User login
Synthetic opioids drive spike in U.S. fatal drug overdoses
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
New federal statistics suggest that the opioid epidemic in the United States is evolving as physicians crack down on the use of prescription painkillers: Fatal drug overdose deaths rose by 12% from 2016 to 2017, boosted by a wave of fatalities linked to illicit synthetic opioids like fentanyl that are now linked to an estimated 60% of opioid-related deaths.
“Overall, the overdose epidemic continues to worsen, and it has grown increasingly complex by coinvolvement of prescription and illicit drugs,” Lawrence Scholl, PhD, MPH, and his associates at the Centers for Disease Control & Prevention wrote in the Morbidity and Mortality Weekly Report.
The new statistics provide more evidence that 2017 marked “a sharp increase in what has characterized as the third wave of the opioid epidemic,” said drug and health policy researcher Stephen Crystal, PhD, of Rutgers University, New Brunswick, N.J., in an interview. He was referring to a wave that experts believe started in 2013 amid a spike in U.S. overdose deaths from fentanyl and other synthetic opioids.
The new report analyzes fatal drug overdose data from 2013 to 2017. According to the findings, the total number of those overdoses rose to 70,237 in 2017, up from 63,632 in 2016. The highest drug overdose death rates in 2017 were in West Virginia, followed by Ohio, Pennsylvania, and the District of Columbia.
Some statistics did not change much from 2016 to 2017: About two-thirds of the drug overdose deaths were linked to opioids in both years, and the death rate of cases linked to prescription drugs and heroin remained steady. (Death rates in the report were age adjusted.)
However, the percentage of fatal overdose cases linked to synthetic opioids grew 45% from 2016 to 2017. Overall, 60% of opioid-related fatal overdoses in 2017 involved synthetic opioids.
The report identifies increases in several areas from 2016 to 2017. Opioid-related drug overdose deaths among black people rose by 25%, and an analysis of data from 34 states and the District of Columbia found the highest increases in death rates in North Carolina (29%), Ohio (19%), and Maine (19%).
In regard to deaths linked to synthetic opioids specifically, the highest death rates in 2017 were in West Virginia (37 per 100,000), Ohio (32 per 100,000), and New Hampshire (30 per 100,000).
“Part of what we’re seeing in these increased numbers are individuals who have pain, can’t get prescribed opioids, and turn to street drugs,” Dr. Crystal said, adding that “abruptly cutting patients off is not good, and leaving patients with a lot of untreated pain is not good. If people are going to be discontinued [from opioids] or have their doses reduced, the taper needs to be done very slowly and carefully.”
Synthetic opioids were not the only drugs that are driving up fatal overdoses, as the death rates of cases linked to cocaine and psychostimulants (such as methamphetamine) jumped by more than a third in 2017.
“The most important thing these numbers are telling me is that it’s becoming more and more attractive to drug dealers to put fentanyl in the heroin, cocaine, and other drugs they sell,” Dr. Crystal said. “When that happens, dependence on street drugs becomes much more deadly. It’s almost impossible to get the dose right. Every time you shoot up, you’re taking a chance that you’ll overdose.”
The report had limitations, including the fact that details about drug use were missing from 12% (2016) and 15% (2017) of death certificates in fatal overdose cases. By state, the percentages of those death certificates that included drug information ranged from as little as 55% to 99%.
There’s some possible positive news: The report points to preliminary data from 2018 suggesting that the number of annual drug overdose deaths may be leveling off – although it says more analysis is needed to confirm the trend.
Dr. Crystal, however, is not celebrating. “I don’t see this as a good news story, really,” he said, adding that there’s “a little too much of people patting themselves on the back” because they’re proud of cutbacks in opioid prescriptions.
“This doesn’t have to do with the huge number of people who got started with opioids years ago” and are now at risk of using street drugs, he said. “We haven’t engaged that population at the rate we need to. And flattening out at 70,000 drug overdoses a year is not a good news story.”
Dr. Crystal reported no relevant disclosures.
SOURCE: Scholl L et al. MMWR. 2019 Jan 4;67(5152):1419-27.
FROM MMWR
Surgeon general takes on teen vaping; medical groups show support
U.S. Surgeon General Jerome Adams, MD, responded Dec. 18 to recent data showing a sharp increase in the use of nicotine-based e-cigarette products among American teens with an urgent call to action.
“I, Surgeon General of the United States Public Health Service, [Vice Admiral] Jerome Adams, am emphasizing the importance of protecting our children from a lifetime of nicotine addiction and associated health risks by immediately addressing the epidemic of youth e-cigarette use,” Dr. Adams said in an advisory. “The recent surge in e-cigarette use among youth, which has been fueled by new types of e-cigarettes that have recently entered the market, is a cause for great concern. We must take action now to protect the health of our nation’s young people.”
The surgeon general’s advisory emphasized that e-cigarette products are not harmless and that, in addition to potentially addictive nicotine, many products contain other dangerous substances, including heavy metals, volatile organic compounds, and ultrafine particles that can affect the lungs. In addition, some e-cigarette products contain potentially harmful chemicals used to add flavoring.
The complete advisory includes information for parents, teachers, and clinicians about the details of current e-cigarette products and strategies for working to reduce their use among teens.
The American Medical Association expressed support of the surgeon general’s call to action.
“The only way to prevent another generation from developing nicotine dependence is to continue to raise awareness that e-cigarettes are harmful, powerfully addictive, and can often lead young people to smoke conventional cigarettes. E-cigarettes have the potential to undermine the public health gains that have been made over the years in combating the smoking epidemic,” Barbara L. McAneny, MD, president of the AMA, said in the statement.
“Recognizing the use of e-cigarettes and vaping as an urgent public health epidemic, the AMA has adopted numerous policies in recent years aimed at preventing youth access to these harmful tobacco products. In line with the surgeon general’s advisory, the AMA also has existing policy urging physicians to educate themselves about e-cigarettes and be prepared to counsel patients about e-cigarette usage and the potential for nicotine addiction,” Dr. McAneny said. she added.
The American Heart Association expressed support for the surgeon general’s call as well.
“That the U.S. Surgeon General is calling teen vaping an ‘epidemic’ should seize the attention of elected officials and the community of organizations working to protect the health of our nation’s children. We commend Surgeon General Adams, Commissioner [Adam] Gottlieb and Secretary [Alex M.] Azar for marshaling parents, educators, health providers, and communities to apply proven methods to overcome the epidemic of e-cigarette use,” Nancy Brown, CEO of the AHA, said in a Dec. 18 statement.
“But more must be done in the face of rapidly rising e-cigarette use among youth. The FDA’s recent announcement that it plans to restrict marketing and sales of flavored tobacco products must be followed by immediate, concrete action that sends an unmistakable message that the tobacco industry’s relentless targeting of our nation’s children will no longer be tolerated,” she emphasized.
View the surgeon general’s video message and access additional e-cigarette information here.
U.S. Surgeon General Jerome Adams, MD, responded Dec. 18 to recent data showing a sharp increase in the use of nicotine-based e-cigarette products among American teens with an urgent call to action.
“I, Surgeon General of the United States Public Health Service, [Vice Admiral] Jerome Adams, am emphasizing the importance of protecting our children from a lifetime of nicotine addiction and associated health risks by immediately addressing the epidemic of youth e-cigarette use,” Dr. Adams said in an advisory. “The recent surge in e-cigarette use among youth, which has been fueled by new types of e-cigarettes that have recently entered the market, is a cause for great concern. We must take action now to protect the health of our nation’s young people.”
The surgeon general’s advisory emphasized that e-cigarette products are not harmless and that, in addition to potentially addictive nicotine, many products contain other dangerous substances, including heavy metals, volatile organic compounds, and ultrafine particles that can affect the lungs. In addition, some e-cigarette products contain potentially harmful chemicals used to add flavoring.
