User login
Ceftolozane-tazobactam found effective in critically ill patients with Pseudomonas aeruginosa infections
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
, according to the results of a retrospective, observational study conducted in critically ill patients.
The multicenter, observational study assessed 95 patients who received C/T for P. aeruginosa serious infections, according to a report published online in the International Journal of Antimicrobial Agents.
C/T is a novel beta-lactam/ beta-lactamase inhibitor combination active against gram-negative bacteria including P. aeruginosa, “This paper presents the largest real-life experience published on C/T therapy for treating serious P. aeruginosa infections according to researchers Barbara Balandin, MD, of the Hospital Universitario Puerta de Hierro, Majadahonda, Spain, and colleagues.
The main infections treated were nosocomial pneumonia (56.2%), intra-abdominal infection (10.5%), tracheobronchitis (8.4%), and urinary tract infection (6.3%). Most infections were complicated with sepsis (49.5%) or septic shock (45.3%), and bacteremia (10.5%).
A total of 46 episodes were treated with high-dose C/T (3 g every 8 hours), and 38 episodes were treated with standard dosage (1.5 g every 8 hours). Almost half (44.2%) of the patients were treated with C/T monotherapy, and the remaining group received combination therapy with other antibiotics, according to the researchers.
The primary outcome of the study was to assess the efficacy and toxicity of C/T therapy. The secondary outcome was to evaluate the risk factors for all-cause 30-day mortality from the first day of therapy.
Favorable results
Most of the infections (93.7%) were severe and included the presence of sepsis (49.5%) or septic shock (45.3%). Bacteremia was observed in 15 (15.7%) patients. Bacteremia was secondary to nosocomial pneumonia in eight cases, catheter infection in five, urinary tract infection in one, and soft tissue infection in one. According to their susceptibility profiles, 46 (48.4%) of the strains were classified as extensively drug-resistant (XDR) P. aeruginosa and 35 (36.5%) were multidrug-resistant (MDR) P. aeruginosa.
Sixty-eight (71.6%) patients presented a favorable clinical response, which was defined as a resolution of presenting symptoms and signs of the infection by the end of therapy. An unfavorable clinical response was considered as persistence or worsening of the presenting symptoms and signs or death occurring during treatment with no other cause identified. Death associated with infection was defined as persistence of signs and symptoms of P. aeruginosa infection during C/T therapy with no other cause identified.
Microbiological eradication was documented in 42.1% (40/95) of the episodes. However, the global ICU mortality was still high, at 36.5%, with mortality mainly related to the severity of the infection.
Mortality was found to be significantly correlated with the Charlson Comorbidity Index (5.7 vs. 4.3; P = .04) and the need for life-supporting therapies such as vasopressors (66.6% vs. 46.9%; P = .03) and renal replacement therapy (46.6% vs. 18.1%; P = .002). In addition, mortality was significantly associated with a higher sequential organ failure assessment (SOFA) score during C/T therapy (SOFA1, SOFA 3, and SOFA 7; P < .001).
No significant differences in outcomes were correlated with demographic features, type and severity of infection, and dose of C/T. Also, there were no differences seen in outcomes between patients treated with C/T monotherapy and combined therapy (30.9% vs. 30.1%; P = .55).
“The lack of a positive effect from combined therapy suggests that C/T monotherapy may be sufficient for treating P. aeruginosa isolates that are susceptible to that agent,” the researchers suggested. “This study shows that C/T appears to be a suitable, effective, and safe drug for treating severe infections due to P. aeruginosa, highlighting nosocomial pneumonia caused by MDR/XDR P. aeruginosa in ICU patients with multiple comorbidities, such as immunosuppression, and needing life-sustaining therapies,” they concluded.
The authors reported that they had no outside funding source and had no conflicts of interest.
FROM THE INTERNATIONAL JOURNAL OF ANTIMICROBIAL AGENTS
Antibiotic prescribing: How to manage patient pressures
Inappropriate antibiotic prescribing in the face of growing microbial resistance is a global public health problem, and a major cause is perceived patient pressure.
At the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Tanya Stivers, PhD, professor of sociology at the University of California, Los Angeles, presented some of her team’s work studying patterns of clinical prescription.
It is widely appreciated that inappropriate prescribing is a common problem that the medical community seems powerless to stop, particularly in primary care. Already, clinicians are running out of effective antibiotics to treat a range of serious infections. Dr. Stivers began by saying that this problem isn’t caused by a lack of understanding about disease causation and microbial resistance or patients overtly demanding antibiotics, which occurs in less than 2% of cases. Instead, the cause appears to lie in doctor-patient interactions during consultations.
In pediatric practice, physicians have previously been found to prescribe antibiotics for a clinically diagnosed respiratory viral infection in 62% of cases when they perceive that this diagnosis was expected by parents, compared with 7% in the absence of such perception. Similarly, associated ear infections were diagnosed three times more often, and sinus infections seven times more often, leading to increased prescribing.
In adult practice, Dr. Stivers reported that patients can exert subtle pressure to prescribe through:
- Priming. Patients help their physician to see the problem as relatively severe (e.g., a sore throat that “feels like a knife”).
- Nudging. Patients redirect physicians back to a bacterial problem (e.g., “I’ve tried all these medicines, and nothing worked”). Nudging was found to occur in 41% of encounters.
- Resisting. Patients contest diagnosis or treatment in 40% of consultations (e.g., “there was pus yesterday”).
Priming or nudging resulted in antibiotic prescribing in 60% of patients without signs of a bacterial infection, compared with 30% where this was not a feature (P < 0.05).
But how can these pressures be countered? Dr. Stivers offered advice based on her original data from 570 video recordings of pediatric encounters. The current findings come from an analysis of 68 adult primary care visits for upper respiratory tract infections in Southern California. Inappropriate prescribing was identified in 37%.
When researching the antibiotic prescribing problem, it is helpful to explore a typical primary care consultation. The acute medical visit structure is a stepwise process involving opening, establishing the problem, gathering information, counseling, and then closing the consultation. It is important is to recognize that patients shape prescribing decisions, and effective communication is vital in influencing the outcome. In Dr. Stivers’ experience, priming, nudging, and resisting result in antibiotic prescribing in 60% of cases in whom clinical signs of bacterial illness are absent, compared with 30% where patient pressure is not a feature.
How can we change practice? Global experience suggests that printed material aimed at physicians is only of marginal benefit. By comparison, patient education does work but needs to be repeated, and there’s always a reason why this consultation should be “special.”
