User login
Novel gene therapy offers hope for some lymphomas
Not all patients with relapsed or refractory large B cell lymphoma (r/r LBCL) are candidates for high-dose chemotherapy or hematopoietic stem cell transplantation (HSCT), and options for second-line therapies for this population are limited, said Dr. Alison Sehgal of the University of Pittsburgh Medical Center in her presentation of the findings.
Lisocabtagene maraleucel (liso-cel) is a CD19-directed CAR T-cell product. In a previous phase 3 randomized trial (the TRANSFORM study), lisocabtagene showed superiority over salvage chemotherapy for LBCL patients who were fit candidates for stem cell transplant, but its use in older, frail patients who are not transplant candidates remains uncertain, wrote Dr. Sehgal and colleagues in their poster at the meeting.
In the study, the researchers identified 74 patients with r/r LBCL. Of these, 61 were treated with liso-cel. The patients ranged in age from 53 to 84 years, with a median age of 74 years, 61% were male, and 89% were white. Approximately half were refractory and half were relapsed.
For the therapy, patients underwent lymphodepletion with cyclophosphamide and fludarabine, followed 2-7 days later by an infusion of liso-cel at a target dose of 100 x 106 CAR+ T cells; all patients had at least 6 months of follow-up from their first response.
The primary endpoint of overall response rate occurred in 80% of the patients, and clinically meaningful complete response occurred in 54% over a median follow-up of 12.3 months.
“Clinically meaningful CRs were observed across all subgroups,” Dr. Sehgal said in her presentation.
The response lasted a median of 21.7 months, and the median follow-up for duration of response was 15.5 months. The median overall survival was not reached, but the median progression-free survival was 9.0 months, with a median follow-up period of 13.0 months.
Responses occurred across all prespecified subgroups, with no significant differences in either safety or efficacy based on hematopoietic cell transplantation–specific comorbidity index (HCT-CI) scores.
“Despite the advanced age and comorbidities of the population, the safety profile was consistent with previous reports,” and no new or increased safety signals appeared, Dr. Sehgal said.
The most common treatment-emergent adverse events of grade 3 or higher were neutropenia (48%), leukopenia (21%), thrombocytopenia (20%), and anemia (11%). Cytokine-release syndrome (CRS) occurred in 23 patients (38%); of these, 1 patient was grade 3 and none were grades 4 or 5.
Approximately one-third of the patients (31%) experienced neurological events during the study; three cases were grade 3, none were grades 4 or 5. Patients with CRS or NE were treated with tocilizumab (10%), corticosteroids (3%), or both (20%). Treatment-emergent adverse events of grade 3 or higher occurred in 79% of patients overall, including grade 5 events in two patients because of COVID-19.
The study findings were limited by the small sample size and lack of controls. However, the results support the potential use of liso-cel as a second-line therapy for r/r LBCL patients who are not candidates for HSCT, Dr. Sehgal concluded.
Addressing an ongoing unmet need
In an interview, study coauthor Dr. Leo I. Gordon of Northwestern University, Chicago, observed, “Patients with relapsed or refractory large B-cell lymphoma who are not considered candidates for stem cell transplant following first-line treatment, based on age, comorbidities, health status, or other prognostic factors, have more difficult-to-treat disease, poor prognosis, and more limited treatment options.”
Dr. Gordon noted that the PILOT study is the only trial to evaluate a CAR T-cell therapy as a second-line treatment for r/r LBCL patients who are not considered candidates for stem cell transplant.
“Data from the primary analysis of the PILOT study further demonstrate the potential value of using CAR T-cell therapies earlier in the treatment paradigm for relapsed or refractory LBCL to help improve clinical outcomes and address ongoing unmet need,” he said.
CAR T-cell therapies have shown benefits in later lines for r/r LBCL and as a second-line treatment for r/r LBCL patients who are deemed candidates for stem cell transplant, “so we were encouraged and not surprised by these data.”
However, Dr. Gordon noted, “There may be some patients with similar presentations that might have a transplant, so one limitation of the trial is how one defines patients where transplant is the intended therapy, and that assessment varies among institutions and clinicians.”
An application for liso-cel as a treatment for patients with r/r LBCL who have failed front-line therapy is currently under Priority Review with the FDA, with a Prescription Drug User Fee Act (PDUFA) goal date of June 24, 2022, he added.
Liso-cel may fill treatment gap as second-line therapy
The current study is important because “the long-term outcomes of patients with relapsed or refractory large B-cell lymphoma who are not candidates for stem cell transplantation is very poor,” said Dr. Brian Till of Fred Hutchinson Cancer Research Center, Seattle, in an interview.
“CAR T therapy leads to about a 40% cure rate, but is currently only available in this population after the failure of second-line therapy,” said Dr. Till, who was not involved in the study.
“Given that liso-cel was shown to improve outcomes in the second-line setting among transplant candidates, it is logical to consider it as second-line therapy in nontransplant candidates as well, who are otherwise fit enough to receive CAR T therapy,” Dr. Till explained.
“This study showed a rate of long-term progression-free survival similar to what has been observed in the third-line setting and was reasonably well tolerated in these older patients,” said Dr. Till. The results suggest “that second-line liso-cel may be an attractive treatment strategy for patients who are not candidates for stem cell transplantation due to advanced age or comorbidities,” he noted.
Dr. Till had no relevant financial conflicts to disclose.
The study was funded by Bristol Myers Squibb.
Not all patients with relapsed or refractory large B cell lymphoma (r/r LBCL) are candidates for high-dose chemotherapy or hematopoietic stem cell transplantation (HSCT), and options for second-line therapies for this population are limited, said Dr. Alison Sehgal of the University of Pittsburgh Medical Center in her presentation of the findings.
Lisocabtagene maraleucel (liso-cel) is a CD19-directed CAR T-cell product. In a previous phase 3 randomized trial (the TRANSFORM study), lisocabtagene showed superiority over salvage chemotherapy for LBCL patients who were fit candidates for stem cell transplant, but its use in older, frail patients who are not transplant candidates remains uncertain, wrote Dr. Sehgal and colleagues in their poster at the meeting.
In the study, the researchers identified 74 patients with r/r LBCL. Of these, 61 were treated with liso-cel. The patients ranged in age from 53 to 84 years, with a median age of 74 years, 61% were male, and 89% were white. Approximately half were refractory and half were relapsed.
For the therapy, patients underwent lymphodepletion with cyclophosphamide and fludarabine, followed 2-7 days later by an infusion of liso-cel at a target dose of 100 x 106 CAR+ T cells; all patients had at least 6 months of follow-up from their first response.
The primary endpoint of overall response rate occurred in 80% of the patients, and clinically meaningful complete response occurred in 54% over a median follow-up of 12.3 months.
“Clinically meaningful CRs were observed across all subgroups,” Dr. Sehgal said in her presentation.
The response lasted a median of 21.7 months, and the median follow-up for duration of response was 15.5 months. The median overall survival was not reached, but the median progression-free survival was 9.0 months, with a median follow-up period of 13.0 months.
Responses occurred across all prespecified subgroups, with no significant differences in either safety or efficacy based on hematopoietic cell transplantation–specific comorbidity index (HCT-CI) scores.
“Despite the advanced age and comorbidities of the population, the safety profile was consistent with previous reports,” and no new or increased safety signals appeared, Dr. Sehgal said.
The most common treatment-emergent adverse events of grade 3 or higher were neutropenia (48%), leukopenia (21%), thrombocytopenia (20%), and anemia (11%). Cytokine-release syndrome (CRS) occurred in 23 patients (38%); of these, 1 patient was grade 3 and none were grades 4 or 5.
Approximately one-third of the patients (31%) experienced neurological events during the study; three cases were grade 3, none were grades 4 or 5. Patients with CRS or NE were treated with tocilizumab (10%), corticosteroids (3%), or both (20%). Treatment-emergent adverse events of grade 3 or higher occurred in 79% of patients overall, including grade 5 events in two patients because of COVID-19.
The study findings were limited by the small sample size and lack of controls. However, the results support the potential use of liso-cel as a second-line therapy for r/r LBCL patients who are not candidates for HSCT, Dr. Sehgal concluded.
Addressing an ongoing unmet need
In an interview, study coauthor Dr. Leo I. Gordon of Northwestern University, Chicago, observed, “Patients with relapsed or refractory large B-cell lymphoma who are not considered candidates for stem cell transplant following first-line treatment, based on age, comorbidities, health status, or other prognostic factors, have more difficult-to-treat disease, poor prognosis, and more limited treatment options.”
Dr. Gordon noted that the PILOT study is the only trial to evaluate a CAR T-cell therapy as a second-line treatment for r/r LBCL patients who are not considered candidates for stem cell transplant.
“Data from the primary analysis of the PILOT study further demonstrate the potential value of using CAR T-cell therapies earlier in the treatment paradigm for relapsed or refractory LBCL to help improve clinical outcomes and address ongoing unmet need,” he said.
CAR T-cell therapies have shown benefits in later lines for r/r LBCL and as a second-line treatment for r/r LBCL patients who are deemed candidates for stem cell transplant, “so we were encouraged and not surprised by these data.”
However, Dr. Gordon noted, “There may be some patients with similar presentations that might have a transplant, so one limitation of the trial is how one defines patients where transplant is the intended therapy, and that assessment varies among institutions and clinicians.”
An application for liso-cel as a treatment for patients with r/r LBCL who have failed front-line therapy is currently under Priority Review with the FDA, with a Prescription Drug User Fee Act (PDUFA) goal date of June 24, 2022, he added.
