User login
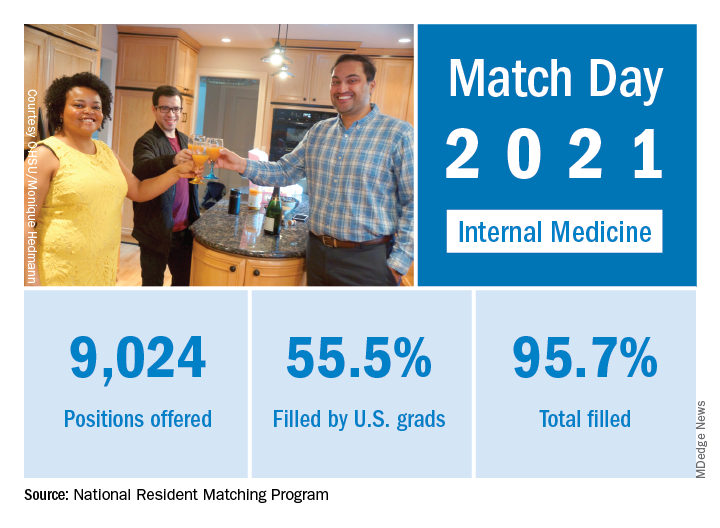
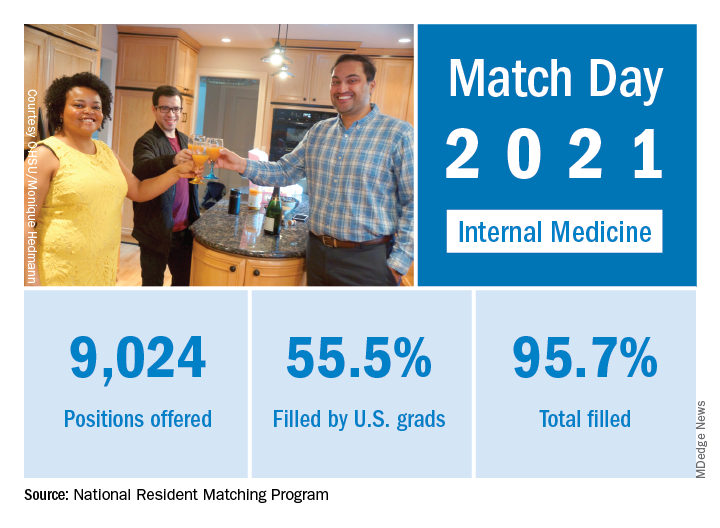
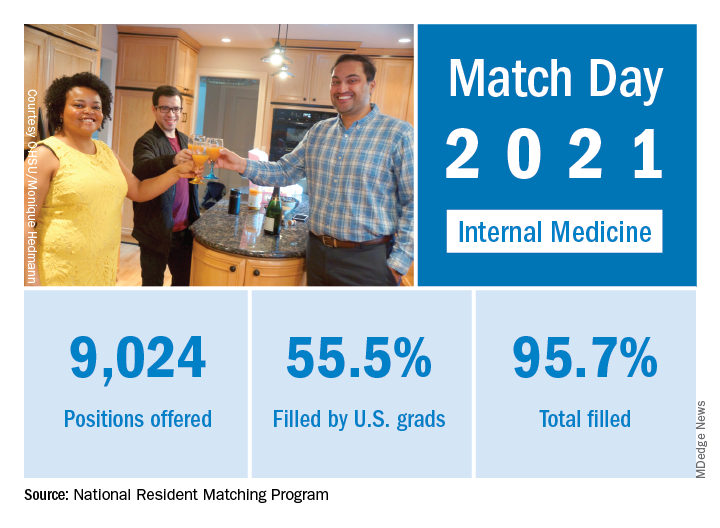
Match Day 2021: Internal medicine keeps growing
according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) record numbers of first-year (PGY-1) slots. That fill rate of 94.8% was up from 94.6% the year before.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, president and CEO of the NRMP.
Internal medicine offered 9,024 positions in this year’s Match, up by 3.8% over 2020, and filled 8,632, for a 1-year increase of 3.7% and a fill rate of 95.7%. Over 55% (5,005) of the available slots were given to U.S. seniors (MDs and DOs), while 37.9% went to international medical graduates. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in internal medicine residencies has increased by 1,791 (24.8%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Internal medicine also increased its share of all available residency positions from 24.9% in 2018 to 25.6% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The internal medicine workforce remains the backbone of our health care system, and expansion of this workforce is imperative to provide access to specialty and subspecialty medical care for future patients,” Philip A. Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in a separate statement.
according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) record numbers of first-year (PGY-1) slots. That fill rate of 94.8% was up from 94.6% the year before.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, president and CEO of the NRMP.
Internal medicine offered 9,024 positions in this year’s Match, up by 3.8% over 2020, and filled 8,632, for a 1-year increase of 3.7% and a fill rate of 95.7%. Over 55% (5,005) of the available slots were given to U.S. seniors (MDs and DOs), while 37.9% went to international medical graduates. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in internal medicine residencies has increased by 1,791 (24.8%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Internal medicine also increased its share of all available residency positions from 24.9% in 2018 to 25.6% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The internal medicine workforce remains the backbone of our health care system, and expansion of this workforce is imperative to provide access to specialty and subspecialty medical care for future patients,” Philip A. Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in a separate statement.
according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) record numbers of first-year (PGY-1) slots. That fill rate of 94.8% was up from 94.6% the year before.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, president and CEO of the NRMP.
Internal medicine offered 9,024 positions in this year’s Match, up by 3.8% over 2020, and filled 8,632, for a 1-year increase of 3.7% and a fill rate of 95.7%. Over 55% (5,005) of the available slots were given to U.S. seniors (MDs and DOs), while 37.9% went to international medical graduates. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in internal medicine residencies has increased by 1,791 (24.8%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Internal medicine also increased its share of all available residency positions from 24.9% in 2018 to 25.6% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The internal medicine workforce remains the backbone of our health care system, and expansion of this workforce is imperative to provide access to specialty and subspecialty medical care for future patients,” Philip A. Masters, MD, vice president of membership and global engagement at the American College of Physicians, said in a separate statement.
