User login
Sepsis patients with hypothermia face greater mortality risk
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
POPCoRN network mobilizes pediatric capacity during pandemic
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Med-Peds hospitalists were an organizing force
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Volunteer surgeon describes working at a New York hospital

In an April 18 Twitter post, Dr. Salles wrote that her unit had experienced three code blues and two deaths in a single night.
“I don’t know how many times I’ve called to tell someone their loved one has died,” she wrote in the post. “I had to do it again last night. ... Of the five patients I’ve personally been responsible for in the past two nights, two have come so close to dying that we called a code blue. That means 40% of my patients have coded. Never in my life has anything close to that happened,” she continued in the thread.
Dr. Salles, a minimally invasive and bariatric surgeon and scholar in residence at Stanford (Calif.) University, headed to New York in mid-April to assist with COVID-19 treatment efforts. Before the trip, she collected as many supplies and as much personal protective equipment as she could acquire, some of which were donated by Good Samaritans. On her first day as a volunteer, Dr. Salles recounted the stark differences between what she is used to seeing and her new environment and the novel challenges she has encountered in New York.
“Things that were not normal now seem normal,” she wrote in an April 15 Twitter post. “ICU patients in [a postanesthesia care unit] and Preop is the new normal. Patients satting in the 70s and 80s seems normal. ICU docs managing [continuous veno-venous hemodialysis] seems normal. Working with strangers seems normal. ... Obviously everyone walking around with barely any skin exposed is also the new normal.”
Similar to a “normal” ICU, new patients are admitted daily, Dr. Salles noted. However, the majority of those who leave the ICU do not go home, she wrote.
“Almost all of the ones who leave are doing so because they’ve died rather than getting better,” she wrote in the same April 19 Twitter thread. “There is a pervasive feeling of helplessness. ... The tools we are working with seem insufficient. For the sickest patients, there are no ventilator settings that seem to work, there are no medications that seem to help. I am not used to this.”
When patients are close to dying, health care workers do their best to connect the patient to loved ones through video calls, watching as family members say their last goodbyes through a screen, Dr. Salles detailed in a later post.
“Their voices cracked, and though they weren’t speaking English, I could hear their pain,” she wrote in an April 20 Twitter post. “For a moment, I imagined having to say goodbye to my mother this way. To not be able to be there, to not be able to hold her hand, to not be able to hug her. And I watched my colleague, who amazingly kept her composure until they had said everything they wanted to say. It was only after they hung up that I saw the tears well up in her eyes.”
But amid the dark days and bleak outcomes, Dr. Salles has found silver linings, humor, and gifts for which to be thankful.
“People are really generous,” she wrote in an April 15 post. “So many have offered to pay for transportation. Other docs in NY have offered to help me with supplies (and I am paying it forward). Grateful to you all!”
In another post, Dr. Salles joked that her “small head” makes it difficult to wear PPE.
“Wearing an N95 for hours really sucks,” she wrote. “It rides up, I pull it down. It digs into my cheeks, I pull it up. Repeat.”
The volunteer experience thus far has also made Dr. Salles question the future and worry about the mental health of her fellow health care professionals.
“The people who have been in NYC since the beginning of this, and those who work in Lombardy, Italy, and in Wuhan, China have faced loss for weeks to months,” she wrote in an April 18 Twitter post. “Not only do we not know when this will end, but it is likely that after it fades, it will come back in a second wave. I am lucky. I’m just a visitor here. I have the privilege to observe and learn and hopefully help, knowing I will be able to walk away. But what about those who can’t walk away? Social distancing is starting to work. But for healthcare workers, the ongoing devastation is very real. What is our long term plan?”
Dr. Salles expressed concern for health care workers who are witnessing “horrible things” with little time to process the experiences.
“It may be especially hard for those who are now working in specialties they are not used to, having to provide care they are not familiar with. They are all doing their best, but inevitably mistakes will be made, and they will likely blame themselves,” she wrote. “How do we best support them?”
Stay tuned for upcoming commentaries from Dr. Salles on her COVID-19 volunteer experience in New York City.

In an April 18 Twitter post, Dr. Salles wrote that her unit had experienced three code blues and two deaths in a single night.
“I don’t know how many times I’ve called to tell someone their loved one has died,” she wrote in the post. “I had to do it again last night. ... Of the five patients I’ve personally been responsible for in the past two nights, two have come so close to dying that we called a code blue. That means 40% of my patients have coded. Never in my life has anything close to that happened,” she continued in the thread.
Dr. Salles, a minimally invasive and bariatric surgeon and scholar in residence at Stanford (Calif.) University, headed to New York in mid-April to assist with COVID-19 treatment efforts. Before the trip, she collected as many supplies and as much personal protective equipment as she could acquire, some of which were donated by Good Samaritans. On her first day as a volunteer, Dr. Salles recounted the stark differences between what she is used to seeing and her new environment and the novel challenges she has encountered in New York.
“Things that were not normal now seem normal,” she wrote in an April 15 Twitter post. “ICU patients in [a postanesthesia care unit] and Preop is the new normal. Patients satting in the 70s and 80s seems normal. ICU docs managing [continuous veno-venous hemodialysis] seems normal. Working with strangers seems normal. ... Obviously everyone walking around with barely any skin exposed is also the new normal.”
Similar to a “normal” ICU, new patients are admitted daily, Dr. Salles noted. However, the majority of those who leave the ICU do not go home, she wrote.
“Almost all of the ones who leave are doing so because they’ve died rather than getting better,” she wrote in the same April 19 Twitter thread. “There is a pervasive feeling of helplessness. ... The tools we are working with seem insufficient. For the sickest patients, there are no ventilator settings that seem to work, there are no medications that seem to help. I am not used to this.”
When patients are close to dying, health care workers do their best to connect the patient to loved ones through video calls, watching as family members say their last goodbyes through a screen, Dr. Salles detailed in a later post.
“Their voices cracked, and though they weren’t speaking English, I could hear their pain,” she wrote in an April 20 Twitter post. “For a moment, I imagined having to say goodbye to my mother this way. To not be able to be there, to not be able to hold her hand, to not be able to hug her. And I watched my colleague, who amazingly kept her composure until they had said everything they wanted to say. It was only after they hung up that I saw the tears well up in her eyes.”
But amid the dark days and bleak outcomes, Dr. Salles has found silver linings, humor, and gifts for which to be thankful.
“People are really generous,” she wrote in an April 15 post. “So many have offered to pay for transportation. Other docs in NY have offered to help me with supplies (and I am paying it forward). Grateful to you all!”
In another post, Dr. Salles joked that her “small head” makes it difficult to wear PPE.
“Wearing an N95 for hours really sucks,” she wrote. “It rides up, I pull it down. It digs into my cheeks, I pull it up. Repeat.”
The volunteer experience thus far has also made Dr. Salles question the future and worry about the mental health of her fellow health care professionals.
“The people who have been in NYC since the beginning of this, and those who work in Lombardy, Italy, and in Wuhan, China have faced loss for weeks to months,” she wrote in an April 18 Twitter post. “Not only do we not know when this will end, but it is likely that after it fades, it will come back in a second wave. I am lucky. I’m just a visitor here. I have the privilege to observe and learn and hopefully help, knowing I will be able to walk away. But what about those who can’t walk away? Social distancing is starting to work. But for healthcare workers, the ongoing devastation is very real. What is our long term plan?”
