User login
Virtual APA vs. the real thing: Which is better?
Every spring, I look forward to attending the American Psychiatric Association’s annual meeting. It has become a ritual that starts many months before the actual conference.
Submissions for presentations are due in September, so the planning often starts in the late summer. Hotel and plane reservations are made in January, and the meeting itself begins in May.
The city that hosts the event changes each year but, for me, many things do not. The Clinical Psychiatry News editorial board meeting takes place on Monday morning at 7 a.m., and I scour the program for what sessions to attend. In recent years, I have made a point of writing an article for about one of the sessions while still at the meeting – in 2019 I wrote about the improv-acting workshops I attended – something that just doesn’t translate to a Zoom experience.
I go with the same friend every year, I always attend the Hopkins alumni reception, and I organize dinner at a nice restaurant for friends. I have collected so many funny stories and memories over the years that it would be hard to catalog them all. There was the time in Toronto that I set up a meal at a restaurant named Susur – a meal like no other I’ve ever had – and the check arrived with a jaw-dropping sum that I had not anticipated. In San Diego, we watched a gorgeous sunset over the Pacific Ocean from the veranda of the Hotel Coronado. There was the time I sunbathed on the beach in Waikiki with my book editor, and the notable distress when my colleague’s husband called from the airport to say he was not permitted to board his plane in Baltimore to join us in California! There are funny stories, but there is the sadness that one friend who joined us for so many of these events has died.
I always find the program options to be overwhelming: There is so much going on at once that it can be hard to decide what to go to. I try to attend a mix of sessions, some that are inspiring or entertaining, and others that will be informative for clinical issues.
The speakers have been incredible and over the years I’ve heard then-Vice President Joseph Biden, retired quarterback Terry Bradshaw, Oliver Sacks, Alan Alda, Archbishop Desmond Tutu, and perhaps my favorite – Lorraine Bracco, the actress who played Dr. Melfi on “The Sopranos” – to name just a few. And, of course, the opportunity to get the continuing medical education credits I need for licensing is just one more reason to attend.
Last year in May I was still adjusting to my “new” career from home with a computer screen. I had been scheduled to participate in several panels for the meeting in Philadelphia, but extra computer hours had no appeal. And while the fatigue of doing telemental health has eased, I still avoid extra hours interacting with my computer screen and I did not attend this year’s meeting. Without the lure of friends, fun, and the novelty of being somewhere new, my APA experience would have to wait for real life.
Virtual APA has had a drop in participation. In 2019, the last real-life convention in San Francisco, there were 700 scientific sessions and 11,000 professionals in attendance. This year’s virtual conference hosted 135 sessions with more than 7,000 attendees. Attendance was down, but so were costs associated with live conventions and
Tom Abdallah is a medical student at Weill Cornell Medicine–Qatar in Education City. He has never attended an in-person APA annual meeting, but he joined for this year’s virtual sessions. “The scientific sessions were fantastic and diverse. Networking was limited in comparison to in-person conferences. The meeting was very well organized, and it gave me the opportunity to attend without worrying about travel.”
Steven Daviss, MD, a psychiatrist in Maryland, also commented on the ease and financial benefit of attending the meeting from his home office. He calculated that the cost was much less: $350 for virtual APA, compared with approximately $3,500 for the real thing, allowing for transportation, hotels, meals out, and lost income. “But,” said Dr. Daviss, “engagement with colleagues was minimal.”
APA Assembly member Annette Hanson, MD, has continued to go into work throughout the pandemic. Still, she noted that meetings and committee work have made sure she does not miss out on the “Zoom fatigue” that everyone else is feeling. The virtual APA was tiring for her.
“It was brutal. There was the APA Assembly 1 weekend, right after evening Zoom reference committee meetings the week before. Then virtual APA the next weekend. By the end of the week, I had worked every day for 3 weeks straight, including my more-than-full-time job!”
It has been a challenging time, to say the least, and it has certainly helped that videoconferencing has allowed us to be there for our patients and for each other in so many different circumstances. Former APA President Paul Summergrad, MD, talked about how virtual meetings can be very good as educational tools, but he conveyed what I have been feeling in a sentence: “I miss the social aspect of meetings.”
Please get your vaccine, and I hope to see you in New Orleans next May!
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Every spring, I look forward to attending the American Psychiatric Association’s annual meeting. It has become a ritual that starts many months before the actual conference.
Submissions for presentations are due in September, so the planning often starts in the late summer. Hotel and plane reservations are made in January, and the meeting itself begins in May.
The city that hosts the event changes each year but, for me, many things do not. The Clinical Psychiatry News editorial board meeting takes place on Monday morning at 7 a.m., and I scour the program for what sessions to attend. In recent years, I have made a point of writing an article for about one of the sessions while still at the meeting – in 2019 I wrote about the improv-acting workshops I attended – something that just doesn’t translate to a Zoom experience.
I go with the same friend every year, I always attend the Hopkins alumni reception, and I organize dinner at a nice restaurant for friends. I have collected so many funny stories and memories over the years that it would be hard to catalog them all. There was the time in Toronto that I set up a meal at a restaurant named Susur – a meal like no other I’ve ever had – and the check arrived with a jaw-dropping sum that I had not anticipated. In San Diego, we watched a gorgeous sunset over the Pacific Ocean from the veranda of the Hotel Coronado. There was the time I sunbathed on the beach in Waikiki with my book editor, and the notable distress when my colleague’s husband called from the airport to say he was not permitted to board his plane in Baltimore to join us in California! There are funny stories, but there is the sadness that one friend who joined us for so many of these events has died.
I always find the program options to be overwhelming: There is so much going on at once that it can be hard to decide what to go to. I try to attend a mix of sessions, some that are inspiring or entertaining, and others that will be informative for clinical issues.
The speakers have been incredible and over the years I’ve heard then-Vice President Joseph Biden, retired quarterback Terry Bradshaw, Oliver Sacks, Alan Alda, Archbishop Desmond Tutu, and perhaps my favorite – Lorraine Bracco, the actress who played Dr. Melfi on “The Sopranos” – to name just a few. And, of course, the opportunity to get the continuing medical education credits I need for licensing is just one more reason to attend.
Last year in May I was still adjusting to my “new” career from home with a computer screen. I had been scheduled to participate in several panels for the meeting in Philadelphia, but extra computer hours had no appeal. And while the fatigue of doing telemental health has eased, I still avoid extra hours interacting with my computer screen and I did not attend this year’s meeting. Without the lure of friends, fun, and the novelty of being somewhere new, my APA experience would have to wait for real life.
Virtual APA has had a drop in participation. In 2019, the last real-life convention in San Francisco, there were 700 scientific sessions and 11,000 professionals in attendance. This year’s virtual conference hosted 135 sessions with more than 7,000 attendees. Attendance was down, but so were costs associated with live conventions and
Tom Abdallah is a medical student at Weill Cornell Medicine–Qatar in Education City. He has never attended an in-person APA annual meeting, but he joined for this year’s virtual sessions. “The scientific sessions were fantastic and diverse. Networking was limited in comparison to in-person conferences. The meeting was very well organized, and it gave me the opportunity to attend without worrying about travel.”
Steven Daviss, MD, a psychiatrist in Maryland, also commented on the ease and financial benefit of attending the meeting from his home office. He calculated that the cost was much less: $350 for virtual APA, compared with approximately $3,500 for the real thing, allowing for transportation, hotels, meals out, and lost income. “But,” said Dr. Daviss, “engagement with colleagues was minimal.”
APA Assembly member Annette Hanson, MD, has continued to go into work throughout the pandemic. Still, she noted that meetings and committee work have made sure she does not miss out on the “Zoom fatigue” that everyone else is feeling. The virtual APA was tiring for her.
“It was brutal. There was the APA Assembly 1 weekend, right after evening Zoom reference committee meetings the week before. Then virtual APA the next weekend. By the end of the week, I had worked every day for 3 weeks straight, including my more-than-full-time job!”
It has been a challenging time, to say the least, and it has certainly helped that videoconferencing has allowed us to be there for our patients and for each other in so many different circumstances. Former APA President Paul Summergrad, MD, talked about how virtual meetings can be very good as educational tools, but he conveyed what I have been feeling in a sentence: “I miss the social aspect of meetings.”
Please get your vaccine, and I hope to see you in New Orleans next May!
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Every spring, I look forward to attending the American Psychiatric Association’s annual meeting. It has become a ritual that starts many months before the actual conference.
Submissions for presentations are due in September, so the planning often starts in the late summer. Hotel and plane reservations are made in January, and the meeting itself begins in May.
The city that hosts the event changes each year but, for me, many things do not. The Clinical Psychiatry News editorial board meeting takes place on Monday morning at 7 a.m., and I scour the program for what sessions to attend. In recent years, I have made a point of writing an article for about one of the sessions while still at the meeting – in 2019 I wrote about the improv-acting workshops I attended – something that just doesn’t translate to a Zoom experience.
I go with the same friend every year, I always attend the Hopkins alumni reception, and I organize dinner at a nice restaurant for friends. I have collected so many funny stories and memories over the years that it would be hard to catalog them all. There was the time in Toronto that I set up a meal at a restaurant named Susur – a meal like no other I’ve ever had – and the check arrived with a jaw-dropping sum that I had not anticipated. In San Diego, we watched a gorgeous sunset over the Pacific Ocean from the veranda of the Hotel Coronado. There was the time I sunbathed on the beach in Waikiki with my book editor, and the notable distress when my colleague’s husband called from the airport to say he was not permitted to board his plane in Baltimore to join us in California! There are funny stories, but there is the sadness that one friend who joined us for so many of these events has died.
I always find the program options to be overwhelming: There is so much going on at once that it can be hard to decide what to go to. I try to attend a mix of sessions, some that are inspiring or entertaining, and others that will be informative for clinical issues.
The speakers have been incredible and over the years I’ve heard then-Vice President Joseph Biden, retired quarterback Terry Bradshaw, Oliver Sacks, Alan Alda, Archbishop Desmond Tutu, and perhaps my favorite – Lorraine Bracco, the actress who played Dr. Melfi on “The Sopranos” – to name just a few. And, of course, the opportunity to get the continuing medical education credits I need for licensing is just one more reason to attend.
