User login
Malpractice Counsel: Don’t Miss Popeye
A 42-year-old man presented to the ED with left arm pain secondary to an injury he sustained at work. The patient stated that he had been helping to lift a heavy steel beam at a construction site when he experienced abrupt onset of pain in his left arm. He further noted that his left arm felt slightly weaker than normal after the injury.
The patient was left-hand dominant, denied any other injury, was otherwise in good health, and on no medications. With the exception of an appendectomy at age 12 years, his medical history was unremarkable. Regarding his social history, he admitted to smoking one pack of cigarettes per day, and to occasional alcohol consumption. He had no known drug allergies.
On physical examination, the patient’s vital signs were: blood pressure, 125/76 mm Hg; heart rate, 78 beats/min; respiratory rate, 16 breaths/min; and temperature, 98.6°F. Oxygen saturation was 99% on room air.
Examination of the patient’s left shoulder revealed no swelling or tenderness; he was able to fully internally/externally rotate the left shoulder, and lift his left hand above his head. The patient did have tenderness along the biceps area of the left arm, but no tenderness in the triceps area. The left elbow was tender in the antecubital fossa, but without swelling. He had full range of motion of the left elbow but with some pain. He likewise had full range of motion in his left wrist, but no tenderness or swelling. The left radial pulse was 2+. The patient had 5/5 grip strength with the left hand and good capillary refill.
The physician assistant (PA) evaluating the patient diagnosed an arm strain. At discharge, he referred the patient to an occupational health physician (OHP) for follow-up. He also instructed the patient to take ibuprofen 400 mg every 6 to 8 hours, and to limit use of his left arm for 3 days.
The patient followed up with the OHP approximately 3 weeks after discharge from the ED. The OHP was concerned the patient had experienced a distal biceps tendon rupture and referred the patient emergently to an orthopedic surgeon. The orthopedic surgeon saw the patient the next day, agreed with the diagnosis of a distal biceps tendon rupture, and attempted surgical repair the following day. The orthopedic surgeon informed the patient prior to the surgery that the delay in the referral and surgery could result in a poor functional outcome. The patient did have a difficult recovery period, and a second surgery was required, which did not result in any significant functional improvement.
The plaintiff sued the treating PA and supervising emergency physician (EP) for failure to properly diagnose the biceps tendon rupture, failure to appreciate the existence of a 3-week window of opportunity to repair the distal biceps tendon rupture, and failure to obtain an urgent orthopedic referral. The experts for the defense argued that the poor outcome was not a consequence of any delay in diagnosis or surgical repair. In addition, the defense disputed the existence of a 3-week window of opportunity for successful repair of a distal biceps tendon rupture. The jury returned a defense verdict.
Discussion
Proximal and Distal Biceps Tendon Ruptures
While both proximal and distal biceps tendon ruptures involve the biceps brachii, they are managed differently and have the potential for very different outcomes.1 At its proximal attachment, the biceps has two distinct tendinous insertions—the long head and the short head. For the distal attachment, the two muscle bellies unite at the midshaft of the humerus and attach as a single tendon on the radial tuberosity. In general, 96% of biceps tendon ruptures involve the long head, 1% involve the short head, and only 3% involve the distal tendon.1 Biceps tendon ruptures occur more commonly in men, patients who use anabolic steroids, cigarette smokers, patient history of tendinopathy, or patients who have a rotator cuff tear.1 Biceps tendon ruptures have not been found to be associated with statin use.2 The mechanism of injury includes heavy-lifting activities, such as weight lifting and rock climbing. However, when associated with a tendinopathy, minimal force may be involved.1
Signs and Symptoms
For proximal biceps tendon rupture, patients usually present with an acute or gradual onset of pain, swelling, and bruising of the upper arm and shoulder. Occasionally, if there is an inciting event, the patient may describe hearing or feeling a “popping” or “snapping” sound. On physical examination, the patient may exhibit a “Popeye” sign—a bulge in the distal biceps area due to the retracted biceps muscle belly. There is also tenderness along the biceps.
On testing, it has been estimated that patients can experience strength loss of approximately 30% with elbow flexion.1 In contrast, patients with distal biceps tendon ruptures usually complain of pain, swelling, and possibly bruising in the antecubital fossa, as was the case with this patient. Similar to proximal ruptures, the patient may admit to hearing or feeling a “popping” sound if there is an inciting event. The patient may exhibit a “reverse Popeye” deformity, with a bulge in the proximal arm secondary to retraction of the biceps muscle belly proximally.1
Diagnosis
There are two tests that can be performed to assist in making the diagnosis—the biceps squeeze test and the hook test.
Biceps Squeeze Test. The first test to assess for distal biceps tendon rupture is the biceps squeeze test, in which the clinician forcefully squeezes the patient’s biceps muscle to observe for forearm flexion/supination. This test is similar in principle to the Thompson test for Achilles tendon rupture. If there is no forearm movement, the injury is suspicious for a complete distal biceps tendon rupture. In one observational study of this test, 21 of 22 patients with a positive biceps squeeze test were found to have a complete distal biceps tendon tear at surgery.3
Hook Test. The second test is the hook test. While the patient actively supinates with the elbow flexed at 900, an intact hook test permits the examiner to “hook” his or her index finger under the intact biceps tendon from the lateral side. The absence of a “hook” means that there is no cord-like structure under which the examiner can hook a finger, indicating distal avulsion.4 In one study comparing the hook test to magnetic resonance imaging (MRI) in 33 patients with this suspected injury, the hook test had 100% sensitivity and specificity, while MRI only demonstrated a 92% sensitivity and 85% specificity.4
Imaging Techniques
The need for diagnostic imaging is based somewhat on the location of the rupture—proximal or distal. Ultrasound has been shown to have a high sensitivity and specificity for identifying normal tendons and complete tears of the long head biceps tendon (ie, proximal). It is not sensitive at identifying proximal partial tears, however. For distal ruptures, ultrasound imaging of the distal biceps tendon is technically difficult and not reliable. For patients with suspected distal biceps tendon ruptures, the EP should consult with orthopedic services prior to ordering an MRI. While MRI is considered the gold standard imaging test, it is neither 100% sensitive nor specific. The bottom line is that the absence of pathologic findings on MRI is not sufficient enough to exclude biceps tendon pathology.5
Treatment and Management
Regarding management, the majority of patients with proximal biceps tendon ruptures tend to do well with conservative management. The exception is for younger, active patients who are less willing to accept the cosmetic deformity, or patients whose occupation makes them unable to tolerate minimal weakness or fatigue cramping (eg, carpenters), in which case referral for a surgical repair (tenodesis) may be appropriate.1 However, multiple systematic reviews examining tenotomy vs tenodesis have not shown any functional improvement, only cosmetic.1,6,7
Distal biceps tendon ruptures are usually treated surgically, since conservative management results in a decrease of 30% to 50% supination strength and 20% flexion strength.1,8 This surgery, however, is not without complications. Approximately 20% of the patients will have a minor complication and 5% will have major complications following surgery on the distal biceps tendon.9 It is preferable to operate on distal ruptures less than 4 weeks from the initial injury; otherwise, these injuries may be more difficult to fix, require a graft, and have less predictable outcomes.1 Nonoperative management should be reserved for the elderly or less active patients with multiple comorbidities, especially if the nondominant arm is involved.10
Summary
The PA clearly missed the correct diagnosis on this patient. A more thorough history and focused physical examination would have led to the correct diagnosis sooner, along with earlier surgical repair. It is impossible, however, to know if the outcome would have been any different in this uncommon injury.
1. Smith D. Proximal versus distal biceps tendon ruptures: when to refer. BCMJ. 2017;59(2):85.
2. Spoendlin J, Layton JB, Mundkur M, Meier C, Jick SS, Meier CR. The risk of achilles or biceps tendon rupture in new statin users: a propensity score-matched sequential cohort study. Drug Safety. 2016;39(12):1229-1237. doi:10.1007/s40264-016-0462-5.
3. Ruland RT, Dunbar RP, Bowen JD. The biceps squeeze test for diagnosis of distal biceps tendon ruptures. Clin Orthop Relat Res. 2005;437:128-131.
4. O’Driscoll SW, Goncalves LBJ, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35(11):1865-1969. doi:10.1177/0363546507305016.
5. Malavolta EA, Assunção JH, Guglielmetti CL, de Souza FF, Gracitelli ME, Ferreira Neto AA. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol. 2015;84(11):2250-2254. doi:10.1016/j.ejrad.2015.07.031.
6. Tangari M, Carbone S, Gallo M, Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20(3):409-413. doi:10.1016/j.jse.2010.08.008.
7. Eakin JL, Bailey JR, Dewing CB, Provencher MT. Subpectoral biceps tenodesis. Oper Tech Sports Med. 2012;20(3):244-252.
8. Thomas JR, Lawton JN. Biceps and triceps ruptures in athletes. Hand Clin. 2017;33(1):35-46. doi:10.1016/j.hcl.2016.08.019.
9. Beks RB, Claessen FM, Oh LS, Ring D, Chen NC. Factors associated with adverse events after distal biceps tendon repair or reconstruction. J Shoulder Elbow Surg. 2016;25(8):1229-1234. doi:10.1016/j.jse.2016.02.032.
10. Savin DD, Watson J, Youderian AR, et al. Surgical management of acute distal biceps tendon ruptures. J Bone Joint Surg. 2017;3(9):785-796. doi:0.2106/JBJS.17.00080.
A 42-year-old man presented to the ED with left arm pain secondary to an injury he sustained at work. The patient stated that he had been helping to lift a heavy steel beam at a construction site when he experienced abrupt onset of pain in his left arm. He further noted that his left arm felt slightly weaker than normal after the injury.
The patient was left-hand dominant, denied any other injury, was otherwise in good health, and on no medications. With the exception of an appendectomy at age 12 years, his medical history was unremarkable. Regarding his social history, he admitted to smoking one pack of cigarettes per day, and to occasional alcohol consumption. He had no known drug allergies.
On physical examination, the patient’s vital signs were: blood pressure, 125/76 mm Hg; heart rate, 78 beats/min; respiratory rate, 16 breaths/min; and temperature, 98.6°F. Oxygen saturation was 99% on room air.
Examination of the patient’s left shoulder revealed no swelling or tenderness; he was able to fully internally/externally rotate the left shoulder, and lift his left hand above his head. The patient did have tenderness along the biceps area of the left arm, but no tenderness in the triceps area. The left elbow was tender in the antecubital fossa, but without swelling. He had full range of motion of the left elbow but with some pain. He likewise had full range of motion in his left wrist, but no tenderness or swelling. The left radial pulse was 2+. The patient had 5/5 grip strength with the left hand and good capillary refill.
The physician assistant (PA) evaluating the patient diagnosed an arm strain. At discharge, he referred the patient to an occupational health physician (OHP) for follow-up. He also instructed the patient to take ibuprofen 400 mg every 6 to 8 hours, and to limit use of his left arm for 3 days.
The patient followed up with the OHP approximately 3 weeks after discharge from the ED. The OHP was concerned the patient had experienced a distal biceps tendon rupture and referred the patient emergently to an orthopedic surgeon. The orthopedic surgeon saw the patient the next day, agreed with the diagnosis of a distal biceps tendon rupture, and attempted surgical repair the following day. The orthopedic surgeon informed the patient prior to the surgery that the delay in the referral and surgery could result in a poor functional outcome. The patient did have a difficult recovery period, and a second surgery was required, which did not result in any significant functional improvement.
The plaintiff sued the treating PA and supervising emergency physician (EP) for failure to properly diagnose the biceps tendon rupture, failure to appreciate the existence of a 3-week window of opportunity to repair the distal biceps tendon rupture, and failure to obtain an urgent orthopedic referral. The experts for the defense argued that the poor outcome was not a consequence of any delay in diagnosis or surgical repair. In addition, the defense disputed the existence of a 3-week window of opportunity for successful repair of a distal biceps tendon rupture. The jury returned a defense verdict.
Discussion
Proximal and Distal Biceps Tendon Ruptures
While both proximal and distal biceps tendon ruptures involve the biceps brachii, they are managed differently and have the potential for very different outcomes.1 At its proximal attachment, the biceps has two distinct tendinous insertions—the long head and the short head. For the distal attachment, the two muscle bellies unite at the midshaft of the humerus and attach as a single tendon on the radial tuberosity. In general, 96% of biceps tendon ruptures involve the long head, 1% involve the short head, and only 3% involve the distal tendon.1 Biceps tendon ruptures occur more commonly in men, patients who use anabolic steroids, cigarette smokers, patient history of tendinopathy, or patients who have a rotator cuff tear.1 Biceps tendon ruptures have not been found to be associated with statin use.2 The mechanism of injury includes heavy-lifting activities, such as weight lifting and rock climbing. However, when associated with a tendinopathy, minimal force may be involved.1
Signs and Symptoms
For proximal biceps tendon rupture, patients usually present with an acute or gradual onset of pain, swelling, and bruising of the upper arm and shoulder. Occasionally, if there is an inciting event, the patient may describe hearing or feeling a “popping” or “snapping” sound. On physical examination, the patient may exhibit a “Popeye” sign—a bulge in the distal biceps area due to the retracted biceps muscle belly. There is also tenderness along the biceps.
On testing, it has been estimated that patients can experience strength loss of approximately 30% with elbow flexion.1 In contrast, patients with distal biceps tendon ruptures usually complain of pain, swelling, and possibly bruising in the antecubital fossa, as was the case with this patient. Similar to proximal ruptures, the patient may admit to hearing or feeling a “popping” sound if there is an inciting event. The patient may exhibit a “reverse Popeye” deformity, with a bulge in the proximal arm secondary to retraction of the biceps muscle belly proximally.1
Diagnosis
There are two tests that can be performed to assist in making the diagnosis—the biceps squeeze test and the hook test.
Biceps Squeeze Test. The first test to assess for distal biceps tendon rupture is the biceps squeeze test, in which the clinician forcefully squeezes the patient’s biceps muscle to observe for forearm flexion/supination. This test is similar in principle to the Thompson test for Achilles tendon rupture. If there is no forearm movement, the injury is suspicious for a complete distal biceps tendon rupture. In one observational study of this test, 21 of 22 patients with a positive biceps squeeze test were found to have a complete distal biceps tendon tear at surgery.3
Hook Test. The second test is the hook test. While the patient actively supinates with the elbow flexed at 900, an intact hook test permits the examiner to “hook” his or her index finger under the intact biceps tendon from the lateral side. The absence of a “hook” means that there is no cord-like structure under which the examiner can hook a finger, indicating distal avulsion.4 In one study comparing the hook test to magnetic resonance imaging (MRI) in 33 patients with this suspected injury, the hook test had 100% sensitivity and specificity, while MRI only demonstrated a 92% sensitivity and 85% specificity.4
Imaging Techniques
The need for diagnostic imaging is based somewhat on the location of the rupture—proximal or distal. Ultrasound has been shown to have a high sensitivity and specificity for identifying normal tendons and complete tears of the long head biceps tendon (ie, proximal). It is not sensitive at identifying proximal partial tears, however. For distal ruptures, ultrasound imaging of the distal biceps tendon is technically difficult and not reliable. For patients with suspected distal biceps tendon ruptures, the EP should consult with orthopedic services prior to ordering an MRI. While MRI is considered the gold standard imaging test, it is neither 100% sensitive nor specific. The bottom line is that the absence of pathologic findings on MRI is not sufficient enough to exclude biceps tendon pathology.5
Treatment and Management
Regarding management, the majority of patients with proximal biceps tendon ruptures tend to do well with conservative management. The exception is for younger, active patients who are less willing to accept the cosmetic deformity, or patients whose occupation makes them unable to tolerate minimal weakness or fatigue cramping (eg, carpenters), in which case referral for a surgical repair (tenodesis) may be appropriate.1 However, multiple systematic reviews examining tenotomy vs tenodesis have not shown any functional improvement, only cosmetic.1,6,7
Distal biceps tendon ruptures are usually treated surgically, since conservative management results in a decrease of 30% to 50% supination strength and 20% flexion strength.1,8 This surgery, however, is not without complications. Approximately 20% of the patients will have a minor complication and 5% will have major complications following surgery on the distal biceps tendon.9 It is preferable to operate on distal ruptures less than 4 weeks from the initial injury; otherwise, these injuries may be more difficult to fix, require a graft, and have less predictable outcomes.1 Nonoperative management should be reserved for the elderly or less active patients with multiple comorbidities, especially if the nondominant arm is involved.10
Summary
The PA clearly missed the correct diagnosis on this patient. A more thorough history and focused physical examination would have led to the correct diagnosis sooner, along with earlier surgical repair. It is impossible, however, to know if the outcome would have been any different in this uncommon injury.
A 42-year-old man presented to the ED with left arm pain secondary to an injury he sustained at work. The patient stated that he had been helping to lift a heavy steel beam at a construction site when he experienced abrupt onset of pain in his left arm. He further noted that his left arm felt slightly weaker than normal after the injury.
The patient was left-hand dominant, denied any other injury, was otherwise in good health, and on no medications. With the exception of an appendectomy at age 12 years, his medical history was unremarkable. Regarding his social history, he admitted to smoking one pack of cigarettes per day, and to occasional alcohol consumption. He had no known drug allergies.
On physical examination, the patient’s vital signs were: blood pressure, 125/76 mm Hg; heart rate, 78 beats/min; respiratory rate, 16 breaths/min; and temperature, 98.6°F. Oxygen saturation was 99% on room air.
Examination of the patient’s left shoulder revealed no swelling or tenderness; he was able to fully internally/externally rotate the left shoulder, and lift his left hand above his head. The patient did have tenderness along the biceps area of the left arm, but no tenderness in the triceps area. The left elbow was tender in the antecubital fossa, but without swelling. He had full range of motion of the left elbow but with some pain. He likewise had full range of motion in his left wrist, but no tenderness or swelling. The left radial pulse was 2+. The patient had 5/5 grip strength with the left hand and good capillary refill.