Dr. Salles expressed concern for health care workers who are witnessing “horrible things” with little time to process the experiences.
“It may be especially hard for those who are now working in specialties they are not used to, having to provide care they are not familiar with. They are all doing their best, but inevitably mistakes will be made, and they will likely blame themselves,” she wrote. “How do we best support them?”
Stay tuned for upcoming commentaries from Dr. Salles on her COVID-19 volunteer experience in New York City.

In an April 18 Twitter post, Dr. Salles wrote that her unit had experienced three code blues and two deaths in a single night.
“I don’t know how many times I’ve called to tell someone their loved one has died,” she wrote in the post. “I had to do it again last night. ... Of the five patients I’ve personally been responsible for in the past two nights, two have come so close to dying that we called a code blue. That means 40% of my patients have coded. Never in my life has anything close to that happened,” she continued in the thread.
Dr. Salles, a minimally invasive and bariatric surgeon and scholar in residence at Stanford (Calif.) University, headed to New York in mid-April to assist with COVID-19 treatment efforts. Before the trip, she collected as many supplies and as much personal protective equipment as she could acquire, some of which were donated by Good Samaritans. On her first day as a volunteer, Dr. Salles recounted the stark differences between what she is used to seeing and her new environment and the novel challenges she has encountered in New York.
“Things that were not normal now seem normal,” she wrote in an April 15 Twitter post. “ICU patients in [a postanesthesia care unit] and Preop is the new normal. Patients satting in the 70s and 80s seems normal. ICU docs managing [continuous veno-venous hemodialysis] seems normal. Working with strangers seems normal. ... Obviously everyone walking around with barely any skin exposed is also the new normal.”
Similar to a “normal” ICU, new patients are admitted daily, Dr. Salles noted. However, the majority of those who leave the ICU do not go home, she wrote.
“Almost all of the ones who leave are doing so because they’ve died rather than getting better,” she wrote in the same April 19 Twitter thread. “There is a pervasive feeling of helplessness. ... The tools we are working with seem insufficient. For the sickest patients, there are no ventilator settings that seem to work, there are no medications that seem to help. I am not used to this.”
When patients are close to dying, health care workers do their best to connect the patient to loved ones through video calls, watching as family members say their last goodbyes through a screen, Dr. Salles detailed in a later post.
“Their voices cracked, and though they weren’t speaking English, I could hear their pain,” she wrote in an April 20 Twitter post. “For a moment, I imagined having to say goodbye to my mother this way. To not be able to be there, to not be able to hold her hand, to not be able to hug her. And I watched my colleague, who amazingly kept her composure until they had said everything they wanted to say. It was only after they hung up that I saw the tears well up in her eyes.”
