User login
Woman dies following cervical cone biopsy: $4.25M award
Woman dies following cervical cone biopsy: $4.25M award
A 46-year-old woman underwent a cervical cone biopsy at a Veterans Administration (VA) hospital on July 18. Following the test, significant bleeding occurred. The gynecologic surgeon attempted to control the hemorrhage by injecting fe
ESTATE'S CLAIM:
The surgeon’s actions were negligent. She removed too much tissue during the biopsy, injured the vaginal and uterine walls, and failed to timely diagnose and appropriately treat the injuries. The ferric subsulfate solution entered the abdominal cavity via the perforation, causing peritonitis and bowel injuries. A pathology report from the bowel resection surgery informed the surgeon that the bowel was not properly reconnected after the damaged portion was removed, but this condition was neither detected intraoperatively nor treated postoperatively.
DEFENDANTS' DEFENSE:
The surgeon moved for summary judgment, countering that, as a federal employee, she was exempt from personal liability for the services performed as an employee of the VA. That motion was denied. She then argued that injury to the vaginal/uterine wall is a known complication of the biopsy procedure.
VERDICT:
A $4.25 million Illinois verdict was returned in federal court.
Related article:
Reducing maternal mortality in the United States—Let’s get organized!
Needle stick not reported to patient
A woman delivered a baby assisted by an on-call ObGyn. When the baby developed fetal tachycardia, the ObGyn recommended expediting delivery and discussed various options and the risks of each option. The mother chose a vaginal forceps delivery. During the procedure, the mother experienced a 3rd-degree perineal laceration and a few minor lacerations, which were repaired. The mother was in pain, so the ObGyn performed a revision repair. During the procedure, the ObGyn accidentally stuck himself with a clean needle. He replaced the needle and changed his glove. The mother reported instant pain relief following revision and was discharged. After the needle incident, the ObGyn’s thumb became red and swollen, so he took antibiotics.
Two days after discharge, the patient reported to the ObGyn’s office with fever, pain, and a foul odor emanating from the surgery site. She was given the diagnosis of pelvic incisional cellulitis and was taken to the operating room for exploration and debridement. The patient developed septic shock and necrotizing fasciitis. She was placed on a ventilator and underwent 13 surgeries.
PATIENTS' CLAIM:
The ObGyn was negligent. The patient claimed breach of duty: the ObGyn did not disclose that his thumb was swollen and that he took antibiotics.
PHYSICIANS' DEFENSE:
There was no breach of duty. He did not feel the need to concern the patient about an injury to himself that did not affect her.
VERDICT:
A Kansas defense verdict was returned.
Related article:
2017 Update on infectious disease
Catheter removal, air embolism: $3.5M settlement
A 44-year-old woman underwent gynecologic surgery on April 22. She developed a rectovaginal fistula and other complications. Intravenous antibiotics were required and parenteral nutrition was delivered through a central venous catheter. On May 22, after a hospital nurse removed the catheter, an air embolism developed, causing a brain injury. The patient has a mental disability and residual leg tremors.
PATIENTS' CLAIM:
Because of the surgeon’s negligence during surgery, a fistula developed. The nurse negligently removed the catheter, causing the embolism.
DEFENDANTS' DEFENSE:
The case settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached, including payments of $1 million from the surgeon and $2.5 million from the hospital.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Woman dies following cervical cone biopsy: $4.25M award
A 46-year-old woman underwent a cervical cone biopsy at a Veterans Administration (VA) hospital on July 18. Following the test, significant bleeding occurred. The gynecologic surgeon attempted to control the hemorrhage by injecting fe
ESTATE'S CLAIM:
The surgeon’s actions were negligent. She removed too much tissue during the biopsy, injured the vaginal and uterine walls, and failed to timely diagnose and appropriately treat the injuries. The ferric subsulfate solution entered the abdominal cavity via the perforation, causing peritonitis and bowel injuries. A pathology report from the bowel resection surgery informed the surgeon that the bowel was not properly reconnected after the damaged portion was removed, but this condition was neither detected intraoperatively nor treated postoperatively.
DEFENDANTS' DEFENSE:
The surgeon moved for summary judgment, countering that, as a federal employee, she was exempt from personal liability for the services performed as an employee of the VA. That motion was denied. She then argued that injury to the vaginal/uterine wall is a known complication of the biopsy procedure.
VERDICT:
A $4.25 million Illinois verdict was returned in federal court.
Related article:
Reducing maternal mortality in the United States—Let’s get organized!
Needle stick not reported to patient
A woman delivered a baby assisted by an on-call ObGyn. When the baby developed fetal tachycardia, the ObGyn recommended expediting delivery and discussed various options and the risks of each option. The mother chose a vaginal forceps delivery. During the procedure, the mother experienced a 3rd-degree perineal laceration and a few minor lacerations, which were repaired. The mother was in pain, so the ObGyn performed a revision repair. During the procedure, the ObGyn accidentally stuck himself with a clean needle. He replaced the needle and changed his glove. The mother reported instant pain relief following revision and was discharged. After the needle incident, the ObGyn’s thumb became red and swollen, so he took antibiotics.
Two days after discharge, the patient reported to the ObGyn’s office with fever, pain, and a foul odor emanating from the surgery site. She was given the diagnosis of pelvic incisional cellulitis and was taken to the operating room for exploration and debridement. The patient developed septic shock and necrotizing fasciitis. She was placed on a ventilator and underwent 13 surgeries.
PATIENTS' CLAIM:
The ObGyn was negligent. The patient claimed breach of duty: the ObGyn did not disclose that his thumb was swollen and that he took antibiotics.
PHYSICIANS' DEFENSE:
There was no breach of duty. He did not feel the need to concern the patient about an injury to himself that did not affect her.
VERDICT:
A Kansas defense verdict was returned.
Related article:
2017 Update on infectious disease
Catheter removal, air embolism: $3.5M settlement
A 44-year-old woman underwent gynecologic surgery on April 22. She developed a rectovaginal fistula and other complications. Intravenous antibiotics were required and parenteral nutrition was delivered through a central venous catheter. On May 22, after a hospital nurse removed the catheter, an air embolism developed, causing a brain injury. The patient has a mental disability and residual leg tremors.
PATIENTS' CLAIM:
Because of the surgeon’s negligence during surgery, a fistula developed. The nurse negligently removed the catheter, causing the embolism.
DEFENDANTS' DEFENSE:
The case settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached, including payments of $1 million from the surgeon and $2.5 million from the hospital.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Woman dies following cervical cone biopsy: $4.25M award
A 46-year-old woman underwent a cervical cone biopsy at a Veterans Administration (VA) hospital on July 18. Following the test, significant bleeding occurred. The gynecologic surgeon attempted to control the hemorrhage by injecting fe
ESTATE'S CLAIM:
The surgeon’s actions were negligent. She removed too much tissue during the biopsy, injured the vaginal and uterine walls, and failed to timely diagnose and appropriately treat the injuries. The ferric subsulfate solution entered the abdominal cavity via the perforation, causing peritonitis and bowel injuries. A pathology report from the bowel resection surgery informed the surgeon that the bowel was not properly reconnected after the damaged portion was removed, but this condition was neither detected intraoperatively nor treated postoperatively.
DEFENDANTS' DEFENSE:
The surgeon moved for summary judgment, countering that, as a federal employee, she was exempt from personal liability for the services performed as an employee of the VA. That motion was denied. She then argued that injury to the vaginal/uterine wall is a known complication of the biopsy procedure.
VERDICT:
A $4.25 million Illinois verdict was returned in federal court.
Related article:
Reducing maternal mortality in the United States—Let’s get organized!
Needle stick not reported to patient
A woman delivered a baby assisted by an on-call ObGyn. When the baby developed fetal tachycardia, the ObGyn recommended expediting delivery and discussed various options and the risks of each option. The mother chose a vaginal forceps delivery. During the procedure, the mother experienced a 3rd-degree perineal laceration and a few minor lacerations, which were repaired. The mother was in pain, so the ObGyn performed a revision repair. During the procedure, the ObGyn accidentally stuck himself with a clean needle. He replaced the needle and changed his glove. The mother reported instant pain relief following revision and was discharged. After the needle incident, the ObGyn’s thumb became red and swollen, so he took antibiotics.
Two days after discharge, the patient reported to the ObGyn’s office with fever, pain, and a foul odor emanating from the surgery site. She was given the diagnosis of pelvic incisional cellulitis and was taken to the operating room for exploration and debridement. The patient developed septic shock and necrotizing fasciitis. She was placed on a ventilator and underwent 13 surgeries.
PATIENTS' CLAIM:
The ObGyn was negligent. The patient claimed breach of duty: the ObGyn did not disclose that his thumb was swollen and that he took antibiotics.
PHYSICIANS' DEFENSE:
There was no breach of duty. He did not feel the need to concern the patient about an injury to himself that did not affect her.
VERDICT:
A Kansas defense verdict was returned.
Related article:
2017 Update on infectious disease
Catheter removal, air embolism: $3.5M settlement
A 44-year-old woman underwent gynecologic surgery on April 22. She developed a rectovaginal fistula and other complications. Intravenous antibiotics were required and parenteral nutrition was delivered through a central venous catheter. On May 22, after a hospital nurse removed the catheter, an air embolism developed, causing a brain injury. The patient has a mental disability and residual leg tremors.
PATIENTS' CLAIM:
Because of the surgeon’s negligence during surgery, a fistula developed. The nurse negligently removed the catheter, causing the embolism.
DEFENDANTS' DEFENSE:
The case settled during the trial.
VERDICT:
A $3.5 million Illinois settlement was reached, including payments of $1 million from the surgeon and $2.5 million from the hospital.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Considering work as an expert witness? Look before you leap!
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
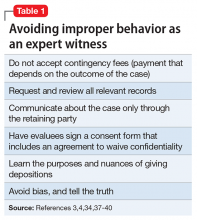
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
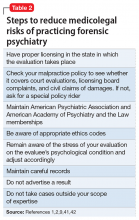
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
Suture found in bladder after hysterectomy
Suture found in bladder after hysterectomy
A 40-year-old woman underwent a hysterectomy due to dysmenorrhea. Despite the presence of blood in the catheter bag after the procedure, the surgeon did not consult a urologist or perform a cystoscopy. Later, when the patient reported urinary retention, urinary leakage, and dyspareunia, a urologist performed a cystoscopy and discovered a suture in the bladder wall and a vesicovaginal fistula.
PATIENTS' CLAIM:
During the procedure, the gynecologic surgeon inadvertently placed a suture in the bladder wall. The presence of blood in the Foley catheter required an immediate urology consult and cystoscopy, during which the presence of the errant suture would have been discovered. Repair surgery then would have prevented subsequent injuries.
