its practice on January 1. The practice borrows $20,000 from the bank to purchase hysteroscopic equipment for office-based tubal sterilizations and an additional $50,000 for an ultrasound machine. Both loans have a 5% annual interest rate amortized over 5 years. The practice leases office space and pays rent 2 months in advance at $8,000 ($4,000 per month). On January 1, the practice pays a $1,200 premium for annual property and liability insurance and $12,500 for the first quarter payment for professional liability insurance ($50,000 annually, paid quarterly). Other costs the practice pays in January include: utilities, $400; EHR licensing, $300; technical support, $200; and salaries, $10,000.
The practice purchases 4 sets of sterilization spring devices at $1,500 each ($6,000) to have in stock. One hysteroscopic sterilization procedure is performed on a patient in January using 1 device. The practice is reimbursed $2,500 for the procedure.
In January, the practice bills $150,000 in charges, but after insurance contractual adjustments, January’s revenue is $50,000. Actual cash payments from billings received are $10,000 in January, $30,000 in February, and $10,000 in March.
At first glance, there is a noticeable difference on the sales or recognition of revenues based on the type of accounting (TABLE). With the accrual method, because the billing charges are submitted in January when the services were provided (minus the insurance contractual adjustments), the $50,000 revenue is immediately counted and recognized, even though the practice only received $10,000 cash for those billings during January. While the benefit to accrual accounting is the timely recognition of the revenue when the service was provided, the downside is that much of those billings might actually be paid over 90 days, and some of those billings may go unpaid by the insurance company or the patients, which would require adjustments in later months.
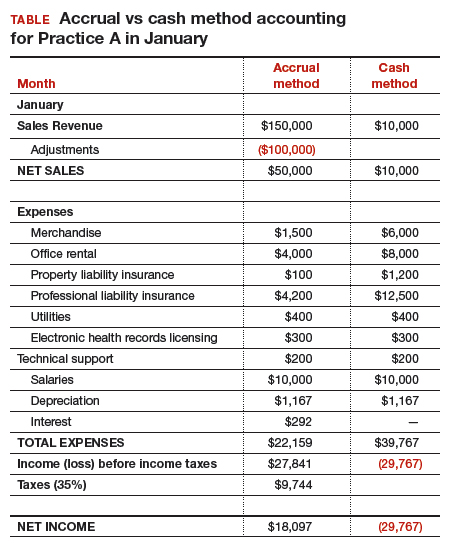
The cash-based method is simpler to understand because the cash received for the month is recognized as the revenue, regardless of the amount charged that month.
Merchandise. In the accrual method, the cost of merchandise sold (the hysteroscopic sterilization implants) is recognized as an expense when the revenue is generated from its sale. In this case, the date that the patient has the hysteroscopic in-office sterilization procedure is when the revenue and the expense of the implant are recognized.
In a cash-based accounting method, the $6,000 cost of the implants is recognized at the time of purchase in January.
Lease. In this scenario, even though 2 months of lease for the office were paid, the accrual method only recognizes the January payment; the second payment is recognized in February. In the cash method, because both months were paid in January, the total expense of $8,000 is recognized in January.
Property liability insurance. The property liability insurance payment is required at the start of the year. In accrual accounting, this expense is divided over 12 months, while in the cash method, the expense is counted at the time the payment is made.
Professional liability insurance. The professional liability insurance expense of $50,000 per year is made in quarterly payments, so for the accrual method, the annual amount would be distributed over 12 months at $4,200 per month. With the cash method, it would be paid—and recognized as an expense—quarterly at $12,500, starting in January.
Capital equipment depreciation. Capital medical equipment (hysteroscopy and ultrasound) can be depreciated using a straight-line 5-year depreciation. A total $70,000 worth of equipment divided by 5 years is $14,000 per year, depreciated over 5 years. One-twelfth of $14,000 equals $1,167, which is recorded as a January depreciation expense. Because the Internal Revenue Code requires capital assets to be depreciated, even for cash-basis taxpayers, the common practice is to record depreciation expense for both cash- and accrual-basis income accounting.6
Interest on loans. A loan’s principal payment will not be included on the income statement. The principal payment, a reduction of a liability (loans payable), is reported on the balance sheet. Only the interest portion of a loan payment is reported on the income statement (interest expense). In accrual accounting, the accrued interest on the loan payment for the year is $3,500 ($292 for January). For the cash-basis method, because the interest is paid annually at year-end, interest will not be expensed until December.
Taxes. The IRS states that, “Individuals, including sole proprietors, partners, and S corporation shareholders, generally have to make estimated tax payments if they expect to owe tax of $1,000 or more when their return is filed. Corporations generally have to make estimated tax payments if they expect to owe tax of $500 or more when their return is filed.”7
Assuming 35% tax liability, the accrual method would create a tax liability of $9,744 on a profit of $27,841. With the cash method, there would be no tax liability because there was no net profit.
Other expenses. The utilities, EHR licensing, tech support, and salaries are expensed the same way for both methods.
Net income. The resulting final net income is vastly different for the month of January depending on the accounting method utilized. The accrual method results in a net income of $18,097, while the cash-basis method results in a net loss of $29,767. Over the course of the year, these imbalances are likely to even out.
Related article:
Business law critical to your practice
Choosing an accounting method
Depending on the accounting method, a practice’s performance and profit will seem very different. The type of accounting method chosen will depend on what goals the owners want to achieve.
The accrual method provides a more accurate picture of business flow and performance and will be less subject to monthly variations due to large purchases or variations in expenses. If the practice chooses this method using an income statement, it should also employ a cash-flow statement.
The cash method of accounting will give a convenient and practical summary of the practice’s cash flow.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Physicians practice medicine and communicate within the world of medical language, yet there is a lack of awareness and understanding by many health care professionals of the universal language of business, which is accounting. Just as Latin provides the basic framework for medically related terminology, accounting is the standard language used to convey financial information to both internal and external stakeholders.
Accounting principles are important to physicians at any level. Whether you are starting out in private practice, running a clinical department, or working as an executive in a health care system, most decisions are based on the interpretation of financial data using accounting principles. Accounting standards in the United States are developed by the Financial Accounting Standard Board (FASB) and established as a set of principles and guidelines called Generally Accepted Accounting Principles (GAAP).1–3
Accrual- vs cash-based accounting
There are 2 approaches to recording financial transactions: accrual- and cash-based accounting methods. The main difference between them is in the timing of the recorded financial transactions (when revenue and expenses are recognized on the accounting books). Under GAAP, the matching principle, which is one of the most basic and utilized guidelines of accounting, specifies that accrual accounting be used. In the United States, most businesses (publically traded companies and moderate- to large-sized companies) use accrual accounting, while some individual and smaller businesses, including health care services such as physician practices, use the cash method.1–4
Accrual-based accounting
Accrual-based accounting specifies that revenues are recorded when they are earned, and expenses are recorded when they occur. A health care business may earn revenue for services on one day, but the cash may not be received or recorded on the accounting books for several weeks or months and at an amount less than billed.
Accrual-based accounting provides a more accurate representation of a business’ financial performance, since it uses the principle in which expenses are matched to revenues in the same time period. This enables a more precise representation of true financial performance during a given time frame.1–4
Cash-based accounting
Cash-based accounting is the easiest method to understand and implement because financial transactions are recorded in the accounting books when money is received or spent without the need for complex accounting techniques or integration of accounts receivable or payable.
Despite the ease of use and simplicity in tracking cash flow, this method can be deceiving because revenue may be received or expenses may need to be paid at times that are not consistent with when the revenue has been earned or expenses incurred. This can result in misleading information on the business’ health and the accuracy of tracking financial performance over time, since revenue and expenses for a particular transaction may occur at different times.1–4
Which accounting process to choose?
Even though accrual-based accounting may provide a more accurate financial representation of a business’ performance, many smaller businesses, including physician practices, prefer to use cash-based accounting. In addition, many health care businesses are eligible to use cash-based accounting per Internal Revenue Service (IRS) rules by qualifying for the Gross Receipts Test and being a qualified Personal Service Corporation (PSC):
- The Gross Receipts Test states that if the average annual gross receipts of the business are less than $5 million, the business can use the cash-based accounting method.
- If at least 95% of a business activity involves performing health care services, and at least 95% of the business is owned by employees performing health care services, then the business qualifies as a PSC that may use the cash-based accounting method.
Many physician practices qualify to use cash-based accounting, which reduces the complexity of following accrual-based accounting rules and simplifies overall cash-flow management.5
Read about insurance, capital equipment depreciation, more
CASE New practice opens
Practice A opens its practice on January 1. The practice borrows $20,000 from the bank to purchase hysteroscopic equipment for office-based tubal sterilizations and an additional $50,000 for an ultrasound machine. Both loans have a 5% annual interest rate amortized over 5 years. The practice leases office space and pays rent 2 months in advance at $8,000 ($4,000 per month). On January 1, the practice pays a $1,200 premium for annual property and liability insurance and $12,500 for the first quarter payment for professional liability insurance ($50,000 annually, paid quarterly). Other costs the practice pays in January include: utilities, $400; EHR licensing, $300; technical support, $200; and salaries, $10,000.
The practice purchases 4 sets of sterilization spring devices at $1,500 each ($6,000) to have in stock. One hysteroscopic sterilization procedure is performed on a patient in January using 1 device. The practice is reimbursed $2,500 for the procedure.
In January, the practice bills $150,000 in charges, but after insurance contractual adjustments, January’s revenue is $50,000. Actual cash payments from billings received are $10,000 in January, $30,000 in February, and $10,000 in March.
At first glance, there is a noticeable difference on the sales or recognition of revenues based on the type of accounting (TABLE). With the accrual method, because the billing charges are submitted in January when the services were provided (minus the insurance contractual adjustments), the $50,000 revenue is immediately counted and recognized, even though the practice only received $10,000 cash for those billings during January. While the benefit to accrual accounting is the timely recognition of the revenue when the service was provided, the downside is that much of those billings might actually be paid over 90 days, and some of those billings may go unpaid by the insurance company or the patients, which would require adjustments in later months.
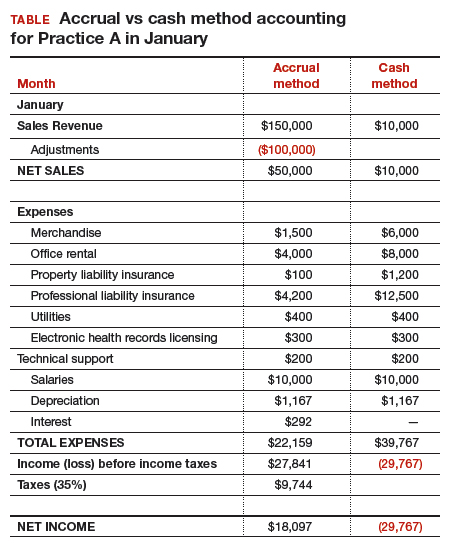
The cash-based method is simpler to understand because the cash received for the month is recognized as the revenue, regardless of the amount charged that month.
Merchandise. In the accrual method, the cost of merchandise sold (the hysteroscopic sterilization implants) is recognized as an expense when the revenue is generated from its sale. In this case, the date that the patient has the hysteroscopic in-office sterilization procedure is when the revenue and the expense of the implant are recognized.
In a cash-based accounting method, the $6,000 cost of the implants is recognized at the time of purchase in January.
Lease. In this scenario, even though 2 months of lease for the office were paid, the accrual method only recognizes the January payment; the second payment is recognized in February. In the cash method, because both months were paid in January, the total expense of $8,000 is recognized in January.
Property liability insurance. The property liability insurance payment is required at the start of the year. In accrual accounting, this expense is divided over 12 months, while in the cash method, the expense is counted at the time the payment is made.
Professional liability insurance. The professional liability insurance expense of $50,000 per year is made in quarterly payments, so for the accrual method, the annual amount would be distributed over 12 months at $4,200 per month. With the cash method, it would be paid—and recognized as an expense—quarterly at $12,500, starting in January.
Capital equipment depreciation. Capital medical equipment (hysteroscopy and ultrasound) can be depreciated using a straight-line 5-year depreciation. A total $70,000 worth of equipment divided by 5 years is $14,000 per year, depreciated over 5 years. One-twelfth of $14,000 equals $1,167, which is recorded as a January depreciation expense. Because the Internal Revenue Code requires capital assets to be depreciated, even for cash-basis taxpayers, the common practice is to record depreciation expense for both cash- and accrual-basis income accounting.6
Interest on loans. A loan’s principal payment will not be included on the income statement. The principal payment, a reduction of a liability (loans payable), is reported on the balance sheet. Only the interest portion of a loan payment is reported on the income statement (interest expense). In accrual accounting, the accrued interest on the loan payment for the year is $3,500 ($292 for January). For the cash-basis method, because the interest is paid annually at year-end, interest will not be expensed until December.
Taxes. The IRS states that, “Individuals, including sole proprietors, partners, and S corporation shareholders, generally have to make estimated tax payments if they expect to owe tax of $1,000 or more when their return is filed. Corporations generally have to make estimated tax payments if they expect to owe tax of $500 or more when their return is filed.”7
Assuming 35% tax liability, the accrual method would create a tax liability of $9,744 on a profit of $27,841. With the cash method, there would be no tax liability because there was no net profit.
Other expenses. The utilities, EHR licensing, tech support, and salaries are expensed the same way for both methods.
Net income. The resulting final net income is vastly different for the month of January depending on the accounting method utilized. The accrual method results in a net income of $18,097, while the cash-basis method results in a net loss of $29,767. Over the course of the year, these imbalances are likely to even out.
Related article:
Business law critical to your practice
Choosing an accounting method
Depending on the accounting method, a practice’s performance and profit will seem very different. The type of accounting method chosen will depend on what goals the owners want to achieve.
The accrual method provides a more accurate picture of business flow and performance and will be less subject to monthly variations due to large purchases or variations in expenses. If the practice chooses this method using an income statement, it should also employ a cash-flow statement.