Last year in May I was still adjusting to my “new” career from home with a computer screen. I had been scheduled to participate in several panels for the meeting in Philadelphia, but extra computer hours had no appeal. And while the fatigue of doing telemental health has eased, I still avoid extra hours interacting with my computer screen and I did not attend this year’s meeting. Without the lure of friends, fun, and the novelty of being somewhere new, my APA experience would have to wait for real life.
Virtual APA has had a drop in participation. In 2019, the last real-life convention in San Francisco, there were 700 scientific sessions and 11,000 professionals in attendance. This year’s virtual conference hosted 135 sessions with more than 7,000 attendees. Attendance was down, but so were costs associated with live conventions and
Tom Abdallah is a medical student at Weill Cornell Medicine–Qatar in Education City. He has never attended an in-person APA annual meeting, but he joined for this year’s virtual sessions. “The scientific sessions were fantastic and diverse. Networking was limited in comparison to in-person conferences. The meeting was very well organized, and it gave me the opportunity to attend without worrying about travel.”
Steven Daviss, MD, a psychiatrist in Maryland, also commented on the ease and financial benefit of attending the meeting from his home office. He calculated that the cost was much less: $350 for virtual APA, compared with approximately $3,500 for the real thing, allowing for transportation, hotels, meals out, and lost income. “But,” said Dr. Daviss, “engagement with colleagues was minimal.”
APA Assembly member Annette Hanson, MD, has continued to go into work throughout the pandemic. Still, she noted that meetings and committee work have made sure she does not miss out on the “Zoom fatigue” that everyone else is feeling. The virtual APA was tiring for her.
“It was brutal. There was the APA Assembly 1 weekend, right after evening Zoom reference committee meetings the week before. Then virtual APA the next weekend. By the end of the week, I had worked every day for 3 weeks straight, including my more-than-full-time job!”
It has been a challenging time, to say the least, and it has certainly helped that videoconferencing has allowed us to be there for our patients and for each other in so many different circumstances. Former APA President Paul Summergrad, MD, talked about how virtual meetings can be very good as educational tools, but he conveyed what I have been feeling in a sentence: “I miss the social aspect of meetings.”
Please get your vaccine, and I hope to see you in New Orleans next May!
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Who can call themselves ‘doctor’? The debate heats up
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Death from despair
I’ve taken care of both Bill and his wife for a few years. They’re a sweet couple, each with their own neurological issues. Bill has also battled depression on and off over time. He can be a challenge, and I’ve never envied his psychiatrist.
Bill committed suicide in the final week of April.
Patient deaths are unavoidable in medicine. It’s part of the job. Suicides, though less common, also happen. Sometimes they’re related to a sad diagnosis we’ve made, but more commonly (as in Bill’s case) they result from demons we had no control over.
I had a patient commit suicide about 6 months after I started my practice, and probably average one every 2 years (that I hear about) since then. They’re still the deaths that surprise me the most, make me take pause for a few minutes, even after doing this for 23 years.
Suicide is as old as humanity, and gets worse during difficult societal and economic times. It disproportionately affects doctors, dentists, veterinarians, and police officers, and leaves devastated families and friends in its wake.
Death because of the progression of time and disease is never easy, but perhaps more psychologically acceptable to those left behind. Death because of a tragic accident at any age is more difficult.
But when the person involved makes a conscious decision to end his or her own life, the effects on those left behind are terrible. Wondering why, questioning if they could have done something different, and, as with any loss, grieving.
In a world where major advances have been made in many areas of medicine, including mental health, death from despair shows no sign of abating.
Maybe it’s part of the price of sentience and reason. Or civilization. I doubt it will ever stop being a public health issue, no matter how many other diseases we cure.
But, as I write a letter to Bill’s wife, that’s little consolation for those they’ve left behind.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’ve taken care of both Bill and his wife for a few years. They’re a sweet couple, each with their own neurological issues. Bill has also battled depression on and off over time. He can be a challenge, and I’ve never envied his psychiatrist.
Bill committed suicide in the final week of April.
Patient deaths are unavoidable in medicine. It’s part of the job. Suicides, though less common, also happen. Sometimes they’re related to a sad diagnosis we’ve made, but more commonly (as in Bill’s case) they result from demons we had no control over.
I had a patient commit suicide about 6 months after I started my practice, and probably average one every 2 years (that I hear about) since then. They’re still the deaths that surprise me the most, make me take pause for a few minutes, even after doing this for 23 years.
Suicide is as old as humanity, and gets worse during difficult societal and economic times. It disproportionately affects doctors, dentists, veterinarians, and police officers, and leaves devastated families and friends in its wake.
Death because of the progression of time and disease is never easy, but perhaps more psychologically acceptable to those left behind. Death because of a tragic accident at any age is more difficult.
But when the person involved makes a conscious decision to end his or her own life, the effects on those left behind are terrible. Wondering why, questioning if they could have done something different, and, as with any loss, grieving.
In a world where major advances have been made in many areas of medicine, including mental health, death from despair shows no sign of abating.
Maybe it’s part of the price of sentience and reason. Or civilization. I doubt it will ever stop being a public health issue, no matter how many other diseases we cure.
But, as I write a letter to Bill’s wife, that’s little consolation for those they’ve left behind.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’ve taken care of both Bill and his wife for a few years. They’re a sweet couple, each with their own neurological issues. Bill has also battled depression on and off over time. He can be a challenge, and I’ve never envied his psychiatrist.
Bill committed suicide in the final week of April.
Patient deaths are unavoidable in medicine. It’s part of the job. Suicides, though less common, also happen. Sometimes they’re related to a sad diagnosis we’ve made, but more commonly (as in Bill’s case) they result from demons we had no control over.
I had a patient commit suicide about 6 months after I started my practice, and probably average one every 2 years (that I hear about) since then. They’re still the deaths that surprise me the most, make me take pause for a few minutes, even after doing this for 23 years.
Suicide is as old as humanity, and gets worse during difficult societal and economic times. It disproportionately affects doctors, dentists, veterinarians, and police officers, and leaves devastated families and friends in its wake.
Death because of the progression of time and disease is never easy, but perhaps more psychologically acceptable to those left behind. Death because of a tragic accident at any age is more difficult.
But when the person involved makes a conscious decision to end his or her own life, the effects on those left behind are terrible. Wondering why, questioning if they could have done something different, and, as with any loss, grieving.
In a world where major advances have been made in many areas of medicine, including mental health, death from despair shows no sign of abating.
Maybe it’s part of the price of sentience and reason. Or civilization. I doubt it will ever stop being a public health issue, no matter how many other diseases we cure.
But, as I write a letter to Bill’s wife, that’s little consolation for those they’ve left behind.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Doctors lose jobs after speaking out about unsafe conditions
In April 2020, hospitalist Samantha Houston, MD, lost her job at Baptist Memorial Hospital–North, in Oxford, Miss., after she publicly campaigned to get donations of N95 masks for nurses. Dr. Houston filed a lawsuit against the hospital, saying she was improperly fired for speaking out. The lawsuit has not yet gone to trial.
In January 2017, emergency physician Raymond Brovont, MD, was fired by EmCare, an emergency physician staffing company, after reporting understaffing at hospitals with which it contracted in the Kansas City, Mo., area. Dr. Brovont sued EmCare, and the company lost the case. In February 2019, it was ordered to pay him $13.1 million in damages.
These are just two of several cases in recent years in which physicians have spoken out about problems involving patient care and have been sanctioned. Other physicians who see problems choose to stay silent.
Doctors often hesitate to speak out because of the prospect of losing their jobs. A 2013 study of emergency physicians found that nearly 20% reported a possible or real threat to their employment if they expressed concerns about quality of care.
When physicians do not speak openly about important medical issues, the quality of care in their institutions suffers, said a coauthor of the study, Larry D. Weiss, MD, JD, a retired professor of emergency medicine at the University of Maryland, Baltimore.
“Physicians can’t effectively represent patients if they are always thinking they can get fired for what they say,” Dr. Weiss said. “If you don’t have protections like due process, which is often the case, you are less likely to speak out.”
In the first few weeks, health care facilities were struggling to obtain personal protective equipment (PPE) and to create policies that would keep patients and caregivers safe.
Physicians such as Dr. Houston took the initiative to make sure their institutions were taking the right steps against COVID-19 and found themselves at loggerheads with administrators who were concerned that their organizations were being portrayed as unsafe.
The case of one physician who spoke out
One of the highest-profile cases of a physician speaking out and being removed from work during the pandemic is that of Ming Lin, MD, an emergency physician who lost a job he had held for 17 years at St. Joseph Medical Center, in Bellingham, Wash. Dr. Lin lost his job after he made a series of Facebook posts that criticized the hospital’s COVID-19 preparedness efforts.
In an interview, Dr. Lin discussed the details of his situation to a degree that rarely occurs in such cases. This is one of the most extensive interviews he has granted.
Postings on Facebook
Dr. Lin said that on the basis of an intense study of the virus at the onset of the pandemic, he developed many ideas as to what could be done to mitigate its spread. While working as a locum tenens physician on his time off, he could see how others dealt with COVID-19.
Dr. Lin said from past experiences he did not feel that he could present his ideas directly to administration and be heard, so he decided to air his ideas about how his hospital could handle COVID-19 on his Facebook page, which drew a large audience.
He said he was certain that hospital administrators were reading his posts. He said receptionists at this hospital were advised not to wear masks, evidently because it would alarm patients. Dr. Lin said he posted concerns about their safety and called for them to wear masks. Soon after, the hospital directed receptionists to wear masks.
Dr. Lin’s Facebook posts also criticized the hospital for taking what he felt was too long to get results on COVID-19 tests. “It was taking them up to 10 days to get test results, because samples were being sent to a lab in California,” he said. He suggested it would be faster to send samples to the University of Washington. Soon after, the hospital started sending samples there.
