User login
ABIM sued over maintenance of certification
Also today, drug test results should not dictate treatment, duodenoscopes contain more bacteria than expected, and weight-loss medications may have a role following bariatric surgery.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, drug test results should not dictate treatment, duodenoscopes contain more bacteria than expected, and weight-loss medications may have a role following bariatric surgery.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, drug test results should not dictate treatment, duodenoscopes contain more bacteria than expected, and weight-loss medications may have a role following bariatric surgery.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Carol Bernstein Part II
Parental leave for residents
Also today, exercise is important for patients with sickle cell, COPD patients are experiencing a risk in non-TB mycobacteria infections, and how to be an influencer on social media.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, exercise is important for patients with sickle cell, COPD patients are experiencing a risk in non-TB mycobacteria infections, and how to be an influencer on social media.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, exercise is important for patients with sickle cell, COPD patients are experiencing a risk in non-TB mycobacteria infections, and how to be an influencer on social media.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Roberto Lewis-Fernandez: Cultural Assessments
More from Dr. Lewis-Fernandez, Curbside Consult: Chinese American man with high risk of psychosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
More from Dr. Lewis-Fernandez, Curbside Consult: Chinese American man with high risk of psychosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
More from Dr. Lewis-Fernandez, Curbside Consult: Chinese American man with high risk of psychosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
AHA reports statins are safe
Also today, acute stroke thrombolysis worked safely despite GI bleed or malignancy, legal advice on what to do if a patient sues you, and the link between childhood asthma and obesity.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, acute stroke thrombolysis worked safely despite GI bleed or malignancy, legal advice on what to do if a patient sues you, and the link between childhood asthma and obesity.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, acute stroke thrombolysis worked safely despite GI bleed or malignancy, legal advice on what to do if a patient sues you, and the link between childhood asthma and obesity.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Carol Bernstein: Burnout or depression?
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
Dr. Bernstein is a professor at NYU Langone in New York City and has been a guest on the MDedge Psychcast.
Apple Podcasts
Google Podcasts
Craig Getting, Luis Aguilar-Montalva: Part I
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
Thomas Jefferson University in Philadelphia partnered with the Lantern Theater Company to offer a class that teaches staging, acting, and playwriting. The class is designed specifically for med students, current residents, attending physicians, and any other medical professionals. The class eliminates hierarchy, encourages artistic exploration, and can lead to increased empathy when dealing with patients and their families. Nick, Luis, and Craig recognize the similarities between medicine and art but also highlight what we can learn from different passions.
Apple Podcasts
Google Podcasts
REDUCE-IT: Fish-derived agent cut CV events 25%
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
REPORTING FROM AMERICAN HEART ASSOCIATION SCIENTIFIC SESSIONS 2018
Key Clinical point: .
Major finding: Cardiovascular death or nonfatal cardiovascular event occurred in 17.7% of treated patients vs. 22% of controls.
Study details: Multicenter, randomized, double-blind, placebo-controlled clinical trial of 8,179 patients with established cardiovascular disease or diabetes and other risk factors.
Disclosures: Dr. Bhatt disclosed having a significant research relationship with Amarin Corp., which funded the trial.
Source: N Engl J Med. 2018; doi: 10.1056/NEJMoa181279.