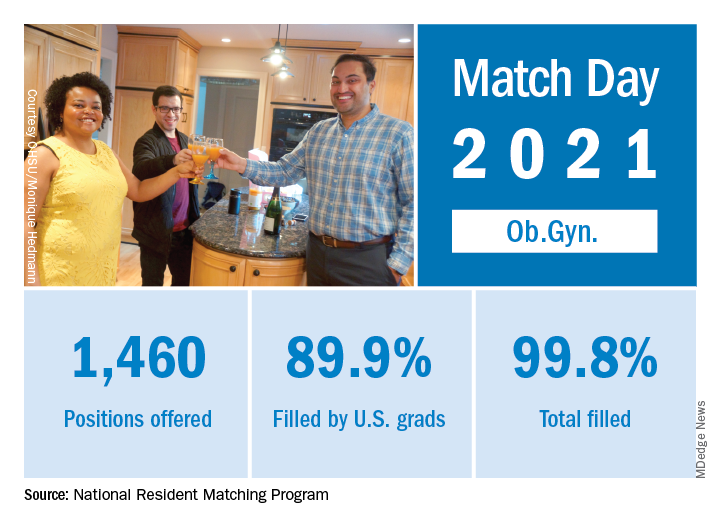
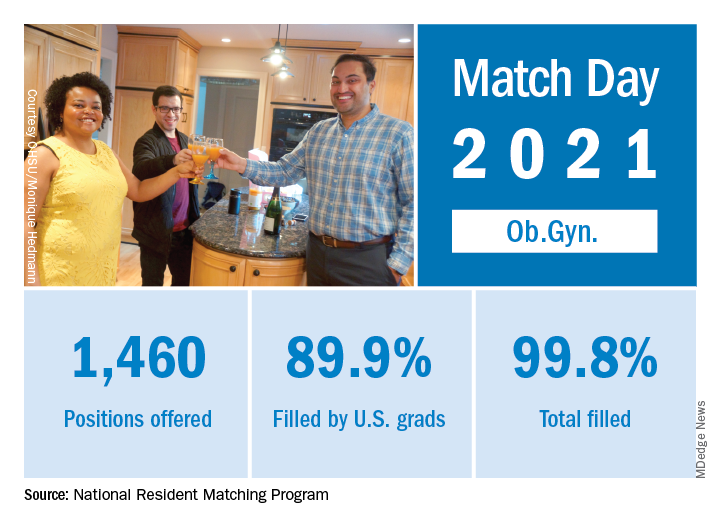
Match Day 2021: Interest in ob.gyn. outpaced growth
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
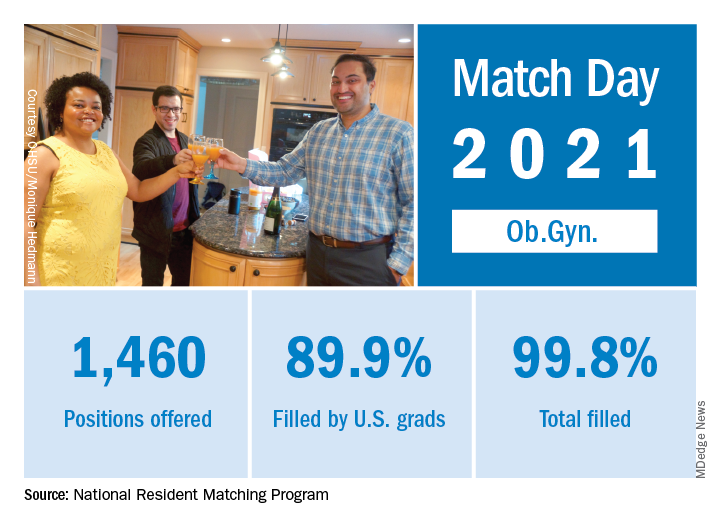
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
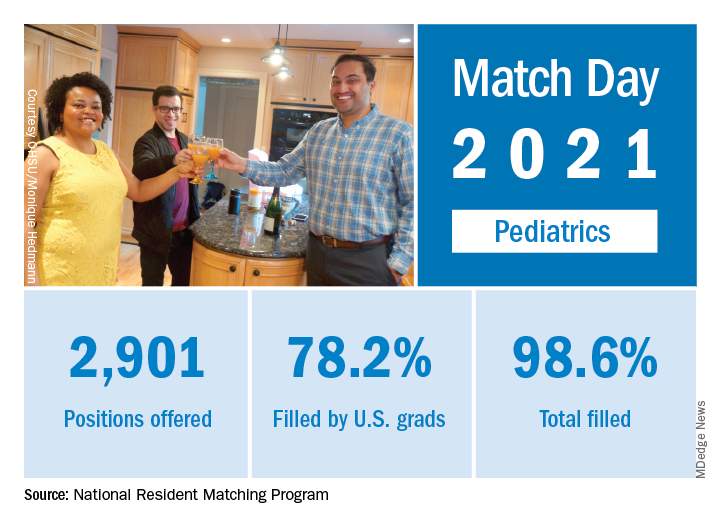
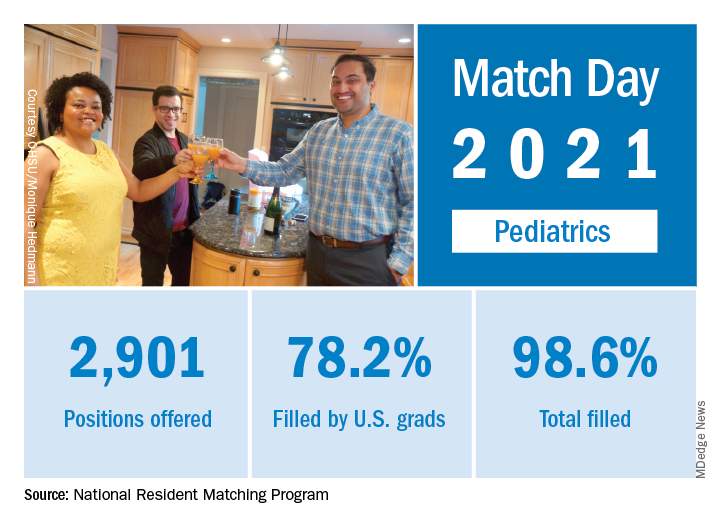
Match Day 2021: Pediatrics experiences slow, steady growth
Match Day 2021 was another record breaker, despite the pandemic, and pediatrics played its part, adding nearly 40 more slots than 2020 and filling nearly 50 more, according to the National Resident Matching Program (NRMP).
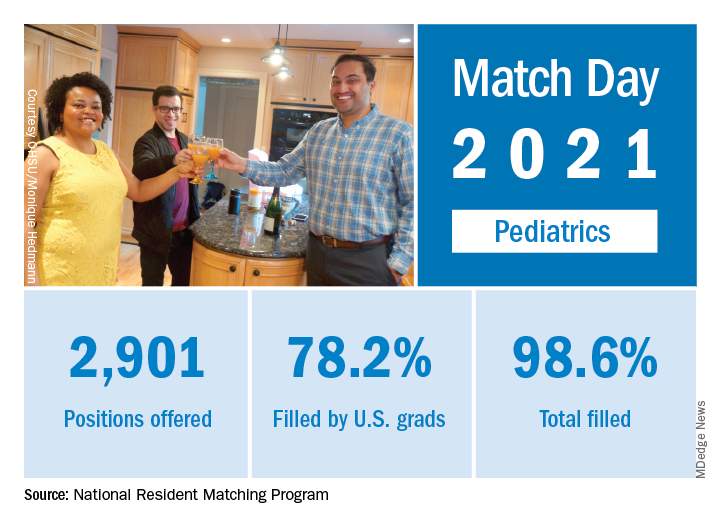
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a press release. Overall, 35,194 first-year (PGY-1) slots were offered and 33,353 were filled, both more than ever before, for a fill rate of 94.8%, a slight increase from the 94.6% fill rate last year.
