User login
The ripple effect
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Dr. G. Gayle Stephens was a teacher, progressive force, and ‘poet laureate of family medicine’
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
What COVID did to MD income in 2020
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
, according to the Medscape Physician Compensation Report 2021: The Recovery Begins.
Almost 18,000 physicians in more than 29 specialties told Medscape about their income, hours worked, greatest challenges, and the unexpected impact of COVID-19 on their compensation.
How many physicians avoided massive losses
When the pandemic started around March 2020, “a great many physicians saw reductions in volume at first,” says Robert Pearl, MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University.
Medscape’s survey report shows that a staggering 44% saw a 1%-25% reduction in patient volume, and 9% saw a 26%-50% decline. “That is indeed breathtaking,” Dr. Pearl says.
Several key factors saved many practices from hemorrhaging money, says Michael Belkin, JD, divisional vice president at Merritt Hawkins and Associates in Dallas. “Many physicians used the federal Paycheck Protection Program [PPP] to help keep themselves afloat,” he says. “A large percentage reduced their staff, which reduced their expenses, and many got some of their volume back by transitioning to telemedicine.”
In a 2020 survey for the Physicians Foundation, conducted by Merritt Hawkins, 48% of physicians said their practice had received PPP support, and most of those said the support was enough to allow them to stay open without reducing staff. Only 6% of practices that received PPP support did not stay open.
Telemedicine helped many practices
Early in the pandemic, Medicare reimbursements for telemedicine were equal with those for face-to-face visits. “Since telemedicine takes a third less time than an inpatient visit, doctors could see more patients,” Dr. Pearl says.
The switch was almost instantaneous in some practices. Within 3 days, a 200-provider multispecialty practice in Wilmington, N.C., went from not using telehealth to its being used by all physicians, the Medical Group Management Association reported. By late April, the practice was already back up to about 70% of normal overall production.
However, telemedicine could not help every specialty equally. “Generally, allergists can’t do their allergy testing virtually, and patients with mild problems probably put off visits,” Dr. Pearl says. Allergists experienced a large percentage decline in compensation, according to Medscape’s survey. For some, income fell from $301,000 the prior year to $274,000 this year.
Primary care struggled
Primary care physicians posted lower compensation than they did the prior year, but most rebounded to some degree. A study released in June 2020 projected that, even with telemedicine, primary care physicians would lose an average of $67,774 for the year.
However, Medscape’s survey found that internists’ average compensation declined from $251,000 in the prior year to $248,000, and average family physicians’ compensation actually rose from $234,000.
Pediatricians had a harder slog. Their average compensation sank from $232,000 to $221,000, according to the report. Even with telemedicine, parents of young children were not contacting the doctor. In May 2020, visits by children aged 3-5 years were down by 56%.
Many proceduralists recovered
Procedure-oriented specialties were particularly hard-hit at first, because many hospitals and some states banned all elective surgeries at the beginning of the pandemic.
“In March and April, ophthalmology practices were virtually at a standstill,” says John B. Pinto, an ophthalmology practice management consultant in San Diego. “But by the fourth quarter, operations were back to normal. Practices were fully open, and patients were coming back in.”
Medscape’s survey shows that, by year’s end, compensation was about the same as the year before for orthopedic surgeons ($511,000 in both the 2020 and 2021 reports); cardiologists actually did better ($438,000 in our 2020 report and $459,000 in 2021); and ophthalmologists’ compensation was about the same ($378,000 in our prior report and $379,000 in 2021).
Some other proceduralists, however, did not do as well. Otolaryngologists’ compensation fell to $417,000, the second-biggest percentage drop. “This may be because otolaryngologists’ chief procedures are tonsillectomies, sinus surgery, and nasal surgery, which can be put off,” Dr. Pearl says.
Anesthesiologists, who depend on surgical volume, also did not earn as much in 2020. Their compensation declined from $398,000 in our 2020 report to $378,000 in Medscape’s 2021 report.
“Not only has 70% of our revenue disappeared, but our physicians are still working every day,” an independent anesthesiology practice in Alabama told the MGMA early in the pandemic.
Plastic surgeons now the top earners
The biggest increase in compensation by far was made by plastic surgeons, whose income rose 9.8% over the year before, to $526,000. This put them at the top of the list
Dr. Pearl adds that plastic surgeons can perform their procedures in their offices, rather than in a hospital, where elective surgeries were often canceled.
Mr. Belkin says specialties other than plastic surgery had been offering more boutique cosmetic care even before the pandemic. In 2020, nonsurgical cosmetic procedures such as neurotoxin therapy, dermal filler procedures, chemical peels, and hair removal earned $3.1 billion in revenue, according to a survey by the Aesthetic Society.
Other specialties that earned more even during COVID
In Medscape’s survey, several specialties actually earned more during the pandemic than in 2019. Some specialties, such as critical care and public health, were integral in managing COVID patients and the pandemic.
However, some specialties involved in COVID care did not see an increase. Compensation for infectious disease specialists (at $245,000) and emergency medicine specialists (at $354,000) remained basically unchanged from the prior year, and for pulmonologists, it was slightly down.
Emergency departments reported decreases in volume of 40% or more early in the pandemic, according to the American College of Emergency Physicians. It was reported that patients were avoiding EDs for fear of contracting COVID, and car accidents were down because people ventured out less.
In this year’s report, psychiatrists saw a modest rise in compensation, to $275,000. “There has been an increase in mental health visits in the pandemic,” Dr. Pearl says. In 2020, about 4 in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from 1 in 10 adults the prior year. In addition, psychiatrists were third on the list of Merritt Hawkins’ most requested recruiting engagements.
Oncologists saw a rise in compensation, from $377,000 to $403,000. “Volume likely did not fall because cancer patients would go through with their chemotherapy in spite of the pandemic,” Dr. Pearl says. “The increase in income might have to do with the usual inflation in the cost of chemotherapy drugs.” Dr. Pinto saw the same trend for retinal surgeons, whose care also cannot be delayed.
Medscape’s survey also reports increases in compensation for rheumatologists, endocrinologists, and neurologists, but it reports small declines among dermatologists, radiologists, and gastroenterologists.
Gender-based pay gap remains in place
The gender-based pay gap in this year’s report is similar to that seen in Medscape’s report for the prior year. Men earned 27% more than women in 2021, compared with 25% more the year before. Some physicians commented that more women physicians maintained flexible or shorter work schedules to help with children who could not go into school.
“Having to be a full-time physician, full-time mom, and full-time teacher during our surge was unbelievable,” a primary care pediatrician in group practice and mother of two reported in November. “I felt pulled in all directions and didn’t do anything well.”
In addition, “men dominate some specialties that seem to have seen a smaller drop in volume in the pandemic, such as emergency medicine, infectious disease, pulmonology, and oncology,” says Halee Fischer-Wright, MD, CEO of MGMA.
Employed physicians shared their employers’ pain
Employed physicians, who typically work at hospitals, shared the financial pains of their institutions, particularly in the early stages of the pandemic. In April, hospital admissions were 34.1% below prepandemic levels, according to a study published in Health Affairs. That figure had risen by June, but it was still 8.3% below prepandemic volume.
By the end of the year, many hospitals and hospital systems were in the black, thanks in large part to generous federal subsidies, but actual operations still lost money for the year. Altogether, 42% of them posted an operational loss in 2020, up from the 23% in 2019, according to a survey by Moody’s Investors Service.
Medscape’s report shows that many employed physicians lost pay in 2020, and for many, pay had not returned to pre-COVID levels. Only 28% of primary care physicians and 32% of specialists who lost pay have seen it restored, according to the report. In addition, 15% of surveyed physicians did not receive an annual raise.
Many employed doctors are paid on the basis of relative value units (RVUs), which is a measure of the value of their work. In many cases, there was not enough work to reach RVU thresholds. Would hospitals and other employers lower RVU targets to meet the problem? “I haven’t seen our clients make concessions to providers along those lines,” Mr. Belkin says.
Physicians had to work longer hours
The Medscape report also found that in 2020, physicians saw fewer patients because each visit took longer.
“With the threat of COVID, in-person visits take more time than before,” Mr. Belkin says. “Physicians and staff have to prepare the exam room after each visit, and doctors must spend more time answering patients’ questions about COVID.”
“The new protocols to keep everyone safe add time between patients, and physicians have to answer patients’ questions about the pandemic and vaccines,” Dr. Fischer-Wright says. “You might see a 20% increase in time spent just on these non–revenue-generating COVID activities.”
Physicians still like their specialty
Although 2020 was a challenging year for physicians, the percentage of those who were satisfied with their specialty choice generally did not slip from the year before. It actually rose for several specialties – most notably, rheumatology, pulmonology, physical medicine and rehabilitation, and nephrology.
One specialty saw a decline in satisfaction with their specialty choice, and that was public health and preventive medicine, which plummeted 16 percentage points to 67% – putting it at the bottom of the list.
Even before the pandemic, many public health departments were chronically underfunded. This problem was possibly exacerbated by the pressures to keep up with COVID reporting and testing responsibilities.
Conclusion
Although 2020 was a wild ride for many physicians, many came out of it with only minor reductions in overall compensation, and some saw increases. Still, some specialties and many individuals experienced terrible financial stress and had to make changes in their lives and their spending in order to stay afloat.
“The biggest inhibitor to getting back to normal had to do with doctors who did not want to return because they did not want to risk getting COVID,” Dr. Pinto reports. But he notes that by February 2021 most doctors were completely vaccinated and could feel safe again.
A version of this article first appeared on Medscape.com.
Open Notes
. While some clinicians consider it an unwelcome intrusion, advocates say it will improve communication and compliance.
Patient access to notes is not new. In many states, patients already have the ability to request copies of their charts, or to access truncated information via clinic websites. The difference is that most patients will now be able to click on a patient portal – such as MyChart, or other similar apps – and gain instantaneous, unfettered access to everything in their records.
Clinicians have traditionally thought of medical notes as private journal entries; but in the last few decades they have become an important component of the documentation necessary for billing, as well as evidence in the event of litigation. Now, with the implementation of the Cures Act, medical notes have evolved into a tool to communicate with the patient, rather than just among health care providers, lawyers, and billing departments.
Supporters contend that this change will make a big difference, because patients will be able to see exactly what their doctors have written, rather than just a list of confusing test results and diagnosis lists in “medicalese.”
