User login
FOTS: Minimally invasive esophagectomy viable option to reduce morbidity, mortality
BOSTON – New and innovative methodologies for conducting minimally invasive esophagectomy (MIE) offer significantly lower rates of morbidity and mortality than those normally associated with the procedure, as presented by Dr. James D. Luketich at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting of the American Association for Thoracic Surgery.
While Dr. Luketich spent the bulk of his oral presentation going over the specifics of performing MIE, the accompanying literature of his presentation delved into four key studies – performed and published over the last 12 years – which show the efficacy of MIE over the more traditional approaches to esophagectomy.
“There are several different approaches to esophagectomy in general [but] the technique has evolved partly because the tumors have evolved in the United States,” explained Dr. Luketich, chairman of cardiothoracic surgery at the University of Pittsburgh. “We started off laparoscopic [and] thoracoscopic. In my opinion, that was kind of a bad idea [and] we gave that up pretty early on [...] we’re chest surgeons, we put a thoracoscope in, and we loved it.”
However, as Dr. Luketich explained, the increasing lack of experience from new general surgery residents and attendings caused esophagectomy to become the more attractive option, as it was a procedure that everyone had experience with. This began a search for an effective but minimally invasive approach, which has slowly been cultivated and refined over the years.
Luketich discussed the outcome of his 2003 study assessing 222 consecutive patients who have undergone MIE at the University of Pittsburgh. In that study, patients had lower mortality rates (1.4%) and shorter hospital stays (7 days) than those with “most open series” invasive esophagectomy procedures, with a quality of life score 19 months post operation that was similar to preoperative scores and population norms.
The success of this trial led to the development of the intergroup ECOG 222 trial to determine MIE’s viability in a multicenter setting. Out of 104 patients eligible for MIE, 95 underwent the procedure. Median length of stay in intensive care units was 2 days, and hospital stay was 9 days, with a 2.1% 30-day mortality rate. At 35.8 months (the median follow-up time), the estimated 3-year overall survival was 58.4%.
Similar work was done in 2012, also headed by Dr. Luketich. In this trial, outcomes were evaluated in 1,033 consecutive MIE patients in order to assess the differences between “the modified McKeown minimally invasive approach (videothoracoscopic surgery, laparoscopy, neck anastomosis [MIE-neck]) with our current approach [and] a modified Ivor Lewis approach (laparoscopy, videothoracoscopic surgery, chest anastomosis [MIE-chest]).” MIE-neck was performed on 481 (48%) subjects and MIE-chest on 530 (52%) subjects.
Both procedures had similar median length of stay in hospital (8 days) and in the intensive care unit (2 days), with slightly lower rates of recurrent nerve injury in the MIE-chest cohort and mortality rate of 0.9%. The median number of lymph nodes resected was 21, and total operative mortality was 1.68%, leading investigators to conclude that MIE was the “preferred approach” for resection (P less than .001).
Dr. Luketich also briefly discussed the findings of a 2012 study by Dr. S.S. Biere – an open-label, randomized controlled trial at five study centers spread across three countries from June 2009 through March 2011. Fifty-six patients were randomized into cohorts receiving open esophagectomy, and 59 received MIE; all patients were aged 18-75 years and had resectable cancer of the esophagus or gastroesophageal junction.
Results showed a statistically significant decrease in postoperative pneumonia in the MIE cohort (9% vs. 29%; relative risk 0.35, P = 0.005), compared with open esophagectomy in the first two weeks after surgery and lower postoperative pulmonary infection in the entire hospital stay. MIE patients also experienced shorter hospital stays (11 vs. 14 days), higher short-term quality of life scores at 6 weeks post surgery, lower postoperative pain scores, lower operative blood loss, and lower rates of early morbidity.
Dr. Luketich disclosed having a “shareholder relationship” with Express Scripts and Intuitive Surgical.
BOSTON – New and innovative methodologies for conducting minimally invasive esophagectomy (MIE) offer significantly lower rates of morbidity and mortality than those normally associated with the procedure, as presented by Dr. James D. Luketich at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting of the American Association for Thoracic Surgery.
While Dr. Luketich spent the bulk of his oral presentation going over the specifics of performing MIE, the accompanying literature of his presentation delved into four key studies – performed and published over the last 12 years – which show the efficacy of MIE over the more traditional approaches to esophagectomy.
“There are several different approaches to esophagectomy in general [but] the technique has evolved partly because the tumors have evolved in the United States,” explained Dr. Luketich, chairman of cardiothoracic surgery at the University of Pittsburgh. “We started off laparoscopic [and] thoracoscopic. In my opinion, that was kind of a bad idea [and] we gave that up pretty early on [...] we’re chest surgeons, we put a thoracoscope in, and we loved it.”
However, as Dr. Luketich explained, the increasing lack of experience from new general surgery residents and attendings caused esophagectomy to become the more attractive option, as it was a procedure that everyone had experience with. This began a search for an effective but minimally invasive approach, which has slowly been cultivated and refined over the years.
Luketich discussed the outcome of his 2003 study assessing 222 consecutive patients who have undergone MIE at the University of Pittsburgh. In that study, patients had lower mortality rates (1.4%) and shorter hospital stays (7 days) than those with “most open series” invasive esophagectomy procedures, with a quality of life score 19 months post operation that was similar to preoperative scores and population norms.
The success of this trial led to the development of the intergroup ECOG 222 trial to determine MIE’s viability in a multicenter setting. Out of 104 patients eligible for MIE, 95 underwent the procedure. Median length of stay in intensive care units was 2 days, and hospital stay was 9 days, with a 2.1% 30-day mortality rate. At 35.8 months (the median follow-up time), the estimated 3-year overall survival was 58.4%.
Similar work was done in 2012, also headed by Dr. Luketich. In this trial, outcomes were evaluated in 1,033 consecutive MIE patients in order to assess the differences between “the modified McKeown minimally invasive approach (videothoracoscopic surgery, laparoscopy, neck anastomosis [MIE-neck]) with our current approach [and] a modified Ivor Lewis approach (laparoscopy, videothoracoscopic surgery, chest anastomosis [MIE-chest]).” MIE-neck was performed on 481 (48%) subjects and MIE-chest on 530 (52%) subjects.
Both procedures had similar median length of stay in hospital (8 days) and in the intensive care unit (2 days), with slightly lower rates of recurrent nerve injury in the MIE-chest cohort and mortality rate of 0.9%. The median number of lymph nodes resected was 21, and total operative mortality was 1.68%, leading investigators to conclude that MIE was the “preferred approach” for resection (P less than .001).
Dr. Luketich also briefly discussed the findings of a 2012 study by Dr. S.S. Biere – an open-label, randomized controlled trial at five study centers spread across three countries from June 2009 through March 2011. Fifty-six patients were randomized into cohorts receiving open esophagectomy, and 59 received MIE; all patients were aged 18-75 years and had resectable cancer of the esophagus or gastroesophageal junction.
Results showed a statistically significant decrease in postoperative pneumonia in the MIE cohort (9% vs. 29%; relative risk 0.35, P = 0.005), compared with open esophagectomy in the first two weeks after surgery and lower postoperative pulmonary infection in the entire hospital stay. MIE patients also experienced shorter hospital stays (11 vs. 14 days), higher short-term quality of life scores at 6 weeks post surgery, lower postoperative pain scores, lower operative blood loss, and lower rates of early morbidity.
Dr. Luketich disclosed having a “shareholder relationship” with Express Scripts and Intuitive Surgical.
BOSTON – New and innovative methodologies for conducting minimally invasive esophagectomy (MIE) offer significantly lower rates of morbidity and mortality than those normally associated with the procedure, as presented by Dr. James D. Luketich at the Focus on Thoracic Surgery: Technical Challenges and Complications meeting of the American Association for Thoracic Surgery.
While Dr. Luketich spent the bulk of his oral presentation going over the specifics of performing MIE, the accompanying literature of his presentation delved into four key studies – performed and published over the last 12 years – which show the efficacy of MIE over the more traditional approaches to esophagectomy.
“There are several different approaches to esophagectomy in general [but] the technique has evolved partly because the tumors have evolved in the United States,” explained Dr. Luketich, chairman of cardiothoracic surgery at the University of Pittsburgh. “We started off laparoscopic [and] thoracoscopic. In my opinion, that was kind of a bad idea [and] we gave that up pretty early on [...] we’re chest surgeons, we put a thoracoscope in, and we loved it.”
However, as Dr. Luketich explained, the increasing lack of experience from new general surgery residents and attendings caused esophagectomy to become the more attractive option, as it was a procedure that everyone had experience with. This began a search for an effective but minimally invasive approach, which has slowly been cultivated and refined over the years.
Luketich discussed the outcome of his 2003 study assessing 222 consecutive patients who have undergone MIE at the University of Pittsburgh. In that study, patients had lower mortality rates (1.4%) and shorter hospital stays (7 days) than those with “most open series” invasive esophagectomy procedures, with a quality of life score 19 months post operation that was similar to preoperative scores and population norms.
The success of this trial led to the development of the intergroup ECOG 222 trial to determine MIE’s viability in a multicenter setting. Out of 104 patients eligible for MIE, 95 underwent the procedure. Median length of stay in intensive care units was 2 days, and hospital stay was 9 days, with a 2.1% 30-day mortality rate. At 35.8 months (the median follow-up time), the estimated 3-year overall survival was 58.4%.
Similar work was done in 2012, also headed by Dr. Luketich. In this trial, outcomes were evaluated in 1,033 consecutive MIE patients in order to assess the differences between “the modified McKeown minimally invasive approach (videothoracoscopic surgery, laparoscopy, neck anastomosis [MIE-neck]) with our current approach [and] a modified Ivor Lewis approach (laparoscopy, videothoracoscopic surgery, chest anastomosis [MIE-chest]).” MIE-neck was performed on 481 (48%) subjects and MIE-chest on 530 (52%) subjects.
Both procedures had similar median length of stay in hospital (8 days) and in the intensive care unit (2 days), with slightly lower rates of recurrent nerve injury in the MIE-chest cohort and mortality rate of 0.9%. The median number of lymph nodes resected was 21, and total operative mortality was 1.68%, leading investigators to conclude that MIE was the “preferred approach” for resection (P less than .001).
Dr. Luketich also briefly discussed the findings of a 2012 study by Dr. S.S. Biere – an open-label, randomized controlled trial at five study centers spread across three countries from June 2009 through March 2011. Fifty-six patients were randomized into cohorts receiving open esophagectomy, and 59 received MIE; all patients were aged 18-75 years and had resectable cancer of the esophagus or gastroesophageal junction.
Results showed a statistically significant decrease in postoperative pneumonia in the MIE cohort (9% vs. 29%; relative risk 0.35, P = 0.005), compared with open esophagectomy in the first two weeks after surgery and lower postoperative pulmonary infection in the entire hospital stay. MIE patients also experienced shorter hospital stays (11 vs. 14 days), higher short-term quality of life scores at 6 weeks post surgery, lower postoperative pain scores, lower operative blood loss, and lower rates of early morbidity.
Dr. Luketich disclosed having a “shareholder relationship” with Express Scripts and Intuitive Surgical.
AT AATS FOCUS ON THORACIC SURGERY: TECHNICAL CHALLENGES AND COMPLICATIONS
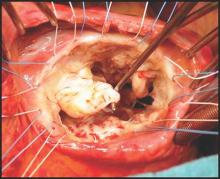
Should annular dilation be a marker for concomitant tricuspid valve repair?
The idea of performing a tricuspid valve repair during a mitral valve procedure has fueled considerable debate among cardiovascular surgeons largely because the grading of tricuspid regurgitation (TR) has been an unreliable marker, so now may be the time to use a new parameter, Dr. Robert Dion of Genk, Belgium, argues in an expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2015 Nov 20;150:1040-3).
“Therefore, we need a parameter hardly depending on preload,” Dr. Dion said. He noted that many authors have validated the use of annual dilatation of 40 mm or 21mm/m2.
Further, preoperative functional New York Heart Association (NYHA) class plays a major role, Dr. Dion said. TR is progressive in nature and the existence of concomitant mitral valve disease can aggravate annular dilation. The earlier surgeons operate on the mitral valve, the less frequently patients will require tricuspid valve repair at the same time, he said.
