User login
Are robotic surgery complications underreported?
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
Although US hospitals have been quick to embrace surgical robot technology over the past decade, a “slapdash” system of reporting complications paints an unclear picture of its safety, according to Johns Hopkins researchers.
The Johns Hopkins team, led by Martin A. Makary, MD, MPH, found that, among the 1 million or so robotic surgeries performed since 2000, only 245 complications—including 71 deaths—were reported to the US Food and Drug Administration (FDA).1 When an adverse event or device malfunction occurs, hospitals are required to report these incidents to the manufacturer, which in turn is required to report them to the FDA—but this reporting doesn’t always happen.
“The number reported is very low for any complex technology used over a million times,” says Dr. Makary, associate professor of surgery at the Johns Hopkins University School of Medicine. “Doctors and patients can’t properly evaluate safety when we have a haphazard system of collecting data that is not independent and not transparent. There may be some complications specific to the use of this device, but we can only learn about them if we accurately track outcomes.”
The use of the robot in surgery has skyrocketed. Between 2007 and 2011, for example, the number of procedures involving the robot increased by more than 400% in the United States and more than 300% internationally. At the end of 2011, there were 1,400 surgical robots installed in US hospitals, up from 800 just 4 years earlier.
Some incidents went unreported until the news media highlighted them
Dr. Makary and colleagues found several incidents reported in the national news media that were not reported to the FDA until after the stories appeared in the press, even though the incidents took place long before the media exposure. Dr. Makary says it’s likely that many other incidents go unreported, never to be captured by research like his or by the FDA.
“We need innovation in medicine and, in this country, we are tremendously good at introducing new technologies,” he says. “But we have to evaluate new technology properly so we don’t over-adopt—or under-adopt—important advances that could benefit patients.”
How the study was conducted
Makary and colleagues reviewed the FDA adverse events database from January 1, 2000, to August 1, 2012. They also searched legal judgments and adverse events using LexisNexis to scan news media, and PACER to scan court records. The cases then were cross-referenced to see if they matched. The investigators found that eight cases were not appropriately reported to the FDA, five of which were never reported and two of which were reported only after a story about them appeared in the press.
Complication rate was highest for hysterectomy
When investigators reviewed complications that were reported, the procedures most commonly associated with death were:
- gynecologic (22 of the 71 deaths)
- urologic (15 deaths)
- cardiothoracic (12 deaths).
The cause of death was most often excessive bleeding. In cases where patients survived, hysterectomy by far had the most complications (43% of injuries).
A call for standardized reporting
Dr. Makary contends that standardized reporting is needed for all adverse events related to robotic devices. One rare complication that occurs, he says, is that a surgeon can accidentally cut the aorta because the surgeon cannot feel its firmness. For reporting purposes, however, it’s unclear whether such an event is surgeon error or device-related error. The FDA currently collects only device-related errors.
Dr. Makary argues that errors such as inadvertent cutting of the aorta, although preventable with proper technique, should be tracked as device-related errors because they are more common with robotic surgery than with conventional surgery. Without better reporting standards, he says, these complications are less likely to be reported to the FDA at all. And if they go unreported, they cannot contribute to the understanding or identification of safety problems.
He suggests one solution: use of a database like the one maintained by the American College of Surgeons, in which independent nurses identify and track adverse events and complications of traditional operations.
Good information on robotic surgery is needed not only for research, but also to ensure that patients are fully informed about potential risks. Right now, Dr. Makary says, it’s too easy for a surgeon to claim that there are no additional risks related to robotic surgery because the evidence is nowhere to be found.
“Decisions should not be made based on the information in the FDA database,” he says. “We need to be able to give patients answers to their questions about safety and how much risk is associated with the robot. We have all suspected the answer has not been zero. We still don’t really know what the true answer is.”
We want to hear from you! Tell us what you think.
An app to help your patient lose weight
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
Inside Hospitalists' Evolving Scope of Practice
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
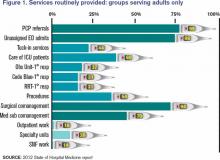
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
In the October 2012 issue of The Hospitalist, the “Survey Insights” article discussed hospitalists’ evolving scope of practice based on information published in the 2012 State of Hospital Medicine report. The report remains the most authoritative, comprehensive source of information about our rapidly developing specialty, and this important topic is worthy of continued attention.
As I begin to orient a new class of hospitalists in my own HM group (HMG), I emphasize the five S’s of HMGs: scope, salary, schedule, structure, and society. HMGs define who they are largely by these constructs. As a specialty, we will define who we are by how we develop these constructs as a community. And it may indeed be the scope that most confirms our identity.
The survey (www.hospitalmedicine.org/survey) paints a self-portrait: What do we see when we look at that image? Figure 1 (below) lists information about services routinely provided by hospitalists, and one could divide the findings into three general categories.
First and foremost, there is the core work. It is clear that virtually all HMGs attended to primary-care-physician referrals and unassigned ED hospitalizations, and they also served as at least consultants for surgical comanagement. Most HMGs are now doing medical subspecialty comanagement, and the data would indicate that we are admitting and attending many of these patients. This raises the question about whether our identity will morph to that of the “universal admitter.” Many contend that health-care change forces will continue to pressure in this direction unless, and until, medical subspecialties develop their own dedicated hospitalists. Many hospitals may not be able to resource this; hence, there will likely be persistent pressure for the HMGs to provide this scope of care.
