User login
Repeat TAVR outcomes ‘reassuring’
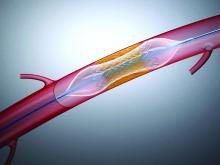
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Substantial very late MACE risk after PCI for SIHD
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
FROM ACC 20
Consensus recommendations on AMI management during COVID-19
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
Low-risk TAVR loses ground at 2 years in PARTNER 3
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
FROM ACC 2020
Radial arteries show CABG survival advantage over saphenous veins
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
FROM ACC 2020
Outcomes-based measurement of TAVR program quality goes live
The long-sought goal of measuring the quality of U.S. transcatheter aortic valve replacement (TAVR) programs by patient outcomes rather than by the surrogate measure of case volume is about to be realized.
Starting more or less immediately, the U.S. national register for all TAVR cases that’s mandated by Food and Drug Administration labeling of these devices and run through a collaboration of the American College of Cardiology and the Society of Thoracic Surgeons will start applying a newly developed and validated five-item metric for measuring 30-day patient outcomes and designed to gauge the quality of TAVR programs.
At first, the only recipients of the data will be the programs themselves, but starting in about a year, by sometime in 2021, the STS/ACC TVT (transcatheter valve therapy) Registry will start to make its star-based rating of TAVR programs available to the public, Nimesh D. Desai, MD, said on March 29 at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. These societies already make star-based ratings of U.S. programs available to the public for several other types of cardiac interventions, including coronary artery bypass surgery and MI management.
The new, composite metric based on 30-day outcome data “is appropriate for high-stakes applications such as public reporting,” said Dr. Desai, a thoracic surgeon and director of thoracic aortic surgery research at the University of Pennsylvania in Philadelphia. “We’re confident this model can be used for public reporting. It’s undergone extensive testing of its validity.” The steering committee of the STS/ACC TVT Registry commissioned development of the metric, and it’s now “considered approved,” and ready for use, he explained.
To create the new metric, Dr. Desai and his associates used data from 52,561 patients who underwent transfemoral TAVR during 2015-2017 at any of 301 U.S. sites. These data came from a total pool of more than 114,000 patients at 556 sites, but data from many sites weren’t usable because they were not adequately complete. The researchers then identified the top four measures taken during the 30 days following intervention (hospitalization included) that best correlated with 1-year survival and patients’ quality-of-life scores on the Kansas City Cardiomyopathy Questionnaire: stroke; major, life-threatening, or disabling bleed; acute kidney injury (stage III); and moderate or severe paravalvular leak. These outcomes “matter most to patients,” Dr. Desai said.
They used these four outcomes plus 30-day mortality to calculate the programs’ ratings. Among the 52,561 patients, 14% had at least one of these adverse outcomes. The researchers then used a logistic regression model that adjusted for 46 measured variables to calculate how each program performed relative to the average performance of all the programs. Programs with outcomes that fell within the 95% confidence intervals of average performance were rated as performing as expected; those outside rated as performing either better or worse than expected. The results showed 34 centers (11%) had worse than expected outcomes and 25 (8%) had better than expected outcomes, Dr. Desai said.
“This is a major step forward in measuring TAVR quality,” commented Michael Mack, MD, a cardiac surgeon with Baylor Scott & White Health in Dallas who has been very active in studying TAVR. “Until now, we used volume as a surrogate for quality, but the precision was not great. This is an extremely welcome metric.” The next step is to eventually use 1-year follow-up data instead of 30-day outcomes, he added.
“With the rapid expansion of TAVR over the past 6-8 years, we’re now at the point to start to do this. It’s an ethical obligation This will be one of the most high-fidelity, valid models for public reporting” of clinical outcomes,” said Joseph Cleveland, MD, a professor of surgery at the University of Colorado at Denver in Aurora. “It’s reassuring that about 90% of the program performed as expected or better than expected,” he added.
“Transparency and outcomes should drive how TAVR is delivered,” commented Ashish Pershad, MD, an interventional cardiologist at Banner-University Medicine Heart Institute in Phoenix who estimated that he performs about 150 TAVR procedures annually. “This is a step forward. I’ve been waiting for this for a long time. Until now, volume has been used as a surrogate outcome, but we know it’s not accurate. I’m confident that this model is a good starting point.” But Dr. Pershad also had concern that this new approach “can lend itself to some degree of gaming,” like a bleeding event getting classified as minor when it was really major, or outlier patients getting dropped from reports.
The temptation to cut corners may be higher for TAVR than it’s been for the cardiac-disease metrics that already get publicly reported, like bypass surgery and myocardial infarction management, because of TAVR’s higher cost and higher profile, Dr. Pershad said. Existing measures “have not been as linked to financial disincentive as TAVR might be” because TAVR reimbursements can run as high as $50,000 per case. “The stakes with TAVR are higher,” he said.
Ultimately, the reliable examination of TAVR outcomes that this new metric allows may lead to a shake-up of TAVR programs, Dr. Pershad predicted. “This is clearly a step toward closing down some programs that [consistently] underperform.”
The STS/ACC TVT Registry receives no commercial funding. Dr. Desai has been a consultant to, speaker on behalf of, and received research funding from Gore, and he has also spoken on behalf of Cook, Medtronic, and Terumo Aortic. Dr. Cleveland, Dr. Mack, and Dr. Pershad had no disclosures.
The long-sought goal of measuring the quality of U.S. transcatheter aortic valve replacement (TAVR) programs by patient outcomes rather than by the surrogate measure of case volume is about to be realized.
Starting more or less immediately, the U.S. national register for all TAVR cases that’s mandated by Food and Drug Administration labeling of these devices and run through a collaboration of the American College of Cardiology and the Society of Thoracic Surgeons will start applying a newly developed and validated five-item metric for measuring 30-day patient outcomes and designed to gauge the quality of TAVR programs.
At first, the only recipients of the data will be the programs themselves, but starting in about a year, by sometime in 2021, the STS/ACC TVT (transcatheter valve therapy) Registry will start to make its star-based rating of TAVR programs available to the public, Nimesh D. Desai, MD, said on March 29 at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. These societies already make star-based ratings of U.S. programs available to the public for several other types of cardiac interventions, including coronary artery bypass surgery and MI management.
The new, composite metric based on 30-day outcome data “is appropriate for high-stakes applications such as public reporting,” said Dr. Desai, a thoracic surgeon and director of thoracic aortic surgery research at the University of Pennsylvania in Philadelphia. “We’re confident this model can be used for public reporting. It’s undergone extensive testing of its validity.” The steering committee of the STS/ACC TVT Registry commissioned development of the metric, and it’s now “considered approved,” and ready for use, he explained.
To create the new metric, Dr. Desai and his associates used data from 52,561 patients who underwent transfemoral TAVR during 2015-2017 at any of 301 U.S. sites. These data came from a total pool of more than 114,000 patients at 556 sites, but data from many sites weren’t usable because they were not adequately complete. The researchers then identified the top four measures taken during the 30 days following intervention (hospitalization included) that best correlated with 1-year survival and patients’ quality-of-life scores on the Kansas City Cardiomyopathy Questionnaire: stroke; major, life-threatening, or disabling bleed; acute kidney injury (stage III); and moderate or severe paravalvular leak. These outcomes “matter most to patients,” Dr. Desai said.
They used these four outcomes plus 30-day mortality to calculate the programs’ ratings. Among the 52,561 patients, 14% had at least one of these adverse outcomes. The researchers then used a logistic regression model that adjusted for 46 measured variables to calculate how each program performed relative to the average performance of all the programs. Programs with outcomes that fell within the 95% confidence intervals of average performance were rated as performing as expected; those outside rated as performing either better or worse than expected. The results showed 34 centers (11%) had worse than expected outcomes and 25 (8%) had better than expected outcomes, Dr. Desai said.