The cash method of accounting will give a convenient and practical summary of the practice’s cash flow.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- About the FASB. Financial Accounting Standards Board website. http://www.fasb.org/jsp/FASB/PageSectionPage&cid=1176154526495. Accessed November 7, 2017.
- What is the difference between accrual accounting and cash accounting? Investopedia. https://www.investopedia.com/ask/answers/121514/what-difference-between-accrual-accounting-and-cash-accounting.asp. Accessed November 7, 2017.
- Accounting Basics (Explanation). Part 2: Income Statement. Accounting Coach. https://www.accountingcoach.com/accounting-basics/explanation/2. Accessed November 7, 2017.
- Stickney C, Weil R. Financial Accounting: An Introduction to Concepts, Methods, and Uses. 11th ed. Nashville, TN: Southwestern College Publishing Group; 2006:97-110.
- Internal Revenue Service. Publication 538 (12/2016), Accounting Periods and Methods. https://www.irs.gov/publications/p538#en_US_201612_publink1000270634. Revised December 2016. Accessed November 7, 2017.
- Klinefelter D, McCorkle D, Klose S. Financial Management: Cash vs. Accrual Accounting. Risk Management. AgriLife Extension. Texas A&M System. http://agrilife.org/agecoext/files/2013/10/rm5-16.pdf. Published 2013. Accessed November 7, 2017.
- Internal Revenue Service. Small Business and Self-Employed Tax Center: Estimated Taxes. https://www.irs.gov/businesses/small-businesses-self-employed/estimated-taxes. Updated November 2, 2017. Accessed November 7, 2017.
- About the FASB. Financial Accounting Standards Board website. http://www.fasb.org/jsp/FASB/PageSectionPage&cid=1176154526495. Accessed November 7, 2017.
- What is the difference between accrual accounting and cash accounting? Investopedia. https://www.investopedia.com/ask/answers/121514/what-difference-between-accrual-accounting-and-cash-accounting.asp. Accessed November 7, 2017.
- Accounting Basics (Explanation). Part 2: Income Statement. Accounting Coach. https://www.accountingcoach.com/accounting-basics/explanation/2. Accessed November 7, 2017.
- Stickney C, Weil R. Financial Accounting: An Introduction to Concepts, Methods, and Uses. 11th ed. Nashville, TN: Southwestern College Publishing Group; 2006:97-110.
- Internal Revenue Service. Publication 538 (12/2016), Accounting Periods and Methods. https://www.irs.gov/publications/p538#en_US_201612_publink1000270634. Revised December 2016. Accessed November 7, 2017.
- Klinefelter D, McCorkle D, Klose S. Financial Management: Cash vs. Accrual Accounting. Risk Management. AgriLife Extension. Texas A&M System. http://agrilife.org/agecoext/files/2013/10/rm5-16.pdf. Published 2013. Accessed November 7, 2017.
- Internal Revenue Service. Small Business and Self-Employed Tax Center: Estimated Taxes. https://www.irs.gov/businesses/small-businesses-self-employed/estimated-taxes. Updated November 2, 2017. Accessed November 7, 2017.
The clear and present future: Telehealth and telemedicine in obstetrics and gynecology
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
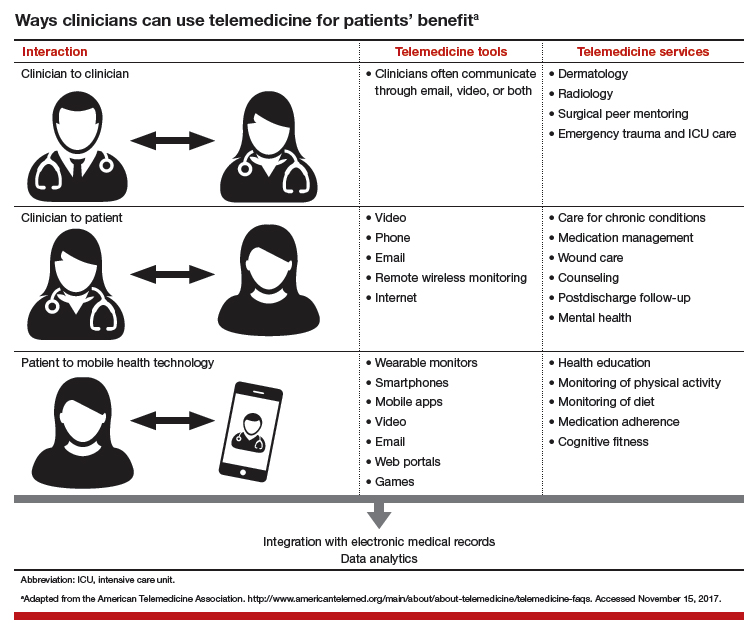
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
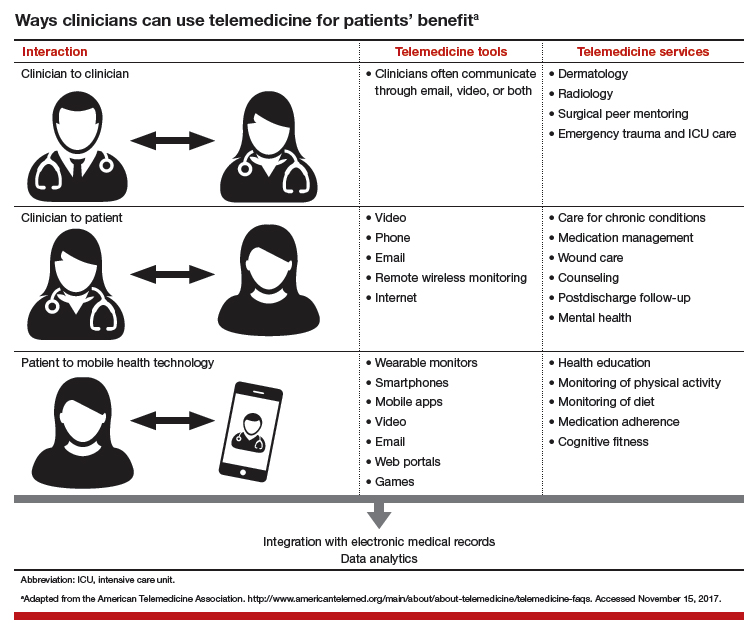
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
I recently spoke with 2 outstanding leaders in our field, members of the American College of Obstetricians and Gynecologists (ACOG) task force on telehealth and telemedicine, about the future of providing health care to women in remote locations.
Haywood Brown, MD, is President of ACOG for 2017–2018 and is F. Bayard Carter Professor of Obstetrics and Gynecology at Duke University Medical Center in Durham, North Carolina, and Peter Nielsen, MD, is Professor and Vice Chair of the Department of Obstetrics and Gynecology at Baylor College of Medicine in Houston, Texas, and Obstetrician-in-Chief at Children’s Hospital of San Antonio. Dr. Nielsen is a retired US Army colonel.
Why an ACOG telehealth task force?
Haywood Brown, MD: Our overall goals in telehealth and telemedicine are to coordinate and better facilitate the health care of women in remote locations and to improve maternal morbidity and mortality. Telehealth can be used on both an outpatient and an inpatient basis.
Outpatient telehealth is used for consultations. In maternal-fetal medicine, for instance, we use it for ultrasonography consultations. I also have used telehealth technology to “see” a pregnant patient with type 1diabetes. During our sessions, I managed her blood sugar levels and did all the other things I would have done if we had been together at my clinic. Without telehealth technology, however, this patient would have needed to drive 4 hours round-trip for each appointment.
Our colleagues in rural communities and at lower-level hospitals can use telehealth and telemedicine as aids in treating their high-risk patients, such as those with preeclampsia, prematurity risk, or other conditions. Physicians can consult with specialists through a face-to-face conversation that takes place through telecommunications. The result is that the quality of care for women in our communities is improved.
Genetic counseling, infertility consultation, and fetal anomaly management are some of the other applications. Our task force is discussing different ways to improve patient care and ways to collaborate with our colleagues around the country. Ultimately, we are developing best practices—a model for the best uses of technology to improve women’s health care in the United States.
Task force focus: Telehealth technology, billing, services
Dr. Brown: Our task force, a diverse group of members from all over the country, represents the spectrum of ObGyns. Although task force members have various levels of telehealth experience, all are very interested in these new channels of communication. The task force also includes billers, who understand billing ramifications, and payers, who know firsthand what will and will not be paid.
Technology and its availability is the most important topic for the task force. While some communities have Internet service, not all do. We need to determine which areas need service, how much it would cost, and who pays for it. Can a hospital afford it? A practice? Their partners? Identifying partners in tertiary care settings is a task force goal.
We are engaging a broad range of experts to study all the components and associated costs of technology, licensing, and cross-state credentialing. Gathering this information will help in developing a best practices model that general ObGyns can use.
Telehealth is redefining aspects of care: prenatal care (how many visits are required?), postpartum care, and other types of services that can be done remotely. Genetic counseling—who can provide it, what education is required—is another topic of discussion. Once we surmount the billing obstacles, we can do much with teleconferencing, such as provide genetic consultation with ObGyns in various settings.
The terms "telehealth" and "telemedicine" are often used interchangeably. Telemedicine is the older phrase, while telehealth entered the vernacular more recently and encompasses a broader definition.
The HealthIT.gov website explains the differences in terminology this way1:
- The Health Resources Services Administration defines telehealth as the use of electronic information and telecommunications technologies to support long-distance clinical health care, patient and professional health-related education, public health and health administration. Technologies include videoconferencing, the Internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.
- Telehealth is different from telemedicine because it refers to a broader scope of remote health care services than telemedicine. While telemedicine refers specifically to remote clinical services, telehealth can refer to remote nonclinical services, such as provider training, administrative meetings, and continuing medical education, in addition to clinical services.
A World Health Organization report, however, uses the 2 terms synonymously and interchangeably, defining telemedicine as2:
- The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.
The American Telemedicine Association (ATA) describes their use of the terms this way3:
- ATA largely views telemedicine and telehealth to be interchangeable terms, encompassing a wide definition of remote healthcare, although telehealth may not always involve clinical care.
References
- HealthIT.gov website. Frequently asked questions. https://www.healthit.gov/providers-professionals/frequently-asked-questions/485. Accessed November 15, 2017.
- World Health Organization. Telemedicine: opportunities and developments in member states. 2010. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Accessed November 15, 2017.
- American Telemedicine Association. About telemedicine: the ultimate frontier for superior healthcare delivery. http://www.americantelemed.org/about/about-telemedicine. Accessed November 15, 2017.
Learn about ways clinicians can use telemedicine.
Making progress in rural and underserved communities
Peter Nielsen, MD: When we saw that some high-risk obstetrics patients were having a difficult time getting to our downtown San Antonio office—the trip from surrounding communities was taking too long, or city driving and parking were stressful or too costly—we looked to improve access to care. Collaborating with a health care network that has a hospital in a town north of San Antonio, we set up a pilot program to provide telemedicine perinatal consultation services.
In this kind of service, which occurs entirely in real time, ultrasound images taken at the hospital are streamed by high-speed fiberoptic cable to our office, where a maternal-fetal medicine physician views them. If a repeat image or a different image is needed, the physician requests another scan. Linked to the physician and listening through an earpiece, the ultrasonographer performs the new scan with little delay and without disturbing the patient. The conversation between physician and ultrasonographer is private.
After ultrasound scanning is complete, the patient goes to a private room at the hospital for a video conference with our physician in San Antonio, who has reviewed the images in the PACS (picture archiving and communication system) or ultrasound recording system. They discuss the images, the findings, and the follow-up.
We tested the technology during a 6-month pilot program to make sure it worked at the highest quality and safety levels. Then the program went live and we started seeing patients remotely. Now we have a robust telemedicine training capability at that hospital outside San Antonio, and we are looking to expand to other south and west Texas areas, some even farther from our office.
I have done some of these remote consultations. In response to my informal queries about the experience, patients said that no one else was offering it, and they were participating for the first time. Naturally they had questions and concerns. Nevertheless, patients, family members, and the ultrasonographer and physicians in the communities seem to think this is a high-quality, safe program that makes it easier for patients to access health care.
Patients uniformly describe these consultations in positive terms. They do not have to drive far, into the city, and deal with traffic; parking is easy and free; and less travel means much less time off from work. Given these very practical advantages, patients are interested in having more appointments done remotely. In addition, they say the appointment itself is easy, being there is effortless, and they feel their physician is sitting in the same room. It is like video chatting with family members—they are comfortable with the technology.
Related article:
Landmark women’s health care remains law of the land
The patients’ perspective
Dr. Brown: Patient satisfaction is an important issue. In psychiatry, dermatology, and other disciplines, patients have indicated that they are very satisfied with telehealth sessions. Telehealth in obstetrics and gynecology, I think, will receive similar positive feedback.
The issue of driving distance led us to reconsider the number of face-to-face prenatal visits a normal, healthy patient needs. These days, a patient can use a prenatal care app to track her weight and blood pressure and send the data to her physician. Besides being convenient, these monitoring apps can give a patient an important sense of control. Our pilot programs found that a patient who self-monitors understands her weight gain better and is more in tune with it. Apps and other technologies can thus improve quality of care and, in reducing the number of trips to an office, increase patient satisfaction.
Many people use or are familiar with the programs Skype and FaceTime (audiovideo chat software), and I envision that our postpartum task force will recommend using such programs for follow-up appointments. For each visit, the question to ask is whether the patient really needs to meet with her physician in person, or can she stay with her new baby and receive postpartum counseling at home. I am excited about the potential of telehealth in obstetrics and gynecology. Our task force is exploring that potential.
