User login
House bill would allow corrective action plan for DEA violators
A new bill aims to clarify the rules of the Controlled Substances Act to ensure that legitimate operators stay in business and patients get needed medication, according to congressional backers of the bill, which was approved by the House of Representatives on July 29.
The bill still has to be taken up by the Senate, where there is no companion legislation.
The Ensuring Patient Access and Effective Drug Enforcement Act of 2014 (H.R. 4709) would ensure that restrictions on distribution of controlled substances are not so onerous as to inhibit access for patients, would require the U.S. Attorney General to give DEA registrant pharmacies and physicians who violate the rules an opportunity to submit a corrective action plan that might defer suspension of their registration, and would establish a working group to make recommendations to Congress on federal policies to reduce prescription drug diversion and abuse.
These measures are among the major policy goals of the Alliance to Prevent the Abuse of Medicines. The Washington, D.C.–based group includes among its members the American Medical Association, Cardinal Health, CVS Caremark, the Health Industry Distributors Association, and Teva.
The National Association of Chain Drug Stores "and chain pharmacy are committed to partnering with federal and state agencies, law enforcement personnel, policymakers, and other stakeholders to work on viable strategies to simultaneously advance patient health and prevent prescription drug abuse," NACDS President and CEO Steven C. Anderson, said in a statement regarding the bill.
Rep. Marsha Blackburn (R-Tenn.), a cosponsor of the bill, said in a statement that simply acknowledging the epidemic of prescription drug abuse isn’t enough. "Congress has a responsibility to make sure the law is crystal clear for both the DEA and legitimate businesses who want to understand what the rules are so they can do the right thing."
In House testimony last April, DEA Deputy Assistant Administrator Joseph Rannazzisi said the agency’s job is getting tougher. The number of registrants that the DEA regulates has mushroomed from 480,000 in 1973 to 1.5 million today, he said. At the same time, diversion and abuse have risen steeply, with opioids selling on the black market for 5-10 times their retail value.
In the last 3 years, the DEA’s Tactical Diversion Squads have increased from 37 to 66, and the agency has been applying its stiffest penalty – an immediate suspension order – in a judicious manner, according to Mr. Rannazzisi. From October 2013 through March 2014, 20 suspensions were ordered.
On Twitter @aliciaault
A new bill aims to clarify the rules of the Controlled Substances Act to ensure that legitimate operators stay in business and patients get needed medication, according to congressional backers of the bill, which was approved by the House of Representatives on July 29.
The bill still has to be taken up by the Senate, where there is no companion legislation.
The Ensuring Patient Access and Effective Drug Enforcement Act of 2014 (H.R. 4709) would ensure that restrictions on distribution of controlled substances are not so onerous as to inhibit access for patients, would require the U.S. Attorney General to give DEA registrant pharmacies and physicians who violate the rules an opportunity to submit a corrective action plan that might defer suspension of their registration, and would establish a working group to make recommendations to Congress on federal policies to reduce prescription drug diversion and abuse.
These measures are among the major policy goals of the Alliance to Prevent the Abuse of Medicines. The Washington, D.C.–based group includes among its members the American Medical Association, Cardinal Health, CVS Caremark, the Health Industry Distributors Association, and Teva.
The National Association of Chain Drug Stores "and chain pharmacy are committed to partnering with federal and state agencies, law enforcement personnel, policymakers, and other stakeholders to work on viable strategies to simultaneously advance patient health and prevent prescription drug abuse," NACDS President and CEO Steven C. Anderson, said in a statement regarding the bill.
Rep. Marsha Blackburn (R-Tenn.), a cosponsor of the bill, said in a statement that simply acknowledging the epidemic of prescription drug abuse isn’t enough. "Congress has a responsibility to make sure the law is crystal clear for both the DEA and legitimate businesses who want to understand what the rules are so they can do the right thing."
In House testimony last April, DEA Deputy Assistant Administrator Joseph Rannazzisi said the agency’s job is getting tougher. The number of registrants that the DEA regulates has mushroomed from 480,000 in 1973 to 1.5 million today, he said. At the same time, diversion and abuse have risen steeply, with opioids selling on the black market for 5-10 times their retail value.
In the last 3 years, the DEA’s Tactical Diversion Squads have increased from 37 to 66, and the agency has been applying its stiffest penalty – an immediate suspension order – in a judicious manner, according to Mr. Rannazzisi. From October 2013 through March 2014, 20 suspensions were ordered.