But amid the dark days and bleak outcomes, Dr. Salles has found silver linings, humor, and gifts for which to be thankful.
“People are really generous,” she wrote in an April 15 post. “So many have offered to pay for transportation. Other docs in NY have offered to help me with supplies (and I am paying it forward). Grateful to you all!”
In another post, Dr. Salles joked that her “small head” makes it difficult to wear PPE.
“Wearing an N95 for hours really sucks,” she wrote. “It rides up, I pull it down. It digs into my cheeks, I pull it up. Repeat.”
The volunteer experience thus far has also made Dr. Salles question the future and worry about the mental health of her fellow health care professionals.
“The people who have been in NYC since the beginning of this, and those who work in Lombardy, Italy, and in Wuhan, China have faced loss for weeks to months,” she wrote in an April 18 Twitter post. “Not only do we not know when this will end, but it is likely that after it fades, it will come back in a second wave. I am lucky. I’m just a visitor here. I have the privilege to observe and learn and hopefully help, knowing I will be able to walk away. But what about those who can’t walk away? Social distancing is starting to work. But for healthcare workers, the ongoing devastation is very real. What is our long term plan?”
Dr. Salles expressed concern for health care workers who are witnessing “horrible things” with little time to process the experiences.
“It may be especially hard for those who are now working in specialties they are not used to, having to provide care they are not familiar with. They are all doing their best, but inevitably mistakes will be made, and they will likely blame themselves,” she wrote. “How do we best support them?”
Stay tuned for upcoming commentaries from Dr. Salles on her COVID-19 volunteer experience in New York City.
Rural ICU capacity could be strained by COVID-19
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
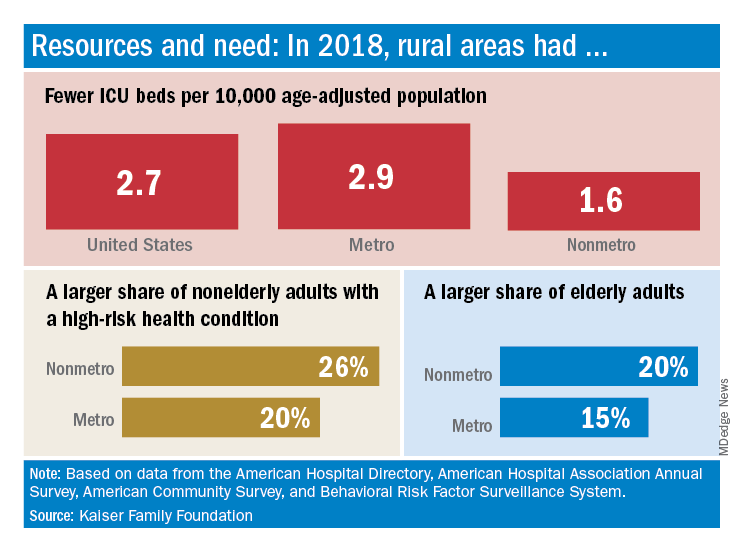
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
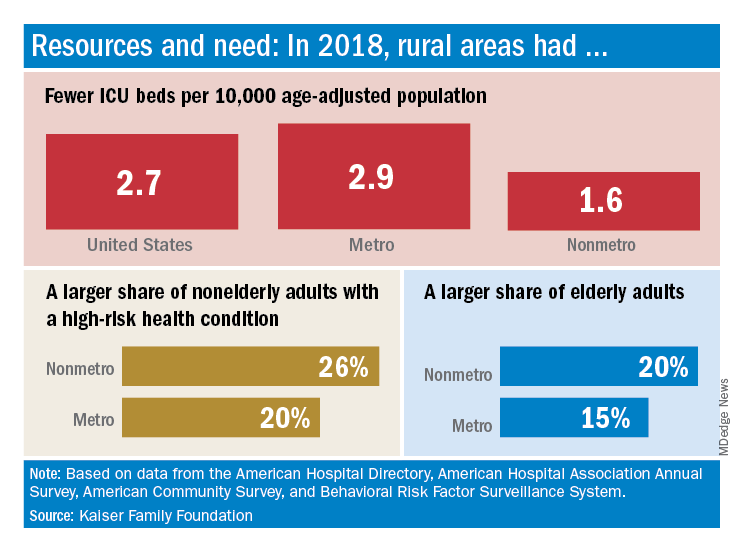
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
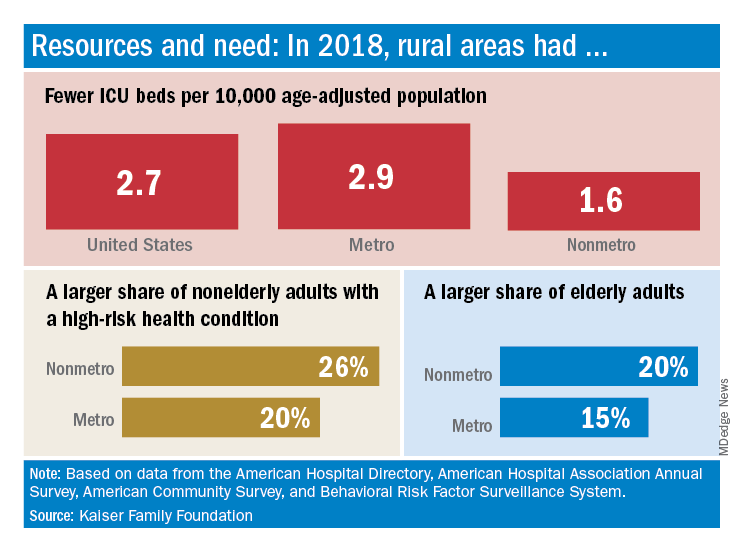
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
Seniors with COVID-19 show unusual symptoms, doctors say
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Get triage plans in place before COVID-19 surge hits, critical care experts say
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
FROM CHEST AND ANNALS OF THE AMERICAN THORACIC SOCIETY
Switching gears at high speed
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
Michigan hospitalists prepare for COVID-19 care
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
COVID-19: Managing resource crunch and ethical challenges
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
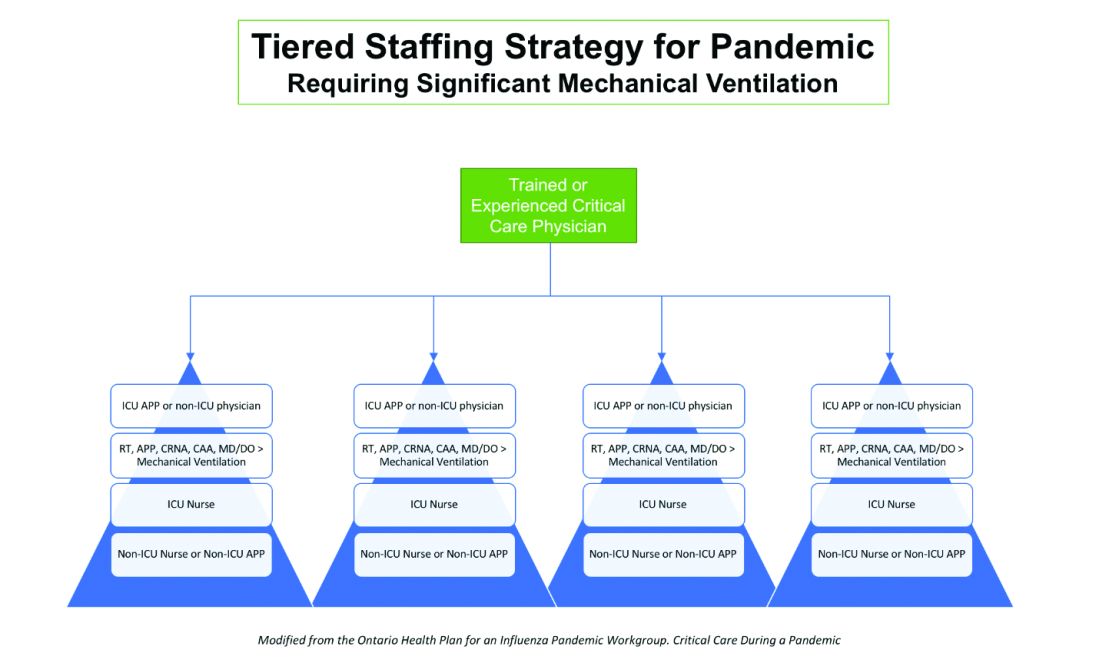
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.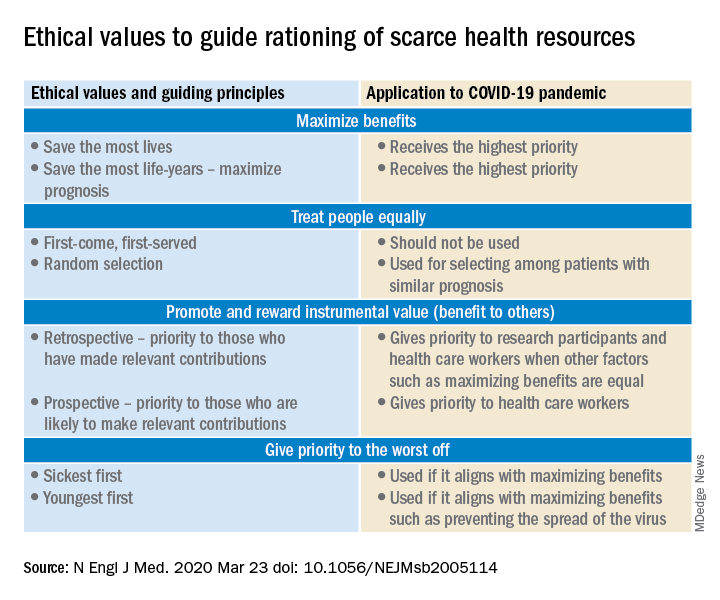
