User login
Camp Discovery: A place for children to be comfortable in their own skin
The talent show, the grand finale of the 1-week camp, was nearly 7 years ago, but Emily Haygood of Houston, now 17 and about to start her senior year, remembers it in detail. She sang “Death of a Bachelor,” an R&B pop song and Billboard No. 1 hit at the time about a former bachelor who had happily married. These days, she said, if she watched the video of her 10-year-old singing self, “I would probably throw up.” But she still treasures the audience response, “having all those people I’d gotten close to cheer for me.”
Emily was at , but share one feature: they are the kind of dermatologic issues that can make doing everyday kid or teen activities like swimming difficult and can elicit mean comments from classmates and other would-be friends.

Emily was first diagnosed with atopic dermatitis at age 4, her mother, Amber Haygood, says. By age 9, it had become severe. Emily remembers being teased some in elementary school. “I did feel bad a lot of the time, when asked insensitive questions.” Her mother still bristles that adults often could be cruel, too.
But at Camp Discovery, those issues were nonexistent. “Camp was so cool,” Emily said. Besides the usual camp activities, it had things that “normal” camp didn’t, like other kids who didn’t stare at your skin condition or make fun of it.
30th anniversary season begins
This year is the 30th anniversary of Camp Discovery. Sessions began July 23 and continue through Aug. 18, with locations in Crosslake, Minn.; Hebron, Conn.; and Millville, Pa., in addition to Burton, Tex. About 300 campers will attend this year, according to the AAD, and 6,151 campers have attended from 1993 to 2022.
The 1-week camp accepts youth with conditions ranging from eczema and psoriasis to vitiligo, alopecia, epidermolysis bullosa, and ichthyosis, according to the academy. A dermatologist first refers a child, downloading and completing the referral form and sending it to the academy.
The 1-week session, including travel, is free for the campers, thanks to donors. As a nonprofit and membership-based organization, the AAD does not release the detailed financial information about the operating budget for the camp. Dermatologists, nurses, and counselors volunteer their time.
In his presidential address at the AAD’s annual meeting in March, outgoing president Mark D. Kaufmann, MD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai in New York, referred to camp volunteering as an antidote to professional burnout. Remembering why as a dermatologist one entered the profession can be one solution, he said, and described his own recent 3-day volunteer stint at the camp.
“Those 3 magical days, being with kids as they discovered they weren’t alone in the world, sharing their experiences and ideas, reminded me why I became a physician in the first place,” he told the audience of meeting attendees. He vowed to expand the program, with a goal of having every dermatology resident attend Camp Discovery.
Mental health effects of skin conditions
Much research has focused on the mental health fallout from living with chronic skin conditions, and even young children can be adversely affected. In one review of the literature, researchers concluded that pediatric skin disease, including acne, atopic dermatitis, and psoriasis, can affect quality of life, carry stigma, and lead to bullying and eventually even suicidal behavior. Another study, published earlier this year, found that atopic dermatitis affected children’s quality of life, impacting sleep and leading to feelings of being ashamed.
“It’s not necessarily about what their skin condition is and more about the psychosocial impact,’’ said Samantha Hill, MD, a pediatric and general dermatologist in Lynchburg, Va., who is the medical director of Camp Discovery in Minnesota this year.
Camp activities, reactions
The overriding theme of camp is allowing all the youth to be “just one of the kids at camp,” Dr. Hill said in an interview. “They come to do all kinds of things they don’t do in normal life because people don’t give them the credit to [be able to] do it.”
Every year, she said, “I tell my staff we are in the business of making things happen, so if there is a kid bandaged head to toe [because of a skin condition] and they want to go tubing and get in the lake, we figure out how to make it happen. We have done that multiple times.”
Newcomers are initially nervous, Dr. Hill acknowledged, but in time let their guard down. Returnees are a different story. “When kids who have been at camp before arrive, you can see them start breathing again, looking for their friends. You can see them relax right before your eyes.”
“The single most empowering thing is the realization you are not alone,” said Meena Julapalli, MD, a Houston dermatologist who is a medical team member and long-time volunteer at Camp Discovery. That, she said, and “You get to be a kid, and you don’t have to have people staring at you.”
Dr. Julapalli remembers one of her patients with keratitis-ichthyosis-deafness (KID) syndrome. “She needed more than what I could offer,” she said. “She needed camp.” At camp, the organizers found a counselor who knew sign language to accompany her. At first, she was quiet and didn’t smile much. By the end of the week, as she was about to observe her birthday, things changed. After breakfast, she was led to the stage, where fellow campers began singing – and signing the song they had just learned.
Camp staff gets it
Allyson Garin, who was diagnosed with vitiligo at age 6 months, is a camp program director at Camp Discovery in Crosslake, Minn. She first went to camp in 1990 at age 11, returning until she “aged out” at 16, then worked as a counselor. She gets it when campers tell her they hear rude comments about their skin conditions.
“I remember being in swimming pools, in lines at fairgrounds or amusement parks,” she said in an interview, “and hearing people say, ‘Don’t touch her,’ ’’ fearing contagion, perhaps. “People would make jokes about cows, since they are spotted,” she said, or people would simply step back.
All those years ago, her mother found out about the camp and decided to figure out how to get her there. She got there, and she met a fellow camper with vitiligo, and they became pen pals. “We still talk,” she said.
Meeting someone with the same skin condition, she said, isn’t just about commiserating. “There is a lot of information sharing,” on topics such as best treatments, strategies, and other conversations.
Other lessons
While campers can feel comfortable around others who also have skin conditions, and understand, the lesson extends beyond that, Ms. Garin said. “It gave me a perspective,” she said of her camp experience. “I always felt, ‘Woe is me.’ ” But when she met others with, as she said, conditions “way worse than vitiligo, it really grounds you.”
Dr. Hill agreed. Campers get the benefit of others accepting and including them, but also practicing that same attitude toward fellow campers, she said. “It insures that we are providing this environment of inclusion, but that they are practicing it as well. They need to practice it like everyone else.”
Getting parents on board
The idea of camp, especially for those at the younger end of the 8- to 16-years age range accepted for Camp Discovery, can take some getting used to for some parents. Ms. Haygood, Emily’s mother, relates to that. Her daughter’s dermatologist at the time, who is now retired, had first suggested the camp. Her first reaction? “I am not sending my chronically ill child to camp with strangers.” She also acknowledged that she, like other parents of children with a chronic illness, can be a helicopter parent.