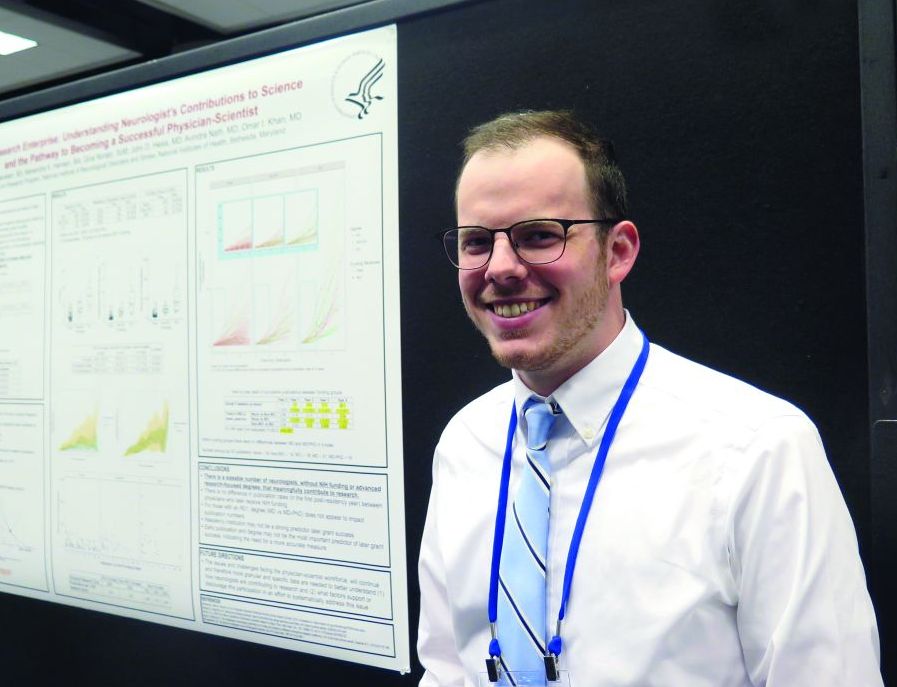
Think research is just for MD-PhDs? Think again
ATLANTA – You don’t have to hold an advanced research degree or secure National Institutes of Health funding in order to contribute to neurology research in a meaningful way.
That’s a key finding from an analysis of 244 neurology residency program graduates.
“Science as a whole is trying to get better,” lead study author Wyatt P. Bensken said in an interview at the annual meeting of the American Neurological Association. “If your goal is to be a clinician, that doesn’t mean you can’t contribute to research. If your goal is to see patients for 80% of your time, that doesn’t mean that other 20% – which is research – disqualifies you from being a physician-scientist.”
In an effort to better understand the current status of the physician-scientist workforce in the neurology field, Mr. Bensken and his colleagues identified neurology residency graduates from the top National Institute of Neurological Disorders and Stroke–funded institutions for 2003, 2004, and 2005 via program websites. Data points collected for each individual included complete NIH and other government funding history, number of post-residency publications by year, and the Hirsch-index, or h-index, which measures an individual’s research publication impact. The researchers conducted data analysis via visualization and ANOVA testing.
Mr. Bensken, a research collaborator with the NINDS who is also a PhD student at Case Western Reserve University in Cleveland, reported that 186 of the 244 neurology residency program graduates had demonstrated interest in research based on their publication activity findings. Specifically, 26 had obtained an R01 grant, 31 were non–R01-funded, and 129 were nonfunded. Of the 26 individuals who had obtained an R01, 15 (58%) were MD-PhDs, from a total of 50 MD‐PhDs in the cohort. In addition, 43 individuals had a K‐series award, with 18 going on to receive R01 funding.
Of those with non‐R01 funding or no funding, a number of individuals performed as well as R01‐funded individuals with respect to post‐residency publication rate and impact factor. However, the publication rate and impact factor were highest in the R01-funded group (6.4 and 28.6, respectively), followed by those in the non‐R01 group (3.0 and 15.9), and those in the nonfunded group (1.2 and 8.0). Further, the publications‐per‐research hour for the three groups revealed varied productivity levels. Specifically, those in the R01-funded group with 80% protected research time produced 3.2 publications per 1,000 research hours, while those in the non–R01-funded group with 40% protected research time produced 3.0 publications per 1,000 research hours. Meanwhile, those without R01 funding overall (those with non-RO1 funding and those without funding) performed at a higher per-hour rate, when estimating 10% or 15% protected time (4.9 and 3.3 publications per 1,000 research hours, respectively).