The physician assistant (PA) evaluating the patient diagnosed an arm strain. At discharge, he referred the patient to an occupational health physician (OHP) for follow-up. He also instructed the patient to take ibuprofen 400 mg every 6 to 8 hours, and to limit use of his left arm for 3 days.
The patient followed up with the OHP approximately 3 weeks after discharge from the ED. The OHP was concerned the patient had experienced a distal biceps tendon rupture and referred the patient emergently to an orthopedic surgeon. The orthopedic surgeon saw the patient the next day, agreed with the diagnosis of a distal biceps tendon rupture, and attempted surgical repair the following day. The orthopedic surgeon informed the patient prior to the surgery that the delay in the referral and surgery could result in a poor functional outcome. The patient did have a difficult recovery period, and a second surgery was required, which did not result in any significant functional improvement.
The plaintiff sued the treating PA and supervising emergency physician (EP) for failure to properly diagnose the biceps tendon rupture, failure to appreciate the existence of a 3-week window of opportunity to repair the distal biceps tendon rupture, and failure to obtain an urgent orthopedic referral. The experts for the defense argued that the poor outcome was not a consequence of any delay in diagnosis or surgical repair. In addition, the defense disputed the existence of a 3-week window of opportunity for successful repair of a distal biceps tendon rupture. The jury returned a defense verdict.
Discussion
Proximal and Distal Biceps Tendon Ruptures
While both proximal and distal biceps tendon ruptures involve the biceps brachii, they are managed differently and have the potential for very different outcomes.1 At its proximal attachment, the biceps has two distinct tendinous insertions—the long head and the short head. For the distal attachment, the two muscle bellies unite at the midshaft of the humerus and attach as a single tendon on the radial tuberosity. In general, 96% of biceps tendon ruptures involve the long head, 1% involve the short head, and only 3% involve the distal tendon.1 Biceps tendon ruptures occur more commonly in men, patients who use anabolic steroids, cigarette smokers, patient history of tendinopathy, or patients who have a rotator cuff tear.1 Biceps tendon ruptures have not been found to be associated with statin use.2 The mechanism of injury includes heavy-lifting activities, such as weight lifting and rock climbing. However, when associated with a tendinopathy, minimal force may be involved.1
Signs and Symptoms
For proximal biceps tendon rupture, patients usually present with an acute or gradual onset of pain, swelling, and bruising of the upper arm and shoulder. Occasionally, if there is an inciting event, the patient may describe hearing or feeling a “popping” or “snapping” sound. On physical examination, the patient may exhibit a “Popeye” sign—a bulge in the distal biceps area due to the retracted biceps muscle belly. There is also tenderness along the biceps.
On testing, it has been estimated that patients can experience strength loss of approximately 30% with elbow flexion.1 In contrast, patients with distal biceps tendon ruptures usually complain of pain, swelling, and possibly bruising in the antecubital fossa, as was the case with this patient. Similar to proximal ruptures, the patient may admit to hearing or feeling a “popping” sound if there is an inciting event. The patient may exhibit a “reverse Popeye” deformity, with a bulge in the proximal arm secondary to retraction of the biceps muscle belly proximally.1
Diagnosis
There are two tests that can be performed to assist in making the diagnosis—the biceps squeeze test and the hook test.
Biceps Squeeze Test. The first test to assess for distal biceps tendon rupture is the biceps squeeze test, in which the clinician forcefully squeezes the patient’s biceps muscle to observe for forearm flexion/supination. This test is similar in principle to the Thompson test for Achilles tendon rupture. If there is no forearm movement, the injury is suspicious for a complete distal biceps tendon rupture. In one observational study of this test, 21 of 22 patients with a positive biceps squeeze test were found to have a complete distal biceps tendon tear at surgery.3
Hook Test. The second test is the hook test. While the patient actively supinates with the elbow flexed at 900, an intact hook test permits the examiner to “hook” his or her index finger under the intact biceps tendon from the lateral side. The absence of a “hook” means that there is no cord-like structure under which the examiner can hook a finger, indicating distal avulsion.4 In one study comparing the hook test to magnetic resonance imaging (MRI) in 33 patients with this suspected injury, the hook test had 100% sensitivity and specificity, while MRI only demonstrated a 92% sensitivity and 85% specificity.4
Imaging Techniques
The need for diagnostic imaging is based somewhat on the location of the rupture—proximal or distal. Ultrasound has been shown to have a high sensitivity and specificity for identifying normal tendons and complete tears of the long head biceps tendon (ie, proximal). It is not sensitive at identifying proximal partial tears, however. For distal ruptures, ultrasound imaging of the distal biceps tendon is technically difficult and not reliable. For patients with suspected distal biceps tendon ruptures, the EP should consult with orthopedic services prior to ordering an MRI. While MRI is considered the gold standard imaging test, it is neither 100% sensitive nor specific. The bottom line is that the absence of pathologic findings on MRI is not sufficient enough to exclude biceps tendon pathology.5
Treatment and Management
Regarding management, the majority of patients with proximal biceps tendon ruptures tend to do well with conservative management. The exception is for younger, active patients who are less willing to accept the cosmetic deformity, or patients whose occupation makes them unable to tolerate minimal weakness or fatigue cramping (eg, carpenters), in which case referral for a surgical repair (tenodesis) may be appropriate.1 However, multiple systematic reviews examining tenotomy vs tenodesis have not shown any functional improvement, only cosmetic.1,6,7
Distal biceps tendon ruptures are usually treated surgically, since conservative management results in a decrease of 30% to 50% supination strength and 20% flexion strength.1,8 This surgery, however, is not without complications. Approximately 20% of the patients will have a minor complication and 5% will have major complications following surgery on the distal biceps tendon.9 It is preferable to operate on distal ruptures less than 4 weeks from the initial injury; otherwise, these injuries may be more difficult to fix, require a graft, and have less predictable outcomes.1 Nonoperative management should be reserved for the elderly or less active patients with multiple comorbidities, especially if the nondominant arm is involved.10
Summary
The PA clearly missed the correct diagnosis on this patient. A more thorough history and focused physical examination would have led to the correct diagnosis sooner, along with earlier surgical repair. It is impossible, however, to know if the outcome would have been any different in this uncommon injury.
1. Smith D. Proximal versus distal biceps tendon ruptures: when to refer. BCMJ. 2017;59(2):85.
2. Spoendlin J, Layton JB, Mundkur M, Meier C, Jick SS, Meier CR. The risk of achilles or biceps tendon rupture in new statin users: a propensity score-matched sequential cohort study. Drug Safety. 2016;39(12):1229-1237. doi:10.1007/s40264-016-0462-5.
3. Ruland RT, Dunbar RP, Bowen JD. The biceps squeeze test for diagnosis of distal biceps tendon ruptures. Clin Orthop Relat Res. 2005;437:128-131.
4. O’Driscoll SW, Goncalves LBJ, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35(11):1865-1969. doi:10.1177/0363546507305016.
5. Malavolta EA, Assunção JH, Guglielmetti CL, de Souza FF, Gracitelli ME, Ferreira Neto AA. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol. 2015;84(11):2250-2254. doi:10.1016/j.ejrad.2015.07.031.
6. Tangari M, Carbone S, Gallo M, Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20(3):409-413. doi:10.1016/j.jse.2010.08.008.
7. Eakin JL, Bailey JR, Dewing CB, Provencher MT. Subpectoral biceps tenodesis. Oper Tech Sports Med. 2012;20(3):244-252.
8. Thomas JR, Lawton JN. Biceps and triceps ruptures in athletes. Hand Clin. 2017;33(1):35-46. doi:10.1016/j.hcl.2016.08.019.
9. Beks RB, Claessen FM, Oh LS, Ring D, Chen NC. Factors associated with adverse events after distal biceps tendon repair or reconstruction. J Shoulder Elbow Surg. 2016;25(8):1229-1234. doi:10.1016/j.jse.2016.02.032.
10. Savin DD, Watson J, Youderian AR, et al. Surgical management of acute distal biceps tendon ruptures. J Bone Joint Surg. 2017;3(9):785-796. doi:0.2106/JBJS.17.00080.
1. Smith D. Proximal versus distal biceps tendon ruptures: when to refer. BCMJ. 2017;59(2):85.
2. Spoendlin J, Layton JB, Mundkur M, Meier C, Jick SS, Meier CR. The risk of achilles or biceps tendon rupture in new statin users: a propensity score-matched sequential cohort study. Drug Safety. 2016;39(12):1229-1237. doi:10.1007/s40264-016-0462-5.
3. Ruland RT, Dunbar RP, Bowen JD. The biceps squeeze test for diagnosis of distal biceps tendon ruptures. Clin Orthop Relat Res. 2005;437:128-131.
4. O’Driscoll SW, Goncalves LBJ, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35(11):1865-1969. doi:10.1177/0363546507305016.
5. Malavolta EA, Assunção JH, Guglielmetti CL, de Souza FF, Gracitelli ME, Ferreira Neto AA. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol. 2015;84(11):2250-2254. doi:10.1016/j.ejrad.2015.07.031.
6. Tangari M, Carbone S, Gallo M, Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20(3):409-413. doi:10.1016/j.jse.2010.08.008.
7. Eakin JL, Bailey JR, Dewing CB, Provencher MT. Subpectoral biceps tenodesis. Oper Tech Sports Med. 2012;20(3):244-252.
8. Thomas JR, Lawton JN. Biceps and triceps ruptures in athletes. Hand Clin. 2017;33(1):35-46. doi:10.1016/j.hcl.2016.08.019.
9. Beks RB, Claessen FM, Oh LS, Ring D, Chen NC. Factors associated with adverse events after distal biceps tendon repair or reconstruction. J Shoulder Elbow Surg. 2016;25(8):1229-1234. doi:10.1016/j.jse.2016.02.032.
10. Savin DD, Watson J, Youderian AR, et al. Surgical management of acute distal biceps tendon ruptures. J Bone Joint Surg. 2017;3(9):785-796. doi:0.2106/JBJS.17.00080.
What Are You Worth? The Basics of Business in Health Care
Dana, an adult nurse practitioner, has been working for two years at a large, suburban primary care practice owned by the regional hospital system. She sees too many patients per day, never has enough time to chart properly, and is concerned by the expanding role of the medical assistants. She sees salary postings on social media and feels she is underpaid. She fantasizes about owning her own practice but would settle for making more money. She’s heard that some NPs have profit-sharing, but she’s not exactly sure what that means.
Kelsey, a PA, is looking for his first job out of school. He’s been offered a full-time, salaried position with benefits at an urgent care center, but he doesn’t know if this is a good deal for him or not. The family physicians there make $85,000 more per year than the PAs, although the roles are quite similar.
DOWN TO BUSINESS
The US health care crisis is, fundamentally, a financial crisis; our system is comprised of both for-profit and not-for-profit (NFP) businesses. Every day, NPs and PAs are making decisions that affect their job satisfaction, performance, and retention. Many lack confidence in their ability to make good decisions about their salaries, because they don’t understand the business of health care.1 To survive and thrive, NPs and PAs must understand the basics of the business end.2
So, what qualifies as a business? Any commercial, retail, or professional entity that earns and spends money. It doesn’t matter if it is a for-profit or NFP organization; it can’t survive unless it makes more money than it spends. How that money is earned varies, from selling services and/or goods to receiving grants, income from interest or rentals, or government subsidies.
The major difference between a for-profit and a NFP organization is who controls the money.3 The owners of a for-profit company control the profits, which may be split among the owners or reinvested in the company. A NFP business may use its profits to provide charity care, offset losses of other programs, or invest in capital improvements (eg, new building, equipment). How the profits are to be used is outlined in the business goals or the mission statement of the entity. There are also federal and state regulations for both types of businesses; visit the Internal Revenue Service website for details (www.irs.gov/charities-non-profits; www.irs.gov/businesses/small-businesses-self-employed).
HOW YOU GET PAID FOR SERVICES
As a PA or NP, you generate income for your employer regardless of whether you work for a for-profit or NFP business. Your patients are billed for services rendered.
If you work for a fee-for-service or NFP practice with insurance contracts, the bill gets coded and electronically submitted for payment. Each insurer, whether private or government (ie, Medicare or Medicaid), has established what they will reimburse you for that service. The reimbursement rate is part of your contract with that insurer. Rates are determined based on your profession, licensure, geographic locale, type of facility, and the market rate. An insurance representative would be able to tell you your reimbursement rate for the most common procedure codes you use. (Your employer has this information but may or may not share it with you.) Medicare rates can be found online at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/.
If you work for a direct-pay practice, you collect what you bill directly from the patient, often at the time of the visit. A direct-pay practice does not have insurance contracts and does not bill insurers for patients who have insurance; rather, they provide a billing statement with procedure and diagnostic codes and NPI numbers to the patient, who can submit it directly to their insurer. If the insurer accepts out-of-network providers (those with whom they have no contract), they will reimburse the patient directly.
If you work in a fee-for-service or NFP practice, you may see patients who do not have insurance or who have very high deductibles and pay cash for their services. This does not make it a direct-pay practice. Also, by law, fee-for-service and NFP practices can only have one fee schedule for the entire practice. So, you can’t charge one patient $55 for a flu shot and another patient $25. These practices can offer discounts for cash payments at the time of service, to help reduce the set fees, if they choose.
TALKIN’ ’BOUT YOUR (REVENUE) GENERATION
To know how much you can negotiate for your salary and benefits—your total compensation package (of which benefits is often about 30%)—it is critical to know how much revenue you can generate for your employer.4 How can you figure this out?
If you are already working, you can ask your practice manager for some data. In some practices, this information is readily shared, perhaps as a means to boost productivity and even allow comparison between employees. If your practice manager is not forthcoming, you can collect the relevant information yourself. It may be challenging, but it is vital information to have. You need to know how many patients you see per day (keep a log for a month), what their payment source is (specific insurer or self-pay), and what the reimbursement rates are. Although reimbursement rates are deemed confidential per your insurance contract and therefore can’t be shared, you can find Medicare and Medicaid rates online. You can also call the provider representative from each insurer and ask for your reimbursement rates for your five or so most commonly used codes.
Another consideration is payment received (ie, not just what you charge). Do all patients pay everything they owe? Not always. Understand the difference between what you bill, what is allowed, and what you collect. The percentage of what is not collected is called the uncollectable rate. Factor that in.
Furthermore, how much do you contribute to the organization by testing? Dana works for a primary care clinic within a hospital system. Let’s assume her practice doesn’t offer colonoscopies or mammograms; how many referrals does she make to the hospital system for these tests? While she may not know the hospital’s profit margin on them, she can figure out how many she orders in a year. And what about the PA who works for a surgeon? Does he or she do the post-surgical checks? How much time does that save the surgeon, who can be providing higher revenue–producing services with the time saved? That contributes to the income of the practice, too! These are points you can make to justify your salary.
MIX IT UP
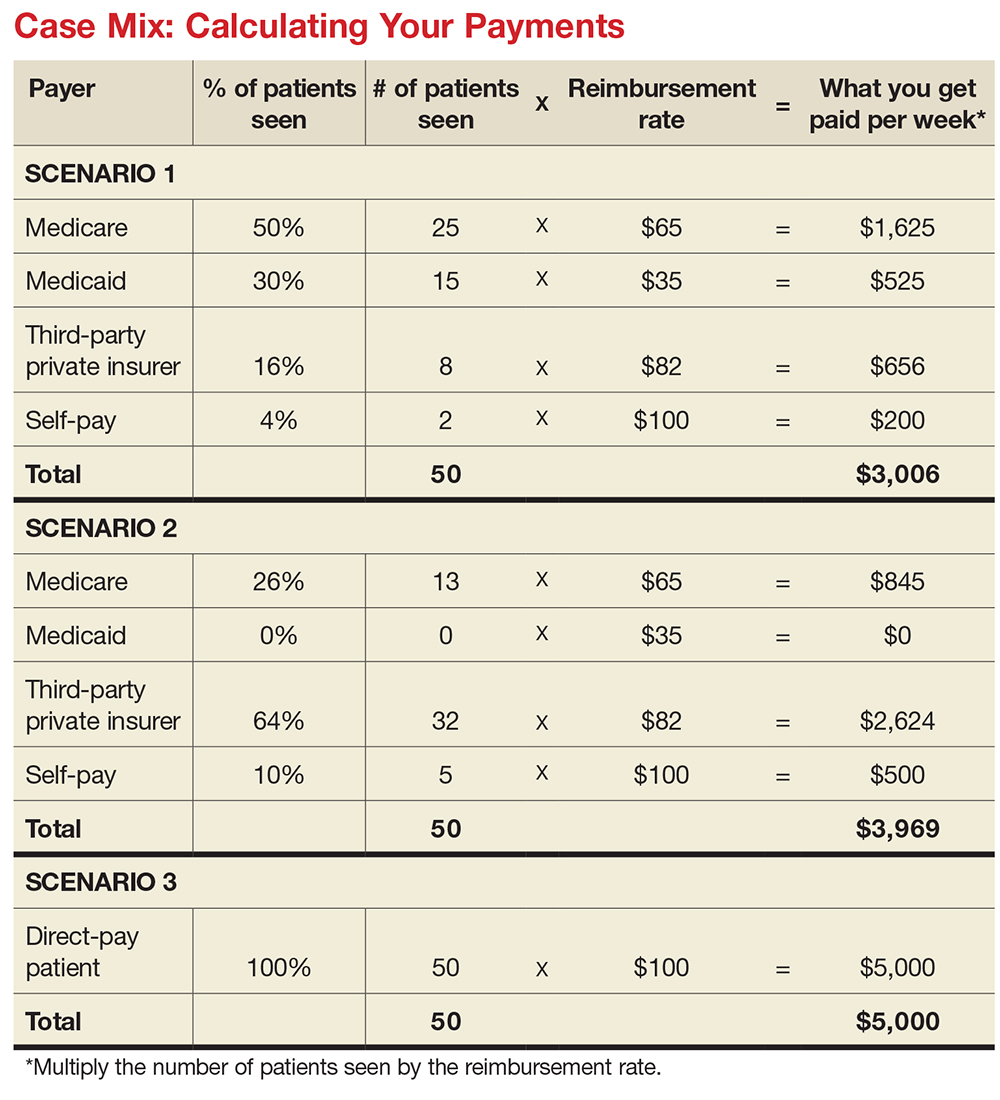
There is another major consideration for computing your financial contribution to the practice: understanding case mix. Let’s say your most common visit is billed as a 99213 and you charge $100 for this visit. You use this code 50 times in a week. Do you collect $100 x 50 or $5,000 per week? If you have a direct-pay practice and you collect all of it, yes, you will. If your practice accepts insurance, the number of patients you see with different insurers is called your case mix.