Then, she noticed that Emily seemed interested, so she got more information, finding out that it was staffed by doctors. It all sounded good, she said, and the social interaction, she knew, would be beneficial. “Then my husband was a no,” she said, concerned about their daughter being with strangers. “Eventually he came around,” Ms. Haygood said. All along, Emily said, “it seemed fun. I was probably trying to talk them into it.” She admits she was very nervous at first, but calmed down when she realized her own dermatologist was going to be there.
Vanessa Hadley of Spring, Tex., was on board the moment she heard about Camp Discovery. “I just thought it was amazing,” she said. Her daughter Isabelle, 13, has been to the camp. “She has alopecia areata and severe eczema,” Ms. Hadley said. Now, Isabelle is returning to camp and coaching her sister Penelope, 8, who has eczema and mild alopecia and is a first-timer this summer.
One tip the 8-year-old has learned so far: Turn to your counselor for support if you’re nervous. That worked, Isabelle said, the first year when she was wary of the zipline – then surprised herself and conquered it.
Dr. Hill and Dr. Julapalli have no disclosures.
The talent show, the grand finale of the 1-week camp, was nearly 7 years ago, but Emily Haygood of Houston, now 17 and about to start her senior year, remembers it in detail. She sang “Death of a Bachelor,” an R&B pop song and Billboard No. 1 hit at the time about a former bachelor who had happily married. These days, she said, if she watched the video of her 10-year-old singing self, “I would probably throw up.” But she still treasures the audience response, “having all those people I’d gotten close to cheer for me.”
Emily was at , but share one feature: they are the kind of dermatologic issues that can make doing everyday kid or teen activities like swimming difficult and can elicit mean comments from classmates and other would-be friends.

Emily was first diagnosed with atopic dermatitis at age 4, her mother, Amber Haygood, says. By age 9, it had become severe. Emily remembers being teased some in elementary school. “I did feel bad a lot of the time, when asked insensitive questions.” Her mother still bristles that adults often could be cruel, too.
But at Camp Discovery, those issues were nonexistent. “Camp was so cool,” Emily said. Besides the usual camp activities, it had things that “normal” camp didn’t, like other kids who didn’t stare at your skin condition or make fun of it.
30th anniversary season begins
This year is the 30th anniversary of Camp Discovery. Sessions began July 23 and continue through Aug. 18, with locations in Crosslake, Minn.; Hebron, Conn.; and Millville, Pa., in addition to Burton, Tex. About 300 campers will attend this year, according to the AAD, and 6,151 campers have attended from 1993 to 2022.
The 1-week camp accepts youth with conditions ranging from eczema and psoriasis to vitiligo, alopecia, epidermolysis bullosa, and ichthyosis, according to the academy. A dermatologist first refers a child, downloading and completing the referral form and sending it to the academy.
The 1-week session, including travel, is free for the campers, thanks to donors. As a nonprofit and membership-based organization, the AAD does not release the detailed financial information about the operating budget for the camp. Dermatologists, nurses, and counselors volunteer their time.
In his presidential address at the AAD’s annual meeting in March, outgoing president Mark D. Kaufmann, MD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai in New York, referred to camp volunteering as an antidote to professional burnout. Remembering why as a dermatologist one entered the profession can be one solution, he said, and described his own recent 3-day volunteer stint at the camp.
“Those 3 magical days, being with kids as they discovered they weren’t alone in the world, sharing their experiences and ideas, reminded me why I became a physician in the first place,” he told the audience of meeting attendees. He vowed to expand the program, with a goal of having every dermatology resident attend Camp Discovery.
Mental health effects of skin conditions
Much research has focused on the mental health fallout from living with chronic skin conditions, and even young children can be adversely affected. In one review of the literature, researchers concluded that pediatric skin disease, including acne, atopic dermatitis, and psoriasis, can affect quality of life, carry stigma, and lead to bullying and eventually even suicidal behavior. Another study, published earlier this year, found that atopic dermatitis affected children’s quality of life, impacting sleep and leading to feelings of being ashamed.
“It’s not necessarily about what their skin condition is and more about the psychosocial impact,’’ said Samantha Hill, MD, a pediatric and general dermatologist in Lynchburg, Va., who is the medical director of Camp Discovery in Minnesota this year.
Camp activities, reactions
The overriding theme of camp is allowing all the youth to be “just one of the kids at camp,” Dr. Hill said in an interview. “They come to do all kinds of things they don’t do in normal life because people don’t give them the credit to [be able to] do it.”
Every year, she said, “I tell my staff we are in the business of making things happen, so if there is a kid bandaged head to toe [because of a skin condition] and they want to go tubing and get in the lake, we figure out how to make it happen. We have done that multiple times.”
Newcomers are initially nervous, Dr. Hill acknowledged, but in time let their guard down. Returnees are a different story. “When kids who have been at camp before arrive, you can see them start breathing again, looking for their friends. You can see them relax right before your eyes.”
“The single most empowering thing is the realization you are not alone,” said Meena Julapalli, MD, a Houston dermatologist who is a medical team member and long-time volunteer at Camp Discovery. That, she said, and “You get to be a kid, and you don’t have to have people staring at you.”
Dr. Julapalli remembers one of her patients with keratitis-ichthyosis-deafness (KID) syndrome. “She needed more than what I could offer,” she said. “She needed camp.” At camp, the organizers found a counselor who knew sign language to accompany her. At first, she was quiet and didn’t smile much. By the end of the week, as she was about to observe her birthday, things changed. After breakfast, she was led to the stage, where fellow campers began singing – and signing the song they had just learned.
Camp staff gets it
Allyson Garin, who was diagnosed with vitiligo at age 6 months, is a camp program director at Camp Discovery in Crosslake, Minn. She first went to camp in 1990 at age 11, returning until she “aged out” at 16, then worked as a counselor. She gets it when campers tell her they hear rude comments about their skin conditions.
“I remember being in swimming pools, in lines at fairgrounds or amusement parks,” she said in an interview, “and hearing people say, ‘Don’t touch her,’ ’’ fearing contagion, perhaps. “People would make jokes about cows, since they are spotted,” she said, or people would simply step back.
All those years ago, her mother found out about the camp and decided to figure out how to get her there. She got there, and she met a fellow camper with vitiligo, and they became pen pals. “We still talk,” she said.