The controversy was aired in a report at the 2015 American Association for Thoracic Surgery meeting when Dr. Joanna Chikwe of Mount Sinai Hospital in New York discussed an approach that led to tricuspid valve repair at the time of mitral valve surgery in almost two-thirds of patients. Dr. Chikwe and her coauthors opted for concomitant surgery when patients had moderate TR or tricuspid annular dilatation of 40 mm or greater – a strategy that Dr. Dion said was validated because they reported comparable outcomes in terms of death, morbidity, or pacemaker need. The concomitant repair cured TR and prevented progression at seven years of follow-up; and it induced right ventricle recovery and reduced pulmonary hypertension.
In this opinion piece, Dr. Dion took issue with comments made by Dr. Tirone E. David of the University of Toronto during Dr. Chikwe’s AATS presentation. Dr. David, for whom the David reimplantation technique for aortic root replacement is named, called the technique “overkill,” according to Dr. Dion.
Specifically, Dr. Dion questioned Dr. David’s assertions that the use of rigid rings in mitral valve repair causes TR and that no evidence validates the 40-mm diameter minimum in patients with degenerative mitral valve disease. On the first point, Dr. Dion said no evidence has linked the rigidity of the mitral valve ring and progression of tricuspid regurgitation. On the second, Dr. Dion cited eight studies of progressive tricuspid annular dilation with mitral regurgitation, most of which proposed the 40-mm threshold for concomitant tricuspid valve repair. Since then, the 40-mm threshold has been adopted for both European and American guidelines and validated by five reports from 2011 to 2014.
Dr. Dion said the rationale for using annular dilation rather than TR grade rests on “three poles”: annular dilation does not depend on preload whereas the right ventricle does; documented discrepancies between clinical and hemodynamic data (J Cardiol Surg. 1994 Mar;9(2 suppl):237-41; J Am Coll Cardiol. 2004 Feb. 4;43:405-9); and the idea that TR is “bad” for the patient. He also cited disparities in the number of concomitant repairs performed at leading centers: 7%-10% at the Mayo Clinic and Dr. David’s Toronto center, 25% in Leipzig, 40%-45% in his own clinic and two others, and 65% in Dr. Chikwe’s facility.
But early intervention for mitral valve dysfunction is a key indicator of the need for concomitant tricuspid valve repair, Dr. Dion said. “The earlier we operate on the MV, the less frequently patients will require tricuspid valve repair,” he said. In his own approach, Dr. Dion uses a transseptal approach of the mitral valve. For TR greater than grade 2, he performs tricuspid repair using a semirigid ring sized on the area of the anterior leaflet tissue; and if the tenting distance is 8 mm or greater, he includes anterior leaflet augmentation. When TR grade is 2 or less, he also performs concomitant tricuspid repair when the tricuspid annulus is 40 mm or greater or when the tricuspid annulus is 3.5-4 mm in the setting of a host of other cardiac problems, from atrial fibrillation to left valve dysfunction. “Otherwise: abstention,” he said.
“The major issue here is to do everything possible to avoid the risk and outcomes of reoperative tricuspid valve surgery,” Dr. Dion said, citing in-hospital death rates of 13.2% that Dr. David reported (Ann Thorac Surg. 2013 Jan;95:119-24.) and 14.6% the Leipzig group reported (J Thorac Cardiovasc Surg. 2013 Oct; 146:841-7).While he acknowledged calls for a prospective, randomized clinical trial, Dr. Dion said the contraindications for concomitant tricuspid valve repair with mitral valve repair have already been well documented.
Dr. Dion reports consulting fees from Sorin, Edwards, Johnson & Johnson, and St. Jude Medical.
In their invited commentary, Dr. Tirone E. David of the University of Toronto and his colleagues said that performing a tricuspid valve annuloplasty (TVA) in the setting of tricuspid regurgitation (TR) or a tricuspid annulus diameter greater than 40 mm does not completely prevent the onset of new TR (J Thorac Cardiovasc Surg. 2015 Nov;150:1043-4). “Other factors play a role in its development,” they said. “Longstanding atrial fibrillation is one of them.”
“Are patients who have mitral valve (MV) repair for degenerative disease of the MV likely to develop functional TR if there is only trivial or mild TR before surgery?” Dr. David and his coauthors asked. “We are certain that some patients do, but it does not appear to be as common as patients who had MV replacement for rheumatic disease. Is it solely because the incidence of atrial fibrillation is higher in rheumatic patients?”
In a second invited commentary, Dr. Richard J. Shemin of the University of California, Los Angeles, said the discrepancies between the rates of concomitant tricuspid repair among the various centers that Dr. Robert A. Dion cited beg for resolution (J Thorac Cardiovasc Surg. 2015 Nov;150:1045-6). “The wide discrepancy can perhaps be partially resolved with a re-review of the Toronto experience and follow-up,” Dr. Shemin said. “The subset of patients with TVA greater than 40 who were not repaired and the late follow-up would be very helpful.”
The cardiothoracic surgeon faces conflicting principles when considering concomitant tricuspid valve repair, Dr. Shemin said: avoiding an unnecessary surgery when functional TR exists, or leaving a residual lesion that could lead to a risky reoperation. Hence, accurate measurements of the tricuspid valve annulus and TR are essential, Dr. Shemin said.
“The tricuspid valve has been rediscovered and further investigation will resolve the questions,” Dr. Shemin said. Likewise, Dr. David and his colleagues said the “time has come” for a multicentered clinical trial to put the issue to rest for both mitral valve replacement and repair.
In their invited commentary, Dr. Tirone E. David of the University of Toronto and his colleagues said that performing a tricuspid valve annuloplasty (TVA) in the setting of tricuspid regurgitation (TR) or a tricuspid annulus diameter greater than 40 mm does not completely prevent the onset of new TR (J Thorac Cardiovasc Surg. 2015 Nov;150:1043-4). “Other factors play a role in its development,” they said. “Longstanding atrial fibrillation is one of them.”
“Are patients who have mitral valve (MV) repair for degenerative disease of the MV likely to develop functional TR if there is only trivial or mild TR before surgery?” Dr. David and his coauthors asked. “We are certain that some patients do, but it does not appear to be as common as patients who had MV replacement for rheumatic disease. Is it solely because the incidence of atrial fibrillation is higher in rheumatic patients?”
In a second invited commentary, Dr. Richard J. Shemin of the University of California, Los Angeles, said the discrepancies between the rates of concomitant tricuspid repair among the various centers that Dr. Robert A. Dion cited beg for resolution (J Thorac Cardiovasc Surg. 2015 Nov;150:1045-6). “The wide discrepancy can perhaps be partially resolved with a re-review of the Toronto experience and follow-up,” Dr. Shemin said. “The subset of patients with TVA greater than 40 who were not repaired and the late follow-up would be very helpful.”
The cardiothoracic surgeon faces conflicting principles when considering concomitant tricuspid valve repair, Dr. Shemin said: avoiding an unnecessary surgery when functional TR exists, or leaving a residual lesion that could lead to a risky reoperation. Hence, accurate measurements of the tricuspid valve annulus and TR are essential, Dr. Shemin said.
“The tricuspid valve has been rediscovered and further investigation will resolve the questions,” Dr. Shemin said. Likewise, Dr. David and his colleagues said the “time has come” for a multicentered clinical trial to put the issue to rest for both mitral valve replacement and repair.
In their invited commentary, Dr. Tirone E. David of the University of Toronto and his colleagues said that performing a tricuspid valve annuloplasty (TVA) in the setting of tricuspid regurgitation (TR) or a tricuspid annulus diameter greater than 40 mm does not completely prevent the onset of new TR (J Thorac Cardiovasc Surg. 2015 Nov;150:1043-4). “Other factors play a role in its development,” they said. “Longstanding atrial fibrillation is one of them.”
“Are patients who have mitral valve (MV) repair for degenerative disease of the MV likely to develop functional TR if there is only trivial or mild TR before surgery?” Dr. David and his coauthors asked. “We are certain that some patients do, but it does not appear to be as common as patients who had MV replacement for rheumatic disease. Is it solely because the incidence of atrial fibrillation is higher in rheumatic patients?”
In a second invited commentary, Dr. Richard J. Shemin of the University of California, Los Angeles, said the discrepancies between the rates of concomitant tricuspid repair among the various centers that Dr. Robert A. Dion cited beg for resolution (J Thorac Cardiovasc Surg. 2015 Nov;150:1045-6). “The wide discrepancy can perhaps be partially resolved with a re-review of the Toronto experience and follow-up,” Dr. Shemin said. “The subset of patients with TVA greater than 40 who were not repaired and the late follow-up would be very helpful.”
The cardiothoracic surgeon faces conflicting principles when considering concomitant tricuspid valve repair, Dr. Shemin said: avoiding an unnecessary surgery when functional TR exists, or leaving a residual lesion that could lead to a risky reoperation. Hence, accurate measurements of the tricuspid valve annulus and TR are essential, Dr. Shemin said.
“The tricuspid valve has been rediscovered and further investigation will resolve the questions,” Dr. Shemin said. Likewise, Dr. David and his colleagues said the “time has come” for a multicentered clinical trial to put the issue to rest for both mitral valve replacement and repair.
The idea of performing a tricuspid valve repair during a mitral valve procedure has fueled considerable debate among cardiovascular surgeons largely because the grading of tricuspid regurgitation (TR) has been an unreliable marker, so now may be the time to use a new parameter, Dr. Robert Dion of Genk, Belgium, argues in an expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2015 Nov 20;150:1040-3).
“Therefore, we need a parameter hardly depending on preload,” Dr. Dion said. He noted that many authors have validated the use of annual dilatation of 40 mm or 21mm/m2.
Further, preoperative functional New York Heart Association (NYHA) class plays a major role, Dr. Dion said. TR is progressive in nature and the existence of concomitant mitral valve disease can aggravate annular dilation. The earlier surgeons operate on the mitral valve, the less frequently patients will require tricuspid valve repair at the same time, he said.
The controversy was aired in a report at the 2015 American Association for Thoracic Surgery meeting when Dr. Joanna Chikwe of Mount Sinai Hospital in New York discussed an approach that led to tricuspid valve repair at the time of mitral valve surgery in almost two-thirds of patients. Dr. Chikwe and her coauthors opted for concomitant surgery when patients had moderate TR or tricuspid annular dilatation of 40 mm or greater – a strategy that Dr. Dion said was validated because they reported comparable outcomes in terms of death, morbidity, or pacemaker need. The concomitant repair cured TR and prevented progression at seven years of follow-up; and it induced right ventricle recovery and reduced pulmonary hypertension.
In this opinion piece, Dr. Dion took issue with comments made by Dr. Tirone E. David of the University of Toronto during Dr. Chikwe’s AATS presentation. Dr. David, for whom the David reimplantation technique for aortic root replacement is named, called the technique “overkill,” according to Dr. Dion.
Specifically, Dr. Dion questioned Dr. David’s assertions that the use of rigid rings in mitral valve repair causes TR and that no evidence validates the 40-mm diameter minimum in patients with degenerative mitral valve disease. On the first point, Dr. Dion said no evidence has linked the rigidity of the mitral valve ring and progression of tricuspid regurgitation. On the second, Dr. Dion cited eight studies of progressive tricuspid annular dilation with mitral regurgitation, most of which proposed the 40-mm threshold for concomitant tricuspid valve repair. Since then, the 40-mm threshold has been adopted for both European and American guidelines and validated by five reports from 2011 to 2014.
Dr. Dion said the rationale for using annular dilation rather than TR grade rests on “three poles”: annular dilation does not depend on preload whereas the right ventricle does; documented discrepancies between clinical and hemodynamic data (J Cardiol Surg. 1994 Mar;9(2 suppl):237-41; J Am Coll Cardiol. 2004 Feb. 4;43:405-9); and the idea that TR is “bad” for the patient. He also cited disparities in the number of concomitant repairs performed at leading centers: 7%-10% at the Mayo Clinic and Dr. David’s Toronto center, 25% in Leipzig, 40%-45% in his own clinic and two others, and 65% in Dr. Chikwe’s facility.
But early intervention for mitral valve dysfunction is a key indicator of the need for concomitant tricuspid valve repair, Dr. Dion said. “The earlier we operate on the MV, the less frequently patients will require tricuspid valve repair,” he said. In his own approach, Dr. Dion uses a transseptal approach of the mitral valve. For TR greater than grade 2, he performs tricuspid repair using a semirigid ring sized on the area of the anterior leaflet tissue; and if the tenting distance is 8 mm or greater, he includes anterior leaflet augmentation. When TR grade is 2 or less, he also performs concomitant tricuspid repair when the tricuspid annulus is 40 mm or greater or when the tricuspid annulus is 3.5-4 mm in the setting of a host of other cardiac problems, from atrial fibrillation to left valve dysfunction. “Otherwise: abstention,” he said.
