User login
AAP advises moderate physical, cognitive activity after sports concussion
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
according to a new clinical report from the American Academy of Pediatrics.
The update to the 2010 guidelines was needed to reflect the latest research “and it was necessary to provide this new information to guide pediatricians in evaluating and treating concussions they may see in their practice,” Mark Halstead, MD, of Washington University, St. Louis, said in an interview.
The biggest changes to the guidelines involve management of concussion, noted Dr. Halstead, who was a coauthor of the AAP clinical report. “The previous recommendation called for cognitive and physical rest, which unfortunately was interpreted as complete removal from all physical activity and limiting many other things including electronic use.
“Because of research that has been conducted since the original report, it has been shown that starting some light physical activity to increase heart rate, provided it does not worsen symptoms, can be beneficial in recovery. Also, the recommendation for complete removal of electronics and computer use has unfortunately created some issues with kids getting socially isolated,” he added.
“For better or for worse, kids are connected through their electronic devices. Removing them, with no evidence that it worsens the concussion, essentially punishes kids for their injury. We also are trying to discourage prolonged removal of kids from school,” Dr. Halstead emphasized.
The new recommendations emphasize the unique nature of sports-related concussion (SRC) from one individual to another, and the need for individualized management.
Symptoms of SRC fall into five categories, according to the guidelines: somatic, vestibular, oculomotor, cognitive, and emotional/sleep. Pediatric health care providers should rule out more severe head injuries and recognize that concussion symptoms are nonspecific and may reflect preexisting conditions, such as migraine or headache disorders, learning disorders, ADHD, mental health conditions, or sleep disorders.
Use of assessments such as the Sport Concussion Management Tool (SCAT5 for 13 years and older or Child SCAT5 for 5-12 years) can help guide clinicians, but should not be used in isolation to diagnose a concussion, the guideline authors wrote.
Strategies for injury prevention are included in the guidelines as well, such as the use of appropriate headgear. As for management, computerized neurocognitive testing can play a role in decisions regarding return to play, but should not be used in isolation.
“The biggest thing we are lacking is an objective diagnostic test to determine the presence of a concussion or its resolution,” coauthor Kody A. Moffatt, MD, of Creighton University, Omaha, Nebraska, said in an interview.
“Mandatory baseline and postinjury computerized neurocognitive testing is not recommended,” he added.
Clinicians can best manage SRC with prompt recognition and diagnosis using the available tools, followed by relative rest and return to school, then noncontact physical activities, and eventually a return to sport if appropriate.
“Most concussions in children and adolescents will resolve within 4 weeks as long as there is not additional injury to the brain during that time,” Dr. Moffat said.
More research is needed in particular about concussions in elementary and middle school children, Dr. Halstead added.
In the meantime, the take-home message to pediatricians for managing SRC is one of common sense. “Extremes of removing all stimulus from a child is not likely to get them better sooner and research suggests may take them longer to get better,” Dr. Halstead noted. “That doesn’t mean they don’t have to reduce anything, as it is important to reduce physical activity and modify school workload while recovering but we should be avoiding the blanket recommendation to ‘stay home and do nothing until you are better’ approach to concussion management.”
Dr. Halstead and Dr. Moffatt reported no relevant financial conflicts to disclose; the same was true for the other report coauthors. There was no external funding for the report.
SOURCE: Halstead M et al. Pediatrics. 2018 Nov 12. doi: 10.1542/peds.2018-3074.
FROM PEDIATRICS
USPSTF advises primary care to screen for unhealthy alcohol use
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
FROM JAMA
You have ‘unique expertise’ to treat opioid use disorder in adolescents
ORLANDO – according to a presentation at the annual meeting of the American Academy of Pediatrics.
“We pediatricians have some unique skills that can really benefit our community of teens,” said Deepa Camenga, MD, of Yale University in New Haven, Conn.
Compared with some other specialists, who may be more reluctant to prescribe buprenorphine, pediatricians are more comfortable and have systems in place to deal with issues surrounding care coordination, adolescent confidentiality, family reassurance, and managing prescriptions for chronic diseases.“We can use those same skills when we’re caring for people with opioid use disorder,” she said.
According to the DSM-5 (Diagnostic and Statistical Manual–5), there are 11 criteria for opioid use disorder based on level of physiological dependence, impaired control, social functioning, and risky use. Meeting two or three criteria constitutes mild substance use disorder, while meeting six or more criteria is associated with severe substance use disorder.
Opioid use disorder in adolescents can be characterized by milder symptoms. Adolescents also tend to be in the early stage of this chronic disease when they seek care for opioid use disorder and need to be informed about the seriousness of the disease, Dr. Camenga noted.
“There is a disconnect about the severity of their illness when they present to me,” she said. “This is a disease that we know is chronic, severe – and without treatment – is progressive. We do know it can progress and get worse, and result in death.”
Treatment options for opioid use disorder in adolescents include behavioral interventions such as residential treatment, intensive outpatient (IOP), and partial hospitalization programs and therapy, as well as pharmacologic interventions like clonidine, buprenorphine, and methadone used for detoxification. Buprenorphine/naloxone has been labeled for use by patients 18 years or older; however, three recent randomized controlled trials have studied the effects of the intervention in 16-year-old and 17-year-old patients. In the trials, there were no serious adverse events reported with support of treatment for a minimum of 12 weeks and “many providers are treating up to a year” based on data from observational studies, Dr. Camenga said. Naltrexone also has been indicated for adolescents with opioid use disorder, with feasibility seen in pilot studies.
If you are interested in providing buprenorphine for patients, you need to apply for a Drug Enforcement Administration X-waiver, have access to their state’s prescription-monitoring program, and have a network of behavioral health providers for therapy and counseling, as well as psychiatrists for evaluation and treatment of other psychiatric disorders. Familiarity with naloxone overdose prevention training also is beneficial.
In addition, you must undergo 8 hours of training and apply for a waiver to prescribe buprenorphine in general medication settings. You can receive ongoing support after training on the AAP and Providers Clinical Support System websites.
Adolescent patients who receive buprenorphine for treatment of opioid use disorder typically undergo induction for 2 days where they are observed by a nurse or provider followed by weekly or biweekly medication-monitoring visits. It is “highly recommended” adolescents take urine drug screens during these visits but the results do not need to be observed. Many patients begin treatment when they are in IOP care, but some patients are not identified until they’ve had more severe consequences of opioid use disorder. Parents are involved in care by providing transportation and picking up and helping to administer medication, but there are confidential portions of the visits with the patient only.
“Parents have to be intimately involved and aware, and that’s an ideal situation,” Dr. Camenga said.
Dr. Camenga reported no relevant conflicts of interest.
ORLANDO – according to a presentation at the annual meeting of the American Academy of Pediatrics.
“We pediatricians have some unique skills that can really benefit our community of teens,” said Deepa Camenga, MD, of Yale University in New Haven, Conn.
Compared with some other specialists, who may be more reluctant to prescribe buprenorphine, pediatricians are more comfortable and have systems in place to deal with issues surrounding care coordination, adolescent confidentiality, family reassurance, and managing prescriptions for chronic diseases.“We can use those same skills when we’re caring for people with opioid use disorder,” she said.