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
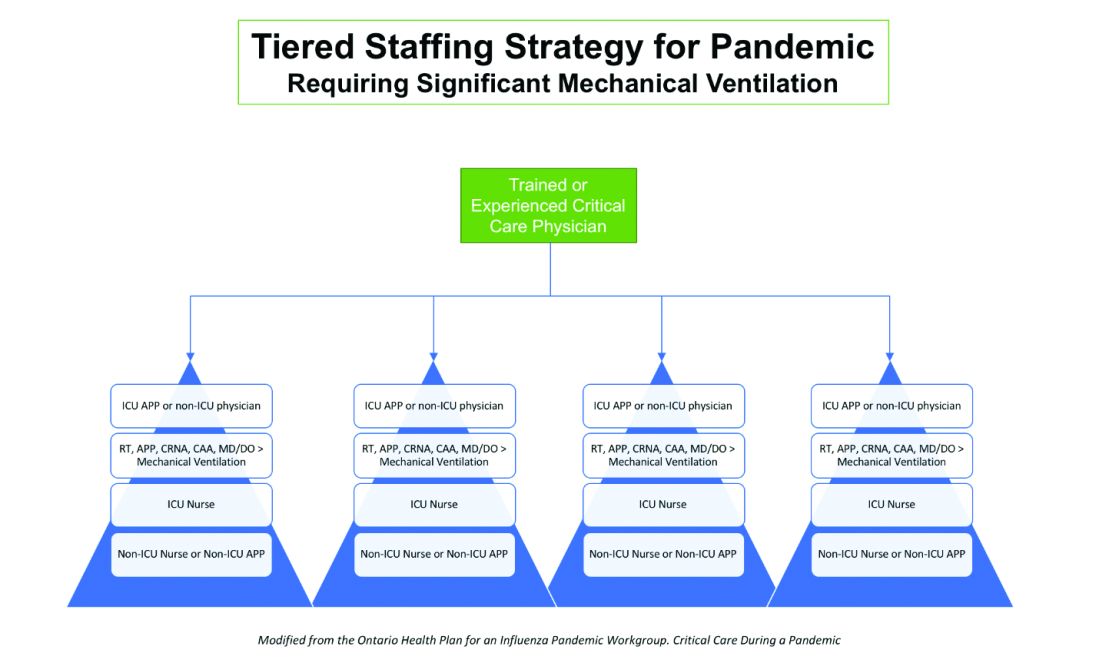
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.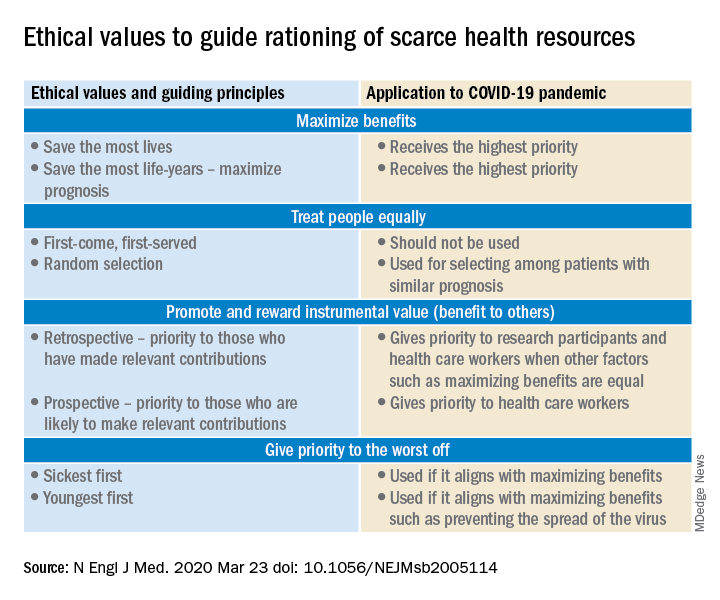
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
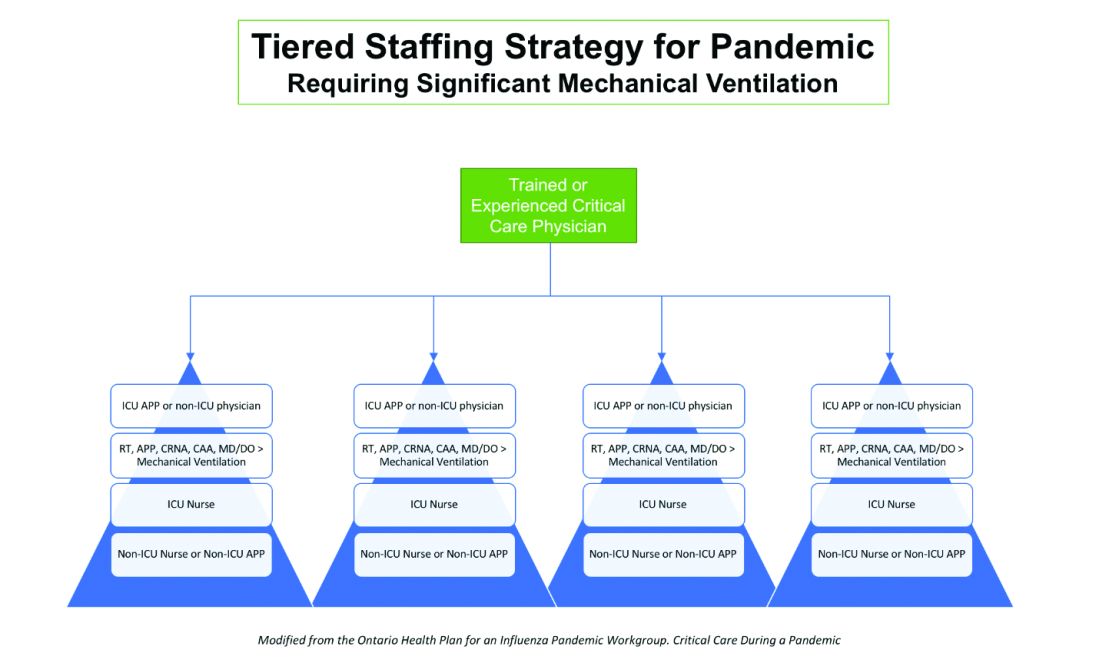
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.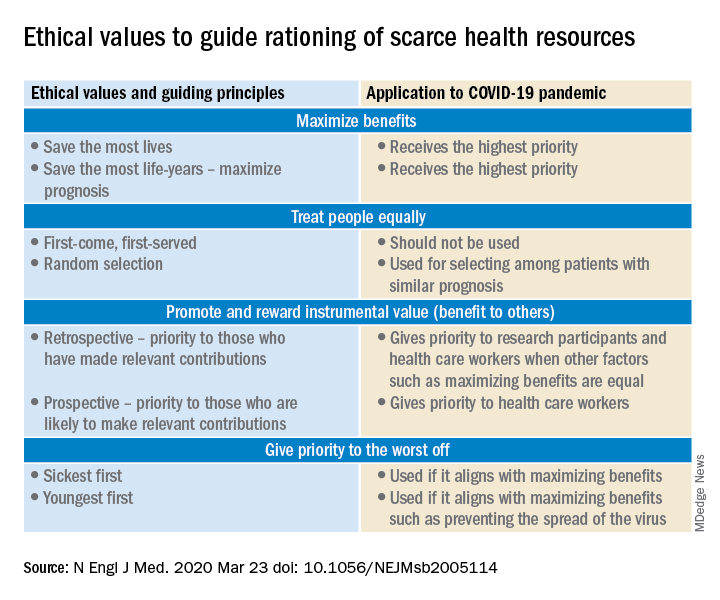
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 and surge capacity in U.S. hospitals
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 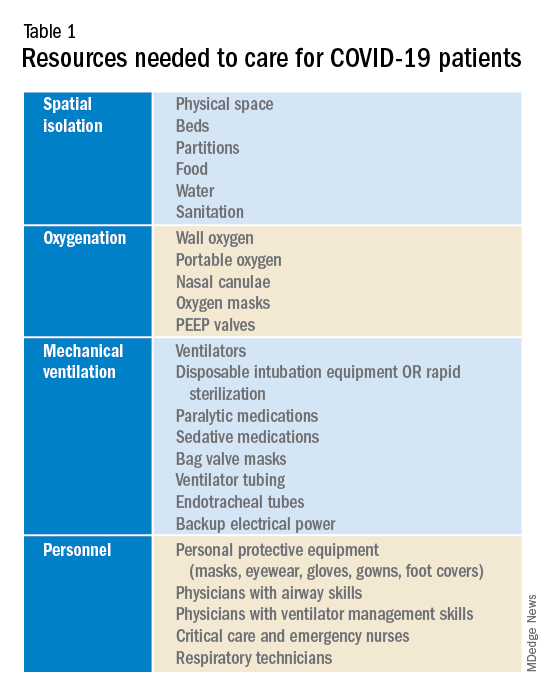
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
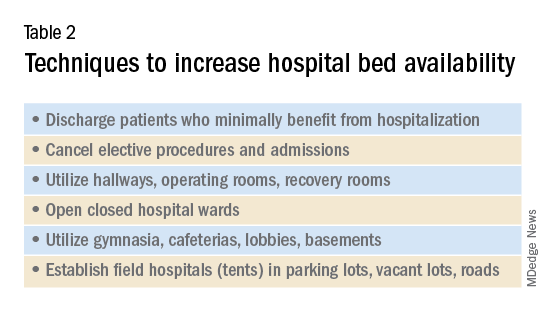
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 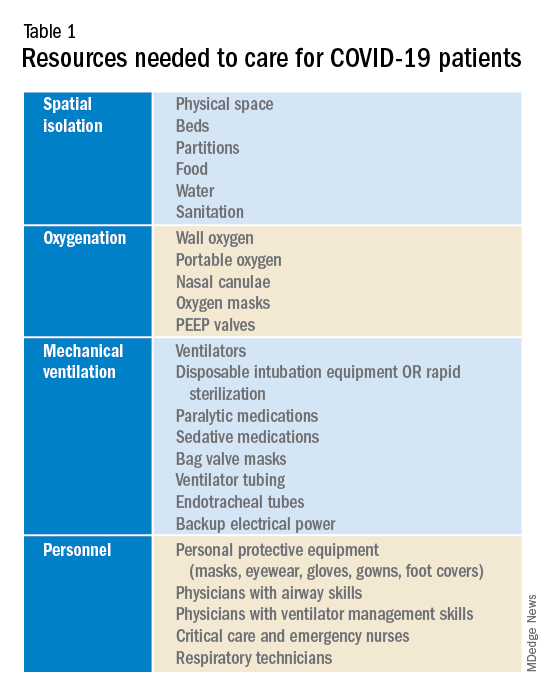
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
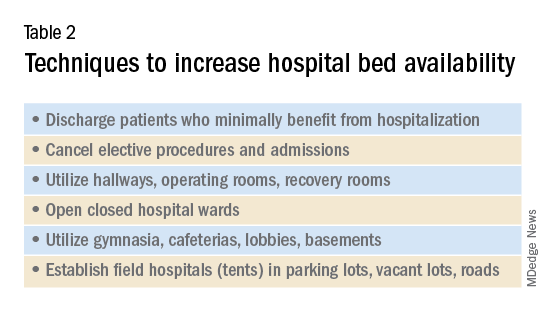
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.
Background
As of April 2020, the United States is faced with the early stages of the coronavirus disease 2019 (COVID-19) pandemic. Experts predict up to 60% of the population will become infected with a fatality rate of 1% and a hospitalization rate of approximately 20%. Efforts to suppress viral spread have been unsuccessful as cases are reported in all 50 states, and fatalities are rising. Currently many American hospitals are ill-prepared for a significant increase in their census of critically ill and contagious patients, i.e., hospitals lack adequate surge capacity to safely handle a nationwide outbreak of COVID-19. As seen in other nations such as Italy, China, and Iran, this leads to rationing of life-saving health care and potentially preventable morbidity and mortality.
Introduction
Hospitals will be unable to provide the current standard of care to patients as the rate of infection with coronavirus disease 2019 (COVID-19) escalates. As of April 9, the World Health Organization has confirmed 1,539,118 cases and 89,998 deaths globally; and the Centers for Disease Control and Prevention has confirmed 435,941 cases and 14,865 deaths in the United States.1,2 Experts predict up to 60% of the population will eventually become infected with a fatality rate of about 1% and a hospitalization rate of approximately 20%.3,4
In the United States, with a population of 300 million people, this represents up to 180 million infected, 36 million requiring hospitalization, 11 million requiring intensive care, and 2 million fatalities over the duration of the pandemic. On March 13, President Donald Trump declared a state of national emergency, authorizing $50 billion dollars in emergency health care spending as well as asking every hospital in the country to immediately activate its emergency response plan. The use of isolation and quarantine may space out casualties over time, however high rates and volumes of hospitalizations are still expected.4,5
As the influx of patients afflicted with COVID-19 grows, needs will outstrip hospital resources forcing clinicians to ration beds and supplies. In Italy, China, and Iran, physicians are already faced with these difficult decisions. Antonio Pesenti, head of the Italian Lombardy regional crisis response unit, characterized the change in health care delivery: “We’re now being forced to set up intensive care treatment in corridors, in operating theaters, in recovery rooms. We’ve emptied entire hospital sections to make space for seriously sick people.”6