Pediatrics offered 2,901 slots in 2021, up from 2,864 in 2020, though the proportion of pediatrics slots in the overall total fell slightly to 8.2% from 8.4% in 2020. Of those 2,901 slots, 2,860 were filled, for a fill rate of 98.6%, up from 98.2% last year. Of those filled positions, 60.3% were filled by MD seniors, and 78.2% were filled by U.S. graduates.
Since 2017, pediatrics has offered more slots every year, rising from 2,738 in 2017 up to the 2,901 in 2021, an overall growth rate of just under 6%.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized, [as] growth in registration was seen in every applicant group,” the NRMP noted. Rank-order lists submissions in 2021 were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen international medical graduates, and 15.0% for non–U.S.-citizen IMGs, compared with 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. ... The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in the press release.
Match Day 2021 was another record breaker, despite the pandemic, and pediatrics played its part, adding nearly 40 more slots than 2020 and filling nearly 50 more, according to the National Resident Matching Program (NRMP).
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a press release. Overall, 35,194 first-year (PGY-1) slots were offered and 33,353 were filled, both more than ever before, for a fill rate of 94.8%, a slight increase from the 94.6% fill rate last year.
Pediatrics offered 2,901 slots in 2021, up from 2,864 in 2020, though the proportion of pediatrics slots in the overall total fell slightly to 8.2% from 8.4% in 2020. Of those 2,901 slots, 2,860 were filled, for a fill rate of 98.6%, up from 98.2% last year. Of those filled positions, 60.3% were filled by MD seniors, and 78.2% were filled by U.S. graduates.
Since 2017, pediatrics has offered more slots every year, rising from 2,738 in 2017 up to the 2,901 in 2021, an overall growth rate of just under 6%.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized, [as] growth in registration was seen in every applicant group,” the NRMP noted. Rank-order lists submissions in 2021 were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen international medical graduates, and 15.0% for non–U.S.-citizen IMGs, compared with 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. ... The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in the press release.
Match Day 2021 was another record breaker, despite the pandemic, and pediatrics played its part, adding nearly 40 more slots than 2020 and filling nearly 50 more, according to the National Resident Matching Program (NRMP).
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a press release. Overall, 35,194 first-year (PGY-1) slots were offered and 33,353 were filled, both more than ever before, for a fill rate of 94.8%, a slight increase from the 94.6% fill rate last year.
Pediatrics offered 2,901 slots in 2021, up from 2,864 in 2020, though the proportion of pediatrics slots in the overall total fell slightly to 8.2% from 8.4% in 2020. Of those 2,901 slots, 2,860 were filled, for a fill rate of 98.6%, up from 98.2% last year. Of those filled positions, 60.3% were filled by MD seniors, and 78.2% were filled by U.S. graduates.
Since 2017, pediatrics has offered more slots every year, rising from 2,738 in 2017 up to the 2,901 in 2021, an overall growth rate of just under 6%.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized, [as] growth in registration was seen in every applicant group,” the NRMP noted. Rank-order lists submissions in 2021 were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen international medical graduates, and 15.0% for non–U.S.-citizen IMGs, compared with 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. ... The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in the press release.
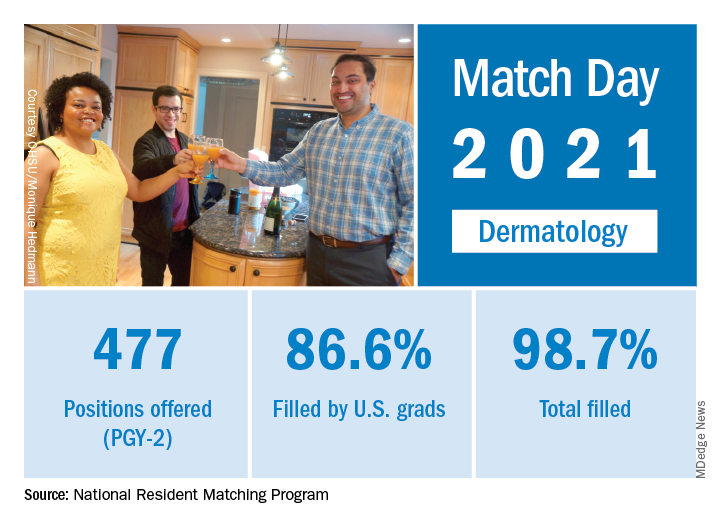
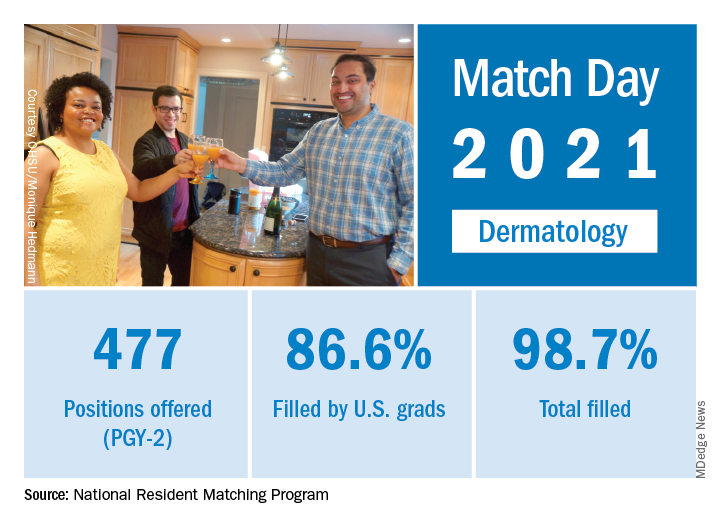
Match Day 2021: Dermatology holds steady
Despite the pandemic, , according to the National Resident Matching Program (NRMP).