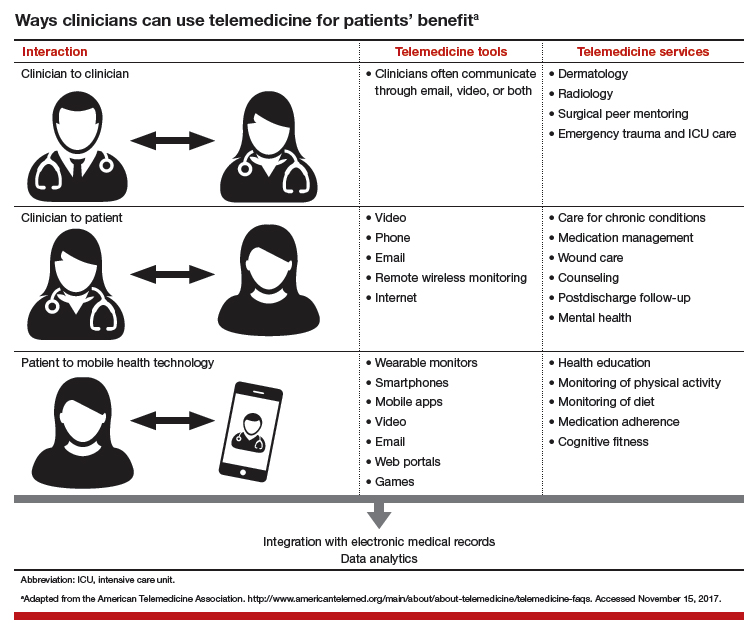
Telehealth for both routine and specialized care
Dr. Brown: Specialized care applications are here. In a pilot program in Wisconsin, a colleague has been providing remote psychiatric care. Perhaps such a program can be used to follow up on patients with postpartum depression. In addition, other psychiatry colleagues have long been using telehealth for adolescent behavior follow-ups, and we can do this too.
Another colleague has been performing remote perinatal follow-up for children with congenital anomalies. The physician interacts with the parent or parents as well as the patient. This seems to represent only the tip of the iceberg of what can be done in terms of follow-up.
We can also use telehealth in infertility settings. High-risk patients can benefit, too. Our guidelines say patients with preeclampsia should be seen within 3 days to 1 week. Many are transferred from low-access hospitals to our office. This follow-up, however, also can be done remotely, with patients at health department clinics or even at home. Reporting blood pressure readings and health-related feelings to a physician during a teleconsultation removes driving as a potential inconvenience or obstacle.
Telemedicine can be advantageous in gynecology. Physicians are doing important work with telecolposcopy as a follow-up to abnormal Pap test findings in patients in sub-Saharan Africa.
Routine wound care, which is commonly needed, can be performed in the home by a home health nurse telecommunicating with a physician. I can see broad telehealth use, and indeed our dermatology colleagues have been practicing telemedicine for quite some time.
Read about solving financial barriers and physician shortages.
An affordable solution to financial barriers and physician shortages
Dr. Nielsen: Telehealth can reduce barriers to care. For example, knowing that our teleconsultation services are covered by insurance, referring physicians and patients are more likely to try them and continue to use them. Payers are on board as well. Other barriers can be harder to overcome, particularly for patients at risk for complex diagnoses and medical decisions. Our pilot program, however, has demonstrated success in this area. It has provided safe, high-quality imaging, accurate diagnoses, productive discussions, and helpful management recommendations.
Telehealth also helps address relative and absolute physician shortages. In some areas, a relative shortage may indicate misdistribution. In other areas, specialists simply are too few in number. This absolute shortage of specialists likely will increase, as many communities are too small to sustain and support having them in person.
Outpatients can obtain care 5 days a week with telemedicine, as opposed to only 1 to 3 times a month in person. Physicians travel to remote clinics that are staffed only 1 or 2 days a month. Where the window for care is so small, patients and physicians are likely to turn to telemedicine. In addition, that utility results in better use of resources. For example, studies that were performed earlier would not need to be repeated, since you could access centrally located archives.
Related article:
ICD-10-CM code changes: What's new for 2018
Dr. Brown: For teleconsultations and televisits, all that payers need do is modify the billing codes they use for our usual services. Once that is done, payers can develop a payment model that works for both themselves and the teleconsultants.
The US health care system is fragmented. Health care is provided in various facilities, including federally qualified health centers and health department clinics. As Dr. Nielsen said, physicians travel to remote facilities once or twice a week or even a month, whereas telehealth can be offered 5 days a week. Many residents go to remote clinics, where an attending physician is required. Instead of an attending driving there, he or she could be teleconsulting—interacting with residents and patients from afar. So, telehealth is a win-win situation. It increases access to physicians and facilitates appropriate interactions with them, wherever they are. Telehealth can be an important contribution to developing a more effective health care delivery system than the fragmented one we have now.
Effective health care delivery is so important for obstetrics and gynecology, and the reported workforce challenges are real. A maternal-fetal medicine physician is unlikely to travel to remote communities once a week or even every 2 weeks, but that same physician can teleconsult multiple days each week.
How telehealth can close service gaps
Dr. Brown: Having established relationships with physicians in other clinics and communities paves the way for teleconsultation and remote supervision. Technology can help Planned Parenthood and other clinics continue to provide contraceptive counseling and other health care services. Even medical abortions can be supervised through teleconsultation.
With funds to Medicaid being cut, with the potential for Planned Parenthood to be defunded, physicians must think of ways they can continue to provide care to all patients and communities. By addressing these issues now, we will be ready to take charge of patient care, wherever it is needed.
But, we need partners, no question. We need hospital partners in all communities, and especially in rural communities. Rural hospitals and maternity care are at risk. Health care in rural communities faces many challenges. Telehealth, teleconferencing, and teleconsultation not only can improve access to services, but also can curb travel costs as well as costs to the communities and hospitals.
Who pays the operating costs, and who benefits
Dr. Brown: Payers are already discovering that teleconsultations are as billable as in-person visits. In addition, physicians are realizing that remote consultation can work as well as in-person consultation, with its own merits and advantages. Education is key—education about billing and about what is doable in telehealth. We can learn from colleagues in other specialties.
Dr. Nielsen: Several entities and groups must start covering the technology costs. Federal and state entities need to determine how the country’s information infrastructure can be improved to give rural areas access to high-quality, high-speed, wide-bandwidth communications, which will help expand telehealth and increase other industries’ opportunities to grow and sustain these communities. Improving the infrastructure also can help keep rural areas sustainable.
Health care systems themselves can join federal, state, and local governments in building this infrastructure. They can also start identifying opportunities to support and sustain physicians and hospitals in smaller towns and start combating the perception that the infrastructure is being developed only to migrate patients over to accessing their care through telehealth provided by physicians in the larger cities.
Many payers see telehealth as improving access and outcomes and already support it, but more payers need to become involved. All need to understand how routine and complex consultations, even inpatient consultations, can be performed remotely and can be properly reimbursed, and incentivized with payments for improved outcomes and value.
As barriers fall and telehealth improves, acceptance by patients and physicians will increase. In addition, telehealth will enter medical education in a significant way. The instruction that students, residents, and Fellows receive will be enhanced by new telehealth approaches in various specialties, and residents will come out of these programs with telehealth experience and a sense of both financial benefits and payment structures. This early exposure will pique their interest in using telehealth and advocating its use where it may never before have been considered, owing to real and perceived barriers.
Read about telehealth solutions for ObGyns.
Learning from other specialties and agencies
Dr. Brown: The physician shortage negatively affects access to health care in rural areas. Many city and suburban physicians, including ObGyns, want to stay where they are. Education is needed to show them that a rural practice can be successful. They would have a good patient base and be able to use telehealth to improve care and maintain contact with tertiary care centers.
Several task force members have described their experience within their health systems, and we hope to borrow from that. A health system in South Dakota received a Health Resources and Services Administration grant to use telehealth and teleconsultation in the Indian Health Service (IHS). To women who access their health care through the IHS, being able to remain in the community is culturally important. Telehealth and teleconsultation bring care to these women where they live.
To develop the best telehealth and teleconsultation model, we are borrowing from these health systems and from the experience of our colleagues in dermatology, behavioral health, psychiatry, and other disciplines. These physicians already have overcome many hurdles and discovered the importance of patient satisfaction in providing remote health care.
Patients will benefit in various ways, and here is another example: A clinic refers a patient to an ObGyn to discuss whether it is possible to have a vaginal birth after a cesarean delivery. The drive to the ObGyn’s office takes an hour, but the patient just as easily could have had all her questions answered during a teleconsultation.
Related articles:
Telehealth and you (4-part audiocast)
Telehealth recommendations for ObGyns
Dr. Brown: Our task force will develop recommended best practices for telehealth. We will outline how a practice can engage with telehealth and will address licensing requirements, as a practice must be licensed in each state where it uses telehealth. Our goal is to help our specialty get started in telehealth and telemedicine.
In practices with telehealth, it will be incumbent on ObGyns to identify any barriers to care. For example, we are concerned about early discontinuation of breastfeeding, particularly among African American communities. Fortunately, we have learned that video chat follow-ups can help improve breastfeeding continuation rates.
It also will be incumbent on ObGyns to think differently about how best to follow up. For a patient who calls to say she thinks she has mastitis, much of the consultation can be handled by telephone or video conference with the physician and a nurse practi‑tioner, and then medication can be prescribed without the need for in-person follow-up. We must then determine how to ensure these follow-up methods are compensated.
Direct-to-patient virtual visits
- Virtual home visits
- Low-risk pregnancy
- Postpartum visits
- Lactation support
- Routine gynecologic care
- Postoperative follow-up
Remote patient monitoring
- Chronic disease management
- Antenatal testing
- Fetal heart rate monitoring
- Transfer of care
Final thoughts
Dr. Nielsen: It is time for all US health care players to more seriously and aggressively consider how telehealth can improve health care access, quality, and safety. Even more important, patients and physicians in small communities need to feel that they can access specialists and care that is as good as those available in larger communities without having to pull up stakes and move.
Telehealth can help small communities become sustainable over the long term. As the majority of the people in this country are born in and receive health care in community hospitals, not large tertiary care centers, the state of US health care should be measured by the ability to provide as much care as is technically possible in the small communities where patients live and work and raise their kids.
Dr. Brown: More than 50% of all babies are born in hospitals where fewer than 1,000 deliveries are performed, and almost 40% are born in hospitals where fewer than 500 are performed. To provide high-level care and have patients feel comfortable, to improve morbidity and mortality, we need telehealth and telemedicine.
If I can help a physician in East Africa place a Bakri balloon for postpartum hemorrhaging, surely I can help a physician in rural areas of Wyoming, South Dakota, or North Carolina deal with this obstetric emergency. In obstetrics and gynecology, telehealth and telemedicine have great potential in terms of morbidity and mortality, but we are also doing genetic counseling and a great deal of patient follow-up, and so much more can be done.
That is the key, and the reason for the training, the task force, the deliberations, and the best practices model that we will be sharing with our colleagues.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Your online reputation
Have you ever run across an unfair or even malicious comment about you or your practice on one of those “doctor-rating” web sites? Some curmudgeon, angry about something totally irrelevant to your clinical skills, decided to publicly trash you; and the site, of course, made no effort to authenticate the writer or fact-check the complaint.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that, once it’s online, it’s online forever; consider the ramifications of anything you post on any site – yours or others – before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Patients appreciate factual information, but they value your opinions too. Add a blog to your web site and write about subjects – medical and otherwise – that interest you. If you have expertise in a particular field, be sure to write about that.
Incidentally, if the URL for your web site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
A web site is a powerful resource, but not the only one. Take advantage of Google’s free profiling tool at https://profiles.google.com/me, where you can create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. Your Google profile will, of course, be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done and updated regularly. Remember that Wikipedia’s conflict of interest rules forbid adding or editing content about yourself, so someone with a theoretically “neutral point of view” will have to do it for you.
Other useful resources are the social networking sites. Whatever your opinion of online networks, the reality is that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Make your (noncontroversial) opinions known on these portals. Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – also need to be mentioned prominently.
Set up an RSS news feed for yourself (directions to follow in the next two columns), so you’ll know immediately if your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect and can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely or corrected within the original article. An erratum on the last page of the next edition will be ignored and will leave the false information online, intact.
Doctor-rating sites typically refuse to remove unfair comments unless they are blatantly libelous or a case of mistaken identity; but there is nothing wrong with encouraging happy patients to post favorable reviews on those sites. Sauce for the goose, and all that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Have you ever run across an unfair or even malicious comment about you or your practice on one of those “doctor-rating” web sites? Some curmudgeon, angry about something totally irrelevant to your clinical skills, decided to publicly trash you; and the site, of course, made no effort to authenticate the writer or fact-check the complaint.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that, once it’s online, it’s online forever; consider the ramifications of anything you post on any site – yours or others – before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Patients appreciate factual information, but they value your opinions too. Add a blog to your web site and write about subjects – medical and otherwise – that interest you. If you have expertise in a particular field, be sure to write about that.
Incidentally, if the URL for your web site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
A web site is a powerful resource, but not the only one. Take advantage of Google’s free profiling tool at https://profiles.google.com/me, where you can create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. Your Google profile will, of course, be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done and updated regularly. Remember that Wikipedia’s conflict of interest rules forbid adding or editing content about yourself, so someone with a theoretically “neutral point of view” will have to do it for you.
Other useful resources are the social networking sites. Whatever your opinion of online networks, the reality is that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Make your (noncontroversial) opinions known on these portals. Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – also need to be mentioned prominently.
Set up an RSS news feed for yourself (directions to follow in the next two columns), so you’ll know immediately if your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect and can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely or corrected within the original article. An erratum on the last page of the next edition will be ignored and will leave the false information online, intact.
Doctor-rating sites typically refuse to remove unfair comments unless they are blatantly libelous or a case of mistaken identity; but there is nothing wrong with encouraging happy patients to post favorable reviews on those sites. Sauce for the goose, and all that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Have you ever run across an unfair or even malicious comment about you or your practice on one of those “doctor-rating” web sites? Some curmudgeon, angry about something totally irrelevant to your clinical skills, decided to publicly trash you; and the site, of course, made no effort to authenticate the writer or fact-check the complaint.