On Twitter @aliciaault
A new bill aims to clarify the rules of the Controlled Substances Act to ensure that legitimate operators stay in business and patients get needed medication, according to congressional backers of the bill, which was approved by the House of Representatives on July 29.
The bill still has to be taken up by the Senate, where there is no companion legislation.
The Ensuring Patient Access and Effective Drug Enforcement Act of 2014 (H.R. 4709) would ensure that restrictions on distribution of controlled substances are not so onerous as to inhibit access for patients, would require the U.S. Attorney General to give DEA registrant pharmacies and physicians who violate the rules an opportunity to submit a corrective action plan that might defer suspension of their registration, and would establish a working group to make recommendations to Congress on federal policies to reduce prescription drug diversion and abuse.
These measures are among the major policy goals of the Alliance to Prevent the Abuse of Medicines. The Washington, D.C.–based group includes among its members the American Medical Association, Cardinal Health, CVS Caremark, the Health Industry Distributors Association, and Teva.
The National Association of Chain Drug Stores "and chain pharmacy are committed to partnering with federal and state agencies, law enforcement personnel, policymakers, and other stakeholders to work on viable strategies to simultaneously advance patient health and prevent prescription drug abuse," NACDS President and CEO Steven C. Anderson, said in a statement regarding the bill.
Rep. Marsha Blackburn (R-Tenn.), a cosponsor of the bill, said in a statement that simply acknowledging the epidemic of prescription drug abuse isn’t enough. "Congress has a responsibility to make sure the law is crystal clear for both the DEA and legitimate businesses who want to understand what the rules are so they can do the right thing."
In House testimony last April, DEA Deputy Assistant Administrator Joseph Rannazzisi said the agency’s job is getting tougher. The number of registrants that the DEA regulates has mushroomed from 480,000 in 1973 to 1.5 million today, he said. At the same time, diversion and abuse have risen steeply, with opioids selling on the black market for 5-10 times their retail value.
In the last 3 years, the DEA’s Tactical Diversion Squads have increased from 37 to 66, and the agency has been applying its stiffest penalty – an immediate suspension order – in a judicious manner, according to Mr. Rannazzisi. From October 2013 through March 2014, 20 suspensions were ordered.
On Twitter @aliciaault
Hearing Impaired Have Fewer Barriers to Healthcare Careers
Since 2008, the American Community Survey, conducted by the U.S. Census Bureau, has queried respondents regarding deafness or hearing difficulties. According to these data, about 3.5% of the U.S. population has serious difficulty hearing. Other estimates vary, putting the number higher, especially those that include the numbers of elderly who experience hearing difficulties.
People who are deaf and hard of hearing (DHoH) work in diverse areas of the healthcare field, according to Samuel Atcherson, PhD, associate professor of audiology at the University of Arkansas in Little Rock and registry co-chair for the Association of Medical Professionals with Hearing Losses (www.amphl.org). AMPHL does not have statistics to report on the numbers of DHoH individuals practicing in medical occupations, but Dr. Atcherson noted that, as of 2011, there were 55 physicians, 41 nurses, and eight physician assistants in the membership.
Dr. Moreland and co-authors recently published a national survey that queried deaf physicians and trainees on a variety of subjects (e.g. career satisfaction, satisfaction with education, workplace accommodations). Due to the Rehabilitation Act of 1973 and the Americans with Disabilities Act of 1990, more people with hearing impairments are entering healthcare professions. Technological advances, such as electronic stethoscopes, also contribute to this surge.
The authors found that DHoH physicians and trainees responding to their survey were satisfied with multimodal employment and educational accommodations. Based on these results, they surmise, there might be an opportunity to recruit these individuals and further reach the underserved DHoH patient population.
—Gretchen Henkel
Since 2008, the American Community Survey, conducted by the U.S. Census Bureau, has queried respondents regarding deafness or hearing difficulties. According to these data, about 3.5% of the U.S. population has serious difficulty hearing. Other estimates vary, putting the number higher, especially those that include the numbers of elderly who experience hearing difficulties.
People who are deaf and hard of hearing (DHoH) work in diverse areas of the healthcare field, according to Samuel Atcherson, PhD, associate professor of audiology at the University of Arkansas in Little Rock and registry co-chair for the Association of Medical Professionals with Hearing Losses (www.amphl.org). AMPHL does not have statistics to report on the numbers of DHoH individuals practicing in medical occupations, but Dr. Atcherson noted that, as of 2011, there were 55 physicians, 41 nurses, and eight physician assistants in the membership.