Meeting someone with the same skin condition, she said, isn’t just about commiserating. “There is a lot of information sharing,” on topics such as best treatments, strategies, and other conversations.
Other lessons
While campers can feel comfortable around others who also have skin conditions, and understand, the lesson extends beyond that, Ms. Garin said. “It gave me a perspective,” she said of her camp experience. “I always felt, ‘Woe is me.’ ” But when she met others with, as she said, conditions “way worse than vitiligo, it really grounds you.”
Dr. Hill agreed. Campers get the benefit of others accepting and including them, but also practicing that same attitude toward fellow campers, she said. “It insures that we are providing this environment of inclusion, but that they are practicing it as well. They need to practice it like everyone else.”
Getting parents on board
The idea of camp, especially for those at the younger end of the 8- to 16-years age range accepted for Camp Discovery, can take some getting used to for some parents. Ms. Haygood, Emily’s mother, relates to that. Her daughter’s dermatologist at the time, who is now retired, had first suggested the camp. Her first reaction? “I am not sending my chronically ill child to camp with strangers.” She also acknowledged that she, like other parents of children with a chronic illness, can be a helicopter parent.
Then, she noticed that Emily seemed interested, so she got more information, finding out that it was staffed by doctors. It all sounded good, she said, and the social interaction, she knew, would be beneficial. “Then my husband was a no,” she said, concerned about their daughter being with strangers. “Eventually he came around,” Ms. Haygood said. All along, Emily said, “it seemed fun. I was probably trying to talk them into it.” She admits she was very nervous at first, but calmed down when she realized her own dermatologist was going to be there.
Vanessa Hadley of Spring, Tex., was on board the moment she heard about Camp Discovery. “I just thought it was amazing,” she said. Her daughter Isabelle, 13, has been to the camp. “She has alopecia areata and severe eczema,” Ms. Hadley said. Now, Isabelle is returning to camp and coaching her sister Penelope, 8, who has eczema and mild alopecia and is a first-timer this summer.
One tip the 8-year-old has learned so far: Turn to your counselor for support if you’re nervous. That worked, Isabelle said, the first year when she was wary of the zipline – then surprised herself and conquered it.
Dr. Hill and Dr. Julapalli have no disclosures.
The talent show, the grand finale of the 1-week camp, was nearly 7 years ago, but Emily Haygood of Houston, now 17 and about to start her senior year, remembers it in detail. She sang “Death of a Bachelor,” an R&B pop song and Billboard No. 1 hit at the time about a former bachelor who had happily married. These days, she said, if she watched the video of her 10-year-old singing self, “I would probably throw up.” But she still treasures the audience response, “having all those people I’d gotten close to cheer for me.”
Emily was at , but share one feature: they are the kind of dermatologic issues that can make doing everyday kid or teen activities like swimming difficult and can elicit mean comments from classmates and other would-be friends.

Emily was first diagnosed with atopic dermatitis at age 4, her mother, Amber Haygood, says. By age 9, it had become severe. Emily remembers being teased some in elementary school. “I did feel bad a lot of the time, when asked insensitive questions.” Her mother still bristles that adults often could be cruel, too.
But at Camp Discovery, those issues were nonexistent. “Camp was so cool,” Emily said. Besides the usual camp activities, it had things that “normal” camp didn’t, like other kids who didn’t stare at your skin condition or make fun of it.
30th anniversary season begins
This year is the 30th anniversary of Camp Discovery. Sessions began July 23 and continue through Aug. 18, with locations in Crosslake, Minn.; Hebron, Conn.; and Millville, Pa., in addition to Burton, Tex. About 300 campers will attend this year, according to the AAD, and 6,151 campers have attended from 1993 to 2022.
The 1-week camp accepts youth with conditions ranging from eczema and psoriasis to vitiligo, alopecia, epidermolysis bullosa, and ichthyosis, according to the academy. A dermatologist first refers a child, downloading and completing the referral form and sending it to the academy.
The 1-week session, including travel, is free for the campers, thanks to donors. As a nonprofit and membership-based organization, the AAD does not release the detailed financial information about the operating budget for the camp. Dermatologists, nurses, and counselors volunteer their time.
In his presidential address at the AAD’s annual meeting in March, outgoing president Mark D. Kaufmann, MD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai in New York, referred to camp volunteering as an antidote to professional burnout. Remembering why as a dermatologist one entered the profession can be one solution, he said, and described his own recent 3-day volunteer stint at the camp.
“Those 3 magical days, being with kids as they discovered they weren’t alone in the world, sharing their experiences and ideas, reminded me why I became a physician in the first place,” he told the audience of meeting attendees. He vowed to expand the program, with a goal of having every dermatology resident attend Camp Discovery.
Mental health effects of skin conditions
Much research has focused on the mental health fallout from living with chronic skin conditions, and even young children can be adversely affected. In one review of the literature, researchers concluded that pediatric skin disease, including acne, atopic dermatitis, and psoriasis, can affect quality of life, carry stigma, and lead to bullying and eventually even suicidal behavior. Another study, published earlier this year, found that atopic dermatitis affected children’s quality of life, impacting sleep and leading to feelings of being ashamed.
“It’s not necessarily about what their skin condition is and more about the psychosocial impact,’’ said Samantha Hill, MD, a pediatric and general dermatologist in Lynchburg, Va., who is the medical director of Camp Discovery in Minnesota this year.
Camp activities, reactions
The overriding theme of camp is allowing all the youth to be “just one of the kids at camp,” Dr. Hill said in an interview. “They come to do all kinds of things they don’t do in normal life because people don’t give them the credit to [be able to] do it.”
Every year, she said, “I tell my staff we are in the business of making things happen, so if there is a kid bandaged head to toe [because of a skin condition] and they want to go tubing and get in the lake, we figure out how to make it happen. We have done that multiple times.”
Newcomers are initially nervous, Dr. Hill acknowledged, but in time let their guard down. Returnees are a different story. “When kids who have been at camp before arrive, you can see them start breathing again, looking for their friends. You can see them relax right before your eyes.”
“The single most empowering thing is the realization you are not alone,” said Meena Julapalli, MD, a Houston dermatologist who is a medical team member and long-time volunteer at Camp Discovery. That, she said, and “You get to be a kid, and you don’t have to have people staring at you.”