In just a couple of weeks, Dr. Lin said, he voiced almost a dozen concerns. Each time the hospital made changes in line with his recommendations. Although he didn’t get any direct acknowledgment from the hospital for his help, he said he felt he was making a positive impact.
How employers react to physicians who speak out
Physicians who speak out about conditions tend to deeply disturb administrators, said William P. Sullivan, DO, JD, an emergency physician and lawyer in Frankfort, Ill., who has written about physicians being terminated by hospitals.
“These physicians go to the news media or they use social media,” Dr. Sullivan said, “but hospital administrators don’t want the public to hear bad things about their hospital.”
Then the public might not come to the hospital, which is an administrator’s worst nightmare. Even if physicians think their criticisms are reasonable, administrators may still fear a resulting drop in patients.
Dr. Houston, for example, was helping her Mississippi hospital by collecting donations of N95 masks for nurses, but to administrators, it showed that the hospital did not have enough masks.
“It is not helpful to stoke fear and anxiety, even if the intent is sincere,” a spokesperson for the hospital said.
Administrator fires back
Dr. Lin’s posts were deeply concerning to Richard DeCarlo, chief operating officer of PeaceHealth, which runs St. Joseph Hospital. Mr. DeCarlo discussed his concerns in a video interview in April with the blogger Zubin Damania, MD, known as ZDoggMD.
Comments on Dr. Lin’s Facebook posts showed that people “were fearful to go to the hospital,” he told Dr. Damania. “They were concluding that they would need to drive to another hospital.”
Mr. DeCarlo said he was also unhappy that Dr. Lin did not directly contact administrators about his concerns. “He didn’t communicate with his medical director,” Mr. DeCarlo said in the interview. “The ED staff had been meeting three times a week with the chief medical officer to make sure they had everything they needed, but he only attended one of these meetings and didn’t ask any questions.”
Dr. Lin maintains he did ask questions at the first meeting but stopped attending because he felt he wasn’t being heeded. “I found their tone not very receptive,” he said.
Doctor allegedly offered “misinformation”
At the start of the pandemic, some hospitals made it clear what would happen to doctors who brought up lack of PPE or other problems to the media. For example, NYU Langone Medical Center in New York sent an email to staff warning that speaking to the media without permission “will be subject to disciplinary action, including termination.”
PeaceHealth took a different tack. “It’s not that we have a policy that says don’t ever talk to the media,” Mr. DeCarlo said in the ZDoggMD interview, but in Dr. Lin’s case, “what was at issue was the misinformation. His leader went to him and said, ‘Look, you’re posting things that aren’t accurate.’ ”
Dr. Lin disputes that he provided any misinformation. In the interview, Mr. DeCarlo cited just one example of alleged misinformation. He said Dr. Lin called for a tent outside the emergency department (ED) to protect patients entering the department from aerosol exposure to COVID-19. Mr. DeCarlo said the tent was not needed because fewer people were using the ED.
“To put it in an extreme way,” Mr. DeCarlo said of Dr. Lin’s posts, “it was like yelling fire in a theater where there is not a fire.”
Dr. Lin said the hospital did briefly erect a tent and then removed it, and he still insisted that a tent was a good idea. He added that Mr. DeCarlo never mentioned any of the other suggestions Dr. Lin made, nor did he state that the hospital adopted them.
Doctor gets a warning
Dr. Lin said that after he started posting his concerns, he got a call from the emergency department director who worked for TeamHealth, an emergency medicine staffing firm that contracted with PeaceHealth and employed Dr. Lin, too.
Dr. Lin said his immediate supervisor at TeamHealth told him the hospital was unhappy with his posts and that he should take them down and suggested he might be fired. Dr. Lin said the supervisor also asked him to apologize to the hospital administration for these posts, but he refused to do so.
“Retracting and apologizing was not only wrong but would have left me vulnerable to being terminated with no repercussions,” he said.
“At that point, I realized I had crossed the Rubicon,” Dr. Lin said. He thought he might well be fired, no matter what he did, so he took his story to The Seattle Times, which had a much wider platform than his Facebook page had.
Dr. Lin lost his job at St. Joseph a week after The Seattle Times story about him appeared. “About 10 minutes before my shift was supposed to start, I received a text message from TeamHealth saying that someone else would be taking the shift,” he said.
In a release, TeamHealth insisted Dr. Lin was not fired and that he was scheduled to be reassigned to work at other hospitals. Dr. Lin, however, said he was not told this at the time and that he found out later that the new assignment would involve a pay cut and a significant commute. He said he has not taken any new assignments from TeamHealth since he lost his job at St. Joseph.
Dr. Lin has filed a lawsuit against PeaceHealth, TeamHealth, and Mr. DeCarlo, asking for his job back and for an apology. He said he has not asked for any financial damages at this point.
Since leaving St. Joseph, Dr. Lin has been working as an administrator for the Indian Health Service in the upper plains states. He said he can do some of the work at home in Washington State, which allows him to be with his wife and three young children.
Dr. Lin no longer sees patients. “I feel I have lost my confidence as a clinician,” he said. “I’m not sure why, but I find it hard to make quick judgments when taking care of patients.”
He said many doctors have told him about their own troubles with speaking out, but they did not want to come forward and talk about it because they feared more repercussions.
Do doctors who speak out have any rights?
Because TeamHealth, Dr. Lin’s actual employer, asserts he was never actually terminated, Dr. Lin has not been able to appeal his case internally in accordance with due process, an option that allows doctors to get a fair hearing and to appeal decisions against them.
The American Academy of Emergency Medicine pointed out this problem. “Dr. Lin, as a member of the medical staff, is entitled to full due process and a fair hearing from his peers on the medical staff,” the academy said in a statement supporting him.
The Joint Commission, the hospital accreditor, requires that hospitals provide due process to doctors before they can be terminated. However, Dr. Sullivan said employers often make physicians waive their due process rights in the employment contract. “The result is that the employer can terminate doctors for no reason,” he said.
In the 2013 survey of emergency physicians, 62% reported that their employers could terminate them without full due process.
Dr. Weiss, the Maryland MD-JD, said that when he advises doctors on their contracts, he generally tells them to cross out the waiver language. The applicant, he says, may also tell the employer that the waivers are considered unethical by many physician professional societies. In some cases, he said, the hospital will back down.
Conclusion
To maintain quality of care, it is essential that physicians feel free to speak out about issues that concern them. They can improve their chances of being heard by working directly with management and attending meetings, but in some cases, management may be unwilling to listen.
A version of this article first appeared on Medscape.com.
In April 2020, hospitalist Samantha Houston, MD, lost her job at Baptist Memorial Hospital–North, in Oxford, Miss., after she publicly campaigned to get donations of N95 masks for nurses. Dr. Houston filed a lawsuit against the hospital, saying she was improperly fired for speaking out. The lawsuit has not yet gone to trial.
In January 2017, emergency physician Raymond Brovont, MD, was fired by EmCare, an emergency physician staffing company, after reporting understaffing at hospitals with which it contracted in the Kansas City, Mo., area. Dr. Brovont sued EmCare, and the company lost the case. In February 2019, it was ordered to pay him $13.1 million in damages.
These are just two of several cases in recent years in which physicians have spoken out about problems involving patient care and have been sanctioned. Other physicians who see problems choose to stay silent.
Doctors often hesitate to speak out because of the prospect of losing their jobs. A 2013 study of emergency physicians found that nearly 20% reported a possible or real threat to their employment if they expressed concerns about quality of care.
When physicians do not speak openly about important medical issues, the quality of care in their institutions suffers, said a coauthor of the study, Larry D. Weiss, MD, JD, a retired professor of emergency medicine at the University of Maryland, Baltimore.
“Physicians can’t effectively represent patients if they are always thinking they can get fired for what they say,” Dr. Weiss said. “If you don’t have protections like due process, which is often the case, you are less likely to speak out.”
In the first few weeks, health care facilities were struggling to obtain personal protective equipment (PPE) and to create policies that would keep patients and caregivers safe.
Physicians such as Dr. Houston took the initiative to make sure their institutions were taking the right steps against COVID-19 and found themselves at loggerheads with administrators who were concerned that their organizations were being portrayed as unsafe.
The case of one physician who spoke out
One of the highest-profile cases of a physician speaking out and being removed from work during the pandemic is that of Ming Lin, MD, an emergency physician who lost a job he had held for 17 years at St. Joseph Medical Center, in Bellingham, Wash. Dr. Lin lost his job after he made a series of Facebook posts that criticized the hospital’s COVID-19 preparedness efforts.
In an interview, Dr. Lin discussed the details of his situation to a degree that rarely occurs in such cases. This is one of the most extensive interviews he has granted.
Postings on Facebook
Dr. Lin said that on the basis of an intense study of the virus at the onset of the pandemic, he developed many ideas as to what could be done to mitigate its spread. While working as a locum tenens physician on his time off, he could see how others dealt with COVID-19.
Dr. Lin said from past experiences he did not feel that he could present his ideas directly to administration and be heard, so he decided to air his ideas about how his hospital could handle COVID-19 on his Facebook page, which drew a large audience.
He said he was certain that hospital administrators were reading his posts. He said receptionists at this hospital were advised not to wear masks, evidently because it would alarm patients. Dr. Lin said he posted concerns about their safety and called for them to wear masks. Soon after, the hospital directed receptionists to wear masks.
Dr. Lin’s Facebook posts also criticized the hospital for taking what he felt was too long to get results on COVID-19 tests. “It was taking them up to 10 days to get test results, because samples were being sent to a lab in California,” he said. He suggested it would be faster to send samples to the University of Washington. Soon after, the hospital started sending samples there.
In just a couple of weeks, Dr. Lin said, he voiced almost a dozen concerns. Each time the hospital made changes in line with his recommendations. Although he didn’t get any direct acknowledgment from the hospital for his help, he said he felt he was making a positive impact.
How employers react to physicians who speak out
Physicians who speak out about conditions tend to deeply disturb administrators, said William P. Sullivan, DO, JD, an emergency physician and lawyer in Frankfort, Ill., who has written about physicians being terminated by hospitals.