Dr. Moreland and co-authors recently published a national survey that queried deaf physicians and trainees on a variety of subjects (e.g. career satisfaction, satisfaction with education, workplace accommodations). Due to the Rehabilitation Act of 1973 and the Americans with Disabilities Act of 1990, more people with hearing impairments are entering healthcare professions. Technological advances, such as electronic stethoscopes, also contribute to this surge.
The authors found that DHoH physicians and trainees responding to their survey were satisfied with multimodal employment and educational accommodations. Based on these results, they surmise, there might be an opportunity to recruit these individuals and further reach the underserved DHoH patient population.
—Gretchen Henkel
Since 2008, the American Community Survey, conducted by the U.S. Census Bureau, has queried respondents regarding deafness or hearing difficulties. According to these data, about 3.5% of the U.S. population has serious difficulty hearing. Other estimates vary, putting the number higher, especially those that include the numbers of elderly who experience hearing difficulties.
People who are deaf and hard of hearing (DHoH) work in diverse areas of the healthcare field, according to Samuel Atcherson, PhD, associate professor of audiology at the University of Arkansas in Little Rock and registry co-chair for the Association of Medical Professionals with Hearing Losses (www.amphl.org). AMPHL does not have statistics to report on the numbers of DHoH individuals practicing in medical occupations, but Dr. Atcherson noted that, as of 2011, there were 55 physicians, 41 nurses, and eight physician assistants in the membership.
Dr. Moreland and co-authors recently published a national survey that queried deaf physicians and trainees on a variety of subjects (e.g. career satisfaction, satisfaction with education, workplace accommodations). Due to the Rehabilitation Act of 1973 and the Americans with Disabilities Act of 1990, more people with hearing impairments are entering healthcare professions. Technological advances, such as electronic stethoscopes, also contribute to this surge.
The authors found that DHoH physicians and trainees responding to their survey were satisfied with multimodal employment and educational accommodations. Based on these results, they surmise, there might be an opportunity to recruit these individuals and further reach the underserved DHoH patient population.
—Gretchen Henkel
Physician Burnout Reduced with Intervention Groups
Clinical question: Does an intervention involving a facilitated physician small group result in improvement in well-being and reduction in burnout?
Background: Burnout affects nearly half of medical students, residents, and practicing physicians in the U.S.; however, very few interventions have been tested to address this problem.
Study design: Randomized controlled trial (RCT).
Setting: Department of Medicine at the Mayo Clinic, Rochester, Minn.
Synopsis: Practicing physicians were randomly assigned to facilitated, small-group intervention curriculum for one hour every two weeks (N=37) or control with unstructured, protected time for one hour every two weeks (N=37). A non-trial cohort of 350 practicing physicians was surveyed annually. This study showed a significant increase in empowerment and engagement at three months that was sustained for 12 months, and a significant decrease in high depersonalization scores was seen at both three and 12 months in the intervention group. There were no significant differences in stress, depression, quality of life, or job satisfaction.
Compared to the non-trial cohort, depersonalization, emotional exhaustion, and overall burnout decreased substantially in the intervention arm and slightly in the control arm.
Sample size was small and results may not be generalizable. Topics covered included reflection, self-awareness, and mindfulness, with a combination of community building and skill acquisition to promote connectedness and meaning in work. It is not clear which elements of the curriculum were most effective.
Bottom line: A facilitated, small-group intervention with institution-provided protected time can improve physician empowerment and engagement and reduce depersonalization, an important component of burnout.
Citation: West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Clinical question: Does an intervention involving a facilitated physician small group result in improvement in well-being and reduction in burnout?
Background: Burnout affects nearly half of medical students, residents, and practicing physicians in the U.S.; however, very few interventions have been tested to address this problem.
Study design: Randomized controlled trial (RCT).
Setting: Department of Medicine at the Mayo Clinic, Rochester, Minn.
Synopsis: Practicing physicians were randomly assigned to facilitated, small-group intervention curriculum for one hour every two weeks (N=37) or control with unstructured, protected time for one hour every two weeks (N=37). A non-trial cohort of 350 practicing physicians was surveyed annually. This study showed a significant increase in empowerment and engagement at three months that was sustained for 12 months, and a significant decrease in high depersonalization scores was seen at both three and 12 months in the intervention group. There were no significant differences in stress, depression, quality of life, or job satisfaction.
Compared to the non-trial cohort, depersonalization, emotional exhaustion, and overall burnout decreased substantially in the intervention arm and slightly in the control arm.
