User login
Sprout Pregnancy Essentials
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
Review your insurance
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Dermatology News.
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Dermatology News.
Insurance – so goes the hoary cliché – is the one product you buy hoping never to use. While no one enjoys foreseeing unforeseeable calamities, regular meetings with your insurance broker are important. Overinsuring is a waste of money, but underinsuring can prove even more costly, should the unforeseeable happen.
Malpractice premiums continue to rise. If yours are getting out of hand, ask your broker about alternatives.
"Occurrence" policies remain the coverage of choice where they are available and affordable, but they are becoming an endangered species as fewer insurers are willing to write them. "Claims-made" policies are usually cheaper, and provide the same coverage as long as you remain in practice. You will need "tail" coverage against belated claims after you retire, but many companies provide free tail coverage after you’ve been insured for a minimum period (usually 5 years).
Other alternatives are gaining popularity as the demand for more reasonably priced insurance increases. The most common, known as reciprocal exchanges, are very similar to traditional insurers, but differ in certain aspects of funding and operations. For example, most exchanges require policyholders to make capital contributions in addition to payment of premiums, at least in their early stages. You get your investment back, with interest, when (if) the exchange becomes solvent.
Another option, called a captive, is an insurance company formed by several noninsurance entities (such as medical practices) to write their own insurance policies. All participants are shareholders, and all premiums (less administrative expenses) go toward building the security of the captive. Most captives purchase reinsurance to protect against catastrophic losses. If all goes well, individual owners sell their shares at retirement for a nice profit, which has grown tax free in the interim.
Risk Retention Groups (RRGs) are a combination of exchanges and captives, in that capital investments are usually required, and the owners are the insureds themselves; but all responsibility for management and adequate funding falls on the insureds’ shoulders, and reinsurance is rarely an option. Most medical malpractice RRGs are licensed in Vermont or South Carolina, because of favorable laws in those states, but they can be based in any state that allows them.
Exchanges, captives, and RRGs all carry risk: A few large claims can eat up all the profits, and may even put you in a financial hole. But of course, traditional malpractice policies offer zero profit opportunity.
If your financial situation has changed since your last insurance review, your life insurance needs have probably changed, too. As your retirement savings accumulate, less insurance is necessary. And if you own any expensive whole life policies, you can probably convert them to much cheaper term insurance.
Disability insurance is not something to skimp on, but if you are approaching retirement age, you may be able to decrease your coverage, or even eliminate it entirely, if your retirement plan is far enough along.
Liability insurance is likewise no place to pinch pennies, but you might be able to add an umbrella policy providing comprehensive catastrophic coverage, which may allow you to decrease your regular coverage, or raise your deductible limits.
One additional policy to consider is Employment Practices Liability Insurance, which protects you from lawsuits brought by militant or disgruntled employees. More on that next month.
Health insurance premiums continue to soar; Obamacare might offer a favorable alternative for your office policy. Open enrollment began Oct. 1, with coverage scheduled to begin Jan. 1, 2014. If you are considering such an option, go to the Center for Consumer Information and Insurance Oversight and pick a plan for your employees to enroll in.
Workers’ compensation insurance is mandatory in most states, and heavily regulated, so there is little room for cutting expenses. However, some states do not require you, as the employer, to cover yourself, and eliminating that coverage could save you a substantial amount. This is only worth considering, of course, if you have adequate health and disability policies in place.
If you’re over 50 years old, look into long-term care insurance as well. It’s relatively inexpensive if you buy it while you’re still healthy, and it could save you and your heirs a load of money on the other end. If you have shouldered the expense of a chronically ill parent or grandparent, you know what I’m talking about.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J., and has been a long-time monthly columnist for Dermatology News.
The Why and How Data Mining Is Applicable to Hospital Medicine
Click here to listen to excerpts of our interview with Dr. Deitelzweig, chair of SHM’s Practice Analysis Committee.
Click here to listen to excerpts of our interview with Dr. Deitelzweig, chair of SHM’s Practice Analysis Committee.
Click here to listen to excerpts of our interview with Dr. Deitelzweig, chair of SHM’s Practice Analysis Committee.
MGMA Surveys Make Hospitalists' Productivity Hard to Assess
The Medical Group Management Association (MGMA) surveys regard both a doctor who works the standard number of annual shifts their practice defines as full time, and a doctor who works many extra shifts, as one full-time equivalent (FTE). This can cause confusion when assessing productivity per FTE (see “SHM and MGMA Survey History,” right).
For example, consider a hospitalist who generated 4,000 wRVUs while working 182 shifts—the standard number of shifts to be full time in that doctor’s practice—during the survey year. In the same practice, another hospitalist worked 39 extra shifts over the same year for a total of 220 shifts, generating 4,860 wRVUs. If the survey contained only these two doctors, it would show them both as full time, with an average productivity per FTE of 4,430 wRVUs. But that would be misleading because 1.0 FTE worth of work as defined by their practice for both doctors would have come to 4,000 wRVUs generated while working 182 shifts.
In prior columns, I’ve highlighted some other numbers in hospitalist productivity and compensation surveys that can lead to confusion. But the MGMA survey methodology, which assigns a particular FTE to a single doctor, may be the most confusing issue, potentially leading to meaningful misunderstandings.
More Details on FTE Definition
MGMA has been conducting physician compensation and productivity surveys across essentially all medical specialties for decades. Competing organizations conduct similar surveys, but most regard the MGMA survey as the most relevant and valuable.
For a long time, MGMA has regarded as “full time” any doctor working 0.75 FTE or greater, using the respondent practice’s definition of an FTE. No single doctor can ever be counted as more than 1.0 FTE, regardless of how much extra the doctor may have worked. Any doctor working 0.35-0.75 FTE is regarded as part time, and those working less than 0.35 FTE are excluded from the survey report. The fact that each practice might have a different definition of what constitutes an FTE is addressed by having a large number of respondents in most medical specialties.
I’m uncertain how MGMA ended up not counting any single doctor as more than 1.0 FTE, even when they work a lot of extra shifts. But my guess is that for the first years, or even decades, that MGMA conducted its survey, few, if any, medical practices even had a strict definition of what constituted 1.0 FTE and simply didn’t keep track of which doctors worked extra shifts or days. So even if MGMA had wanted to know, for example, when a doctor worked extra shifts and should be counted as more than 1.0 FTE, few if any practices even thought about the precise number of shifts or days worked constituting full time versus what was an “extra” shift. So it probably made sense to simply have two categories: full time and part time.
As more practices began assigning FTE with greater precision, like nearly all hospitalist practices do, then using 0.75 FTE to separate full time and part time seemed practical, though imprecise. But keep in mind it also means that all of the doctors who work from 0.75 to 0.99 FTE (that is, something less than 1.0) offset, at least partially, those who work lots of extra shifts (i.e., above 1.0 FTE).
Data Application
My anecdotal experience is that a large portion of hospitalists, probably around half, work more shifts than what their practice regards as full time. I don’t know of any survey database that quantifies this, but my guess is that 25% to 35% of full-time hospitalists work extra shifts at their own practice, and maybe another 15% to 20% moonlight at a different practice. Let’s consider only those in the first category.
Chronic staffing shortages is one of the reasons hospitalists so commonly work extra shifts at their own practice. Extra shifts are sometimes even required by the practice to make up for open positions. And in some places, the hospitalists choose not to fill positions to preserve their ability to continue working more than the number of shifts required to be full time.
It would be great if we had a precise way to adjust the MGMA survey data for hospitalists who work above 1.0 FTE. For example, let’s make three assumptions so that we can then adjust the reported compensation and productivity data to remove the effect of the many doctors working extra shifts, thereby more clearly matching 1.0 FTE. These numbers are my guesses based on lots of anecdotal experience. But they are only guesses. Don’t make too much of them.
Assume 25% of hospitalists nationally work an average of 20% more than the full-time number of shifts for their practice. That is my best guess and intentionally leaves out those who moonlight for a practice other than their own.
