User login
Prescribe This Combined OC With CV Safety in Mind
A 28-year-old woman presents to your office for a routine health maintenance exam. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a pa
In general, when compared with nonusers, women who use COCs have a two- to four-fold increase in risk for venous thromboembolism (VTE) and an increased risk for myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk for VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk for VTE than other preparations, despite similar estrogen content.7 The FDA produced a similar statement that same year, recommending that providers carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks for ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One COC comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks for pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included nearly 5 million women ages 15 to 49, living in France, who had at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks for first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 µg) or high-dose estrogen (30-40 µg) combined with one of five progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI, with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 for PE, 0.82 for ischemic stroke, and 0.56 for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7,143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs for PE but not arterial events (2.16 for desogestrel and 1.63 for gestodene). For PE, the ARR with levonorgestrel compared to desogestrel and gestodene, respectively, was 19/100,000 and 12/100,000 person-years of use (NNH, 5,263 and 8,333, respectively). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk for PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks for PE and arterial thromboembolism.

WHAT’S NEW?
Low-dose estrogen + levonorgestrel confer lowest risk
Prior studies have shown that COCs increase the risk for PE and may also increase the risks for ischemic stroke and MI.3,11 Studies have also suggested that a higher dose of estrogen in COCs is associated with an increased risk for VTE.11,12 This study shows that 20 µg of estrogen combined with levonorgestrel is associated with the lowest risks for PE, MI, and ischemic stroke.
CAVEATS
Cohort study, no start date, incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk for VTE is highest in the first three months to one year of COC use.12 Data on tobacco use, a significant independent risk factor for arterial but not venous thromboembolism, was incomplete; however, in other studies, it has only marginally affected outcomes.3,13
CHALLENGES TO IMPLEMENTATION
Increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 µg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[7]:454-456).
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. FDA. Combined hormonal contraceptives (CHCs) and the risk of cardiovascular disease endpoints. www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed July 5, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP monthly report on safety concerns, guidelines and general matters. 2012. www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed July 5, 2017.
8. FDA. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed July 5, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
A 28-year-old woman presents to your office for a routine health maintenance exam. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a pa
In general, when compared with nonusers, women who use COCs have a two- to four-fold increase in risk for venous thromboembolism (VTE) and an increased risk for myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk for VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk for VTE than other preparations, despite similar estrogen content.7 The FDA produced a similar statement that same year, recommending that providers carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks for ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One COC comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks for pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included nearly 5 million women ages 15 to 49, living in France, who had at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks for first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 µg) or high-dose estrogen (30-40 µg) combined with one of five progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI, with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 for PE, 0.82 for ischemic stroke, and 0.56 for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7,143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs for PE but not arterial events (2.16 for desogestrel and 1.63 for gestodene). For PE, the ARR with levonorgestrel compared to desogestrel and gestodene, respectively, was 19/100,000 and 12/100,000 person-years of use (NNH, 5,263 and 8,333, respectively). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk for PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks for PE and arterial thromboembolism.

WHAT’S NEW?
Low-dose estrogen + levonorgestrel confer lowest risk
Prior studies have shown that COCs increase the risk for PE and may also increase the risks for ischemic stroke and MI.3,11 Studies have also suggested that a higher dose of estrogen in COCs is associated with an increased risk for VTE.11,12 This study shows that 20 µg of estrogen combined with levonorgestrel is associated with the lowest risks for PE, MI, and ischemic stroke.
CAVEATS
Cohort study, no start date, incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk for VTE is highest in the first three months to one year of COC use.12 Data on tobacco use, a significant independent risk factor for arterial but not venous thromboembolism, was incomplete; however, in other studies, it has only marginally affected outcomes.3,13
CHALLENGES TO IMPLEMENTATION
Increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 µg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[7]:454-456).
A 28-year-old woman presents to your office for a routine health maintenance exam. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a pa
In general, when compared with nonusers, women who use COCs have a two- to four-fold increase in risk for venous thromboembolism (VTE) and an increased risk for myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk for VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk for VTE than other preparations, despite similar estrogen content.7 The FDA produced a similar statement that same year, recommending that providers carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks for ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One COC comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks for pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included nearly 5 million women ages 15 to 49, living in France, who had at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks for first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 µg) or high-dose estrogen (30-40 µg) combined with one of five progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI, with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 for PE, 0.82 for ischemic stroke, and 0.56 for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7,143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs for PE but not arterial events (2.16 for desogestrel and 1.63 for gestodene). For PE, the ARR with levonorgestrel compared to desogestrel and gestodene, respectively, was 19/100,000 and 12/100,000 person-years of use (NNH, 5,263 and 8,333, respectively). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk for PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks for PE and arterial thromboembolism.

WHAT’S NEW?
Low-dose estrogen + levonorgestrel confer lowest risk
Prior studies have shown that COCs increase the risk for PE and may also increase the risks for ischemic stroke and MI.3,11 Studies have also suggested that a higher dose of estrogen in COCs is associated with an increased risk for VTE.11,12 This study shows that 20 µg of estrogen combined with levonorgestrel is associated with the lowest risks for PE, MI, and ischemic stroke.
CAVEATS
Cohort study, no start date, incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk for VTE is highest in the first three months to one year of COC use.12 Data on tobacco use, a significant independent risk factor for arterial but not venous thromboembolism, was incomplete; however, in other studies, it has only marginally affected outcomes.3,13
CHALLENGES TO IMPLEMENTATION
Increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 µg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[7]:454-456).
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. FDA. Combined hormonal contraceptives (CHCs) and the risk of cardiovascular disease endpoints. www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed July 5, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP monthly report on safety concerns, guidelines and general matters. 2012. www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed July 5, 2017.
8. FDA. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed July 5, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. FDA. Combined hormonal contraceptives (CHCs) and the risk of cardiovascular disease endpoints. www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed July 5, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP monthly report on safety concerns, guidelines and general matters. 2012. www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed July 5, 2017.
8. FDA. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed July 5, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
Direct oral anticoagulants or warfarin for A fib?
ILLUSTRATIVE CASE
A 66-year-old man with a history of hypertension and diabetes mellitus type 2 is hospitalized for palpitations and dizziness, and is given a diagnosis of atrial fibrillation (AF). His heart rate is successfully controlled with a beta-blocker. His CHA2DS2-VASc score is 3, meaning he is a candidate for anticoagulation. Which agent should you start?
Thromboembolism in patients with AF results in stroke and death and can be decreased with appropriate use of antithrombotic therapy. Evidence-based guidelines recommend patients with AF at intermediate or high risk of stroke (CHADS2 score ≥ 2 or prior history of cardioembolic stroke or transient ischemic attack) receive antithrombotic therapy with oral anticoagulation, rather than receive no therapy or therapy with antiplatelets.2,3
The American College of Chest Physicians also recommends the use of the direct oral anticoagulant (DOAC) dabigatran over warfarin for those patients with nonvalvular AF with an estimated glomerular filtration rate (eGFR) ≥15 mL/min/1.73 m2.3
A meta-analysis of large randomized controlled trials (RCTs) of individual DOACs (dabigatran [a direct thrombin inhibitor], rivaroxaban, apixaban, and edoxaban [factor Xa inhibitors]) revealed similar or lower rates of ischemic stroke and major bleeding (except gastrointestinal bleeds; relative risk=1.25; 95% CI, 1.01 to 1.55) when compared with warfarin (at an international normalized ratio [INR] goal of 2-3).4 In addition, 3 separate meta-analyses that pooled results from large RCTs involving dabigatran, apixaban, and rivaroxaban also concluded that these medications result in a significant reduction in embolic stroke and reduced the risk of major bleeds and hemorrhagic stroke when compared with warfarin.5-7
However, we know less about the comparative effectiveness and safety of the DOACs when they are used in clinical practice, and it is not clear which, if any of these agents, are superior to others. Moreover, only about half of the patients in the United States with AF who are eligible to take DOACs are currently managed with them.8
STUDY SUMMARY
One DOAC is better than warfarin at one thing; 2 others are better at another
This large cohort study examined the effectiveness of 3 DOACs compared with warfarin in 61,678 patients with AF by combining data from 3 Danish national databases. The patients had newly diagnosed AF (without valvular disease or venous thromboembolism) and were prescribed standard doses of DOACs (dabigatran 150 bid [N=12,701], rivaroxaban 20 mg/d [N=7192], apixaban 5 mg bid [N=6349]) or dose-adjusted warfarin to an INR goal of 2 to 3 (N=35,436). Patients were followed for an average of 1.9 years.