Sample size was small and results may not be generalizable. Topics covered included reflection, self-awareness, and mindfulness, with a combination of community building and skill acquisition to promote connectedness and meaning in work. It is not clear which elements of the curriculum were most effective.
Bottom line: A facilitated, small-group intervention with institution-provided protected time can improve physician empowerment and engagement and reduce depersonalization, an important component of burnout.
Citation: West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Clinical question: Does an intervention involving a facilitated physician small group result in improvement in well-being and reduction in burnout?
Background: Burnout affects nearly half of medical students, residents, and practicing physicians in the U.S.; however, very few interventions have been tested to address this problem.
Study design: Randomized controlled trial (RCT).
Setting: Department of Medicine at the Mayo Clinic, Rochester, Minn.
Synopsis: Practicing physicians were randomly assigned to facilitated, small-group intervention curriculum for one hour every two weeks (N=37) or control with unstructured, protected time for one hour every two weeks (N=37). A non-trial cohort of 350 practicing physicians was surveyed annually. This study showed a significant increase in empowerment and engagement at three months that was sustained for 12 months, and a significant decrease in high depersonalization scores was seen at both three and 12 months in the intervention group. There were no significant differences in stress, depression, quality of life, or job satisfaction.
Compared to the non-trial cohort, depersonalization, emotional exhaustion, and overall burnout decreased substantially in the intervention arm and slightly in the control arm.
Sample size was small and results may not be generalizable. Topics covered included reflection, self-awareness, and mindfulness, with a combination of community building and skill acquisition to promote connectedness and meaning in work. It is not clear which elements of the curriculum were most effective.
Bottom line: A facilitated, small-group intervention with institution-provided protected time can improve physician empowerment and engagement and reduce depersonalization, an important component of burnout.
Citation: West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Hospital Medicine Upcoming Events, Meetings, Symposiums
Safety and Brazilian Hospital
Medicine 2014
August 6-8
Rio de Janeiro, Brazil
SHM’s Glycemic Control Program Informational Webinar
August 14, 2 p.m.
https://www4.gotomeeting.com/register/907579183
Palliative Medicine and Supportive Oncology 2014, The 17th International Symposium
September 18-20
Green Valley Ranch, Las Vegas
Society of OB/GYN Hospitalists Annual Clinical Meeting OB/GYN Hospitalists: Recognition, Response, Results
September 18-20
Embassy Suites Downtown, Denver
www.societyofobgynhospitalists.com
Academic Hospitalist Academy
October 20-23
Inverness Hotel and Conference
Center, Englewood, Colo.
Adult Hospital Medicine Boot Camp
October 1-5
The Westin Peachtree Plaza, Atlanta, Ga.
SHM Leadership Academy
November 3-6
Hilton Hawaiian Village Waikiki Beach Resort, Honolulu
www.hospitalmedicine.org/leadership
Hospital Medicine 2015
March 29-April 1, 2015
Gaylord National Resort & Convention Center, National Harbor, Md.
Safety and Brazilian Hospital
Medicine 2014
August 6-8
Rio de Janeiro, Brazil
SHM’s Glycemic Control Program Informational Webinar
August 14, 2 p.m.
https://www4.gotomeeting.com/register/907579183
Palliative Medicine and Supportive Oncology 2014, The 17th International Symposium
September 18-20
Green Valley Ranch, Las Vegas
Society of OB/GYN Hospitalists Annual Clinical Meeting OB/GYN Hospitalists: Recognition, Response, Results
September 18-20
Embassy Suites Downtown, Denver
www.societyofobgynhospitalists.com
Academic Hospitalist Academy
October 20-23
Inverness Hotel and Conference
Center, Englewood, Colo.
Adult Hospital Medicine Boot Camp
October 1-5
The Westin Peachtree Plaza, Atlanta, Ga.
SHM Leadership Academy
November 3-6
Hilton Hawaiian Village Waikiki Beach Resort, Honolulu
www.hospitalmedicine.org/leadership
Hospital Medicine 2015
March 29-April 1, 2015
Gaylord National Resort & Convention Center, National Harbor, Md.
Safety and Brazilian Hospital
Medicine 2014
August 6-8
Rio de Janeiro, Brazil
SHM’s Glycemic Control Program Informational Webinar
August 14, 2 p.m.
https://www4.gotomeeting.com/register/907579183
Palliative Medicine and Supportive Oncology 2014, The 17th International Symposium
September 18-20
Green Valley Ranch, Las Vegas
Society of OB/GYN Hospitalists Annual Clinical Meeting OB/GYN Hospitalists: Recognition, Response, Results
September 18-20
Embassy Suites Downtown, Denver
www.societyofobgynhospitalists.com
Academic Hospitalist Academy
October 20-23
Inverness Hotel and Conference
Center, Englewood, Colo.