Try a 3-prong communication plan
To counteract these pressures, Dr. Stivers recommends a three-prong communication plan to influence the consultation:
- Foreshadowing, where suggesting that the cause of the patient’s symptoms is likely to be viral is introduced early in the consultation. This approach was found to reduce antibiotic prescribing to 33%, compared with 59% without foreshadowing (P < .05). Resistance may also be reduced.
- Affirmative nonantibiotic treatment plans, where specific positive recommendations given early (e.g., “I’m going to put you on some medicine to try to dry that out”) are less likely to be resisted than is vague negative advice at the end of a consultation.
- Persuasion, which involves explaining the diagnosis and nature of a cough and cold, educating about viral and bacterial differences, and presenting the risks of antibiotics. When persuasion is employed, antibiotic prescribing is reduced to 33%, compared with 63% (P < .05) without persuasion. In general, effective foreshadowing and affirmation should avoid the need for persuasion.
Dr. Stivers’ research suggests that these techniques work, but to do so, they should be delivered naturally as part of routine practice. Interestingly, her data showed that physicians rarely foreshadowed, and when they encountered resistance, they adopted persuasion in 53% of cases. By comparison, affirmative recommendations were used in 89% of cases, but their effects were reduced by the physician being vague and nonspecific.
In conclusion, Dr. Stivers said that addressing inappropriate prescribing requires awareness but that is not enough. The challenge is to reconsider health policies and ways of communicating about antibiotics. There is no downside to foreshadowing a likely viral origin, delivering affirmation, or using persuasion. She added, “If we can make even a 5%-10% reduction [in prescribing], wouldn’t it be worth it?”
Questions answered
A question-and-answer session followed Dr. Stivers’ presentation, and points raised included:
- Physicians have a desire to please. Dr. Stivers countered this point by saying that satisfaction is not tied to antibiotic prescription, and that physicians often misjudge what patients want. It’s important to communicate other treatment options because patients often just want “something they can do.”
- Decision fatigue is often a factor. Evidence shows that antibiotic prescription is more frequent toward the end of a shift. Doctors should avoid negotiation because it increases consultation time. Here, foreshadowing early on may help. Setting may also be important – prescription is more frequent in the ED.
- Vaccine-resistant parents often want active treatment. Here, conversations can be challenging. Trying to persuade may be a less successful than giving positive instruction (e.g., “we’ll give you a vaccine today.”) Resistance is likely to be lower.
- Concern was expressed about manipulating patients ahead of a firm diagnosis. Could this lead to missing a serious bacterial infection? Dr. Stivers acknowledged that this was a gamble. She recommended a “neutral” early foreshadowing statement such as “we are seeing a lot of viral infections at the present.”
- Cultural differences can have an effect. In China, for example, the argument between parents and physicians no longer focuses on antibiotics versus nonantibiotics but rather on oral versus intravenous administration.
- Litigation is a factor in prescribing, especially in the United States. Dr. Stivers stated that her proposed approach to prescribing should not interfere with appropriate management. The clinical picture can change, and antibiotics should be prescribed where needed.
- Audits improve prescribing in the short term. These results were based on recorded consultations, and that factor may have influenced management. In unrecorded consultations, inappropriate antibiotic prescription would be higher.
- Increased point-of-care testing can reduce unnecessary prescribing. This has been documented in countries such as Sweden. Evidence from China suggests that many patients will still receive antibiotics even if a bacterial cause is excluded.
When patients dictate treatment, sometimes we must tell them what is best. Dr. Stivers closed her presentation by emphasizing that, “how you say things will matter.”
Louis Bont, MD, PhD, chair of this session and pediatric infectious diseases specialist at the University Medical Center Utrecht (the Netherlands), commented: “Antimicrobial resistance is a global health threat which jeopardizes sustainable health goals. The World Health Organization has declared that antimicrobial resistance is one of the top 10 global public health threats facing humanity. Resistance to ciprofloxacin varies from 8%-93% in Escherichia coli and 4%-80% in Klebsiella pneumoniae. Colistin is the only last-resort treatment for life-threatening infections caused by carbapenem-resistant enterobacteriaceae.”
Dr. Stivers stated that she has nothing to disclose.
Inappropriate antibiotic prescribing in the face of growing microbial resistance is a global public health problem, and a major cause is perceived patient pressure.
At the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Tanya Stivers, PhD, professor of sociology at the University of California, Los Angeles, presented some of her team’s work studying patterns of clinical prescription.
It is widely appreciated that inappropriate prescribing is a common problem that the medical community seems powerless to stop, particularly in primary care. Already, clinicians are running out of effective antibiotics to treat a range of serious infections. Dr. Stivers began by saying that this problem isn’t caused by a lack of understanding about disease causation and microbial resistance or patients overtly demanding antibiotics, which occurs in less than 2% of cases. Instead, the cause appears to lie in doctor-patient interactions during consultations.
In pediatric practice, physicians have previously been found to prescribe antibiotics for a clinically diagnosed respiratory viral infection in 62% of cases when they perceive that this diagnosis was expected by parents, compared with 7% in the absence of such perception. Similarly, associated ear infections were diagnosed three times more often, and sinus infections seven times more often, leading to increased prescribing.
In adult practice, Dr. Stivers reported that patients can exert subtle pressure to prescribe through:
- Priming. Patients help their physician to see the problem as relatively severe (e.g., a sore throat that “feels like a knife”).
- Nudging. Patients redirect physicians back to a bacterial problem (e.g., “I’ve tried all these medicines, and nothing worked”). Nudging was found to occur in 41% of encounters.
- Resisting. Patients contest diagnosis or treatment in 40% of consultations (e.g., “there was pus yesterday”).
Priming or nudging resulted in antibiotic prescribing in 60% of patients without signs of a bacterial infection, compared with 30% where this was not a feature (P < 0.05).
But how can these pressures be countered? Dr. Stivers offered advice based on her original data from 570 video recordings of pediatric encounters. The current findings come from an analysis of 68 adult primary care visits for upper respiratory tract infections in Southern California. Inappropriate prescribing was identified in 37%.
When researching the antibiotic prescribing problem, it is helpful to explore a typical primary care consultation. The acute medical visit structure is a stepwise process involving opening, establishing the problem, gathering information, counseling, and then closing the consultation. It is important is to recognize that patients shape prescribing decisions, and effective communication is vital in influencing the outcome. In Dr. Stivers’ experience, priming, nudging, and resisting result in antibiotic prescribing in 60% of cases in whom clinical signs of bacterial illness are absent, compared with 30% where patient pressure is not a feature.
