User login
FDA approves new antibiotic for HABP/VABP treatment
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
The most common adverse events associated with Recarbrio are increased alanine aminotransferase/ aspartate aminotransferase, anemia, diarrhea, hypokalemia, and hyponatremia. Recarbrio was previously approved by the FDA to treat patients with complicated urinary tract infections and complicated intra-abdominal infections who have limited or no alternative treatment options, according to an FDA press release.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, director of the division of anti-infectives within the office of infectious disease at the Center for Drug Evaluation and Research.
Pulmonology, critical care earnings on the upswing before pandemic
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
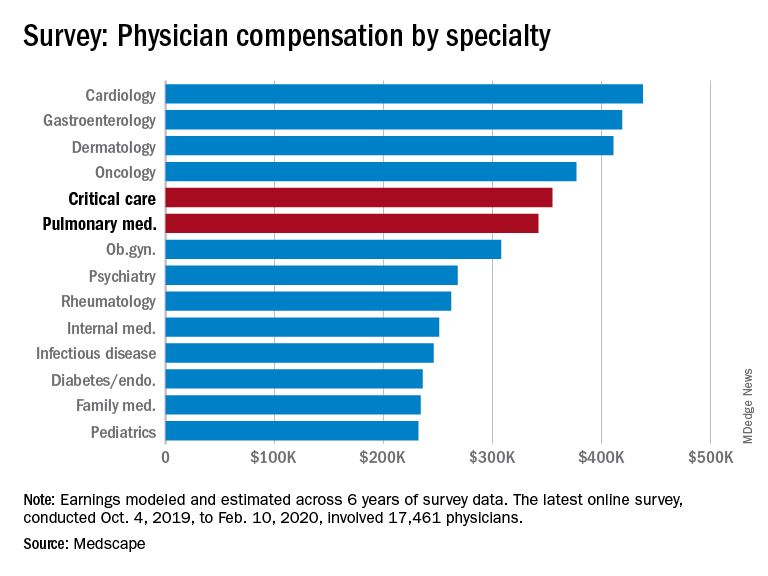
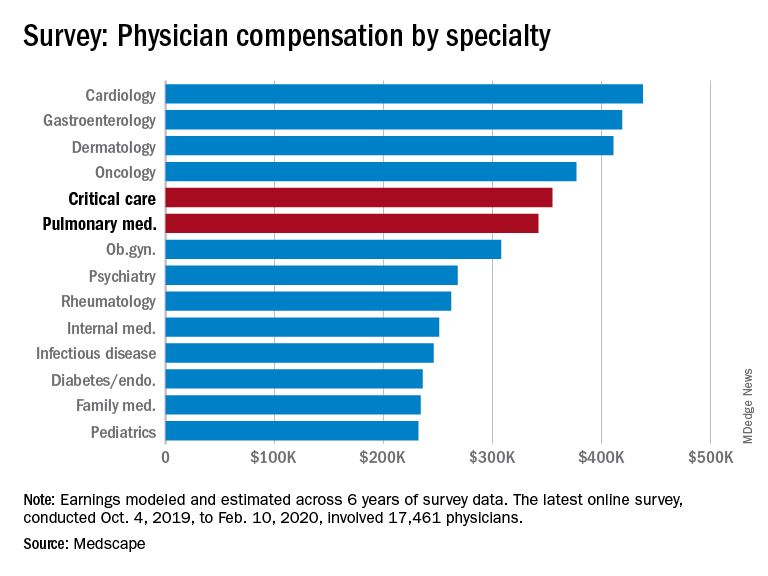
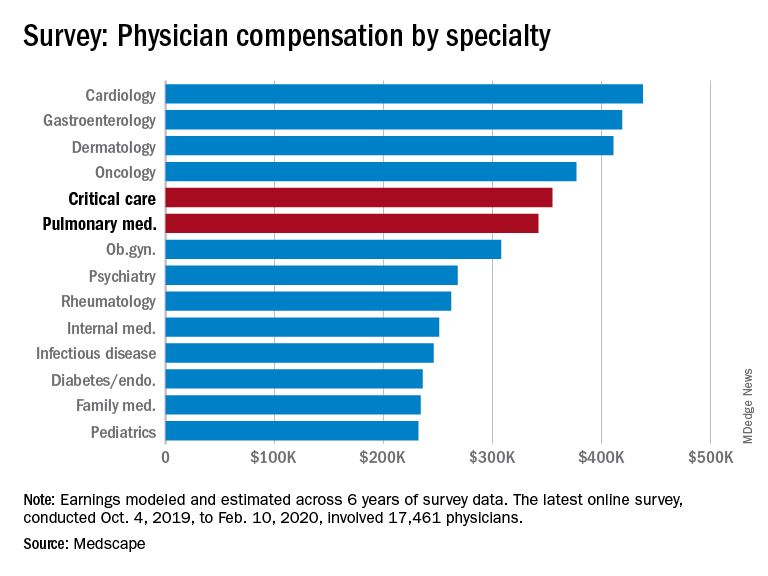
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Vitamin D: A low-hanging fruit in COVID-19?
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Mainstream media outlets have been flooded recently with reports speculating on what role, if any, vitamin D may play in reducing the severity of COVID-19 infection.
as well as mortality, with the further suggestion of an effect of vitamin D on the immune response to infection.
But other studies question such a link, including any association between vitamin D concentration and differences in COVID-19 severity by ethnic group.
And while some researchers and clinicians believe people should get tested to see if they have adequate vitamin D levels during this pandemic – in particular frontline health care workers – most doctors say the best way to ensure that people have adequate levels of vitamin D during COVID-19 is to simply take supplements at currently recommended levels.
This is especially important given the fact that, during “lockdown” scenarios, many people are spending more time than usual indoors.
Clifford Rosen, MD, senior scientist at Maine Medical Center’s Research Institute in Scarborough, has been researching vitamin D for 25 years.
“There’s no randomized, controlled trial for sure, and that’s the gold standard,” he said in an interview, and “the observational data are so confounded, it’s difficult to know.”
Whether from diet or supplementation, having adequate vitamin D is important, especially for those at the highest risk of COVID-19, he said. Still, robust data supporting a role of vitamin D in prevention of COVID-19, or as any kind of “therapy” for the infection, are currently lacking.
Rose Anne Kenny, MD, professor of medical gerontology at Trinity College Dublin, recently coauthored an article detailing an inverse association between vitamin D levels and mortality from COVID-19 across countries in Europe.
“At no stage are any of us saying this is a given, but there’s a probability that [vitamin D] – a low-hanging fruit – is a contributory factor and we can do something about it now,” she said in an interview.
Dr. Kenny is calling for the Irish government to formally change their recommendations. “We call on the Irish government to update guidelines as a matter of urgency and encourage all adults to take [vitamin D] supplements during the COVID-19 crisis.” Northern Ireland, part of the United Kingdom, also has not yet made this recommendation, she said.
Meanwhile, Harpreet S. Bajaj, MD, MPH, a practicing endocrinologist from Mount Sinai Hospital, Toronto, said: “Vitamin D could have any of three potential roles in risk for COVID-19 and/or its severity: no role, simply a marker, or a causal factor.”
Dr. Bajaj said – as did Dr. Rosen and Dr. Kenny – that randomized, controlled trials (RCTs) are sorely needed to help ascertain whether there is a specific role of vitamin D.
“Until then, we should continue to follow established public health recommendations for vitamin D supplementation, in addition to following COVID-19 prevention guidance and evolving guidelines for COVID-19 treatment.”
What is the role of vitamin D fortification?
In their study in the Irish Medical Journal, Dr. Kenny and colleagues noted that, in Europe, despite being sunny, Spain and Northern Italy had high rates of vitamin D deficiency and have experienced some of the highest COVID-19 infection and mortality rates in the world.
But these countries do not formally fortify foods or recommend supplementation with vitamin D.
Conversely, the northern countries of Norway, Finland, and Sweden had higher vitamin D levels despite less UVB sunlight exposure, as a result of common supplementation and formal fortification of foods. These Nordic countries also had lower levels of COVID-19 infection and mortality.
Overall, the correlation between low vitamin D levels and mortality from COVID-19 was statistically significant (P = .046), the investigators reported.
“Optimizing vitamin D status to recommendations by national and international public health agencies will certainly have ... potential benefits for COVID-19,” they concluded.
“We’re not saying there aren’t any confounders. This can absolutely be the case, but this [finding] needs to be in the mix of evidence,” Dr. Kenny said.
Dr. Kenny also noted that countries in the Southern Hemisphere have been seeing a relatively low mortality from COVID-19, although she acknowledged the explanation could be that the virus spread later to those countries.
Dr. Rosen has doubts on this issue, too.
“Sure, vitamin D supplementation may have worked for [Nordic countries], their COVID-19 has been better controlled, but there’s no causality here; there’s another step to actually prove this. Other factors might be at play,” he said.
“Look at Brazil, it’s at the equator but the disease is devastating the country. Right now, I just don’t believe it.”
Does vitamin D have a role to play in immune modulation?
One theory currently circulating is that, if vitamin D does have any role to play in modulating response to COVID-19, this may be via a blunting of the immune system reaction to the virus.
In a recent preprint study, Ali Daneshkhah, PhD, and colleagues from Northwestern University, Chicago, interrogated hospital data from China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the United Kingdom, and the United States.
Specifically, the risk of severe COVID-19 cases among patients with severe vitamin D deficiency was 17.3%, whereas the equivalent figure for patients with normal vitamin D levels was 14.6% (a reduction of 15.6%).