Let’s look at the impact of case mix on what you generate. Remember, it will take you about the same amount of time and effort to see these patients regardless of their insurer. Ask your practice manager what your case mix is. If he/she is not willing to share this information, you can get an estimate by looking at the demographics of your patient community. How many are older than 65? How many are on public assistance? Community needs assessments will provide you with this data; you can also check the patient’s chart or ask what insurance they have and add this to your log.
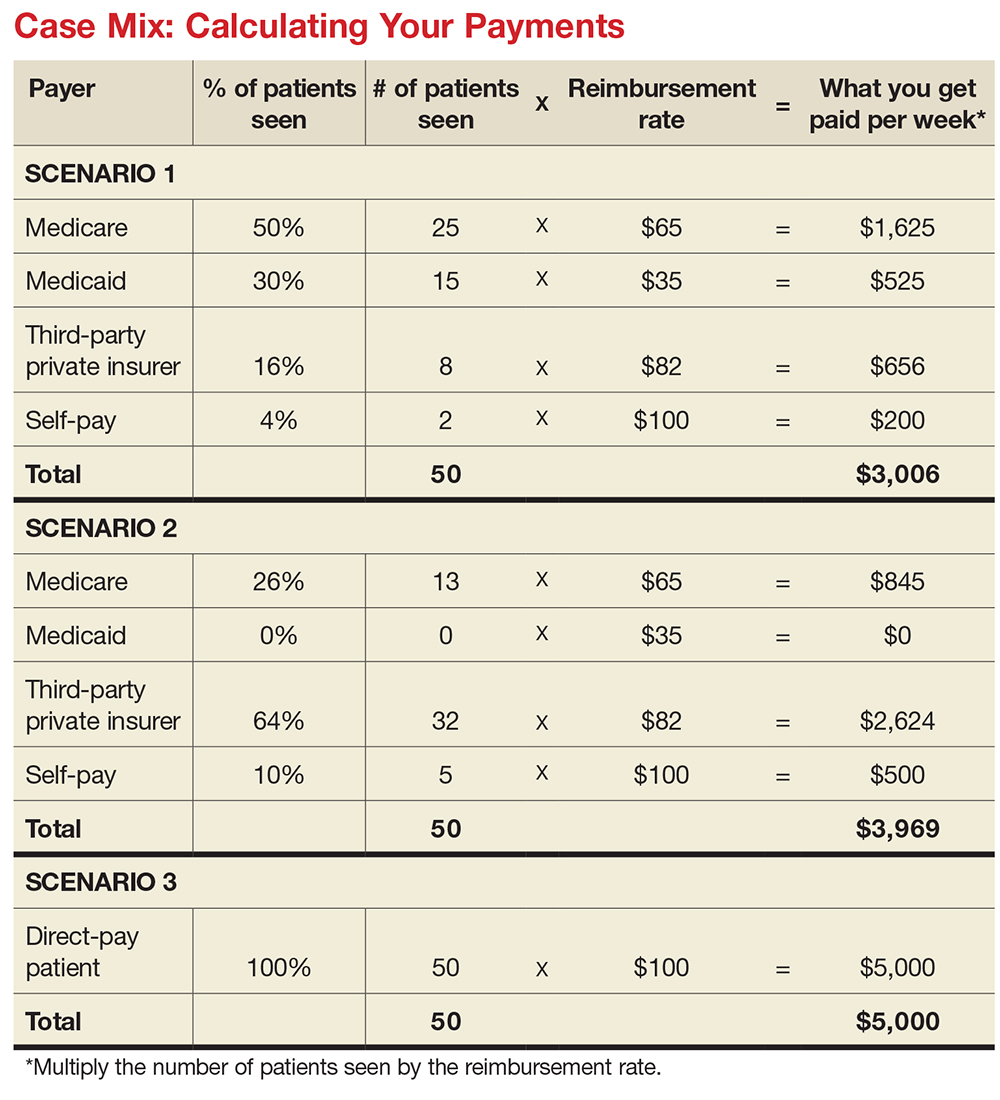
How much will you generate by seeing 50 patients in a week for a 99213 for which you charge $100? Let’s start with sample (not actual) base rates to illustrate the concept: $65 for Medicare, $35 for Medicaid, $82 for third-party private insurance, and $100 for self-pay.
Now let’s explore how case mix impacts revenue, with three different scenarios (see charts). In Scenario 1, 50% of your patients have Medicare, 30% have Medicaid, 16% have third-party private insurance, and 4% pay cash (self-pay). In Scenario 2, 26% have Medicare, 0% have Medicaid, 64% have private insurance, and 10% self-pay. In Scenario 3, your practice is a direct-pay practice with 100% self-payers and a 0% uncollectable rate.
In Scenario 1, with a case mix of 80% of your patient payments from Medicare or Medicaid, you generate $3,006 per week. If you see patients 48 weeks per year, you generate $144,288. In Scenario 2, with a case mix of 74% of your patient payments from private insurance, you generate $3,969 per week. In a year, you generate $190,512. And in Scenario 3, with 100% direct-pay patients, you generate $5,000 per week or $240,000 per year.
This example illustrates how case mix influences health care business, based on the current US reimbursement system. If you work for a practice that serves mostly Medicare and Medicaid patients, you do not command the same salary as an NP or PA who works for a direct-pay practice or one with a majority of privately insured patients.
OVERHEAD, OR IN OVER YOUR HEAD?
Now you have a better understanding of what your worth is to a practice. But what does it cost a practice to employ you? What’s your practice’s overhead?
Overhead includes the cost of processing claims; salaries and benefits; physician collaboration, if needed; rent, utilities, insurance, and depreciation. Overhead rates can range from 20% to 50%—meaning, if you generate $225,000 in revenue, it costs $45,000 to $112,500 to employ you. That leaves $112,500 (with higher overhead) to $180,000 (with lower overhead) for your salary. This revenue generation is an average: Many clinicians generate more than $225,000, while new graduates often generate less.
But in addition to generating more revenue, it can be beneficial to examine what you can do to help decrease the practice overhead. Because the bulk of overhead costs is salary, consider how many full-time-equivalent employees are needed to support you. Some NPs and PAs work with a full-time medical assistant or nurse, while others function very efficiently without one.
While providers like Dana and Kelsey can’t control what their practices pay for rent, utilities, or staffing, they can suggest improvements. Suggestions about scheduling, decreasing no-show rates, and improving recalls, immunization rates, and follow-up visits can all help increase revenue by decreasing day-to-day operating costs.
CONCLUSION
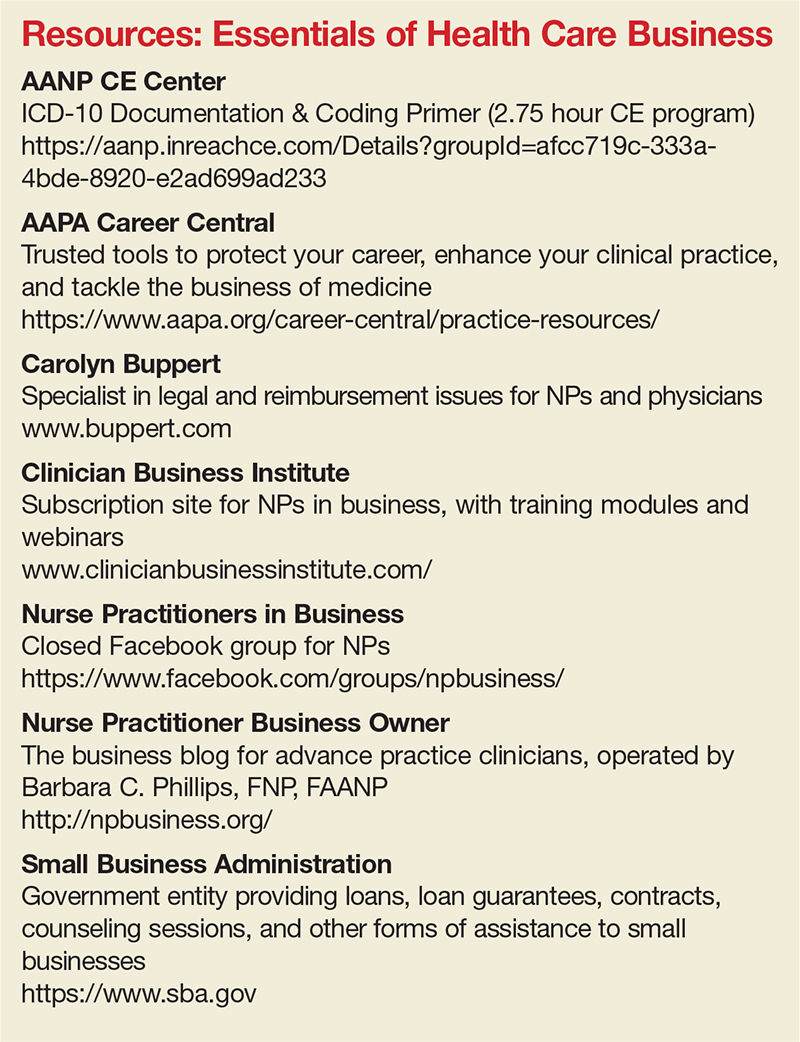
Most NPs and PAs went into their profession to help people—but that altruistic goal doesn’t mean you have to undervalue your own worth. Understanding the basic business of health care can help you negotiate your salary, maximize your income, and create new revenue models for patient care. While this may seem daunting to anyone who went to nursing or medical school, there are great resources to help you educate yourself on the essentials of health care business (see box).
Understanding the infrastructure of the health care system will help NPs and PAs become leaders who can impact health care change. These basic business skills are necessary to ensure fair and full compensation for the roles they play.
1. LaFevers D, Ward-Smith P, Wright W. Essential nurse practitioner business knowledge: an interprofessional perspective. J Am Assoc Nurse Pract. 2015;4:181-184.
2. Buppert C. Nurse Practitioner’s Business and Legal Guide. 6th ed. Burlington, MA: Jones and Bartlett Learning; 2018: 311-324.
3. Fritz J. How is a nonprofit different from a for-profit business? Getting beyond the myths. The Balance. April 3, 2017. www.thebalance.com/how-is-a-nonprofit-different-from-for-profit-business-2502472. Accessed November 20, 2017.
4. Dillon D, Hoyson P. Beginning employment: a guide for the new nurse practitioner. J Nurse Pract. 2014;1:55-59.
Dana, an adult nurse practitioner, has been working for two years at a large, suburban primary care practice owned by the regional hospital system. She sees too many patients per day, never has enough time to chart properly, and is concerned by the expanding role of the medical assistants. She sees salary postings on social media and feels she is underpaid. She fantasizes about owning her own practice but would settle for making more money. She’s heard that some NPs have profit-sharing, but she’s not exactly sure what that means.
Kelsey, a PA, is looking for his first job out of school. He’s been offered a full-time, salaried position with benefits at an urgent care center, but he doesn’t know if this is a good deal for him or not. The family physicians there make $85,000 more per year than the PAs, although the roles are quite similar.
DOWN TO BUSINESS
The US health care crisis is, fundamentally, a financial crisis; our system is comprised of both for-profit and not-for-profit (NFP) businesses. Every day, NPs and PAs are making decisions that affect their job satisfaction, performance, and retention. Many lack confidence in their ability to make good decisions about their salaries, because they don’t understand the business of health care.1 To survive and thrive, NPs and PAs must understand the basics of the business end.2
So, what qualifies as a business? Any commercial, retail, or professional entity that earns and spends money. It doesn’t matter if it is a for-profit or NFP organization; it can’t survive unless it makes more money than it spends. How that money is earned varies, from selling services and/or goods to receiving grants, income from interest or rentals, or government subsidies.
The major difference between a for-profit and a NFP organization is who controls the money.3 The owners of a for-profit company control the profits, which may be split among the owners or reinvested in the company. A NFP business may use its profits to provide charity care, offset losses of other programs, or invest in capital improvements (eg, new building, equipment). How the profits are to be used is outlined in the business goals or the mission statement of the entity. There are also federal and state regulations for both types of businesses; visit the Internal Revenue Service website for details (www.irs.gov/charities-non-profits; www.irs.gov/businesses/small-businesses-self-employed).
HOW YOU GET PAID FOR SERVICES
As a PA or NP, you generate income for your employer regardless of whether you work for a for-profit or NFP business. Your patients are billed for services rendered.
If you work for a fee-for-service or NFP practice with insurance contracts, the bill gets coded and electronically submitted for payment. Each insurer, whether private or government (ie, Medicare or Medicaid), has established what they will reimburse you for that service. The reimbursement rate is part of your contract with that insurer. Rates are determined based on your profession, licensure, geographic locale, type of facility, and the market rate. An insurance representative would be able to tell you your reimbursement rate for the most common procedure codes you use. (Your employer has this information but may or may not share it with you.) Medicare rates can be found online at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/.
If you work for a direct-pay practice, you collect what you bill directly from the patient, often at the time of the visit. A direct-pay practice does not have insurance contracts and does not bill insurers for patients who have insurance; rather, they provide a billing statement with procedure and diagnostic codes and NPI numbers to the patient, who can submit it directly to their insurer. If the insurer accepts out-of-network providers (those with whom they have no contract), they will reimburse the patient directly.
If you work in a fee-for-service or NFP practice, you may see patients who do not have insurance or who have very high deductibles and pay cash for their services. This does not make it a direct-pay practice. Also, by law, fee-for-service and NFP practices can only have one fee schedule for the entire practice. So, you can’t charge one patient $55 for a flu shot and another patient $25. These practices can offer discounts for cash payments at the time of service, to help reduce the set fees, if they choose.
TALKIN’ ’BOUT YOUR (REVENUE) GENERATION
To know how much you can negotiate for your salary and benefits—your total compensation package (of which benefits is often about 30%)—it is critical to know how much revenue you can generate for your employer.4 How can you figure this out?
If you are already working, you can ask your practice manager for some data. In some practices, this information is readily shared, perhaps as a means to boost productivity and even allow comparison between employees. If your practice manager is not forthcoming, you can collect the relevant information yourself. It may be challenging, but it is vital information to have. You need to know how many patients you see per day (keep a log for a month), what their payment source is (specific insurer or self-pay), and what the reimbursement rates are. Although reimbursement rates are deemed confidential per your insurance contract and therefore can’t be shared, you can find Medicare and Medicaid rates online. You can also call the provider representative from each insurer and ask for your reimbursement rates for your five or so most commonly used codes.
Another consideration is payment received (ie, not just what you charge). Do all patients pay everything they owe? Not always. Understand the difference between what you bill, what is allowed, and what you collect. The percentage of what is not collected is called the uncollectable rate. Factor that in.
Furthermore, how much do you contribute to the organization by testing? Dana works for a primary care clinic within a hospital system. Let’s assume her practice doesn’t offer colonoscopies or mammograms; how many referrals does she make to the hospital system for these tests? While she may not know the hospital’s profit margin on them, she can figure out how many she orders in a year. And what about the PA who works for a surgeon? Does he or she do the post-surgical checks? How much time does that save the surgeon, who can be providing higher revenue–producing services with the time saved? That contributes to the income of the practice, too! These are points you can make to justify your salary.
MIX IT UP
There is another major consideration for computing your financial contribution to the practice: understanding case mix. Let’s say your most common visit is billed as a 99213 and you charge $100 for this visit. You use this code 50 times in a week. Do you collect $100 x 50 or $5,000 per week? If you have a direct-pay practice and you collect all of it, yes, you will. If your practice accepts insurance, the number of patients you see with different insurers is called your case mix.
Let’s look at the impact of case mix on what you generate. Remember, it will take you about the same amount of time and effort to see these patients regardless of their insurer. Ask your practice manager what your case mix is. If he/she is not willing to share this information, you can get an estimate by looking at the demographics of your patient community. How many are older than 65? How many are on public assistance? Community needs assessments will provide you with this data; you can also check the patient’s chart or ask what insurance they have and add this to your log.