Ischemic stroke, systemic emboli. In the first year of observation, there were 1702 ischemic strokes or systemic emboli. The incidence of ischemic stroke or systemic embolism was either the same or better for each of the 3 DOAC treatments than for warfarin (DOACs, 2.9-3.9 events per 100 person-years; warfarin, 3.3 events per 100 person-years; no P value provided). Ischemic stroke or systemic emboli events occurred less frequently in the rivaroxaban group compared with warfarin at one year (hazard ratio [HR]=0.83; 95% confidence interval [CI], 0.69-0.99) and after 2.5 years (HR=0.80; 95% CI, 0.69-0.94). The rates of ischemic stroke and systemic emboli for both apixaban and dabigatran were not significantly different than that for warfarin at one year and 2.5 years.
Bleeding events (defined as intracranial, major gastrointestinal, and traumatic intracranial) were lower in the apixaban group (HR=0.63; 95% CI, 0.53-0.76) and dabigatran group (HR=0.61; 95% CI, 0.51-0.74) than in the warfarin group at one year. Significant reductions remained after 2.5 years. There was no difference in bleeding events between rivaroxaban and warfarin.
Risk of death. Compared with warfarin, the risk of death after one year of treatment was lower in the apixaban (HR=0.65; 95% CI, 0.56-0.75) and dabigatran (HR=0.63; 95% CI, 0.48-0.82) groups, and there was no significant difference in the rivaroxaban group (HR=0.92; 95% CI, 0.82-1.03).
WHAT’S NEW
No agent “has it all,” but DOACs have advantages
This comparative effectiveness and safety analysis reveals that all of the DOACs are at least as effective as warfarin in preventing ischemic stroke and systemic emboli, and that rivaroxaban may be more effective, and that apixaban and dabigatran have a lower risk of bleeding than warfarin.
CAVEATS
This non-randomized cohort trial lacked INR data
This study was a non-randomized cohort trial. And, while propensity weighting helps, the researchers were unable to completely control for underlying risk factors or unknown confounders.
INR data for patients on warfarin was not provided, so it is not clear how often patients were out of therapeutic range, which could affect the stroke and bleeding results in the warfarin group. This, however, is seen with routine use of warfarin. We feel that this study reflects the challenge of maintaining patients in warfarin’s narrow therapeutic range.
CHALLENGES TO IMPLEMENTATION
It comes down to cost
Cost could be a barrier, as health insurance coverage for DOACs varies. Patients with high-deductible health insurance plans, or who find themselves in the Medicare “donut hole,” may be at a particular disadvantage.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Larsen TB, Skjøth F, Nielsen PB, et al. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.
2. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. J Am Coll Cardiol. 2014;64:2246-2280.
3. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S-e575S.
4. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955-962.
5. Dentali F, Riva N, Crowther M, et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126:2381-2391.
6. Adam SS, McDuffie JR, Ortel TL, et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism. Ann Intern Med. 2012;157:796-807.
7. Ntaios G, Papavasileiou V, Diener H, et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298-3304.
8. Barnes GD, Lucas E, Alexander GC, et al. National trends in ambulatory oral anticoagulant use. Am J Med. 2015;128:1300-1305.
ILLUSTRATIVE CASE
A 66-year-old man with a history of hypertension and diabetes mellitus type 2 is hospitalized for palpitations and dizziness, and is given a diagnosis of atrial fibrillation (AF). His heart rate is successfully controlled with a beta-blocker. His CHA2DS2-VASc score is 3, meaning he is a candidate for anticoagulation. Which agent should you start?
Thromboembolism in patients with AF results in stroke and death and can be decreased with appropriate use of antithrombotic therapy. Evidence-based guidelines recommend patients with AF at intermediate or high risk of stroke (CHADS2 score ≥ 2 or prior history of cardioembolic stroke or transient ischemic attack) receive antithrombotic therapy with oral anticoagulation, rather than receive no therapy or therapy with antiplatelets.2,3
The American College of Chest Physicians also recommends the use of the direct oral anticoagulant (DOAC) dabigatran over warfarin for those patients with nonvalvular AF with an estimated glomerular filtration rate (eGFR) ≥15 mL/min/1.73 m2.3
A meta-analysis of large randomized controlled trials (RCTs) of individual DOACs (dabigatran [a direct thrombin inhibitor], rivaroxaban, apixaban, and edoxaban [factor Xa inhibitors]) revealed similar or lower rates of ischemic stroke and major bleeding (except gastrointestinal bleeds; relative risk=1.25; 95% CI, 1.01 to 1.55) when compared with warfarin (at an international normalized ratio [INR] goal of 2-3).4 In addition, 3 separate meta-analyses that pooled results from large RCTs involving dabigatran, apixaban, and rivaroxaban also concluded that these medications result in a significant reduction in embolic stroke and reduced the risk of major bleeds and hemorrhagic stroke when compared with warfarin.5-7
However, we know less about the comparative effectiveness and safety of the DOACs when they are used in clinical practice, and it is not clear which, if any of these agents, are superior to others. Moreover, only about half of the patients in the United States with AF who are eligible to take DOACs are currently managed with them.8
STUDY SUMMARY
One DOAC is better than warfarin at one thing; 2 others are better at another
This large cohort study examined the effectiveness of 3 DOACs compared with warfarin in 61,678 patients with AF by combining data from 3 Danish national databases. The patients had newly diagnosed AF (without valvular disease or venous thromboembolism) and were prescribed standard doses of DOACs (dabigatran 150 bid [N=12,701], rivaroxaban 20 mg/d [N=7192], apixaban 5 mg bid [N=6349]) or dose-adjusted warfarin to an INR goal of 2 to 3 (N=35,436). Patients were followed for an average of 1.9 years.
Ischemic stroke, systemic emboli. In the first year of observation, there were 1702 ischemic strokes or systemic emboli. The incidence of ischemic stroke or systemic embolism was either the same or better for each of the 3 DOAC treatments than for warfarin (DOACs, 2.9-3.9 events per 100 person-years; warfarin, 3.3 events per 100 person-years; no P value provided). Ischemic stroke or systemic emboli events occurred less frequently in the rivaroxaban group compared with warfarin at one year (hazard ratio [HR]=0.83; 95% confidence interval [CI], 0.69-0.99) and after 2.5 years (HR=0.80; 95% CI, 0.69-0.94). The rates of ischemic stroke and systemic emboli for both apixaban and dabigatran were not significantly different than that for warfarin at one year and 2.5 years.
Bleeding events (defined as intracranial, major gastrointestinal, and traumatic intracranial) were lower in the apixaban group (HR=0.63; 95% CI, 0.53-0.76) and dabigatran group (HR=0.61; 95% CI, 0.51-0.74) than in the warfarin group at one year. Significant reductions remained after 2.5 years. There was no difference in bleeding events between rivaroxaban and warfarin.
Risk of death. Compared with warfarin, the risk of death after one year of treatment was lower in the apixaban (HR=0.65; 95% CI, 0.56-0.75) and dabigatran (HR=0.63; 95% CI, 0.48-0.82) groups, and there was no significant difference in the rivaroxaban group (HR=0.92; 95% CI, 0.82-1.03).
WHAT’S NEW
No agent “has it all,” but DOACs have advantages
This comparative effectiveness and safety analysis reveals that all of the DOACs are at least as effective as warfarin in preventing ischemic stroke and systemic emboli, and that rivaroxaban may be more effective, and that apixaban and dabigatran have a lower risk of bleeding than warfarin.
CAVEATS
This non-randomized cohort trial lacked INR data
This study was a non-randomized cohort trial. And, while propensity weighting helps, the researchers were unable to completely control for underlying risk factors or unknown confounders.
INR data for patients on warfarin was not provided, so it is not clear how often patients were out of therapeutic range, which could affect the stroke and bleeding results in the warfarin group. This, however, is seen with routine use of warfarin. We feel that this study reflects the challenge of maintaining patients in warfarin’s narrow therapeutic range.
CHALLENGES TO IMPLEMENTATION
It comes down to cost
Cost could be a barrier, as health insurance coverage for DOACs varies. Patients with high-deductible health insurance plans, or who find themselves in the Medicare “donut hole,” may be at a particular disadvantage.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 66-year-old man with a history of hypertension and diabetes mellitus type 2 is hospitalized for palpitations and dizziness, and is given a diagnosis of atrial fibrillation (AF). His heart rate is successfully controlled with a beta-blocker. His CHA2DS2-VASc score is 3, meaning he is a candidate for anticoagulation. Which agent should you start?