According to the DSM-5 (Diagnostic and Statistical Manual–5), there are 11 criteria for opioid use disorder based on level of physiological dependence, impaired control, social functioning, and risky use. Meeting two or three criteria constitutes mild substance use disorder, while meeting six or more criteria is associated with severe substance use disorder.
Opioid use disorder in adolescents can be characterized by milder symptoms. Adolescents also tend to be in the early stage of this chronic disease when they seek care for opioid use disorder and need to be informed about the seriousness of the disease, Dr. Camenga noted.
“There is a disconnect about the severity of their illness when they present to me,” she said. “This is a disease that we know is chronic, severe – and without treatment – is progressive. We do know it can progress and get worse, and result in death.”
Treatment options for opioid use disorder in adolescents include behavioral interventions such as residential treatment, intensive outpatient (IOP), and partial hospitalization programs and therapy, as well as pharmacologic interventions like clonidine, buprenorphine, and methadone used for detoxification. Buprenorphine/naloxone has been labeled for use by patients 18 years or older; however, three recent randomized controlled trials have studied the effects of the intervention in 16-year-old and 17-year-old patients. In the trials, there were no serious adverse events reported with support of treatment for a minimum of 12 weeks and “many providers are treating up to a year” based on data from observational studies, Dr. Camenga said. Naltrexone also has been indicated for adolescents with opioid use disorder, with feasibility seen in pilot studies.
If you are interested in providing buprenorphine for patients, you need to apply for a Drug Enforcement Administration X-waiver, have access to their state’s prescription-monitoring program, and have a network of behavioral health providers for therapy and counseling, as well as psychiatrists for evaluation and treatment of other psychiatric disorders. Familiarity with naloxone overdose prevention training also is beneficial.
In addition, you must undergo 8 hours of training and apply for a waiver to prescribe buprenorphine in general medication settings. You can receive ongoing support after training on the AAP and Providers Clinical Support System websites.
Adolescent patients who receive buprenorphine for treatment of opioid use disorder typically undergo induction for 2 days where they are observed by a nurse or provider followed by weekly or biweekly medication-monitoring visits. It is “highly recommended” adolescents take urine drug screens during these visits but the results do not need to be observed. Many patients begin treatment when they are in IOP care, but some patients are not identified until they’ve had more severe consequences of opioid use disorder. Parents are involved in care by providing transportation and picking up and helping to administer medication, but there are confidential portions of the visits with the patient only.
“Parents have to be intimately involved and aware, and that’s an ideal situation,” Dr. Camenga said.
Dr. Camenga reported no relevant conflicts of interest.
ORLANDO – according to a presentation at the annual meeting of the American Academy of Pediatrics.
“We pediatricians have some unique skills that can really benefit our community of teens,” said Deepa Camenga, MD, of Yale University in New Haven, Conn.
Compared with some other specialists, who may be more reluctant to prescribe buprenorphine, pediatricians are more comfortable and have systems in place to deal with issues surrounding care coordination, adolescent confidentiality, family reassurance, and managing prescriptions for chronic diseases.“We can use those same skills when we’re caring for people with opioid use disorder,” she said.
According to the DSM-5 (Diagnostic and Statistical Manual–5), there are 11 criteria for opioid use disorder based on level of physiological dependence, impaired control, social functioning, and risky use. Meeting two or three criteria constitutes mild substance use disorder, while meeting six or more criteria is associated with severe substance use disorder.
Opioid use disorder in adolescents can be characterized by milder symptoms. Adolescents also tend to be in the early stage of this chronic disease when they seek care for opioid use disorder and need to be informed about the seriousness of the disease, Dr. Camenga noted.
“There is a disconnect about the severity of their illness when they present to me,” she said. “This is a disease that we know is chronic, severe – and without treatment – is progressive. We do know it can progress and get worse, and result in death.”
Treatment options for opioid use disorder in adolescents include behavioral interventions such as residential treatment, intensive outpatient (IOP), and partial hospitalization programs and therapy, as well as pharmacologic interventions like clonidine, buprenorphine, and methadone used for detoxification. Buprenorphine/naloxone has been labeled for use by patients 18 years or older; however, three recent randomized controlled trials have studied the effects of the intervention in 16-year-old and 17-year-old patients. In the trials, there were no serious adverse events reported with support of treatment for a minimum of 12 weeks and “many providers are treating up to a year” based on data from observational studies, Dr. Camenga said. Naltrexone also has been indicated for adolescents with opioid use disorder, with feasibility seen in pilot studies.
If you are interested in providing buprenorphine for patients, you need to apply for a Drug Enforcement Administration X-waiver, have access to their state’s prescription-monitoring program, and have a network of behavioral health providers for therapy and counseling, as well as psychiatrists for evaluation and treatment of other psychiatric disorders. Familiarity with naloxone overdose prevention training also is beneficial.
In addition, you must undergo 8 hours of training and apply for a waiver to prescribe buprenorphine in general medication settings. You can receive ongoing support after training on the AAP and Providers Clinical Support System websites.
Adolescent patients who receive buprenorphine for treatment of opioid use disorder typically undergo induction for 2 days where they are observed by a nurse or provider followed by weekly or biweekly medication-monitoring visits. It is “highly recommended” adolescents take urine drug screens during these visits but the results do not need to be observed. Many patients begin treatment when they are in IOP care, but some patients are not identified until they’ve had more severe consequences of opioid use disorder. Parents are involved in care by providing transportation and picking up and helping to administer medication, but there are confidential portions of the visits with the patient only.
“Parents have to be intimately involved and aware, and that’s an ideal situation,” Dr. Camenga said.
Dr. Camenga reported no relevant conflicts of interest.
EXPERT ANALYSIS AT AAP 18
Concerns over discretion, efficacy lead teen females to use emergency contraception
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
This study was very well conducted and provides genuine insight into adolescents who access contraception and their views about the difference between emergency contraception and nonemergent contraception. It also highlights that we have so much more work to do, from a public health perspective, when it comes to educating youth about the efficacy of contraception. If young people who have easier access to emergency contraception still believe incorrect information, what about those people who have minimal access?
Catherine Cansino, MD, MPH , is an associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the article by Fink et al.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Emergency contraception is perceived as “easy, effective, and discrete,” especially when compared with nonemergent contraception and condoms, according to a qualitative study of contraceptive behaviors and decision making among adolescent females who had previously used emergency contraception (EC) or planned to use it.
“Three main themes emerged from our interviews: There are multiple perceived benefits to using EC, nonemergent contraception (NEC) use is challenging, and the decision to use NEC is multifactorial,” lead author Geetha N. Fink, MD, MPH, and her coauthors wrote in the Journal of Pediatric and Adolescent Gynecology.
The investigators reviewed interview transcripts and questionnaire responses from 28 adolescent females who had all used or were planning to use EC. The participants, who were recruited from school-based health centers (SBHC) in New York, reported having used EC a mean of 3.5 times (range 0-30 times), noted Dr. Fink of the department of obstetrics, gynecology and reproductive sciences at the Icahn School of Medicine at Mount Sinai in New York and her colleagues.