Dr. Julapalli remembers one of her patients with keratitis-ichthyosis-deafness (KID) syndrome. “She needed more than what I could offer,” she said. “She needed camp.” At camp, the organizers found a counselor who knew sign language to accompany her. At first, she was quiet and didn’t smile much. By the end of the week, as she was about to observe her birthday, things changed. After breakfast, she was led to the stage, where fellow campers began singing – and signing the song they had just learned.
Camp staff gets it
Allyson Garin, who was diagnosed with vitiligo at age 6 months, is a camp program director at Camp Discovery in Crosslake, Minn. She first went to camp in 1990 at age 11, returning until she “aged out” at 16, then worked as a counselor. She gets it when campers tell her they hear rude comments about their skin conditions.
“I remember being in swimming pools, in lines at fairgrounds or amusement parks,” she said in an interview, “and hearing people say, ‘Don’t touch her,’ ’’ fearing contagion, perhaps. “People would make jokes about cows, since they are spotted,” she said, or people would simply step back.
All those years ago, her mother found out about the camp and decided to figure out how to get her there. She got there, and she met a fellow camper with vitiligo, and they became pen pals. “We still talk,” she said.
Meeting someone with the same skin condition, she said, isn’t just about commiserating. “There is a lot of information sharing,” on topics such as best treatments, strategies, and other conversations.
Other lessons
While campers can feel comfortable around others who also have skin conditions, and understand, the lesson extends beyond that, Ms. Garin said. “It gave me a perspective,” she said of her camp experience. “I always felt, ‘Woe is me.’ ” But when she met others with, as she said, conditions “way worse than vitiligo, it really grounds you.”
Dr. Hill agreed. Campers get the benefit of others accepting and including them, but also practicing that same attitude toward fellow campers, she said. “It insures that we are providing this environment of inclusion, but that they are practicing it as well. They need to practice it like everyone else.”
Getting parents on board
The idea of camp, especially for those at the younger end of the 8- to 16-years age range accepted for Camp Discovery, can take some getting used to for some parents. Ms. Haygood, Emily’s mother, relates to that. Her daughter’s dermatologist at the time, who is now retired, had first suggested the camp. Her first reaction? “I am not sending my chronically ill child to camp with strangers.” She also acknowledged that she, like other parents of children with a chronic illness, can be a helicopter parent.
Then, she noticed that Emily seemed interested, so she got more information, finding out that it was staffed by doctors. It all sounded good, she said, and the social interaction, she knew, would be beneficial. “Then my husband was a no,” she said, concerned about their daughter being with strangers. “Eventually he came around,” Ms. Haygood said. All along, Emily said, “it seemed fun. I was probably trying to talk them into it.” She admits she was very nervous at first, but calmed down when she realized her own dermatologist was going to be there.
Vanessa Hadley of Spring, Tex., was on board the moment she heard about Camp Discovery. “I just thought it was amazing,” she said. Her daughter Isabelle, 13, has been to the camp. “She has alopecia areata and severe eczema,” Ms. Hadley said. Now, Isabelle is returning to camp and coaching her sister Penelope, 8, who has eczema and mild alopecia and is a first-timer this summer.
One tip the 8-year-old has learned so far: Turn to your counselor for support if you’re nervous. That worked, Isabelle said, the first year when she was wary of the zipline – then surprised herself and conquered it.
Dr. Hill and Dr. Julapalli have no disclosures.
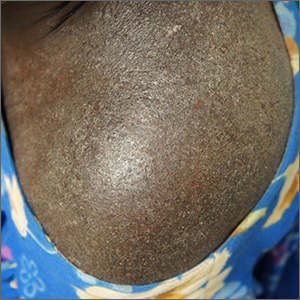
Clothing provides Dx clue

A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003

A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

A close examination of the patient’s scalp and hair was unhelpful, but a close look at the weave and seams of her dress revealed multiple nits and lice, consistent with a diagnosis of body lice.
Head lice and body lice are 2 different ecotypes of the species Pediculus humanus and occupy different environments on the body. They differ slightly in body shape caused by variable expression of the same genes.1 Body lice primarily live and lay eggs on clothing, especially along seams and within knit weaves. They travel to the skin to feed, causing significant itching in the host from the inflammatory and allergic effects of their saliva and feces. Additionally, body lice are vectors of several serious diseases including epidemic typhus (Rickettsia prowasekii), trench fever (Bartonella quintana), and relapsing fever (Borrelia recurrentis).1
A diagnosis of body lice is a sign of severe lack of access to basic human needs—uncrowded shelter, clean clothes, and clean water for bathing. A patient who has been given this diagnosis should be offered and receive a bath or shower with generous soap and warm water. Clothes should be cleaned with hot water (up to 149 °F) or discarded. Patients also may be treated once with topical permethrin 5% cream applied from the top of the neck to the toes in the event that mites survived bathing by attaching to body hairs. Any systemic illness or fever should be evaluated for the above epidemic pathogens. Patients should also be put in touch with social services and mental health services, as appropriate.
This patient received all of the above treatments and had already accessed social services. That said, she continued to struggle with housing instability.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003
1. Veracx A, Raoult D. Biology and genetics of human head and body lice. Trends Parasitol. 2012;28:563-571. doi: 10.1016/j.pt.2012.09.003
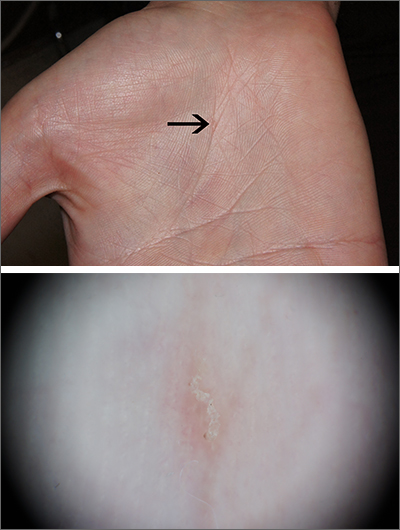
Intensely itchy normal skin
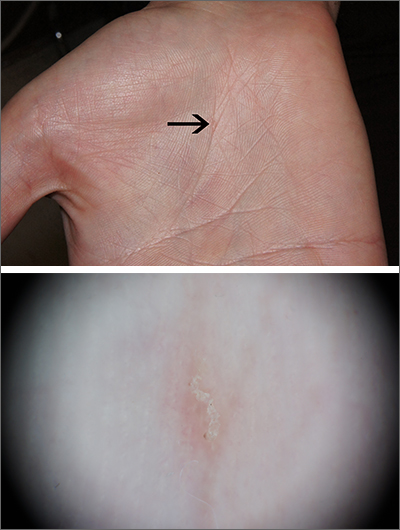
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
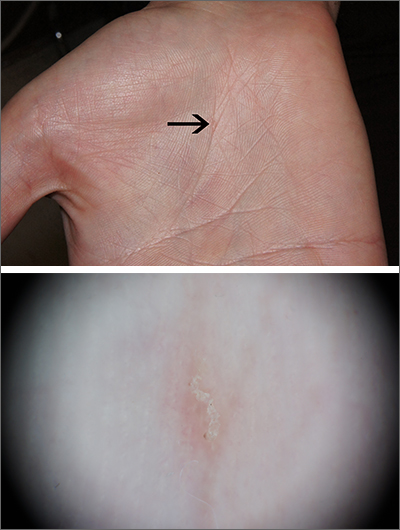
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Severe itching should prompt suspicion for scabies and the hands are the highest-yield location. In this patient’s case, there weren’t findings in the web spaces and, in general, skin findings were largely absent; dermoscopy confirmed the diagnosis of scabies.