The complete advisory includes information for parents, teachers, and clinicians about the details of current e-cigarette products and strategies for working to reduce their use among teens.
The American Medical Association expressed support of the surgeon general’s call to action.
“The only way to prevent another generation from developing nicotine dependence is to continue to raise awareness that e-cigarettes are harmful, powerfully addictive, and can often lead young people to smoke conventional cigarettes. E-cigarettes have the potential to undermine the public health gains that have been made over the years in combating the smoking epidemic,” Barbara L. McAneny, MD, president of the AMA, said in the statement.
“Recognizing the use of e-cigarettes and vaping as an urgent public health epidemic, the AMA has adopted numerous policies in recent years aimed at preventing youth access to these harmful tobacco products. In line with the surgeon general’s advisory, the AMA also has existing policy urging physicians to educate themselves about e-cigarettes and be prepared to counsel patients about e-cigarette usage and the potential for nicotine addiction,” Dr. McAneny said. she added.
The American Heart Association expressed support for the surgeon general’s call as well.
“That the U.S. Surgeon General is calling teen vaping an ‘epidemic’ should seize the attention of elected officials and the community of organizations working to protect the health of our nation’s children. We commend Surgeon General Adams, Commissioner [Adam] Gottlieb and Secretary [Alex M.] Azar for marshaling parents, educators, health providers, and communities to apply proven methods to overcome the epidemic of e-cigarette use,” Nancy Brown, CEO of the AHA, said in a Dec. 18 statement.
“But more must be done in the face of rapidly rising e-cigarette use among youth. The FDA’s recent announcement that it plans to restrict marketing and sales of flavored tobacco products must be followed by immediate, concrete action that sends an unmistakable message that the tobacco industry’s relentless targeting of our nation’s children will no longer be tolerated,” she emphasized.
View the surgeon general’s video message and access additional e-cigarette information here.
U.S. Surgeon General Jerome Adams, MD, responded Dec. 18 to recent data showing a sharp increase in the use of nicotine-based e-cigarette products among American teens with an urgent call to action.
“I, Surgeon General of the United States Public Health Service, [Vice Admiral] Jerome Adams, am emphasizing the importance of protecting our children from a lifetime of nicotine addiction and associated health risks by immediately addressing the epidemic of youth e-cigarette use,” Dr. Adams said in an advisory. “The recent surge in e-cigarette use among youth, which has been fueled by new types of e-cigarettes that have recently entered the market, is a cause for great concern. We must take action now to protect the health of our nation’s young people.”
The surgeon general’s advisory emphasized that e-cigarette products are not harmless and that, in addition to potentially addictive nicotine, many products contain other dangerous substances, including heavy metals, volatile organic compounds, and ultrafine particles that can affect the lungs. In addition, some e-cigarette products contain potentially harmful chemicals used to add flavoring.
The complete advisory includes information for parents, teachers, and clinicians about the details of current e-cigarette products and strategies for working to reduce their use among teens.
The American Medical Association expressed support of the surgeon general’s call to action.
“The only way to prevent another generation from developing nicotine dependence is to continue to raise awareness that e-cigarettes are harmful, powerfully addictive, and can often lead young people to smoke conventional cigarettes. E-cigarettes have the potential to undermine the public health gains that have been made over the years in combating the smoking epidemic,” Barbara L. McAneny, MD, president of the AMA, said in the statement.
“Recognizing the use of e-cigarettes and vaping as an urgent public health epidemic, the AMA has adopted numerous policies in recent years aimed at preventing youth access to these harmful tobacco products. In line with the surgeon general’s advisory, the AMA also has existing policy urging physicians to educate themselves about e-cigarettes and be prepared to counsel patients about e-cigarette usage and the potential for nicotine addiction,” Dr. McAneny said. she added.
The American Heart Association expressed support for the surgeon general’s call as well.
“That the U.S. Surgeon General is calling teen vaping an ‘epidemic’ should seize the attention of elected officials and the community of organizations working to protect the health of our nation’s children. We commend Surgeon General Adams, Commissioner [Adam] Gottlieb and Secretary [Alex M.] Azar for marshaling parents, educators, health providers, and communities to apply proven methods to overcome the epidemic of e-cigarette use,” Nancy Brown, CEO of the AHA, said in a Dec. 18 statement.
“But more must be done in the face of rapidly rising e-cigarette use among youth. The FDA’s recent announcement that it plans to restrict marketing and sales of flavored tobacco products must be followed by immediate, concrete action that sends an unmistakable message that the tobacco industry’s relentless targeting of our nation’s children will no longer be tolerated,” she emphasized.
View the surgeon general’s video message and access additional e-cigarette information here.
Heavy menstrual bleeding in teens often linked to bleeding disorders
Over one-third of adolescents presenting with heavy menstrual bleeding were diagnosed with a bleeding disorder after screening, according to results of a retrospective study.
The high incidence of bleeding disorders detected argues for routine screening of adolescents with heavy menstrual bleeding (HMB), Brooke O’Brien, MD, of the University of Queensland, Brisbane, Australia, and her colleagues wrote in the Journal of Pediatric & Adolescent Gynecology.
“These findings support comprehensive and systematic hemostatic evaluation in adolescents with HMB,” Dr. O’Brien and her colleagues wrote. “A higher level of awareness of bleeding disorders as a cause for HMB in adolescence, especially [von Willebrand disease] and platelet function disorders, is needed and close multidisciplinary collaboration between the pediatric and adolescent gynecologist and hematologist in a specialized tertiary center should be established in the management of these patients.”
In their study, Dr. O’Brien and her colleagues retrospectively evaluated 124 adolescents with HMB at a pediatric and adolescent gynecology tertiary care center between July 2007 and July 2017. Of these, 77 patients (62.1%) underwent screening for blood disorders.
The researchers found 27 adolescents overall were diagnosed with a blood disorder, which consisted of 35.0% of patients screened and 21.7% of all patients studied. Specifically, 14 of 27 patients (51.6%) screened were diagnosed with von Willebrand disease, 9 of 27 patients (33.3%) screened were found to have inherited platelet function disorders, 3 of 27 patients (11.1%) had inherited or acquired thrombocytopenia, and 1 of 27 patients (3.7%) had factor IX deficiency. The researchers also screened for iron deficiency and/or anemia and found 53 of 107 patients (49.5%) who were screened received a diagnosis, and 19 of 27 patients (70.3%) who were diagnosed with a bleeding disorder also had iron deficiency and/or anemia.
“In adolescents who are already known to have a bleeding disorder, consultation with a pediatric gynecologist and/or hematologist prior to menarche may be helpful to outline abnormal patterns of menstrual bleeding and to discuss options of treatment in the event of heavy menstrual bleeding,” Dr. O’Brien and her colleagues wrote.
Potential limitations in the study include the refractory nature of referrals at a tertiary care center potentially overestimating the prevalence of HMB in this population as well as the study’s retrospective design when investigating and measuring heavy menstrual bleeding, but researchers noted patients were reviewed and classified by a specialist pediatric hematologist.
The authors reported no relevant conflicts of interest.
SOURCE: O’Brien B et al. J Pediatr Adolesc Gynecol. 2018 Nov 22. doi: 10.1016/j.jpag.2018.11.005.
Over one-third of adolescents presenting with heavy menstrual bleeding were diagnosed with a bleeding disorder after screening, according to results of a retrospective study.
The high incidence of bleeding disorders detected argues for routine screening of adolescents with heavy menstrual bleeding (HMB), Brooke O’Brien, MD, of the University of Queensland, Brisbane, Australia, and her colleagues wrote in the Journal of Pediatric & Adolescent Gynecology.