Adult Hospital Medicine Boot Camp
October 1-5
The Westin Peachtree Plaza, Atlanta, Ga.
SHM Leadership Academy
November 3-6
Hilton Hawaiian Village Waikiki Beach Resort, Honolulu
www.hospitalmedicine.org/leadership
Hospital Medicine 2015
March 29-April 1, 2015
Gaylord National Resort & Convention Center, National Harbor, Md.
Common Coding Mistakes Hospitalists Should Avoid
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
CODE-H Medical Coding Education Program Becomes Interactive
SHM’s coding education program, CODE-H, now has an interactive component through the SHM Learning Portal. CODE-H originally was developed as a series of live and on-demand webinars complemented by online forums; today, CODE-H Interactive brings the same expertise to an interactive platform ideal for new hospitalists learning the nuances of coding, hospital medicine groups assessing the coding skills of their caregivers, or even coders using it as a training tool for conducting audits of hospital medicine groups.
To learn more about CODE-H and CODE-H Interactive, visit www.hospitalmedicine.org/codeh.
SHM’s coding education program, CODE-H, now has an interactive component through the SHM Learning Portal. CODE-H originally was developed as a series of live and on-demand webinars complemented by online forums; today, CODE-H Interactive brings the same expertise to an interactive platform ideal for new hospitalists learning the nuances of coding, hospital medicine groups assessing the coding skills of their caregivers, or even coders using it as a training tool for conducting audits of hospital medicine groups.
To learn more about CODE-H and CODE-H Interactive, visit www.hospitalmedicine.org/codeh.
SHM’s coding education program, CODE-H, now has an interactive component through the SHM Learning Portal. CODE-H originally was developed as a series of live and on-demand webinars complemented by online forums; today, CODE-H Interactive brings the same expertise to an interactive platform ideal for new hospitalists learning the nuances of coding, hospital medicine groups assessing the coding skills of their caregivers, or even coders using it as a training tool for conducting audits of hospital medicine groups.
To learn more about CODE-H and CODE-H Interactive, visit www.hospitalmedicine.org/codeh.
TeamHealth Hospital Medicine Shares Performance Stats
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
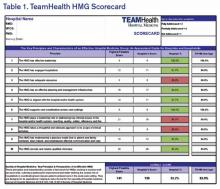
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.
Medical Decision-Making: Avoid These Common Coding & Documentation Mistakes
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Medical decision-making (MDM) mistakes are common. Here are the coding and documentation mistakes hospitalists make most often, along with some tips on how to avoid them.
Listing the problem without a plan. Healthcare professionals are able to infer the acuity and severity of a case without superfluous or redundant documentation, but auditors may not have this ability. Adequate documentation for every service date helps to convey patient complexity during a medical record review. Although the problem list may not change dramatically from day to day during a hospitalization, the auditor only reviews the service date in question, not the entire medical record.
Hospitalists should be sure to formulate a complete and accurate description of the patient’s condition with an analogous plan of care for each encounter. Listing problems without a corresponding plan of care does not corroborate physician management of that problem and could cause a downgrade of complexity. Listing problems with a brief, generalized comment (e.g. “DM, CKD, CHF: Continue current treatment plan”) equally diminishes the complexity and effort put forth by the physician.
Clearly document the plan. The care plan represents problems the physician personally manages, along with those that must also be considered when he or she formulates the management options, even if another physician is primarily managing the problem. For example, the hospitalist can monitor the patient’s diabetic management while the nephrologist oversees the chronic kidney disease (CKD). Since the CKD impacts the hospitalist’s diabetic care plan, the hospitalist may also receive credit for any CKD consideration if the documentation supports a hospitalist-related care plan, or comment about CKD that does not overlap or replicate the nephrologist’s plan. In other words, there must be some “value-added” input by the hospitalist.
Credit is given for the quantity of problems addressed as well as the quality. For inpatient care, an established problem is defined as one in which a care plan has been generated by the physician (or same specialty group practice member) during the current hospitalization. Established problems are less complex than new problems, for which a diagnosis, prognosis, or care plan has not been developed. Severity of the problem also influences complexity. A “worsening” problem is considered more complex than an “improving” problem, since the worsening problem likely requires revisions to the current care plan and, thus, more physician effort. Physician documentation should always:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- Note management options to be continued somewhere in the progress note for that encounter (e.g. medication list) when documentation indicates a continuation of current management options (e.g. “continue meds”).