Thromboembolism in patients with AF results in stroke and death and can be decreased with appropriate use of antithrombotic therapy. Evidence-based guidelines recommend patients with AF at intermediate or high risk of stroke (CHADS2 score ≥ 2 or prior history of cardioembolic stroke or transient ischemic attack) receive antithrombotic therapy with oral anticoagulation, rather than receive no therapy or therapy with antiplatelets.2,3
The American College of Chest Physicians also recommends the use of the direct oral anticoagulant (DOAC) dabigatran over warfarin for those patients with nonvalvular AF with an estimated glomerular filtration rate (eGFR) ≥15 mL/min/1.73 m2.3
A meta-analysis of large randomized controlled trials (RCTs) of individual DOACs (dabigatran [a direct thrombin inhibitor], rivaroxaban, apixaban, and edoxaban [factor Xa inhibitors]) revealed similar or lower rates of ischemic stroke and major bleeding (except gastrointestinal bleeds; relative risk=1.25; 95% CI, 1.01 to 1.55) when compared with warfarin (at an international normalized ratio [INR] goal of 2-3).4 In addition, 3 separate meta-analyses that pooled results from large RCTs involving dabigatran, apixaban, and rivaroxaban also concluded that these medications result in a significant reduction in embolic stroke and reduced the risk of major bleeds and hemorrhagic stroke when compared with warfarin.5-7
However, we know less about the comparative effectiveness and safety of the DOACs when they are used in clinical practice, and it is not clear which, if any of these agents, are superior to others. Moreover, only about half of the patients in the United States with AF who are eligible to take DOACs are currently managed with them.8
STUDY SUMMARY
One DOAC is better than warfarin at one thing; 2 others are better at another
This large cohort study examined the effectiveness of 3 DOACs compared with warfarin in 61,678 patients with AF by combining data from 3 Danish national databases. The patients had newly diagnosed AF (without valvular disease or venous thromboembolism) and were prescribed standard doses of DOACs (dabigatran 150 bid [N=12,701], rivaroxaban 20 mg/d [N=7192], apixaban 5 mg bid [N=6349]) or dose-adjusted warfarin to an INR goal of 2 to 3 (N=35,436). Patients were followed for an average of 1.9 years.
Ischemic stroke, systemic emboli. In the first year of observation, there were 1702 ischemic strokes or systemic emboli. The incidence of ischemic stroke or systemic embolism was either the same or better for each of the 3 DOAC treatments than for warfarin (DOACs, 2.9-3.9 events per 100 person-years; warfarin, 3.3 events per 100 person-years; no P value provided). Ischemic stroke or systemic emboli events occurred less frequently in the rivaroxaban group compared with warfarin at one year (hazard ratio [HR]=0.83; 95% confidence interval [CI], 0.69-0.99) and after 2.5 years (HR=0.80; 95% CI, 0.69-0.94). The rates of ischemic stroke and systemic emboli for both apixaban and dabigatran were not significantly different than that for warfarin at one year and 2.5 years.
Bleeding events (defined as intracranial, major gastrointestinal, and traumatic intracranial) were lower in the apixaban group (HR=0.63; 95% CI, 0.53-0.76) and dabigatran group (HR=0.61; 95% CI, 0.51-0.74) than in the warfarin group at one year. Significant reductions remained after 2.5 years. There was no difference in bleeding events between rivaroxaban and warfarin.
Risk of death. Compared with warfarin, the risk of death after one year of treatment was lower in the apixaban (HR=0.65; 95% CI, 0.56-0.75) and dabigatran (HR=0.63; 95% CI, 0.48-0.82) groups, and there was no significant difference in the rivaroxaban group (HR=0.92; 95% CI, 0.82-1.03).
WHAT’S NEW
No agent “has it all,” but DOACs have advantages
This comparative effectiveness and safety analysis reveals that all of the DOACs are at least as effective as warfarin in preventing ischemic stroke and systemic emboli, and that rivaroxaban may be more effective, and that apixaban and dabigatran have a lower risk of bleeding than warfarin.
CAVEATS
This non-randomized cohort trial lacked INR data
This study was a non-randomized cohort trial. And, while propensity weighting helps, the researchers were unable to completely control for underlying risk factors or unknown confounders.
INR data for patients on warfarin was not provided, so it is not clear how often patients were out of therapeutic range, which could affect the stroke and bleeding results in the warfarin group. This, however, is seen with routine use of warfarin. We feel that this study reflects the challenge of maintaining patients in warfarin’s narrow therapeutic range.
CHALLENGES TO IMPLEMENTATION
It comes down to cost
Cost could be a barrier, as health insurance coverage for DOACs varies. Patients with high-deductible health insurance plans, or who find themselves in the Medicare “donut hole,” may be at a particular disadvantage.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Larsen TB, Skjøth F, Nielsen PB, et al. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.
2. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. J Am Coll Cardiol. 2014;64:2246-2280.
3. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S-e575S.
4. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955-962.
5. Dentali F, Riva N, Crowther M, et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126:2381-2391.
6. Adam SS, McDuffie JR, Ortel TL, et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism. Ann Intern Med. 2012;157:796-807.
7. Ntaios G, Papavasileiou V, Diener H, et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298-3304.
8. Barnes GD, Lucas E, Alexander GC, et al. National trends in ambulatory oral anticoagulant use. Am J Med. 2015;128:1300-1305.
1. Larsen TB, Skjøth F, Nielsen PB, et al. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.
2. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. J Am Coll Cardiol. 2014;64:2246-2280.
3. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e531S-e575S.
4. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955-962.
5. Dentali F, Riva N, Crowther M, et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126:2381-2391.
6. Adam SS, McDuffie JR, Ortel TL, et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism. Ann Intern Med. 2012;157:796-807.
7. Ntaios G, Papavasileiou V, Diener H, et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43:3298-3304.
8. Barnes GD, Lucas E, Alexander GC, et al. National trends in ambulatory oral anticoagulant use. Am J Med. 2015;128:1300-1305.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
PRACTICE CHANGER
Use direct oral anticoagulants instead of warfarin in patients with atrial fibrillation because they are just as effective at preventing ischemic stroke and systemic emboli as warfarin, and because apixaban and dabigatran have lower bleeding rates.
STRENGTH OF RECOMMENDATION
B: Based on a single, prospective, cohort study.
Larsen TB, Skjøth F, Nielsen PB, et al. Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189.1
Which combined OC to prescribe with CV safety in mind?
ILLUSTRATIVE CASE
A 28-year-old woman presents to your office for a routine health maintenance examination. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a patient, physicians often have “go-to” favorites—tried and true agents that are easy to prescribe on a busy clinic day. However, some of these may be placing patients at increased risk for venous thromboembolic events.
In general, when compared with nonusers, women who use COCs have a 2- to 4-fold increase in risk of venous thromboembolism (VTE) and an increased risk of myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk of VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk of VTE than other preparations, despite similar estrogen content.7 The US Food and Drug Administration (FDA) produced a similar statement that same year, recommending that physicians carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks of ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One combined oral contraceptive comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks of pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included just under 5 million women 15 to 49 years of age, living in France, with at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks of first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 mcg) or high-dose estrogen (30-40 mcg) combined with one of 5 progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 (95% confidence interval [CI], 0.67-0.85) for PE, 0.82 (95% CI, 0.7-0.96) for ischemic stroke, and 0.56 (95% CI, 0.39-0.79) for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs of PE but not arterial events (2.16; 95% CI, 1.93-2.41 for desogestrel and 1.63; 95% CI, 1.34-1.97 for gestodene). The ARR with levonorgestrel use as opposed to desogestrel for PE was 19/100,000 person-years of use (NNH=5263); the ARR with levonorgestrel use as opposed to gestodene was 12/100,000 person-years of use (NNH=8333). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk of PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks of PE and arterial thromboembolism.
WHAT’S NEW?
Low-dose estrogen and levonorgestrel confer lowest risk of 3 CV conditions
Prior studies have shown that COCs increase the risk of PE and may also increase the risks of ischemic stroke and MI.
CAVEATS
A cohort study, no contraceptive start date, and incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk of VTE is highest in the first 3 months to one year of COC use.
CHALLENGES TO IMPLEMENTATION
Low-dose estrogen is associated with increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 mcg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. US Food and Drug Administration. Combined Hormonal Contraceptives (CHCs) and the Risk of Cardiovascular Disease Endpoints. Available at: https://www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed February 23, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP Monthly report on safety concerns, guidelines and general matters. 2012. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed February 23, 2017.
8. US Food and Drug Administration. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed February 23, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
ILLUSTRATIVE CASE
A 28-year-old woman presents to your office for a routine health maintenance examination. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a patient, physicians often have “go-to” favorites—tried and true agents that are easy to prescribe on a busy clinic day. However, some of these may be placing patients at increased risk for venous thromboembolic events.
In general, when compared with nonusers, women who use COCs have a 2- to 4-fold increase in risk of venous thromboembolism (VTE) and an increased risk of myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk of VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk of VTE than other preparations, despite similar estrogen content.7 The US Food and Drug Administration (FDA) produced a similar statement that same year, recommending that physicians carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks of ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One combined oral contraceptive comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks of pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included just under 5 million women 15 to 49 years of age, living in France, with at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks of first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 mcg) or high-dose estrogen (30-40 mcg) combined with one of 5 progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 (95% confidence interval [CI], 0.67-0.85) for PE, 0.82 (95% CI, 0.7-0.96) for ischemic stroke, and 0.56 (95% CI, 0.39-0.79) for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs of PE but not arterial events (2.16; 95% CI, 1.93-2.41 for desogestrel and 1.63; 95% CI, 1.34-1.97 for gestodene). The ARR with levonorgestrel use as opposed to desogestrel for PE was 19/100,000 person-years of use (NNH=5263); the ARR with levonorgestrel use as opposed to gestodene was 12/100,000 person-years of use (NNH=8333). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk of PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks of PE and arterial thromboembolism.