Perhaps half of HMGs provide the second group of services, which includes primary clinical care for rapid-response teams, code blue teams, and observation units. Forty-four percent of adult hospitalist programs provide a “tuck-in” service (nighttime coverage for other providers), and about 50% of HMGs reported performing procedures. Although this graph might suggest a decline in the proportion of groups caring for ICU patients compared with the 78% that was reported in 2011, this data set includes academic practices (the 2011 data didn’t). For nonacademic adult medicine practices, the proportion doing ICU work actually rose to 83.5% in 2012 from 78% in 2011. Larger hospitals and university settings are increasingly employing intensivists for ICU coverage, but the national deficit of intensivists will likely continue the external pressure for hospitalists to provide ICU care in many settings.
The final group of services represents the “road less traveled”—work in outpatient settings in such specialty units as long-term acute care, psychiatric wings, and skilled nursing facilities. These might prove to be niche opportunities or possible distractions.
There remains, however, the core work that identifies our specialty. We all do it, people depend on us to have it done, and it largely defines who we are as individuals, as HMGs, and as the fastest-growing specialty in American medical history.
Dr. Landis is medical director of Wellspan Hospitalists in York, Pa., and a member of SHM’s Practice Analysis Committee.
Multiple Approaches to Combat High Hospital Patient Census
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
In this age of cost containment and fiscal frugality, how do you handle high-census periods without jeopardizing patient care?
–Michael P. Mason, Tulsa, Okla.
Dr. Hospitalist responds:
Your group must first define the term “high census,” because workload is based on many factors. Seeing 20 patients a day in a large inner-city hospital is much different from seeing 20 patients in a suburban hospital in an affluent part of town. Also, seeing 20 patients geographically located on the same floor is much easier than 20 patients spread all over the hospital. Mid-level or nurse case-management support also makes a difference.
Once defined, there are many different ways to handle the high census; each hospitalist group must decide what works for them.
Many groups rely on their compensation structure to entice their physicians to see higher numbers of patients. The pay structure may be production-based and entice many of the group members to see more patients. Typically, for the member that does not want to see the large volumes, there are usually colleagues who are more than happy to cover the excess patients.
Some groups employ a hybrid system, with their compensation based on production and salary. Generally, bonuses or incentives are applied after meeting a specific relative value unit (RVU) threshold. These thresholds vary and usually are raised periodically based on the percentage of staff able to collect. Again, some group members may volunteer to see the excess patients for higher compensation. It is up to the group to develop mechanisms to measure the quality of care of these high producers and monitor for burnout.
Then there are groups that have no volume incentives and everyone is paid a salary. Many groups that utilize any of these compensation models have group members “on call” to come in when needed and see the excess patients. Many pay the on-call person some nominal amount just for being on call, or a per-patient or hourly rate if they have to come in. Others make it a mandatory part of the schedule without any additional compensation.
Many groups have integrated advanced-practice providers (nurse practitioners and physician assistants) into their systems. They can help hospitalists improve efficiency by seeing patients that are less ill or awaiting placement, or by performing such labor-intensive tasks as admissions and discharges.
HM groups should collaborate with the hospital’s chief financial officer. Like clinicians, most administrators recognize it is very difficult to deliver high-quality and efficient care when the numbers get high. It is in their best interest to help devise strategies and models that deliver quality care and the metrics needed to sustain support.
HM has become such a large specialty that there is no-one-size-fits-all solution to high censuses. In the end, you have to be comfortable with the system created by your group, work to help improve it, or seek a better fit.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
Among Physicians, 59% Would Not Recommend a Medical Career
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
Percentage of practicing physicians who would not recommend a medical career to a young person, according to Filling The Void: 2013 Physician Outlook Practice Trends, a national physician practice survey conducted by health-care staffing firm Jackson Healthcare.6 “Physician discontent appears to be creating a void in the health-care field,” with dissatisfaction and burnout leading to early retirement, the report stated. Discontent is driven by decreased autonomy, decreased reimbursement, administrative and regulatory distractions, corporatization of medicine, and fear of litigation, according to the report. Thirty-six percent of the respondents reported a generally negative outlook about their career, compared with only 16% who had a generally favorable outlook.
Larry Beresford is a freelance writer in San Francisco.
References
- Hartocollis A. With money at risk, hospitals push staff to wash hands. The New York Times website. Available at: http://www.nytimes.com/2013/05/29/nyregion/hospitals-struggle-to-get-workers-to-wash-their-hands.html?pagewanted=all&_r=0. Accessed May 28, 2013.
- Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013 May 10 [Epub ahead of print].
- Bernhard B. High tech hand washing comes to St. Louis hospital. St. Louis Post-Dispatch website. Available at: http://www.stltoday.com/lifestyles/health-med-fit/health/high-tech-hand-washing-comes-to-st-louis-hospital/article_9379065d-85ff-5643-bae2-899254cb22fa.html. Accessed June 27, 2013.
- Lowe TJ, Partovian C, Kroch E, Martin J, Bankowitz R. Measuring cardiac waste: the Premier cardiac waste measures. Am J Med Qual. 2013 May 29 [Epub ahead of print].
- Elixhauser A, Steiner C. Readmissions to U.S. hospitals by diagnosis, 2010. Healthcare Cost and Utilization Project website. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Accessed July 15, 2013.