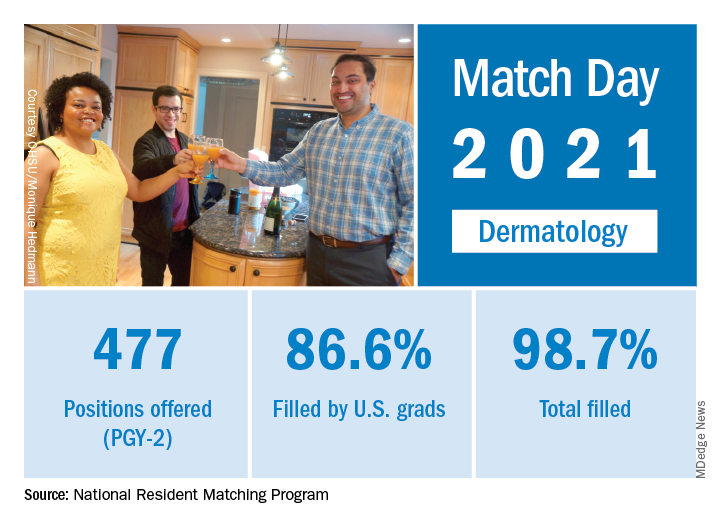
Available dermatology PGY-2 slots fell by 0.2% from 478 in 2020 to 477 in 2021, but 471 slots were filled in 2021, 2 more than last year, for an increase of 0.4%. The overall fill rate was 98.7% in 2021, with 86.6% being filled by U.S. graduates. Just under 88% of filled positions went to MD and DO seniors.
While Match Day 2021 set a record for positions offered and filled at 38,106 slots and 36,179, respectively, an overall total of 2,699 PGY-2 slots were offered in 2021, which is a decrease of 1.6% from last year’s total of 2,742 slots. Of the available PGY-2 slots, 97.6% were filled in 2021, compared with 96.6% in 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. We admire all the Match participants for their hard work and their commitment to train and serve alongside their peers. The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in a press release.
Despite the pandemic, , according to the National Resident Matching Program (NRMP).
Available dermatology PGY-2 slots fell by 0.2% from 478 in 2020 to 477 in 2021, but 471 slots were filled in 2021, 2 more than last year, for an increase of 0.4%. The overall fill rate was 98.7% in 2021, with 86.6% being filled by U.S. graduates. Just under 88% of filled positions went to MD and DO seniors.
While Match Day 2021 set a record for positions offered and filled at 38,106 slots and 36,179, respectively, an overall total of 2,699 PGY-2 slots were offered in 2021, which is a decrease of 1.6% from last year’s total of 2,742 slots. Of the available PGY-2 slots, 97.6% were filled in 2021, compared with 96.6% in 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. We admire all the Match participants for their hard work and their commitment to train and serve alongside their peers. The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in a press release.
Despite the pandemic, , according to the National Resident Matching Program (NRMP).
Available dermatology PGY-2 slots fell by 0.2% from 478 in 2020 to 477 in 2021, but 471 slots were filled in 2021, 2 more than last year, for an increase of 0.4%. The overall fill rate was 98.7% in 2021, with 86.6% being filled by U.S. graduates. Just under 88% of filled positions went to MD and DO seniors.
While Match Day 2021 set a record for positions offered and filled at 38,106 slots and 36,179, respectively, an overall total of 2,699 PGY-2 slots were offered in 2021, which is a decrease of 1.6% from last year’s total of 2,742 slots. Of the available PGY-2 slots, 97.6% were filled in 2021, compared with 96.6% in 2020.
“The NRMP is honored to have delivered a strong Match to the many applicants pursuing their dreams of medicine. We admire all the Match participants for their hard work and their commitment to train and serve alongside their peers. The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP President and CEO, said in a press release.
How family medicine has changed over the past half century
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.
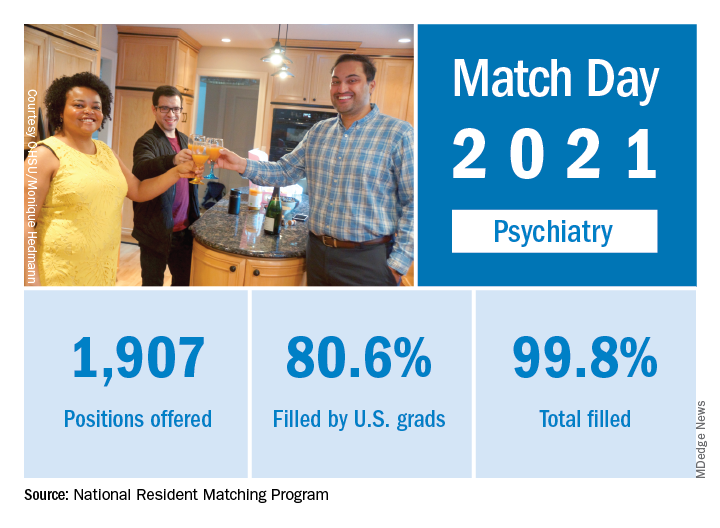
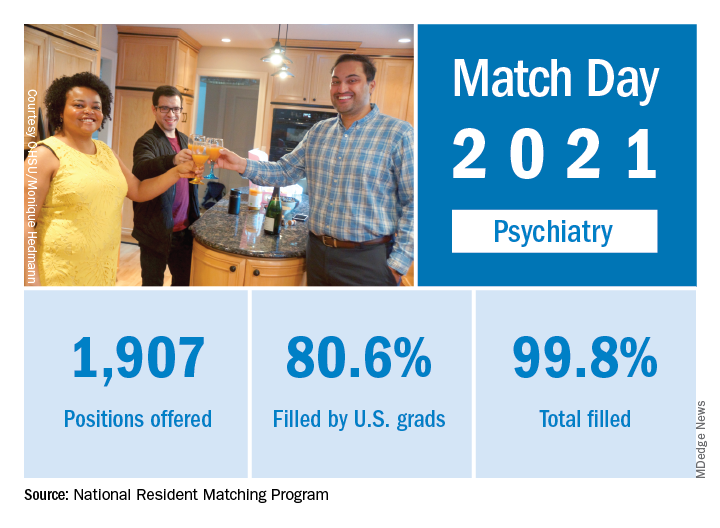
Match Day 2021: Psychiatry continues strong growth
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
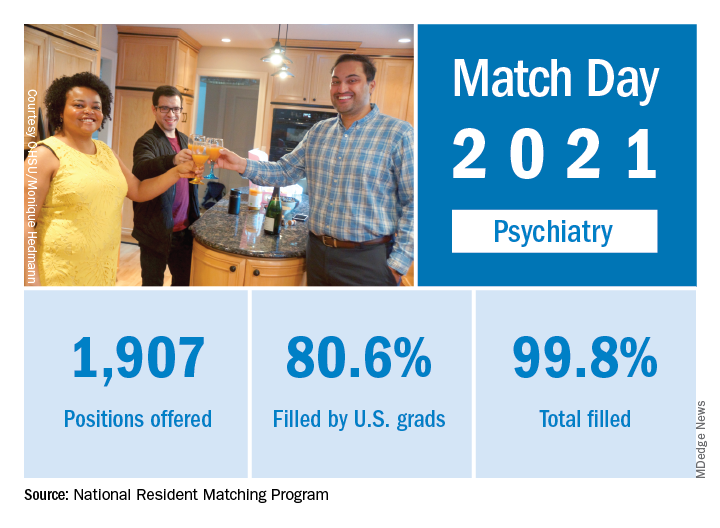
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
Dr. Richard W. Cohen joins CPN’s Editorial Advisory Board
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
2021 match sets records: Who matched and who didn’t?