“This potential effect may be attributed to vitamin D’s ability to suppress the adaptive immune system, regulating cytokine levels and thereby reducing the risk of developing severe COVID-19,” said the researchers.
Likewise, JoAnn E. Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital in Boston, in a recent commentary, noted evidence from an observational study from three South Asian hospitals, in which the prevalence of vitamin D deficiency was much higher among those with severe COVID-19 illness compared with those with mild illness.
“We also know that vitamin D has an immune-modulating effect and can lower inflammation, and this may be relevant to the respiratory response during COVID-19 and the cytokine storm that’s been demonstrated,” she noted.
Dr. Rosen said he is willing to listen on the issue of a potential role of vitamin D in immune modulation.
“I’ve been a huge skeptic from the get-go, and loudly criticized the data for doing nothing. I am surprised at myself for saying there might be some effect,” he said.
“Clearly most people don’t get this [cytokine storm] but of those that do, it’s unclear why they do. Maybe if you are vitamin D sufficient, it might have some impact down the road on your response to an infection,” Dr. Rosen said. “Vitamin D may induce proteins important in modulating the function of macrophages of the immune system.”
Ethnic minorities disproportionately affected
It is also well recognized that COVID-19 disproportionately affects black and Asian minority ethnic individuals.
But on the issue of vitamin D in this context, one recent peer-reviewed study using UK Biobank data found no evidence to support a potential role for vitamin D concentration to explain susceptibility to COVID-19 infection either overall or in explaining differences between ethnic groups.
“Vitamin D is unlikely to be the underlying mechanism for the higher risk observed in black and minority ethnic individuals, and vitamin D supplements are unlikely to provide an effective intervention,” Claire Hastie, PhD, of the University of Glasgow and colleagues concluded.
But this hasn’t stopped two endocrinologists from appealing to members of the British Association of Physicians of Indian Origin (BAPIO) to get their vitamin D levels tested.
The black and Asian minority ethnic population, “especially frontline staff, should get their Vitamin D3 levels checked and get appropriate replacement as required,” said Parag Singhal, MD, of Weston General Hospital, Weston-Super-Mare, England, and David C. Anderson, a retired endocrinologist, said in a letter to BAPIO members.
Indeed, they suggested a booster dose of 100,000 IU as a one-off for black and Asian minority ethnic health care staff that should raise vitamin D levels for 2-3 months. They referred to a systematic review that concludes that “single vitamin D3 doses ≥300,000 IU are most effective at improving vitamin D status ... for up to 3 months”.
Commenting on the idea, Dr. Rosen remarked that, in general, the high-dose 50,000-500,000 IU given as a one-off does not confer any greater benefit than a single dose of 1,000 IU per day, except that the blood levels go up quicker and higher.
“Really there is no evidence that getting to super-high levels of vitamin D confer a greater benefit than normal levels,” he said. “So if health care workers suspect vitamin D deficiency, daily doses of 1,000 IU seem reasonable; even if they miss doses, the blood levels are relatively stable.”
On the specific question of vitamin D needs in ethnic minorities, Dr. Rosen said while such individuals do have lower serum levels of vitamin D, the issue is whether there are meaningful clinical implications related to this.
“The real question is whether [ethnic minority individuals] have physiologically adapted for this in other ways because these low levels have been so for thousands of years. In fact, African Americans have lower vitamin D levels but they absolutely have better bones than [whites],” he pointed out.
Testing and governmental recommendations during COVID-19
The U.S. National Institutes of Health in general advises 400 IU to 800 IU per day intake of vitamin D, depending on age, with those over 70 years requiring the highest daily dose. This will result in blood levels that are sufficient to maintain bone health and normal calcium metabolism in healthy people. There are no additional recommendations specific to vitamin D intake during the COVID-19 pandemic, however.
And Dr. Rosen pointed out that there is no evidence for mass screening of vitamin D levels among the U.S. population.
“U.S. public health guidance was pre-COVID, and I think high-risk individuals might want to think about their levels; for example, someone with inflammatory bowel disease or liver or pancreatic disease. These people are at higher risk anyway, and it could be because their vitamin D is low,” he said.
“Skip the test and ensure you are getting adequate levels of vitamin D whether via diet or supplement [400-800 IU per day],” he suggested. “It won’t harm.”
The U.K.’s Public Health England (PHE) clarified its advice on vitamin D supplementation during COVID-19. Alison Tedstone, PhD, chief nutritionist at PHE, said: “Many people are spending more time indoors and may not get all the vitamin D they need from sunlight. To protect their bone and muscle health, they should consider taking a daily supplement containing 10 micrograms [400 IU] of vitamin D.”
However, “there is no sufficient evidence to support recommending Vitamin D for reducing the risk of COVID-19,” she stressed.
Dr. Bajaj is on the advisory board of Medscape Diabetes & Endocrinology. He has ties with Amgen, AstraZeneca Boehringer Ingelheim, Janssen, Merck, Novo Nordisk, Sanofi, Eli Lilly,Valeant, Canadian Collaborative Research Network, CMS Knowledge Translation, Diabetes Canada Scientific Group, LMC Healthcare,mdBriefCase,Medscape, andMeducom. Dr. Kenny, Dr. Rosen, and Dr. Singhal have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hazard pay included in new COVID-19 relief bill
Hazard pay for frontline health care workers – an idea that has been championed by President Donald J. Trump and Senate Minority Leader Chuck Schumer, among others – is included in a just-released COVID-19 relief package assembled by Democrats in the House of Representatives.
according to a report in the Washington Post.
But it is far from a done deal. “The Democrats’ spending bill is a Pelosi-led pipe dream written in private,” said House Republican Leader Kevin McCarthy (Calif.) in a Fox News interview posted May 12 on Facebook.
Senate Majority Leader Mitch McConnell condemned the package. “This is exactly the wrong approach,” he said in a prepared statement that instead laid out a variety of liability protections, which he said should be the first priority.
“We are not going to let health care heroes emerge from this crisis facing a tidal wave of medical malpractice lawsuits so that trial lawyers can line their pockets,” said Sen. McConnell, adding that his plan would “raise the liability threshold for COVID-related malpractice lawsuits.”
Ingrida Lusis, vice president of government affairs and health policy at the American Nurses Association, said in an interview that the ANA had lobbied for hazard pay and was told it would be in the next relief package.
“Though there is an inherent risk in the nursing profession, we think that this is really critical to ensuring that we have a workforce to meet the intense demands of this pandemic,” said Ms. Lusis.
“If health care workers are not treated and compensated appropriately for what they’re going through right now, then we may not have a next generation that will want to enter the field,” she said.
Various nursing organizations, nurses’ unions, and health care unions, such as the American Federation of State, County and Municipal Employees (AFSCME) and the Service Employees International Union, have advocated for hazard pay.
Physicians’ organizations have not been vocal on the issue, however. The American Medical Association, for instance, pushed for hazard pay for residents but has not made any further public statements. An AMA spokesman said that the group was monitoring the situation but declined further comment.
Multiple online petitions seeking hazard pay for health care workers have been circulated, including one seeking the same $600 bump for essential workers that was given out as part of unemployment benefits in the first COVID-19 relief package. More than 1.2 million had signed the petition as of May 12.
‘Heroes fund’
The president first suggested hazard pay for health care workers on March 30 Fox News broadcast. “These are really brave people,” he said, adding that the administration was considering different ways of boosting pay, primarily through hospitals.
“We are asking the hospitals to do it and to consider something, including bonuses,” said Trump. “If anybody’s entitled to it, they are.”
On April 7, Sen. Schumer proposed a “Heroes Fund.” It would give public, private, and tribal frontline employees – including doctors, nurses, first responders, and transit, grocery, and postal workers – a $13 per hour raise up to $25,000 in additional pay through Dec. 31 for workers earning up to $200,000 and $5,000 in additional pay for those earning more than $200,000. It would also provide a $15,000 signing bonus to those who agree to take on such a position.
Rep. Matt Cartwright (D-Pa.) introduced a bill in mid-April, the Coronavirus Frontline Workers Fair Pay Act (HR 6709), that would provide similar pay increases. Health care workers would receive an additional $13 per hour. It would be retroactive to Jan. 31, 2020, and would be available through the end of 2020.
Molly Kinder of the Brookings Institution, a self-described nonpartisan Washington policy institute, estimates that Sen. Schumer’s proposal would represent the equivalent of double-time pay for the average low-wage worker, a 50% pay increase for a mail carrier, a 20% boost for a pharmacist, and less than a 15% increase for a surgeon, as determined from median 2018 wages.
Before the House Democrats unveiled their bill, Isabel Soto of the center-right group American Action Forum estimated that a $13 per hour wage increase could cost $398.9 billion just from the end of March to the end of September. A great proportion of that amount – $264 billion – would go to some 10 million health care workers, Ms. Soto calculated.
Some already offering pay boost
A few states and hospital systems are already offering hazard pay.
On April 12, Massachusetts agreed to give about 6,500 AFSCME union members who work at state human services facilities and group homes a $5 or a $10 per hour pay increase, depending on duties. It was to stay in effect until at least May 30.
Maine Governor Janet Mills (D) also agreed to increase pay by $3-$5 an hour for AFSCME workers in state correctional and mental health facilities beginning March 29.
In New York City, the biggest hospital network, Northwell Health, in late April gave 45,000 workers – including nurses, physicians, respiratory therapists, environmental services workers, housekeepers, and people in outpatient and corporate roles – a lump sum bonus payment of up to $2,500 and 1 week of paid time off. The money came out of the system’s general fund.