- Jackson Healthcare. Filling the void: 2013 physician outlook & practice trends. Jackson Healthcare website. Available at: http://www.jacksonhealthcare.com/media/193525/jc-2013physiciantrends-void_ebk0513.pdf. Accessed July 15, 2013.
MGMA Physician Compensation Survey Raises Questions About Performance Pay
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Sorting out whether a hospitalist’s bonus and other compensation elements are in line with survey data often leads to confusion. The 2013 MGMA Physician Compensation and Production Survey report, based on 2012 data, shows median compensation of $240,352 for internal-medicine hospitalists (I’ll round it to $240,000 for the rest of this piece). So is your compensation in line with survey medians if your base pay is $230,000 and you have a performance bonus of up to $20,000?
The problem is that you can’t know in advance how much of the $20,000 performance bonus you will earn. And isn’t a bonus supposed to be on top of typical compensation? To be in line with the survey, shouldn’t your base pay equal the $240,000 median, with any available bonus dollars on top of that? (Base pay means all forms of compensation other than a performance bonus; it could be productivity-based compensation, pay connected to numbers of shifts or hours worked, or a fixed annual salary, etc.)
The short answer is no, and to demonstrate why, I’ll first review some facts about the survey itself, then apply that knowledge to the hospitalist marketplace.
I want to emphasize that in this article, I’m not taking a position on the right amount of workload, compensation, or bonus for any hospitalist practice. And I’m using survey medians just to simplify the discussion, not because they’re optimal for any particular practice.
Survey Data
The most important thing to know about the survey data is that the $240,000 figure takes into account all forms of pay, including extra shift pay and any bonuses that might have been paid to each provider in the data set. Such benefits as health insurance and retirement-plan contribution are not included in this figure.
There are several ways a hospitalist might have earned compensation that matches the survey median. He or she might have a fixed annual salary equal to the median with no bonus available or had a meaningful bonus (e.g. $10,000 to $20,000) available and failed to earn any of it. Or the base might have come to $230,000, and he or she earned half of the available $20,000 performance bonus. Many other permutations of bonus and other salary elements could occur to arrive at the same $240,000 figure.
The important thing to remember is that whatever bonus dollars were paid, they are included in the salary figure from the survey—not added on top of that figure. So if all bonus dollars earned were subtracted from the survey, the total “nonbonus” compensation would be lower than $240,000.
How much lower?
Typical Hospitalist Bonus Amounts
The MGMA survey doesn’t report the portion of compensation tied to a bonus, but SHM’s does. SHM’s 2012 State of Hospital Medicine Report, based on 2011 data (www.hospitalmedicine.org/survey), is based on the most recent data available, and it showed (on page 60) that an average of 7% of pay was tied to performance for nonacademic hospitalist groups serving adults only. This included any payments for good individual or group performance on quality, efficiency, service, satisfaction, and/or other nonproduction measures. In conversation, this often is referred to as a “bonus” rather than “performance compensation.”
One way to estimate the nonbonus compensation would be to reduce the total pay by 7%, which comes to $223,200. Keep in mind that there are all kinds of mathematical and methodological problems in manipulating the reported survey numbers from two separate surveys to derive additional benchmarks. But this seems like a reasonable guess.
An increasing portion of hospitalist groups have some pay tied to performance, and the portion of total pay tied to performance seems to be going up at least a little. It was 5% of pay in 2010 and 4% in 2011, compared with 7% in the 2012 survey.
Keep in mind two things. First, this 7% reflects the performance or bonus dollars actually paid out, not the total amount available. In other words, even if the median total bonus dollars available were 20% of compensation, hospitalists earned less than that. Some hospitalists earned all dollars available, and some earned only a portion of what was available. And second, some hospitalists fail to earn any bonus or don’t have one available at all. So the survey would show for them zero compensation tied to bonus.
Making Sense of the Numbers
If you follow the reasoning above, then you probably agree that if your goal is to match mean compensation from the MGMA survey (I’m not suggesting that is the best goal, merely using it for simplicity), then you would set nonbonus compensation 7% below median—as long as you’re likely to get the same portion of a bonus as the median practice.
In some practices, performance thresholds are set at a level that is very easy to achieve, meaning the hospitalists are almost guaranteed to get all of the bonus compensation available. To be consistent with survey medians, it would be appropriate for them to set nonbonus compensation by subtracting all bonus dollars from the survey median. For example, if a $20,000 bonus is available and all of it is likely to be earned by the hospitalists, then total nonbonus compensation would be $220,000.
However, what if the bonus requires significant improvements in performance by the doctors (which seems most appropriate to me; why have a bonus otherwise?) and it is likely they will earn only 25% of all bonus dollars available? If the total available bonus is $20,000, then something like 25%, or $5,000, should be subtracted from the median to yield a total nonbonus compensation of $235,000.
Simple Thinking
I think it makes most sense to set total nonbonus compensation below the targeted total compensation. Failure to achieve any performance thresholds means no bonus and compensation will be below target that year. Meeting some thresholds (some improvement in performance) should result in matching the target compensation, and truly terrific performance that meets or exceeds all thresholds should result in the doctor being paid above the target.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Patient Satisfaction Surveys Not Accurate Measure of Hospitalists’ Performance
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
Feeling frustrated with your group’s patient-satisfaction performance? Wondering why your chief (fill in the blank) officer glazes over when you try to explain why your hospitalist group’s Hospital Consumer Assessment of Healthcare Providers and System (HCAHPS) scores for doctor communication are in a percentile rivaling the numeric age of your children?