“These findings support comprehensive and systematic hemostatic evaluation in adolescents with HMB,” Dr. O’Brien and her colleagues wrote. “A higher level of awareness of bleeding disorders as a cause for HMB in adolescence, especially [von Willebrand disease] and platelet function disorders, is needed and close multidisciplinary collaboration between the pediatric and adolescent gynecologist and hematologist in a specialized tertiary center should be established in the management of these patients.”
In their study, Dr. O’Brien and her colleagues retrospectively evaluated 124 adolescents with HMB at a pediatric and adolescent gynecology tertiary care center between July 2007 and July 2017. Of these, 77 patients (62.1%) underwent screening for blood disorders.
The researchers found 27 adolescents overall were diagnosed with a blood disorder, which consisted of 35.0% of patients screened and 21.7% of all patients studied. Specifically, 14 of 27 patients (51.6%) screened were diagnosed with von Willebrand disease, 9 of 27 patients (33.3%) screened were found to have inherited platelet function disorders, 3 of 27 patients (11.1%) had inherited or acquired thrombocytopenia, and 1 of 27 patients (3.7%) had factor IX deficiency. The researchers also screened for iron deficiency and/or anemia and found 53 of 107 patients (49.5%) who were screened received a diagnosis, and 19 of 27 patients (70.3%) who were diagnosed with a bleeding disorder also had iron deficiency and/or anemia.
“In adolescents who are already known to have a bleeding disorder, consultation with a pediatric gynecologist and/or hematologist prior to menarche may be helpful to outline abnormal patterns of menstrual bleeding and to discuss options of treatment in the event of heavy menstrual bleeding,” Dr. O’Brien and her colleagues wrote.
Potential limitations in the study include the refractory nature of referrals at a tertiary care center potentially overestimating the prevalence of HMB in this population as well as the study’s retrospective design when investigating and measuring heavy menstrual bleeding, but researchers noted patients were reviewed and classified by a specialist pediatric hematologist.
The authors reported no relevant conflicts of interest.
SOURCE: O’Brien B et al. J Pediatr Adolesc Gynecol. 2018 Nov 22. doi: 10.1016/j.jpag.2018.11.005.
Over one-third of adolescents presenting with heavy menstrual bleeding were diagnosed with a bleeding disorder after screening, according to results of a retrospective study.
The high incidence of bleeding disorders detected argues for routine screening of adolescents with heavy menstrual bleeding (HMB), Brooke O’Brien, MD, of the University of Queensland, Brisbane, Australia, and her colleagues wrote in the Journal of Pediatric & Adolescent Gynecology.
“These findings support comprehensive and systematic hemostatic evaluation in adolescents with HMB,” Dr. O’Brien and her colleagues wrote. “A higher level of awareness of bleeding disorders as a cause for HMB in adolescence, especially [von Willebrand disease] and platelet function disorders, is needed and close multidisciplinary collaboration between the pediatric and adolescent gynecologist and hematologist in a specialized tertiary center should be established in the management of these patients.”
In their study, Dr. O’Brien and her colleagues retrospectively evaluated 124 adolescents with HMB at a pediatric and adolescent gynecology tertiary care center between July 2007 and July 2017. Of these, 77 patients (62.1%) underwent screening for blood disorders.
The researchers found 27 adolescents overall were diagnosed with a blood disorder, which consisted of 35.0% of patients screened and 21.7% of all patients studied. Specifically, 14 of 27 patients (51.6%) screened were diagnosed with von Willebrand disease, 9 of 27 patients (33.3%) screened were found to have inherited platelet function disorders, 3 of 27 patients (11.1%) had inherited or acquired thrombocytopenia, and 1 of 27 patients (3.7%) had factor IX deficiency. The researchers also screened for iron deficiency and/or anemia and found 53 of 107 patients (49.5%) who were screened received a diagnosis, and 19 of 27 patients (70.3%) who were diagnosed with a bleeding disorder also had iron deficiency and/or anemia.
“In adolescents who are already known to have a bleeding disorder, consultation with a pediatric gynecologist and/or hematologist prior to menarche may be helpful to outline abnormal patterns of menstrual bleeding and to discuss options of treatment in the event of heavy menstrual bleeding,” Dr. O’Brien and her colleagues wrote.
Potential limitations in the study include the refractory nature of referrals at a tertiary care center potentially overestimating the prevalence of HMB in this population as well as the study’s retrospective design when investigating and measuring heavy menstrual bleeding, but researchers noted patients were reviewed and classified by a specialist pediatric hematologist.
The authors reported no relevant conflicts of interest.
SOURCE: O’Brien B et al. J Pediatr Adolesc Gynecol. 2018 Nov 22. doi: 10.1016/j.jpag.2018.11.005.
FROM THE JOURNAL OF PEDIATRIC & ADOLESCENT GYNECOLOGY
Key clinical point: More than one-third of adolescents with heavy menstrual bleeding were diagnosed with a bleeding disorder.
Major finding: After screening, 35% of women with heavy menstrual bleeding had a bleeding disorder; over half of those screened had von Willebrand disease.
Study details: A retrospective study of 124 adolescents at the Queensland Paediatric and Adolescent Gynaecology Service between July 2007 and July 2017.
Disclosures: The authors reported no relevant conflicts of interest.
Source: O’Brien B et al. J Pediatr Adolesc Gynecol. 2018 Nov 22 . doi: 10.1016/j.jpag.2018.11.005.
Teenagers with epilepsy may benefit from depression screening
NEW ORLEANS – Referral to a mental health provider is adequate for most patients with moderately severe symptoms of depression, but some patients may require active intervention during the clinical visit, said the researchers.
“We know that depression is more common in people with epilepsy, compared to the general population, but there is less information about depression in children and teens than adults, and little is known about the factors that increase the likelihood of depressive symptoms,” said Hillary Thomas, PhD, a pediatric psychologist at Children’s Medical Center in Dallas. “Depression screening should be routine at epilepsy treatment centers and can identify children and teens who would benefit from intervention.”
Following 2015 guidelines from the American Academy of Neurology, the Comprehensive Epilepsy Center at Children’s Health System in Dallas developed a behavioral health screening protocol for teens with epilepsy. The center aims to identify patients with depressive symptoms and ensure that they are referred to appropriate behavioral health practitioners. Clinicians also review the screening data and seizure variables for their potential implications for clinical care. Researchers at the center also seek to elucidate the relationship between depressive symptoms and seizure diagnosis and treatment.
As part of the protocol, Dr. Thomas and her colleagues administer the Patient Health Questionnaire-9 (adolescent version) to all patients aged 15-18 years during their visit to the epilepsy clinic. Patients with intellectual disability or other factors that prevent them from providing valid responses are excluded. If a patient’s PHQ-9 score indicates at least moderately severe depressive symptoms, or if he or she reports suicidal ideation, clinicians follow a specific response protocol that includes providing referrals, encouraging follow-up with the patient’s current mental health provider, and obtaining a suicide risk assessment from a psychologist or social worker. After the screener is completed, clinicians retrieve demographic and clinical data (e.g., seizure diagnosis, medication, number of clinic or emergency department visits) from the patient’s medical record and include them in a database for subsequent analysis.
Dr. Thomas and her colleagues presented data from 394 youth with epilepsy whom they had screened. Patients’ mean age was 16 years, and half of the population was female. The study population had rates of depression similar to those identified in previous studies, said Dr. Thomas. Approximately 87% of patients had minimal or mild depressive symptoms, and 8% had moderately severe depressive symptoms. Furthermore, 5% of the patients reported suicidal ideation or previous suicide attempt. Several of the patients with suicidal ideation had a current mental health provider, and the others required an in-clinic risk assessment. Overall, 13% of the population required behavioral health referral or intervention. When the researchers conducted chi-squared analysis, they found no significant association between seizure type and depression severity.