“As an organization, we want to continue to support, motivate and inspire our team members,” said Northwell President and CEO Michael Dowling in a statement at the time.
On April 2, New York–Presbyterian Hospital’s chair of the department of surgery, Craig Smith, MD, announced that the facility was “providing a $1,250 bonus for everyone who has worked in or supported the COVID-19 front lines, for at least 1 week.”
Advocate Aurora, with 15 hospitals and 32,000 employees in Wisconsin, said in early April that it was giving increases of $6.25-$15.00 an hour at least through the end of May.
A version of this article originally appeared on Medscape.com.
Hazard pay for frontline health care workers – an idea that has been championed by President Donald J. Trump and Senate Minority Leader Chuck Schumer, among others – is included in a just-released COVID-19 relief package assembled by Democrats in the House of Representatives.
according to a report in the Washington Post.
But it is far from a done deal. “The Democrats’ spending bill is a Pelosi-led pipe dream written in private,” said House Republican Leader Kevin McCarthy (Calif.) in a Fox News interview posted May 12 on Facebook.
Senate Majority Leader Mitch McConnell condemned the package. “This is exactly the wrong approach,” he said in a prepared statement that instead laid out a variety of liability protections, which he said should be the first priority.
“We are not going to let health care heroes emerge from this crisis facing a tidal wave of medical malpractice lawsuits so that trial lawyers can line their pockets,” said Sen. McConnell, adding that his plan would “raise the liability threshold for COVID-related malpractice lawsuits.”
Ingrida Lusis, vice president of government affairs and health policy at the American Nurses Association, said in an interview that the ANA had lobbied for hazard pay and was told it would be in the next relief package.
“Though there is an inherent risk in the nursing profession, we think that this is really critical to ensuring that we have a workforce to meet the intense demands of this pandemic,” said Ms. Lusis.
“If health care workers are not treated and compensated appropriately for what they’re going through right now, then we may not have a next generation that will want to enter the field,” she said.
Various nursing organizations, nurses’ unions, and health care unions, such as the American Federation of State, County and Municipal Employees (AFSCME) and the Service Employees International Union, have advocated for hazard pay.
Physicians’ organizations have not been vocal on the issue, however. The American Medical Association, for instance, pushed for hazard pay for residents but has not made any further public statements. An AMA spokesman said that the group was monitoring the situation but declined further comment.
Multiple online petitions seeking hazard pay for health care workers have been circulated, including one seeking the same $600 bump for essential workers that was given out as part of unemployment benefits in the first COVID-19 relief package. More than 1.2 million had signed the petition as of May 12.
‘Heroes fund’
The president first suggested hazard pay for health care workers on March 30 Fox News broadcast. “These are really brave people,” he said, adding that the administration was considering different ways of boosting pay, primarily through hospitals.
“We are asking the hospitals to do it and to consider something, including bonuses,” said Trump. “If anybody’s entitled to it, they are.”
On April 7, Sen. Schumer proposed a “Heroes Fund.” It would give public, private, and tribal frontline employees – including doctors, nurses, first responders, and transit, grocery, and postal workers – a $13 per hour raise up to $25,000 in additional pay through Dec. 31 for workers earning up to $200,000 and $5,000 in additional pay for those earning more than $200,000. It would also provide a $15,000 signing bonus to those who agree to take on such a position.
Rep. Matt Cartwright (D-Pa.) introduced a bill in mid-April, the Coronavirus Frontline Workers Fair Pay Act (HR 6709), that would provide similar pay increases. Health care workers would receive an additional $13 per hour. It would be retroactive to Jan. 31, 2020, and would be available through the end of 2020.
Molly Kinder of the Brookings Institution, a self-described nonpartisan Washington policy institute, estimates that Sen. Schumer’s proposal would represent the equivalent of double-time pay for the average low-wage worker, a 50% pay increase for a mail carrier, a 20% boost for a pharmacist, and less than a 15% increase for a surgeon, as determined from median 2018 wages.
Before the House Democrats unveiled their bill, Isabel Soto of the center-right group American Action Forum estimated that a $13 per hour wage increase could cost $398.9 billion just from the end of March to the end of September. A great proportion of that amount – $264 billion – would go to some 10 million health care workers, Ms. Soto calculated.
Some already offering pay boost
A few states and hospital systems are already offering hazard pay.
On April 12, Massachusetts agreed to give about 6,500 AFSCME union members who work at state human services facilities and group homes a $5 or a $10 per hour pay increase, depending on duties. It was to stay in effect until at least May 30.
Maine Governor Janet Mills (D) also agreed to increase pay by $3-$5 an hour for AFSCME workers in state correctional and mental health facilities beginning March 29.
In New York City, the biggest hospital network, Northwell Health, in late April gave 45,000 workers – including nurses, physicians, respiratory therapists, environmental services workers, housekeepers, and people in outpatient and corporate roles – a lump sum bonus payment of up to $2,500 and 1 week of paid time off. The money came out of the system’s general fund.
“As an organization, we want to continue to support, motivate and inspire our team members,” said Northwell President and CEO Michael Dowling in a statement at the time.
On April 2, New York–Presbyterian Hospital’s chair of the department of surgery, Craig Smith, MD, announced that the facility was “providing a $1,250 bonus for everyone who has worked in or supported the COVID-19 front lines, for at least 1 week.”
Advocate Aurora, with 15 hospitals and 32,000 employees in Wisconsin, said in early April that it was giving increases of $6.25-$15.00 an hour at least through the end of May.
A version of this article originally appeared on Medscape.com.
Hazard pay for frontline health care workers – an idea that has been championed by President Donald J. Trump and Senate Minority Leader Chuck Schumer, among others – is included in a just-released COVID-19 relief package assembled by Democrats in the House of Representatives.
according to a report in the Washington Post.
But it is far from a done deal. “The Democrats’ spending bill is a Pelosi-led pipe dream written in private,” said House Republican Leader Kevin McCarthy (Calif.) in a Fox News interview posted May 12 on Facebook.
Senate Majority Leader Mitch McConnell condemned the package. “This is exactly the wrong approach,” he said in a prepared statement that instead laid out a variety of liability protections, which he said should be the first priority.
“We are not going to let health care heroes emerge from this crisis facing a tidal wave of medical malpractice lawsuits so that trial lawyers can line their pockets,” said Sen. McConnell, adding that his plan would “raise the liability threshold for COVID-related malpractice lawsuits.”
Ingrida Lusis, vice president of government affairs and health policy at the American Nurses Association, said in an interview that the ANA had lobbied for hazard pay and was told it would be in the next relief package.
“Though there is an inherent risk in the nursing profession, we think that this is really critical to ensuring that we have a workforce to meet the intense demands of this pandemic,” said Ms. Lusis.
“If health care workers are not treated and compensated appropriately for what they’re going through right now, then we may not have a next generation that will want to enter the field,” she said.
Various nursing organizations, nurses’ unions, and health care unions, such as the American Federation of State, County and Municipal Employees (AFSCME) and the Service Employees International Union, have advocated for hazard pay.
Physicians’ organizations have not been vocal on the issue, however. The American Medical Association, for instance, pushed for hazard pay for residents but has not made any further public statements. An AMA spokesman said that the group was monitoring the situation but declined further comment.
Multiple online petitions seeking hazard pay for health care workers have been circulated, including one seeking the same $600 bump for essential workers that was given out as part of unemployment benefits in the first COVID-19 relief package. More than 1.2 million had signed the petition as of May 12.
‘Heroes fund’
The president first suggested hazard pay for health care workers on March 30 Fox News broadcast. “These are really brave people,” he said, adding that the administration was considering different ways of boosting pay, primarily through hospitals.
“We are asking the hospitals to do it and to consider something, including bonuses,” said Trump. “If anybody’s entitled to it, they are.”
On April 7, Sen. Schumer proposed a “Heroes Fund.” It would give public, private, and tribal frontline employees – including doctors, nurses, first responders, and transit, grocery, and postal workers – a $13 per hour raise up to $25,000 in additional pay through Dec. 31 for workers earning up to $200,000 and $5,000 in additional pay for those earning more than $200,000. It would also provide a $15,000 signing bonus to those who agree to take on such a position.
Rep. Matt Cartwright (D-Pa.) introduced a bill in mid-April, the Coronavirus Frontline Workers Fair Pay Act (HR 6709), that would provide similar pay increases. Health care workers would receive an additional $13 per hour. It would be retroactive to Jan. 31, 2020, and would be available through the end of 2020.
Molly Kinder of the Brookings Institution, a self-described nonpartisan Washington policy institute, estimates that Sen. Schumer’s proposal would represent the equivalent of double-time pay for the average low-wage worker, a 50% pay increase for a mail carrier, a 20% boost for a pharmacist, and less than a 15% increase for a surgeon, as determined from median 2018 wages.
Before the House Democrats unveiled their bill, Isabel Soto of the center-right group American Action Forum estimated that a $13 per hour wage increase could cost $398.9 billion just from the end of March to the end of September. A great proportion of that amount – $264 billion – would go to some 10 million health care workers, Ms. Soto calculated.
Some already offering pay boost
A few states and hospital systems are already offering hazard pay.
On April 12, Massachusetts agreed to give about 6,500 AFSCME union members who work at state human services facilities and group homes a $5 or a $10 per hour pay increase, depending on duties. It was to stay in effect until at least May 30.
Maine Governor Janet Mills (D) also agreed to increase pay by $3-$5 an hour for AFSCME workers in state correctional and mental health facilities beginning March 29.