PHYSICIANS' DEFENSE:
The surgeon used reasonable judgment, as there were explanations for the blood in the catheter due to a difficult catheter placement and lysis of bladder adhesions.
VERDICT:
A Michigan defense verdict was returned.
Related article:
How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy
Bowel injury during tubal ligation
A 40-year-old woman underwent laparoscopic tubal ligation using cauterization at an outpatient surgery center. Two hours after the procedure, her BP began to drop. She was promptly transferred to a hospital and underwent emergency surgery that revealed a bowel injury. Part of the patient’s small intestine was resected.
PATIENTS' CLAIM:
The gynecologic surgeon committed a medical error when she injured the bowel during trocar insertion.
DEFENDANTS' DEFENSE:
The bowel injury was a known complication of the surgery.
VERDICT:
A Louisiana defense verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Colon injured twice: $1M settlement
A 59-year-old woman underwent laparoscopic total hysterectomy and salpingectomy. Her history included an umbilical hernia repair.
Two days after surgery, the patient experienced abdominal pain, chills, abdominal distention, and a foul-smelling discharge from her umbilical suture site. She went to the emergency department where a computed tomography scan revealed 2 injuries in the bowel. Emergency laparotomy included transverse colon resection and right colon colostomy with Hartmann’s pouch. She wore an ostomy bag for 8 months. She developed an infection because of the colostomy and also required operations to resolve a bowel obstruction and repair incisional hernias.
PATIENTS' CLAIM:
The gynecologic surgeon was negligent when performing the surgery. When he inserted the Veress needle and trocar through the patient’s umbilicus, the transverse colon was injured twice with a 3-cm anterior tear and a 1-cm posterior laceration. The injuries were not discovered during the procedure. He should have been more careful knowing that she had undergone prior umbilical hernia surgery.
PHYSICIANS' DEFENSE:
The case was settled before the trial began.
VERDICT:
A $1 million Virginia settlement was reached.
Chronic pain after sling procedure: $2M verdict
A 63-year-old woman reported urinary incontinence to her gynecologist, who performed a transobturator midurethral sling procedure. After surgery, the patient experienced pelvic pain, urinary urgency, intermittent incontinence, and dyspareunia. She returned to the gynecologist twice. He performed a cystoscopy after the second visit but found nothing wrong.
The patient sought a second opinion. A gynecologic surgeon found a large mass in the patient’s bladder consisting of a crystallized piece of tape that had been used to secure the sling supporting the bladder. The mass was removed and the patient reported that, although surgery alleviated many symptoms, she was not pain-free.
PATIENTS' CLAIM:
The gynecologist negligently inserted the end of the sling through one wall of her bladder and failed to detect the malpositioning during surgery or later. He failed to diagnose and treat bladder stones that resulted from the sling’s malpositioning. He failed to perform a cystoscopy when she first reported symptoms and improperly performed cystoscopy at the second visit.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the gynecologist. The patient did not report ongoing symptoms until 1 year after sling insertion.
VERDICT:
A $2 million Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Suture found in bladder after hysterectomy
A 40-year-old woman underwent a hysterectomy due to dysmenorrhea. Despite the presence of blood in the catheter bag after the procedure, the surgeon did not consult a urologist or perform a cystoscopy. Later, when the patient reported urinary retention, urinary leakage, and dyspareunia, a urologist performed a cystoscopy and discovered a suture in the bladder wall and a vesicovaginal fistula.
PATIENTS' CLAIM:
During the procedure, the gynecologic surgeon inadvertently placed a suture in the bladder wall. The presence of blood in the Foley catheter required an immediate urology consult and cystoscopy, during which the presence of the errant suture would have been discovered. Repair surgery then would have prevented subsequent injuries.
PHYSICIANS' DEFENSE:
The surgeon used reasonable judgment, as there were explanations for the blood in the catheter due to a difficult catheter placement and lysis of bladder adhesions.
VERDICT:
A Michigan defense verdict was returned.
Related article:
How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy
Bowel injury during tubal ligation
A 40-year-old woman underwent laparoscopic tubal ligation using cauterization at an outpatient surgery center. Two hours after the procedure, her BP began to drop. She was promptly transferred to a hospital and underwent emergency surgery that revealed a bowel injury. Part of the patient’s small intestine was resected.
PATIENTS' CLAIM:
The gynecologic surgeon committed a medical error when she injured the bowel during trocar insertion.
DEFENDANTS' DEFENSE:
The bowel injury was a known complication of the surgery.
VERDICT:
A Louisiana defense verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Colon injured twice: $1M settlement
A 59-year-old woman underwent laparoscopic total hysterectomy and salpingectomy. Her history included an umbilical hernia repair.
Two days after surgery, the patient experienced abdominal pain, chills, abdominal distention, and a foul-smelling discharge from her umbilical suture site. She went to the emergency department where a computed tomography scan revealed 2 injuries in the bowel. Emergency laparotomy included transverse colon resection and right colon colostomy with Hartmann’s pouch. She wore an ostomy bag for 8 months. She developed an infection because of the colostomy and also required operations to resolve a bowel obstruction and repair incisional hernias.
PATIENTS' CLAIM:
The gynecologic surgeon was negligent when performing the surgery. When he inserted the Veress needle and trocar through the patient’s umbilicus, the transverse colon was injured twice with a 3-cm anterior tear and a 1-cm posterior laceration. The injuries were not discovered during the procedure. He should have been more careful knowing that she had undergone prior umbilical hernia surgery.
PHYSICIANS' DEFENSE:
The case was settled before the trial began.
VERDICT:
A $1 million Virginia settlement was reached.
Chronic pain after sling procedure: $2M verdict
A 63-year-old woman reported urinary incontinence to her gynecologist, who performed a transobturator midurethral sling procedure. After surgery, the patient experienced pelvic pain, urinary urgency, intermittent incontinence, and dyspareunia. She returned to the gynecologist twice. He performed a cystoscopy after the second visit but found nothing wrong.
The patient sought a second opinion. A gynecologic surgeon found a large mass in the patient’s bladder consisting of a crystallized piece of tape that had been used to secure the sling supporting the bladder. The mass was removed and the patient reported that, although surgery alleviated many symptoms, she was not pain-free.
PATIENTS' CLAIM:
The gynecologist negligently inserted the end of the sling through one wall of her bladder and failed to detect the malpositioning during surgery or later. He failed to diagnose and treat bladder stones that resulted from the sling’s malpositioning. He failed to perform a cystoscopy when she first reported symptoms and improperly performed cystoscopy at the second visit.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the gynecologist. The patient did not report ongoing symptoms until 1 year after sling insertion.
VERDICT:
A $2 million Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Suture found in bladder after hysterectomy
A 40-year-old woman underwent a hysterectomy due to dysmenorrhea. Despite the presence of blood in the catheter bag after the procedure, the surgeon did not consult a urologist or perform a cystoscopy. Later, when the patient reported urinary retention, urinary leakage, and dyspareunia, a urologist performed a cystoscopy and discovered a suture in the bladder wall and a vesicovaginal fistula.
PATIENTS' CLAIM:
During the procedure, the gynecologic surgeon inadvertently placed a suture in the bladder wall. The presence of blood in the Foley catheter required an immediate urology consult and cystoscopy, during which the presence of the errant suture would have been discovered. Repair surgery then would have prevented subsequent injuries.
PHYSICIANS' DEFENSE:
The surgeon used reasonable judgment, as there were explanations for the blood in the catheter due to a difficult catheter placement and lysis of bladder adhesions.
VERDICT:
A Michigan defense verdict was returned.
Related article:
How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy
Bowel injury during tubal ligation
A 40-year-old woman underwent laparoscopic tubal ligation using cauterization at an outpatient surgery center. Two hours after the procedure, her BP began to drop. She was promptly transferred to a hospital and underwent emergency surgery that revealed a bowel injury. Part of the patient’s small intestine was resected.
PATIENTS' CLAIM:
The gynecologic surgeon committed a medical error when she injured the bowel during trocar insertion.
DEFENDANTS' DEFENSE:
The bowel injury was a known complication of the surgery.
VERDICT:
A Louisiana defense verdict was returned.
Related article:
How to avoid major vessel injury during gynecologic laparoscopy
Colon injured twice: $1M settlement
A 59-year-old woman underwent laparoscopic total hysterectomy and salpingectomy. Her history included an umbilical hernia repair.
Two days after surgery, the patient experienced abdominal pain, chills, abdominal distention, and a foul-smelling discharge from her umbilical suture site. She went to the emergency department where a computed tomography scan revealed 2 injuries in the bowel. Emergency laparotomy included transverse colon resection and right colon colostomy with Hartmann’s pouch. She wore an ostomy bag for 8 months. She developed an infection because of the colostomy and also required operations to resolve a bowel obstruction and repair incisional hernias.
PATIENTS' CLAIM:
The gynecologic surgeon was negligent when performing the surgery. When he inserted the Veress needle and trocar through the patient’s umbilicus, the transverse colon was injured twice with a 3-cm anterior tear and a 1-cm posterior laceration. The injuries were not discovered during the procedure. He should have been more careful knowing that she had undergone prior umbilical hernia surgery.
PHYSICIANS' DEFENSE:
The case was settled before the trial began.
VERDICT:
A $1 million Virginia settlement was reached.
Chronic pain after sling procedure: $2M verdict
A 63-year-old woman reported urinary incontinence to her gynecologist, who performed a transobturator midurethral sling procedure. After surgery, the patient experienced pelvic pain, urinary urgency, intermittent incontinence, and dyspareunia. She returned to the gynecologist twice. He performed a cystoscopy after the second visit but found nothing wrong.
The patient sought a second opinion. A gynecologic surgeon found a large mass in the patient’s bladder consisting of a crystallized piece of tape that had been used to secure the sling supporting the bladder. The mass was removed and the patient reported that, although surgery alleviated many symptoms, she was not pain-free.
PATIENTS' CLAIM:
The gynecologist negligently inserted the end of the sling through one wall of her bladder and failed to detect the malpositioning during surgery or later. He failed to diagnose and treat bladder stones that resulted from the sling’s malpositioning. He failed to perform a cystoscopy when she first reported symptoms and improperly performed cystoscopy at the second visit.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the gynecologist. The patient did not report ongoing symptoms until 1 year after sling insertion.
VERDICT:
A $2 million Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Premature birth after preeclampsia: $23.1M verdict
Premature birth after preeclampsia: $23.1M verdict
When a woman saw her ObGyn on August 16 at 24 weeks’ gestation, test results showed proteinuria and high blood pressure (BP). The following day, she was hospitalized for a 24-hour urine test and BP evaluation supervised by an on-call ObGyn and her ObGyn. Test results confirmed preeclampsia. She was released from the hospital. A few days later, she was found to have continued high BP and increased proteinuria, and restricted fetal growth was detected. On August 29 at 26 weeks’ gestation, the baby girl was born with severe cystic periventricular leukomalacia by emergency cesarean delivery. She cannot perform basic tasks and will need 24-hour care for the rest of her life.