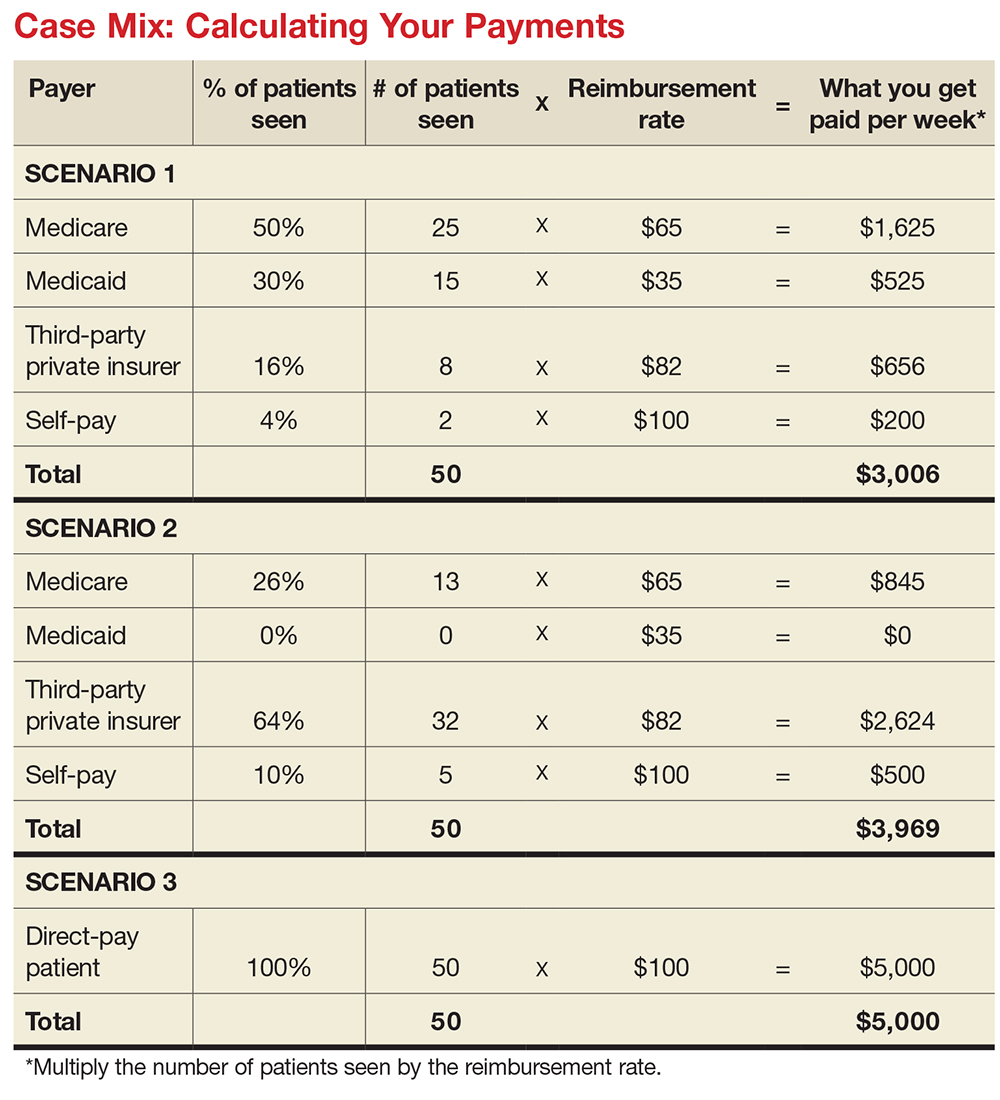
How much will you generate by seeing 50 patients in a week for a 99213 for which you charge $100? Let’s start with sample (not actual) base rates to illustrate the concept: $65 for Medicare, $35 for Medicaid, $82 for third-party private insurance, and $100 for self-pay.
Now let’s explore how case mix impacts revenue, with three different scenarios (see charts). In Scenario 1, 50% of your patients have Medicare, 30% have Medicaid, 16% have third-party private insurance, and 4% pay cash (self-pay). In Scenario 2, 26% have Medicare, 0% have Medicaid, 64% have private insurance, and 10% self-pay. In Scenario 3, your practice is a direct-pay practice with 100% self-payers and a 0% uncollectable rate.
In Scenario 1, with a case mix of 80% of your patient payments from Medicare or Medicaid, you generate $3,006 per week. If you see patients 48 weeks per year, you generate $144,288. In Scenario 2, with a case mix of 74% of your patient payments from private insurance, you generate $3,969 per week. In a year, you generate $190,512. And in Scenario 3, with 100% direct-pay patients, you generate $5,000 per week or $240,000 per year.
This example illustrates how case mix influences health care business, based on the current US reimbursement system. If you work for a practice that serves mostly Medicare and Medicaid patients, you do not command the same salary as an NP or PA who works for a direct-pay practice or one with a majority of privately insured patients.
OVERHEAD, OR IN OVER YOUR HEAD?
Now you have a better understanding of what your worth is to a practice. But what does it cost a practice to employ you? What’s your practice’s overhead?
Overhead includes the cost of processing claims; salaries and benefits; physician collaboration, if needed; rent, utilities, insurance, and depreciation. Overhead rates can range from 20% to 50%—meaning, if you generate $225,000 in revenue, it costs $45,000 to $112,500 to employ you. That leaves $112,500 (with higher overhead) to $180,000 (with lower overhead) for your salary. This revenue generation is an average: Many clinicians generate more than $225,000, while new graduates often generate less.
But in addition to generating more revenue, it can be beneficial to examine what you can do to help decrease the practice overhead. Because the bulk of overhead costs is salary, consider how many full-time-equivalent employees are needed to support you. Some NPs and PAs work with a full-time medical assistant or nurse, while others function very efficiently without one.
While providers like Dana and Kelsey can’t control what their practices pay for rent, utilities, or staffing, they can suggest improvements. Suggestions about scheduling, decreasing no-show rates, and improving recalls, immunization rates, and follow-up visits can all help increase revenue by decreasing day-to-day operating costs.
CONCLUSION
Most NPs and PAs went into their profession to help people—but that altruistic goal doesn’t mean you have to undervalue your own worth. Understanding the basic business of health care can help you negotiate your salary, maximize your income, and create new revenue models for patient care. While this may seem daunting to anyone who went to nursing or medical school, there are great resources to help you educate yourself on the essentials of health care business (see box).
Understanding the infrastructure of the health care system will help NPs and PAs become leaders who can impact health care change. These basic business skills are necessary to ensure fair and full compensation for the roles they play.
Dana, an adult nurse practitioner, has been working for two years at a large, suburban primary care practice owned by the regional hospital system. She sees too many patients per day, never has enough time to chart properly, and is concerned by the expanding role of the medical assistants. She sees salary postings on social media and feels she is underpaid. She fantasizes about owning her own practice but would settle for making more money. She’s heard that some NPs have profit-sharing, but she’s not exactly sure what that means.
Kelsey, a PA, is looking for his first job out of school. He’s been offered a full-time, salaried position with benefits at an urgent care center, but he doesn’t know if this is a good deal for him or not. The family physicians there make $85,000 more per year than the PAs, although the roles are quite similar.
DOWN TO BUSINESS
The US health care crisis is, fundamentally, a financial crisis; our system is comprised of both for-profit and not-for-profit (NFP) businesses. Every day, NPs and PAs are making decisions that affect their job satisfaction, performance, and retention. Many lack confidence in their ability to make good decisions about their salaries, because they don’t understand the business of health care.1 To survive and thrive, NPs and PAs must understand the basics of the business end.2
So, what qualifies as a business? Any commercial, retail, or professional entity that earns and spends money. It doesn’t matter if it is a for-profit or NFP organization; it can’t survive unless it makes more money than it spends. How that money is earned varies, from selling services and/or goods to receiving grants, income from interest or rentals, or government subsidies.
The major difference between a for-profit and a NFP organization is who controls the money.3 The owners of a for-profit company control the profits, which may be split among the owners or reinvested in the company. A NFP business may use its profits to provide charity care, offset losses of other programs, or invest in capital improvements (eg, new building, equipment). How the profits are to be used is outlined in the business goals or the mission statement of the entity. There are also federal and state regulations for both types of businesses; visit the Internal Revenue Service website for details (www.irs.gov/charities-non-profits; www.irs.gov/businesses/small-businesses-self-employed).
HOW YOU GET PAID FOR SERVICES
As a PA or NP, you generate income for your employer regardless of whether you work for a for-profit or NFP business. Your patients are billed for services rendered.
If you work for a fee-for-service or NFP practice with insurance contracts, the bill gets coded and electronically submitted for payment. Each insurer, whether private or government (ie, Medicare or Medicaid), has established what they will reimburse you for that service. The reimbursement rate is part of your contract with that insurer. Rates are determined based on your profession, licensure, geographic locale, type of facility, and the market rate. An insurance representative would be able to tell you your reimbursement rate for the most common procedure codes you use. (Your employer has this information but may or may not share it with you.) Medicare rates can be found online at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/.
If you work for a direct-pay practice, you collect what you bill directly from the patient, often at the time of the visit. A direct-pay practice does not have insurance contracts and does not bill insurers for patients who have insurance; rather, they provide a billing statement with procedure and diagnostic codes and NPI numbers to the patient, who can submit it directly to their insurer. If the insurer accepts out-of-network providers (those with whom they have no contract), they will reimburse the patient directly.
If you work in a fee-for-service or NFP practice, you may see patients who do not have insurance or who have very high deductibles and pay cash for their services. This does not make it a direct-pay practice. Also, by law, fee-for-service and NFP practices can only have one fee schedule for the entire practice. So, you can’t charge one patient $55 for a flu shot and another patient $25. These practices can offer discounts for cash payments at the time of service, to help reduce the set fees, if they choose.
TALKIN’ ’BOUT YOUR (REVENUE) GENERATION
To know how much you can negotiate for your salary and benefits—your total compensation package (of which benefits is often about 30%)—it is critical to know how much revenue you can generate for your employer.4 How can you figure this out?
If you are already working, you can ask your practice manager for some data. In some practices, this information is readily shared, perhaps as a means to boost productivity and even allow comparison between employees. If your practice manager is not forthcoming, you can collect the relevant information yourself. It may be challenging, but it is vital information to have. You need to know how many patients you see per day (keep a log for a month), what their payment source is (specific insurer or self-pay), and what the reimbursement rates are. Although reimbursement rates are deemed confidential per your insurance contract and therefore can’t be shared, you can find Medicare and Medicaid rates online. You can also call the provider representative from each insurer and ask for your reimbursement rates for your five or so most commonly used codes.
Another consideration is payment received (ie, not just what you charge). Do all patients pay everything they owe? Not always. Understand the difference between what you bill, what is allowed, and what you collect. The percentage of what is not collected is called the uncollectable rate. Factor that in.
Furthermore, how much do you contribute to the organization by testing? Dana works for a primary care clinic within a hospital system. Let’s assume her practice doesn’t offer colonoscopies or mammograms; how many referrals does she make to the hospital system for these tests? While she may not know the hospital’s profit margin on them, she can figure out how many she orders in a year. And what about the PA who works for a surgeon? Does he or she do the post-surgical checks? How much time does that save the surgeon, who can be providing higher revenue–producing services with the time saved? That contributes to the income of the practice, too! These are points you can make to justify your salary.
MIX IT UP
There is another major consideration for computing your financial contribution to the practice: understanding case mix. Let’s say your most common visit is billed as a 99213 and you charge $100 for this visit. You use this code 50 times in a week. Do you collect $100 x 50 or $5,000 per week? If you have a direct-pay practice and you collect all of it, yes, you will. If your practice accepts insurance, the number of patients you see with different insurers is called your case mix.
Let’s look at the impact of case mix on what you generate. Remember, it will take you about the same amount of time and effort to see these patients regardless of their insurer. Ask your practice manager what your case mix is. If he/she is not willing to share this information, you can get an estimate by looking at the demographics of your patient community. How many are older than 65? How many are on public assistance? Community needs assessments will provide you with this data; you can also check the patient’s chart or ask what insurance they have and add this to your log.
How much will you generate by seeing 50 patients in a week for a 99213 for which you charge $100? Let’s start with sample (not actual) base rates to illustrate the concept: $65 for Medicare, $35 for Medicaid, $82 for third-party private insurance, and $100 for self-pay.
Now let’s explore how case mix impacts revenue, with three different scenarios (see charts). In Scenario 1, 50% of your patients have Medicare, 30% have Medicaid, 16% have third-party private insurance, and 4% pay cash (self-pay). In Scenario 2, 26% have Medicare, 0% have Medicaid, 64% have private insurance, and 10% self-pay. In Scenario 3, your practice is a direct-pay practice with 100% self-payers and a 0% uncollectable rate.
In Scenario 1, with a case mix of 80% of your patient payments from Medicare or Medicaid, you generate $3,006 per week. If you see patients 48 weeks per year, you generate $144,288. In Scenario 2, with a case mix of 74% of your patient payments from private insurance, you generate $3,969 per week. In a year, you generate $190,512. And in Scenario 3, with 100% direct-pay patients, you generate $5,000 per week or $240,000 per year.
This example illustrates how case mix influences health care business, based on the current US reimbursement system. If you work for a practice that serves mostly Medicare and Medicaid patients, you do not command the same salary as an NP or PA who works for a direct-pay practice or one with a majority of privately insured patients.
OVERHEAD, OR IN OVER YOUR HEAD?
Now you have a better understanding of what your worth is to a practice. But what does it cost a practice to employ you? What’s your practice’s overhead?
Overhead includes the cost of processing claims; salaries and benefits; physician collaboration, if needed; rent, utilities, insurance, and depreciation. Overhead rates can range from 20% to 50%—meaning, if you generate $225,000 in revenue, it costs $45,000 to $112,500 to employ you. That leaves $112,500 (with higher overhead) to $180,000 (with lower overhead) for your salary. This revenue generation is an average: Many clinicians generate more than $225,000, while new graduates often generate less.
But in addition to generating more revenue, it can be beneficial to examine what you can do to help decrease the practice overhead. Because the bulk of overhead costs is salary, consider how many full-time-equivalent employees are needed to support you. Some NPs and PAs work with a full-time medical assistant or nurse, while others function very efficiently without one.
While providers like Dana and Kelsey can’t control what their practices pay for rent, utilities, or staffing, they can suggest improvements. Suggestions about scheduling, decreasing no-show rates, and improving recalls, immunization rates, and follow-up visits can all help increase revenue by decreasing day-to-day operating costs.
CONCLUSION
Most NPs and PAs went into their profession to help people—but that altruistic goal doesn’t mean you have to undervalue your own worth. Understanding the basic business of health care can help you negotiate your salary, maximize your income, and create new revenue models for patient care. While this may seem daunting to anyone who went to nursing or medical school, there are great resources to help you educate yourself on the essentials of health care business (see box).
Understanding the infrastructure of the health care system will help NPs and PAs become leaders who can impact health care change. These basic business skills are necessary to ensure fair and full compensation for the roles they play.
1. LaFevers D, Ward-Smith P, Wright W. Essential nurse practitioner business knowledge: an interprofessional perspective. J Am Assoc Nurse Pract. 2015;4:181-184.
2. Buppert C. Nurse Practitioner’s Business and Legal Guide. 6th ed. Burlington, MA: Jones and Bartlett Learning; 2018: 311-324.
3. Fritz J. How is a nonprofit different from a for-profit business? Getting beyond the myths. The Balance. April 3, 2017. www.thebalance.com/how-is-a-nonprofit-different-from-for-profit-business-2502472. Accessed November 20, 2017.
4. Dillon D, Hoyson P. Beginning employment: a guide for the new nurse practitioner. J Nurse Pract. 2014;1:55-59.
1. LaFevers D, Ward-Smith P, Wright W. Essential nurse practitioner business knowledge: an interprofessional perspective. J Am Assoc Nurse Pract. 2015;4:181-184.
2. Buppert C. Nurse Practitioner’s Business and Legal Guide. 6th ed. Burlington, MA: Jones and Bartlett Learning; 2018: 311-324.
3. Fritz J. How is a nonprofit different from a for-profit business? Getting beyond the myths. The Balance. April 3, 2017. www.thebalance.com/how-is-a-nonprofit-different-from-for-profit-business-2502472. Accessed November 20, 2017.