How can we change practice? Global experience suggests that printed material aimed at physicians is only of marginal benefit. By comparison, patient education does work but needs to be repeated, and there’s always a reason why this consultation should be “special.”
Try a 3-prong communication plan
To counteract these pressures, Dr. Stivers recommends a three-prong communication plan to influence the consultation:
- Foreshadowing, where suggesting that the cause of the patient’s symptoms is likely to be viral is introduced early in the consultation. This approach was found to reduce antibiotic prescribing to 33%, compared with 59% without foreshadowing (P < .05). Resistance may also be reduced.
- Affirmative nonantibiotic treatment plans, where specific positive recommendations given early (e.g., “I’m going to put you on some medicine to try to dry that out”) are less likely to be resisted than is vague negative advice at the end of a consultation.
- Persuasion, which involves explaining the diagnosis and nature of a cough and cold, educating about viral and bacterial differences, and presenting the risks of antibiotics. When persuasion is employed, antibiotic prescribing is reduced to 33%, compared with 63% (P < .05) without persuasion. In general, effective foreshadowing and affirmation should avoid the need for persuasion.
Dr. Stivers’ research suggests that these techniques work, but to do so, they should be delivered naturally as part of routine practice. Interestingly, her data showed that physicians rarely foreshadowed, and when they encountered resistance, they adopted persuasion in 53% of cases. By comparison, affirmative recommendations were used in 89% of cases, but their effects were reduced by the physician being vague and nonspecific.
In conclusion, Dr. Stivers said that addressing inappropriate prescribing requires awareness but that is not enough. The challenge is to reconsider health policies and ways of communicating about antibiotics. There is no downside to foreshadowing a likely viral origin, delivering affirmation, or using persuasion. She added, “If we can make even a 5%-10% reduction [in prescribing], wouldn’t it be worth it?”
Questions answered
A question-and-answer session followed Dr. Stivers’ presentation, and points raised included:
- Physicians have a desire to please. Dr. Stivers countered this point by saying that satisfaction is not tied to antibiotic prescription, and that physicians often misjudge what patients want. It’s important to communicate other treatment options because patients often just want “something they can do.”
- Decision fatigue is often a factor. Evidence shows that antibiotic prescription is more frequent toward the end of a shift. Doctors should avoid negotiation because it increases consultation time. Here, foreshadowing early on may help. Setting may also be important – prescription is more frequent in the ED.
- Vaccine-resistant parents often want active treatment. Here, conversations can be challenging. Trying to persuade may be a less successful than giving positive instruction (e.g., “we’ll give you a vaccine today.”) Resistance is likely to be lower.
- Concern was expressed about manipulating patients ahead of a firm diagnosis. Could this lead to missing a serious bacterial infection? Dr. Stivers acknowledged that this was a gamble. She recommended a “neutral” early foreshadowing statement such as “we are seeing a lot of viral infections at the present.”
- Cultural differences can have an effect. In China, for example, the argument between parents and physicians no longer focuses on antibiotics versus nonantibiotics but rather on oral versus intravenous administration.
- Litigation is a factor in prescribing, especially in the United States. Dr. Stivers stated that her proposed approach to prescribing should not interfere with appropriate management. The clinical picture can change, and antibiotics should be prescribed where needed.
- Audits improve prescribing in the short term. These results were based on recorded consultations, and that factor may have influenced management. In unrecorded consultations, inappropriate antibiotic prescription would be higher.
- Increased point-of-care testing can reduce unnecessary prescribing. This has been documented in countries such as Sweden. Evidence from China suggests that many patients will still receive antibiotics even if a bacterial cause is excluded.
When patients dictate treatment, sometimes we must tell them what is best. Dr. Stivers closed her presentation by emphasizing that, “how you say things will matter.”
Louis Bont, MD, PhD, chair of this session and pediatric infectious diseases specialist at the University Medical Center Utrecht (the Netherlands), commented: “Antimicrobial resistance is a global health threat which jeopardizes sustainable health goals. The World Health Organization has declared that antimicrobial resistance is one of the top 10 global public health threats facing humanity. Resistance to ciprofloxacin varies from 8%-93% in Escherichia coli and 4%-80% in Klebsiella pneumoniae. Colistin is the only last-resort treatment for life-threatening infections caused by carbapenem-resistant enterobacteriaceae.”
Dr. Stivers stated that she has nothing to disclose.
Inappropriate antibiotic prescribing in the face of growing microbial resistance is a global public health problem, and a major cause is perceived patient pressure.
At the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Tanya Stivers, PhD, professor of sociology at the University of California, Los Angeles, presented some of her team’s work studying patterns of clinical prescription.
It is widely appreciated that inappropriate prescribing is a common problem that the medical community seems powerless to stop, particularly in primary care. Already, clinicians are running out of effective antibiotics to treat a range of serious infections. Dr. Stivers began by saying that this problem isn’t caused by a lack of understanding about disease causation and microbial resistance or patients overtly demanding antibiotics, which occurs in less than 2% of cases. Instead, the cause appears to lie in doctor-patient interactions during consultations.
In pediatric practice, physicians have previously been found to prescribe antibiotics for a clinically diagnosed respiratory viral infection in 62% of cases when they perceive that this diagnosis was expected by parents, compared with 7% in the absence of such perception. Similarly, associated ear infections were diagnosed three times more often, and sinus infections seven times more often, leading to increased prescribing.
In adult practice, Dr. Stivers reported that patients can exert subtle pressure to prescribe through:
- Priming. Patients help their physician to see the problem as relatively severe (e.g., a sore throat that “feels like a knife”).
- Nudging. Patients redirect physicians back to a bacterial problem (e.g., “I’ve tried all these medicines, and nothing worked”). Nudging was found to occur in 41% of encounters.
- Resisting. Patients contest diagnosis or treatment in 40% of consultations (e.g., “there was pus yesterday”).
Priming or nudging resulted in antibiotic prescribing in 60% of patients without signs of a bacterial infection, compared with 30% where this was not a feature (P < 0.05).
But how can these pressures be countered? Dr. Stivers offered advice based on her original data from 570 video recordings of pediatric encounters. The current findings come from an analysis of 68 adult primary care visits for upper respiratory tract infections in Southern California. Inappropriate prescribing was identified in 37%.
When researching the antibiotic prescribing problem, it is helpful to explore a typical primary care consultation. The acute medical visit structure is a stepwise process involving opening, establishing the problem, gathering information, counseling, and then closing the consultation. It is important is to recognize that patients shape prescribing decisions, and effective communication is vital in influencing the outcome. In Dr. Stivers’ experience, priming, nudging, and resisting result in antibiotic prescribing in 60% of cases in whom clinical signs of bacterial illness are absent, compared with 30% where patient pressure is not a feature.