Surge capacity
Surge capacity is a hospital’s ability to adequately care for a significant influx of patients.7 Since 2011, the American College of Emergency Physicians has published guidelines calling for hospitals to have a surge capacity accounting for infectious disease outbreaks, and demands on supplies, personnel, and physical space.7 Even prior to the development of COVID-19, many hospitals faced emergency department crowding and strains on hospital capacity.8 The Organization for Economic Co-operation and Development (OECD) estimates hospital beds per 1,000 inhabitants at 2.77 for the USA, 3.18 for Italy, 4.34 for China, and 13.05 for Japan.9 Before COVID-19 many American hospitals had an insufficient number of beds. Now, in the initial phase of the pandemic, it is even more important to optimize surge capacity across the American health care system.
Requirements for COVID-19 preparation
To prepare for the increased number of seriously and critically ill patients, individual hospitals and regions must perform a needs assessment. The fundamental disease process of COVID-19 is a contagious viral pneumonia; treatment hinges on four major categories of intervention: spatial isolation (including physical space, beds, partitions, droplet precautions, food, water, and sanitation), oxygenation (including wall and portable oxygen, nasal canulae, and masks), mechanical ventilation (including ventilator machines, tubing, anesthetics, and reliable electrical power) and personnel (including physicians, nurses, technicians, and adequate personal protective equipment).10 In special circumstances and where available, extra corporeal membrane oxygenation may be considered.10 The necessary interventions are summarized in Table 1. 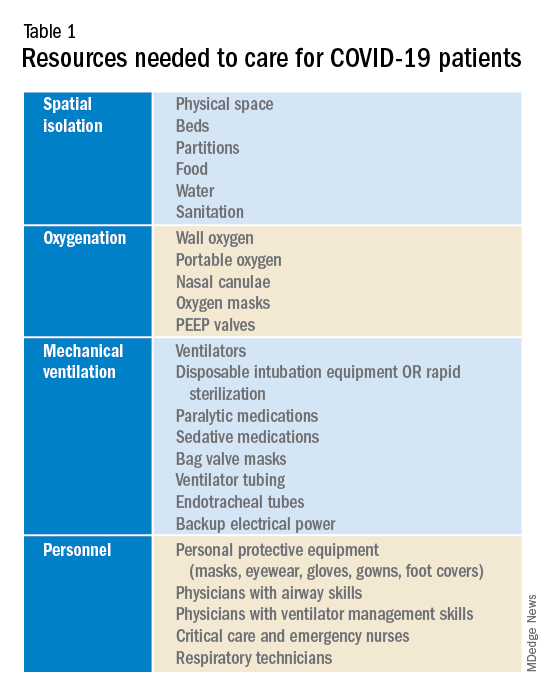
Emergency, critical care, nursing, and medical leadership should consider what sort of space, personnel, and supplies will be needed to care for a large volume of patients with contagious viral pneumonia at the same time as other hospital patients. Attention should also be given to potential need for morgue expansion. Hospitals must be proactive in procuring supplies and preparing for demands on beds and physical space. Specifically, logistics coordinators should start stockpiling ventilators, oxygen, respiratory equipment, and personal protective equipment. Reallocating supplies from other regions of the hospital such as operating rooms and ambulatory surgery centers may be considered. These resources, particularly ventilators and ventilator supplies, are already in disturbingly limited supply, and they are likely to be single most important limiting factor for survival rates. To prevent regional shortages, stockpiling efforts should ideally be aided by state and federal governments. The production and acquisition of ventilators should be immediately and significantly increased.
