User login
VIDEO: Which lesions are best for bronchoscopic endoluminal treatment?
PHOENIX – According to Dr. Moishe Liberman, promising lesions for bronchoscopic endoluminal treatment include endobronchial lesions and intraluminal exophytic tumors within the trachea or main bronchus, provided that the distal airway lumen is visible and you can get past the tumor with a flexible endoscope.
“We always teach the fellows that if you get pus back when you’re trying to get around the tumor or play with the tumor, you’re usually going to have a very good result,” said Dr. Liberman, a thoracic surgeon who directs the endoscopic tracheo-bronchial and oesophageal center at the Centre hospitalier de l’Université de Montréal, Quebec, Canada. “If you play with the tumor and you get the tumor out and you get nothing back, usually the CT scan or the X-ray postoperatively is going to look just like it did preoperatively, even though endoscopically you might have a good result.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Central lesions are also excellent candidates for endoluminal therapy, he said in a video interview at the meeting. Distal lesions in the small bronchi “are candidates but are much more difficult and require more specialized tools. The shorter the lesion, the more likely you are to have good success.”
Available options for delivering energy endoscopically include electrocautery, argon plasma coagulation, laser, and cryotherapy. A disadvantage of all of the thermal modalities except for cryotherapy “include the potential for airway fire and you have to work with low FiO2s [fraction of inspired oxygen],” Dr. Liberman noted. “A lot of these patients need high FiO2s to saturate, so I think that’s always an issue. We never go on cardiopulmonary bypass to do these cases and we never cannulate patients to do these cases. You also have to worry about gas emboli, especially when you open up big vessels. These modalities can also cause inadvertent airway injury, delayed effects, and bronchoscope damage.”
In general, he continued, laser-tissue interactions depend on the power and the wavelength of the laser as well as the color and the water content of the target tissue. “The power density of the wavelength you choose determines its ability to cut, coagulate, or vaporize the tissue,” he said.
“As the power density increases, the laser fiber approaches the target tissue. Power density is more important than the energy delivered.”
The Nd:YAG (neodymium-doped yttrium aluminium garnet) laser, which causes more destruction in the deep tissue than on the surface, is the most common laser used in interventional airway procedures, he said. Two other commonly used lasers include the KTP (potassium titanyl phosphate) and the CO2. “I like CO2s a lot for upper airway and subglottic problems as well as vocal cord problems,” Dr. Liberman said. “It’s very precise and has low penetration. The Nd:YAG is very good for deep penetration. You need familiarity with these. I don’t think you can just take one of these off the shelf if you’ve never used it before. Sometimes your ENT [ear nose and throat] or urology colleagues can help you, because they’re using a lot more of these lasers than we are.”
Contraindications for laser bronchoscopy include operable lesions. Dr. Liberman said that while he and his associates use lasers in a preoperative setting, “we’re very careful not to damage proximal or distal airway when we know we’re going to do a sleeve resection or pneumonectomy.”
Other contraindications for laser bronchoscopy include patients with a poor short-term prognosis, severe coagulation disorder, extrinsic airway obstruction, tracheoesophageal fistula or T-Med fistula, those with extensive submucosal disease causing obstruction, and those with lesion adjacent to the esophagus or to a major vessel.
Dr. Liberman reported having received research grants from Ethicon, Boston Scientific, Olympus, Covidien, and Baxter.
PHOENIX – According to Dr. Moishe Liberman, promising lesions for bronchoscopic endoluminal treatment include endobronchial lesions and intraluminal exophytic tumors within the trachea or main bronchus, provided that the distal airway lumen is visible and you can get past the tumor with a flexible endoscope.
“We always teach the fellows that if you get pus back when you’re trying to get around the tumor or play with the tumor, you’re usually going to have a very good result,” said Dr. Liberman, a thoracic surgeon who directs the endoscopic tracheo-bronchial and oesophageal center at the Centre hospitalier de l’Université de Montréal, Quebec, Canada. “If you play with the tumor and you get the tumor out and you get nothing back, usually the CT scan or the X-ray postoperatively is going to look just like it did preoperatively, even though endoscopically you might have a good result.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Central lesions are also excellent candidates for endoluminal therapy, he said in a video interview at the meeting. Distal lesions in the small bronchi “are candidates but are much more difficult and require more specialized tools. The shorter the lesion, the more likely you are to have good success.”
Available options for delivering energy endoscopically include electrocautery, argon plasma coagulation, laser, and cryotherapy. A disadvantage of all of the thermal modalities except for cryotherapy “include the potential for airway fire and you have to work with low FiO2s [fraction of inspired oxygen],” Dr. Liberman noted. “A lot of these patients need high FiO2s to saturate, so I think that’s always an issue. We never go on cardiopulmonary bypass to do these cases and we never cannulate patients to do these cases. You also have to worry about gas emboli, especially when you open up big vessels. These modalities can also cause inadvertent airway injury, delayed effects, and bronchoscope damage.”
In general, he continued, laser-tissue interactions depend on the power and the wavelength of the laser as well as the color and the water content of the target tissue. “The power density of the wavelength you choose determines its ability to cut, coagulate, or vaporize the tissue,” he said.
“As the power density increases, the laser fiber approaches the target tissue. Power density is more important than the energy delivered.”
The Nd:YAG (neodymium-doped yttrium aluminium garnet) laser, which causes more destruction in the deep tissue than on the surface, is the most common laser used in interventional airway procedures, he said. Two other commonly used lasers include the KTP (potassium titanyl phosphate) and the CO2. “I like CO2s a lot for upper airway and subglottic problems as well as vocal cord problems,” Dr. Liberman said. “It’s very precise and has low penetration. The Nd:YAG is very good for deep penetration. You need familiarity with these. I don’t think you can just take one of these off the shelf if you’ve never used it before. Sometimes your ENT [ear nose and throat] or urology colleagues can help you, because they’re using a lot more of these lasers than we are.”
Contraindications for laser bronchoscopy include operable lesions. Dr. Liberman said that while he and his associates use lasers in a preoperative setting, “we’re very careful not to damage proximal or distal airway when we know we’re going to do a sleeve resection or pneumonectomy.”
Other contraindications for laser bronchoscopy include patients with a poor short-term prognosis, severe coagulation disorder, extrinsic airway obstruction, tracheoesophageal fistula or T-Med fistula, those with extensive submucosal disease causing obstruction, and those with lesion adjacent to the esophagus or to a major vessel.
Dr. Liberman reported having received research grants from Ethicon, Boston Scientific, Olympus, Covidien, and Baxter.
PHOENIX – According to Dr. Moishe Liberman, promising lesions for bronchoscopic endoluminal treatment include endobronchial lesions and intraluminal exophytic tumors within the trachea or main bronchus, provided that the distal airway lumen is visible and you can get past the tumor with a flexible endoscope.
“We always teach the fellows that if you get pus back when you’re trying to get around the tumor or play with the tumor, you’re usually going to have a very good result,” said Dr. Liberman, a thoracic surgeon who directs the endoscopic tracheo-bronchial and oesophageal center at the Centre hospitalier de l’Université de Montréal, Quebec, Canada. “If you play with the tumor and you get the tumor out and you get nothing back, usually the CT scan or the X-ray postoperatively is going to look just like it did preoperatively, even though endoscopically you might have a good result.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Central lesions are also excellent candidates for endoluminal therapy, he said in a video interview at the meeting. Distal lesions in the small bronchi “are candidates but are much more difficult and require more specialized tools. The shorter the lesion, the more likely you are to have good success.”
Available options for delivering energy endoscopically include electrocautery, argon plasma coagulation, laser, and cryotherapy. A disadvantage of all of the thermal modalities except for cryotherapy “include the potential for airway fire and you have to work with low FiO2s [fraction of inspired oxygen],” Dr. Liberman noted. “A lot of these patients need high FiO2s to saturate, so I think that’s always an issue. We never go on cardiopulmonary bypass to do these cases and we never cannulate patients to do these cases. You also have to worry about gas emboli, especially when you open up big vessels. These modalities can also cause inadvertent airway injury, delayed effects, and bronchoscope damage.”
In general, he continued, laser-tissue interactions depend on the power and the wavelength of the laser as well as the color and the water content of the target tissue. “The power density of the wavelength you choose determines its ability to cut, coagulate, or vaporize the tissue,” he said.
“As the power density increases, the laser fiber approaches the target tissue. Power density is more important than the energy delivered.”
The Nd:YAG (neodymium-doped yttrium aluminium garnet) laser, which causes more destruction in the deep tissue than on the surface, is the most common laser used in interventional airway procedures, he said. Two other commonly used lasers include the KTP (potassium titanyl phosphate) and the CO2. “I like CO2s a lot for upper airway and subglottic problems as well as vocal cord problems,” Dr. Liberman said. “It’s very precise and has low penetration. The Nd:YAG is very good for deep penetration. You need familiarity with these. I don’t think you can just take one of these off the shelf if you’ve never used it before. Sometimes your ENT [ear nose and throat] or urology colleagues can help you, because they’re using a lot more of these lasers than we are.”