“These physicians go to the news media or they use social media,” Dr. Sullivan said, “but hospital administrators don’t want the public to hear bad things about their hospital.”
Then the public might not come to the hospital, which is an administrator’s worst nightmare. Even if physicians think their criticisms are reasonable, administrators may still fear a resulting drop in patients.
Dr. Houston, for example, was helping her Mississippi hospital by collecting donations of N95 masks for nurses, but to administrators, it showed that the hospital did not have enough masks.
“It is not helpful to stoke fear and anxiety, even if the intent is sincere,” a spokesperson for the hospital said.
Administrator fires back
Dr. Lin’s posts were deeply concerning to Richard DeCarlo, chief operating officer of PeaceHealth, which runs St. Joseph Hospital. Mr. DeCarlo discussed his concerns in a video interview in April with the blogger Zubin Damania, MD, known as ZDoggMD.
Comments on Dr. Lin’s Facebook posts showed that people “were fearful to go to the hospital,” he told Dr. Damania. “They were concluding that they would need to drive to another hospital.”
Mr. DeCarlo said he was also unhappy that Dr. Lin did not directly contact administrators about his concerns. “He didn’t communicate with his medical director,” Mr. DeCarlo said in the interview. “The ED staff had been meeting three times a week with the chief medical officer to make sure they had everything they needed, but he only attended one of these meetings and didn’t ask any questions.”
Dr. Lin maintains he did ask questions at the first meeting but stopped attending because he felt he wasn’t being heeded. “I found their tone not very receptive,” he said.
Doctor allegedly offered “misinformation”
At the start of the pandemic, some hospitals made it clear what would happen to doctors who brought up lack of PPE or other problems to the media. For example, NYU Langone Medical Center in New York sent an email to staff warning that speaking to the media without permission “will be subject to disciplinary action, including termination.”
PeaceHealth took a different tack. “It’s not that we have a policy that says don’t ever talk to the media,” Mr. DeCarlo said in the ZDoggMD interview, but in Dr. Lin’s case, “what was at issue was the misinformation. His leader went to him and said, ‘Look, you’re posting things that aren’t accurate.’ ”
Dr. Lin disputes that he provided any misinformation. In the interview, Mr. DeCarlo cited just one example of alleged misinformation. He said Dr. Lin called for a tent outside the emergency department (ED) to protect patients entering the department from aerosol exposure to COVID-19. Mr. DeCarlo said the tent was not needed because fewer people were using the ED.
“To put it in an extreme way,” Mr. DeCarlo said of Dr. Lin’s posts, “it was like yelling fire in a theater where there is not a fire.”
Dr. Lin said the hospital did briefly erect a tent and then removed it, and he still insisted that a tent was a good idea. He added that Mr. DeCarlo never mentioned any of the other suggestions Dr. Lin made, nor did he state that the hospital adopted them.
Doctor gets a warning
Dr. Lin said that after he started posting his concerns, he got a call from the emergency department director who worked for TeamHealth, an emergency medicine staffing firm that contracted with PeaceHealth and employed Dr. Lin, too.
Dr. Lin said his immediate supervisor at TeamHealth told him the hospital was unhappy with his posts and that he should take them down and suggested he might be fired. Dr. Lin said the supervisor also asked him to apologize to the hospital administration for these posts, but he refused to do so.
“Retracting and apologizing was not only wrong but would have left me vulnerable to being terminated with no repercussions,” he said.
“At that point, I realized I had crossed the Rubicon,” Dr. Lin said. He thought he might well be fired, no matter what he did, so he took his story to The Seattle Times, which had a much wider platform than his Facebook page had.
Dr. Lin lost his job at St. Joseph a week after The Seattle Times story about him appeared. “About 10 minutes before my shift was supposed to start, I received a text message from TeamHealth saying that someone else would be taking the shift,” he said.
In a release, TeamHealth insisted Dr. Lin was not fired and that he was scheduled to be reassigned to work at other hospitals. Dr. Lin, however, said he was not told this at the time and that he found out later that the new assignment would involve a pay cut and a significant commute. He said he has not taken any new assignments from TeamHealth since he lost his job at St. Joseph.
Dr. Lin has filed a lawsuit against PeaceHealth, TeamHealth, and Mr. DeCarlo, asking for his job back and for an apology. He said he has not asked for any financial damages at this point.
Since leaving St. Joseph, Dr. Lin has been working as an administrator for the Indian Health Service in the upper plains states. He said he can do some of the work at home in Washington State, which allows him to be with his wife and three young children.
Dr. Lin no longer sees patients. “I feel I have lost my confidence as a clinician,” he said. “I’m not sure why, but I find it hard to make quick judgments when taking care of patients.”
He said many doctors have told him about their own troubles with speaking out, but they did not want to come forward and talk about it because they feared more repercussions.
Do doctors who speak out have any rights?
Because TeamHealth, Dr. Lin’s actual employer, asserts he was never actually terminated, Dr. Lin has not been able to appeal his case internally in accordance with due process, an option that allows doctors to get a fair hearing and to appeal decisions against them.
The American Academy of Emergency Medicine pointed out this problem. “Dr. Lin, as a member of the medical staff, is entitled to full due process and a fair hearing from his peers on the medical staff,” the academy said in a statement supporting him.
The Joint Commission, the hospital accreditor, requires that hospitals provide due process to doctors before they can be terminated. However, Dr. Sullivan said employers often make physicians waive their due process rights in the employment contract. “The result is that the employer can terminate doctors for no reason,” he said.
In the 2013 survey of emergency physicians, 62% reported that their employers could terminate them without full due process.
Dr. Weiss, the Maryland MD-JD, said that when he advises doctors on their contracts, he generally tells them to cross out the waiver language. The applicant, he says, may also tell the employer that the waivers are considered unethical by many physician professional societies. In some cases, he said, the hospital will back down.
Conclusion
To maintain quality of care, it is essential that physicians feel free to speak out about issues that concern them. They can improve their chances of being heard by working directly with management and attending meetings, but in some cases, management may be unwilling to listen.
A version of this article first appeared on Medscape.com.
In April 2020, hospitalist Samantha Houston, MD, lost her job at Baptist Memorial Hospital–North, in Oxford, Miss., after she publicly campaigned to get donations of N95 masks for nurses. Dr. Houston filed a lawsuit against the hospital, saying she was improperly fired for speaking out. The lawsuit has not yet gone to trial.
In January 2017, emergency physician Raymond Brovont, MD, was fired by EmCare, an emergency physician staffing company, after reporting understaffing at hospitals with which it contracted in the Kansas City, Mo., area. Dr. Brovont sued EmCare, and the company lost the case. In February 2019, it was ordered to pay him $13.1 million in damages.
These are just two of several cases in recent years in which physicians have spoken out about problems involving patient care and have been sanctioned. Other physicians who see problems choose to stay silent.
Doctors often hesitate to speak out because of the prospect of losing their jobs. A 2013 study of emergency physicians found that nearly 20% reported a possible or real threat to their employment if they expressed concerns about quality of care.
When physicians do not speak openly about important medical issues, the quality of care in their institutions suffers, said a coauthor of the study, Larry D. Weiss, MD, JD, a retired professor of emergency medicine at the University of Maryland, Baltimore.
“Physicians can’t effectively represent patients if they are always thinking they can get fired for what they say,” Dr. Weiss said. “If you don’t have protections like due process, which is often the case, you are less likely to speak out.”
In the first few weeks, health care facilities were struggling to obtain personal protective equipment (PPE) and to create policies that would keep patients and caregivers safe.
Physicians such as Dr. Houston took the initiative to make sure their institutions were taking the right steps against COVID-19 and found themselves at loggerheads with administrators who were concerned that their organizations were being portrayed as unsafe.
The case of one physician who spoke out
One of the highest-profile cases of a physician speaking out and being removed from work during the pandemic is that of Ming Lin, MD, an emergency physician who lost a job he had held for 17 years at St. Joseph Medical Center, in Bellingham, Wash. Dr. Lin lost his job after he made a series of Facebook posts that criticized the hospital’s COVID-19 preparedness efforts.
In an interview, Dr. Lin discussed the details of his situation to a degree that rarely occurs in such cases. This is one of the most extensive interviews he has granted.
Postings on Facebook
Dr. Lin said that on the basis of an intense study of the virus at the onset of the pandemic, he developed many ideas as to what could be done to mitigate its spread. While working as a locum tenens physician on his time off, he could see how others dealt with COVID-19.
Dr. Lin said from past experiences he did not feel that he could present his ideas directly to administration and be heard, so he decided to air his ideas about how his hospital could handle COVID-19 on his Facebook page, which drew a large audience.
He said he was certain that hospital administrators were reading his posts. He said receptionists at this hospital were advised not to wear masks, evidently because it would alarm patients. Dr. Lin said he posted concerns about their safety and called for them to wear masks. Soon after, the hospital directed receptionists to wear masks.
Dr. Lin’s Facebook posts also criticized the hospital for taking what he felt was too long to get results on COVID-19 tests. “It was taking them up to 10 days to get test results, because samples were being sent to a lab in California,” he said. He suggested it would be faster to send samples to the University of Washington. Soon after, the hospital started sending samples there.
In just a couple of weeks, Dr. Lin said, he voiced almost a dozen concerns. Each time the hospital made changes in line with his recommendations. Although he didn’t get any direct acknowledgment from the hospital for his help, he said he felt he was making a positive impact.
How employers react to physicians who speak out
Physicians who speak out about conditions tend to deeply disturb administrators, said William P. Sullivan, DO, JD, an emergency physician and lawyer in Frankfort, Ill., who has written about physicians being terminated by hospitals.
“These physicians go to the news media or they use social media,” Dr. Sullivan said, “but hospital administrators don’t want the public to hear bad things about their hospital.”
Then the public might not come to the hospital, which is an administrator’s worst nightmare. Even if physicians think their criticisms are reasonable, administrators may still fear a resulting drop in patients.
Dr. Houston, for example, was helping her Mississippi hospital by collecting donations of N95 masks for nurses, but to administrators, it showed that the hospital did not have enough masks.