SBHCs in New York can distribute EC for free and – once general consent to care at the SBHC is provided at the start of each school year– without parental notification. This ease of access contributed to EC use, along with its minimal side effects. EC also can “be used discretely without the involvement of the partner,” Dr. Fink and her coauthors noted. Although the majority of participants stated being comfortable discussing their EC use, “they still appreciated that EC does not require partner involvement or awareness, unlike condoms or withdrawal.”
The participants’ decision making often was influenced by misperception; 65% incorrectly stated that EC was 90%-99% effective, and NEC use was ascribed to beliefs that “excess EC decreases efficacy or is detrimental to health and social interactions.” At the same time, Dr. Fink and her colleagues found that NEC use was associated with participants who had more sexual experience or who correctly identified it as more effective than EC.
“Our findings suggest that as adolescents gained more experience with sex and counseling, and also matured, they appeared to be more likely to utilize NEC,” they wrote.
Dr. Fink and her associates shared limitations of their study, including the uniqueness of SBHCs in New York City in providing comprehensive health care options, compared with those in the rest of the United States. However, they also noted the value in interviewing adolescent EC users and therefore better understanding why they’ve made these contraceptive decisions.
“We suspect many more students would benefit from access to EC and the SBHC, but may be unaware of these resources. We recommend increased efforts to promote awareness of these resources in schools, especially incorporated into sexual education. EC should be readily available for all adolescents,” they wrote.
The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
SOURCE: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
Key clinical point: 65% of adolescent females who were interviewed incorrectly believed that emergency contraception is 90%-99% effective.
Major finding: Adolescents who use emergency contraception prefer it over nonemergent contraception because it is perceived as easy to use and a more private alternative.
Study details: A study of 28 interviews of adolescent females who self-reported emergency contraception use.
Disclosures: The study was funded through a grant from the Society of Family Planning. No conflicts of interest were reported.
Source: Fink GN et al. J Pediatr Adolesc Gynecol. 2018. doi: 10.1016/j.jpag.2018.10.005.
Trump administration rule erodes ACA contraceptive mandate
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
More employers can opt out of providing contraception coverage to their employees under final regulations from the Trump administration that narrow the Affordable Care Act’s contraceptive mandate.
The two regulations, released Nov. 7, allow an expanded group of employers and insurers to get out of covering contraception methods by objecting on either religious or moral grounds.
The first rule broadens exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. The second rule protects nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions apply to institutions of education, issuers, and individuals, but not to governmental entities.
When first proposed in 2017, Trump administration officials said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” The U.S. Department of Health & Human Services estimates that the rules, which take effect in January 2019, will affect no more than 200 employers.
The American College of Obstetricians and Gynecologists expressed concern that the final rules will restrict patient access to meaningful contraceptive methods and will erode decades of progress in increasing women’s reproductive autonomy and restrict patient access to contraception.
“Women, families and our nation all benefit from seamless, affordable access to contraception,” ACOG President Lisa M. Hollier, MD, said in a statement. “Contraception improves women’s health and well-being, reduces unintended pregnancy, enables pregnancy spacing for safer pregnancies and deliveries, and empowers women’s engagement in the workforce and economic self-sufficiency. A woman’s employer should not determine whether or not she has this access.”
Marjorie Dannenfelser, president of Susan B. Anthony List, an anti-abortion group, praised the final rules, calling them needed protections from the burdensome Obama-era ACA abortifacient drug mandate.
“President Trump and HHS Secretary Azar delivered a huge victory for conscience rights and religious liberty in America,” Ms. Dannenfelser said in a statement. “No longer will Catholic nuns who care for the elderly poor be forced by the government to provide abortion-inducing drugs in their health care plans. Not only that, moral objectors such as Susan B. Anthony List, will also no longer have to pay for life-ending drugs that are antithetical to their mission and for which we have argued there is certainly no compelling state interest.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
Under the approved regulations, employers or insurers can stop their coverage of contraceptive services if they have religious beliefs or moral convictions against covering birth control. Exempted entities and individuals also can choose to cover some, but not all, contraceptive services, depending on their specific religious or moral objection, according to an HHS fact sheet.
The agency emphasized that the regulations leave in place government programs that provide free or subsidized contraceptive coverage to low-income women, such as through community health centers, and that the rules do not ban any employer from covering contraceptives.
The regulations become effective 60 days after they are published in the Federal Register.
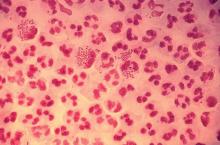
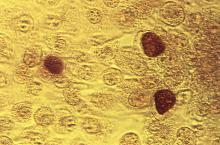
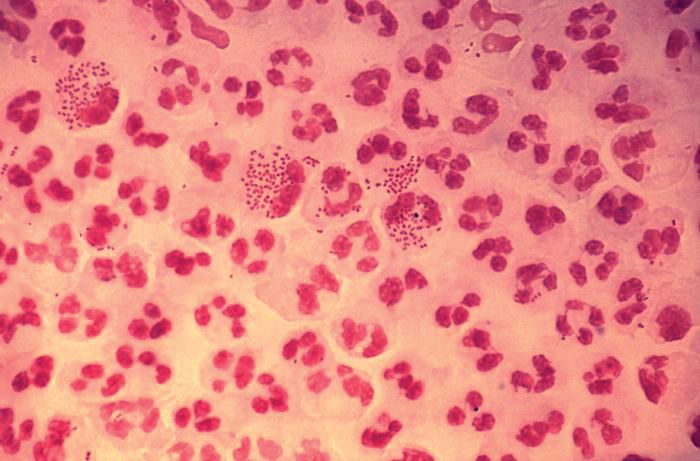
Rate of STIs is rising, and many U.S. teens are sexually active
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
ORLANDO – Consider point-of-care testing and treat potentially infected partners when diagnosing and treating adolescents for STIs, Diane M. Straub, MD, MPH, said at the annual meeting of the American Academy of Pediatrics.
In addition, adolescents are sometimes reluctant to disclose their full sexual history to their health care provider, which can complicate diagnosis and treatment, noted Dr. Straub, professor of pediatrics at the University of South Florida, Tampa. “That sometimes takes a few questions,” but can be achieved by asking the same questions in different ways and emphasizing the clinical importance of testing.
According to the 2017 Youth Risk Behavior Surveillance survey, 40% of adolescents reported ever having sexual intercourse, with 20% of 9th-grade, 36% of 10th-grade, 47% of 11th-grade, and 57% of 12th-grade students reporting they had sexual intercourse. By gender, 41% of adolescent males and 38% of adolescent females reported ever having sexual intercourse; by race, 39% of white, 41% of Hispanic, and 46% of black participants reported any sexual activity. Overall, 10% of adolescents said they had four or more partners, 3% said they had intercourse before age 13 years, 54% used a condom the last time they had intercourse, and 7% said they were raped.