Hospitals must additionally prepare for demands for physical space and beds. Techniques to maximize space and bed availability (see Table 2) include discharging patients who do not require hospitalization, and canceling elective procedures and admissions. Additional methods would be to utilize unconventional preexisting spaces such as hallways, operating rooms, recovery rooms, hallways, closed hospital wards, basements, lobbies, cafeterias, and parking lots. Administrators should also consider establishing field hospitals or field wards, such as tents in open spaces and nearby roads. Medical care performed in unconventional environments will need to account for electricity, temperature control, oxygen delivery, and sanitation.
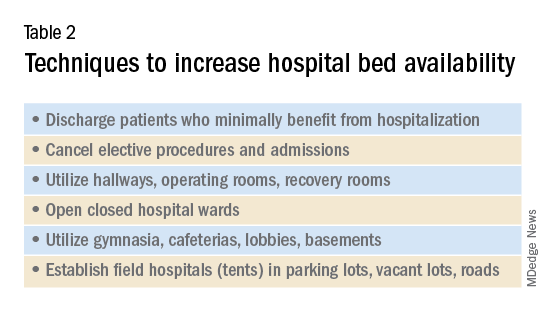
Conclusion
To minimize unnecessary loss of life and suffering, hospitals must expand their surge capacities in preparation for the predictable rise in demand for health care resources related to COVID-19. Numerous hospitals, particularly those that serve low-income and underserved communities, operate with a narrow financial margin.11 Independently preparing for the surge capacity needed to face COVID-19 may be infeasible for several hospitals. As a result, many health care systems will rely on government aid during this period for financial and material support. To maximize preparedness and response, hospitals should ask for and receive aid from the Federal Emergency Management Agency (FEMA), American Red Cross, state governments, and the military; these resources should be mobilized now.
Dr. Blumenberg, Dr. Noble, and Dr. Hendrickson are based in the department of emergency medicine & toxicology, Oregon Health and Science University, Portland.
References
1. Coronavirus disease 2019 (COVID-19) situation report – 60. 2020 Mar 19.
2. Coronavirus disease 2019 (COVID-19) Cases in the U.S. CDC. 2020 Apr 8.
3. Li Q et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 Jan. doi: 10.1056/NEJMoa2001316.
4. Anderson RM et al. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar. doi: 10.1016/S0140-6736(20)30567-5.
5. Fraser C et al. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci U S A. 2004;101(16):6146-51. doi: 10.1073/pnas.0307506101.
6. Mackenzie J and Balmer C. Italy locks down millions as its coronavirus deaths jump. Reuters. 2020 Mar 9.
7. Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2012;59(3):240-1. doi: 10.1016/j.annemergmed.2011.11.030.
8. Pitts SR et al. A cross-sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21(5):497-503. doi: 10.1111/acem.12375.
9. Health at a Glance 2019. OECD; 2019. doi: 10.1787/4dd50c09-en.
10. Murthy S et al. Care for critically ill patients with COVID-19. JAMA. 2020 Mar. doi: 10.1001/jama.2020.3633.
11. Ly DP et al. The association between hospital margins, quality of care, and closure or other change in operating status. J Gen Intern Med. 2011;26(11):1291-6. doi: 10.1007/s11606-011-1815-5.
Is protocol-driven COVID-19 respiratory therapy doing more harm than good?
Physicians in the COVID-19 trenches are beginning to question whether standard respiratory therapy protocols for acute respiratory distress syndrome (ARDS) are the best approach for treating patients with COVID-19 pneumonia.
At issue is the standard use of ventilators for a virus whose presentation has not followed the standard for ARDS, but is looking more like high-altitude pulmonary edema (HAPE) in some patients.
In a letter to the editor published in the American Journal of Respiratory and Critical Care Medicine on March 30, and in an editorial accepted for publication in Intensive Care Medicine, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues make the case that protocol-driven ventilator use for patients with COVID-19 could be doing more harm than good.
Dr. Gattinoni noted that COVID-19 patients in ICUs in northern Italy had an atypical ARDS presentation with severe hypoxemia and well-preserved lung gas volume. He and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation–practicing patience to “buy time with minimum additional damage.”
Similar observations were made by Cameron Kyle-Sidell, MD, a critical care physician working in New York City, who has been speaking out about this issue on Twitter and who shared his own experiences in this video interview with WebMD chief medical officer John Whyte, MD.
The bottom line, as Dr. Kyle-Sidell and Dr. Gattinoni agree, is that protocol-driven ventilator use may be causing lung injury in COVID-19 patients.
Consider disease phenotype
In the editorial, Dr. Gattinoni and colleagues explained further that ventilator settings should be based on physiological findings – with different respiratory treatment based on disease phenotype rather than using standard protocols.
‘“This, of course, is a conceptual model, but based on the observations we have this far, I don’t know of any model which is better,” he said in an interview.
Anecdotal evidence has increasingly demonstrated that this proposed physiological approach is associated with much lower mortality rates among COVID-19 patients, he said.
While not willing to name the hospitals at this time, he said that one center in Europe has had a 0% mortality rate among COVID-19 patients in the ICU when using this approach, compared with a 60% mortality rate at a nearby hospital using a protocol-driven approach.
In his editorial, Dr. Gattinoni disputed the recently published recommendation from the Surviving Sepsis Campaign that “mechanically ventilated patients with COVID-19 should be managed similarly to other patients with acute respiratory failure in the ICU.”
“Yet, COVID-19 pneumonia, despite falling in most of the circumstances under the Berlin definition of ARDS, is a specific disease, whose distinctive features are severe hypoxemia often associated with near normal respiratory system compliance,” Dr. Gattinoni and colleagues wrote, noting that this was true for more than half of the 150 patients he and his colleagues had assessed, and that several other colleagues in northern Italy reported similar findings. “This remarkable combination is almost never seen in severe ARDS.”
Dr. Gattinoni and colleagues hypothesized that COVID-19 patterns at patient presentation depend on interaction between three sets of factors: 1) disease severity, host response, physiological reserve and comorbidities; 2) ventilatory responsiveness of the patient to hypoxemia; and 3) time elapsed between disease onset and hospitalization.