PARENTS' CLAIM:
The hospital staff and 2 ObGyns failed to timely diagnose and treat preeclampsia. The treating ObGyn neither prescribed medication to treat preeclampsia nor administered antenatal corticosteroids to enhance fetal lung and brain development, both of which should have been started on August 17. Hospital health care providers failed to transfer her to a Level III facility equipped to handle a premature birth of less than 33 weeks’ gestation.
DEFENDANTS' DEFENSE:
The hospital and ObGyn denied negligence.
VERDICT:
Prior to trial, the mother settled with the on-call ObGyn for an undisclosed amount. A $23.15 million Florida verdict was returned, apportioning 70% liability to the treating ObGyn and 30% to the hospital.
Related article:
For the management of labor, patience is a virtue
Shoulder dystocia, paralysis: $950,000 settlement
During delivery, shoulder dystocia was encountered. The ObGyn used maneuvers to release the shoulder and completed the delivery. The child has a brachial plexus injury. Despite nerve graft surgery, her right arm, shoulder, and hand are paralyzed.
PARENTS' CLAIM:
The ObGyn failed to properly manage the delivery. Shoulder dystocia had been encountered during the delivery of a sibling, but the ObGyn failed to communicate the need for cesarean delivery in future pregnancies.
DEFENDANTS' DEFENSE:
There was no negligence. The case settled during trial.
VERDICT:
A $950,000 California settlement was reached with the hospital and ObGyn.
Related article:
Shoulder dystocia: Taking the fear out of management
Child has brachial plexus injury
A mother was admitted to the hospital shortly after her membranes broke. Meconium was detected but the fetal heart-rate (FHR) monitor results were normal. About 15 minutes after admission, she was seen by an attending ObGyn, who started oxytocin to induce labor. FHR monitoring results were acceptable throughout the day, and by midafternoon, the mother was ready to deliver. A fetal baseline heart rate of less than 110 bpm was detected as staff prepared for the delivery. Less than an hour later, the baby’s head crowned and the ObGyn quickly identified shoulder dystocia. Nurses repositioned the mother, the baby rotated, and was delivered. Apgar scores were normal despite a shoulder injury.
PARENTS' CLAIM:
The ObGyn caused the injury by using excessive force during delivery. After attempting gentle traction, the ObGyn should have changed strategies.
DEFENDANTS' DEFENSE:
The ObGyn asserted that she used gentle traction that prevented twisting or stretching the baby’s nerves. The birth was normal and she followed all protocols, resulting in the birth of a cognitively intact baby, as evidenced by the child’s Apgar scores. The baby was large and labor and delivery went very quickly, both factors that could have led to the baby’s injuries. The ObGyn’s actions did not cause the injuries.
VERDICT:
A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Premature birth after preeclampsia: $23.1M verdict
When a woman saw her ObGyn on August 16 at 24 weeks’ gestation, test results showed proteinuria and high blood pressure (BP). The following day, she was hospitalized for a 24-hour urine test and BP evaluation supervised by an on-call ObGyn and her ObGyn. Test results confirmed preeclampsia. She was released from the hospital. A few days later, she was found to have continued high BP and increased proteinuria, and restricted fetal growth was detected. On August 29 at 26 weeks’ gestation, the baby girl was born with severe cystic periventricular leukomalacia by emergency cesarean delivery. She cannot perform basic tasks and will need 24-hour care for the rest of her life.
PARENTS' CLAIM:
The hospital staff and 2 ObGyns failed to timely diagnose and treat preeclampsia. The treating ObGyn neither prescribed medication to treat preeclampsia nor administered antenatal corticosteroids to enhance fetal lung and brain development, both of which should have been started on August 17. Hospital health care providers failed to transfer her to a Level III facility equipped to handle a premature birth of less than 33 weeks’ gestation.
DEFENDANTS' DEFENSE:
The hospital and ObGyn denied negligence.
VERDICT:
Prior to trial, the mother settled with the on-call ObGyn for an undisclosed amount. A $23.15 million Florida verdict was returned, apportioning 70% liability to the treating ObGyn and 30% to the hospital.
Related article:
For the management of labor, patience is a virtue
Shoulder dystocia, paralysis: $950,000 settlement
During delivery, shoulder dystocia was encountered. The ObGyn used maneuvers to release the shoulder and completed the delivery. The child has a brachial plexus injury. Despite nerve graft surgery, her right arm, shoulder, and hand are paralyzed.
PARENTS' CLAIM:
The ObGyn failed to properly manage the delivery. Shoulder dystocia had been encountered during the delivery of a sibling, but the ObGyn failed to communicate the need for cesarean delivery in future pregnancies.
DEFENDANTS' DEFENSE:
There was no negligence. The case settled during trial.
VERDICT:
A $950,000 California settlement was reached with the hospital and ObGyn.
Related article:
Shoulder dystocia: Taking the fear out of management
Child has brachial plexus injury
A mother was admitted to the hospital shortly after her membranes broke. Meconium was detected but the fetal heart-rate (FHR) monitor results were normal. About 15 minutes after admission, she was seen by an attending ObGyn, who started oxytocin to induce labor. FHR monitoring results were acceptable throughout the day, and by midafternoon, the mother was ready to deliver. A fetal baseline heart rate of less than 110 bpm was detected as staff prepared for the delivery. Less than an hour later, the baby’s head crowned and the ObGyn quickly identified shoulder dystocia. Nurses repositioned the mother, the baby rotated, and was delivered. Apgar scores were normal despite a shoulder injury.
PARENTS' CLAIM:
The ObGyn caused the injury by using excessive force during delivery. After attempting gentle traction, the ObGyn should have changed strategies.
DEFENDANTS' DEFENSE:
The ObGyn asserted that she used gentle traction that prevented twisting or stretching the baby’s nerves. The birth was normal and she followed all protocols, resulting in the birth of a cognitively intact baby, as evidenced by the child’s Apgar scores. The baby was large and labor and delivery went very quickly, both factors that could have led to the baby’s injuries. The ObGyn’s actions did not cause the injuries.
VERDICT:
A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Premature birth after preeclampsia: $23.1M verdict
When a woman saw her ObGyn on August 16 at 24 weeks’ gestation, test results showed proteinuria and high blood pressure (BP). The following day, she was hospitalized for a 24-hour urine test and BP evaluation supervised by an on-call ObGyn and her ObGyn. Test results confirmed preeclampsia. She was released from the hospital. A few days later, she was found to have continued high BP and increased proteinuria, and restricted fetal growth was detected. On August 29 at 26 weeks’ gestation, the baby girl was born with severe cystic periventricular leukomalacia by emergency cesarean delivery. She cannot perform basic tasks and will need 24-hour care for the rest of her life.
PARENTS' CLAIM:
The hospital staff and 2 ObGyns failed to timely diagnose and treat preeclampsia. The treating ObGyn neither prescribed medication to treat preeclampsia nor administered antenatal corticosteroids to enhance fetal lung and brain development, both of which should have been started on August 17. Hospital health care providers failed to transfer her to a Level III facility equipped to handle a premature birth of less than 33 weeks’ gestation.
DEFENDANTS' DEFENSE:
The hospital and ObGyn denied negligence.
VERDICT:
Prior to trial, the mother settled with the on-call ObGyn for an undisclosed amount. A $23.15 million Florida verdict was returned, apportioning 70% liability to the treating ObGyn and 30% to the hospital.
Related article:
For the management of labor, patience is a virtue
Shoulder dystocia, paralysis: $950,000 settlement
During delivery, shoulder dystocia was encountered. The ObGyn used maneuvers to release the shoulder and completed the delivery. The child has a brachial plexus injury. Despite nerve graft surgery, her right arm, shoulder, and hand are paralyzed.
PARENTS' CLAIM:
The ObGyn failed to properly manage the delivery. Shoulder dystocia had been encountered during the delivery of a sibling, but the ObGyn failed to communicate the need for cesarean delivery in future pregnancies.
DEFENDANTS' DEFENSE:
There was no negligence. The case settled during trial.
VERDICT:
A $950,000 California settlement was reached with the hospital and ObGyn.
Related article:
Shoulder dystocia: Taking the fear out of management
Child has brachial plexus injury
A mother was admitted to the hospital shortly after her membranes broke. Meconium was detected but the fetal heart-rate (FHR) monitor results were normal. About 15 minutes after admission, she was seen by an attending ObGyn, who started oxytocin to induce labor. FHR monitoring results were acceptable throughout the day, and by midafternoon, the mother was ready to deliver. A fetal baseline heart rate of less than 110 bpm was detected as staff prepared for the delivery. Less than an hour later, the baby’s head crowned and the ObGyn quickly identified shoulder dystocia. Nurses repositioned the mother, the baby rotated, and was delivered. Apgar scores were normal despite a shoulder injury.
PARENTS' CLAIM:
The ObGyn caused the injury by using excessive force during delivery. After attempting gentle traction, the ObGyn should have changed strategies.
DEFENDANTS' DEFENSE:
The ObGyn asserted that she used gentle traction that prevented twisting or stretching the baby’s nerves. The birth was normal and she followed all protocols, resulting in the birth of a cognitively intact baby, as evidenced by the child’s Apgar scores. The baby was large and labor and delivery went very quickly, both factors that could have led to the baby’s injuries. The ObGyn’s actions did not cause the injuries.
VERDICT:
A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Malpractice Counsel: Never Too Young to Have a Heart Attack
Case
A 21-year-old woman presented to the ED for evaluation of severe chest pain radiating to her left arm, and associated shortness of breath, nausea, and vomiting. She stated that the pain started 2 hours earlier while she was resting and had become progressively worse. She denied any history of similar symptoms. The patient denied fever, chills, or cough. She stated that she was otherwise in good health and did not take any medication on a regular basis. Regarding her social history, she admitted to smoking one pack of cigarettes a day and drinking alcohol on occasion.
On physical examination, the patient appeared uncomfortable. Her vital signs were: blood pressure, 136/86 mm Hg; heart rate, 102 beats/min; respiratory rate, 22 breaths/min; and temperature, 98.60F. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. Auscultation of the lungs revealed clear breath sounds bilaterally. The heart examination revealed tachycardia, but with regular rhythm and without murmurs, rubs, or gallops. The abdomen was soft and nontender. No lower extremity examination was documented.