“It is not helpful to stoke fear and anxiety, even if the intent is sincere,” a spokesperson for the hospital said.
Administrator fires back
Dr. Lin’s posts were deeply concerning to Richard DeCarlo, chief operating officer of PeaceHealth, which runs St. Joseph Hospital. Mr. DeCarlo discussed his concerns in a video interview in April with the blogger Zubin Damania, MD, known as ZDoggMD.
Comments on Dr. Lin’s Facebook posts showed that people “were fearful to go to the hospital,” he told Dr. Damania. “They were concluding that they would need to drive to another hospital.”
Mr. DeCarlo said he was also unhappy that Dr. Lin did not directly contact administrators about his concerns. “He didn’t communicate with his medical director,” Mr. DeCarlo said in the interview. “The ED staff had been meeting three times a week with the chief medical officer to make sure they had everything they needed, but he only attended one of these meetings and didn’t ask any questions.”
Dr. Lin maintains he did ask questions at the first meeting but stopped attending because he felt he wasn’t being heeded. “I found their tone not very receptive,” he said.
Doctor allegedly offered “misinformation”
At the start of the pandemic, some hospitals made it clear what would happen to doctors who brought up lack of PPE or other problems to the media. For example, NYU Langone Medical Center in New York sent an email to staff warning that speaking to the media without permission “will be subject to disciplinary action, including termination.”
PeaceHealth took a different tack. “It’s not that we have a policy that says don’t ever talk to the media,” Mr. DeCarlo said in the ZDoggMD interview, but in Dr. Lin’s case, “what was at issue was the misinformation. His leader went to him and said, ‘Look, you’re posting things that aren’t accurate.’ ”
Dr. Lin disputes that he provided any misinformation. In the interview, Mr. DeCarlo cited just one example of alleged misinformation. He said Dr. Lin called for a tent outside the emergency department (ED) to protect patients entering the department from aerosol exposure to COVID-19. Mr. DeCarlo said the tent was not needed because fewer people were using the ED.
“To put it in an extreme way,” Mr. DeCarlo said of Dr. Lin’s posts, “it was like yelling fire in a theater where there is not a fire.”
Dr. Lin said the hospital did briefly erect a tent and then removed it, and he still insisted that a tent was a good idea. He added that Mr. DeCarlo never mentioned any of the other suggestions Dr. Lin made, nor did he state that the hospital adopted them.
Doctor gets a warning
Dr. Lin said that after he started posting his concerns, he got a call from the emergency department director who worked for TeamHealth, an emergency medicine staffing firm that contracted with PeaceHealth and employed Dr. Lin, too.
Dr. Lin said his immediate supervisor at TeamHealth told him the hospital was unhappy with his posts and that he should take them down and suggested he might be fired. Dr. Lin said the supervisor also asked him to apologize to the hospital administration for these posts, but he refused to do so.
“Retracting and apologizing was not only wrong but would have left me vulnerable to being terminated with no repercussions,” he said.
“At that point, I realized I had crossed the Rubicon,” Dr. Lin said. He thought he might well be fired, no matter what he did, so he took his story to The Seattle Times, which had a much wider platform than his Facebook page had.
Dr. Lin lost his job at St. Joseph a week after The Seattle Times story about him appeared. “About 10 minutes before my shift was supposed to start, I received a text message from TeamHealth saying that someone else would be taking the shift,” he said.
In a release, TeamHealth insisted Dr. Lin was not fired and that he was scheduled to be reassigned to work at other hospitals. Dr. Lin, however, said he was not told this at the time and that he found out later that the new assignment would involve a pay cut and a significant commute. He said he has not taken any new assignments from TeamHealth since he lost his job at St. Joseph.
Dr. Lin has filed a lawsuit against PeaceHealth, TeamHealth, and Mr. DeCarlo, asking for his job back and for an apology. He said he has not asked for any financial damages at this point.
Since leaving St. Joseph, Dr. Lin has been working as an administrator for the Indian Health Service in the upper plains states. He said he can do some of the work at home in Washington State, which allows him to be with his wife and three young children.
Dr. Lin no longer sees patients. “I feel I have lost my confidence as a clinician,” he said. “I’m not sure why, but I find it hard to make quick judgments when taking care of patients.”
He said many doctors have told him about their own troubles with speaking out, but they did not want to come forward and talk about it because they feared more repercussions.
Do doctors who speak out have any rights?
Because TeamHealth, Dr. Lin’s actual employer, asserts he was never actually terminated, Dr. Lin has not been able to appeal his case internally in accordance with due process, an option that allows doctors to get a fair hearing and to appeal decisions against them.
The American Academy of Emergency Medicine pointed out this problem. “Dr. Lin, as a member of the medical staff, is entitled to full due process and a fair hearing from his peers on the medical staff,” the academy said in a statement supporting him.
The Joint Commission, the hospital accreditor, requires that hospitals provide due process to doctors before they can be terminated. However, Dr. Sullivan said employers often make physicians waive their due process rights in the employment contract. “The result is that the employer can terminate doctors for no reason,” he said.
In the 2013 survey of emergency physicians, 62% reported that their employers could terminate them without full due process.
Dr. Weiss, the Maryland MD-JD, said that when he advises doctors on their contracts, he generally tells them to cross out the waiver language. The applicant, he says, may also tell the employer that the waivers are considered unethical by many physician professional societies. In some cases, he said, the hospital will back down.
Conclusion
To maintain quality of care, it is essential that physicians feel free to speak out about issues that concern them. They can improve their chances of being heard by working directly with management and attending meetings, but in some cases, management may be unwilling to listen.
A version of this article first appeared on Medscape.com.
Is common courtesy no longer contagious?
The other day, in a fairly common occurrence, I needed to fax a records request over to another office.
Not having memorized all the fax numbers in my area, I turned to the internet and quickly had their website and the needed information in front of me.
But at the top of the page, before you got to phone numbers and directions, was this statement in bold print (caps as seen):
“NOTICE TO ALL PATIENTS:
“Please show RESPECT AND KINDNESS to other patients and staff.
“We have a ZERO TOLERANCE policy for aggressive behavior, vulgar language, and violence, whether in person, on the phone, or online.”
A veterinarian I know recently put something similar up, saying: “We DO NOT TOLERATE physically or verbally abusive behavior by clients. We are compassionate and understand you are under stress, but we are also human and deserve respect. Thank you.”
I absolutely agree with this. Hell, I’m the same way.
But what is wrong with people that we actually need to have notices like that up?
Realistically, the vast majority of patients don’t need the reminder. They treat each other, and my staff, with politeness and respect, and we do the same. To me that’s part of the whole sandbox thing. Personally, I prefer my office to have the same atmosphere as a library, and am known to “shhhh” people who are too loud.
But the real point here is that we shouldn’t have to remind anyone else to behave with common courtesy. If you’re an adult, I’m going to assume your parents and teachers taught you the importance of manners and the Golden Rule.
I’ve been in practice for 23 years now, and I’ve never had to deal with this sort of behavior, this frequently, before. Is it that the pandemic, and its economic and social consequences, has gotten on everyone’s nerves? If so, hopefully it will gradually fade away as the crisis does. I’m vaccinated. My family and the majority of my patients are vaccinated. I encourage pretty much everyone who asks me about it to get vaccinated.
But I’m more concerned that isn’t really the issue. Maybe our polarized, divided society is moving in that direction. Common good is now often reduced to us against them, and the conditions of the times have just aggravated a problem that was festering.
The majority of people, of all beliefs, remain decent people. But
Decency and manners, unfortunately, can’t be legislated. If you’ve forgotten yours, though, don’t think others will put up with you.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The other day, in a fairly common occurrence, I needed to fax a records request over to another office.
Not having memorized all the fax numbers in my area, I turned to the internet and quickly had their website and the needed information in front of me.
But at the top of the page, before you got to phone numbers and directions, was this statement in bold print (caps as seen):
“NOTICE TO ALL PATIENTS:
“Please show RESPECT AND KINDNESS to other patients and staff.
“We have a ZERO TOLERANCE policy for aggressive behavior, vulgar language, and violence, whether in person, on the phone, or online.”
A veterinarian I know recently put something similar up, saying: “We DO NOT TOLERATE physically or verbally abusive behavior by clients. We are compassionate and understand you are under stress, but we are also human and deserve respect. Thank you.”
I absolutely agree with this. Hell, I’m the same way.
But what is wrong with people that we actually need to have notices like that up?
Realistically, the vast majority of patients don’t need the reminder. They treat each other, and my staff, with politeness and respect, and we do the same. To me that’s part of the whole sandbox thing. Personally, I prefer my office to have the same atmosphere as a library, and am known to “shhhh” people who are too loud.
But the real point here is that we shouldn’t have to remind anyone else to behave with common courtesy. If you’re an adult, I’m going to assume your parents and teachers taught you the importance of manners and the Golden Rule.
I’ve been in practice for 23 years now, and I’ve never had to deal with this sort of behavior, this frequently, before. Is it that the pandemic, and its economic and social consequences, has gotten on everyone’s nerves? If so, hopefully it will gradually fade away as the crisis does. I’m vaccinated. My family and the majority of my patients are vaccinated. I encourage pretty much everyone who asks me about it to get vaccinated.
But I’m more concerned that isn’t really the issue. Maybe our polarized, divided society is moving in that direction. Common good is now often reduced to us against them, and the conditions of the times have just aggravated a problem that was festering.
The majority of people, of all beliefs, remain decent people. But
Decency and manners, unfortunately, can’t be legislated. If you’ve forgotten yours, though, don’t think others will put up with you.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The other day, in a fairly common occurrence, I needed to fax a records request over to another office.
Not having memorized all the fax numbers in my area, I turned to the internet and quickly had their website and the needed information in front of me.
But at the top of the page, before you got to phone numbers and directions, was this statement in bold print (caps as seen):
“NOTICE TO ALL PATIENTS:
“Please show RESPECT AND KINDNESS to other patients and staff.