OpenNotes, a think tank that has promoted the sharing of clinical notes with patients for years, calls the Cures Act legislation a “new world” where shared notes are valuable tools to improve communication between patients and physicians while strengthening their relationship. They cite evidence indicating that “when health professionals offer patients and families ready access to clinical notes, the quality and safety of care improves.”
Not all doctors are as enthusiastic. Many are concerned that patients might misinterpret what they see in their doctors’ notes, including complex descriptions of clinical assessments and decisions.
Others worry about patients having immediate access to their records, perhaps even before their physicians. The American Academy of Dermatology is working with the American Medical Association and other groups to gather real-world instances where the release of lab results, reports, or notes directly to patients before their physician could review the information with them caused emotional harm or other adverse consequences.
Undoubtedly, there are scenarios where unrestricted display of clinical notes could be problematic. One example is the issue of adolescents and reproductive health. Since parents now have access to their children’s records, some teenagers might hesitate to confide in their physicians and deny themselves important medical care.
The new rules permit blocking access to records if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or third parties. Psychotherapy counseling notes, for example, are completely exempt from the new requirements.
There are also state-level laws that can supersede the new federal law and block access to notes. For example, California law forbids providers from posting cancer test results without discussing them with the patient first.
Research indicates that shared notes have benefits that should outweigh the concerns of most physicians. One study showed that about 70% of patients said reviewing their notes helped them understand why medications were prescribed, which improved their compliance. This was particularly true for patients whose primary language is not English. A British study found that patients felt empowered by shared notes, and thought they improved their relationship with their physicians.
Other advantages of sharing notes include the ability of family members to review what happened at visits, which can be particularly important when dementia or other disabilities are involved. Patients will also be able to share their medical records with physicians outside of their health network, thus avoiding unnecessary or repetitious workups.
OpenNotes contends that when patients review their doctors’ notes, they gain “a newfound, deeper respect for what physicians have to understand to do their jobs.” Other predicted advantages include improved medical record accuracy and less miscommunication. In a study published in 2019 that evaluated experiences of patients who read ambulatory visit notes, only 5% were more worried after reading the notes and 3% were confused.
Alleviating worry among clinicians may be a bigger problem; but as a general principle, you should avoid judgmental language, and never write anything in a chart that you wouldn’t want your patients or their family members – or lawyers – to see.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. While some clinicians consider it an unwelcome intrusion, advocates say it will improve communication and compliance.
Patient access to notes is not new. In many states, patients already have the ability to request copies of their charts, or to access truncated information via clinic websites. The difference is that most patients will now be able to click on a patient portal – such as MyChart, or other similar apps – and gain instantaneous, unfettered access to everything in their records.
Clinicians have traditionally thought of medical notes as private journal entries; but in the last few decades they have become an important component of the documentation necessary for billing, as well as evidence in the event of litigation. Now, with the implementation of the Cures Act, medical notes have evolved into a tool to communicate with the patient, rather than just among health care providers, lawyers, and billing departments.
Supporters contend that this change will make a big difference, because patients will be able to see exactly what their doctors have written, rather than just a list of confusing test results and diagnosis lists in “medicalese.”
OpenNotes, a think tank that has promoted the sharing of clinical notes with patients for years, calls the Cures Act legislation a “new world” where shared notes are valuable tools to improve communication between patients and physicians while strengthening their relationship. They cite evidence indicating that “when health professionals offer patients and families ready access to clinical notes, the quality and safety of care improves.”
Not all doctors are as enthusiastic. Many are concerned that patients might misinterpret what they see in their doctors’ notes, including complex descriptions of clinical assessments and decisions.
Others worry about patients having immediate access to their records, perhaps even before their physicians. The American Academy of Dermatology is working with the American Medical Association and other groups to gather real-world instances where the release of lab results, reports, or notes directly to patients before their physician could review the information with them caused emotional harm or other adverse consequences.
Undoubtedly, there are scenarios where unrestricted display of clinical notes could be problematic. One example is the issue of adolescents and reproductive health. Since parents now have access to their children’s records, some teenagers might hesitate to confide in their physicians and deny themselves important medical care.
The new rules permit blocking access to records if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or third parties. Psychotherapy counseling notes, for example, are completely exempt from the new requirements.
There are also state-level laws that can supersede the new federal law and block access to notes. For example, California law forbids providers from posting cancer test results without discussing them with the patient first.
Research indicates that shared notes have benefits that should outweigh the concerns of most physicians. One study showed that about 70% of patients said reviewing their notes helped them understand why medications were prescribed, which improved their compliance. This was particularly true for patients whose primary language is not English. A British study found that patients felt empowered by shared notes, and thought they improved their relationship with their physicians.
Other advantages of sharing notes include the ability of family members to review what happened at visits, which can be particularly important when dementia or other disabilities are involved. Patients will also be able to share their medical records with physicians outside of their health network, thus avoiding unnecessary or repetitious workups.
OpenNotes contends that when patients review their doctors’ notes, they gain “a newfound, deeper respect for what physicians have to understand to do their jobs.” Other predicted advantages include improved medical record accuracy and less miscommunication. In a study published in 2019 that evaluated experiences of patients who read ambulatory visit notes, only 5% were more worried after reading the notes and 3% were confused.
Alleviating worry among clinicians may be a bigger problem; but as a general principle, you should avoid judgmental language, and never write anything in a chart that you wouldn’t want your patients or their family members – or lawyers – to see.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. While some clinicians consider it an unwelcome intrusion, advocates say it will improve communication and compliance.
Patient access to notes is not new. In many states, patients already have the ability to request copies of their charts, or to access truncated information via clinic websites. The difference is that most patients will now be able to click on a patient portal – such as MyChart, or other similar apps – and gain instantaneous, unfettered access to everything in their records.
Clinicians have traditionally thought of medical notes as private journal entries; but in the last few decades they have become an important component of the documentation necessary for billing, as well as evidence in the event of litigation. Now, with the implementation of the Cures Act, medical notes have evolved into a tool to communicate with the patient, rather than just among health care providers, lawyers, and billing departments.
Supporters contend that this change will make a big difference, because patients will be able to see exactly what their doctors have written, rather than just a list of confusing test results and diagnosis lists in “medicalese.”
OpenNotes, a think tank that has promoted the sharing of clinical notes with patients for years, calls the Cures Act legislation a “new world” where shared notes are valuable tools to improve communication between patients and physicians while strengthening their relationship. They cite evidence indicating that “when health professionals offer patients and families ready access to clinical notes, the quality and safety of care improves.”
Not all doctors are as enthusiastic. Many are concerned that patients might misinterpret what they see in their doctors’ notes, including complex descriptions of clinical assessments and decisions.
Others worry about patients having immediate access to their records, perhaps even before their physicians. The American Academy of Dermatology is working with the American Medical Association and other groups to gather real-world instances where the release of lab results, reports, or notes directly to patients before their physician could review the information with them caused emotional harm or other adverse consequences.
Undoubtedly, there are scenarios where unrestricted display of clinical notes could be problematic. One example is the issue of adolescents and reproductive health. Since parents now have access to their children’s records, some teenagers might hesitate to confide in their physicians and deny themselves important medical care.
The new rules permit blocking access to records if there is clear evidence that doing so “will substantially reduce the risk of harm” to patients or third parties. Psychotherapy counseling notes, for example, are completely exempt from the new requirements.
There are also state-level laws that can supersede the new federal law and block access to notes. For example, California law forbids providers from posting cancer test results without discussing them with the patient first.
Research indicates that shared notes have benefits that should outweigh the concerns of most physicians. One study showed that about 70% of patients said reviewing their notes helped them understand why medications were prescribed, which improved their compliance. This was particularly true for patients whose primary language is not English. A British study found that patients felt empowered by shared notes, and thought they improved their relationship with their physicians.
Other advantages of sharing notes include the ability of family members to review what happened at visits, which can be particularly important when dementia or other disabilities are involved. Patients will also be able to share their medical records with physicians outside of their health network, thus avoiding unnecessary or repetitious workups.
OpenNotes contends that when patients review their doctors’ notes, they gain “a newfound, deeper respect for what physicians have to understand to do their jobs.” Other predicted advantages include improved medical record accuracy and less miscommunication. In a study published in 2019 that evaluated experiences of patients who read ambulatory visit notes, only 5% were more worried after reading the notes and 3% were confused.
Alleviating worry among clinicians may be a bigger problem; but as a general principle, you should avoid judgmental language, and never write anything in a chart that you wouldn’t want your patients or their family members – or lawyers – to see.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Say my name
Dr. Ben-a-bo?
Nope.
Ben-nabi?
Nope.
Ben-NO-bo?
Also no.
My surname is tricky to pronounce for some people. I sometimes exaggerate to help patients get it right: “Beh-NAAH-bee-oh.” Almost daily someone will reply: “Oh, you’re Italian!” Well, no actually, my friend Enzo who was born in Sicily and lives in Milan, he’s Italian. I’m just a Rhode Islander who knows some Italian words from his grandmother. Most times though, I just answer: ‘Yep, I’m Italian.” It’s faster.
We use names as a shortcut to identify people. In clinic, it can help to find things in common quickly, similar to asking where you’re from. (East Coast patients seem to love that I’m from New England and if they’re Italian and from New York, well then, we’re paisans right from the start.)
However, using names to guess how someone identifies can be risky. In some instances, it could even be seen as microaggressive, particularly if you got it wrong.
Like most of you I’ll bet, I’m pretty good at pronouncing names – we practice thousands of times! Other than accepting a compliment for getting a tricky one right, such as Radivojevic (I think it’s Ra-di-VOI-ye-vich), I hadn’t thought much about names until I heard a great podcast on the topic. I thought I’d share a couple tips.
First, if you’re not particularly good at names or if you struggle with certain types of names, it’s better to ask than to butcher it. Like learning the wrong way to hit a golf ball, you may never be able to do it properly once you’ve done it wrong. (Trust me, I know from both.)
If I’m feeling confident, I’ll give it a try. But if unsure, I ask the patient to pronounce it for me, then I repeat it to confirm I’ve gotten it correct. Then I say it once or twice more during the visit. Lastly, for the knotty tongue-twisting ones, I write it phonetically in their chart.
It is important because mispronouncing names can alienate patients. It might make them feel like we don’t “know” them or that we don’t care about them. and eliminating ethnic disparities in care. Just think how much harder it might be to convince skeptical patients to take their lisinopril if you can’t even get their names right.