In New York City, the biggest hospital network, Northwell Health, in late April gave 45,000 workers – including nurses, physicians, respiratory therapists, environmental services workers, housekeepers, and people in outpatient and corporate roles – a lump sum bonus payment of up to $2,500 and 1 week of paid time off. The money came out of the system’s general fund.
“As an organization, we want to continue to support, motivate and inspire our team members,” said Northwell President and CEO Michael Dowling in a statement at the time.
On April 2, New York–Presbyterian Hospital’s chair of the department of surgery, Craig Smith, MD, announced that the facility was “providing a $1,250 bonus for everyone who has worked in or supported the COVID-19 front lines, for at least 1 week.”
Advocate Aurora, with 15 hospitals and 32,000 employees in Wisconsin, said in early April that it was giving increases of $6.25-$15.00 an hour at least through the end of May.
A version of this article originally appeared on Medscape.com.
ER docs ask, “Where are our patients?”
according to an expert panel on unanticipated consequences of pandemic care hosted by the presidents of the Society of Critical Care Medicine and the American College of Emergency Physicians.*
“At the peak of exposure to COVID-19 illness or infection, ED volumes in my system, which are really not much different from others across the country, were cut in half, if not more. And those changes happened across virtually every form of ED presentation, from the highest acuity to the lowest. We’re now beyond our highest level of exposure to COVID-19 clinically symptomatic patients in western Pennsylvania, but that recovery in volume hasn’t occurred yet, although there are some embers,” explained Donald M. Yealy, MD, professor and chair of the department of emergency medicine at the University of Pittsburgh.
He and other panelists also addressed some of the other unanticipated developments in the COVID-19 pandemic, including a recently recognized childhood manifestation called for now COVID-associated pediatric multisystem inflammatory syndrome, an anticipated massive second wave of non-COVID patients expected to present late to EDs and primary care clinics after having avoided needed medical care out of fear of infection, and the pandemic’s negative impact upon medical education.
Who’s not showing up in the ED
Dr. Yealy said that across the country, the number of patients arriving in EDs with acute ST-elevation MI, stroke, trauma, and other highest-acuity presentations is down substantially. But the volume of patients with more routine, bread-and-butter conditions typically seen in EDs is down even more.
“You might say, if I was designing from the insurance side, this is exactly what I’d hope for. I’ve heard that some people on the insurance-only side of the business really are experiencing a pretty good deal right now: They’re collecting premiums and not having to pay out on the ED or hospital side,” he said.
Tweaking the public health message on seeking medical care
“One of the unanticipated casualties of the pandemic are the patients who don’t have it. It will take a whole lot of work and coordinated effort to re-engage with those patients,” predicted SCCM President Lewis J. Kaplan, MD, professor of surgery at the University of Pennsylvania, Philadelphia.
Evie G. Marcolini, MD, described what she believes is necessary now: “We need to have a big focus on getting the word out to the public that acute MI, stroke, and other acute injuries are still a time-sensitive problem and they warrant at least a call to their physician or consideration of coming in to the ED.
“I think when we started out, we were telling people, ‘Don’t come in.’ Now we’re trying to dial it back a little bit and say, ‘Listen, there are things you really do need to come in for. And we will keep you safe,’” said Dr. Marcolini, an emergency medicine and neurocritical care specialist at Dartmouth-Hitchcock Medical Center, Hanover, N.H.
“It is safe,” Dr. Yealy agreed. “The safest place in the world to be right now is the ED. Everybody’s cordoned off. There’s way more PPE [personal protective equipment]. There’s a level of precision now that should have existed but never did in our previous influenza seasons. So we have something very unique to offer, and we can put people’s minds at rest.”
He spoke of a coming “tsunami of untreated illness.”
“My concern is there is a significant subset of people who are not only eschewing ED care but staying away from their primary care provider. My fear is that we’re not as well aware of this,” he said. “Together with our primary care partners, we have to figure out ways to reach the people who are ignoring illnesses and injuries that they’re making long-term decisions about without realizing it. We have to find a way to reach those people and say it’s okay to reach for care.”
SCCM Immediate Past President Heatherlee Bailey, MD, also sees a problematic looming wave.
“I’m quite concerned about the coming second wave of non-COVID patients who’ve sat home with their worsening renal failure that’s gone from 2 to 5 because they’ve been taking a lot of NSAIDs, or the individual who’s had several TIAs that self-resolved, and we’ve missed an opportunity to prevent some significant disease. At some point they’re going to come back, and we need to figure out how to get these individuals hooked up with care, either through the ED or with their primary care provider, to prevent these potential bad outcomes,” said Dr. Bailey of the Durham (N.C.) Veterans Affairs Medical Center.
Interim guidance for pediatricians on an alarming new syndrome
Edward E. Conway Jr., MD, recalled that early in the U.S. pandemic, pediatricians felt a sense of relief that children appeared to be spared from severe COVID-19 disease. But, in just the past few weeks, a new syndrome has emerged. New York City has recorded more than 100 cases of what’s provisionally being called COVID-associated pediatric multisystem inflammatory syndrome. Dr. Conway and others are working with the Centers for Disease Control and Prevention to develop a case definition for the syndrome, first reported by pediatricians in Italy and the United Kingdom.
“We’re trying to get the word out to general pediatricians as to the common signs and symptoms that should prompt parents to bring their children in for medical care,” according to Dr. Conway, chief of pediatric critical care medicine and vice-chair of pediatrics at Jacobi Medical Center in New York.
Ninety percent of affected children have abdominal symptoms early on, including abdominal pain, diarrhea, emesis, or enteritis upon imaging. A nondescript rash, headache, conjunctivitis, and irritability are common, cough much less so – under 25%.
“The thought is that if any one of these is associated with a fever lasting more than 4 days, we suggest these children be brought in and seen by a pediatrician. We don’t have a formal guideline – we’re working on that – but basically the current recommendation is to screen them initially with a CBC with differential, a chem 10, and liver function tests, but also to look for inflammatory markers that we see in our COVID patients. We’ve been quite surprised: These patients have C-reactive proteins of about 240 mg/L on average, ferritin is quite high at around 1,200 ng/mL, and d-dimers of 2,300 ng/mL. We’ve also found very high brain natriuretic peptides and troponins in these patients,” according to Dr. Conway.
Analogies have been made between this COVID-19 pediatric syndrome and Kawasaki disease. Dr. Conway is unconvinced.
“This is quite different from Kawasaki in that these children are usually thrombocytopenic and usually present with DIC [disseminated intravascular coagulation], and the d-dimers are extraordinarily high, compared to what we’re used to seeing in pediatric patients,” he said.
Symptomatic children with laboratory red flags should be hospitalized. Most of the affected New York City children have recovered after 5 or 6 days in the pediatric ICU with empiric treatment using intravenous immunoglobulin (IVIG), corticosteroids, and/or interleukin-6 inhibitors. However, five recent deaths are now under study.
Dr. Yealy commented that this new pediatric syndrome is “really interesting,” but to date, it affects only a very small percentage of children, and children overall have been much less affected by the pandemic than are adults.
“The populations being disproportionately impacted are the elderly, the elderly, the elderly, and then other vulnerable populations, particularly congregants and the poor,” he said. “At my site, three-quarters of the patients coming in are either patients at assisted-living facilities or work at one of those congregant facilities.”
The pandemic’s impact on medical education
In many hospitals, grand rounds are being done virtually via videoconferencing, often with attendant challenges in asking and answering questions. Hospital patient volumes are diminished. Medical students aren’t coming in to do clinical rotations. Medical students and residents can’t travel to interview for future residencies or jobs.
“It’s affecting education across all of the components of medicine. It’s hard to say how long this pandemic is going to last. We’re all trying to be innovative in using online tools, but I believe it’s going to have a long-lasting effect on our education system,” Dr. Marcolini predicted.
Remote interface while working from home has become frustrating, especially during peak Internet use hours.
“It’s staggering how slow my home system has become in comparison to what’s wired at work. Now many times when you try to get into your work system from home, you time out while you’re waiting for the next piece of information to come across,” Dr. Kaplan commented.
All panel participants reported having no financial conflicts of interest.
*Correction, 5/15/20: An earlier version of this article misstated the name of the American College of Emergency Physicians.)
according to an expert panel on unanticipated consequences of pandemic care hosted by the presidents of the Society of Critical Care Medicine and the American College of Emergency Physicians.*
“At the peak of exposure to COVID-19 illness or infection, ED volumes in my system, which are really not much different from others across the country, were cut in half, if not more. And those changes happened across virtually every form of ED presentation, from the highest acuity to the lowest. We’re now beyond our highest level of exposure to COVID-19 clinically symptomatic patients in western Pennsylvania, but that recovery in volume hasn’t occurred yet, although there are some embers,” explained Donald M. Yealy, MD, professor and chair of the department of emergency medicine at the University of Pittsburgh.
He and other panelists also addressed some of the other unanticipated developments in the COVID-19 pandemic, including a recently recognized childhood manifestation called for now COVID-associated pediatric multisystem inflammatory syndrome, an anticipated massive second wave of non-COVID patients expected to present late to EDs and primary care clinics after having avoided needed medical care out of fear of infection, and the pandemic’s negative impact upon medical education.
Who’s not showing up in the ED
Dr. Yealy said that across the country, the number of patients arriving in EDs with acute ST-elevation MI, stroke, trauma, and other highest-acuity presentations is down substantially. But the volume of patients with more routine, bread-and-butter conditions typically seen in EDs is down even more.