“The major issue here is to do everything possible to avoid the risk and outcomes of reoperative tricuspid valve surgery,” Dr. Dion said, citing in-hospital death rates of 13.2% that Dr. David reported (Ann Thorac Surg. 2013 Jan;95:119-24.) and 14.6% the Leipzig group reported (J Thorac Cardiovasc Surg. 2013 Oct; 146:841-7).While he acknowledged calls for a prospective, randomized clinical trial, Dr. Dion said the contraindications for concomitant tricuspid valve repair with mitral valve repair have already been well documented.
Dr. Dion reports consulting fees from Sorin, Edwards, Johnson & Johnson, and St. Jude Medical.
The idea of performing a tricuspid valve repair during a mitral valve procedure has fueled considerable debate among cardiovascular surgeons largely because the grading of tricuspid regurgitation (TR) has been an unreliable marker, so now may be the time to use a new parameter, Dr. Robert Dion of Genk, Belgium, argues in an expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2015 Nov 20;150:1040-3).
“Therefore, we need a parameter hardly depending on preload,” Dr. Dion said. He noted that many authors have validated the use of annual dilatation of 40 mm or 21mm/m2.
Further, preoperative functional New York Heart Association (NYHA) class plays a major role, Dr. Dion said. TR is progressive in nature and the existence of concomitant mitral valve disease can aggravate annular dilation. The earlier surgeons operate on the mitral valve, the less frequently patients will require tricuspid valve repair at the same time, he said.
The controversy was aired in a report at the 2015 American Association for Thoracic Surgery meeting when Dr. Joanna Chikwe of Mount Sinai Hospital in New York discussed an approach that led to tricuspid valve repair at the time of mitral valve surgery in almost two-thirds of patients. Dr. Chikwe and her coauthors opted for concomitant surgery when patients had moderate TR or tricuspid annular dilatation of 40 mm or greater – a strategy that Dr. Dion said was validated because they reported comparable outcomes in terms of death, morbidity, or pacemaker need. The concomitant repair cured TR and prevented progression at seven years of follow-up; and it induced right ventricle recovery and reduced pulmonary hypertension.
In this opinion piece, Dr. Dion took issue with comments made by Dr. Tirone E. David of the University of Toronto during Dr. Chikwe’s AATS presentation. Dr. David, for whom the David reimplantation technique for aortic root replacement is named, called the technique “overkill,” according to Dr. Dion.
Specifically, Dr. Dion questioned Dr. David’s assertions that the use of rigid rings in mitral valve repair causes TR and that no evidence validates the 40-mm diameter minimum in patients with degenerative mitral valve disease. On the first point, Dr. Dion said no evidence has linked the rigidity of the mitral valve ring and progression of tricuspid regurgitation. On the second, Dr. Dion cited eight studies of progressive tricuspid annular dilation with mitral regurgitation, most of which proposed the 40-mm threshold for concomitant tricuspid valve repair. Since then, the 40-mm threshold has been adopted for both European and American guidelines and validated by five reports from 2011 to 2014.
Dr. Dion said the rationale for using annular dilation rather than TR grade rests on “three poles”: annular dilation does not depend on preload whereas the right ventricle does; documented discrepancies between clinical and hemodynamic data (J Cardiol Surg. 1994 Mar;9(2 suppl):237-41; J Am Coll Cardiol. 2004 Feb. 4;43:405-9); and the idea that TR is “bad” for the patient. He also cited disparities in the number of concomitant repairs performed at leading centers: 7%-10% at the Mayo Clinic and Dr. David’s Toronto center, 25% in Leipzig, 40%-45% in his own clinic and two others, and 65% in Dr. Chikwe’s facility.
But early intervention for mitral valve dysfunction is a key indicator of the need for concomitant tricuspid valve repair, Dr. Dion said. “The earlier we operate on the MV, the less frequently patients will require tricuspid valve repair,” he said. In his own approach, Dr. Dion uses a transseptal approach of the mitral valve. For TR greater than grade 2, he performs tricuspid repair using a semirigid ring sized on the area of the anterior leaflet tissue; and if the tenting distance is 8 mm or greater, he includes anterior leaflet augmentation. When TR grade is 2 or less, he also performs concomitant tricuspid repair when the tricuspid annulus is 40 mm or greater or when the tricuspid annulus is 3.5-4 mm in the setting of a host of other cardiac problems, from atrial fibrillation to left valve dysfunction. “Otherwise: abstention,” he said.
“The major issue here is to do everything possible to avoid the risk and outcomes of reoperative tricuspid valve surgery,” Dr. Dion said, citing in-hospital death rates of 13.2% that Dr. David reported (Ann Thorac Surg. 2013 Jan;95:119-24.) and 14.6% the Leipzig group reported (J Thorac Cardiovasc Surg. 2013 Oct; 146:841-7).While he acknowledged calls for a prospective, randomized clinical trial, Dr. Dion said the contraindications for concomitant tricuspid valve repair with mitral valve repair have already been well documented.
Dr. Dion reports consulting fees from Sorin, Edwards, Johnson & Johnson, and St. Jude Medical.
Key clinical point: Controversy surrounds the need for concomitant tricuspid valve repair with a mitral valve procedure and what parameters the decision should be based on.
Major finding: Increasing reports have supported the use of annular dilation of 40 mm or greater as a threshold for performing concomitant tricuspid valve repair rather than grading of tricuspid regurgitation.
Data source: This Expert Opinion piece cites studies along with American and European clinical guidelines that support the 40-mm threshold.
Disclosures: Dr. Dion reports consulting fees from Sorin, Edwards, Johnson & Johnson, and St. Jude Medical.
Setting a new standard for aortic root repair?
Over the past 3 decades surgery for aortic root replacement has seen a dramatic decline in rates of death and complications, but there have been few studies comparing which technique would be best for specific patients, and those that have been done have been limited by selection bias or small patient numbers.
But a team of investigators from Weill Cornell Medical College in New York have analyzed results of three different aortic root replacement (ARR) procedures over a 17-year period and found that the rates of death during surgery and complications were less than 1% regardless of the technique. They published their results in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1120-9).

“In the current era, aortic root replacement can be performed with very low perioperative risk in high-volume aortic centers,” said Dr. Mario Gaudino and coauthors. “The type of operation performed does not affect early or late survival.”
They compared results of three different approaches to ARR performed in 890 consecutive patients in their institution from May 1997 to January 2014: mechanical composite valved graft (mCVG) in 289 patients; biologic composite valved graft (bCVG) in 421; and valve-sparing reconstruction (VSR) in 180. Then the researchers applied propensity matching to neutralize the differences in the baseline characteristics between the different procedures.
The overall rate of death from the operation was 0.2%, but the two patients who died did so in the first 5 years of the study. There were no deaths in the VSR group, and the incidence of complications after surgery was less than 0.5%. Three-year survival was 94.8% and 5-year survival was 89.4%, and reintervention rates at 5 years were 0% for the mCVG group, 2.4% for the bCVG group, and 7.3% for those who had VSR. “Although mCVG remains the gold standard for durability, bCVG and VSR are excellent options for those who either cannot take or wish to avoid long-term anticoagulation,” Dr. Gaudino and colleagues said.
At the time of surgery, 332 patients (37.3%) had at least one associated cardiac procedure, led by arch replacement (149 patients) and coronary artery bypass (81 patients). Eighty-four patients (9.4%) had two or more associated procedures. The bCVG and mCVG groups had the highest rates of associated cardiac procedures.
Before propensity matching, bCVG patients were older and had more comorbidities and worse functional class, while the mCVG group had higher rates of redo procedures and urgent or emergent operations. Connective tissue disorders were most common in the VSR group.
The results paralleled data from the Society of Thoracic Surgery’s Adult Cardiac Surgery Database, Dr. Gaudino and colleagues said, including a fivefold increase in the number of root replacements performed annually during the study period and a shift away from the traditional mCVG operation to widespread adoption of the bCVG and VSR procedures in the later years of the study.
“Surgeons with extensive experience in aortic surgery can tailor their choice of ARR to the procedure that best suits the individual patient based on their baseline characteristics,” Dr. Gaudino and coauthors said.
Dr. Gaudino and his coauthors had no disclosures.
The results of elective aortic root surgery that Dr. Mario Gaudino and his colleagues reported are “the most impressive … ever published and probably difficult, if not impossible, to reproduce,” Dr. Tirone David of the University of Toronto said in his invited commentary in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1130-1).
Dr. David cited the study’s low rates of deaths and complications. “They had only two deaths early on in their experience and no deaths among the most recent 804 patients operated on since 2002,” he said. “And there is more,” he said: only four strokes, one heart attack, one sternal infection, and only 11.2% of patients receiving blood transfusion. “And to make us ordinary surgeons even more envious, more than one-third of their patients had combined procedures,” Dr. David said.

|
Dr. Tirone David |
He said Dr. Gaudino and his colleagues have set a new standard for early outcomes of elective aortic root surgery. “These outcomes are difficult to emulate but we have to try,” Dr. David said. “To be an obsessive-compulsive surgeon who pays enormous attention to technical details is not enough because even patients who have perfectly executed operations may suffer serious and occasionally fatal postoperative complications.”
The results of elective aortic root surgery that Dr. Mario Gaudino and his colleagues reported are “the most impressive … ever published and probably difficult, if not impossible, to reproduce,” Dr. Tirone David of the University of Toronto said in his invited commentary in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1130-1).
Dr. David cited the study’s low rates of deaths and complications. “They had only two deaths early on in their experience and no deaths among the most recent 804 patients operated on since 2002,” he said. “And there is more,” he said: only four strokes, one heart attack, one sternal infection, and only 11.2% of patients receiving blood transfusion. “And to make us ordinary surgeons even more envious, more than one-third of their patients had combined procedures,” Dr. David said.

|
Dr. Tirone David |
He said Dr. Gaudino and his colleagues have set a new standard for early outcomes of elective aortic root surgery. “These outcomes are difficult to emulate but we have to try,” Dr. David said. “To be an obsessive-compulsive surgeon who pays enormous attention to technical details is not enough because even patients who have perfectly executed operations may suffer serious and occasionally fatal postoperative complications.”
The results of elective aortic root surgery that Dr. Mario Gaudino and his colleagues reported are “the most impressive … ever published and probably difficult, if not impossible, to reproduce,” Dr. Tirone David of the University of Toronto said in his invited commentary in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1130-1).
Dr. David cited the study’s low rates of deaths and complications. “They had only two deaths early on in their experience and no deaths among the most recent 804 patients operated on since 2002,” he said. “And there is more,” he said: only four strokes, one heart attack, one sternal infection, and only 11.2% of patients receiving blood transfusion. “And to make us ordinary surgeons even more envious, more than one-third of their patients had combined procedures,” Dr. David said.

|
Dr. Tirone David |
He said Dr. Gaudino and his colleagues have set a new standard for early outcomes of elective aortic root surgery. “These outcomes are difficult to emulate but we have to try,” Dr. David said. “To be an obsessive-compulsive surgeon who pays enormous attention to technical details is not enough because even patients who have perfectly executed operations may suffer serious and occasionally fatal postoperative complications.”
Over the past 3 decades surgery for aortic root replacement has seen a dramatic decline in rates of death and complications, but there have been few studies comparing which technique would be best for specific patients, and those that have been done have been limited by selection bias or small patient numbers.
But a team of investigators from Weill Cornell Medical College in New York have analyzed results of three different aortic root replacement (ARR) procedures over a 17-year period and found that the rates of death during surgery and complications were less than 1% regardless of the technique. They published their results in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1120-9).

“In the current era, aortic root replacement can be performed with very low perioperative risk in high-volume aortic centers,” said Dr. Mario Gaudino and coauthors. “The type of operation performed does not affect early or late survival.”
They compared results of three different approaches to ARR performed in 890 consecutive patients in their institution from May 1997 to January 2014: mechanical composite valved graft (mCVG) in 289 patients; biologic composite valved graft (bCVG) in 421; and valve-sparing reconstruction (VSR) in 180. Then the researchers applied propensity matching to neutralize the differences in the baseline characteristics between the different procedures.