Considering relevant data. “Data” is organized as pathology/laboratory testing, radiology, and medicine-based diagnostic testing that contributes to diagnosing or managing patient problems. Pertinent orders or results may appear in the medical record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note, or make an entry that refers to another auditor-accessible location for ordered tests and studies; however, this latter option jeopardizes a medical record review due to potential lack of awareness of the need to submit this extraneous information during a payer record request or appeal.
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”); credit is not given for entries lacking a comment on the findings (e.g. “CXR reviewed”).
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary; be sure to identify the increased efforts of reviewing the considerable number of old records by stating, “OSH (outside hospital) records reviewed and shows…” or “Records from previous hospitalization(s) reveal….”
- Indicate when images, tracings, or specimens are “personally reviewed,” or the auditor will assume the physician merely reviewed the written report; be sure to include a comment on the findings.
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Data credit may be more substantial during the initial investigative phase of the hospitalization, before diagnoses or treatment options have been confirmed. Routine monitoring of the stabilized patient may not yield as many “points.”
Undervaluing the patient’s complexity. A general lack of understanding of the MDM component of the documentation guidelines often results in physicians undervaluing their services. Some physicians may consider a case “low complexity” simply because of the frequency with which they encounter the case type. The speed with which the care plan is developed should have no bearing on how complex the patient’s condition really is. Hospitalists need to better identify the risk involved for the patient.
Patient risk is categorized as minimal, low, moderate, or high based on pre-assigned items pertaining to the presenting problem, diagnostic procedures ordered, and management options selected. The single highest-rated item detected on the Table of Risk determines the overall patient risk for an encounter.1 Chronic conditions with exacerbations and invasive procedures offer more patient risk than acute, uncomplicated illnesses or noninvasive procedures. Stable or improving problems are considered “less risky” than progressing problems; conditions that pose a threat to life/bodily function outweigh undiagnosed problems where it is difficult to determine the patient’s prognosis; and medication risk varies with the administration (e.g. oral vs. parenteral), type, and potential for adverse effects. Medication risk for a particular drug is invariable whether the dosage is increased, decreased, or continued without change. Physicians should:
- Provide status for all problems in the plan of care and identify them as stable, worsening, or progressing (mild or severe), when applicable; don’t assume that the auditor can infer this from the documentation details.
- Document all diagnostic or therapeutic procedures considered.
- Identify surgical risk factors involving co-morbid conditions that place the patient at greater risk than the average patient, when appropriate.
- Associate the labs ordered to monitor for medication toxicity with the corresponding medication; don’t assume that the auditor knows which labs are used to check for toxicity.
Varying levels of complexity. Remember that decision-making is just one of three components in evaluation and management (E&M) services, along with history and exam. MDM is identical for both the 1995 and 1997 guidelines, rooted in the complexity of the patient’s problem(s) addressed during a given encounter.1,2 Complexity is categorized as straightforward, low, moderate, or high, and directly correlates to the content of physician documentation.
Each visit level represents a particular level of complexity (see Table 1). Auditors only consider the care plan for a given service date when reviewing MDM. More specifically, the auditor reviews three areas of MDM for each encounter (see Table 2), and the physician receives credit for: a) the number of diagnoses and/or treatment options; b) the amount and/or complexity of data ordered/reviewed; c) the risk of complications/morbidity/mortality.
To determine MDM complexity, each MDM category is assigned a point level. Complexity correlates to the second-highest MDM category. For example, if the auditor assigns “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician attains moderate complexity decision-making (see Table 3).
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation and Management Services. Available at: www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/95Docguidelines.pdf. Accessed July 7, 2014.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation and Management Services. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf. Accessed July 7, 2014.
- American Medical Association. Current Procedural Terminology: 2014 Professional Edition. Chicago: American Medical Association; 2013:14-21.
- Novitas Solutions. Novitas Solutions documentation worksheet. Available at: www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00004966. Accessed July 7, 2014.
Deaf Hospitalist Focuses on Teaching, Co-Management, Patient-Centered Care
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
"What’s the bigger picture here?” Hospitalist Christopher Moreland, MD, MPH, FACP, drops his question neatly into the pause in resident Adrienne Victor, MD’s presentation of patient status and lab results.
