User login
Applying lessons from Oprah to your practice
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
In my last column, I explained how I’m like Tom Brady. I’m not really. Brady is a Super Bowl–winning quarterback worth over $200 million. No, I’m like Oprah. Well, trying anyway.
Brady and Oprah, in addition to being gazillionaires, have in common that they’re arguably the GOATs (Greatest Of All Time) in their fields. Watching Oprah interview Meghan Markle and Prince Harry was like watching Tom Brady on the jumbotron – she made it look easy. Her ability to create conversation and coax information from guests is hall-of-fame good. But although they are both admirable, trying to be like Brady is useful only for next Thanksgiving when you’re trying to beat your cousins from Massachusetts in touch football. .
1. Prepare ahead. It’s clear that Oprah has binders of notes about her guests and thoroughly reviewed them before she invites them to sit down. We should do the same. Open the chart and read as much as you can before you open the door. Have important information in your head so you don’t have to break from your interview to refer to it.
2. Sprinkle pleasantry. She’d never start an interview with: So why are you here? Nor should we. Even one nonscripted question or comment can help build a little rapport before getting to the work.
3. Be brief. Oprah gets her question out fast, then gets out of the way. And as a bonus, this is the easiest place to shave a few minutes from your appointments from your own end. Think for a second before you speak and try to find the shortest route to your question. Try to keep your questions to just a sentence or two.
4. Stay on it. Once you’ve discovered something relevant, stay with it, resisting the urge to finish the review of symptoms. This is not just to make a diagnosis, but as importantly, trying to diagnose “the real reason” for the visit. Then, when the question is done, own the transition. Oprah uses: “Let’s move on.” This is a bit abrupt for us, but it can be helpful if used sparingly and gently. I might soften this a little by adding “I want to be sure we have enough time to get through everything for you.”
5. Wait. A few seconds seems an eternity on the air (and in clinic), but sometimes the silent pause is just what’s needed to help the patient expand and share.
6. Be nonjudgmental. Most of us believe we’re pretty good at this, yet, it’s sometimes a blind spot. It’s easy to blame the obese patient for his stasis dermatitis or the hidradenitis patient who hasn’t stop smoking for her cysts. It also helps to be nontransactional. If you make patients feel that you’re asking questions only to extract information, you’ll never reach Oprah level.
7. Be in the moment. It is difficult, but when possible, avoid typing notes while you’re still interviewing. We’re not just there to get the facts, we’re also trying to get the story and that sometimes takes really listening.
I’m no more like Oprah than Brady, of course. But it is more fun to close my eyes and imagine myself being her when I see my next patient. That is, until Thanksgiving. Watch out, Bedards from Attleboro.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Survey explores impact of pandemic on dermatologist happiness, burnout
, according to Medscape’s 2021 Dermatologist Lifestyle, Happiness & Burnout Report.
In addition, 15% reported being burned out, and 3% reported being depressed, yet about half reported being too busy to seek help for burnout and/or depression.
Those are among the key findings from the Medscape report, which was published online on Feb. 19, 2021. More than 12,000 physicians from 29 specialties, including dermatology, participated in the survey, which explores how physicians are coping with burnout, maintaining their personal wellness, and viewing their workplaces and futures amid the COVID-19 pandemic.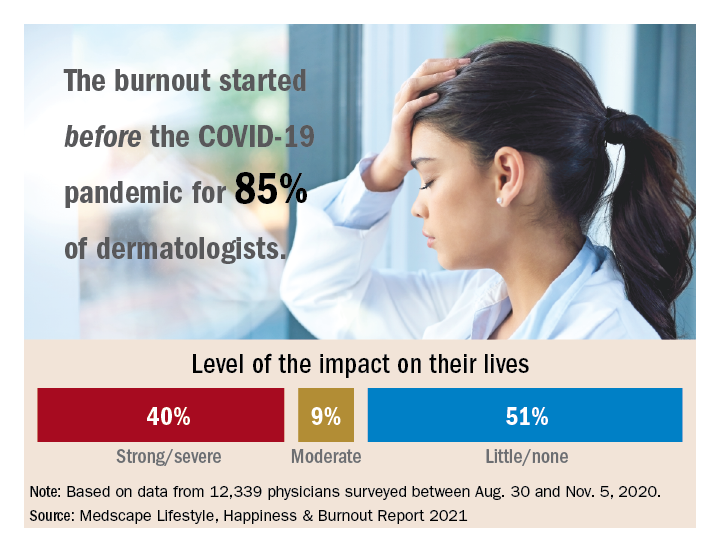
Among dermatologists who reported burnout, 85% said that it started prior to the pandemic, but 15% said it began with the pandemic. That finding resonates with Diane L. Whitaker-Worth, MD, a dermatologist with the University of Connecticut Health Center, Farmington. “A lot of dermatology practices closed down for a while, which was a huge economic hit,” she said in an interview. “I work for a university, so the stress wasn’t quite as bad. We shut down for about a week, but we canceled a lot of visits. We ramped up quickly, and I would say by the summer more people were coming in. Then we got backlogged. We’re still drowning in the number of patients who want to get in sooner, who can’t get an appointment, who need to be seen. It’s unbelievable, and it’s unrelenting.”
Dermatology trainees were also upended, with many residency programs going virtual. “We had to quickly figure out how to continue educating our residents,” said Dr. Whitaker-Worth, who also directs the university’s dermatology residency program. “What’s reasonable to expect them to be doing in clinic? There were fears about becoming infected [with the] virus. Every week, I had double the amount of work in the bureaucratic realm, trying to figure out how we run our clinic and keep our residents safe but learning. That was hard and the residents were really stressed. They were afraid they were going to get pulled to the ICUs. At that time, we didn’t have adequate PPE, and patients and doctors were dying.”