Liso-cel may fill treatment gap as second-line therapy
The current study is important because “the long-term outcomes of patients with relapsed or refractory large B-cell lymphoma who are not candidates for stem cell transplantation is very poor,” said Dr. Brian Till of Fred Hutchinson Cancer Research Center, Seattle, in an interview.
“CAR T therapy leads to about a 40% cure rate, but is currently only available in this population after the failure of second-line therapy,” said Dr. Till, who was not involved in the study.
“Given that liso-cel was shown to improve outcomes in the second-line setting among transplant candidates, it is logical to consider it as second-line therapy in nontransplant candidates as well, who are otherwise fit enough to receive CAR T therapy,” Dr. Till explained.
“This study showed a rate of long-term progression-free survival similar to what has been observed in the third-line setting and was reasonably well tolerated in these older patients,” said Dr. Till. The results suggest “that second-line liso-cel may be an attractive treatment strategy for patients who are not candidates for stem cell transplantation due to advanced age or comorbidities,” he noted.
Dr. Till had no relevant financial conflicts to disclose.
The study was funded by Bristol Myers Squibb.
Not all patients with relapsed or refractory large B cell lymphoma (r/r LBCL) are candidates for high-dose chemotherapy or hematopoietic stem cell transplantation (HSCT), and options for second-line therapies for this population are limited, said Dr. Alison Sehgal of the University of Pittsburgh Medical Center in her presentation of the findings.
Lisocabtagene maraleucel (liso-cel) is a CD19-directed CAR T-cell product. In a previous phase 3 randomized trial (the TRANSFORM study), lisocabtagene showed superiority over salvage chemotherapy for LBCL patients who were fit candidates for stem cell transplant, but its use in older, frail patients who are not transplant candidates remains uncertain, wrote Dr. Sehgal and colleagues in their poster at the meeting.
In the study, the researchers identified 74 patients with r/r LBCL. Of these, 61 were treated with liso-cel. The patients ranged in age from 53 to 84 years, with a median age of 74 years, 61% were male, and 89% were white. Approximately half were refractory and half were relapsed.
For the therapy, patients underwent lymphodepletion with cyclophosphamide and fludarabine, followed 2-7 days later by an infusion of liso-cel at a target dose of 100 x 106 CAR+ T cells; all patients had at least 6 months of follow-up from their first response.
The primary endpoint of overall response rate occurred in 80% of the patients, and clinically meaningful complete response occurred in 54% over a median follow-up of 12.3 months.
“Clinically meaningful CRs were observed across all subgroups,” Dr. Sehgal said in her presentation.
The response lasted a median of 21.7 months, and the median follow-up for duration of response was 15.5 months. The median overall survival was not reached, but the median progression-free survival was 9.0 months, with a median follow-up period of 13.0 months.
Responses occurred across all prespecified subgroups, with no significant differences in either safety or efficacy based on hematopoietic cell transplantation–specific comorbidity index (HCT-CI) scores.
“Despite the advanced age and comorbidities of the population, the safety profile was consistent with previous reports,” and no new or increased safety signals appeared, Dr. Sehgal said.
The most common treatment-emergent adverse events of grade 3 or higher were neutropenia (48%), leukopenia (21%), thrombocytopenia (20%), and anemia (11%). Cytokine-release syndrome (CRS) occurred in 23 patients (38%); of these, 1 patient was grade 3 and none were grades 4 or 5.
Approximately one-third of the patients (31%) experienced neurological events during the study; three cases were grade 3, none were grades 4 or 5. Patients with CRS or NE were treated with tocilizumab (10%), corticosteroids (3%), or both (20%). Treatment-emergent adverse events of grade 3 or higher occurred in 79% of patients overall, including grade 5 events in two patients because of COVID-19.
The study findings were limited by the small sample size and lack of controls. However, the results support the potential use of liso-cel as a second-line therapy for r/r LBCL patients who are not candidates for HSCT, Dr. Sehgal concluded.
Addressing an ongoing unmet need
In an interview, study coauthor Dr. Leo I. Gordon of Northwestern University, Chicago, observed, “Patients with relapsed or refractory large B-cell lymphoma who are not considered candidates for stem cell transplant following first-line treatment, based on age, comorbidities, health status, or other prognostic factors, have more difficult-to-treat disease, poor prognosis, and more limited treatment options.”
Dr. Gordon noted that the PILOT study is the only trial to evaluate a CAR T-cell therapy as a second-line treatment for r/r LBCL patients who are not considered candidates for stem cell transplant.
“Data from the primary analysis of the PILOT study further demonstrate the potential value of using CAR T-cell therapies earlier in the treatment paradigm for relapsed or refractory LBCL to help improve clinical outcomes and address ongoing unmet need,” he said.
CAR T-cell therapies have shown benefits in later lines for r/r LBCL and as a second-line treatment for r/r LBCL patients who are deemed candidates for stem cell transplant, “so we were encouraged and not surprised by these data.”
However, Dr. Gordon noted, “There may be some patients with similar presentations that might have a transplant, so one limitation of the trial is how one defines patients where transplant is the intended therapy, and that assessment varies among institutions and clinicians.”
An application for liso-cel as a treatment for patients with r/r LBCL who have failed front-line therapy is currently under Priority Review with the FDA, with a Prescription Drug User Fee Act (PDUFA) goal date of June 24, 2022, he added.
Liso-cel may fill treatment gap as second-line therapy
The current study is important because “the long-term outcomes of patients with relapsed or refractory large B-cell lymphoma who are not candidates for stem cell transplantation is very poor,” said Dr. Brian Till of Fred Hutchinson Cancer Research Center, Seattle, in an interview.
“CAR T therapy leads to about a 40% cure rate, but is currently only available in this population after the failure of second-line therapy,” said Dr. Till, who was not involved in the study.
“Given that liso-cel was shown to improve outcomes in the second-line setting among transplant candidates, it is logical to consider it as second-line therapy in nontransplant candidates as well, who are otherwise fit enough to receive CAR T therapy,” Dr. Till explained.
“This study showed a rate of long-term progression-free survival similar to what has been observed in the third-line setting and was reasonably well tolerated in these older patients,” said Dr. Till. The results suggest “that second-line liso-cel may be an attractive treatment strategy for patients who are not candidates for stem cell transplantation due to advanced age or comorbidities,” he noted.
Dr. Till had no relevant financial conflicts to disclose.
The study was funded by Bristol Myers Squibb.
FROM ASCO 2022
Glofitamab prevails against r/r DLBCL
“We know that relapsed diffuse large B-cell lymphoma has a particularly poor prognosis,” especially for patients who have undergone at least two therapies, Dr. Michael Dickinson, MBBS, of the University of Melbourne said in a presentation at the annual meeting of the American Society of Clinical Oncology.
Bispecific T cell–recruiting antibodies are emerging as a novel treatment option for B-cell cancers, said Dr. Dickinson.
Glofitamab is distinct among these therapies for its configuration that is bivalent for CD20 and monovalent for CD3, providing more potency than a 1:1 format, Dr. Dickinson explained in his presentation.
The study population included 154 adults aged 21-90 years with DLBCL who had received at least two prior treatments; all had received prior anti-CD20 Ab, and 149 had received anthracycline. The median age of the patients was 66 years, 65% were male, 75% had Ann Arbor stage III or IV disease, and 90% were refractory to any prior therapy.
The patients received intravenous glutamate-pyruvate transaminase, followed by an initial intravenous dose of glofitamab 7 days later. Glofitamab was given as step-up doses starting with 2.5 mg to a target of 30 mg.
The primary endpoint was complete response (CR) during initial treatment using Independent Review Committee (IRC) criteria, with overall response rate, duration of response, duration of complete response, progression-free survival, and overall survival as key secondary outcomes.
At a median of 12.6 months’ follow-up, the CR and overall response rates were 39.4% and 51.6%, respectively.
“Responses were achieved early; the median time to first complete response was 42 days,” Dr. Dickinson reported. Of the 38 patients with CR at the data cutoff point, 33 remained in complete remission (87%) based on IRC criteria. Complete response rates were consistent across prespecified subgroups, notably 42% of patients with no prior chimeric antigen receptor T-cell therapy and 70% and 34%, of those who were relapsed or refractory, respectively, to their last prior treatments.
The median duration of overall response was 18.4 months, and the median duration of complete response had not yet been estimated, Dr. Dickinson said. The median progression-free survival and overall survival rates were 4.9 months and 11.5 months, respectively, and the estimated 12-month overall survival was 49.8%.
“These are highly clinically significant results for this difficult to treat population,” Dr. Dickinson said in his presentation.
The most common adverse event was cytokine release syndrome (CRS), which occurred in 63% of patients. Of these, 3.9% were grade 3 or 4. Patients received corticosteroids (27.8%) or tocilizumab for management of CRS.
“As we have shown before, this is a first-course phenomenon, becoming far less frequent once step up dosing is complete,” Dr. Dickinson said in the presentation. “The median time to CRS is predictable, occurring around 10 hours after the IV infusion,” he said. Overall, 3.2% of the patients discontinued because of an adverse event.
A total of eight deaths occurred during the study; five of these were related to COVID-19 and the remaining three were in patients with manifest progression of disease.
Infections are to be expected in such a heavily treated population, and 14.9% of patients developed infections of grade 3 or higher, said Dr. Dickinson. Neutropenia of any grade occurred in 37.7%, febrile neutropenia in 2.6%. Neurological events occurred in 38.3% of patients; 3.2% were grade 3 or higher.