The patient was seen by a physician assistant (PA) in the ED. An electrocardiogram (ECG), complete blood count (CBC), basic metabolic profile (BMP), troponin level, chest X-ray (CXR), and urine pregnancy test were ordered. The patient was given intravenous (IV) fluids and prochlorperazine 10 mg IV. The ECG and CXR were interpreted as normal. The urine pregnancy test was negative, and the remaining blood test results were within normal limits.
The PA believed the patient suffered from gastroenteritis, coupled with anxiety. He discharged the patient home with instructions to drink clear liquids for 24 hours, and take the prescribed prochlorperazine tablets as needed for continued nausea and vomiting.
At home, the patient continued to experience increasingly severe chest pain, shortness of breath, and vomiting. The next morning, she could no longer tolerate the pain and returned to the same ED via emergency medical services.
The patient’s history and physical examination remained unchanged from her presentation 16 hours earlier. At this ED visit, the patient was seen by an emergency physician (EP) who, concerned the patient had suffered an ischemic coronary event, ordered repeat ECG, CBC, BMP, and troponin evaluation. The EP also contacted cardiology services, but the cardiologist did not see the patient for several hours. When the cardiologist evaluated the patient and interpreted the ECG, he was concerned for an ST-segment elevation myocardial infarction (STEMI), and activated the catheterization lab.
Unfortunately, the patient had significant myocardial damage, with a resulting ejection fraction of only 10%. She was judged to be a candidate for heart transplantation, and received a left ventricular assist device (LVAD) as a bridge until a suitable donor heart could be identified. One month after implantation of the LVAD, the patient experienced an ischemic stroke that resulted in dense left-side weakness, leaving her confined to bed.
The patient sued the PA, the EP, the hospital, and the cardiologist for failing to identify and treat the acute STEMI in a timely manner. The plaintiff claimed the STEMI began at her first presentation to the ED, and that it should have been diagnosed and treated at that time. The plaintiff further argued that she should at least have been monitored and undergone repeat testing (ie, ECG and troponin level evaluation) at the first visit, stating that if she had received proper treatment, she would not have required an LVAD and therefore would not have had a stroke. The patient also alleged that at the second ED visit, there was a significant time delay before she was taken to the catheterization lab, which resulted in additional myocardial injury.
The defendants argued the patient was appropriately evaluated and treated at the first presentation, and that there was no evidence to suggest an MI. The EP argued that the delay in the patient’s care at the second visit was not his fault. All of the parties involved negotiated a settlement in the amount of $6 million in favor of the plaintiff.
Discussion
Myocardial infarction in adults younger than age 45 years is relatively rare, comprising only 2% to 10% of all MIs.1,2 The percentage of MI in patients younger than age 25 years must be even smaller, but no good data are available. In fact, age 40 years and younger is usually an exclusion criteria in many of the multicenter studies involving MI. Women are relatively spared from coronary artery disease (CAD) before menopause, thanks to the cardioprotective effects of estrogen. Young women who do experience an MI usually will have cardiovascular risk factors, especially smoking.
Risk Factors for MI in Young Patients
Cigarette Smoking. When examining common risk factors in young patients who had an MI (defined as patients younger than age 45 years), cigarette smoking is the most common risk factor.1,2 Between 76% and 91% of young patients with an MI are smokers, compared to only 40% incidence in older patients.1 It is thought that cigarette smoking produces endothelial dysfunction and can precipitate coronary spasm.1
Nonatherosclerotic Etiology. Interestingly, several studies of MI in young patients found a higher incidence of nonatherosclerotic causes of MI in women compared to men.2 One explanation for this finding is that women experience vasospastic syndromes and hypercoagulable states, secondary to oral contraceptive use or hereditary coagulation disorders.2 It has also been shown that young women have more active platelets following an MI and experience plaque erosions, rather than the plaque ruptures that occur in men and older women.2,3
Hyperlipidemia. Hyperlipidemia is an additional risk factor for MI in the younger adult patient population. In one study of young patients who had an MI, hyperlipidemia was the most important risk factor, in the absence of other obvious risk factors.1,4 In fact, some researchers think hyperlipidemia may be a more reliable predictor of MI in patients aged 30 to 39 years than in older patients.1,5 Unfortunately, many of these young adults are not aware that they have hyperlipidemia until they experience a complication such as an acute coronary syndrome. With respect to the patient in this case, it is not clear from the published report whether or not she had hyperlipidemia.
Family History. Another risk factor for MI in younger patients is a positive family history of CAD in a first-degree relative younger than age 55 years.1 Siblings of a young patient who experienced an MI have up to a 10-fold increase for developing CAD.1 It is currently not known why a positive family history increases the risk of MI in younger patients, but it may be related to inherited disorders of lipid metabolism, blood coagulation, or other genetic factors.1
Drug Abuse. Finally, drug abuse must be considered in young patients presenting with an MI. The use of cocaine, methamphetamine, marijuana, and K2 (synthetic marijuana) have all been associated with MI, especially in young patients,6-9 who typically do not have cardiac risk factors and do not show evidence of atherosclerotic disease on cardiac catheterization. As for the patient in this case, we do not know if she used any illicit drugs prior to presentation.
Summary
This case underscores the importance of not excluding MI in the differential diagnosis based simply on age or sex. While MI is uncommon in a 21-year-old woman, it can and does occur. In young patients presenting with chest pain, it is important to obtain a thorough history, including smoking, family history of MI, hyperlipidemia, and illicit drug use. While MI may be low on the differential diagnosis, it still needs to be considered.
1. Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107(3):254-261.
2. Lawesson SS, Stenestrand U, Lagerqvist B, Wallentin L, Swahn E. Gender perspective on risk factors, coronary lesions and long-term outcome in young patients with ST-elevation myocardial infarction. Heart. 2010;96(6):453-459. doi:10.1136/hrt.2009.175463.
3. Burke AP, Farb A, Malcom G,Virmani R. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis. Am Heart J. 2001;141(2 Suppl):S58-S62.
4. Tomono S, Ohshima S, Murata K. The risk factors for ischemic heart disease in young adults. Jpn Circ J. 1990;54(4):436-441.
5. Gofman JW, Young W, Tandy R. Ischemic heart disease, atherosclerosis, and longevity. Circulation. 1966;34(4):679-697.
6. Zimmerman JL. Cocaine intoxication. Crit Care Clin. 2012;28(4):517-525. doi:10.1016/j.ccc.2012.07.003.
7. Hawley LA, Auten JD, Matteucci MJ, et al. Cardiac complications of adult methamphetamine exposures. J Emerg Med. 2013;45(6):821-827. doi:10.1016/j.jemermed.2013.04.061.
8. Bachs L, Mørland H. Acute cardiovascular fatalities following cannabis use. Forensic Sci Int. 2001;124(2-3):200-203.
9. Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128(6):e1622-e1627. doi:10.1542 peds.2010-3823.
Case
A 21-year-old woman presented to the ED for evaluation of severe chest pain radiating to her left arm, and associated shortness of breath, nausea, and vomiting. She stated that the pain started 2 hours earlier while she was resting and had become progressively worse. She denied any history of similar symptoms. The patient denied fever, chills, or cough. She stated that she was otherwise in good health and did not take any medication on a regular basis. Regarding her social history, she admitted to smoking one pack of cigarettes a day and drinking alcohol on occasion.
On physical examination, the patient appeared uncomfortable. Her vital signs were: blood pressure, 136/86 mm Hg; heart rate, 102 beats/min; respiratory rate, 22 breaths/min; and temperature, 98.60F. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. Auscultation of the lungs revealed clear breath sounds bilaterally. The heart examination revealed tachycardia, but with regular rhythm and without murmurs, rubs, or gallops. The abdomen was soft and nontender. No lower extremity examination was documented.
The patient was seen by a physician assistant (PA) in the ED. An electrocardiogram (ECG), complete blood count (CBC), basic metabolic profile (BMP), troponin level, chest X-ray (CXR), and urine pregnancy test were ordered. The patient was given intravenous (IV) fluids and prochlorperazine 10 mg IV. The ECG and CXR were interpreted as normal. The urine pregnancy test was negative, and the remaining blood test results were within normal limits.
The PA believed the patient suffered from gastroenteritis, coupled with anxiety. He discharged the patient home with instructions to drink clear liquids for 24 hours, and take the prescribed prochlorperazine tablets as needed for continued nausea and vomiting.
At home, the patient continued to experience increasingly severe chest pain, shortness of breath, and vomiting. The next morning, she could no longer tolerate the pain and returned to the same ED via emergency medical services.
The patient’s history and physical examination remained unchanged from her presentation 16 hours earlier. At this ED visit, the patient was seen by an emergency physician (EP) who, concerned the patient had suffered an ischemic coronary event, ordered repeat ECG, CBC, BMP, and troponin evaluation. The EP also contacted cardiology services, but the cardiologist did not see the patient for several hours. When the cardiologist evaluated the patient and interpreted the ECG, he was concerned for an ST-segment elevation myocardial infarction (STEMI), and activated the catheterization lab.
Unfortunately, the patient had significant myocardial damage, with a resulting ejection fraction of only 10%. She was judged to be a candidate for heart transplantation, and received a left ventricular assist device (LVAD) as a bridge until a suitable donor heart could be identified. One month after implantation of the LVAD, the patient experienced an ischemic stroke that resulted in dense left-side weakness, leaving her confined to bed.
The patient sued the PA, the EP, the hospital, and the cardiologist for failing to identify and treat the acute STEMI in a timely manner. The plaintiff claimed the STEMI began at her first presentation to the ED, and that it should have been diagnosed and treated at that time. The plaintiff further argued that she should at least have been monitored and undergone repeat testing (ie, ECG and troponin level evaluation) at the first visit, stating that if she had received proper treatment, she would not have required an LVAD and therefore would not have had a stroke. The patient also alleged that at the second ED visit, there was a significant time delay before she was taken to the catheterization lab, which resulted in additional myocardial injury.
The defendants argued the patient was appropriately evaluated and treated at the first presentation, and that there was no evidence to suggest an MI. The EP argued that the delay in the patient’s care at the second visit was not his fault. All of the parties involved negotiated a settlement in the amount of $6 million in favor of the plaintiff.
Discussion
Myocardial infarction in adults younger than age 45 years is relatively rare, comprising only 2% to 10% of all MIs.1,2 The percentage of MI in patients younger than age 25 years must be even smaller, but no good data are available. In fact, age 40 years and younger is usually an exclusion criteria in many of the multicenter studies involving MI. Women are relatively spared from coronary artery disease (CAD) before menopause, thanks to the cardioprotective effects of estrogen. Young women who do experience an MI usually will have cardiovascular risk factors, especially smoking.