WHAT’S NEW?
Low-dose estrogen and levonorgestrel confer lowest risk of 3 CV conditions
Prior studies have shown that COCs increase the risk of PE and may also increase the risks of ischemic stroke and MI.
CAVEATS
A cohort study, no contraceptive start date, and incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk of VTE is highest in the first 3 months to one year of COC use.
CHALLENGES TO IMPLEMENTATION
Low-dose estrogen is associated with increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 mcg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 28-year-old woman presents to your office for a routine health maintenance examination. She is currently using an oral contraceptive containing desogestrel and ethinyl estradiol for contraception and is inquiring about a refill for the coming year. What would you recommend?
When choosing a combined oral contraceptive (COC) for a patient, physicians often have “go-to” favorites—tried and true agents that are easy to prescribe on a busy clinic day. However, some of these may be placing patients at increased risk for venous thromboembolic events.
In general, when compared with nonusers, women who use COCs have a 2- to 4-fold increase in risk of venous thromboembolism (VTE) and an increased risk of myocardial infarction (MI) and stroke.2,3 More specifically, higher doses of estrogen combined with the progesterones gestodene, desogestrel, and levonorgestrel, are associated with a higher risk of VTE.2-6
In 2012, the European Medicines Agency warned that COCs containing drospirenone were associated with a higher risk of VTE than other preparations, despite similar estrogen content.7 The US Food and Drug Administration (FDA) produced a similar statement that same year, recommending that physicians carefully consider the risks and benefits before prescribing contraceptives containing drospirenone.8
The risks of ischemic stroke and MI have not been clearly established for varying doses of estrogen and different progesterones. This large observational study fills that informational gap by providing risk estimates for the various COC options.
STUDY SUMMARY
One combined oral contraceptive comes out ahead
The authors used an observational cohort model to determine the effects of different doses of estrogen combined with different progesterones in COCs on the risks of pulmonary embolism (PE), ischemic stroke, and MI.1 Data were collected from the French national health insurance database and the French national hospital discharge database.9,10 The study included just under 5 million women 15 to 49 years of age, living in France, with at least one prescription filled for COCs between July 2010 and September 2012.
The investigators calculated the absolute and relative risks of first PE, ischemic stroke, and MI in women using COC formulations containing either low-dose estrogen (20 mcg) or high-dose estrogen (30-40 mcg) combined with one of 5 progesterones (norethisterone, norgestrel, levonorgestrel, desogestrel, gestodene). The relative risk (RR) was adjusted for confounding factors, including age, complimentary universal health insurance, socioeconomic status, hypertension, diabetes, and consultation with a gynecologist in the previous year.
The absolute risk per 100,000 woman-years for all COC use was 33 for PE, 19 for ischemic stroke, and 7 for MI with a composite risk of 60. The RRs for low-dose estrogen vs high-dose estrogen were 0.75 (95% confidence interval [CI], 0.67-0.85) for PE, 0.82 (95% CI, 0.7-0.96) for ischemic stroke, and 0.56 (95% CI, 0.39-0.79) for MI. The absolute risk reduction (ARR) with low-dose estrogen vs high-dose estrogen was 14/100,000 person-years of use; the number needed to harm (NNH) was 7143.
Compared with levonorgestrel, desogestrel and gestodene were associated with higher RRs of PE but not arterial events (2.16; 95% CI, 1.93-2.41 for desogestrel and 1.63; 95% CI, 1.34-1.97 for gestodene). The ARR with levonorgestrel use as opposed to desogestrel for PE was 19/100,000 person-years of use (NNH=5263); the ARR with levonorgestrel use as opposed to gestodene was 12/100,000 person-years of use (NNH=8333). The authors concluded that for the same progesterone, using a lower dose of estrogen decreases risk of PE, ischemic stroke, and MI, and that oral contraceptives containing levonorgestrel and low-dose estrogen resulted in the lowest overall risks of PE and arterial thromboembolism.
WHAT’S NEW?
Low-dose estrogen and levonorgestrel confer lowest risk of 3 CV conditions
Prior studies have shown that COCs increase the risk of PE and may also increase the risks of ischemic stroke and MI.
CAVEATS
A cohort study, no contraceptive start date, and incomplete tobacco use data
This is an observational cohort study, so it is subject to confounding factors and biases. It does, however, include a very large population, which improves validity. The study did not account for COC start date, which may be confounding because the risk of VTE is highest in the first 3 months to one year of COC use.
CHALLENGES TO IMPLEMENTATION
Low-dose estrogen is associated with increased vaginal spotting
One potential challenge to implementing this practice changer may be the increased rate of vaginal spotting associated with low-dose estrogen. COCs containing 20 mcg of estrogen are associated with spotting in approximately two-thirds of menstrual cycles over the course of a year.14 That said, women may prefer to endure the spotting in light of the improved safety profile of a lower-dose estrogen pill.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. US Food and Drug Administration. Combined Hormonal Contraceptives (CHCs) and the Risk of Cardiovascular Disease Endpoints. Available at: https://www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed February 23, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP Monthly report on safety concerns, guidelines and general matters. 2012. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed February 23, 2017.
8. US Food and Drug Administration. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed February 23, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
1. Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.
2. Lidegaard Ø, Løkkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
3. Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012;366:2257-2266.
4. Stegeman BH, de Bastos M, Rosendaal FR, et al. Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis. BMJ. 2013;347:f5298.
5. US Food and Drug Administration. Combined Hormonal Contraceptives (CHCs) and the Risk of Cardiovascular Disease Endpoints. Available at: https://www.fda.gov/downloads/drugs/drugsafety/ucm277384. Accessed February 23, 2017.
6. Seeger JD, Loughlin J, Eng PM, et al. Risk of thromboembolism in women taking ethinyl estradiol/drospirenone and other oral contraceptives. Obstet Gynecol. 2007;110:587-593.
7. European Medicines Agency. PhVWP Monthly report on safety concerns, guidelines and general matters. 2012. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2012/01/WC500121387.pdf. Accessed February 23, 2017.
8. US Food and Drug Administration. FDA Drug Safety Communication: Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. 2012. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Accessed February 23, 2017.
9. Tuppin P, de Roquefeuil L, Weill A, et al. French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique. 2010;58:286-290.
10. Moulis G, Lapeyre-Mestre M, Palmaro A, et al. French health insurance databases: what interest for medical research? Rev Med Interne. 2015;36:411-417.
11. Farmer RD, Lawrenson RA, Thompson CR, et al. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83-88.
12. Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ. 2011;343:d6423.
13. Zhang G, Xu X, Su W, et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736-745.
14. Akerlund M, Røde A, Westergaard J. Comparative profiles of reliability, cycle control and side effects of two oral contraceptive formulations containing 150 micrograms desogestrel and either 30 micrograms or 20 micrograms ethinyl oestradiol. Br J Obstet Gynaecol. 1993;100:832-838.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
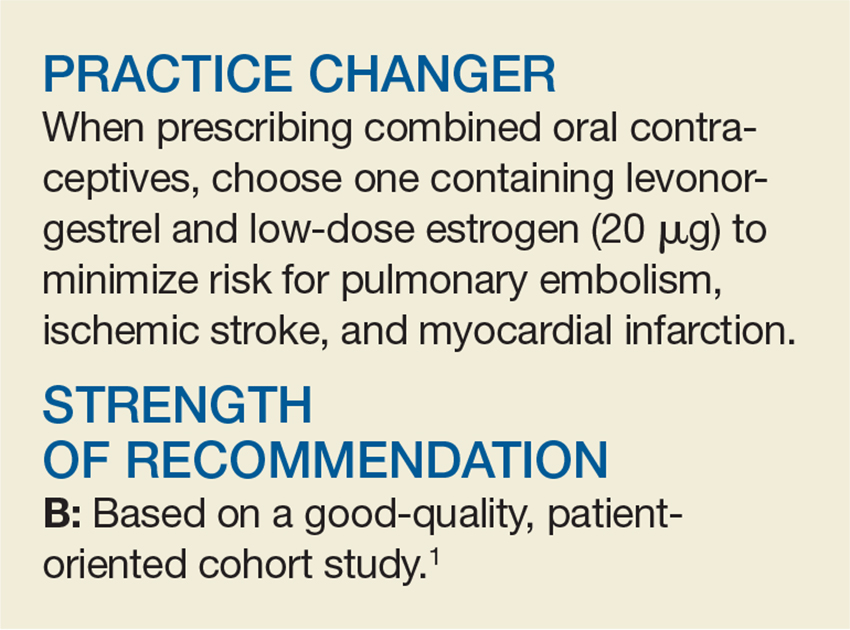
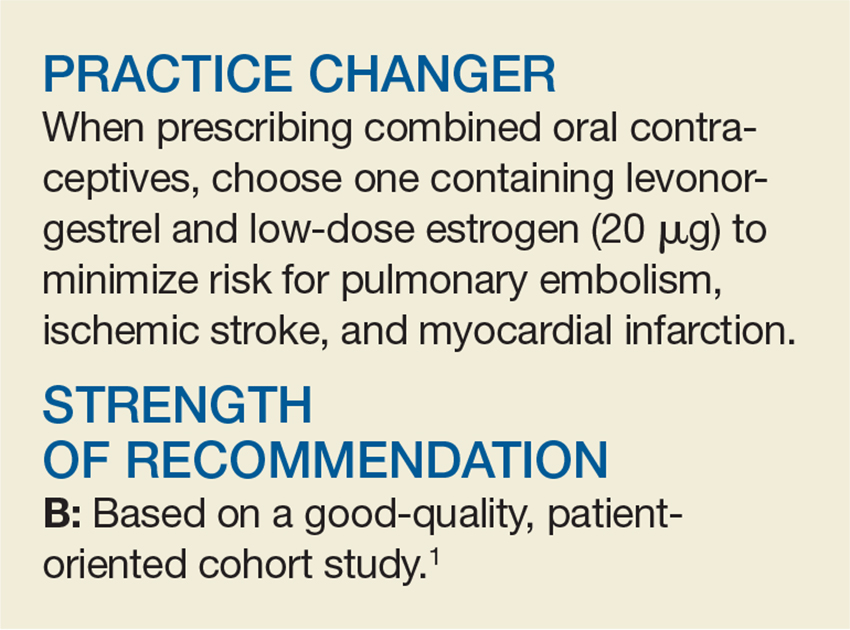
PRACTICE CHANGER
When prescribing combined oral contraceptives, choose one containing levonorgestrel and low-dose estrogen (20 mcg) to minimize the risks of pulmonary embolism, ischemic stroke, and myocardial infarction.