Worse perhaps than getting the pronunciation wrong is to turn the name into an issue. Saying: “Oh, that’s hard to pronounce” could be felt as a subtly racist remark – it’s not hard for them to pronounce of course, only for you. Also, guessing a patient’s nationality from the name is risky. Asking “are you Russian?” to someone from Ukraine or “is that Chinese?” to someone from Vietnam can quickly turn a nice office visit down a road named “Awkward.” It can give the impression that they “all look the same” to you, exactly the type of exclusion we’re trying to eliminate in medicine.
Saying a patient’s name perfectly is rewarding and a super-efficient way to connect. It can make salient the truth that you care about the patient and about his or her story, even if the name happens to be Mrs. Xiomara Winyuwongse Khosrowshahi Sundararajan Ngoc. Go ahead, give it a try.
Want more on how properly pronounce names correctly? You might like this episode of NPR’s Life Kit.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Dr. Ben-a-bo?
Nope.
Ben-nabi?
Nope.
Ben-NO-bo?
Also no.
My surname is tricky to pronounce for some people. I sometimes exaggerate to help patients get it right: “Beh-NAAH-bee-oh.” Almost daily someone will reply: “Oh, you’re Italian!” Well, no actually, my friend Enzo who was born in Sicily and lives in Milan, he’s Italian. I’m just a Rhode Islander who knows some Italian words from his grandmother. Most times though, I just answer: ‘Yep, I’m Italian.” It’s faster.
We use names as a shortcut to identify people. In clinic, it can help to find things in common quickly, similar to asking where you’re from. (East Coast patients seem to love that I’m from New England and if they’re Italian and from New York, well then, we’re paisans right from the start.)
However, using names to guess how someone identifies can be risky. In some instances, it could even be seen as microaggressive, particularly if you got it wrong.
Like most of you I’ll bet, I’m pretty good at pronouncing names – we practice thousands of times! Other than accepting a compliment for getting a tricky one right, such as Radivojevic (I think it’s Ra-di-VOI-ye-vich), I hadn’t thought much about names until I heard a great podcast on the topic. I thought I’d share a couple tips.
First, if you’re not particularly good at names or if you struggle with certain types of names, it’s better to ask than to butcher it. Like learning the wrong way to hit a golf ball, you may never be able to do it properly once you’ve done it wrong. (Trust me, I know from both.)
If I’m feeling confident, I’ll give it a try. But if unsure, I ask the patient to pronounce it for me, then I repeat it to confirm I’ve gotten it correct. Then I say it once or twice more during the visit. Lastly, for the knotty tongue-twisting ones, I write it phonetically in their chart.
It is important because mispronouncing names can alienate patients. It might make them feel like we don’t “know” them or that we don’t care about them. and eliminating ethnic disparities in care. Just think how much harder it might be to convince skeptical patients to take their lisinopril if you can’t even get their names right.
Worse perhaps than getting the pronunciation wrong is to turn the name into an issue. Saying: “Oh, that’s hard to pronounce” could be felt as a subtly racist remark – it’s not hard for them to pronounce of course, only for you. Also, guessing a patient’s nationality from the name is risky. Asking “are you Russian?” to someone from Ukraine or “is that Chinese?” to someone from Vietnam can quickly turn a nice office visit down a road named “Awkward.” It can give the impression that they “all look the same” to you, exactly the type of exclusion we’re trying to eliminate in medicine.
Saying a patient’s name perfectly is rewarding and a super-efficient way to connect. It can make salient the truth that you care about the patient and about his or her story, even if the name happens to be Mrs. Xiomara Winyuwongse Khosrowshahi Sundararajan Ngoc. Go ahead, give it a try.
Want more on how properly pronounce names correctly? You might like this episode of NPR’s Life Kit.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Dr. Ben-a-bo?
Nope.
Ben-nabi?
Nope.
Ben-NO-bo?
Also no.
My surname is tricky to pronounce for some people. I sometimes exaggerate to help patients get it right: “Beh-NAAH-bee-oh.” Almost daily someone will reply: “Oh, you’re Italian!” Well, no actually, my friend Enzo who was born in Sicily and lives in Milan, he’s Italian. I’m just a Rhode Islander who knows some Italian words from his grandmother. Most times though, I just answer: ‘Yep, I’m Italian.” It’s faster.
We use names as a shortcut to identify people. In clinic, it can help to find things in common quickly, similar to asking where you’re from. (East Coast patients seem to love that I’m from New England and if they’re Italian and from New York, well then, we’re paisans right from the start.)
However, using names to guess how someone identifies can be risky. In some instances, it could even be seen as microaggressive, particularly if you got it wrong.
Like most of you I’ll bet, I’m pretty good at pronouncing names – we practice thousands of times! Other than accepting a compliment for getting a tricky one right, such as Radivojevic (I think it’s Ra-di-VOI-ye-vich), I hadn’t thought much about names until I heard a great podcast on the topic. I thought I’d share a couple tips.
First, if you’re not particularly good at names or if you struggle with certain types of names, it’s better to ask than to butcher it. Like learning the wrong way to hit a golf ball, you may never be able to do it properly once you’ve done it wrong. (Trust me, I know from both.)
If I’m feeling confident, I’ll give it a try. But if unsure, I ask the patient to pronounce it for me, then I repeat it to confirm I’ve gotten it correct. Then I say it once or twice more during the visit. Lastly, for the knotty tongue-twisting ones, I write it phonetically in their chart.
It is important because mispronouncing names can alienate patients. It might make them feel like we don’t “know” them or that we don’t care about them. and eliminating ethnic disparities in care. Just think how much harder it might be to convince skeptical patients to take their lisinopril if you can’t even get their names right.
Worse perhaps than getting the pronunciation wrong is to turn the name into an issue. Saying: “Oh, that’s hard to pronounce” could be felt as a subtly racist remark – it’s not hard for them to pronounce of course, only for you. Also, guessing a patient’s nationality from the name is risky. Asking “are you Russian?” to someone from Ukraine or “is that Chinese?” to someone from Vietnam can quickly turn a nice office visit down a road named “Awkward.” It can give the impression that they “all look the same” to you, exactly the type of exclusion we’re trying to eliminate in medicine.
Saying a patient’s name perfectly is rewarding and a super-efficient way to connect. It can make salient the truth that you care about the patient and about his or her story, even if the name happens to be Mrs. Xiomara Winyuwongse Khosrowshahi Sundararajan Ngoc. Go ahead, give it a try.
Want more on how properly pronounce names correctly? You might like this episode of NPR’s Life Kit.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Female rheumatologists see fewer patients, earn less than males
A new study on the changing rheumatology workforce found that, although there has been a notable rise in female rheumatologists, they see fewer patients and have lower earnings than their male counterparts.
“In order for future health workforce policy and planning to be effective and equitable, it is essential to consider policies and other solutions to support the sustainability of rheumatology workforces in light of increasing feminization,” wrote Jessica Widdifield, PhD, of the Sunnybrook Research Institute in Toronto and her colleagues. The study was published in the Journal of Rheumatology.
To investigate potential workload and earnings disparities between male and female rheumatologists, the researchers launched a population-based study of rheumatologists practicing in Ontario, Canada, and their patient visits between April 1, 2000, and March 31, 2015. To quantify clinical activity, they calculated full-time equivalents (FTEs) using annual fee-for-service billing claims and defined rheumatologists practicing at least one clinical FTE as those at or above the 40th percentile of total billings each year. Any rheumatologists practicing less than one FTE were not included in the larger analysis.
Overall, they found that the total number of rheumatologists increased from 146 in 2000 to 194 in 2015, with 49% of the latter workforce being women. When assessing only rheumatologists practicing at greater than one FTE, the number increased from 89 in 2000 to 120 in 2015, with women making up 41.7% of the 2015 workforce. Although practice sizes decreased for both genders over the course of the study, in 2015 the median practice size was 1,948.5 patients (interquartile range, 1,433-2,562) for men, compared with 1,468.5 patients (IQR, 1,212-1,984) for women. In every year but 2001, men had larger median practice sizes than women.
Total patient visits remained relatively stable for men throughout the study period but declined for women, with the gap between genders widening over time. The peak gap in visits was 1,486 (95% confidence interval, 628-2,517) in 2008. And while median payments increased over time for all rheumatologists, median renumeration peaked in 2015 at $362,522 (IQR, $309,503-$437,127) for women, compared with $403,903 (IQR, $313,297-$544,703) for men. That said, the median difference that year – $45,556.10 (95% confidence interval, $951.60-$92,470.40; P = .04) – was the smallest for any in the study period. The largest difference was $102,176.10 (95% CI, $58,457.50-$152,821.20; P < .0001) in 2011.
An opportunity for female rheumatologists to reshape the specialty
Of course, gender gaps like these are not limited to rheumatology or even medicine, wrote Grace C. Wright, MD, PhD, president of the Association of Women in Rheumatology, in an accompanying editorial. “This issue exists across industries as well as across boundaries.”
“Particularly for women physicians, we do have additional demands on our time,” agreed April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, in an interview. “For example, we know that women who work often have additional caregiving responsibilities at home, for kids and/or elderly relatives. I do think those are real reasons why certain providers, particularly women, might have a lower clinical volume.”
Despite the significant gender gaps that still exist, Dr. Jorge – who authored a previous study on the gaps in academic rheumatology – was heartened by the data that indicated more women finding their way into the specialty.
“I think it’s good news for rheumatology to be so balanced between men and women as providers,” she said. “For young women trainees, it’s really important to see role models in their field. For patients, it’s incredibly important for them to have a doctor who can relate and who can advocate for them. So many rheumatic conditions that we treat disproportionately affect women, often women of childbearing age. So it’s really important to have women involved in leading the specialty of rheumatology, including clinical practice but also research, education, and policy.”
Dr. Wright concurred in her editorial, stating that “this feminization of rheumatology provides an opportunity to assess the needs of working women, the generational shifts in attitudes toward work-life balance, and a change in clinical practice toward value over volume.”
The study’s authors shared its possible limitations, including the lack of a standard definition of a clinical FTE rheumatologist – thus their decision to define one – and a lack of context as to why certain rheumatologists were practicing less than others. In addition, they preemptively acknowledged Dr. Jorge’s concern by noting their inability to access gender-related details like marital status, family size, and childcare roles, all of which “could contribute to the relationship between physician gender and practice-level activity.”