Sarcoptes scabiei, is a parasitic mite that lives and reproduces in and on human skin and is transmitted by very close contact, either skin-to-skin or by living within a household or institution with shared linens and furnishings. After infection, itching develops within days to weeks from both the physical movement and burrowing of mites within the skin and from the allergic and inflammatory response to mite bodies and their waste.1 Symptoms and infections may persist for years in the absence of treatment.
Sometimes (as in this case), burrows are few and very subtle. More often, there are widespread burrows and excoriated papules over the hands, trunk, extremities, and genitals. A burrowed mite is often adjacent to, but not directly in, an excoriation. Dermoscopy has transformed the ability to diagnose this condition quickly by enabling clinicians to visualize the triangular shape of the head and front legs of a mite (called the “delta sign”). This localization allows easy microscopic confirmation by paring the mite from the skin with a small scalpel blade. (A #11 or #15 blade works very well.)
Topical permethrin 5% cream is highly curative. The cream should be applied from the top of the neck to the tips of the patient’s toes and left on for 8 hours; the process should be repeated a week later. Very close contacts (eg, symptomatic household members or sexual partners) should be treated concurrently. A 60 g tube will treat 1 adult twice. (A 60 g tube of permethrin with a refill, therefore, will treat 2 adults twice.) Oral ivermectin 3 mg dosed at 200 mcg/kg in a single dose repeated in 1 to 2 weeks is an alternative.
Outbreaks in an institutional setting present a significant challenge and require population-based control and often the assistance of infection control specialists or local public health officials. Often this involves weekly treatment with ivermectin for all potentially affected individuals for 3 to 4 weeks and surveillance for follow-up. While there is some resistance to ivermectin, many failures relate more to reinfection from unidentified sources.
This patient received topical permethrin 5% cream dosed as noted above. Itching can be expected to persist for 3 to 4 weeks, so topical triamcinolone 0.1% cream was prescribed as needed for itching on days when permethrin wasn’t applied. At 6 weeks, this patient’s symptoms had resolved.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
1. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021;25:95-101. doi: 10.1177/1203475420960446
Oral IL-23 receptor antagonist for psoriasis promising: Phase 2b study
SINGAPORE – across all doses, compared with placebo, according to results of the FRONTIER 1 trial.
In the 16-week phase 2b study, 255 adults with moderate to severe plaque psoriasis were randomly assigned into six treatment groups: placebo (n = 43), JNJ-2113 25 mg daily (n = 43), 25 mg twice daily (n = 41), 50 mg daily (n = 43), 100 mg daily (n = 43), or 100 mg twice daily (n = 42).
Of those who took the placebo, only 9.3% achieved the study’s primary endpoint of a 75% or greater improvement in the Psoriasis Area and Severity Index (PASI-75) by week 16. This was compared with 78.6% in the group that took the highest dose.
“Additionally, the onset of action was fairly fast: at week 4, more than 20% of patients had achieved PASI 75,” said Robert Bissonnette, MD, CEO of Innovaderm Research in Montreal, who presented the findings during a late-breaker session at the World Congress of Dermatology.
Patients in the remaining groups demonstrated a response that corresponded to dosing level: with 37.2%, 51.2%, 58.1%, and 65.1% achieving PASI-75 in the 25 mg daily, 25 mg twice-daily, 50 mg daily, and 100 mg daily groups, respectively.
“These results are very interesting because in terms of psoriasis treatment, if this is confirmed in phase 3, it would give us an oral alternative that would be selective for IL-23,” said Dr. Bissonnette, referring to the signaling pathway that plays a critical role in the pathogenesis of several immune-mediated inflammatory diseases, including plaque psoriasis.
Although rarely life-threatening, the skin disorder is often intractable to treatment. In recent years, therapies that block IL-23 signaling and downstream inflammatory cytokine production have proven useful. “We have on the market a number of biological agents targeting IL-23 that we use on a regular basis,” said Dr. Bissonnette. “However, there are currently no orally delivered therapies.”
If successful, JNJ-2113 – a first-in-class oral IL-23 antagonist peptide developed by Janssen – could change the treatment paradigm for patients with moderate to severe plaque psoriasis. “When I was first introduced to the concept, I thought it wouldn’t work as it’s a peptide, that it would be digested by the stomach,” he told the audience. “But because of its GI stability and its potency, when you administer it orally, you can detect pharmacological activity.”
A well-tolerated alternative
Participants in the FRONTIER 1 trial were on average about 44 years old and weighed 88.9 kg (195 lb). Most had been living with psoriasis for about 18 years, with a total PASI score of 19.05. In addition, 43.1% had been treated with phototherapy in the past, 22% with biologics, and 78.4% with systemics.
PASI 90 and 100 were among some of the secondary outcomes measured. Similar to the primary outcome of PASI 75, all treatment groups demonstrated a statistically significant dose-response in PASI 90, compared with placebo. For those on the highest dose of JNJ-2113, 59.5% and 40.5% achieved PASI 90 and PASI 100, respectively, by week 16. The corresponding figures for those receiving placebo were 2.3% and 0%.
The safety profile for JNJ-2113 across all doses was similar to that of placebo, with no evidence of a dose-dependent increase in the occurrence of adverse events (AEs). The most frequently reported AEs were COVID-19 and nasopharyngitis. There were three serious AEs (COVID-19, infected cyst, suicide attempt) among those on the active drug, but the investigators assessed that they were not related to the study intervention. No deaths, major adverse cardiac events, or malignancies were reported during the study.