4. Dillon D, Hoyson P. Beginning employment: a guide for the new nurse practitioner. J Nurse Pract. 2014;1:55-59.
The end of the line: Concluding your practice when facing serious illness
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
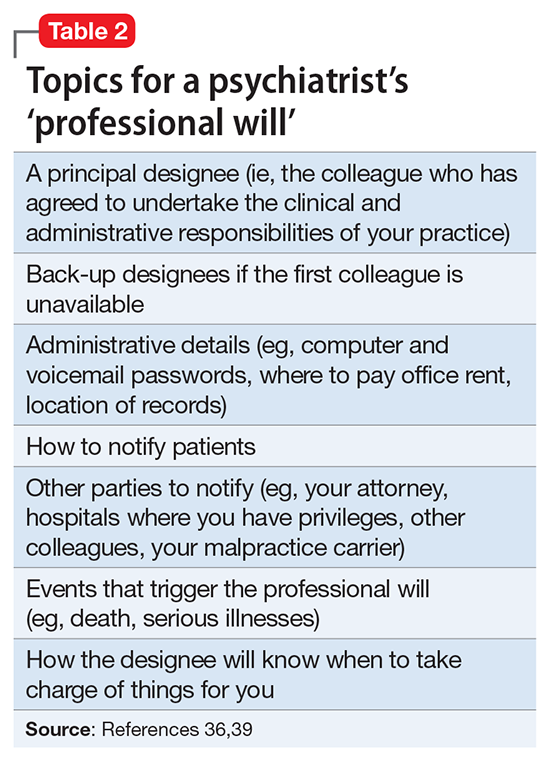
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27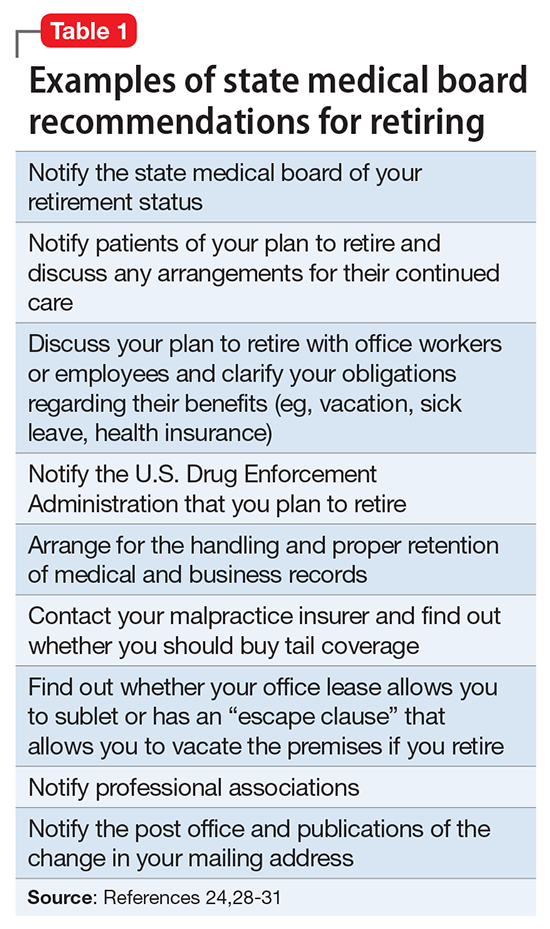
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
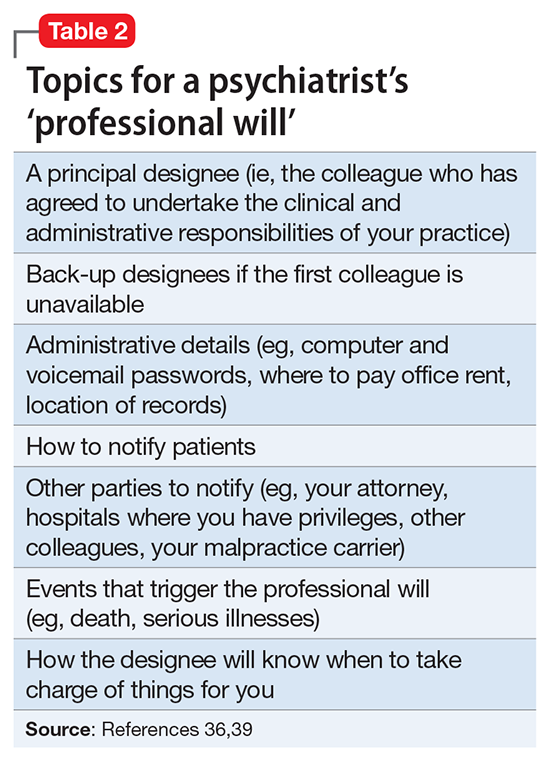
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27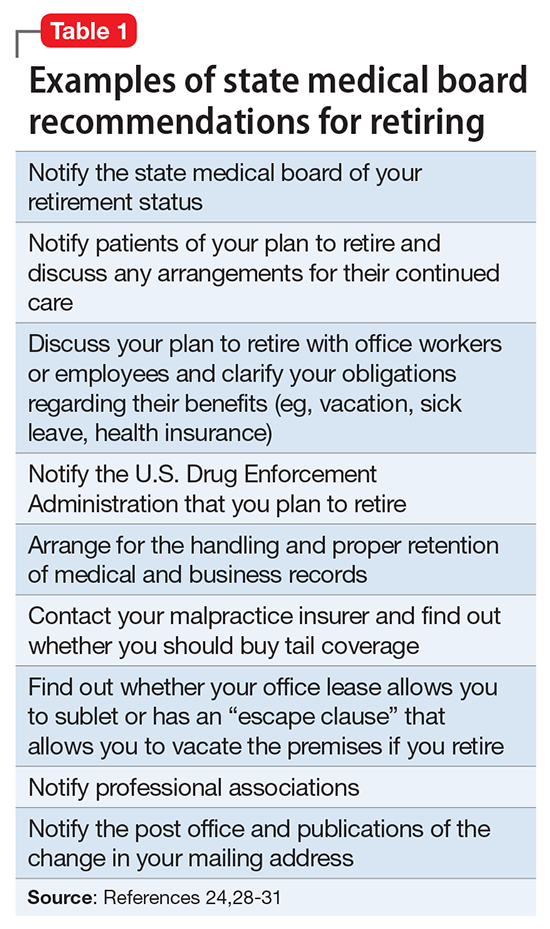
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
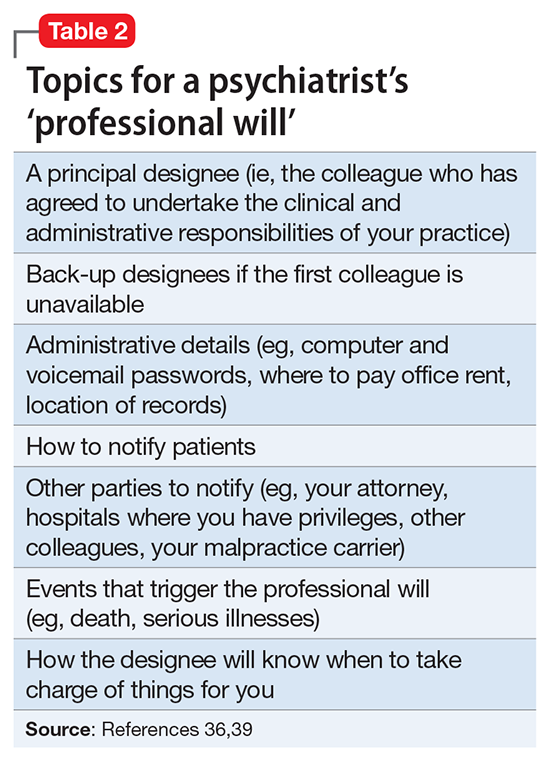
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
Supreme Court decisions in 2017 that affected your practice
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Despite being short-handed (there were only 8 justices for most of the Term), the United States Supreme Court decided a number of important cases during its most recent Term, which concluded on June 27, 2017. Among the 69 cases, several are of particular interest to ObGyns.
1. Arbitration in health care
In Kindred Nursing Centers v Clark, the Court decided an important case involving arbitration in health care.1
At stake. The families of 2 people who died after being in a long-term care facility filed lawsuits against the facility, claiming personal injury, violations of Kentucky statutes regarding long-term care facilities, and wrongful death. However, during admission to the facility, the patients (technically, their agents under a power of attorney) signed an agreement that any disputes would be taken to arbitration. The facility successfully had the lawsuits dismissed.
Final ruling. The Supreme Court agreed that the case had to go to arbitration rather than to court, even though the arbitration clause violated state law. The Federal Arbitration Act (FAA) preempts state law. The Court has been very aggressive in enforcing arbitration agreements and striking down state laws that are inconsistent with the FAA. This case emphasizes that the FAA applies in the health care context.
The case suggests both a warning and an opportunity for health care providers. The warning is that arbitration clauses will be enforced; thoughtlessly entering into arbitration for future disputes may be dangerous. Among other things, the decision of arbitrators is essentially unreviewable. Appellate courts review the decisions of lower courts, but there is no such review in arbitration. Furthermore, arbitration may be stacked in favor of commercial entities that often use arbitrators.
The opportunity for health care providers lies in that it may be possible to include arbitration clauses in agreements with patients. This should be considered only after obtaining legal advice. The agreements should, for example, be consistent with the obligations to patients (in the case of the Kentucky facility, it made clear that accepting the arbitration agreement was not necessary in order to receive care or be admitted to the facility). Because arbitration agreements are becoming ubiquitous and rigorously enforced by federal courts, arbitration is bound to have an important function in health care.
2. Pharmaceuticals
Biologics and biosimilars
Biologics play an important role in health care. Eight of the top 10 selling drugs in 2016 were biologics.2 The case of Sandoz v Amgen involved biosimilar pharmaceuticals, essentially the generics of biologic drugs.3
At stake. While biologics hold great promise in medicine, they are generally very expensive. Just as with generics, brand-name companies (generally referred to as “reference” biologics) want to keep biosimilars off the market for as long as possible, thereby extending the advantages of monopolistic pricing. This Term the Supreme Court considered the statutory rules for licensing biosimilar drugs.
Final ruling. The Court’s decision will allow biosimilar companies to speed up the licensing process by at least 180 days. This is a modest win for patients and their physicians, but the legal issues around biosimilars will need additional attention.
Class action suits
In another case, the Court made it more difficult to file class action suits against pharmaceutical companies in state courts.4 Although this is a fairly technical decision, it is likely to have a significant impact in pharmaceutical liability by limiting classactions.
3. The travel ban
The American College of Obstetricians and Gynecologists joined other medical organizations in an amicus curiae (friend of the court) brief to challenge President Trump’s “travel ban.”5
At stake. The brief argued that the United States “relies upon a significant number of health professionals and scientists who have entered the country through the immigration system.”5
Final ruling. The Court allowed most of the travel ban to stay in place, but did permit entry into the United States by foreign nationals “with a close familial relationship,” or pre-existing ties to US businesses or institutions (such as students who have been admitted to American colleges, workers who have accepted US employment, or lecturers invited to address American audiences).6 Following the Term, the Administration issued a different travel ban, so the issue was taken off the Court’s calendar for the moment. There undoubtedly will be additional chapters to come.
4. Birth certificates and same-sex marriage
In Pavan v Smith, the legal question concerned whether married same-sex couples may have both parents listed on the birth certificate of children born during the marriage.7 Two same-sex couples conceived children through anonymous sperm donation and gave birth in Arkansas. The Department of Health in Arkansas issued birth certificates listing the mother’s name, but refused to list the spouse on the birth certificate.
At stake. The couples brought suit claiming a constitutional right to have both parents listed. In particular, they noted that under Arkansas law, the woman who gives birth is deemed to be the mother. When the woman is married, the husband’s name is “entered on the certificate as the father of the child.”8 The same-sex parents argued that a 2015 decision of the Supreme Court, which held that the Constitution requires states to recognize same-sex marriages, made it clear that same-sex couples should have the benefits of marriage.9 Eventually the case wound its way to the Supreme Court.
Final ruling. The Court held that if the state ordinarily lists the names of both husband and wife on such certificates, then same-sex couples are entitled to have birth certificates listing both parents. The Court noted that laws are unconstitutional if they treat same-sex couples differently than opposite-sex couples. Based on this principle, the Court held that parental birth certificate registration is part of the “constellations of benefits” linked to marriage that the Constitution affords same-sex couples. This ruling applies as a matter of constitutional right in all states.
Read about more interesting Supreme Court decisions
5. Sexual offenders and social media
States struggle to protect children from convicted sex offenders. North Carolina, for example, made it a felony for sex offenders (who had completed their sentences) to use social media sites that “permit minor children to become members or create and maintain personal web pages.”10
At stake. In Packingham v North Carolina, the Court was asked to decide whether this statute violates the First Amendment (free speech) rights of sex offenders.11
Final ruling. The Court held that the North Carolina limitation on sex offenders’ use of social media was too broad. It noted the wide range of political, employment, news, personal, commercial, and religious websites that are off limits to sex offenders under the statute—hardly narrowly tailored. It suggested, however, that it probably would be constitutional for a state to prohibit sex offenders “from engaging in conduct that often presages a sexual crime, like contacting a minor or using a website to gather information about a minor.”11
It was important in this case that the defendant had already served his entire sentence and was “no longer subject to the supervision of the criminal justice system.”11 If he had still been in prison, the state could limit or prohibit his Internet use. Even if he had been on probation or parole (under the supervision of the criminal justice system) the restrictions may well have been permitted. In addition, the state could impose new, narrowly tailored restrictions.
This case is also a reminder that ObGyns are very important in the efforts to eliminate child sexual abuse. All states have laws that require the reporting of known or suspected sexual abuse. In addition to complying with the law, such reports are often critical to discovering and ending the abuse.
6. Transgender rights
The Court had accepted a “transgender bathroom case” in Gloucester County School Board v G.G.12
At stake. This case essentially challenged the Obama Administration’s requirement that schools allow transgender students to use the restrooms in which they feel most comfortable. It was one of the most anticipated cases of the Term, but it essentially disappeared. Following the presidential election, the Department of Education rescinded the earlier guidance on which the case was based.
Final ruling. The Court returned the case to the Fourth Circuit for reconsideration. This issue, however, may reappear before the Court in the form of a claim that the states must provide this accommodation as a matter of federal statutory right, or even Equal Protection.
- In an important First Amendment decision, the Court held that it is a violation of the Freedom of Religion to deny a church-related school access to generally available state grant funds solely because of its religious status (in this case the program funded playground surfacing grants).1
- In several cases, it was apparent that the Court is uncomfortable with the way death penalty cases are handled in some states.2
- Juries may be questioned about racial bias that was expressed during jury deliberations--a substantial change for many courts.3
- The failure of the Patent and Trademark Office (PTO) to register the trademark for the band "The Slants" was a First Amendment violation. One reason that this case was watched was because of the effort of the PTO to deregister the trademark of the Washington Redskins.4
- The Court considered 9 cases involving revoking citizenship, deportation, and cross-border liability (an extraordinary number). Two cases that could change the nature and process of deportation were held over to the next Term for reargument.
- Individualized educational plans under the federal Individuals with Disabilities Education Act (IDEA) must target more than trivial progress for the students.5
References
- Trinity Lutheran Church of Columbia, Inc. v Comer, 582 US 15 577 (2017).
- McAllister S. Death-penalty symposium: A court increasingly uncomfortable with the death penalty. SCOTUSblog.com. http://www.scotusblog.com/2017/06/death-penalty-symposium-court-increasingly-uncomfortable-death-penalty/. Published June 29, 2017. Accessed November 2, 2017.
- Pena-Rodriguez v Colorado, 580 US 15 606 (2017).
- Matal v Tam, 582 US 15 1293 (2017).
- Endrew F v Douglas County School District, RE-1, 580 US 15 827 (2017).
Summary of the Term
The Term was notable for the level of agreement. With 69 decided cases, 41 (69%) were unanimous. In 59 cases (85%), there was a strong consensus, with no more than 2 justices dissenting. Only 7 decisions (10%) were 5 to 4. Justice Kennedy was, as usual, the deciding vote in most of the close cases. He voted in the majority in 97% of the decisions. Justice Gorsuch took the place of Justice Scalia (who passed away in February 2016), so arguably the Court is ideologically close to where it has been for a number of years. Despite rumors that Justice Kennedy would announce his resignation from the Court, neither he nor any other justice has left. The Supreme Court began its new Term on October 2, 2017, with a full complement of 9 justices.
What’s to come
The Court will add cases through much of its new Term, but it has already accepted cases dealing with arbitration agreements (again); public employees’ union dues; immigration (again); the privacy of information held by mobile phone companies; a constitutional challenge to political gerrymandering; bakeries and gay-marriage ceremonies; whistleblowers and Dodd-Frank regulations; sports gambling and the NCAA; and more.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
- Kindred Nursing Centers, LP v Clark, 581 US 16 32 (2017).
- Anderson L. Looking Ahead: Pharma Projections for 2016 - & Beyond. Perma.cc Website. . Reviewed March 30, 2017. Accessed November 2, 2017.
- Sandoz Inc v Amgen Inc, 581 US 15 1039 1195 (2017).
- Bristol-Myers Squibb Co v Superior Court of California, San Francisco County, 582 US 16 466 (2017).
- Trinity FR, Sterling AM, Rogaczewski JD, et al. Motion for Leave to File and Brief for the Association of American Medical Colleges and Others as Amici Curiae Supporting Respondents. SCOTUSblog. http://www.scotusblog.com/wp-content/uploads/2017/06/16-1436-ac-AAMC-supporting-respondents.pdf. Accessed November 2, 2017.
- Donald J. Trump, President of the United States v International Refugee Assistance Project, 582 US 16 1436 (2017).
- Pavan v Smith, 582 US 16 992 (2017).
- Arkansas Code, §20 18 401(f)(1) (2014).
- Obergefell v Hodges, 576 US ___ (2015).
- NC Gen. Stat. Ann. §§14-202.5(a),(e).
- Packingham v North Carolina, 582 US 15 1194 (2017).
- Gloucester County School Board v G.G. SCOTUSblog. http://www.scotusblog.com/case-files/cases/gloucester-county-school-board-v-g-g/. Published March 6, 2017. Accessed November 2, 2017.
Miscarriages after IUD is missing
Miscarriages after IUD is missing: $488,157 verdict
After the patient had miscarriages in 2009 and 2011, she asked her ObGyn if the missing IUD, which she had never seen leave her body, might have contributed to the miscarriages. She was told that the device was not present. No further testing was performed.
After the patient switched providers in 2013, an abdominal x-ray located the IUD. The patient became pregnant after the IUD was successfully removed.
PATIENT'S CLAIM:
The patient sued the ObGyn and his clinic for personal injury and wrongful death of the unborn fetuses. She claimed that it is below the standard of care not to perform an abdominal x-ray when a patient's IUD is missing.
The patient's attorney objected to the tests of the miscarried fetuses, contending that the tissues were sent without consent and that misinformation was conveyed on the pathology requisition.
DEFENDANTS' DEFENSE:
The standard of care set by the American College of Obstetricians and Gynecologists (ACOG) did not specify the use of an abdominal x-ray until Practice Bulletin No. 121 in July 2011 stated that the location of a lost IUD should be confirmed by x-ray.1
The IUD did not produce the miscarriages; testing of remains of 2 miscarried fetuses showed trisomic abnormalities that could not be attributed to the IUD.
The defense countered the patient's attorney that the testing forms had the patient's signed consent and that nothing was misrepresented on the forms.
VERDICT:
A Missouri defense verdict was returned for the wrongful death counts, but the jury awarded the patient $488,157 on the injury claim.
Reference
- Espey E, Singh RH; Committee on Practice Bulletins--Gynecology. American College of Gynecologists and Obstetricians Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184-196.
Related article:
Pregnancy test missed before IUD placement? Your liability.
Needle left behind during mastectomy reconstruction
After a woman was diagnosed with invasive ductal cancer in her left breast, she underwent a double mastectomy with simple mastectomy reconstruction on the left breast. During the operation, the surgical count could not account for 1 pop-off needle. The surgeon searched for the missing needle and ordered an x-ray but the needle could not be located. The surgeon did not tell the patient that the needle count was incomplete.
The patient underwent several other breast reconstruction procedures and the needle was never found.
Five years after the initial surgery, the needle was discovered and surgically removed.
PATIENT'S CLAIM:
The surgeon was negligent in not finding the needle on the x-ray and not notifying her that the needle was missing.
PHYSICIAN'S DEFENSE:
The surgeon contended that his search for the needle and reliance on x-ray were in line with the standard of care. Since his actions were within the standard of care, he was not required to inform the patient.
VERDICT:
A Mississippi defense verdict was returned.