The study was funded by an operating grant from the Canadian Initiative for Outcomes in Rheumatology Care and supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Two of the authors reported receiving support from the Arthritis Society Stars Career Development Award.
A new study on the changing rheumatology workforce found that, although there has been a notable rise in female rheumatologists, they see fewer patients and have lower earnings than their male counterparts.
“In order for future health workforce policy and planning to be effective and equitable, it is essential to consider policies and other solutions to support the sustainability of rheumatology workforces in light of increasing feminization,” wrote Jessica Widdifield, PhD, of the Sunnybrook Research Institute in Toronto and her colleagues. The study was published in the Journal of Rheumatology.
To investigate potential workload and earnings disparities between male and female rheumatologists, the researchers launched a population-based study of rheumatologists practicing in Ontario, Canada, and their patient visits between April 1, 2000, and March 31, 2015. To quantify clinical activity, they calculated full-time equivalents (FTEs) using annual fee-for-service billing claims and defined rheumatologists practicing at least one clinical FTE as those at or above the 40th percentile of total billings each year. Any rheumatologists practicing less than one FTE were not included in the larger analysis.
Overall, they found that the total number of rheumatologists increased from 146 in 2000 to 194 in 2015, with 49% of the latter workforce being women. When assessing only rheumatologists practicing at greater than one FTE, the number increased from 89 in 2000 to 120 in 2015, with women making up 41.7% of the 2015 workforce. Although practice sizes decreased for both genders over the course of the study, in 2015 the median practice size was 1,948.5 patients (interquartile range, 1,433-2,562) for men, compared with 1,468.5 patients (IQR, 1,212-1,984) for women. In every year but 2001, men had larger median practice sizes than women.
Total patient visits remained relatively stable for men throughout the study period but declined for women, with the gap between genders widening over time. The peak gap in visits was 1,486 (95% confidence interval, 628-2,517) in 2008. And while median payments increased over time for all rheumatologists, median renumeration peaked in 2015 at $362,522 (IQR, $309,503-$437,127) for women, compared with $403,903 (IQR, $313,297-$544,703) for men. That said, the median difference that year – $45,556.10 (95% confidence interval, $951.60-$92,470.40; P = .04) – was the smallest for any in the study period. The largest difference was $102,176.10 (95% CI, $58,457.50-$152,821.20; P < .0001) in 2011.
An opportunity for female rheumatologists to reshape the specialty
Of course, gender gaps like these are not limited to rheumatology or even medicine, wrote Grace C. Wright, MD, PhD, president of the Association of Women in Rheumatology, in an accompanying editorial. “This issue exists across industries as well as across boundaries.”
“Particularly for women physicians, we do have additional demands on our time,” agreed April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, in an interview. “For example, we know that women who work often have additional caregiving responsibilities at home, for kids and/or elderly relatives. I do think those are real reasons why certain providers, particularly women, might have a lower clinical volume.”
Despite the significant gender gaps that still exist, Dr. Jorge – who authored a previous study on the gaps in academic rheumatology – was heartened by the data that indicated more women finding their way into the specialty.
“I think it’s good news for rheumatology to be so balanced between men and women as providers,” she said. “For young women trainees, it’s really important to see role models in their field. For patients, it’s incredibly important for them to have a doctor who can relate and who can advocate for them. So many rheumatic conditions that we treat disproportionately affect women, often women of childbearing age. So it’s really important to have women involved in leading the specialty of rheumatology, including clinical practice but also research, education, and policy.”
Dr. Wright concurred in her editorial, stating that “this feminization of rheumatology provides an opportunity to assess the needs of working women, the generational shifts in attitudes toward work-life balance, and a change in clinical practice toward value over volume.”
The study’s authors shared its possible limitations, including the lack of a standard definition of a clinical FTE rheumatologist – thus their decision to define one – and a lack of context as to why certain rheumatologists were practicing less than others. In addition, they preemptively acknowledged Dr. Jorge’s concern by noting their inability to access gender-related details like marital status, family size, and childcare roles, all of which “could contribute to the relationship between physician gender and practice-level activity.”
The study was funded by an operating grant from the Canadian Initiative for Outcomes in Rheumatology Care and supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Two of the authors reported receiving support from the Arthritis Society Stars Career Development Award.
A new study on the changing rheumatology workforce found that, although there has been a notable rise in female rheumatologists, they see fewer patients and have lower earnings than their male counterparts.
“In order for future health workforce policy and planning to be effective and equitable, it is essential to consider policies and other solutions to support the sustainability of rheumatology workforces in light of increasing feminization,” wrote Jessica Widdifield, PhD, of the Sunnybrook Research Institute in Toronto and her colleagues. The study was published in the Journal of Rheumatology.
To investigate potential workload and earnings disparities between male and female rheumatologists, the researchers launched a population-based study of rheumatologists practicing in Ontario, Canada, and their patient visits between April 1, 2000, and March 31, 2015. To quantify clinical activity, they calculated full-time equivalents (FTEs) using annual fee-for-service billing claims and defined rheumatologists practicing at least one clinical FTE as those at or above the 40th percentile of total billings each year. Any rheumatologists practicing less than one FTE were not included in the larger analysis.
Overall, they found that the total number of rheumatologists increased from 146 in 2000 to 194 in 2015, with 49% of the latter workforce being women. When assessing only rheumatologists practicing at greater than one FTE, the number increased from 89 in 2000 to 120 in 2015, with women making up 41.7% of the 2015 workforce. Although practice sizes decreased for both genders over the course of the study, in 2015 the median practice size was 1,948.5 patients (interquartile range, 1,433-2,562) for men, compared with 1,468.5 patients (IQR, 1,212-1,984) for women. In every year but 2001, men had larger median practice sizes than women.
Total patient visits remained relatively stable for men throughout the study period but declined for women, with the gap between genders widening over time. The peak gap in visits was 1,486 (95% confidence interval, 628-2,517) in 2008. And while median payments increased over time for all rheumatologists, median renumeration peaked in 2015 at $362,522 (IQR, $309,503-$437,127) for women, compared with $403,903 (IQR, $313,297-$544,703) for men. That said, the median difference that year – $45,556.10 (95% confidence interval, $951.60-$92,470.40; P = .04) – was the smallest for any in the study period. The largest difference was $102,176.10 (95% CI, $58,457.50-$152,821.20; P < .0001) in 2011.
An opportunity for female rheumatologists to reshape the specialty
Of course, gender gaps like these are not limited to rheumatology or even medicine, wrote Grace C. Wright, MD, PhD, president of the Association of Women in Rheumatology, in an accompanying editorial. “This issue exists across industries as well as across boundaries.”
“Particularly for women physicians, we do have additional demands on our time,” agreed April Jorge, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, in an interview. “For example, we know that women who work often have additional caregiving responsibilities at home, for kids and/or elderly relatives. I do think those are real reasons why certain providers, particularly women, might have a lower clinical volume.”
Despite the significant gender gaps that still exist, Dr. Jorge – who authored a previous study on the gaps in academic rheumatology – was heartened by the data that indicated more women finding their way into the specialty.
“I think it’s good news for rheumatology to be so balanced between men and women as providers,” she said. “For young women trainees, it’s really important to see role models in their field. For patients, it’s incredibly important for them to have a doctor who can relate and who can advocate for them. So many rheumatic conditions that we treat disproportionately affect women, often women of childbearing age. So it’s really important to have women involved in leading the specialty of rheumatology, including clinical practice but also research, education, and policy.”
Dr. Wright concurred in her editorial, stating that “this feminization of rheumatology provides an opportunity to assess the needs of working women, the generational shifts in attitudes toward work-life balance, and a change in clinical practice toward value over volume.”
The study’s authors shared its possible limitations, including the lack of a standard definition of a clinical FTE rheumatologist – thus their decision to define one – and a lack of context as to why certain rheumatologists were practicing less than others. In addition, they preemptively acknowledged Dr. Jorge’s concern by noting their inability to access gender-related details like marital status, family size, and childcare roles, all of which “could contribute to the relationship between physician gender and practice-level activity.”
The study was funded by an operating grant from the Canadian Initiative for Outcomes in Rheumatology Care and supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Two of the authors reported receiving support from the Arthritis Society Stars Career Development Award.
FROM THE JOURNAL OF RHEUMATOLOGY
The cost of pediatric specialization
I suspect that very few of you chose to go into pediatrics as part of a get-rich-quick scheme. But, like me, you may have assumed that by going into medicine you would always have a job buffered from the erratic winds of the economy, an assumption that it turns out did not take into account the risk of a global pandemic.
I also bet that if you chose to subspecialize it was not because you felt you might make more money. I and most of the lay public have always naively assumed that specialists generally make more money because … well, because they spent more time training. You, on the other hand, may have discovered belatedly that becoming a pediatric subspecialist isn’t as lucrative as you thought it might be.
It turns out that, when subjected to some standard money-crunching exercises, the lifetime earning potential of most pediatric subspecialists falls significantly behind that of general pediatricians. In a paper published in the April 2021 issue of Pediatrics, investigators from the departments of neurology and pediatric neurology at Johns Hopkins University have reported that, with the exception of three hospital-based, procedure-oriented specialties (cardiology, critical care, and neonatology) the earning time lost during training is usually not recouped over the course of a subspecialist’s career. This observation may be explained in many cases by the fact that the income generated by most subspecialists is similar to and not greater than that of general pediatricians. Even when the income of a subspecialist is greater, it is generally not enough to allow for catch up for the earning power lost during training. The researchers observed this effect both in academic and nonacademic settings.
It is possible that, as the results of this study become more widely distributed, more pediatricians in training will begin to think a bit more about the bottom line when they are considering fellowship training. I suspect that drift is already underway, and if it continues, we will find more subspecialties experiencing shortages. And the importance of this lack of subspecialists on both a local and national level is not something to ignore.
The authors discuss several possible solutions. One option might be to shorten the subspecialty training period. Obviously, this would raise some concerns about quality. Another might be for the government to begin a program in which student loans were selectively forgiven based on a physician’s decision to pursue a subspecialty that is experiencing a shortage.
Another option might be to subsidize the income of some subspecialists. Although this might have a similar effect as loan forgiveness, as a physician with a longstanding pride in being a generalist I would hate to see subspecialists guaranteed a higher income merely because of the narrower mix of patients they have chosen to see. I have always felt that the challenge faced by a primary care generalist who must be prepared to deal with the breadth of complaints that present themselves at the door is at least as great and in many cases greater than that of a specialist whose patients to a large extent have been presorted.