The overall rate of death from the operation was 0.2%, but the two patients who died did so in the first 5 years of the study. There were no deaths in the VSR group, and the incidence of complications after surgery was less than 0.5%. Three-year survival was 94.8% and 5-year survival was 89.4%, and reintervention rates at 5 years were 0% for the mCVG group, 2.4% for the bCVG group, and 7.3% for those who had VSR. “Although mCVG remains the gold standard for durability, bCVG and VSR are excellent options for those who either cannot take or wish to avoid long-term anticoagulation,” Dr. Gaudino and colleagues said.
At the time of surgery, 332 patients (37.3%) had at least one associated cardiac procedure, led by arch replacement (149 patients) and coronary artery bypass (81 patients). Eighty-four patients (9.4%) had two or more associated procedures. The bCVG and mCVG groups had the highest rates of associated cardiac procedures.
Before propensity matching, bCVG patients were older and had more comorbidities and worse functional class, while the mCVG group had higher rates of redo procedures and urgent or emergent operations. Connective tissue disorders were most common in the VSR group.
The results paralleled data from the Society of Thoracic Surgery’s Adult Cardiac Surgery Database, Dr. Gaudino and colleagues said, including a fivefold increase in the number of root replacements performed annually during the study period and a shift away from the traditional mCVG operation to widespread adoption of the bCVG and VSR procedures in the later years of the study.
“Surgeons with extensive experience in aortic surgery can tailor their choice of ARR to the procedure that best suits the individual patient based on their baseline characteristics,” Dr. Gaudino and coauthors said.
Dr. Gaudino and his coauthors had no disclosures.
Over the past 3 decades surgery for aortic root replacement has seen a dramatic decline in rates of death and complications, but there have been few studies comparing which technique would be best for specific patients, and those that have been done have been limited by selection bias or small patient numbers.
But a team of investigators from Weill Cornell Medical College in New York have analyzed results of three different aortic root replacement (ARR) procedures over a 17-year period and found that the rates of death during surgery and complications were less than 1% regardless of the technique. They published their results in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1120-9).

“In the current era, aortic root replacement can be performed with very low perioperative risk in high-volume aortic centers,” said Dr. Mario Gaudino and coauthors. “The type of operation performed does not affect early or late survival.”
They compared results of three different approaches to ARR performed in 890 consecutive patients in their institution from May 1997 to January 2014: mechanical composite valved graft (mCVG) in 289 patients; biologic composite valved graft (bCVG) in 421; and valve-sparing reconstruction (VSR) in 180. Then the researchers applied propensity matching to neutralize the differences in the baseline characteristics between the different procedures.
The overall rate of death from the operation was 0.2%, but the two patients who died did so in the first 5 years of the study. There were no deaths in the VSR group, and the incidence of complications after surgery was less than 0.5%. Three-year survival was 94.8% and 5-year survival was 89.4%, and reintervention rates at 5 years were 0% for the mCVG group, 2.4% for the bCVG group, and 7.3% for those who had VSR. “Although mCVG remains the gold standard for durability, bCVG and VSR are excellent options for those who either cannot take or wish to avoid long-term anticoagulation,” Dr. Gaudino and colleagues said.
At the time of surgery, 332 patients (37.3%) had at least one associated cardiac procedure, led by arch replacement (149 patients) and coronary artery bypass (81 patients). Eighty-four patients (9.4%) had two or more associated procedures. The bCVG and mCVG groups had the highest rates of associated cardiac procedures.
Before propensity matching, bCVG patients were older and had more comorbidities and worse functional class, while the mCVG group had higher rates of redo procedures and urgent or emergent operations. Connective tissue disorders were most common in the VSR group.
The results paralleled data from the Society of Thoracic Surgery’s Adult Cardiac Surgery Database, Dr. Gaudino and colleagues said, including a fivefold increase in the number of root replacements performed annually during the study period and a shift away from the traditional mCVG operation to widespread adoption of the bCVG and VSR procedures in the later years of the study.
“Surgeons with extensive experience in aortic surgery can tailor their choice of ARR to the procedure that best suits the individual patient based on their baseline characteristics,” Dr. Gaudino and coauthors said.
Dr. Gaudino and his coauthors had no disclosures.
Key clinical point: Aortic root replacement surgery can be performed with minimal risk of death and complications regardless of the approach taken.
Major finding: Overall rate of death was 0.2%, with none since 2002, and the overall rate of complications was below 0.5% in the study cohort.
Data source: Review of prospective data on 890 aortic root replacement operations performed over a 17-year period at a single center.
Disclosures: The study authors had no relationships to disclose.
Perioperative statins for cardiac surgery didn’t reduce kidney injury
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
AT KIDNEY WEEK 2015
Key clinical point: The use of high-dose perioperative atorvastatin did not reduce acute kidney injury in patients undergoing elective cardiac surgery.
Major finding: Among all patients, acute kidney injury occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that is neither clinically nor statistically significant (P = .75).
Data source: A randomized, controlled trial of 653 patients to test the hypothesis that short-term, high-dose perioperative atorvastatin reduces acute kidney injury following elective cardiac surgery.
Disclosures: The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
Endobronchial valves improve pulmonary function in emphysema
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Endobronchial valves improved pulmonary function, exercise capacity, and QOL in severe emphysema.
Major finding: Patients who received endobronchial valves showed improved FEV1 by 191 mL, forced vital capacity by 442 mL, residual lung volume, 6-minute walk distance by 106 meters, and QOL scores.
Data source: A prospective randomized controlled trial involving 68 patients treated during a 3-year period at a single medical center.
Disclosures: The Netherlands Organization for Health Research and Development and the University Medical Center Groningen funded the study. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for this study.
Does position matter in ViV implantation?
With transcatheter valve-in-valve implantation emerging as a novel treatment for high-risk patients whose existing bioprostheses have deteriorated, a team of investigators at University Heart Center in Hamburg, Germany, has found that the procedure can be done successfully in four different anatomic positions with a variety of bioprostheses.
The findings from the single-center study were published in the December issue of the Journal of Thoracic and Cardiovascular Surgery. (J Thorac Cardiovasc Surg. 2015;150:1557-67). They retrospectively analyzed results of 75 patients who had transcatheter valve-in-valve (ViV) replacement at their institution from 2008 to 2014.
“ViV can be performed in all anatomic positions with acceptable hemodynamic and clinical outcome in high-risk patients,” wrote Dr. Lenard Conradi and coauthors. “Increasing importance of ViV can be anticipated considering growing use of surgical bioprostheses.”
Replacement of biological valves is becoming more common. For surgical aortic valve replacement (SAVR), biological procedures have largely replaced mechanical valve implantation, comprising 87% of all such procedures by 2014, according to data from the German Society for Thoracic and Cardiovascular Surgery (Thorac Cardiovasc Surg. 2014;62:380-92). “Therefore, increasing caseload of patients with deteriorated bioprostheses can be expected,” wrote Dr. Conradi and coauthors.
The four anatomic positions in which the investigators performed the procedures and their share of cases are: aortic (54 patients/72%), mitral (17/22.7%), and tricuspid and pulmonary positions (2/2.7% each). The average interval between the index procedure and ViV was 9 years, with a deviation of nearly 5 years among all procedures. Dr. Conradi and coinvestigators said their study focused on technical aspects of ViV procedures from each position to provide guidance for surgeons.
Overall, the study authors performed ViV successfully in 97.3% of patients, with two patients requiring sequential transcatheter heart valve implantation for initial malpositioning. Thirty-day mortality was 8%, which “ranged lower” than expected when compared to standard preoperative risk stratification, they wrote. Mortality was at 5.6% in the aortic group and 17.6% in the mitral group.
That none of the currently available surgical bioprostheses or transcatheter heart valves (THV) were designed for later ViV procedures in deteriorated bioprostheses – although the CoreValve and Sapein THV have approvals for the indication – “may explain some of the apparent shortcomings of ViV therapy,” the researchers wrote.
The most significant challenge of ViV therapy is dealing with elevated residual gradients, which positioning can influence, according to the study findings. “This is not so much an issue for mitral, tricuspid, or pulmonary positions since surgical bioprostheses implanted in these positions are usually of sufficient size to accommodate the THV,” the researchers noted. “However, in the aortic position, more severe spatial restrictions may apply.”
They cited other reports that described a reverse relationship between size of the bioprosthetic and resulting transvalvular gradient after ViV (JACC Cardiovasc Interv. 2011;4:1218-27; JAMA 2014;312:162-70).
To reduce gradients, the investigators used post-ballooning after aortic ViV with a self-expandable THV in 16 cases, succeeding in 12. “Likely, further THV expansion with active compression of soft leaflet and/or pannus tissue and tighter apposition of THV against the frames of surgical bioprostheses contributed to this desired effect,” wrote the researchers. Patient-prosthesis mismatch probably explained the four cases in which gradients could not be further reduced, they noted.
They issued one “word of caution” regarding aortic ViV in small-sized surgical bioprostheses: “Elevated postprocedural gradients have to be expected and must be weighed against expected benefits and against risk of repeat open heart surgery.”
The six transcatheter heart valves the investigators used were Edwards Sapien (XT)/Sapien3 (52%, 39/75); Medtronic CoreValve/CoreValveEvolut (34.7%, 26); St. Jude Portico and Boston Scientific Lotus (4%, three each); and JenaValve and Medtronic Engager (2.7%, two each). The study also looked at different access routes: transapical in 53.3% (40), transfemoral (transarterial or transvenous) in 42.7% (32), transaortic in 2.7% (2), and transjugular in 1.3% (1).
Dr. Conradi and coauthors Dr. Moritz Seiffert, Dr. Ulrich Schaefer, and Dr. Hendrik Treede disclosed ties with Edwards Lifesciences, JenaValve Technology, Medtronic, Symetis, and St. Jude Medical. Four other coauthors reported no disclosures.
As the population ages and younger patients choose bioprosthetic valves to avoid lifelong warfarin, surgeons are going to face more situations where they will have to decide whether to perform surgical or transcatheter reoperative valve surgery, Dr. Jessica Forcillo of Emory University, Atlanta, and coauthors wrote in an invited commentary (J Thorac Cardiovasc Surg. 2015;150:1568-9).
They called the 8% 30-day mortality rate in the Hamburg study “high” even though the average age of the study population was a “relatively young” 74 years. The Hamburg authors may have learned more had they evaluated fewer prostheses. “With a small number of patients and at the beginning of an experience, focusing on one or two available prostheses may have resulted in more accurate and reliable results,” noted Dr. Forcillo and her colleagues. That 53% of the procedures were done via the transapical approach may also explain the mortality rate, they said.
The overall 30-day mortality rate along with a 17.6% mortality in the mitral ViV group are causes for “some caution against overzealous performance of this procedure and continued monitoring of outcomes in other series,” wrote Dr. Forcillo and her colleagues.
But ViV implantation is a “transformative” technology, they said. “For the elderly, high-risk patients with [structural valve degeneration], transcatheter options may provide improved short-term outcomes,” they added. “The valve community eagerly awaits larger series with adjudicated outcomes of the transcatheter valve-in-valve procedure.”
Dr. Forcillo and coauthor Lillian Tsai had no disclosures. Dr. Vinod Thourani disclosed ties with St. Jude Medical, Edwards Lifesciences, Boston Scientific, Abbott Medical, Medtronic, Directflow, and Sorin Medical.
As the population ages and younger patients choose bioprosthetic valves to avoid lifelong warfarin, surgeons are going to face more situations where they will have to decide whether to perform surgical or transcatheter reoperative valve surgery, Dr. Jessica Forcillo of Emory University, Atlanta, and coauthors wrote in an invited commentary (J Thorac Cardiovasc Surg. 2015;150:1568-9).
They called the 8% 30-day mortality rate in the Hamburg study “high” even though the average age of the study population was a “relatively young” 74 years. The Hamburg authors may have learned more had they evaluated fewer prostheses. “With a small number of patients and at the beginning of an experience, focusing on one or two available prostheses may have resulted in more accurate and reliable results,” noted Dr. Forcillo and her colleagues. That 53% of the procedures were done via the transapical approach may also explain the mortality rate, they said.
The overall 30-day mortality rate along with a 17.6% mortality in the mitral ViV group are causes for “some caution against overzealous performance of this procedure and continued monitoring of outcomes in other series,” wrote Dr. Forcillo and her colleagues.
But ViV implantation is a “transformative” technology, they said. “For the elderly, high-risk patients with [structural valve degeneration], transcatheter options may provide improved short-term outcomes,” they added. “The valve community eagerly awaits larger series with adjudicated outcomes of the transcatheter valve-in-valve procedure.”