“You might say, if I was designing from the insurance side, this is exactly what I’d hope for. I’ve heard that some people on the insurance-only side of the business really are experiencing a pretty good deal right now: They’re collecting premiums and not having to pay out on the ED or hospital side,” he said.
Tweaking the public health message on seeking medical care
“One of the unanticipated casualties of the pandemic are the patients who don’t have it. It will take a whole lot of work and coordinated effort to re-engage with those patients,” predicted SCCM President Lewis J. Kaplan, MD, professor of surgery at the University of Pennsylvania, Philadelphia.
Evie G. Marcolini, MD, described what she believes is necessary now: “We need to have a big focus on getting the word out to the public that acute MI, stroke, and other acute injuries are still a time-sensitive problem and they warrant at least a call to their physician or consideration of coming in to the ED.
“I think when we started out, we were telling people, ‘Don’t come in.’ Now we’re trying to dial it back a little bit and say, ‘Listen, there are things you really do need to come in for. And we will keep you safe,’” said Dr. Marcolini, an emergency medicine and neurocritical care specialist at Dartmouth-Hitchcock Medical Center, Hanover, N.H.
“It is safe,” Dr. Yealy agreed. “The safest place in the world to be right now is the ED. Everybody’s cordoned off. There’s way more PPE [personal protective equipment]. There’s a level of precision now that should have existed but never did in our previous influenza seasons. So we have something very unique to offer, and we can put people’s minds at rest.”
He spoke of a coming “tsunami of untreated illness.”
“My concern is there is a significant subset of people who are not only eschewing ED care but staying away from their primary care provider. My fear is that we’re not as well aware of this,” he said. “Together with our primary care partners, we have to figure out ways to reach the people who are ignoring illnesses and injuries that they’re making long-term decisions about without realizing it. We have to find a way to reach those people and say it’s okay to reach for care.”
SCCM Immediate Past President Heatherlee Bailey, MD, also sees a problematic looming wave.
“I’m quite concerned about the coming second wave of non-COVID patients who’ve sat home with their worsening renal failure that’s gone from 2 to 5 because they’ve been taking a lot of NSAIDs, or the individual who’s had several TIAs that self-resolved, and we’ve missed an opportunity to prevent some significant disease. At some point they’re going to come back, and we need to figure out how to get these individuals hooked up with care, either through the ED or with their primary care provider, to prevent these potential bad outcomes,” said Dr. Bailey of the Durham (N.C.) Veterans Affairs Medical Center.
Interim guidance for pediatricians on an alarming new syndrome
Edward E. Conway Jr., MD, recalled that early in the U.S. pandemic, pediatricians felt a sense of relief that children appeared to be spared from severe COVID-19 disease. But, in just the past few weeks, a new syndrome has emerged. New York City has recorded more than 100 cases of what’s provisionally being called COVID-associated pediatric multisystem inflammatory syndrome. Dr. Conway and others are working with the Centers for Disease Control and Prevention to develop a case definition for the syndrome, first reported by pediatricians in Italy and the United Kingdom.
“We’re trying to get the word out to general pediatricians as to the common signs and symptoms that should prompt parents to bring their children in for medical care,” according to Dr. Conway, chief of pediatric critical care medicine and vice-chair of pediatrics at Jacobi Medical Center in New York.
Ninety percent of affected children have abdominal symptoms early on, including abdominal pain, diarrhea, emesis, or enteritis upon imaging. A nondescript rash, headache, conjunctivitis, and irritability are common, cough much less so – under 25%.
“The thought is that if any one of these is associated with a fever lasting more than 4 days, we suggest these children be brought in and seen by a pediatrician. We don’t have a formal guideline – we’re working on that – but basically the current recommendation is to screen them initially with a CBC with differential, a chem 10, and liver function tests, but also to look for inflammatory markers that we see in our COVID patients. We’ve been quite surprised: These patients have C-reactive proteins of about 240 mg/L on average, ferritin is quite high at around 1,200 ng/mL, and d-dimers of 2,300 ng/mL. We’ve also found very high brain natriuretic peptides and troponins in these patients,” according to Dr. Conway.
Analogies have been made between this COVID-19 pediatric syndrome and Kawasaki disease. Dr. Conway is unconvinced.
“This is quite different from Kawasaki in that these children are usually thrombocytopenic and usually present with DIC [disseminated intravascular coagulation], and the d-dimers are extraordinarily high, compared to what we’re used to seeing in pediatric patients,” he said.
Symptomatic children with laboratory red flags should be hospitalized. Most of the affected New York City children have recovered after 5 or 6 days in the pediatric ICU with empiric treatment using intravenous immunoglobulin (IVIG), corticosteroids, and/or interleukin-6 inhibitors. However, five recent deaths are now under study.
Dr. Yealy commented that this new pediatric syndrome is “really interesting,” but to date, it affects only a very small percentage of children, and children overall have been much less affected by the pandemic than are adults.
“The populations being disproportionately impacted are the elderly, the elderly, the elderly, and then other vulnerable populations, particularly congregants and the poor,” he said. “At my site, three-quarters of the patients coming in are either patients at assisted-living facilities or work at one of those congregant facilities.”
The pandemic’s impact on medical education
In many hospitals, grand rounds are being done virtually via videoconferencing, often with attendant challenges in asking and answering questions. Hospital patient volumes are diminished. Medical students aren’t coming in to do clinical rotations. Medical students and residents can’t travel to interview for future residencies or jobs.
“It’s affecting education across all of the components of medicine. It’s hard to say how long this pandemic is going to last. We’re all trying to be innovative in using online tools, but I believe it’s going to have a long-lasting effect on our education system,” Dr. Marcolini predicted.
Remote interface while working from home has become frustrating, especially during peak Internet use hours.
“It’s staggering how slow my home system has become in comparison to what’s wired at work. Now many times when you try to get into your work system from home, you time out while you’re waiting for the next piece of information to come across,” Dr. Kaplan commented.
All panel participants reported having no financial conflicts of interest.
*Correction, 5/15/20: An earlier version of this article misstated the name of the American College of Emergency Physicians.)
according to an expert panel on unanticipated consequences of pandemic care hosted by the presidents of the Society of Critical Care Medicine and the American College of Emergency Physicians.*
“At the peak of exposure to COVID-19 illness or infection, ED volumes in my system, which are really not much different from others across the country, were cut in half, if not more. And those changes happened across virtually every form of ED presentation, from the highest acuity to the lowest. We’re now beyond our highest level of exposure to COVID-19 clinically symptomatic patients in western Pennsylvania, but that recovery in volume hasn’t occurred yet, although there are some embers,” explained Donald M. Yealy, MD, professor and chair of the department of emergency medicine at the University of Pittsburgh.
He and other panelists also addressed some of the other unanticipated developments in the COVID-19 pandemic, including a recently recognized childhood manifestation called for now COVID-associated pediatric multisystem inflammatory syndrome, an anticipated massive second wave of non-COVID patients expected to present late to EDs and primary care clinics after having avoided needed medical care out of fear of infection, and the pandemic’s negative impact upon medical education.
Who’s not showing up in the ED
Dr. Yealy said that across the country, the number of patients arriving in EDs with acute ST-elevation MI, stroke, trauma, and other highest-acuity presentations is down substantially. But the volume of patients with more routine, bread-and-butter conditions typically seen in EDs is down even more.
“You might say, if I was designing from the insurance side, this is exactly what I’d hope for. I’ve heard that some people on the insurance-only side of the business really are experiencing a pretty good deal right now: They’re collecting premiums and not having to pay out on the ED or hospital side,” he said.
Tweaking the public health message on seeking medical care
“One of the unanticipated casualties of the pandemic are the patients who don’t have it. It will take a whole lot of work and coordinated effort to re-engage with those patients,” predicted SCCM President Lewis J. Kaplan, MD, professor of surgery at the University of Pennsylvania, Philadelphia.
Evie G. Marcolini, MD, described what she believes is necessary now: “We need to have a big focus on getting the word out to the public that acute MI, stroke, and other acute injuries are still a time-sensitive problem and they warrant at least a call to their physician or consideration of coming in to the ED.
“I think when we started out, we were telling people, ‘Don’t come in.’ Now we’re trying to dial it back a little bit and say, ‘Listen, there are things you really do need to come in for. And we will keep you safe,’” said Dr. Marcolini, an emergency medicine and neurocritical care specialist at Dartmouth-Hitchcock Medical Center, Hanover, N.H.
“It is safe,” Dr. Yealy agreed. “The safest place in the world to be right now is the ED. Everybody’s cordoned off. There’s way more PPE [personal protective equipment]. There’s a level of precision now that should have existed but never did in our previous influenza seasons. So we have something very unique to offer, and we can put people’s minds at rest.”
He spoke of a coming “tsunami of untreated illness.”
“My concern is there is a significant subset of people who are not only eschewing ED care but staying away from their primary care provider. My fear is that we’re not as well aware of this,” he said. “Together with our primary care partners, we have to figure out ways to reach the people who are ignoring illnesses and injuries that they’re making long-term decisions about without realizing it. We have to find a way to reach those people and say it’s okay to reach for care.”
SCCM Immediate Past President Heatherlee Bailey, MD, also sees a problematic looming wave.
“I’m quite concerned about the coming second wave of non-COVID patients who’ve sat home with their worsening renal failure that’s gone from 2 to 5 because they’ve been taking a lot of NSAIDs, or the individual who’s had several TIAs that self-resolved, and we’ve missed an opportunity to prevent some significant disease. At some point they’re going to come back, and we need to figure out how to get these individuals hooked up with care, either through the ED or with their primary care provider, to prevent these potential bad outcomes,” said Dr. Bailey of the Durham (N.C.) Veterans Affairs Medical Center.