Another solution that comes to mind is that, instead of shortening fellowship programs, one could restructure basic pediatric training programs to allow physicians who have already chosen to become subspecialists to enter a fellowship program after 2 years of house officer training. Restructuring of this magnitude would not be as simple as lopping off the last year of house officer training. It would require tailoring each physician’s shortened prefellowship learning experience to maximize his or her exposure to clinical situations that will be most relevant to the anticipated subspecialty they have chosen. A plan like this also assumes that a significant number of recent medical school graduates will be ready to make choices during their internship that will channel them into careers that will span decades.
Becoming a generalist was an easy decision for me. Any of the subspecialties I was considering would have meant I would have had to live and work in or near a high-density population. I am and always have been a small town kind of guy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that very few of you chose to go into pediatrics as part of a get-rich-quick scheme. But, like me, you may have assumed that by going into medicine you would always have a job buffered from the erratic winds of the economy, an assumption that it turns out did not take into account the risk of a global pandemic.
I also bet that if you chose to subspecialize it was not because you felt you might make more money. I and most of the lay public have always naively assumed that specialists generally make more money because … well, because they spent more time training. You, on the other hand, may have discovered belatedly that becoming a pediatric subspecialist isn’t as lucrative as you thought it might be.
It turns out that, when subjected to some standard money-crunching exercises, the lifetime earning potential of most pediatric subspecialists falls significantly behind that of general pediatricians. In a paper published in the April 2021 issue of Pediatrics, investigators from the departments of neurology and pediatric neurology at Johns Hopkins University have reported that, with the exception of three hospital-based, procedure-oriented specialties (cardiology, critical care, and neonatology) the earning time lost during training is usually not recouped over the course of a subspecialist’s career. This observation may be explained in many cases by the fact that the income generated by most subspecialists is similar to and not greater than that of general pediatricians. Even when the income of a subspecialist is greater, it is generally not enough to allow for catch up for the earning power lost during training. The researchers observed this effect both in academic and nonacademic settings.
It is possible that, as the results of this study become more widely distributed, more pediatricians in training will begin to think a bit more about the bottom line when they are considering fellowship training. I suspect that drift is already underway, and if it continues, we will find more subspecialties experiencing shortages. And the importance of this lack of subspecialists on both a local and national level is not something to ignore.
The authors discuss several possible solutions. One option might be to shorten the subspecialty training period. Obviously, this would raise some concerns about quality. Another might be for the government to begin a program in which student loans were selectively forgiven based on a physician’s decision to pursue a subspecialty that is experiencing a shortage.
Another option might be to subsidize the income of some subspecialists. Although this might have a similar effect as loan forgiveness, as a physician with a longstanding pride in being a generalist I would hate to see subspecialists guaranteed a higher income merely because of the narrower mix of patients they have chosen to see. I have always felt that the challenge faced by a primary care generalist who must be prepared to deal with the breadth of complaints that present themselves at the door is at least as great and in many cases greater than that of a specialist whose patients to a large extent have been presorted.
Another solution that comes to mind is that, instead of shortening fellowship programs, one could restructure basic pediatric training programs to allow physicians who have already chosen to become subspecialists to enter a fellowship program after 2 years of house officer training. Restructuring of this magnitude would not be as simple as lopping off the last year of house officer training. It would require tailoring each physician’s shortened prefellowship learning experience to maximize his or her exposure to clinical situations that will be most relevant to the anticipated subspecialty they have chosen. A plan like this also assumes that a significant number of recent medical school graduates will be ready to make choices during their internship that will channel them into careers that will span decades.
Becoming a generalist was an easy decision for me. Any of the subspecialties I was considering would have meant I would have had to live and work in or near a high-density population. I am and always have been a small town kind of guy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that very few of you chose to go into pediatrics as part of a get-rich-quick scheme. But, like me, you may have assumed that by going into medicine you would always have a job buffered from the erratic winds of the economy, an assumption that it turns out did not take into account the risk of a global pandemic.
I also bet that if you chose to subspecialize it was not because you felt you might make more money. I and most of the lay public have always naively assumed that specialists generally make more money because … well, because they spent more time training. You, on the other hand, may have discovered belatedly that becoming a pediatric subspecialist isn’t as lucrative as you thought it might be.
It turns out that, when subjected to some standard money-crunching exercises, the lifetime earning potential of most pediatric subspecialists falls significantly behind that of general pediatricians. In a paper published in the April 2021 issue of Pediatrics, investigators from the departments of neurology and pediatric neurology at Johns Hopkins University have reported that, with the exception of three hospital-based, procedure-oriented specialties (cardiology, critical care, and neonatology) the earning time lost during training is usually not recouped over the course of a subspecialist’s career. This observation may be explained in many cases by the fact that the income generated by most subspecialists is similar to and not greater than that of general pediatricians. Even when the income of a subspecialist is greater, it is generally not enough to allow for catch up for the earning power lost during training. The researchers observed this effect both in academic and nonacademic settings.
It is possible that, as the results of this study become more widely distributed, more pediatricians in training will begin to think a bit more about the bottom line when they are considering fellowship training. I suspect that drift is already underway, and if it continues, we will find more subspecialties experiencing shortages. And the importance of this lack of subspecialists on both a local and national level is not something to ignore.
The authors discuss several possible solutions. One option might be to shorten the subspecialty training period. Obviously, this would raise some concerns about quality. Another might be for the government to begin a program in which student loans were selectively forgiven based on a physician’s decision to pursue a subspecialty that is experiencing a shortage.
Another option might be to subsidize the income of some subspecialists. Although this might have a similar effect as loan forgiveness, as a physician with a longstanding pride in being a generalist I would hate to see subspecialists guaranteed a higher income merely because of the narrower mix of patients they have chosen to see. I have always felt that the challenge faced by a primary care generalist who must be prepared to deal with the breadth of complaints that present themselves at the door is at least as great and in many cases greater than that of a specialist whose patients to a large extent have been presorted.
Another solution that comes to mind is that, instead of shortening fellowship programs, one could restructure basic pediatric training programs to allow physicians who have already chosen to become subspecialists to enter a fellowship program after 2 years of house officer training. Restructuring of this magnitude would not be as simple as lopping off the last year of house officer training. It would require tailoring each physician’s shortened prefellowship learning experience to maximize his or her exposure to clinical situations that will be most relevant to the anticipated subspecialty they have chosen. A plan like this also assumes that a significant number of recent medical school graduates will be ready to make choices during their internship that will channel them into careers that will span decades.
Becoming a generalist was an easy decision for me. Any of the subspecialties I was considering would have meant I would have had to live and work in or near a high-density population. I am and always have been a small town kind of guy.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
New global telepsychiatry guidelines released
The World Psychiatric Association (WPA) has released new global telemedicine guidelines.
Prompted by the worldwide explosion of interest in telepsychiatry driven by the COVID-19 pandemic, the guidelines emphasize the need for international collaboration in psychiatry.
“Global teamwork is the light at the end of the tunnel” of the current crisis, lead author Davor Mucic, MD, The Little Prince Treatment Center, Copenhagen, told meeting attendees.
“Now is the time to build a user-friendly digital health care system that can better meet the inevitable future challenges,” Dr. Mucic said. “The hope is that WPA’s global guidelines for telepsychiatry can help us to move forward.”
The guidelines, which also address concerns over data security and device intercompatibility, were presented at the virtual European Psychiatric Association (EPA) 2021 Congress.
Breaking down barriers
Although telepsychiatry has been around since 1959, only with the rapid technologic advances of the past decade has it become available to the majority of psychiatric patients, Dr. Mucic noted.
“Unfortunately, regulatory constraints, in combination with clinicians’ concerns, kept telepsychiatry from being widely adopted and implemented prior to the current COVID-19 pandemic,” he added.
Concerns have been with regard to data safety, reimbursement for consultations, quality of care, lack of technical experience, and difficulties in changing routines.
For many clinicians, the pandemic was the “first time they used telepsychiatry, and very few have received training in how to do it,” Dr. Mucic said.
He pointed out that , including the 2018 Best Practices in Videoconferencing-Based Telemental Health, released by the American Psychiatric Association and the American Telemedicine Association.
Dr. Mucic noted that because these documents are relevant and useful, clinicians may wonder, “Why do we need another set of guidelines?”
He explained that the current WPA guidelines outline universal recommendations that apply “regardless of local or regional regulations.” Therefore, they can be used just as easily in low- and middle-income countries as in countries where telepsychiatry is already established.
A new paradigm
Similar to other guidelines, the WPA’s guidelines discuss legal and regulatory requirements, informed consent, billing and reimbursement, patient selection, clinician training, the clinical setting, and more.
However, what makes the new document “so new and special” is that it opens the door to “some new and previously undiscussed aspects of telepsychiatry ... that are capable of changing the whole delivery of mental health care,” Dr. Mucic said.
The first of these new aspects is in regard to cross-cultural telepsychiatry. The goal is to eliminate the need for interpreters or competency in a different language for patients who do not speak the host country’s language by connecting them remotely with a bilingual health care professional who shares their cultural or ethnic background.
This “ethnic matching” model may lead to a “more precise and detailed symptomatology,” the authors note. They add that minimizing the risk for misinterpretation and misunderstanding can enable better diagnosis and treatment.
The second area highlighted by Dr. Mucic is in regard to international telepsychiatry; the technology could be used to obtain a second opinion from colleagues who share the relevant cultural and linguistic background.
“Further, international expertise may be brought via [telepsychiatry] to local health workers as a part of education, supervision, and scientific collaboration,” he said.
“The hope is the guidelines will pave the way for improved international collaboration, not only by clinicians but also by policymakers.”
A blended future?
Also at EPA 2021, two experts debated whether the COVID-19 pandemic represented a turning point for e-health in psychiatry.
Taking the pro stance, Heleen Riper, PhD, professor of eMental-Health at the Vrije Universiteit Amsterdam, argued that the future is likely to blend face-to-face interaction with video conferencing.
She believes that to maintain current progress, the focus should be on treatment personalization, engagement, and improvement, rather than cost-effectiveness.
Hans-Jürgen Möller, MD, professor emeritus, department of psychiatry, Ludwig-Maximilians-University, Munich, argued against the idea that e-health represented a turning point in psychiatry. He noted that a survey of German psychotherapists indicated that there have been a number of drawbacks to video sessions during the pandemic.