The rate of STIs in the United States is rising. There has been a sharp increase in the number of combined diagnoses of gonorrhea, syphilis, and chlamydia, with an increase from 1.8 million in 2013 to 2.3 million cases in 2017, according to the Centers for Disease Control and Prevention. During that same time period, gonorrhea increased 67% from 333,004 to 555,608 cases, syphilis (primary and secondary) rose 76% from 17,375 to 30,644 cases, and chlamydia increased 22% to 1.7 million cases.
According to a 2013 CDC infographic shown by Dr. Straub, young people in the United States aged 15-24 years old represent 27% of the total sexually active population but account for 50% of new STI cases each year. Persons in this population account for 70% of gonorrhea cases, 63% of chlamydia cases, 49% of human papillomavirus (HPV) cases, 45% of genital herpes cases, and 20% of syphilis cases.
All sexually active females aged 25 years or younger should be screened for chlamydia and gonorrhea, as well as “at-risk” young men who have sex with men (YMSM), Dr. Straub said. All adolescent males and females aged over 13 years should be offered HIV screening, and HIV screening should be discussed “at least once.” And depending on how at risk each subpopulation is, health care providers should be have that conversation and offer screening multiple times.
Women who have sex with women (WSW) are a diverse population and should be treated based on their individual sexual identities, behaviors, and practices. “Most self-identified WSWs report having sex with men, so therefore adolescent WSWs and females with both male and female sex partners might be at increased risk for STIs, such as syphillis, chlamydia, and HPV as well as HIV, so you may want to adjust your screening accordingly,” she said.
Pregnant women, if at risk, should be screened for HIV, syphilis, hepatitis B, gonorrhea, and chlamydia.
YMSM should have annual screenings for syphilis and HIV, screenings for chlamydia and gonorrhea by infection site; also consider herpes simplex virus serology and anal cytology in these patients, Dr. Straub said. They also should be screened for hepatitis B surface antigen, vaccinated for hepatitis A, hepatitis B and, if using drugs, screened* for hepatitis C virus.
Dr. Straub recommended licensed health care professionals who may treat minor patients review their state’s laws on minors and their legal ability to consent to treatment of STIs without the involvement of their parent or guardian, including disclosure of positive results and in the case of HIV care.
In places where index insured are allowed to find out about any services a beneficiary receives on their insurance, “this is a little problematic, because in some states, this is in direct conflict with the explanation of benefits requirement,” she said. “There are certain ways to get around that, but it’s really important for you to know what the statutes are where you’re practicing and where the breaches of confidentiality [are].”
Expedited partner therapy, or treating one or multiple partners of patients with an STI, is recommended for certain patients and infections, such as male partners of female patients with chlamydia and gonorrhea. While this is recommended less for YMSM because of a higher rate of concurrent infection, “if you have a young person who has partners who are unlikely to have access to care and get treated, it’s recommended you give that treatment to your index patient and to then treat their partners,” Dr. Straub said.
A recent and frequently updated resource on STI treatment can be found at the CDC website.
Dr. Straub reported no relevant conflicts of interest.
*This article was updated 1/11/19.
EXPERT ANALYSIS FROM AAP 18
Many teens don’t know e-cigarettes contain nicotine
ORLANDO – Flavoring and lack of Food and Drug Administration regulation of e-cigarettes has led to more children and adolescents using these devices, according to American Academy of Pediatrics President Colleen A. Kraft, MD.
In an interview, Dr. Kraft said the FDA should regulate these products and limit their purchase to adults who are at least 21 years old. E-cigarettes were initially intended as an aid for adults to reduce their cigarette use, but the addition of flavoring has attracted children and adolescents to the devices, Dr. Kraft noted.
“When you have these devices that have flavors like gummy bear and cotton candy and bubblegum, you are marketing to children, and we are calling out the FDA because they could actually stop this today,” she said. In fact, Dr. Kraft added, many children and adolescents don’t even realize that e-cigarettes contain nicotine.
Dr. Kraft reported no relevant conflicts of interest.
ORLANDO – Flavoring and lack of Food and Drug Administration regulation of e-cigarettes has led to more children and adolescents using these devices, according to American Academy of Pediatrics President Colleen A. Kraft, MD.
In an interview, Dr. Kraft said the FDA should regulate these products and limit their purchase to adults who are at least 21 years old. E-cigarettes were initially intended as an aid for adults to reduce their cigarette use, but the addition of flavoring has attracted children and adolescents to the devices, Dr. Kraft noted.
“When you have these devices that have flavors like gummy bear and cotton candy and bubblegum, you are marketing to children, and we are calling out the FDA because they could actually stop this today,” she said. In fact, Dr. Kraft added, many children and adolescents don’t even realize that e-cigarettes contain nicotine.
Dr. Kraft reported no relevant conflicts of interest.
ORLANDO – Flavoring and lack of Food and Drug Administration regulation of e-cigarettes has led to more children and adolescents using these devices, according to American Academy of Pediatrics President Colleen A. Kraft, MD.
In an interview, Dr. Kraft said the FDA should regulate these products and limit their purchase to adults who are at least 21 years old. E-cigarettes were initially intended as an aid for adults to reduce their cigarette use, but the addition of flavoring has attracted children and adolescents to the devices, Dr. Kraft noted.
“When you have these devices that have flavors like gummy bear and cotton candy and bubblegum, you are marketing to children, and we are calling out the FDA because they could actually stop this today,” she said. In fact, Dr. Kraft added, many children and adolescents don’t even realize that e-cigarettes contain nicotine.
Dr. Kraft reported no relevant conflicts of interest.
REPORTING FROM AAP 2018
ACOG: First gynecologist visit between ages 13 and 15
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists recommends that the first reproductive health visit occur between the ages of 13 and 15, and I agree with them. Often patients attending this appointment don’t have physical complaints, and we can focus on prevention and education. The visit can be about building the provider-patient relationship and may serve to ease fears and develop trust before visits for problem management.
There are a number of important health education topics to cover from puberty and menses to confidentiality and minor-access laws. Because many young people will begin to initiate romantic relationships during middle school, the topic of healthy relationships is critical. Unhealthy relationships, in their many forms, can have far reaching impacts on a young person’s health and wellness. For years, we’ve been talking with young people about preventing STIs or preventing unwanted pregnancy, but we’ve spent less energy working towards something.
I’m excited to see these recommendations and look forward to helping my younger patients think through relationships as important aspects of life and health, what they want from them, and how they can work towards them.
Melissa Kottke , MD is an obstetrician-gynecologist specializing in family planning and adolescent reproductive health at Emory University in Atlanta.
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
The American College of Obstetricians and Gynecologists (ACOG) recommends that girls receive their first reproductive health visit between the ages of 13 and 15 years to discuss healthy relationships in addition to general reproductive health, according to a new committee opinion.
The recommendation, published online Oct. 24, emphasizes that such early visits provide opportunities for ob.gyns. to educate teenage girls and their guardians about age-appropriate health issues, such as sexual relationships, dating violence, and sexual coercion. Between the ages of 13 years and 15 years is an ideal window because middle school is a time that some adolescents develop their first romantic and sexual relationships (Obstet Gynecol. 2018; 132[5]:1317-18 doi: 10.1097/AOG.0000000000002946).