The study did not prospectively record immune effector cell–associated neurotoxicity syndrome, Dr. Dickinson said, but an estimate suggests a rate of 2.6%, and none of the events were considered to be related to glofitamab, he noted.
The researchers also looked at a supporting cohort of 35 patients with a median follow up of more than 2 years. In this group, the complete remission rate was 35% and the median duration of remission was 34.2 months. “Our six longest patients have been in remission for longer than 3 years,” Dr. Dickinson said.
The latest glofitamab data “reflect routine practice and an area of need for this disease,” said Dr. Dickinson.
“I think these results will prove to be very meaningful for our patients with large cell lymphoma, and this drug will prove to be an important treatment option,” he said.
More follow-up needed, but findings show promise
A number of CD20/CD3-bispecific antibodies are in development for patients with relapsed/refractory B-cell lymphomas, said study discussant Kerry J. Savage, MD, of the University of British Columbia, Vancouver, who served as the discussant for the session.
Glofitamab differs from other treatments in that it is bivalent for CD20 and monovalent for CD3, “which imparts greater potency,” she noted. Glofitamab also has a silent Fc region that is designed to extend half-life and reduce toxicity.
Patients in the current study had at least two prior regimens, and importantly, “CR rates were similar, regardless of prior therapy,” said Dr. Savage. The longer follow-up cohort provides “a hint that the response may be durable.”
Looking ahead, “the important thing will be response durability” with longer follow-up, she added. “We don’t know the curative potential yet, but the results are encouraging so far.”
In the meantime, “the best use of bispecific antibodies is through clinical trials,” Dr. Savage said. “Keep an eye out for bispecific antibody combination trials as well.”
The study was funded by F. Hoffmann–La Roche. Dr. Dickinson disclosed honoraria from or serving as a consultant to companies including Amgen, Bristol Myers-Squibb, Gilead Sciences, Janssen, MSD, Novartis, and Roche. Dr. Savage disclosed relationships, funding, and support from multiple companies including Bristol Myers-Squibb, Janssen Oncology, Kyowa, Merck, Novartis Canada Pharmaceuticals, Seattle Genetics and Roche.
“We know that relapsed diffuse large B-cell lymphoma has a particularly poor prognosis,” especially for patients who have undergone at least two therapies, Dr. Michael Dickinson, MBBS, of the University of Melbourne said in a presentation at the annual meeting of the American Society of Clinical Oncology.
Bispecific T cell–recruiting antibodies are emerging as a novel treatment option for B-cell cancers, said Dr. Dickinson.
Glofitamab is distinct among these therapies for its configuration that is bivalent for CD20 and monovalent for CD3, providing more potency than a 1:1 format, Dr. Dickinson explained in his presentation.
The study population included 154 adults aged 21-90 years with DLBCL who had received at least two prior treatments; all had received prior anti-CD20 Ab, and 149 had received anthracycline. The median age of the patients was 66 years, 65% were male, 75% had Ann Arbor stage III or IV disease, and 90% were refractory to any prior therapy.
The patients received intravenous glutamate-pyruvate transaminase, followed by an initial intravenous dose of glofitamab 7 days later. Glofitamab was given as step-up doses starting with 2.5 mg to a target of 30 mg.
The primary endpoint was complete response (CR) during initial treatment using Independent Review Committee (IRC) criteria, with overall response rate, duration of response, duration of complete response, progression-free survival, and overall survival as key secondary outcomes.
At a median of 12.6 months’ follow-up, the CR and overall response rates were 39.4% and 51.6%, respectively.
“Responses were achieved early; the median time to first complete response was 42 days,” Dr. Dickinson reported. Of the 38 patients with CR at the data cutoff point, 33 remained in complete remission (87%) based on IRC criteria. Complete response rates were consistent across prespecified subgroups, notably 42% of patients with no prior chimeric antigen receptor T-cell therapy and 70% and 34%, of those who were relapsed or refractory, respectively, to their last prior treatments.
The median duration of overall response was 18.4 months, and the median duration of complete response had not yet been estimated, Dr. Dickinson said. The median progression-free survival and overall survival rates were 4.9 months and 11.5 months, respectively, and the estimated 12-month overall survival was 49.8%.
“These are highly clinically significant results for this difficult to treat population,” Dr. Dickinson said in his presentation.
The most common adverse event was cytokine release syndrome (CRS), which occurred in 63% of patients. Of these, 3.9% were grade 3 or 4. Patients received corticosteroids (27.8%) or tocilizumab for management of CRS.
“As we have shown before, this is a first-course phenomenon, becoming far less frequent once step up dosing is complete,” Dr. Dickinson said in the presentation. “The median time to CRS is predictable, occurring around 10 hours after the IV infusion,” he said. Overall, 3.2% of the patients discontinued because of an adverse event.
A total of eight deaths occurred during the study; five of these were related to COVID-19 and the remaining three were in patients with manifest progression of disease.
Infections are to be expected in such a heavily treated population, and 14.9% of patients developed infections of grade 3 or higher, said Dr. Dickinson. Neutropenia of any grade occurred in 37.7%, febrile neutropenia in 2.6%. Neurological events occurred in 38.3% of patients; 3.2% were grade 3 or higher.
The study did not prospectively record immune effector cell–associated neurotoxicity syndrome, Dr. Dickinson said, but an estimate suggests a rate of 2.6%, and none of the events were considered to be related to glofitamab, he noted.
The researchers also looked at a supporting cohort of 35 patients with a median follow up of more than 2 years. In this group, the complete remission rate was 35% and the median duration of remission was 34.2 months. “Our six longest patients have been in remission for longer than 3 years,” Dr. Dickinson said.
The latest glofitamab data “reflect routine practice and an area of need for this disease,” said Dr. Dickinson.
“I think these results will prove to be very meaningful for our patients with large cell lymphoma, and this drug will prove to be an important treatment option,” he said.
More follow-up needed, but findings show promise
A number of CD20/CD3-bispecific antibodies are in development for patients with relapsed/refractory B-cell lymphomas, said study discussant Kerry J. Savage, MD, of the University of British Columbia, Vancouver, who served as the discussant for the session.
Glofitamab differs from other treatments in that it is bivalent for CD20 and monovalent for CD3, “which imparts greater potency,” she noted. Glofitamab also has a silent Fc region that is designed to extend half-life and reduce toxicity.
Patients in the current study had at least two prior regimens, and importantly, “CR rates were similar, regardless of prior therapy,” said Dr. Savage. The longer follow-up cohort provides “a hint that the response may be durable.”
Looking ahead, “the important thing will be response durability” with longer follow-up, she added. “We don’t know the curative potential yet, but the results are encouraging so far.”
In the meantime, “the best use of bispecific antibodies is through clinical trials,” Dr. Savage said. “Keep an eye out for bispecific antibody combination trials as well.”
The study was funded by F. Hoffmann–La Roche. Dr. Dickinson disclosed honoraria from or serving as a consultant to companies including Amgen, Bristol Myers-Squibb, Gilead Sciences, Janssen, MSD, Novartis, and Roche. Dr. Savage disclosed relationships, funding, and support from multiple companies including Bristol Myers-Squibb, Janssen Oncology, Kyowa, Merck, Novartis Canada Pharmaceuticals, Seattle Genetics and Roche.
“We know that relapsed diffuse large B-cell lymphoma has a particularly poor prognosis,” especially for patients who have undergone at least two therapies, Dr. Michael Dickinson, MBBS, of the University of Melbourne said in a presentation at the annual meeting of the American Society of Clinical Oncology.
Bispecific T cell–recruiting antibodies are emerging as a novel treatment option for B-cell cancers, said Dr. Dickinson.
Glofitamab is distinct among these therapies for its configuration that is bivalent for CD20 and monovalent for CD3, providing more potency than a 1:1 format, Dr. Dickinson explained in his presentation.
The study population included 154 adults aged 21-90 years with DLBCL who had received at least two prior treatments; all had received prior anti-CD20 Ab, and 149 had received anthracycline. The median age of the patients was 66 years, 65% were male, 75% had Ann Arbor stage III or IV disease, and 90% were refractory to any prior therapy.
The patients received intravenous glutamate-pyruvate transaminase, followed by an initial intravenous dose of glofitamab 7 days later. Glofitamab was given as step-up doses starting with 2.5 mg to a target of 30 mg.
The primary endpoint was complete response (CR) during initial treatment using Independent Review Committee (IRC) criteria, with overall response rate, duration of response, duration of complete response, progression-free survival, and overall survival as key secondary outcomes.
At a median of 12.6 months’ follow-up, the CR and overall response rates were 39.4% and 51.6%, respectively.
“Responses were achieved early; the median time to first complete response was 42 days,” Dr. Dickinson reported. Of the 38 patients with CR at the data cutoff point, 33 remained in complete remission (87%) based on IRC criteria. Complete response rates were consistent across prespecified subgroups, notably 42% of patients with no prior chimeric antigen receptor T-cell therapy and 70% and 34%, of those who were relapsed or refractory, respectively, to their last prior treatments.
The median duration of overall response was 18.4 months, and the median duration of complete response had not yet been estimated, Dr. Dickinson said. The median progression-free survival and overall survival rates were 4.9 months and 11.5 months, respectively, and the estimated 12-month overall survival was 49.8%.
“These are highly clinically significant results for this difficult to treat population,” Dr. Dickinson said in his presentation.
The most common adverse event was cytokine release syndrome (CRS), which occurred in 63% of patients. Of these, 3.9% were grade 3 or 4. Patients received corticosteroids (27.8%) or tocilizumab for management of CRS.