“Our results don’t mean that only 13% of the teens with epilepsy had depressive symptoms,” said Susan Arnold, MD, director of the Comprehensive Epilepsy Center and a coauthor of the study. “They indicate the significant percentage of teens whose level of depressive symptoms warranted behavioral health referrals or further evaluation or even intervention during a clinic visit. Health care providers need to be vigilant about continually screening children and teens for depression.” As part of each patient’s comprehensive care, epilepsy treatment centers should provide psychosocial teams that include social workers or psychologists, she added.
The investigators plan to continue analyzing the data for specific depression symptoms that are most common in teens. These symptoms could be the basis for developing additional resources for families, such as lists of warning signs and guides to symptom management, as well as group therapy and support groups.
SOURCE: Thomas HM et al. Abstract 1.388.
NEW ORLEANS – Referral to a mental health provider is adequate for most patients with moderately severe symptoms of depression, but some patients may require active intervention during the clinical visit, said the researchers.
“We know that depression is more common in people with epilepsy, compared to the general population, but there is less information about depression in children and teens than adults, and little is known about the factors that increase the likelihood of depressive symptoms,” said Hillary Thomas, PhD, a pediatric psychologist at Children’s Medical Center in Dallas. “Depression screening should be routine at epilepsy treatment centers and can identify children and teens who would benefit from intervention.”
Following 2015 guidelines from the American Academy of Neurology, the Comprehensive Epilepsy Center at Children’s Health System in Dallas developed a behavioral health screening protocol for teens with epilepsy. The center aims to identify patients with depressive symptoms and ensure that they are referred to appropriate behavioral health practitioners. Clinicians also review the screening data and seizure variables for their potential implications for clinical care. Researchers at the center also seek to elucidate the relationship between depressive symptoms and seizure diagnosis and treatment.
As part of the protocol, Dr. Thomas and her colleagues administer the Patient Health Questionnaire-9 (adolescent version) to all patients aged 15-18 years during their visit to the epilepsy clinic. Patients with intellectual disability or other factors that prevent them from providing valid responses are excluded. If a patient’s PHQ-9 score indicates at least moderately severe depressive symptoms, or if he or she reports suicidal ideation, clinicians follow a specific response protocol that includes providing referrals, encouraging follow-up with the patient’s current mental health provider, and obtaining a suicide risk assessment from a psychologist or social worker. After the screener is completed, clinicians retrieve demographic and clinical data (e.g., seizure diagnosis, medication, number of clinic or emergency department visits) from the patient’s medical record and include them in a database for subsequent analysis.
Dr. Thomas and her colleagues presented data from 394 youth with epilepsy whom they had screened. Patients’ mean age was 16 years, and half of the population was female. The study population had rates of depression similar to those identified in previous studies, said Dr. Thomas. Approximately 87% of patients had minimal or mild depressive symptoms, and 8% had moderately severe depressive symptoms. Furthermore, 5% of the patients reported suicidal ideation or previous suicide attempt. Several of the patients with suicidal ideation had a current mental health provider, and the others required an in-clinic risk assessment. Overall, 13% of the population required behavioral health referral or intervention. When the researchers conducted chi-squared analysis, they found no significant association between seizure type and depression severity.
“Our results don’t mean that only 13% of the teens with epilepsy had depressive symptoms,” said Susan Arnold, MD, director of the Comprehensive Epilepsy Center and a coauthor of the study. “They indicate the significant percentage of teens whose level of depressive symptoms warranted behavioral health referrals or further evaluation or even intervention during a clinic visit. Health care providers need to be vigilant about continually screening children and teens for depression.” As part of each patient’s comprehensive care, epilepsy treatment centers should provide psychosocial teams that include social workers or psychologists, she added.
The investigators plan to continue analyzing the data for specific depression symptoms that are most common in teens. These symptoms could be the basis for developing additional resources for families, such as lists of warning signs and guides to symptom management, as well as group therapy and support groups.
SOURCE: Thomas HM et al. Abstract 1.388.
NEW ORLEANS – Referral to a mental health provider is adequate for most patients with moderately severe symptoms of depression, but some patients may require active intervention during the clinical visit, said the researchers.
“We know that depression is more common in people with epilepsy, compared to the general population, but there is less information about depression in children and teens than adults, and little is known about the factors that increase the likelihood of depressive symptoms,” said Hillary Thomas, PhD, a pediatric psychologist at Children’s Medical Center in Dallas. “Depression screening should be routine at epilepsy treatment centers and can identify children and teens who would benefit from intervention.”
Following 2015 guidelines from the American Academy of Neurology, the Comprehensive Epilepsy Center at Children’s Health System in Dallas developed a behavioral health screening protocol for teens with epilepsy. The center aims to identify patients with depressive symptoms and ensure that they are referred to appropriate behavioral health practitioners. Clinicians also review the screening data and seizure variables for their potential implications for clinical care. Researchers at the center also seek to elucidate the relationship between depressive symptoms and seizure diagnosis and treatment.
As part of the protocol, Dr. Thomas and her colleagues administer the Patient Health Questionnaire-9 (adolescent version) to all patients aged 15-18 years during their visit to the epilepsy clinic. Patients with intellectual disability or other factors that prevent them from providing valid responses are excluded. If a patient’s PHQ-9 score indicates at least moderately severe depressive symptoms, or if he or she reports suicidal ideation, clinicians follow a specific response protocol that includes providing referrals, encouraging follow-up with the patient’s current mental health provider, and obtaining a suicide risk assessment from a psychologist or social worker. After the screener is completed, clinicians retrieve demographic and clinical data (e.g., seizure diagnosis, medication, number of clinic or emergency department visits) from the patient’s medical record and include them in a database for subsequent analysis.
Dr. Thomas and her colleagues presented data from 394 youth with epilepsy whom they had screened. Patients’ mean age was 16 years, and half of the population was female. The study population had rates of depression similar to those identified in previous studies, said Dr. Thomas. Approximately 87% of patients had minimal or mild depressive symptoms, and 8% had moderately severe depressive symptoms. Furthermore, 5% of the patients reported suicidal ideation or previous suicide attempt. Several of the patients with suicidal ideation had a current mental health provider, and the others required an in-clinic risk assessment. Overall, 13% of the population required behavioral health referral or intervention. When the researchers conducted chi-squared analysis, they found no significant association between seizure type and depression severity.
“Our results don’t mean that only 13% of the teens with epilepsy had depressive symptoms,” said Susan Arnold, MD, director of the Comprehensive Epilepsy Center and a coauthor of the study. “They indicate the significant percentage of teens whose level of depressive symptoms warranted behavioral health referrals or further evaluation or even intervention during a clinic visit. Health care providers need to be vigilant about continually screening children and teens for depression.” As part of each patient’s comprehensive care, epilepsy treatment centers should provide psychosocial teams that include social workers or psychologists, she added.
The investigators plan to continue analyzing the data for specific depression symptoms that are most common in teens. These symptoms could be the basis for developing additional resources for families, such as lists of warning signs and guides to symptom management, as well as group therapy and support groups.
SOURCE: Thomas HM et al. Abstract 1.388.
REPORTING FROM AES 2018
Key clinical point: Screening children with epilepsy regularly for depression may be advisable.
Major finding: About 13% of patients screened required referral or intervention.
Study details: Prospective study of 394 patients with epilepsy.
Disclosures: The investigators have no disclosures and received no funding for this study.
Source: Thomas HM et al. Abstract 1.388.