According to the dermatologists who responded to the Medscape survey and reported burnout, the seven chief contributors to burnout were too many bureaucratic tasks (70%); increasing computerization of practice (47%); insufficient compensation/reimbursement (31%); lack of respect from patients (27%); government regulations (26%); lack of respect from administrators/employers, colleagues, or staff (23%); and stress from social distancing/societal issues related to COVID-19 (15%).
“Even though dermatologists seemingly have such a nice schedule, compared to a lot of other doctors, it’s still a very stressful occupation,” said Dr. Whitaker-Worth, who coauthored a study on the topic of burnout among female dermatologists. “It is harder to practice now because there are so many people telling us how we have to do things. That will burn you out over time, when control is taken away, when tasks are handed to you randomly by different entities – insurance companies, the government, the electronic medical record.”
Among dermatologists who self-reported burnout on the survey, 51% said it had no impact on their life, 9% said the impact was moderate, while 40% indicated that it had a strong/severe impact. About half (49%) use exercise to cope with burnout, while other key coping strategies include talking with family members/close friends (40%), playing or listening to music (39%), isolating themselves from others (35%), eating junk food (35%), and drinking alcohol (30%). At the same time, only 6% indicated that they are currently seeking professional health for their burnout and/or depression, and 3% indicated that they are planning to seek professional help. When asked why they hadn’t sought help for their burnout and/or depression, 51% of respondents said they were too busy and 36% said their symptoms weren’t severe enough.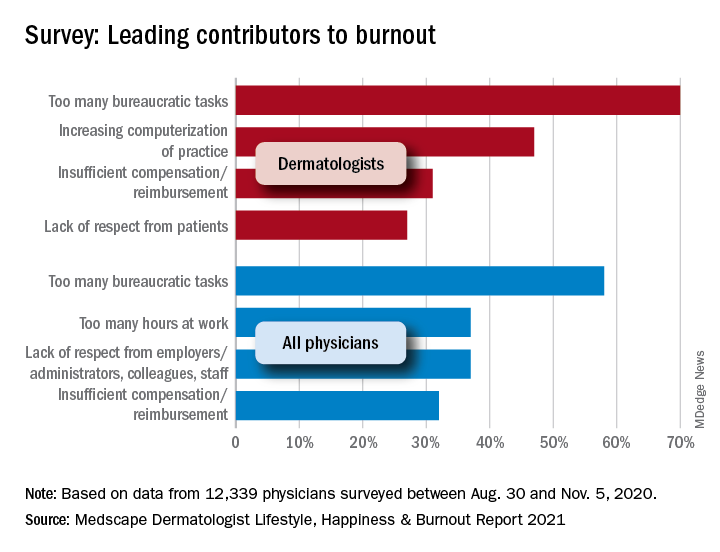
Dr. Whitaker-Worth characterized bureaucratic tasks as “a huge cause” of her burnout, but the larger contributor, she said, is managing her role as wife and mother of four children who are currently at home attending online school classes or working remotely, while she juggles her own work responsibilities. “They were stressed,” she said of her children. “The whole world was stressed. There are exceptions, but I still think that women are mostly shouldering the tasks at home. Even if they’re not doing them, they’re still feeling responsible for them. During the pandemic, every aspect of life became harder. Work was harder. Getting kids focused on school was harder. Doing basic tasks like errands was harder.”
Despite the stress and uncertainty generated by the pandemic, Dr. Whitaker-Worth considers dermatology as one of the happier specialties in medicine. “We still have a little more control of our time,” she said. “We are lucky in that we have reasonable hours, not as much in-house call, and a little more control over our day. I think work-life balance is the main thing that drives burnout – over bureaucracy, over everything.”
, according to Medscape’s 2021 Dermatologist Lifestyle, Happiness & Burnout Report.
In addition, 15% reported being burned out, and 3% reported being depressed, yet about half reported being too busy to seek help for burnout and/or depression.
Those are among the key findings from the Medscape report, which was published online on Feb. 19, 2021. More than 12,000 physicians from 29 specialties, including dermatology, participated in the survey, which explores how physicians are coping with burnout, maintaining their personal wellness, and viewing their workplaces and futures amid the COVID-19 pandemic.
Among dermatologists who reported burnout, 85% said that it started prior to the pandemic, but 15% said it began with the pandemic. That finding resonates with Diane L. Whitaker-Worth, MD, a dermatologist with the University of Connecticut Health Center, Farmington. “A lot of dermatology practices closed down for a while, which was a huge economic hit,” she said in an interview. “I work for a university, so the stress wasn’t quite as bad. We shut down for about a week, but we canceled a lot of visits. We ramped up quickly, and I would say by the summer more people were coming in. Then we got backlogged. We’re still drowning in the number of patients who want to get in sooner, who can’t get an appointment, who need to be seen. It’s unbelievable, and it’s unrelenting.”
Dermatology trainees were also upended, with many residency programs going virtual. “We had to quickly figure out how to continue educating our residents,” said Dr. Whitaker-Worth, who also directs the university’s dermatology residency program. “What’s reasonable to expect them to be doing in clinic? There were fears about becoming infected [with the] virus. Every week, I had double the amount of work in the bureaucratic realm, trying to figure out how we run our clinic and keep our residents safe but learning. That was hard and the residents were really stressed. They were afraid they were going to get pulled to the ICUs. At that time, we didn’t have adequate PPE, and patients and doctors were dying.”