“As we have shown before, this is a first-course phenomenon, becoming far less frequent once step up dosing is complete,” Dr. Dickinson said in the presentation. “The median time to CRS is predictable, occurring around 10 hours after the IV infusion,” he said. Overall, 3.2% of the patients discontinued because of an adverse event.
A total of eight deaths occurred during the study; five of these were related to COVID-19 and the remaining three were in patients with manifest progression of disease.
Infections are to be expected in such a heavily treated population, and 14.9% of patients developed infections of grade 3 or higher, said Dr. Dickinson. Neutropenia of any grade occurred in 37.7%, febrile neutropenia in 2.6%. Neurological events occurred in 38.3% of patients; 3.2% were grade 3 or higher.
The study did not prospectively record immune effector cell–associated neurotoxicity syndrome, Dr. Dickinson said, but an estimate suggests a rate of 2.6%, and none of the events were considered to be related to glofitamab, he noted.
The researchers also looked at a supporting cohort of 35 patients with a median follow up of more than 2 years. In this group, the complete remission rate was 35% and the median duration of remission was 34.2 months. “Our six longest patients have been in remission for longer than 3 years,” Dr. Dickinson said.
The latest glofitamab data “reflect routine practice and an area of need for this disease,” said Dr. Dickinson.
“I think these results will prove to be very meaningful for our patients with large cell lymphoma, and this drug will prove to be an important treatment option,” he said.
More follow-up needed, but findings show promise
A number of CD20/CD3-bispecific antibodies are in development for patients with relapsed/refractory B-cell lymphomas, said study discussant Kerry J. Savage, MD, of the University of British Columbia, Vancouver, who served as the discussant for the session.
Glofitamab differs from other treatments in that it is bivalent for CD20 and monovalent for CD3, “which imparts greater potency,” she noted. Glofitamab also has a silent Fc region that is designed to extend half-life and reduce toxicity.
Patients in the current study had at least two prior regimens, and importantly, “CR rates were similar, regardless of prior therapy,” said Dr. Savage. The longer follow-up cohort provides “a hint that the response may be durable.”
Looking ahead, “the important thing will be response durability” with longer follow-up, she added. “We don’t know the curative potential yet, but the results are encouraging so far.”
In the meantime, “the best use of bispecific antibodies is through clinical trials,” Dr. Savage said. “Keep an eye out for bispecific antibody combination trials as well.”
The study was funded by F. Hoffmann–La Roche. Dr. Dickinson disclosed honoraria from or serving as a consultant to companies including Amgen, Bristol Myers-Squibb, Gilead Sciences, Janssen, MSD, Novartis, and Roche. Dr. Savage disclosed relationships, funding, and support from multiple companies including Bristol Myers-Squibb, Janssen Oncology, Kyowa, Merck, Novartis Canada Pharmaceuticals, Seattle Genetics and Roche.
FROM ASCO 2022
‘Exciting’ new gene therapy yields promising results
In the first-in-human, phase 1 open-label study, known as ANTLER, 5 out of 5 patients with relapsed or refractory B cell non-Hodgkin lymphoma (r/r B-NHL) responded to a single dose of CB-010, an allogeneic CAR-T cell therapy designed to boost antitumor activity, according to the company.
The use of chimeric antigen receptor (CAR) T-cell therapy involves taking T cells out of the body, reprogramming them with CAR to better equip them to kill cancer cells, and putting them back into the body.
The study consists of two sections: an initial dose escalation following a 3 + 3 design, with prespecified, increasing doses, followed by an expanded trial in which all patients receive CB-010 at the dose determined in the first section.
The study population included 6 adults with r/r B-NHL who had relapsed after previous treatment with a median of 3 prior therapies. At baseline, all 6 patients underwent a lymphodepletion regimen consisting of cyclophosphamide at 60 mg/kg/day for 2 days, followed by 5 days of fludarabine at 25 mg/m2/day.
Then all patients received a single dose of 40x106 CAR-T cells. As of the Feb. 23, 2022, data cutoff date, 5 of the 6 patients had completed the 28-day dose-limiting toxicity (DLT) evaluation period. All 5 patients (100%) achieved a response; 4 achieved complete response and 1 achieved partial response. All 4 of the complete responders had ongoing complete response at 3 months, and the longest measured complete response was 6 months, according to the company.
“We are excited to see a 100% overall response rate with CB-010 at dose level 1 for these patients who have limited treatment options,” said Dr. Syed Rizvi, chief medical officer for Caribou Biosciences, in the press release. “We believe this initial level of activity is unparalleled for a single, starting dose of cell therapy. CB-010 was generally well-tolerated, with adverse events routinely observed in autologous or allogeneic anti-CD19 CAR-T cell therapies,” he said.
Based on the promising safety and efficacy results, the company is enrolling patients in a second cohort for treatment at dose level 2 (80x106 CAR-T cells), according to the news release.
Another allogeneic CAR-T cell therapy known as ALLO-501A is being studied in a similar trial conducted by the Moffitt Cancer Center.
Overall, CB-010 was well-tolerated, according to Caribou Biosciences. No cases of graft-versus-host disease were reported. A total of 3 patients developed grade 3 or 4 adverse events (AEs) within the first 28 days; the most common were neutropenia (50%), thrombocytopenia (33%), anemia (17%), and hypogammaglobulinemia (17%). One patient experienced both grade 1 cytokine release syndrome (CRS) and grade 3 Immune effector cell-Associated Neurotoxicity Syndrome (ICANS). This response was characterized as a dose-limiting toxicity. The patient was treated with tocilizumab and steroids, recovered within 39 hours, and went on to achieve a complete response, according to the company.
Although the safety profile in the current study was promising, prior research suggest that concerns associated with CRS and ICANS should not be ignored and may be barriers to treatment.
In an article published in Bone Marrow Transplant in 2021, Dr. Vipul Sheth and Dr. Jordan Gauthier of the Fred Hutchinson Cancer Center, Seattle, noted that adverse effects may remain a challenge to widespread use of CAR-T in patients with refractory or relapsed acute lymphoblastic leukemia, for which it has been approved by the U.S. Food and Drug Administration and several European agencies. However, “there is mounting evidence that earlier, and potentially more targeted, interventions can reduce these toxicities,” they wrote.
Study provides solid stepping stone
“CRS and ICANS are mild in most patients but can be severe and sometimes life-threatening in a subset of patients undergoing CD19 CAR T-cell therapy,” Dr. Gauthier said in an interview. “Different strategies are being investigated to mitigate or treat severe toxicities, such as the use of prophylactic corticosteroids, anakinra, lenzilumab, itacitinib. I am hopeful we will soon manage to prevent toxicities while maintaining potent anti-tumor effects,” he said.
“While autologous CD19 CAR-T cells have high efficacy in patients with refractory/relapsed large B-cell lymphoma, product manufacturing remains a complicated and lengthy process in the autologous setting,” Dr. Gauthier noted. “Commercial CAR T-cell manufacturing takes approximately 3-4 weeks, sometimes longer. Some patients won’t survive long enough to receive their infusion. In some patients, T-cell function is dramatically impaired, due to prior therapies or to the disease itself,” he said.
Dr. Gauthier said he was not surprised but that he was encouraged by the apparent early success of the ANTLER study. “The proof-of-concept that allogeneic CD19-targeted CAR T cells can induce high response rates in r/r LBCL has already been established,” he said. “Having said that, it is comforting to see prior findings confirmed by this new study, and those results are exciting for the field,” he added.
As for additional research, “we need longer follow-up after allogeneic CD19-targeted CAR T-cell therapy to ensure responses are durable,” Dr. Gauthier explained. “We also need to better understand the biology driving the antitumor effects and the side effects of CAR T-cells. This will help us build more efficacious and safer CAR T-cell therapies,” he said.
Response and side effects show promise for future research
The therapy is “the best CAR-T product” that clinicians can provide for patients knowing that autologous CAR-T works, said Dr. Ahmed Galal, of Duke University, Durham, N.C., in an interview. The current research supports the use of this treatment immediately for patients, he added.
Dr. Galal said he was somewhat surprised, but pleasantly so, by the 100% response rate. This rate is likely because of the small number of patients and may not hold up in further research, but “even 90% would be an amazing achievement,” he said. The tolerable safety profile is encouraging as well, he emphasized. Dr. Galal said that he did not foresee any real barriers to expanded use of the therapy and that technology should make it easier to deliver at authorized centers.
Limitations to the current study are those common to all phase 1 trials, such as the strict inclusion criteria, Dr. Galal said. As research progresses to phase 2, “I don’t think it will be an obstacle to find patients,” he said. However, patients should be aware of side effects, and clinicians should maintain a culture of education to help them understand the value of the therapy, he added.
The complete data from the preliminary findings are scheduled to be presented at the European Hematology Association (EHA) 2022 Hybrid Congress, Vienna, in June, as abstract P1455, titled “First-in-human trial of CB-010, a CRISPR-edited allogeneic anti-CD19 CAR-T cell therapy with a PD-1 knock out, in patients with relapsed or refractory B cell non-Hodgkin lymphoma (ANTLER study).” The findings are scheduled to be presented by Loretta J. Nastoupil, MD, of the University of Texas MD Anderson Cancer Center, according to Caribou Biosciences.
Dr. Gauthier had no financial conflicts to disclose. Dr. Galal had no financial conflicts to disclose.
In the first-in-human, phase 1 open-label study, known as ANTLER, 5 out of 5 patients with relapsed or refractory B cell non-Hodgkin lymphoma (r/r B-NHL) responded to a single dose of CB-010, an allogeneic CAR-T cell therapy designed to boost antitumor activity, according to the company.