How can we change practice? Global experience suggests that printed material aimed at physicians is only of marginal benefit. By comparison, patient education does work but needs to be repeated, and there’s always a reason why this consultation should be “special.”
Try a 3-prong communication plan
To counteract these pressures, Dr. Stivers recommends a three-prong communication plan to influence the consultation:
- Foreshadowing, where suggesting that the cause of the patient’s symptoms is likely to be viral is introduced early in the consultation. This approach was found to reduce antibiotic prescribing to 33%, compared with 59% without foreshadowing (P < .05). Resistance may also be reduced.
- Affirmative nonantibiotic treatment plans, where specific positive recommendations given early (e.g., “I’m going to put you on some medicine to try to dry that out”) are less likely to be resisted than is vague negative advice at the end of a consultation.
- Persuasion, which involves explaining the diagnosis and nature of a cough and cold, educating about viral and bacterial differences, and presenting the risks of antibiotics. When persuasion is employed, antibiotic prescribing is reduced to 33%, compared with 63% (P < .05) without persuasion. In general, effective foreshadowing and affirmation should avoid the need for persuasion.
Dr. Stivers’ research suggests that these techniques work, but to do so, they should be delivered naturally as part of routine practice. Interestingly, her data showed that physicians rarely foreshadowed, and when they encountered resistance, they adopted persuasion in 53% of cases. By comparison, affirmative recommendations were used in 89% of cases, but their effects were reduced by the physician being vague and nonspecific.
In conclusion, Dr. Stivers said that addressing inappropriate prescribing requires awareness but that is not enough. The challenge is to reconsider health policies and ways of communicating about antibiotics. There is no downside to foreshadowing a likely viral origin, delivering affirmation, or using persuasion. She added, “If we can make even a 5%-10% reduction [in prescribing], wouldn’t it be worth it?”
Questions answered
A question-and-answer session followed Dr. Stivers’ presentation, and points raised included:
- Physicians have a desire to please. Dr. Stivers countered this point by saying that satisfaction is not tied to antibiotic prescription, and that physicians often misjudge what patients want. It’s important to communicate other treatment options because patients often just want “something they can do.”
- Decision fatigue is often a factor. Evidence shows that antibiotic prescription is more frequent toward the end of a shift. Doctors should avoid negotiation because it increases consultation time. Here, foreshadowing early on may help. Setting may also be important – prescription is more frequent in the ED.
- Vaccine-resistant parents often want active treatment. Here, conversations can be challenging. Trying to persuade may be a less successful than giving positive instruction (e.g., “we’ll give you a vaccine today.”) Resistance is likely to be lower.
- Concern was expressed about manipulating patients ahead of a firm diagnosis. Could this lead to missing a serious bacterial infection? Dr. Stivers acknowledged that this was a gamble. She recommended a “neutral” early foreshadowing statement such as “we are seeing a lot of viral infections at the present.”
- Cultural differences can have an effect. In China, for example, the argument between parents and physicians no longer focuses on antibiotics versus nonantibiotics but rather on oral versus intravenous administration.
- Litigation is a factor in prescribing, especially in the United States. Dr. Stivers stated that her proposed approach to prescribing should not interfere with appropriate management. The clinical picture can change, and antibiotics should be prescribed where needed.
- Audits improve prescribing in the short term. These results were based on recorded consultations, and that factor may have influenced management. In unrecorded consultations, inappropriate antibiotic prescription would be higher.
- Increased point-of-care testing can reduce unnecessary prescribing. This has been documented in countries such as Sweden. Evidence from China suggests that many patients will still receive antibiotics even if a bacterial cause is excluded.
When patients dictate treatment, sometimes we must tell them what is best. Dr. Stivers closed her presentation by emphasizing that, “how you say things will matter.”
Louis Bont, MD, PhD, chair of this session and pediatric infectious diseases specialist at the University Medical Center Utrecht (the Netherlands), commented: “Antimicrobial resistance is a global health threat which jeopardizes sustainable health goals. The World Health Organization has declared that antimicrobial resistance is one of the top 10 global public health threats facing humanity. Resistance to ciprofloxacin varies from 8%-93% in Escherichia coli and 4%-80% in Klebsiella pneumoniae. Colistin is the only last-resort treatment for life-threatening infections caused by carbapenem-resistant enterobacteriaceae.”
Dr. Stivers stated that she has nothing to disclose.
FROM ESPID 2020
C. difficile control could require integrated approach
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
Clostridioides difficile (C. diff) infection (CDI) is a pathogen of both humans and animals, and to control it will require an integrated approach that encompasses human health care, veterinary health care, environmental regulation, and public policy. That is the conclusion of a group led by Su-Chen Lim, MD, and Tom Riley, MD, of Edith Cowan University in Australia, who published a review in Clinical Microbiology and Infection.
CDI was generally considered a nuisance infection until the early 21st century, when a hypervirulent fluoroquinolone-resistant strain emerged in North America. The strain is now documented In the United States, Canada, and most countries in Europe.
Another new feature of CDI is increased evidence of community transmission, which was previously rare. This is defined as cases where the patient experienced symptom onset outside the hospital, and had no history of hospitalization in the previous 12 weeks or symptom onset within 48 hours of hospital admission. Community-associated CDI now accounts for 41% of U.S. cases, nearly 30% of Australian cases, and about 14% in Europe, according to recent studies.
Several features of CDI suggest a need for an integrated management plan. The preferred habitat of C. diff is the gastrointestinal track of mammals, and likely colonizes all mammalian neonates. Over time, colonization by other microbes likely crowd it out and prevent overgrowth. But widespread use of antimicrobials in animal production can lead to the creation of an environment resembling that of the neonate, allowing C. diff to expand. That has led to food animals becoming a major C. diff reservoir, and whole-genome studies showed that strains found in humans, food, animals, and the environment are closely related and sometimes genetically indistinguishable, suggesting transmission between humans and animals that may be attributable to contaminated food and environments.
The authors suggest that C. diff infection control should be guided by the One Health initiative, which seeks cooperation between physicians, osteopathic physicians, veterinarians, dentists, nurses, and other scientific and environmental disciplines. The goal is to enhance surveillance and interdisciplinary communication, as well as integrated policies. The authors note that C. diff is often thought of by physicians as primarily a hospital problem, who may be unaware of the increased prevalence of community-acquired disease. It is also a significant problem in agriculture, since as many as 50% of piglets succumb to the disease. Other studies have recently shown that asymptomatic carriers of toxigenic strains are likely to transmit the bacteria to C. diff-negative patients. Asymptomatic carriers cluster with symptomatic patients. In one Cleveland hospital, more than 25% of hospital-associated CDI cases were found to have been colonized prior to admission, suggesting that these were not true hospital-associated cases.