A total of 38,106 positions were offered, up 850 spots (2.3%) from 2020. Of those, 35,194 were first-year (PGY-1) positions, which was 928 more than the previous year (2.7%). A record 5,915 programs were part of the Match, 88 more than 2020.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP president and CEO, said in a new release.
The report comes amid a year of Zoom interview fatigue, canceled testing, and virus fears and work-arounds, which the NMRP has never had to wrestle with since it was established in 1952.
Despite challenges, fill rates increased across the board. Of the 38,106 total positions offered, 36,179 were filled, representing a 2.6% increase over 2020. Of the 35,194 first-year positions available, 33,535 were filled, representing a 2.9% increase.
Those rates drove the percentage of all positions filled to 94.9% (up from 94.6%) and the percentage of PGY-1 positions filled to 94.8% (also up from 94.6%). There were 1,927 unfilled positions, a decline of 71 (3.6%) from 2020.
Primary care results strong
Of the first-year positions offered, 17,649 (49.6%) were in family medicine, internal medicine, and pediatrics. That’s an increase of 514 positions (3%) over 2020.
Of first-year positions offered in 2021, 16,860 (95.5%) were filled. U.S. seniors took 11,013 (65.3%) of those slots; that represents a slight decline (0.3%) from 2020. Family medicine saw a gain of 63 U.S. MD seniors who matched, and internal medicine saw a gain of 93 U.S. DO seniors who matched.
Some specialties filled all positions
PGY-1 specialties with 30 positions or more that filled all available positions include dermatology, medicine – emergency medicine, medicine – pediatrics, neurologic surgery, otolaryngology, integrated plastic surgery, and vascular surgery.*
PGY-1 specialties with 30 positions or more that filled more than 90% with U.S. seniors include dermatology (100%), medicine – emergency medicine (93.6%), medicine – pediatrics (93.5%), otolaryngology (93.2%), orthopedic surgery (92.8%), and integrated plastic surgery (90.4%).*
PGY-1 specialties with at least 30 positions that filled less than 50% with U.S. seniors include pathology (41.4 %) and surgery–preliminary (28%).
The number of U.S. citizen international medical graduates who submitted rank-ordered lists was 5,295, an increase of 128 (2.5%) over 2020 and the highest in 6 years; 3,152 of them matched to first-year positions, down two PGY-1 matched applicants over last year.
Full data are available on the NRMP’s website.
Correction, 3/22/21: An earlier version of this article misstated the affected specialties.
A version of this article first appeared on Medscape.com.
A total of 38,106 positions were offered, up 850 spots (2.3%) from 2020. Of those, 35,194 were first-year (PGY-1) positions, which was 928 more than the previous year (2.7%). A record 5,915 programs were part of the Match, 88 more than 2020.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP president and CEO, said in a new release.
The report comes amid a year of Zoom interview fatigue, canceled testing, and virus fears and work-arounds, which the NMRP has never had to wrestle with since it was established in 1952.
Despite challenges, fill rates increased across the board. Of the 38,106 total positions offered, 36,179 were filled, representing a 2.6% increase over 2020. Of the 35,194 first-year positions available, 33,535 were filled, representing a 2.9% increase.
Those rates drove the percentage of all positions filled to 94.9% (up from 94.6%) and the percentage of PGY-1 positions filled to 94.8% (also up from 94.6%). There were 1,927 unfilled positions, a decline of 71 (3.6%) from 2020.
Primary care results strong
Of the first-year positions offered, 17,649 (49.6%) were in family medicine, internal medicine, and pediatrics. That’s an increase of 514 positions (3%) over 2020.
Of first-year positions offered in 2021, 16,860 (95.5%) were filled. U.S. seniors took 11,013 (65.3%) of those slots; that represents a slight decline (0.3%) from 2020. Family medicine saw a gain of 63 U.S. MD seniors who matched, and internal medicine saw a gain of 93 U.S. DO seniors who matched.
Some specialties filled all positions
PGY-1 specialties with 30 positions or more that filled all available positions include dermatology, medicine – emergency medicine, medicine – pediatrics, neurologic surgery, otolaryngology, integrated plastic surgery, and vascular surgery.*
PGY-1 specialties with 30 positions or more that filled more than 90% with U.S. seniors include dermatology (100%), medicine – emergency medicine (93.6%), medicine – pediatrics (93.5%), otolaryngology (93.2%), orthopedic surgery (92.8%), and integrated plastic surgery (90.4%).*
PGY-1 specialties with at least 30 positions that filled less than 50% with U.S. seniors include pathology (41.4 %) and surgery–preliminary (28%).
The number of U.S. citizen international medical graduates who submitted rank-ordered lists was 5,295, an increase of 128 (2.5%) over 2020 and the highest in 6 years; 3,152 of them matched to first-year positions, down two PGY-1 matched applicants over last year.
Full data are available on the NRMP’s website.
Correction, 3/22/21: An earlier version of this article misstated the affected specialties.
A version of this article first appeared on Medscape.com.
A total of 38,106 positions were offered, up 850 spots (2.3%) from 2020. Of those, 35,194 were first-year (PGY-1) positions, which was 928 more than the previous year (2.7%). A record 5,915 programs were part of the Match, 88 more than 2020.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” Donna L. Lamb, DHSc, MBA, BSN, NRMP president and CEO, said in a new release.
The report comes amid a year of Zoom interview fatigue, canceled testing, and virus fears and work-arounds, which the NMRP has never had to wrestle with since it was established in 1952.
Despite challenges, fill rates increased across the board. Of the 38,106 total positions offered, 36,179 were filled, representing a 2.6% increase over 2020. Of the 35,194 first-year positions available, 33,535 were filled, representing a 2.9% increase.
Those rates drove the percentage of all positions filled to 94.9% (up from 94.6%) and the percentage of PGY-1 positions filled to 94.8% (also up from 94.6%). There were 1,927 unfilled positions, a decline of 71 (3.6%) from 2020.
Primary care results strong
Of the first-year positions offered, 17,649 (49.6%) were in family medicine, internal medicine, and pediatrics. That’s an increase of 514 positions (3%) over 2020.
Of first-year positions offered in 2021, 16,860 (95.5%) were filled. U.S. seniors took 11,013 (65.3%) of those slots; that represents a slight decline (0.3%) from 2020. Family medicine saw a gain of 63 U.S. MD seniors who matched, and internal medicine saw a gain of 93 U.S. DO seniors who matched.