The use of chimeric antigen receptor (CAR) T-cell therapy involves taking T cells out of the body, reprogramming them with CAR to better equip them to kill cancer cells, and putting them back into the body.
The study consists of two sections: an initial dose escalation following a 3 + 3 design, with prespecified, increasing doses, followed by an expanded trial in which all patients receive CB-010 at the dose determined in the first section.
The study population included 6 adults with r/r B-NHL who had relapsed after previous treatment with a median of 3 prior therapies. At baseline, all 6 patients underwent a lymphodepletion regimen consisting of cyclophosphamide at 60 mg/kg/day for 2 days, followed by 5 days of fludarabine at 25 mg/m2/day.
Then all patients received a single dose of 40x106 CAR-T cells. As of the Feb. 23, 2022, data cutoff date, 5 of the 6 patients had completed the 28-day dose-limiting toxicity (DLT) evaluation period. All 5 patients (100%) achieved a response; 4 achieved complete response and 1 achieved partial response. All 4 of the complete responders had ongoing complete response at 3 months, and the longest measured complete response was 6 months, according to the company.
“We are excited to see a 100% overall response rate with CB-010 at dose level 1 for these patients who have limited treatment options,” said Dr. Syed Rizvi, chief medical officer for Caribou Biosciences, in the press release. “We believe this initial level of activity is unparalleled for a single, starting dose of cell therapy. CB-010 was generally well-tolerated, with adverse events routinely observed in autologous or allogeneic anti-CD19 CAR-T cell therapies,” he said.
Based on the promising safety and efficacy results, the company is enrolling patients in a second cohort for treatment at dose level 2 (80x106 CAR-T cells), according to the news release.
Another allogeneic CAR-T cell therapy known as ALLO-501A is being studied in a similar trial conducted by the Moffitt Cancer Center.
Overall, CB-010 was well-tolerated, according to Caribou Biosciences. No cases of graft-versus-host disease were reported. A total of 3 patients developed grade 3 or 4 adverse events (AEs) within the first 28 days; the most common were neutropenia (50%), thrombocytopenia (33%), anemia (17%), and hypogammaglobulinemia (17%). One patient experienced both grade 1 cytokine release syndrome (CRS) and grade 3 Immune effector cell-Associated Neurotoxicity Syndrome (ICANS). This response was characterized as a dose-limiting toxicity. The patient was treated with tocilizumab and steroids, recovered within 39 hours, and went on to achieve a complete response, according to the company.
Although the safety profile in the current study was promising, prior research suggest that concerns associated with CRS and ICANS should not be ignored and may be barriers to treatment.
In an article published in Bone Marrow Transplant in 2021, Dr. Vipul Sheth and Dr. Jordan Gauthier of the Fred Hutchinson Cancer Center, Seattle, noted that adverse effects may remain a challenge to widespread use of CAR-T in patients with refractory or relapsed acute lymphoblastic leukemia, for which it has been approved by the U.S. Food and Drug Administration and several European agencies. However, “there is mounting evidence that earlier, and potentially more targeted, interventions can reduce these toxicities,” they wrote.
Study provides solid stepping stone
“CRS and ICANS are mild in most patients but can be severe and sometimes life-threatening in a subset of patients undergoing CD19 CAR T-cell therapy,” Dr. Gauthier said in an interview. “Different strategies are being investigated to mitigate or treat severe toxicities, such as the use of prophylactic corticosteroids, anakinra, lenzilumab, itacitinib. I am hopeful we will soon manage to prevent toxicities while maintaining potent anti-tumor effects,” he said.
“While autologous CD19 CAR-T cells have high efficacy in patients with refractory/relapsed large B-cell lymphoma, product manufacturing remains a complicated and lengthy process in the autologous setting,” Dr. Gauthier noted. “Commercial CAR T-cell manufacturing takes approximately 3-4 weeks, sometimes longer. Some patients won’t survive long enough to receive their infusion. In some patients, T-cell function is dramatically impaired, due to prior therapies or to the disease itself,” he said.
Dr. Gauthier said he was not surprised but that he was encouraged by the apparent early success of the ANTLER study. “The proof-of-concept that allogeneic CD19-targeted CAR T cells can induce high response rates in r/r LBCL has already been established,” he said. “Having said that, it is comforting to see prior findings confirmed by this new study, and those results are exciting for the field,” he added.
As for additional research, “we need longer follow-up after allogeneic CD19-targeted CAR T-cell therapy to ensure responses are durable,” Dr. Gauthier explained. “We also need to better understand the biology driving the antitumor effects and the side effects of CAR T-cells. This will help us build more efficacious and safer CAR T-cell therapies,” he said.
Response and side effects show promise for future research
The therapy is “the best CAR-T product” that clinicians can provide for patients knowing that autologous CAR-T works, said Dr. Ahmed Galal, of Duke University, Durham, N.C., in an interview. The current research supports the use of this treatment immediately for patients, he added.
Dr. Galal said he was somewhat surprised, but pleasantly so, by the 100% response rate. This rate is likely because of the small number of patients and may not hold up in further research, but “even 90% would be an amazing achievement,” he said. The tolerable safety profile is encouraging as well, he emphasized. Dr. Galal said that he did not foresee any real barriers to expanded use of the therapy and that technology should make it easier to deliver at authorized centers.
Limitations to the current study are those common to all phase 1 trials, such as the strict inclusion criteria, Dr. Galal said. As research progresses to phase 2, “I don’t think it will be an obstacle to find patients,” he said. However, patients should be aware of side effects, and clinicians should maintain a culture of education to help them understand the value of the therapy, he added.
The complete data from the preliminary findings are scheduled to be presented at the European Hematology Association (EHA) 2022 Hybrid Congress, Vienna, in June, as abstract P1455, titled “First-in-human trial of CB-010, a CRISPR-edited allogeneic anti-CD19 CAR-T cell therapy with a PD-1 knock out, in patients with relapsed or refractory B cell non-Hodgkin lymphoma (ANTLER study).” The findings are scheduled to be presented by Loretta J. Nastoupil, MD, of the University of Texas MD Anderson Cancer Center, according to Caribou Biosciences.
Dr. Gauthier had no financial conflicts to disclose. Dr. Galal had no financial conflicts to disclose.
In the first-in-human, phase 1 open-label study, known as ANTLER, 5 out of 5 patients with relapsed or refractory B cell non-Hodgkin lymphoma (r/r B-NHL) responded to a single dose of CB-010, an allogeneic CAR-T cell therapy designed to boost antitumor activity, according to the company.
The use of chimeric antigen receptor (CAR) T-cell therapy involves taking T cells out of the body, reprogramming them with CAR to better equip them to kill cancer cells, and putting them back into the body.
The study consists of two sections: an initial dose escalation following a 3 + 3 design, with prespecified, increasing doses, followed by an expanded trial in which all patients receive CB-010 at the dose determined in the first section.
The study population included 6 adults with r/r B-NHL who had relapsed after previous treatment with a median of 3 prior therapies. At baseline, all 6 patients underwent a lymphodepletion regimen consisting of cyclophosphamide at 60 mg/kg/day for 2 days, followed by 5 days of fludarabine at 25 mg/m2/day.
Then all patients received a single dose of 40x106 CAR-T cells. As of the Feb. 23, 2022, data cutoff date, 5 of the 6 patients had completed the 28-day dose-limiting toxicity (DLT) evaluation period. All 5 patients (100%) achieved a response; 4 achieved complete response and 1 achieved partial response. All 4 of the complete responders had ongoing complete response at 3 months, and the longest measured complete response was 6 months, according to the company.
“We are excited to see a 100% overall response rate with CB-010 at dose level 1 for these patients who have limited treatment options,” said Dr. Syed Rizvi, chief medical officer for Caribou Biosciences, in the press release. “We believe this initial level of activity is unparalleled for a single, starting dose of cell therapy. CB-010 was generally well-tolerated, with adverse events routinely observed in autologous or allogeneic anti-CD19 CAR-T cell therapies,” he said.
Based on the promising safety and efficacy results, the company is enrolling patients in a second cohort for treatment at dose level 2 (80x106 CAR-T cells), according to the news release.
Another allogeneic CAR-T cell therapy known as ALLO-501A is being studied in a similar trial conducted by the Moffitt Cancer Center.
Overall, CB-010 was well-tolerated, according to Caribou Biosciences. No cases of graft-versus-host disease were reported. A total of 3 patients developed grade 3 or 4 adverse events (AEs) within the first 28 days; the most common were neutropenia (50%), thrombocytopenia (33%), anemia (17%), and hypogammaglobulinemia (17%). One patient experienced both grade 1 cytokine release syndrome (CRS) and grade 3 Immune effector cell-Associated Neurotoxicity Syndrome (ICANS). This response was characterized as a dose-limiting toxicity. The patient was treated with tocilizumab and steroids, recovered within 39 hours, and went on to achieve a complete response, according to the company.
Although the safety profile in the current study was promising, prior research suggest that concerns associated with CRS and ICANS should not be ignored and may be barriers to treatment.
In an article published in Bone Marrow Transplant in 2021, Dr. Vipul Sheth and Dr. Jordan Gauthier of the Fred Hutchinson Cancer Center, Seattle, noted that adverse effects may remain a challenge to widespread use of CAR-T in patients with refractory or relapsed acute lymphoblastic leukemia, for which it has been approved by the U.S. Food and Drug Administration and several European agencies. However, “there is mounting evidence that earlier, and potentially more targeted, interventions can reduce these toxicities,” they wrote.