Failure to diagnose breast cancer on mammography
A 62-year-old woman started having routine mammographies in 2003. From 2006 to 2010, her annual mammographies were read by the same radiologist (Dr. A), who reported them as normal. Her 2011 mammography was read by a second radiologist (Dr. B), who reported it as normal. A year later, the patient was found to have several breast masses. Testing revealed that the cancer had metastasized. She underwent radical mastectomy and aggressive radiation treatment, but her cancer was deemed incurable.
PATIENT'S CLAIM:
Dr. A misread her mammograms from 2006 to 2010. There was evidence of asymmetric density suggestive of cancer on the 2006 mammography film.
PHYSICIAN'S DEFENSE:
There was no negligence. His reading of the mammographies was reasonable.
VERDICT:
A Kentucky defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Miscarriages after IUD is missing: $488,157 verdict
After the patient had miscarriages in 2009 and 2011, she asked her ObGyn if the missing IUD, which she had never seen leave her body, might have contributed to the miscarriages. She was told that the device was not present. No further testing was performed.
After the patient switched providers in 2013, an abdominal x-ray located the IUD. The patient became pregnant after the IUD was successfully removed.
PATIENT'S CLAIM:
The patient sued the ObGyn and his clinic for personal injury and wrongful death of the unborn fetuses. She claimed that it is below the standard of care not to perform an abdominal x-ray when a patient's IUD is missing.
The patient's attorney objected to the tests of the miscarried fetuses, contending that the tissues were sent without consent and that misinformation was conveyed on the pathology requisition.
DEFENDANTS' DEFENSE:
The standard of care set by the American College of Obstetricians and Gynecologists (ACOG) did not specify the use of an abdominal x-ray until Practice Bulletin No. 121 in July 2011 stated that the location of a lost IUD should be confirmed by x-ray.1
The IUD did not produce the miscarriages; testing of remains of 2 miscarried fetuses showed trisomic abnormalities that could not be attributed to the IUD.
The defense countered the patient's attorney that the testing forms had the patient's signed consent and that nothing was misrepresented on the forms.
VERDICT:
A Missouri defense verdict was returned for the wrongful death counts, but the jury awarded the patient $488,157 on the injury claim.
Reference
- Espey E, Singh RH; Committee on Practice Bulletins--Gynecology. American College of Gynecologists and Obstetricians Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184-196.
Related article:
Pregnancy test missed before IUD placement? Your liability.
Needle left behind during mastectomy reconstruction
After a woman was diagnosed with invasive ductal cancer in her left breast, she underwent a double mastectomy with simple mastectomy reconstruction on the left breast. During the operation, the surgical count could not account for 1 pop-off needle. The surgeon searched for the missing needle and ordered an x-ray but the needle could not be located. The surgeon did not tell the patient that the needle count was incomplete.
The patient underwent several other breast reconstruction procedures and the needle was never found.
Five years after the initial surgery, the needle was discovered and surgically removed.
PATIENT'S CLAIM:
The surgeon was negligent in not finding the needle on the x-ray and not notifying her that the needle was missing.
PHYSICIAN'S DEFENSE:
The surgeon contended that his search for the needle and reliance on x-ray were in line with the standard of care. Since his actions were within the standard of care, he was not required to inform the patient.
VERDICT:
A Mississippi defense verdict was returned.
Failure to diagnose breast cancer on mammography
A 62-year-old woman started having routine mammographies in 2003. From 2006 to 2010, her annual mammographies were read by the same radiologist (Dr. A), who reported them as normal. Her 2011 mammography was read by a second radiologist (Dr. B), who reported it as normal. A year later, the patient was found to have several breast masses. Testing revealed that the cancer had metastasized. She underwent radical mastectomy and aggressive radiation treatment, but her cancer was deemed incurable.
PATIENT'S CLAIM:
Dr. A misread her mammograms from 2006 to 2010. There was evidence of asymmetric density suggestive of cancer on the 2006 mammography film.
PHYSICIAN'S DEFENSE:
There was no negligence. His reading of the mammographies was reasonable.
VERDICT:
A Kentucky defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Miscarriages after IUD is missing: $488,157 verdict
After the patient had miscarriages in 2009 and 2011, she asked her ObGyn if the missing IUD, which she had never seen leave her body, might have contributed to the miscarriages. She was told that the device was not present. No further testing was performed.
After the patient switched providers in 2013, an abdominal x-ray located the IUD. The patient became pregnant after the IUD was successfully removed.
PATIENT'S CLAIM:
The patient sued the ObGyn and his clinic for personal injury and wrongful death of the unborn fetuses. She claimed that it is below the standard of care not to perform an abdominal x-ray when a patient's IUD is missing.
The patient's attorney objected to the tests of the miscarried fetuses, contending that the tissues were sent without consent and that misinformation was conveyed on the pathology requisition.
DEFENDANTS' DEFENSE:
The standard of care set by the American College of Obstetricians and Gynecologists (ACOG) did not specify the use of an abdominal x-ray until Practice Bulletin No. 121 in July 2011 stated that the location of a lost IUD should be confirmed by x-ray.1
The IUD did not produce the miscarriages; testing of remains of 2 miscarried fetuses showed trisomic abnormalities that could not be attributed to the IUD.
The defense countered the patient's attorney that the testing forms had the patient's signed consent and that nothing was misrepresented on the forms.
VERDICT:
A Missouri defense verdict was returned for the wrongful death counts, but the jury awarded the patient $488,157 on the injury claim.
Reference
- Espey E, Singh RH; Committee on Practice Bulletins--Gynecology. American College of Gynecologists and Obstetricians Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011;118(1):184-196.
Related article:
Pregnancy test missed before IUD placement? Your liability.
Needle left behind during mastectomy reconstruction
After a woman was diagnosed with invasive ductal cancer in her left breast, she underwent a double mastectomy with simple mastectomy reconstruction on the left breast. During the operation, the surgical count could not account for 1 pop-off needle. The surgeon searched for the missing needle and ordered an x-ray but the needle could not be located. The surgeon did not tell the patient that the needle count was incomplete.
The patient underwent several other breast reconstruction procedures and the needle was never found.
Five years after the initial surgery, the needle was discovered and surgically removed.
PATIENT'S CLAIM:
The surgeon was negligent in not finding the needle on the x-ray and not notifying her that the needle was missing.
PHYSICIAN'S DEFENSE:
The surgeon contended that his search for the needle and reliance on x-ray were in line with the standard of care. Since his actions were within the standard of care, he was not required to inform the patient.
VERDICT:
A Mississippi defense verdict was returned.
Failure to diagnose breast cancer on mammography
A 62-year-old woman started having routine mammographies in 2003. From 2006 to 2010, her annual mammographies were read by the same radiologist (Dr. A), who reported them as normal. Her 2011 mammography was read by a second radiologist (Dr. B), who reported it as normal. A year later, the patient was found to have several breast masses. Testing revealed that the cancer had metastasized. She underwent radical mastectomy and aggressive radiation treatment, but her cancer was deemed incurable.
PATIENT'S CLAIM:
Dr. A misread her mammograms from 2006 to 2010. There was evidence of asymmetric density suggestive of cancer on the 2006 mammography film.
PHYSICIAN'S DEFENSE:
There was no negligence. His reading of the mammographies was reasonable.
VERDICT:
A Kentucky defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Late delivery of macrosomic baby
Late delivery of macrosomic baby: $5.5M settlement
After a woman was admitted to the hospital, her labor was complicated by very slow progress, maternal fever, and multiple fetal heart-rate (FHR) monitor strip abnormalities. A baby boy was born by cesarean delivery 26 hours after the mother's admission, weighing almost 11 lb. At birth, the baby was asphyxiated, with an arterial cord blood pH of 7.01 and a base excess of -14.4. He was resuscitated and sent to the neonatal intensive care unit (NICU). Nine days after birth, he began to have seizures. The placental pathology report revealed infection; placental cultures grew Group B strep. The infant was diagnosed 6 days later with hypoxic ischemic encephalopathy after magnetic resonance imaging.
PARENTS' CLAIM:
The ObGyn and hospital failed to recognize that the baby was macrosomic. The ObGyn should have delivered the baby when the FHR monitor first showed fetal distress.
DEFENDANTS' DEFENSE:
The case was settled during the trial.
VERDICT:
A $5.5 million Washington settlement was reached.
Size of perineal tear and its consequences disputed: $1.8M verdict
A 34-year-old woman gave birth vaginally. During forceps delivery, she suffered a 4th-degree perineal tear, running from her vagina to her rectum, which was misidentified by the ObGyn as a 2nd-degree tear. The perineal tear lead to complications including infection and a persistent rectovaginal fistula. She underwent several operations over the next 5 years.
PARENTS' CLAIM:
The ObGyn did not appropriately address the wound. Had a cesarean delivery been performed, the wound would not have occurred.
DEFENDANTS' DEFENSE:
The decisions to allow labor to continue and to use forceps were reasonable. The ObGyn contended that the patient sustained only a 2nd-degree tear in the delivery room, with the 4th-degree tear occurring the next day due to attenuated tissue.
VERDICT:
A $1.8 million Illinois verdict was returned.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Macrosomic baby, cerebral palsy: $5.5M settlement
At 42 weeks' gestation, a mother was sent to the hospital in labor. During delivery, thick meconium was encountered. At birth, the baby weighed more than 9 lb. At age 16 years, the child has cerebral palsy, a seizure disorder, and developmental and cognitive deficits. She functions at the level of an 8-year-old child.
PARENTS' CLAIM:
The ObGyn and nurses did not deliver the baby in a timely manner by cesarean delivery. The estimated weight and a deteriorating in utero environment, as evidenced by the thick meconium, caused the child's brain injury.
DEFENDANTS' DEFENSE:
The case settled during trial.
VERDICT:
A $5.5 million Illinois settlement was reached.
Did baby get Group B strep from her mother?
During prenatal care by an ObGyn, a woman underwent a routine test for Group B strep, the results of which were negative. The child, with APGAR scores of 9 at 1 and 5 minutes after birth, was admitted to the well-baby nursery. Four hours after birth, the baby appeared to be in distress and was moved to the NICU. She was found to have respiratory distress, metabolic acidosis, and sepsis, allegedly caused by Group B strep, and was placed on a ventilator and prescribed medications. When the baby's condition worsened, she was transferred to a children's hospital. She was discharged 3 months later with bronchopulmonary dysplasia and a chronic lung disease that requires continuous treatment.
PARENTS' CLAIM:
The baby's injuries were attributable to Group B strep. The ObGyn's prenatal treatment did not meet the standard of care.
PHYSICIAN'S DEFENSE:
There was no negligence on the part of the ObGyn. The standard of care was met.
VERDICT:
An Alabama defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Late delivery of macrosomic baby: $5.5M settlement
After a woman was admitted to the hospital, her labor was complicated by very slow progress, maternal fever, and multiple fetal heart-rate (FHR) monitor strip abnormalities. A baby boy was born by cesarean delivery 26 hours after the mother's admission, weighing almost 11 lb. At birth, the baby was asphyxiated, with an arterial cord blood pH of 7.01 and a base excess of -14.4. He was resuscitated and sent to the neonatal intensive care unit (NICU). Nine days after birth, he began to have seizures. The placental pathology report revealed infection; placental cultures grew Group B strep. The infant was diagnosed 6 days later with hypoxic ischemic encephalopathy after magnetic resonance imaging.
PARENTS' CLAIM:
The ObGyn and hospital failed to recognize that the baby was macrosomic. The ObGyn should have delivered the baby when the FHR monitor first showed fetal distress.
DEFENDANTS' DEFENSE:
The case was settled during the trial.
VERDICT:
A $5.5 million Washington settlement was reached.
Size of perineal tear and its consequences disputed: $1.8M verdict
A 34-year-old woman gave birth vaginally. During forceps delivery, she suffered a 4th-degree perineal tear, running from her vagina to her rectum, which was misidentified by the ObGyn as a 2nd-degree tear. The perineal tear lead to complications including infection and a persistent rectovaginal fistula. She underwent several operations over the next 5 years.
PARENTS' CLAIM:
The ObGyn did not appropriately address the wound. Had a cesarean delivery been performed, the wound would not have occurred.
DEFENDANTS' DEFENSE:
The decisions to allow labor to continue and to use forceps were reasonable. The ObGyn contended that the patient sustained only a 2nd-degree tear in the delivery room, with the 4th-degree tear occurring the next day due to attenuated tissue.
VERDICT:
A $1.8 million Illinois verdict was returned.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Macrosomic baby, cerebral palsy: $5.5M settlement
At 42 weeks' gestation, a mother was sent to the hospital in labor. During delivery, thick meconium was encountered. At birth, the baby weighed more than 9 lb. At age 16 years, the child has cerebral palsy, a seizure disorder, and developmental and cognitive deficits. She functions at the level of an 8-year-old child.
PARENTS' CLAIM:
The ObGyn and nurses did not deliver the baby in a timely manner by cesarean delivery. The estimated weight and a deteriorating in utero environment, as evidenced by the thick meconium, caused the child's brain injury.
DEFENDANTS' DEFENSE:
The case settled during trial.
VERDICT:
A $5.5 million Illinois settlement was reached.
Did baby get Group B strep from her mother?
During prenatal care by an ObGyn, a woman underwent a routine test for Group B strep, the results of which were negative. The child, with APGAR scores of 9 at 1 and 5 minutes after birth, was admitted to the well-baby nursery. Four hours after birth, the baby appeared to be in distress and was moved to the NICU. She was found to have respiratory distress, metabolic acidosis, and sepsis, allegedly caused by Group B strep, and was placed on a ventilator and prescribed medications. When the baby's condition worsened, she was transferred to a children's hospital. She was discharged 3 months later with bronchopulmonary dysplasia and a chronic lung disease that requires continuous treatment.
PARENTS' CLAIM:
The baby's injuries were attributable to Group B strep. The ObGyn's prenatal treatment did not meet the standard of care.
PHYSICIAN'S DEFENSE:
There was no negligence on the part of the ObGyn. The standard of care was met.
VERDICT:
An Alabama defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Late delivery of macrosomic baby: $5.5M settlement
After a woman was admitted to the hospital, her labor was complicated by very slow progress, maternal fever, and multiple fetal heart-rate (FHR) monitor strip abnormalities. A baby boy was born by cesarean delivery 26 hours after the mother's admission, weighing almost 11 lb. At birth, the baby was asphyxiated, with an arterial cord blood pH of 7.01 and a base excess of -14.4. He was resuscitated and sent to the neonatal intensive care unit (NICU). Nine days after birth, he began to have seizures. The placental pathology report revealed infection; placental cultures grew Group B strep. The infant was diagnosed 6 days later with hypoxic ischemic encephalopathy after magnetic resonance imaging.
PARENTS' CLAIM:
The ObGyn and hospital failed to recognize that the baby was macrosomic. The ObGyn should have delivered the baby when the FHR monitor first showed fetal distress.
DEFENDANTS' DEFENSE:
The case was settled during the trial.
VERDICT:
A $5.5 million Washington settlement was reached.
Size of perineal tear and its consequences disputed: $1.8M verdict
A 34-year-old woman gave birth vaginally. During forceps delivery, she suffered a 4th-degree perineal tear, running from her vagina to her rectum, which was misidentified by the ObGyn as a 2nd-degree tear. The perineal tear lead to complications including infection and a persistent rectovaginal fistula. She underwent several operations over the next 5 years.
PARENTS' CLAIM:
The ObGyn did not appropriately address the wound. Had a cesarean delivery been performed, the wound would not have occurred.
DEFENDANTS' DEFENSE:
The decisions to allow labor to continue and to use forceps were reasonable. The ObGyn contended that the patient sustained only a 2nd-degree tear in the delivery room, with the 4th-degree tear occurring the next day due to attenuated tissue.
VERDICT:
A $1.8 million Illinois verdict was returned.
Related article:
Develop and use a checklist for 3rd- and 4th-degree perineal lacerations
Macrosomic baby, cerebral palsy: $5.5M settlement
At 42 weeks' gestation, a mother was sent to the hospital in labor. During delivery, thick meconium was encountered. At birth, the baby weighed more than 9 lb. At age 16 years, the child has cerebral palsy, a seizure disorder, and developmental and cognitive deficits. She functions at the level of an 8-year-old child.
PARENTS' CLAIM:
The ObGyn and nurses did not deliver the baby in a timely manner by cesarean delivery. The estimated weight and a deteriorating in utero environment, as evidenced by the thick meconium, caused the child's brain injury.
DEFENDANTS' DEFENSE:
The case settled during trial.
VERDICT:
A $5.5 million Illinois settlement was reached.
Did baby get Group B strep from her mother?
During prenatal care by an ObGyn, a woman underwent a routine test for Group B strep, the results of which were negative. The child, with APGAR scores of 9 at 1 and 5 minutes after birth, was admitted to the well-baby nursery. Four hours after birth, the baby appeared to be in distress and was moved to the NICU. She was found to have respiratory distress, metabolic acidosis, and sepsis, allegedly caused by Group B strep, and was placed on a ventilator and prescribed medications. When the baby's condition worsened, she was transferred to a children's hospital. She was discharged 3 months later with bronchopulmonary dysplasia and a chronic lung disease that requires continuous treatment.
PARENTS' CLAIM:
The baby's injuries were attributable to Group B strep. The ObGyn's prenatal treatment did not meet the standard of care.
PHYSICIAN'S DEFENSE:
There was no negligence on the part of the ObGyn. The standard of care was met.
VERDICT:
An Alabama defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Malpractice Counsel: A Pain in the…Scrotum
Case
A 52-year-old man presented to the ED for evaluation of right scrotal pain and swelling. The patient stated that the pain started several hours prior to presentation and had gradually worsened. He denied any trauma or inciting event to the affected area; he further denied abdominal pain, nausea, vomiting, dysuria, polyuria, or fever. The patient’s remote medical history was significant for type 2 diabetes mellitus (DM), which he managed through dietary modification-only as he had refused pharmacological therapy. The patient admitted to smoking one half-pack of cigarettes per week, but denied alcohol or illicit drug use.