Contraindications for laser bronchoscopy include operable lesions. Dr. Liberman said that while he and his associates use lasers in a preoperative setting, “we’re very careful not to damage proximal or distal airway when we know we’re going to do a sleeve resection or pneumonectomy.”
Other contraindications for laser bronchoscopy include patients with a poor short-term prognosis, severe coagulation disorder, extrinsic airway obstruction, tracheoesophageal fistula or T-Med fistula, those with extensive submucosal disease causing obstruction, and those with lesion adjacent to the esophagus or to a major vessel.
Dr. Liberman reported having received research grants from Ethicon, Boston Scientific, Olympus, Covidien, and Baxter.
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
Hypertrophic cardiomyopathy: Who should get an ICD?
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Since the 2011 release of the current American College of Cardiology/American Heart Association guidelines on hypertrophic cardiomyopathy, several new evidence-based tools have emerged as being helpful in decision making regarding which patients should receive an implantable cardioverter-defibrillator (ICD) for primary prevention of sudden cardiac death, Dr. Rick A. Nishimura said at the annual Cardiovascular Conference at Snowmass.
These three tools – gadolinium-enhanced cardiovascular magnetic resonance imaging, a novel European risk score calculator, and a new appreciation of the importance of age-related risk – are most useful in the many cases of hypertrophic cardiomyopathy (HCM) where the cardiologist is on the fence regarding ICD placement because the patient doesn’t clearly meet the conventional major criteria for an ICD, according to Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Nishimura, a member of the writing panel for the current guidelines (Circulation. 2011 Dec 13;124[24]:2761-96), predicted these tools will be incorporated into the next iteration of the HCM guidelines.
Notably absent from Dr. Nishimura’s list of useful tools was genetic testing for assessment of SCD risk in a patient with HCM.
“You should not spend $6,000 to do a genetic study to try to predict who’s at risk for sudden death. It turns out that most mutations are neither inherently benign nor malignant. High-risk mutations come from high-risk families, so you can do just as well by taking a family history,” according to the cardiologist.
Dr. Nishimura explained that the clinical dilemma in trying to evaluate SCD risk in a patient who presents with HCM is that the overall risk is quite low – probably 1% or less per year in the total HCM population – yet HCM is the number-one cause of SCD in younger patients. And it can occur unpredictably years or decades after diagnosis of HCM.
While ICDs are of proven effectiveness in preventing SCD in patients with HCM, reliance solely upon the conventional risk predictors to identify those who should get a device is clearly inadequate. Those criteria have a positive predictive accuracy of less than 15%; in other words, roughly 85% of HCM patients who get an ICD never receive an appropriate, life-saving shock, Dr. Nishimura said.
“We have a lot of work left to do in order to better identify these patients. In our own data from the Mayo Clinic, 20%-25% of patients have inappropriate ICD shocks despite efforts to program the device to prevent such shocks. That’s especially common in younger, active patients with HCM, and when it occurs patients find it absolutely devastating,” according to the cardiologist.
As stated in the current guidelines, the established SCD risk factors that provide a strong indication for an ICD in a patient with HCM are prior documented cardiac arrest, ventricular fibrillation, or hemodynamically significant ventricular tachycardia. Additionally, risk factors which, in Dr. Nishimura’s view, probably warrant insertion of an ICD and, at the very least should trigger a physician-patient discussion about the risks and benefits of preventive device therapy, include a family history of HCM-related sudden death in a first-degree relative, massive left ventricular (LV) hypertrophy as defined by a maximum wall thickness of at least 30 mm, and recent unexplained syncope inconsistent with neurocardiogenic origin.
Less potent risk predictors where savvy clinical judgment becomes imperative include nonsustained ventricular tachycardia on 24-hour Holter monitoring, a hypotensive blood pressure response to exercise, and an increased LV wall thickness in a younger patient that doesn’t rise to the 30-mm standard. These are situations where gadolinium-enhanced MRI, consideration of patient age, and the European risk scoring system can help in the decision-making process, he said.
Gadolinium-enhanced MRI: Contrast-enhanced cardiovascular MRI with late gadolinium enhancement has emerged as a reliable marker of the myocyte disarray and interstitial fibrosis which serves as a substrate for ventricular arrhythmias. In a recent study of 1,293 HCM patients followed for a median of 3.3 years, the incidence of SCD events increased progressively with the extent of late gadolinium enhancement. Extensive late gadolinium enhancement, defined as involving at least 15% of LV mass, was associated with a doubled risk of SCD events in patients otherwise considered at low risk (Circulation. 2014 Aug 5;130[6]:484-95).
“This is probably going to become one of the key markers that can help you when you’re on the fence as to whether or not to put in an ICD. We’re getting MRIs with gadolinium now in all of our HCM patients. What matters is not gadolinium enhancement at the insertion of the left ventricle into the septum – a lot of people have that – but diffuse gadolinium enhancement throughout the septum,” Dr. Nishimura said.
Because SCD risk increases linearly with greater maximal LV wall thickness, gadolinium-enhanced MRI is particularly helpful in assessing risk in a younger patient with a maximal LV wall thickness of, say, 26 mm, he added.
Age: A study by led by Dr. Barry J. Maron, the cochair of the 2011 guideline committee and director of the HCM center at the Minneapolis Heart Institute, provides a new understanding that prophylactic ICD implantation is not warranted in patients with HCM who present at age 60 or older. In their study of 428 consecutive patients presenting with HCM at age 60 or above, the investigators found during 5.8 years of follow-up that the incidence of arrhythmic sudden death events was just 0.2% per year (Circulation. 2013 Feb 5;127[5]:585-93).
“They’ve shown that if you look at patients age 60 or above who have HCM, the risk of sudden cardiac death is almost nonexistent. That’s incredibly important to remember. Sudden death is something that’s going to happen in the younger population, under age 30,” Dr. Nishimura emphasized.
European SCD risk prediction tool: This tool was hailed as a major advance in the current European Society of Cardiology guidelines on HCM (Eur Heart J. 2014;35:2733-2779). The tool was incorporated into the guidelines. It is also available as a smartphone app.
The risk prediction tool (Eur Heart J. 2014 Aug 7;35[30]:2010-20) is a complex equation that incorporates seven predictive factors: age, maximal LV wall thickness, left atrial diameter, LV outflow tract gradient, family history of SCD, nonsustained VT, and unexplained syncope. After input on these seven factors, the equation spits out an individual’s estimated 5-year SCD risk. Based on the study of 3,675 consecutive HCM patients with a median 5.7 years of follow-up that was used to develop the risk equation, the current ESC guidelines state that an ICD is not warranted in HCM patients with a 5-year risk below 4%, device implantation should be considered in those whose risk is 4%-6%, and an ICD should be even more strongly considered in patients with a 5-year risk in excess of 6%.
“A lot of people across the pond are using this risk score. But there are some problems with it,” according to Dr. Nishimura.
In his view, it “doesn’t make much sense” to include left ventricular outflow tract gradient or left atrial diameter in the risk equation. Nor is unexplained syncope carefully defined. Also, the equation would be improved by incorporation of late gadolinium enhancement on MRI, left ventricular dysfunction, and presence or absence of apical aneurysm as predictive variables. But on the plus side, the European equation treats maximal LV wall thickness as a continuous variable, which is more appropriate than the single 30-mm cutoff used in the ACC/AHA guidelines.
The biggest limitation of the European prognostic score, however, is that it hasn’t yet been validated in an independent patient cohort, Dr. Nishimura said. He noted that when Dr. Maron and coworkers recently applied the European SCD risk equation retrospectively to 1,629 consecutive U.S. patients with HCM, the investigators concluded that the risk equation proved unreliable for prediction of future SCD events. Fifty-nine percent of patients who got an appropriate ICD shock or experienced SCD were misclassified as low risk and hence would not have received an ICD under the European guidelines (Am J Cardiol. 2015 Sep 1;116[5]:757-64).
Nonetheless, because of the limited predictive accuracy of today’s standard methods of assessing SCD risk, Dr. Nishimura considers application of the European risk score to be “reasonable” in HCM patients who don’t have any of the strong indications for an ICD.
“If it comes up with an estimated 5-year risk greater than 6%, I think it’s very reasonable to consider implantation of an ICD,” he said.
Dr. Nishimura observed that in addition to assessing SCD risk, cardiologists have two other separate essential tasks when a patient presents with HCM. One is to screen and counsel the first-degree relatives. The other is to determine whether a left ventricular outflow tract obstruction is present in a symptomatic patient and, if so, to improve symptoms by treating the associated hemodynamic abnormalities medically and if need be by septal ablation or septal myectomy.
He reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Presurgery radiation shows benefit in lung cancer
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).
 |
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).
 |
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
Implementing the treatment regimen for malignant pleural mesothelioma (MPM) that the Toronto researchers studied poses “several high stakes challenges,” Dr. Valerie Rusch and coauthors at Memorial Sloan-Kettering Cancer Center, New York, said in their invited commentary (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.10.038).
 |
Dr. Valerie W. Rusch |
But they noted challenges involved with conventional multi-modality treatment for MPM, namely the 6 months of intensive treatment. However, the experience of the Toronto researchers will be difficult to replicate, they said. “Such outstanding results reflect the expertise of Dr. de Perrot and colleagues in the surgical care of MPM and the excellence of their multidisciplinary program,” Dr. Rusch and coauthors said.
The study results are among the best reported for MPM to date, they added, but they asked why. “Are they solely related to patient selection or do they reflect the true impact of a novel approach to treatment?”
Patients selected for the treatment need to be able to undergo the extrapleural pneumonectomy (EPP) and the surgeon has to be able to predict the resectability of the tumor. But limitations in existing staging methods for MPM make it difficult to predict tumor resectability. “To avoid bronchial stump leaks and other serious complications after EPP requires experience along with meticulous surgical technique and postoperative care,” Dr. Rusch and colleagues said. “Only high-volume centers of excellence could potentially reproduce these results.”
Despite the waning in popularity of EPP, the study results underscore its effectiveness in carefully selected patients – “those with epithelioid tumor histology and no tumor metastases.” To corroborate the findings, reports on other centers’ experience along with human and animal studies rather than a randomized clinical trial are needed. “Dr. de Perrot and colleagues may have been not only bold but SMART,” Dr. Rusch and colleagues said.
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
The popularity of extrapleural pneumonectomy to treat asbestos-related thoracic mesothelioma has yielded to extended pleurectomy/decortication in recent years, but a recent study suggests that the extrapleural pneumonectomy procedure can achieve good results in a new protocol that involves administering radiation therapy before surgery as opposed the more conventional approach of radiation after surgery.
Researchers at the University of Toronto reported on their protocol that uses accelerated intensity modulated radiation therapy (IMRT) for malignant pleural mesothelioma (MPM) (J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2015.09.129). They call the protocol SMART, for Surgery for Mesothelioma After Radiation Therapy.
“The rationale to develop this protocol was to optimize the delivery of radiation to the whole tumor bed, sterilize the edges of the tumor to limit the risk of spillage at the time of surgery, develop a shorter treatment plan and potentiate the activation of the immune system by using a hypofractionated regimen,” wrote Dr. Marc de Perrot and colleagues.
The protocol involves delivering 25 Gy of radiation in five daily fractions over a week to the entire side of the thorax with 5 Gy boosts based on imaging, followed by extrapleural pneumonectomy (EPP) 4-6 days later. Patients with three or more positive lymph notes (ypN2 disease) also are offered adjuvant chemotherapy.
The researchers performed the protocol on 62 patients from November 2008 to October 2014, which represents 24% of all patients with MPM seen at the institution in that period. Fifty-two patients were men and ages ranged from 41 to 75 years. Clinical stage of cancer ranged from T1N0 in 10 patients, to T2N0 in 35 and T3N0 in 13 (two had T4N0 and two had T3N2). Forty-five had right-side cancers. Six patients received an extended protocol for various reasons, including tumor extending to the chest wall.
All 62 patients completed IMRT and EPP. All but one had resection and reconstruction of the diaphragm, and all but four had resection and reconstruction of the pericardium.
Overall death rate was 4.8% (three patients). Results were better in patients with epithelioid tumors, with a median survival of 51 months and disease-free survival of 47 months. Those with biphasic subtypes had median survival of 10 months and disease-free survival of 8 months. Eight patients had ipsilateral chest recurrence. “This analysis demonstrates that the SMART approach is particularly encouraging for patients with epithelial subtype,” Dr. de Perrot and coauthors said. They no longer perform the SMART protocol on patients with biphasic subtype.
The protocol was not without complications. Twenty-four patients, about 38%, had serious complications that required intervention or worse. Twelve had atrial fibrillation, but none advanced to life-threatening disease. Among other complications, four had empyema – one resulting in death – and three had pulmonary emboli. One other patient in the complications group died from pneumonia, and another died from a heart attack at home.
This is the Toronto researchers’ second attempt at studying the three-modality approach. In their first attempt, only half the patients who started with preoperative chemotherapy went onto complete the radiation after surgery because of difficulties administering it (J Thorac Cardiovasc Surg. 2007;133:111-6; J Clin Oncol. 2009;27:1413-8). Also, about 25% of patients had disease progression during induction chemotherapy and could not go onto surgery.
They designed the most recent trial to deliver radiation before surgery because of the excellent local control of cancer along with evidence that MPM tumors were radio-sensitive. “Considering the risk of disease progression on induction chemotherapy, we felt that switching the order of therapy was potentially a better option for patients with surgically resectable disease,” Dr. de Perrott and colleagues said.
The researchers cited the study’s single-center nature with a single treatment arm, and the lack of longer-term follow-up, as limitations. “However, in our own experience, this approach has been very encouraging and has become our primary option for patients with surgically resectable MPM,” they noted.
The study authors had no conflicts to disclose.
Key clinical point: A new protocol that involves accelerated hemithoracic intensity modulated radiation before surgery for lung mesothelioma delivered encouraging results in patients with epithelioid tumors.
Major finding: Disease-free survival was 47 months in epithelial subtypes compared with 8 months in biphasic subtypes.
Data source: A single-center population of 62 patients with malignant pleural mesothelioma treated between November 2008 and October 2014.
Disclosures: The study authors had no relationships to disclose.
Off-pump bypass may confer stroke benefit
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
That off-pump coronary artery bypass (OPCAB) grafting provides no benefit or, at best, a negligible benefit over conventional on-pump surgery in terms of 30-day death rates and risk of myocardial infarction is a question that can be laid “safely to bed,” Dr. Fraser Rubens of the University of Ottawa Heart Institute said in his invited commentary (J Thorac Cardiovasc Surg. 2016;151:78-9).
However, less clear cut is the meta-analysis researchers’ assertion that off-pump CABG can significantly reduce the risk of future stroke, and that requires a close examination of the structural shortcomings of any meta-analysis, Dr. Rubens said. He cited a report that stated meta-analyses may inaccurately predict the outcomes of subsequent large randomized clinical trials in about one-third of all cases (N Engl J Med 1997;337:536-42).
Smaller trials like those used in a meta-analysis are more likely to be flawed because of a lax peer review or compromised methodology, Dr. Rubens said. The largest randomized trial the authors used in the meta-analysis showed “certainly no difference in stroke,” and when all trials with 200 or fewer patients were excluded, the stroke rates were 1.4% in the off-pump group vs. 1.6% in the on-pump population, he said.
To validate that difference would require a number needed to treat of 500 patients to prevent one stroke, Dr. Rubens said, “and the sample size required to prove this difference would exceed 58,000 patients per group” – whereas the large-trial cohort in this meta-analysis population was about a tenth of that.
“One must therefore assimilate this information with the worrisome evidence that off-pump surgery is associated with an increased incidence of incomplete revascularization, which is likely related to the subsequent increased need for repeat revascularization,” Dr. Rubens said.
Dr. Rubens had no disclosures.
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
Claims that off-pump coronary artery bypass (OPCAB) carries a lower risk of short-term stroke than conventional on-pump coronary artery bypass grafting (CABG) have been the subject of contradicting evidence, mostly because of the small size of the studies that showed a benefit, but European investigators published a meta-analysis involving more than 19,000 cases that showed what they called a “significant reduction” in the odds of a stroke.
“OPCAB was associated with a significant (28%) reduction in the odds of stroke compared with CABG,” said lead author Dr. Mariusz Kowalewski of Copernicus University in Bydgoszcz, Poland, and coauthors. The meta-analysis appeared in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:60-77).
The coauthors represent 10 different centers throughout Europe. Dr. Kowalewski and three other coauthors are also with the Systemic Investigation and Research on Interventions and Outcomes MEDICINE Research Network based in Düsseldorf, Germany.
Dr. Kowalewski and colleagues said this is the largest meta-analysis of randomized clinical trials comparing short-term outcomes of the two approaches to coronary bypass. “By its unique design, this analysis is the first report to investigate the causal relationship between underlying patient risk profile and the benefits of off-pump coronary revascularization,” they noted.
The meta-analysis looked at results of three primary outcomes: death within 30 days of the operation (2.25% overall, 2% in the OPCAB group and 2.04% in the CABG group); MI 30 days after surgery (4.49% overall, 4.3% for OPCAB and 4.67% for CABG); and 30-day occurrence of stroke (1.67% overall, 1.34% for OPCAB group and 2% for CABG).
In the meta-analysis, the researchers evaluated 100 studies for potential bias and conducted three separate analyses: one of all studies; and then separate analyses of studies of more than 50 and 100 subjects, respectively. Their goal was to check if small studies were driving the results.