C. diff has been isolated from a wide range of sources, including food animals, meat, seafood, vegetables, household environments, and natural environments like rivers, lakes, and soil. About 20% of calves and 70% of piglets are colonized with C. diff. It has a high prevalence in meat products in the United States, but lower in the Europe, possibly because of different slaughtering practices.
The authors suggest that zoonotic C. diff spread is unlikely to be confined to any geographic region or population, and that widespread C. diff contamination is occurring through food or the environment. This could be occurring because spores can withstand cooking temperatures and disseminate through the air, and even through manure from food animals made into compost or fertilizer.
Veterinary efforts mimicking hospital measures have reduced animal CDI, but there are no rapid diagnostic tests for CDI in animals, making it challenging to control its spread in this context.
The authors call for enhanced antimicrobial stewardship in both human and animal settings, including banning of antimicrobial agents as growth promoters. This has been done in the United States and Europe, but not in Brazil, China, Canada, India, and Australia. They also call for research on inactivation of C. diff spores during waste treatment.
Even better, the authors suggest that vaccines should be developed and employed in both animals and humans. No such vaccine exists in animals, but Pfizer has one for humans in a phase 3 clinical trial, but it does not prevent colonization. Others are in development.
The epidemiology of CDI is an ongoing challenge, with emerging new strains and changing social and environmental conditions. “However, it is with the collaborative efforts of industry partners, policymakers, veterinarians, clinicians, and researchers that CDI needs to be approached, a perfect example of One Health. Opening an interdisciplinary dialogue to address CDI and One Health issues has to be the focus of future studies,” the authors concluded.
SOURCE: SC Lim et al. Clinical Microbiology and Infection. 2020;26:85-863.
FROM CLINICAL MICROBIOLOGY AND INFECTION
Real-world safety, efficacy found for fecal transplants
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Antibiotic resistance: Personal responsibility in somewhat short supply
Most primary care physicians agree that antibiotic resistance and inappropriate prescribing are problems in the United States, but they are much less inclined to recognize these issues in their own practices, according to the results of a nationwide survey.
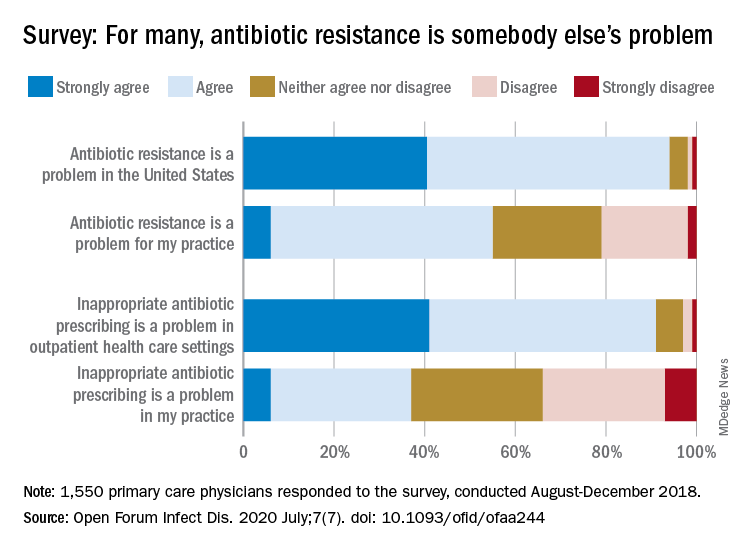
Rachel M. Zetts, MPH, of the Pew Charitable Trusts, Washington, D.C., and associates wrote in Open Forum Infectious Diseases.
Almost all (94%) of the 1,550 internists, family physicians, and pediatricians who responded to the survey said that antibiotic resistance is a national problem, and nearly that many (91%) agreed that “inappropriate antibiotic prescribing is a problem in outpatient health care settings,” the investigators acknowledged.
Narrowing the focus to their own practices, however, changed some opinions. At that level, only 55% of the respondents said that resistance was a problem for their practices, and just 37% said that there any sort of inappropriate prescribing going on, based on data from the survey, which was conducted from August to October 2018 by Pew and the American Medical Association.
Antibiotic stewardship, defined as activities meant to ensure appropriate prescribing of antibiotics, should include “staff and patient education, clinician-level antibiotic prescribing feedback, and communications training on how to discuss antibiotic prescribing with patients,” Ms. Zetts and associates explained.
The need for such stewardship in health care settings was acknowledged by 72% of respondents, but 53% of those surveyed also said that all they need to do to support such efforts “is to talk with their patients about the value of an antibiotic for their symptoms,” they noted.
The bacteria, it seems, are not the only ones with some resistance. Half of the primary care physicians believe that it would be difficult to fairly and accurately track the appropriate use of antibiotics, and 52% agreed with the statement that “practice-based reporting requirements for antibiotic use would be too onerous,” the researchers pointed out.
“Antibiotic resistance is an impending public health crisis. We are seeing today, as we respond to the COVID-19 pandemic, what our health system looks like with no or limited treatments available to tackle an outbreak. … We must all remain vigilant in combating the spread of antibiotic resistant bacteria and be prudent when prescribing antibiotics,” AMA President Susan R. Bailey, MD, said in a written statement.
SOURCE: Zetts RM et al. Open Forum Infect Dis. 2020 July;7(7). doi: 10.1093/ofid/ofaa244.
Most primary care physicians agree that antibiotic resistance and inappropriate prescribing are problems in the United States, but they are much less inclined to recognize these issues in their own practices, according to the results of a nationwide survey.