What to do? You could hire one of the many companies in the rapidly burgeoning field of online reputation management; but that can cost hundreds to thousands of dollars per month for monitoring and intervention, and there are no guarantees of success.
Leave design and SEO to the pros, but don’t delegate the content itself; as captain of the ship you are responsible for all the facts and opinions on your site. And remember that, once it’s online, it’s online forever; consider the ramifications of anything you post on any site – yours or others – before hitting the “send” button. “The most damaging item about you,” one consultant told me, “could well be something you posted yourself.” Just ask any of several prominent politicians who have famously sabotaged their own careers online.
That said, don’t be shy about creating content. Patients appreciate factual information, but they value your opinions too. Add a blog to your web site and write about subjects – medical and otherwise – that interest you. If you have expertise in a particular field, be sure to write about that.
Incidentally, if the URL for your web site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
A web site is a powerful resource, but not the only one. Take advantage of Google’s free profiling tool at https://profiles.google.com/me, where you can create a sterling bio, complete with links to URLs, photos, and anything else that shows you in the best possible light. Your Google profile will, of course, be at or near the top of any Google search.
Wikipedia articles also go to the top of most searches, so if you’re notable enough to merit mention in one – or to have one of your own – see that it is done and updated regularly. Remember that Wikipedia’s conflict of interest rules forbid adding or editing content about yourself, so someone with a theoretically “neutral point of view” will have to do it for you.
Other useful resources are the social networking sites. Whatever your opinion of online networks, the reality is that personal pages on Facebook, LinkedIn, and Twitter rank very high on major search engines. (Some consultants say a favorable LinkedIn profile is particularly helpful because of that site’s reputation as a “professional” network.) Make your (noncontroversial) opinions known on these portals. Your community activities, charitable work, interesting hobbies – anything that casts you in a favorable light – also need to be mentioned prominently.
Set up an RSS news feed for yourself (directions to follow in the next two columns), so you’ll know immediately if your name pops up in news or gossip sites, or on blogs. If something untrue is posted about you, take action. Reputable news sites and blogs have their own reputations to protect and can usually be persuaded to correct anything that is demonstrably false. Try to get the error removed entirely or corrected within the original article. An erratum on the last page of the next edition will be ignored and will leave the false information online, intact.
Doctor-rating sites typically refuse to remove unfair comments unless they are blatantly libelous or a case of mistaken identity; but there is nothing wrong with encouraging happy patients to post favorable reviews on those sites. Sauce for the goose, and all that.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
High Deductible Health Plans: Take Accounts Receivable Action Now
If you missed the recent headlines, Why Patients Delay Medical Payments: 12 findings 1 and You think your health insurance costs too much. Try being a farmer.2, you may not be too worried about your ever-rising accounts receivables. But you should be.
The facts in these stories and the 2017 Employer Health Benefits Survey,3 released on September 19 by the non-partisan Kaiser Family Foundation and Health Research & Educational Trust (HRET), are alarming. Let’s look at some of the survey results.
Since 2007, the average family premium has increased 55% and the average worker contribution toward the premium has increased 74%.3 How does that translate into dollars and cents? Well, the average annual premiums this year are $6690 for single coverage and $18,764 for family coverage.
What does that mean exactly to the farm couple in the Crain’s story? The farmer who “will be lucky to net $75,000” on his hay crop this year has a policy premium with Blue Cross Blue Shield of Illinois that was $22,000 last year. And then there is a $5000 deductible for each him and his wife. Do the math: it means they’d spend 43% of their income before health insurance covers anything.
Do premiums vary significantly by firm size or region? Should surgeons in certain areas of the country be less concerned about these trends? No, the premiums don’t significantly vary by size or region.
The point here is not to write an essay about health insurance premiums, but rather to discuss what this economic reality means to patients who are seeing you tomorrow, next week, and next month. Given these economic realities, what is their attitude about your bill?
For insight, let’s look at an Advisory Board Company brief, “Minimizing Bad Debt: Point-of-Service Collections,”4 which states: “Patient propensity to pay decreases as patient obligation increases.” According to the brief, “Our analysis indicates that as the dollar value of a patient’s obligation increases, their propensity to pay any portion of the obligation decreases—for all patients, at all income levels.” See Figure 1.
Given that market statistics show that more than a quarter of the commercially insured patients are covered by high deductible health plans (HDHPs), your practice must adapt to these changing times.
Review Your Pay or Mix
Smart practice administrators will keep their finger on the pulse of the insurance local market as more employers move toward offering HDHPs or health savings accounts. Knowing what the largest manufacturers are offering, along with local hospitals that are typically sizable employers in most communities, is critical. The coverage for school systems, police departments, fire departments, and governments should also be the practice radar.
A recent West Corporation survey5 reveals more about the demographic profile of patients who are less likely to pay or delay payments. Their study shows that 79% of patients cite affordability as the largest healthcare problem with 93% of patients saying it costs too much. So it should be no surprise that 67% say their financial situation makes it challenging to submit timely payments. If you are not familiar with the company name, you’ll be familiar with West Corporation’s products, like Televox, which are automated tools used by practices to remind patients about appointments and copays.
Here are other relevant findings from the West Corporation survey:
- 56% delay payments of medical bills at least some of the time.
- 70% of millennials have missed medical payment deadlines.
- 42% of patients cite their HDHP as the reason for delaying their payments.
- 36% of patients said they have difficulty remembering to make timely medical payments.
It’s no surprise that orthopedic surgeons are not discussing fees with patients. Although only 9% admitted that they don’t discuss costs with patients, it is safe to estimate that few surgeons have their fee schedules memorized.
In a 2013 article, Ubel and colleagues7 said, “Because treatments can be ‘financially toxic,’ physicians need to disclose the financial consequences of treatment alternatives just as they inform patients about treatments’ side effects.”
While uniquely qualified to discuss treatment options, few orthopedic surgeons have the time or the facts to personally discuss fees, out-of-pocket expenses, uncovered services and payment plans. Detailed discussions about patients’ financial liabilities are better done by qualified staff, who verify benefits and use modern technology tools to generate an electronic “estimate of costs and benefits.”
Target Your Efforts
What steps can your practice take to help patients pay their portion, even when it’s large, as well as help your practice reduce receivables and avoid collection problems and bad debt write-offs?
Start by analyzing the top Current Procedural Terminology (CPT) codes with patient responsibility, so you can focus your efforts. One such analysis, conducted by our firm, is shown in Figure 3. Although you might think the highest percent of patient financial responsibilities are for surgical procedures, notice that 4 of the top 5 services this practice identified as having the highest amount of patient collectible dollars are rendered in the office-carpal tunnel surgery being the only exception.
Take Action
After conducting a thorough analysis and reviewing the results, here are 5 actionable steps your practice could take:
1. Make sure your patient portal has the capacity to take patient payments. Offering online payment options increases the opportunity for patients to pay. Promote this option on the patient statement.
2. Implement a system of collecting from patients before they leave the office. After a new visit, which involves a more expensive evaluation and management code, and possibly imaging and durable medical device, counsel patients to leave a credit card on file, so the minute insurance pays, their credit card can be charged.
The 2017 Navicure Patient Payment Check-Up survey8 conducted by Healthcare Information and Management Systems Society (HIMSS) Analytics shows that 78% of patients would provide a card to be charged for one time up to $200. Think about the previously illustrated collection amounts this would alleviate.
3. Provide all surgery patients with a cost estimate. Generating cost estimates has been possible for close to 10 years. It’s done through your clearinghouse and practice management software by entering the CPT codes and diagnosis codes, along with the patient’s information. Save time and avoid tying staff up on hold.
According to the Navicure Patient Payment Check-Up survey,8 75% of provider organizations are able to provide a cost estimate upon request. It makes good business sense.
4. Collect a pre-treatment or pre-surgery scheduling deposit. In the KarenZupko & Associates/American Academy of Orthopaedic Surgeons (AAOS) pre-course survey of those attending the 2017 coding and reimbursement workshops, 55% of orthopedic practices reported that they have instituted such a practice. With the proliferation of HDHPs, asking for a scheduling deposit is fast becoming a must for all surgeons.
5. Offer patients a healthcare financing option through a third party. In response to another pre-course survey question, about offering CareCredit or another healthcare credit card, 28% of orthopedic practices say they do. Still, that leaves >70% of the orthopedic patients without a financing option. Given the reality of high deductible HDHPs and the patient responsibilities going uncollected, it’s time surgeons take a look at financing. It’s a fool’s wish to believe the practice is “saving” the service fee by sending dozens of statements, having staff make calls, and ultimately writing off unpaid balances as uncollectible.
Practices that fail to change, will fail to prosper. Those who have technology-phobic staff will suffer as healthcare continues to automate. Practices led by surgeons like one recently interviewed who said, “If patients knew how much it cost, they’d never schedule” will see patient accounts receivable soar and patient online ratings sink. The first quarter of 2018 means the number of patients with HDHPs will increase and that deductibles will have to be met. It’s wise to have a full staff meeting, share the facts, and put an action plan in place.
1. Gooch K. Why patients delay medical payments: 12 findings. Becker’s ASC. https://www.beckershospitalreview.com/finance/why-patients-delay-medical-payments-12-findings.html. Published August 28, 2017.
2. Murphy HL. You think your health insurance costs too much. Try being a farmer. Crain’s Chicago Business. http://www.chicagobusiness.com/article/20170929/ISSUE01/170929835. Published September 29, 2017. Accessed October 2, 2017.
3. 2017 Employer Health Benefits Survey. The Henry J. Kaiser Family Foundation and the Health Research & Educational Trust (HRET). https://www.kff.org/health-costs/report/2017-employer-health-benefits-survey/. Published September 19, 2017.
4. Minimizing Bad Debt: Point-of-Service Collections. The Advisory Board Company. https://www.advisory.com/-/media/Advisory-com/Research/FLC/Resources/2015/CFO-Brief-POS.pdf. Published August 21, 2015.
5. Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology-Enabled Communications. West Corporation. https://cdn2.hubspot.net/hubfs/402746/Assets/West%20Assets/Optimizing%20Revenue%20Report/Reports%20and%20Handouts/WEST-Optimizing%20Revenue%20Report%20final.pdf?t=1508789915319. Accessed October 26, 2017.
6. Peckham C. Medscape Orthopedist Compensation Report 2016. Medscape. https://www.medscape.com/features/slideshow/compensation/2016/orthopedics. Published April 1, 2016.
7. Ubel PA, Abernathy AP, Zafar SY. Full disclosure - out-of-pocket costs as side effects. N Engl J. Med. 2013;369:1484-1486. doi:10.1056/NEJMp1306826.
8. Patient Payment Check-Up 2017. Navicure. http://info.navicure.com/rs/669-OIJ-380/images/Navicure-Survey-Report-2017-Patient-Payment-Check-Up.pdf?mkt_tok=eyJpIjoiTVdKak1HUmhObVV6WkRVeSIsInQiOiJRcFNyRGVrOXlTS0pjalwvWEw3c2s1UmRMRHJVXC9EQzRkSnBkWCs0S2FEbUt3Z1I1a2Y3d1BBY3FKY0I1QWpEdkJRWU9ibmFlUlpnYVRIbVJMcStTVmdkRVwvSTJzcHE1cDVTajBRM3B1Q25lbDQwamViWnMwWGd1c1QzVk1cL2hYdkYifQ%3D%3D. Accessed October 26, 2017.
If you missed the recent headlines, Why Patients Delay Medical Payments: 12 findings 1 and You think your health insurance costs too much. Try being a farmer.2, you may not be too worried about your ever-rising accounts receivables. But you should be.
The facts in these stories and the 2017 Employer Health Benefits Survey,3 released on September 19 by the non-partisan Kaiser Family Foundation and Health Research & Educational Trust (HRET), are alarming. Let’s look at some of the survey results.
Since 2007, the average family premium has increased 55% and the average worker contribution toward the premium has increased 74%.3 How does that translate into dollars and cents? Well, the average annual premiums this year are $6690 for single coverage and $18,764 for family coverage.
What does that mean exactly to the farm couple in the Crain’s story? The farmer who “will be lucky to net $75,000” on his hay crop this year has a policy premium with Blue Cross Blue Shield of Illinois that was $22,000 last year. And then there is a $5000 deductible for each him and his wife. Do the math: it means they’d spend 43% of their income before health insurance covers anything.
Do premiums vary significantly by firm size or region? Should surgeons in certain areas of the country be less concerned about these trends? No, the premiums don’t significantly vary by size or region.
The point here is not to write an essay about health insurance premiums, but rather to discuss what this economic reality means to patients who are seeing you tomorrow, next week, and next month. Given these economic realities, what is their attitude about your bill?
For insight, let’s look at an Advisory Board Company brief, “Minimizing Bad Debt: Point-of-Service Collections,”4 which states: “Patient propensity to pay decreases as patient obligation increases.” According to the brief, “Our analysis indicates that as the dollar value of a patient’s obligation increases, their propensity to pay any portion of the obligation decreases—for all patients, at all income levels.” See Figure 1.
Given that market statistics show that more than a quarter of the commercially insured patients are covered by high deductible health plans (HDHPs), your practice must adapt to these changing times.
Review Your Pay or Mix
Smart practice administrators will keep their finger on the pulse of the insurance local market as more employers move toward offering HDHPs or health savings accounts. Knowing what the largest manufacturers are offering, along with local hospitals that are typically sizable employers in most communities, is critical. The coverage for school systems, police departments, fire departments, and governments should also be the practice radar.