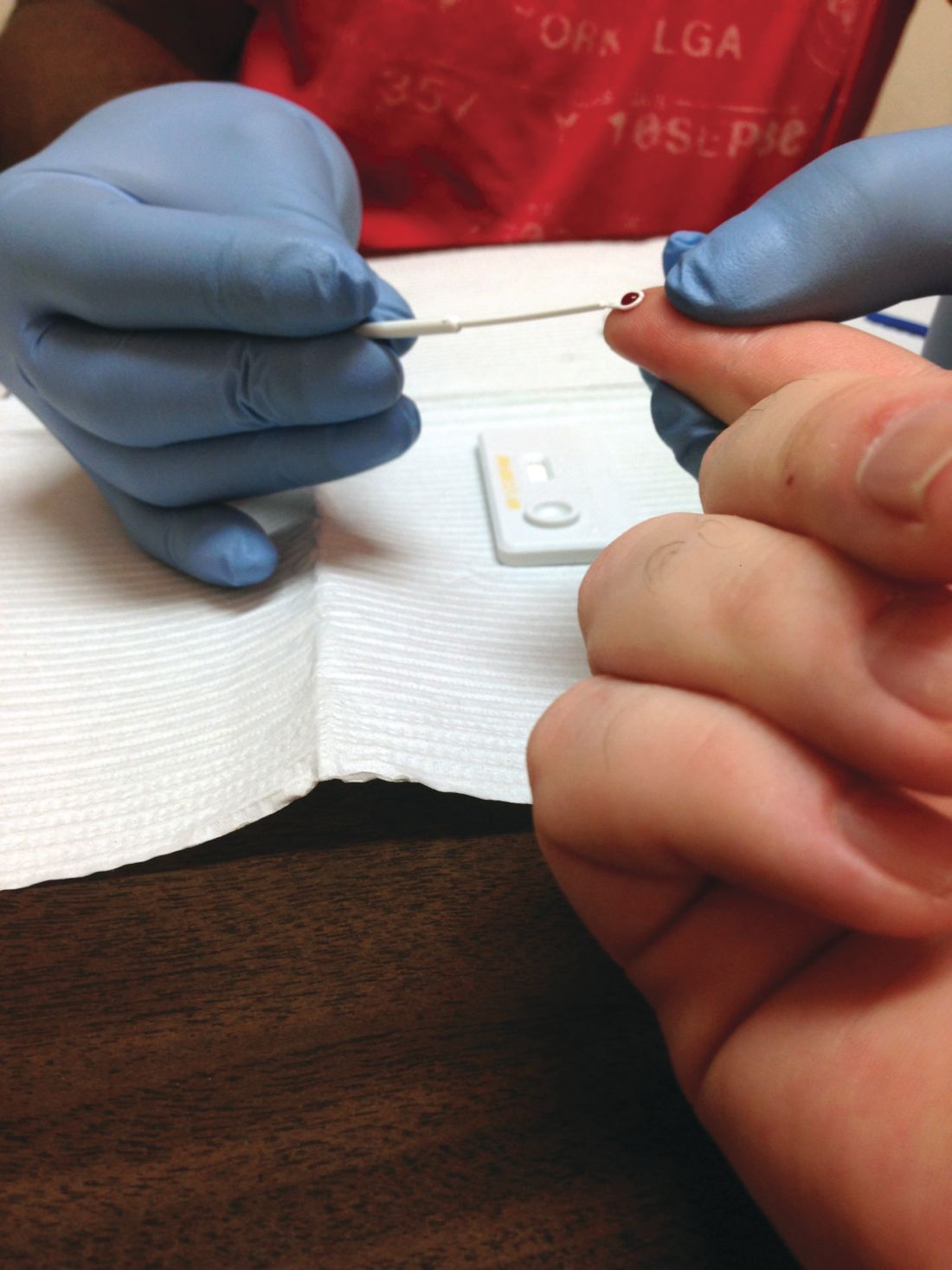
Missed HIV screening opportunities found among subsequently infected youth
In the year prior to HIV diagnosis, there were high rates of missed opportunities for HIV testing and sexual history documentation, according to a retrospective study of youth with HIV aged 14-26 years who were treated at an HIV clinic. These results demonstrate a failed need for routine HIV screening and counseling in adolescents, according to Nellie Riendeau Lazar, MPH, of Children’s Hospital of Philadelphia, and her colleagues.
The researchers retrospectively identified 301 subjects between January 2009 and April 2015 who met their study criteria. A total of 58 of these (19%) had at least one visit in the care network in the year prior to diagnosis and their entry into the adolescent HIV clinic, and they were analyzed for missed diagnosis. The adolescent HIV clinic is part of a large care network in the Philadelphia area that includes a pediatric emergency department and a tertiary care hospital. At the time of the study, there were 31 primary care sites, according to the authors.
The mean age of the subjects in the study was 17. The majority (80%) were young men, African-American (93%), and men who have sex with men (81%). There were no significant differences seen in demographics between those with and without prior visits in the health system (J Adolesc Health. 2018;63:799-802).
The 58 subjects were seen in 179 health care visits in the year prior to their diagnosis: 56% outpatient, 40% emergency department, and 4% inpatient visits. Only 59% of these visits had any documentation of sexual history and “the overwhelming majority of those noting sexual activity included no other information,” such as number of partners, sex of partners, or condom use, according to the researchers.
Among the total cohort, 183 of 301 had never had an HIV test prior to their first positive test, even though 26% had been seen in the care network in the 3 years prior to their diagnosis. Among the 58 in the missed opportunity analysis, only 48% had HIV testing, even though 88% (51) had documented symptoms in their visits that could have been consistent with acute infection.
“Our findings support the most recent guidelines from the Centers for Disease Control and Prevention, American Academy of Pediatrics (AAP), and United States Preventive Services Task Force (USPSTF), recommending routine HIV screening for all adolescents, regardless of risk,” the researchers stated. “Adolescents may not always disclose sexual activity during routine assessment, and provider level barriers limit the reach of risk-based testing algorithms,” they added.
The authors reported that they had no conflicts of interest.
SOURCE: Lazar NR et al. J Adolesc Health. 2018;63:799-802.
In the year prior to HIV diagnosis, there were high rates of missed opportunities for HIV testing and sexual history documentation, according to a retrospective study of youth with HIV aged 14-26 years who were treated at an HIV clinic. These results demonstrate a failed need for routine HIV screening and counseling in adolescents, according to Nellie Riendeau Lazar, MPH, of Children’s Hospital of Philadelphia, and her colleagues.
The researchers retrospectively identified 301 subjects between January 2009 and April 2015 who met their study criteria. A total of 58 of these (19%) had at least one visit in the care network in the year prior to diagnosis and their entry into the adolescent HIV clinic, and they were analyzed for missed diagnosis. The adolescent HIV clinic is part of a large care network in the Philadelphia area that includes a pediatric emergency department and a tertiary care hospital. At the time of the study, there were 31 primary care sites, according to the authors.
The mean age of the subjects in the study was 17. The majority (80%) were young men, African-American (93%), and men who have sex with men (81%). There were no significant differences seen in demographics between those with and without prior visits in the health system (J Adolesc Health. 2018;63:799-802).
The 58 subjects were seen in 179 health care visits in the year prior to their diagnosis: 56% outpatient, 40% emergency department, and 4% inpatient visits. Only 59% of these visits had any documentation of sexual history and “the overwhelming majority of those noting sexual activity included no other information,” such as number of partners, sex of partners, or condom use, according to the researchers.
Among the total cohort, 183 of 301 had never had an HIV test prior to their first positive test, even though 26% had been seen in the care network in the 3 years prior to their diagnosis. Among the 58 in the missed opportunity analysis, only 48% had HIV testing, even though 88% (51) had documented symptoms in their visits that could have been consistent with acute infection.