These included that the technology was not available or could be used by all patients, especially the elderly, and that unstable internet connections have posed a problem. Moreover, video conferencing is considered a “poor substitute” for face-to-face interactions by many patients.
In the subsequent discussion, Dr. Möller told this news organization that he believes guidelines in this area are important, especially to differentiate among various offerings on the internet, some of which are “not very good,” and to help patients identify those that are “very well established.”
Dr. Riper agreed, saying that several initiatives to introduce guidelines at the European level are now underway.
The biggest challenge from a technological standpoint is to offer flexibility to patients while still applying “therapeutic principles,” she noted.
“There is a need for guidelines, but those guidelines need to be open to a certain amount of flexibility if you really want to upscale technology into routine care,” Dr. Riper said.
Cautious optimism
Session chair Judit Simon, MD, DPhil, professor of health economics, Medical University of Vienna, asked the debaters whether video interventions will continue to replace in-person interventions once the pandemic is over or whether things will return to “where we were prepandemic.”
Dr. Riper said she did not believe that clinicians will return completely to in-patient practice. However, she emphasized the need for training and the development of new skills to improve the therapeutic relationship with patients.
Although Dr. Riper believes there is still a need for in-person doctor/patient interactions, “we will never get back to the pre-COVID phase, both in terms of diagnostics and treatment,” she said.
Dr. Möller added that although he has “some reservations” regarding the adoption of technologies by older patients and the lack of long-term data on telepsychiatry, he partially shares Dr. Riper’s optimism.
He suggested that there is an opportunity in psychiatry to use video conferencing for multidisciplinary team meetings similar to those seen in oncology.
This would allow discussion of patient diagnosis and treatment and would enable experts in mental health to help clinicians in other specialties. For example, it could help a general practitioner differentiate between depression and a depressive phase of schizophrenia, Dr. Riper said.
The presenters have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Psychiatric Association (WPA) has released new global telemedicine guidelines.
Prompted by the worldwide explosion of interest in telepsychiatry driven by the COVID-19 pandemic, the guidelines emphasize the need for international collaboration in psychiatry.
“Global teamwork is the light at the end of the tunnel” of the current crisis, lead author Davor Mucic, MD, The Little Prince Treatment Center, Copenhagen, told meeting attendees.
“Now is the time to build a user-friendly digital health care system that can better meet the inevitable future challenges,” Dr. Mucic said. “The hope is that WPA’s global guidelines for telepsychiatry can help us to move forward.”
The guidelines, which also address concerns over data security and device intercompatibility, were presented at the virtual European Psychiatric Association (EPA) 2021 Congress.
Breaking down barriers
Although telepsychiatry has been around since 1959, only with the rapid technologic advances of the past decade has it become available to the majority of psychiatric patients, Dr. Mucic noted.
“Unfortunately, regulatory constraints, in combination with clinicians’ concerns, kept telepsychiatry from being widely adopted and implemented prior to the current COVID-19 pandemic,” he added.
Concerns have been with regard to data safety, reimbursement for consultations, quality of care, lack of technical experience, and difficulties in changing routines.
For many clinicians, the pandemic was the “first time they used telepsychiatry, and very few have received training in how to do it,” Dr. Mucic said.
He pointed out that , including the 2018 Best Practices in Videoconferencing-Based Telemental Health, released by the American Psychiatric Association and the American Telemedicine Association.
Dr. Mucic noted that because these documents are relevant and useful, clinicians may wonder, “Why do we need another set of guidelines?”
He explained that the current WPA guidelines outline universal recommendations that apply “regardless of local or regional regulations.” Therefore, they can be used just as easily in low- and middle-income countries as in countries where telepsychiatry is already established.
A new paradigm
Similar to other guidelines, the WPA’s guidelines discuss legal and regulatory requirements, informed consent, billing and reimbursement, patient selection, clinician training, the clinical setting, and more.
However, what makes the new document “so new and special” is that it opens the door to “some new and previously undiscussed aspects of telepsychiatry ... that are capable of changing the whole delivery of mental health care,” Dr. Mucic said.
The first of these new aspects is in regard to cross-cultural telepsychiatry. The goal is to eliminate the need for interpreters or competency in a different language for patients who do not speak the host country’s language by connecting them remotely with a bilingual health care professional who shares their cultural or ethnic background.
This “ethnic matching” model may lead to a “more precise and detailed symptomatology,” the authors note. They add that minimizing the risk for misinterpretation and misunderstanding can enable better diagnosis and treatment.
The second area highlighted by Dr. Mucic is in regard to international telepsychiatry; the technology could be used to obtain a second opinion from colleagues who share the relevant cultural and linguistic background.
“Further, international expertise may be brought via [telepsychiatry] to local health workers as a part of education, supervision, and scientific collaboration,” he said.
“The hope is the guidelines will pave the way for improved international collaboration, not only by clinicians but also by policymakers.”
A blended future?
Also at EPA 2021, two experts debated whether the COVID-19 pandemic represented a turning point for e-health in psychiatry.
Taking the pro stance, Heleen Riper, PhD, professor of eMental-Health at the Vrije Universiteit Amsterdam, argued that the future is likely to blend face-to-face interaction with video conferencing.
She believes that to maintain current progress, the focus should be on treatment personalization, engagement, and improvement, rather than cost-effectiveness.
Hans-Jürgen Möller, MD, professor emeritus, department of psychiatry, Ludwig-Maximilians-University, Munich, argued against the idea that e-health represented a turning point in psychiatry. He noted that a survey of German psychotherapists indicated that there have been a number of drawbacks to video sessions during the pandemic.
These included that the technology was not available or could be used by all patients, especially the elderly, and that unstable internet connections have posed a problem. Moreover, video conferencing is considered a “poor substitute” for face-to-face interactions by many patients.
In the subsequent discussion, Dr. Möller told this news organization that he believes guidelines in this area are important, especially to differentiate among various offerings on the internet, some of which are “not very good,” and to help patients identify those that are “very well established.”
Dr. Riper agreed, saying that several initiatives to introduce guidelines at the European level are now underway.
The biggest challenge from a technological standpoint is to offer flexibility to patients while still applying “therapeutic principles,” she noted.
“There is a need for guidelines, but those guidelines need to be open to a certain amount of flexibility if you really want to upscale technology into routine care,” Dr. Riper said.
Cautious optimism
Session chair Judit Simon, MD, DPhil, professor of health economics, Medical University of Vienna, asked the debaters whether video interventions will continue to replace in-person interventions once the pandemic is over or whether things will return to “where we were prepandemic.”
Dr. Riper said she did not believe that clinicians will return completely to in-patient practice. However, she emphasized the need for training and the development of new skills to improve the therapeutic relationship with patients.
Although Dr. Riper believes there is still a need for in-person doctor/patient interactions, “we will never get back to the pre-COVID phase, both in terms of diagnostics and treatment,” she said.
Dr. Möller added that although he has “some reservations” regarding the adoption of technologies by older patients and the lack of long-term data on telepsychiatry, he partially shares Dr. Riper’s optimism.
He suggested that there is an opportunity in psychiatry to use video conferencing for multidisciplinary team meetings similar to those seen in oncology.
This would allow discussion of patient diagnosis and treatment and would enable experts in mental health to help clinicians in other specialties. For example, it could help a general practitioner differentiate between depression and a depressive phase of schizophrenia, Dr. Riper said.
The presenters have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Psychiatric Association (WPA) has released new global telemedicine guidelines.
Prompted by the worldwide explosion of interest in telepsychiatry driven by the COVID-19 pandemic, the guidelines emphasize the need for international collaboration in psychiatry.
“Global teamwork is the light at the end of the tunnel” of the current crisis, lead author Davor Mucic, MD, The Little Prince Treatment Center, Copenhagen, told meeting attendees.
“Now is the time to build a user-friendly digital health care system that can better meet the inevitable future challenges,” Dr. Mucic said. “The hope is that WPA’s global guidelines for telepsychiatry can help us to move forward.”
The guidelines, which also address concerns over data security and device intercompatibility, were presented at the virtual European Psychiatric Association (EPA) 2021 Congress.
Breaking down barriers
Although telepsychiatry has been around since 1959, only with the rapid technologic advances of the past decade has it become available to the majority of psychiatric patients, Dr. Mucic noted.
“Unfortunately, regulatory constraints, in combination with clinicians’ concerns, kept telepsychiatry from being widely adopted and implemented prior to the current COVID-19 pandemic,” he added.
Concerns have been with regard to data safety, reimbursement for consultations, quality of care, lack of technical experience, and difficulties in changing routines.
For many clinicians, the pandemic was the “first time they used telepsychiatry, and very few have received training in how to do it,” Dr. Mucic said.
He pointed out that , including the 2018 Best Practices in Videoconferencing-Based Telemental Health, released by the American Psychiatric Association and the American Telemedicine Association.
Dr. Mucic noted that because these documents are relevant and useful, clinicians may wonder, “Why do we need another set of guidelines?”
He explained that the current WPA guidelines outline universal recommendations that apply “regardless of local or regional regulations.” Therefore, they can be used just as easily in low- and middle-income countries as in countries where telepsychiatry is already established.
A new paradigm
Similar to other guidelines, the WPA’s guidelines discuss legal and regulatory requirements, informed consent, billing and reimbursement, patient selection, clinician training, the clinical setting, and more.
However, what makes the new document “so new and special” is that it opens the door to “some new and previously undiscussed aspects of telepsychiatry ... that are capable of changing the whole delivery of mental health care,” Dr. Mucic said.
The first of these new aspects is in regard to cross-cultural telepsychiatry. The goal is to eliminate the need for interpreters or competency in a different language for patients who do not speak the host country’s language by connecting them remotely with a bilingual health care professional who shares their cultural or ethnic background.
This “ethnic matching” model may lead to a “more precise and detailed symptomatology,” the authors note. They add that minimizing the risk for misinterpretation and misunderstanding can enable better diagnosis and treatment.
The second area highlighted by Dr. Mucic is in regard to international telepsychiatry; the technology could be used to obtain a second opinion from colleagues who share the relevant cultural and linguistic background.
“Further, international expertise may be brought via [telepsychiatry] to local health workers as a part of education, supervision, and scientific collaboration,” he said.
“The hope is the guidelines will pave the way for improved international collaboration, not only by clinicians but also by policymakers.”
A blended future?