It is likely that the C-suite administrator overseeing your hospitalist group has a portion of their pay based on HCAHPS or other patient-satisfaction (also called patient experience) scores. And for good reason: The Centers for Medicare & Medicaid Services (CMS) Hospital Value-Based Purchasing (HVBP) program that started Oct. 1, 2012, has placed your hospital’s Medicare reimbursement at risk based on its HCAHPS scores.
HVBP and Patient Satisfaction
Patient satisfaction will remain an important part of HVBP in the coming years. Table 1 (below) shows the domains that will be included in fiscal years 2014 (which starts Oct. 1, 2013), 2015, and 2016. Table 2 (below) depicts the percent weighting the patient-satisfaction domain will receive through 2016. You may recall that HVBP is a program in which all hospitals place 1% to 2% (2013 through 2017, starting at 1% and increasing each year by 0.25% so that by 2017%, it is 2%) of their CMS inpatient payments in a withhold pool and, based on performance, can make back some, all, or an amount in excess of the amount placed in the withhold pool.
Source: Federal Register Vol. 78, No. 91; May 10, 2013; Proposed Rules, pp. 27609-27622.
Source: Federal Register Vol.78, No.91; May 10, 2013; Proposed Rules, pp. 27609-27622.
End In Itself
A colleague of mine recently asked, “Is an increase in patient satisfaction associated with higher quality of care and better patient safety?” The point here: It doesn’t matter. Patient satisfaction is an end in itself, and we should strive to maximize it, or at least put ourselves in the place of the patient and design care accordingly.
For Hospitalists: A Starting Point
There is a conundrum for hospitalists vis-à-vis patient satisfaction. Follow this chain of logic: The hospitals at which we work are incented to perform well on the HCAHPS domains. Hospitals pay a lot for hospitalists. Hospitalists can impact many of the HCAHPS domains. So shouldn’t hospitalists be judged according to HCAHPS scores?
Yes and no.
HCAHPS as a survey is intended to measure a patient’s overall experience of receiving care in the hospital. For example, from the “Doctor Communication” domain, we have questions like “how often did doctors treat you with courtesy and respect?” And “how often did doctors explain things in a way you could understand?”
These questions, like all in HCAHPS, are not designed to get at individual doctor performance, or even performance of a group of doctors, such as hospitalists. Instead, they are designed to measure a patient’s overall experience with the hospitalization, and “Doctor Communication” questions are designed to assess satisfaction with “doctors” collectively.
The Need for Hospitalist-Specific Satisfaction Surveys
So while HCAHPS is not designed to measure hospitalist performance with regard to patient satisfaction, it is a reasonable interim step for hospitals to judge hospitalists according to HCAHPS. However, this should be a bridge to a strategy that adopts hospitalist-specific patient-satisfaction questionnaires in the future and not an end in itself.
Why? Perhaps the biggest reason is that HCAHPS scores are neither specific nor timely enough to form the basis of improvement efforts for hospitalists. If a hospitalist receives a low score on the “Doctor Communication” domain, the scores are likely to be three to nine months old. How can we legitimately assign (and then modify) behaviors based on those scores?
Further, because the survey is not built to measure patient satisfaction specifically with hospitalists, the results are unlikely to engender meaningful and sustained behavior change. Hospitalists I talk to are generally bewildered and confused by HCAHPS scores attributed to them or their groups. Even if they understand the scores, I almost never see true quality improvement (plan-do-study-act) based on specific HCAHPS results. Instead, I see hospitalists trying to adhere to “best practices,” with no adjustments made along the way based on performance.
Nearly all the prominent patient satisfaction vendors have developed a survey instrument specifically designed for hospitalists. Each has an approach to appropriately attribute performance to the hospitalist in question, and each has a battery of questions that is designed to capture patient satisfaction with the hospitalist. Although use of these surveys involves an added financial commitment, I submit that because hospitalists have an unparalleled proximity to hospitalized patients, such an investment is worthy of consideration and has an accompanying business case, thanks to HVBP. The results of these surveys may form the basis of legitimate, targeted feedback to hospitalists, who may then adjust their approach to patient interactions. Such performance improvement should result in improved HCAHPS scores.
In sum, hospitalists should pay close attention to patient satisfaction and embrace HCAHPS. However, we should be looking beyond HCAHPS to survey instruments that fairly and accurately measure our performance. Such surveys will be more widely accepted by the hospitalists they are measuring, and will allow hospitalists to perform meaningful quality improvement based on the results. Although hospitalist-specific surveys will require an investment, the increased patient satisfaction that results should be the basis of a favorable return on that investment.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
Pediatric Hospital Medicine Marks 10th Anniversary
With a record number of attendees, Pediatric Hospital Medicine 2013 (PHM) swept into New Orleans last month, carrying with it unbridled enthusiasm about the past, present, and future.
Virginia Moyer, MD, MPH, vice president for maintenance of certification and quality for the American Board of Pediatrics (ABP) and professor of pediatrics and chief of academic general pediatrics at Texas Children’s Hospital, delivered a keynote address to 700 attendees that focused on the challenges and opportunities of providing evidence-based, high-quality care in the hospital, as well as ABP’s role in meeting these challenges.
“If evidence-based medicine is an individual sport,” Dr. Moyer said, “then quality improvement is a team sport.”