STRENGTH OF RECOMMENDATION
B: Based on a good quality, patient-oriented cohort study.
Weill A, Dalichampt M, Raguideau F, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353:i2002.1
Oral Agent Offers Relief From Generalized Hyperhidrosis

A 34-year-old woman presents to your office for unbearable sweating on her hands, face, and axillary regions. It occurs nearly daily, causing social embarrassment. She has tried multiple antiperspirants to no avail. What can she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem that affects 2% to 3% of the United States population.2 Patients may complain of localized sweating of the hands, feet, face, or underarms, or more systemic, generalized sweating in multiple locations. Either way, patients note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research by both subjective report and objective measurements has shown that antiperspirants containing aluminum salt are effective at reducing sweating, particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis, with minimal adverse effects.5 The availability of low-cost prescription and OTC aluminum-based antiperspirant agents makes topicals the firstline choice.
More invasive treatments are available for hyperhidrosis refractory to topicals. In a double-blind RCT, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating four weeks after initial injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are thus not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist has historically been used to treat overactive bladder. But oxybutynin not only reduces urinary frequency, it also decreases secretions in various locations and can therefore reduce perspiration and cause dry mouth.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomly assigned to either oxybutynin (titrated from 2.5 mg orally once daily to 5 mg orally twice daily) or placebo for six weeks.7 Seventeen patients (73.9%) receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms, compared with six patients (27.3%) in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin versus 9.1% of those who received placebo; however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter RCT compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with both localized and generalized forms of the condition.
Patients were included if they were older than 18, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥ 2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomly assigned to oxybutynin took 2.5 mg/d by mouth initially and increased gradually over eight days until reaching an effective dose that was no more than 7.5 mg/d. They then continued at that dose for six weeks.
The primary outcome was improvement on the HDSS by one or more points, measured at the beginning of the trial and again at six weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where disease has no impact on quality of life) to 30 (maximum impact of disease on quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-30s. Sixty percent of patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS, compared to 27% in the placebo group. DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group.
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in three patients (11%) in the placebo group; it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (four patients; 13%).
WHAT’S NEW
This is the first RCT to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few, if any, challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[6]:392-394).
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015; 173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003; 139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012; 55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.

A 34-year-old woman presents to your office for unbearable sweating on her hands, face, and axillary regions. It occurs nearly daily, causing social embarrassment. She has tried multiple antiperspirants to no avail. What can she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem that affects 2% to 3% of the United States population.2 Patients may complain of localized sweating of the hands, feet, face, or underarms, or more systemic, generalized sweating in multiple locations. Either way, patients note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research by both subjective report and objective measurements has shown that antiperspirants containing aluminum salt are effective at reducing sweating, particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis, with minimal adverse effects.5 The availability of low-cost prescription and OTC aluminum-based antiperspirant agents makes topicals the firstline choice.
More invasive treatments are available for hyperhidrosis refractory to topicals. In a double-blind RCT, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating four weeks after initial injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are thus not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist has historically been used to treat overactive bladder. But oxybutynin not only reduces urinary frequency, it also decreases secretions in various locations and can therefore reduce perspiration and cause dry mouth.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomly assigned to either oxybutynin (titrated from 2.5 mg orally once daily to 5 mg orally twice daily) or placebo for six weeks.7 Seventeen patients (73.9%) receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms, compared with six patients (27.3%) in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin versus 9.1% of those who received placebo; however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter RCT compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with both localized and generalized forms of the condition.
Patients were included if they were older than 18, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥ 2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomly assigned to oxybutynin took 2.5 mg/d by mouth initially and increased gradually over eight days until reaching an effective dose that was no more than 7.5 mg/d. They then continued at that dose for six weeks.
The primary outcome was improvement on the HDSS by one or more points, measured at the beginning of the trial and again at six weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where disease has no impact on quality of life) to 30 (maximum impact of disease on quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-30s. Sixty percent of patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS, compared to 27% in the placebo group. DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group.
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in three patients (11%) in the placebo group; it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (four patients; 13%).
WHAT’S NEW
This is the first RCT to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few, if any, challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[6]:392-394).

A 34-year-old woman presents to your office for unbearable sweating on her hands, face, and axillary regions. It occurs nearly daily, causing social embarrassment. She has tried multiple antiperspirants to no avail. What can she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem that affects 2% to 3% of the United States population.2 Patients may complain of localized sweating of the hands, feet, face, or underarms, or more systemic, generalized sweating in multiple locations. Either way, patients note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research by both subjective report and objective measurements has shown that antiperspirants containing aluminum salt are effective at reducing sweating, particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis, with minimal adverse effects.5 The availability of low-cost prescription and OTC aluminum-based antiperspirant agents makes topicals the firstline choice.
More invasive treatments are available for hyperhidrosis refractory to topicals. In a double-blind RCT, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating four weeks after initial injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are thus not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist has historically been used to treat overactive bladder. But oxybutynin not only reduces urinary frequency, it also decreases secretions in various locations and can therefore reduce perspiration and cause dry mouth.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomly assigned to either oxybutynin (titrated from 2.5 mg orally once daily to 5 mg orally twice daily) or placebo for six weeks.7 Seventeen patients (73.9%) receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms, compared with six patients (27.3%) in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin versus 9.1% of those who received placebo; however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter RCT compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with both localized and generalized forms of the condition.
Patients were included if they were older than 18, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥ 2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomly assigned to oxybutynin took 2.5 mg/d by mouth initially and increased gradually over eight days until reaching an effective dose that was no more than 7.5 mg/d. They then continued at that dose for six weeks.
The primary outcome was improvement on the HDSS by one or more points, measured at the beginning of the trial and again at six weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where disease has no impact on quality of life) to 30 (maximum impact of disease on quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-30s. Sixty percent of patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS, compared to 27% in the placebo group. DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group.
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in three patients (11%) in the placebo group; it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (four patients; 13%).
WHAT’S NEW
This is the first RCT to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few, if any, challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[6]:392-394).
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015; 173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003; 139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012; 55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015; 173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003; 139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012; 55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
Consider Melatonin for Migraine Prevention
A 32-year-old woman comes to your office for help with her recurrent migraines, which she’s had since her early 20s. She is otherwise healthy and active. She is frustrated by the frequency of her migraines and the resulting debilitation. She has tried prophylactic medications in the past but stopped taking them because of the adverse effects. What do you recommend for treatment?