Approached for an independent comment, Marius-Anton Ionescu, MD, PhD, from the University Hospital Saint Louis, Paris, who specializes in psoriasis, told this news organization that the new development with JNJ-2113 “is really promising.”
Treatment for plaque psoriasis has improved to the point where some biologics, such as risankizumab (Skyrizi), only require patients to have “four shots a year,” he says. “This is the future of psoriasis treatment; it might go down to two shots a year” – a regimen that will be easier than taking an oral medication once or twice a day.
“But it’s good to have an oral option because you will always have some patients who say: ‘Shots are not for me, I’m afraid,’ ” he says.
However, Dr. Ionescu noted that if JNJ-2113 were to pass phase 3 trials, it might face stiff competition from the selective tyrosine kinase 2 (TYK2) inhibitor deucravacitinib (Sotyktu), which the U.S. Food and Drug Administration approved for use in adults with moderate to severe plaque psoriasis last September. “It has very good results and is the first oral therapy that is comparable with biologics for plaque psoriasis,” he says.
But Dr. Bissonnette remains hopeful for the future. “I think JNJ-2113 goes way beyond psoriasis because this type of strategy using oral peptide–blocking receptors could be used in other immune-mediated diseases, including atopic dermatitis and other diseases outside of dermatology.” In addition to running a phase 3 study for moderate to severe plaque psoriasis, Janssen is planning to initiate a phase 2b clinical trial of JNJ-2113 in adults with ulcerative colitis.
The study was funded by Janssen. Dr. Bissonnette reports consulting and investigating for Janssen, and being on advisory panels and receiving research funding from multiple other pharmaceutical companies. Dr. Ionescu is an investigator for Psoriasis National Register France Psobioteq (no honoraria), and an investigator and speaker for Uriage cosmetics (honoraria).
A version of this article first appeared on Medscape.com.
SINGAPORE – across all doses, compared with placebo, according to results of the FRONTIER 1 trial.
In the 16-week phase 2b study, 255 adults with moderate to severe plaque psoriasis were randomly assigned into six treatment groups: placebo (n = 43), JNJ-2113 25 mg daily (n = 43), 25 mg twice daily (n = 41), 50 mg daily (n = 43), 100 mg daily (n = 43), or 100 mg twice daily (n = 42).
Of those who took the placebo, only 9.3% achieved the study’s primary endpoint of a 75% or greater improvement in the Psoriasis Area and Severity Index (PASI-75) by week 16. This was compared with 78.6% in the group that took the highest dose.
“Additionally, the onset of action was fairly fast: at week 4, more than 20% of patients had achieved PASI 75,” said Robert Bissonnette, MD, CEO of Innovaderm Research in Montreal, who presented the findings during a late-breaker session at the World Congress of Dermatology.
Patients in the remaining groups demonstrated a response that corresponded to dosing level: with 37.2%, 51.2%, 58.1%, and 65.1% achieving PASI-75 in the 25 mg daily, 25 mg twice-daily, 50 mg daily, and 100 mg daily groups, respectively.
“These results are very interesting because in terms of psoriasis treatment, if this is confirmed in phase 3, it would give us an oral alternative that would be selective for IL-23,” said Dr. Bissonnette, referring to the signaling pathway that plays a critical role in the pathogenesis of several immune-mediated inflammatory diseases, including plaque psoriasis.
Although rarely life-threatening, the skin disorder is often intractable to treatment. In recent years, therapies that block IL-23 signaling and downstream inflammatory cytokine production have proven useful. “We have on the market a number of biological agents targeting IL-23 that we use on a regular basis,” said Dr. Bissonnette. “However, there are currently no orally delivered therapies.”
If successful, JNJ-2113 – a first-in-class oral IL-23 antagonist peptide developed by Janssen – could change the treatment paradigm for patients with moderate to severe plaque psoriasis. “When I was first introduced to the concept, I thought it wouldn’t work as it’s a peptide, that it would be digested by the stomach,” he told the audience. “But because of its GI stability and its potency, when you administer it orally, you can detect pharmacological activity.”
A well-tolerated alternative
Participants in the FRONTIER 1 trial were on average about 44 years old and weighed 88.9 kg (195 lb). Most had been living with psoriasis for about 18 years, with a total PASI score of 19.05. In addition, 43.1% had been treated with phototherapy in the past, 22% with biologics, and 78.4% with systemics.
PASI 90 and 100 were among some of the secondary outcomes measured. Similar to the primary outcome of PASI 75, all treatment groups demonstrated a statistically significant dose-response in PASI 90, compared with placebo. For those on the highest dose of JNJ-2113, 59.5% and 40.5% achieved PASI 90 and PASI 100, respectively, by week 16. The corresponding figures for those receiving placebo were 2.3% and 0%.
The safety profile for JNJ-2113 across all doses was similar to that of placebo, with no evidence of a dose-dependent increase in the occurrence of adverse events (AEs). The most frequently reported AEs were COVID-19 and nasopharyngitis. There were three serious AEs (COVID-19, infected cyst, suicide attempt) among those on the active drug, but the investigators assessed that they were not related to the study intervention. No deaths, major adverse cardiac events, or malignancies were reported during the study.
Approached for an independent comment, Marius-Anton Ionescu, MD, PhD, from the University Hospital Saint Louis, Paris, who specializes in psoriasis, told this news organization that the new development with JNJ-2113 “is really promising.”
Treatment for plaque psoriasis has improved to the point where some biologics, such as risankizumab (Skyrizi), only require patients to have “four shots a year,” he says. “This is the future of psoriasis treatment; it might go down to two shots a year” – a regimen that will be easier than taking an oral medication once or twice a day.
“But it’s good to have an oral option because you will always have some patients who say: ‘Shots are not for me, I’m afraid,’ ” he says.
However, Dr. Ionescu noted that if JNJ-2113 were to pass phase 3 trials, it might face stiff competition from the selective tyrosine kinase 2 (TYK2) inhibitor deucravacitinib (Sotyktu), which the U.S. Food and Drug Administration approved for use in adults with moderate to severe plaque psoriasis last September. “It has very good results and is the first oral therapy that is comparable with biologics for plaque psoriasis,” he says.