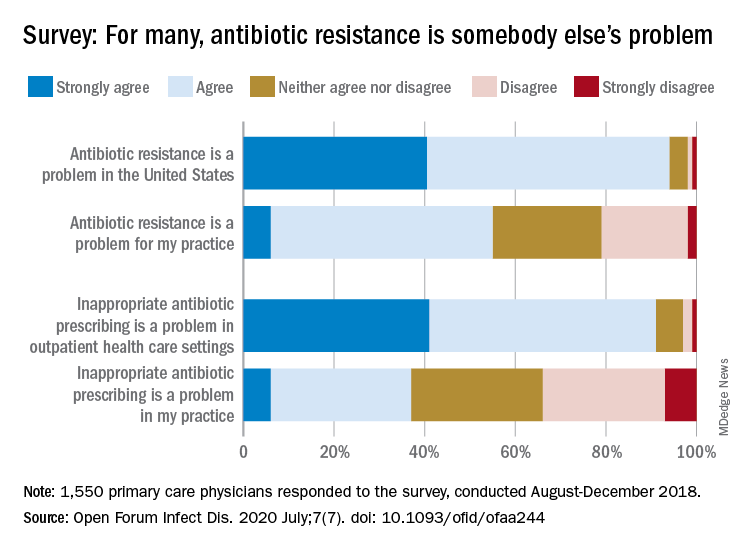
Rachel M. Zetts, MPH, of the Pew Charitable Trusts, Washington, D.C., and associates wrote in Open Forum Infectious Diseases.
Almost all (94%) of the 1,550 internists, family physicians, and pediatricians who responded to the survey said that antibiotic resistance is a national problem, and nearly that many (91%) agreed that “inappropriate antibiotic prescribing is a problem in outpatient health care settings,” the investigators acknowledged.
Narrowing the focus to their own practices, however, changed some opinions. At that level, only 55% of the respondents said that resistance was a problem for their practices, and just 37% said that there any sort of inappropriate prescribing going on, based on data from the survey, which was conducted from August to October 2018 by Pew and the American Medical Association.
Antibiotic stewardship, defined as activities meant to ensure appropriate prescribing of antibiotics, should include “staff and patient education, clinician-level antibiotic prescribing feedback, and communications training on how to discuss antibiotic prescribing with patients,” Ms. Zetts and associates explained.
The need for such stewardship in health care settings was acknowledged by 72% of respondents, but 53% of those surveyed also said that all they need to do to support such efforts “is to talk with their patients about the value of an antibiotic for their symptoms,” they noted.
The bacteria, it seems, are not the only ones with some resistance. Half of the primary care physicians believe that it would be difficult to fairly and accurately track the appropriate use of antibiotics, and 52% agreed with the statement that “practice-based reporting requirements for antibiotic use would be too onerous,” the researchers pointed out.
“Antibiotic resistance is an impending public health crisis. We are seeing today, as we respond to the COVID-19 pandemic, what our health system looks like with no or limited treatments available to tackle an outbreak. … We must all remain vigilant in combating the spread of antibiotic resistant bacteria and be prudent when prescribing antibiotics,” AMA President Susan R. Bailey, MD, said in a written statement.
SOURCE: Zetts RM et al. Open Forum Infect Dis. 2020 July;7(7). doi: 10.1093/ofid/ofaa244.
Most primary care physicians agree that antibiotic resistance and inappropriate prescribing are problems in the United States, but they are much less inclined to recognize these issues in their own practices, according to the results of a nationwide survey.
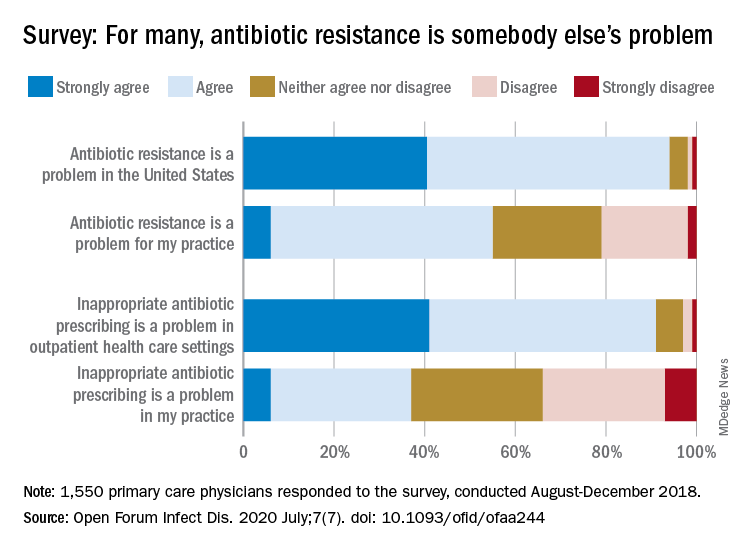
Rachel M. Zetts, MPH, of the Pew Charitable Trusts, Washington, D.C., and associates wrote in Open Forum Infectious Diseases.
Almost all (94%) of the 1,550 internists, family physicians, and pediatricians who responded to the survey said that antibiotic resistance is a national problem, and nearly that many (91%) agreed that “inappropriate antibiotic prescribing is a problem in outpatient health care settings,” the investigators acknowledged.
Narrowing the focus to their own practices, however, changed some opinions. At that level, only 55% of the respondents said that resistance was a problem for their practices, and just 37% said that there any sort of inappropriate prescribing going on, based on data from the survey, which was conducted from August to October 2018 by Pew and the American Medical Association.
Antibiotic stewardship, defined as activities meant to ensure appropriate prescribing of antibiotics, should include “staff and patient education, clinician-level antibiotic prescribing feedback, and communications training on how to discuss antibiotic prescribing with patients,” Ms. Zetts and associates explained.
The need for such stewardship in health care settings was acknowledged by 72% of respondents, but 53% of those surveyed also said that all they need to do to support such efforts “is to talk with their patients about the value of an antibiotic for their symptoms,” they noted.
The bacteria, it seems, are not the only ones with some resistance. Half of the primary care physicians believe that it would be difficult to fairly and accurately track the appropriate use of antibiotics, and 52% agreed with the statement that “practice-based reporting requirements for antibiotic use would be too onerous,” the researchers pointed out.
“Antibiotic resistance is an impending public health crisis. We are seeing today, as we respond to the COVID-19 pandemic, what our health system looks like with no or limited treatments available to tackle an outbreak. … We must all remain vigilant in combating the spread of antibiotic resistant bacteria and be prudent when prescribing antibiotics,” AMA President Susan R. Bailey, MD, said in a written statement.
SOURCE: Zetts RM et al. Open Forum Infect Dis. 2020 July;7(7). doi: 10.1093/ofid/ofaa244.
FROM OPEN FORUM INFECTIOUS DISEASES
Simplifying the antibiotic selection process
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
Hospitalists are constantly battling infection.
James Soo Kim, MD, a hospitalist and assistant professor at Emory Healthcare in Atlanta, a presenter of the session “Antibiotics Made Ridiculously Simple” during HM20 Virtual, said that while he has given this talk at previous Society of Hospital Medicine Annual Conferences, the presentation has undergone significant changes over the years as the landscape of infectious disease treatment has shifted.