“This is a major step forward in measuring TAVR quality,” commented Michael Mack, MD, a cardiac surgeon with Baylor Scott & White Health in Dallas who has been very active in studying TAVR. “Until now, we used volume as a surrogate for quality, but the precision was not great. This is an extremely welcome metric.” The next step is to eventually use 1-year follow-up data instead of 30-day outcomes, he added.
“With the rapid expansion of TAVR over the past 6-8 years, we’re now at the point to start to do this. It’s an ethical obligation This will be one of the most high-fidelity, valid models for public reporting” of clinical outcomes,” said Joseph Cleveland, MD, a professor of surgery at the University of Colorado at Denver in Aurora. “It’s reassuring that about 90% of the program performed as expected or better than expected,” he added.
“Transparency and outcomes should drive how TAVR is delivered,” commented Ashish Pershad, MD, an interventional cardiologist at Banner-University Medicine Heart Institute in Phoenix who estimated that he performs about 150 TAVR procedures annually. “This is a step forward. I’ve been waiting for this for a long time. Until now, volume has been used as a surrogate outcome, but we know it’s not accurate. I’m confident that this model is a good starting point.” But Dr. Pershad also had concern that this new approach “can lend itself to some degree of gaming,” like a bleeding event getting classified as minor when it was really major, or outlier patients getting dropped from reports.
The temptation to cut corners may be higher for TAVR than it’s been for the cardiac-disease metrics that already get publicly reported, like bypass surgery and myocardial infarction management, because of TAVR’s higher cost and higher profile, Dr. Pershad said. Existing measures “have not been as linked to financial disincentive as TAVR might be” because TAVR reimbursements can run as high as $50,000 per case. “The stakes with TAVR are higher,” he said.
Ultimately, the reliable examination of TAVR outcomes that this new metric allows may lead to a shake-up of TAVR programs, Dr. Pershad predicted. “This is clearly a step toward closing down some programs that [consistently] underperform.”
The STS/ACC TVT Registry receives no commercial funding. Dr. Desai has been a consultant to, speaker on behalf of, and received research funding from Gore, and he has also spoken on behalf of Cook, Medtronic, and Terumo Aortic. Dr. Cleveland, Dr. Mack, and Dr. Pershad had no disclosures.
The long-sought goal of measuring the quality of U.S. transcatheter aortic valve replacement (TAVR) programs by patient outcomes rather than by the surrogate measure of case volume is about to be realized.
Starting more or less immediately, the U.S. national register for all TAVR cases that’s mandated by Food and Drug Administration labeling of these devices and run through a collaboration of the American College of Cardiology and the Society of Thoracic Surgeons will start applying a newly developed and validated five-item metric for measuring 30-day patient outcomes and designed to gauge the quality of TAVR programs.
At first, the only recipients of the data will be the programs themselves, but starting in about a year, by sometime in 2021, the STS/ACC TVT (transcatheter valve therapy) Registry will start to make its star-based rating of TAVR programs available to the public, Nimesh D. Desai, MD, said on March 29 at the joint scientific sessions of the ACC and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. These societies already make star-based ratings of U.S. programs available to the public for several other types of cardiac interventions, including coronary artery bypass surgery and MI management.
The new, composite metric based on 30-day outcome data “is appropriate for high-stakes applications such as public reporting,” said Dr. Desai, a thoracic surgeon and director of thoracic aortic surgery research at the University of Pennsylvania in Philadelphia. “We’re confident this model can be used for public reporting. It’s undergone extensive testing of its validity.” The steering committee of the STS/ACC TVT Registry commissioned development of the metric, and it’s now “considered approved,” and ready for use, he explained.
To create the new metric, Dr. Desai and his associates used data from 52,561 patients who underwent transfemoral TAVR during 2015-2017 at any of 301 U.S. sites. These data came from a total pool of more than 114,000 patients at 556 sites, but data from many sites weren’t usable because they were not adequately complete. The researchers then identified the top four measures taken during the 30 days following intervention (hospitalization included) that best correlated with 1-year survival and patients’ quality-of-life scores on the Kansas City Cardiomyopathy Questionnaire: stroke; major, life-threatening, or disabling bleed; acute kidney injury (stage III); and moderate or severe paravalvular leak. These outcomes “matter most to patients,” Dr. Desai said.
They used these four outcomes plus 30-day mortality to calculate the programs’ ratings. Among the 52,561 patients, 14% had at least one of these adverse outcomes. The researchers then used a logistic regression model that adjusted for 46 measured variables to calculate how each program performed relative to the average performance of all the programs. Programs with outcomes that fell within the 95% confidence intervals of average performance were rated as performing as expected; those outside rated as performing either better or worse than expected. The results showed 34 centers (11%) had worse than expected outcomes and 25 (8%) had better than expected outcomes, Dr. Desai said.
“This is a major step forward in measuring TAVR quality,” commented Michael Mack, MD, a cardiac surgeon with Baylor Scott & White Health in Dallas who has been very active in studying TAVR. “Until now, we used volume as a surrogate for quality, but the precision was not great. This is an extremely welcome metric.” The next step is to eventually use 1-year follow-up data instead of 30-day outcomes, he added.
“With the rapid expansion of TAVR over the past 6-8 years, we’re now at the point to start to do this. It’s an ethical obligation This will be one of the most high-fidelity, valid models for public reporting” of clinical outcomes,” said Joseph Cleveland, MD, a professor of surgery at the University of Colorado at Denver in Aurora. “It’s reassuring that about 90% of the program performed as expected or better than expected,” he added.
“Transparency and outcomes should drive how TAVR is delivered,” commented Ashish Pershad, MD, an interventional cardiologist at Banner-University Medicine Heart Institute in Phoenix who estimated that he performs about 150 TAVR procedures annually. “This is a step forward. I’ve been waiting for this for a long time. Until now, volume has been used as a surrogate outcome, but we know it’s not accurate. I’m confident that this model is a good starting point.” But Dr. Pershad also had concern that this new approach “can lend itself to some degree of gaming,” like a bleeding event getting classified as minor when it was really major, or outlier patients getting dropped from reports.
The temptation to cut corners may be higher for TAVR than it’s been for the cardiac-disease metrics that already get publicly reported, like bypass surgery and myocardial infarction management, because of TAVR’s higher cost and higher profile, Dr. Pershad said. Existing measures “have not been as linked to financial disincentive as TAVR might be” because TAVR reimbursements can run as high as $50,000 per case. “The stakes with TAVR are higher,” he said.
Ultimately, the reliable examination of TAVR outcomes that this new metric allows may lead to a shake-up of TAVR programs, Dr. Pershad predicted. “This is clearly a step toward closing down some programs that [consistently] underperform.”
The STS/ACC TVT Registry receives no commercial funding. Dr. Desai has been a consultant to, speaker on behalf of, and received research funding from Gore, and he has also spoken on behalf of Cook, Medtronic, and Terumo Aortic. Dr. Cleveland, Dr. Mack, and Dr. Pershad had no disclosures.
REPORTING FROM ACC 20
UK TAVI: Similar outcomes to surgery in real world
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Transcatheter aortic valve replacement (TAVR) was not inferior to conventional surgery with respect to death from any cause at 1 year in a new real-world study in patients age 70 years or older with severe symptomatic aortic stenosis at increased operative risk due to age or comorbidity.
The UK TAVI study was presented March 29 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC).
The trial involved a broad group of patients who were treated at every medical center that performs the transcatheter procedure across the United Kingdom.
“The importance of this trial is that it confirms the effectiveness of the TAVR strategy in a real-world setting,” said lead author, William D. Toff, MD, professor of cardiology at the University of Leicester, United Kingdom.
Previous clinical trials have found TAVR to be noninferior or superior to open-heart surgery for various patient groups, but most trials have been limited to medical centers that perform a high volume of procedures or focus on the use of specific types of replacement valves, he noted.