Some portion of those working extra shifts (above 1.0 FTE) is offset by survey respondents working between 0.75 and 1.0 FTE, resulting in a wild guess of a net 20% of hospitalists working extra shifts.
Last, let’s assume that their productivity and compensation on extra shifts is identical to their “normal” shifts. This is not true for many practices, but when aggregating the data, it is probably reasonably close.
Using these assumptions (guesses, really), we can decrease both the reported survey mean and median productivity and compensation by about 5% to more accurately reflect results for hospitalists doing only the number of shifts required by the practice to be full time—no extra shifts. I’ll spare you the simple math showing how I arrived at the approximately 5%, but basically it is removing the 20% additional compensation and productivity generated by the net 20% of hospitalists who work extra shifts above 1.0 FTE.
Does It Really Matter?
The whole issue of hospitalists working many extra shifts yet only counting as 1.0 FTE in the MGMA survey might matter a lot for some, and others might see it as useless hand-wringing. As long as a meaningful number of hospitalists work extra shifts, then survey values for productivity and compensation will always be a little higher than the “average” 1.0 FTE hospitalists working no extra shifts. But it may still be well within the range of error of the survey anyway. And the compensation per unit of work (wRVUs or encounters) probably isn’t much affected by this FTE issue.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
The Medical Group Management Association (MGMA) surveys regard both a doctor who works the standard number of annual shifts their practice defines as full time, and a doctor who works many extra shifts, as one full-time equivalent (FTE). This can cause confusion when assessing productivity per FTE (see “SHM and MGMA Survey History,” right).
For example, consider a hospitalist who generated 4,000 wRVUs while working 182 shifts—the standard number of shifts to be full time in that doctor’s practice—during the survey year. In the same practice, another hospitalist worked 39 extra shifts over the same year for a total of 220 shifts, generating 4,860 wRVUs. If the survey contained only these two doctors, it would show them both as full time, with an average productivity per FTE of 4,430 wRVUs. But that would be misleading because 1.0 FTE worth of work as defined by their practice for both doctors would have come to 4,000 wRVUs generated while working 182 shifts.
In prior columns, I’ve highlighted some other numbers in hospitalist productivity and compensation surveys that can lead to confusion. But the MGMA survey methodology, which assigns a particular FTE to a single doctor, may be the most confusing issue, potentially leading to meaningful misunderstandings.
More Details on FTE Definition
MGMA has been conducting physician compensation and productivity surveys across essentially all medical specialties for decades. Competing organizations conduct similar surveys, but most regard the MGMA survey as the most relevant and valuable.
For a long time, MGMA has regarded as “full time” any doctor working 0.75 FTE or greater, using the respondent practice’s definition of an FTE. No single doctor can ever be counted as more than 1.0 FTE, regardless of how much extra the doctor may have worked. Any doctor working 0.35-0.75 FTE is regarded as part time, and those working less than 0.35 FTE are excluded from the survey report. The fact that each practice might have a different definition of what constitutes an FTE is addressed by having a large number of respondents in most medical specialties.
I’m uncertain how MGMA ended up not counting any single doctor as more than 1.0 FTE, even when they work a lot of extra shifts. But my guess is that for the first years, or even decades, that MGMA conducted its survey, few, if any, medical practices even had a strict definition of what constituted 1.0 FTE and simply didn’t keep track of which doctors worked extra shifts or days. So even if MGMA had wanted to know, for example, when a doctor worked extra shifts and should be counted as more than 1.0 FTE, few if any practices even thought about the precise number of shifts or days worked constituting full time versus what was an “extra” shift. So it probably made sense to simply have two categories: full time and part time.
As more practices began assigning FTE with greater precision, like nearly all hospitalist practices do, then using 0.75 FTE to separate full time and part time seemed practical, though imprecise. But keep in mind it also means that all of the doctors who work from 0.75 to 0.99 FTE (that is, something less than 1.0) offset, at least partially, those who work lots of extra shifts (i.e., above 1.0 FTE).
Data Application
My anecdotal experience is that a large portion of hospitalists, probably around half, work more shifts than what their practice regards as full time. I don’t know of any survey database that quantifies this, but my guess is that 25% to 35% of full-time hospitalists work extra shifts at their own practice, and maybe another 15% to 20% moonlight at a different practice. Let’s consider only those in the first category.
Chronic staffing shortages is one of the reasons hospitalists so commonly work extra shifts at their own practice. Extra shifts are sometimes even required by the practice to make up for open positions. And in some places, the hospitalists choose not to fill positions to preserve their ability to continue working more than the number of shifts required to be full time.
It would be great if we had a precise way to adjust the MGMA survey data for hospitalists who work above 1.0 FTE. For example, let’s make three assumptions so that we can then adjust the reported compensation and productivity data to remove the effect of the many doctors working extra shifts, thereby more clearly matching 1.0 FTE. These numbers are my guesses based on lots of anecdotal experience. But they are only guesses. Don’t make too much of them.
Assume 25% of hospitalists nationally work an average of 20% more than the full-time number of shifts for their practice. That is my best guess and intentionally leaves out those who moonlight for a practice other than their own.
Some portion of those working extra shifts (above 1.0 FTE) is offset by survey respondents working between 0.75 and 1.0 FTE, resulting in a wild guess of a net 20% of hospitalists working extra shifts.
Last, let’s assume that their productivity and compensation on extra shifts is identical to their “normal” shifts. This is not true for many practices, but when aggregating the data, it is probably reasonably close.
Using these assumptions (guesses, really), we can decrease both the reported survey mean and median productivity and compensation by about 5% to more accurately reflect results for hospitalists doing only the number of shifts required by the practice to be full time—no extra shifts. I’ll spare you the simple math showing how I arrived at the approximately 5%, but basically it is removing the 20% additional compensation and productivity generated by the net 20% of hospitalists who work extra shifts above 1.0 FTE.
Does It Really Matter?
The whole issue of hospitalists working many extra shifts yet only counting as 1.0 FTE in the MGMA survey might matter a lot for some, and others might see it as useless hand-wringing. As long as a meaningful number of hospitalists work extra shifts, then survey values for productivity and compensation will always be a little higher than the “average” 1.0 FTE hospitalists working no extra shifts. But it may still be well within the range of error of the survey anyway. And the compensation per unit of work (wRVUs or encounters) probably isn’t much affected by this FTE issue.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
The Medical Group Management Association (MGMA) surveys regard both a doctor who works the standard number of annual shifts their practice defines as full time, and a doctor who works many extra shifts, as one full-time equivalent (FTE). This can cause confusion when assessing productivity per FTE (see “SHM and MGMA Survey History,” right).
For example, consider a hospitalist who generated 4,000 wRVUs while working 182 shifts—the standard number of shifts to be full time in that doctor’s practice—during the survey year. In the same practice, another hospitalist worked 39 extra shifts over the same year for a total of 220 shifts, generating 4,860 wRVUs. If the survey contained only these two doctors, it would show them both as full time, with an average productivity per FTE of 4,430 wRVUs. But that would be misleading because 1.0 FTE worth of work as defined by their practice for both doctors would have come to 4,000 wRVUs generated while working 182 shifts.
In prior columns, I’ve highlighted some other numbers in hospitalist productivity and compensation surveys that can lead to confusion. But the MGMA survey methodology, which assigns a particular FTE to a single doctor, may be the most confusing issue, potentially leading to meaningful misunderstandings.
More Details on FTE Definition
MGMA has been conducting physician compensation and productivity surveys across essentially all medical specialties for decades. Competing organizations conduct similar surveys, but most regard the MGMA survey as the most relevant and valuable.