Interim guidance for pediatricians on an alarming new syndrome
Edward E. Conway Jr., MD, recalled that early in the U.S. pandemic, pediatricians felt a sense of relief that children appeared to be spared from severe COVID-19 disease. But, in just the past few weeks, a new syndrome has emerged. New York City has recorded more than 100 cases of what’s provisionally being called COVID-associated pediatric multisystem inflammatory syndrome. Dr. Conway and others are working with the Centers for Disease Control and Prevention to develop a case definition for the syndrome, first reported by pediatricians in Italy and the United Kingdom.
“We’re trying to get the word out to general pediatricians as to the common signs and symptoms that should prompt parents to bring their children in for medical care,” according to Dr. Conway, chief of pediatric critical care medicine and vice-chair of pediatrics at Jacobi Medical Center in New York.
Ninety percent of affected children have abdominal symptoms early on, including abdominal pain, diarrhea, emesis, or enteritis upon imaging. A nondescript rash, headache, conjunctivitis, and irritability are common, cough much less so – under 25%.
“The thought is that if any one of these is associated with a fever lasting more than 4 days, we suggest these children be brought in and seen by a pediatrician. We don’t have a formal guideline – we’re working on that – but basically the current recommendation is to screen them initially with a CBC with differential, a chem 10, and liver function tests, but also to look for inflammatory markers that we see in our COVID patients. We’ve been quite surprised: These patients have C-reactive proteins of about 240 mg/L on average, ferritin is quite high at around 1,200 ng/mL, and d-dimers of 2,300 ng/mL. We’ve also found very high brain natriuretic peptides and troponins in these patients,” according to Dr. Conway.
Analogies have been made between this COVID-19 pediatric syndrome and Kawasaki disease. Dr. Conway is unconvinced.
“This is quite different from Kawasaki in that these children are usually thrombocytopenic and usually present with DIC [disseminated intravascular coagulation], and the d-dimers are extraordinarily high, compared to what we’re used to seeing in pediatric patients,” he said.
Symptomatic children with laboratory red flags should be hospitalized. Most of the affected New York City children have recovered after 5 or 6 days in the pediatric ICU with empiric treatment using intravenous immunoglobulin (IVIG), corticosteroids, and/or interleukin-6 inhibitors. However, five recent deaths are now under study.
Dr. Yealy commented that this new pediatric syndrome is “really interesting,” but to date, it affects only a very small percentage of children, and children overall have been much less affected by the pandemic than are adults.
“The populations being disproportionately impacted are the elderly, the elderly, the elderly, and then other vulnerable populations, particularly congregants and the poor,” he said. “At my site, three-quarters of the patients coming in are either patients at assisted-living facilities or work at one of those congregant facilities.”
The pandemic’s impact on medical education
In many hospitals, grand rounds are being done virtually via videoconferencing, often with attendant challenges in asking and answering questions. Hospital patient volumes are diminished. Medical students aren’t coming in to do clinical rotations. Medical students and residents can’t travel to interview for future residencies or jobs.
“It’s affecting education across all of the components of medicine. It’s hard to say how long this pandemic is going to last. We’re all trying to be innovative in using online tools, but I believe it’s going to have a long-lasting effect on our education system,” Dr. Marcolini predicted.
Remote interface while working from home has become frustrating, especially during peak Internet use hours.
“It’s staggering how slow my home system has become in comparison to what’s wired at work. Now many times when you try to get into your work system from home, you time out while you’re waiting for the next piece of information to come across,” Dr. Kaplan commented.
All panel participants reported having no financial conflicts of interest.
*Correction, 5/15/20: An earlier version of this article misstated the name of the American College of Emergency Physicians.)
Modify risk factors to manage ICU delirium in patients with COVID-19
, and a bedside risk management strategy based on modifiable risk factors can help prevent lingering effects on cognition, according to an article published in Critical Care.
Several factors can contribute to an increased risk of ICU delirium in COVID-19 patients, wrote Katarzyna Kotfis, MD, of Pomeranian Medical University, Szczecin, Poland, and colleagues.
“In patients with COVID-19, delirium may be a manifestation of direct central nervous system invasion, induction of CNS inflammatory mediators, a secondary effect of other organ system failure, an effect of sedative strategies, prolonged mechanical ventilation time, or environmental factors, including social isolation,” they said.
Delirium in the context of COVID-19 can mean an early sign of infection, so patients should be screened using dedicated psychometric tools, the researchers wrote. Also, COVID-19 has been shown to cause pneumonia in elderly patients, who are at high risk for severe pulmonary disease related to COVID-19 and for ICU delirium generally, they said.
In addition, don’t underestimate the impact of social isolation created by quarantines, the researchers said.
“What is needed now, is not only high-quality ICU care, concentrated on providing adequate respiratory support to critically ill patients, but an identification of the source and degree of mental and spiritual suffering of patients as well as their families to provide the most ethical and person-centered care during this humanitarian crisis,” they emphasized. However, they acknowledged that nonpharmacologic interventions such as mobility outside the ICU room and interactions with family members are limited by the COVID-19 situation.
The researchers noted several mechanisms by which the COVID-19 virus may cause brain damage, including through the dysfunction of the renin-angiotensin system.
“Inflammatory response of the CNS to viral infection seems to be another important reason for poor neurological outcome and occurrence of delirium,” in COVID-19 patients, they said.
As for risk-reduction strategies, the researchers noted that “delirium in mechanically ventilated patients can be reduced dramatically to 50% using a culture of lighter sedation and mobilization via the implementation of the safety bundle called the ABCDEFs promoted by the Society of Critical Care Medicine in their ICU Liberation Collaborative,” although COVID-19 isolation is a barrier, they said.
The ABCDEF bundle consists of Assessment of pain, Both spontaneous awakening trials and spontaneous breathing trials, Choice of sedation, Delirium (hyperactive or hypoactive), Early mobility, and Family presence; all of which are challenging in the COVID-19 environment, the researchers said.
They advised implementing easy screening methods for delirium to reduce the burden on medical staff, and emphasized the importance of regular patient orientation, despite social separation from family and caregivers.
“No drugs can be recommended for the prevention or treatment of ICU delirium other than avoidance of overuse of potent psychoactive agents like sedatives and neuromuscular blockers (NMB) unless patients absolutely require such management,” they added.
“Delirium is so common and so hard to manage in the COVID-19 population,” Mangala Narasimhan, DO, of Northwell Health in New Hyde Park, N.Y., said in an interview. Delirium is impacted by many sources including a viral encephalopathy, the amount and duration of sedation medications, and prolonged intubation and hypoxemia, she said. “Managing the delirium allows you to wake the patient up successfully and without a lot of discoordination. This will help with weaning,” she noted. Barriers to delirium management for COVID-19 patients include the length of time on a ventilator, as well as amount of sedatives and paralytics, and the added issues of renal insufficiency, she noted. “How they can be addressed is thoughtful plans on the addition of long-term sedation for withdrawal symptoms, and anxiolytics for the profound anxiety associated with arousal from this type of sedation on ventilators, she said. The take-home message for clinicians is the need to perform weaning trials to manage delirium in the ICU. “We have to combat this delirium in order to be successful in taking these patients off of ventilators,” she said. Dr. Narasimhan added that more research is needed on areas including drug-to-drug interactions, duration of efficacy of various drugs, and how the virus affects the brain.
“Adherence to the ABCDEF bundle can reduce the incidence of delirium, from approximately 75% of mechanically ventilated patients to 50% or less,” David L. Bowton, MD, of Wake Forest Baptist Health in Winston-Salem, N.C., said in an interview.
“Importantly, in most studies, bundle adherence reduces mortality and ICU length of stay and lowers the total cost of care. However, isolation of patients and protection of staff, visitor restrictions, and potentially stressed staffing will likely alter how most institutions approach bundle compliance,” he said. “Gathering input from infection control clinicians and bedside providers from multiple disciplines that consider these factors to critically examine current bundle procedures and workflow will be essential to the creation and/or revision of bundle processes of care that maintain the integrity of the ABCDEF bundle yet preserve staff, patient, and family safety,” he said.
“We did not have strong evidence to suggest an optimal approach to treating delirium before the advent of the COVID-19 pandemic, so I do not believe we know what the best approach is in the current environment,” Dr. Bowton added. “Further, vigilance will be necessary to ensure that altered consciousness or cognition is ICU delirium and not attributable to another cause such as drug withdrawal, drug adverse effect, or primary central nervous system infection or immune response that mandates specific therapy,” he emphasized.
For clinicians, “this study reminds us of the importance of the ABCDEF bundle to improve outcomes of critical illness,” said Dr. Bowton. “It highlights the difficulties of providing frequent reassessment of pain, comfort, reassurance, and reorientation to critically ill patients. To me, it underscores the importance of each institution critically examining staffing needs and staffing roles to mitigate these difficulties and to explore novel methods of maintaining staff-patient and family-patient interactions to enhance compliance with all elements of the ABCDEF bundle while maintaining the safety of staff and families.”
Dr. Bowton added, “When necessary, explicit modifications to existing ABCDEF bundles should be developed and disseminated to provide realistic, readily understood guidance to achieve the best possible compliance with each bundle element. One potentially underrecognized issue will be the large, hopefully temporary, number of people requiring post–critical illness rehabilitation and mental health services,” he said. “In many regions these services are already underfunded and ill-equipped to handle an increased demand for these services,” he noted.