Barriers to quality improvement (QI)— such as lack of will, lack of data, and lack of training—can be surmounted in a team environment, she said. ABP is continuing in its efforts to support QI education through its Maintenance of Certification (MOC) Part 4 modules, as well as other educational activities.
Other highlights of the 10th annual Pediatric Hospital Medicine meeting:
- The addition of a new “Community Hospitalists” track was given high marks by those in attendance. It covered such topics as perioperative management of medically complex pediatric patients, community-acquired pneumonia, and osteomyelitis.
- A 10-year retrospective of pediatric hospital medicine was given by a panel of notable pediatric hospitalists, including Erin Stucky Fisher, MD, FAAP, MHM, chief of hospital medicine at Rady Children’s Hospital in San Diego; Mary Ottolini, MD, MPH, chief of hospital medicine at Children’s National Medical Center in Washington; Jack Percelay, MD, MPH, FAAP, associate clinical professor at Pace University; and Daniel Rauch, MD, FAAP, pediatric hospitalist program director at the NYU School of Medicine in New York City. A host of new programs has been established by the PHM community, including the Quality Improvement Innovation Networks (QuIIN); the Value in Pediatrics (VIP) network; the International Network for Simulation-Based Pediatric Innovation, Research, and Education (INSPIRE); patient- and family-centered rounds; and the I-PASS Handoff Program. The panel also discussed future challenges, including reduction of unnecessary treatments, interfacing, and perhaps incorporating “hyphen hospitalists,” and learning from advances made by the adult HM community.
- The ever-popular “Top Articles in Pediatric Hospital Medicine” session was presented by H. Barrett Fromme, MD, associate professor of pediatrics at the University of Chicago, and Ben Bauer, MD, director of pediatric hospital medicine at Riley Hospital for Children at Indiana University Health in Indianapolis, which was met with raucous approval by the audience. The presentation not only educated those in attendance about the most cutting-edge pediatric literature, but it also included dance moves most likely to attract the opposite sex and clothing appropriate for the Australian pediatric hospitalist.
- The three presidents of the sponsoring societies—Thomas McInerney, MD, FAAP, of the American Academy of Pediatrics, David Keller, MD, of the Academic Pediatric Association, and Eric Howell, MD, SFHM, of SHM—presented each society’s contributions to the growth of PHM, as well as future areas for cooperative sponsorship. These include the development of the AAP Section of Hospital Medicine Library website (sohmlibrary.org), the APA Quality Scholars program, and SHM’s efforts to increase interest in hospital medicine in medical students and trainees. “Ask not what hospital medicine can do for you,” Dr. Howell implored, “ask what you can do for hospital medicine!”
- Members of the Joint Council of Pediatric Hospital Medicine (JCPHM) presented the recent recommendations of the council arising from an April 2013 meeting with the ABP in Chapel Hill, N.C. Despite acknowledgements that no decision will be met with uniform satisfaction by all the stakeholders, the JCPHM concluded that the path that would best advance the field of PHM, provide for high-quality care of hospitalized children, and ensure the public trust would be a two-year fellowship sponsored by ABP. This would ultimately lead to approved certification eligibility for fellowship graduates by the American Board of Medical Specialties (ABMS); it would also make provisions for “grandfathering” in current pediatric hospitalists. Concerns from med-peds, community hospitalists, and recent residency graduate communities were addressed by the panel.
- A recurrent theme of reducing unnecessary treatments, interventions, and, perhaps, hospitalizations was summarized eloquently by Alan Schroeder, MD, director of the pediatric ICU and chief of pediatric inpatient care at Santa Clara (Calif.) Valley Health. Barriers to reducing unnecessary care can be substantial, including pressure from families, pressure from colleagues, profit motive, and the “n’s of 1,” according to Dr. Schroeder. Ultimately, however, avoiding testing and treatments that have no benefit to children will improve care. “Ask, ‘How will this test benefit my patient?’ not ‘How will this test change management?’” Dr. Schroeder advised.
Dr. Chang is The Hospitalist’s pediatric editor and a med-peds-trained hospitalist working at the University of California San Diego and Rady Children’s Hospital.
With a record number of attendees, Pediatric Hospital Medicine 2013 (PHM) swept into New Orleans last month, carrying with it unbridled enthusiasm about the past, present, and future.
Virginia Moyer, MD, MPH, vice president for maintenance of certification and quality for the American Board of Pediatrics (ABP) and professor of pediatrics and chief of academic general pediatrics at Texas Children’s Hospital, delivered a keynote address to 700 attendees that focused on the challenges and opportunities of providing evidence-based, high-quality care in the hospital, as well as ABP’s role in meeting these challenges.
“If evidence-based medicine is an individual sport,” Dr. Moyer said, “then quality improvement is a team sport.”
Barriers to quality improvement (QI)— such as lack of will, lack of data, and lack of training—can be surmounted in a team environment, she said. ABP is continuing in its efforts to support QI education through its Maintenance of Certification (MOC) Part 4 modules, as well as other educational activities.
Other highlights of the 10th annual Pediatric Hospital Medicine meeting:
- The addition of a new “Community Hospitalists” track was given high marks by those in attendance. It covered such topics as perioperative management of medically complex pediatric patients, community-acquired pneumonia, and osteomyelitis.