Daily preventive medication can be helpful for patients whose chronic migraines have a significant impact on their lives. Many have a goal of reducing headache frequency, severity, and/or disability, while avoiding acute medication escalation.2 An estimated 38% of patients with migraine are appropriate candidates for prophylactic therapy, but only 3% to 13% are taking preventive medications.3
Evidence-based guidelines from the American Academy of Neurology and the American Headache Society state that antiepileptic drugs (divalproex sodium, sodium valproate, topiramate) and many ß-blockers (metoprolol, propranolol, timolol) are effective and should be recommended for migraine prevention.2 Medications such as antidepressants (amitriptyline, venlafaxine) and other ß-blockers (atenolol, nadolol) are probably effective and can be considered.2 However, adverse effects—including somnolence—are listed as “frequent” with amitriptyline and “occasional to frequent” with topiramate.4
Researchers have investigated melatonin before. But a 2010 double-blind, crossover RCT of 46 patients with two to seven migraine attacks per month found no significant difference in reduction of headache frequency between extended-release melatonin (2 mg taken 1 h before bed) and placebo over an eight-week period.5
STUDY SUMMARY
More than 50% reduction in headache frequency
This RCT, conducted in Brazil, compared the effectiveness of melatonin to amitriptyline and placebo for migraine prevention in 196 adults (ages 18 to 65) with chronic migraine.1 Eligible patients had a history of at least three migraine attacks or four migraine headache days per month. Patients were randomized to take identical-appearing melatonin (3 mg), amitriptyline (25 mg), or placebo nightly. The investigators appear to have concealed allocation adequately and used double-blinding.
The primary outcome was the number of headache days per month, compared to baseline. Secondary endpoints included reduction in migraine intensity, duration, number of analgesics used, and percentage of patients with more than 50% reduction in migraine headache days.
Compared to placebo, headache days per month were reduced in both the melatonin group (6.2 d vs 4.6 d, respectively; mean difference [MD], –1.6) and the amitriptyline group (6.2 d vs 5 d, respectively; MD, –1.2) at 12 weeks, based on intention-to-treat analysis. Mean headache intensity (0-10 pain scale) was also lower at 12 weeks in the melatonin group (4.8 vs 3.6; MD, –1.2) and in the amitriptyline group (4.8 vs 3.5; MD, –1.3), compared to placebo.
Headache duration (hours/month) at 12 weeks was reduced in both groups (MD, –4.4 h for amitriptyline and –4.8 h for melatonin), as was the number of analgesics used (MD for amitriptyline and for melatonin, –1) when compared to placebo. There was no significant difference between the melatonin and amitriptyline groups for these outcomes.
Patients taking melatonin were more likely to have more than 50% improvement in headache frequency compared to those taking amitriptyline (54% vs 39%; number needed to treat [NNT], 7). Melatonin worked much better than placebo (54% vs 20%; NNT, 3).
Adverse events were reported more often in the amitriptyline group than in the melatonin group (46 vs 16), with daytime sleepiness being the most frequent complaint (41% of patients in the amitriptyline group vs 18% of the melatonin group; number needed to harm [NNH], 5). There was no significant difference in adverse events between melatonin and placebo (16 vs 17). Melatonin resulted in weight loss (mean, –0.14 kg), whereas those taking amitriptyline gained weight (+0.97 kg).
WHAT’S NEW
Effective alternative with minimal adverse effects
Melatonin is an accessible and affordable option for prevention of migraine. The 3-mg dosing reduces headache frequency—measured by both the number of migraine headache days per month and the percentage of patients with a more than 50% reduction in headache events—as well as headache intensity, with minimal adverse effects.
CAVEATS
Product consistency, missing study data
This trial used 3-mg dosing, so it is not clear if other doses are also effective. In addition, melatonin’s OTC status means there could be a lack of consistency in quality/actual doses between brands.
Furthermore, in this trial, neither the amitriptyline nor the melatonin dose was titrated according to patient response or adverse effects, as it might be in clinical practice. As a result, we are not sure of the actual lowest effective dose or if greater effect (with continued minimal adverse effects) could be achieved with higher doses.
Lastly, 69% to 75% of patients in the treatment groups completed the 16-week trial, and the researchers reported using three different analytic techniques to estimate missing data. (For example, the primary endpoint analysis included data for 90.8% of randomized patients [178 of 196], and the authors treated all missing data as nonheadache days.) It is unclear how the missing data would affect the outcome—although in this type of analysis, it would tend toward a null effect.
CHALLENGES TO IMPLEMENTATION
Challenges are negligible
There are really no challenges to implementing this practice changer; melatonin is readily available and is affordable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[5]:320-322).
1. Gonçalves AL, Martini Ferreira A, Ribeiro RT, et al. Randomised clinical trial comparing melatonin 3 mg, amitriptyline 25 mg and placebo for migraine prevention. J Neurol Neurosurg Psychiatry. 2016;87:1127-1132.
2. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
3. Lipton RB, Bigal ME, Diamond M, et al; The American Migraine Prevalence and Prevention Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349.
4. Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55:754-762.
5. Alstadhaug KB, Odeh F, Salvesen R, et al. Prophylaxis of migraine with melatonin: a randomized controlled trial. Neurology. 2010;75:1527-1532.
A 32-year-old woman comes to your office for help with her recurrent migraines, which she’s had since her early 20s. She is otherwise healthy and active. She is frustrated by the frequency of her migraines and the resulting debilitation. She has tried prophylactic medications in the past but stopped taking them because of the adverse effects. What do you recommend for treatment?
Daily preventive medication can be helpful for patients whose chronic migraines have a significant impact on their lives. Many have a goal of reducing headache frequency, severity, and/or disability, while avoiding acute medication escalation.2 An estimated 38% of patients with migraine are appropriate candidates for prophylactic therapy, but only 3% to 13% are taking preventive medications.3
Evidence-based guidelines from the American Academy of Neurology and the American Headache Society state that antiepileptic drugs (divalproex sodium, sodium valproate, topiramate) and many ß-blockers (metoprolol, propranolol, timolol) are effective and should be recommended for migraine prevention.2 Medications such as antidepressants (amitriptyline, venlafaxine) and other ß-blockers (atenolol, nadolol) are probably effective and can be considered.2 However, adverse effects—including somnolence—are listed as “frequent” with amitriptyline and “occasional to frequent” with topiramate.4
Researchers have investigated melatonin before. But a 2010 double-blind, crossover RCT of 46 patients with two to seven migraine attacks per month found no significant difference in reduction of headache frequency between extended-release melatonin (2 mg taken 1 h before bed) and placebo over an eight-week period.5
STUDY SUMMARY
More than 50% reduction in headache frequency
This RCT, conducted in Brazil, compared the effectiveness of melatonin to amitriptyline and placebo for migraine prevention in 196 adults (ages 18 to 65) with chronic migraine.1 Eligible patients had a history of at least three migraine attacks or four migraine headache days per month. Patients were randomized to take identical-appearing melatonin (3 mg), amitriptyline (25 mg), or placebo nightly. The investigators appear to have concealed allocation adequately and used double-blinding.
The primary outcome was the number of headache days per month, compared to baseline. Secondary endpoints included reduction in migraine intensity, duration, number of analgesics used, and percentage of patients with more than 50% reduction in migraine headache days.
Compared to placebo, headache days per month were reduced in both the melatonin group (6.2 d vs 4.6 d, respectively; mean difference [MD], –1.6) and the amitriptyline group (6.2 d vs 5 d, respectively; MD, –1.2) at 12 weeks, based on intention-to-treat analysis. Mean headache intensity (0-10 pain scale) was also lower at 12 weeks in the melatonin group (4.8 vs 3.6; MD, –1.2) and in the amitriptyline group (4.8 vs 3.5; MD, –1.3), compared to placebo.
Headache duration (hours/month) at 12 weeks was reduced in both groups (MD, –4.4 h for amitriptyline and –4.8 h for melatonin), as was the number of analgesics used (MD for amitriptyline and for melatonin, –1) when compared to placebo. There was no significant difference between the melatonin and amitriptyline groups for these outcomes.
Patients taking melatonin were more likely to have more than 50% improvement in headache frequency compared to those taking amitriptyline (54% vs 39%; number needed to treat [NNT], 7). Melatonin worked much better than placebo (54% vs 20%; NNT, 3).
Adverse events were reported more often in the amitriptyline group than in the melatonin group (46 vs 16), with daytime sleepiness being the most frequent complaint (41% of patients in the amitriptyline group vs 18% of the melatonin group; number needed to harm [NNH], 5). There was no significant difference in adverse events between melatonin and placebo (16 vs 17). Melatonin resulted in weight loss (mean, –0.14 kg), whereas those taking amitriptyline gained weight (+0.97 kg).
WHAT’S NEW
Effective alternative with minimal adverse effects
Melatonin is an accessible and affordable option for prevention of migraine. The 3-mg dosing reduces headache frequency—measured by both the number of migraine headache days per month and the percentage of patients with a more than 50% reduction in headache events—as well as headache intensity, with minimal adverse effects.
CAVEATS
Product consistency, missing study data
This trial used 3-mg dosing, so it is not clear if other doses are also effective. In addition, melatonin’s OTC status means there could be a lack of consistency in quality/actual doses between brands.
Furthermore, in this trial, neither the amitriptyline nor the melatonin dose was titrated according to patient response or adverse effects, as it might be in clinical practice. As a result, we are not sure of the actual lowest effective dose or if greater effect (with continued minimal adverse effects) could be achieved with higher doses.