For a long time, MGMA has regarded as “full time” any doctor working 0.75 FTE or greater, using the respondent practice’s definition of an FTE. No single doctor can ever be counted as more than 1.0 FTE, regardless of how much extra the doctor may have worked. Any doctor working 0.35-0.75 FTE is regarded as part time, and those working less than 0.35 FTE are excluded from the survey report. The fact that each practice might have a different definition of what constitutes an FTE is addressed by having a large number of respondents in most medical specialties.
I’m uncertain how MGMA ended up not counting any single doctor as more than 1.0 FTE, even when they work a lot of extra shifts. But my guess is that for the first years, or even decades, that MGMA conducted its survey, few, if any, medical practices even had a strict definition of what constituted 1.0 FTE and simply didn’t keep track of which doctors worked extra shifts or days. So even if MGMA had wanted to know, for example, when a doctor worked extra shifts and should be counted as more than 1.0 FTE, few if any practices even thought about the precise number of shifts or days worked constituting full time versus what was an “extra” shift. So it probably made sense to simply have two categories: full time and part time.
As more practices began assigning FTE with greater precision, like nearly all hospitalist practices do, then using 0.75 FTE to separate full time and part time seemed practical, though imprecise. But keep in mind it also means that all of the doctors who work from 0.75 to 0.99 FTE (that is, something less than 1.0) offset, at least partially, those who work lots of extra shifts (i.e., above 1.0 FTE).
Data Application
My anecdotal experience is that a large portion of hospitalists, probably around half, work more shifts than what their practice regards as full time. I don’t know of any survey database that quantifies this, but my guess is that 25% to 35% of full-time hospitalists work extra shifts at their own practice, and maybe another 15% to 20% moonlight at a different practice. Let’s consider only those in the first category.
Chronic staffing shortages is one of the reasons hospitalists so commonly work extra shifts at their own practice. Extra shifts are sometimes even required by the practice to make up for open positions. And in some places, the hospitalists choose not to fill positions to preserve their ability to continue working more than the number of shifts required to be full time.
It would be great if we had a precise way to adjust the MGMA survey data for hospitalists who work above 1.0 FTE. For example, let’s make three assumptions so that we can then adjust the reported compensation and productivity data to remove the effect of the many doctors working extra shifts, thereby more clearly matching 1.0 FTE. These numbers are my guesses based on lots of anecdotal experience. But they are only guesses. Don’t make too much of them.
Assume 25% of hospitalists nationally work an average of 20% more than the full-time number of shifts for their practice. That is my best guess and intentionally leaves out those who moonlight for a practice other than their own.
Some portion of those working extra shifts (above 1.0 FTE) is offset by survey respondents working between 0.75 and 1.0 FTE, resulting in a wild guess of a net 20% of hospitalists working extra shifts.
Last, let’s assume that their productivity and compensation on extra shifts is identical to their “normal” shifts. This is not true for many practices, but when aggregating the data, it is probably reasonably close.
Using these assumptions (guesses, really), we can decrease both the reported survey mean and median productivity and compensation by about 5% to more accurately reflect results for hospitalists doing only the number of shifts required by the practice to be full time—no extra shifts. I’ll spare you the simple math showing how I arrived at the approximately 5%, but basically it is removing the 20% additional compensation and productivity generated by the net 20% of hospitalists who work extra shifts above 1.0 FTE.
Does It Really Matter?
The whole issue of hospitalists working many extra shifts yet only counting as 1.0 FTE in the MGMA survey might matter a lot for some, and others might see it as useless hand-wringing. As long as a meaningful number of hospitalists work extra shifts, then survey values for productivity and compensation will always be a little higher than the “average” 1.0 FTE hospitalists working no extra shifts. But it may still be well within the range of error of the survey anyway. And the compensation per unit of work (wRVUs or encounters) probably isn’t much affected by this FTE issue.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
New Rules for Value-Based Purchasing, Readmission Penalties, Admissions
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
October is the beginning of a new year—in this case, fiscal-year 2014 for the Centers for Medicare & Medicaid Services (CMS). It’s a time when the new rules kick in. This month, we’ll look at some highlights, focusing on the new developments affecting your practice. Because you are held accountable for hospital-side performance on programs such as hospital value-based purchasing (HVBP) and the Readmissions Reduction Program, a working knowledge of the 2014 edition of the programs is crucial.
Close the Loop on HVBP
How will your hospital get paid under the 2014 version of HVBP? This past July, your hospital received a report outlining how its Medicare payments will be affected based on your hospital’s performance on process of care (heart failure, pneumonia, myocardial infarction, and surgery), patient experience (HCAHPS), and outcomes (30-day mortality for heart failure, pneumonia, and myocardial infarction).
Here are two hypothetical hospitals and how their performance in the program affects their 2014 payment. As background, in 2014, all hospitals have their base diagnosis related group (DRG) payments reduced by 1.25% for HVBP. They can earn back some, all, or an amount in excess of the 1.25% based on their performance. Payment is based on performance during the April 1 to Dec. 31, 2012, period. Under HVBP, CMS incentive payments occur at the level of individual patients, each of which is assigned a DRG.
Let’s look at two examples:
Hospital 1
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.48%.
- Net change in base DRG payment: +0.23%.
Hospital 2
- Base DRG payment reduction: 1.25% (all hospitals).
- Portion of base DRG earned back based on performance (process/patient experience/outcome metrics): 1.08%.
- Net change in base DRG payment: -0.17%.
Hospital 1 performed relatively well, getting a bump of 0.23% in its base DRG rate. Hospital 2 did not perform so well, so it took a 0.17% hit on its base DRG rate.
In order to determine total dollars made or lost for your hospital, one multiplies the total number of eligible Medicare inpatients for 2014 times the base DRG payment times the percent change in base DRG payment. If Hospital 1 has 10,000 eligible patients in 2014 and a base DRG payment of $5,000, the value is 10,000 x $5,000 x 0.0023 (0.23%) = $115,000 gained. Hospital 2, with the same number of patients and base DRG payment, loses (10,000 x $5,000 x 0.0017 = $85,000).
Readmissions and Penalties
For 2014, CMS is adding 30-day readmissions for COPD to readmissions for heart failure, pneumonia, and myocardial infarction for its penalty program. CMS added COPD because it is the fourth-leading cause of readmissions, according to a recent Medicare Payment Advisory Commission report, and because there is wide variation in the rates (from 18% to 25%) of COPD hospital readmissions.
For 2014, CMS raises the ceiling on readmission penalties to a maximum of 2% of reimbursement for all of a hospital’s Medicare inpatients. (The maximum hit during the first round of readmission penalties, which began in October 2012, was 1%.) More than 2,200 U.S. hospitals will face some financial penalty for excess 30-day readmissions.
Disappointingly, CMS did not add a risk adjustment for socioeconomic status despite being under pressure to do so. There is growing evidence that these factors have a major impact on readmission rates.1,2
New Definition of an Admission
Amidst confusion from many and major blowback from beneficiaries saddled with large out-of-pocket expenses for observation stays and subsequent skilled-nursing-facility stays, CMS is clarifying the definition of an inpatient admission. The agency will define an admission as a hospital stay that spans at least two midnights. If a patient is in the hospital for a shorter period of time, CMS will deem the patient to be on observation status, unless medical record documentation supports a physician’s expectation “that the beneficiary would need care spanning at least two midnights” but unanticipated events led to a shorter stay.
Plan of Attack
For HVBP, make contact with your director of quality to understand your hospital’s performance and payment for 2014. If you have incentive compensation riding on HVBP, make sure you understand how your employer or contracted hospital is calculating the payout (because, for example, the performance period was in 2012!) and that your hospitalist group understands the payout calculation.
For COPD readmissions prevention, ensure patients have a home management plan; appropriate specialist follow-up and that they understand medication use, including inhalers and supplemental oxygen; and that you consider early referral for pulmonary rehabilitation for eligible patients.
For the new definition of inpatient admission, work with your hospital’s physician advisor and case management to ensure your group is getting appropriate guidance on documentation requirements. You are probably being held accountable for your hospital’s total number of observation hours, so remember to track these metrics following implementation of the new rule, as they (hopefully) should decrease. If they do, take some of the credit!