At presentation, the patient’s vital signs were all within normal range. The physical examination was remarkable only for right testicular tenderness and mild scrotal swelling, and there were no hernias or lymphadenopathy present.
The emergency physician (EP) ordered a urinalysis and color-flow Doppler ultrasound study of both testes, which the radiologist interpreted as an enlarged right epididymis with hyperemia; the left testicle was normal. The urinalysis was normal.
The patient was diagnosed with epididymitis and discharged home with a prescription for oral levofloxacin 500 mg daily for 10 days. He also was instructed to take ibuprofen for pain, apply ice to the affected area, keep the scrotal area elevated, and follow-up with a urologist in 1 week.
Approximately 8 hours after discharge, the patient returned to the same ED with complaints of increasing right testicular pain and swelling. The history and physical examination at this visit were essentially unchanged from his initial presentation. No laboratory evaluation, imaging studies, or other tests were ordered at the second visit.
The patient was discharged home with a prescription for a narcotic analgesic, which he was instructed to take in addition to the ibuprofen; he was also instructed to follow-up with a urologist within the next 2 to 3 days, instead of in 1 week.
The patient returned the following morning to the same ED with complaints of increased swelling and pain of the right testicle. In addition to the worsening testicular pain and swelling, he also had right inguinal pain, nausea, vomiting, and fever. Vital signs at this third presentation were: blood pressure (BP), 124/64 mm Hg; heart rate (HR), 110 beats/min; respiratory rate, 20 breaths/min; and temperature, 99.8o F. Oxygen saturation was 98% on room air.
The patient was tachycardic on heart examination, but with regular rhythm and no murmurs, rubs, or gallops. The lung and abdominal examinations were normal. The genital examination revealed marked right scrotal swelling and tenderness, as well as tender right inguinal lymphadenopathy.
The EP ordered an intravenous (IV) bolus of 1 L normal saline and laboratory studies, which included lactic acid, blood cultures, urinalysis, and urine culture and sensitivity. The EP was concerned for a scrotal abscess and ordered a testicular Doppler color-flow ultrasound study. The laboratory studies revealed an elevated white blood count of 16.5 K/uL, elevated blood glucose of 364 mg/dL, and elevated lactate of 2.8 mg/dL. As demonstrated on the ultrasound study performed at the patient’s first presentation, the ultrasound again showed an enlarged right epididymis, but without orchitis or abscess. The scrotal wall had significant thickening, consistent with cellulitis. The EP ordered broad spectrum IV antibiotics and admitted the patient to the hospitalist with a consult request for urology services.
The patient continued to receive IV fluids and antibiotics throughout the evening. In the morning, he was seen by the same hospitalist/admitting physician from the previous evening. Upon physical examination, the hospitalist noted tenderness, swelling, and erythema in the patient’s perineal area. The patient’s BP had dropped to 100/60 mm Hg, and his HR had increased to 115 beats/min despite receiving nearly 2 L of normal saline IV throughout the previous evening and night.
The urologist examined the patient soon after the consult request and diagnosed him with Fournier’s gangrene. He started the patient on aggressive IV fluid resuscitation, after which the patient was immediately taken to the operating room for extensive surgical debridement and scrotectomy. The patient’s postoperative course was complicated by acute kidney injury, respiratory failure requiring ventilator support, and sepsis. After a lengthy hospital stay, the patient was discharged home, but required a scrotal skin graft, and experienced erectile dysfunction and depression.
The patient sued all of the EPs involved in his care, the hospital, the hospitalist/admitting physician, and the urologist for negligence. The plaintiff’s attorney argued that since the patient progressively deteriorated over the 24 to 36 hours during his three presentations to the ED, urology services should have been consulted earlier, and that the urologist should have seen the patient immediately at the time of hospital admission.
The attorneys for the defendants claimed the patient denied dysuria, penile lesions, or urethral discharge and that the history, physical examination, and testicular ultrasound were all consistent with the diagnosis of epididymitis. For this reason, they argued, there was no indication for an emergent consultation with urology services. The jury returned a defense verdict.
Discussion
It is easy for a busy EP to have a differential diagnosis of only two disorders when evaluating a patient for unilateral testicular pain and swelling—in this case, testicular torsion and epididymitis. While these are the most common causes of testicular pain and swelling, this case emphasizes the need to also consider Fournier’s gangrene in the differential. A thorough history and physical examination, coupled with appropriate testing, will usually identify the correct diagnosis. While the differential diagnosis is broader than just these three disease processes (see the Box), we will review the evaluation and management of the three most serious: epididymitis, testicular torsion, and Fournier’s gangrene.
Noninfectious and Bacterial Epididymitis
Epididymitis is the most common cause of acute scrotal pain among US adults, accounting for approximately 600,000 cases each year.1 Infectious epididymitis is typically classified as acute (symptom duration of <6 weeks) or chronic (symptom duration of ≥6 weeks).2
Cases of noninfectious epididymitis are typically due to a chronic condition, such as autoimmune disease, cancer, or vasculitis. Although not as common, noninfectious epididymitis can also occur due to testicular trauma or amiodarone therapy.3,4
Patients with acute bacterial epididymitis typically present with scrotal pain and swelling ranging from mild to marked. These patients may also exhibit fever and chills, along with dysuria, frequency, and urgency, if associated with a urinary tract infection.2 The chronic presentation is more common though, and usually not associated with voiding issues.
Chronic epididymis is frequently seen in postpubertal boys and men following sexual activity, heavy physical exertion, and bicycle/motorcycle riding.2 On physical examination, palpation reveals induration and swelling of the involved epididymis with exquisite tenderness.2 Testicular swelling and pain, along with scrotal wall erythema, may be present in more advanced cases.2 The cremasteric reflex should be intact (ie, scratching the medial proximal thigh will cause ipsilateral testicle retraction). Similarly, the lie of both testicles while the patient is standing should be equal and symmetrical—ie, both testicles descended equally. However, in the presence of moderate-to-severe scrotal swelling, both of these physical findings may be impossible to confirm.
A urinalysis and urine culture should be ordered if there is any suspicion of epididymitis; pyuria will be present in approximately 50% of cases. However, since pyuria is neither sensitive nor specific for epididymitis, in most cases, a testicular ultrasound with Doppler flow is required to exclude testicular torsion. In cases of epididymitis, ultrasound usually demonstrates increased flow on the affected side, whereas in testicular torsion, there is decreased or absent blood flow.
The treatment for epididymitis involves antibiotics and symptomatic care. If epididymitis from chlamydia and/or gonorrhea is the suspected cause, or if the patient is younger than age 35 years, he should be given ceftriaxone 250 mg intramuscularly plus oral doxycycline 100 mg twice a day for 10 days. Patients who practice insertive anal sex should be treated with ceftriaxone, plus either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.
In cases in which enteric organisms are suspected, the patient is older than age 35 years, or if patient status is posturinary tract instrumentation or vasectomy, he should be treated with either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.2
For symptomatic relief, scrotal elevation, ice application, and nonsteroidal anti-inflammatory drugs are recommended.
Patients with epididymitis, regardless of etiology, should be instructed to follow-up with a urologist within 1 week. If the patient appears ill, septic, or in significant pain, admission to the hospital with IV antibiotics, IV fluids, and an urgent consult with urology services is required.
Testicular Torsion
Testicular torsion is a time-sensitive issue, requiring early diagnosis and rapid treatment to preserve the patient’s fertility. Most clinicians recommend detorsion within 6 hours of torsion onset because salvage rates are excellent when performed within this timeframe; after 12 hours, the testis will likely suffer irreversible damage due to ischemia.5,6
Testicular torsion can occur at any age, but is most commonly seen in a bimodal distribution—ie, neonates and postpubertal boys. The prevalence of testicular torsion in adult patients hospitalized with acute scrotal pain is approximately 25% to 50%.2
Patients with testicular torsion usually describe a sudden onset of severe, acute pain. The pain frequently occurs a few hours after vigorous physical activity or minor testicular trauma.2 Occasionally, the patient may complain of lower quadrant abdominal pain rather than testicular or scrotal pain. Nausea with vomiting can also be present.
On physical examination, significant testicular swelling is usually present. Examining the patient in the standing position will often reveal an asymmetrical, high-riding testis with a transverse lie on the affected side. The cremasteric reflex is usually absent in patients with testicular torsion.
Because of the significant overlap in history and physical examination findings for epididymitis and testicular torsion, a testicular ultrasound with color Doppler should be ordered. Multiple studies have confirmed the high sensitivity and specificity of ultrasound in the diagnosis of testicular torsion.
The treatment for suspected or confirmed testicular torsion is immediate surgical exploration with intraoperative detorsion and fixation of the testes. The EP can attempt manual detorsion (ie, performed in a medial to lateral motion, similar to opening a book). However, this should not delay the EP from consulting with urology services.
Pediatric patients with testicular torsion usually have a more favorable outcome than do adults. In one retrospective study, patients younger than age 21 years had a 70% testicular salvage rate compared to only 41% of patients aged 21 years and older.7 Regardless of age, better outcomes are associated with shorter periods of torsion.
Fournier’s Gangrene
Fournier’s gangrene is a polymicrobial necrotizing fasciitis of the perineum and scrotum that typically develops initially as a benign infection or abscess but quickly spreads. Risk factors for Fournier’s gangrene include DM, alcohol abuse, and any immunocompromised state (eg, HIV, cancer).
If the patient presents early in onset, there may be only mild tenderness, erythema, or swelling of the affected area; however, this infection progresses rapidly. Later findings include marked tenderness, swelling, crepitus, blisters, and ecchymoses. Patients with Fournier’s gangrene also develop systemic signs of infection, including fever, tachycardia, tachypnea, and hypotension. The key to diagnosis is careful examination of the perineal and scrotal area in any patient presenting with acute scrotal pain.
In the majority of cases, the diagnosis of Fournier’s gangrene is made clinically. Once the diagnosis is made, patients require immediate and aggressive IV fluid resuscitation, broad-spectrum IV antibiotics (typically vancomycin and piperacillin/tazobactam), and emergent evaluation by a urologist. It is essential that these patients undergo early and aggressive surgical exploration and debridement of necrotic tissue.2 Antibiotic therapy alone is associated with a 100% mortality rate, emphasizing the need for urgent surgery.2 Even with optimal medical and surgical management, the mortality rate remains significant.
Summary
This case emphasizes several important teaching points. The EP should be mindful of the patient who keeps returning to the ED with the same complaint—despite “appropriate” treatment—as the initial diagnosis may not be the correct one. Such returning patients require greater, not less, scrutiny. As with any patient, the EP should always take a complete history and perform a thorough physical examination at each presentation—as one would with a de novo patient. Finally, the EP should consider Fournier’s gangrene in addition to testicular torsion and epididymitis in the differential diagnosis for acute scrotal pain.
1. Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
2. Eyre RC. Evaluation of acute scrotal pain in adults. UpToDate Web site. https://www.uptodate.com/contents/evaluation-of-acute-scrotal-pain-in-adults. Updated July 31, 2017. Accessed September 7, 2017.
3. Shen Y, Liu H, Cheng J, Bu P. Amiodarone-induced epididymitis: a pathologically confirmed case report and review of the literature. Cardiology. 2014;128(4):349-351. doi:10.1159/000361038.
4. Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35(1):101-108. doi:10.1016/j.ucl.2007.09.013.
5. Wampler SM, Llanes M. Common scrotal and testicular problems. Prim Care. 2010;37(3):613-626. doi:10.1016/j.pop.2010.04.009.
6. Dunne PJ, O’Loughlin BS. Testicular torsion: time is the enemy. Aust NZ J Surg. 2000;70(6):441-442.
7. Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002;167(5):2109-2110.
Case
A 52-year-old man presented to the ED for evaluation of right scrotal pain and swelling. The patient stated that the pain started several hours prior to presentation and had gradually worsened. He denied any trauma or inciting event to the affected area; he further denied abdominal pain, nausea, vomiting, dysuria, polyuria, or fever. The patient’s remote medical history was significant for type 2 diabetes mellitus (DM), which he managed through dietary modification-only as he had refused pharmacological therapy. The patient admitted to smoking one half-pack of cigarettes per week, but denied alcohol or illicit drug use.
At presentation, the patient’s vital signs were all within normal range. The physical examination was remarkable only for right testicular tenderness and mild scrotal swelling, and there were no hernias or lymphadenopathy present.
The emergency physician (EP) ordered a urinalysis and color-flow Doppler ultrasound study of both testes, which the radiologist interpreted as an enlarged right epididymis with hyperemia; the left testicle was normal. The urinalysis was normal.
The patient was diagnosed with epididymitis and discharged home with a prescription for oral levofloxacin 500 mg daily for 10 days. He also was instructed to take ibuprofen for pain, apply ice to the affected area, keep the scrotal area elevated, and follow-up with a urologist in 1 week.
Approximately 8 hours after discharge, the patient returned to the same ED with complaints of increasing right testicular pain and swelling. The history and physical examination at this visit were essentially unchanged from his initial presentation. No laboratory evaluation, imaging studies, or other tests were ordered at the second visit.
The patient was discharged home with a prescription for a narcotic analgesic, which he was instructed to take in addition to the ibuprofen; he was also instructed to follow-up with a urologist within the next 2 to 3 days, instead of in 1 week.
The patient returned the following morning to the same ED with complaints of increased swelling and pain of the right testicle. In addition to the worsening testicular pain and swelling, he also had right inguinal pain, nausea, vomiting, and fever. Vital signs at this third presentation were: blood pressure (BP), 124/64 mm Hg; heart rate (HR), 110 beats/min; respiratory rate, 20 breaths/min; and temperature, 99.8o F. Oxygen saturation was 98% on room air.
The patient was tachycardic on heart examination, but with regular rhythm and no murmurs, rubs, or gallops. The lung and abdominal examinations were normal. The genital examination revealed marked right scrotal swelling and tenderness, as well as tender right inguinal lymphadenopathy.
The EP ordered an intravenous (IV) bolus of 1 L normal saline and laboratory studies, which included lactic acid, blood cultures, urinalysis, and urine culture and sensitivity. The EP was concerned for a scrotal abscess and ordered a testicular Doppler color-flow ultrasound study. The laboratory studies revealed an elevated white blood count of 16.5 K/uL, elevated blood glucose of 364 mg/dL, and elevated lactate of 2.8 mg/dL. As demonstrated on the ultrasound study performed at the patient’s first presentation, the ultrasound again showed an enlarged right epididymis, but without orchitis or abscess. The scrotal wall had significant thickening, consistent with cellulitis. The EP ordered broad spectrum IV antibiotics and admitted the patient to the hospitalist with a consult request for urology services.
The patient continued to receive IV fluids and antibiotics throughout the evening. In the morning, he was seen by the same hospitalist/admitting physician from the previous evening. Upon physical examination, the hospitalist noted tenderness, swelling, and erythema in the patient’s perineal area. The patient’s BP had dropped to 100/60 mm Hg, and his HR had increased to 115 beats/min despite receiving nearly 2 L of normal saline IV throughout the previous evening and night.
The urologist examined the patient soon after the consult request and diagnosed him with Fournier’s gangrene. He started the patient on aggressive IV fluid resuscitation, after which the patient was immediately taken to the operating room for extensive surgical debridement and scrotectomy. The patient’s postoperative course was complicated by acute kidney injury, respiratory failure requiring ventilator support, and sepsis. After a lengthy hospital stay, the patient was discharged home, but required a scrotal skin graft, and experienced erectile dysfunction and depression.
The patient sued all of the EPs involved in his care, the hospital, the hospitalist/admitting physician, and the urologist for negligence. The plaintiff’s attorney argued that since the patient progressively deteriorated over the 24 to 36 hours during his three presentations to the ED, urology services should have been consulted earlier, and that the urologist should have seen the patient immediately at the time of hospital admission.
The attorneys for the defendants claimed the patient denied dysuria, penile lesions, or urethral discharge and that the history, physical examination, and testicular ultrasound were all consistent with the diagnosis of epididymitis. For this reason, they argued, there was no indication for an emergent consultation with urology services. The jury returned a defense verdict.
Discussion
It is easy for a busy EP to have a differential diagnosis of only two disorders when evaluating a patient for unilateral testicular pain and swelling—in this case, testicular torsion and epididymitis. While these are the most common causes of testicular pain and swelling, this case emphasizes the need to also consider Fournier’s gangrene in the differential. A thorough history and physical examination, coupled with appropriate testing, will usually identify the correct diagnosis. While the differential diagnosis is broader than just these three disease processes (see the Box), we will review the evaluation and management of the three most serious: epididymitis, testicular torsion, and Fournier’s gangrene.
Noninfectious and Bacterial Epididymitis
Epididymitis is the most common cause of acute scrotal pain among US adults, accounting for approximately 600,000 cases each year.1 Infectious epididymitis is typically classified as acute (symptom duration of <6 weeks) or chronic (symptom duration of ≥6 weeks).2
Cases of noninfectious epididymitis are typically due to a chronic condition, such as autoimmune disease, cancer, or vasculitis. Although not as common, noninfectious epididymitis can also occur due to testicular trauma or amiodarone therapy.3,4
Patients with acute bacterial epididymitis typically present with scrotal pain and swelling ranging from mild to marked. These patients may also exhibit fever and chills, along with dysuria, frequency, and urgency, if associated with a urinary tract infection.2 The chronic presentation is more common though, and usually not associated with voiding issues.
Chronic epididymis is frequently seen in postpubertal boys and men following sexual activity, heavy physical exertion, and bicycle/motorcycle riding.2 On physical examination, palpation reveals induration and swelling of the involved epididymis with exquisite tenderness.2 Testicular swelling and pain, along with scrotal wall erythema, may be present in more advanced cases.2 The cremasteric reflex should be intact (ie, scratching the medial proximal thigh will cause ipsilateral testicle retraction). Similarly, the lie of both testicles while the patient is standing should be equal and symmetrical—ie, both testicles descended equally. However, in the presence of moderate-to-severe scrotal swelling, both of these physical findings may be impossible to confirm.