“Our results are concordant with those from earlier trials in intermediate- and low-risk patients, but those earlier trials were performed in the best centers and had many exclusion criteria. We have replicated those results in populations more representative of the real world.”
“I think it is a very important message that supports the findings in earlier trials that were focused on showing whether TAVR can work under ideal conditions, while our trial shows that it does work in real-world clinical practice,” he added.
The UK TAVI trial enrolled 913 patients referred for treatment of severe aortic stenosis at 34 UK sites from 2014 to 2018. They were randomly assigned to receive TAVR or open-heart surgery.
Enrollment was limited to participants age 70 years or older (with additional risk factors) or age 80 years or older (with or without additional risk factors). The average age was 81 years.
Overall, participants were at intermediate to low risk from surgery, with a median Society of Thoracic Surgeons (STS) risk score of 2.6%. However, researchers did not specify a particular risk score cutoff for enrollment.
“This allowed the trial to evolve along with changes in guidelines and practice regarding TAVR over the course of the study and to reflect physicians’ nuanced, real-world approach to considering risk in decision-making rather than taking a formulaic approach,” Toff said.
At 1 year, the rate of death from any cause (the primary endpoint) was 4.6% in the TAVR group and 6.6% in the surgery group, a difference that met the trial’s prespecified threshold for noninferiority of TAVR.
Rates of death from cardiovascular disease or stroke were also similar between the two groups.
Patients who received TAVR had a significantly higher rate of vascular complications (4.8%) than those receiving surgery (1.3%).
TAVR patients were also more likely to have a pacemaker implanted. This occurred in 12.2% of TAVR patients and 6.6% of those undergoing surgery.
In addition, patients who underwent TAVR had a higher rate of aortic regurgitation. Mild aortic regurgitation occurred at 1 year in 38.3% of the TAVR group and 11.7% of the surgery group, whereas moderate regurgitation occurred in 2.3% of TAVR patients and 0.6% of surgery patients.
On the other hand, patients undergoing TAVR had a significantly lower rate of major bleeding complications, which occurred in 6.3% of patients having TAVR and 17.1% of those undergoing surgery.
TAVR was also associated with a shorter hospital stay, fewer days in intensive care, and a faster improvement in functional capacity and quality of life. Functional capacity and quality-of-life measures at 6 weeks after the procedure were better in the TAVR group but by 1 year they were similar in the two groups.
“Longer follow-up is required to confirm sustained clinical benefit and valve durability to inform clinical practice, particularly in younger patients,” Toff concluded.
“The results from our trial and others are encouraging, but patients need to be fully informed and know that the long-term durability of the TAVR valves and the long-term implications of the increased risk of aortic regurgitation are still uncertain,” he added.
The researchers plan to continue to track outcomes for a minimum of 5 years.
Discussant of the UK TAVI trial at an ACC press conference, Julia Grapsa, MD, Guys and St Thomas NHS Trust, London, United Kingdom, said it was a well-designed study.
“It was impressive to see so many UK sites and the age range of patients from 70 to 91 years, and the shorter hospital stays and functional recoveries as well as reduced major bleeding in the TAVR group,” Grapsa said.
“But something that was very striking to me was the increase in moderate aortic regurgitation in the TAVR arm, 2.3% versus 0.6% in the surgical arm, so it is very important to keep following these patients long term,” she added.
In answer to a question during the main session about using age alone as an inclusion criterion in those over 80 years old, Toff said, “We were more comfortable taking all comers over 80 years of age because of the uncertainty about TAVR is more in relation to its durability and the clinical significance of the aortic regurgitation, which may have consequences in the longer term. But the longer term for the over 80s is obviously less of a problem than for those in their 70s.”
This study was funded by the UK National Institute for Health Research Health Technology Assessment Programme. Toff reports no disclosures.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20410-ACC. Presented March 29, 2020.
This article first appeared on Medscape.com.
Novel mitral valve device shows encouraging mortality data
NATIONAL HARBOR, MD. – In a pooled analysis of three trials conducted with the transcatheter Carillon Mitral Contour System for mitral valve repair, the 5-year survival is 56.2%, which is an encouraging outcome that justifies the ongoing multinational pivotal Carillon trial, according to the principal investigator of the analysis presented at CRT 2020 sponsored by MedStar Heart & Vascular Institute.
In patients with functional mitral valve regurgitation (FMR), “the Carillon device shows extremely encouraging long-term mortality data from prospective controlled trials in comparison with guideline-directed medical therapy or with the COAPT results,” according to Janusz Lipiecki, MD, PhD, department of cardiology, University Hospital, Clermont-Ferrand, France.
The COAPT trial is an important benchmark, because it was the first large, randomized trial to show benefit for a percutaneous device in the treatment of heart failure patients with moderate to severe FMR (N Engl J Med. 2018;379:2307-18). The study associated the MitraClip with a nearly 40% reduction in all-cause mortality (29.1% vs. 46.1%) at 24 months, relative to guideline-directed medical therapy (GDMT).
The Carillon device, which is also delivered percutaneously, does not engage the valve leaflets to treat FMR. Rather, it is anchored in coronary sinus to reform the mitral annulus. This reduces FMR without damage to the mitral valve, thus preserving the potential for future valve repairs, according to Dr. Lipiecki, who reported that more than 1,100 devices have now been implanted, mostly in Europe.
The data so far are encouraging, said Dr. Lipiecki, who provided survival data in 74 patients followed for at least 5 years. Of these, 23 were drawn from the REDUCE FMR trial, which was blinded and sham controlled, and the remainder from the TITAN and TITAN II studies, which were prospective but not controlled.
In this series of 74 patients, there were no serious complications associated with the procedure, and all achieved a reduction in mitral regurgitation at 12 months, Dr. Lipiecki said. Furthermore, the reduction in FMR was associated with improvements in symptoms and “favorable remodeling” reflected in reduced left ventricular volume, he said.
In this series, the 5-year survival is 56%, which substantially exceeds what would be expected with GDMT, according to Dr. Lipiecki.
There were no baseline predictors of long-term survival, but improvements within the 6 months in functional heart class, 6-minute walk distance (6MWD), and mitral regurgitation were significantly associated with a greater likelihood of being alive at 5 years.
Although there is no comparable follow-up with other devices, including the MitraClip, Dr. Lipiecki did compare the 67.9% survival at 3 years in this series to that of the COAPT trial. He restricted the comparison to those treated for grade 3+ or 4+ mitral regurgitation. At 36 months, survival rates were 57.2% and 44.5% for those treated with MitraClip and GDMT, respectively.
“COAPT patients might not be comparable for a variety of reasons, including the anatomic restrictions important to the use of either of these devices,” Dr. Lipiecki acknowledged, but he said the long-term data with the Carillon device provide support for the pivotal Carillon trial now enrolling.
In this blinded trial, more than 350 patients at 75 sites are being randomized to placement of the Carillon device, which has been available in Europe since 2011, or a sham procedure. The trial is scheduled for completion in 2025.
NATIONAL HARBOR, MD. – In a pooled analysis of three trials conducted with the transcatheter Carillon Mitral Contour System for mitral valve repair, the 5-year survival is 56.2%, which is an encouraging outcome that justifies the ongoing multinational pivotal Carillon trial, according to the principal investigator of the analysis presented at CRT 2020 sponsored by MedStar Heart & Vascular Institute.
In patients with functional mitral valve regurgitation (FMR), “the Carillon device shows extremely encouraging long-term mortality data from prospective controlled trials in comparison with guideline-directed medical therapy or with the COAPT results,” according to Janusz Lipiecki, MD, PhD, department of cardiology, University Hospital, Clermont-Ferrand, France.