References
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681.
- Lindenauer PK, Lagu T, Rothberg MB, et al. Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ. 2013;346:f521.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at [email protected].
How To Avoid Medicare Denials for Critical-Care Billing
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
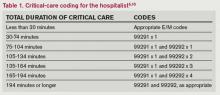
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Hospitalist Compensation Models Evolve Toward Production, Performance-Based Variables
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalists have long recognized that compensation varies significantly by geographic location and by the type of hospitalist medicine group (HMG) you work in: private vs. hospital-owned vs. national-management-owned. A review of SHM’s 2012 State of Hospital Medicine report suggests that hospitalist compensation is also evolving toward a model that more routinely includes both some production variable and performance-based pay (see Figure 1). Although the proportion of compensation paid as a base salary has been trending up over the last few years, so has the proportion paid as a performance incentive.
Source: 2012 State of Hospital Medicine report; www.hospitalmedicine.org/survey
The pay distribution of adult-medicine hospitalists employed by management companies is composed of a high base percentage (mean 88.3% by survey data) and relatively low production and performance variables (mean 6.8% and 4.9%, respectively) compared with other employment models. Contrast that with private hospitalist-only groups, where the mean base is 76.3% with an emphasis on a production component (19.4%) and slightly less on performance pay at 4.2%.
Of the three employment models, however, hospital-/health-system-employed groups have the highest proportion of compensation based on performance metrics with a mean of 7.8%. This makes sense given the financial penalties hospitals and health systems are facing from the Centers for Medicare & Medicaid Services (CMS) around pay-for-performance measures. Hospitals are looking for help from hospitalists in improving quality of care and patient satisfaction and avoiding incurring future penalties. Compensation models in these groups reflect the goals of aligning performance on these measures with financial incentives/risk for hospitalists working in these environments.
What are the top performance metrics hospitalists are being compensated for? CMS’ hospital value-based purchasing (HVBP) core measures and patient satisfaction scores are at the top of the list. More than 70% of all HMGs identify these two measures as part of their performance pay incentive, which is seen consistently by geographic location and by type of hospitalist group.
Beyond these top two metrics, management-company-employed groups also focus on ED throughput measures and early morning discharge times, with more than 70% of these groups having pay incentives aligned with these goals. They also have a higher proportion of their groups participating in several other measures, such as clinical protocols, medication reconciliation, EHR utilization, transitions of care, and readmission rates. In comparison, both hospital-employed and private groups have a wider variety of performance measures in which they participate. Differences are seen geographically, too, with hospitalists located in the Western region having a wider variety of performance measures than other regions.
How hospitalists are compensated for their work will likely continue to evolve. Overall, for nonacademic HMGs serving adults only, we are seeing an upward trend in percentage paid as base pay (from 76% in 2010 to 81% in 2012) and in performance (from 5% in 2010 to 7% in 2012). Hospitalists should anticipate that performance-based pay will continue to account for an increasingly larger percentage of their overall compensation, especially as CMS’ pay-for-performance measures for hospital systems really start to take effect.
Hospital CEOs and CFOs are looking to hospitalists to help deliver on quality, satisfaction, and other performance measures. Incentives will be put in place to reward those groups who do it well.
Dr. Sites is senior medical director of hospitalist programs at Providence Health and Services in Oregon. She is a member of SHM’s Practice Analysis Committee.
Hospitalist Groups Extract New Solutions Via Data Mining
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Estate planning
The latest anniversary of my birth is fast approaching; but fortunately, I have learned to celebrate these annual events rather than dread them. I now understand that life gets better as we get older, on all levels – except, perhaps, the physical.
But I have also found that birthdays are a good time to pause and consider the various financial arrangements that I’ve set up over the years and to determine whether any of them need updating.
Estate plans, in particular, need regular review and revision. Nothing important has changed in your life since you drafted your will, you say? Well, chances are the laws have changed; or, other factors may have rendered your plan obsolete without your even realizing it.
I am assuming, of course, that you have in fact drafted a will. If not, do it now. Things happen; if you die without one ("intestate," in lawyers’ lingo), your heirs will be at the mercy of attorneys, bureaucrats, state and federal laws, and greed. Quarrels will ensue; decisions will be made that are almost certainly at variance with what you would have wanted; and a substantial chunk of your estate, which could have gone to loved ones or to charity, will be lost to taxes and fees. If you don’t have a will, regardless of your age or current financial status, have one written at your earliest possible convenience.
That said, let’s consider some variables that mandate your constant vigilance:
• Laws change. Trust laws, in particular, have changed a great deal in recent years, and trust strategies have changed with them. New instruments like perpetual trusts, trust protectors, directed trusts, and total return trusts may or may not work to your advantage, but you won\'t know without asking. State laws change, too, all the time.
Once a year my wife and I meet with our estate lawyer to learn about any new legislation that may have affected our plan. Last year, I learned that my irrevocable trust is no longer irrevocable; new laws now permit certain provisions to be modified.
Laws that don’t directly regulate wills and trusts can affect them as well. For instance, the ever-popular Health Insurance Portability and Accountability Act (HIPAA) affects your estate as well as your practice; under its provisions, your family cannot access your medical information or make treatment and life-support decisions without your specific permission. So if a Health Care Power of Attorney is not already part of your will, add it. And remember to modify it if your medical status, or your philosophy of life, change.
• Financial markets change. It’s not exactly a secret that asset values and interest rates are way different than they were even a few years ago. Real estate or securities bequests could now be significantly larger, or smaller. Your accountant and estate lawyer should take a look at your assets periodically and their apportionment in your will, to be sure all arrangements remain as you intend. And be sure to notify them whenever the composition of your assets changes, even if the value doesn’t. Let’s say you sell a business or property and reinvest the proceeds in something completely different; that will change how you leave that asset to your heirs, because a different set of tax laws will apply.
• Fiduciaries change. The executor of your estate and the trustee(s) of your trust(s) need periodic review. If your brother-in-law is your executor, and your sister divorces him, you may want to find a new executor. A once-vigorous trustee who is now old or sick should be replaced. Trustees are often financial institutions; if one of your corporate trustees goes belly up, or the employee you were working with retires or changes firms, you’ll need a replacement. Keep track of your fiduciaries and be prepared to make changes as needed.
• Personal circumstances change. Some changes – marriage, divorce, the death of an heir, or the birth of a new one – obviously require modifications to wills and trusts. But any significant alteration of your personal or financial circumstances probably merits at least a phone call to your financial planners. The need for changes, and your options should changes be necessary, are not always obvious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past-president of the Dermatological Society of New Jersey and currently serves on its executive board. He holds teaching positions at a number of hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters and is a long-time monthly columnist for Skin & Allergy News, a publication of IMNG Medical Media.
The latest anniversary of my birth is fast approaching; but fortunately, I have learned to celebrate these annual events rather than dread them. I now understand that life gets better as we get older, on all levels – except, perhaps, the physical.
But I have also found that birthdays are a good time to pause and consider the various financial arrangements that I’ve set up over the years and to determine whether any of them need updating.
Estate plans, in particular, need regular review and revision. Nothing important has changed in your life since you drafted your will, you say? Well, chances are the laws have changed; or, other factors may have rendered your plan obsolete without your even realizing it.
I am assuming, of course, that you have in fact drafted a will. If not, do it now. Things happen; if you die without one ("intestate," in lawyers’ lingo), your heirs will be at the mercy of attorneys, bureaucrats, state and federal laws, and greed. Quarrels will ensue; decisions will be made that are almost certainly at variance with what you would have wanted; and a substantial chunk of your estate, which could have gone to loved ones or to charity, will be lost to taxes and fees. If you don’t have a will, regardless of your age or current financial status, have one written at your earliest possible convenience.