“We have a ZERO TOLERANCE policy for aggressive behavior, vulgar language, and violence, whether in person, on the phone, or online.”
A veterinarian I know recently put something similar up, saying: “We DO NOT TOLERATE physically or verbally abusive behavior by clients. We are compassionate and understand you are under stress, but we are also human and deserve respect. Thank you.”
I absolutely agree with this. Hell, I’m the same way.
But what is wrong with people that we actually need to have notices like that up?
Realistically, the vast majority of patients don’t need the reminder. They treat each other, and my staff, with politeness and respect, and we do the same. To me that’s part of the whole sandbox thing. Personally, I prefer my office to have the same atmosphere as a library, and am known to “shhhh” people who are too loud.
But the real point here is that we shouldn’t have to remind anyone else to behave with common courtesy. If you’re an adult, I’m going to assume your parents and teachers taught you the importance of manners and the Golden Rule.
I’ve been in practice for 23 years now, and I’ve never had to deal with this sort of behavior, this frequently, before. Is it that the pandemic, and its economic and social consequences, has gotten on everyone’s nerves? If so, hopefully it will gradually fade away as the crisis does. I’m vaccinated. My family and the majority of my patients are vaccinated. I encourage pretty much everyone who asks me about it to get vaccinated.
But I’m more concerned that isn’t really the issue. Maybe our polarized, divided society is moving in that direction. Common good is now often reduced to us against them, and the conditions of the times have just aggravated a problem that was festering.
The majority of people, of all beliefs, remain decent people. But
Decency and manners, unfortunately, can’t be legislated. If you’ve forgotten yours, though, don’t think others will put up with you.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Experts say teledermatology’s postpandemic role is unclear
over those provided prior to the COVID-19 pandemic. But it is not clear whether the current rate will fall further, be sustained, or even climb again, according to data presented and opinions expressed in a forum on this topic at the American Academy of Dermatology Virtual Meeting Experience.
There are many unknowns, not least of which is future reimbursement from the Centers for Medicare & Medicaid Services and other third-party payers, according to several participants in a scientific session devoted to this topic. The CARES Act, which was passed in the early stages of the pandemic, provided only a temporary increase in reimbursement for telehealth. Postpandemic payments for telehealth services are yet undetermined.
Many of the assembled experts are convinced that teledermatology will continue to be offered at far higher rates than prior to the pandemic, but many issues, including physician acceptance of this approach remain unresolved. This was reflected in an AAD survey of members conducted in June 2020.
“Seventy percent of dermatologists responded that teledermatology will continue, but only 58% reported that they intend to offer it,” after the pandemic, reported Jules Lipoff, MD, assistant professor of dermatology at the University of Pennsylvania, Philadelphia, who is one of the authors of the paper that reported the results.
The low relative proportion of dermatologists planning to participate in teledermatology might at least in part reflect uncertainty about reimbursement, according to Dr. Lipoff, who is the outgoing chair of the AAD teledermatology task force
Many dermatologists might find it difficult to opt out of telehealth. In some types of care, such as follow-up visits, a combination of patient demand and institutional policy, particularly if reimbursement is adequate, might compel or at least strongly incentivize teledermatology services.
“Now that telemedicine has gotten out there, we will never go back to what once was normal practice,” Dr. Lipoff predicted. According to Dr. Lipoff, there was a great deal of data even prior to the pandemic to conclude that mobile dermatology is “an acceptable equivalent” for delivering many types of dermatologic care.
The rapid evolution in telemedicine is remarkable. According to the results of the AAD survey, 14.1% of dermatologists had experience with teledermatology prior to the COVID-19 pandemic, which increased to 96.9% by June, 2020, when the survey was conducted. Nearly 600 dermatologists completed the survey, for a 13.6% response rate.
At the beginning of the pandemic, the CARES act, along with other pandemic legislation and policy changes, changed the landscape of telemedicine by providing reimbursement commensurate with in-office visits, modifying HIPAA regulations, and permitting reciprocal licensing to allow physicians to provide care to patients who had moved out of the state. While these were among the factors that facilitated the phenomenal growth in telemedicine, nearly all of these changes were temporary or are subject to revision.
“Reimbursement [for telehealth] was very low prior to the pandemic,” noted Elizabeth K. Jones, MD, assistant professor of dermatology, Thomas Jefferson University, Philadelphia. While many physicians and policy makers were convinced that reimbursement levels had to be increased temporarily to provide medical care when in-office visits were unsafe, Dr. Jones said it is unlikely that pandemic reimbursement rates will be preserved. But recent statements from the CMS foreshadow lower rates for most video and telephone consults, she added.
Reimbursement is not the only consideration. George Han, MD, PhD, chief of teledermatology at the Icahn School of Medicine at Mount Sinai, New York, spoke about the frustration of using imperfect tools. He, like many dermatologists, have become familiar with the difficulty of making a definitive diagnosis from transmitted images of skin lesions.
As long as patients communicate with personal computers and phones under variable lighting conditions, this problem might never go away, but suboptimal quality images do not necessarily preclude other types of consults, particularly follow-up visits, according to Dr. Han, who is also system medical director for dermatology at Mount Sinai Health System.
“Now that patients know about teledermatology, they are for it,” he said. He suggested that increased efficiency of follow-up using telemedicine for both patients and physicians might increase the frequency with which these types of visits are scheduled. Citing evidence that follow-up visits increase patient retention rates, Dr. Han sees these visits among the routine uses of telemedicine when the pandemic is over.
At the height of the pandemic, teledermatology was employed broadly, but after the pandemic, Dr. Han and others predict a narrower focus. Some consults, such as those for acne or other conditions reasonably treated on the basis of patient history, appear to lend themselves to telemedicine. Others, such as a skin check for malignancy, might not.
As the role of telemedicine is sorted out and finds its equilibrium in a postpandemic world, Dr. Lipoff pointed out the need to consider populations without good-quality internet access. Without specific strategies to ensure these patients are not forgotten, he warned of “wealthier patients consuming more than their fair share” of health care resources, further widening an existing disparity.
“Is telemedicine here to stay? It is clear that, yes, it is in some way,” said Dr. Lipoff, who sees no reason for dermatology to be an exception.
Dr. Lipoff reported a financial relationship with AcneAway. The other investigators reported no potential conflicts of interest related to telemedicine.
over those provided prior to the COVID-19 pandemic. But it is not clear whether the current rate will fall further, be sustained, or even climb again, according to data presented and opinions expressed in a forum on this topic at the American Academy of Dermatology Virtual Meeting Experience.
There are many unknowns, not least of which is future reimbursement from the Centers for Medicare & Medicaid Services and other third-party payers, according to several participants in a scientific session devoted to this topic. The CARES Act, which was passed in the early stages of the pandemic, provided only a temporary increase in reimbursement for telehealth. Postpandemic payments for telehealth services are yet undetermined.
Many of the assembled experts are convinced that teledermatology will continue to be offered at far higher rates than prior to the pandemic, but many issues, including physician acceptance of this approach remain unresolved. This was reflected in an AAD survey of members conducted in June 2020.
“Seventy percent of dermatologists responded that teledermatology will continue, but only 58% reported that they intend to offer it,” after the pandemic, reported Jules Lipoff, MD, assistant professor of dermatology at the University of Pennsylvania, Philadelphia, who is one of the authors of the paper that reported the results.
The low relative proportion of dermatologists planning to participate in teledermatology might at least in part reflect uncertainty about reimbursement, according to Dr. Lipoff, who is the outgoing chair of the AAD teledermatology task force
Many dermatologists might find it difficult to opt out of telehealth. In some types of care, such as follow-up visits, a combination of patient demand and institutional policy, particularly if reimbursement is adequate, might compel or at least strongly incentivize teledermatology services.
“Now that telemedicine has gotten out there, we will never go back to what once was normal practice,” Dr. Lipoff predicted. According to Dr. Lipoff, there was a great deal of data even prior to the pandemic to conclude that mobile dermatology is “an acceptable equivalent” for delivering many types of dermatologic care.
The rapid evolution in telemedicine is remarkable. According to the results of the AAD survey, 14.1% of dermatologists had experience with teledermatology prior to the COVID-19 pandemic, which increased to 96.9% by June, 2020, when the survey was conducted. Nearly 600 dermatologists completed the survey, for a 13.6% response rate.
At the beginning of the pandemic, the CARES act, along with other pandemic legislation and policy changes, changed the landscape of telemedicine by providing reimbursement commensurate with in-office visits, modifying HIPAA regulations, and permitting reciprocal licensing to allow physicians to provide care to patients who had moved out of the state. While these were among the factors that facilitated the phenomenal growth in telemedicine, nearly all of these changes were temporary or are subject to revision.
“Reimbursement [for telehealth] was very low prior to the pandemic,” noted Elizabeth K. Jones, MD, assistant professor of dermatology, Thomas Jefferson University, Philadelphia. While many physicians and policy makers were convinced that reimbursement levels had to be increased temporarily to provide medical care when in-office visits were unsafe, Dr. Jones said it is unlikely that pandemic reimbursement rates will be preserved. But recent statements from the CMS foreshadow lower rates for most video and telephone consults, she added.
Reimbursement is not the only consideration. George Han, MD, PhD, chief of teledermatology at the Icahn School of Medicine at Mount Sinai, New York, spoke about the frustration of using imperfect tools. He, like many dermatologists, have become familiar with the difficulty of making a definitive diagnosis from transmitted images of skin lesions.
As long as patients communicate with personal computers and phones under variable lighting conditions, this problem might never go away, but suboptimal quality images do not necessarily preclude other types of consults, particularly follow-up visits, according to Dr. Han, who is also system medical director for dermatology at Mount Sinai Health System.
“Now that patients know about teledermatology, they are for it,” he said. He suggested that increased efficiency of follow-up using telemedicine for both patients and physicians might increase the frequency with which these types of visits are scheduled. Citing evidence that follow-up visits increase patient retention rates, Dr. Han sees these visits among the routine uses of telemedicine when the pandemic is over.