According to the dermatologists who responded to the Medscape survey and reported burnout, the seven chief contributors to burnout were too many bureaucratic tasks (70%); increasing computerization of practice (47%); insufficient compensation/reimbursement (31%); lack of respect from patients (27%); government regulations (26%); lack of respect from administrators/employers, colleagues, or staff (23%); and stress from social distancing/societal issues related to COVID-19 (15%).
“Even though dermatologists seemingly have such a nice schedule, compared to a lot of other doctors, it’s still a very stressful occupation,” said Dr. Whitaker-Worth, who coauthored a study on the topic of burnout among female dermatologists. “It is harder to practice now because there are so many people telling us how we have to do things. That will burn you out over time, when control is taken away, when tasks are handed to you randomly by different entities – insurance companies, the government, the electronic medical record.”
Among dermatologists who self-reported burnout on the survey, 51% said it had no impact on their life, 9% said the impact was moderate, while 40% indicated that it had a strong/severe impact. About half (49%) use exercise to cope with burnout, while other key coping strategies include talking with family members/close friends (40%), playing or listening to music (39%), isolating themselves from others (35%), eating junk food (35%), and drinking alcohol (30%). At the same time, only 6% indicated that they are currently seeking professional health for their burnout and/or depression, and 3% indicated that they are planning to seek professional help. When asked why they hadn’t sought help for their burnout and/or depression, 51% of respondents said they were too busy and 36% said their symptoms weren’t severe enough.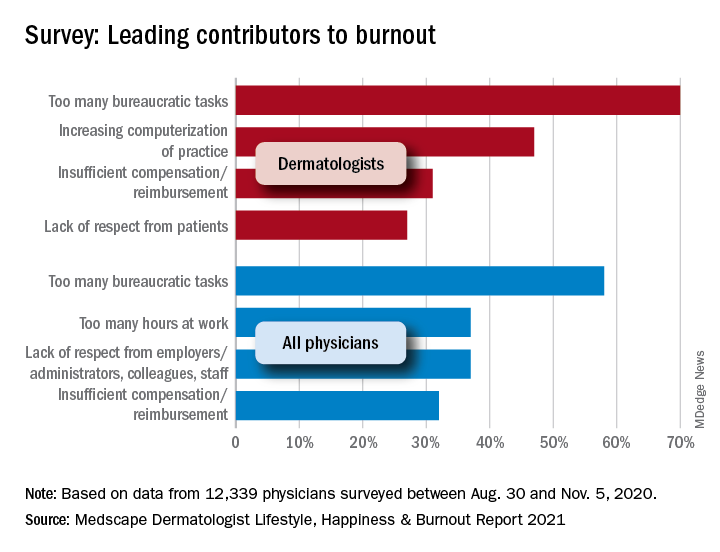
Dr. Whitaker-Worth characterized bureaucratic tasks as “a huge cause” of her burnout, but the larger contributor, she said, is managing her role as wife and mother of four children who are currently at home attending online school classes or working remotely, while she juggles her own work responsibilities. “They were stressed,” she said of her children. “The whole world was stressed. There are exceptions, but I still think that women are mostly shouldering the tasks at home. Even if they’re not doing them, they’re still feeling responsible for them. During the pandemic, every aspect of life became harder. Work was harder. Getting kids focused on school was harder. Doing basic tasks like errands was harder.”
Despite the stress and uncertainty generated by the pandemic, Dr. Whitaker-Worth considers dermatology as one of the happier specialties in medicine. “We still have a little more control of our time,” she said. “We are lucky in that we have reasonable hours, not as much in-house call, and a little more control over our day. I think work-life balance is the main thing that drives burnout – over bureaucracy, over everything.”
, according to Medscape’s 2021 Dermatologist Lifestyle, Happiness & Burnout Report.
In addition, 15% reported being burned out, and 3% reported being depressed, yet about half reported being too busy to seek help for burnout and/or depression.
Those are among the key findings from the Medscape report, which was published online on Feb. 19, 2021. More than 12,000 physicians from 29 specialties, including dermatology, participated in the survey, which explores how physicians are coping with burnout, maintaining their personal wellness, and viewing their workplaces and futures amid the COVID-19 pandemic.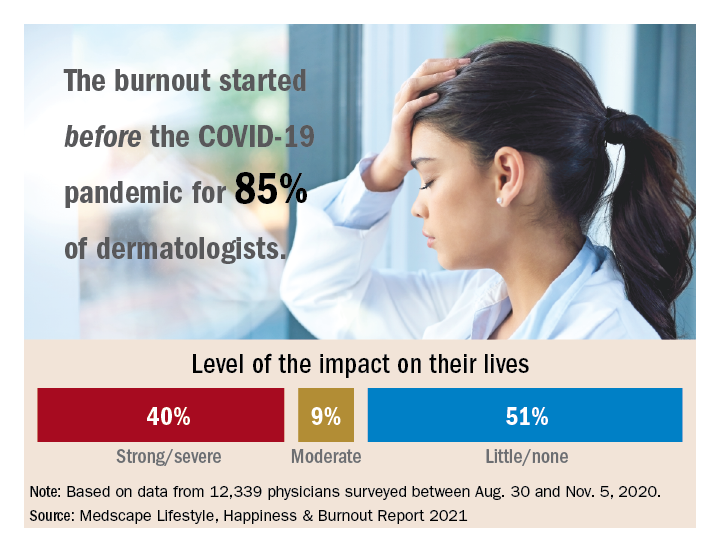
Among dermatologists who reported burnout, 85% said that it started prior to the pandemic, but 15% said it began with the pandemic. That finding resonates with Diane L. Whitaker-Worth, MD, a dermatologist with the University of Connecticut Health Center, Farmington. “A lot of dermatology practices closed down for a while, which was a huge economic hit,” she said in an interview. “I work for a university, so the stress wasn’t quite as bad. We shut down for about a week, but we canceled a lot of visits. We ramped up quickly, and I would say by the summer more people were coming in. Then we got backlogged. We’re still drowning in the number of patients who want to get in sooner, who can’t get an appointment, who need to be seen. It’s unbelievable, and it’s unrelenting.”