A recent West Corporation survey5 reveals more about the demographic profile of patients who are less likely to pay or delay payments. Their study shows that 79% of patients cite affordability as the largest healthcare problem with 93% of patients saying it costs too much. So it should be no surprise that 67% say their financial situation makes it challenging to submit timely payments. If you are not familiar with the company name, you’ll be familiar with West Corporation’s products, like Televox, which are automated tools used by practices to remind patients about appointments and copays.
Here are other relevant findings from the West Corporation survey:
- 56% delay payments of medical bills at least some of the time.
- 70% of millennials have missed medical payment deadlines.
- 42% of patients cite their HDHP as the reason for delaying their payments.
- 36% of patients said they have difficulty remembering to make timely medical payments.
It’s no surprise that orthopedic surgeons are not discussing fees with patients. Although only 9% admitted that they don’t discuss costs with patients, it is safe to estimate that few surgeons have their fee schedules memorized.
In a 2013 article, Ubel and colleagues7 said, “Because treatments can be ‘financially toxic,’ physicians need to disclose the financial consequences of treatment alternatives just as they inform patients about treatments’ side effects.”
While uniquely qualified to discuss treatment options, few orthopedic surgeons have the time or the facts to personally discuss fees, out-of-pocket expenses, uncovered services and payment plans. Detailed discussions about patients’ financial liabilities are better done by qualified staff, who verify benefits and use modern technology tools to generate an electronic “estimate of costs and benefits.”
Target Your Efforts
What steps can your practice take to help patients pay their portion, even when it’s large, as well as help your practice reduce receivables and avoid collection problems and bad debt write-offs?
Start by analyzing the top Current Procedural Terminology (CPT) codes with patient responsibility, so you can focus your efforts. One such analysis, conducted by our firm, is shown in Figure 3. Although you might think the highest percent of patient financial responsibilities are for surgical procedures, notice that 4 of the top 5 services this practice identified as having the highest amount of patient collectible dollars are rendered in the office-carpal tunnel surgery being the only exception.
Take Action
After conducting a thorough analysis and reviewing the results, here are 5 actionable steps your practice could take:
1. Make sure your patient portal has the capacity to take patient payments. Offering online payment options increases the opportunity for patients to pay. Promote this option on the patient statement.
2. Implement a system of collecting from patients before they leave the office. After a new visit, which involves a more expensive evaluation and management code, and possibly imaging and durable medical device, counsel patients to leave a credit card on file, so the minute insurance pays, their credit card can be charged.
The 2017 Navicure Patient Payment Check-Up survey8 conducted by Healthcare Information and Management Systems Society (HIMSS) Analytics shows that 78% of patients would provide a card to be charged for one time up to $200. Think about the previously illustrated collection amounts this would alleviate.
3. Provide all surgery patients with a cost estimate. Generating cost estimates has been possible for close to 10 years. It’s done through your clearinghouse and practice management software by entering the CPT codes and diagnosis codes, along with the patient’s information. Save time and avoid tying staff up on hold.
According to the Navicure Patient Payment Check-Up survey,8 75% of provider organizations are able to provide a cost estimate upon request. It makes good business sense.
4. Collect a pre-treatment or pre-surgery scheduling deposit. In the KarenZupko & Associates/American Academy of Orthopaedic Surgeons (AAOS) pre-course survey of those attending the 2017 coding and reimbursement workshops, 55% of orthopedic practices reported that they have instituted such a practice. With the proliferation of HDHPs, asking for a scheduling deposit is fast becoming a must for all surgeons.
5. Offer patients a healthcare financing option through a third party. In response to another pre-course survey question, about offering CareCredit or another healthcare credit card, 28% of orthopedic practices say they do. Still, that leaves >70% of the orthopedic patients without a financing option. Given the reality of high deductible HDHPs and the patient responsibilities going uncollected, it’s time surgeons take a look at financing. It’s a fool’s wish to believe the practice is “saving” the service fee by sending dozens of statements, having staff make calls, and ultimately writing off unpaid balances as uncollectible.
Practices that fail to change, will fail to prosper. Those who have technology-phobic staff will suffer as healthcare continues to automate. Practices led by surgeons like one recently interviewed who said, “If patients knew how much it cost, they’d never schedule” will see patient accounts receivable soar and patient online ratings sink. The first quarter of 2018 means the number of patients with HDHPs will increase and that deductibles will have to be met. It’s wise to have a full staff meeting, share the facts, and put an action plan in place.
If you missed the recent headlines, Why Patients Delay Medical Payments: 12 findings 1 and You think your health insurance costs too much. Try being a farmer.2, you may not be too worried about your ever-rising accounts receivables. But you should be.
The facts in these stories and the 2017 Employer Health Benefits Survey,3 released on September 19 by the non-partisan Kaiser Family Foundation and Health Research & Educational Trust (HRET), are alarming. Let’s look at some of the survey results.
Since 2007, the average family premium has increased 55% and the average worker contribution toward the premium has increased 74%.3 How does that translate into dollars and cents? Well, the average annual premiums this year are $6690 for single coverage and $18,764 for family coverage.
What does that mean exactly to the farm couple in the Crain’s story? The farmer who “will be lucky to net $75,000” on his hay crop this year has a policy premium with Blue Cross Blue Shield of Illinois that was $22,000 last year. And then there is a $5000 deductible for each him and his wife. Do the math: it means they’d spend 43% of their income before health insurance covers anything.
Do premiums vary significantly by firm size or region? Should surgeons in certain areas of the country be less concerned about these trends? No, the premiums don’t significantly vary by size or region.
The point here is not to write an essay about health insurance premiums, but rather to discuss what this economic reality means to patients who are seeing you tomorrow, next week, and next month. Given these economic realities, what is their attitude about your bill?
For insight, let’s look at an Advisory Board Company brief, “Minimizing Bad Debt: Point-of-Service Collections,”4 which states: “Patient propensity to pay decreases as patient obligation increases.” According to the brief, “Our analysis indicates that as the dollar value of a patient’s obligation increases, their propensity to pay any portion of the obligation decreases—for all patients, at all income levels.” See Figure 1.
Given that market statistics show that more than a quarter of the commercially insured patients are covered by high deductible health plans (HDHPs), your practice must adapt to these changing times.
Review Your Pay or Mix
Smart practice administrators will keep their finger on the pulse of the insurance local market as more employers move toward offering HDHPs or health savings accounts. Knowing what the largest manufacturers are offering, along with local hospitals that are typically sizable employers in most communities, is critical. The coverage for school systems, police departments, fire departments, and governments should also be the practice radar.
A recent West Corporation survey5 reveals more about the demographic profile of patients who are less likely to pay or delay payments. Their study shows that 79% of patients cite affordability as the largest healthcare problem with 93% of patients saying it costs too much. So it should be no surprise that 67% say their financial situation makes it challenging to submit timely payments. If you are not familiar with the company name, you’ll be familiar with West Corporation’s products, like Televox, which are automated tools used by practices to remind patients about appointments and copays.
Here are other relevant findings from the West Corporation survey:
- 56% delay payments of medical bills at least some of the time.
- 70% of millennials have missed medical payment deadlines.
- 42% of patients cite their HDHP as the reason for delaying their payments.
- 36% of patients said they have difficulty remembering to make timely medical payments.
It’s no surprise that orthopedic surgeons are not discussing fees with patients. Although only 9% admitted that they don’t discuss costs with patients, it is safe to estimate that few surgeons have their fee schedules memorized.
In a 2013 article, Ubel and colleagues7 said, “Because treatments can be ‘financially toxic,’ physicians need to disclose the financial consequences of treatment alternatives just as they inform patients about treatments’ side effects.”
While uniquely qualified to discuss treatment options, few orthopedic surgeons have the time or the facts to personally discuss fees, out-of-pocket expenses, uncovered services and payment plans. Detailed discussions about patients’ financial liabilities are better done by qualified staff, who verify benefits and use modern technology tools to generate an electronic “estimate of costs and benefits.”
Target Your Efforts
What steps can your practice take to help patients pay their portion, even when it’s large, as well as help your practice reduce receivables and avoid collection problems and bad debt write-offs?
Start by analyzing the top Current Procedural Terminology (CPT) codes with patient responsibility, so you can focus your efforts. One such analysis, conducted by our firm, is shown in Figure 3. Although you might think the highest percent of patient financial responsibilities are for surgical procedures, notice that 4 of the top 5 services this practice identified as having the highest amount of patient collectible dollars are rendered in the office-carpal tunnel surgery being the only exception.
Take Action
After conducting a thorough analysis and reviewing the results, here are 5 actionable steps your practice could take:
1. Make sure your patient portal has the capacity to take patient payments. Offering online payment options increases the opportunity for patients to pay. Promote this option on the patient statement.
2. Implement a system of collecting from patients before they leave the office. After a new visit, which involves a more expensive evaluation and management code, and possibly imaging and durable medical device, counsel patients to leave a credit card on file, so the minute insurance pays, their credit card can be charged.
The 2017 Navicure Patient Payment Check-Up survey8 conducted by Healthcare Information and Management Systems Society (HIMSS) Analytics shows that 78% of patients would provide a card to be charged for one time up to $200. Think about the previously illustrated collection amounts this would alleviate.
3. Provide all surgery patients with a cost estimate. Generating cost estimates has been possible for close to 10 years. It’s done through your clearinghouse and practice management software by entering the CPT codes and diagnosis codes, along with the patient’s information. Save time and avoid tying staff up on hold.
According to the Navicure Patient Payment Check-Up survey,8 75% of provider organizations are able to provide a cost estimate upon request. It makes good business sense.
4. Collect a pre-treatment or pre-surgery scheduling deposit. In the KarenZupko & Associates/American Academy of Orthopaedic Surgeons (AAOS) pre-course survey of those attending the 2017 coding and reimbursement workshops, 55% of orthopedic practices reported that they have instituted such a practice. With the proliferation of HDHPs, asking for a scheduling deposit is fast becoming a must for all surgeons.
5. Offer patients a healthcare financing option through a third party. In response to another pre-course survey question, about offering CareCredit or another healthcare credit card, 28% of orthopedic practices say they do. Still, that leaves >70% of the orthopedic patients without a financing option. Given the reality of high deductible HDHPs and the patient responsibilities going uncollected, it’s time surgeons take a look at financing. It’s a fool’s wish to believe the practice is “saving” the service fee by sending dozens of statements, having staff make calls, and ultimately writing off unpaid balances as uncollectible.
Practices that fail to change, will fail to prosper. Those who have technology-phobic staff will suffer as healthcare continues to automate. Practices led by surgeons like one recently interviewed who said, “If patients knew how much it cost, they’d never schedule” will see patient accounts receivable soar and patient online ratings sink. The first quarter of 2018 means the number of patients with HDHPs will increase and that deductibles will have to be met. It’s wise to have a full staff meeting, share the facts, and put an action plan in place.
1. Gooch K. Why patients delay medical payments: 12 findings. Becker’s ASC. https://www.beckershospitalreview.com/finance/why-patients-delay-medical-payments-12-findings.html. Published August 28, 2017.
2. Murphy HL. You think your health insurance costs too much. Try being a farmer. Crain’s Chicago Business. http://www.chicagobusiness.com/article/20170929/ISSUE01/170929835. Published September 29, 2017. Accessed October 2, 2017.
3. 2017 Employer Health Benefits Survey. The Henry J. Kaiser Family Foundation and the Health Research & Educational Trust (HRET). https://www.kff.org/health-costs/report/2017-employer-health-benefits-survey/. Published September 19, 2017.
4. Minimizing Bad Debt: Point-of-Service Collections. The Advisory Board Company. https://www.advisory.com/-/media/Advisory-com/Research/FLC/Resources/2015/CFO-Brief-POS.pdf. Published August 21, 2015.
5. Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology-Enabled Communications. West Corporation. https://cdn2.hubspot.net/hubfs/402746/Assets/West%20Assets/Optimizing%20Revenue%20Report/Reports%20and%20Handouts/WEST-Optimizing%20Revenue%20Report%20final.pdf?t=1508789915319. Accessed October 26, 2017.
6. Peckham C. Medscape Orthopedist Compensation Report 2016. Medscape. https://www.medscape.com/features/slideshow/compensation/2016/orthopedics. Published April 1, 2016.
7. Ubel PA, Abernathy AP, Zafar SY. Full disclosure - out-of-pocket costs as side effects. N Engl J. Med. 2013;369:1484-1486. doi:10.1056/NEJMp1306826.
8. Patient Payment Check-Up 2017. Navicure. http://info.navicure.com/rs/669-OIJ-380/images/Navicure-Survey-Report-2017-Patient-Payment-Check-Up.pdf?mkt_tok=eyJpIjoiTVdKak1HUmhObVV6WkRVeSIsInQiOiJRcFNyRGVrOXlTS0pjalwvWEw3c2s1UmRMRHJVXC9EQzRkSnBkWCs0S2FEbUt3Z1I1a2Y3d1BBY3FKY0I1QWpEdkJRWU9ibmFlUlpnYVRIbVJMcStTVmdkRVwvSTJzcHE1cDVTajBRM3B1Q25lbDQwamViWnMwWGd1c1QzVk1cL2hYdkYifQ%3D%3D. Accessed October 26, 2017.
1. Gooch K. Why patients delay medical payments: 12 findings. Becker’s ASC. https://www.beckershospitalreview.com/finance/why-patients-delay-medical-payments-12-findings.html. Published August 28, 2017.
2. Murphy HL. You think your health insurance costs too much. Try being a farmer. Crain’s Chicago Business. http://www.chicagobusiness.com/article/20170929/ISSUE01/170929835. Published September 29, 2017. Accessed October 2, 2017.
3. 2017 Employer Health Benefits Survey. The Henry J. Kaiser Family Foundation and the Health Research & Educational Trust (HRET). https://www.kff.org/health-costs/report/2017-employer-health-benefits-survey/. Published September 19, 2017.
4. Minimizing Bad Debt: Point-of-Service Collections. The Advisory Board Company. https://www.advisory.com/-/media/Advisory-com/Research/FLC/Resources/2015/CFO-Brief-POS.pdf. Published August 21, 2015.