At the height of the pandemic, teledermatology was employed broadly, but after the pandemic, Dr. Han and others predict a narrower focus. Some consults, such as those for acne or other conditions reasonably treated on the basis of patient history, appear to lend themselves to telemedicine. Others, such as a skin check for malignancy, might not.
As the role of telemedicine is sorted out and finds its equilibrium in a postpandemic world, Dr. Lipoff pointed out the need to consider populations without good-quality internet access. Without specific strategies to ensure these patients are not forgotten, he warned of “wealthier patients consuming more than their fair share” of health care resources, further widening an existing disparity.
“Is telemedicine here to stay? It is clear that, yes, it is in some way,” said Dr. Lipoff, who sees no reason for dermatology to be an exception.
Dr. Lipoff reported a financial relationship with AcneAway. The other investigators reported no potential conflicts of interest related to telemedicine.
over those provided prior to the COVID-19 pandemic. But it is not clear whether the current rate will fall further, be sustained, or even climb again, according to data presented and opinions expressed in a forum on this topic at the American Academy of Dermatology Virtual Meeting Experience.
There are many unknowns, not least of which is future reimbursement from the Centers for Medicare & Medicaid Services and other third-party payers, according to several participants in a scientific session devoted to this topic. The CARES Act, which was passed in the early stages of the pandemic, provided only a temporary increase in reimbursement for telehealth. Postpandemic payments for telehealth services are yet undetermined.
Many of the assembled experts are convinced that teledermatology will continue to be offered at far higher rates than prior to the pandemic, but many issues, including physician acceptance of this approach remain unresolved. This was reflected in an AAD survey of members conducted in June 2020.
“Seventy percent of dermatologists responded that teledermatology will continue, but only 58% reported that they intend to offer it,” after the pandemic, reported Jules Lipoff, MD, assistant professor of dermatology at the University of Pennsylvania, Philadelphia, who is one of the authors of the paper that reported the results.
The low relative proportion of dermatologists planning to participate in teledermatology might at least in part reflect uncertainty about reimbursement, according to Dr. Lipoff, who is the outgoing chair of the AAD teledermatology task force
Many dermatologists might find it difficult to opt out of telehealth. In some types of care, such as follow-up visits, a combination of patient demand and institutional policy, particularly if reimbursement is adequate, might compel or at least strongly incentivize teledermatology services.
“Now that telemedicine has gotten out there, we will never go back to what once was normal practice,” Dr. Lipoff predicted. According to Dr. Lipoff, there was a great deal of data even prior to the pandemic to conclude that mobile dermatology is “an acceptable equivalent” for delivering many types of dermatologic care.
The rapid evolution in telemedicine is remarkable. According to the results of the AAD survey, 14.1% of dermatologists had experience with teledermatology prior to the COVID-19 pandemic, which increased to 96.9% by June, 2020, when the survey was conducted. Nearly 600 dermatologists completed the survey, for a 13.6% response rate.
At the beginning of the pandemic, the CARES act, along with other pandemic legislation and policy changes, changed the landscape of telemedicine by providing reimbursement commensurate with in-office visits, modifying HIPAA regulations, and permitting reciprocal licensing to allow physicians to provide care to patients who had moved out of the state. While these were among the factors that facilitated the phenomenal growth in telemedicine, nearly all of these changes were temporary or are subject to revision.
“Reimbursement [for telehealth] was very low prior to the pandemic,” noted Elizabeth K. Jones, MD, assistant professor of dermatology, Thomas Jefferson University, Philadelphia. While many physicians and policy makers were convinced that reimbursement levels had to be increased temporarily to provide medical care when in-office visits were unsafe, Dr. Jones said it is unlikely that pandemic reimbursement rates will be preserved. But recent statements from the CMS foreshadow lower rates for most video and telephone consults, she added.
Reimbursement is not the only consideration. George Han, MD, PhD, chief of teledermatology at the Icahn School of Medicine at Mount Sinai, New York, spoke about the frustration of using imperfect tools. He, like many dermatologists, have become familiar with the difficulty of making a definitive diagnosis from transmitted images of skin lesions.
As long as patients communicate with personal computers and phones under variable lighting conditions, this problem might never go away, but suboptimal quality images do not necessarily preclude other types of consults, particularly follow-up visits, according to Dr. Han, who is also system medical director for dermatology at Mount Sinai Health System.
“Now that patients know about teledermatology, they are for it,” he said. He suggested that increased efficiency of follow-up using telemedicine for both patients and physicians might increase the frequency with which these types of visits are scheduled. Citing evidence that follow-up visits increase patient retention rates, Dr. Han sees these visits among the routine uses of telemedicine when the pandemic is over.
At the height of the pandemic, teledermatology was employed broadly, but after the pandemic, Dr. Han and others predict a narrower focus. Some consults, such as those for acne or other conditions reasonably treated on the basis of patient history, appear to lend themselves to telemedicine. Others, such as a skin check for malignancy, might not.
As the role of telemedicine is sorted out and finds its equilibrium in a postpandemic world, Dr. Lipoff pointed out the need to consider populations without good-quality internet access. Without specific strategies to ensure these patients are not forgotten, he warned of “wealthier patients consuming more than their fair share” of health care resources, further widening an existing disparity.
“Is telemedicine here to stay? It is clear that, yes, it is in some way,” said Dr. Lipoff, who sees no reason for dermatology to be an exception.
Dr. Lipoff reported a financial relationship with AcneAway. The other investigators reported no potential conflicts of interest related to telemedicine.
FROM AAD VMX 2021
Percentage of doctors who are Black barely changed in 120 years
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vaccinating homebound patients is an uphill battle

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
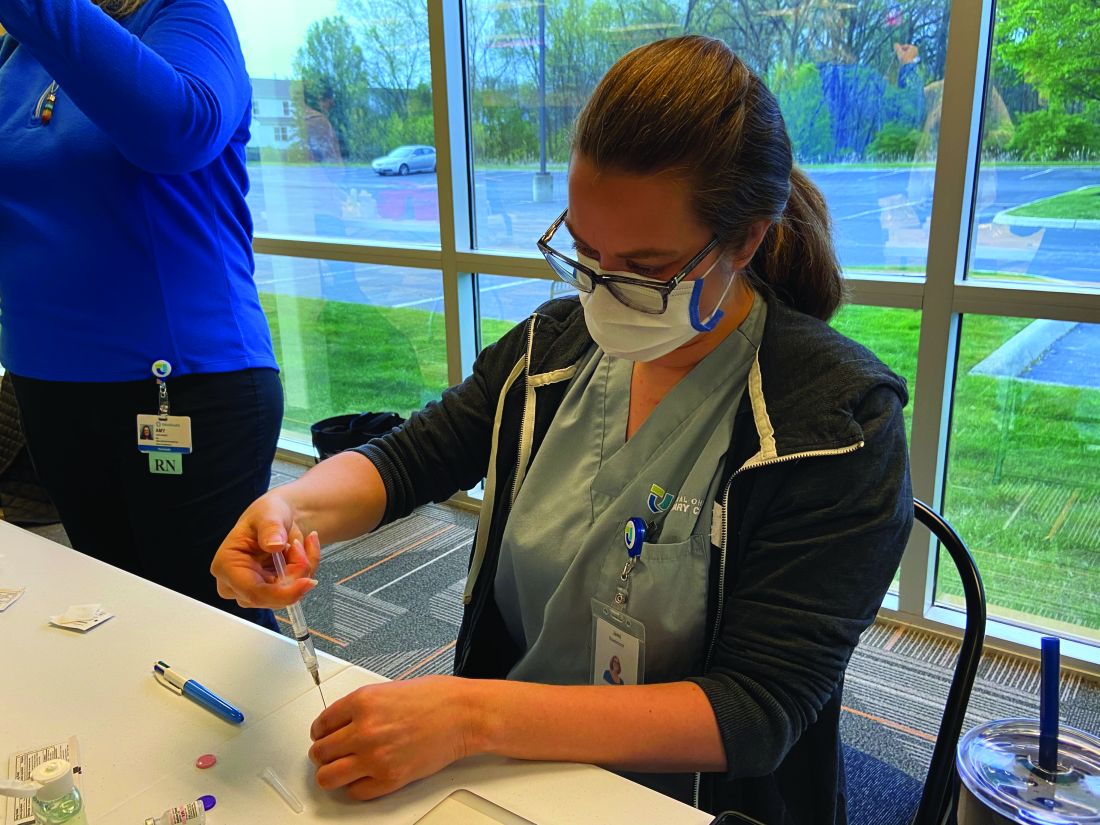
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
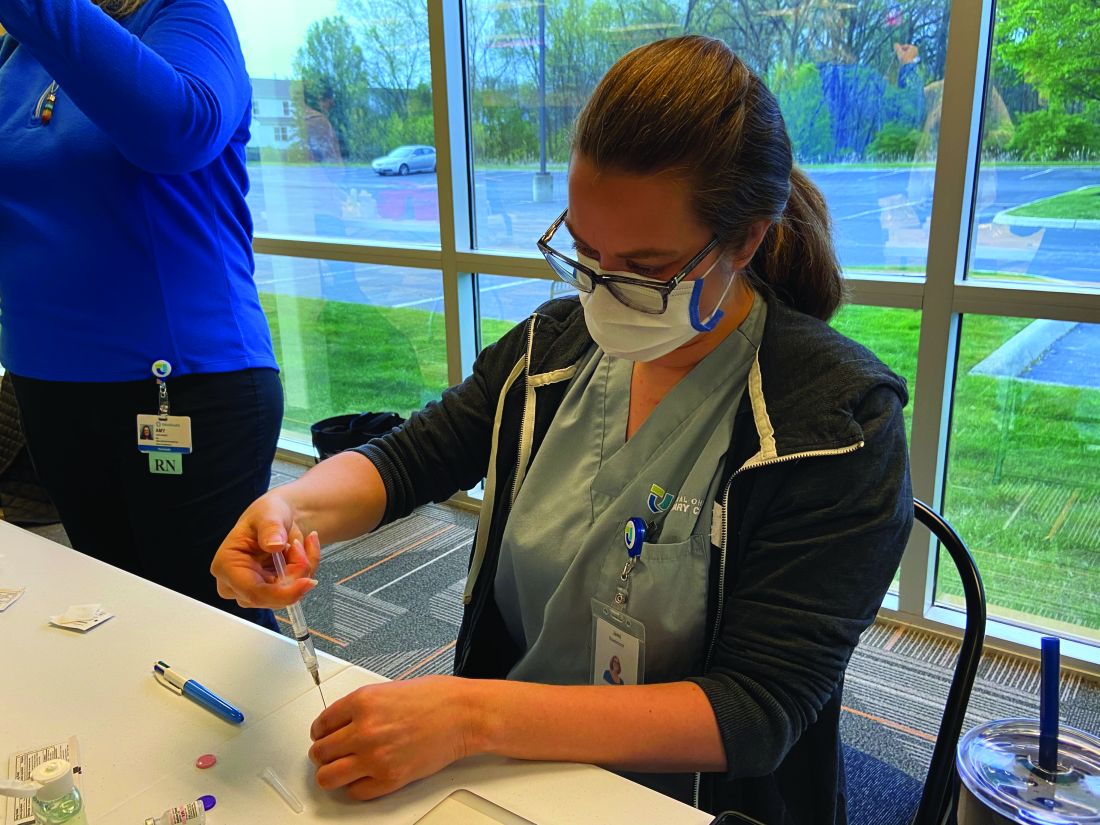
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