But Dr. Bissonnette remains hopeful for the future. “I think JNJ-2113 goes way beyond psoriasis because this type of strategy using oral peptide–blocking receptors could be used in other immune-mediated diseases, including atopic dermatitis and other diseases outside of dermatology.” In addition to running a phase 3 study for moderate to severe plaque psoriasis, Janssen is planning to initiate a phase 2b clinical trial of JNJ-2113 in adults with ulcerative colitis.
The study was funded by Janssen. Dr. Bissonnette reports consulting and investigating for Janssen, and being on advisory panels and receiving research funding from multiple other pharmaceutical companies. Dr. Ionescu is an investigator for Psoriasis National Register France Psobioteq (no honoraria), and an investigator and speaker for Uriage cosmetics (honoraria).
A version of this article first appeared on Medscape.com.
SINGAPORE – across all doses, compared with placebo, according to results of the FRONTIER 1 trial.
In the 16-week phase 2b study, 255 adults with moderate to severe plaque psoriasis were randomly assigned into six treatment groups: placebo (n = 43), JNJ-2113 25 mg daily (n = 43), 25 mg twice daily (n = 41), 50 mg daily (n = 43), 100 mg daily (n = 43), or 100 mg twice daily (n = 42).
Of those who took the placebo, only 9.3% achieved the study’s primary endpoint of a 75% or greater improvement in the Psoriasis Area and Severity Index (PASI-75) by week 16. This was compared with 78.6% in the group that took the highest dose.
“Additionally, the onset of action was fairly fast: at week 4, more than 20% of patients had achieved PASI 75,” said Robert Bissonnette, MD, CEO of Innovaderm Research in Montreal, who presented the findings during a late-breaker session at the World Congress of Dermatology.
Patients in the remaining groups demonstrated a response that corresponded to dosing level: with 37.2%, 51.2%, 58.1%, and 65.1% achieving PASI-75 in the 25 mg daily, 25 mg twice-daily, 50 mg daily, and 100 mg daily groups, respectively.
“These results are very interesting because in terms of psoriasis treatment, if this is confirmed in phase 3, it would give us an oral alternative that would be selective for IL-23,” said Dr. Bissonnette, referring to the signaling pathway that plays a critical role in the pathogenesis of several immune-mediated inflammatory diseases, including plaque psoriasis.
Although rarely life-threatening, the skin disorder is often intractable to treatment. In recent years, therapies that block IL-23 signaling and downstream inflammatory cytokine production have proven useful. “We have on the market a number of biological agents targeting IL-23 that we use on a regular basis,” said Dr. Bissonnette. “However, there are currently no orally delivered therapies.”
If successful, JNJ-2113 – a first-in-class oral IL-23 antagonist peptide developed by Janssen – could change the treatment paradigm for patients with moderate to severe plaque psoriasis. “When I was first introduced to the concept, I thought it wouldn’t work as it’s a peptide, that it would be digested by the stomach,” he told the audience. “But because of its GI stability and its potency, when you administer it orally, you can detect pharmacological activity.”
A well-tolerated alternative
Participants in the FRONTIER 1 trial were on average about 44 years old and weighed 88.9 kg (195 lb). Most had been living with psoriasis for about 18 years, with a total PASI score of 19.05. In addition, 43.1% had been treated with phototherapy in the past, 22% with biologics, and 78.4% with systemics.
PASI 90 and 100 were among some of the secondary outcomes measured. Similar to the primary outcome of PASI 75, all treatment groups demonstrated a statistically significant dose-response in PASI 90, compared with placebo. For those on the highest dose of JNJ-2113, 59.5% and 40.5% achieved PASI 90 and PASI 100, respectively, by week 16. The corresponding figures for those receiving placebo were 2.3% and 0%.
The safety profile for JNJ-2113 across all doses was similar to that of placebo, with no evidence of a dose-dependent increase in the occurrence of adverse events (AEs). The most frequently reported AEs were COVID-19 and nasopharyngitis. There were three serious AEs (COVID-19, infected cyst, suicide attempt) among those on the active drug, but the investigators assessed that they were not related to the study intervention. No deaths, major adverse cardiac events, or malignancies were reported during the study.
Approached for an independent comment, Marius-Anton Ionescu, MD, PhD, from the University Hospital Saint Louis, Paris, who specializes in psoriasis, told this news organization that the new development with JNJ-2113 “is really promising.”
Treatment for plaque psoriasis has improved to the point where some biologics, such as risankizumab (Skyrizi), only require patients to have “four shots a year,” he says. “This is the future of psoriasis treatment; it might go down to two shots a year” – a regimen that will be easier than taking an oral medication once or twice a day.
“But it’s good to have an oral option because you will always have some patients who say: ‘Shots are not for me, I’m afraid,’ ” he says.
However, Dr. Ionescu noted that if JNJ-2113 were to pass phase 3 trials, it might face stiff competition from the selective tyrosine kinase 2 (TYK2) inhibitor deucravacitinib (Sotyktu), which the U.S. Food and Drug Administration approved for use in adults with moderate to severe plaque psoriasis last September. “It has very good results and is the first oral therapy that is comparable with biologics for plaque psoriasis,” he says.
But Dr. Bissonnette remains hopeful for the future. “I think JNJ-2113 goes way beyond psoriasis because this type of strategy using oral peptide–blocking receptors could be used in other immune-mediated diseases, including atopic dermatitis and other diseases outside of dermatology.” In addition to running a phase 3 study for moderate to severe plaque psoriasis, Janssen is planning to initiate a phase 2b clinical trial of JNJ-2113 in adults with ulcerative colitis.
The study was funded by Janssen. Dr. Bissonnette reports consulting and investigating for Janssen, and being on advisory panels and receiving research funding from multiple other pharmaceutical companies. Dr. Ionescu is an investigator for Psoriasis National Register France Psobioteq (no honoraria), and an investigator and speaker for Uriage cosmetics (honoraria).
A version of this article first appeared on Medscape.com.
AT WCD 2023
JAK inhibitors efficacious for atopic dermatitis in Asian patients, study finds
SINGAPORE – conducted in Singapore has found.
“Abrocitinib and upadacitinib surprisingly appeared to have better treatment efficacy compared to baricitinib,” said study lead Yik Weng Yew, MD, PhD, MPH, deputy head of research at Singapore’s National Skin Centre (NSC), who presented the results at the 25th World Congress of Dermatology. “But overall, as a group, I think they show a very good treatment response, as well as a good effect on itch response.”