Lastly, 69% to 75% of patients in the treatment groups completed the 16-week trial, and the researchers reported using three different analytic techniques to estimate missing data. (For example, the primary endpoint analysis included data for 90.8% of randomized patients [178 of 196], and the authors treated all missing data as nonheadache days.) It is unclear how the missing data would affect the outcome—although in this type of analysis, it would tend toward a null effect.
CHALLENGES TO IMPLEMENTATION
Challenges are negligible
There are really no challenges to implementing this practice changer; melatonin is readily available and is affordable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[5]:320-322).
A 32-year-old woman comes to your office for help with her recurrent migraines, which she’s had since her early 20s. She is otherwise healthy and active. She is frustrated by the frequency of her migraines and the resulting debilitation. She has tried prophylactic medications in the past but stopped taking them because of the adverse effects. What do you recommend for treatment?
Daily preventive medication can be helpful for patients whose chronic migraines have a significant impact on their lives. Many have a goal of reducing headache frequency, severity, and/or disability, while avoiding acute medication escalation.2 An estimated 38% of patients with migraine are appropriate candidates for prophylactic therapy, but only 3% to 13% are taking preventive medications.3
Evidence-based guidelines from the American Academy of Neurology and the American Headache Society state that antiepileptic drugs (divalproex sodium, sodium valproate, topiramate) and many ß-blockers (metoprolol, propranolol, timolol) are effective and should be recommended for migraine prevention.2 Medications such as antidepressants (amitriptyline, venlafaxine) and other ß-blockers (atenolol, nadolol) are probably effective and can be considered.2 However, adverse effects—including somnolence—are listed as “frequent” with amitriptyline and “occasional to frequent” with topiramate.4
Researchers have investigated melatonin before. But a 2010 double-blind, crossover RCT of 46 patients with two to seven migraine attacks per month found no significant difference in reduction of headache frequency between extended-release melatonin (2 mg taken 1 h before bed) and placebo over an eight-week period.5
STUDY SUMMARY
More than 50% reduction in headache frequency
This RCT, conducted in Brazil, compared the effectiveness of melatonin to amitriptyline and placebo for migraine prevention in 196 adults (ages 18 to 65) with chronic migraine.1 Eligible patients had a history of at least three migraine attacks or four migraine headache days per month. Patients were randomized to take identical-appearing melatonin (3 mg), amitriptyline (25 mg), or placebo nightly. The investigators appear to have concealed allocation adequately and used double-blinding.
The primary outcome was the number of headache days per month, compared to baseline. Secondary endpoints included reduction in migraine intensity, duration, number of analgesics used, and percentage of patients with more than 50% reduction in migraine headache days.
Compared to placebo, headache days per month were reduced in both the melatonin group (6.2 d vs 4.6 d, respectively; mean difference [MD], –1.6) and the amitriptyline group (6.2 d vs 5 d, respectively; MD, –1.2) at 12 weeks, based on intention-to-treat analysis. Mean headache intensity (0-10 pain scale) was also lower at 12 weeks in the melatonin group (4.8 vs 3.6; MD, –1.2) and in the amitriptyline group (4.8 vs 3.5; MD, –1.3), compared to placebo.
Headache duration (hours/month) at 12 weeks was reduced in both groups (MD, –4.4 h for amitriptyline and –4.8 h for melatonin), as was the number of analgesics used (MD for amitriptyline and for melatonin, –1) when compared to placebo. There was no significant difference between the melatonin and amitriptyline groups for these outcomes.
Patients taking melatonin were more likely to have more than 50% improvement in headache frequency compared to those taking amitriptyline (54% vs 39%; number needed to treat [NNT], 7). Melatonin worked much better than placebo (54% vs 20%; NNT, 3).
Adverse events were reported more often in the amitriptyline group than in the melatonin group (46 vs 16), with daytime sleepiness being the most frequent complaint (41% of patients in the amitriptyline group vs 18% of the melatonin group; number needed to harm [NNH], 5). There was no significant difference in adverse events between melatonin and placebo (16 vs 17). Melatonin resulted in weight loss (mean, –0.14 kg), whereas those taking amitriptyline gained weight (+0.97 kg).
WHAT’S NEW
Effective alternative with minimal adverse effects
Melatonin is an accessible and affordable option for prevention of migraine. The 3-mg dosing reduces headache frequency—measured by both the number of migraine headache days per month and the percentage of patients with a more than 50% reduction in headache events—as well as headache intensity, with minimal adverse effects.
CAVEATS
Product consistency, missing study data
This trial used 3-mg dosing, so it is not clear if other doses are also effective. In addition, melatonin’s OTC status means there could be a lack of consistency in quality/actual doses between brands.
Furthermore, in this trial, neither the amitriptyline nor the melatonin dose was titrated according to patient response or adverse effects, as it might be in clinical practice. As a result, we are not sure of the actual lowest effective dose or if greater effect (with continued minimal adverse effects) could be achieved with higher doses.
Lastly, 69% to 75% of patients in the treatment groups completed the 16-week trial, and the researchers reported using three different analytic techniques to estimate missing data. (For example, the primary endpoint analysis included data for 90.8% of randomized patients [178 of 196], and the authors treated all missing data as nonheadache days.) It is unclear how the missing data would affect the outcome—although in this type of analysis, it would tend toward a null effect.
CHALLENGES TO IMPLEMENTATION
Challenges are negligible
There are really no challenges to implementing this practice changer; melatonin is readily available and is affordable.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2017;66[5]:320-322).
1. Gonçalves AL, Martini Ferreira A, Ribeiro RT, et al. Randomised clinical trial comparing melatonin 3 mg, amitriptyline 25 mg and placebo for migraine prevention. J Neurol Neurosurg Psychiatry. 2016;87:1127-1132.
2. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
3. Lipton RB, Bigal ME, Diamond M, et al; The American Migraine Prevalence and Prevention Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349.
4. Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55:754-762.
5. Alstadhaug KB, Odeh F, Salvesen R, et al. Prophylaxis of migraine with melatonin: a randomized controlled trial. Neurology. 2010;75:1527-1532.
1. Gonçalves AL, Martini Ferreira A, Ribeiro RT, et al. Randomised clinical trial comparing melatonin 3 mg, amitriptyline 25 mg and placebo for migraine prevention. J Neurol Neurosurg Psychiatry. 2016;87:1127-1132.
2. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
3. Lipton RB, Bigal ME, Diamond M, et al; The American Migraine Prevalence and Prevention Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349.
4. Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55:754-762.
5. Alstadhaug KB, Odeh F, Salvesen R, et al. Prophylaxis of migraine with melatonin: a randomized controlled trial. Neurology. 2010;75:1527-1532.
Oral agent offers relief from generalized hyperhidrosis
ILLUSTRATIVE CASE
A 34-year-old woman presents to your office for unbearable sweating. She notes that the sweating occurs nearly daily on her hands, face, and in her axillary regions, causing social embarrassment. She has tried multiple antiperspirants to no avail. Is there anything she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem affecting 2% to 3% of the population in the United States.2 Patients may complain of localized sweating of the hands, feet, face, or underarms or more systemic, generalized sweating in multiple locations. Either way, patients always note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research has shown that localized treatment with antiperspirants containing aluminum salt is effective by both subjective report and objective measurements at reducing sweating—particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis with minimal adverse effects.5 The availability of low-cost prescription and over-the-counter aluminum-based antiperspirant agents makes topicals the first-line choice.
More invasive treatments are available for hyperhidrosis that is refractory to topicals. In a double-blind, randomized controlled trial, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating at 4 weeks after one injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are, thus, not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist had historically been used to treat overactive bladder. As a cholinergic antagonist, oxybutynin not only reduces urinary frequency, but also decreases secretions in various locations and, thus, can cause dry mouth and reduce perspiration.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomized to receive either oxybutynin titrated from 2.5 mg orally once daily to 5 mg orally twice daily or placebo for 6 weeks.7 Seventeen (73.9%) patients receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms compared with 6 (27.3%) patients in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin vs 9.1% of those who received placebo (P=.038); however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter, randomized controlled trial compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with a localized, as well as a generalized form of the condition.
Patients were included if they were >18 years of age, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomized to oxybutynin took 2.5 mg/d orally initially and increased gradually over 8 days until reaching an effective dose that was not more than 7.5 mg/d. They then continued at that dose for 6 weeks. The primary outcome was improvement on the HDSS by one or more points measured at the beginning of the trial and at 6 weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where their disease has no impact on their quality of life) to 30 (maximum impact of their disease on their quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-thirties. Sixty percent of the patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS compared to 27% in the placebo group (P<.01). DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group (P<.01).
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in 3 patients (11%) in the placebo group (P<.01); it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (4 patients; 13%).