Dermatology trainees were also upended, with many residency programs going virtual. “We had to quickly figure out how to continue educating our residents,” said Dr. Whitaker-Worth, who also directs the university’s dermatology residency program. “What’s reasonable to expect them to be doing in clinic? There were fears about becoming infected [with the] virus. Every week, I had double the amount of work in the bureaucratic realm, trying to figure out how we run our clinic and keep our residents safe but learning. That was hard and the residents were really stressed. They were afraid they were going to get pulled to the ICUs. At that time, we didn’t have adequate PPE, and patients and doctors were dying.”
According to the dermatologists who responded to the Medscape survey and reported burnout, the seven chief contributors to burnout were too many bureaucratic tasks (70%); increasing computerization of practice (47%); insufficient compensation/reimbursement (31%); lack of respect from patients (27%); government regulations (26%); lack of respect from administrators/employers, colleagues, or staff (23%); and stress from social distancing/societal issues related to COVID-19 (15%).
“Even though dermatologists seemingly have such a nice schedule, compared to a lot of other doctors, it’s still a very stressful occupation,” said Dr. Whitaker-Worth, who coauthored a study on the topic of burnout among female dermatologists. “It is harder to practice now because there are so many people telling us how we have to do things. That will burn you out over time, when control is taken away, when tasks are handed to you randomly by different entities – insurance companies, the government, the electronic medical record.”
Among dermatologists who self-reported burnout on the survey, 51% said it had no impact on their life, 9% said the impact was moderate, while 40% indicated that it had a strong/severe impact. About half (49%) use exercise to cope with burnout, while other key coping strategies include talking with family members/close friends (40%), playing or listening to music (39%), isolating themselves from others (35%), eating junk food (35%), and drinking alcohol (30%). At the same time, only 6% indicated that they are currently seeking professional health for their burnout and/or depression, and 3% indicated that they are planning to seek professional help. When asked why they hadn’t sought help for their burnout and/or depression, 51% of respondents said they were too busy and 36% said their symptoms weren’t severe enough.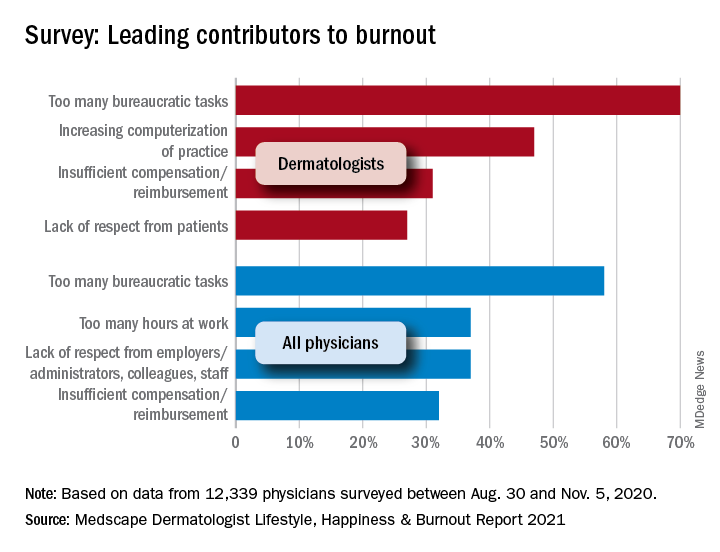
Dr. Whitaker-Worth characterized bureaucratic tasks as “a huge cause” of her burnout, but the larger contributor, she said, is managing her role as wife and mother of four children who are currently at home attending online school classes or working remotely, while she juggles her own work responsibilities. “They were stressed,” she said of her children. “The whole world was stressed. There are exceptions, but I still think that women are mostly shouldering the tasks at home. Even if they’re not doing them, they’re still feeling responsible for them. During the pandemic, every aspect of life became harder. Work was harder. Getting kids focused on school was harder. Doing basic tasks like errands was harder.”
Despite the stress and uncertainty generated by the pandemic, Dr. Whitaker-Worth considers dermatology as one of the happier specialties in medicine. “We still have a little more control of our time,” she said. “We are lucky in that we have reasonable hours, not as much in-house call, and a little more control over our day. I think work-life balance is the main thing that drives burnout – over bureaucracy, over everything.”
Office etiquette: Answering patient phone calls
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
In my office, one of the many consequences of the COVID-19 pandemic has been a dramatic increase in telephone traffic. I’m sure there are multiple reasons for this, but a major one is calls from patients who remain reluctant to visit our office in person.
Our veteran front-office staff members were adept at handling phone traffic at any level, but most of them retired because of the pandemic. The young folks who replaced them have struggled at times. You would think that millennials, who spend so much time on phones, would have little to learn in that department – until you remember that Twitter, Twitch, and TikTok do not demand polished interpersonal skills.
To address this issue, I have a memo in my office, which I have written, that establishes clear rules for proper professional telephone etiquette. If you want to adapt it for your own office, feel free to do so:
1. You only have one chance to make a first impression. The way we answer it determines, to a significant extent, how the community thinks of us, as people and as health care providers.
2. Answer all incoming calls before the third ring.
3. Answer warmly, enthusiastically, and professionally. Since the caller cannot see you, your voice is the only impression of our office a first-time caller will get.