Dr. Kowalewski and the study team acknowledged the conflicting science surrounding the benefits of the off-pump vs. conventional bypass. They pointed out that a host of randomized studies failed to show significant differences in stroke rates between the two approaches, and that conflicting European and American guidelines on the role of off-pump surgery to provide a better neurologic outcome do not help to clarify the relative risk.
“This apparent contradiction with the available registries’ data reporting a significantly decreased incidence of stroke with OPCAB may be explained by the fact that cerebral stroke represents a relatively rare entity after CABG, and thus even the largest randomized studies are underpowered to prove a possible advantage of one technique over the other,” Dr. Kowalewski and colleagues said.
They cited the CORONARY trial (N Engl J Med. 2012;366:1489-97), the largest trial to date, with 4,752 patients, which found no difference in the rate of stroke between the two groups. Three previous meta-analyses demonstrated 30%-50% reductions in stroke, but a systemic review called those results into question (Cochrane Database Syst. Rev. 2012;3:CD007224).
The “most important” finding of their study may be the confirmation of what large registries have reported: that OPCAB is safer and more effective than conventional bypass surgery in older and sicker patients. But they acknowledged that why this is the case “remains a subject of ongoing debate.”
Dr. Kowalewski and coresearchers acknowledged a number of limitations of their meta-analysis, namely that sensitivity analysis may have missed clinically important differences in patient results and broad patient inclusion criteria. However, the random-effects model they used accounted for study variations. “The findings on significant risk profile meta-regression are further corroborated in the analysis of MI and stroke,” they said.
Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Off-pump coronary artery bypass is associated with a significant reduction in the odds of stroke compared with conventional coronary artery bypass grafting and should be considered in high-risk patients.
Major finding: Off-pump coronary artery bypass was associated with a 28% reduction in the odds of patients having a cerebral stroke when compared with the conventional on-pump procedure.
Data source: Meta-analysis of 100 studies with a total of 19,192 patients.
Disclosures: Coauthor Dr. Eliano Pio Navarese disclosed honoraria from Eli Lilly. The other authors had no relationships to disclose.
Post-repair MR may be worse than thought
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In interpreting the findings of the Italian study and applying them in the clinic, one must consider the etiology of mitral valve regurgitation (MR) because that can determine the outcome of transcatheter mitral valve repair, Dr. Vincent Chan and Dr. Marc Ruel of the University of Ottawa Heart Institute said in their invited commentary (J Thorac Cardiovasc Surg 2016;151:97-8).
“In patients with coronary artery disease, it is well known that the presence of moderate chronic ischemic MR is associated with worse survival and more congestive heart failure compared to patients without MR,” Dr. Chan and Dr. Ruel said.
In a series his group studied, they noted that recurrent moderate MR was more common after MV repair than replacement; the survival rates between the two groups were similar (Ann Thorac Surg. 2011;92:1358-1365). That may be because late left ventricle (LV) function was similar between patients who had recurrent moderate MR and those that did not, but the Italian study did not clarify difference in late LV function between functional MR patients. “Perhaps differences in clinical outcome between patients with MR 2+ and MR ≤1+ relate to differences in ventricular function that portend mortality?” they asked.
They also called the researchers’ assertion that moderate MR impacts outcomes after repair “interesting.” They cited studies that linked effective worse outcomes to effective regurgitant orifice area (EROA) of 20-39 mm2, but that the complexity of echocardiographic measurement raises challenges in calculating EROA (Circulation. 2001;103:1759-64; N Engl J Med. 2005;352:875-83). “Also residual prolapse following MitraClip, as with any prolapse, may be brief and therefore instantaneous measures or regurgitation with pulse wave Doppler may be limited,” they said.
While percutaneous approaches to treat MR have “revolutionized” the care of these patients, the technology has its limitations, Dr. Chan and Dr. Ruel said. “Although many patients benefit from this therapy, the understanding of incomplete MR reduction with this technology continues to evolve.”
They had no disclosures.
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
In patients who undergo transcatheter mitral valve repair for mitral valve regurgitation (MR), residual mild (+2) regurgitation has been considered procedural success, but a team of Italian investigators has provided evidence that such a result may actually foretell far worse long-term outcomes than residual trace (≤1) MR.
The investigators from San Raffaele Scientific Institute in Milan reported their findings in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg 2016;151:88-96). They compared follow-up outcomes of 223 consecutive patients with residual MR 2+ and MR ≤1 after implantation of the MitraClip system (Abbott Vascular). The procedures were performed between October 2008 and December 2014.
“In this study we found a clear unfavorable impact on follow-up outcomes of acute residual 2+ MR after MitraClip repair when compared to residual ≤1+ MR,” lead author Dr. Nicola Buzzatti and colleagues said.
The study cited a scarcity of data on the long-term impact of residual mild MR. “This topic is therefore particularly of interest, especially when assessing the convenience to expand transcatheter mitral repair procedures to intermediate or low-risk patients,” Dr. Buzzatti and coauthors said.
The study group all had moderate or greater (≥3+) MR when they underwent mitral valve repair (MVR). The post-MVR study cohort excluded patients who had residual MR of 3 or greater, which was considered a procedural failure. Four patients died within 30 days, each from a different cause: multi-organ failure, lung rupture, pneumonia with heart failure, and sudden death. The overall 30-day death rate was 1.8%.
Among the remainder of patients, the average follow-up was 20.5 months, with some follow-up extending to 75 months. The overall survival was 74.4% at 24 months and 63% at 48 months.
The study calculated the cumulative incidence function, or the probability of failure, of cardiac death in patients with residual MR ≤1 at 7.1% at 24 months and 10.9% at 48 months, compared with 26.9% at 24 months and 35.3% at 48 months in those with MR 2+. The probability of failure of recurrence of moderate or severe MR with residual MR ≤1 was 5.6% at 24 months and 13.3% at 48 months, compared with 45.2% at both 24 and 48 months with residual MR 2+. “The difference between MR ≤1 and MR=2 was significant,” Dr. Buzzatti and colleagues said.
The researchers separately evaluated outcomes among those who had functional MR (FMR) and degenerative MR (DMR). In FMR, patients with MR 2+ had a higher risk profile at baseline because of a slightly higher rate of advanced heart disease; they typically had larger ventricles with larger mitral valves and greater pulmonary pressure than the ≤1 MR patients. “Notably, these features could have impaired the surgeon’s ability to achieve acute optimal MR reduction during the MitraClip procedure,” Dr. Buzzatti and coauthors said. “For sure, advanced left ventricle remodeling was a strong independent predictor of increased cardiac death.” The study authors could not draw a similar conclusion with DMR because only three patients in the group died of cardiac causes.
MR recurrence was “remarkably higher” in MR 2+ patients, compared with the MR ≤1 group with FMR and DMR, and MR 2+ developed in 21.4% of the FMR group within 30 days of the procedure. “This poor efficacy results in a population of patients who were supposed to have had a ‘procedural success’ is striking,” Dr. Buzzatti and coauthors noted.
Dr. Buzzatti and coauthor Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Coauthor Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Residual mild mitral valve regurgitation (MR) after implantation of the MitraClip device (Abbott Vascular) was associated with worse survival, symptom relief, and risk of moderate or severe MR than residual trace MR after implantation.
Major finding: Patients with residual mild MR after MitraClip implantation had a 45% probability of recurrence of moderate or severe MR within 4 years, more than three times that of those who had residual trace MR.
Data source: Population of 223 consecutive patients with acute residual trace or mild MR after MitraClip implantation between 2008 and 2014 at a single institution.
Disclosures: Dr. Nicola Buzzatti and Dr. Paolo Denti disclosed receiving consultant fees from Abbott Vascular. Dr. Fabio Barili disclosed receiving consultant fees from St. Jude Medical. The other authors had no relationships to disclose.
Bronchoscopic nitinol coils improve severe emphysema
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
The improvement in health-related quality of life scores in this study represents a mean response of approximately three times the established minimal clinically important difference. By comparison, trials of pharmacologic interventions rarely achieve even the minimal clinically important difference.
Despite the high cost-effectiveness ratio of more than $700,000 per QALY – when ratios of $50,000 to $100,000 per QALY are commonly deemed to be the maximal acceptable limit – clinicians shouldn’t hesitate to use this treatment if these findings are confirmed in larger trials. Bronchoscopically placed nitinol coils are largely palliative, but the response is meaningful and offers realistic hope to patients who have few other treatment choices.
Dr. Frank C. Sciurba, Dr. Divay Chandra, and Dr. Jessica Bon are all in the division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh. Dr. Sciurba reported receiving grants from PneumRX, maker of the coils used in this study, and PulmonX. Dr. Sciurba, Dr. Chandra, and Dr. Bon made these remarks in an editorial accompanying Dr. Deslee’s report (JAMA 2016;315:139-41).