5. Optimizing Revenue: Solving Healthcare’s Revenue Cycle Challenges Using Technology-Enabled Communications. West Corporation. https://cdn2.hubspot.net/hubfs/402746/Assets/West%20Assets/Optimizing%20Revenue%20Report/Reports%20and%20Handouts/WEST-Optimizing%20Revenue%20Report%20final.pdf?t=1508789915319. Accessed October 26, 2017.
6. Peckham C. Medscape Orthopedist Compensation Report 2016. Medscape. https://www.medscape.com/features/slideshow/compensation/2016/orthopedics. Published April 1, 2016.
7. Ubel PA, Abernathy AP, Zafar SY. Full disclosure - out-of-pocket costs as side effects. N Engl J. Med. 2013;369:1484-1486. doi:10.1056/NEJMp1306826.
8. Patient Payment Check-Up 2017. Navicure. http://info.navicure.com/rs/669-OIJ-380/images/Navicure-Survey-Report-2017-Patient-Payment-Check-Up.pdf?mkt_tok=eyJpIjoiTVdKak1HUmhObVV6WkRVeSIsInQiOiJRcFNyRGVrOXlTS0pjalwvWEw3c2s1UmRMRHJVXC9EQzRkSnBkWCs0S2FEbUt3Z1I1a2Y3d1BBY3FKY0I1QWpEdkJRWU9ibmFlUlpnYVRIbVJMcStTVmdkRVwvSTJzcHE1cDVTajBRM3B1Q25lbDQwamViWnMwWGd1c1QzVk1cL2hYdkYifQ%3D%3D. Accessed October 26, 2017.
Business law critical to your practice
It is no surprise that the law is playing an ever more important role in the practice of medicine. Concerns about legal issues are a source of stress for ObGyns, including increasing worries about the economics of professional liability, the anxiety of defending a legal claim, and ambiguity about what is required for compliance.1 In this article my goal is to demystify some of the most important legal principles affecting your practice and provide suggestions for avoiding legal problems.
Medical malpractice: A form of negligence
Most ObGyns instinctively think first of medical malpractice when “legal problems” are mentioned—not an unreasonable response because obstetrics has a high incidence of malpractice claims. In one study, 77% of the American College of Obstetricians and Gynecologists (ACOG) Fellows reported that they have been sued.2
At its core, malpractice is a form of negligence, or, medical practice that falls below the quality of care that a reasonably careful practitioner would provide under the circumstances. When practice falls below that “standard of care,” and it causes injury, there may be malpractice liability. Insurance usually covers the cost of defending malpractice lawsuits and paying liability (although liability is the result of a minority of malpractice suits). There are, however, collateral consequences, including the time, stress, and disruption associated with defending the suit. In addition, malpractice may trigger review by the institutions with which the physician is associated, or in extreme cases, by licensing authorities. Large malpractice settlements or verdicts must be reported to the National Practitioner Database (sometimes colloquially referred to the “problem physician” database) or a similar state database.
This article is the third installment of the new series, "The Business of Medicine," edited by Joseph Sanfilippo, MD, MBA. In September, David Kim, MD, MBA, MPH, offered marketing strategies using social media. Last month, Dr. Sanfilippo presented ways to ensure patient satisfaction and service excellence in your practice. Watch next time for "Accounting 101." Other featured topics will include investing in your practice, billing and coding, gaining the competitive advantage, understanding "best practices," and striving for cost-effective care.
Related article:
Who is liable when a surgical error occurs?
Regulation and reimbursement (“compliance”) policies
The practice of medicine is closely regulated by federal and state bodies. Many regulations apply through reimbursement policies related to Medicare and Medicaid. While malpractice liability may, at worst, result in a financial award (with the cost of defense and any award paid by insurance), regulatory problems may result in a number of unpleasant consequences, most of which are not covered by insurance. In addition to loss of reimbursement, civil penalties (even criminalpenalties in extreme cases), loss of hospital privileges, licensure discipline, and loss of Medicare-Medicaid eligibility may result from regulatory noncompliance.3
There are multivolume sets discussing these legal requirements, so here we will look only at a tiny tip of the regulatory iceberg by mentioning some common regulatory areas.
Fraud and abuse laws refer to a bundle of federal (and some state) statutes and regulations that are intended to ensure that public-funded programs such as Medicare and Medicaid are not cheated or overpaying for services. It is a violation to provide low-quality services to government-funded programs. Proper payment and coding and ensuring that services were actually performed by the professional listed (not someone else) are examples of traps for the unwary. Submitting inaccurate records may result in action to recover incorrect payments and in civil penalties. In extreme cases where there is intentional misrepresentation, there have been criminal charges and loss of future Medicare-Medicaid eligibility.
Anti-kickback, self-referral, and Stark limitations are intended to avoid unnecessary or overpriced services. When someone is receiving a benefit for ordering or recommending a product or service, it is reasonable to expect that an incentive might affect the decision to order it, likely resulting in unnecessary or suboptimal services. It is illegal to receive a kickback for using, ordering, or recommending a product or service (a pharmaceutical company could not pay a physician $10 for each prescription written for its product). It is also illegal for physicians to refer patients to other entities in which they have a financial interest (a physician could not refer a patient to a lab in which the physician has partial ownership). The Stark laws and state prohibitions on self-referral have complex series of “safe harbor” exceptions in an ocean of prohibitions.4
HIPAA and confidentiality regulations are intended to protect patient privacy. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) has extensive regulations concerning both privacy and security. The medical community is well-versed in HIPAA regulations and sensitive (perhaps hypersensitive) to its requirements. Most states have patient privacy regulations that apply in addition to HIPAA and are commonly less well known.
Protecting patient confidentiality is an ethical, legal, and licensure obligation. Protecting patient confidentiality is, therefore, general duty and not tied to a specific federal program.5
Related article:
Patient with a breast mass: Why did she pursue litigation?
Insurance Fraud is the private side of fraud and abuse. Submitting private insurance claims that are false or a misrepresentation of service is generally a violation of the contract between the provider and the insurance company. It may also be a crime—it is, after all, a form of theft. Serious fraud may result in the loss of the license to practice.
The False Claims Act and Whistleblower laws make it a civil offense (and, in extreme cases, a criminal offense), to present to the government a false claim for payment of services. It may be false in the sense that the service was not provided or in the sense that service was of inadequate quality. These statutes (both federal and state) also allow for a private whistleblower to receive some of the proceeds if he or she helps the government recoup wrongful payments. Disgruntled former employees are a common source of whistleblowing.6
Abuse-reporting statutes are part of every state’s law but vary considerably. They require certain professions, including physicians, to report known or suspected abuse of children, dependent adults, and often, other groups. The failure to make required reports can result in civil liability or even (rarely) criminal charges.
Read about how organizational law affects ObGyns.
How organizational and commercial law affects ObGyns
Physicians are generally members of organizations that are engaged in the business of health care (even nonprofit organizations have business interests). There are 2 major legal building blocks of these business relationships: contracts and agency.7
Contracts are agreements between 2 or more persons or entities that carry with them legally enforceable obligations. The 3 common elements are an offer by one party, acceptance by another, and consideration (exchanging one thing of value for another). Contracts are binding in the sense that, if there is a breach of the promise by one party, the other party may seek monetary damages for the loss of the benefit of the bargain (and in limited circumstances, require that the contract be performed).
Agency is essentially the mechanism that allows a person to legally work for or on behalf of another. A “principal” authorizes an agent to take actions for, and bind, the principal. All employment, partnership, and “agent” relationships create an agency. The principal is generally responsible for the actions of the agent—at least within the scope of the agent’s authority. For example, the principal is responsible for the torts (civil liability resulting from the breach of a socially imposed duty, but generally not arising from a contract) of an agent doing the principal’s business. The agent has the obligation to act in good faith for the benefit of the principal and to abide by the instructions of the principal.
Corporate structures
There are a variety of corporate organizational structures; the basic types are corporations, partnerships, and unincorporated associations. These generally are available to nonprofit and for-profit organizations. As a general matter, corporations limit the owners’ personal liability; partnerships have tax advantages. A number of laws now allow the creation of entities that have both liability and tax advantages (subchapter S corporations, limited liability companies, and limited liability partnerships).
Other areas of business law
Employment law, which now affects almost every aspect of hiring, dismissal, payment, and fringe benefits, is not a single law but a series of state and federal statutes, regulations, and court decisions.8
Competition is regulated through a number of antitrust laws as well as fair business practices. These affect the ability of health care entities to merge, fix prices, and split markets.9
There are literally hundreds of other laws that affect the way health care entities can operate. Conducting a careful compliance review is of considerable importance.10
Read about the dos and don’ts of preventive law.
Dos and don’ts of preventive law
The business of medicine is subject to many laws and keeping track of all of these is generally beyond the expertise of the ObGyn. Here are a few practical suggestions for thriving in this legal milieu.
Understanding the law
DO establish an ongoing relationship with an attorney you can trust who is knowledgeable in health law. Consult with this attorney not only on an as-needed basis but also for an “annual checkup” of legal issues affecting your practice.
DON’T guess what the law is. Laws vary from state to state and change frequently. Taking curbstone advice or suggestions from a podcast is a good way to develop problems.
Error reduction
DO take risk management seriously. Implement plans to improve patient safety and reduce errors.11
DON’T ignore angry or hostile patients. Their hostility may be directed at you—an undesirable state. The same goes for disgruntled (or former) employees, who may become whistleblowers.
Insurance
DO review your insurance coverage annually, preferably with an expert or your attorney. Insurance policies and your insurance needs change frequently.
DON’T assume you have all the insurance you need or that insurance will cover all legal claims arising from your practice. Intentional torts, some antitrust claims, licensure discipline, and civil fines, for example, may not be covered.
Informed consent and ethics
DO use the informed consent process as a means of improving communication between you and your patients to address their concerns and discuss expectations. Autonomy is a basic ethical value of medicine and informed consent helps to achieve that goal.
DON’T ignore ethics. Ethical obligations are not just essential to maintaining a license, hospital privileges, and professional standing.12 They also help guide you toward good practice that avoids liability.
Related articles:
Informed consent: The more you know, the more you and your patient are protected
Compliance, disputes, and arbitration
DO engage in continuing compliance review. That includes understanding the contracts and professional arrangements in which you practice and all of the requirements of third-party payers (especially government entities). There are a wide range of other compliance obligations that require ongoing attention.
DON’T sign arbitration agreements without understanding exactly what you are agreeing to. There are advantages to arbitration,13 but there are disadvantages, too.14 The courts generally enforce arbitration agreements, even ones that are unfair or one-sided.15
The law need not be a mystery or the enemy. Preventive law, like preventive medicine, can make all the difference.16
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Carpentieri AM, Lumalcuri JJ, Shaw J, Joseph GF Jr. Overview of the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability. https://www.acog.org/-/media/Departments/Professional-Liability/2015PLSurveyNationalSummary11315.pdf?dmc=1&ts=20171003T150028497. Published November 3, 2015. Accessed October 3, 2017.
- American College of Obstetrics and Gynecology Committee on Professional Liability. ACOG Opinion No. 551: Coping with the stress of professional liability litigation. Obstet Gynecol. 2013;121(1):220–222.
- Teitlebaum JB, Wilensky SE. Essential of Health Policy and Law. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2012:31–43, 127–134.
- Fabrikant R, Kalb PE, Bucy PH, Hopson MD. Health Care Fraud: Enforcement and Compliance. Newark, NJ: Law Journal Press; 2017;4:44–140.
- Health Information Privacy. Department of Health and Human Services. https://www.hhs.gov/hipaa. Updated 2017. Accessed October 3, 2017.
- Kropf S. Healthcare Fraud 101: The False Claims Act. ObGyn.Net. http://www.obgyn.net/blog/healthcare-fraud-101-false-claims-act. Published March 10, 2017. Accessed October 3, 2017.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91–126.
- Todd MK. The Physician Employment Contract Handbook: A Guide to Structuring Equitable Arrangements. 2nd ed. New York, NY: Productivity Press; 2011:67–77, 93–118.
- Federal Trade Commission. Competition in the Health Care Marketplace. https://www.ftc.gov/tips-advice/competition-guidance/industry-guidance/health-care. Updated 2017. Accessed October 3, 2017.
- Shwayder JM. What is new in medical-legal issues in obstetrics and gynecology?: Best articles from the past 2 years. Obstet Gynecol. 2016;128(6):1441–1442.
- Sanfilippo JS, Smith SR. Risk Management. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:277–298.
- Smith SR, Sanfilippo JS. Ethics and the Business of the Healthcare Professional. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:71–89.
- Knag PE, Kagan DJ. Why arbitration is the preferred dispute resolution vehicle for most integrated delivery system disputes. Dispute Resolution J. 2016;71(3):127–137.
- Larson DA, Dahl D. Medical malpractice arbitration: Not business as usual. Yearbook Arbitration Mediation. 2016;8:69–92.
- Trantina TL. What law applies to an agreement to arbitrate? American Bar Association. Dispute Resolution Magazine. Fall 2015:29–31.
- Curran M. Preventative law: Interdisciplinary from medical-legal partnership. NYU Rev Law Social Change. 2014;38(4):595–606.
It is no surprise that the law is playing an ever more important role in the practice of medicine. Concerns about legal issues are a source of stress for ObGyns, including increasing worries about the economics of professional liability, the anxiety of defending a legal claim, and ambiguity about what is required for compliance.1 In this article my goal is to demystify some of the most important legal principles affecting your practice and provide suggestions for avoiding legal problems.