- A 10-year retrospective of pediatric hospital medicine was given by a panel of notable pediatric hospitalists, including Erin Stucky Fisher, MD, FAAP, MHM, chief of hospital medicine at Rady Children’s Hospital in San Diego; Mary Ottolini, MD, MPH, chief of hospital medicine at Children’s National Medical Center in Washington; Jack Percelay, MD, MPH, FAAP, associate clinical professor at Pace University; and Daniel Rauch, MD, FAAP, pediatric hospitalist program director at the NYU School of Medicine in New York City. A host of new programs has been established by the PHM community, including the Quality Improvement Innovation Networks (QuIIN); the Value in Pediatrics (VIP) network; the International Network for Simulation-Based Pediatric Innovation, Research, and Education (INSPIRE); patient- and family-centered rounds; and the I-PASS Handoff Program. The panel also discussed future challenges, including reduction of unnecessary treatments, interfacing, and perhaps incorporating “hyphen hospitalists,” and learning from advances made by the adult HM community.
- The ever-popular “Top Articles in Pediatric Hospital Medicine” session was presented by H. Barrett Fromme, MD, associate professor of pediatrics at the University of Chicago, and Ben Bauer, MD, director of pediatric hospital medicine at Riley Hospital for Children at Indiana University Health in Indianapolis, which was met with raucous approval by the audience. The presentation not only educated those in attendance about the most cutting-edge pediatric literature, but it also included dance moves most likely to attract the opposite sex and clothing appropriate for the Australian pediatric hospitalist.
- The three presidents of the sponsoring societies—Thomas McInerney, MD, FAAP, of the American Academy of Pediatrics, David Keller, MD, of the Academic Pediatric Association, and Eric Howell, MD, SFHM, of SHM—presented each society’s contributions to the growth of PHM, as well as future areas for cooperative sponsorship. These include the development of the AAP Section of Hospital Medicine Library website (sohmlibrary.org), the APA Quality Scholars program, and SHM’s efforts to increase interest in hospital medicine in medical students and trainees. “Ask not what hospital medicine can do for you,” Dr. Howell implored, “ask what you can do for hospital medicine!”
- Members of the Joint Council of Pediatric Hospital Medicine (JCPHM) presented the recent recommendations of the council arising from an April 2013 meeting with the ABP in Chapel Hill, N.C. Despite acknowledgements that no decision will be met with uniform satisfaction by all the stakeholders, the JCPHM concluded that the path that would best advance the field of PHM, provide for high-quality care of hospitalized children, and ensure the public trust would be a two-year fellowship sponsored by ABP. This would ultimately lead to approved certification eligibility for fellowship graduates by the American Board of Medical Specialties (ABMS); it would also make provisions for “grandfathering” in current pediatric hospitalists. Concerns from med-peds, community hospitalists, and recent residency graduate communities were addressed by the panel.
- A recurrent theme of reducing unnecessary treatments, interventions, and, perhaps, hospitalizations was summarized eloquently by Alan Schroeder, MD, director of the pediatric ICU and chief of pediatric inpatient care at Santa Clara (Calif.) Valley Health. Barriers to reducing unnecessary care can be substantial, including pressure from families, pressure from colleagues, profit motive, and the “n’s of 1,” according to Dr. Schroeder. Ultimately, however, avoiding testing and treatments that have no benefit to children will improve care. “Ask, ‘How will this test benefit my patient?’ not ‘How will this test change management?’” Dr. Schroeder advised.
Dr. Chang is The Hospitalist’s pediatric editor and a med-peds-trained hospitalist working at the University of California San Diego and Rady Children’s Hospital.
With a record number of attendees, Pediatric Hospital Medicine 2013 (PHM) swept into New Orleans last month, carrying with it unbridled enthusiasm about the past, present, and future.
Virginia Moyer, MD, MPH, vice president for maintenance of certification and quality for the American Board of Pediatrics (ABP) and professor of pediatrics and chief of academic general pediatrics at Texas Children’s Hospital, delivered a keynote address to 700 attendees that focused on the challenges and opportunities of providing evidence-based, high-quality care in the hospital, as well as ABP’s role in meeting these challenges.
“If evidence-based medicine is an individual sport,” Dr. Moyer said, “then quality improvement is a team sport.”
Barriers to quality improvement (QI)— such as lack of will, lack of data, and lack of training—can be surmounted in a team environment, she said. ABP is continuing in its efforts to support QI education through its Maintenance of Certification (MOC) Part 4 modules, as well as other educational activities.
Other highlights of the 10th annual Pediatric Hospital Medicine meeting:
- The addition of a new “Community Hospitalists” track was given high marks by those in attendance. It covered such topics as perioperative management of medically complex pediatric patients, community-acquired pneumonia, and osteomyelitis.
- A 10-year retrospective of pediatric hospital medicine was given by a panel of notable pediatric hospitalists, including Erin Stucky Fisher, MD, FAAP, MHM, chief of hospital medicine at Rady Children’s Hospital in San Diego; Mary Ottolini, MD, MPH, chief of hospital medicine at Children’s National Medical Center in Washington; Jack Percelay, MD, MPH, FAAP, associate clinical professor at Pace University; and Daniel Rauch, MD, FAAP, pediatric hospitalist program director at the NYU School of Medicine in New York City. A host of new programs has been established by the PHM community, including the Quality Improvement Innovation Networks (QuIIN); the Value in Pediatrics (VIP) network; the International Network for Simulation-Based Pediatric Innovation, Research, and Education (INSPIRE); patient- and family-centered rounds; and the I-PASS Handoff Program. The panel also discussed future challenges, including reduction of unnecessary treatments, interfacing, and perhaps incorporating “hyphen hospitalists,” and learning from advances made by the adult HM community.