Additional research is needed in many areas, said Dr. Bowton. “While compliance with the ABCDEF bundle decreases the incidence and duration of delirium, decreases ICU length of stay, decreases duration of mechanical ventilation, and improves mortality, many questions remain. Individual elements of the bundle have been inconsistently associated with improved outcomes,” he said. “What is the relative importance of specific elements and what are the mechanisms by which they improve outcomes?” he asked. “We still do not know how to best achieve physical/functional recovery following critical illness, which, in light of these authors’ studies relating persisting physical debility to depression (Lancet Respir Med. 2014; 2[5]:369-79), may be a key component to improving long-term outcomes,” he said.
The study received no specific funding, although several coauthors disclosed grants from agencies including the National Center for Advancing Translational Sciences, National Institute of General Medical Sciences, National Heart, Lung, and Blood Institute, and National Institute on Aging. Dr. Narasimhan and Dr. Bowton had no financial conflicts to disclose.
SOURCE: Kotfis K et al. Critical Care. 2020 Apr 28. doi: 10.1186/s13054-020-02882-x.
, and a bedside risk management strategy based on modifiable risk factors can help prevent lingering effects on cognition, according to an article published in Critical Care.
Several factors can contribute to an increased risk of ICU delirium in COVID-19 patients, wrote Katarzyna Kotfis, MD, of Pomeranian Medical University, Szczecin, Poland, and colleagues.
“In patients with COVID-19, delirium may be a manifestation of direct central nervous system invasion, induction of CNS inflammatory mediators, a secondary effect of other organ system failure, an effect of sedative strategies, prolonged mechanical ventilation time, or environmental factors, including social isolation,” they said.
Delirium in the context of COVID-19 can mean an early sign of infection, so patients should be screened using dedicated psychometric tools, the researchers wrote. Also, COVID-19 has been shown to cause pneumonia in elderly patients, who are at high risk for severe pulmonary disease related to COVID-19 and for ICU delirium generally, they said.
In addition, don’t underestimate the impact of social isolation created by quarantines, the researchers said.
“What is needed now, is not only high-quality ICU care, concentrated on providing adequate respiratory support to critically ill patients, but an identification of the source and degree of mental and spiritual suffering of patients as well as their families to provide the most ethical and person-centered care during this humanitarian crisis,” they emphasized. However, they acknowledged that nonpharmacologic interventions such as mobility outside the ICU room and interactions with family members are limited by the COVID-19 situation.
The researchers noted several mechanisms by which the COVID-19 virus may cause brain damage, including through the dysfunction of the renin-angiotensin system.
“Inflammatory response of the CNS to viral infection seems to be another important reason for poor neurological outcome and occurrence of delirium,” in COVID-19 patients, they said.
As for risk-reduction strategies, the researchers noted that “delirium in mechanically ventilated patients can be reduced dramatically to 50% using a culture of lighter sedation and mobilization via the implementation of the safety bundle called the ABCDEFs promoted by the Society of Critical Care Medicine in their ICU Liberation Collaborative,” although COVID-19 isolation is a barrier, they said.
The ABCDEF bundle consists of Assessment of pain, Both spontaneous awakening trials and spontaneous breathing trials, Choice of sedation, Delirium (hyperactive or hypoactive), Early mobility, and Family presence; all of which are challenging in the COVID-19 environment, the researchers said.
They advised implementing easy screening methods for delirium to reduce the burden on medical staff, and emphasized the importance of regular patient orientation, despite social separation from family and caregivers.
“No drugs can be recommended for the prevention or treatment of ICU delirium other than avoidance of overuse of potent psychoactive agents like sedatives and neuromuscular blockers (NMB) unless patients absolutely require such management,” they added.
“Delirium is so common and so hard to manage in the COVID-19 population,” Mangala Narasimhan, DO, of Northwell Health in New Hyde Park, N.Y., said in an interview. Delirium is impacted by many sources including a viral encephalopathy, the amount and duration of sedation medications, and prolonged intubation and hypoxemia, she said. “Managing the delirium allows you to wake the patient up successfully and without a lot of discoordination. This will help with weaning,” she noted. Barriers to delirium management for COVID-19 patients include the length of time on a ventilator, as well as amount of sedatives and paralytics, and the added issues of renal insufficiency, she noted. “How they can be addressed is thoughtful plans on the addition of long-term sedation for withdrawal symptoms, and anxiolytics for the profound anxiety associated with arousal from this type of sedation on ventilators, she said. The take-home message for clinicians is the need to perform weaning trials to manage delirium in the ICU. “We have to combat this delirium in order to be successful in taking these patients off of ventilators,” she said. Dr. Narasimhan added that more research is needed on areas including drug-to-drug interactions, duration of efficacy of various drugs, and how the virus affects the brain.
“Adherence to the ABCDEF bundle can reduce the incidence of delirium, from approximately 75% of mechanically ventilated patients to 50% or less,” David L. Bowton, MD, of Wake Forest Baptist Health in Winston-Salem, N.C., said in an interview.
“Importantly, in most studies, bundle adherence reduces mortality and ICU length of stay and lowers the total cost of care. However, isolation of patients and protection of staff, visitor restrictions, and potentially stressed staffing will likely alter how most institutions approach bundle compliance,” he said. “Gathering input from infection control clinicians and bedside providers from multiple disciplines that consider these factors to critically examine current bundle procedures and workflow will be essential to the creation and/or revision of bundle processes of care that maintain the integrity of the ABCDEF bundle yet preserve staff, patient, and family safety,” he said.
“We did not have strong evidence to suggest an optimal approach to treating delirium before the advent of the COVID-19 pandemic, so I do not believe we know what the best approach is in the current environment,” Dr. Bowton added. “Further, vigilance will be necessary to ensure that altered consciousness or cognition is ICU delirium and not attributable to another cause such as drug withdrawal, drug adverse effect, or primary central nervous system infection or immune response that mandates specific therapy,” he emphasized.
For clinicians, “this study reminds us of the importance of the ABCDEF bundle to improve outcomes of critical illness,” said Dr. Bowton. “It highlights the difficulties of providing frequent reassessment of pain, comfort, reassurance, and reorientation to critically ill patients. To me, it underscores the importance of each institution critically examining staffing needs and staffing roles to mitigate these difficulties and to explore novel methods of maintaining staff-patient and family-patient interactions to enhance compliance with all elements of the ABCDEF bundle while maintaining the safety of staff and families.”
Dr. Bowton added, “When necessary, explicit modifications to existing ABCDEF bundles should be developed and disseminated to provide realistic, readily understood guidance to achieve the best possible compliance with each bundle element. One potentially underrecognized issue will be the large, hopefully temporary, number of people requiring post–critical illness rehabilitation and mental health services,” he said. “In many regions these services are already underfunded and ill-equipped to handle an increased demand for these services,” he noted.
Additional research is needed in many areas, said Dr. Bowton. “While compliance with the ABCDEF bundle decreases the incidence and duration of delirium, decreases ICU length of stay, decreases duration of mechanical ventilation, and improves mortality, many questions remain. Individual elements of the bundle have been inconsistently associated with improved outcomes,” he said. “What is the relative importance of specific elements and what are the mechanisms by which they improve outcomes?” he asked. “We still do not know how to best achieve physical/functional recovery following critical illness, which, in light of these authors’ studies relating persisting physical debility to depression (Lancet Respir Med. 2014; 2[5]:369-79), may be a key component to improving long-term outcomes,” he said.
The study received no specific funding, although several coauthors disclosed grants from agencies including the National Center for Advancing Translational Sciences, National Institute of General Medical Sciences, National Heart, Lung, and Blood Institute, and National Institute on Aging. Dr. Narasimhan and Dr. Bowton had no financial conflicts to disclose.
SOURCE: Kotfis K et al. Critical Care. 2020 Apr 28. doi: 10.1186/s13054-020-02882-x.
, and a bedside risk management strategy based on modifiable risk factors can help prevent lingering effects on cognition, according to an article published in Critical Care.
Several factors can contribute to an increased risk of ICU delirium in COVID-19 patients, wrote Katarzyna Kotfis, MD, of Pomeranian Medical University, Szczecin, Poland, and colleagues.
“In patients with COVID-19, delirium may be a manifestation of direct central nervous system invasion, induction of CNS inflammatory mediators, a secondary effect of other organ system failure, an effect of sedative strategies, prolonged mechanical ventilation time, or environmental factors, including social isolation,” they said.
Delirium in the context of COVID-19 can mean an early sign of infection, so patients should be screened using dedicated psychometric tools, the researchers wrote. Also, COVID-19 has been shown to cause pneumonia in elderly patients, who are at high risk for severe pulmonary disease related to COVID-19 and for ICU delirium generally, they said.
In addition, don’t underestimate the impact of social isolation created by quarantines, the researchers said.
“What is needed now, is not only high-quality ICU care, concentrated on providing adequate respiratory support to critically ill patients, but an identification of the source and degree of mental and spiritual suffering of patients as well as their families to provide the most ethical and person-centered care during this humanitarian crisis,” they emphasized. However, they acknowledged that nonpharmacologic interventions such as mobility outside the ICU room and interactions with family members are limited by the COVID-19 situation.
The researchers noted several mechanisms by which the COVID-19 virus may cause brain damage, including through the dysfunction of the renin-angiotensin system.
“Inflammatory response of the CNS to viral infection seems to be another important reason for poor neurological outcome and occurrence of delirium,” in COVID-19 patients, they said.