Medical malpractice: A form of negligence
Most ObGyns instinctively think first of medical malpractice when “legal problems” are mentioned—not an unreasonable response because obstetrics has a high incidence of malpractice claims. In one study, 77% of the American College of Obstetricians and Gynecologists (ACOG) Fellows reported that they have been sued.2
At its core, malpractice is a form of negligence, or, medical practice that falls below the quality of care that a reasonably careful practitioner would provide under the circumstances. When practice falls below that “standard of care,” and it causes injury, there may be malpractice liability. Insurance usually covers the cost of defending malpractice lawsuits and paying liability (although liability is the result of a minority of malpractice suits). There are, however, collateral consequences, including the time, stress, and disruption associated with defending the suit. In addition, malpractice may trigger review by the institutions with which the physician is associated, or in extreme cases, by licensing authorities. Large malpractice settlements or verdicts must be reported to the National Practitioner Database (sometimes colloquially referred to the “problem physician” database) or a similar state database.
This article is the third installment of the new series, "The Business of Medicine," edited by Joseph Sanfilippo, MD, MBA. In September, David Kim, MD, MBA, MPH, offered marketing strategies using social media. Last month, Dr. Sanfilippo presented ways to ensure patient satisfaction and service excellence in your practice. Watch next time for "Accounting 101." Other featured topics will include investing in your practice, billing and coding, gaining the competitive advantage, understanding "best practices," and striving for cost-effective care.
Related article:
Who is liable when a surgical error occurs?
Regulation and reimbursement (“compliance”) policies
The practice of medicine is closely regulated by federal and state bodies. Many regulations apply through reimbursement policies related to Medicare and Medicaid. While malpractice liability may, at worst, result in a financial award (with the cost of defense and any award paid by insurance), regulatory problems may result in a number of unpleasant consequences, most of which are not covered by insurance. In addition to loss of reimbursement, civil penalties (even criminalpenalties in extreme cases), loss of hospital privileges, licensure discipline, and loss of Medicare-Medicaid eligibility may result from regulatory noncompliance.3
There are multivolume sets discussing these legal requirements, so here we will look only at a tiny tip of the regulatory iceberg by mentioning some common regulatory areas.
Fraud and abuse laws refer to a bundle of federal (and some state) statutes and regulations that are intended to ensure that public-funded programs such as Medicare and Medicaid are not cheated or overpaying for services. It is a violation to provide low-quality services to government-funded programs. Proper payment and coding and ensuring that services were actually performed by the professional listed (not someone else) are examples of traps for the unwary. Submitting inaccurate records may result in action to recover incorrect payments and in civil penalties. In extreme cases where there is intentional misrepresentation, there have been criminal charges and loss of future Medicare-Medicaid eligibility.
Anti-kickback, self-referral, and Stark limitations are intended to avoid unnecessary or overpriced services. When someone is receiving a benefit for ordering or recommending a product or service, it is reasonable to expect that an incentive might affect the decision to order it, likely resulting in unnecessary or suboptimal services. It is illegal to receive a kickback for using, ordering, or recommending a product or service (a pharmaceutical company could not pay a physician $10 for each prescription written for its product). It is also illegal for physicians to refer patients to other entities in which they have a financial interest (a physician could not refer a patient to a lab in which the physician has partial ownership). The Stark laws and state prohibitions on self-referral have complex series of “safe harbor” exceptions in an ocean of prohibitions.4
HIPAA and confidentiality regulations are intended to protect patient privacy. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) has extensive regulations concerning both privacy and security. The medical community is well-versed in HIPAA regulations and sensitive (perhaps hypersensitive) to its requirements. Most states have patient privacy regulations that apply in addition to HIPAA and are commonly less well known.
Protecting patient confidentiality is an ethical, legal, and licensure obligation. Protecting patient confidentiality is, therefore, general duty and not tied to a specific federal program.5
Related article:
Patient with a breast mass: Why did she pursue litigation?
Insurance Fraud is the private side of fraud and abuse. Submitting private insurance claims that are false or a misrepresentation of service is generally a violation of the contract between the provider and the insurance company. It may also be a crime—it is, after all, a form of theft. Serious fraud may result in the loss of the license to practice.
The False Claims Act and Whistleblower laws make it a civil offense (and, in extreme cases, a criminal offense), to present to the government a false claim for payment of services. It may be false in the sense that the service was not provided or in the sense that service was of inadequate quality. These statutes (both federal and state) also allow for a private whistleblower to receive some of the proceeds if he or she helps the government recoup wrongful payments. Disgruntled former employees are a common source of whistleblowing.6
Abuse-reporting statutes are part of every state’s law but vary considerably. They require certain professions, including physicians, to report known or suspected abuse of children, dependent adults, and often, other groups. The failure to make required reports can result in civil liability or even (rarely) criminal charges.
Read about how organizational law affects ObGyns.
How organizational and commercial law affects ObGyns
Physicians are generally members of organizations that are engaged in the business of health care (even nonprofit organizations have business interests). There are 2 major legal building blocks of these business relationships: contracts and agency.7
Contracts are agreements between 2 or more persons or entities that carry with them legally enforceable obligations. The 3 common elements are an offer by one party, acceptance by another, and consideration (exchanging one thing of value for another). Contracts are binding in the sense that, if there is a breach of the promise by one party, the other party may seek monetary damages for the loss of the benefit of the bargain (and in limited circumstances, require that the contract be performed).
Agency is essentially the mechanism that allows a person to legally work for or on behalf of another. A “principal” authorizes an agent to take actions for, and bind, the principal. All employment, partnership, and “agent” relationships create an agency. The principal is generally responsible for the actions of the agent—at least within the scope of the agent’s authority. For example, the principal is responsible for the torts (civil liability resulting from the breach of a socially imposed duty, but generally not arising from a contract) of an agent doing the principal’s business. The agent has the obligation to act in good faith for the benefit of the principal and to abide by the instructions of the principal.
Corporate structures
There are a variety of corporate organizational structures; the basic types are corporations, partnerships, and unincorporated associations. These generally are available to nonprofit and for-profit organizations. As a general matter, corporations limit the owners’ personal liability; partnerships have tax advantages. A number of laws now allow the creation of entities that have both liability and tax advantages (subchapter S corporations, limited liability companies, and limited liability partnerships).
Other areas of business law
Employment law, which now affects almost every aspect of hiring, dismissal, payment, and fringe benefits, is not a single law but a series of state and federal statutes, regulations, and court decisions.8
Competition is regulated through a number of antitrust laws as well as fair business practices. These affect the ability of health care entities to merge, fix prices, and split markets.9
There are literally hundreds of other laws that affect the way health care entities can operate. Conducting a careful compliance review is of considerable importance.10
Read about the dos and don’ts of preventive law.
Dos and don’ts of preventive law
The business of medicine is subject to many laws and keeping track of all of these is generally beyond the expertise of the ObGyn. Here are a few practical suggestions for thriving in this legal milieu.
Understanding the law
DO establish an ongoing relationship with an attorney you can trust who is knowledgeable in health law. Consult with this attorney not only on an as-needed basis but also for an “annual checkup” of legal issues affecting your practice.
DON’T guess what the law is. Laws vary from state to state and change frequently. Taking curbstone advice or suggestions from a podcast is a good way to develop problems.
Error reduction
DO take risk management seriously. Implement plans to improve patient safety and reduce errors.11
DON’T ignore angry or hostile patients. Their hostility may be directed at you—an undesirable state. The same goes for disgruntled (or former) employees, who may become whistleblowers.
Insurance
DO review your insurance coverage annually, preferably with an expert or your attorney. Insurance policies and your insurance needs change frequently.
DON’T assume you have all the insurance you need or that insurance will cover all legal claims arising from your practice. Intentional torts, some antitrust claims, licensure discipline, and civil fines, for example, may not be covered.
Informed consent and ethics
DO use the informed consent process as a means of improving communication between you and your patients to address their concerns and discuss expectations. Autonomy is a basic ethical value of medicine and informed consent helps to achieve that goal.
DON’T ignore ethics. Ethical obligations are not just essential to maintaining a license, hospital privileges, and professional standing.12 They also help guide you toward good practice that avoids liability.
Related articles:
Informed consent: The more you know, the more you and your patient are protected
Compliance, disputes, and arbitration
DO engage in continuing compliance review. That includes understanding the contracts and professional arrangements in which you practice and all of the requirements of third-party payers (especially government entities). There are a wide range of other compliance obligations that require ongoing attention.
DON’T sign arbitration agreements without understanding exactly what you are agreeing to. There are advantages to arbitration,13 but there are disadvantages, too.14 The courts generally enforce arbitration agreements, even ones that are unfair or one-sided.15
The law need not be a mystery or the enemy. Preventive law, like preventive medicine, can make all the difference.16
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
It is no surprise that the law is playing an ever more important role in the practice of medicine. Concerns about legal issues are a source of stress for ObGyns, including increasing worries about the economics of professional liability, the anxiety of defending a legal claim, and ambiguity about what is required for compliance.1 In this article my goal is to demystify some of the most important legal principles affecting your practice and provide suggestions for avoiding legal problems.
Medical malpractice: A form of negligence
Most ObGyns instinctively think first of medical malpractice when “legal problems” are mentioned—not an unreasonable response because obstetrics has a high incidence of malpractice claims. In one study, 77% of the American College of Obstetricians and Gynecologists (ACOG) Fellows reported that they have been sued.2
At its core, malpractice is a form of negligence, or, medical practice that falls below the quality of care that a reasonably careful practitioner would provide under the circumstances. When practice falls below that “standard of care,” and it causes injury, there may be malpractice liability. Insurance usually covers the cost of defending malpractice lawsuits and paying liability (although liability is the result of a minority of malpractice suits). There are, however, collateral consequences, including the time, stress, and disruption associated with defending the suit. In addition, malpractice may trigger review by the institutions with which the physician is associated, or in extreme cases, by licensing authorities. Large malpractice settlements or verdicts must be reported to the National Practitioner Database (sometimes colloquially referred to the “problem physician” database) or a similar state database.
This article is the third installment of the new series, "The Business of Medicine," edited by Joseph Sanfilippo, MD, MBA. In September, David Kim, MD, MBA, MPH, offered marketing strategies using social media. Last month, Dr. Sanfilippo presented ways to ensure patient satisfaction and service excellence in your practice. Watch next time for "Accounting 101." Other featured topics will include investing in your practice, billing and coding, gaining the competitive advantage, understanding "best practices," and striving for cost-effective care.
Related article:
Who is liable when a surgical error occurs?
Regulation and reimbursement (“compliance”) policies
The practice of medicine is closely regulated by federal and state bodies. Many regulations apply through reimbursement policies related to Medicare and Medicaid. While malpractice liability may, at worst, result in a financial award (with the cost of defense and any award paid by insurance), regulatory problems may result in a number of unpleasant consequences, most of which are not covered by insurance. In addition to loss of reimbursement, civil penalties (even criminalpenalties in extreme cases), loss of hospital privileges, licensure discipline, and loss of Medicare-Medicaid eligibility may result from regulatory noncompliance.3
There are multivolume sets discussing these legal requirements, so here we will look only at a tiny tip of the regulatory iceberg by mentioning some common regulatory areas.
Fraud and abuse laws refer to a bundle of federal (and some state) statutes and regulations that are intended to ensure that public-funded programs such as Medicare and Medicaid are not cheated or overpaying for services. It is a violation to provide low-quality services to government-funded programs. Proper payment and coding and ensuring that services were actually performed by the professional listed (not someone else) are examples of traps for the unwary. Submitting inaccurate records may result in action to recover incorrect payments and in civil penalties. In extreme cases where there is intentional misrepresentation, there have been criminal charges and loss of future Medicare-Medicaid eligibility.
Anti-kickback, self-referral, and Stark limitations are intended to avoid unnecessary or overpriced services. When someone is receiving a benefit for ordering or recommending a product or service, it is reasonable to expect that an incentive might affect the decision to order it, likely resulting in unnecessary or suboptimal services. It is illegal to receive a kickback for using, ordering, or recommending a product or service (a pharmaceutical company could not pay a physician $10 for each prescription written for its product). It is also illegal for physicians to refer patients to other entities in which they have a financial interest (a physician could not refer a patient to a lab in which the physician has partial ownership). The Stark laws and state prohibitions on self-referral have complex series of “safe harbor” exceptions in an ocean of prohibitions.4
HIPAA and confidentiality regulations are intended to protect patient privacy. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) has extensive regulations concerning both privacy and security. The medical community is well-versed in HIPAA regulations and sensitive (perhaps hypersensitive) to its requirements. Most states have patient privacy regulations that apply in addition to HIPAA and are commonly less well known.
Protecting patient confidentiality is an ethical, legal, and licensure obligation. Protecting patient confidentiality is, therefore, general duty and not tied to a specific federal program.5
Related article:
Patient with a breast mass: Why did she pursue litigation?
Insurance Fraud is the private side of fraud and abuse. Submitting private insurance claims that are false or a misrepresentation of service is generally a violation of the contract between the provider and the insurance company. It may also be a crime—it is, after all, a form of theft. Serious fraud may result in the loss of the license to practice.
The False Claims Act and Whistleblower laws make it a civil offense (and, in extreme cases, a criminal offense), to present to the government a false claim for payment of services. It may be false in the sense that the service was not provided or in the sense that service was of inadequate quality. These statutes (both federal and state) also allow for a private whistleblower to receive some of the proceeds if he or she helps the government recoup wrongful payments. Disgruntled former employees are a common source of whistleblowing.6
Abuse-reporting statutes are part of every state’s law but vary considerably. They require certain professions, including physicians, to report known or suspected abuse of children, dependent adults, and often, other groups. The failure to make required reports can result in civil liability or even (rarely) criminal charges.
Read about how organizational law affects ObGyns.
How organizational and commercial law affects ObGyns
Physicians are generally members of organizations that are engaged in the business of health care (even nonprofit organizations have business interests). There are 2 major legal building blocks of these business relationships: contracts and agency.7
Contracts are agreements between 2 or more persons or entities that carry with them legally enforceable obligations. The 3 common elements are an offer by one party, acceptance by another, and consideration (exchanging one thing of value for another). Contracts are binding in the sense that, if there is a breach of the promise by one party, the other party may seek monetary damages for the loss of the benefit of the bargain (and in limited circumstances, require that the contract be performed).