4. Identify yourself and our office immediately. “Good morning, Doctor Eastern’s office. This is _____. How may I help you?” No one should ever have to ask what office they have reached, or to whom they are speaking.
5. Speak softly. This is to ensure confidentiality (more on that next), and because most people find loud telephone voices unpleasant.
6. Maintaining patient confidentiality is a top priority. It makes patients feel secure about being treated in our office, and it is also the law. Keep in mind that patients and others in the office may be able to overhear your phone conversations. Keep your voice down; never use the phone’s hands-free “speaker” function.
Be cautious about all information that is given over the phone. Don’t disclose any personal information unless you are absolutely certain you are talking to the correct patient. If the caller is not the patient, never discuss personal information without the patient’s permission.
7. Adopt a positive vocabulary – one that focuses on helping people. For example, rather than saying, “I don’t know,” say, “Let me find out for you,” or “I’ll find out who can help you with that.”
8. Offer to take a message if the caller has a question or issue you cannot address. Assure the patient that the appropriate staffer will call back later that day. That way, office workflow is not interrupted, and the patient still receives a prompt (and correct) answer.
9. All messages left overnight with the answering service must be returned as early as possible the very next business day. This is a top priority each morning. Few things annoy callers trying to reach their doctors more than unreturned calls. If the office will be closed for a holiday, or a response will be delayed for any other reason, make sure the service knows, and passes it on to patients.
10. Everyone in the office must answer calls when necessary. If you notice that a phone is ringing and the receptionists are swamped, please answer it; an incoming call must never go unanswered.
11. If the phone rings while you are dealing with a patient in person, the patient in front of you is your first priority. Put the caller on hold, but always ask permission before doing so, and wait for an answer. Never leave a caller on hold for more than a minute or two unless absolutely unavoidable.
12. NEVER answer, “Doctor’s office, please hold.” To a patient, that is even worse than not answering at all. No matter how often your hold message tells callers how important they are, they know they are being ignored. Such encounters never end well: Those who wait will be grumpy and rude when you get back to them; those who hang up will be even more grumpy and rude when they call back. Worst of all are those who don’t call back and seek care elsewhere – often leaving a nasty comment on social media besides.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Dermatology News. Write to him at [email protected].
We’re all vaccinated: Can we go back to the office (unmasked) now?
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Neurologic drug prices jump 50% in five years
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Telerheumatology will thrive post pandemic
Telemedicine has had a profound effect upon the practice of rheumatology during the COVID-19 pandemic and will continue to do so afterward, speakers predicted at the 2021 Rheumatology Winter Clinical Symposium.
“Telemedicine will change the way we do business. It already has,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University in Chicago.
“All of a sudden in March of last year we all turned on a dime and went 100% remote, and we made it work. And it has worked well. It’s not the same as seeing people in person, but I’m pretty sure that going forward probably somewhere in the range of 30% of our visits are going to be telemedicine. It’s an incredible way to deal with people who are stable and are driving in from an hour-and-a-half away to get their prescription refilled,” he said.
Conditions well suited for video patient visits are those where the physical exam isn’t informative or necessary, such as polymyalgia rheumatica, axial spondyloarthritis with axial disease only, childhood periodic fever syndromes, and even many cases of rheumatoid arthritis, in Dr. Ruderman’s view.
“People who are stable – maybe not in remission, but we’ve decided they’re at that their target – a lot of those visits can be done remotely. It’s way more efficient. Everybody loves it: We like it, the patients like it. But we have to get to where we can do it better. The technology is clumsy right now,” he said.
“We do need better and smarter platforms,” agreed Alvin F. Wells, MD, PhD, a telerheumatology pioneer who has been involved in digital/video communication with his patients for nearly 6 years. “But the biggest issue is connectivity. Not all of our patients can get on the Internet.”
The telerheumatology paradigm he has used during the pandemic and will continue to use afterward is to see every new patient in the office, then do the follow-up visits virtually.
“They don’t need to come back into the office in 4 weeks. I’ve done my physical exam, ordered the x-rays and lab work. At the virtual 4-week follow-up we go over everything and I tell them if they need to come in for training in giving their injections,” explained Dr. Wells, a rheumatologist in Franklin, Wisc.
“The telemedicine visit doesn’t take the place of an in-person visit, but it allows you to stratify, to say who needs to be seen sooner rather than later,” he added.
While he anticipates that physician-patient virtual visits will continue to be an important part of clinical practice post pandemic, he predicted the major growth areas for telerheumatology once COVID-19 is squashed will be in clinician-to-clinician interactions and remote patient monitoring using smart devices.
Dr. Wells hasn’t gone into the hospital once since the pandemic began. Initially, that was because he didn’t want to deal with the personal protective equipment shortage or expose himself to the virus. Now, it’s because it’s just a more efficient use of his time to conduct virtual – and billable – 15-minute e-consults with clinicians in the hospital.
“I’ve had a lot of appropriate consults with the hospitalists,” he said. He can walk a hospitalist through a real-time physical exam at a gout patient’s bedside and order the right laboratory tests.
“I don’t need to go into the hospital. The interventional radiologist can tap an ankle or toe as well as I can,” the rheumatologist said.
Dermatologist George Martin, MD, rose from the audience to say that while he recognizes that pandemic telemedicine has been a good fit for rheumatologists, it’s been a very different story in dermatology.