“Creating a nonjudgmental environment and educating staff on the unique concerns of adolescents are helpful ways to provide effective and appropriate care to this group of patients,” the authors wrote.
Ob.gyns. can use the early meeting to discuss key aspects of a healthy relationship with patients, including communication, self-respect, and mutual respect, while helping adolescents identify the characteristics of an unhealthy relationships such as dishonesty, intimidation, disrespect, and abuse, according to the opinion. As part of the discussion, ob.gyns. also may counsel patients to define their current relationship and their expectations for future relationships. Both relationships with and without sexual intimacy should be discussed, the opinion advises.
The recommendation reminds health care professionals to be mindful of federal and state confidentiality laws and that they be aware of mandatory reporting laws when intimate partner violence, teen dating violence, or statutory rape is suspected. In addition, the opinion notes that pregnant and parenting adolescents; lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ) individuals; and adolescents with physical and mental disabilities are at particular risk of disparities in the health care system.
“The promotion of healthy relationships in these groups requires the obstetrician-gynecologist to be aware of the unique barriers and hurdles to sexual and nonsexual expression, as well as to health care,” the opinion states. “Interventions to promote healthy relationships and a strong sexual health framework are more effective when started early and can affect indicators of long-term individual health and public health.”
FROM OBSTETRICS & GYNECOLOGY
Talk to adolescents about sexual assault
SEATTLE – Recent events have highlighted the issue of sexual assault in adolescents. But the onus still is on psychiatrists and other clinicians to ask patients whether they’ve ever been a victim of sexual assault or other kinds of trauma, according to an expert.
“It turns out that these experiences are common for kids, and they’re very correlated with the development of all kinds of psychiatric disorders. And if we ask, they will tell us. If we don’t ask they probably won’t,” said Lucy Berliner, director of the Harborview Center for Sexual Assault and Traumatic Stress, who discussed the epidemiology of sexual trauma in adolescents at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
A common misconception is that victims of sexual assault have endured multiple, chronic traumas. A more common scenario, however, is a single incident, much like the one described by Christine Blasey Ford, PhD, in her testimony before Congress, and clinicians should be more on the lookout for such cases. “I think those young people get a little bit lost,” Ms. Berliner said at the meeting.
Unlike the incident described by Dr. Ford, coercion often was not physical. Fifty-two percent of the time, the adolescents experienced abuse by authority figures, such as an assault by a teacher or coach, or even someone who used social advantage such as being older or more popular. In 17% of the cases, the victim was drugged or unconscious. Physical restraint was reported in 20% of cases. Weapons were involved only 7% of the time.
Twenty-eight percent of the adolescents were victims of a teenager, compared with 54% who attributed the assault to an adult. Overall, 72% of the subjects presented at an emergency department rather than a counseling clinic, which suggests that screening in medical environments also is a key factor in identifying and responding to people who have been assaulted.
All study subjects were offered counseling, but the uptake was low: The median was 2 sessions.
“My guess is that in the beginning, a lot of people say, ‘I just want to put it behind me, or I want to try to figure it out myself,’ and it only comes around later, in mental health settings, where these kids are in there for some type of psychiatric disorder. And unless we ask, we’re not going to find out (about a previous assault), and we won’t be able to give them the help that would help them with this psychiatric disorder,” said Ms. Berliner, also a clinical associate professor at the University of Washington School of Social Work in Seattle.
Clinicians might not ask about these experiences, she said, because of fears of triggering raw emotions. But such fears are unfounded, she stated. “We need to get over ourselves,” Ms. Berliner said. “If we don’t create the opportunity, why would they tell us? And if they don’t want to tell us, they won’t. But you can’t traumatize a kid by talking about something that’s already actually happened to them.”
That point can even extend to the legal system. Also during the session, Emily Petersen, senior deputy prosecuting attorney in the Special Assault Unit in King County, Washington, emphasized that, in her experience, young people who are victims of sexual and other forms of assault are resilient – and they will not be traumatized by speaking with a prosecutor or to police about their experiences.
But the legal system cannot provide healing, she and Ms. Berliner noted. That must come from the victim’s support system. “These experiences don’t have to define victims of sexual assault as long as the adults in their lives are responding appropriately to them,” Ms. Petersen said.
Ms. Berliner and Ms. Petersen disclosed no conflicts of interest.
SEATTLE – Recent events have highlighted the issue of sexual assault in adolescents. But the onus still is on psychiatrists and other clinicians to ask patients whether they’ve ever been a victim of sexual assault or other kinds of trauma, according to an expert.
“It turns out that these experiences are common for kids, and they’re very correlated with the development of all kinds of psychiatric disorders. And if we ask, they will tell us. If we don’t ask they probably won’t,” said Lucy Berliner, director of the Harborview Center for Sexual Assault and Traumatic Stress, who discussed the epidemiology of sexual trauma in adolescents at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
A common misconception is that victims of sexual assault have endured multiple, chronic traumas. A more common scenario, however, is a single incident, much like the one described by Christine Blasey Ford, PhD, in her testimony before Congress, and clinicians should be more on the lookout for such cases. “I think those young people get a little bit lost,” Ms. Berliner said at the meeting.
Unlike the incident described by Dr. Ford, coercion often was not physical. Fifty-two percent of the time, the adolescents experienced abuse by authority figures, such as an assault by a teacher or coach, or even someone who used social advantage such as being older or more popular. In 17% of the cases, the victim was drugged or unconscious. Physical restraint was reported in 20% of cases. Weapons were involved only 7% of the time.
Twenty-eight percent of the adolescents were victims of a teenager, compared with 54% who attributed the assault to an adult. Overall, 72% of the subjects presented at an emergency department rather than a counseling clinic, which suggests that screening in medical environments also is a key factor in identifying and responding to people who have been assaulted.
All study subjects were offered counseling, but the uptake was low: The median was 2 sessions.
“My guess is that in the beginning, a lot of people say, ‘I just want to put it behind me, or I want to try to figure it out myself,’ and it only comes around later, in mental health settings, where these kids are in there for some type of psychiatric disorder. And unless we ask, we’re not going to find out (about a previous assault), and we won’t be able to give them the help that would help them with this psychiatric disorder,” said Ms. Berliner, also a clinical associate professor at the University of Washington School of Social Work in Seattle.
Clinicians might not ask about these experiences, she said, because of fears of triggering raw emotions. But such fears are unfounded, she stated. “We need to get over ourselves,” Ms. Berliner said. “If we don’t create the opportunity, why would they tell us? And if they don’t want to tell us, they won’t. But you can’t traumatize a kid by talking about something that’s already actually happened to them.”
That point can even extend to the legal system. Also during the session, Emily Petersen, senior deputy prosecuting attorney in the Special Assault Unit in King County, Washington, emphasized that, in her experience, young people who are victims of sexual and other forms of assault are resilient – and they will not be traumatized by speaking with a prosecutor or to police about their experiences.