That said, let’s consider some variables that mandate your constant vigilance:
• Laws change. Trust laws, in particular, have changed a great deal in recent years, and trust strategies have changed with them. New instruments like perpetual trusts, trust protectors, directed trusts, and total return trusts may or may not work to your advantage, but you won\'t know without asking. State laws change, too, all the time.
Once a year my wife and I meet with our estate lawyer to learn about any new legislation that may have affected our plan. Last year, I learned that my irrevocable trust is no longer irrevocable; new laws now permit certain provisions to be modified.
Laws that don’t directly regulate wills and trusts can affect them as well. For instance, the ever-popular Health Insurance Portability and Accountability Act (HIPAA) affects your estate as well as your practice; under its provisions, your family cannot access your medical information or make treatment and life-support decisions without your specific permission. So if a Health Care Power of Attorney is not already part of your will, add it. And remember to modify it if your medical status, or your philosophy of life, change.
• Financial markets change. It’s not exactly a secret that asset values and interest rates are way different than they were even a few years ago. Real estate or securities bequests could now be significantly larger, or smaller. Your accountant and estate lawyer should take a look at your assets periodically and their apportionment in your will, to be sure all arrangements remain as you intend. And be sure to notify them whenever the composition of your assets changes, even if the value doesn’t. Let’s say you sell a business or property and reinvest the proceeds in something completely different; that will change how you leave that asset to your heirs, because a different set of tax laws will apply.
• Fiduciaries change. The executor of your estate and the trustee(s) of your trust(s) need periodic review. If your brother-in-law is your executor, and your sister divorces him, you may want to find a new executor. A once-vigorous trustee who is now old or sick should be replaced. Trustees are often financial institutions; if one of your corporate trustees goes belly up, or the employee you were working with retires or changes firms, you’ll need a replacement. Keep track of your fiduciaries and be prepared to make changes as needed.
• Personal circumstances change. Some changes – marriage, divorce, the death of an heir, or the birth of a new one – obviously require modifications to wills and trusts. But any significant alteration of your personal or financial circumstances probably merits at least a phone call to your financial planners. The need for changes, and your options should changes be necessary, are not always obvious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past-president of the Dermatological Society of New Jersey and currently serves on its executive board. He holds teaching positions at a number of hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters and is a long-time monthly columnist for Skin & Allergy News, a publication of IMNG Medical Media.
The latest anniversary of my birth is fast approaching; but fortunately, I have learned to celebrate these annual events rather than dread them. I now understand that life gets better as we get older, on all levels – except, perhaps, the physical.
But I have also found that birthdays are a good time to pause and consider the various financial arrangements that I’ve set up over the years and to determine whether any of them need updating.
Estate plans, in particular, need regular review and revision. Nothing important has changed in your life since you drafted your will, you say? Well, chances are the laws have changed; or, other factors may have rendered your plan obsolete without your even realizing it.
I am assuming, of course, that you have in fact drafted a will. If not, do it now. Things happen; if you die without one ("intestate," in lawyers’ lingo), your heirs will be at the mercy of attorneys, bureaucrats, state and federal laws, and greed. Quarrels will ensue; decisions will be made that are almost certainly at variance with what you would have wanted; and a substantial chunk of your estate, which could have gone to loved ones or to charity, will be lost to taxes and fees. If you don’t have a will, regardless of your age or current financial status, have one written at your earliest possible convenience.
That said, let’s consider some variables that mandate your constant vigilance:
• Laws change. Trust laws, in particular, have changed a great deal in recent years, and trust strategies have changed with them. New instruments like perpetual trusts, trust protectors, directed trusts, and total return trusts may or may not work to your advantage, but you won\'t know without asking. State laws change, too, all the time.
Once a year my wife and I meet with our estate lawyer to learn about any new legislation that may have affected our plan. Last year, I learned that my irrevocable trust is no longer irrevocable; new laws now permit certain provisions to be modified.
Laws that don’t directly regulate wills and trusts can affect them as well. For instance, the ever-popular Health Insurance Portability and Accountability Act (HIPAA) affects your estate as well as your practice; under its provisions, your family cannot access your medical information or make treatment and life-support decisions without your specific permission. So if a Health Care Power of Attorney is not already part of your will, add it. And remember to modify it if your medical status, or your philosophy of life, change.
• Financial markets change. It’s not exactly a secret that asset values and interest rates are way different than they were even a few years ago. Real estate or securities bequests could now be significantly larger, or smaller. Your accountant and estate lawyer should take a look at your assets periodically and their apportionment in your will, to be sure all arrangements remain as you intend. And be sure to notify them whenever the composition of your assets changes, even if the value doesn’t. Let’s say you sell a business or property and reinvest the proceeds in something completely different; that will change how you leave that asset to your heirs, because a different set of tax laws will apply.
• Fiduciaries change. The executor of your estate and the trustee(s) of your trust(s) need periodic review. If your brother-in-law is your executor, and your sister divorces him, you may want to find a new executor. A once-vigorous trustee who is now old or sick should be replaced. Trustees are often financial institutions; if one of your corporate trustees goes belly up, or the employee you were working with retires or changes firms, you’ll need a replacement. Keep track of your fiduciaries and be prepared to make changes as needed.
• Personal circumstances change. Some changes – marriage, divorce, the death of an heir, or the birth of a new one – obviously require modifications to wills and trusts. But any significant alteration of your personal or financial circumstances probably merits at least a phone call to your financial planners. The need for changes, and your options should changes be necessary, are not always obvious.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past-president of the Dermatological Society of New Jersey and currently serves on its executive board. He holds teaching positions at a number of hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters and is a long-time monthly columnist for Skin & Allergy News, a publication of IMNG Medical Media.
ACOG’s push for medical liability reform: What’s the latest?
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
It’s a conundrum. There seems to be no doubt about the need for medical liability reform—in fact, there is wide-spread support for it. And yet....
Four years after Captain Chesley “Sully” Sullenberger saved a planeload of passengers during an emergency landing—the “miracle on the Hudson”—he’s become a national champion of medical liability reform. In a recent interview with Politico, Sullenberger equated the 200,000 lives estimated to be lost each year due to medical errors to “20 jetliners crashing per week,” a situation he insists would close airports and ground flights until the problem was solved. But these 200,000 deaths cause little more than a ripple of concern, he claims.1
Among the solutions he proposes is “a whole different approach to reviewing medical errors, figuring out what’s behind them, not just blaming doctors and nurses.”1
Captain Sullenberger is discovering the difficult reality we’ve experienced for too many years: Solutions just don’t come very fast to medical liability reform, despite wide-spread support for it.
At the American Congress of Obstetricians and Gynecologists (ACOG), our campaign for medical liability reform has focused, as always, on patients, using the campaign line: “Who will delivery my baby?” ACOG supports caps on noneconomic damages and other reforms, such as those contained in the California Medical Injury Compensation Reform Act (MICRA), the gold standard for medical liability reform. We will continue to push for national MICRA reform until we’ve won that important protection for all ObGyns and their patients.
Until we reach that goal, we’re working to accomplish meaningful steps to liability reform where we can, including testing state alternatives. And our colleague organizations? Many of them, once insisting on federal adoption of MICRA or nothing at all, now actively support meaningful alternatives, too.
What do we want?
Proposals for tort reform, based on California’s MICRA statute, include:
- mandatory periodic payments of all future damages exceeding $100,000
- a $250,000 ceiling on noneconomic damage awards
- a requirement that claims must be filed within 2 years of the date by which the alleged injury reasonably should have been discovered but in no event more than 4 years from the time of the alleged injury. In the case of alleged injury to children under 4 years of age, claims must be filed by the child’s 8th birthday.
- limits on punitive damages, with 50% of punitive damage awards going to a state disciplinary fund
- limits on attorney contingency fees
- reductions in awards based on the amount paid from another source, such as health or disability insurance
- a requirement for “clear and convincing evidence” rather than the usual “preponderance of evidence” when a health-care professional who provided delivery services but not prenatal care is sued
- alternative systems for dispute resolution.