He hopes attendees of HM20 Virtual will appreciate the changes and encourages those who have attended his presentation in previous years to come see what is new, but admitted newcomers may think the presentation’s title is a bit of a misnomer.
“Despite the title of the talk, there really isn’t any way to make antibiotics ridiculously simple,” he said.
Dr. Kim, who is also an editorial board member for The Hospitalist, said the origin of “Antibiotics Made Ridiculously Simple” took place during his residency, where he had an interest in infectious disease. This interest carried over to his time in fellowship at the Keck School of Medicine of the University of Southern California – and was enough to become board certified in infectious disease by the American Board of Internal Medicine. Infectious disease continues to interest him now as an attending, he said, and since he joined Emory Healthcare in 2012, he has given a version of this presentation every year.
HM20 Virtual attendees will come away from the presentation with an idea of how to choose an antibiotic regimen, Dr. Kim said, including how to select an antibiotic when you’re worried about Pseudomonas, methicillin-resistant Staphylococcus aureus, and vancomycin-resistant Enterococcus or other likely organisms. “There are a variety of drugs out there that have activity against our ‘usual suspects,’ ” he said.
Attendees will also learn to select antibiotic options that have empiric coverage during a shortage of piperacillin/tazobactam (Zosyn), vancomycin, or your preferred drug of choice for treating common infections. He will also review the latest drugs that have been released over the past few years so attendees can add them to their armamentarium.
“I won’t necessarily expect attendees to use everything I talk about, but if you have a patient on service that infectious disease started Vabomere on, you’ll at least have a general idea of what they were worried about,” Dr. Kim said.
One practice pearl he hopes attendees take away from his presentation: Allergies to beta-lactam antibiotics like penicillin (PCN) derivatives are not as common as most providers and patients believe, and not giving these antibiotics to patients can actually decrease the chance that the patient gets appropriate therapy while also increasing the cost of care.
“I hope that my talk changes practice by making people aware of how infrequent true clinically significant PCN cross-reactions are so that patients can get more cost-effective and medically effective therapy,” he said.Dr. Kim reports no relevant financial disclosures.
Antibiotics Made Ridiculously Simple Live Q&A: Tuesday, August 18, 3:30-4:30 p.m.
ID dermatology: Advancements, but new challenges, over 50 years
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
When Stephen Tyring, MD, PhD, an infectious disease dermatologist, started his career in the early 1980s, he said “we were diagnosing Kaposi’s sarcoma right and left. We would see a new case every day or two.”
It was the early days of the HIV/AIDS epidemic, and dermatologists were at the forefront because HIV/AIDS often presented with skin manifestations. Dr. Tyring, clinical professor in the departments of dermatology, microbiology & molecular genetics and internal medicine at the University of Texas Health Science Center, Houston, and his colleagues referred Kaposi’s patients for chemotherapy and radiation, but the outlook was often grim, especially if lesions developed in the lungs.
Dermatologist don’t see much Kaposi’s anymore because of highly effective treatments for HIV.
Members of the original editorial advisory board saw it coming. In a feature in which board members provided their prediction for the 1970s that appeared in the first issue, New York dermatologist Norman Orentreich, MD, counted the “probable introduction of virucidal agents” as one of the “significant advances or changes that I foresee in the next 10 years.” J. Lamar Callaway, MD, professor of dermatology at Duke University, Durham, N.C., predicted that “the next 10 years should develop effective anti-viral agents for warts, herpes simplex, and herpes zoster.”
To celebrate the 50th anniversary of Dermatology News, we are looking back at how the field has changed since that first issue. The focus this month is infectious disease. There’s a lot to be grateful for but there are also challenges like antibiotic resistance that weren’t on the radar screens of Dr. Orentreich, Dr. Callaway, and their peers in 1970.
All in all, “the only thing I wish we did the old way is sit at the bedside and talk to patients more. We rely so much on technology now that we sometimes lose the art of medicine, which is comforting to the patient,” said Theodore Rosen, MD, an ID dermatologist and professor of dermatology at Baylor College of Medicine, Houston, who’s been in practice for 42 years.
“A lot of advancements against herpes viruses”
One of the biggest wins for ID dermatology over the last 5 decades has been the management of herpes, both herpes simplex virus 1 and 2, as well as herpes zoster virus. It started with the approval of acyclovir in 1981. Before then, “we had no direct therapy for genital herpes, herpes zoster, or disseminated herpes in immunosuppressed or cancer patients,” Dr. Rosen said.
“I can remember doing an interview with Good Morning America when I gave the first IV dose of acyclovir in the city of Houston for really bad disseminated herpes” in an HIV patient, he said, and it worked.
Two derivatives, valacyclovir and famciclovir, became available in the mid-1990s, so today “we have three drugs and some others at the periphery that are all highly effective not only” against herpes, but also for preventing outbreaks; valacyclovir can even prevent asymptomatic shedding, therefore possibly preventing new infections. “That’s a concept we didn’t even have 40 years ago,” Dr. Rosen said.
Cidofovir has also made a difference. The IV formulation was approved for AIDS-associated cytomegalovirus retinitis in 1996 but discontinued a few years later amid concerns of severe renal toxicity. It’s found a new home in dermatology since then, explained ID dermatologist Carrie Kovarik, MD, associate professor of dermatology at the University of Pennsylvania, Philadelphia.
Dermatologists see acyclovir-resistant herpes “heaped up on the genitals in HIV patients,” and there weren’t many options in the past. A few years ago, “we [tried] injecting cidofovir directly into the skin lesions, and it’s been remarkably successful. It is a good way to treat these lesions” if dermatologists can get it compounded, she said.
Shingles vaccines, first the live attenuated zoster vaccine (Zostavax) approved by the Food and Drug Administration in 2006 and the more effective recombinant zoster vaccine (Shingrix) approved in 2017, have also had a significant impact.
Dr. Rosen remembers what it was like when he first started practicing over 40 years ago. Not uncommonly, “we saw horrible cases of shingles,” including one in his uncle, who was left with permanent hand pain long after the rash subsided.
Today, “I see much less shingles, and when I do see it, it’s in a much-attenuated form. [Shingrix], even if it doesn’t prevent the disease, often prevents postherpetic neuralgia,” he said.
Also, with pediatric vaccinations against chicken pox, “we’re probably going to see a whole new generation without shingles, which is huge. We’ve made a lot of advancements against herpes viruses,” Dr. Kovarik said.
“We finally found something that helps”
“We’ve [also] come a really long way with genital wart treatment,” Dr. Kovarik said.