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance and lung function in a preliminary study of patients with severe emphysema, which was published online Jan. 12 in JAMA.
The magnitude and severity of serious and nonserious adverse effects were far less than has been reported for more invasive lung volume reduction surgery in this patient population. However, the short-term financial costs of coil placement were substantial, said Dr. Gaetan Deslee of University of Reims (France) Hospital and his associates.
Nitinol coils are shape-memory devices delivered into subsegmental airways to reduce regional parenchymal volume, which increases expansion of adjacent nontargeted lung. This increases the nontargeted tissue’s elastic recoil and reestablishes small-airway tethering, which improves expiratory flow and reduces air trapping.
The investigators compared this procedure against usual care in 100 patients with severe emphysema who were treated and followed for 1 year at 10 university hospitals across France. Both groups underwent pretreatment pulmonary rehabilitation and received inhaled bronchodilators with or without inhaled corticosteroids and with or without supplemental oxygen at the discretion of their treating physicians. Then patients were randomly assigned – 50 to receive the coils and 50 to receive usual care.
The coils were inserted under general anesthesia, and approximately 10 coils were placed per targeted lobe. Most patients later underwent the procedure on the opposite side, so that 47 patients received bilateral and 3 received unilateral coils during 97 bronchoscopies. The mean procedure time was 54 minutes, and the treatment significantly decreased lung hyperinflation.
The primary efficacy endpoint, improvement in 6-minute walk test scores after 6 months, was evaluable for 44 patients in each study group. A total of 18 patients (36%) who underwent coil placement and 9 (18%) who received usual care improved their scores by at least 54 m, which was a significant difference, the investigators said (JAMA. 2016 Jan 12. doi: 10.1001/jama.2015.17821).
In addition, all secondary endpoints were significantly better after coil placement than after usual care at both 6 months and 12 months. This included forced expiratory volume in 1 second, forced vital capacity, residual volume, and residual volume/total lung capacity, scores on the Medical Research Council dyspnea scale, and scores on a measure of health-related quality of life.
A cost-benefit analysis at 1 year showed that the mean increase in expenditures was $47,908 per person in the coil group, compared with the usual-care group. The 1-year incremental cost-effectiveness ratio was $782,598 per quality-adjusted life year (QALY). Assuming that the quality of life gains would be maintained over 3 years and that the costs of follow-up care would be identically low in both study groups, this ratio would decrease to $270,000 per QALY at 3 years.
However, neither of these cost-effectiveness ratios would be considered economical enough to warrant adopting this technology in most countries, Dr. Deslee and his associates noted.
At least one serious adverse event developed in 52% of the coil group and in 38% of the usual-care group, and there were four deaths (8%) in the coil group and three deaths (6%) in the usual-care group. The most frequent adverse event was pneumonia, which resolved with medical care in all cases. “The mechanism involved in pneumonia may result from local airway irritation, subsegmental airway closure, tension-induced inflammation, or local ischemia rather than from an infectious mechanism,” the researchers said.
This study was limited in that coil placement was not compared with either a sham or control procedure, patients were not blinded to treatment assignment, the sample size was relatively small, and follow-up was short. Larger studies using more rigorous statistical methods are needed “to draw a definitive conclusion regarding the long-term efficacy of coil treatment,” they added.
FROM JAMA
Key clinical point: Bronchoscopically placed nitinol coils to reduce lung volume markedly improved quality of life and modestly improved walk distance in severe emphysema.
Major finding: 36% of patients who underwent coil placement achieved an improvement of at least 54 m in the 6-minute walk test, compared with only 18% who received usual care.
Data source: A preliminary randomized trial involving 100 patients treated at 10 university hospitals in France and followed for 1 year.
Disclosures: This study was supported by the French Ministry of Health. Dr. Deslee reported ties to PneumRx, maker of the coils tested in this study; his associates reported ties to PneumRx, Novatech, GlaxoSmithKline, Boehringer Ingelheim, Novartis, AstraZeneca, and Pulmonix.
No benefit in open massage over closed compressions in trauma cardiac arrest
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
SAN ANTONIO – Open-chest cardiac massage offers no benefit over closed-chest compressions in patients with traumatic cardiac arrest, according to a prospective observational study from the University of Maryland Shock Trauma Center in Baltimore.
The investigators compared 16 open-chest cardiac massage (OCCM) patients with 17 closed-chest compression (CCC) patients delivered directly to the level 1 trauma center in cardiac arrest. The open-massage group received closed compressions for a mean of 66 seconds before being converted to open massage for reasons that weren’t captured by the data.
End-tidal carbon dioxide (ETCO2) – the gold standard for determining the effectiveness of chest compressions and return of spontaneous circulation – was used as a surrogate for cardiac output and adequacy of resuscitation. Continuous high-resolution ETCO2 measurements were collected every 6 seconds in both groups.
When periods of OCCM were compared to equivalent periods of CCC, there were no differences in the initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
“Unless the patient has a thoracic injury that you need to get into the chest to fix, we didn’t see any benefit in opening the chest just to massage the heart. The data suggest that maybe we shouldn’t be so aggressive in doing open cardiac massage. There’s renewed interest in performing endovascular balloon occlusion techniques for the aorta to obtain hemorrhage control; if you do that and you do closed-chest compressions, it’s just as effective as opening up the chest and doing cardiac massage,” said investigator Dr. Matthew Bradley, a trauma surgeon at the Shock Trauma Center, at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
Most of the patients were men, and there was a higher percentage of penetrating trauma in the OCCM group (81% versus 47%; P = .04).
The results were the same, however, in subgroup analyses limited to blunt and penetrating trauma.
All of the open massage patients died, but there were a few survivors in the CCC group. Dr. Bradley didn’t think the closed versus open approach was the reason for the survival difference.
Resuscitative endovascular balloon occlusion of the aorta patients were excluded from the trial to prevent confounding.
The investigators have no relevant disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: There’s no benefit in opening the chest just to massage the heart.
Major finding: When periods of OCCM were compared to equivalent periods of CCC, there were no differences in initial, final, peak, or mean ETCO2 values, and there was no difference in return of spontaneous circulation (OCCM, 23.5% versus CCC, 38.9%; P = .53).
Data source: Prospective observational study in 33 patients
Disclosures: The investigators have no relevant disclosures.
3D imaging tracks causes of post-TAVR aortic regurgitation
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
This study is important because it reinforces the important role that 3D TEE can play in procedural planning for TAVR and in predicting which patients are more likely to suffer from post-TAVR AR. It is the first study that has highlighted the practical utilization of 3D TEE in this way.
Multislice computed tomography is the preferred imaging modality for TAVR planning in many centers. However, since the imaging resolution of both techniques is similar, and they both have software capable of generating multiplane reconstructions from 3D datasets, I believe that the skill and experience of the imaging expert analyzing the datasets are more important than the modality itself, and the results from this study could probably translate to MSCT.
Although the manufacturers of TAVR valves would have us believe that the issue of postimplant AR has largely been solved by newer valve design, it still remains an important issue and will continue to be so as the technique competes with surgical alternatives. Imaging will continue to play a pivotal role in procedure planning and guidance and, as has been demonstrated by Shibayama et al., 3D TEE can be extremely useful for anticipating and potentially avoiding post-TAVR AR.
Mark Monaghan, Ph.D., is the FESC director of noninvasive cardiology at King’s College Hospital Denmark Hill in London. These comments were taken from his editorial (JACC Cardiovasc Imaging 2016 Jan. 6).
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
Three-dimensional transesophageal echocardiography identified several significant predictors of aortic regurgitation after transcatheter aortic valve replacement, according to a study published online Jan. 5 in JACC Cardiovascular Imaging.
“This is the first study to demonstrate that large prosthetic expansion, elliptical prosthetic shape, and anti-anatomical position are 3D features associated with transvalvular AR,” said Dr. Kentaro Shibayama of Cedars-Sinai Heart Institute in Los Angeles, and his associates. The study also showed that paravalvular AR was inversely related to effective area oversizing, the investigators said (JACC Cardiovasc Imag. 2016 Jan. 6).
Post-TAVR AR continues to affect substantial numbers of patients, despite progress in prosthesis design. Past research has linked paravalvular AR to prosthetic undersizing, long-axis malpositioning, and aortic annular calcification, but the causes of transvalvular AR have not been adequately studied, the researchers said. Using intraprocedural 3D transesophageal echocardiography, they imaged the native annuluses and postoperative prosthetic valves of 201 patients with severe aortic stenosis who received the Edwards SAPIEN device. The investigators also used transthoracic echocardiography to separately grade post-TAVR transvalvular and paravalvular AR as none or trivial, mild, moderate, or severe according to the 2012 Valve Academic Research Consortium criteria (J Am Coll Cardiol. 2012;60:1438-54).Fully 44% of patients developed mild or moderate aortic regurgitation after TAVR, while the rest had no or trivial AR, the investigators said. About three-quarters of AR cases were mild, nearly 25% were moderate, and none were severe. Only 3% of patients had transvalvular AR only, 34% had paravalvular AR only, and 7% had both types of AR. Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape at the level of the prosthetic commissure (P less than .01), and malpositioning of the prosthetic commissures in relation to the native commissures (P less than .001), compared with patients without transvalvular AR.