They identified two primary phenotypes based on the interaction of these factors: Type L, characterized by low elastance, low ventilator perfusion ratio, low lung weight, and low recruitability; and Type H, characterized by high elastance, high right-to-left shunt, high lung weight, and high recruitability.
“Given this conceptual model, it follows that the respiratory treatment offered to Type L and Type H patients must be different,” Dr. Gattinoni said.
Patients may transition between phenotypes as their disease evolves. “If you start with the wrong protocol, at the end they become similar,” he said.
Rather, it is important to identify the phenotype at presentation to understand the pathophysiology and treat accordingly, he advised.
The phenotypes are best identified by CT scan, but signs implicit in each of the phenotypes, including respiratory system elastance and recruitability, can be used as surrogates if CT is unavailable, he noted.
“This is a kind of disease in which you don’t have to follow the protocol – you have to follow the physiology,” he said. “Unfortunately, many, many doctors around the world cannot think outside the protocol.”
In his interview with Dr. Whyte, Dr. Kyle-Sidell stressed that doctors must begin to consider other approaches. “We are desperate now, in the sense that everything we are doing does not seem to be working,” Dr. Kyle-Sidell said, noting that the first step toward improving outcomes is admitting that “this is something new.”
“I think it all starts from there, and I think we have the kind of scientific technology and the human capital in this country to solve this or at least have a very good shot at it,” he said.
Proposed treatment model
Dr. Gattinoni and his colleagues offered a proposed treatment model based on their conceptualization:
- Reverse hypoxemia through an increase in FiO2 to a level at which the Type L patient responds well, particularly for Type L patients who are not experiencing dyspnea.
- In Type L patients with dyspnea, try noninvasive options such as high-flow nasal cannula, continuous positive airway pressure, or noninvasive ventilation, and be sure to measure inspiratory esophageal pressure using esophageal manometry or surrogate measures. In intubated patients, determine P0.1 and P occlusion. High PEEP may decrease pleural pressure swings “and stop the vicious cycle that exacerbates lung injury,” but may be associated with high failure rates and delayed intubation.
- Intubate as soon as possible for esophageal pressure swings that increase from 5-10 cm H2O to above 15 cm H2O, which marks a transition from Type L to Type H phenotype and represents the level at which lung injury risk increases.
- For intubated and deeply sedated Type L patients who are hypercapnic, ventilate with volumes greater than 6 mL/kg up to 8-9 mL/kg as this high compliance results in tolerable strain without risk of ventilator-associated lung injury. Prone positioning should be used only as a rescue maneuver. Reduce PEEP to 8-10 cm H2O, given that the recruitability is low and the risk of hemodynamic failure increases at higher levels. Early intubation may avert the transition to Type H phenotype.
- Treat Type H phenotype like severe ARDS, including with higher PEEP if compatible with hemodynamics, and with prone positioning and extracorporeal support.
Dr. Gattinoni reported having no financial disclosures.
[email protected]
Physicians in the COVID-19 trenches are beginning to question whether standard respiratory therapy protocols for acute respiratory distress syndrome (ARDS) are the best approach for treating patients with COVID-19 pneumonia.
At issue is the standard use of ventilators for a virus whose presentation has not followed the standard for ARDS, but is looking more like high-altitude pulmonary edema (HAPE) in some patients.
In a letter to the editor published in the American Journal of Respiratory and Critical Care Medicine on March 30, and in an editorial accepted for publication in Intensive Care Medicine, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues make the case that protocol-driven ventilator use for patients with COVID-19 could be doing more harm than good.
Dr. Gattinoni noted that COVID-19 patients in ICUs in northern Italy had an atypical ARDS presentation with severe hypoxemia and well-preserved lung gas volume. He and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation–practicing patience to “buy time with minimum additional damage.”
Similar observations were made by Cameron Kyle-Sidell, MD, a critical care physician working in New York City, who has been speaking out about this issue on Twitter and who shared his own experiences in this video interview with WebMD chief medical officer John Whyte, MD.
The bottom line, as Dr. Kyle-Sidell and Dr. Gattinoni agree, is that protocol-driven ventilator use may be causing lung injury in COVID-19 patients.
Consider disease phenotype
In the editorial, Dr. Gattinoni and colleagues explained further that ventilator settings should be based on physiological findings – with different respiratory treatment based on disease phenotype rather than using standard protocols.
‘“This, of course, is a conceptual model, but based on the observations we have this far, I don’t know of any model which is better,” he said in an interview.
Anecdotal evidence has increasingly demonstrated that this proposed physiological approach is associated with much lower mortality rates among COVID-19 patients, he said.
While not willing to name the hospitals at this time, he said that one center in Europe has had a 0% mortality rate among COVID-19 patients in the ICU when using this approach, compared with a 60% mortality rate at a nearby hospital using a protocol-driven approach.
In his editorial, Dr. Gattinoni disputed the recently published recommendation from the Surviving Sepsis Campaign that “mechanically ventilated patients with COVID-19 should be managed similarly to other patients with acute respiratory failure in the ICU.”
“Yet, COVID-19 pneumonia, despite falling in most of the circumstances under the Berlin definition of ARDS, is a specific disease, whose distinctive features are severe hypoxemia often associated with near normal respiratory system compliance,” Dr. Gattinoni and colleagues wrote, noting that this was true for more than half of the 150 patients he and his colleagues had assessed, and that several other colleagues in northern Italy reported similar findings. “This remarkable combination is almost never seen in severe ARDS.”
Dr. Gattinoni and colleagues hypothesized that COVID-19 patterns at patient presentation depend on interaction between three sets of factors: 1) disease severity, host response, physiological reserve and comorbidities; 2) ventilatory responsiveness of the patient to hypoxemia; and 3) time elapsed between disease onset and hospitalization.
They identified two primary phenotypes based on the interaction of these factors: Type L, characterized by low elastance, low ventilator perfusion ratio, low lung weight, and low recruitability; and Type H, characterized by high elastance, high right-to-left shunt, high lung weight, and high recruitability.
“Given this conceptual model, it follows that the respiratory treatment offered to Type L and Type H patients must be different,” Dr. Gattinoni said.
Patients may transition between phenotypes as their disease evolves. “If you start with the wrong protocol, at the end they become similar,” he said.
Rather, it is important to identify the phenotype at presentation to understand the pathophysiology and treat accordingly, he advised.
The phenotypes are best identified by CT scan, but signs implicit in each of the phenotypes, including respiratory system elastance and recruitability, can be used as surrogates if CT is unavailable, he noted.
“This is a kind of disease in which you don’t have to follow the protocol – you have to follow the physiology,” he said. “Unfortunately, many, many doctors around the world cannot think outside the protocol.”
In his interview with Dr. Whyte, Dr. Kyle-Sidell stressed that doctors must begin to consider other approaches. “We are desperate now, in the sense that everything we are doing does not seem to be working,” Dr. Kyle-Sidell said, noting that the first step toward improving outcomes is admitting that “this is something new.”
“I think it all starts from there, and I think we have the kind of scientific technology and the human capital in this country to solve this or at least have a very good shot at it,” he said.
Proposed treatment model
Dr. Gattinoni and his colleagues offered a proposed treatment model based on their conceptualization:
- Reverse hypoxemia through an increase in FiO2 to a level at which the Type L patient responds well, particularly for Type L patients who are not experiencing dyspnea.