Dr. Forcillo and coauthor Lillian Tsai had no disclosures. Dr. Vinod Thourani disclosed ties with St. Jude Medical, Edwards Lifesciences, Boston Scientific, Abbott Medical, Medtronic, Directflow, and Sorin Medical.
As the population ages and younger patients choose bioprosthetic valves to avoid lifelong warfarin, surgeons are going to face more situations where they will have to decide whether to perform surgical or transcatheter reoperative valve surgery, Dr. Jessica Forcillo of Emory University, Atlanta, and coauthors wrote in an invited commentary (J Thorac Cardiovasc Surg. 2015;150:1568-9).
They called the 8% 30-day mortality rate in the Hamburg study “high” even though the average age of the study population was a “relatively young” 74 years. The Hamburg authors may have learned more had they evaluated fewer prostheses. “With a small number of patients and at the beginning of an experience, focusing on one or two available prostheses may have resulted in more accurate and reliable results,” noted Dr. Forcillo and her colleagues. That 53% of the procedures were done via the transapical approach may also explain the mortality rate, they said.
The overall 30-day mortality rate along with a 17.6% mortality in the mitral ViV group are causes for “some caution against overzealous performance of this procedure and continued monitoring of outcomes in other series,” wrote Dr. Forcillo and her colleagues.
But ViV implantation is a “transformative” technology, they said. “For the elderly, high-risk patients with [structural valve degeneration], transcatheter options may provide improved short-term outcomes,” they added. “The valve community eagerly awaits larger series with adjudicated outcomes of the transcatheter valve-in-valve procedure.”
Dr. Forcillo and coauthor Lillian Tsai had no disclosures. Dr. Vinod Thourani disclosed ties with St. Jude Medical, Edwards Lifesciences, Boston Scientific, Abbott Medical, Medtronic, Directflow, and Sorin Medical.
With transcatheter valve-in-valve implantation emerging as a novel treatment for high-risk patients whose existing bioprostheses have deteriorated, a team of investigators at University Heart Center in Hamburg, Germany, has found that the procedure can be done successfully in four different anatomic positions with a variety of bioprostheses.
The findings from the single-center study were published in the December issue of the Journal of Thoracic and Cardiovascular Surgery. (J Thorac Cardiovasc Surg. 2015;150:1557-67). They retrospectively analyzed results of 75 patients who had transcatheter valve-in-valve (ViV) replacement at their institution from 2008 to 2014.
“ViV can be performed in all anatomic positions with acceptable hemodynamic and clinical outcome in high-risk patients,” wrote Dr. Lenard Conradi and coauthors. “Increasing importance of ViV can be anticipated considering growing use of surgical bioprostheses.”
Replacement of biological valves is becoming more common. For surgical aortic valve replacement (SAVR), biological procedures have largely replaced mechanical valve implantation, comprising 87% of all such procedures by 2014, according to data from the German Society for Thoracic and Cardiovascular Surgery (Thorac Cardiovasc Surg. 2014;62:380-92). “Therefore, increasing caseload of patients with deteriorated bioprostheses can be expected,” wrote Dr. Conradi and coauthors.
The four anatomic positions in which the investigators performed the procedures and their share of cases are: aortic (54 patients/72%), mitral (17/22.7%), and tricuspid and pulmonary positions (2/2.7% each). The average interval between the index procedure and ViV was 9 years, with a deviation of nearly 5 years among all procedures. Dr. Conradi and coinvestigators said their study focused on technical aspects of ViV procedures from each position to provide guidance for surgeons.
Overall, the study authors performed ViV successfully in 97.3% of patients, with two patients requiring sequential transcatheter heart valve implantation for initial malpositioning. Thirty-day mortality was 8%, which “ranged lower” than expected when compared to standard preoperative risk stratification, they wrote. Mortality was at 5.6% in the aortic group and 17.6% in the mitral group.
That none of the currently available surgical bioprostheses or transcatheter heart valves (THV) were designed for later ViV procedures in deteriorated bioprostheses – although the CoreValve and Sapein THV have approvals for the indication – “may explain some of the apparent shortcomings of ViV therapy,” the researchers wrote.
The most significant challenge of ViV therapy is dealing with elevated residual gradients, which positioning can influence, according to the study findings. “This is not so much an issue for mitral, tricuspid, or pulmonary positions since surgical bioprostheses implanted in these positions are usually of sufficient size to accommodate the THV,” the researchers noted. “However, in the aortic position, more severe spatial restrictions may apply.”
They cited other reports that described a reverse relationship between size of the bioprosthetic and resulting transvalvular gradient after ViV (JACC Cardiovasc Interv. 2011;4:1218-27; JAMA 2014;312:162-70).
To reduce gradients, the investigators used post-ballooning after aortic ViV with a self-expandable THV in 16 cases, succeeding in 12. “Likely, further THV expansion with active compression of soft leaflet and/or pannus tissue and tighter apposition of THV against the frames of surgical bioprostheses contributed to this desired effect,” wrote the researchers. Patient-prosthesis mismatch probably explained the four cases in which gradients could not be further reduced, they noted.
They issued one “word of caution” regarding aortic ViV in small-sized surgical bioprostheses: “Elevated postprocedural gradients have to be expected and must be weighed against expected benefits and against risk of repeat open heart surgery.”
The six transcatheter heart valves the investigators used were Edwards Sapien (XT)/Sapien3 (52%, 39/75); Medtronic CoreValve/CoreValveEvolut (34.7%, 26); St. Jude Portico and Boston Scientific Lotus (4%, three each); and JenaValve and Medtronic Engager (2.7%, two each). The study also looked at different access routes: transapical in 53.3% (40), transfemoral (transarterial or transvenous) in 42.7% (32), transaortic in 2.7% (2), and transjugular in 1.3% (1).
Dr. Conradi and coauthors Dr. Moritz Seiffert, Dr. Ulrich Schaefer, and Dr. Hendrik Treede disclosed ties with Edwards Lifesciences, JenaValve Technology, Medtronic, Symetis, and St. Jude Medical. Four other coauthors reported no disclosures.
With transcatheter valve-in-valve implantation emerging as a novel treatment for high-risk patients whose existing bioprostheses have deteriorated, a team of investigators at University Heart Center in Hamburg, Germany, has found that the procedure can be done successfully in four different anatomic positions with a variety of bioprostheses.
The findings from the single-center study were published in the December issue of the Journal of Thoracic and Cardiovascular Surgery. (J Thorac Cardiovasc Surg. 2015;150:1557-67). They retrospectively analyzed results of 75 patients who had transcatheter valve-in-valve (ViV) replacement at their institution from 2008 to 2014.
“ViV can be performed in all anatomic positions with acceptable hemodynamic and clinical outcome in high-risk patients,” wrote Dr. Lenard Conradi and coauthors. “Increasing importance of ViV can be anticipated considering growing use of surgical bioprostheses.”
Replacement of biological valves is becoming more common. For surgical aortic valve replacement (SAVR), biological procedures have largely replaced mechanical valve implantation, comprising 87% of all such procedures by 2014, according to data from the German Society for Thoracic and Cardiovascular Surgery (Thorac Cardiovasc Surg. 2014;62:380-92). “Therefore, increasing caseload of patients with deteriorated bioprostheses can be expected,” wrote Dr. Conradi and coauthors.
The four anatomic positions in which the investigators performed the procedures and their share of cases are: aortic (54 patients/72%), mitral (17/22.7%), and tricuspid and pulmonary positions (2/2.7% each). The average interval between the index procedure and ViV was 9 years, with a deviation of nearly 5 years among all procedures. Dr. Conradi and coinvestigators said their study focused on technical aspects of ViV procedures from each position to provide guidance for surgeons.
Overall, the study authors performed ViV successfully in 97.3% of patients, with two patients requiring sequential transcatheter heart valve implantation for initial malpositioning. Thirty-day mortality was 8%, which “ranged lower” than expected when compared to standard preoperative risk stratification, they wrote. Mortality was at 5.6% in the aortic group and 17.6% in the mitral group.
That none of the currently available surgical bioprostheses or transcatheter heart valves (THV) were designed for later ViV procedures in deteriorated bioprostheses – although the CoreValve and Sapein THV have approvals for the indication – “may explain some of the apparent shortcomings of ViV therapy,” the researchers wrote.
The most significant challenge of ViV therapy is dealing with elevated residual gradients, which positioning can influence, according to the study findings. “This is not so much an issue for mitral, tricuspid, or pulmonary positions since surgical bioprostheses implanted in these positions are usually of sufficient size to accommodate the THV,” the researchers noted. “However, in the aortic position, more severe spatial restrictions may apply.”
They cited other reports that described a reverse relationship between size of the bioprosthetic and resulting transvalvular gradient after ViV (JACC Cardiovasc Interv. 2011;4:1218-27; JAMA 2014;312:162-70).
To reduce gradients, the investigators used post-ballooning after aortic ViV with a self-expandable THV in 16 cases, succeeding in 12. “Likely, further THV expansion with active compression of soft leaflet and/or pannus tissue and tighter apposition of THV against the frames of surgical bioprostheses contributed to this desired effect,” wrote the researchers. Patient-prosthesis mismatch probably explained the four cases in which gradients could not be further reduced, they noted.
They issued one “word of caution” regarding aortic ViV in small-sized surgical bioprostheses: “Elevated postprocedural gradients have to be expected and must be weighed against expected benefits and against risk of repeat open heart surgery.”
The six transcatheter heart valves the investigators used were Edwards Sapien (XT)/Sapien3 (52%, 39/75); Medtronic CoreValve/CoreValveEvolut (34.7%, 26); St. Jude Portico and Boston Scientific Lotus (4%, three each); and JenaValve and Medtronic Engager (2.7%, two each). The study also looked at different access routes: transapical in 53.3% (40), transfemoral (transarterial or transvenous) in 42.7% (32), transaortic in 2.7% (2), and transjugular in 1.3% (1).
Dr. Conradi and coauthors Dr. Moritz Seiffert, Dr. Ulrich Schaefer, and Dr. Hendrik Treede disclosed ties with Edwards Lifesciences, JenaValve Technology, Medtronic, Symetis, and St. Jude Medical. Four other coauthors reported no disclosures.
Key clinical point: Transcatheter valve-in-valve (ViV) implantation is a relatively safe treatment for patients with a deteriorated bioprostheses.
Major finding: A ViV implantation when performed in four different positions with six different transcatheter heart valves had a 30-day mortality of 8%.
Data source: Retrospective analysis of 75 consecutive patients receiving ViV procedures from 2008 to 2014 at a single institution.
Disclosures: Dr. Conradi and coauthors Dr. Moritz Seiffert, Dr. Ulrich Schaefer, and Dr. Hendrik Treede disclosed relationships with Edwards Lifesciences, JenaValve Technology, Medtronic, Symetis, and St. Jude Medical. Four other coauthors reported no disclosures.
Pediatric heart transplant results not improving
A 25-year study of heart transplants in children with congenital heart disease (CHD) at one institution has found that results haven’t improved over time despite advances in technology and techniques. To improve outcomes, transplant surgeons may need to do a better job of selecting patients and matching patients and donors, according to study in the December issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015;150:1455-62).
“Strategies to improve outcomes in CHD patients might need to address selection criteria, transplantation timing, pretransplant and posttransplant care,” noted Dr. Bahaaldin Alsoufi, of the division of cardiothoracic surgery, Children’s Healthcare of Atlanta, Emory University. “The effect of donor/recipient race mismatch warrants further investigation and might impact organ allocation algorithms or immunosuppression management,” wrote Dr. Alsoufi and his colleagues.
The researchers analyzed results of 124 children with CHD who had heart transplants from 1988 to 2013 at Emory University and Children’s Healthcare of Atlanta. Median age was 3.8 years; 61% were boys. Ten years after heart transplantation, 44% (54) of patients were alive without a second transplant, 13% (17) had a second transplant and 43% (53) died without a second transplant. After the second transplant, 9 of the 17 patients were alive, but 3 of them had gone onto a third transplant. Overall 15-year survival following the first transplant was 41% (51).
The study cited data from the Registry of the International Society for Heart and Lung Transplantation that reported more than 11,000 pediatric heart transplants worldwide in 2013, and CHD represents about 54% of all heart transplants in infants.
A multivariate analysis identified the following risk factors for early mortality after transplant: age younger than 12 months (hazard ration [HR] 7.2) and prolonged cardiopulmonary bypass (HR 5). Late-phase mortality risk factors were age younger than 12 months (HR 3) and donor/recipient race mismatch (HR 2.2).