The COAPT trial is an important benchmark, because it was the first large, randomized trial to show benefit for a percutaneous device in the treatment of heart failure patients with moderate to severe FMR (N Engl J Med. 2018;379:2307-18). The study associated the MitraClip with a nearly 40% reduction in all-cause mortality (29.1% vs. 46.1%) at 24 months, relative to guideline-directed medical therapy (GDMT).
The Carillon device, which is also delivered percutaneously, does not engage the valve leaflets to treat FMR. Rather, it is anchored in coronary sinus to reform the mitral annulus. This reduces FMR without damage to the mitral valve, thus preserving the potential for future valve repairs, according to Dr. Lipiecki, who reported that more than 1,100 devices have now been implanted, mostly in Europe.
The data so far are encouraging, said Dr. Lipiecki, who provided survival data in 74 patients followed for at least 5 years. Of these, 23 were drawn from the REDUCE FMR trial, which was blinded and sham controlled, and the remainder from the TITAN and TITAN II studies, which were prospective but not controlled.
In this series of 74 patients, there were no serious complications associated with the procedure, and all achieved a reduction in mitral regurgitation at 12 months, Dr. Lipiecki said. Furthermore, the reduction in FMR was associated with improvements in symptoms and “favorable remodeling” reflected in reduced left ventricular volume, he said.
In this series, the 5-year survival is 56%, which substantially exceeds what would be expected with GDMT, according to Dr. Lipiecki.
There were no baseline predictors of long-term survival, but improvements within the 6 months in functional heart class, 6-minute walk distance (6MWD), and mitral regurgitation were significantly associated with a greater likelihood of being alive at 5 years.
Although there is no comparable follow-up with other devices, including the MitraClip, Dr. Lipiecki did compare the 67.9% survival at 3 years in this series to that of the COAPT trial. He restricted the comparison to those treated for grade 3+ or 4+ mitral regurgitation. At 36 months, survival rates were 57.2% and 44.5% for those treated with MitraClip and GDMT, respectively.
“COAPT patients might not be comparable for a variety of reasons, including the anatomic restrictions important to the use of either of these devices,” Dr. Lipiecki acknowledged, but he said the long-term data with the Carillon device provide support for the pivotal Carillon trial now enrolling.
In this blinded trial, more than 350 patients at 75 sites are being randomized to placement of the Carillon device, which has been available in Europe since 2011, or a sham procedure. The trial is scheduled for completion in 2025.
NATIONAL HARBOR, MD. – In a pooled analysis of three trials conducted with the transcatheter Carillon Mitral Contour System for mitral valve repair, the 5-year survival is 56.2%, which is an encouraging outcome that justifies the ongoing multinational pivotal Carillon trial, according to the principal investigator of the analysis presented at CRT 2020 sponsored by MedStar Heart & Vascular Institute.
In patients with functional mitral valve regurgitation (FMR), “the Carillon device shows extremely encouraging long-term mortality data from prospective controlled trials in comparison with guideline-directed medical therapy or with the COAPT results,” according to Janusz Lipiecki, MD, PhD, department of cardiology, University Hospital, Clermont-Ferrand, France.
The COAPT trial is an important benchmark, because it was the first large, randomized trial to show benefit for a percutaneous device in the treatment of heart failure patients with moderate to severe FMR (N Engl J Med. 2018;379:2307-18). The study associated the MitraClip with a nearly 40% reduction in all-cause mortality (29.1% vs. 46.1%) at 24 months, relative to guideline-directed medical therapy (GDMT).
The Carillon device, which is also delivered percutaneously, does not engage the valve leaflets to treat FMR. Rather, it is anchored in coronary sinus to reform the mitral annulus. This reduces FMR without damage to the mitral valve, thus preserving the potential for future valve repairs, according to Dr. Lipiecki, who reported that more than 1,100 devices have now been implanted, mostly in Europe.
The data so far are encouraging, said Dr. Lipiecki, who provided survival data in 74 patients followed for at least 5 years. Of these, 23 were drawn from the REDUCE FMR trial, which was blinded and sham controlled, and the remainder from the TITAN and TITAN II studies, which were prospective but not controlled.
In this series of 74 patients, there were no serious complications associated with the procedure, and all achieved a reduction in mitral regurgitation at 12 months, Dr. Lipiecki said. Furthermore, the reduction in FMR was associated with improvements in symptoms and “favorable remodeling” reflected in reduced left ventricular volume, he said.
In this series, the 5-year survival is 56%, which substantially exceeds what would be expected with GDMT, according to Dr. Lipiecki.
There were no baseline predictors of long-term survival, but improvements within the 6 months in functional heart class, 6-minute walk distance (6MWD), and mitral regurgitation were significantly associated with a greater likelihood of being alive at 5 years.
Although there is no comparable follow-up with other devices, including the MitraClip, Dr. Lipiecki did compare the 67.9% survival at 3 years in this series to that of the COAPT trial. He restricted the comparison to those treated for grade 3+ or 4+ mitral regurgitation. At 36 months, survival rates were 57.2% and 44.5% for those treated with MitraClip and GDMT, respectively.
“COAPT patients might not be comparable for a variety of reasons, including the anatomic restrictions important to the use of either of these devices,” Dr. Lipiecki acknowledged, but he said the long-term data with the Carillon device provide support for the pivotal Carillon trial now enrolling.
In this blinded trial, more than 350 patients at 75 sites are being randomized to placement of the Carillon device, which has been available in Europe since 2011, or a sham procedure. The trial is scheduled for completion in 2025.
REPORTING FROM CRT 2020
Societies dig in to EXCEL trial controversy
Thoracic surgery societies on both sides of the Atlantic have released new statements on a continuing controversy dogging the EXCEL trial, one that has fueled a highly public war of words over how the study was conducted, interpreted, and reported by its investigators.
In a statement dated Dec. 19, 2019, the European Association for Cardio-Thoracic Surgery (EACTS) offered new details on why it withdrew its endorsement of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines section covering left-main coronary artery disease.
That part of the guideline had relied in part on 3-year outcomes from EXCEL, which were published in the New England Journal of Medicine in 2016 (2016 Dec 8;375[23]:2223-35) and are central to the ongoing dispute. The trial, in essence, was a comparison of percutaneous coronary intervention (PCI) and coronary bypass surgery (CABG) in left-main disease. In that report, PCI was noninferior to CABG with respect to the composite endpoint of death, stroke, or myocardial infarction at 3 years in patients with left-main disease and low or intermediate anatomical complexity.
The new statement, signed by the society’s secretary general Domenico Pagano, MD, also calls for a new EACTS-ESC evidence review and development of updated recommendations for left-main disease “as a matter of urgency.”
For its part, the ESC had earlier declared its continuing support for the full guideline but hinted that might change pending further details on EXCEL yet to be made public.
The EACTS statement follows the society’s earlier announcement that it would pull support of the guideline section on left-main disease in response to a Dec. 9, 2019, news report from BBC Newsnight that was critical of the EXCEL trial’s methodology and reporting.
The news story made a number of allegations regarding the interpretation and reporting of EXCEL based largely on unpublished data it had obtained through unofficial channels.
Key among them was that reanalysis of myocardial infarction outcomes using the Third Universal Definition of MI, rather than the primarily enzymatic definition on which the reported outcomes were based, substantially raised the MI count in the PCI group, compared with those who had CABG.
The data for that alternative analysis, which had not been publicly reported, seemed to recast the published EXCEL primary outcome from one of parity for PCI and CABG in left-main disease to one that significantly favored CABG, noted the BBC Newsnight story.
Also, the news story claimed that EXCEL investigators had promised to publicly release the trial’s data based on the Third Universal Definition of MI, but had not done so, and had not adequately heeded concerns raised by its Data Safety Monitoring Board (DSMB) over signs of an apparently increased mortality risk from PCI.
Another society weighs in
The unreported data and other issues have led the American Association for Thoracic Surgery (AATS) to issue a statement acknowledging the possibility of misguided treatment recommendations, and therefore patient care, stemming from incomplete reporting of EXCEL.