- In Type L patients with dyspnea, try noninvasive options such as high-flow nasal cannula, continuous positive airway pressure, or noninvasive ventilation, and be sure to measure inspiratory esophageal pressure using esophageal manometry or surrogate measures. In intubated patients, determine P0.1 and P occlusion. High PEEP may decrease pleural pressure swings “and stop the vicious cycle that exacerbates lung injury,” but may be associated with high failure rates and delayed intubation.
- Intubate as soon as possible for esophageal pressure swings that increase from 5-10 cm H2O to above 15 cm H2O, which marks a transition from Type L to Type H phenotype and represents the level at which lung injury risk increases.
- For intubated and deeply sedated Type L patients who are hypercapnic, ventilate with volumes greater than 6 mL/kg up to 8-9 mL/kg as this high compliance results in tolerable strain without risk of ventilator-associated lung injury. Prone positioning should be used only as a rescue maneuver. Reduce PEEP to 8-10 cm H2O, given that the recruitability is low and the risk of hemodynamic failure increases at higher levels. Early intubation may avert the transition to Type H phenotype.
- Treat Type H phenotype like severe ARDS, including with higher PEEP if compatible with hemodynamics, and with prone positioning and extracorporeal support.
Dr. Gattinoni reported having no financial disclosures.
[email protected]
Physicians in the COVID-19 trenches are beginning to question whether standard respiratory therapy protocols for acute respiratory distress syndrome (ARDS) are the best approach for treating patients with COVID-19 pneumonia.
At issue is the standard use of ventilators for a virus whose presentation has not followed the standard for ARDS, but is looking more like high-altitude pulmonary edema (HAPE) in some patients.
In a letter to the editor published in the American Journal of Respiratory and Critical Care Medicine on March 30, and in an editorial accepted for publication in Intensive Care Medicine, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues make the case that protocol-driven ventilator use for patients with COVID-19 could be doing more harm than good.
Dr. Gattinoni noted that COVID-19 patients in ICUs in northern Italy had an atypical ARDS presentation with severe hypoxemia and well-preserved lung gas volume. He and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation–practicing patience to “buy time with minimum additional damage.”
Similar observations were made by Cameron Kyle-Sidell, MD, a critical care physician working in New York City, who has been speaking out about this issue on Twitter and who shared his own experiences in this video interview with WebMD chief medical officer John Whyte, MD.
The bottom line, as Dr. Kyle-Sidell and Dr. Gattinoni agree, is that protocol-driven ventilator use may be causing lung injury in COVID-19 patients.
Consider disease phenotype
In the editorial, Dr. Gattinoni and colleagues explained further that ventilator settings should be based on physiological findings – with different respiratory treatment based on disease phenotype rather than using standard protocols.
‘“This, of course, is a conceptual model, but based on the observations we have this far, I don’t know of any model which is better,” he said in an interview.
Anecdotal evidence has increasingly demonstrated that this proposed physiological approach is associated with much lower mortality rates among COVID-19 patients, he said.
While not willing to name the hospitals at this time, he said that one center in Europe has had a 0% mortality rate among COVID-19 patients in the ICU when using this approach, compared with a 60% mortality rate at a nearby hospital using a protocol-driven approach.
In his editorial, Dr. Gattinoni disputed the recently published recommendation from the Surviving Sepsis Campaign that “mechanically ventilated patients with COVID-19 should be managed similarly to other patients with acute respiratory failure in the ICU.”
“Yet, COVID-19 pneumonia, despite falling in most of the circumstances under the Berlin definition of ARDS, is a specific disease, whose distinctive features are severe hypoxemia often associated with near normal respiratory system compliance,” Dr. Gattinoni and colleagues wrote, noting that this was true for more than half of the 150 patients he and his colleagues had assessed, and that several other colleagues in northern Italy reported similar findings. “This remarkable combination is almost never seen in severe ARDS.”
Dr. Gattinoni and colleagues hypothesized that COVID-19 patterns at patient presentation depend on interaction between three sets of factors: 1) disease severity, host response, physiological reserve and comorbidities; 2) ventilatory responsiveness of the patient to hypoxemia; and 3) time elapsed between disease onset and hospitalization.
They identified two primary phenotypes based on the interaction of these factors: Type L, characterized by low elastance, low ventilator perfusion ratio, low lung weight, and low recruitability; and Type H, characterized by high elastance, high right-to-left shunt, high lung weight, and high recruitability.
“Given this conceptual model, it follows that the respiratory treatment offered to Type L and Type H patients must be different,” Dr. Gattinoni said.
Patients may transition between phenotypes as their disease evolves. “If you start with the wrong protocol, at the end they become similar,” he said.
Rather, it is important to identify the phenotype at presentation to understand the pathophysiology and treat accordingly, he advised.
The phenotypes are best identified by CT scan, but signs implicit in each of the phenotypes, including respiratory system elastance and recruitability, can be used as surrogates if CT is unavailable, he noted.
“This is a kind of disease in which you don’t have to follow the protocol – you have to follow the physiology,” he said. “Unfortunately, many, many doctors around the world cannot think outside the protocol.”
In his interview with Dr. Whyte, Dr. Kyle-Sidell stressed that doctors must begin to consider other approaches. “We are desperate now, in the sense that everything we are doing does not seem to be working,” Dr. Kyle-Sidell said, noting that the first step toward improving outcomes is admitting that “this is something new.”
“I think it all starts from there, and I think we have the kind of scientific technology and the human capital in this country to solve this or at least have a very good shot at it,” he said.
Proposed treatment model
Dr. Gattinoni and his colleagues offered a proposed treatment model based on their conceptualization:
- Reverse hypoxemia through an increase in FiO2 to a level at which the Type L patient responds well, particularly for Type L patients who are not experiencing dyspnea.
- In Type L patients with dyspnea, try noninvasive options such as high-flow nasal cannula, continuous positive airway pressure, or noninvasive ventilation, and be sure to measure inspiratory esophageal pressure using esophageal manometry or surrogate measures. In intubated patients, determine P0.1 and P occlusion. High PEEP may decrease pleural pressure swings “and stop the vicious cycle that exacerbates lung injury,” but may be associated with high failure rates and delayed intubation.
- Intubate as soon as possible for esophageal pressure swings that increase from 5-10 cm H2O to above 15 cm H2O, which marks a transition from Type L to Type H phenotype and represents the level at which lung injury risk increases.
- For intubated and deeply sedated Type L patients who are hypercapnic, ventilate with volumes greater than 6 mL/kg up to 8-9 mL/kg as this high compliance results in tolerable strain without risk of ventilator-associated lung injury. Prone positioning should be used only as a rescue maneuver. Reduce PEEP to 8-10 cm H2O, given that the recruitability is low and the risk of hemodynamic failure increases at higher levels. Early intubation may avert the transition to Type H phenotype.
- Treat Type H phenotype like severe ARDS, including with higher PEEP if compatible with hemodynamics, and with prone positioning and extracorporeal support.
Dr. Gattinoni reported having no financial disclosures.
[email protected]
