A urinalysis and urine culture should be ordered if there is any suspicion of epididymitis; pyuria will be present in approximately 50% of cases. However, since pyuria is neither sensitive nor specific for epididymitis, in most cases, a testicular ultrasound with Doppler flow is required to exclude testicular torsion. In cases of epididymitis, ultrasound usually demonstrates increased flow on the affected side, whereas in testicular torsion, there is decreased or absent blood flow.
The treatment for epididymitis involves antibiotics and symptomatic care. If epididymitis from chlamydia and/or gonorrhea is the suspected cause, or if the patient is younger than age 35 years, he should be given ceftriaxone 250 mg intramuscularly plus oral doxycycline 100 mg twice a day for 10 days. Patients who practice insertive anal sex should be treated with ceftriaxone, plus either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.
In cases in which enteric organisms are suspected, the patient is older than age 35 years, or if patient status is posturinary tract instrumentation or vasectomy, he should be treated with either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.2
For symptomatic relief, scrotal elevation, ice application, and nonsteroidal anti-inflammatory drugs are recommended.
Patients with epididymitis, regardless of etiology, should be instructed to follow-up with a urologist within 1 week. If the patient appears ill, septic, or in significant pain, admission to the hospital with IV antibiotics, IV fluids, and an urgent consult with urology services is required.
Testicular Torsion
Testicular torsion is a time-sensitive issue, requiring early diagnosis and rapid treatment to preserve the patient’s fertility. Most clinicians recommend detorsion within 6 hours of torsion onset because salvage rates are excellent when performed within this timeframe; after 12 hours, the testis will likely suffer irreversible damage due to ischemia.5,6
Testicular torsion can occur at any age, but is most commonly seen in a bimodal distribution—ie, neonates and postpubertal boys. The prevalence of testicular torsion in adult patients hospitalized with acute scrotal pain is approximately 25% to 50%.2
Patients with testicular torsion usually describe a sudden onset of severe, acute pain. The pain frequently occurs a few hours after vigorous physical activity or minor testicular trauma.2 Occasionally, the patient may complain of lower quadrant abdominal pain rather than testicular or scrotal pain. Nausea with vomiting can also be present.
On physical examination, significant testicular swelling is usually present. Examining the patient in the standing position will often reveal an asymmetrical, high-riding testis with a transverse lie on the affected side. The cremasteric reflex is usually absent in patients with testicular torsion.
Because of the significant overlap in history and physical examination findings for epididymitis and testicular torsion, a testicular ultrasound with color Doppler should be ordered. Multiple studies have confirmed the high sensitivity and specificity of ultrasound in the diagnosis of testicular torsion.
The treatment for suspected or confirmed testicular torsion is immediate surgical exploration with intraoperative detorsion and fixation of the testes. The EP can attempt manual detorsion (ie, performed in a medial to lateral motion, similar to opening a book). However, this should not delay the EP from consulting with urology services.
Pediatric patients with testicular torsion usually have a more favorable outcome than do adults. In one retrospective study, patients younger than age 21 years had a 70% testicular salvage rate compared to only 41% of patients aged 21 years and older.7 Regardless of age, better outcomes are associated with shorter periods of torsion.
Fournier’s Gangrene
Fournier’s gangrene is a polymicrobial necrotizing fasciitis of the perineum and scrotum that typically develops initially as a benign infection or abscess but quickly spreads. Risk factors for Fournier’s gangrene include DM, alcohol abuse, and any immunocompromised state (eg, HIV, cancer).
If the patient presents early in onset, there may be only mild tenderness, erythema, or swelling of the affected area; however, this infection progresses rapidly. Later findings include marked tenderness, swelling, crepitus, blisters, and ecchymoses. Patients with Fournier’s gangrene also develop systemic signs of infection, including fever, tachycardia, tachypnea, and hypotension. The key to diagnosis is careful examination of the perineal and scrotal area in any patient presenting with acute scrotal pain.
In the majority of cases, the diagnosis of Fournier’s gangrene is made clinically. Once the diagnosis is made, patients require immediate and aggressive IV fluid resuscitation, broad-spectrum IV antibiotics (typically vancomycin and piperacillin/tazobactam), and emergent evaluation by a urologist. It is essential that these patients undergo early and aggressive surgical exploration and debridement of necrotic tissue.2 Antibiotic therapy alone is associated with a 100% mortality rate, emphasizing the need for urgent surgery.2 Even with optimal medical and surgical management, the mortality rate remains significant.
Summary
This case emphasizes several important teaching points. The EP should be mindful of the patient who keeps returning to the ED with the same complaint—despite “appropriate” treatment—as the initial diagnosis may not be the correct one. Such returning patients require greater, not less, scrutiny. As with any patient, the EP should always take a complete history and perform a thorough physical examination at each presentation—as one would with a de novo patient. Finally, the EP should consider Fournier’s gangrene in addition to testicular torsion and epididymitis in the differential diagnosis for acute scrotal pain.
Case
A 52-year-old man presented to the ED for evaluation of right scrotal pain and swelling. The patient stated that the pain started several hours prior to presentation and had gradually worsened. He denied any trauma or inciting event to the affected area; he further denied abdominal pain, nausea, vomiting, dysuria, polyuria, or fever. The patient’s remote medical history was significant for type 2 diabetes mellitus (DM), which he managed through dietary modification-only as he had refused pharmacological therapy. The patient admitted to smoking one half-pack of cigarettes per week, but denied alcohol or illicit drug use.
At presentation, the patient’s vital signs were all within normal range. The physical examination was remarkable only for right testicular tenderness and mild scrotal swelling, and there were no hernias or lymphadenopathy present.
The emergency physician (EP) ordered a urinalysis and color-flow Doppler ultrasound study of both testes, which the radiologist interpreted as an enlarged right epididymis with hyperemia; the left testicle was normal. The urinalysis was normal.
The patient was diagnosed with epididymitis and discharged home with a prescription for oral levofloxacin 500 mg daily for 10 days. He also was instructed to take ibuprofen for pain, apply ice to the affected area, keep the scrotal area elevated, and follow-up with a urologist in 1 week.
Approximately 8 hours after discharge, the patient returned to the same ED with complaints of increasing right testicular pain and swelling. The history and physical examination at this visit were essentially unchanged from his initial presentation. No laboratory evaluation, imaging studies, or other tests were ordered at the second visit.
The patient was discharged home with a prescription for a narcotic analgesic, which he was instructed to take in addition to the ibuprofen; he was also instructed to follow-up with a urologist within the next 2 to 3 days, instead of in 1 week.
The patient returned the following morning to the same ED with complaints of increased swelling and pain of the right testicle. In addition to the worsening testicular pain and swelling, he also had right inguinal pain, nausea, vomiting, and fever. Vital signs at this third presentation were: blood pressure (BP), 124/64 mm Hg; heart rate (HR), 110 beats/min; respiratory rate, 20 breaths/min; and temperature, 99.8o F. Oxygen saturation was 98% on room air.
The patient was tachycardic on heart examination, but with regular rhythm and no murmurs, rubs, or gallops. The lung and abdominal examinations were normal. The genital examination revealed marked right scrotal swelling and tenderness, as well as tender right inguinal lymphadenopathy.
The EP ordered an intravenous (IV) bolus of 1 L normal saline and laboratory studies, which included lactic acid, blood cultures, urinalysis, and urine culture and sensitivity. The EP was concerned for a scrotal abscess and ordered a testicular Doppler color-flow ultrasound study. The laboratory studies revealed an elevated white blood count of 16.5 K/uL, elevated blood glucose of 364 mg/dL, and elevated lactate of 2.8 mg/dL. As demonstrated on the ultrasound study performed at the patient’s first presentation, the ultrasound again showed an enlarged right epididymis, but without orchitis or abscess. The scrotal wall had significant thickening, consistent with cellulitis. The EP ordered broad spectrum IV antibiotics and admitted the patient to the hospitalist with a consult request for urology services.
The patient continued to receive IV fluids and antibiotics throughout the evening. In the morning, he was seen by the same hospitalist/admitting physician from the previous evening. Upon physical examination, the hospitalist noted tenderness, swelling, and erythema in the patient’s perineal area. The patient’s BP had dropped to 100/60 mm Hg, and his HR had increased to 115 beats/min despite receiving nearly 2 L of normal saline IV throughout the previous evening and night.
The urologist examined the patient soon after the consult request and diagnosed him with Fournier’s gangrene. He started the patient on aggressive IV fluid resuscitation, after which the patient was immediately taken to the operating room for extensive surgical debridement and scrotectomy. The patient’s postoperative course was complicated by acute kidney injury, respiratory failure requiring ventilator support, and sepsis. After a lengthy hospital stay, the patient was discharged home, but required a scrotal skin graft, and experienced erectile dysfunction and depression.
The patient sued all of the EPs involved in his care, the hospital, the hospitalist/admitting physician, and the urologist for negligence. The plaintiff’s attorney argued that since the patient progressively deteriorated over the 24 to 36 hours during his three presentations to the ED, urology services should have been consulted earlier, and that the urologist should have seen the patient immediately at the time of hospital admission.
The attorneys for the defendants claimed the patient denied dysuria, penile lesions, or urethral discharge and that the history, physical examination, and testicular ultrasound were all consistent with the diagnosis of epididymitis. For this reason, they argued, there was no indication for an emergent consultation with urology services. The jury returned a defense verdict.
Discussion
It is easy for a busy EP to have a differential diagnosis of only two disorders when evaluating a patient for unilateral testicular pain and swelling—in this case, testicular torsion and epididymitis. While these are the most common causes of testicular pain and swelling, this case emphasizes the need to also consider Fournier’s gangrene in the differential. A thorough history and physical examination, coupled with appropriate testing, will usually identify the correct diagnosis. While the differential diagnosis is broader than just these three disease processes (see the Box), we will review the evaluation and management of the three most serious: epididymitis, testicular torsion, and Fournier’s gangrene.
Noninfectious and Bacterial Epididymitis
Epididymitis is the most common cause of acute scrotal pain among US adults, accounting for approximately 600,000 cases each year.1 Infectious epididymitis is typically classified as acute (symptom duration of <6 weeks) or chronic (symptom duration of ≥6 weeks).2
Cases of noninfectious epididymitis are typically due to a chronic condition, such as autoimmune disease, cancer, or vasculitis. Although not as common, noninfectious epididymitis can also occur due to testicular trauma or amiodarone therapy.3,4
Patients with acute bacterial epididymitis typically present with scrotal pain and swelling ranging from mild to marked. These patients may also exhibit fever and chills, along with dysuria, frequency, and urgency, if associated with a urinary tract infection.2 The chronic presentation is more common though, and usually not associated with voiding issues.
Chronic epididymis is frequently seen in postpubertal boys and men following sexual activity, heavy physical exertion, and bicycle/motorcycle riding.2 On physical examination, palpation reveals induration and swelling of the involved epididymis with exquisite tenderness.2 Testicular swelling and pain, along with scrotal wall erythema, may be present in more advanced cases.2 The cremasteric reflex should be intact (ie, scratching the medial proximal thigh will cause ipsilateral testicle retraction). Similarly, the lie of both testicles while the patient is standing should be equal and symmetrical—ie, both testicles descended equally. However, in the presence of moderate-to-severe scrotal swelling, both of these physical findings may be impossible to confirm.
A urinalysis and urine culture should be ordered if there is any suspicion of epididymitis; pyuria will be present in approximately 50% of cases. However, since pyuria is neither sensitive nor specific for epididymitis, in most cases, a testicular ultrasound with Doppler flow is required to exclude testicular torsion. In cases of epididymitis, ultrasound usually demonstrates increased flow on the affected side, whereas in testicular torsion, there is decreased or absent blood flow.
The treatment for epididymitis involves antibiotics and symptomatic care. If epididymitis from chlamydia and/or gonorrhea is the suspected cause, or if the patient is younger than age 35 years, he should be given ceftriaxone 250 mg intramuscularly plus oral doxycycline 100 mg twice a day for 10 days. Patients who practice insertive anal sex should be treated with ceftriaxone, plus either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.
In cases in which enteric organisms are suspected, the patient is older than age 35 years, or if patient status is posturinary tract instrumentation or vasectomy, he should be treated with either oral ofloxacin 300 mg twice a day or oral levofloxacin 500 mg daily for 10 days.2
For symptomatic relief, scrotal elevation, ice application, and nonsteroidal anti-inflammatory drugs are recommended.
Patients with epididymitis, regardless of etiology, should be instructed to follow-up with a urologist within 1 week. If the patient appears ill, septic, or in significant pain, admission to the hospital with IV antibiotics, IV fluids, and an urgent consult with urology services is required.
Testicular Torsion
Testicular torsion is a time-sensitive issue, requiring early diagnosis and rapid treatment to preserve the patient’s fertility. Most clinicians recommend detorsion within 6 hours of torsion onset because salvage rates are excellent when performed within this timeframe; after 12 hours, the testis will likely suffer irreversible damage due to ischemia.5,6
Testicular torsion can occur at any age, but is most commonly seen in a bimodal distribution—ie, neonates and postpubertal boys. The prevalence of testicular torsion in adult patients hospitalized with acute scrotal pain is approximately 25% to 50%.2
Patients with testicular torsion usually describe a sudden onset of severe, acute pain. The pain frequently occurs a few hours after vigorous physical activity or minor testicular trauma.2 Occasionally, the patient may complain of lower quadrant abdominal pain rather than testicular or scrotal pain. Nausea with vomiting can also be present.
On physical examination, significant testicular swelling is usually present. Examining the patient in the standing position will often reveal an asymmetrical, high-riding testis with a transverse lie on the affected side. The cremasteric reflex is usually absent in patients with testicular torsion.
Because of the significant overlap in history and physical examination findings for epididymitis and testicular torsion, a testicular ultrasound with color Doppler should be ordered. Multiple studies have confirmed the high sensitivity and specificity of ultrasound in the diagnosis of testicular torsion.
The treatment for suspected or confirmed testicular torsion is immediate surgical exploration with intraoperative detorsion and fixation of the testes. The EP can attempt manual detorsion (ie, performed in a medial to lateral motion, similar to opening a book). However, this should not delay the EP from consulting with urology services.
Pediatric patients with testicular torsion usually have a more favorable outcome than do adults. In one retrospective study, patients younger than age 21 years had a 70% testicular salvage rate compared to only 41% of patients aged 21 years and older.7 Regardless of age, better outcomes are associated with shorter periods of torsion.
Fournier’s Gangrene
Fournier’s gangrene is a polymicrobial necrotizing fasciitis of the perineum and scrotum that typically develops initially as a benign infection or abscess but quickly spreads. Risk factors for Fournier’s gangrene include DM, alcohol abuse, and any immunocompromised state (eg, HIV, cancer).
If the patient presents early in onset, there may be only mild tenderness, erythema, or swelling of the affected area; however, this infection progresses rapidly. Later findings include marked tenderness, swelling, crepitus, blisters, and ecchymoses. Patients with Fournier’s gangrene also develop systemic signs of infection, including fever, tachycardia, tachypnea, and hypotension. The key to diagnosis is careful examination of the perineal and scrotal area in any patient presenting with acute scrotal pain.
In the majority of cases, the diagnosis of Fournier’s gangrene is made clinically. Once the diagnosis is made, patients require immediate and aggressive IV fluid resuscitation, broad-spectrum IV antibiotics (typically vancomycin and piperacillin/tazobactam), and emergent evaluation by a urologist. It is essential that these patients undergo early and aggressive surgical exploration and debridement of necrotic tissue.2 Antibiotic therapy alone is associated with a 100% mortality rate, emphasizing the need for urgent surgery.2 Even with optimal medical and surgical management, the mortality rate remains significant.
Summary
This case emphasizes several important teaching points. The EP should be mindful of the patient who keeps returning to the ED with the same complaint—despite “appropriate” treatment—as the initial diagnosis may not be the correct one. Such returning patients require greater, not less, scrutiny. As with any patient, the EP should always take a complete history and perform a thorough physical examination at each presentation—as one would with a de novo patient. Finally, the EP should consider Fournier’s gangrene in addition to testicular torsion and epididymitis in the differential diagnosis for acute scrotal pain.
1. Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
2. Eyre RC. Evaluation of acute scrotal pain in adults. UpToDate Web site. https://www.uptodate.com/contents/evaluation-of-acute-scrotal-pain-in-adults. Updated July 31, 2017. Accessed September 7, 2017.
3. Shen Y, Liu H, Cheng J, Bu P. Amiodarone-induced epididymitis: a pathologically confirmed case report and review of the literature. Cardiology. 2014;128(4):349-351. doi:10.1159/000361038.
4. Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35(1):101-108. doi:10.1016/j.ucl.2007.09.013.
5. Wampler SM, Llanes M. Common scrotal and testicular problems. Prim Care. 2010;37(3):613-626. doi:10.1016/j.pop.2010.04.009.
6. Dunne PJ, O’Loughlin BS. Testicular torsion: time is the enemy. Aust NZ J Surg. 2000;70(6):441-442.
7. Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002;167(5):2109-2110.
1. Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
2. Eyre RC. Evaluation of acute scrotal pain in adults. UpToDate Web site. https://www.uptodate.com/contents/evaluation-of-acute-scrotal-pain-in-adults. Updated July 31, 2017. Accessed September 7, 2017.
3. Shen Y, Liu H, Cheng J, Bu P. Amiodarone-induced epididymitis: a pathologically confirmed case report and review of the literature. Cardiology. 2014;128(4):349-351. doi:10.1159/000361038.
4. Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35(1):101-108. doi:10.1016/j.ucl.2007.09.013.
5. Wampler SM, Llanes M. Common scrotal and testicular problems. Prim Care. 2010;37(3):613-626. doi:10.1016/j.pop.2010.04.009.
6. Dunne PJ, O’Loughlin BS. Testicular torsion: time is the enemy. Aust NZ J Surg. 2000;70(6):441-442.
7. Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002;167(5):2109-2110.