“I realize telemedicine works really well when you don’t have to lay your hands on a patient, or when you’re just doing a stable follow-up and talking about test results. But we in dermatology have found as a group that telemedicine is pretty worthless. When patients are trying to send you a video stream of what their melanoma looks like, or maybe it’s a benign seborrheic keratosis, you’re going to hang their life on that? Dermatology is a very hands-on, visual thing, and unless the camera work becomes better telemedicine is worthless, with the exception of a laboratory follow-up or a stable visit where a physical exam is not required,” declared Dr. Martin, who is in private practice in Maui.
Dr. Wells reported serving as a consultant to MiCare Path, a remote health and monitoring company.
Telemedicine has had a profound effect upon the practice of rheumatology during the COVID-19 pandemic and will continue to do so afterward, speakers predicted at the 2021 Rheumatology Winter Clinical Symposium.
“Telemedicine will change the way we do business. It already has,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University in Chicago.
“All of a sudden in March of last year we all turned on a dime and went 100% remote, and we made it work. And it has worked well. It’s not the same as seeing people in person, but I’m pretty sure that going forward probably somewhere in the range of 30% of our visits are going to be telemedicine. It’s an incredible way to deal with people who are stable and are driving in from an hour-and-a-half away to get their prescription refilled,” he said.
Conditions well suited for video patient visits are those where the physical exam isn’t informative or necessary, such as polymyalgia rheumatica, axial spondyloarthritis with axial disease only, childhood periodic fever syndromes, and even many cases of rheumatoid arthritis, in Dr. Ruderman’s view.
“People who are stable – maybe not in remission, but we’ve decided they’re at that their target – a lot of those visits can be done remotely. It’s way more efficient. Everybody loves it: We like it, the patients like it. But we have to get to where we can do it better. The technology is clumsy right now,” he said.
“We do need better and smarter platforms,” agreed Alvin F. Wells, MD, PhD, a telerheumatology pioneer who has been involved in digital/video communication with his patients for nearly 6 years. “But the biggest issue is connectivity. Not all of our patients can get on the Internet.”
The telerheumatology paradigm he has used during the pandemic and will continue to use afterward is to see every new patient in the office, then do the follow-up visits virtually.
“They don’t need to come back into the office in 4 weeks. I’ve done my physical exam, ordered the x-rays and lab work. At the virtual 4-week follow-up we go over everything and I tell them if they need to come in for training in giving their injections,” explained Dr. Wells, a rheumatologist in Franklin, Wisc.
“The telemedicine visit doesn’t take the place of an in-person visit, but it allows you to stratify, to say who needs to be seen sooner rather than later,” he added.
While he anticipates that physician-patient virtual visits will continue to be an important part of clinical practice post pandemic, he predicted the major growth areas for telerheumatology once COVID-19 is squashed will be in clinician-to-clinician interactions and remote patient monitoring using smart devices.
Dr. Wells hasn’t gone into the hospital once since the pandemic began. Initially, that was because he didn’t want to deal with the personal protective equipment shortage or expose himself to the virus. Now, it’s because it’s just a more efficient use of his time to conduct virtual – and billable – 15-minute e-consults with clinicians in the hospital.
“I’ve had a lot of appropriate consults with the hospitalists,” he said. He can walk a hospitalist through a real-time physical exam at a gout patient’s bedside and order the right laboratory tests.
“I don’t need to go into the hospital. The interventional radiologist can tap an ankle or toe as well as I can,” the rheumatologist said.
Dermatologist George Martin, MD, rose from the audience to say that while he recognizes that pandemic telemedicine has been a good fit for rheumatologists, it’s been a very different story in dermatology.
“I realize telemedicine works really well when you don’t have to lay your hands on a patient, or when you’re just doing a stable follow-up and talking about test results. But we in dermatology have found as a group that telemedicine is pretty worthless. When patients are trying to send you a video stream of what their melanoma looks like, or maybe it’s a benign seborrheic keratosis, you’re going to hang their life on that? Dermatology is a very hands-on, visual thing, and unless the camera work becomes better telemedicine is worthless, with the exception of a laboratory follow-up or a stable visit where a physical exam is not required,” declared Dr. Martin, who is in private practice in Maui.
Dr. Wells reported serving as a consultant to MiCare Path, a remote health and monitoring company.
Telemedicine has had a profound effect upon the practice of rheumatology during the COVID-19 pandemic and will continue to do so afterward, speakers predicted at the 2021 Rheumatology Winter Clinical Symposium.
“Telemedicine will change the way we do business. It already has,” observed Eric M. Ruderman, MD, professor of medicine (rheumatology) at Northwestern University in Chicago.
“All of a sudden in March of last year we all turned on a dime and went 100% remote, and we made it work. And it has worked well. It’s not the same as seeing people in person, but I’m pretty sure that going forward probably somewhere in the range of 30% of our visits are going to be telemedicine. It’s an incredible way to deal with people who are stable and are driving in from an hour-and-a-half away to get their prescription refilled,” he said.
Conditions well suited for video patient visits are those where the physical exam isn’t informative or necessary, such as polymyalgia rheumatica, axial spondyloarthritis with axial disease only, childhood periodic fever syndromes, and even many cases of rheumatoid arthritis, in Dr. Ruderman’s view.
“People who are stable – maybe not in remission, but we’ve decided they’re at that their target – a lot of those visits can be done remotely. It’s way more efficient. Everybody loves it: We like it, the patients like it. But we have to get to where we can do it better. The technology is clumsy right now,” he said.
“We do need better and smarter platforms,” agreed Alvin F. Wells, MD, PhD, a telerheumatology pioneer who has been involved in digital/video communication with his patients for nearly 6 years. “But the biggest issue is connectivity. Not all of our patients can get on the Internet.”