“Survival was not affected by era, underlying anomaly, prior Fontan, sensitization or pulmonary artery augmentation,” wrote Dr. Alsoufi and his colleagues.
Among the risk factors, longer bypass times may be a surrogate for a more complicated operation, the authors said. But where prior sternotomy is a risk factor following a heart transplant in adults, the study found no such risk in children. Another risk factor previous reports identified is pulmonary artery augmentation, but, again, this study found no risk in the pediatric group.
The researchers looked at days on the waiting list, with a median wait of 39 days in the study group. In all, 175 children were listed for transplants, but 51 did not go through for various reasons. Most of the children with CHD who had a heart transplant had previous surgery; only 13% had a primary heart transplant, mostly in the earlier phase of the study.
Dr. Alsoufi and coauthors also identified African American race as a risk factor for lower survival, which is consistent with other reports. But this study agreed with a previous report that donor/recipient race mismatch was a significant risk factor in white and African American patients (Ann Thorac Surg. 2009;87:204-9). “While our finding might be anecdotal and specific to our geographic population, this warrants some investigation and might have some impact on future organ allocation algorithms and immunosuppression management,” the researchers wrote.
The authors had no relevant disclosures. Emory University School of Medicine, Children’s Healthcare of Atlanta provided study funding.
In his invited commentary, Dr. Robert D.B. Jaquiss of Duke University, Durham, N.C., took issue with the study authors’ “distress” at the lack of improvement in survival over the 25-year term of the study (J Thorac Cardiovasc Surg. 2015;150:1463-4) . Using the year 2000 as a demarcation line for early and late-phase results, Dr. Jaquiss said, “It must be pointed out that in the latter period recipients were much more ill.” He noted that 89% of post-2000 heart transplant patients had UNOS status 1 vs. 49% in the pre-2000 period.

|
Dr. Robert Jaquiss |
“Considering these between-era differences, an alternative, less ‘discouraging’ interpretation is that excellent outcomes were maintained despite the trend toward transplantation in sicker patients, undergoing more complex transplants, with longer ischemic times,” he said.
Dr. Jaquiss also cited “remarkably outstanding outcomes” in Fontan patients, reporting only one operative death in 33 patients. He found the lower survival for African-American patients in the study group “more sobering,” but also controversial because, among other reasons, “a complete mechanistic explanation remains elusive.” How these findings influence pediatric heart transplant practice “requires thoughtful and extensive investigation and discussion,” he said.
Wait-list mortality and mechanical bridge to transplant also deserve mention, he noted. “Though they are only briefly mentioned, the patients who died prior to transplant provide mute testimony to the lack of timely access to suitable donors,” Dr. Jaquiss said. Durable mechanical circulatory support can provide a bridge for these patients, but was not available through the majority of the study period.
“It is striking that no patient in this report was supported by a ventricular assist device (VAD), and only a small number (5%) had been on [extracorporeal membrane oxygenation] support,” Dr. Jaquiss said. “This is an unfortunate and unavoidable weakness of this report, given the recent introduction of VADs for pediatric heart transplant candidates.” The use of VAD in patients with CHD is “increasing rapidly,” he said.
Dr. Jaquiss had no disclosures.
In his invited commentary, Dr. Robert D.B. Jaquiss of Duke University, Durham, N.C., took issue with the study authors’ “distress” at the lack of improvement in survival over the 25-year term of the study (J Thorac Cardiovasc Surg. 2015;150:1463-4) . Using the year 2000 as a demarcation line for early and late-phase results, Dr. Jaquiss said, “It must be pointed out that in the latter period recipients were much more ill.” He noted that 89% of post-2000 heart transplant patients had UNOS status 1 vs. 49% in the pre-2000 period.

|
Dr. Robert Jaquiss |
“Considering these between-era differences, an alternative, less ‘discouraging’ interpretation is that excellent outcomes were maintained despite the trend toward transplantation in sicker patients, undergoing more complex transplants, with longer ischemic times,” he said.
Dr. Jaquiss also cited “remarkably outstanding outcomes” in Fontan patients, reporting only one operative death in 33 patients. He found the lower survival for African-American patients in the study group “more sobering,” but also controversial because, among other reasons, “a complete mechanistic explanation remains elusive.” How these findings influence pediatric heart transplant practice “requires thoughtful and extensive investigation and discussion,” he said.
Wait-list mortality and mechanical bridge to transplant also deserve mention, he noted. “Though they are only briefly mentioned, the patients who died prior to transplant provide mute testimony to the lack of timely access to suitable donors,” Dr. Jaquiss said. Durable mechanical circulatory support can provide a bridge for these patients, but was not available through the majority of the study period.
“It is striking that no patient in this report was supported by a ventricular assist device (VAD), and only a small number (5%) had been on [extracorporeal membrane oxygenation] support,” Dr. Jaquiss said. “This is an unfortunate and unavoidable weakness of this report, given the recent introduction of VADs for pediatric heart transplant candidates.” The use of VAD in patients with CHD is “increasing rapidly,” he said.
Dr. Jaquiss had no disclosures.
In his invited commentary, Dr. Robert D.B. Jaquiss of Duke University, Durham, N.C., took issue with the study authors’ “distress” at the lack of improvement in survival over the 25-year term of the study (J Thorac Cardiovasc Surg. 2015;150:1463-4) . Using the year 2000 as a demarcation line for early and late-phase results, Dr. Jaquiss said, “It must be pointed out that in the latter period recipients were much more ill.” He noted that 89% of post-2000 heart transplant patients had UNOS status 1 vs. 49% in the pre-2000 period.

|
Dr. Robert Jaquiss |
“Considering these between-era differences, an alternative, less ‘discouraging’ interpretation is that excellent outcomes were maintained despite the trend toward transplantation in sicker patients, undergoing more complex transplants, with longer ischemic times,” he said.
Dr. Jaquiss also cited “remarkably outstanding outcomes” in Fontan patients, reporting only one operative death in 33 patients. He found the lower survival for African-American patients in the study group “more sobering,” but also controversial because, among other reasons, “a complete mechanistic explanation remains elusive.” How these findings influence pediatric heart transplant practice “requires thoughtful and extensive investigation and discussion,” he said.
Wait-list mortality and mechanical bridge to transplant also deserve mention, he noted. “Though they are only briefly mentioned, the patients who died prior to transplant provide mute testimony to the lack of timely access to suitable donors,” Dr. Jaquiss said. Durable mechanical circulatory support can provide a bridge for these patients, but was not available through the majority of the study period.
“It is striking that no patient in this report was supported by a ventricular assist device (VAD), and only a small number (5%) had been on [extracorporeal membrane oxygenation] support,” Dr. Jaquiss said. “This is an unfortunate and unavoidable weakness of this report, given the recent introduction of VADs for pediatric heart transplant candidates.” The use of VAD in patients with CHD is “increasing rapidly,” he said.
Dr. Jaquiss had no disclosures.
A 25-year study of heart transplants in children with congenital heart disease (CHD) at one institution has found that results haven’t improved over time despite advances in technology and techniques. To improve outcomes, transplant surgeons may need to do a better job of selecting patients and matching patients and donors, according to study in the December issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015;150:1455-62).
“Strategies to improve outcomes in CHD patients might need to address selection criteria, transplantation timing, pretransplant and posttransplant care,” noted Dr. Bahaaldin Alsoufi, of the division of cardiothoracic surgery, Children’s Healthcare of Atlanta, Emory University. “The effect of donor/recipient race mismatch warrants further investigation and might impact organ allocation algorithms or immunosuppression management,” wrote Dr. Alsoufi and his colleagues.
The researchers analyzed results of 124 children with CHD who had heart transplants from 1988 to 2013 at Emory University and Children’s Healthcare of Atlanta. Median age was 3.8 years; 61% were boys. Ten years after heart transplantation, 44% (54) of patients were alive without a second transplant, 13% (17) had a second transplant and 43% (53) died without a second transplant. After the second transplant, 9 of the 17 patients were alive, but 3 of them had gone onto a third transplant. Overall 15-year survival following the first transplant was 41% (51).
The study cited data from the Registry of the International Society for Heart and Lung Transplantation that reported more than 11,000 pediatric heart transplants worldwide in 2013, and CHD represents about 54% of all heart transplants in infants.
A multivariate analysis identified the following risk factors for early mortality after transplant: age younger than 12 months (hazard ration [HR] 7.2) and prolonged cardiopulmonary bypass (HR 5). Late-phase mortality risk factors were age younger than 12 months (HR 3) and donor/recipient race mismatch (HR 2.2).
“Survival was not affected by era, underlying anomaly, prior Fontan, sensitization or pulmonary artery augmentation,” wrote Dr. Alsoufi and his colleagues.
Among the risk factors, longer bypass times may be a surrogate for a more complicated operation, the authors said. But where prior sternotomy is a risk factor following a heart transplant in adults, the study found no such risk in children. Another risk factor previous reports identified is pulmonary artery augmentation, but, again, this study found no risk in the pediatric group.
The researchers looked at days on the waiting list, with a median wait of 39 days in the study group. In all, 175 children were listed for transplants, but 51 did not go through for various reasons. Most of the children with CHD who had a heart transplant had previous surgery; only 13% had a primary heart transplant, mostly in the earlier phase of the study.
Dr. Alsoufi and coauthors also identified African American race as a risk factor for lower survival, which is consistent with other reports. But this study agreed with a previous report that donor/recipient race mismatch was a significant risk factor in white and African American patients (Ann Thorac Surg. 2009;87:204-9). “While our finding might be anecdotal and specific to our geographic population, this warrants some investigation and might have some impact on future organ allocation algorithms and immunosuppression management,” the researchers wrote.
The authors had no relevant disclosures. Emory University School of Medicine, Children’s Healthcare of Atlanta provided study funding.
A 25-year study of heart transplants in children with congenital heart disease (CHD) at one institution has found that results haven’t improved over time despite advances in technology and techniques. To improve outcomes, transplant surgeons may need to do a better job of selecting patients and matching patients and donors, according to study in the December issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015;150:1455-62).
“Strategies to improve outcomes in CHD patients might need to address selection criteria, transplantation timing, pretransplant and posttransplant care,” noted Dr. Bahaaldin Alsoufi, of the division of cardiothoracic surgery, Children’s Healthcare of Atlanta, Emory University. “The effect of donor/recipient race mismatch warrants further investigation and might impact organ allocation algorithms or immunosuppression management,” wrote Dr. Alsoufi and his colleagues.
The researchers analyzed results of 124 children with CHD who had heart transplants from 1988 to 2013 at Emory University and Children’s Healthcare of Atlanta. Median age was 3.8 years; 61% were boys. Ten years after heart transplantation, 44% (54) of patients were alive without a second transplant, 13% (17) had a second transplant and 43% (53) died without a second transplant. After the second transplant, 9 of the 17 patients were alive, but 3 of them had gone onto a third transplant. Overall 15-year survival following the first transplant was 41% (51).
The study cited data from the Registry of the International Society for Heart and Lung Transplantation that reported more than 11,000 pediatric heart transplants worldwide in 2013, and CHD represents about 54% of all heart transplants in infants.
A multivariate analysis identified the following risk factors for early mortality after transplant: age younger than 12 months (hazard ration [HR] 7.2) and prolonged cardiopulmonary bypass (HR 5). Late-phase mortality risk factors were age younger than 12 months (HR 3) and donor/recipient race mismatch (HR 2.2).
“Survival was not affected by era, underlying anomaly, prior Fontan, sensitization or pulmonary artery augmentation,” wrote Dr. Alsoufi and his colleagues.
Among the risk factors, longer bypass times may be a surrogate for a more complicated operation, the authors said. But where prior sternotomy is a risk factor following a heart transplant in adults, the study found no such risk in children. Another risk factor previous reports identified is pulmonary artery augmentation, but, again, this study found no risk in the pediatric group.
The researchers looked at days on the waiting list, with a median wait of 39 days in the study group. In all, 175 children were listed for transplants, but 51 did not go through for various reasons. Most of the children with CHD who had a heart transplant had previous surgery; only 13% had a primary heart transplant, mostly in the earlier phase of the study.
Dr. Alsoufi and coauthors also identified African American race as a risk factor for lower survival, which is consistent with other reports. But this study agreed with a previous report that donor/recipient race mismatch was a significant risk factor in white and African American patients (Ann Thorac Surg. 2009;87:204-9). “While our finding might be anecdotal and specific to our geographic population, this warrants some investigation and might have some impact on future organ allocation algorithms and immunosuppression management,” the researchers wrote.