Also at EPA 2021, two experts debated whether the COVID-19 pandemic represented a turning point for e-health in psychiatry.
Taking the pro stance, Heleen Riper, PhD, professor of eMental-Health at the Vrije Universiteit Amsterdam, argued that the future is likely to blend face-to-face interaction with video conferencing.
She believes that to maintain current progress, the focus should be on treatment personalization, engagement, and improvement, rather than cost-effectiveness.
Hans-Jürgen Möller, MD, professor emeritus, department of psychiatry, Ludwig-Maximilians-University, Munich, argued against the idea that e-health represented a turning point in psychiatry. He noted that a survey of German psychotherapists indicated that there have been a number of drawbacks to video sessions during the pandemic.
These included that the technology was not available or could be used by all patients, especially the elderly, and that unstable internet connections have posed a problem. Moreover, video conferencing is considered a “poor substitute” for face-to-face interactions by many patients.
In the subsequent discussion, Dr. Möller told this news organization that he believes guidelines in this area are important, especially to differentiate among various offerings on the internet, some of which are “not very good,” and to help patients identify those that are “very well established.”
Dr. Riper agreed, saying that several initiatives to introduce guidelines at the European level are now underway.
The biggest challenge from a technological standpoint is to offer flexibility to patients while still applying “therapeutic principles,” she noted.
“There is a need for guidelines, but those guidelines need to be open to a certain amount of flexibility if you really want to upscale technology into routine care,” Dr. Riper said.
Cautious optimism
Session chair Judit Simon, MD, DPhil, professor of health economics, Medical University of Vienna, asked the debaters whether video interventions will continue to replace in-person interventions once the pandemic is over or whether things will return to “where we were prepandemic.”
Dr. Riper said she did not believe that clinicians will return completely to in-patient practice. However, she emphasized the need for training and the development of new skills to improve the therapeutic relationship with patients.
Although Dr. Riper believes there is still a need for in-person doctor/patient interactions, “we will never get back to the pre-COVID phase, both in terms of diagnostics and treatment,” she said.
Dr. Möller added that although he has “some reservations” regarding the adoption of technologies by older patients and the lack of long-term data on telepsychiatry, he partially shares Dr. Riper’s optimism.
He suggested that there is an opportunity in psychiatry to use video conferencing for multidisciplinary team meetings similar to those seen in oncology.
This would allow discussion of patient diagnosis and treatment and would enable experts in mental health to help clinicians in other specialties. For example, it could help a general practitioner differentiate between depression and a depressive phase of schizophrenia, Dr. Riper said.
The presenters have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Survey shines light on pediatric dermatologists’ earnings
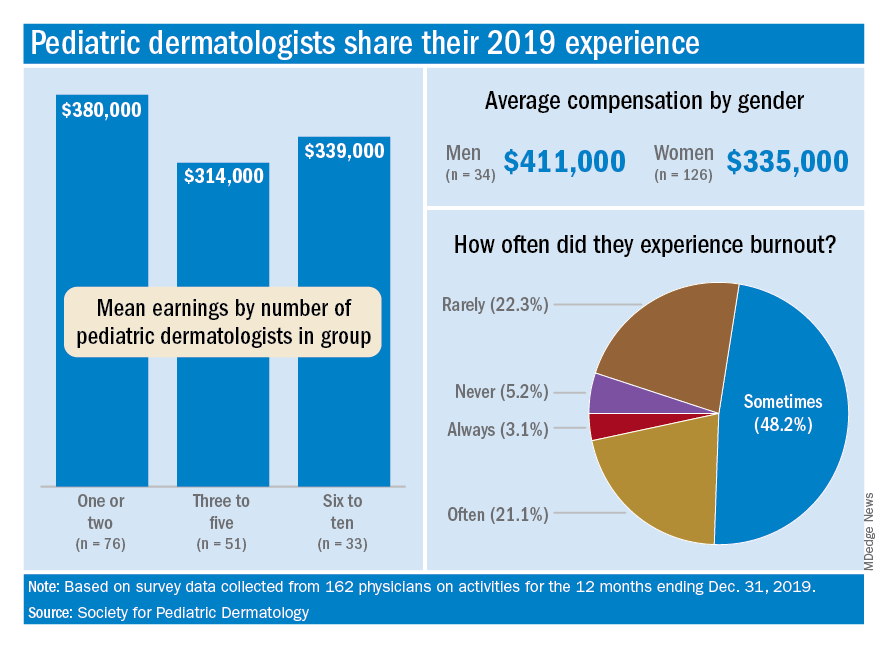
For one thing, the median total compensation for the 162 pediatric dermatologists whose survey responses were included in the final data set was a somewhat lower $335,000, the SPD said in its 2020 Pediatric Dermatology Physician Compensation Report.
Getting back to the mean, average earnings were highest, over $505,000, among those working in hospitals/health systems, followed by independent group practices at $436,000, while those working in academic hospitals/health systems – the most popular type of ownership entity (69% of all respondents) – had a mean compensation of $323,000, the SPD said in the report.
At a more basic level, average earnings tilted toward men over women, $411,000-$335,000, although a majority of the respondents (78%) were female, according to the SPD.
Patient mix produced a strong trend of increasing earnings with decreasing pediatric case load. Average compensation was lowest among those who saw 98%-100% pediatric patients ($330,000), rose for physicians who saw 80%-97% ($345,000) and 50%-79% children ($398,000), and topped out at $444,000 for those who saw fewer than 50% children, the SPD data show.
The number of pediatric dermatologists working in a practice also had an effect: Average compensation in practices with 1-2 such specialists was almost $380,000 in 2019, compared with $340,000 in groups with 6-10 pediatric dermatologists and $314,000 for those with 3-5. There were too few groups with more than 10 to meet the sample-size criteria, the SPD noted.
Average starting salary was $286,000 for the 17 respondents who reported that they were newly hired for full-time positions, with a median of $262,500, which was “22% lower than the median clinical compensation reported by pediatric dermatology physicians hired prior to 2019,” the report indicated.
Respondents also were asked about issues of satisfaction and burnout, and these data include responses from additional physicians (for a total of 193) not included in the compensation data set.
The largest share, 79%, said that patient relationships were most satisfying factor of their profession, with intellectual stimulation next at 59% and interaction with colleagues third at 42%. The least satisfying elements were regulatory/paperwork burdens (80%), inefficient EHR design/interoperability (37%), and the commoditization of medicine (21%), the SPD said.
Feelings of burnout were common among almost a quarter of pediatric dermatologists, with 3.1% saying they always have such feelings and 21.2% disclosing that they often feel burned out. Only 5.2% said that they never have feelings of burnout, the SPD reported.
Demographically speaking, 71% of those surveyed identified as White, 22% as Asian, 8.5% as Hispanic/Latino/Spanish, 2.5% as Middle Eastern or North African, and 2.5% as Black or African American. The largest age group, with 61% of all respondents, was 36-50 years, and geography gave the East a slight edge over the West, 30% to 28%, although California had the largest share by state, 17.4%, the report said.
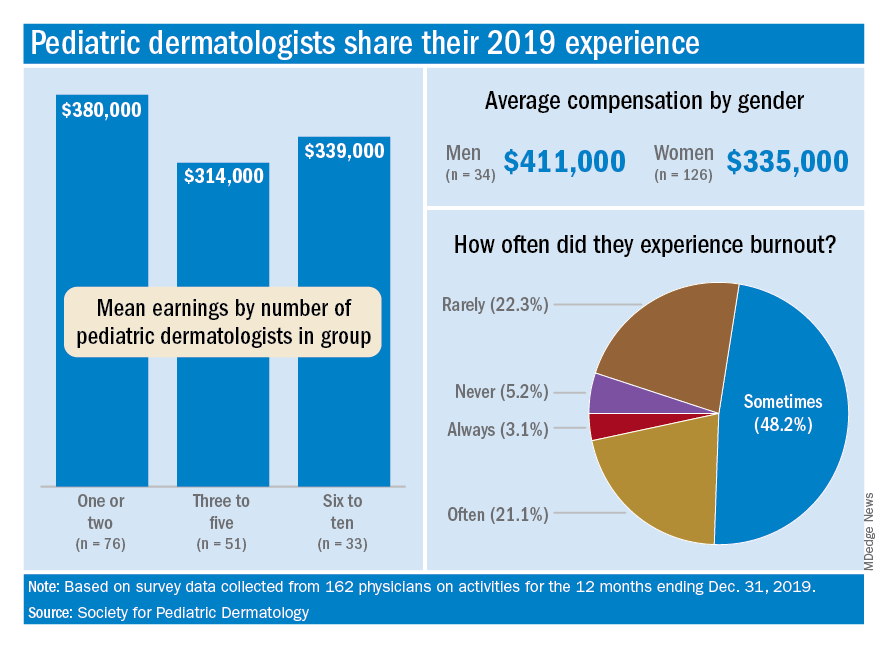
For one thing, the median total compensation for the 162 pediatric dermatologists whose survey responses were included in the final data set was a somewhat lower $335,000, the SPD said in its 2020 Pediatric Dermatology Physician Compensation Report.
Getting back to the mean, average earnings were highest, over $505,000, among those working in hospitals/health systems, followed by independent group practices at $436,000, while those working in academic hospitals/health systems – the most popular type of ownership entity (69% of all respondents) – had a mean compensation of $323,000, the SPD said in the report.
At a more basic level, average earnings tilted toward men over women, $411,000-$335,000, although a majority of the respondents (78%) were female, according to the SPD.
Patient mix produced a strong trend of increasing earnings with decreasing pediatric case load. Average compensation was lowest among those who saw 98%-100% pediatric patients ($330,000), rose for physicians who saw 80%-97% ($345,000) and 50%-79% children ($398,000), and topped out at $444,000 for those who saw fewer than 50% children, the SPD data show.
The number of pediatric dermatologists working in a practice also had an effect: Average compensation in practices with 1-2 such specialists was almost $380,000 in 2019, compared with $340,000 in groups with 6-10 pediatric dermatologists and $314,000 for those with 3-5. There were too few groups with more than 10 to meet the sample-size criteria, the SPD noted.
Average starting salary was $286,000 for the 17 respondents who reported that they were newly hired for full-time positions, with a median of $262,500, which was “22% lower than the median clinical compensation reported by pediatric dermatology physicians hired prior to 2019,” the report indicated.