Risk Factors for MI in Young Patients
Cigarette Smoking. When examining common risk factors in young patients who had an MI (defined as patients younger than age 45 years), cigarette smoking is the most common risk factor.1,2 Between 76% and 91% of young patients with an MI are smokers, compared to only 40% incidence in older patients.1 It is thought that cigarette smoking produces endothelial dysfunction and can precipitate coronary spasm.1
Nonatherosclerotic Etiology. Interestingly, several studies of MI in young patients found a higher incidence of nonatherosclerotic causes of MI in women compared to men.2 One explanation for this finding is that women experience vasospastic syndromes and hypercoagulable states, secondary to oral contraceptive use or hereditary coagulation disorders.2 It has also been shown that young women have more active platelets following an MI and experience plaque erosions, rather than the plaque ruptures that occur in men and older women.2,3
Hyperlipidemia. Hyperlipidemia is an additional risk factor for MI in the younger adult patient population. In one study of young patients who had an MI, hyperlipidemia was the most important risk factor, in the absence of other obvious risk factors.1,4 In fact, some researchers think hyperlipidemia may be a more reliable predictor of MI in patients aged 30 to 39 years than in older patients.1,5 Unfortunately, many of these young adults are not aware that they have hyperlipidemia until they experience a complication such as an acute coronary syndrome. With respect to the patient in this case, it is not clear from the published report whether or not she had hyperlipidemia.
Family History. Another risk factor for MI in younger patients is a positive family history of CAD in a first-degree relative younger than age 55 years.1 Siblings of a young patient who experienced an MI have up to a 10-fold increase for developing CAD.1 It is currently not known why a positive family history increases the risk of MI in younger patients, but it may be related to inherited disorders of lipid metabolism, blood coagulation, or other genetic factors.1
Drug Abuse. Finally, drug abuse must be considered in young patients presenting with an MI. The use of cocaine, methamphetamine, marijuana, and K2 (synthetic marijuana) have all been associated with MI, especially in young patients,6-9 who typically do not have cardiac risk factors and do not show evidence of atherosclerotic disease on cardiac catheterization. As for the patient in this case, we do not know if she used any illicit drugs prior to presentation.
Summary
This case underscores the importance of not excluding MI in the differential diagnosis based simply on age or sex. While MI is uncommon in a 21-year-old woman, it can and does occur. In young patients presenting with chest pain, it is important to obtain a thorough history, including smoking, family history of MI, hyperlipidemia, and illicit drug use. While MI may be low on the differential diagnosis, it still needs to be considered.
Case
A 21-year-old woman presented to the ED for evaluation of severe chest pain radiating to her left arm, and associated shortness of breath, nausea, and vomiting. She stated that the pain started 2 hours earlier while she was resting and had become progressively worse. She denied any history of similar symptoms. The patient denied fever, chills, or cough. She stated that she was otherwise in good health and did not take any medication on a regular basis. Regarding her social history, she admitted to smoking one pack of cigarettes a day and drinking alcohol on occasion.
On physical examination, the patient appeared uncomfortable. Her vital signs were: blood pressure, 136/86 mm Hg; heart rate, 102 beats/min; respiratory rate, 22 breaths/min; and temperature, 98.60F. Oxygen saturation was 97% on room air. The head, eyes, ears, nose, and throat examination was unremarkable. Auscultation of the lungs revealed clear breath sounds bilaterally. The heart examination revealed tachycardia, but with regular rhythm and without murmurs, rubs, or gallops. The abdomen was soft and nontender. No lower extremity examination was documented.
The patient was seen by a physician assistant (PA) in the ED. An electrocardiogram (ECG), complete blood count (CBC), basic metabolic profile (BMP), troponin level, chest X-ray (CXR), and urine pregnancy test were ordered. The patient was given intravenous (IV) fluids and prochlorperazine 10 mg IV. The ECG and CXR were interpreted as normal. The urine pregnancy test was negative, and the remaining blood test results were within normal limits.
The PA believed the patient suffered from gastroenteritis, coupled with anxiety. He discharged the patient home with instructions to drink clear liquids for 24 hours, and take the prescribed prochlorperazine tablets as needed for continued nausea and vomiting.
At home, the patient continued to experience increasingly severe chest pain, shortness of breath, and vomiting. The next morning, she could no longer tolerate the pain and returned to the same ED via emergency medical services.
The patient’s history and physical examination remained unchanged from her presentation 16 hours earlier. At this ED visit, the patient was seen by an emergency physician (EP) who, concerned the patient had suffered an ischemic coronary event, ordered repeat ECG, CBC, BMP, and troponin evaluation. The EP also contacted cardiology services, but the cardiologist did not see the patient for several hours. When the cardiologist evaluated the patient and interpreted the ECG, he was concerned for an ST-segment elevation myocardial infarction (STEMI), and activated the catheterization lab.
Unfortunately, the patient had significant myocardial damage, with a resulting ejection fraction of only 10%. She was judged to be a candidate for heart transplantation, and received a left ventricular assist device (LVAD) as a bridge until a suitable donor heart could be identified. One month after implantation of the LVAD, the patient experienced an ischemic stroke that resulted in dense left-side weakness, leaving her confined to bed.
The patient sued the PA, the EP, the hospital, and the cardiologist for failing to identify and treat the acute STEMI in a timely manner. The plaintiff claimed the STEMI began at her first presentation to the ED, and that it should have been diagnosed and treated at that time. The plaintiff further argued that she should at least have been monitored and undergone repeat testing (ie, ECG and troponin level evaluation) at the first visit, stating that if she had received proper treatment, she would not have required an LVAD and therefore would not have had a stroke. The patient also alleged that at the second ED visit, there was a significant time delay before she was taken to the catheterization lab, which resulted in additional myocardial injury.
The defendants argued the patient was appropriately evaluated and treated at the first presentation, and that there was no evidence to suggest an MI. The EP argued that the delay in the patient’s care at the second visit was not his fault. All of the parties involved negotiated a settlement in the amount of $6 million in favor of the plaintiff.
Discussion
Myocardial infarction in adults younger than age 45 years is relatively rare, comprising only 2% to 10% of all MIs.1,2 The percentage of MI in patients younger than age 25 years must be even smaller, but no good data are available. In fact, age 40 years and younger is usually an exclusion criteria in many of the multicenter studies involving MI. Women are relatively spared from coronary artery disease (CAD) before menopause, thanks to the cardioprotective effects of estrogen. Young women who do experience an MI usually will have cardiovascular risk factors, especially smoking.
Risk Factors for MI in Young Patients
Cigarette Smoking. When examining common risk factors in young patients who had an MI (defined as patients younger than age 45 years), cigarette smoking is the most common risk factor.1,2 Between 76% and 91% of young patients with an MI are smokers, compared to only 40% incidence in older patients.1 It is thought that cigarette smoking produces endothelial dysfunction and can precipitate coronary spasm.1
Nonatherosclerotic Etiology. Interestingly, several studies of MI in young patients found a higher incidence of nonatherosclerotic causes of MI in women compared to men.2 One explanation for this finding is that women experience vasospastic syndromes and hypercoagulable states, secondary to oral contraceptive use or hereditary coagulation disorders.2 It has also been shown that young women have more active platelets following an MI and experience plaque erosions, rather than the plaque ruptures that occur in men and older women.2,3
Hyperlipidemia. Hyperlipidemia is an additional risk factor for MI in the younger adult patient population. In one study of young patients who had an MI, hyperlipidemia was the most important risk factor, in the absence of other obvious risk factors.1,4 In fact, some researchers think hyperlipidemia may be a more reliable predictor of MI in patients aged 30 to 39 years than in older patients.1,5 Unfortunately, many of these young adults are not aware that they have hyperlipidemia until they experience a complication such as an acute coronary syndrome. With respect to the patient in this case, it is not clear from the published report whether or not she had hyperlipidemia.
Family History. Another risk factor for MI in younger patients is a positive family history of CAD in a first-degree relative younger than age 55 years.1 Siblings of a young patient who experienced an MI have up to a 10-fold increase for developing CAD.1 It is currently not known why a positive family history increases the risk of MI in younger patients, but it may be related to inherited disorders of lipid metabolism, blood coagulation, or other genetic factors.1
Drug Abuse. Finally, drug abuse must be considered in young patients presenting with an MI. The use of cocaine, methamphetamine, marijuana, and K2 (synthetic marijuana) have all been associated with MI, especially in young patients,6-9 who typically do not have cardiac risk factors and do not show evidence of atherosclerotic disease on cardiac catheterization. As for the patient in this case, we do not know if she used any illicit drugs prior to presentation.
Summary
This case underscores the importance of not excluding MI in the differential diagnosis based simply on age or sex. While MI is uncommon in a 21-year-old woman, it can and does occur. In young patients presenting with chest pain, it is important to obtain a thorough history, including smoking, family history of MI, hyperlipidemia, and illicit drug use. While MI may be low on the differential diagnosis, it still needs to be considered.
1. Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107(3):254-261.
2. Lawesson SS, Stenestrand U, Lagerqvist B, Wallentin L, Swahn E. Gender perspective on risk factors, coronary lesions and long-term outcome in young patients with ST-elevation myocardial infarction. Heart. 2010;96(6):453-459. doi:10.1136/hrt.2009.175463.
3. Burke AP, Farb A, Malcom G,Virmani R. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis. Am Heart J. 2001;141(2 Suppl):S58-S62.
4. Tomono S, Ohshima S, Murata K. The risk factors for ischemic heart disease in young adults. Jpn Circ J. 1990;54(4):436-441.
5. Gofman JW, Young W, Tandy R. Ischemic heart disease, atherosclerosis, and longevity. Circulation. 1966;34(4):679-697.
6. Zimmerman JL. Cocaine intoxication. Crit Care Clin. 2012;28(4):517-525. doi:10.1016/j.ccc.2012.07.003.
7. Hawley LA, Auten JD, Matteucci MJ, et al. Cardiac complications of adult methamphetamine exposures. J Emerg Med. 2013;45(6):821-827. doi:10.1016/j.jemermed.2013.04.061.
8. Bachs L, Mørland H. Acute cardiovascular fatalities following cannabis use. Forensic Sci Int. 2001;124(2-3):200-203.
9. Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128(6):e1622-e1627. doi:10.1542 peds.2010-3823.
1. Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107(3):254-261.
2. Lawesson SS, Stenestrand U, Lagerqvist B, Wallentin L, Swahn E. Gender perspective on risk factors, coronary lesions and long-term outcome in young patients with ST-elevation myocardial infarction. Heart. 2010;96(6):453-459. doi:10.1136/hrt.2009.175463.
3. Burke AP, Farb A, Malcom G,Virmani R. Effect of menopause on plaque morphologic characteristics in coronary atherosclerosis. Am Heart J. 2001;141(2 Suppl):S58-S62.
4. Tomono S, Ohshima S, Murata K. The risk factors for ischemic heart disease in young adults. Jpn Circ J. 1990;54(4):436-441.