“Our findings support the most recent guidelines from the Centers for Disease Control and Prevention, American Academy of Pediatrics (AAP), and United States Preventive Services Task Force (USPSTF), recommending routine HIV screening for all adolescents, regardless of risk,” the researchers stated. “Adolescents may not always disclose sexual activity during routine assessment, and provider level barriers limit the reach of risk-based testing algorithms,” they added.
The authors reported that they had no conflicts of interest.
SOURCE: Lazar NR et al. J Adolesc Health. 2018;63:799-802.
In the year prior to HIV diagnosis, there were high rates of missed opportunities for HIV testing and sexual history documentation, according to a retrospective study of youth with HIV aged 14-26 years who were treated at an HIV clinic. These results demonstrate a failed need for routine HIV screening and counseling in adolescents, according to Nellie Riendeau Lazar, MPH, of Children’s Hospital of Philadelphia, and her colleagues.
The researchers retrospectively identified 301 subjects between January 2009 and April 2015 who met their study criteria. A total of 58 of these (19%) had at least one visit in the care network in the year prior to diagnosis and their entry into the adolescent HIV clinic, and they were analyzed for missed diagnosis. The adolescent HIV clinic is part of a large care network in the Philadelphia area that includes a pediatric emergency department and a tertiary care hospital. At the time of the study, there were 31 primary care sites, according to the authors.
The mean age of the subjects in the study was 17. The majority (80%) were young men, African-American (93%), and men who have sex with men (81%). There were no significant differences seen in demographics between those with and without prior visits in the health system (J Adolesc Health. 2018;63:799-802).
The 58 subjects were seen in 179 health care visits in the year prior to their diagnosis: 56% outpatient, 40% emergency department, and 4% inpatient visits. Only 59% of these visits had any documentation of sexual history and “the overwhelming majority of those noting sexual activity included no other information,” such as number of partners, sex of partners, or condom use, according to the researchers.
Among the total cohort, 183 of 301 had never had an HIV test prior to their first positive test, even though 26% had been seen in the care network in the 3 years prior to their diagnosis. Among the 58 in the missed opportunity analysis, only 48% had HIV testing, even though 88% (51) had documented symptoms in their visits that could have been consistent with acute infection.
“Our findings support the most recent guidelines from the Centers for Disease Control and Prevention, American Academy of Pediatrics (AAP), and United States Preventive Services Task Force (USPSTF), recommending routine HIV screening for all adolescents, regardless of risk,” the researchers stated. “Adolescents may not always disclose sexual activity during routine assessment, and provider level barriers limit the reach of risk-based testing algorithms,” they added.
The authors reported that they had no conflicts of interest.
SOURCE: Lazar NR et al. J Adolesc Health. 2018;63:799-802.
FROM THE JOURNAL OF ADOLESCENT HEALTH
Key clinical point: Only 51% of youth with symptoms suggesting acute retroviral syndrome were tested.
Major finding: HIV testing was performed in only 48% of the subjects seen in the year prior to their diagnosis.
Study details: Retrospective review of subjects with HIV aged 14-26 years, comparing those with and without HIV screening within the year prior to diagnosis.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Lazar NR et al. J Adolesc Health. 2018;63:799-802.
Recognize gender expression in youth
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
It has been known for decades that sex and gender cannot be determined solely by birth anatomy and chromosomes.1 Over the past decade, the medical community has been able to better understand the biologic underpinnings of gender identity, and we are gaining a better appreciation for the diversity of gender identities and gender expressions that exist.
Gender expression can be defined as the manner in which an individual chooses to present their gender to others through physical appearance and behaviors, such as style of hair or dress, voice or movement.2 Gender nonconformity (GNC) is when an individual’s gender expression does not fully conform with societal expectations often based on an individual’s sex assigned at birth. It is important to note that gender expression is independent of gender identity and may or may not align with gender identity. For example, a person whose sex assigned at birth is female may adopt hairstyles and clothing that are considered more masculine and enjoy activities that are typically associated with masculinity (for example, sports) yet identify as female. The majority of research to date focuses most on transgender individuals, broadly defined as those whose gender identity does not fully align with the sex assigned at birth.3,4 As our understanding of gender expression and GNC expands, more research is emerging on the prevalence of gender nonconformity in youth and potential associations with various health outcomes.
Stigma, discrimination, and harassment are known to have documented effects on health. GNC youth have been shown to experience discrimination and harassment at rates higher than their gender conforming peers.5,6 A recent study by Lowry et al. sought to examine the association between GNC and indicators of mental distress and substance use in adolescents.7 The authors analyzed a subset of cross-sectional data from more than 6,000 youth who had participated in the Youth Risk Behavior Surveillance–United States, 2015 (YRBS) in three large urban school districts (two in California and one in Florida). In addition to the standard YRBS questions, students at these three school districts were asked about their gender expression using the following question: “A person’s appearance style, dress, or the way they walk or talk may affect how people describe them. How do you think people at your school would describe you?” Based on responses, youth were categorized on a 7-point GNC scale with 1 being most gender conforming (a very feminine female student or very masculine male student) to 7 being most GNC (a very masculine female student or a very feminine male student). The study sample was ethnically diverse with 16% of students identifying as white non-Hispanic, 19% identifying as black non-Hispanic, and 55% identifying as Hispanic of any race.
In the study population, approximately one in five students reported either moderate (students who described themselves as equally feminine and masculine) or high (female students who described themselves as very/mostly/somewhat masculine or male students who described themselves as very/mostly/somewhat feminine) levels of GNC. Among female students, moderate GNC was significantly associated with feeling sad and hopeless, seriously considering attempting suicide, and making a suicide plan. However, in female students substance use was not associated with GNC. Among male students, suicidal thoughts, plans, and attempts all demonstrated a linear increase with GNC, with the greatest prevalence occurring in male students expressing high levels of GNC. Prevalence of substance use, specifically nonmedical use of prescription drugs, cocaine use, methamphetamine use, heroin use, and intravenous drug also was associated with high GNC in male students. Study authors hypothesize that these differences occur because GNC male youth experience more overt harassment, compared with GNC female youth, but further study is needed.
Our understanding of the diversity of gender expressions present in youth populations continues to evolve. Findings from this study add to a growing body of evidence demonstrating a relatively high prevalence of GNC in youth populations, and potential health disparities these youth may face. This study underscores the need for continued study in this area. Family support and acceptance have been demonstrated to be strong protective factors for transgender-, lesbian-, and gay-identified youth. Studies identifying protective factors for GNC youth are needed.4
As health care providers, we need to continue to ask patients and families about gender identity and be aware of gender expression. When youth present as GNC, we should recognize that they may be at increased risk and, in addition to assessing overall mental health and risk for substance use, also assess for degree of social/familial support and potential stressors.4 We also should continue to advocate for support systems within schools sensitive to the needs of GNC students, as these may be a potential avenue to improve overall mental health for students. It is important to continue to expand our understanding of the diverse gender identities and expressions of the youth we serve. This hopefully will allow us to identify not only potential risk factors and health disparities, but also protective factors that can help better inform the development of effective interventions so all youth can reach their full potential.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at the Ohio State University, both in Columbus. Email her at [email protected].
References
1. “WPATH (World Professional Association of Transgender Health) Board Responds to Federal Effort to Redefine Gender,” press release, Oct. 23, 2018.
2. “LGBTQ+ Definitions” at Trans Student Educational Resources.3. J Sex Res. 2013;50(3-4):299-317.
4. JAMA Pediatr. 2018 Nov 1;172(11):1010-1.
5. Psychol Sex Orientat Gend Divers. 2016 Dec;3(4):489-98.
6. J Adolesc Health. 2016; 58(2)(supple):S1-2.
7. JAMA Pediatr. 2018 Nov;172(11):1020-8.
Draft guidelines advise HIV screening for most teens and adults
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Sandy Hook Promise: Four programs help people recognize signs of a threat
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
ORLANDO – “The caretaker of all living things” – that was the good-natured moniker 7-year-old Daniel Barden had earned from his family – according to his dad, Mark Barden. Daniel would pick up black ants and take them outside “to be with their families,” even when the ant bit his fingers.