We’re on the bustling 9th floor of University Hospital at the University of Texas Health Science Center (UTHSCSA) in San Antonio during fast-paced morning rounds. As attending physician, Dr. Moreland is focusing intently on Dr. Victor’s face, simultaneously monitoring the American Sign Language (ASL) interpretation of Todd Agan, CI/CT, BEI Master Interpreter. Immediately after his question to Dr. Victor, the discussion—conducted in both ASL and spoken English—shifts to the patient’s psychosocial issues and whether a palliative care consult would be advisable.
It’s clear that for Dr. Moreland, the work, not his lack of hearing, is the main point here. A hospitalist with the UTHSCSA team since 2010, Dr. Moreland quickly established himself not only as a valuable HM team member and educator, but also as a leader in other domains. For example, in addition to his academic appointment as assistant clinical professor of medicine, he previously was co-director of the medicine consult and co-management service at University Hospital and now serves as UTHSCSA’s associate program director for the internal medicine residency program.
Dr. Moreland’s question this morning is typical of his teaching, says Bret Simon, PhD, an educational development specialist and assistant professor with the division of hospital medicine at UTHSCSA.

–Christopher Moreland, MD, MPH, FACP
“He’s very good at using questions to teach, promoting reflection rather than simply telling the student what to do,” Dr. Simon explains.
Why Medicine?
Chris Moreland’s parents discovered their son was deaf at age two, by which time he had acquired very few spoken words. After multiple visits to healthcare professionals, a physician finally identified his deafness. The family then embarked on a bimodal approach to his education, using both signed and spoken English. He learned ASL in college. As a result, he communicates through a variety of channels: ASL with interpreters Agan and Keri Richardson, speech reading, and spoken English. When examining patients, he uses an electronic stethoscope that interfaces with his cochlear implant.
Medicine was not Dr. Moreland’s first academic choice.
“I went into college thinking I wanted to do computer science,” he says, speaking of his undergraduate studies at the University of Texas in Austin. When he realized computers were not for him, he switched his major to theater arts, continuing an interest he had had in high school. After that, research seemed appealing, and he became a research assistant in a lab in the Department of Anthropology. Finally, after shadowing a number of physicians, his interest in medical science was stimulated.
“Medicine,” he says, “became a nice culmination of everything I was interested in doing.” From computer science, he learned to appreciate an understanding of algorithms; from theater arts came the ability to understand where people are coming from; and from his link with research in linguistics and anthropology came the contribution of problem solving and methodology.
Fearless Communicator
Dr. Moreland says his deafness presents no impediments to his practice of medicine. “I grew up working with interpreters, so I’m used to that process,” he says. “It forces you to become less inhibited about what you’re doing. People have questions [‘who is that other person in the room?’], and you learn how to handle those questions quickly, without interfering with communication in order to advance the work.”
When Dr. Moreland started his clinical rotations as a third-year medical student, he grappled with the best way to introduce himself and his interpreter to patients. His first attempt at explaining the interpretive process “went on for quite a while” and was too much information. “It ended up overwhelming the patient,” he says.
The next time he chose not to introduce the interpreter but to simply address the patient directly. “That didn’t work either, because the patient’s eyes kept wandering to that other person in the room.”
Finally, “I realized that it wasn’t about me,” he says. “It was about the patient.” So he simply shortened the introduction to himself and the interpreter and asked the patients how they were doing.
“Once I became more professional about the situation, the more positive and patient-centered it became, and it went well.” He says he’s had no negative experiences since then, at least not related to his deafness. He approaches each new patient interaction proactively, and he and his interpreters become part of the flow of care.
Teaching’s Missing Pieces
As illustrated with his first question, Dr. Moreland intends for his trainees to learn to think globally about their patients.
“Although rote information has its role,” he explains later in the conference room, “I’m always afraid of overemphasizing it. When I trained in medical school, we didn’t learn that much about communication skills and teamwork. We talked a lot about information we use as physicians—the mechanism of disease, the drugs we use.
“What I try to emphasize with trainees is, what skills in communication, teamwork, and self-education can we develop so that we can use those skills continuously throughout our practice?”
Dr. Moreland takes setting resident-generated learning goals seriously, says Dr. Simon, for which he and trainees give him high marks.
“He is very supportive and encourages us to make our own management decisions,” Dr. Victor says. “Though, of course, he will let us know if something is likely the wrong choice, usually by discussing it first.”
Patrick S. Romano, MD, MPH, professor of general medicine and pediatrics and former director of the Primary Care Outcomes Research (PCOR) faculty development program at the University of California Davis, where Dr. Moreland was a resident and then a fellow, found his trainee was always “very thoughtful and conscientious, presenting different ways of looking at problems and asking the right questions. And, of course, that’s what we look for in teachers: people who know how to ask the right questions, because, then, of course, they are able to answer students’ questions.”