5. Gofman JW, Young W, Tandy R. Ischemic heart disease, atherosclerosis, and longevity. Circulation. 1966;34(4):679-697.
6. Zimmerman JL. Cocaine intoxication. Crit Care Clin. 2012;28(4):517-525. doi:10.1016/j.ccc.2012.07.003.
7. Hawley LA, Auten JD, Matteucci MJ, et al. Cardiac complications of adult methamphetamine exposures. J Emerg Med. 2013;45(6):821-827. doi:10.1016/j.jemermed.2013.04.061.
8. Bachs L, Mørland H. Acute cardiovascular fatalities following cannabis use. Forensic Sci Int. 2001;124(2-3):200-203.
9. Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128(6):e1622-e1627. doi:10.1542 peds.2010-3823.
Woman dies after robotic hysterectomy: $5M verdict
Woman dies after robotic hysterectomy: $5M verdict
When a 36-year-old woman underwent robotic hysterectomy, the gynecologist inserted a plastic trocar and sleeve through the patient's umbilicus to access the abdominal cavity at 7:30 am.
The certified registered nurse anesthetist (CRNA) noted a significant abnormality in the patient's vital signs at 8:07 am and administered medication and fluids to treat a suspected blood loss. When the patient's heart rate became extremely elevated at 8:25 am, the CRNA administered another drug, which failed to bring the patient's heart rate down. At 8:37 am, the monitoring machine could not record the patient's blood pressure. The CRNA informed the surgeon of the patient's condition. The supervising anesthesiologist was called; he arrived at 8:45 am and determined that the patient was bleeding internally. He asked the surgeon if he could visualize any bleeding; the surgeon could not.
The patient's condition continued to deteriorate. At 9:05 am, her blood pressure was still undetectable on the monitor. A Code Blue was called at 9:30 am. Exploratory surgery and blood transfusions begun at 9:43 am were not able to counteract the patient's massive blood loss. After cardiac arrest, she was pronounced dead at 11:18 am.
ESTATE'S CLAIM:
The surgeon was negligent in lacerating the left common iliac artery when inserting the trocar, and in not detecting the injury intraoperatively.
The anesthesia staff was negligent. The CRNA did not inform the surgeon until the situation was dire. A simple procedure could have been performed at any time to check the patient's hematocrit and hemoglobin levels, but that was not done until 9:30 am. If the severity of the patient's condition had been determined earlier, blood transfusions and further treatment could have saved her life.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the surgeon or anesthesia team. The standard of care was met. Arterial laceration is a known risk of the surgery.
VERDICT:
A $5,008,922 Illinois verdict was returned against all defendants except the CRNA.
A woman with MS becomes incontinent after surgery
A 43-year-old woman with multiple sclerosis (MS) underwent a hysterectomy performed by a gynecologic surgeon. During surgery, the patient's ureter was injured, requiring additional surgery. The patient is now permanently incontinent.
PATIENT'S CLAIM:
During surgery, the surgeon constricted the ureter with stitches. A second surgery was needed to remove the stitches and reimplant the ureter. The second surgery left her permanently incontinent. Although incontinence is a known complication of the second surgery, the second surgery would not have been necessary if the surgeon had not injured the ureter during the first surgery. Incontinence was not a result of her MS as she was not incontinent before the second surgery.
DEFENDANTS' DEFENSE:
There was no deviation from the standard of care. There was no stitching around the ureter. The ureter was damaged by kinking, which was addressed during the second surgery. Incontinence was a result of her MS.
VERDICT:
A $700,000 South Carolina verdict was returned.
Bowel injury during robotic procedure: $6.25M settlement
A woman in her late 60s reported minor urinary incontinence to her gynecologist. She underwent robot-assisted laparoscopic hysterectomy with a sling procedure for pelvic prolapse. During the sling procedure, the transverse colon was injured. The patient developed sepsis, requiring multiple attempts at surgical repair, including colostomy. The patient requires a permanent colostomy. She has a malabsorption disorder and needs frequent intravenous treatment for dehydration.
PATIENT'S CLAIM:
The surgeon failed to properly control the robotic device, causing injury to the patient's bowel. The surgeon deviated from the standard of care by failing to convert from the robot-assisted laparoscopic procedure to an open procedure when complications arose. The injury was not properly treated before the surgeon closed the initial surgery, causing the patient to develop sepsis.
PHYSICIAN'S DEFENSE:
The surgeon claimed that the injuries and resulting sepsis were the fault of other physicians and hospital staff. The case settled during trial.
VERDICT:
A $6.25 million New Jersey settlement was reached.
Hydrothermal ablation led to genital burns
A woman SAW AN OBGYN on October 2 to report menorrhagia. She had been treated for uterine fibroids with a Mirena intrauterine device and hydrothermal ablation. Another physician had suggested hysterectomy, which she declined.
When the ObGyn found that the patient had an enlarged uterus, he ordered ultrasonography and an endometrial biopsy. On follow-up, the ObGyn provided options of robotic hysterectomy or operative hysteroscopy with hydrothermal ablation. The patient chose hysteroscopy and the procedure was scheduled for December 28.
During surgery, an improper seal to the cervix around the hydrothermal ablation sheath was detected before heating the fluid. A tenaculum and 2 sponges were placed on the cervix to help form a seal and the fluid was heated for 4 minutes. The procedure was aborted when fluid was seen to be leaking again. Instruments were removed after a cooling period. The patient was discharged from the surgery center the same day with a prescription for oral hydrocodone bitartrate and acetaminophen for pain.
On January 4, the patient reported severe vulvar pain. The ObGyn found thermal burns on both labia with possible cellulitis. He prescribed silver sulfadiazine cream twice daily, levofloxacin 500 mg for 7 days, and warm-water soaks. When the patient called to report continued pain on January 7, the hydrocodone and acetaminophen prescription was renewed. On January 8, the ObGyn found continued evidence of labia and introitus burns with no signs of infection. The patient was told to continue taking the oral pain medication and to apply topical lidocaine gel and silver sulfadiazine cream.
Examinations on January 11, 17, 24, and 31 showed continued evidence of active healing. When new evidence of vulvar ulceration with inflammation and infection appeared, supportive care and antibiotics were given. On February 7, granulation tissue had developed at the introitus with continued healing.
On March 27, she saw a gynecologist for dyspareunia. The skin was healed but a tender band of scar tissue was noted at the burn site. She was referred for physical therapy and given estradiol vaginal cream.
On December 11, the patient reported dyspareunia and depression to the gynecologist, who prescribed medication for depression and referred her to counseling.
PATIENT'S CLAIM:
The ObGyn was negligent in failing to maintain a proper seal around the hydrothermal ablation shield. The patient sustained second-degree burns to her genital area from the hot saline solution that leaked from the uterus. The injury caused lasting dyspareunia and depression.
PHYSICIAN'S DEFENSE:
There was no negligence. Once the ObGyn realized that the seal was incomplete, the procedure was stopped and the fluid cooled before being released. Burns were treated within the standard of care.
VERDICT:
A Texas defense verdict was returned based on a no- evidence partial summary judgment: neither the patient nor the expert witness supplied evidence to support the claims of gross negligence or exemplary damages against the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Woman dies after robotic hysterectomy: $5M verdict
When a 36-year-old woman underwent robotic hysterectomy, the gynecologist inserted a plastic trocar and sleeve through the patient's umbilicus to access the abdominal cavity at 7:30 am.
The certified registered nurse anesthetist (CRNA) noted a significant abnormality in the patient's vital signs at 8:07 am and administered medication and fluids to treat a suspected blood loss. When the patient's heart rate became extremely elevated at 8:25 am, the CRNA administered another drug, which failed to bring the patient's heart rate down. At 8:37 am, the monitoring machine could not record the patient's blood pressure. The CRNA informed the surgeon of the patient's condition. The supervising anesthesiologist was called; he arrived at 8:45 am and determined that the patient was bleeding internally. He asked the surgeon if he could visualize any bleeding; the surgeon could not.
The patient's condition continued to deteriorate. At 9:05 am, her blood pressure was still undetectable on the monitor. A Code Blue was called at 9:30 am. Exploratory surgery and blood transfusions begun at 9:43 am were not able to counteract the patient's massive blood loss. After cardiac arrest, she was pronounced dead at 11:18 am.
ESTATE'S CLAIM:
The surgeon was negligent in lacerating the left common iliac artery when inserting the trocar, and in not detecting the injury intraoperatively.
The anesthesia staff was negligent. The CRNA did not inform the surgeon until the situation was dire. A simple procedure could have been performed at any time to check the patient's hematocrit and hemoglobin levels, but that was not done until 9:30 am. If the severity of the patient's condition had been determined earlier, blood transfusions and further treatment could have saved her life.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the surgeon or anesthesia team. The standard of care was met. Arterial laceration is a known risk of the surgery.
VERDICT:
A $5,008,922 Illinois verdict was returned against all defendants except the CRNA.
A woman with MS becomes incontinent after surgery
A 43-year-old woman with multiple sclerosis (MS) underwent a hysterectomy performed by a gynecologic surgeon. During surgery, the patient's ureter was injured, requiring additional surgery. The patient is now permanently incontinent.
PATIENT'S CLAIM:
During surgery, the surgeon constricted the ureter with stitches. A second surgery was needed to remove the stitches and reimplant the ureter. The second surgery left her permanently incontinent. Although incontinence is a known complication of the second surgery, the second surgery would not have been necessary if the surgeon had not injured the ureter during the first surgery. Incontinence was not a result of her MS as she was not incontinent before the second surgery.
DEFENDANTS' DEFENSE:
There was no deviation from the standard of care. There was no stitching around the ureter. The ureter was damaged by kinking, which was addressed during the second surgery. Incontinence was a result of her MS.
VERDICT:
A $700,000 South Carolina verdict was returned.
Bowel injury during robotic procedure: $6.25M settlement
A woman in her late 60s reported minor urinary incontinence to her gynecologist. She underwent robot-assisted laparoscopic hysterectomy with a sling procedure for pelvic prolapse. During the sling procedure, the transverse colon was injured. The patient developed sepsis, requiring multiple attempts at surgical repair, including colostomy. The patient requires a permanent colostomy. She has a malabsorption disorder and needs frequent intravenous treatment for dehydration.
PATIENT'S CLAIM:
The surgeon failed to properly control the robotic device, causing injury to the patient's bowel. The surgeon deviated from the standard of care by failing to convert from the robot-assisted laparoscopic procedure to an open procedure when complications arose. The injury was not properly treated before the surgeon closed the initial surgery, causing the patient to develop sepsis.
PHYSICIAN'S DEFENSE:
The surgeon claimed that the injuries and resulting sepsis were the fault of other physicians and hospital staff. The case settled during trial.
VERDICT:
A $6.25 million New Jersey settlement was reached.