But the legal system cannot provide healing, she and Ms. Berliner noted. That must come from the victim’s support system. “These experiences don’t have to define victims of sexual assault as long as the adults in their lives are responding appropriately to them,” Ms. Petersen said.
Ms. Berliner and Ms. Petersen disclosed no conflicts of interest.
SEATTLE – Recent events have highlighted the issue of sexual assault in adolescents. But the onus still is on psychiatrists and other clinicians to ask patients whether they’ve ever been a victim of sexual assault or other kinds of trauma, according to an expert.
“It turns out that these experiences are common for kids, and they’re very correlated with the development of all kinds of psychiatric disorders. And if we ask, they will tell us. If we don’t ask they probably won’t,” said Lucy Berliner, director of the Harborview Center for Sexual Assault and Traumatic Stress, who discussed the epidemiology of sexual trauma in adolescents at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
A common misconception is that victims of sexual assault have endured multiple, chronic traumas. A more common scenario, however, is a single incident, much like the one described by Christine Blasey Ford, PhD, in her testimony before Congress, and clinicians should be more on the lookout for such cases. “I think those young people get a little bit lost,” Ms. Berliner said at the meeting.
Unlike the incident described by Dr. Ford, coercion often was not physical. Fifty-two percent of the time, the adolescents experienced abuse by authority figures, such as an assault by a teacher or coach, or even someone who used social advantage such as being older or more popular. In 17% of the cases, the victim was drugged or unconscious. Physical restraint was reported in 20% of cases. Weapons were involved only 7% of the time.
Twenty-eight percent of the adolescents were victims of a teenager, compared with 54% who attributed the assault to an adult. Overall, 72% of the subjects presented at an emergency department rather than a counseling clinic, which suggests that screening in medical environments also is a key factor in identifying and responding to people who have been assaulted.
All study subjects were offered counseling, but the uptake was low: The median was 2 sessions.
“My guess is that in the beginning, a lot of people say, ‘I just want to put it behind me, or I want to try to figure it out myself,’ and it only comes around later, in mental health settings, where these kids are in there for some type of psychiatric disorder. And unless we ask, we’re not going to find out (about a previous assault), and we won’t be able to give them the help that would help them with this psychiatric disorder,” said Ms. Berliner, also a clinical associate professor at the University of Washington School of Social Work in Seattle.
Clinicians might not ask about these experiences, she said, because of fears of triggering raw emotions. But such fears are unfounded, she stated. “We need to get over ourselves,” Ms. Berliner said. “If we don’t create the opportunity, why would they tell us? And if they don’t want to tell us, they won’t. But you can’t traumatize a kid by talking about something that’s already actually happened to them.”
That point can even extend to the legal system. Also during the session, Emily Petersen, senior deputy prosecuting attorney in the Special Assault Unit in King County, Washington, emphasized that, in her experience, young people who are victims of sexual and other forms of assault are resilient – and they will not be traumatized by speaking with a prosecutor or to police about their experiences.
But the legal system cannot provide healing, she and Ms. Berliner noted. That must come from the victim’s support system. “These experiences don’t have to define victims of sexual assault as long as the adults in their lives are responding appropriately to them,” Ms. Petersen said.
Ms. Berliner and Ms. Petersen disclosed no conflicts of interest.
REPORTING FROM AACAP 2018
What infectious disease should parents be most worried about?
I think the question was intended as polite, dinner party chit chat ... maybe an attempt by a gracious hostess to make sure everyone was engaged in conversation.
“So what pediatric infectious disease should parents be most worried about?” she asked me.
I’ll admit that a couple of perfectly respectable and noncontroversial possibilities crossed my mind before I answered.
Acute flaccid myelitis? Measles?
When I replied, “gonorrhea,” conversation at the table pretty much stopped.
Let me explain. Acute flaccid myelitis is a polio-like neurologic condition that has been grabbing headlines. Yes, it is concerning that most cases have occurred in children and some affected children are left with long-term deficits. Technically though, AFM is a neurologic rather than an infectious disease. When cases occur, we suspect a viral infection but according to the Centers for Disease Control and Prevention, no pathogen has been consistently identified from the spinal fluid of infected patients. From August 2014 to September 2018, the CDC received information on 368 confirmed cases, so AFM fortunately is still rare.
News reports describe measles outbreaks raging in Europe – more than 41,000 cases so far this year, and 40 deaths – and warn that the United States could be next. But let’s be honest: We have a safe and effective vaccine for measles and outbreaks like this don’t happen when individuals are appropriately immunized. Parents, immunize your children. If you are lucky enough to be traveling to Europe with your baby, remember that MMR vaccine is indicated for 6- to 11-month olds, but it doesn’t count in the 2-dose series.
But gonorrhea?
In 2017, the World Health Organization included Neisseria gonorrhoeae on its list of bacteria that pose the greatest threat to human health and for which new antibiotics are urgently needed. The popular media are calling N. gonorrhoeae one of the new “superbugs.” Globally, patients are being diagnosed with strains of gonorrhea that are resistant to all commonly used antibiotics. As reported during IDWeek 2018 this October, patients also are being diagnosed in the United States.
Sancta St. Cyr, MD, of the Centers for Disease Control and Prevention, and her colleagues reported data from the Gonococcal Isolate Surveillance Project (GISP) and trends in multidrug resistant (MDR) and extensively-drug resistant (XDR) gonorrhea in the United States. A gonococcal isolate with resistance or elevated minimum inhibitory concentrations (MIC) to greater than or equal to two classes of antimicrobials is classified as MDR and an isolate with elevated MICs to greater than or equal to three classes of antimicrobials is classified as XDR. The MIC is the lowest antimicrobial concentration that inhibits growth of bacteria in the laboratory and rising MICs – evidence that higher levels of an antibiotic are needed to stop bacterial growth – can be an early indicator that resistance is emerging.
More than 150,000 gonococcal isolates were tested between 1987 and 2016. The first isolates with elevated MICs to cephalosporins and macrolides were identified in 1998, and since 2011, MDR resistance rates have hovered around 1%. In 2016, the rate was 1.1%, down from 1.3% in 2011. A single XDR isolate with resistance to fluoroquinolones with elevated MICs to both cephalosporins and macrolides was identified in 2011.
One could look at these data and ask if this is a “glass half full or half empty” situation, but I propose that clinicians and public health officials should not look at these data and be reassured that rates of MDR-gonorrhea remained stable between 2010 and 2016. According to a recent surveillance report released by the CDC, the absolute number of cases of gonorrhea has continued to rise. In 2017, there were 555,608 cases reported in the United States, a 67% increase since 2013. If we assume that rates of resistance in 2017 were similar to those in 2016, that’s more than 5,000 cases of MDR-gonorrhea in a single year.
“That’s bad,” one of my dining companions agreed. “But is gonorrhea really a pediatric issue?”