It started with approval of topical imiquimod in 1997. “Before that, we were just killing one wart here and one wart there” but they would often come back and pop up in other areas. Injectable interferon was an option at the time, but people didn’t like all the needles.
With imiquimod, “we finally [had] a way to target HPV [human papillomavirus] and not just scrape” or freeze one wart at a time, and “we were able to generate an inflammatory response in the whole area to clear the virus.” Working with HIV patients, “I see sheets and sheets of confluent warts throughout the whole genital area; to try to freeze that is impossible. Now I have a way to get rid of [genital] warts and keep them away even if you have a big cluster,” she said.
“Sometimes, we’ll do both liquid nitrogen and imiquimod. That’s a good way to tackle people who have a high burden of warts,” Dr. Kovarik noted. Other effective treatments have come out as well, including an ointment formulation of sinecatechins, extracted from green tea, “but you have to put it on several times a day, and insurance companies don’t cover it often,” she said.
Intralesional cidofovir is also proving to be boon for potentially malignant refractory warts in HIV and transplant patients. “It’s an incredible treatment. We can inject that antiviral into warts and get rid of them. We finally found something that helps” these people, Dr. Kovarik said.
The HPV vaccine Gardasil is making a difference, as well. In addition to cervical dysplasia and anogenital cancers, it protects against two condyloma strains. Dr. Rosen said he’s seeing fewer cases of genital warts now than when he started practicing, likely because of the vaccine.
“Organisms that weren’t pathogens are now pathogens”
Antibiotic resistance probably tops the list for what’s changed in a bad way in ID dermatology since 1970. Dr. Rosen remembers at the start of his career that “we never worried about antibiotic resistance. We’d put people on antibiotics for acne, rosacea, and we’d keep them on them for 3 years, 6 years”; resistance wasn’t on the radar screen and was not mentioned once in the first issue of Dermatology News, which was packed with articles and ran 24 pages.
The situation is different now. Driven by decades of overuse in agriculture and the medical system, antibiotic resistance is a concern throughout medicine, and unfortunately, “we have not come nearly as far as fast with antibiotics,” at least the ones dermatologists use, “as we have with antivirals,” Dr. Tyring said.
For instance, methicillin-resistant Staphylococcus aureus (MRSA), first described in the United States in 1968, is “no longer the exception to the rule, but the rule” itself, he said, with carbuncles, furuncles, and abscesses not infrequently growing out MRSA. There are also new drug-resistant forms of old problems like gonorrhea and tuberculosis, among other developments, and impetigo has shifted since 1970 from mostly a Streptococcus infection easily treated with penicillin to often a Staphylococcus disease that’s resistant to it. There’s also been a steady march of new pathogens, including the latest one, SARS-CoV-2, the virus that causes COVID-19, which has been recognized as having a variety of skin manifestations.
“No matter how smart we think we are, nature has a way of putting us back in our place,” Dr. Rosen said.
The bright spot is that “we’ve become very adept at identifying and characterizing” microbes “based on techniques we didn’t even have when I started practicing,” such as polymerase chain reaction. “It has taken a lot of guess work out of treating infectious diseases,” he said.
The widespread use of immunosuppressives such as cyclophosphamide, mycophenolate, azathioprine, rituximab, and other agents used in conjunction with solid organ transplantation, has also been a challenge. “We are seeing infections with really odd organisms. Just recently, I had a patient with fusarium in the skin; it’s a fungus that lives in the dirt. I saw a patient with a species of algae” that normally lives in stagnant water, he commented. “We used to get [things like that] back on reports, and we’d throw them away. You can’t do that anymore. Organisms that weren’t pathogens in the past are now pathogens,” particularly in immunosuppressed people, Dr. Rosen said.
Venereologists no more
There’s been another big change in the field. “Back in the not too distant past, dermatologists in the U.S. were referred to as ‘dermatologist-venereologists.’ ” It goes back to the time when syphilis wasn’t diagnosed and treated early, so patients often presented with secondary skin complications and went to dermatologists for help. As a result, “dermatologists became the most experienced at treating it,” Dr. Tyring said.
That’s faded from practice. Part of the reason is that as late as 2000, syphilis seemed to be on the way out; the Centers for Disease and Control and Prevention even raised the possibility of elimination. Dermatologists turned their attention to other areas.
It might have been short-sighted, Dr. Rosen said. Syphilis has made a strong comeback, and drug-resistant gonorrhea has also emerged globally and in at least a few states. No other medical field has stepped in to take up the slack. “Ob.gyns. are busy delivering babies, ID [physicians are] concerned about HIV, and urologists are worried about kidney stones and cancer.” Other than herpes and genital warts, “we have not done well” with management of sexually transmitted diseases, he said.
“I could sense” his frustration
The first issue of Dermatology News carried an article and photospread about scabies that could run today, except that topical permethrin and oral ivermectin have largely replaced benzyl benzoate and sulfur ointments for treatment in the United States. In the article, Scottish dermatologist J. O’D. Alexander, MD, called scabies “the scourge of mankind” and blamed it’s prevalence on “an offhand attitude to the disease which makes control very difficult.”
“I could sense this man’s frustration that people were not recognizing scabies,” Dr. Kovarik said, and it’s no closer to being eradicated than it was in 1970. “It’s still around, and we see it in our clinics. It’s a horrible disease in kids we see in dermatology not infrequently,” and treatment has only advanced a bit.
The article highlights what hasn’t changed much in ID dermatology over the years. Common warts are another one. “With all the evolution in medicine, we don’t have any better treatments approved for common warts than we ever had.” Injecting cidofovir “works great,” but access is a problem, Dr. Tyring said.
Onychomycosis has also proven a tough nut to crack. Readers back in 1970 counted the introduction of the antifungal, griseofulvin, as a major advancement in the 1960s; it’s still a go-to for tinea capitis, but it didn’t work very well for toenail fungus. Terbinafine (Lamisil), approved in 1993, and subsequent developments have helped, but the field still awaits more effective options; a few potential new agents are in the pipeline.
Although there have been major advancements for serious systemic fungal infections, “we’ve mainly seen small steps forward” in ID dermatology, Dr. Tyring said.
Dr. Tyring, Dr. Kovarik, and Dr. Rosen said they had no relevant disclosures.
FMT may improve outcomes without clearing multidrug-resistant organisms
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
FROM DDW 2020
Antibiotic resistance rises among pneumococcus strains in kids
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
FROM CLINICAL INFECTIOUS DISEASES
Children with resistant UTIs unexpectedly may respond to discordant antibiotics
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
FROM PEDIATRICS