Study provides solid stepping stone
“CRS and ICANS are mild in most patients but can be severe and sometimes life-threatening in a subset of patients undergoing CD19 CAR T-cell therapy,” Dr. Gauthier said in an interview. “Different strategies are being investigated to mitigate or treat severe toxicities, such as the use of prophylactic corticosteroids, anakinra, lenzilumab, itacitinib. I am hopeful we will soon manage to prevent toxicities while maintaining potent anti-tumor effects,” he said.
“While autologous CD19 CAR-T cells have high efficacy in patients with refractory/relapsed large B-cell lymphoma, product manufacturing remains a complicated and lengthy process in the autologous setting,” Dr. Gauthier noted. “Commercial CAR T-cell manufacturing takes approximately 3-4 weeks, sometimes longer. Some patients won’t survive long enough to receive their infusion. In some patients, T-cell function is dramatically impaired, due to prior therapies or to the disease itself,” he said.
Dr. Gauthier said he was not surprised but that he was encouraged by the apparent early success of the ANTLER study. “The proof-of-concept that allogeneic CD19-targeted CAR T cells can induce high response rates in r/r LBCL has already been established,” he said. “Having said that, it is comforting to see prior findings confirmed by this new study, and those results are exciting for the field,” he added.
As for additional research, “we need longer follow-up after allogeneic CD19-targeted CAR T-cell therapy to ensure responses are durable,” Dr. Gauthier explained. “We also need to better understand the biology driving the antitumor effects and the side effects of CAR T-cells. This will help us build more efficacious and safer CAR T-cell therapies,” he said.
Response and side effects show promise for future research
The therapy is “the best CAR-T product” that clinicians can provide for patients knowing that autologous CAR-T works, said Dr. Ahmed Galal, of Duke University, Durham, N.C., in an interview. The current research supports the use of this treatment immediately for patients, he added.
Dr. Galal said he was somewhat surprised, but pleasantly so, by the 100% response rate. This rate is likely because of the small number of patients and may not hold up in further research, but “even 90% would be an amazing achievement,” he said. The tolerable safety profile is encouraging as well, he emphasized. Dr. Galal said that he did not foresee any real barriers to expanded use of the therapy and that technology should make it easier to deliver at authorized centers.
Limitations to the current study are those common to all phase 1 trials, such as the strict inclusion criteria, Dr. Galal said. As research progresses to phase 2, “I don’t think it will be an obstacle to find patients,” he said. However, patients should be aware of side effects, and clinicians should maintain a culture of education to help them understand the value of the therapy, he added.
The complete data from the preliminary findings are scheduled to be presented at the European Hematology Association (EHA) 2022 Hybrid Congress, Vienna, in June, as abstract P1455, titled “First-in-human trial of CB-010, a CRISPR-edited allogeneic anti-CD19 CAR-T cell therapy with a PD-1 knock out, in patients with relapsed or refractory B cell non-Hodgkin lymphoma (ANTLER study).” The findings are scheduled to be presented by Loretta J. Nastoupil, MD, of the University of Texas MD Anderson Cancer Center, according to Caribou Biosciences.
Dr. Gauthier had no financial conflicts to disclose. Dr. Galal had no financial conflicts to disclose.
Third-generation Black woman physician makes cancer research history
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
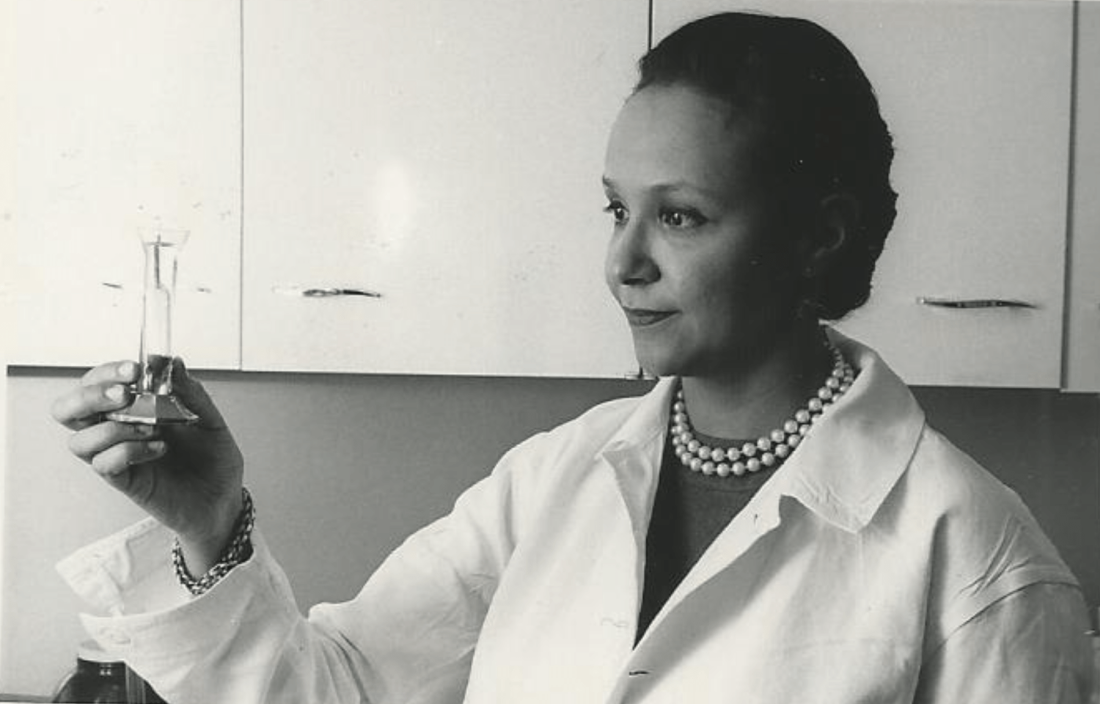
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
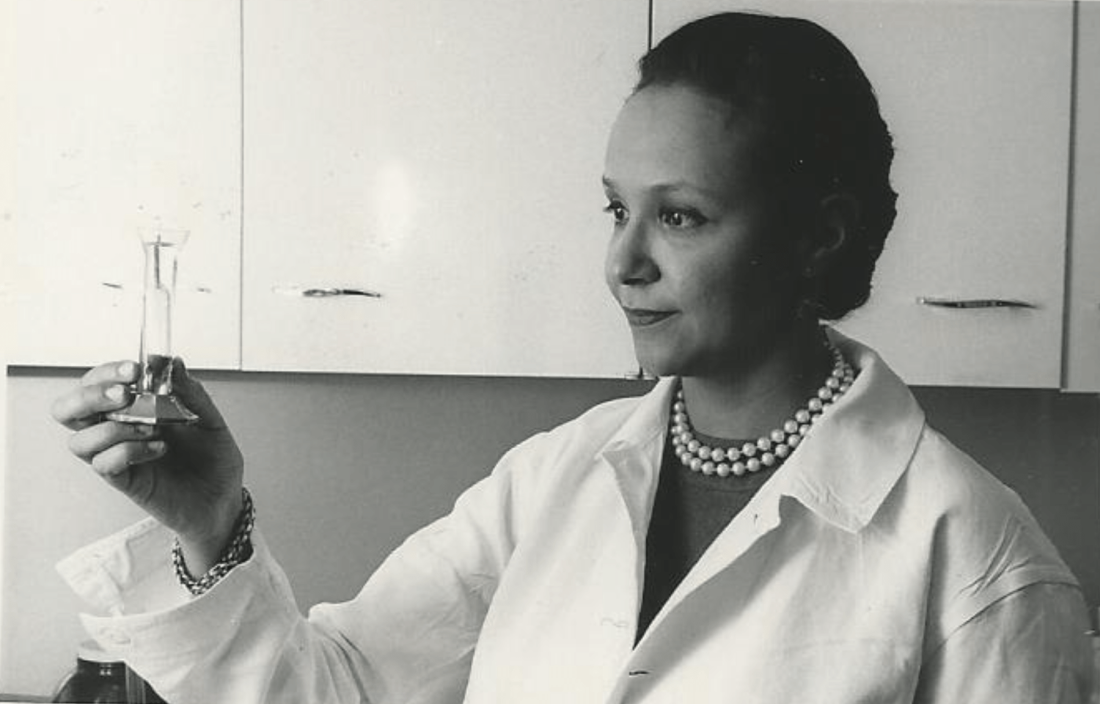
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
Ex–hospital porter a neglected giant of cancer research
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
Repurposed drug could revolutionize stem cell transplantation
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
EMA gives green light to new CAR T-cell therapy
At its late January meeting, the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended for approval lisocabtagene maraleucel (Breyanzi, Bristol-Myers Squibb). This chimeric antigen receptor T-cell therapy is indicated for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal large B-cell lymphoma (PMBCL), and follicular lymphoma grade 3B (FL3B). The indication is for use in patients who have received at least two lines of treatment.
The benefits of lisocabtagene maraleucel, noted the CHMP, are its ability to provide high and durable responses in patients with relapsed or refractory DLBCL, PMBCL, and FL3B. The most common side effects reported are neutropenia, anemia, cytokine release syndrome, fatigue, and thrombocytopenia.
The product is already approved in the United States for the same indication. The Food and Drug Administration’s approval came with a Risk Evaluation and Mitigation Strategy because of the risk for serious adverse events, including cytokine release syndrome.
During development, it was designated as an orphan medicine. The EMA will now review the information available to date to determine if the orphan designation can be maintained.