To answer that question, we just have to look at the numbers. According to the 2017 Youth Risk Behavior Survey, the percentage of high school students who had ever had sex was approximately 40% and about 10% of students had four or more lifetime partners. More than 45% of sexually active students denied the use of a condom during the last sexual intercourse. Certainly, that puts many teenagers at risk for sexually transmitted infections (STIs). Perhaps it shouldn’t be surprising that public health authorities report that half of all new STIs occur in individuals aged 15-24 years. Moreover, 25% of sexually active adolescent girls contract at least one STI.
Gonorrhea is the second most commonly reported notifiable disease in the United States, and according to the CDC, rates of disease in 2017 were highest among adolescents and young adults. In females specifically, the highest rates of gonorrhea were observed among those aged 20-24 years (684.8 cases per 100,000 females) and 15-19 years (557.4 cases per 100,000 females).
It makes sense that pediatricians and parents advocate for making the reduction of gonorrhea transmission rates a public health priority. We also need to recognize that prompt diagnosis and appropriate treatment are critical. Since 2015, dual therapy with ceftriaxone and azithromycin is the only CDC-recommended treatment for gonorrhea.
At that dinner party, my closest friend, who also happens to be a pediatrician, rolled her eyes and shot me look that I’m sure meant, “Nobody really wants to talk about gonorrhea over dessert.” Still, because she is a good friend she said, “So basically you’re saying that and if this keeps up, we may see kids with untreatable infection. Now that is scary.”
I kept quiet after that but I wanted to mention that in 2017, less than 85% of patients diagnosed with gonorrhea at selected surveillance sites received the recommended treatment with two antibiotics. Patients with inadequately treated gonorrhea are at risk for a host of sequelae. Women can develop pelvic inflammatory disease, abscesses, chronic pelvic pain, and damage of the fallopian tubes that can lead to infertility. Men can develop epididymitis, which occasionally results in infertility. Rarely, N. gonorrhoeae can spread to the blood and cause life-threatening infection. Of course, patients who aren’t treated appropriately may continue to spread the bacteria. Scary? You bet.
For pediatricians who need a refresher course in the treatment of STIs, there are free resources available. The CDC’s 2015 STD Treatment Guidelines are available in a free app; the app contains a nice refresher on taking a sexual history. There also is a print version, wall chart, and pocket guide. Providers also may want to check out the National STD Curriculum offered by the University of Washington STD Prevention Training Center and the University of Washington. Visit https://www.std.uw.edu/.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
I think the question was intended as polite, dinner party chit chat ... maybe an attempt by a gracious hostess to make sure everyone was engaged in conversation.
“So what pediatric infectious disease should parents be most worried about?” she asked me.
I’ll admit that a couple of perfectly respectable and noncontroversial possibilities crossed my mind before I answered.
Acute flaccid myelitis? Measles?
When I replied, “gonorrhea,” conversation at the table pretty much stopped.
Let me explain. Acute flaccid myelitis is a polio-like neurologic condition that has been grabbing headlines. Yes, it is concerning that most cases have occurred in children and some affected children are left with long-term deficits. Technically though, AFM is a neurologic rather than an infectious disease. When cases occur, we suspect a viral infection but according to the Centers for Disease Control and Prevention, no pathogen has been consistently identified from the spinal fluid of infected patients. From August 2014 to September 2018, the CDC received information on 368 confirmed cases, so AFM fortunately is still rare.
News reports describe measles outbreaks raging in Europe – more than 41,000 cases so far this year, and 40 deaths – and warn that the United States could be next. But let’s be honest: We have a safe and effective vaccine for measles and outbreaks like this don’t happen when individuals are appropriately immunized. Parents, immunize your children. If you are lucky enough to be traveling to Europe with your baby, remember that MMR vaccine is indicated for 6- to 11-month olds, but it doesn’t count in the 2-dose series.
But gonorrhea?
In 2017, the World Health Organization included Neisseria gonorrhoeae on its list of bacteria that pose the greatest threat to human health and for which new antibiotics are urgently needed. The popular media are calling N. gonorrhoeae one of the new “superbugs.” Globally, patients are being diagnosed with strains of gonorrhea that are resistant to all commonly used antibiotics. As reported during IDWeek 2018 this October, patients also are being diagnosed in the United States.
Sancta St. Cyr, MD, of the Centers for Disease Control and Prevention, and her colleagues reported data from the Gonococcal Isolate Surveillance Project (GISP) and trends in multidrug resistant (MDR) and extensively-drug resistant (XDR) gonorrhea in the United States. A gonococcal isolate with resistance or elevated minimum inhibitory concentrations (MIC) to greater than or equal to two classes of antimicrobials is classified as MDR and an isolate with elevated MICs to greater than or equal to three classes of antimicrobials is classified as XDR. The MIC is the lowest antimicrobial concentration that inhibits growth of bacteria in the laboratory and rising MICs – evidence that higher levels of an antibiotic are needed to stop bacterial growth – can be an early indicator that resistance is emerging.
More than 150,000 gonococcal isolates were tested between 1987 and 2016. The first isolates with elevated MICs to cephalosporins and macrolides were identified in 1998, and since 2011, MDR resistance rates have hovered around 1%. In 2016, the rate was 1.1%, down from 1.3% in 2011. A single XDR isolate with resistance to fluoroquinolones with elevated MICs to both cephalosporins and macrolides was identified in 2011.
One could look at these data and ask if this is a “glass half full or half empty” situation, but I propose that clinicians and public health officials should not look at these data and be reassured that rates of MDR-gonorrhea remained stable between 2010 and 2016. According to a recent surveillance report released by the CDC, the absolute number of cases of gonorrhea has continued to rise. In 2017, there were 555,608 cases reported in the United States, a 67% increase since 2013. If we assume that rates of resistance in 2017 were similar to those in 2016, that’s more than 5,000 cases of MDR-gonorrhea in a single year.
“That’s bad,” one of my dining companions agreed. “But is gonorrhea really a pediatric issue?”
To answer that question, we just have to look at the numbers. According to the 2017 Youth Risk Behavior Survey, the percentage of high school students who had ever had sex was approximately 40% and about 10% of students had four or more lifetime partners. More than 45% of sexually active students denied the use of a condom during the last sexual intercourse. Certainly, that puts many teenagers at risk for sexually transmitted infections (STIs). Perhaps it shouldn’t be surprising that public health authorities report that half of all new STIs occur in individuals aged 15-24 years. Moreover, 25% of sexually active adolescent girls contract at least one STI.
Gonorrhea is the second most commonly reported notifiable disease in the United States, and according to the CDC, rates of disease in 2017 were highest among adolescents and young adults. In females specifically, the highest rates of gonorrhea were observed among those aged 20-24 years (684.8 cases per 100,000 females) and 15-19 years (557.4 cases per 100,000 females).
It makes sense that pediatricians and parents advocate for making the reduction of gonorrhea transmission rates a public health priority. We also need to recognize that prompt diagnosis and appropriate treatment are critical. Since 2015, dual therapy with ceftriaxone and azithromycin is the only CDC-recommended treatment for gonorrhea.
At that dinner party, my closest friend, who also happens to be a pediatrician, rolled her eyes and shot me look that I’m sure meant, “Nobody really wants to talk about gonorrhea over dessert.” Still, because she is a good friend she said, “So basically you’re saying that and if this keeps up, we may see kids with untreatable infection. Now that is scary.”