Agency is essentially the mechanism that allows a person to legally work for or on behalf of another. A “principal” authorizes an agent to take actions for, and bind, the principal. All employment, partnership, and “agent” relationships create an agency. The principal is generally responsible for the actions of the agent—at least within the scope of the agent’s authority. For example, the principal is responsible for the torts (civil liability resulting from the breach of a socially imposed duty, but generally not arising from a contract) of an agent doing the principal’s business. The agent has the obligation to act in good faith for the benefit of the principal and to abide by the instructions of the principal.
Corporate structures
There are a variety of corporate organizational structures; the basic types are corporations, partnerships, and unincorporated associations. These generally are available to nonprofit and for-profit organizations. As a general matter, corporations limit the owners’ personal liability; partnerships have tax advantages. A number of laws now allow the creation of entities that have both liability and tax advantages (subchapter S corporations, limited liability companies, and limited liability partnerships).
Other areas of business law
Employment law, which now affects almost every aspect of hiring, dismissal, payment, and fringe benefits, is not a single law but a series of state and federal statutes, regulations, and court decisions.8
Competition is regulated through a number of antitrust laws as well as fair business practices. These affect the ability of health care entities to merge, fix prices, and split markets.9
There are literally hundreds of other laws that affect the way health care entities can operate. Conducting a careful compliance review is of considerable importance.10
Read about the dos and don’ts of preventive law.
Dos and don’ts of preventive law
The business of medicine is subject to many laws and keeping track of all of these is generally beyond the expertise of the ObGyn. Here are a few practical suggestions for thriving in this legal milieu.
Understanding the law
DO establish an ongoing relationship with an attorney you can trust who is knowledgeable in health law. Consult with this attorney not only on an as-needed basis but also for an “annual checkup” of legal issues affecting your practice.
DON’T guess what the law is. Laws vary from state to state and change frequently. Taking curbstone advice or suggestions from a podcast is a good way to develop problems.
Error reduction
DO take risk management seriously. Implement plans to improve patient safety and reduce errors.11
DON’T ignore angry or hostile patients. Their hostility may be directed at you—an undesirable state. The same goes for disgruntled (or former) employees, who may become whistleblowers.
Insurance
DO review your insurance coverage annually, preferably with an expert or your attorney. Insurance policies and your insurance needs change frequently.
DON’T assume you have all the insurance you need or that insurance will cover all legal claims arising from your practice. Intentional torts, some antitrust claims, licensure discipline, and civil fines, for example, may not be covered.
Informed consent and ethics
DO use the informed consent process as a means of improving communication between you and your patients to address their concerns and discuss expectations. Autonomy is a basic ethical value of medicine and informed consent helps to achieve that goal.
DON’T ignore ethics. Ethical obligations are not just essential to maintaining a license, hospital privileges, and professional standing.12 They also help guide you toward good practice that avoids liability.
Related articles:
Informed consent: The more you know, the more you and your patient are protected
Compliance, disputes, and arbitration
DO engage in continuing compliance review. That includes understanding the contracts and professional arrangements in which you practice and all of the requirements of third-party payers (especially government entities). There are a wide range of other compliance obligations that require ongoing attention.
DON’T sign arbitration agreements without understanding exactly what you are agreeing to. There are advantages to arbitration,13 but there are disadvantages, too.14 The courts generally enforce arbitration agreements, even ones that are unfair or one-sided.15
The law need not be a mystery or the enemy. Preventive law, like preventive medicine, can make all the difference.16
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Carpentieri AM, Lumalcuri JJ, Shaw J, Joseph GF Jr. Overview of the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability. https://www.acog.org/-/media/Departments/Professional-Liability/2015PLSurveyNationalSummary11315.pdf?dmc=1&ts=20171003T150028497. Published November 3, 2015. Accessed October 3, 2017.
- American College of Obstetrics and Gynecology Committee on Professional Liability. ACOG Opinion No. 551: Coping with the stress of professional liability litigation. Obstet Gynecol. 2013;121(1):220–222.
- Teitlebaum JB, Wilensky SE. Essential of Health Policy and Law. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2012:31–43, 127–134.
- Fabrikant R, Kalb PE, Bucy PH, Hopson MD. Health Care Fraud: Enforcement and Compliance. Newark, NJ: Law Journal Press; 2017;4:44–140.
- Health Information Privacy. Department of Health and Human Services. https://www.hhs.gov/hipaa. Updated 2017. Accessed October 3, 2017.
- Kropf S. Healthcare Fraud 101: The False Claims Act. ObGyn.Net. http://www.obgyn.net/blog/healthcare-fraud-101-false-claims-act. Published March 10, 2017. Accessed October 3, 2017.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91–126.
- Todd MK. The Physician Employment Contract Handbook: A Guide to Structuring Equitable Arrangements. 2nd ed. New York, NY: Productivity Press; 2011:67–77, 93–118.
- Federal Trade Commission. Competition in the Health Care Marketplace. https://www.ftc.gov/tips-advice/competition-guidance/industry-guidance/health-care. Updated 2017. Accessed October 3, 2017.
- Shwayder JM. What is new in medical-legal issues in obstetrics and gynecology?: Best articles from the past 2 years. Obstet Gynecol. 2016;128(6):1441–1442.
- Sanfilippo JS, Smith SR. Risk Management. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:277–298.
- Smith SR, Sanfilippo JS. Ethics and the Business of the Healthcare Professional. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:71–89.
- Knag PE, Kagan DJ. Why arbitration is the preferred dispute resolution vehicle for most integrated delivery system disputes. Dispute Resolution J. 2016;71(3):127–137.
- Larson DA, Dahl D. Medical malpractice arbitration: Not business as usual. Yearbook Arbitration Mediation. 2016;8:69–92.
- Trantina TL. What law applies to an agreement to arbitrate? American Bar Association. Dispute Resolution Magazine. Fall 2015:29–31.
- Curran M. Preventative law: Interdisciplinary from medical-legal partnership. NYU Rev Law Social Change. 2014;38(4):595–606.
- Carpentieri AM, Lumalcuri JJ, Shaw J, Joseph GF Jr. Overview of the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability. https://www.acog.org/-/media/Departments/Professional-Liability/2015PLSurveyNationalSummary11315.pdf?dmc=1&ts=20171003T150028497. Published November 3, 2015. Accessed October 3, 2017.
- American College of Obstetrics and Gynecology Committee on Professional Liability. ACOG Opinion No. 551: Coping with the stress of professional liability litigation. Obstet Gynecol. 2013;121(1):220–222.
- Teitlebaum JB, Wilensky SE. Essential of Health Policy and Law. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2012:31–43, 127–134.
- Fabrikant R, Kalb PE, Bucy PH, Hopson MD. Health Care Fraud: Enforcement and Compliance. Newark, NJ: Law Journal Press; 2017;4:44–140.
- Health Information Privacy. Department of Health and Human Services. https://www.hhs.gov/hipaa. Updated 2017. Accessed October 3, 2017.
- Kropf S. Healthcare Fraud 101: The False Claims Act. ObGyn.Net. http://www.obgyn.net/blog/healthcare-fraud-101-false-claims-act. Published March 10, 2017. Accessed October 3, 2017.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91–126.
- Todd MK. The Physician Employment Contract Handbook: A Guide to Structuring Equitable Arrangements. 2nd ed. New York, NY: Productivity Press; 2011:67–77, 93–118.
- Federal Trade Commission. Competition in the Health Care Marketplace. https://www.ftc.gov/tips-advice/competition-guidance/industry-guidance/health-care. Updated 2017. Accessed October 3, 2017.
- Shwayder JM. What is new in medical-legal issues in obstetrics and gynecology?: Best articles from the past 2 years. Obstet Gynecol. 2016;128(6):1441–1442.
- Sanfilippo JS, Smith SR. Risk Management. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:277–298.
- Smith SR, Sanfilippo JS. Ethics and the Business of the Healthcare Professional. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:71–89.
- Knag PE, Kagan DJ. Why arbitration is the preferred dispute resolution vehicle for most integrated delivery system disputes. Dispute Resolution J. 2016;71(3):127–137.
- Larson DA, Dahl D. Medical malpractice arbitration: Not business as usual. Yearbook Arbitration Mediation. 2016;8:69–92.
- Trantina TL. What law applies to an agreement to arbitrate? American Bar Association. Dispute Resolution Magazine. Fall 2015:29–31.
- Curran M. Preventative law: Interdisciplinary from medical-legal partnership. NYU Rev Law Social Change. 2014;38(4):595–606.
MACRA in a nutshell
Much has been written over the past year about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and its primary vehicle, the Merit-Based Incentive System (MIPS); but many small practices seem reluctant to take it seriously, despite the fact that it puts yet another significant percentage of our Medicare reimbursements at risk.
Those much-publicized attempts to “repeal and replace” the Affordable Care Act earlier this year undoubtedly contributed to the apathy; but the ACA is apparently here to stay, and the first MIPS “performance period” ends on Dec. 31, so now would be an excellent time to get up to speed. Herewith, the basics:
Each practice must choose between two payment tracks: either MIPS or one of the so-called Alternate Payment Models (APM). The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries (QCDRs), such as Approved Quality Improvement (AQI); total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The final MACRA regulations, issued last October, allow a more gradual MIPS implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty in 2019 – but not qualify for a bonus – by reporting your performance in only one quality-of-care or practice-improvement category by the end of this year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss, as very few models have been presented – or even defined – to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most of those have failed miserably in real-world settings. The Episode of Care (EOC) model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but this remains untested and in the end may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as APMs that are better and more efficient become available, as it appears that there will be more financial security there, with less risk of penalties; but you will probably need to start in the MIPS program, since most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do so.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of the Center for Medicare & Medicaid Services’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Much has been written over the past year about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and its primary vehicle, the Merit-Based Incentive System (MIPS); but many small practices seem reluctant to take it seriously, despite the fact that it puts yet another significant percentage of our Medicare reimbursements at risk.
Those much-publicized attempts to “repeal and replace” the Affordable Care Act earlier this year undoubtedly contributed to the apathy; but the ACA is apparently here to stay, and the first MIPS “performance period” ends on Dec. 31, so now would be an excellent time to get up to speed. Herewith, the basics:
Each practice must choose between two payment tracks: either MIPS or one of the so-called Alternate Payment Models (APM). The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries (QCDRs), such as Approved Quality Improvement (AQI); total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The final MACRA regulations, issued last October, allow a more gradual MIPS implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty in 2019 – but not qualify for a bonus – by reporting your performance in only one quality-of-care or practice-improvement category by the end of this year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss, as very few models have been presented – or even defined – to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most of those have failed miserably in real-world settings. The Episode of Care (EOC) model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but this remains untested and in the end may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as APMs that are better and more efficient become available, as it appears that there will be more financial security there, with less risk of penalties; but you will probably need to start in the MIPS program, since most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do so.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of the Center for Medicare & Medicaid Services’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Much has been written over the past year about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and its primary vehicle, the Merit-Based Incentive System (MIPS); but many small practices seem reluctant to take it seriously, despite the fact that it puts yet another significant percentage of our Medicare reimbursements at risk.
Those much-publicized attempts to “repeal and replace” the Affordable Care Act earlier this year undoubtedly contributed to the apathy; but the ACA is apparently here to stay, and the first MIPS “performance period” ends on Dec. 31, so now would be an excellent time to get up to speed. Herewith, the basics:
Each practice must choose between two payment tracks: either MIPS or one of the so-called Alternate Payment Models (APM). The MIPS track will use the four reporting programs just mentioned to compile a composite score between 0 and 100 each year for every practitioner, based on four performance metrics: quality measures listed in Qualified Clinical Data Registries (QCDRs), such as Approved Quality Improvement (AQI); total resources used by each practitioner, as measured by VBM; “improvement activities” (MOC); and MU, in some new, as-yet-undefined form. You can earn a bonus of 4% of reimbursement in 2019, rising to 5% in 2020, 7% in 2021, and 9% in 2022 – or you can be penalized those amounts (“negative adjustments”) if your performance doesn’t measure up.
The final MACRA regulations, issued last October, allow a more gradual MIPS implementation that should decrease the penalty burden for small practices, at least initially. For example, you can avoid a penalty in 2019 – but not qualify for a bonus – by reporting your performance in only one quality-of-care or practice-improvement category by the end of this year. A decrease in penalties, however, means a smaller pot for bonuses – and reprieves will be temporary.
The alternative, APM, is difficult to discuss, as very few models have been presented – or even defined – to date. Only Accountable Care Organizations (ACOs) have been introduced in any quantity, and most of those have failed miserably in real-world settings. The Episode of Care (EOC) model, which pays providers a fixed amount for all services rendered in a bundle (“episode”) of care, has been discussed at some length, but this remains untested and in the end may turn out to be just another variant of capitation.
So, which to choose? Long term, I strongly suggest that everyone prepare for the APM track as soon as APMs that are better and more efficient become available, as it appears that there will be more financial security there, with less risk of penalties; but you will probably need to start in the MIPS program, since most projections indicate that the great majority of practitioners, particularly those in smaller operations, will do so.
While some may be prompted to join a larger organization or network to decrease their risk of MIPS penalties and gain quicker access to the APM track – which may well be one of the Center for Medicare & Medicaid Services’ surreptitious goals in introducing MACRA in the first place – there are steps that those individuals and small groups who choose to remain independent can take now to maximize their chances of landing on the bonus side of the MIPS ledger.
If the alphabet soup above has your head swimming, join the club – you’re far from alone; but don’t be discouraged. CMS has indicated its willingness to make changes aimed at decreasing the administrative burden and, in its words, “making the transition to MACRA as simple and as flexible as possible.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].