- The ever-popular “Top Articles in Pediatric Hospital Medicine” session was presented by H. Barrett Fromme, MD, associate professor of pediatrics at the University of Chicago, and Ben Bauer, MD, director of pediatric hospital medicine at Riley Hospital for Children at Indiana University Health in Indianapolis, which was met with raucous approval by the audience. The presentation not only educated those in attendance about the most cutting-edge pediatric literature, but it also included dance moves most likely to attract the opposite sex and clothing appropriate for the Australian pediatric hospitalist.
- The three presidents of the sponsoring societies—Thomas McInerney, MD, FAAP, of the American Academy of Pediatrics, David Keller, MD, of the Academic Pediatric Association, and Eric Howell, MD, SFHM, of SHM—presented each society’s contributions to the growth of PHM, as well as future areas for cooperative sponsorship. These include the development of the AAP Section of Hospital Medicine Library website (sohmlibrary.org), the APA Quality Scholars program, and SHM’s efforts to increase interest in hospital medicine in medical students and trainees. “Ask not what hospital medicine can do for you,” Dr. Howell implored, “ask what you can do for hospital medicine!”
- Members of the Joint Council of Pediatric Hospital Medicine (JCPHM) presented the recent recommendations of the council arising from an April 2013 meeting with the ABP in Chapel Hill, N.C. Despite acknowledgements that no decision will be met with uniform satisfaction by all the stakeholders, the JCPHM concluded that the path that would best advance the field of PHM, provide for high-quality care of hospitalized children, and ensure the public trust would be a two-year fellowship sponsored by ABP. This would ultimately lead to approved certification eligibility for fellowship graduates by the American Board of Medical Specialties (ABMS); it would also make provisions for “grandfathering” in current pediatric hospitalists. Concerns from med-peds, community hospitalists, and recent residency graduate communities were addressed by the panel.
- A recurrent theme of reducing unnecessary treatments, interventions, and, perhaps, hospitalizations was summarized eloquently by Alan Schroeder, MD, director of the pediatric ICU and chief of pediatric inpatient care at Santa Clara (Calif.) Valley Health. Barriers to reducing unnecessary care can be substantial, including pressure from families, pressure from colleagues, profit motive, and the “n’s of 1,” according to Dr. Schroeder. Ultimately, however, avoiding testing and treatments that have no benefit to children will improve care. “Ask, ‘How will this test benefit my patient?’ not ‘How will this test change management?’” Dr. Schroeder advised.
Dr. Chang is The Hospitalist’s pediatric editor and a med-peds-trained hospitalist working at the University of California San Diego and Rady Children’s Hospital.
Medicare Penalties Make Hospital-Acquired-Infection Solutions a Priority
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
A shift in governmental regulations regarding reimbursement for hospital-acquired infections (HAIs) is forcing hospitals to take a closer look at how to reduce them. A recent study in Infection Control and Hospital Epidemiology shows that copper-alloy surfaces may be one such solution.3 According to the study, although only 9% of the touch surfaces in each ICU were replaced with copper components, there were 58% fewer HAI cases.1
“Before these regulations, hospitals didn’t necessarily want technology to decrease HAI rates, because the more infections and complications, the longer the length of patient stay, the greater the reimbursement, and the better the bottom line,” says Archelle Georgiou, MD, president of Georgiou Consulting LLC in Minneapolis and an advisor to the Copper Development Association.
Three regulations that have resulted in reimbursements to hospitals getting cut include:
- The Deficit Reduction Act of 2005, which was implemented on Oct. 1, 2008, which states that Medicare will not reimburse for certain types of HAIs;
- Section 3025 of the Affordable Care Act (signed into law in 2010), which incentivizes hospitals to decrease their readmission rates, which frequently are caused by HAIs. Beginning this fall, hospitals are getting reduced reimbursement when their readmission rates exceed a certain threshold. The maximum penalty in 2013 is 1% and will increase to 3% by 2015; and
- Section 1886 of the Affordable Care Act, which describes value-based purchasing and makes hospitals eligible to receive incentive payments for achieving better care on certain quality metrics. Funding for the program comes from withholding payment from poor-performing hospitals. The financial impact to hospitals started this year. In 2014, urinary tract infections and vascular-catheter-associated infections will be among the targeted conditions measured by CMS to calculate incentives and penalties.
“Hospitals are now feeling a direct impact from all of this,” Dr. Georgiou says. “Back in 2008, hospitals were noticing, but it was hard to get their attention since only one program was impacting their bottom line. But, pretty soon, hospitals risk losing upwards of 5% of their Medicare reimbursement for decreased quality.
“Reducing HAIs is clearly on the priority list of chief operating officers. They are very aware of the impact to their bottom line. They are looking to their vendors and suppliers to develop strategies to work with their hospitals to improve performance around these metrics.”
Karen Appold is a freelance writer in Pennsylvania.
Ill-advised genetic counseling: $1M verdict
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A mother had given birth to two children with thalamic abnormalities that resulted in seizures, developmental delays, and death. Before getting pregnant again, the parents sought genetic counseling and were told that identifying the specific defective gene would be impossible. The geneticist advised them that a child conceived with a donor egg and father’s sperm would have essentially the same risk as the general population. The parents asked in writing if it would be safer to
use both donor egg and donor sperm; the geneticist responded that the difference in risk was negligible.