If there are serious concerns about the “presentation or interpretation” of clinical trials, “then the best way forward is the public release of all trial data for an independent analysis to confirm that the original trial conclusions are valid,” says the statement, signed by AATS president Vaughn A. Starnes, MD, and secretary David R. Jones, MD.
“The AATS agrees with others that all of the data should be made publicly available for analysis and interpretation, as a way to resolve the current controversy around the EXCEL trial, in order to provide patients with the best possible counsel and informed consent,” it states.
The BBC Newsnight story “raised legitimate questions regarding what data was/was not presented to the other EXCEL investigators and to [the] ESC/EACTS guideline committee, and what, when, and to whom were safety warnings raised by the DSMB,” David Taggart, MD, PhD, wrote in an email interview.
“Until these issues are resolved, both EACTS and AATS have expressed concerns about what has happened and, most importantly, the potential implications for patient safety. This stance underpins their sincerity that patient safety, genuine informed consent, and scientific integrity are amongst their highest priorities. Consequently they have my complete support,” said Dr. Taggart, of the University of Oxford (England) a former EXCEL trialist who has been among the most vocal critics of how the EXCEL leadership has interpreted and reported the trial’s outcomes.
“Personally, I do not feel that the current controversy over the EXCEL trial will be resolved until there is full and independent reanalysis of its data. I feel that this would be absolutely crucial in reassuring our patients, the wider medical community, and the general public of the validity of current recommendations.”
An EXCEL principal investigator and prominent public voice for the trial, Gregg W. Stone, MD, of Icahn School of Medicine at Mount Sinai, New York, has not responded to requests for comment on the new society statements.
Point-counterpoint
As previously reported, allegations about EXCEL in news reports and the sometimes fiery public debate led the trialists to release a long and wide-ranging public communique that forcefully disputes the charges. Among them, that they were either remiss or willfully deceptive in not reporting an analysis based on the Third Universal Definition of MI.
In response, Dr. Taggart provided a toughly worded statement that disputes the EXCEL leadership’s missive nearly point by point. It variously describes the assertions as “simplistic,” seemingly “illogical,” “disingenuous,” and “factually completely incorrect,” among other terms.
The document provides Dr. Taggart’s perspective on how MI was defined and interpreted while he was an active member of the EXCEL trial’s leadership, and alleged shortfalls in how outcomes were interpreted and reported.
In it, Taggart also wonders whether or not EXCEL leadership had possibly been aware of a tilt favoring CABG in the analysis based on Third Universal Definition of MI but “decided to suppress it,” and also whether the trial’s sponsor, Abbott Vascular, had influenced the trial’s conduct.
Despite the EXCEL leadership’s communique, “my profound concerns remain the same and, in my opinion, the very long rebuttal response by the EXCEL investigators does not adequately respond to the core issues,” Dr. Taggart writes.
He withdrew his name as an author on the trial’s 5-year outcomes publication, Dr. Taggart says, because “I believed, and still do, that the final interpretation of the actual data in the [New England Journal of Medicine] manuscript did not appropriately reflect its clinical reality, and especially with regards to mortality, and would therefore have potential to do real harm to patients.”
Dr. Taggart has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.
Thoracic surgery societies on both sides of the Atlantic have released new statements on a continuing controversy dogging the EXCEL trial, one that has fueled a highly public war of words over how the study was conducted, interpreted, and reported by its investigators.
In a statement dated Dec. 19, 2019, the European Association for Cardio-Thoracic Surgery (EACTS) offered new details on why it withdrew its endorsement of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines section covering left-main coronary artery disease.
That part of the guideline had relied in part on 3-year outcomes from EXCEL, which were published in the New England Journal of Medicine in 2016 (2016 Dec 8;375[23]:2223-35) and are central to the ongoing dispute. The trial, in essence, was a comparison of percutaneous coronary intervention (PCI) and coronary bypass surgery (CABG) in left-main disease. In that report, PCI was noninferior to CABG with respect to the composite endpoint of death, stroke, or myocardial infarction at 3 years in patients with left-main disease and low or intermediate anatomical complexity.
The new statement, signed by the society’s secretary general Domenico Pagano, MD, also calls for a new EACTS-ESC evidence review and development of updated recommendations for left-main disease “as a matter of urgency.”
For its part, the ESC had earlier declared its continuing support for the full guideline but hinted that might change pending further details on EXCEL yet to be made public.
The EACTS statement follows the society’s earlier announcement that it would pull support of the guideline section on left-main disease in response to a Dec. 9, 2019, news report from BBC Newsnight that was critical of the EXCEL trial’s methodology and reporting.
The news story made a number of allegations regarding the interpretation and reporting of EXCEL based largely on unpublished data it had obtained through unofficial channels.
Key among them was that reanalysis of myocardial infarction outcomes using the Third Universal Definition of MI, rather than the primarily enzymatic definition on which the reported outcomes were based, substantially raised the MI count in the PCI group, compared with those who had CABG.
The data for that alternative analysis, which had not been publicly reported, seemed to recast the published EXCEL primary outcome from one of parity for PCI and CABG in left-main disease to one that significantly favored CABG, noted the BBC Newsnight story.
Also, the news story claimed that EXCEL investigators had promised to publicly release the trial’s data based on the Third Universal Definition of MI, but had not done so, and had not adequately heeded concerns raised by its Data Safety Monitoring Board (DSMB) over signs of an apparently increased mortality risk from PCI.
Another society weighs in
The unreported data and other issues have led the American Association for Thoracic Surgery (AATS) to issue a statement acknowledging the possibility of misguided treatment recommendations, and therefore patient care, stemming from incomplete reporting of EXCEL.
If there are serious concerns about the “presentation or interpretation” of clinical trials, “then the best way forward is the public release of all trial data for an independent analysis to confirm that the original trial conclusions are valid,” says the statement, signed by AATS president Vaughn A. Starnes, MD, and secretary David R. Jones, MD.
“The AATS agrees with others that all of the data should be made publicly available for analysis and interpretation, as a way to resolve the current controversy around the EXCEL trial, in order to provide patients with the best possible counsel and informed consent,” it states.
The BBC Newsnight story “raised legitimate questions regarding what data was/was not presented to the other EXCEL investigators and to [the] ESC/EACTS guideline committee, and what, when, and to whom were safety warnings raised by the DSMB,” David Taggart, MD, PhD, wrote in an email interview.
“Until these issues are resolved, both EACTS and AATS have expressed concerns about what has happened and, most importantly, the potential implications for patient safety. This stance underpins their sincerity that patient safety, genuine informed consent, and scientific integrity are amongst their highest priorities. Consequently they have my complete support,” said Dr. Taggart, of the University of Oxford (England) a former EXCEL trialist who has been among the most vocal critics of how the EXCEL leadership has interpreted and reported the trial’s outcomes.
“Personally, I do not feel that the current controversy over the EXCEL trial will be resolved until there is full and independent reanalysis of its data. I feel that this would be absolutely crucial in reassuring our patients, the wider medical community, and the general public of the validity of current recommendations.”
An EXCEL principal investigator and prominent public voice for the trial, Gregg W. Stone, MD, of Icahn School of Medicine at Mount Sinai, New York, has not responded to requests for comment on the new society statements.
Point-counterpoint
As previously reported, allegations about EXCEL in news reports and the sometimes fiery public debate led the trialists to release a long and wide-ranging public communique that forcefully disputes the charges. Among them, that they were either remiss or willfully deceptive in not reporting an analysis based on the Third Universal Definition of MI.
In response, Dr. Taggart provided a toughly worded statement that disputes the EXCEL leadership’s missive nearly point by point. It variously describes the assertions as “simplistic,” seemingly “illogical,” “disingenuous,” and “factually completely incorrect,” among other terms.