I kept quiet after that but I wanted to mention that in 2017, less than 85% of patients diagnosed with gonorrhea at selected surveillance sites received the recommended treatment with two antibiotics. Patients with inadequately treated gonorrhea are at risk for a host of sequelae. Women can develop pelvic inflammatory disease, abscesses, chronic pelvic pain, and damage of the fallopian tubes that can lead to infertility. Men can develop epididymitis, which occasionally results in infertility. Rarely, N. gonorrhoeae can spread to the blood and cause life-threatening infection. Of course, patients who aren’t treated appropriately may continue to spread the bacteria. Scary? You bet.
For pediatricians who need a refresher course in the treatment of STIs, there are free resources available. The CDC’s 2015 STD Treatment Guidelines are available in a free app; the app contains a nice refresher on taking a sexual history. There also is a print version, wall chart, and pocket guide. Providers also may want to check out the National STD Curriculum offered by the University of Washington STD Prevention Training Center and the University of Washington. Visit https://www.std.uw.edu/.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
I think the question was intended as polite, dinner party chit chat ... maybe an attempt by a gracious hostess to make sure everyone was engaged in conversation.
“So what pediatric infectious disease should parents be most worried about?” she asked me.
I’ll admit that a couple of perfectly respectable and noncontroversial possibilities crossed my mind before I answered.
Acute flaccid myelitis? Measles?
When I replied, “gonorrhea,” conversation at the table pretty much stopped.
Let me explain. Acute flaccid myelitis is a polio-like neurologic condition that has been grabbing headlines. Yes, it is concerning that most cases have occurred in children and some affected children are left with long-term deficits. Technically though, AFM is a neurologic rather than an infectious disease. When cases occur, we suspect a viral infection but according to the Centers for Disease Control and Prevention, no pathogen has been consistently identified from the spinal fluid of infected patients. From August 2014 to September 2018, the CDC received information on 368 confirmed cases, so AFM fortunately is still rare.
News reports describe measles outbreaks raging in Europe – more than 41,000 cases so far this year, and 40 deaths – and warn that the United States could be next. But let’s be honest: We have a safe and effective vaccine for measles and outbreaks like this don’t happen when individuals are appropriately immunized. Parents, immunize your children. If you are lucky enough to be traveling to Europe with your baby, remember that MMR vaccine is indicated for 6- to 11-month olds, but it doesn’t count in the 2-dose series.
But gonorrhea?
In 2017, the World Health Organization included Neisseria gonorrhoeae on its list of bacteria that pose the greatest threat to human health and for which new antibiotics are urgently needed. The popular media are calling N. gonorrhoeae one of the new “superbugs.” Globally, patients are being diagnosed with strains of gonorrhea that are resistant to all commonly used antibiotics. As reported during IDWeek 2018 this October, patients also are being diagnosed in the United States.
Sancta St. Cyr, MD, of the Centers for Disease Control and Prevention, and her colleagues reported data from the Gonococcal Isolate Surveillance Project (GISP) and trends in multidrug resistant (MDR) and extensively-drug resistant (XDR) gonorrhea in the United States. A gonococcal isolate with resistance or elevated minimum inhibitory concentrations (MIC) to greater than or equal to two classes of antimicrobials is classified as MDR and an isolate with elevated MICs to greater than or equal to three classes of antimicrobials is classified as XDR. The MIC is the lowest antimicrobial concentration that inhibits growth of bacteria in the laboratory and rising MICs – evidence that higher levels of an antibiotic are needed to stop bacterial growth – can be an early indicator that resistance is emerging.
More than 150,000 gonococcal isolates were tested between 1987 and 2016. The first isolates with elevated MICs to cephalosporins and macrolides were identified in 1998, and since 2011, MDR resistance rates have hovered around 1%. In 2016, the rate was 1.1%, down from 1.3% in 2011. A single XDR isolate with resistance to fluoroquinolones with elevated MICs to both cephalosporins and macrolides was identified in 2011.
One could look at these data and ask if this is a “glass half full or half empty” situation, but I propose that clinicians and public health officials should not look at these data and be reassured that rates of MDR-gonorrhea remained stable between 2010 and 2016. According to a recent surveillance report released by the CDC, the absolute number of cases of gonorrhea has continued to rise. In 2017, there were 555,608 cases reported in the United States, a 67% increase since 2013. If we assume that rates of resistance in 2017 were similar to those in 2016, that’s more than 5,000 cases of MDR-gonorrhea in a single year.
“That’s bad,” one of my dining companions agreed. “But is gonorrhea really a pediatric issue?”
To answer that question, we just have to look at the numbers. According to the 2017 Youth Risk Behavior Survey, the percentage of high school students who had ever had sex was approximately 40% and about 10% of students had four or more lifetime partners. More than 45% of sexually active students denied the use of a condom during the last sexual intercourse. Certainly, that puts many teenagers at risk for sexually transmitted infections (STIs). Perhaps it shouldn’t be surprising that public health authorities report that half of all new STIs occur in individuals aged 15-24 years. Moreover, 25% of sexually active adolescent girls contract at least one STI.
Gonorrhea is the second most commonly reported notifiable disease in the United States, and according to the CDC, rates of disease in 2017 were highest among adolescents and young adults. In females specifically, the highest rates of gonorrhea were observed among those aged 20-24 years (684.8 cases per 100,000 females) and 15-19 years (557.4 cases per 100,000 females).
It makes sense that pediatricians and parents advocate for making the reduction of gonorrhea transmission rates a public health priority. We also need to recognize that prompt diagnosis and appropriate treatment are critical. Since 2015, dual therapy with ceftriaxone and azithromycin is the only CDC-recommended treatment for gonorrhea.
At that dinner party, my closest friend, who also happens to be a pediatrician, rolled her eyes and shot me look that I’m sure meant, “Nobody really wants to talk about gonorrhea over dessert.” Still, because she is a good friend she said, “So basically you’re saying that and if this keeps up, we may see kids with untreatable infection. Now that is scary.”
I kept quiet after that but I wanted to mention that in 2017, less than 85% of patients diagnosed with gonorrhea at selected surveillance sites received the recommended treatment with two antibiotics. Patients with inadequately treated gonorrhea are at risk for a host of sequelae. Women can develop pelvic inflammatory disease, abscesses, chronic pelvic pain, and damage of the fallopian tubes that can lead to infertility. Men can develop epididymitis, which occasionally results in infertility. Rarely, N. gonorrhoeae can spread to the blood and cause life-threatening infection. Of course, patients who aren’t treated appropriately may continue to spread the bacteria. Scary? You bet.
For pediatricians who need a refresher course in the treatment of STIs, there are free resources available. The CDC’s 2015 STD Treatment Guidelines are available in a free app; the app contains a nice refresher on taking a sexual history. There also is a print version, wall chart, and pocket guide. Providers also may want to check out the National STD Curriculum offered by the University of Washington STD Prevention Training Center and the University of Washington. Visit https://www.std.uw.edu/.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].