“I think this reinforces the notion that there are far more neurologists out there who aren’t trained as MD-PhDs, who aren’t receiving R01s, but who are making meaningful contributions,” Mr. Bensken said. “Our ultimate goal is to maximize the potential of everybody in this environment to contribute. If everyone was able to contribute what they could, I think research would be far more successful and far more impactful than it is now.”
The study was funded by the NINDS. Mr. Bensken reported having no financial disclosures.
SOURCE: Bensken WP et al. Ann Neurol. 2018;84[S22]:S72-3, Abstract S176.
ATLANTA – You don’t have to hold an advanced research degree or secure National Institutes of Health funding in order to contribute to neurology research in a meaningful way.
That’s a key finding from an analysis of 244 neurology residency program graduates.
“Science as a whole is trying to get better,” lead study author Wyatt P. Bensken said in an interview at the annual meeting of the American Neurological Association. “If your goal is to be a clinician, that doesn’t mean you can’t contribute to research. If your goal is to see patients for 80% of your time, that doesn’t mean that other 20% – which is research – disqualifies you from being a physician-scientist.”
In an effort to better understand the current status of the physician-scientist workforce in the neurology field, Mr. Bensken and his colleagues identified neurology residency graduates from the top National Institute of Neurological Disorders and Stroke–funded institutions for 2003, 2004, and 2005 via program websites. Data points collected for each individual included complete NIH and other government funding history, number of post-residency publications by year, and the Hirsch-index, or h-index, which measures an individual’s research publication impact. The researchers conducted data analysis via visualization and ANOVA testing.
Mr. Bensken, a research collaborator with the NINDS who is also a PhD student at Case Western Reserve University in Cleveland, reported that 186 of the 244 neurology residency program graduates had demonstrated interest in research based on their publication activity findings. Specifically, 26 had obtained an R01 grant, 31 were non–R01-funded, and 129 were nonfunded. Of the 26 individuals who had obtained an R01, 15 (58%) were MD-PhDs, from a total of 50 MD‐PhDs in the cohort. In addition, 43 individuals had a K‐series award, with 18 going on to receive R01 funding.
Of those with non‐R01 funding or no funding, a number of individuals performed as well as R01‐funded individuals with respect to post‐residency publication rate and impact factor. However, the publication rate and impact factor were highest in the R01-funded group (6.4 and 28.6, respectively), followed by those in the non‐R01 group (3.0 and 15.9), and those in the nonfunded group (1.2 and 8.0). Further, the publications‐per‐research hour for the three groups revealed varied productivity levels. Specifically, those in the R01-funded group with 80% protected research time produced 3.2 publications per 1,000 research hours, while those in the non–R01-funded group with 40% protected research time produced 3.0 publications per 1,000 research hours. Meanwhile, those without R01 funding overall (those with non-RO1 funding and those without funding) performed at a higher per-hour rate, when estimating 10% or 15% protected time (4.9 and 3.3 publications per 1,000 research hours, respectively).
“I think this reinforces the notion that there are far more neurologists out there who aren’t trained as MD-PhDs, who aren’t receiving R01s, but who are making meaningful contributions,” Mr. Bensken said. “Our ultimate goal is to maximize the potential of everybody in this environment to contribute. If everyone was able to contribute what they could, I think research would be far more successful and far more impactful than it is now.”
The study was funded by the NINDS. Mr. Bensken reported having no financial disclosures.
SOURCE: Bensken WP et al. Ann Neurol. 2018;84[S22]:S72-3, Abstract S176.
ATLANTA – You don’t have to hold an advanced research degree or secure National Institutes of Health funding in order to contribute to neurology research in a meaningful way.
That’s a key finding from an analysis of 244 neurology residency program graduates.
“Science as a whole is trying to get better,” lead study author Wyatt P. Bensken said in an interview at the annual meeting of the American Neurological Association. “If your goal is to be a clinician, that doesn’t mean you can’t contribute to research. If your goal is to see patients for 80% of your time, that doesn’t mean that other 20% – which is research – disqualifies you from being a physician-scientist.”