Respondents also were asked about issues of satisfaction and burnout, and these data include responses from additional physicians (for a total of 193) not included in the compensation data set.
The largest share, 79%, said that patient relationships were most satisfying factor of their profession, with intellectual stimulation next at 59% and interaction with colleagues third at 42%. The least satisfying elements were regulatory/paperwork burdens (80%), inefficient EHR design/interoperability (37%), and the commoditization of medicine (21%), the SPD said.
Feelings of burnout were common among almost a quarter of pediatric dermatologists, with 3.1% saying they always have such feelings and 21.2% disclosing that they often feel burned out. Only 5.2% said that they never have feelings of burnout, the SPD reported.
Demographically speaking, 71% of those surveyed identified as White, 22% as Asian, 8.5% as Hispanic/Latino/Spanish, 2.5% as Middle Eastern or North African, and 2.5% as Black or African American. The largest age group, with 61% of all respondents, was 36-50 years, and geography gave the East a slight edge over the West, 30% to 28%, although California had the largest share by state, 17.4%, the report said.
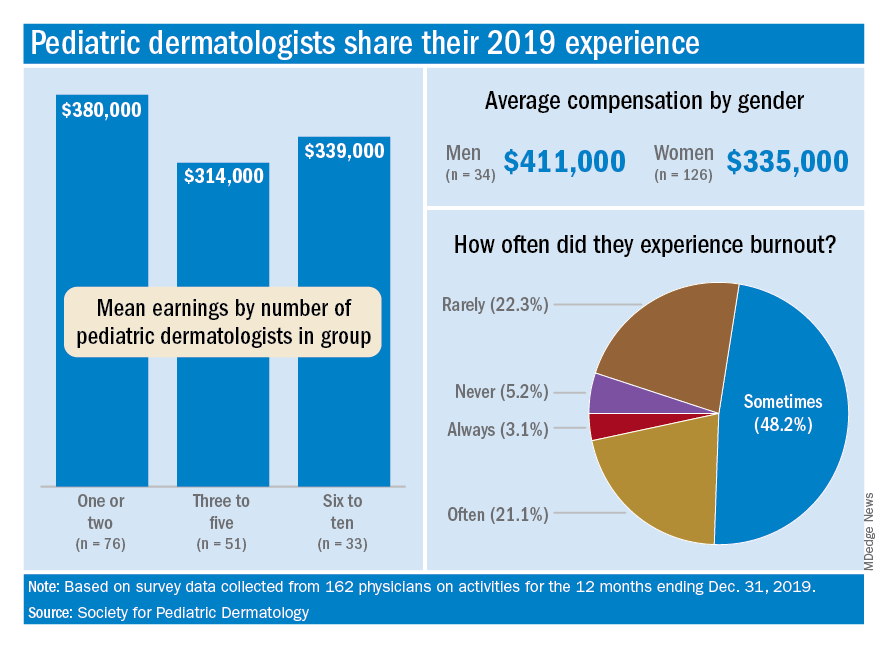
For one thing, the median total compensation for the 162 pediatric dermatologists whose survey responses were included in the final data set was a somewhat lower $335,000, the SPD said in its 2020 Pediatric Dermatology Physician Compensation Report.
Getting back to the mean, average earnings were highest, over $505,000, among those working in hospitals/health systems, followed by independent group practices at $436,000, while those working in academic hospitals/health systems – the most popular type of ownership entity (69% of all respondents) – had a mean compensation of $323,000, the SPD said in the report.
At a more basic level, average earnings tilted toward men over women, $411,000-$335,000, although a majority of the respondents (78%) were female, according to the SPD.
Patient mix produced a strong trend of increasing earnings with decreasing pediatric case load. Average compensation was lowest among those who saw 98%-100% pediatric patients ($330,000), rose for physicians who saw 80%-97% ($345,000) and 50%-79% children ($398,000), and topped out at $444,000 for those who saw fewer than 50% children, the SPD data show.
The number of pediatric dermatologists working in a practice also had an effect: Average compensation in practices with 1-2 such specialists was almost $380,000 in 2019, compared with $340,000 in groups with 6-10 pediatric dermatologists and $314,000 for those with 3-5. There were too few groups with more than 10 to meet the sample-size criteria, the SPD noted.
Average starting salary was $286,000 for the 17 respondents who reported that they were newly hired for full-time positions, with a median of $262,500, which was “22% lower than the median clinical compensation reported by pediatric dermatology physicians hired prior to 2019,” the report indicated.
Respondents also were asked about issues of satisfaction and burnout, and these data include responses from additional physicians (for a total of 193) not included in the compensation data set.
The largest share, 79%, said that patient relationships were most satisfying factor of their profession, with intellectual stimulation next at 59% and interaction with colleagues third at 42%. The least satisfying elements were regulatory/paperwork burdens (80%), inefficient EHR design/interoperability (37%), and the commoditization of medicine (21%), the SPD said.
Feelings of burnout were common among almost a quarter of pediatric dermatologists, with 3.1% saying they always have such feelings and 21.2% disclosing that they often feel burned out. Only 5.2% said that they never have feelings of burnout, the SPD reported.
Demographically speaking, 71% of those surveyed identified as White, 22% as Asian, 8.5% as Hispanic/Latino/Spanish, 2.5% as Middle Eastern or North African, and 2.5% as Black or African American. The largest age group, with 61% of all respondents, was 36-50 years, and geography gave the East a slight edge over the West, 30% to 28%, although California had the largest share by state, 17.4%, the report said.
Remote cardio visits expand access for underserved during COVID
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Remote cardiology clinic visits during COVID-19 were used more often by certain traditionally underserved patient groups, but were also associated with less frequent testing and prescribing, new research shows.
“The COVID-19 pandemic has led to an unprecedented shift in ambulatory cardiovascular care from in-person to remote visits,” lead author Neal Yuan, MD, a cardiology fellow at the Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, said in an interview.
Their findings were published online April 5 in JAMA Network Open.
“We wanted to explore whether the transition to remote visits was associated with disparities in how patients accessed care, and also how this transition affected diagnostic test ordering and medication prescribing,” Dr. Yuan said.
The researchers used electronic health records data for all ambulatory cardiology visits at an urban, multisite health system in Los Angeles County during two periods: April 1 to Dec. 31, 2019, the pre-COVID era; and April 1 to Dec. 31, 2020, the COVID era.
The investigators compared patient characteristics and frequencies of medication ordering and cardiology-specific testing across four visit types: pre-COVID in person, used as reference; COVID-era in person; COVID-era video; and COVID-era telephone.
The study looked at 176,781 ambulatory cardiology visits. Of these visits, 87,182 were conducted in person in the pre-COVID period; 74,498 were conducted in person in the COVID era; 4,720 were COVID-era video visits; and 10,381 were COVID-era telephone visits.
In the study cohort, 79,572 patients (45.0%) were female, 127,080 patients (71.9%) were non-Hispanic White, and the mean age was 68.1 years (standard deviation, 17.0).
Patients accessing COVID-era remote visits were more likely to be Asian, Black, or Hispanic, to have private insurance, and to have cardiovascular comorbidities, such as hypertension and heart failure.
Also, patients whose visits were conducted by video were significantly younger than patients whose visits were conducted in person or by telephone (P < .001).
In addition, the study found that clinicians ordered fewer diagnostic tests, such as electrocardiograms and echocardiograms, and were less likely to order any medication, in the pre-COVID era than during the COVID era.
“If you don’t have a patient in front of you, it’s much more difficult to get a physical exam or obtain reliable vital signs,” said Dr. Yuan. Communication can sometimes be difficult, often because of technical issues, like a bad connection. “You might be more reticent to get testing or to prescribe medications if you don’t feel confident knowing what the patient’s vital signs are.”
In addition, he added, “a lot of medications used in the cardiology setting require monitoring patients’ kidney function and electrolytes, and if you can’t do that reliably, you might be more cautious about prescribing those types of medications.”
An eye-opening study
Cardiologist Nieca Goldberg, MD, medical director of the New York University Langone womens’ heart program and spokesperson for the American Heart Association, recounted her experience with telemedicine at the height of the pandemic in New York, when everything, including medical outpatient offices, had to close.
“We were experienced with telemedicine because we had started a virtual urgent care program well ahead of the pandemic,” she said. “We started using that to screen people with potential COVID symptoms so that they wouldn’t have to come into the hospital, the medical center, or to the offices and expose people. We learned that it was great to have the telemedicine option from the infectious disease standpoint, and I did visits like that for my own patient population.”
An equally if not more important finding from the study is the fact that telemedicine increased access to care among traditionally underserved demographics, she said.
“This is eye-opening, that you can actually improve access to care by doing telemedicine visits. It was really important to see that telemedicine has added benefit to the way we can see people in the health care system.”
Telemedicine visits had a positive impact at a time when people were isolated at home, Dr. Goldberg said.
“It was a way for them to connect with their doctor and in some ways it was more personal,” she added. “I actually got to meet some of my patients’ family members. It was like making a remote house call.”
Stable cardiology patients can take their blood pressure at home, weigh themselves, and take their own pulse to give an excellent set of vital signs that will indicate how they are doing, said Dr. Goldberg.
“During a remote visit, we can talk to the patient and notice whether or not they are short of breath or coughing, but we can’t listen to their heart or do an EKG or any of the traditional cardiac testing. Still, for someone who is not having symptoms and is able to reliably monitor their blood pressure and weight, a remote visit is sufficient to give you a good sense of how that patient is doing,” she said. “We can talk to them about their medications, any potential side effects, and we can use their blood pressure information to adjust their medications.”
Many patients are becoming more savvy about using tech gadgets and devices to monitor their health.
“Some of my patients were using Apple watches and the Kardia app to address their heart rate. Many had purchased inexpensive pulse oximeters to check their oxygen during the pandemic, and that also reads the pulse,” Dr. Goldberg said.
In-person visits were reserved for symptomatic cardiac patients, she explained.
“Initially during the pandemic, we did mostly telemedicine visits and we organized the office so that each cardiologist would come in 1 day a week to take care of symptomatic cardiac patients. In that way, we were able to socially distance – they provided us with [personal protective equipment]; at NYU there was no problem with that – and nobody waited in the waiting room. To this day, office issues are more efficient and people are not waiting in the waiting room,” she added. “Telemedicine improves access to health care in populations where such access is limited.”
Dr. Yuan’s research is supported by a grant from the National Institutes of Health. Dr. Goldberg reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.