As for risk-reduction strategies, the researchers noted that “delirium in mechanically ventilated patients can be reduced dramatically to 50% using a culture of lighter sedation and mobilization via the implementation of the safety bundle called the ABCDEFs promoted by the Society of Critical Care Medicine in their ICU Liberation Collaborative,” although COVID-19 isolation is a barrier, they said.
The ABCDEF bundle consists of Assessment of pain, Both spontaneous awakening trials and spontaneous breathing trials, Choice of sedation, Delirium (hyperactive or hypoactive), Early mobility, and Family presence; all of which are challenging in the COVID-19 environment, the researchers said.
They advised implementing easy screening methods for delirium to reduce the burden on medical staff, and emphasized the importance of regular patient orientation, despite social separation from family and caregivers.
“No drugs can be recommended for the prevention or treatment of ICU delirium other than avoidance of overuse of potent psychoactive agents like sedatives and neuromuscular blockers (NMB) unless patients absolutely require such management,” they added.
“Delirium is so common and so hard to manage in the COVID-19 population,” Mangala Narasimhan, DO, of Northwell Health in New Hyde Park, N.Y., said in an interview. Delirium is impacted by many sources including a viral encephalopathy, the amount and duration of sedation medications, and prolonged intubation and hypoxemia, she said. “Managing the delirium allows you to wake the patient up successfully and without a lot of discoordination. This will help with weaning,” she noted. Barriers to delirium management for COVID-19 patients include the length of time on a ventilator, as well as amount of sedatives and paralytics, and the added issues of renal insufficiency, she noted. “How they can be addressed is thoughtful plans on the addition of long-term sedation for withdrawal symptoms, and anxiolytics for the profound anxiety associated with arousal from this type of sedation on ventilators, she said. The take-home message for clinicians is the need to perform weaning trials to manage delirium in the ICU. “We have to combat this delirium in order to be successful in taking these patients off of ventilators,” she said. Dr. Narasimhan added that more research is needed on areas including drug-to-drug interactions, duration of efficacy of various drugs, and how the virus affects the brain.
“Adherence to the ABCDEF bundle can reduce the incidence of delirium, from approximately 75% of mechanically ventilated patients to 50% or less,” David L. Bowton, MD, of Wake Forest Baptist Health in Winston-Salem, N.C., said in an interview.
“Importantly, in most studies, bundle adherence reduces mortality and ICU length of stay and lowers the total cost of care. However, isolation of patients and protection of staff, visitor restrictions, and potentially stressed staffing will likely alter how most institutions approach bundle compliance,” he said. “Gathering input from infection control clinicians and bedside providers from multiple disciplines that consider these factors to critically examine current bundle procedures and workflow will be essential to the creation and/or revision of bundle processes of care that maintain the integrity of the ABCDEF bundle yet preserve staff, patient, and family safety,” he said.
“We did not have strong evidence to suggest an optimal approach to treating delirium before the advent of the COVID-19 pandemic, so I do not believe we know what the best approach is in the current environment,” Dr. Bowton added. “Further, vigilance will be necessary to ensure that altered consciousness or cognition is ICU delirium and not attributable to another cause such as drug withdrawal, drug adverse effect, or primary central nervous system infection or immune response that mandates specific therapy,” he emphasized.
For clinicians, “this study reminds us of the importance of the ABCDEF bundle to improve outcomes of critical illness,” said Dr. Bowton. “It highlights the difficulties of providing frequent reassessment of pain, comfort, reassurance, and reorientation to critically ill patients. To me, it underscores the importance of each institution critically examining staffing needs and staffing roles to mitigate these difficulties and to explore novel methods of maintaining staff-patient and family-patient interactions to enhance compliance with all elements of the ABCDEF bundle while maintaining the safety of staff and families.”
Dr. Bowton added, “When necessary, explicit modifications to existing ABCDEF bundles should be developed and disseminated to provide realistic, readily understood guidance to achieve the best possible compliance with each bundle element. One potentially underrecognized issue will be the large, hopefully temporary, number of people requiring post–critical illness rehabilitation and mental health services,” he said. “In many regions these services are already underfunded and ill-equipped to handle an increased demand for these services,” he noted.
Additional research is needed in many areas, said Dr. Bowton. “While compliance with the ABCDEF bundle decreases the incidence and duration of delirium, decreases ICU length of stay, decreases duration of mechanical ventilation, and improves mortality, many questions remain. Individual elements of the bundle have been inconsistently associated with improved outcomes,” he said. “What is the relative importance of specific elements and what are the mechanisms by which they improve outcomes?” he asked. “We still do not know how to best achieve physical/functional recovery following critical illness, which, in light of these authors’ studies relating persisting physical debility to depression (Lancet Respir Med. 2014; 2[5]:369-79), may be a key component to improving long-term outcomes,” he said.
The study received no specific funding, although several coauthors disclosed grants from agencies including the National Center for Advancing Translational Sciences, National Institute of General Medical Sciences, National Heart, Lung, and Blood Institute, and National Institute on Aging. Dr. Narasimhan and Dr. Bowton had no financial conflicts to disclose.
SOURCE: Kotfis K et al. Critical Care. 2020 Apr 28. doi: 10.1186/s13054-020-02882-x.
FROM CRITICAL CARE
How to expand the APP role in a crisis
An opportunity to better appreciate the value of PAs, NPs
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
An opportunity to better appreciate the value of PAs, NPs
An opportunity to better appreciate the value of PAs, NPs
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
With life in the balance, a pediatric palliative care program expands its work to adults
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
Volunteering during the pandemic: What doctors need to know
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
Pandemic-related stress rising among ICU clinicians
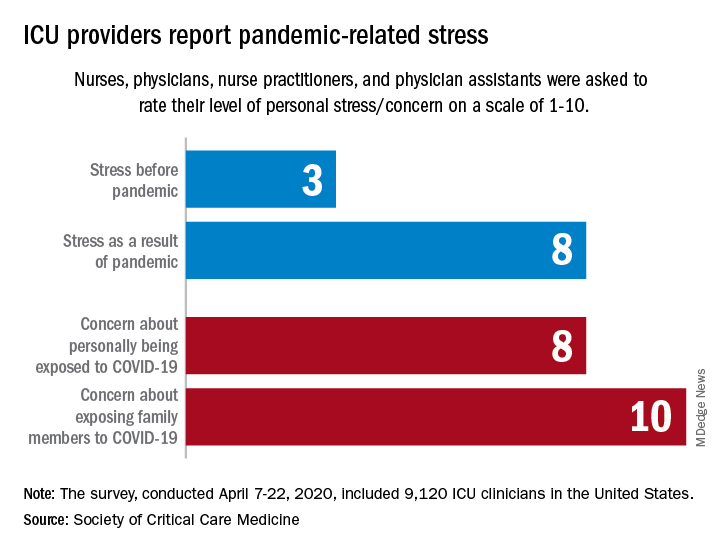
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.
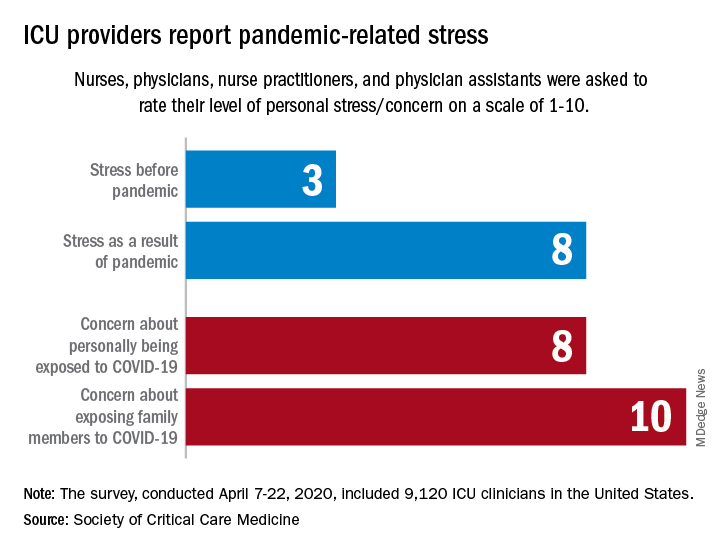
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.
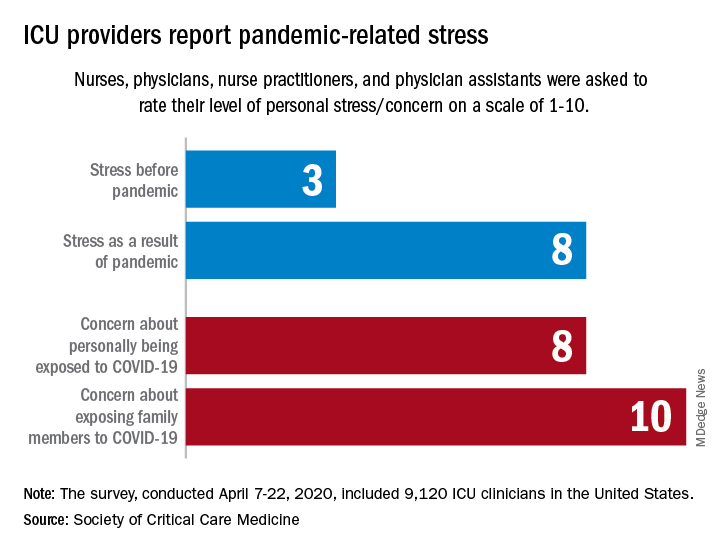
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.






