The telerheumatology paradigm he has used during the pandemic and will continue to use afterward is to see every new patient in the office, then do the follow-up visits virtually.
“They don’t need to come back into the office in 4 weeks. I’ve done my physical exam, ordered the x-rays and lab work. At the virtual 4-week follow-up we go over everything and I tell them if they need to come in for training in giving their injections,” explained Dr. Wells, a rheumatologist in Franklin, Wisc.
“The telemedicine visit doesn’t take the place of an in-person visit, but it allows you to stratify, to say who needs to be seen sooner rather than later,” he added.
While he anticipates that physician-patient virtual visits will continue to be an important part of clinical practice post pandemic, he predicted the major growth areas for telerheumatology once COVID-19 is squashed will be in clinician-to-clinician interactions and remote patient monitoring using smart devices.
Dr. Wells hasn’t gone into the hospital once since the pandemic began. Initially, that was because he didn’t want to deal with the personal protective equipment shortage or expose himself to the virus. Now, it’s because it’s just a more efficient use of his time to conduct virtual – and billable – 15-minute e-consults with clinicians in the hospital.
“I’ve had a lot of appropriate consults with the hospitalists,” he said. He can walk a hospitalist through a real-time physical exam at a gout patient’s bedside and order the right laboratory tests.
“I don’t need to go into the hospital. The interventional radiologist can tap an ankle or toe as well as I can,” the rheumatologist said.
Dermatologist George Martin, MD, rose from the audience to say that while he recognizes that pandemic telemedicine has been a good fit for rheumatologists, it’s been a very different story in dermatology.
“I realize telemedicine works really well when you don’t have to lay your hands on a patient, or when you’re just doing a stable follow-up and talking about test results. But we in dermatology have found as a group that telemedicine is pretty worthless. When patients are trying to send you a video stream of what their melanoma looks like, or maybe it’s a benign seborrheic keratosis, you’re going to hang their life on that? Dermatology is a very hands-on, visual thing, and unless the camera work becomes better telemedicine is worthless, with the exception of a laboratory follow-up or a stable visit where a physical exam is not required,” declared Dr. Martin, who is in private practice in Maui.
Dr. Wells reported serving as a consultant to MiCare Path, a remote health and monitoring company.
FROM RWCS 2021
Nota bene: Don’t change a note
A man I saw earlier this year called my office recently. He’d read my note, and after discussing it with his attorney, wanted me to make changes. He said that the way I’d described his symptoms would be damaging to a legal action he was involved in, and so he wanted it reworded.
Obviously, I said “no.” I’m not a fiction writer. My notes are what people tell me happened. I don’t make them up.
He wasn’t happy about this, and a few days later I got a request to send his records to another neurologist, which I gladly did.
In this business a large measure of what we do is based on the patient’s symptoms. what they report to us, and how they describe it. When I put their story into a written note, my goal is to be as accurate to what they told me as possible. I’m not here to embellish, disparage, or minimize their history.
To do so is to look bad at the very least and open yourself up to malpractice and legal charges at worst.
This isn’t to say errors can’t be modified. I’m far from perfect. Sometimes I might misunderstand something a patient tells me, or get information crossed up. When that happens there’s nothing wrong with writing an addendum, clarifying or correcting what my earlier note said – but not changing the original note.
I asked the unhappy patient to write down what he thought was incorrect, and I’d be willing to include that in his chart. He wasn’t willing to do that, and there was no way I would ever change a note. I tried to politely explain the reasons why, but he wasn’t listening.
So I lost him as a patient. After 23 years of practice, that doesn’t bother me. I learned a long time ago that I can’t please everyone, nor can I be everyone’s doctor. Saying “no” is just as important as saying “yes,” though at times more difficult.
This time, though, the answer was pretty obvious, and will be the same next time I get the same request from a patient.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A man I saw earlier this year called my office recently. He’d read my note, and after discussing it with his attorney, wanted me to make changes. He said that the way I’d described his symptoms would be damaging to a legal action he was involved in, and so he wanted it reworded.
Obviously, I said “no.” I’m not a fiction writer. My notes are what people tell me happened. I don’t make them up.
He wasn’t happy about this, and a few days later I got a request to send his records to another neurologist, which I gladly did.
In this business a large measure of what we do is based on the patient’s symptoms. what they report to us, and how they describe it. When I put their story into a written note, my goal is to be as accurate to what they told me as possible. I’m not here to embellish, disparage, or minimize their history.
To do so is to look bad at the very least and open yourself up to malpractice and legal charges at worst.
This isn’t to say errors can’t be modified. I’m far from perfect. Sometimes I might misunderstand something a patient tells me, or get information crossed up. When that happens there’s nothing wrong with writing an addendum, clarifying or correcting what my earlier note said – but not changing the original note.
I asked the unhappy patient to write down what he thought was incorrect, and I’d be willing to include that in his chart. He wasn’t willing to do that, and there was no way I would ever change a note. I tried to politely explain the reasons why, but he wasn’t listening.
So I lost him as a patient. After 23 years of practice, that doesn’t bother me. I learned a long time ago that I can’t please everyone, nor can I be everyone’s doctor. Saying “no” is just as important as saying “yes,” though at times more difficult.
This time, though, the answer was pretty obvious, and will be the same next time I get the same request from a patient.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A man I saw earlier this year called my office recently. He’d read my note, and after discussing it with his attorney, wanted me to make changes. He said that the way I’d described his symptoms would be damaging to a legal action he was involved in, and so he wanted it reworded.
Obviously, I said “no.” I’m not a fiction writer. My notes are what people tell me happened. I don’t make them up.
He wasn’t happy about this, and a few days later I got a request to send his records to another neurologist, which I gladly did.