The document provides Dr. Taggart’s perspective on how MI was defined and interpreted while he was an active member of the EXCEL trial’s leadership, and alleged shortfalls in how outcomes were interpreted and reported.
In it, Taggart also wonders whether or not EXCEL leadership had possibly been aware of a tilt favoring CABG in the analysis based on Third Universal Definition of MI but “decided to suppress it,” and also whether the trial’s sponsor, Abbott Vascular, had influenced the trial’s conduct.
Despite the EXCEL leadership’s communique, “my profound concerns remain the same and, in my opinion, the very long rebuttal response by the EXCEL investigators does not adequately respond to the core issues,” Dr. Taggart writes.
He withdrew his name as an author on the trial’s 5-year outcomes publication, Dr. Taggart says, because “I believed, and still do, that the final interpretation of the actual data in the [New England Journal of Medicine] manuscript did not appropriately reflect its clinical reality, and especially with regards to mortality, and would therefore have potential to do real harm to patients.”
Dr. Taggart has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.
Thoracic surgery societies on both sides of the Atlantic have released new statements on a continuing controversy dogging the EXCEL trial, one that has fueled a highly public war of words over how the study was conducted, interpreted, and reported by its investigators.
In a statement dated Dec. 19, 2019, the European Association for Cardio-Thoracic Surgery (EACTS) offered new details on why it withdrew its endorsement of the 2018 EACTS-European Society of Cardiology (ESC) clinical guidelines section covering left-main coronary artery disease.
That part of the guideline had relied in part on 3-year outcomes from EXCEL, which were published in the New England Journal of Medicine in 2016 (2016 Dec 8;375[23]:2223-35) and are central to the ongoing dispute. The trial, in essence, was a comparison of percutaneous coronary intervention (PCI) and coronary bypass surgery (CABG) in left-main disease. In that report, PCI was noninferior to CABG with respect to the composite endpoint of death, stroke, or myocardial infarction at 3 years in patients with left-main disease and low or intermediate anatomical complexity.
The new statement, signed by the society’s secretary general Domenico Pagano, MD, also calls for a new EACTS-ESC evidence review and development of updated recommendations for left-main disease “as a matter of urgency.”
For its part, the ESC had earlier declared its continuing support for the full guideline but hinted that might change pending further details on EXCEL yet to be made public.
The EACTS statement follows the society’s earlier announcement that it would pull support of the guideline section on left-main disease in response to a Dec. 9, 2019, news report from BBC Newsnight that was critical of the EXCEL trial’s methodology and reporting.
The news story made a number of allegations regarding the interpretation and reporting of EXCEL based largely on unpublished data it had obtained through unofficial channels.
Key among them was that reanalysis of myocardial infarction outcomes using the Third Universal Definition of MI, rather than the primarily enzymatic definition on which the reported outcomes were based, substantially raised the MI count in the PCI group, compared with those who had CABG.
The data for that alternative analysis, which had not been publicly reported, seemed to recast the published EXCEL primary outcome from one of parity for PCI and CABG in left-main disease to one that significantly favored CABG, noted the BBC Newsnight story.
Also, the news story claimed that EXCEL investigators had promised to publicly release the trial’s data based on the Third Universal Definition of MI, but had not done so, and had not adequately heeded concerns raised by its Data Safety Monitoring Board (DSMB) over signs of an apparently increased mortality risk from PCI.
Another society weighs in
The unreported data and other issues have led the American Association for Thoracic Surgery (AATS) to issue a statement acknowledging the possibility of misguided treatment recommendations, and therefore patient care, stemming from incomplete reporting of EXCEL.
If there are serious concerns about the “presentation or interpretation” of clinical trials, “then the best way forward is the public release of all trial data for an independent analysis to confirm that the original trial conclusions are valid,” says the statement, signed by AATS president Vaughn A. Starnes, MD, and secretary David R. Jones, MD.
“The AATS agrees with others that all of the data should be made publicly available for analysis and interpretation, as a way to resolve the current controversy around the EXCEL trial, in order to provide patients with the best possible counsel and informed consent,” it states.
The BBC Newsnight story “raised legitimate questions regarding what data was/was not presented to the other EXCEL investigators and to [the] ESC/EACTS guideline committee, and what, when, and to whom were safety warnings raised by the DSMB,” David Taggart, MD, PhD, wrote in an email interview.
“Until these issues are resolved, both EACTS and AATS have expressed concerns about what has happened and, most importantly, the potential implications for patient safety. This stance underpins their sincerity that patient safety, genuine informed consent, and scientific integrity are amongst their highest priorities. Consequently they have my complete support,” said Dr. Taggart, of the University of Oxford (England) a former EXCEL trialist who has been among the most vocal critics of how the EXCEL leadership has interpreted and reported the trial’s outcomes.
“Personally, I do not feel that the current controversy over the EXCEL trial will be resolved until there is full and independent reanalysis of its data. I feel that this would be absolutely crucial in reassuring our patients, the wider medical community, and the general public of the validity of current recommendations.”
An EXCEL principal investigator and prominent public voice for the trial, Gregg W. Stone, MD, of Icahn School of Medicine at Mount Sinai, New York, has not responded to requests for comment on the new society statements.
Point-counterpoint
As previously reported, allegations about EXCEL in news reports and the sometimes fiery public debate led the trialists to release a long and wide-ranging public communique that forcefully disputes the charges. Among them, that they were either remiss or willfully deceptive in not reporting an analysis based on the Third Universal Definition of MI.
In response, Dr. Taggart provided a toughly worded statement that disputes the EXCEL leadership’s missive nearly point by point. It variously describes the assertions as “simplistic,” seemingly “illogical,” “disingenuous,” and “factually completely incorrect,” among other terms.
The document provides Dr. Taggart’s perspective on how MI was defined and interpreted while he was an active member of the EXCEL trial’s leadership, and alleged shortfalls in how outcomes were interpreted and reported.
In it, Taggart also wonders whether or not EXCEL leadership had possibly been aware of a tilt favoring CABG in the analysis based on Third Universal Definition of MI but “decided to suppress it,” and also whether the trial’s sponsor, Abbott Vascular, had influenced the trial’s conduct.
Despite the EXCEL leadership’s communique, “my profound concerns remain the same and, in my opinion, the very long rebuttal response by the EXCEL investigators does not adequately respond to the core issues,” Dr. Taggart writes.
He withdrew his name as an author on the trial’s 5-year outcomes publication, Dr. Taggart says, because “I believed, and still do, that the final interpretation of the actual data in the [New England Journal of Medicine] manuscript did not appropriately reflect its clinical reality, and especially with regards to mortality, and would therefore have potential to do real harm to patients.”
Dr. Taggart has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.
Health benefits of TAVR over SAVR sustained at 1 year
SAN FRANCISCO – Among patients with severe aortic stenosis at low surgical risk, both transcatheter and surgical aortic valve replacement resulted in substantial health status benefits at 1 year despite most patients having New York Heart Association class I or II symptoms at baseline.
However, when compared with surgical replacement,
The findings come from an analysis of patients enrolled in the randomized PARTNER 3 trial, which showed that transcatheter aortic valve replacement (TAVR) with the SAPIEN 3 valve. At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with surgical aortic valve replacement (SAVR), for a highly significant 46% relative risk reduction (N Engl J Med 2019 May 2;380:1695-705).
“The PARTNER 3 and Evolut Low Risk trials have demonstrated that transfemoral TAVR is both safe and effective when compared with SAVR in patients with severe aortic stenosis at low surgical risk,” Suzanne J. Baron, MD, MSc, said at the Transcatheter Cardiovascular Therapeutics annual meeting. “While prior studies have demonstrated improved early health status with transfemoral TAVR, compared with SAVR in intermediate and high-risk patients, there is little evidence of any late health status benefit with TAVR.”