Biosimilar pegfilgrastim
At the same meeting, the committee recommended approval of a biosimilar product for pegfilgrastim (Stimufend, Fresenius Kabi Deutschland), which is used to reduce the duration of neutropenia and the incidence of febrile neutropenia after cytotoxic chemotherapy.
The committee noted that this product has been shown to be highly similar to the reference product Neulasta (pegfilgrastim), which has been available in the EU for 2 decades (authorized in 2002). Data have demonstrated that Stimufend has comparable quality, safety, and efficacy to Neulasta.
Its full indication is to reduce the duration of neutropenia and incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancies, with the exception of chronic myeloid leukemia (CML) and myelodysplastic syndromes.
Generic versions of dasatinib
Also recommended for approval were for two generic formulations of dasatinib (Dasatinib Accord and Dasatinib Accordpharma, both from Accord Healthcare) for the treatment of various leukemias.
These are generic versions of dasatinib (Sprycel), which has been available in the European Union since 2006.
The CHMP noted that studies have demonstrated the satisfactory quality of Dasatinib Accord, as well as its bioequivalence to the reference product. This generic is indicated for the treatment of adult patients with Philadelphia chromosome–positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy and pediatric patients with newly diagnosed Ph+ ALL in combination with chemotherapy.
Dasatinib Accordpharma has a wider set of indications, which include the treatment of adult patients with newly diagnosed Ph+ CML in the chronic phase; chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib; and Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy. In addition, this generic is indicated for the treatment of pediatric patients with newly diagnosed Ph+ CML in the chronic phase or Ph+ CML-CP resistant or intolerant to prior therapy including imatinib and newly diagnosed Ph+ ALL in combination with chemotherapy.
A version of this article first appeared on Medscape.com.
At its late January meeting, the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended for approval lisocabtagene maraleucel (Breyanzi, Bristol-Myers Squibb). This chimeric antigen receptor T-cell therapy is indicated for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal large B-cell lymphoma (PMBCL), and follicular lymphoma grade 3B (FL3B). The indication is for use in patients who have received at least two lines of treatment.
The benefits of lisocabtagene maraleucel, noted the CHMP, are its ability to provide high and durable responses in patients with relapsed or refractory DLBCL, PMBCL, and FL3B. The most common side effects reported are neutropenia, anemia, cytokine release syndrome, fatigue, and thrombocytopenia.
The product is already approved in the United States for the same indication. The Food and Drug Administration’s approval came with a Risk Evaluation and Mitigation Strategy because of the risk for serious adverse events, including cytokine release syndrome.
During development, it was designated as an orphan medicine. The EMA will now review the information available to date to determine if the orphan designation can be maintained.
Biosimilar pegfilgrastim
At the same meeting, the committee recommended approval of a biosimilar product for pegfilgrastim (Stimufend, Fresenius Kabi Deutschland), which is used to reduce the duration of neutropenia and the incidence of febrile neutropenia after cytotoxic chemotherapy.
The committee noted that this product has been shown to be highly similar to the reference product Neulasta (pegfilgrastim), which has been available in the EU for 2 decades (authorized in 2002). Data have demonstrated that Stimufend has comparable quality, safety, and efficacy to Neulasta.
Its full indication is to reduce the duration of neutropenia and incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancies, with the exception of chronic myeloid leukemia (CML) and myelodysplastic syndromes.
Generic versions of dasatinib
Also recommended for approval were for two generic formulations of dasatinib (Dasatinib Accord and Dasatinib Accordpharma, both from Accord Healthcare) for the treatment of various leukemias.
These are generic versions of dasatinib (Sprycel), which has been available in the European Union since 2006.
The CHMP noted that studies have demonstrated the satisfactory quality of Dasatinib Accord, as well as its bioequivalence to the reference product. This generic is indicated for the treatment of adult patients with Philadelphia chromosome–positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy and pediatric patients with newly diagnosed Ph+ ALL in combination with chemotherapy.
Dasatinib Accordpharma has a wider set of indications, which include the treatment of adult patients with newly diagnosed Ph+ CML in the chronic phase; chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib; and Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy. In addition, this generic is indicated for the treatment of pediatric patients with newly diagnosed Ph+ CML in the chronic phase or Ph+ CML-CP resistant or intolerant to prior therapy including imatinib and newly diagnosed Ph+ ALL in combination with chemotherapy.
A version of this article first appeared on Medscape.com.
At its late January meeting, the Committee for Medicinal Products for Human Use of the European Medicines Agency recommended for approval lisocabtagene maraleucel (Breyanzi, Bristol-Myers Squibb). This chimeric antigen receptor T-cell therapy is indicated for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL), primary mediastinal large B-cell lymphoma (PMBCL), and follicular lymphoma grade 3B (FL3B). The indication is for use in patients who have received at least two lines of treatment.
The benefits of lisocabtagene maraleucel, noted the CHMP, are its ability to provide high and durable responses in patients with relapsed or refractory DLBCL, PMBCL, and FL3B. The most common side effects reported are neutropenia, anemia, cytokine release syndrome, fatigue, and thrombocytopenia.
The product is already approved in the United States for the same indication. The Food and Drug Administration’s approval came with a Risk Evaluation and Mitigation Strategy because of the risk for serious adverse events, including cytokine release syndrome.
During development, it was designated as an orphan medicine. The EMA will now review the information available to date to determine if the orphan designation can be maintained.
Biosimilar pegfilgrastim
At the same meeting, the committee recommended approval of a biosimilar product for pegfilgrastim (Stimufend, Fresenius Kabi Deutschland), which is used to reduce the duration of neutropenia and the incidence of febrile neutropenia after cytotoxic chemotherapy.
The committee noted that this product has been shown to be highly similar to the reference product Neulasta (pegfilgrastim), which has been available in the EU for 2 decades (authorized in 2002). Data have demonstrated that Stimufend has comparable quality, safety, and efficacy to Neulasta.
Its full indication is to reduce the duration of neutropenia and incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancies, with the exception of chronic myeloid leukemia (CML) and myelodysplastic syndromes.
Generic versions of dasatinib
Also recommended for approval were for two generic formulations of dasatinib (Dasatinib Accord and Dasatinib Accordpharma, both from Accord Healthcare) for the treatment of various leukemias.
These are generic versions of dasatinib (Sprycel), which has been available in the European Union since 2006.
The CHMP noted that studies have demonstrated the satisfactory quality of Dasatinib Accord, as well as its bioequivalence to the reference product. This generic is indicated for the treatment of adult patients with Philadelphia chromosome–positive acute lymphoblastic leukemia with resistance or intolerance to prior therapy and pediatric patients with newly diagnosed Ph+ ALL in combination with chemotherapy.
Dasatinib Accordpharma has a wider set of indications, which include the treatment of adult patients with newly diagnosed Ph+ CML in the chronic phase; chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib; and Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy. In addition, this generic is indicated for the treatment of pediatric patients with newly diagnosed Ph+ CML in the chronic phase or Ph+ CML-CP resistant or intolerant to prior therapy including imatinib and newly diagnosed Ph+ ALL in combination with chemotherapy.
A version of this article first appeared on Medscape.com.
100 coauthored papers, 10 years: Cancer transplant pioneers model 'team science'
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
Rituximab and COVID-19 vaccines: Studies begin to answer key questions
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.
Rituximab has presented something of a conundrum for patients taking the monoclonal antibody during the COVID-19 pandemic.
Used to manage a variety of autoimmune diseases and cancers, rituximab acts against CD20 proteins expressed on the surface of B cells, causing B-cell depletion. However, it is this B-cell depletion that may put these patients at greater risk of COVID-19 development, progression to more severe disease, and in-hospital mortality. Evidence for this appears to be mixed, with studies showing both that patients using rituximab to manage various diseases are and are not at increased risk for SARS-CoV-2 infection, COVID-19 progression, and mortality.
As COVID-19 vaccine rollouts take place across the world, more questions have been raised about the relationship between B-cell depletion from anti-CD20 therapies and COVID-19 vaccines. Do rituximab and other anti-CD20 therapies affect a patient’s response to COVID-19 vaccines? If this is the case, does the timing of anti-CD20 treatment matter to maximize B-cell levels and improve the vaccine’s effectiveness? And how do COVID-19 vaccine booster doses factor into the equation?
Humoral and cell-mediated responses following COVID-19 vaccination
First, the bad news: The vaccine is unquestionably safe to administer in patients taking rituximab, but one thing that has been well established is that antibody response to COVID-19 vaccination in these individuals does is reduced. This isn’t entirely unprecedented, as previous studies have shown a weakened immune response to pneumococcal polysaccharide and keyhole limpet hemocyanin vaccines among patients taking rituximab.
“Compromised immunogenicity to the SARS-CoV-2 vaccines has been demonstrated in rituximab-treated patients, which is of particular concern given the observation that B-cell–depleting therapies may be associated with worse COVID outcomes,” Robert F. Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, said in an interview.
For example, in a recent study from the Medical University of Vienna, 29 (39%) of 74 patients receiving rituximab (43% as monotherapy, 57% with conventional-synthetic disease-modifying antirheumatic drugs) who were vaccinated with either the Comirnaty (Pfizer-BioNTech) or Spikevax (Moderna) COVID-19 vaccine achieved seroconversion, compared with 100% of patients in a healthy control group, and all but 1 patient without detectable CD19+ peripheral B cells did not develop anti–SARS-CoV-2 receptor-binding domain antibodies.
“There is an increasing number of studies in this field, and they confirm that patients treated with rituximab and other anti-CD20 agents have severely reduced serological responses to COVID-19 vaccines,” Ingrid Jyssum, MD, of the division of rheumatology and research at Diakonhjemmet Hospital in Oslo, said in an interview.