The authors had no relevant disclosures. Emory University School of Medicine, Children’s Healthcare of Atlanta provided study funding.
Key clinical point: Pediatric heart transplantation outcomes for congenital heart disease haven’t improved in the current era, indicating ongoing challenges.
Major finding: Ten years following heart transplantation, 13% of patients had undergone retransplantation, 43% had died without retransplantation, and 44% were alive without retransplantation.
Data source: A review of 124 children with congenital heart disease who had heart transplantation at a single center.
Disclosures: The study authors had no relationships to disclose.
AHA: Broadening evidence for CABG over PCI in diabetics
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
ORLANDO – New evidence further strengthens the case for coronary artery bypass grafting over percutaneous coronary intervention as the preferred revascularization strategy in diabetic patients with multivessel coronary artery disease.
An analysis of 4,819 such patients in a British Columbia province-wide registry who underwent revascularization during 2007-2014 led to the conclusion that the 30-day adjusted risk of the primary composite endpoint of death, MI, or stroke was 39% lower in those who underwent coronary artery bypass grafting (CABG), Dr. Krishnan Ramanathan reported at the American Heart Association scientific sessions.
From day 31 through 5 years of follow-up, the relative risk reduction was 36% in favor of CABG, again after adjustment for age, sex, presentation with stable ischemic heart disease or stabilized acute coronary syndrome (ACS), urgency, renal insufficiency, liver disease, peripheral arterial disease, and left ventricular ejection fraction, added Dr. Ramanathan of the University of British Columbia in Vancouver.
These results in a broad patient population in real-world clinical practice, albeit in an observational, nonrandomized setting, mirror those in the earlier randomized FREEDOM trial sponsored by the National Heart, Lung, and Blood Institute. The 5-year rate of the composite of death, MI, or stroke in FREEDOM was 18.7% in the CABG group and 26.6% with percutaneous coronary intervention (PCI). The number needed to treat with CABG instead of PCI in FREEDOM in order to avoid one case of the composite endpoint was 12.6 (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
An important difference between the British Columbia and the FREEDOM trial is that the registry contained a much higher proportion of diabetic patients with multivessel disease who presented with acute coronary syndrome. Indeed, the ratio of stabilized ACS to stable ischemic heart disease patients in the registry was 62% to 38% as compared with 36% to 64% in FREEDOM. The registry patients underwent a median of 7.8 days of stabilization from the time of initial catheterization to CABG.
The registry data really shore up the advantages of CABG over PCI in diabetics with multivessel disease and ACS, Dr. Ramanathan noted. In the registry, the 30-day composite endpoint occurred in 4.4% of CABG-treated ACS patients, compared with 8.3% with PCI. For 31 days through 5 years, the rates were 21.4% versus 34.7%. The differences favoring CABG were highly significant at both time points.
FREEDOM led to two important revisions in the 2014 guidelines on coronary revascularization, issued by the American College of Cardiology, American Heart Association, American Academy of Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiac Angiography and Interventions, and Society of Thoracic Surgeons. In a focused update issued earlier this year, a new class I recommendation was issued calling for a heart team approach to revascularization in patients with diabetes mellitus and complex multivessel coronary artery disease (CAD). And a recommendation for CABG over PCI for improving survival in diabetic patients with multivessel CAD was upgraded from class IIa to class I.
Even though FREEDOM was a major randomized trial that might be expected to be practice changing, that hasn’t happened. A report from the ACC’s National Cardiovascular Data ACTION Registry presented earlier this year at the ACC annual scientific session documented that the most common revascularization strategy for diabetic patients with multivessel CAD following a non–ST elevation ACS remains PCI, as has been the case since the registry was created. In fact, following the 2012 publication of FREEDOM, the proportion of such patients treated by PCI took a sharp uptick in 2013-2014, according to Dr. Ramanathan.
In the British Columbia registry, 64% of diabetic patients with multivessel disease and an ACS were treated by PCI, 36% by CABG.
“Overall, CABG in stabilized ACS patients is underutilized,” he said.
Discussant Dr. Marc Ruel declared, “The salient finding about the British Columbia study is not so much about the stable ischemic heart disease patients, but about the high proportion of ACS patients in the study. CABG was better than PCI for all major adverse cardiovascular events and each component of the endpoint.”
Dr. Ruel, professor and chair of cardiac surgery at the University of Ottawa Heart Institute, coauthored a meta-analysis of randomized controlled trials comparing CABG to PCI in diabetic patients. Half of the trials used later-generation drug-eluting stents. At 5 years of follow-up, the relative risk of all-cause mortality in diabetic patients allocated to CABG was 0.67 (Lancet Diabetes Endocrinol. 2013 Dec;1[4]:317-28).
“Remember that 0.67 because it’s a recurring number in our literature,” he advised.
For example, in the British Columbia study the relative risk of death, MI, or stroke from 31 days to 5 years was 0.64 in the CABG as compared with the PCI group. And in a patient-level meta-analysis of the FREEDOM, BARI-2D, and COURAGE trials presented by Dr. John Mancini earlier at the AHA scientific sessions in Orlando, CABG plus optimal medical therapy was associated with a 0.65 relative risk of death, MI, or stroke, compared with PCI plus optimal medical therapy, which in turn wasn’t significantly better than optimal medical therapy alone, Dr. Ruel noted.
The 2015 European Society of Cardiology guidelines on management of ACS state that a heart team discussion involving a cardiologist and cardiac surgeon does not need to take place for every patient presenting with multivessel disease and a non–ST elevation ACS. The British Columbia study, coupled with the other evidence, “gives new credence” to a call for revision of that recommendation in diabetic patients, he said.
The British Columbia study was supported by the British Columbia Provincial Health Services Authority. Dr. Ramanathan reported having no financial conflicts.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: New evidence reinforces CABG as preferred over PCI for revascularization in diabetic patients with multivessel CAD.
Major finding: Diabetic patients with multivessel CAD were 36% less likely to experience death, MI, or stroke within the next 5 years if they underwent revascularization with CABG than PCI.
Data source: This observational registry study included 4,819 diabetic patients with multivessel CAD who underwent CABG or isolated PCI for stable ischemic heart disease or stabilized acute coronary syndrome.
Disclosures: The study was supported by the British Columbia Provincial Health Services Authority. The presenter reported having no financial conflicts of interest.
Steroids did not reduce kidney injury in CABG
SAN DIEGO – Among patients undergoing cardiac bypass surgery, perioperative use of corticosteroids did not alter the risk of acute kidney injury, results from a large randomized trial showed.
“Worldwide, over 20 million cardiac surgeries are done each year, but 4 million are complicated by acute kidney injury, and 200,000 are complicated by severe kidney injury treated with dialysis,” Dr. Amit X. Garg said during a press briefing at the annual meeting of the American Society of Nephrology. “So certainly people would benefit from a therapy to prevent acute kidney injury (AKI) and improve the safety of surgery.”
Dr. Garg, a nephrologist at the London Health Sciences Centre in London, Ontario, Canada, noted that cardiopulmonary bypass initiates a systemic inflammatory response syndrome, “which activates complement, inflammatory cytokines, and other inflammatory mediators, which in turn increases endothelial permeability, organ damage, and increased morbidity and mortality, including acute kidney injury.” Researchers are interested in corticosteroids, “because they suppress this inflammatory response. In other settings, such as acute glomerulonephritis, we successfully use corticosteroids to treat acute inflammation in the kidney,” he said.
In a study known as the Steroids in caRdiac Surgery Trial (SIRS), researchers at 79 centers in 18 countries set out to investigate if methylprednisolone alters the risk of acute kidney injury in patients undergoing cardiac surgery with cardiopulmonary bypass. Between June 2007 and December 2013, 7,286 patients were randomized to intravenous methylprednisolone 250 mg at anesthetic induction and 250 mg at initiation of coronary bypass, or placebo.
AKI was defined as a 0.3 mg/dL increase or greater in postoperative serum creatinine concentration from the preoperative concentration within 14 days following surgery, or a 50% increase from the preoperative value within 14 days following surgery. Secondary outcomes included different stages of AKI and receipt of acute dialysis in the 30 days following surgery. Patients, caregivers, and researchers were blinded to the treatment allocation.
Of the 7,286 patients, 3,647 received methylprednisolone and 3,639 received placebo. The mean age of patients was 60 years, 60% were men, 26% were diabetic, and 25% of patients had combined CABG and valve surgery.
The SIRS Investigators reported that the risk of AKI was similar among patients who received methylprednisolone and those who received placebo (40.9% vs. 39.5%, respectively; relative risk 1.03). Results were similar across multiple categorical definitions of AKI, including AKI or death (41.5% vs 40.2%; RR 1.03); AKI stage of 2 or greater (9.9% vs 9.9%; RR 1.01); AKI stage of 3 or greater (4% vs. 4.5%; RR .89), and being on acute dialysis (2.6% vs. 2.4%; RR 1.08).
“There was no benefit of steroids on the risk of AKI in those with or without preoperative chronic kidney disease,” Dr. Garg said. “The result was also not different in the subpopulation of patients with AKI as defined by Kidney Disease Improving Global Outcomes.” Results from SIRS “would suggest that patients undergoing cardiac surgery with cardiopulmonary bypass should not use prophylactic steroids to prevent AKI. When we consider the side effect profile, the most clinically relevant outcomes, and apply the GRADE framework [the Grading of Recommendations Assessment, Development, and Evaluation] to the available evidence, we would recommend that steroids not be used in this way, with a grade 1B recommendation.”
The study was sponsored by the Population Health Research Institute in Hamilton, Ontario and the Canadian Institutes of Health Research. Dr. Garg reported having no relevant financial disclosures for this study.
SAN DIEGO – Among patients undergoing cardiac bypass surgery, perioperative use of corticosteroids did not alter the risk of acute kidney injury, results from a large randomized trial showed.
“Worldwide, over 20 million cardiac surgeries are done each year, but 4 million are complicated by acute kidney injury, and 200,000 are complicated by severe kidney injury treated with dialysis,” Dr. Amit X. Garg said during a press briefing at the annual meeting of the American Society of Nephrology. “So certainly people would benefit from a therapy to prevent acute kidney injury (AKI) and improve the safety of surgery.”
Dr. Garg, a nephrologist at the London Health Sciences Centre in London, Ontario, Canada, noted that cardiopulmonary bypass initiates a systemic inflammatory response syndrome, “which activates complement, inflammatory cytokines, and other inflammatory mediators, which in turn increases endothelial permeability, organ damage, and increased morbidity and mortality, including acute kidney injury.” Researchers are interested in corticosteroids, “because they suppress this inflammatory response. In other settings, such as acute glomerulonephritis, we successfully use corticosteroids to treat acute inflammation in the kidney,” he said.
In a study known as the Steroids in caRdiac Surgery Trial (SIRS), researchers at 79 centers in 18 countries set out to investigate if methylprednisolone alters the risk of acute kidney injury in patients undergoing cardiac surgery with cardiopulmonary bypass. Between June 2007 and December 2013, 7,286 patients were randomized to intravenous methylprednisolone 250 mg at anesthetic induction and 250 mg at initiation of coronary bypass, or placebo.
AKI was defined as a 0.3 mg/dL increase or greater in postoperative serum creatinine concentration from the preoperative concentration within 14 days following surgery, or a 50% increase from the preoperative value within 14 days following surgery. Secondary outcomes included different stages of AKI and receipt of acute dialysis in the 30 days following surgery. Patients, caregivers, and researchers were blinded to the treatment allocation.
Of the 7,286 patients, 3,647 received methylprednisolone and 3,639 received placebo. The mean age of patients was 60 years, 60% were men, 26% were diabetic, and 25% of patients had combined CABG and valve surgery.
The SIRS Investigators reported that the risk of AKI was similar among patients who received methylprednisolone and those who received placebo (40.9% vs. 39.5%, respectively; relative risk 1.03). Results were similar across multiple categorical definitions of AKI, including AKI or death (41.5% vs 40.2%; RR 1.03); AKI stage of 2 or greater (9.9% vs 9.9%; RR 1.01); AKI stage of 3 or greater (4% vs. 4.5%; RR .89), and being on acute dialysis (2.6% vs. 2.4%; RR 1.08).