Hydrothermal ablation led to genital burns
A woman SAW AN OBGYN on October 2 to report menorrhagia. She had been treated for uterine fibroids with a Mirena intrauterine device and hydrothermal ablation. Another physician had suggested hysterectomy, which she declined.
When the ObGyn found that the patient had an enlarged uterus, he ordered ultrasonography and an endometrial biopsy. On follow-up, the ObGyn provided options of robotic hysterectomy or operative hysteroscopy with hydrothermal ablation. The patient chose hysteroscopy and the procedure was scheduled for December 28.
During surgery, an improper seal to the cervix around the hydrothermal ablation sheath was detected before heating the fluid. A tenaculum and 2 sponges were placed on the cervix to help form a seal and the fluid was heated for 4 minutes. The procedure was aborted when fluid was seen to be leaking again. Instruments were removed after a cooling period. The patient was discharged from the surgery center the same day with a prescription for oral hydrocodone bitartrate and acetaminophen for pain.
On January 4, the patient reported severe vulvar pain. The ObGyn found thermal burns on both labia with possible cellulitis. He prescribed silver sulfadiazine cream twice daily, levofloxacin 500 mg for 7 days, and warm-water soaks. When the patient called to report continued pain on January 7, the hydrocodone and acetaminophen prescription was renewed. On January 8, the ObGyn found continued evidence of labia and introitus burns with no signs of infection. The patient was told to continue taking the oral pain medication and to apply topical lidocaine gel and silver sulfadiazine cream.
Examinations on January 11, 17, 24, and 31 showed continued evidence of active healing. When new evidence of vulvar ulceration with inflammation and infection appeared, supportive care and antibiotics were given. On February 7, granulation tissue had developed at the introitus with continued healing.
On March 27, she saw a gynecologist for dyspareunia. The skin was healed but a tender band of scar tissue was noted at the burn site. She was referred for physical therapy and given estradiol vaginal cream.
On December 11, the patient reported dyspareunia and depression to the gynecologist, who prescribed medication for depression and referred her to counseling.
PATIENT'S CLAIM:
The ObGyn was negligent in failing to maintain a proper seal around the hydrothermal ablation shield. The patient sustained second-degree burns to her genital area from the hot saline solution that leaked from the uterus. The injury caused lasting dyspareunia and depression.
PHYSICIAN'S DEFENSE:
There was no negligence. Once the ObGyn realized that the seal was incomplete, the procedure was stopped and the fluid cooled before being released. Burns were treated within the standard of care.
VERDICT:
A Texas defense verdict was returned based on a no- evidence partial summary judgment: neither the patient nor the expert witness supplied evidence to support the claims of gross negligence or exemplary damages against the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Woman dies after robotic hysterectomy: $5M verdict
When a 36-year-old woman underwent robotic hysterectomy, the gynecologist inserted a plastic trocar and sleeve through the patient's umbilicus to access the abdominal cavity at 7:30 am.
The certified registered nurse anesthetist (CRNA) noted a significant abnormality in the patient's vital signs at 8:07 am and administered medication and fluids to treat a suspected blood loss. When the patient's heart rate became extremely elevated at 8:25 am, the CRNA administered another drug, which failed to bring the patient's heart rate down. At 8:37 am, the monitoring machine could not record the patient's blood pressure. The CRNA informed the surgeon of the patient's condition. The supervising anesthesiologist was called; he arrived at 8:45 am and determined that the patient was bleeding internally. He asked the surgeon if he could visualize any bleeding; the surgeon could not.
The patient's condition continued to deteriorate. At 9:05 am, her blood pressure was still undetectable on the monitor. A Code Blue was called at 9:30 am. Exploratory surgery and blood transfusions begun at 9:43 am were not able to counteract the patient's massive blood loss. After cardiac arrest, she was pronounced dead at 11:18 am.
ESTATE'S CLAIM:
The surgeon was negligent in lacerating the left common iliac artery when inserting the trocar, and in not detecting the injury intraoperatively.
The anesthesia staff was negligent. The CRNA did not inform the surgeon until the situation was dire. A simple procedure could have been performed at any time to check the patient's hematocrit and hemoglobin levels, but that was not done until 9:30 am. If the severity of the patient's condition had been determined earlier, blood transfusions and further treatment could have saved her life.
DEFENDANTS' DEFENSE:
There was no negligence on the part of the surgeon or anesthesia team. The standard of care was met. Arterial laceration is a known risk of the surgery.
VERDICT:
A $5,008,922 Illinois verdict was returned against all defendants except the CRNA.
A woman with MS becomes incontinent after surgery
A 43-year-old woman with multiple sclerosis (MS) underwent a hysterectomy performed by a gynecologic surgeon. During surgery, the patient's ureter was injured, requiring additional surgery. The patient is now permanently incontinent.
PATIENT'S CLAIM:
During surgery, the surgeon constricted the ureter with stitches. A second surgery was needed to remove the stitches and reimplant the ureter. The second surgery left her permanently incontinent. Although incontinence is a known complication of the second surgery, the second surgery would not have been necessary if the surgeon had not injured the ureter during the first surgery. Incontinence was not a result of her MS as she was not incontinent before the second surgery.
DEFENDANTS' DEFENSE:
There was no deviation from the standard of care. There was no stitching around the ureter. The ureter was damaged by kinking, which was addressed during the second surgery. Incontinence was a result of her MS.
VERDICT:
A $700,000 South Carolina verdict was returned.
Bowel injury during robotic procedure: $6.25M settlement
A woman in her late 60s reported minor urinary incontinence to her gynecologist. She underwent robot-assisted laparoscopic hysterectomy with a sling procedure for pelvic prolapse. During the sling procedure, the transverse colon was injured. The patient developed sepsis, requiring multiple attempts at surgical repair, including colostomy. The patient requires a permanent colostomy. She has a malabsorption disorder and needs frequent intravenous treatment for dehydration.
PATIENT'S CLAIM:
The surgeon failed to properly control the robotic device, causing injury to the patient's bowel. The surgeon deviated from the standard of care by failing to convert from the robot-assisted laparoscopic procedure to an open procedure when complications arose. The injury was not properly treated before the surgeon closed the initial surgery, causing the patient to develop sepsis.
PHYSICIAN'S DEFENSE:
The surgeon claimed that the injuries and resulting sepsis were the fault of other physicians and hospital staff. The case settled during trial.
VERDICT:
A $6.25 million New Jersey settlement was reached.
Hydrothermal ablation led to genital burns
A woman SAW AN OBGYN on October 2 to report menorrhagia. She had been treated for uterine fibroids with a Mirena intrauterine device and hydrothermal ablation. Another physician had suggested hysterectomy, which she declined.
When the ObGyn found that the patient had an enlarged uterus, he ordered ultrasonography and an endometrial biopsy. On follow-up, the ObGyn provided options of robotic hysterectomy or operative hysteroscopy with hydrothermal ablation. The patient chose hysteroscopy and the procedure was scheduled for December 28.
During surgery, an improper seal to the cervix around the hydrothermal ablation sheath was detected before heating the fluid. A tenaculum and 2 sponges were placed on the cervix to help form a seal and the fluid was heated for 4 minutes. The procedure was aborted when fluid was seen to be leaking again. Instruments were removed after a cooling period. The patient was discharged from the surgery center the same day with a prescription for oral hydrocodone bitartrate and acetaminophen for pain.
On January 4, the patient reported severe vulvar pain. The ObGyn found thermal burns on both labia with possible cellulitis. He prescribed silver sulfadiazine cream twice daily, levofloxacin 500 mg for 7 days, and warm-water soaks. When the patient called to report continued pain on January 7, the hydrocodone and acetaminophen prescription was renewed. On January 8, the ObGyn found continued evidence of labia and introitus burns with no signs of infection. The patient was told to continue taking the oral pain medication and to apply topical lidocaine gel and silver sulfadiazine cream.
Examinations on January 11, 17, 24, and 31 showed continued evidence of active healing. When new evidence of vulvar ulceration with inflammation and infection appeared, supportive care and antibiotics were given. On February 7, granulation tissue had developed at the introitus with continued healing.
On March 27, she saw a gynecologist for dyspareunia. The skin was healed but a tender band of scar tissue was noted at the burn site. She was referred for physical therapy and given estradiol vaginal cream.
On December 11, the patient reported dyspareunia and depression to the gynecologist, who prescribed medication for depression and referred her to counseling.
PATIENT'S CLAIM:
The ObGyn was negligent in failing to maintain a proper seal around the hydrothermal ablation shield. The patient sustained second-degree burns to her genital area from the hot saline solution that leaked from the uterus. The injury caused lasting dyspareunia and depression.
PHYSICIAN'S DEFENSE:
There was no negligence. Once the ObGyn realized that the seal was incomplete, the procedure was stopped and the fluid cooled before being released. Burns were treated within the standard of care.
VERDICT:
A Texas defense verdict was returned based on a no- evidence partial summary judgment: neither the patient nor the expert witness supplied evidence to support the claims of gross negligence or exemplary damages against the ObGyn.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Delay in delivery--mother and child die: $1.4M settlement
Delay in delivery--mother and child die: $1.4M settlement
ESTATE'S CLAIM:
The standard of care for placenta accreta requires delivery between 34 and 36 weeks of gestation. The mother died from a placental abruption and amniotic fluid embolism. Placenta accreta increases the risk of catastrophic hemorrhage. If delivery had occurred on January 14, both the mother and child would be alive.
DEFENDANTS' DEFENSE:
The case settled before trial.
VERDICT:
A $1.425 million Georgia settlement was reached. The settlement amount was limited by a damages cap unique to the defendant hospital.
Placental abruption not detected: $6.2M settlement
At 24 weeks of gestation, a mother presented to the hospital with premature contractions that subsided after her arrival. She was discharged from the hospital. The woman gave birth in her bathtub several hours later. The baby was 10 weeks premature. He suffered profound brain damage and has significant physical defects.
PARENT'S CLAIM:
Neither the ObGyn nor the hospital staff appreciated that the mother was experiencing placental abruption. If diagnosed, treatment could have prevented fetal injury.
DEFENDANTS' DEFENSE:
The case was settled prior to trial.
VERDICT:
A $6.2 million New York settlement was reached.
Child has brachial plexus injury: $2M award
A woman was admitted to the hospital for elective induction of labor. She gained a significant amount of weight while pregnant. During delivery, her family practitioner (FP) determined that vacuum extraction was needed but he was not qualified to use the device. An in-house ObGyn was called in to use the vacuum extractor. The FP delivered the baby's shoulders. The infant was born with a floppy right arm and later diagnosed with rupture injuries to the C-5 and C-6 vertebrae and permanent brachial plexus damage. She has limited range of motion in her right arm and shoulder.