10 alternative reforms
Good ideas include:
1. Require a certificate of merit from the plaintiff
This proposal would require the plaintiff to file an affidavit with the court to demonstrate that the case has merit before the complaint can move forward. Certificates would necessitate the written opinion of a legally qualified health-care provider affirming that the defendant failed to meet the care standards that would be followed by a reasonably prudent health-care provider—and that this failure caused or directly contributed to the damages claimed.
2. Facilitate early settlement offers
Under this idea, a physician or hospital would be allowed to offer economic damages to an injured party without involving the courts. This offer would not constitute an admission of liability and would be inadmissible if a lawsuit were later filed in the case. Physicians would have an incentive to make a good-faith offer as early as possible after the injury is discovered, and patients would have an incentive to accept legitimate offers of compensation. Early-offer programs would require the injured party to meet a higher burden of proof for alleged negligence if that party chooses to reject the offer and file a lawsuit.
3. Create health-care courts
Health-care courts would allow for a bench or jury trial presided over by a specially trained judge to exclusively hear medical liability cases. Such courts have the potential to correct severe deficiencies in the current medical justice system and to reduce health-system errors and improve patient safety.
4. Allow a physician to say, “I’m sorry”
This proposal would encourage physicians to directly discuss errors and injuries with patients, to apologize and outline corrective action. Such discussions would be inadmissible if a patient later files a lawsuit.
5. Establish medical review panels
Any claim against a physician would be reviewed by a panel of experts who would provide an opinion on whether the physician failed to act within the relevant standards of care.
6. Require a claim to be screened and mediated
A plaintiff ’s claim would have to be evaluated by a screening panel before it could proceed to litigation. The panel would identify claims hat merit compensation and encourage early resolution of those claims. It also would encourage withdrawal or dismissal of non-meritorious claims.
7. Protect physicians who follow evidence-based guidelines
Health-care providers who follow guidelines based on solid evidence, and those who have legitimate justifications for departing from guidelines, would be protected from liability claims.
8. Allow the voluntary resolution of disputes
This proposal would motivate states to encourage the creation of other innovative systems to compensate individuals who are injured in the course of receiving health-care services.
9. Require expert witnesses to meet certain standards
This alternative would limit expert-witness standing to individuals who:
- are licensed and trained in the same specialty as the defendant
- have particular expertise in the disease process or procedure performed in the case
- have been in active medical practice in the same specialty as the defendant within 5 years of the claim or who have been taught at an accredited medical school on the care and type of treatment at issue.
10. Create catastrophic injury systems
These systems would establish a fund for individuals who have experienced bad outcomes. Birth injury funds are an example of this model.
Who’s on our side?
Congressional policy wonks give liability reform a thumbs up
In early 2010, the Medicare Payment Advisory Commission (MedPAC), a nonpartisan advisory counsel to the US Congress, identified three important ways that our current malpractice system harms the Medicare program and Medicare beneficiaries, the aged, and disabled:
- Medicare payments to providers include some liability costs (folded into hospital diagnosis-related group [DRG] payments; factored into physician fee schedule calculation)
- Defensive medicine drives up costs for Medicare
- Malpractice impairs the quality and safety of care to beneficiaries. That is, the current system does not improve patient safety.
MedPAC staff recommended that the commissioners urge Congress to pass government-subsidized malpractice reinsurance for providers who meet certain safety criteria or create a federal administrative adjudication process. The commissioners expressed an interest in alternatives to address the costs of medical malpractice, including ways to encourage states and providers to address medical malpractice in a manner most appropriate for them. However, when MedPAC returned to this topic at its next meeting later the same year, the commissioners mentioned medical liability only to dismiss it as an incidental issue in opening remarks.
The Congressional Budget Office (CBO) estimates that medical malpractice costs our health-care system $35 billion in direct costs, with billions more as a result of defensive medicine.
CBO has scored these medical liability reform proposals as providing significant savings to our federal budget:
- a $250,000 cap on subjective, noneconomic damages (with no limit on economic damages)
- collateral source rule allowing evidence of outside payments to be submitted in court
- a ban on subrogation by certain collateral sources
- caps on attorney contingency fees
- periodic payments of future damages
- a reasonable statute of limitations.
In addition, in 2011, CBO scored comprehensive medical liability reform as saving the federal government $62.4 billion over 10 years. As longtime Illinois Senator Everett Dirksen was known to say, “A billion here, a billion there, and pretty soon you’re talking real money.”
Many Republican congressional leaders “walk the walk”
Republicans have long claimed medical liability reform as their issue. And they walk the walk.
Representative Phil Gingrey, MD, of Georgia, an ACOG Fellow, has led the medical liability reform fight on Capitol Hill for a number of years. His bill, the Protecting Access to Healthcare Act (HR 5), which would have brought MICRA to the national level, was repeatedly passed by the Republican majority of the House of Representatives, only to be ignored by the Democrats controlling the Senate.
Again this year, Dr. Gingrey introduced legislation to protect physicians from unexpected liability. His Standard of Care Protection Act (HR 1473) would ensure that provisions of the Affordable Care Act (ACA) cannot be used to create new causes of action against medical professionals. HR 1473 would ensure that Medicare, Medicaid, and other federal programs that establish government standards and guidelines for health-care providers cannot be used to create new causes of action.
Federal health-care programs are changing to ensure that payment reflects quality of care. As a result, new payment rules, guidelines, and standards are being written into federal laws and regulations. HR 1473 would make clear that these cannot be used to define the applicable standard of care or duty of care in a medical liability lawsuit.
ACOG supports Dr. Gingrey’s bill, as well as a second, companion approach that would ensure that ObGyns who follow guidelines and standards of care developed by their medical society are protected from liability, with sensible exceptions for egregious harm and negligence.
Representative Charlie Dent, Republican of Pennsylvania, also has introduced ACOG-supported medical liability legislation. The Health Care Safety Net Enhancement Act (HR 36) would provide federal liability protection for physicians providing care under the Emergency Medical Treatment and Active Labor Act (EMTALA). HR 36 is commonly referred to as Good Samaritan legislation, intended to protect doctors who rush to the aid of a sick individual. The likelihood of any of these bills getting enacted into law is slim. Even some conservative Republicans oppose federal liability reform as an intrusion into states’ rights.
Some Democrats have said good things
In his proposed budget for fiscal year 2012, President Barack Obama asked Congress for funding to address medical liability issues.
He proposed “to restrain health-care costs” through “a more aggressive effort to reform our medical malpractice system to reduce defensive medicine, promote patient safety, and improve patient outcomes.” He encouraged Republicans to work constructively with him on medical malpractice as part of an overall effort to restrain health-care costs.2
The President asked Congress for “$250 million in grants to states to reform the way they resolve medical malpractice disputes,” including health courts, safe harbors, early disclosure and offer, and other legal reforms such as joint and several liability and collateral source rules.2
Congress never funded the President’s request.
President Obama repeated his request in his fiscal year 2013 budget proposal. Congress didn’t fund it then, either.
Earlier, in March 2009, in remarks to the Business Roundtable, President Obama noted that “the cost issue is the thing that we actually think is the big driver in this whole debate...things like comparative effectiveness, health IT, prevention, figuring out how our reimbursement structures are designed under Medicare and Medicaid. Medical liability issues—I think all those things have to be on the table.”3
In an interview the same month, Senator Ron Wyden, Democrat of Oregon, said, “I think [medical liability reform is] an essential piece for there to be enduring reform, reform that will stick and will get a significant bipar-tisan vote in the United States Senate.”4
Senator Wyden’s Healthy Americans Act (S 391) included incentives to get states to enact malpractice reforms as a key to overhauling the health-care system.
Also in March 2009, Representative Rob Andrews, Democrat of New Jersey, Chairman of the House Education and Labor, Health Subcommittee, pointed to the need for medical liability reform.