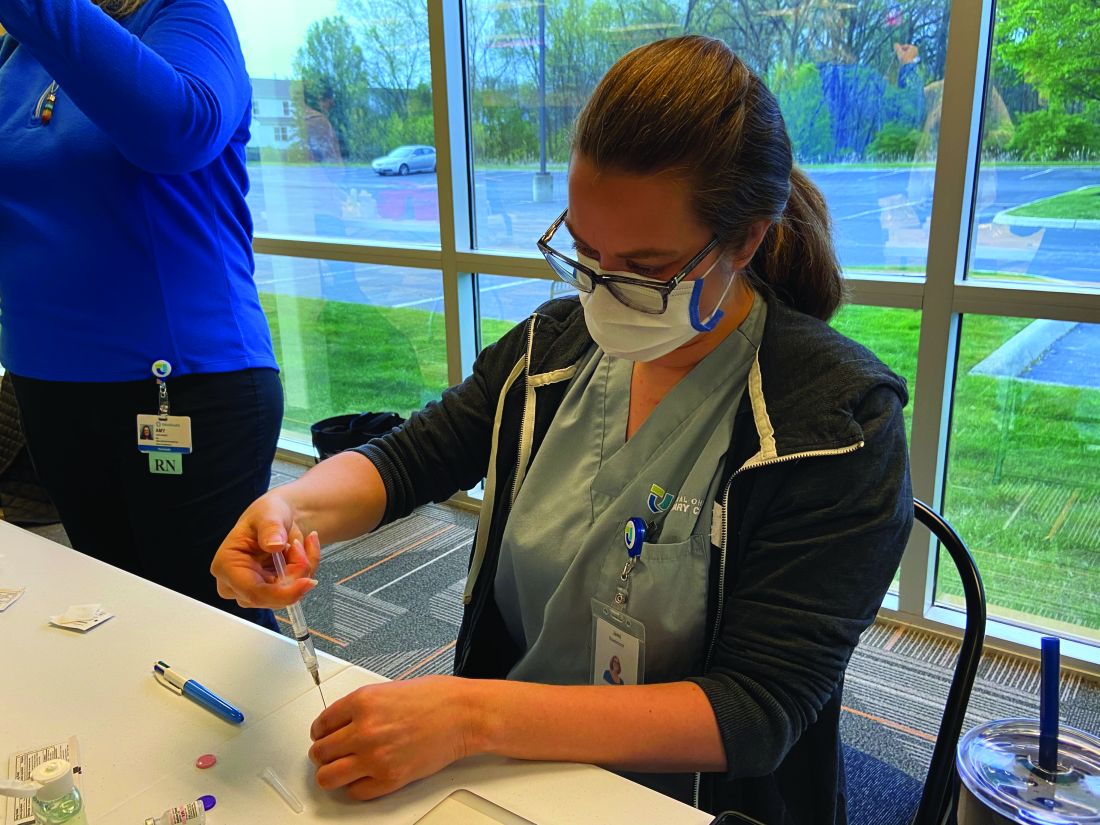
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.
Hispanic diabetes patients receive less guideline-based care
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
based on data from more than 7,000 individuals.
Racial and ethnic disparities in diabetes care remain a pervasive health problem, and minorities including non-Hispanic Blacks and Hispanics experience higher rates of complications, including retinopathy and neuropathy, compared with other groups, Felippe Ottoni Marcondes, MD, of Massachusetts General Hospital, Boston, and colleagues noted in a poster presented at the annual meeting of the Society for General Internal Medicine.
Data from previous studies have shown that diabetes patients who receive guideline-directed preventive care soon after diagnosis can reduce their risk of complications, they said.
To identify disparities in the provision of guideline-directed preventive care, the researchers analyzed data from 7,341 individuals who participated in the National Health Interview Survey from 2011 to 2017. They reviewed associations between race/ethnicity and visits to an eye specialist, a foot specialist, and checks of blood pressure and cholesterol in the past year among individuals diagnosed with diabetes within the past 5 years.
Overall, Hispanics had significantly lower rates of insurance coverage (75.9%), compared with non-Hispanic Whites (93.2%) and non-Hispanic Blacks (88.1%; P < .001).
Hispanics also were significantly less likely than Whites to have had a prior year eye exam (odds ratio, 0.80) and blood pressure check (OR, 0.45), after controlling for variables including age, sex, socioeconomic status, health insurance, general health status, U.S. region, marital status, body mass index, and various comorbidities.
Although insurance coverage mediated 42.8% of the total effect of race/ethnicity on annual eye specialist visits for Hispanics as compared with Whites, there was no significant effect for Blacks, compared with Whites.
COVID concerns impact diabetes disparities
“As the diabetes epidemic continues in the U.S., it is important to bring to the front of the diabetes care conversation racial/ethnic disparities that persisted or have been only partially addressed,” Dr. Marcondes said in an interview. “It is also important to emphasize that patients with diabetes are at higher risk for COVID-19 hospitalizations, complications, and death, and COVID-19 has disproportionately affected racial/ethnic minorities, so racial/ethnic minorities with diabetes have compounded risk of complications not only from diabetes but also from COVID-19.
“Importantly, our study highlights disparities in health care that are likely the product of systemic inequalities in access to care and insurance coverage at a moment when conversations about the race/racism and their health impact are fresh in the minds of public and health policy officials and the general public,” he emphasized.
“Unfortunately, I cannot say that I am surprised by our findings,” Dr. Marcondes said. “We expected to see some differences in the receipt of care for racial/ethnic minorities compared to white individuals for those recently diagnosed with diabetes, and that is exactly what our findings show.”
However, “what was perhaps intriguing is that disparities in the receipt of guideline-directed care were greater for Hispanic compared to White individuals than for Black compared to White individuals,” said Dr. Marcondes. “The causes of these differences are many. Hispanic individuals are less likely than White and Black persons to have insurance coverage.” Other unmeasured factors include language barriers that Hispanic individuals may face, as well as the bias and discrimination experienced by Hispanic and Black individuals alike.
Focus on equitable early intervention
“There is plenty of evidence in the medical literature that Black and Hispanic individuals with diabetes, as well as other minorities, have higher risk of complications of diabetes such as retinopathy, nephropathy, as well as cardiovascular risk factors such as high blood pressure and cholesterol,” Dr. Marcondes said. “Yet, complications in the time that immediately follows the diagnosis of diabetes are likely to be low.”
To reduce the risk of complications in the future, “physicians and health providers need to focus on providing equitable, guideline-directed treatment for their minority patients recently diagnosed with diabetes,” Dr. Marcondes emphasized. “Intervening early in the disease course will hopefully lead to a decrease in the rate of complications for racial/ethnic minorities. Clinicians, especially primary care physicians and providers, need to be aware that they are often the first encounter of many patients with the health care system. Effective communication and unbiased language on the part of clinicians will lead to stronger patient-physician relationships that foster opportunity to discuss disease prevention.
“Additional research is needed to evaluate the attitudes and biases of primary care providers and access the impact of patient navigation resources when treating minority patients with diabetes,” he concluded.
Digging Deeper into Disparities
“In diabetes, there are known racial and ethnic disparities such that minorities receive suboptimal screening and treatment, and have worse outcomes,” said Scott J. Pilla, MD, of The Johns Hopkins University School of Medicine, Baltimore, in an interview.
“This study examines disparities in diabetes preventive measures in the U.S. using a national survey (NHIS) over the past decade. They took the important step of stratifying their analyses by health insurance and socioeconomic status which, in addition to race, may have a large impact,” said Dr. Pilla. However, “One critique of the poster is that it is unclear whether the researchers weighted their analyses to account for the nationally representative sampling of the NHIS survey,” he noted.
Dr. Pilla said the finding that Hispanic patients had fewer diabetes preventive measures lines up with previous research in this area.
“I was surprised that the disparities did not extend to black patients, who have been found to also receive suboptimal care compared to white patients in other studies,” he noted.
The message for clinical practice: “Minorities with diabetes are at a higher risk of adverse diabetes outcomes and may need extra support and resources to achieve their evidence-based diabetes prevention,” Dr. Pilla said.
“More research is needed to understand the root cause of racial and ethnic disparities in diabetes management to tease apart possible contributors including health insurance coverage, socioeconomic factors, cultural and community factors, and systemic racism. This will help inform targeted approaches to reducing disparities in diabetes care,” he emphasized.
The researchers had no relevant financial conflicts to disclose. Dr. Pilla had no financial conflicts to disclose.
FROM SGIM 2021
Early pediatric rheumatology residency exposure key to solving workforce shortages
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
FROM CARRA 2021