In an effort to better understand the current status of the physician-scientist workforce in the neurology field, Mr. Bensken and his colleagues identified neurology residency graduates from the top National Institute of Neurological Disorders and Stroke–funded institutions for 2003, 2004, and 2005 via program websites. Data points collected for each individual included complete NIH and other government funding history, number of post-residency publications by year, and the Hirsch-index, or h-index, which measures an individual’s research publication impact. The researchers conducted data analysis via visualization and ANOVA testing.
Mr. Bensken, a research collaborator with the NINDS who is also a PhD student at Case Western Reserve University in Cleveland, reported that 186 of the 244 neurology residency program graduates had demonstrated interest in research based on their publication activity findings. Specifically, 26 had obtained an R01 grant, 31 were non–R01-funded, and 129 were nonfunded. Of the 26 individuals who had obtained an R01, 15 (58%) were MD-PhDs, from a total of 50 MD‐PhDs in the cohort. In addition, 43 individuals had a K‐series award, with 18 going on to receive R01 funding.
Of those with non‐R01 funding or no funding, a number of individuals performed as well as R01‐funded individuals with respect to post‐residency publication rate and impact factor. However, the publication rate and impact factor were highest in the R01-funded group (6.4 and 28.6, respectively), followed by those in the non‐R01 group (3.0 and 15.9), and those in the nonfunded group (1.2 and 8.0). Further, the publications‐per‐research hour for the three groups revealed varied productivity levels. Specifically, those in the R01-funded group with 80% protected research time produced 3.2 publications per 1,000 research hours, while those in the non–R01-funded group with 40% protected research time produced 3.0 publications per 1,000 research hours. Meanwhile, those without R01 funding overall (those with non-RO1 funding and those without funding) performed at a higher per-hour rate, when estimating 10% or 15% protected time (4.9 and 3.3 publications per 1,000 research hours, respectively).
“I think this reinforces the notion that there are far more neurologists out there who aren’t trained as MD-PhDs, who aren’t receiving R01s, but who are making meaningful contributions,” Mr. Bensken said. “Our ultimate goal is to maximize the potential of everybody in this environment to contribute. If everyone was able to contribute what they could, I think research would be far more successful and far more impactful than it is now.”
The study was funded by the NINDS. Mr. Bensken reported having no financial disclosures.
SOURCE: Bensken WP et al. Ann Neurol. 2018;84[S22]:S72-3, Abstract S176.
REPORTING FROM ANA 2018
Key clinical point:
Major finding: Those in the R01-funded group with 80% protected research time produced 3.2 publications per 1,000 research hours, while those in the non–R01-funded group with 40% protected research time produced 3.0 publications per 1,000 research hours.
Study details: An analysis of 244 neurology residency program graduates.
Disclosures: The study was funded by the NINDS. Mr. Bensken reported having no financial disclosures.
Source: Bensken WP et al. Ann Neurol. 2018;84[S 22]:S72-3, Abstract S176.
Jaya Aysola: Gender inclusivity
Dr. Aysola is an assistant professor of medicine and pediatrics at the Perelman School of Medicine. Her primary appointment in the Divisions of General Internal Medicine.
In early August 2018, Dr. Aysola and her colleagues published a qualitative narrative analysis regarding the perceptions of the factors associated with inclusive workplaces in healthcare.
Dr. Aysola is an assistant professor of medicine and pediatrics at the Perelman School of Medicine. Her primary appointment in the Divisions of General Internal Medicine.
In early August 2018, Dr. Aysola and her colleagues published a qualitative narrative analysis regarding the perceptions of the factors associated with inclusive workplaces in healthcare.
Dr. Aysola is an assistant professor of medicine and pediatrics at the Perelman School of Medicine. Her primary appointment in the Divisions of General Internal Medicine.
In early August 2018, Dr. Aysola and her colleagues published a qualitative narrative analysis regarding the perceptions of the factors associated with inclusive workplaces in healthcare.