One silver lining is that patients treated with anti-CD20 therapies appear to have a cell-mediated response following vaccination even if they don’t develop SARS-CoV-2 antibodies. “Studies that also investigate T-cell responses are starting to emerge, and so far, they show that, even if the patients do not have antibodies, they may have T-cell responses,” Dr. Jyssum said.
One study of 24 patients with autoimmune diseases taking rituximab that evaluated humoral and T-cell responses following vaccination with the Comirnaty vaccine found that none had a humoral response to the vaccine, but the T-cell response from that group did not significantly differ from 35 patients receiving other immunosuppressants and 26 patients in a healthy control group. In another study of rituximab- or ocrelizumab-treated patients who received mRNA-based COVID-19 vaccines, 69.4% developed SARS-CoV-2–specific antibodies, compared with a control group, but 96.2% of patients taking ocrelizumab and 81.8% of patients taking rituximab mounted a spike-specific CD8+ T-cell response, compared with 66.7% in the control group, and there were comparable rates (85%-90%) of spike-specific CD4+ T cells in all groups. In the study from the Medical University of Vienna, T-cell response was detected in rituximab-treated patients who both did and did not mount an antibody response.
The clinical relevance of how a blunted humoral immune response but a respectable T-cell response to COVID-19 vaccines affects patients treated with anti-CD20 therapies isn’t currently known, Dr. Jyssum said.
While these data are reassuring, they’re also incomplete, Dr. Spiera noted. “The ultimate outcome of relevance to assess vaccine efficacy is protection from COVID and from severe outcomes of COVID infection (i.e., hospitalization, mechanical ventilation, death). That data will require assessment of very large numbers of rituximab-treated vaccinated patients to be compared with rituximab-treated unvaccinated patients, and is unlikely to be forthcoming in the very near future.
“In the meantime, however, achieving serologic positivity, meaning having evidence of serologic as well as cellular immunity following vaccination, is a desired outcome, and likely implies more robust immunity.”
Does treatment timing impact COVID-19 vaccine response?
Given enough time, B-cell reconstitution will occur in patients taking rituximab. With that in mind, is it beneficial to wait a certain amount of time after a patient has stopped rituximab therapy or time since their last dose before giving them a COVID-19 vaccine? In their guidance on COVID-19 vaccines for patients with rheumatic and musculoskeletal diseases, the American College of Rheumatology said there is moderate evidence to consider “optimal timing of dosing and vaccination with the rheumatology provider before proceeding.”
“Guidelines and preliminary studies of serologic response to COVID vaccine in rituximab-treated patients have suggested that longer time from last rituximab exposure is associated with a greater likelihood of a serologic response,” Dr. Spiera said.
In a brief report published in Arthritis & Rheumatology, Dr. Spiera and colleagues performed a retrospective chart review of 56 patients with varying levels of last exposure to rituximab who received a COVID-19 vaccine. Their results showed that, when patients were vaccinated 6-12 months after the last rituximab dose, 55% were seronegative, and when this was more than 12 months, only 13% were seronegative, compared with seronegativity in 86% who were vaccinated less than 6 months after their last rituximab dose.
The RituxiVac trial, conducted by researchers in Switzerland, also examined vaccine responses of 96 rituximab-treated patients who received Comirnaty or Spikevax; results recently published in The Lancet Rheumatology showed findings similar to other studies, with reduced humoral and cell-mediated responses. In the RituxiVac trial, the median time to last anti-CD20 treatment was 1.07 years.
“The typical interval between rituximab doses [for treatment of rheumatoid arthritis, as well as for remission maintenance in antineutrophil cytoplasmic antibody–associated vasculitis] is typically 6 months, and this has become widely used as the interval from last rituximab to time of COVID vaccination, with a recommendation to wait 4 weeks (if possible) from time of vaccination until the next rituximab administration,” Dr. Spiera explained. However, this window seems to vary depending on the study.
Recent research published in Arthritis & Rheumatology indicates B-cell levels could be a relevant indicator for humoral and cell-mediated response in patients with rheumatic diseases treated with rituximab, with a level of 10 B cells/mcL (0.4% of lymphocytes) identified as one potential marker for likely seroconversion following COVID-19 vaccination.
“In some smaller case series, it has been further recognized that rituximab-treated patients who were beginning to reconstitute peripheral B cells were most likely to respond serologically. Our present study confirmed those findings, demonstrating that the presence of detectable B cells was strongly associated with vaccine responsiveness, and affords complementary information to time from last [rituximab dose] in informing the likelihood of a vaccine response,” Dr. Spiera said.
However, the literature is limited in this area, and an exact cutoff for B-cell counts in these patients isn’t currently known, Dr. Jyssum said. A better metric is time away from anti-CD20 therapies, with CD19 cell count being highly correlated with last infusion.
Dr. Spiera agreed that there is no consistent B-cell percentage that works as a cutoff. “In our study, we looked at it as a binary variable, although we did find that a higher percentage of B cells in the peripheral lymphocyte population was associated with a higher likelihood of seroconversion. We did not, however, identify a ‘threshold’ for vaccine serologic responsiveness.”
Should clinicians measure antibodies?
The Food and Drug Administration and the Centers for Disease Control and Prevention have recommended that health care providers and the public not use COVID-19 antibody tests as a way to gauge immunity after exposure to SARS-CoV-2 and after receiving a COVID-19 vaccination. The ACR’s guidance on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases strongly recommends against ordering antibody tests for patients with autoimmune inflammatory rheumatic diseases as a way to measure immunity.
“Generally, such measurements are not recommended as the clinical correlate of various antibody levels are not known,” Dr. Jyssum said. “With regular infusions of rituximab or other anti-CD20 agents, one cannot expect that these patients will develop significant levels of antibodies.”
However, she said there might be situations where it’s useful to know whether a patient has developed antibodies at all. “Assessing the significance of specific antibody levels is difficult, and the subject of scientific studies. Patients lacking a humoral vaccine response are left to rely on their T-cell responses and on infectious control measures to prevent disease.”
Dr. Spiera said he disagreed with guidelines recommending against checking antibody levels after vaccination, “particularly in patients treated with immunosuppressive medications that might be expected to blunt their serologic response to the vaccines.
“Although we cannot be sure what level of measurable antibodies offer what level of protection, most clinicians would agree that patients who demonstrate no detectable antibodies (which is a common finding in rituximab-treated patients) should be considered at higher risk,” he said. “Indeed, recommendations regarding booster vaccine administration in general was initially based on the observation of declining antibody levels with longer time from vaccination.”
Do COVID-19 vaccine boosters help patients on anti-CD20 therapy?
As of January 2022, the FDA and CDC have recommended a third primary series shot of COVID-19 vaccines for some moderately to severely immunocompromised patients as young as 5 years old (for Comirnaty vaccine) or a booster shot of either Comirnaty or Spikevax for everyone aged 12 years and older, including immunocompromised people, while the ACR goes into more detail and recommends clinicians time a patient’s booster shot with temporary treatment interruption.
In The Lancet Rheumatology, Dr. Jyssum and colleagues recently published results from the prospective Nor-vaC study examining the humoral and cell-mediated immune responses of 87 patients with RA being treated with rituximab who received the Comirnaty, Spikevax, or Vaxzevria (AstraZeneca) COVID-19 vaccines; of these, 49 patients received a booster dose at a median of 70 days after completing their primary series. The results showed 19 patients (28.1%) had a serologic response after their primary series, while 8 of 49 patients (16.3%) who received their booster dose had a serologic response.
All patients who received a third dose in the study had a T-cell response, Dr. Jyssum said. “This is reassuring for patients and clinicians. T cells have been found to be important in countering COVID-19 disease, but whether we can rely on the T-cell response alone in the absence of antibodies to protect patients from infection or from serious COVID disease is still not determined,” she said.
When asked if she would recommend COVID-19 vaccine booster doses for patients on rituximab, Dr. Jyssum replied: “Absolutely.”
Another study, recently published in Annals of the Rheumatic Diseases, examined heterologous and homologous booster doses for 60 patients receiving rituximab without seroconversion after their COVID-19 vaccine primary series. The results showed no significant difference in new seroconversion at 4 weeks based on whether the patient received a vector or mRNA vaccine (22% vs. 32%), but all patients who received a booster dose with a vector vaccine had specific T-cell responses, compared with 81% of patients who received an mRNA vaccine booster. There was a new humoral and/or cellular response in 9 of 11 patients (82%), and most patients with peripheral B cells (12 of 18 patients; 67%) achieved seroconversion.
“Our data show that a cellular and/or humoral immune response can be achieved on a third COVID-19 vaccination in most of the patients who initially developed neither a humoral nor a cellular immune response,” the researchers concluded. “The efficacy data together with the safety data seen in our trial provide a favorable risk/benefit ratio and support the implementation of a third vaccination for nonseroconverted high-risk autoimmune disease patients treated with B-cell–depleting agents.”
Dr. Spiera said booster doses are an important part of the equation, and “it is important to consider factors that would be associated with a greater likelihood of achieving a serologic response, particularly in those patients who did not demonstrate a serologic response to the initial vaccines series.
“Preliminary data shows that the beginnings of B-cell reconstitution is also associated with a positive serologic response following a booster of the COVID-19 vaccine,” he said.
The authors of the cited studies reported numerous relevant financial disclosures. Dr. Spiera and Dr. Jyssum reported no relevant financial disclosures.
DKMS: Small nonprofit to world’s largest stem cell donor registry
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.