Some specialties filled all positions
PGY-1 specialties with 30 positions or more that filled all available positions include dermatology, medicine – emergency medicine, medicine – pediatrics, neurologic surgery, otolaryngology, integrated plastic surgery, and vascular surgery.*
PGY-1 specialties with 30 positions or more that filled more than 90% with U.S. seniors include dermatology (100%), medicine – emergency medicine (93.6%), medicine – pediatrics (93.5%), otolaryngology (93.2%), orthopedic surgery (92.8%), and integrated plastic surgery (90.4%).*
PGY-1 specialties with at least 30 positions that filled less than 50% with U.S. seniors include pathology (41.4 %) and surgery–preliminary (28%).
The number of U.S. citizen international medical graduates who submitted rank-ordered lists was 5,295, an increase of 128 (2.5%) over 2020 and the highest in 6 years; 3,152 of them matched to first-year positions, down two PGY-1 matched applicants over last year.
Full data are available on the NRMP’s website.
Correction, 3/22/21: An earlier version of this article misstated the affected specialties.
A version of this article first appeared on Medscape.com.
Price transparency comes to medicine
There is a Chinese curse which says “May he live in interesting times.” Like it or not, we live in interesting times. They are times of danger and uncertainty; but they are also more open to the creative energy of men than any other time in history.
–Robert Kennedy, Cape Town, South Africa, 1966
Well, you may not know it, but price transparency is coming to medicine, including dermatology. . It has survived a challenge by the American Hospital Association in federal court, which generally means it is going to “stick.” Its effects should start to appear on Jan. 1, 2022.
The newly finalized rule will require insurers to publicly disclose in-network provider-negotiated rates, historical out-of-network allowed amounts, associated facility fees, and drug-pricing information in easily accessible machine-readable files. This information will be disclosed for the 500 most commonly billed physician services starting Jan. 1, 2022, and expanded to include all services the following year. Understand that you, as a practitioner, do not have to do anything, as insurers will do it for you, but your charge data will be on display. It is not clear if there is an appeal mechanism for physicians to correct erroneous data.
This should provide a fascinating look at just what things really cost, and may prove, as we suspect, small practices are less expensive. Important exemptions to reporting include emergency services, anesthesia, lab tests, and pathology fees, which will not be required, but recommended, to be disclosed.
Bear in mind that this rule was not designed to benefit physicians or hospitals, but rather to allow patients to comparison shop and drive down the cost of medical care. True price transparency may well accomplish this, particularly in our age of sky-high deductibles, if the information is accurate and readily accessible.
Although studies of patient behavior have shown that few patients actually use price comparison tools, the data required to be publicly disclosed and accessible will make this much easier. The Wall Street Journal or ProPublica will likely be all over this with applications to make comparisons easier. Still, many patients are price insensitive, particularly if they are Medicare recipients and only responsible for a nominal deductible.
Almost all the evaluation and management codes, as well as many dermatology procedure codes, are listed in the top 500 items and services included in the initial stage of the finalized rule. These include skin biopsies, destructions, drainages, several different benign and malignant excisions and, of course, Mohs surgery (but only the first stage, the 2nd stage will be listed in 2023).
While it is unlikely for patients to doctor shop for services that are performed on the same day as the office visit, such as a biopsies or destructions, we would expect comparisons for more expensive, planned procedures such as Mohs surgery and cancer excisions. Considering the rule, Mohs surgery may compare favorably to excisions performed in the hospital if the operating room charges are included, but not so well if the pathology and anesthesia charges are not included in the cost. It is inherently unfair to compare Mohs to excision in an operating room since the Mohs procedure has the anesthesia and pathology work embedded in the code (at 55% of the value of the code), and the multiple frozen sections taken by the surgeon in the operating room will not be listed as they are technically considered to be exempt additional pathology services.
This could put the Mohs surgeon in the interesting position of billing for excisions and frozen sections instead of Mohs surgery in order to compete with the hospital-based surgeon. This is not unbundling, if overall charges are lower and if distinctly different procedures are followed and different paperwork is generated. This is how I currently handle patients who demand Mohs surgery for inappropriate sites.
The effect on hospital groups that can charge facility fees could be quite dramatic, as it could be on large groups and on private equity groups who may have negotiated better rates. These increased costs will be revealed to consumers. In January 2023, the insurers will have to deploy a tool on their web site, updated monthly, that details rates for the 500 most common procedures for all in- and out-of-network providers and how much the patient can expect to pay out of pocket. All facility fees for procedures will be included. As noted earlier, we would expect third parties to already have done this. The historical and current costs for medications will also be included, which should make for interesting times in the pharmaceutical industry.
In January 2024, insurers will be required to post all the additional codes they cover, including complex closures, flaps, and grafts and any associated facility fees. Of course, a patient or a surgeon does not know what sort of repair a patient will need after Mohs surgery, but with high deductibles hitting harder, we would expect more patients requesting healing by second intent.
Whether these price comparisons will drive patients from relatively high-cost centers to less costly ones is unclear. This has certainly been the case for MRI and CT imaging. Price transparency for MRIs increased use of less costly providers and triggered provider competition.
Whether the price differentials will allow smaller practices some leverage in negotiating rates is also uncertain. Who knows, perhaps the out-of-network rate is greater than what your contract currently specifies, which could spur you to drop their network entirely. There may be great opportunity here for the smaller practitioner who has been boxed out of the big-group pricing and networks.
Be prepared in January 2022, to discuss these issues with patients and insurers, and be sure to check where you fall in cost comparisons. What possible logic could an insurer have for excluding you from a network where your average charges are less than their current panel? As noted before, this may be a boon for small practices that have been forced to the fringes of reimbursement and an opportunity to demonstrate that they are really much less expensive. We live in interesting times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Bishop is doing a fellowship in micrographic surgery and dermatologic oncology with Dr. Coldiron at the Skin Cancer Center in Cincinnati. Write to Dr. Coldiron at [email protected].
There is a Chinese curse which says “May he live in interesting times.” Like it or not, we live in interesting times. They are times of danger and uncertainty; but they are also more open to the creative energy of men than any other time in history.
–Robert Kennedy, Cape Town, South Africa, 1966
Well, you may not know it, but price transparency is coming to medicine, including dermatology. . It has survived a challenge by the American Hospital Association in federal court, which generally means it is going to “stick.” Its effects should start to appear on Jan. 1, 2022.
The newly finalized rule will require insurers to publicly disclose in-network provider-negotiated rates, historical out-of-network allowed amounts, associated facility fees, and drug-pricing information in easily accessible machine-readable files. This information will be disclosed for the 500 most commonly billed physician services starting Jan. 1, 2022, and expanded to include all services the following year. Understand that you, as a practitioner, do not have to do anything, as insurers will do it for you, but your charge data will be on display. It is not clear if there is an appeal mechanism for physicians to correct erroneous data.