Patients were more likely to have paravalvular AR if they had a lower percentage of effective area oversizing, defined as the prosthetic frame area divided by the area of the native aortic annulus (odds ratio, 0.97; 95% CI: 0.93-0.99, P less than .05). “A mismatch between a larger native aortic valve annulus area and a smaller deployed prosthesis found by intra-procedural 3D TEE may increase the risk of developing mild or greater paravalvular AR,” the researchers explained. Older age also was slightly but significantly linked with mild or moderate paravalvular AR(OR, 1.05; 95% CI, 1.01-1.09, P less than .05).
“Abnormalities related to transvalvular AR after TAVR found in this study may contribute to further deterioration of the prosthesis, warranting careful prospective studies to assess the long-term prognosis of these patients,” the investigators concluded. They cautioned that the number of patients with post-TAVR transvalvular AR was too small to carry out detailed analyses.
The researchers reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
FROM JACC CARDIOVASCULAR IMAGING
Key clinical point: Three-dimensional transesophageal echocardiography identified significant predictors of aortic regurgitation after transcatheter aortic valve replacement.
Major finding: Patients with post-TAVR transvalvular AR had significantly more prosthetic expansion (P less than .05), a more elliptical prosthetic shape (P less than .01), and malpositioning of the prosthetic commissures (P less than .001) compared with patients without transvalvular AR.
Data source: A 3D TEE study of 201 patients with severe aortic stenosis who underwent TAVR with the Edwards SAPIEN device.
Disclosures: The investigators reported no funding sources. Senior author Dr. Takahiro Shiota reported being a speaker for Philips Ultrasound, and three of the other seven coinvestigators reported financial relationships with Edwards, Medtronic, Abbott, Capricor, St. Jude Medical, Philips Ultrasound, and Venus Medtech.
Aortic valve replacement: Transcatheter soars past surgical
In Germany, almost all of the marked increase in the use of transcatheter aortic valve replacement (TAVR) since the procedure’s introduction in 2007 occurred in patients unsuited to a surgical approach because of their advanced age or elevated risk, according to an analysis published online Dec. 17 in the New England Journal of Medicine.
The surgical aortic valve replacement (SAVR) is still the standard of care, but many have questioned how the relatively new transcatheter approach has affected clinical practice overall, said Dr. Jochen Reinöhl of the Heart Center, University of Freiburg (Germany) and his associates.
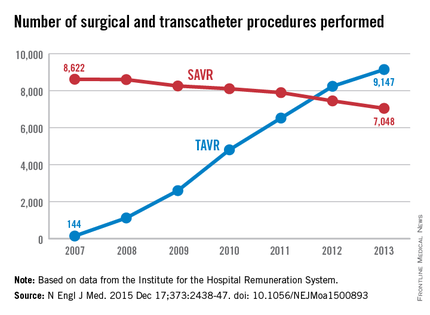
To assess the evolution of treatment since TAVR was introduced, the investigators analyzed data from the Institute for the Hospital Remuneration System, which tracks all patient data regarding diagnoses, comorbidities, and procedures throughout the country. They focused on all 88,573 admissions for isolated surgical aortic valve replacements (55,992 procedures) and for isolated TAVR (32,581 procedures) performed in Germany during 2007-2013.
The number of TAVR procedures increased markedly over time, from 144 to 9,147 per year, while the number of SAVRs declined only slightly, from 8,622 to 7,048 per year. Patients aged 80 years and older accounted for almost all of the dramatic increase in transcatheter procedures, the investigators said (N Engl J Med. 2015 Dec 17;373:2438-47 [doi:10.1056/NEJMoa1500893]).
Overall in-hospital mortality was significantly higher with TAVR (6.5%) than with SAVR (2.8%), for an odds ratio of 2.41. This likely reflects the significantly greater risk of patients selected for TAVR, compared with those undergoing surgery, they said.
Mortality decreased over time in both patient groups, from 3.8% to 2.2% with surgery and from 13.2% to 5.4% with TAVR. In the case of TAVR, this decline is likely from a “learning curve” effect among clinicians, improvements in patient care, and advances in treatment devices. In the case of surgery, the mortality decline is probably due in part to the shift of high-risk patients from SAVR to the transcatheter approach, Dr. Reinöhl and his associates said.
Similarly, complications were significantly more common with TAVR. The need for permanent pacemaker implantation was the most frequently reported complication of TAVR, occurring in 17.7% of the transcatheter group but only 4.0% of the surgical group. Stroke rates (2.5% vs. 1.8%) and rates of acute kidney injury (5.5% vs. 3.0%) followed a similar pattern. In contrast, bleeding complications were more frequent with surgery (14.0% vs. 8.2%).
In Germany, almost all of the marked increase in the use of transcatheter aortic valve replacement (TAVR) since the procedure’s introduction in 2007 occurred in patients unsuited to a surgical approach because of their advanced age or elevated risk, according to an analysis published online Dec. 17 in the New England Journal of Medicine.
The surgical aortic valve replacement (SAVR) is still the standard of care, but many have questioned how the relatively new transcatheter approach has affected clinical practice overall, said Dr. Jochen Reinöhl of the Heart Center, University of Freiburg (Germany) and his associates.
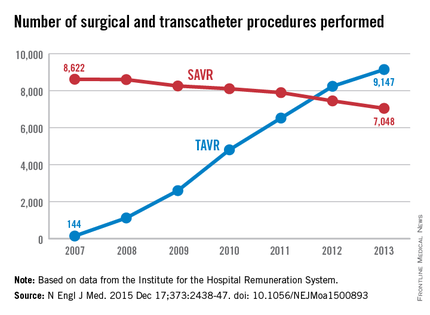
To assess the evolution of treatment since TAVR was introduced, the investigators analyzed data from the Institute for the Hospital Remuneration System, which tracks all patient data regarding diagnoses, comorbidities, and procedures throughout the country. They focused on all 88,573 admissions for isolated surgical aortic valve replacements (55,992 procedures) and for isolated TAVR (32,581 procedures) performed in Germany during 2007-2013.
The number of TAVR procedures increased markedly over time, from 144 to 9,147 per year, while the number of SAVRs declined only slightly, from 8,622 to 7,048 per year. Patients aged 80 years and older accounted for almost all of the dramatic increase in transcatheter procedures, the investigators said (N Engl J Med. 2015 Dec 17;373:2438-47 [doi:10.1056/NEJMoa1500893]).
Overall in-hospital mortality was significantly higher with TAVR (6.5%) than with SAVR (2.8%), for an odds ratio of 2.41. This likely reflects the significantly greater risk of patients selected for TAVR, compared with those undergoing surgery, they said.
Mortality decreased over time in both patient groups, from 3.8% to 2.2% with surgery and from 13.2% to 5.4% with TAVR. In the case of TAVR, this decline is likely from a “learning curve” effect among clinicians, improvements in patient care, and advances in treatment devices. In the case of surgery, the mortality decline is probably due in part to the shift of high-risk patients from SAVR to the transcatheter approach, Dr. Reinöhl and his associates said.
Similarly, complications were significantly more common with TAVR. The need for permanent pacemaker implantation was the most frequently reported complication of TAVR, occurring in 17.7% of the transcatheter group but only 4.0% of the surgical group. Stroke rates (2.5% vs. 1.8%) and rates of acute kidney injury (5.5% vs. 3.0%) followed a similar pattern. In contrast, bleeding complications were more frequent with surgery (14.0% vs. 8.2%).
In Germany, almost all of the marked increase in the use of transcatheter aortic valve replacement (TAVR) since the procedure’s introduction in 2007 occurred in patients unsuited to a surgical approach because of their advanced age or elevated risk, according to an analysis published online Dec. 17 in the New England Journal of Medicine.
The surgical aortic valve replacement (SAVR) is still the standard of care, but many have questioned how the relatively new transcatheter approach has affected clinical practice overall, said Dr. Jochen Reinöhl of the Heart Center, University of Freiburg (Germany) and his associates.
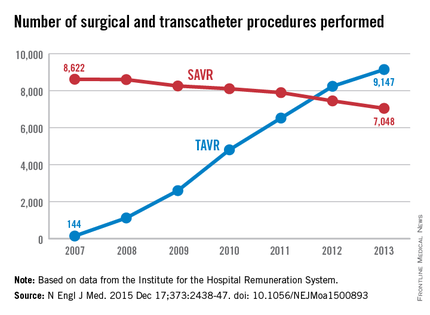
To assess the evolution of treatment since TAVR was introduced, the investigators analyzed data from the Institute for the Hospital Remuneration System, which tracks all patient data regarding diagnoses, comorbidities, and procedures throughout the country. They focused on all 88,573 admissions for isolated surgical aortic valve replacements (55,992 procedures) and for isolated TAVR (32,581 procedures) performed in Germany during 2007-2013.