A walk down the sidewalk after a rain would take three times longer than it should because Daniel stopped to pick up every worm on the pavement and put it in the grass, lest it dry out in the sun, Mr. Barden said with a chuckle at the annual meeting of the American Academy of Pediatrics.
Daniel was his youngest and full of pure joy, Mr. Barden said, but that ended with his son’s murder during the Sandy Hook Elementary mass shooting Dec. 14, 2012. To honor his son and work to reduce the likelihood of similar mass shootings, Mr. Barden, now the managing director of Sandy Hook Promise in Newtown, Conn., shared with the pediatrician audience the work of the organization formed by Sandy Hook parents to attempt to prevent gun violence before it happens.
“We’re moms and dads and a couple of families who have lost loved ones in that tragedy, and we are growing as an organization,” Mr. Barden said. “Our basic, most fundamental objective is to prevent other families from living with the pain I will live with for the rest of my life.”
Their mission involves “creating a culture engaged and committed to identifying, intervening, and getting help for individuals who may be at risk of hurting themselves or others,” Mr. Barden said.
Sandy Hook Promise accomplishes this goal by educating and empowering communities through their four programs: Start with Hello, SOS Suicide Prevention Program, SaySomething, and Safety Assessment & Intervention. The organization delivers these programs through multiple platforms, including national and local trainers, digital curriculum downloads, interactive online training videos, and using multilingual presenters and English and Spanish materials.
The organization also especially works with schools and student’s clubs to change their culture and feel empowered to speak up and do their part to prevent gun violence too.
These programs resulted from extensive qualitative and quantitative research that Sandy Hook Promise conducted after the shooting with academic researchers, law enforcement, educators, school administrators, mental health professionals, and social movement experts.
“As we see these stories play themselves out over and over again, we start to reveal the story of somebody who didn’t just snap overnight,” Mr. Barden said. Signs that a person may be at risk for committing mass violence include suicidality, preoccupation with weapons, talking about committing violent acts, and general signs of depression and anxiety. “If we can train people how to not only recognize but to look for those signs, we can make a sustainable difference,” he said.
Most mass shootings are planned at least 6 months in advance, he said. About 80% of school shooters tell someone about their plans, and 69% tell multiple people. Similarly, up to 70% of people who die by suicide tell someone they plan to do it or give some other warning sign.
Further, more than a third of violent threats and bullying occurs electronically, so students are well equipped to watch for the signs and report them if they know how and feel comfortable doing so.
Mr. Barden outlined the goals of each of the four Sandy Hook Promise programs.
Start With Hello
This program “teaches youth how to identify and minimize social isolation, marginalization, and rejection in order to create an inclusive, connected community,” Mr. Barden explained. The goals of the program are to reduce bullying, foster socialization, increase engagement, and change a culture from within.
SOS Signs of Suicide
This is Sandy Hook Promise’s newest program and is built on a program developed by the Federal Bureau of Investigation following the Virginia Tech shooting and adapted for school-based applications.
“It also develops a multidisciplinary team within the school who acts as various touch points who know how to recognize a potential warning sign and then triage that information and take steps to get to the root cause of that behavior and not just bandage the wound,” Mr. Barden explained.
SaySomething
The organization’s flagship program does the most to recruit student involvement in recognizing the signs of a potential threat, particularly in social media, and report the individual and their behavior to a trusted adult or through Sandy Hook Promise’s Anonymous Reporting System.
“The kids take this one, and they run with it and do amazing things with it,” Mr. Barden said, noting that it particularly helps students recognize warning signs on social media. “We have growing evidence of kids following this model, and we’ve already prevented mass shootings and numerous suicides with this.”
Safety Assessment & Intervention (SAI) program
This program “trains a multidisciplinary team how to identify, assess, and respond to threats and observed at-risk behaviors,” Mr. Barden said. SAI aims to create a safer, more open school environment with less violence, bullying, and threats. That includes reducing educators’ fear and anxiety, and leading students to have a more positive view of teachers and staff.
Students can report tips to the Anonymous Reporting System through the website, calling the hot line or via a free mobile app. Regardless of the method, the anonymous tips go to a 24/7 multilingual crisis center and, if needed, law enforcement. The crisis center contacts the appropriate school official via text, email, or a phone call, and the case is tracked in real time until it’s addressed, resolved, and closed.
All of these programs are freely available to any school or institution who wants to use them, Mr. Barden said, because the organization does not want cost to get in the way of any school or community that is taking advantage of tools to reduce the risk of violence.
In fact, more than 3.5 million youth and adults in more than 7,000 schools in every state have been trained in these programs, helping hundreds of youth access mental health and wellness help, he said. The program has reduced truancy, bullying, and other forms of violence and victimization, and it has intervened in multiple school shooting plans across the United States.
Mr. Barden wrapped up his address with his gratitude for pediatricians’ willingness to be partners in reducing gun violence.
“I want to tell you how much it means to me that you took the time to come here and listen to my story and the work I’m doing,” he said, “and how proud I am to be able to share it with you, and how proud I am to be able to honor that little kid who truly was the caretaker of all living things and to continue that spirit in his honor and in his absence.”
EXPERT ANALYSIS FROM AAP 18
FDA aims to squash youth vaping, smoking
The Food and Drug Administration once again has upped the ante in its war on youth smoking and vaping.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
First and foremost, the FDA wants to reduce the lure of e-cigarettes by limiting the variety of flavored products for sale in retail outlets. Under the proposal unveiled Nov. 15, only electronic nicotine delivery systems (ENDS) that are unflavored or have tobacco, mint, or menthol flavors would be widely available. Flavored products – think cherry, cotton candy, and mango – would be sold in age-restricted environments, such as stand-alone tobacco retailers like vape shops. The FDA also seeks more stringent enforcement of age verification on ENDS products sold online.
The proposal also would reexamine regulations governing flavored cigars, with the possible aim of banning them.
“These efforts to address flavors and protect youth would dramatically impact the ability of American kids to access tobacco products that we know are both appealing and addicting,” Dr. Gottlieb said in a statement. “This policy framework reflects a redoubling of the FDA’s efforts to protect kids from all nicotine-containing products.”
In a move that seems to be aimed at youth-oriented products like Juul, the FDA will be seeking to remove from the market any ENDS product that is marketed specifically to young people.
Finally, the FDA intends to pursue regulation that would ban menthol from combustible tobacco products.
“I believe these menthol-flavored products represent one of the most common and pernicious routes by which kids initiate on combustible cigarettes,” Dr. Gottlieb said. “The menthol serves to mask some of the unattractive features of smoking that might otherwise discourage a child from smoking. Moreover, I believe that menthol products disproportionately and adversely affect underserved communities. And as a matter of public health, they exacerbate troubling disparities in health related to race and socioeconomic status.”
The policy shift comes as the Centers for Disease Control and Prevention released data from the 2018 National Youth Tobacco Survey showing that use of e-cigarettes among high schoolers is on the rise, growing from 1.5% in 2011 to 20.8% in 2018. Middle schoolers saw use over the same time period increase from 0.6% to 4.9%.
The rise of current use of e-cigarettes was enough to reverse a declining trend in overall tobacco use in recent years between 2015 and 2017.
“FDA’s enforcement efforts and policy framework would restrict access to most flavored e-cigarettes and limit the chances of youth beginning to use these products, while ensuring the products are available to adult smokers as an alternative to combustible cigarettes,” Alex M. Azar II, secretary of the Department of Health & Human Services, said in a statement supporting the FDA’s efforts. “Our obligation at HHS is always to the public health, and we believe FDA’s goals strike the right public health balance in addressing the multifaceted challenge we have before us today.”