This should provide a fascinating look at just what things really cost, and may prove, as we suspect, small practices are less expensive. Important exemptions to reporting include emergency services, anesthesia, lab tests, and pathology fees, which will not be required, but recommended, to be disclosed.
Bear in mind that this rule was not designed to benefit physicians or hospitals, but rather to allow patients to comparison shop and drive down the cost of medical care. True price transparency may well accomplish this, particularly in our age of sky-high deductibles, if the information is accurate and readily accessible.
Although studies of patient behavior have shown that few patients actually use price comparison tools, the data required to be publicly disclosed and accessible will make this much easier. The Wall Street Journal or ProPublica will likely be all over this with applications to make comparisons easier. Still, many patients are price insensitive, particularly if they are Medicare recipients and only responsible for a nominal deductible.
Almost all the evaluation and management codes, as well as many dermatology procedure codes, are listed in the top 500 items and services included in the initial stage of the finalized rule. These include skin biopsies, destructions, drainages, several different benign and malignant excisions and, of course, Mohs surgery (but only the first stage, the 2nd stage will be listed in 2023).
While it is unlikely for patients to doctor shop for services that are performed on the same day as the office visit, such as a biopsies or destructions, we would expect comparisons for more expensive, planned procedures such as Mohs surgery and cancer excisions. Considering the rule, Mohs surgery may compare favorably to excisions performed in the hospital if the operating room charges are included, but not so well if the pathology and anesthesia charges are not included in the cost. It is inherently unfair to compare Mohs to excision in an operating room since the Mohs procedure has the anesthesia and pathology work embedded in the code (at 55% of the value of the code), and the multiple frozen sections taken by the surgeon in the operating room will not be listed as they are technically considered to be exempt additional pathology services.
This could put the Mohs surgeon in the interesting position of billing for excisions and frozen sections instead of Mohs surgery in order to compete with the hospital-based surgeon. This is not unbundling, if overall charges are lower and if distinctly different procedures are followed and different paperwork is generated. This is how I currently handle patients who demand Mohs surgery for inappropriate sites.
The effect on hospital groups that can charge facility fees could be quite dramatic, as it could be on large groups and on private equity groups who may have negotiated better rates. These increased costs will be revealed to consumers. In January 2023, the insurers will have to deploy a tool on their web site, updated monthly, that details rates for the 500 most common procedures for all in- and out-of-network providers and how much the patient can expect to pay out of pocket. All facility fees for procedures will be included. As noted earlier, we would expect third parties to already have done this. The historical and current costs for medications will also be included, which should make for interesting times in the pharmaceutical industry.
In January 2024, insurers will be required to post all the additional codes they cover, including complex closures, flaps, and grafts and any associated facility fees. Of course, a patient or a surgeon does not know what sort of repair a patient will need after Mohs surgery, but with high deductibles hitting harder, we would expect more patients requesting healing by second intent.
Whether these price comparisons will drive patients from relatively high-cost centers to less costly ones is unclear. This has certainly been the case for MRI and CT imaging. Price transparency for MRIs increased use of less costly providers and triggered provider competition.
Whether the price differentials will allow smaller practices some leverage in negotiating rates is also uncertain. Who knows, perhaps the out-of-network rate is greater than what your contract currently specifies, which could spur you to drop their network entirely. There may be great opportunity here for the smaller practitioner who has been boxed out of the big-group pricing and networks.
Be prepared in January 2022, to discuss these issues with patients and insurers, and be sure to check where you fall in cost comparisons. What possible logic could an insurer have for excluding you from a network where your average charges are less than their current panel? As noted before, this may be a boon for small practices that have been forced to the fringes of reimbursement and an opportunity to demonstrate that they are really much less expensive. We live in interesting times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Bishop is doing a fellowship in micrographic surgery and dermatologic oncology with Dr. Coldiron at the Skin Cancer Center in Cincinnati. Write to Dr. Coldiron at [email protected].
There is a Chinese curse which says “May he live in interesting times.” Like it or not, we live in interesting times. They are times of danger and uncertainty; but they are also more open to the creative energy of men than any other time in history.
–Robert Kennedy, Cape Town, South Africa, 1966
Well, you may not know it, but price transparency is coming to medicine, including dermatology. . It has survived a challenge by the American Hospital Association in federal court, which generally means it is going to “stick.” Its effects should start to appear on Jan. 1, 2022.
The newly finalized rule will require insurers to publicly disclose in-network provider-negotiated rates, historical out-of-network allowed amounts, associated facility fees, and drug-pricing information in easily accessible machine-readable files. This information will be disclosed for the 500 most commonly billed physician services starting Jan. 1, 2022, and expanded to include all services the following year. Understand that you, as a practitioner, do not have to do anything, as insurers will do it for you, but your charge data will be on display. It is not clear if there is an appeal mechanism for physicians to correct erroneous data.
This should provide a fascinating look at just what things really cost, and may prove, as we suspect, small practices are less expensive. Important exemptions to reporting include emergency services, anesthesia, lab tests, and pathology fees, which will not be required, but recommended, to be disclosed.
Bear in mind that this rule was not designed to benefit physicians or hospitals, but rather to allow patients to comparison shop and drive down the cost of medical care. True price transparency may well accomplish this, particularly in our age of sky-high deductibles, if the information is accurate and readily accessible.
Although studies of patient behavior have shown that few patients actually use price comparison tools, the data required to be publicly disclosed and accessible will make this much easier. The Wall Street Journal or ProPublica will likely be all over this with applications to make comparisons easier. Still, many patients are price insensitive, particularly if they are Medicare recipients and only responsible for a nominal deductible.
Almost all the evaluation and management codes, as well as many dermatology procedure codes, are listed in the top 500 items and services included in the initial stage of the finalized rule. These include skin biopsies, destructions, drainages, several different benign and malignant excisions and, of course, Mohs surgery (but only the first stage, the 2nd stage will be listed in 2023).
While it is unlikely for patients to doctor shop for services that are performed on the same day as the office visit, such as a biopsies or destructions, we would expect comparisons for more expensive, planned procedures such as Mohs surgery and cancer excisions. Considering the rule, Mohs surgery may compare favorably to excisions performed in the hospital if the operating room charges are included, but not so well if the pathology and anesthesia charges are not included in the cost. It is inherently unfair to compare Mohs to excision in an operating room since the Mohs procedure has the anesthesia and pathology work embedded in the code (at 55% of the value of the code), and the multiple frozen sections taken by the surgeon in the operating room will not be listed as they are technically considered to be exempt additional pathology services.
This could put the Mohs surgeon in the interesting position of billing for excisions and frozen sections instead of Mohs surgery in order to compete with the hospital-based surgeon. This is not unbundling, if overall charges are lower and if distinctly different procedures are followed and different paperwork is generated. This is how I currently handle patients who demand Mohs surgery for inappropriate sites.