The number of TAVR procedures increased markedly over time, from 144 to 9,147 per year, while the number of SAVRs declined only slightly, from 8,622 to 7,048 per year. Patients aged 80 years and older accounted for almost all of the dramatic increase in transcatheter procedures, the investigators said (N Engl J Med. 2015 Dec 17;373:2438-47 [doi:10.1056/NEJMoa1500893]).
Overall in-hospital mortality was significantly higher with TAVR (6.5%) than with SAVR (2.8%), for an odds ratio of 2.41. This likely reflects the significantly greater risk of patients selected for TAVR, compared with those undergoing surgery, they said.
Mortality decreased over time in both patient groups, from 3.8% to 2.2% with surgery and from 13.2% to 5.4% with TAVR. In the case of TAVR, this decline is likely from a “learning curve” effect among clinicians, improvements in patient care, and advances in treatment devices. In the case of surgery, the mortality decline is probably due in part to the shift of high-risk patients from SAVR to the transcatheter approach, Dr. Reinöhl and his associates said.
Similarly, complications were significantly more common with TAVR. The need for permanent pacemaker implantation was the most frequently reported complication of TAVR, occurring in 17.7% of the transcatheter group but only 4.0% of the surgical group. Stroke rates (2.5% vs. 1.8%) and rates of acute kidney injury (5.5% vs. 3.0%) followed a similar pattern. In contrast, bleeding complications were more frequent with surgery (14.0% vs. 8.2%).
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: In Germany, almost all of the marked increase in the use of transcatheter aortic valve replacement occurred among patients unsuited for a surgical approach.
Major finding: The number of TAVR procedures increased markedly over time, from 144 to 9,147 per year, while the number of surgical procedures declined only slightly, from 8,622 to 7,048 per year.
Data source: A retrospective analysis of all 88,573 surgical and TAVR performed in Germany in 2007-2013.
Disclosures: This study was supported by the Heart Center at Freiburg University. Dr. Reinöhl and one of his associates reported receiving personal fees from Edwards Lifesciences and Direct Flow Medical.
Six-year Norwood-RVPA results in matched patients outperformed BT-shunt
Concerns with delayed right ventricle dysfunction have offset the early survival advantages after Norwood procedure with right ventricle to pulmonary artery conduit (NW-RVPA) over the Norwood with Blalock-Taussig shunt (NW-BT) in newborns with left ventricular outflow tract obstruction, but a recent report provides evidence that RV function between the two procedures is comparable for up to six years.
Reporting in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 Dec;150:1440–52), investigators for the Congenital Heart Surgeons’ Society (CHSS) trial found that NW-RVPA has better overall six-year survival and superior right ventricle function in the short term after surgery than NW-BT. The study involved 454 newborns with critical left ventricular outflow tract obstruction (LVOTO) in the CHSS database who had Norwood stage-1 from 2005 to 2014. Propensity matching paired 169 NW-RVPA patients with the same number of NW-BT patients for comparison. CHSS along with the Hospital for Sick Children in Toronto provided funding for the study.
“For neonates with critical LVOTO and similar baseline characteristics undergoing a Norwood stage-1 operation, the six-year overall survival and transplant-free survival were significantly better after NW-RVPA vs. NW-BT,” said Dr. Travis J. Wilder and his colleagues from the Hospital for Sick Children in Toronto.
Key questions the study sought to answer involved the clinical implications of the small variations in RV function between the two procedures, as well as the association between Norwood procedures and tricuspid valve regurgitation (TR) and overall survival.
Overall six-year survival was 70% for the NW-RVPA group vs. 55% for the NW-BT group. Right ventricle dysfunction rates three months after the procedure were lower for the NW-RVPA group, 6% vs. 16%, but rates of late RV dysfunction were less than 5% for both groups. Likewise, rates of moderate or greater TR at two years were lower in the NW-RVPA group: 11% vs. 16%.
Rates of Fontan operation after six years were higher among the NW-RVPA group (54% vs. 49%), as were transplantation rates (6% vs. 2%). Overall, 2% converted to a biventricular repair, but only after NW-RVPA; and seven patients who had NW-RVPA underwent a tricuspid valve repair, compared with four in the NW-BT group.
“For all survivors not undergoing transplantation or biventricular repair, the prevalence of late moderate or greater RV dysfunction and TR were similar between NW-BT and NW-RVPA at six years, without evidence of increased RV dysfunction for patients who underwent NW-RVPA,” Dr. Wilder and his colleagues said.
Consistent with previous studies, the CHSS study showed an early risk of death after a Norwood stage-1 operation, which may be due to a greater prevalence of significant RV dysfunction as the operation transitions from stage 1 to stage 2, Dr. Wilder and his coauthors said. “Although causation between these two time-related events cannot directly be made, it suggests that poor RV function contributes to early hazard for death,” they said.
The authors acknowledge a number of limitations with their study: the variation in the quality of echocardiogram reports from the multiple institutions involved, the inability of propensity matching to account for unmeasured factors and the influence of center and surgeon volume among participating sites. They also said that the ventriculotomy the NW-RVPA involves can lead to late aneurysm, arrhythmias, and ventricular failure. The adverse effects of ventriculotomy on long-term RV function “may not become apparent for years,” Dr. Wilder and his coauthors said.
Dr. Wilder presented a report of the original results at the 2015 American Association for Thoracic Surgery Annual meeting.
The authors had no relationships to disclose.
“It is time to have the courage to confess that we need a more overarching quality improvement strategy,” Dr. James S. Tweddell of the Children’s Hospital of Wisconsin said of the results of the Congenital Heart Surgeons’ Society (CHSS) study in his invited commentary (J Thorac Cardiovasc Surg. 2015 Dec;150:1453–4).
Dr. Tweddell said the findings of the CHSS study and the earlier Single Ventricle Reconstruction (SVR) trial (N Engl J Med. 2010;362:1980-1992) are similar in terms of transplant-free survival in newborns. And while the dates of the studies’ enrollments overlap – 2005-2008 for SVR and 2005-2014 for CHSS – the more recent findings of the CHSS study would imply an advantage in terms of survival and right ventricle function. Nonetheless, the survival rates are similar, he said. “Only about 60% of patients remain alive.”
 |
Dr. James S. Tweddell |
Dr. Tweddell pointed out the CHSS study is not a randomized, controlled trial, “and the shortcomings of the prospective observational study are well known.”
In calling for a “more overarching” quality improvement measure, Dr. Tweddell said that many programs use Norwood performance as a benchmark for outcomes. He proposed collaboration among high and low performing centers, imitating the adult cardiology model. He also suggested consolidation of programs performing the Norwood procedure to eliminate low-volume centers and develop centers of excellence. “The outcome of the Norwood procedure is dependent on both program and surgeon volume,” Dr. Tweddell said.
The CHSS study “is important and identifies a potentially durable benefit to the NW-RVPA,” Dr. Tweddell said, “but perhaps now is the time to focus on strategies between programs rather than solely within programs.”
“It is time to have the courage to confess that we need a more overarching quality improvement strategy,” Dr. James S. Tweddell of the Children’s Hospital of Wisconsin said of the results of the Congenital Heart Surgeons’ Society (CHSS) study in his invited commentary (J Thorac Cardiovasc Surg. 2015 Dec;150:1453–4).
Dr. Tweddell said the findings of the CHSS study and the earlier Single Ventricle Reconstruction (SVR) trial (N Engl J Med. 2010;362:1980-1992) are similar in terms of transplant-free survival in newborns. And while the dates of the studies’ enrollments overlap – 2005-2008 for SVR and 2005-2014 for CHSS – the more recent findings of the CHSS study would imply an advantage in terms of survival and right ventricle function. Nonetheless, the survival rates are similar, he said. “Only about 60% of patients remain alive.”
 |
Dr. James S. Tweddell |
Dr. Tweddell pointed out the CHSS study is not a randomized, controlled trial, “and the shortcomings of the prospective observational study are well known.”
In calling for a “more overarching” quality improvement measure, Dr. Tweddell said that many programs use Norwood performance as a benchmark for outcomes. He proposed collaboration among high and low performing centers, imitating the adult cardiology model. He also suggested consolidation of programs performing the Norwood procedure to eliminate low-volume centers and develop centers of excellence. “The outcome of the Norwood procedure is dependent on both program and surgeon volume,” Dr. Tweddell said.
The CHSS study “is important and identifies a potentially durable benefit to the NW-RVPA,” Dr. Tweddell said, “but perhaps now is the time to focus on strategies between programs rather than solely within programs.”