Under Dr. Gottlieb, the FDA has been aggressively pursuing ways to reduce tobacco consumption, targeting both ENDS and combustible tobacco regulations in an effort to limit nicotine exposure and reduce the number of people addicted to nicotine and the health issues that come with it.
The American College of Cardiology voiced its support of the FDA’s actions.
“The FDA’s announcement restricting the sale of flavored e-cigarettes and other tobacco products shows they are ready to do their part in making tobacco products less available to our children,” ACC President C. Michael Valentine, MD, said in a statement, adding that the medical community needs to continue to do its part to make sure tobacco use continues to decline, especially in the nonadult population.
The FDA proposals were published as part of an advance notice of proposed rulemaking in the Federal Register. Comments can be made at www.regulations.gov through June 19.
The Food and Drug Administration once again has upped the ante in its war on youth smoking and vaping.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
First and foremost, the FDA wants to reduce the lure of e-cigarettes by limiting the variety of flavored products for sale in retail outlets. Under the proposal unveiled Nov. 15, only electronic nicotine delivery systems (ENDS) that are unflavored or have tobacco, mint, or menthol flavors would be widely available. Flavored products – think cherry, cotton candy, and mango – would be sold in age-restricted environments, such as stand-alone tobacco retailers like vape shops. The FDA also seeks more stringent enforcement of age verification on ENDS products sold online.
The proposal also would reexamine regulations governing flavored cigars, with the possible aim of banning them.
“These efforts to address flavors and protect youth would dramatically impact the ability of American kids to access tobacco products that we know are both appealing and addicting,” Dr. Gottlieb said in a statement. “This policy framework reflects a redoubling of the FDA’s efforts to protect kids from all nicotine-containing products.”
In a move that seems to be aimed at youth-oriented products like Juul, the FDA will be seeking to remove from the market any ENDS product that is marketed specifically to young people.
Finally, the FDA intends to pursue regulation that would ban menthol from combustible tobacco products.
“I believe these menthol-flavored products represent one of the most common and pernicious routes by which kids initiate on combustible cigarettes,” Dr. Gottlieb said. “The menthol serves to mask some of the unattractive features of smoking that might otherwise discourage a child from smoking. Moreover, I believe that menthol products disproportionately and adversely affect underserved communities. And as a matter of public health, they exacerbate troubling disparities in health related to race and socioeconomic status.”
The policy shift comes as the Centers for Disease Control and Prevention released data from the 2018 National Youth Tobacco Survey showing that use of e-cigarettes among high schoolers is on the rise, growing from 1.5% in 2011 to 20.8% in 2018. Middle schoolers saw use over the same time period increase from 0.6% to 4.9%.
The rise of current use of e-cigarettes was enough to reverse a declining trend in overall tobacco use in recent years between 2015 and 2017.
“FDA’s enforcement efforts and policy framework would restrict access to most flavored e-cigarettes and limit the chances of youth beginning to use these products, while ensuring the products are available to adult smokers as an alternative to combustible cigarettes,” Alex M. Azar II, secretary of the Department of Health & Human Services, said in a statement supporting the FDA’s efforts. “Our obligation at HHS is always to the public health, and we believe FDA’s goals strike the right public health balance in addressing the multifaceted challenge we have before us today.”
Under Dr. Gottlieb, the FDA has been aggressively pursuing ways to reduce tobacco consumption, targeting both ENDS and combustible tobacco regulations in an effort to limit nicotine exposure and reduce the number of people addicted to nicotine and the health issues that come with it.
The American College of Cardiology voiced its support of the FDA’s actions.
“The FDA’s announcement restricting the sale of flavored e-cigarettes and other tobacco products shows they are ready to do their part in making tobacco products less available to our children,” ACC President C. Michael Valentine, MD, said in a statement, adding that the medical community needs to continue to do its part to make sure tobacco use continues to decline, especially in the nonadult population.
The FDA proposals were published as part of an advance notice of proposed rulemaking in the Federal Register. Comments can be made at www.regulations.gov through June 19.
The Food and Drug Administration once again has upped the ante in its war on youth smoking and vaping.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” FDA Commissioner Scott Gottlieb, MD, said in a statement.
First and foremost, the FDA wants to reduce the lure of e-cigarettes by limiting the variety of flavored products for sale in retail outlets. Under the proposal unveiled Nov. 15, only electronic nicotine delivery systems (ENDS) that are unflavored or have tobacco, mint, or menthol flavors would be widely available. Flavored products – think cherry, cotton candy, and mango – would be sold in age-restricted environments, such as stand-alone tobacco retailers like vape shops. The FDA also seeks more stringent enforcement of age verification on ENDS products sold online.
The proposal also would reexamine regulations governing flavored cigars, with the possible aim of banning them.
“These efforts to address flavors and protect youth would dramatically impact the ability of American kids to access tobacco products that we know are both appealing and addicting,” Dr. Gottlieb said in a statement. “This policy framework reflects a redoubling of the FDA’s efforts to protect kids from all nicotine-containing products.”
In a move that seems to be aimed at youth-oriented products like Juul, the FDA will be seeking to remove from the market any ENDS product that is marketed specifically to young people.
Finally, the FDA intends to pursue regulation that would ban menthol from combustible tobacco products.
“I believe these menthol-flavored products represent one of the most common and pernicious routes by which kids initiate on combustible cigarettes,” Dr. Gottlieb said. “The menthol serves to mask some of the unattractive features of smoking that might otherwise discourage a child from smoking. Moreover, I believe that menthol products disproportionately and adversely affect underserved communities. And as a matter of public health, they exacerbate troubling disparities in health related to race and socioeconomic status.”
The policy shift comes as the Centers for Disease Control and Prevention released data from the 2018 National Youth Tobacco Survey showing that use of e-cigarettes among high schoolers is on the rise, growing from 1.5% in 2011 to 20.8% in 2018. Middle schoolers saw use over the same time period increase from 0.6% to 4.9%.
The rise of current use of e-cigarettes was enough to reverse a declining trend in overall tobacco use in recent years between 2015 and 2017.
“FDA’s enforcement efforts and policy framework would restrict access to most flavored e-cigarettes and limit the chances of youth beginning to use these products, while ensuring the products are available to adult smokers as an alternative to combustible cigarettes,” Alex M. Azar II, secretary of the Department of Health & Human Services, said in a statement supporting the FDA’s efforts. “Our obligation at HHS is always to the public health, and we believe FDA’s goals strike the right public health balance in addressing the multifaceted challenge we have before us today.”
Under Dr. Gottlieb, the FDA has been aggressively pursuing ways to reduce tobacco consumption, targeting both ENDS and combustible tobacco regulations in an effort to limit nicotine exposure and reduce the number of people addicted to nicotine and the health issues that come with it.
The American College of Cardiology voiced its support of the FDA’s actions.
“The FDA’s announcement restricting the sale of flavored e-cigarettes and other tobacco products shows they are ready to do their part in making tobacco products less available to our children,” ACC President C. Michael Valentine, MD, said in a statement, adding that the medical community needs to continue to do its part to make sure tobacco use continues to decline, especially in the nonadult population.
The FDA proposals were published as part of an advance notice of proposed rulemaking in the Federal Register. Comments can be made at www.regulations.gov through June 19.
Despite declines in prenatal use of alcohol and cigarettes, cannabis use is on the rise
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: Greatest increase in use of cannabis over the 14 years of the study was seen during the first trimester; the increase in use of cannabis in the second and third trimesters was not significant.
Study details: A study of 12,058 pregnant women from 2002-2016.
Disclosures: The authors had no relevant financial disclosures. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
Source: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.