To address this gap in knowledge, Dr. Baron, director of interventional cardiology research at Lahey Hospital and Medical Center in Burlington, Mass., and associates performed a prospective study alongside the PARTNER 3 randomized trial to understand the impact of valve replacement strategy on early and late health status in aortic stenosis patients at low surgical risk. She reported results from 449 low-risk patients with severe aortic stenosis who were assigned to transfemoral TAVR using a balloon-expandable valve, and 449 who were assigned to surgery in PARTNER 3. At baseline, the mean age of patients was 73 years, 69% were male, and the average STS (Society of Thoracic Surgeons) Risk Score was 1.9%. Rates of other comorbidities were generally low.
Patients in both groups reported a mild baseline impairment in health status. The mean Kansas City Cardiomyopathy Questionnaire–Overall Summary (KCCQ-OS) score was 70, “which corresponds to only New York Heart Association Class II symptoms,” Dr. Baron said. “The SF-36 [Short Form 36] physical summary score was 44 for both groups, which is approximately half of a standard deviation below the population mean.”
As expected, patients who underwent TAVR showed substantially improved health status at 1 month based on the KCCQ-OS (mean difference,16 points; P less than .001). However, in contrast to prior studies, the researchers observed a persistent, although attenuated, benefit of TAVR over SAVR in disease-specific health status at 6 and 12 months (mean difference in KCCQ-OS of 2.6 and 1.8 points respectively; P less than .04 for both).
Dr. Baron said that a sustained benefit of TAVR over SAVR at 6 months and 1 year was observed on several KCCQ subscales, but a similar benefit was not noted on the generic health status measures such as the SF-36 physical summary score. “That’s likely reflective of the fact that, as a disease-specific measure, the KCCQ is much more sensitive in detecting meaningful differences in this population,” she explained. When change in health status was analyzed as an ordinal variable, with death as the worst outcome and large clinical improvement, which was defined as a 20-point or greater increase in the KCCQ-OS score, TAVR showed a significant benefit, compared with surgery at all time points (P less than .05).
In an effort to better understand the mechanism underlying this persistent albeit small late benefit in disease-specific health status with TAVR, the researchers generated cumulative distribution curves to display the proportion of patients who achieved a given change on the KCCQ-OS. A clear separation of the curves emerged, with 5.2% more patients in the TAVR group experiencing a change of at least 20 points, compared with the surgery group. “This suggests that the difference in late health status between the two groups is driven by this 5.2% absolute risk difference in the proportion of patients who experienced a large clinical improvement,” Dr. Baron said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Next, the researchers performed subgroup analyses to examine the interaction between the 1-year health status benefit of TAVR over surgery and prespecified baseline characteristics including age, gender, STS risk score, ejection fraction, atrial fibrillation, and New York Heart Association (NYHA) class. They observed a significant interaction between NYHA class and treatment effect such that patients who had NYHA class III or IV symptoms at baseline derived greater benefit from TAVR, compared with those who had NYHA class I or II symptoms at baseline.
“This finding suggests that it’s the patients with worse functional impairment at baseline who may be that subset of patients on the cumulative responder curves who gained better health status outcomes with TAVR, compared with surgery in the low-risk population,” Dr. Baron said.
Suzanne V. Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo., who was an invited discussant, said that it was “remarkable” that patients in the substudy were not particularly symptomatic and yet they still experienced close to a 20-point improvement in the KCCQ-OS score following TAVR, and asked whether frailty may have played a role in the 1.8-point adjusted difference in the KCCQ-OS score between TAVR and surgery at 1 year. Dr. Baron responded that she and her colleagues performed a subgroup analysis of patients who had two or more markers of frailty versus those who had one or less. Noting that there were only 20 patients in that subgroup, she said there was a significant signal that patients who were considered have two or more frail measures were considered to do much better with TAVR.
Dr. Baron concluded that the study’s overall findings, taken together with the clinical outcomes of the PARTNER 3 trial, “further support the use of TAVR in patients with severe [aortic stenosis] at low surgical risk. Longer-term follow up is needed (and ongoing) to determine whether the health status benefits of TAVR at 1 year are durable.”
The content of the study was published online at the time of presentation (J Am Coll Cardiol 2019 Sep 29. doi: 10.1016/j.jacc.2019.09.007). The PARTNER 3 quality of life substudy was funded by Edwards Lifesciences. Dr. Baron disclosed research funding and advisory board compensation from Boston Scientific Corp and consulting fees from Edwards Lifesciences.
SAN FRANCISCO – Among patients with severe aortic stenosis at low surgical risk, both transcatheter and surgical aortic valve replacement resulted in substantial health status benefits at 1 year despite most patients having New York Heart Association class I or II symptoms at baseline.
However, when compared with surgical replacement,
The findings come from an analysis of patients enrolled in the randomized PARTNER 3 trial, which showed that transcatheter aortic valve replacement (TAVR) with the SAPIEN 3 valve. At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with surgical aortic valve replacement (SAVR), for a highly significant 46% relative risk reduction (N Engl J Med 2019 May 2;380:1695-705).
“The PARTNER 3 and Evolut Low Risk trials have demonstrated that transfemoral TAVR is both safe and effective when compared with SAVR in patients with severe aortic stenosis at low surgical risk,” Suzanne J. Baron, MD, MSc, said at the Transcatheter Cardiovascular Therapeutics annual meeting. “While prior studies have demonstrated improved early health status with transfemoral TAVR, compared with SAVR in intermediate and high-risk patients, there is little evidence of any late health status benefit with TAVR.”
To address this gap in knowledge, Dr. Baron, director of interventional cardiology research at Lahey Hospital and Medical Center in Burlington, Mass., and associates performed a prospective study alongside the PARTNER 3 randomized trial to understand the impact of valve replacement strategy on early and late health status in aortic stenosis patients at low surgical risk. She reported results from 449 low-risk patients with severe aortic stenosis who were assigned to transfemoral TAVR using a balloon-expandable valve, and 449 who were assigned to surgery in PARTNER 3. At baseline, the mean age of patients was 73 years, 69% were male, and the average STS (Society of Thoracic Surgeons) Risk Score was 1.9%. Rates of other comorbidities were generally low.
Patients in both groups reported a mild baseline impairment in health status. The mean Kansas City Cardiomyopathy Questionnaire–Overall Summary (KCCQ-OS) score was 70, “which corresponds to only New York Heart Association Class II symptoms,” Dr. Baron said. “The SF-36 [Short Form 36] physical summary score was 44 for both groups, which is approximately half of a standard deviation below the population mean.”
As expected, patients who underwent TAVR showed substantially improved health status at 1 month based on the KCCQ-OS (mean difference,16 points; P less than .001). However, in contrast to prior studies, the researchers observed a persistent, although attenuated, benefit of TAVR over SAVR in disease-specific health status at 6 and 12 months (mean difference in KCCQ-OS of 2.6 and 1.8 points respectively; P less than .04 for both).
Dr. Baron said that a sustained benefit of TAVR over SAVR at 6 months and 1 year was observed on several KCCQ subscales, but a similar benefit was not noted on the generic health status measures such as the SF-36 physical summary score. “That’s likely reflective of the fact that, as a disease-specific measure, the KCCQ is much more sensitive in detecting meaningful differences in this population,” she explained. When change in health status was analyzed as an ordinal variable, with death as the worst outcome and large clinical improvement, which was defined as a 20-point or greater increase in the KCCQ-OS score, TAVR showed a significant benefit, compared with surgery at all time points (P less than .05).