Transformational and Inspirational
For many of Dr. Moreland’s colleagues and trainees, working with him has been their first exposure to a hearing-impaired physician. Richard L. Kravitz, MD, MSPH, professor and co-vice chair of research in the department of medicine at UC Davis, supervised Dr. Moreland during his residency and later during his PCOR fellowship. The American Disabilities Act-mandated interpreter for Dr. Moreland introduced a “change in standard operating procedure,” Dr. Kravitz notes. “None of us knew what to expect when he came onboard the residency program. But, very quickly, any unease was put to rest because he was just so talented.”
For visitors, Dr. Moreland seamlessly addresses his hearing impairment and makes sure that everyone on the team is following the discussion. Luci K. Leykum, MD, MBA, MSc, hospital medicine division chief and associate dean for clinical affairs at UTHSCSA, says that Dr. Moreland has brought “a lot of positive energy to the group—and in ways I would not have expected.” She praised his talents as both a clinician and teacher.
John G. Rees, DBA, RN, patient care coordinator in the 5th Acute Care Unit, says that Dr. Moreland immediately “blended” with the staff on his service. “The rapport was perfect,” he adds.
Robert L. Talbert, PharmD, the SmithKline Centennial Professor of Pharmacy at the College of Pharmacy at the University of Texas at Austin, often participates in teaching rounds. Dr. Moreland, he says, “has an excellent fund of knowledge; he’s very rational and evidence-based in decisions he makes. He’s exactly what a physician should be.”
Watching interpreters Agan and Richardson during group meetings, Dr. Leykum believes, has influenced their group dynamics. “On a subtle level, having Chris in the group has made us more aware of how we interact with each other.”
Nilam Soni, MD, FHM associate professor in the department of medicine and leader of ultrasound education, has noticed that he has become attuned to Dr. Moreland’s way of communicating and often does not need the interpreters to decipher the conversation between them. Working with Dr. Moreland has given Dr. Soni “a better understanding of how to communicate effectively with patients that have difficulty hearing.”
After working with Dr. Moreland at UC Davis, Dr. Kravitz observed that employing physicians with hearing impairment or other disabilities brings additional benefits to the institution. Dr. Moreland’s presence “probably raised the level of understanding of the entire internal medicine staff, because it demonstrated that a disability is what you make of it,” he says. “One recognizes how porous the barriers are, provided that people with disabilities are supported appropriately. In that way, Chris was inspiring, and may have changed the way some of us look at this specific disability that he had, but also other disabilities.”
A bigger picture, indeed.
Gretchen Henkel is a freelance writer in California.
Reference
It’s official: Oct. 1, 2015, is the ICD-10 compliance date
Go ahead and mark your calendar: Medicare officials have issued a final regulation setting Oct. 1, 2015, as the official compliance date for switching to the ICD-10 coding system.
Earlier this year, Congress delayed the transition from the ICD-9 to ICD-10 coding systems for at least a year but did not specify the exact compliance date, leaving that to the discretion of officials at the Center for Medicare & Medicaid Services.
CMS first announced the Oct. 1, 2015 compliance date – the earliest start allowed under the law – in May. But the new date wasn’t official until the agency released an interim final rule, which it did July 31.
On Twitter @maryellenny
Go ahead and mark your calendar: Medicare officials have issued a final regulation setting Oct. 1, 2015, as the official compliance date for switching to the ICD-10 coding system.
Earlier this year, Congress delayed the transition from the ICD-9 to ICD-10 coding systems for at least a year but did not specify the exact compliance date, leaving that to the discretion of officials at the Center for Medicare & Medicaid Services.
CMS first announced the Oct. 1, 2015 compliance date – the earliest start allowed under the law – in May. But the new date wasn’t official until the agency released an interim final rule, which it did July 31.
On Twitter @maryellenny
Go ahead and mark your calendar: Medicare officials have issued a final regulation setting Oct. 1, 2015, as the official compliance date for switching to the ICD-10 coding system.
Earlier this year, Congress delayed the transition from the ICD-9 to ICD-10 coding systems for at least a year but did not specify the exact compliance date, leaving that to the discretion of officials at the Center for Medicare & Medicaid Services.
CMS first announced the Oct. 1, 2015 compliance date – the earliest start allowed under the law – in May. But the new date wasn’t official until the agency released an interim final rule, which it did July 31.
On Twitter @maryellenny