PARENT'S CLAIM:
The FP was relatively inexperienced in labor and delivery. He should not have ordered vacuum extraction because of risk factors including the mother's small stature, her significant weight gain during pregnancy, the use of epidural anesthesia, and induction of labor. Using vacuum extraction increases the risk of shoulder dystocia.
The FP improperly applied excessive downward traction on the fetus causing the infant to sustain a brachial plexus injury.
The FP did not notify the parents of the child's injury immediately after birth; he told them about the injury just before discharge.
DEFENDANTS' DEFENSE:
There is no evidence in the medical records of a shoulder dystocia; "no shoulder dystocia" was charted shortly after delivery. No one in the delivery room testified to a delay in delivering the infant's shoulders. The mother's internal contractions caused the injury. The baby was not injured to the extent claimed.
VERDICT:
The ObGyn who used the vacuum extractor settled before the trial for $300,000. A $2 million Illinois verdict was returned against the FP.
Delay in treating infant in respiratory distress: $7.27M settlement
A child was delivered by a certified nurse midwife at a birthing center. At birth, the baby had a heart rate of 60 bpm and was in respiratory distress but there was no one at the clinic qualified to intubate the infant. Emergency personnel were called but the infant remained in respiratory distress for 8 minutes. The baby experienced birth asphyxia with hypoxic ischemic encephalopathy resulting in severe cerebral palsy.
PARENT'S CLAIM:
The birthing center was poorly staffed and unprepared to treat an emergency situation.
DEFENDANTS' DEFENSE:
The defendants denied all allegations of negligence. The case was settled during trial.
VERDICT:
A $7.27 million Pennsylvania settlement was reached.
Was the spinal block given at wrong level?
A MOTHER WENT TO THE HOSPITAL in labor. Prior to cesarean delivery, she underwent an anesthetic spinal block administered by a CRNA. Initially, the patient reported pain shortly after the injection was performed until the block worked. The baby's delivery was uneventful.
In recovery a few hours later, the patient reported intense and uncontrollable pain in her legs. Magnetic resonance imaging revealed a fluid pocket on her spinal cord at the L1-L2 level. The patient has permanent pain, numbness, and tingling in in both legs.
PATIENT'S CLAIM:
The CRNA failed to insert the spinal block needle in the proper location.
DEFENDANTS' DEFENSE:
The CRNA contended that he complied with the standard of care. He claimed that the patient had an unusual spinal cord anatomy: it was tethered down to the L3-L4 level.
VERDICT:
A $509,152 Kentucky verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Delay in delivery--mother and child die: $1.4M settlement
ESTATE'S CLAIM:
The standard of care for placenta accreta requires delivery between 34 and 36 weeks of gestation. The mother died from a placental abruption and amniotic fluid embolism. Placenta accreta increases the risk of catastrophic hemorrhage. If delivery had occurred on January 14, both the mother and child would be alive.
DEFENDANTS' DEFENSE:
The case settled before trial.
VERDICT:
A $1.425 million Georgia settlement was reached. The settlement amount was limited by a damages cap unique to the defendant hospital.
Placental abruption not detected: $6.2M settlement
At 24 weeks of gestation, a mother presented to the hospital with premature contractions that subsided after her arrival. She was discharged from the hospital. The woman gave birth in her bathtub several hours later. The baby was 10 weeks premature. He suffered profound brain damage and has significant physical defects.
PARENT'S CLAIM:
Neither the ObGyn nor the hospital staff appreciated that the mother was experiencing placental abruption. If diagnosed, treatment could have prevented fetal injury.
DEFENDANTS' DEFENSE:
The case was settled prior to trial.
VERDICT:
A $6.2 million New York settlement was reached.
Child has brachial plexus injury: $2M award
A woman was admitted to the hospital for elective induction of labor. She gained a significant amount of weight while pregnant. During delivery, her family practitioner (FP) determined that vacuum extraction was needed but he was not qualified to use the device. An in-house ObGyn was called in to use the vacuum extractor. The FP delivered the baby's shoulders. The infant was born with a floppy right arm and later diagnosed with rupture injuries to the C-5 and C-6 vertebrae and permanent brachial plexus damage. She has limited range of motion in her right arm and shoulder.
PARENT'S CLAIM:
The FP was relatively inexperienced in labor and delivery. He should not have ordered vacuum extraction because of risk factors including the mother's small stature, her significant weight gain during pregnancy, the use of epidural anesthesia, and induction of labor. Using vacuum extraction increases the risk of shoulder dystocia.
The FP improperly applied excessive downward traction on the fetus causing the infant to sustain a brachial plexus injury.
The FP did not notify the parents of the child's injury immediately after birth; he told them about the injury just before discharge.
DEFENDANTS' DEFENSE:
There is no evidence in the medical records of a shoulder dystocia; "no shoulder dystocia" was charted shortly after delivery. No one in the delivery room testified to a delay in delivering the infant's shoulders. The mother's internal contractions caused the injury. The baby was not injured to the extent claimed.
VERDICT:
The ObGyn who used the vacuum extractor settled before the trial for $300,000. A $2 million Illinois verdict was returned against the FP.
Delay in treating infant in respiratory distress: $7.27M settlement
A child was delivered by a certified nurse midwife at a birthing center. At birth, the baby had a heart rate of 60 bpm and was in respiratory distress but there was no one at the clinic qualified to intubate the infant. Emergency personnel were called but the infant remained in respiratory distress for 8 minutes. The baby experienced birth asphyxia with hypoxic ischemic encephalopathy resulting in severe cerebral palsy.
PARENT'S CLAIM:
The birthing center was poorly staffed and unprepared to treat an emergency situation.
DEFENDANTS' DEFENSE:
The defendants denied all allegations of negligence. The case was settled during trial.
VERDICT:
A $7.27 million Pennsylvania settlement was reached.
Was the spinal block given at wrong level?
A MOTHER WENT TO THE HOSPITAL in labor. Prior to cesarean delivery, she underwent an anesthetic spinal block administered by a CRNA. Initially, the patient reported pain shortly after the injection was performed until the block worked. The baby's delivery was uneventful.
In recovery a few hours later, the patient reported intense and uncontrollable pain in her legs. Magnetic resonance imaging revealed a fluid pocket on her spinal cord at the L1-L2 level. The patient has permanent pain, numbness, and tingling in in both legs.
PATIENT'S CLAIM:
The CRNA failed to insert the spinal block needle in the proper location.
DEFENDANTS' DEFENSE:
The CRNA contended that he complied with the standard of care. He claimed that the patient had an unusual spinal cord anatomy: it was tethered down to the L3-L4 level.
VERDICT:
A $509,152 Kentucky verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Delay in delivery--mother and child die: $1.4M settlement
ESTATE'S CLAIM:
The standard of care for placenta accreta requires delivery between 34 and 36 weeks of gestation. The mother died from a placental abruption and amniotic fluid embolism. Placenta accreta increases the risk of catastrophic hemorrhage. If delivery had occurred on January 14, both the mother and child would be alive.
DEFENDANTS' DEFENSE:
The case settled before trial.
VERDICT:
A $1.425 million Georgia settlement was reached. The settlement amount was limited by a damages cap unique to the defendant hospital.
Placental abruption not detected: $6.2M settlement
At 24 weeks of gestation, a mother presented to the hospital with premature contractions that subsided after her arrival. She was discharged from the hospital. The woman gave birth in her bathtub several hours later. The baby was 10 weeks premature. He suffered profound brain damage and has significant physical defects.
PARENT'S CLAIM:
Neither the ObGyn nor the hospital staff appreciated that the mother was experiencing placental abruption. If diagnosed, treatment could have prevented fetal injury.
DEFENDANTS' DEFENSE:
The case was settled prior to trial.
VERDICT:
A $6.2 million New York settlement was reached.
Child has brachial plexus injury: $2M award
A woman was admitted to the hospital for elective induction of labor. She gained a significant amount of weight while pregnant. During delivery, her family practitioner (FP) determined that vacuum extraction was needed but he was not qualified to use the device. An in-house ObGyn was called in to use the vacuum extractor. The FP delivered the baby's shoulders. The infant was born with a floppy right arm and later diagnosed with rupture injuries to the C-5 and C-6 vertebrae and permanent brachial plexus damage. She has limited range of motion in her right arm and shoulder.
PARENT'S CLAIM:
The FP was relatively inexperienced in labor and delivery. He should not have ordered vacuum extraction because of risk factors including the mother's small stature, her significant weight gain during pregnancy, the use of epidural anesthesia, and induction of labor. Using vacuum extraction increases the risk of shoulder dystocia.
The FP improperly applied excessive downward traction on the fetus causing the infant to sustain a brachial plexus injury.
The FP did not notify the parents of the child's injury immediately after birth; he told them about the injury just before discharge.
DEFENDANTS' DEFENSE:
There is no evidence in the medical records of a shoulder dystocia; "no shoulder dystocia" was charted shortly after delivery. No one in the delivery room testified to a delay in delivering the infant's shoulders. The mother's internal contractions caused the injury. The baby was not injured to the extent claimed.
VERDICT:
The ObGyn who used the vacuum extractor settled before the trial for $300,000. A $2 million Illinois verdict was returned against the FP.
Delay in treating infant in respiratory distress: $7.27M settlement
A child was delivered by a certified nurse midwife at a birthing center. At birth, the baby had a heart rate of 60 bpm and was in respiratory distress but there was no one at the clinic qualified to intubate the infant. Emergency personnel were called but the infant remained in respiratory distress for 8 minutes. The baby experienced birth asphyxia with hypoxic ischemic encephalopathy resulting in severe cerebral palsy.
PARENT'S CLAIM:
The birthing center was poorly staffed and unprepared to treat an emergency situation.
DEFENDANTS' DEFENSE:
The defendants denied all allegations of negligence. The case was settled during trial.
VERDICT:
A $7.27 million Pennsylvania settlement was reached.
Was the spinal block given at wrong level?
A MOTHER WENT TO THE HOSPITAL in labor. Prior to cesarean delivery, she underwent an anesthetic spinal block administered by a CRNA. Initially, the patient reported pain shortly after the injection was performed until the block worked. The baby's delivery was uneventful.
In recovery a few hours later, the patient reported intense and uncontrollable pain in her legs. Magnetic resonance imaging revealed a fluid pocket on her spinal cord at the L1-L2 level. The patient has permanent pain, numbness, and tingling in in both legs.
PATIENT'S CLAIM:
The CRNA failed to insert the spinal block needle in the proper location.
DEFENDANTS' DEFENSE:
The CRNA contended that he complied with the standard of care. He claimed that the patient had an unusual spinal cord anatomy: it was tethered down to the L3-L4 level.
VERDICT:
A $509,152 Kentucky verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.