In an effort to better understand the mechanism underlying this persistent albeit small late benefit in disease-specific health status with TAVR, the researchers generated cumulative distribution curves to display the proportion of patients who achieved a given change on the KCCQ-OS. A clear separation of the curves emerged, with 5.2% more patients in the TAVR group experiencing a change of at least 20 points, compared with the surgery group. “This suggests that the difference in late health status between the two groups is driven by this 5.2% absolute risk difference in the proportion of patients who experienced a large clinical improvement,” Dr. Baron said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Next, the researchers performed subgroup analyses to examine the interaction between the 1-year health status benefit of TAVR over surgery and prespecified baseline characteristics including age, gender, STS risk score, ejection fraction, atrial fibrillation, and New York Heart Association (NYHA) class. They observed a significant interaction between NYHA class and treatment effect such that patients who had NYHA class III or IV symptoms at baseline derived greater benefit from TAVR, compared with those who had NYHA class I or II symptoms at baseline.
“This finding suggests that it’s the patients with worse functional impairment at baseline who may be that subset of patients on the cumulative responder curves who gained better health status outcomes with TAVR, compared with surgery in the low-risk population,” Dr. Baron said.
Suzanne V. Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo., who was an invited discussant, said that it was “remarkable” that patients in the substudy were not particularly symptomatic and yet they still experienced close to a 20-point improvement in the KCCQ-OS score following TAVR, and asked whether frailty may have played a role in the 1.8-point adjusted difference in the KCCQ-OS score between TAVR and surgery at 1 year. Dr. Baron responded that she and her colleagues performed a subgroup analysis of patients who had two or more markers of frailty versus those who had one or less. Noting that there were only 20 patients in that subgroup, she said there was a significant signal that patients who were considered have two or more frail measures were considered to do much better with TAVR.
Dr. Baron concluded that the study’s overall findings, taken together with the clinical outcomes of the PARTNER 3 trial, “further support the use of TAVR in patients with severe [aortic stenosis] at low surgical risk. Longer-term follow up is needed (and ongoing) to determine whether the health status benefits of TAVR at 1 year are durable.”
The content of the study was published online at the time of presentation (J Am Coll Cardiol 2019 Sep 29. doi: 10.1016/j.jacc.2019.09.007). The PARTNER 3 quality of life substudy was funded by Edwards Lifesciences. Dr. Baron disclosed research funding and advisory board compensation from Boston Scientific Corp and consulting fees from Edwards Lifesciences.
SAN FRANCISCO – Among patients with severe aortic stenosis at low surgical risk, both transcatheter and surgical aortic valve replacement resulted in substantial health status benefits at 1 year despite most patients having New York Heart Association class I or II symptoms at baseline.
However, when compared with surgical replacement,
The findings come from an analysis of patients enrolled in the randomized PARTNER 3 trial, which showed that transcatheter aortic valve replacement (TAVR) with the SAPIEN 3 valve. At 1 year post procedure, the rate of the primary composite endpoint comprising death, stroke, or cardiovascular rehospitalization was 8.5% in the TAVR group and 15.1% with surgical aortic valve replacement (SAVR), for a highly significant 46% relative risk reduction (N Engl J Med 2019 May 2;380:1695-705).
“The PARTNER 3 and Evolut Low Risk trials have demonstrated that transfemoral TAVR is both safe and effective when compared with SAVR in patients with severe aortic stenosis at low surgical risk,” Suzanne J. Baron, MD, MSc, said at the Transcatheter Cardiovascular Therapeutics annual meeting. “While prior studies have demonstrated improved early health status with transfemoral TAVR, compared with SAVR in intermediate and high-risk patients, there is little evidence of any late health status benefit with TAVR.”
To address this gap in knowledge, Dr. Baron, director of interventional cardiology research at Lahey Hospital and Medical Center in Burlington, Mass., and associates performed a prospective study alongside the PARTNER 3 randomized trial to understand the impact of valve replacement strategy on early and late health status in aortic stenosis patients at low surgical risk. She reported results from 449 low-risk patients with severe aortic stenosis who were assigned to transfemoral TAVR using a balloon-expandable valve, and 449 who were assigned to surgery in PARTNER 3. At baseline, the mean age of patients was 73 years, 69% were male, and the average STS (Society of Thoracic Surgeons) Risk Score was 1.9%. Rates of other comorbidities were generally low.
Patients in both groups reported a mild baseline impairment in health status. The mean Kansas City Cardiomyopathy Questionnaire–Overall Summary (KCCQ-OS) score was 70, “which corresponds to only New York Heart Association Class II symptoms,” Dr. Baron said. “The SF-36 [Short Form 36] physical summary score was 44 for both groups, which is approximately half of a standard deviation below the population mean.”
As expected, patients who underwent TAVR showed substantially improved health status at 1 month based on the KCCQ-OS (mean difference,16 points; P less than .001). However, in contrast to prior studies, the researchers observed a persistent, although attenuated, benefit of TAVR over SAVR in disease-specific health status at 6 and 12 months (mean difference in KCCQ-OS of 2.6 and 1.8 points respectively; P less than .04 for both).
Dr. Baron said that a sustained benefit of TAVR over SAVR at 6 months and 1 year was observed on several KCCQ subscales, but a similar benefit was not noted on the generic health status measures such as the SF-36 physical summary score. “That’s likely reflective of the fact that, as a disease-specific measure, the KCCQ is much more sensitive in detecting meaningful differences in this population,” she explained. When change in health status was analyzed as an ordinal variable, with death as the worst outcome and large clinical improvement, which was defined as a 20-point or greater increase in the KCCQ-OS score, TAVR showed a significant benefit, compared with surgery at all time points (P less than .05).
In an effort to better understand the mechanism underlying this persistent albeit small late benefit in disease-specific health status with TAVR, the researchers generated cumulative distribution curves to display the proportion of patients who achieved a given change on the KCCQ-OS. A clear separation of the curves emerged, with 5.2% more patients in the TAVR group experiencing a change of at least 20 points, compared with the surgery group. “This suggests that the difference in late health status between the two groups is driven by this 5.2% absolute risk difference in the proportion of patients who experienced a large clinical improvement,” Dr. Baron said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Next, the researchers performed subgroup analyses to examine the interaction between the 1-year health status benefit of TAVR over surgery and prespecified baseline characteristics including age, gender, STS risk score, ejection fraction, atrial fibrillation, and New York Heart Association (NYHA) class. They observed a significant interaction between NYHA class and treatment effect such that patients who had NYHA class III or IV symptoms at baseline derived greater benefit from TAVR, compared with those who had NYHA class I or II symptoms at baseline.
“This finding suggests that it’s the patients with worse functional impairment at baseline who may be that subset of patients on the cumulative responder curves who gained better health status outcomes with TAVR, compared with surgery in the low-risk population,” Dr. Baron said.
Suzanne V. Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo., who was an invited discussant, said that it was “remarkable” that patients in the substudy were not particularly symptomatic and yet they still experienced close to a 20-point improvement in the KCCQ-OS score following TAVR, and asked whether frailty may have played a role in the 1.8-point adjusted difference in the KCCQ-OS score between TAVR and surgery at 1 year. Dr. Baron responded that she and her colleagues performed a subgroup analysis of patients who had two or more markers of frailty versus those who had one or less. Noting that there were only 20 patients in that subgroup, she said there was a significant signal that patients who were considered have two or more frail measures were considered to do much better with TAVR.
Dr. Baron concluded that the study’s overall findings, taken together with the clinical outcomes of the PARTNER 3 trial, “further support the use of TAVR in patients with severe [aortic stenosis] at low surgical risk. Longer-term follow up is needed (and ongoing) to determine whether the health status benefits of TAVR at 1 year are durable.”
The content of the study was published online at the time of presentation (J Am Coll Cardiol 2019 Sep 29. doi: 10.1016/j.jacc.2019.09.007). The PARTNER 3 quality of life substudy was funded by Edwards Lifesciences. Dr. Baron disclosed research funding and advisory board compensation from Boston Scientific Corp and consulting fees from Edwards Lifesciences.
REPORTING FROM TCT 2019