WHAT'S NEW
This is the first randomized controlled trial to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few if any challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015;173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type a is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012;55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
ILLUSTRATIVE CASE
A 34-year-old woman presents to your office for unbearable sweating. She notes that the sweating occurs nearly daily on her hands, face, and in her axillary regions, causing social embarrassment. She has tried multiple antiperspirants to no avail. Is there anything she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem affecting 2% to 3% of the population in the United States.2 Patients may complain of localized sweating of the hands, feet, face, or underarms or more systemic, generalized sweating in multiple locations. Either way, patients always note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research has shown that localized treatment with antiperspirants containing aluminum salt is effective by both subjective report and objective measurements at reducing sweating—particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis with minimal adverse effects.5 The availability of low-cost prescription and over-the-counter aluminum-based antiperspirant agents makes topicals the first-line choice.
More invasive treatments are available for hyperhidrosis that is refractory to topicals. In a double-blind, randomized controlled trial, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating at 4 weeks after one injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are, thus, not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist had historically been used to treat overactive bladder. As a cholinergic antagonist, oxybutynin not only reduces urinary frequency, but also decreases secretions in various locations and, thus, can cause dry mouth and reduce perspiration.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomized to receive either oxybutynin titrated from 2.5 mg orally once daily to 5 mg orally twice daily or placebo for 6 weeks.7 Seventeen (73.9%) patients receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms compared with 6 (27.3%) patients in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin vs 9.1% of those who received placebo (P=.038); however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter, randomized controlled trial compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with a localized, as well as a generalized form of the condition.
Patients were included if they were >18 years of age, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomized to oxybutynin took 2.5 mg/d orally initially and increased gradually over 8 days until reaching an effective dose that was not more than 7.5 mg/d. They then continued at that dose for 6 weeks. The primary outcome was improvement on the HDSS by one or more points measured at the beginning of the trial and at 6 weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where their disease has no impact on their quality of life) to 30 (maximum impact of their disease on their quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-thirties. Sixty percent of the patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS compared to 27% in the placebo group (P<.01). DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group (P<.01).
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in 3 patients (11%) in the placebo group (P<.01); it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (4 patients; 13%).
WHAT'S NEW
This is the first randomized controlled trial to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few if any challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 34-year-old woman presents to your office for unbearable sweating. She notes that the sweating occurs nearly daily on her hands, face, and in her axillary regions, causing social embarrassment. She has tried multiple antiperspirants to no avail. Is there anything she can take to reduce the sweating?
Hyperhidrosis is a common, self-limiting problem affecting 2% to 3% of the population in the United States.2 Patients may complain of localized sweating of the hands, feet, face, or underarms or more systemic, generalized sweating in multiple locations. Either way, patients always note a significant impact on their quality of life.
Treatment of hyperhidrosis has traditionally focused on topical therapies to the affected areas. Research has shown that localized treatment with antiperspirants containing aluminum salt is effective by both subjective report and objective measurements at reducing sweating—particularly in the axilla, hands, and feet.3,4 Additionally, a systematic review of observational and experimental studies found topical glycopyrrolate to be efficacious for craniofacial hyperhidrosis with minimal adverse effects.5 The availability of low-cost prescription and over-the-counter aluminum-based antiperspirant agents makes topicals the first-line choice.
More invasive treatments are available for hyperhidrosis that is refractory to topicals. In a double-blind, randomized controlled trial, researchers injected either botulinum toxin type A (BTX-A) 50 U or placebo in patients with bilateral primary axillary hyperhidrosis.6 Of the 207 patients who received treatment injections, 96.1% had at least a 50% reduction of axillary sweating at 4 weeks after one injection, as measured by gravimetric assessment. The BTX-A injections also produced a prolonged effect; mean duration between injections was 30.6 weeks.
Other invasive treatments include iontophoresis, surgery, and laser therapy; however, these methods are not suitable for body-wide application and are, thus, not appropriate for patients with generalized hyperhidrosis.
Oxybutynin is the first oral agent to emerge as a treatment option for hyperhidrosis. This cholinergic antagonist had historically been used to treat overactive bladder. As a cholinergic antagonist, oxybutynin not only reduces urinary frequency, but also decreases secretions in various locations and, thus, can cause dry mouth and reduce perspiration.
In one prospective placebo-controlled trial, 50 patients with generalized hyperhidrosis were randomized to receive either oxybutynin titrated from 2.5 mg orally once daily to 5 mg orally twice daily or placebo for 6 weeks.7 Seventeen (73.9%) patients receiving oxybutynin for palmar or axillary hyperhidrosis reported moderate to “great” resolution of their symptoms compared with 6 (27.3%) patients in the placebo group. Dry mouth was reported in 34.8% of patients receiving oxybutynin vs 9.1% of those who received placebo (P=.038); however, no patients dropped out of the study due to this adverse effect.7
STUDY SUMMARY
This multicenter, randomized controlled trial compared oxybutynin to placebo in 62 adults with localized or generalized hyperhidrosis from 12 outpatient dermatology practices in France. It is the first study to include patients with a localized, as well as a generalized form of the condition.
Patients were included if they were >18 years of age, enrolled in the National Health Insurance system in France, and reported a Hyperhidrosis Disease Severity Scale (HDSS) score ≥2. The HDSS is a validated, one-question tool (“How would you rate the severity of your sweating?”). Patients provide a score of 1 (no perceptible sweating and no interference with everyday life) to 4 (intolerable sweating with constant interference with everyday life).8 Patients were excluded if they had any contraindications to the use of an anticholinergic medication.
Patients randomized to oxybutynin took 2.5 mg/d orally initially and increased gradually over 8 days until reaching an effective dose that was not more than 7.5 mg/d. They then continued at that dose for 6 weeks. The primary outcome was improvement on the HDSS by one or more points measured at the beginning of the trial and at 6 weeks. Secondary outcomes included change in quality of life, as measured by the Dermatology Life Quality Index (DLQI) and reported adverse effects. The DLQI is a dermatology-specific quality-of-life measure consisting of 10 questions. Scores range from 0 (where their disease has no impact on their quality of life) to 30 (maximum impact of their disease on their quality of life).9
Improved HDSS and DLQI scores. Most patients (83%) in the study had generalized hyperhidrosis. Patients were in their mid-thirties. Sixty percent of the patients in the oxybutynin group had an improvement of one point or more on the 4-point HDSS compared to 27% in the placebo group (P<.01). DLQI scores improved by 6.9 points in the oxybutynin group and 2.3 points in the placebo group (P<.01).
The most common adverse effect was dry mouth, which occurred in 13 patients (43%) in the oxybutynin group and in 3 patients (11%) in the placebo group (P<.01); it did not cause any patients to drop out of the study. The second most common adverse effect was blurred vision, which only occurred in the oxybutynin group (4 patients; 13%).
WHAT'S NEW
This is the first randomized controlled trial to demonstrate the efficacy of an oral agent for generalized primary hyperhidrosis. This trial used a relatively low dose of oxybutynin, which produced significant benefit while minimizing anticholinergic adverse effects.
CAVEATS
There are many situations for which anticholinergic medications are inappropriate, including use by geriatric patients and those with gastrointestinal disorders, urinary retention, or glaucoma.
CHALLENGES TO IMPLEMENTATION
Few if any challenges exist to the utilization of oxybutynin; inexpensive generic versions are widely available.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015;173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type a is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012;55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
1. Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015;173:1163-1168.
2. Grabell DA, Hebert AA. Current and emerging medical therapies for primary hyperhidrosis. Dermatol Ther (Heidelb). 2017;7:25-36.
3. Innocenzi D, Lupi F, Bruni F, et al. Efficacy of a new aluminium salt thermophobic foam in the treatment of axillary and palmar primary hyperhidrosis: a pilot exploratory trial. Curr Med Res Opin. 2005;21:1949-1953.
4. Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29:368-370.
5. Nicholas R, Quddus A, Baker DM. Treatment of primary craniofacial hyperhidrosis: a systematic review. Am J Clin Dermatol. 2015;16:361-370.
6. Naumann M, Lowe NJ, Kumar CR, et al. Botulinum toxin type a is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736.
7. Wolosker N, de Campos JR, Kauffman P, et al. A randomized placebo-controlled trial of oxybutynin for the initial treatment of palmar and axillary hyperhidrosis. J Vasc Surg. 2012;55:1696-1700.
8. Varella AY, Fukuda JM, Teivelis MP, et al. Translation and validation of Hyperhidrosis Disease Severity Scale. Rev Assoc Med Bras. 2016;62:843-847.
9. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
PRACTICE CHANGER
Use low-dose oxybutynin as a first-line treatment option for patients with primary hyperhidrosis to improve symptoms and quality of life.1
STRENGTH OF RECOMMENDATION
B: Based on a single, good quality, randomized controlled trial.
Schollhammer M, Brenaut E, Menard-Andivot N, et al. Oxybutynin as a treatment for generalized hyperhidrosis: a randomized, placebo-controlled trial. Br J Dermatol. 2015;173:1163-1168.