“It is time to have the courage to confess that we need a more overarching quality improvement strategy,” Dr. James S. Tweddell of the Children’s Hospital of Wisconsin said of the results of the Congenital Heart Surgeons’ Society (CHSS) study in his invited commentary (J Thorac Cardiovasc Surg. 2015 Dec;150:1453–4).
Dr. Tweddell said the findings of the CHSS study and the earlier Single Ventricle Reconstruction (SVR) trial (N Engl J Med. 2010;362:1980-1992) are similar in terms of transplant-free survival in newborns. And while the dates of the studies’ enrollments overlap – 2005-2008 for SVR and 2005-2014 for CHSS – the more recent findings of the CHSS study would imply an advantage in terms of survival and right ventricle function. Nonetheless, the survival rates are similar, he said. “Only about 60% of patients remain alive.”
 |
Dr. James S. Tweddell |
Dr. Tweddell pointed out the CHSS study is not a randomized, controlled trial, “and the shortcomings of the prospective observational study are well known.”
In calling for a “more overarching” quality improvement measure, Dr. Tweddell said that many programs use Norwood performance as a benchmark for outcomes. He proposed collaboration among high and low performing centers, imitating the adult cardiology model. He also suggested consolidation of programs performing the Norwood procedure to eliminate low-volume centers and develop centers of excellence. “The outcome of the Norwood procedure is dependent on both program and surgeon volume,” Dr. Tweddell said.
The CHSS study “is important and identifies a potentially durable benefit to the NW-RVPA,” Dr. Tweddell said, “but perhaps now is the time to focus on strategies between programs rather than solely within programs.”
Concerns with delayed right ventricle dysfunction have offset the early survival advantages after Norwood procedure with right ventricle to pulmonary artery conduit (NW-RVPA) over the Norwood with Blalock-Taussig shunt (NW-BT) in newborns with left ventricular outflow tract obstruction, but a recent report provides evidence that RV function between the two procedures is comparable for up to six years.
Reporting in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 Dec;150:1440–52), investigators for the Congenital Heart Surgeons’ Society (CHSS) trial found that NW-RVPA has better overall six-year survival and superior right ventricle function in the short term after surgery than NW-BT. The study involved 454 newborns with critical left ventricular outflow tract obstruction (LVOTO) in the CHSS database who had Norwood stage-1 from 2005 to 2014. Propensity matching paired 169 NW-RVPA patients with the same number of NW-BT patients for comparison. CHSS along with the Hospital for Sick Children in Toronto provided funding for the study.
“For neonates with critical LVOTO and similar baseline characteristics undergoing a Norwood stage-1 operation, the six-year overall survival and transplant-free survival were significantly better after NW-RVPA vs. NW-BT,” said Dr. Travis J. Wilder and his colleagues from the Hospital for Sick Children in Toronto.
Key questions the study sought to answer involved the clinical implications of the small variations in RV function between the two procedures, as well as the association between Norwood procedures and tricuspid valve regurgitation (TR) and overall survival.
Overall six-year survival was 70% for the NW-RVPA group vs. 55% for the NW-BT group. Right ventricle dysfunction rates three months after the procedure were lower for the NW-RVPA group, 6% vs. 16%, but rates of late RV dysfunction were less than 5% for both groups. Likewise, rates of moderate or greater TR at two years were lower in the NW-RVPA group: 11% vs. 16%.
Rates of Fontan operation after six years were higher among the NW-RVPA group (54% vs. 49%), as were transplantation rates (6% vs. 2%). Overall, 2% converted to a biventricular repair, but only after NW-RVPA; and seven patients who had NW-RVPA underwent a tricuspid valve repair, compared with four in the NW-BT group.
“For all survivors not undergoing transplantation or biventricular repair, the prevalence of late moderate or greater RV dysfunction and TR were similar between NW-BT and NW-RVPA at six years, without evidence of increased RV dysfunction for patients who underwent NW-RVPA,” Dr. Wilder and his colleagues said.
Consistent with previous studies, the CHSS study showed an early risk of death after a Norwood stage-1 operation, which may be due to a greater prevalence of significant RV dysfunction as the operation transitions from stage 1 to stage 2, Dr. Wilder and his coauthors said. “Although causation between these two time-related events cannot directly be made, it suggests that poor RV function contributes to early hazard for death,” they said.
The authors acknowledge a number of limitations with their study: the variation in the quality of echocardiogram reports from the multiple institutions involved, the inability of propensity matching to account for unmeasured factors and the influence of center and surgeon volume among participating sites. They also said that the ventriculotomy the NW-RVPA involves can lead to late aneurysm, arrhythmias, and ventricular failure. The adverse effects of ventriculotomy on long-term RV function “may not become apparent for years,” Dr. Wilder and his coauthors said.
Dr. Wilder presented a report of the original results at the 2015 American Association for Thoracic Surgery Annual meeting.
The authors had no relationships to disclose.
Concerns with delayed right ventricle dysfunction have offset the early survival advantages after Norwood procedure with right ventricle to pulmonary artery conduit (NW-RVPA) over the Norwood with Blalock-Taussig shunt (NW-BT) in newborns with left ventricular outflow tract obstruction, but a recent report provides evidence that RV function between the two procedures is comparable for up to six years.
Reporting in the January issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 Dec;150:1440–52), investigators for the Congenital Heart Surgeons’ Society (CHSS) trial found that NW-RVPA has better overall six-year survival and superior right ventricle function in the short term after surgery than NW-BT. The study involved 454 newborns with critical left ventricular outflow tract obstruction (LVOTO) in the CHSS database who had Norwood stage-1 from 2005 to 2014. Propensity matching paired 169 NW-RVPA patients with the same number of NW-BT patients for comparison. CHSS along with the Hospital for Sick Children in Toronto provided funding for the study.
“For neonates with critical LVOTO and similar baseline characteristics undergoing a Norwood stage-1 operation, the six-year overall survival and transplant-free survival were significantly better after NW-RVPA vs. NW-BT,” said Dr. Travis J. Wilder and his colleagues from the Hospital for Sick Children in Toronto.
Key questions the study sought to answer involved the clinical implications of the small variations in RV function between the two procedures, as well as the association between Norwood procedures and tricuspid valve regurgitation (TR) and overall survival.
Overall six-year survival was 70% for the NW-RVPA group vs. 55% for the NW-BT group. Right ventricle dysfunction rates three months after the procedure were lower for the NW-RVPA group, 6% vs. 16%, but rates of late RV dysfunction were less than 5% for both groups. Likewise, rates of moderate or greater TR at two years were lower in the NW-RVPA group: 11% vs. 16%.
Rates of Fontan operation after six years were higher among the NW-RVPA group (54% vs. 49%), as were transplantation rates (6% vs. 2%). Overall, 2% converted to a biventricular repair, but only after NW-RVPA; and seven patients who had NW-RVPA underwent a tricuspid valve repair, compared with four in the NW-BT group.
“For all survivors not undergoing transplantation or biventricular repair, the prevalence of late moderate or greater RV dysfunction and TR were similar between NW-BT and NW-RVPA at six years, without evidence of increased RV dysfunction for patients who underwent NW-RVPA,” Dr. Wilder and his colleagues said.
Consistent with previous studies, the CHSS study showed an early risk of death after a Norwood stage-1 operation, which may be due to a greater prevalence of significant RV dysfunction as the operation transitions from stage 1 to stage 2, Dr. Wilder and his coauthors said. “Although causation between these two time-related events cannot directly be made, it suggests that poor RV function contributes to early hazard for death,” they said.
The authors acknowledge a number of limitations with their study: the variation in the quality of echocardiogram reports from the multiple institutions involved, the inability of propensity matching to account for unmeasured factors and the influence of center and surgeon volume among participating sites. They also said that the ventriculotomy the NW-RVPA involves can lead to late aneurysm, arrhythmias, and ventricular failure. The adverse effects of ventriculotomy on long-term RV function “may not become apparent for years,” Dr. Wilder and his coauthors said.
Dr. Wilder presented a report of the original results at the 2015 American Association for Thoracic Surgery Annual meeting.
The authors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOTHORACIC SURGERY
Key clinical point: For newborns with critical left ventricular outflow tract obstruction (LVOTO) undergoing Norwood stage-1 procedures, Norwood with right ventricle to pulmonary artery conduit (NW-RVPA) resulted in better survival and less short-term right-ventricle dysfunction than matched patients who had the Norwood procedure with Blalock-Taussig shunt (NW-BT).
Major finding: Overall six-year survival was 70% for the NW-RVPA group vs. 55% for the NW-BT group, and RV dysfunction rates three months after the procedure were 6% for NW-RVPA vs. 16% for NW-BT.
Data source: Prospective group of 454 newborns with LVOTO in the Congenital Heart Surgeons’ Society database.
Disclosures: The Congenital Heart Surgeons’ Society and Hospital for Sick Children, Toronto, provided funding for the study. The authors had no relationships to disclose.