In this business a large measure of what we do is based on the patient’s symptoms. what they report to us, and how they describe it. When I put their story into a written note, my goal is to be as accurate to what they told me as possible. I’m not here to embellish, disparage, or minimize their history.
To do so is to look bad at the very least and open yourself up to malpractice and legal charges at worst.
This isn’t to say errors can’t be modified. I’m far from perfect. Sometimes I might misunderstand something a patient tells me, or get information crossed up. When that happens there’s nothing wrong with writing an addendum, clarifying or correcting what my earlier note said – but not changing the original note.
I asked the unhappy patient to write down what he thought was incorrect, and I’d be willing to include that in his chart. He wasn’t willing to do that, and there was no way I would ever change a note. I tried to politely explain the reasons why, but he wasn’t listening.
So I lost him as a patient. After 23 years of practice, that doesn’t bother me. I learned a long time ago that I can’t please everyone, nor can I be everyone’s doctor. Saying “no” is just as important as saying “yes,” though at times more difficult.
This time, though, the answer was pretty obvious, and will be the same next time I get the same request from a patient.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Point-Counterpoint: The future of rheumatology is sub-subspecialization
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
Sub-subspecialization would be counterproductive: Orrin M. Troum, MD
The much-discussed looming rheumatology workforce shortage is actually here already. And it’s going to worsen rapidly. Add to that the striking geographic maldistribution of rheumatologists across the United States, and it makes little sense for some rheumatologists to declare they’re only going to see patients with psoriatic arthritis, or gout, or lupus. Such sub-subspecialization will only worsen the workforce problem, Orrin M. Troum, MD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
Besides, surveys indicate that most rheumatologists like what they do now, despite their status as the lowest-paid subspecialists within internal medicine. They enjoy a sense of satisfaction stemming from their ability to help patients with chronic debilitating diseases turn their lives around as a result of revolutionary treatment advances in the last 2 decades, said Dr. Troum, a rheumatologist at the University of Southern California, Los Angeles, and in private practice in Santa Monica.
The 2015 American College of Rheumatology Workforce Study concluded that the demand for adult rheumatology services already outstripped the supply by 12.9% in 2015. And as current rheumatologists retire in tandem with a growing aged general population saddled with an accompanying burgeoning prevalence of rheumatic and musculoskeletal diseases, demand is expected to exceed supply by a whopping 102% in 2030.
The Workforce Study also highlighted the geographic maldistribution problem, with 21% of all adult rheumatologists now practicing in the Northeast and only 3.9% in the Southwest. Rheumatologists are also few and far between across large swaths of the South Central, North Central, and Northwest United States.
Today rheumatologists spend about half their working hours seeing patients with rheumatic diseases, one-quarter of their time in administrative tasks, 20% seeing patients with nonrheumatic diseases such as osteoarthritis, and the rest in teaching or research. It could be argued that, if rheumatologists declined to see patients with osteoarthritis, a nonrheumatic disease, it would put a sizeable dent in the workforce shortage, but it’s clear that nonrheumatologists can’t reliably differentiate inflammatory from noninflammatory arthritis. And there’s another problem with the idea of rheumatologists barring the office door to patients with nonrheumatic diseases: imagine a young clinical rheumatologist going out into practice and trying to tell referring internists, family physicians, and orthopedists that he or she doesn’t want to see patients with osteoarthritis, noninflammatory back pain, or fibromyalgia.
“How busy do you think you’re going to be, ever, if you tell the referring docs that you’re not going to see patients they think they need help with? And who’s going to make the correct diagnosis if we don’t at least see these patients initially?” Dr. Troum asked.
The case for sub-subspecialization: Martin J. Bergman, MD
Think about how many patients you’re treating for vasculitis, systemic lupus erythematosus, Behçet’s disease, or systemic sclerosis. Do you think you’re doing the best job that’s possible when you’re seeing just a handful of these patients, or would outcomes be better if they were seen at centers where the focus is specifically on these somewhat rare diseases? asked Martin J. Bergman, MD, a rheumatologist at Drexel University, Philadelphia, and in private practice in Ridley Park, Pa.
We can take a lesson from other specialties. It’s well-documented that higher surgical volume brings better care and better outcomes for cardiovascular and cancer surgery. Specialized high-level trauma centers achieve 20%-30% better outcomes. And outcomes are also improved when joint replacement surgery is done at specialty centers. Why would we expect rheumatology to be any different?
Actually, there is already evidence from within our own field to support this concept. A longitudinal study of 150 consecutive SLE patients – half treated at the general rheumatology clinic at Rush University, Chicago, and the other half at the medical center’s specialized lupus clinic – showed demonstrably better quality-of-care outcomes for the patients seen in the dedicated lupus clinic. They were roughly twice as likely to undergo antiphospholipid antibody testing and were also significantly more likely to have bone mineral density testing, pneumococcal vaccination, and sunscreen counseling.
Look, I get it. This is not going to be possible everywhere. In underserved geographic areas, it may not be feasible. But I would think that, even in places where you can’t have sub-subspecialty clinics, maybe it’s time for rheumatologists to start thinking in terms of sub-specializing their own practice and getting out of areas where we can make little or no impact beyond what other physicians can accomplish. Most of us provide very little value for patients with fibromyalgia and chronic fatigue syndrome. We have only so much time, and rather than taking care of anybody who has an ache or a pain we should focus on where we can make the most impact, and that’s inflammatory disease.
The speakers reported having no financial conflicts regarding their presentations.
FROM RWCS 2021
Is pediatric subspecialty training financially worth it?
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
I am the best. Sometimes.
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].