“There was no benefit of steroids on the risk of AKI in those with or without preoperative chronic kidney disease,” Dr. Garg said. “The result was also not different in the subpopulation of patients with AKI as defined by Kidney Disease Improving Global Outcomes.” Results from SIRS “would suggest that patients undergoing cardiac surgery with cardiopulmonary bypass should not use prophylactic steroids to prevent AKI. When we consider the side effect profile, the most clinically relevant outcomes, and apply the GRADE framework [the Grading of Recommendations Assessment, Development, and Evaluation] to the available evidence, we would recommend that steroids not be used in this way, with a grade 1B recommendation.”
The study was sponsored by the Population Health Research Institute in Hamilton, Ontario and the Canadian Institutes of Health Research. Dr. Garg reported having no relevant financial disclosures for this study.
SAN DIEGO – Among patients undergoing cardiac bypass surgery, perioperative use of corticosteroids did not alter the risk of acute kidney injury, results from a large randomized trial showed.
“Worldwide, over 20 million cardiac surgeries are done each year, but 4 million are complicated by acute kidney injury, and 200,000 are complicated by severe kidney injury treated with dialysis,” Dr. Amit X. Garg said during a press briefing at the annual meeting of the American Society of Nephrology. “So certainly people would benefit from a therapy to prevent acute kidney injury (AKI) and improve the safety of surgery.”
Dr. Garg, a nephrologist at the London Health Sciences Centre in London, Ontario, Canada, noted that cardiopulmonary bypass initiates a systemic inflammatory response syndrome, “which activates complement, inflammatory cytokines, and other inflammatory mediators, which in turn increases endothelial permeability, organ damage, and increased morbidity and mortality, including acute kidney injury.” Researchers are interested in corticosteroids, “because they suppress this inflammatory response. In other settings, such as acute glomerulonephritis, we successfully use corticosteroids to treat acute inflammation in the kidney,” he said.
In a study known as the Steroids in caRdiac Surgery Trial (SIRS), researchers at 79 centers in 18 countries set out to investigate if methylprednisolone alters the risk of acute kidney injury in patients undergoing cardiac surgery with cardiopulmonary bypass. Between June 2007 and December 2013, 7,286 patients were randomized to intravenous methylprednisolone 250 mg at anesthetic induction and 250 mg at initiation of coronary bypass, or placebo.
AKI was defined as a 0.3 mg/dL increase or greater in postoperative serum creatinine concentration from the preoperative concentration within 14 days following surgery, or a 50% increase from the preoperative value within 14 days following surgery. Secondary outcomes included different stages of AKI and receipt of acute dialysis in the 30 days following surgery. Patients, caregivers, and researchers were blinded to the treatment allocation.
Of the 7,286 patients, 3,647 received methylprednisolone and 3,639 received placebo. The mean age of patients was 60 years, 60% were men, 26% were diabetic, and 25% of patients had combined CABG and valve surgery.
The SIRS Investigators reported that the risk of AKI was similar among patients who received methylprednisolone and those who received placebo (40.9% vs. 39.5%, respectively; relative risk 1.03). Results were similar across multiple categorical definitions of AKI, including AKI or death (41.5% vs 40.2%; RR 1.03); AKI stage of 2 or greater (9.9% vs 9.9%; RR 1.01); AKI stage of 3 or greater (4% vs. 4.5%; RR .89), and being on acute dialysis (2.6% vs. 2.4%; RR 1.08).
“There was no benefit of steroids on the risk of AKI in those with or without preoperative chronic kidney disease,” Dr. Garg said. “The result was also not different in the subpopulation of patients with AKI as defined by Kidney Disease Improving Global Outcomes.” Results from SIRS “would suggest that patients undergoing cardiac surgery with cardiopulmonary bypass should not use prophylactic steroids to prevent AKI. When we consider the side effect profile, the most clinically relevant outcomes, and apply the GRADE framework [the Grading of Recommendations Assessment, Development, and Evaluation] to the available evidence, we would recommend that steroids not be used in this way, with a grade 1B recommendation.”
The study was sponsored by the Population Health Research Institute in Hamilton, Ontario and the Canadian Institutes of Health Research. Dr. Garg reported having no relevant financial disclosures for this study.
AT KIDNEY WEEK 2015
Key clinical point: Perioperative use of steroids did not affect the risk of acute kidney injury (AKI) in patients undergoing coronary bypass surgery.
Major finding: The risk of AKI was similar among patients who received methylprednisolone and those who received placebo (40.9% vs. 39.5%, respectively; relative risk 1.03).
Data source: A study of 7,286 patients undergoing cardiopulmonary bypass surgery who were randomized to intravenous methylprednisolone 250 mg at anesthetic induction and 250 mg at initiation of coronary bypass, or placebo.
Disclosures: The study was sponsored by the Population Health Research Institute in Hamilton, Ontario and the Canadian Institutes of Health Research. Dr. Garg reported having no relevant financial disclosures for this study.
IVUS-guided stent cuts MACE rate
Coronary stent implantation guided by intravascular ultrasound reduces the 1-year rate of major adverse cardiac events in patients who have long lesions, compared with standard angiography-guided stent implantation, Dr. Sung-Jin Hong reported at the American Heart Association annual scientific sessions, a presentation that was simultaneously published online Nov. 10 in JAMA.
Even though four meta-analyses have demonstrated the superiority of IVUS-guided implantation and recent guidelines recommend IVUS guidance for select patients to optimize results, “the effect of IVUS-guided drug-eluting stent implantation on clinical outcomes remains uncertain because of the limited number of properly powered randomized clinical trials,” said Dr. Hong of Sanggye Paik Hospital at Inje University and of Severance Cardiovascular Hospital at Yonsei University, both in Seoul, South Korea.
Dr. Hong and his associates performed a 4-year industry-sponsored randomized trial comparing the two techniques in 1,400 patients who had typical chest pain or evidence of myocardial ischemia and were eligible to receive an everolimus-eluting stent of 28 mm or more in length. The study participants were randomly assigned to undergo either IVUS-guided (700 patients) or angiography-guided (700 patients) stent implantation at 20 Korean medical centers and were followed up for 1 year. The mean patient age was 64 years, and 69% of the participants were men. The mean stent length of the targeted lesions was 39.3 mm.
The primary endpoint – a composite of major adverse cardiac events such as death, target-lesion-related MI, or ischemia-driven revascularization of the target lesion at 1 year – occurred in 2.9% of the IVUS group and 5.8% of the angiography group. This is a significant difference, with the IVUS group showing a 2.9% absolute reduction and a 48% relative reduction in the primary endpoint, the investigators said (JAMA 2015 Nov 10. doi: 10.1001/jama.2015.15454).
The superiority of IVUS-guided stent implantation was attributable primarily to a marked decrease in target-lesion revascularization in that group (2.5% of patients) compared with the angiography-guided group (5.0%). This in turn was likely due to the fact that adjunctive poststent balloon dilation was done more frequently in the IVUS group (76% vs 57%) and that the mean final balloon size was larger. Consequently, the minimum lumen diameter was greater in the IVUS-guided stent group than in the angiography-guided stent group.
“To our knowledge, [this] is the first demonstration of the clinical benefit of IVUS guidance in second-generation drug-eluting stent implantation in an adequately powered randomized clinical trial,” the investigators added.
Coronary stent implantation guided by intravascular ultrasound reduces the 1-year rate of major adverse cardiac events in patients who have long lesions, compared with standard angiography-guided stent implantation, Dr. Sung-Jin Hong reported at the American Heart Association annual scientific sessions, a presentation that was simultaneously published online Nov. 10 in JAMA.
Even though four meta-analyses have demonstrated the superiority of IVUS-guided implantation and recent guidelines recommend IVUS guidance for select patients to optimize results, “the effect of IVUS-guided drug-eluting stent implantation on clinical outcomes remains uncertain because of the limited number of properly powered randomized clinical trials,” said Dr. Hong of Sanggye Paik Hospital at Inje University and of Severance Cardiovascular Hospital at Yonsei University, both in Seoul, South Korea.
Dr. Hong and his associates performed a 4-year industry-sponsored randomized trial comparing the two techniques in 1,400 patients who had typical chest pain or evidence of myocardial ischemia and were eligible to receive an everolimus-eluting stent of 28 mm or more in length. The study participants were randomly assigned to undergo either IVUS-guided (700 patients) or angiography-guided (700 patients) stent implantation at 20 Korean medical centers and were followed up for 1 year. The mean patient age was 64 years, and 69% of the participants were men. The mean stent length of the targeted lesions was 39.3 mm.
The primary endpoint – a composite of major adverse cardiac events such as death, target-lesion-related MI, or ischemia-driven revascularization of the target lesion at 1 year – occurred in 2.9% of the IVUS group and 5.8% of the angiography group. This is a significant difference, with the IVUS group showing a 2.9% absolute reduction and a 48% relative reduction in the primary endpoint, the investigators said (JAMA 2015 Nov 10. doi: 10.1001/jama.2015.15454).
The superiority of IVUS-guided stent implantation was attributable primarily to a marked decrease in target-lesion revascularization in that group (2.5% of patients) compared with the angiography-guided group (5.0%). This in turn was likely due to the fact that adjunctive poststent balloon dilation was done more frequently in the IVUS group (76% vs 57%) and that the mean final balloon size was larger. Consequently, the minimum lumen diameter was greater in the IVUS-guided stent group than in the angiography-guided stent group.
“To our knowledge, [this] is the first demonstration of the clinical benefit of IVUS guidance in second-generation drug-eluting stent implantation in an adequately powered randomized clinical trial,” the investigators added.
Coronary stent implantation guided by intravascular ultrasound reduces the 1-year rate of major adverse cardiac events in patients who have long lesions, compared with standard angiography-guided stent implantation, Dr. Sung-Jin Hong reported at the American Heart Association annual scientific sessions, a presentation that was simultaneously published online Nov. 10 in JAMA.
Even though four meta-analyses have demonstrated the superiority of IVUS-guided implantation and recent guidelines recommend IVUS guidance for select patients to optimize results, “the effect of IVUS-guided drug-eluting stent implantation on clinical outcomes remains uncertain because of the limited number of properly powered randomized clinical trials,” said Dr. Hong of Sanggye Paik Hospital at Inje University and of Severance Cardiovascular Hospital at Yonsei University, both in Seoul, South Korea.
Dr. Hong and his associates performed a 4-year industry-sponsored randomized trial comparing the two techniques in 1,400 patients who had typical chest pain or evidence of myocardial ischemia and were eligible to receive an everolimus-eluting stent of 28 mm or more in length. The study participants were randomly assigned to undergo either IVUS-guided (700 patients) or angiography-guided (700 patients) stent implantation at 20 Korean medical centers and were followed up for 1 year. The mean patient age was 64 years, and 69% of the participants were men. The mean stent length of the targeted lesions was 39.3 mm.
The primary endpoint – a composite of major adverse cardiac events such as death, target-lesion-related MI, or ischemia-driven revascularization of the target lesion at 1 year – occurred in 2.9% of the IVUS group and 5.8% of the angiography group. This is a significant difference, with the IVUS group showing a 2.9% absolute reduction and a 48% relative reduction in the primary endpoint, the investigators said (JAMA 2015 Nov 10. doi: 10.1001/jama.2015.15454).
The superiority of IVUS-guided stent implantation was attributable primarily to a marked decrease in target-lesion revascularization in that group (2.5% of patients) compared with the angiography-guided group (5.0%). This in turn was likely due to the fact that adjunctive poststent balloon dilation was done more frequently in the IVUS group (76% vs 57%) and that the mean final balloon size was larger. Consequently, the minimum lumen diameter was greater in the IVUS-guided stent group than in the angiography-guided stent group.
“To our knowledge, [this] is the first demonstration of the clinical benefit of IVUS guidance in second-generation drug-eluting stent implantation in an adequately powered randomized clinical trial,” the investigators added.
FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: IVUS-guided stent implantation decreases the 1-year rate of major adverse cardiac events in patients with long coronary lesions, compared with angiography-guided stent implantation.
Major finding: The IVUS group showed a 2.9% absolute reduction and a 48% relative reduction in the primary endpoint, a composite of major adverse cardiac events at 1 year.
Data source: A multicenter randomized trial involving 1,400 patients with long coronary lesions who underwent stent implantation at 20 Korean medical centers during a 4-year period and were followed up for 1 year.
Disclosures: This study was supported by the Cardiovascular Research Center in Seoul and funded by Abbott Vascular, maker of the everolimus-eluting stent. Dr. Hong and his associates reported having no relevant financial conflicts of interest.