“It’s hard for me to imagine a [health-care reform] result that gets to the president’s desk that doesn’t deal with the medical mal-practice issue in some way.”4
And Senator Max Baucus, Democrat of Montana, Chairman of the Senate Finance Committee, proposed providing states grant money to develop alternative litigation models, such as encouraging disclosure and compensation in the case of error, and establishing health courts whose judges have health-care expertise.
As early as May 2006, President Obama (then a Senator from Illinois) and Senator Hillary Rodham Clinton, Democrat of New York, urged a focus on patient safety.
“Instead of focusing on the few areas of intense disagreement,” they wrote in the New England Journal of Medicine, “such as the possibility of mandating caps on the financial damages awarded to patients, we believe that the discussion should center on a more fundamental issue: the need to improve patient safety....”
“To improve both patient safety and the medical liability climate, the tort system must achieve four goals: reduce the rates of preventable patient injuries, promote open communication between physicians and patients, ensure patients access to fair compensation for legitimate medical injuries, and reduce liability insurance premiums for health-care providers. Addressing just one of these issues is not sufficient.”5
And then there are the trial lawyers
Readers of OBG Management know all too well that the role of trial lawyers in medical liability reform has been to block meaningful reforms from passing and to repeal reforms currently in place. The Association of Trial Lawyers of America, now known as the American Association for Justice, tries to portray itself as defending vulnerable patients against a few bad apples. Its Web site (www.justice.org) points to recent National Practitioner Data Bank (NPDB) figures indicating that “just 6% of doctors are responsible for 58% of all negligence incidents. The civil justice system seeks to weed out those few doctors whose actions have such devastating impact on patients.”
The Web site includes these bullet points:
- 6% of doctors have been responsible for 58% of all malpractice payments since 1991
- 2% of doctors having three or more mal-practice payments were responsible for 33% of all payments
- 1% of doctors having four or more malprac-tice payments were responsible for 20% of all payments
- 82% of doctors have never had a medical malpractice payment.
Tell that to ObGyns, who, in 2012, paid an average of 12.4% of their gross income for liability insurance premiums in 2012, and nearly 60% of whom changed their practices based on the risk or fear of professional liability claims or litigation. And this despite the fact that 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn.
Action at the state level
We need a federal solution, but since that isn’t within reach, we’re looking to the states for action. And there’s a lot of action in some states, including Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Missouri, Oregon, Rhode Island, Tennessee, and Utah.
Advocates in these states are trying a number of different approaches, hoping that some type of meaningful reform will be signed into law. Here’s a sampling of what’s under way.
Connecticut
HB 6687, amend certificates of merit in medical liability actions. Status: April 1, 2013: Joint Committee on Judiciary hearing. The bill would eliminate the need for a detailed basis for the formation of an opinion and replace it with a lower threshold stating the appearance of one or more specific breaches of the prevailing professional standard of care.
In addition, HB 6687 would allow any expert who may testify in court to satisfy the certificate of merit requirement, but at trial the “expert,” in order to testify, needs to have the court determine him or her to be qualified to testify based on discovery and evidentiary issues that are decided at trial. This expert then could sign a certificate of merit but have the court determine that he or she is indeed not an expert for that case. HB 6687 delays the challenging of qualifications of an expert only after the completion of discovery, adding substantial time and cost to defending meritless suits. Finally, the bill allows for a second bite of the apple for cases that did not meet this watered down standard for certificate of merit and would eliminate the automatic dismissal of cases filed with inadequate certificates that did not meet the rules of the court.
SB 1154, amend Connecticut’s failure of suit statute to allow a plaintiff whose lawsuit was dismissed due to a failure to file a certificate of good faith as required by statute, to commence a new action.
HB 5229, limit noneconomic damages in medical liability cases to $250,000 for each health-care provider and institution per event, and $750,000 overall for each event.
HB 5270, establish peer-review panels in medical liability actions. The panels would consist of physicians, medical professionals, and individuals outside the medical profession who would review claims of alleged negligence and determine whether there is probable cause that the medical liability claims have been made in good faith prior to the action being referred to mandatory mediation.
SB 97, extend the statute of limitations in medical liability cases, allowing for an action to be brought no more than 10 years from the date of the act or omission that serves as the basis for the claim.
Florida
The Birth-Related Neurological Injury Compensation Association (NICA). NICA is a statutory organization that manages the compensation plan used to pay for the care of infants born with certain neurological injuries. This plan is available to eligible families statewide without litigation. By eliminating costly legal proceedings, and through professional management of its disbursements, NICA ensures that birth-injured infants receive the care they need while reducing the financial burden on medical providers and families. Defensive work continues on the NICA Board and trial bar.
HB 7015, expert witness. Status: March 28, 2013, the House Justice Appropriations Subcommittee reported favorably. This bill would adopt the Daubert standard for expert witness testimony. It provides that a witness qualified as an expert by knowledge, skill, experience, training, or education may testify in the form of an opinion as to the facts at issue in a case.
Georgia
HB 499, Provider Shield Act. Georgia is the first state to introduce legislation based on the American Medical Association’s model bill, “The Provider Shield Act,” which clarifies language in the Affordable Care Act by providing that a physician’s failure to comply with, or a breach of, any federal statute, regulation, program, guideline, or other provision shall not: (1) be admissible; (2) be used to determine the standard of care; or (3) be the legal basis for a presumption of negligence.
Status: Enacted May 6, 2013. The law prohibits the use of payer guidelines and quality criteria outlined in federal law as a legal basis for negligence or standard of care in determining medical liability. Physicians are concerned that without such protections, the medical profession could be exposed to charges of negligence that aren’t based on clinical standards or the patient’s unique medical needs. Implementation of any guideline by any public or private payor, or the establishment of any payment standard or reimbursement criteria under any federal laws or regulations related to health care, shall not be construed, without competent expert testimony establishing the appropriate standard of care, to establish a legal basis for negligence or the standard of care or duty of care owed by a health-care provider to a patient in any civil action for medical malpractice or product liability.
This first-of-its-kind legislation reinforces the concept that medical decisions should be based on a patient’s unique medical needs. HB 499 makes it clear that federal standards or guidelines designed to enhance access to high-quality health care cannot be used to invent new legal actions against physicians.
Hawaii
SB 1308, health-care provider benevolent gesture legislation.
Illinois
On March 22, 2013, several pieces of tort-reform legislation were re-referred to the House Committee on Rules, effectively killing the bills for the session. The House Speaker would have to choose to “release” any of the bills in order for them to move again; this is highly unlikely.
HB 138 would have deleted existing-venue language providing that an action may commence in any county if all defendants are nonresidents of the state, and replaced it with language providing that, if no defendants that are joined in good faith and with probable cause for the purpose of obtaining a judgment against them are residents of the state, an action may be commenced only in the county in which the transaction or some part thereof occurred out of which the cause of action arose.
HB 2220 and HB 2222 provided that, with respect to certain types of actions, for any defendant whose fault is less than 25% of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendant who could have been sued by the plaintiff (instead of any third-party defendant except the plaintiff’s employer), shall be severally liable for all other damages. In addition, these bills provided that, for any defendant whose fault is 25% or greater of the total fault attributable to the plaintiff, the defendants sued by the plaintiff, and any third-party defendants who could have been sued by the plaintiff (instead of any third-party defendants except the plaintiff’s employer), shall be jointly and severally liable for all other damages.
HB 2221 created requirements regarding qualifications, testimony, disclosure and compensation of expert testimony and standards for reviewing courts to follow in ruling on the admissibility of expert testimony.
Iowa
SSB 1054 and HSB 36, expert’s certificate of merit affidavit and noneconomic cap. These bills provide that in any medical liability action, the plaintiff is required, within 180 days of the defendant’s answer, to serve the defendant with an expert’s certificate of merit affidavit for each expert scheduled to testify. They also would limit noneconomic damage awards in medical liability cases to $1 million.