The mother gave birth in June 2007 to a child conceived with a donated egg and the father’s sperm. After the child began to show the same symptoms as the others, an MRI of the child’s brain revealed a thalamic abnormality, and testing revealed Alpers syndrome caused by POLG gene mutations. The third child died in September 2008.
PARENTS’ CLAIM The chances of having a child with Alpers syndrome are
about 1:200,000 in the general population; if one parent is a known carrier, the chance is 1:1,000. If the parents had known this risk, they would have used donor egg and donor sperm to conceive or adopted. They were not told about Alpers syndrome and its relationship to the POLG gene until after their third child was born. The geneticist was negligent in failing to provide this information.
PHYSICIAN’S DEFENSE The parents received appropriate and accurate genetic counseling.
VERDICT A $1 million Florida verdict was returned.
What caused a delay in breast cancer diagnosis?
A 39-year-old woman underwent mammography in October 2004. After recommending a spotcompression film of a left-breast lesion, and then ultrasonography, the radiologist concluded that the lesion was benign, and suggested a 1-year follow-up. Reports were sent to the patient and her primary care physician.
In August 2006, when mammography was suspicious for breast cancer, a biopsy diagnosed infiltrating ductal carcinoma of the left breast. After undergoing a mastectomy, radiation therapy, and chemotherapy, the patient was cancer-free at the time of the trial.
patient’s CLAIM The radiologist failed to properly interpret the 2004 mammography.
physician’s DEFENSE The radiologist’s interpretations of the 2004 tests were correct. The patient failed to follow up in 1 year, as recommended, and this delayed the cancer diagnosis. The patient’s survival indicated that she had been cured of her breast cancer.
VERDICT A confidential settlement was reached with the hospital before the trial. An Illinois defense verdict was returned for the radiologist.
Heparin overdose for preemie
At 27 weeks' gestation, a woman went to a clinic with preeclampsia. After she was stabilized, the baby was born by emergency cesarean delivery.
At birth, the baby was thrombocytopenic (platelet count, 37,000/mL) with a heart rate of 60 bpm. The child’s cord blood pH was 7.27, indicating no significant hypoxia. At 1 minute of life, the child’s heart rate had not improved. After trying three times to place an endotracheal tube, chest compressions were begun at 10 minutes of life. An umbilical vein catheter (UVC) was placed at 22 minutes. Heparin was used to flush the UVC. After 40 minutes, the baby’s pH was 6.88, indicating severe acidosis. The infant was transferred to another hospital 3 hours after birth.
Head ultrasonography at 5 days of life revealed hemorrhagic and ischemic changes in the baby’s brain. The child suffered massive brain damage, is ventilator-dependent, and has a G-tube for feeding. She cannot sit up, walk, or speak, and will require specialized care for life.
Parent's claim Emergency resuscitation was not performed at birth: the low heart rate and thrombocytopenia were not treated; the UVC was not immediately placed. Twice, adult doses of heparin were used instead of normal saline to flush the UVC; heparin caused bleeding in the baby’s brain.
Defendant's Defense The case was settled during trial.
Verdict A $3 million Maryland settlement was reached.
Uterine rupture: $130M verdict
After a woman's first child was born by cesarean delivery, vaginal birth after cesarean (VBAC) was planned for her second pregnancy. When a nurse recognized a ruptured uterus, the ObGyn ordered a cesarean delivery. The newborn suffered severe brain damage, with seizures. She has cerebral palsy with near-normal intelligence, but cannot talk or walk and continues to have seizures.
Parents' claim The baby’s injuries occurred due to a failure to respond to fetal distress. When the intrauterine pressure catheter (IUPC) stopped working for 27 minutes, the nurse did not notify the ObGyn or apply an external monitor. Fetal heart decelerations occurred, including a prolonged deceleration for 3 minutes; the nurse did not notify the ObGyn, reposition the mother, provide oxygen and extra fluids, or discontinue oxytocin. A cesarean delivery should have occurred 30 to 60 minutes earlier.
Defendants' defense The fetal heart rates were what typically occur during the second stage of labor. The hospital’s accepted practices were followed. When the IUPC failed, the nurse measured contractions by hand and analyzed the fetal heartbeat from audible sounds; therefore, it was not necessary to notify the ObGyn. The physician was promptly called when uterine rupture was suspected. Uterine rupture and placental abruption caused the child’s injury. Uterine rupture cannot be predicted or prevented and is a known complication of VBAC.
Verdict After the parents declined an $8 million settlement, the matter was tried to a defense verdict. That decision was overturned on appeal, and, at a second trial, a $130 million New York verdict was returned against the hospital that employed the ObGyn and nurse.
Uterus, small bowel injured during D&C
A 65-year-old woman underwent dilation and curettage (D&C) to screen for uterine cancer performed by an ObGyn and a general surgeon. Her uterus and small intestine were perforated during the procedure, and a second operation was required to repair the damage.
Patient's claim Both physicians were negligent in performing D&C.
Physician's defense The ObGyn denied negligence and countered that the injuries are known complications of the procedure.
Verdict The surgeon settled for a confidential amount before trial. A New Jersey defense verdict was returned for the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.