The effect on hospital groups that can charge facility fees could be quite dramatic, as it could be on large groups and on private equity groups who may have negotiated better rates. These increased costs will be revealed to consumers. In January 2023, the insurers will have to deploy a tool on their web site, updated monthly, that details rates for the 500 most common procedures for all in- and out-of-network providers and how much the patient can expect to pay out of pocket. All facility fees for procedures will be included. As noted earlier, we would expect third parties to already have done this. The historical and current costs for medications will also be included, which should make for interesting times in the pharmaceutical industry.
In January 2024, insurers will be required to post all the additional codes they cover, including complex closures, flaps, and grafts and any associated facility fees. Of course, a patient or a surgeon does not know what sort of repair a patient will need after Mohs surgery, but with high deductibles hitting harder, we would expect more patients requesting healing by second intent.
Whether these price comparisons will drive patients from relatively high-cost centers to less costly ones is unclear. This has certainly been the case for MRI and CT imaging. Price transparency for MRIs increased use of less costly providers and triggered provider competition.
Whether the price differentials will allow smaller practices some leverage in negotiating rates is also uncertain. Who knows, perhaps the out-of-network rate is greater than what your contract currently specifies, which could spur you to drop their network entirely. There may be great opportunity here for the smaller practitioner who has been boxed out of the big-group pricing and networks.
Be prepared in January 2022, to discuss these issues with patients and insurers, and be sure to check where you fall in cost comparisons. What possible logic could an insurer have for excluding you from a network where your average charges are less than their current panel? As noted before, this may be a boon for small practices that have been forced to the fringes of reimbursement and an opportunity to demonstrate that they are really much less expensive. We live in interesting times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Dr. Bishop is doing a fellowship in micrographic surgery and dermatologic oncology with Dr. Coldiron at the Skin Cancer Center in Cincinnati. Write to Dr. Coldiron at [email protected].
Let’s not criticize off-label prescribing
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.
The public health crisis sparked by COVID-19 has engendered much debate in the realm where politics, journalism, law, and medicine meet.
Doctors have used the media to name other doctors as sources of harmful misinformation, in some cases going so far as to invoke medical practice board oversight as a potential intervention when doctors make public statements deemed too far out of bounds scientifically. Over the past year, some physicians have been harshly criticized for speaking about off-label prescribing, a widely accepted part of everyday medical practice.
The science and ethics of off-label prescribing have not changed; what has changed is the quality of dialogue around it. As psychiatrists, it does not fall within our scope of practice to offer definitive public opinions on the treatment of COVID-19, nor is that our purpose here. However, we can speak to a process that damages patients and doctors alike by undermining trust. All of this heat around bad medical information, in our opinion, amounts to using the methods of other fields to evaluate science and clinical practice. A remedy, then, to improve the quality of public medical intelligence would be to clarify the rules of scientific debate and to once again clearly state that off-label prescribing is part and parcel of the good practice of clinical medicine.
Physicians who work in the field of professional discipline have thought about the limits of propriety in making charges of impropriety. We (R.S.E. and R.S.K.) asked the American Psychiatric Association’s Ethics Committee to expand upon its existing commentary on innovative practice and making allegations of professional misconduct. We used the committee’s answers to our questions as the basis for the arguments we are making in this piece.
The APA’s Ethics Committee uses clear-cut benchmarks to define innovative medical care: “The standards of care ... evolve with evidence from research and observations of practice. Among the expected supports for innovative practice are scientific testing, peer-reviewed publication, replication, and broad or widespread acceptance within a relevant scientific or professional community.” When it comes to off-label prescribing for any medical condition, it is easy enough to ascertain whether clinical reports have appeared in peer-reviewed journals.
Two of the biggest blockbusters in psychiatry, chlorpromazine and lithium, began as drugs used for other conditions almost since the inception of our field. In other words, the use of these drugs for mental illness began, in today’s jargon, as off-label. We practitioners of psychiatry live in the land of off-label prescribing and have always comfortably done so. In fact, almost all of medicine does. The key in today’s world of best-practice medicine is obtaining a truly informed consent.
For COVID-19, our incredible psychotropic molecules may once again be doing some trail-blazing off-label work. Late last year, Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University in St. Louis, reported in a preliminary study of adult outpatients with symptomatic COVID-19 that those treated with fluvoxamine “had a lower likelihood of clinical deterioration over 15 days,” compared with those on placebo (JAMA. 2020;324[22]:2292-300). We were heartened to see Dr. Lenze discuss his work on a recent “60 Minutes” segment. David Seftel, MD, MBA, a clinician who administered fluvoxamine as early treatment for a COVID-19 outbreak that occurred in a community of racetrack employees and their families in the San Francisco Bay Area, also was featured. Rather than waiting for the results of large clinical trials, Dr. Lenze and Dr. Seftel proceeded, based on reports published in peer-reviewed journals, to treat patients whose lives were at risk.
If we find ourselves strongly disagreeing about the science of off-label prescribing, the proper response is to critique methodologies, not the character or competence of colleagues. The APA Ethics Committee discourages use of the media as a forum for making allegations of incompetent or unethical practice: “Judgments regarding violations of established norms of ethical or professional conduct should be made not by individuals but by bodies authorized to take evidence and make informed decisions.”
At least one state legislature is taking action to protect patients’ access to the doctors they trust. In Arizona, SB 1416 passed in the Senate and is now working its way through the House. This bill would prohibit medical boards from disciplining doctors for speaking out about or prescribing off-label drugs when a reasonable basis for use exists.
Psychological research on the “backfire effect” suggests that heavy-handed campaigns to enforce medical consensus will only harden minds in ways that neither advance science nor improve the quality of clinical decision-making.
Medical disciplinary boards and the news media were neither designed nor are they equipped to adjudicate scientific debates. Science is never settled: Hypothesis and theory are always open to testing and revision as new evidence emerges. There is a place in medicine for formal disciplinary processes, as well-delineated by professional bodies such as the APA Ethics Committee. Another important part of protecting the public is to support an environment of scientific inquiry in which diversity of opinion is welcomed. As physicians, we translate science into excellent clinical care every day in our practices, and we advance science by sharing what we learn through friendly collegial communication and collaboration.
Dr. Emmons is part-time clinical associate professor in the department of psychiatry at the University of Vermont, Burlington, and is a past chair of the Ethics Committee for the Vermont District Branch of the American Psychiatric Association. He is in private practice in Moretown, Vt., and disclosed no relevant financial relationships. Dr. Kohanski is in private practice in Dayton, N.J., and is a diplomate of the American Board of Psychiatry & Neurology. She also is the host and author of Clinical Correlation, a series of the Psychcast. Dr. Kohanski disclosed no relevant financial relationships.