Missouri
HJR 6 proposes a constitutional amendment allowing the legislature to cap noneconomic damages in medical liability cases.
SJR 1 grants the legislature the power to limit, by statute, jury awards for noneconomic damages.
SB 64 changes the evidentiary standard in medical liability cases to “clear and convincing” for noneconomic damages.
Oregon
SB 483, early discussion and resolution. Status: Passed by the legislature. This bill establishes an early discussion and resolution (EDC) process within the Oregon Patient Safety Commission. This voluntary process is intended to facilitate open communication about all outcomes of care, including serious events, between the provider, health-care facility, and the patient. When an adverse health-care incident occurs, the patient, health-care provider or health-care facility where the incident occurred may file a notice of adverse health-care incident with the Commission. This notice triggers discussion of the health-care incident and, if appropriate, an offer of compensation. If discussion does not result in the resolution of the claim, the bill gives the parties the option of participating in Commission-facilitated mediation. The entire process is voluntary.
SJR 30, proposed amendment to constitution, $1 million limit on noneconomic awards in medical liability cases. Slated for next general election.
Rhode Island
HB 5380, apology bill. Status: Heard in House Judiciary Committee on March 27, 2013; no action was taken. This bill provides that statements by a health-care provider to a patient or to the patient’s family regarding the outcome of such patient’s medical care and treatment, such as an apology or expression of sympathy, shall be inadmissible as evidence or an admission of liability in any claim or action against the provider.
Tennessee
Joint and several liability. Status: On March 26, 2013, the House Civil Justice Subcommittee reported favorably. This bill would codify current state law by providing that if multiple defendants are found liable in a civil action governed by comparative fault, a defendant shall only be severally liable for the percentage of damages for which fault is attributed to such defendant by the trier of fact, and no defendant shall be held jointly liable for any damages.
SB 274, medical liability expert witness reform.
Utah
HB 135, rules, arbitration. Status: March 21, 2013, sent to Governor Gary Herbert for his approval. HB 135 provides that a party in a medical liability action or arbitration may not attempt to allocate fault to any health-care provider unless a certificate of compliance has been issued. HB 135 also requires that evidence from a medical review panel remain unreportable to a health-care facility or health insurance plan.
Summing up
Medical liability reform—the obvious need for it, the good reasons to do it, and the fact that it remains beyond reach—is a constant source of frustration among many ObGyns. Maybe Captain Sully can save the day.
How medical liability affects the ObGyn specialty
ACOG’s 2012 Survey on Professional Liability, our 11th survey since 1983, assessed the effects of professional liability litigation and insurance issues on the practice of obstetrics and gynecology.6 The survey, conducted under the direction of ACOG’s Vice President for Fellowship and Deputy Executive Vice President Albert Strunk, MD, JD, included segments on demographics, patient care, liability claims experience, and practice changes associated with the cost of liability insurance and the fear of litigation. The survey went to 32,238 Fellows and Junior Fellows. Of these, 9,006 completed the questionnaire. Here are major findings.
Provider profiles
A total of 72.5% of respondents provided both obstetric and gynecologic care, slightly lower than the percentage identified in the 2009 survey, which was 74.3%. Fewer than 7% of respondents provided obstetric care only; 19.8% provided gynecologic care only. Of those restricting their services to gynecology, 88.9% had previously offered obstetric care. The average age at which these physicians stopped practicing obstetrics was 49 years.
Cost of liability insurance
ObGyns spent an average of 12.4% of their gross income on liability insurance premiums in 2012, down from 18% in 2009.
How liability issues affected practice
Since the previous survey in 2009, 57.9% of respondents made one or more changes to their practice to mitigate the risk or fear of professional liability claims or litigation.
Obstetric practice. Among respondents who made changes to their obstetric practice, 27.4% decreased the number of high-risk patients they see, 23.8% increased the number of cesarean deliveries they perform, 18.9% stopped offering and performing vaginal birth after cesarean (VBAC), 11.5% reduced the total number of deliveries, and 6.2% stopped practicing obstetrics altogether.
Gynecologic practice. Respondents who changed their gynecologic practice cut back on surgical procedures (18.9%), stopped performing major gynecologic surgery (6.7%), and stopped performing all surgery (1.8%).
Other changes. Medical liability issues contributed to the decisions of 12.3% of respondents to choose salaried employment with a hospital, government, or other institution.
Claims experience
Obstetric claims were likely to involve a neurologically impaired infant (28.8%) as the primary allegation, followed by stillbirth or neonatal death (14.4%).
Other variables involved in obstetric claims included electronic fetal monitoring (20.9%), shoulder dystocia and/or brachial plexus injury (15.5%), and actions of ObGyn residents (11.4%).
Gynecologic claims. Survey respondents reported a total of 1,496 gynecologic claims. Major injury to the patient was the primary allegation of 29.1% of these claims. A delay in diagnosis or failure to diagnose was the second most common primary allegation (22.1%), followed by minor injury to the patient (20.7%).Of the claims involving a delayed or missed diagnosis, 41.8% involved cancer. Of these, breast cancer was the most frequent type of cancer (39.1%), followed by uterine cancer (20.3%), ovarian cancer (14.5%), and cervical cancer (10.9%).
Many gynecologic claims (44.4%) involved surgical complications arising from hysterectomy (28.7%) and laparoscopic procedures (14.6%).
Claims outcomes. A total of 43.9% of claims were dropped or settled without any payment on behalf of the ObGyn. Of these, 29.0% were dropped by the plaintiff, 11.2% were dismissed by the court, and 3.7% were settled without payment on behalf of the ObGyn.The average for all paid claims was $510,473.
The average payment for claims involving a neurologically impaired infant was $982,051. Other average payments for obstetric claims include $364,794 for “other infant injury–major” and $271,149 for stillbirth or neonatal death.
Average payments for gynecologic claims include $407,500 for a failure to diagnose breast cancer and $315,633 for “patient injury–major.”
Most challenging locales. It will come as no surprise to many readers that average medical liability payouts are especially high in six states:
New York - $677,866,050
Pennsylvania - $319,710,250
Illinois - $242,108,800
New Jersey - $221,170,750
Florida - $218,123,050
California - $215,519,200.
Fifty-eight percent of payouts nationwide were for female patients.7
Tell us what you think, at [email protected]. Please include your name and city and state.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
1.Cheney K. ‘Miracle’ pilot on mission against medical errors. Politico.com. August 1, 2013. http://www.politico.com/story/2013/08/sully-sullenberger-mission-medical-erros-95009.html. Accessed August 6, 2013.
2.Office of Management and Budget. Fiscal Year 2012 Budget of the US Government. http://www.whitehouse.gov/files/documents/budget_2012.pdf. Accessed August 8, 2013.
3.Obama’s remarks to the Business Roundtable, March 12, 2009. Wall Street Journal: Washington Wire. http://blogs.wsj.com/washwire/2009/03/12/obamas-remarks-to-the-business-roundtable/. Accessed August 8, 2013.
4.Werner E. Health debate could spur malpractice changes. Salt Lake Tribune. March 17, 2009. http://www.sltrib.com/ci_11933162. Accessed August 8, 2013.
5.Clinton HR, Obama B. Perspective: Making patient safety the centerpiece of medical liability reform. N Engl J Med. 2006;354(21):2205–2208.
6.American Congress of Obstetricians and Gynecologists. Survey on Professional Liability. 2012 Survey Results. http://www.acog.org/About_ACOG/ACOG_Departments/Professional_Liability/2012_Survey_Results. Accessed August 7, 2013.
7. Latner AW. Six states account for 50% of malpractice payouts. Clinical Advisor. April 17, 2012. http://www.clinicaladvisor.com/six-states-account-for-50-of-malpractice-payouts/article/236931. Accessed August 7, 2013.
- ACOG proposals for reform
- Action at the state level
- How medical liability affects the ObGyn specialty