JAK inhibitors are used to treat a variety of inflammatory diseases including alopecia areata, rheumatoid arthritis, and inflammatory bowel disease. Although treatment for severe eczema was previously limited to topical steroids and oral immunosuppressants, there are now two oral JAK inhibitors – abrocitinib and upadacitinib – approved in 2022 by the Food and Drug Administration for treating AD, which affects up to 2.4% of the global population. (A topical formulation of ruxolitinib, a JAK inhibitor, was approved for AD in 2021.)
The Singapore study is one of the few that have examined the safety and efficacy of JAK inhibitors for treatment of AD in a non-White population.
Chinese population
For the 12-week trial, conducted in 2022, Dr. Yew and associates recruited 35 patients from the NSC. More than half of participants (64%) were men and most (96%) were of Chinese ethnicity. Four of every five patients had previously received systemic agents: 17% had been treated with one systemic agent, 18.9% with two, 15.1% with three, 22.6% with four, and 3.8% with five. The most commonly used agents were cyclosporine (62.3%), methotrexate (47.2%), azathioprine (39.6%), and dupilumab (35.8%).
“The switch in therapy could have been a result of inadequate efficacy or cost reasons because in Singapore patients pay out of pocket for AD treatments,” said Dr. Yew.
Additionally, he offered a caveat on the profile of participants: “Perhaps they were more difficult atopic eczema patients, and therefore, the efficacy [of JAK inhibitors] might be a bit different.”
Clearer skin, less itch
Patients received one of the three study drugs: baricitinib (66%), abrocitinib (21%), and upadacitinib (13%). The distribution was “affected by reimbursement patterns and availability of the drug,” explained Dr. Yew.
They were assessed at weeks 4 and 12. By study end, the proportion of patients who self-reported an improvement in their condition was 100% for upadacitinib, 90% for abrocitinib, and 69% for baricitinib.
Scores on the Investigator Global Assessment (IGA) also improved with treatment. Patients in the baricitinib group saw their mean score fall from 4.0 to 3.0 by week 4, then to 2.0 by week 12. With upadacitinib and abrocitinib, “you can see that there is a nice decrease in IGA responses,” said Dr. Yew, referring to the larger improvement in scores experienced by patients on those two treatments. For patients on upadacitinib, IGA decreased from 3.5 to 2 at 4 weeks, then to 0.5 at 12 weeks, while those taking abrocitinib had their scores drop from 4.0 to 2.0 at 4 weeks, then to 1.0 at 12 weeks.
When it came to itch reduction, the abrocitinib group experienced the biggest reduction, with a median reduction of 5.5 points in itch score. Median reduction in itch score was 4 points for the other two groups. “Oral JAK inhibitors appear to have a good effect on itch response,” said Dr. Yew.
However, the researchers observed no significant reduction in percentage of body surface area affected, the last outcome assessed.
The most commonly reported adverse events were increased creatine kinase levels (11.3% of patients), increased LDL cholesterol levels (9.4%), and herpes zoster (9.4%). Those in the abrocitinib reported a higher number of these adverse events, compared with the other two treatment groups. (There were no herpes zoster cases among those taking baricitinib.)
For herpes zoster, Dr. Yew said “the common recommendation” is to give the inactivated shingles vaccine. “But the problem is that, number one, these patients would have probably failed multiple agents so they probably can’t wait for you to vaccinate before you initiate treatment.”
In addition, people in Singapore have to pay out-of-pocket for the two vaccine doses, “which is probably a month’s worth of medication,” he noted. “So we have a lot of resistance from patients.”
Additionally, Dr. Yew noted that contrary to what has previously been reported in the literature, there were few complaints of acne as a side effect in the Singaporean study population.
Toward greater representation
Dr. Yew pointed out that the study was limited by a few factors: neither the Eczema Area and Severity Index or Scoring of Atopic Dermatitis index data was used, and the study population was small and not representative of the real world.
Still, the new findings contribute to the overall safety and efficacy profile of JAK inhibitors in AD, which has so far been scarce in non-White populations.
“In Western studies, unfortunately, the representation of the population of skin of color or different ethnicities is underrepresented,” said Yousef Binamer, MD, chair of the dermatology department at King Faisal Specialist Hospital, Riyadh, Saudi Arabia, when approached for an independent comment on the results.
“This is now why researchers are looking into specific groups to study them,” which he pointed out, is crucial because “the immunophenotyping of AD is different for each background.”
The incidence and severity of AD tend to be higher in Asian and Middle Eastern populations, for instance, he noted. “It’s very common in Asia, and not so common in very white skin. I did my training in Canada so I see the difference,” said Dr. Binamer. “Asian people tend to be more itchy and have a tendency to scar on pigmentation.” Whereas White people “usually do not have this issue.”
“So I think real-world evidence of JAK inhibitors in the other populations is important,” he said. Studies such as the one conducted in Singapore, as well as the recently reported QUARTZ3 study, which examined the use of the JAK inhibitor ivarmacitinib in 256 Chinese patients with AD, are helping to pave the way.
The study was independently supported. Dr. Yew and Dr. Binamer have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SINGAPORE – conducted in Singapore has found.
“Abrocitinib and upadacitinib surprisingly appeared to have better treatment efficacy compared to baricitinib,” said study lead Yik Weng Yew, MD, PhD, MPH, deputy head of research at Singapore’s National Skin Centre (NSC), who presented the results at the 25th World Congress of Dermatology. “But overall, as a group, I think they show a very good treatment response, as well as a good effect on itch response.”
JAK inhibitors are used to treat a variety of inflammatory diseases including alopecia areata, rheumatoid arthritis, and inflammatory bowel disease. Although treatment for severe eczema was previously limited to topical steroids and oral immunosuppressants, there are now two oral JAK inhibitors – abrocitinib and upadacitinib – approved in 2022 by the Food and Drug Administration for treating AD, which affects up to 2.4% of the global population. (A topical formulation of ruxolitinib, a JAK inhibitor, was approved for AD in 2021.)
The Singapore study is one of the few that have examined the safety and efficacy of JAK inhibitors for treatment of AD in a non-White population.
Chinese population
For the 12-week trial, conducted in 2022, Dr. Yew and associates recruited 35 patients from the NSC. More than half of participants (64%) were men and most (96%) were of Chinese ethnicity. Four of every five patients had previously received systemic agents: 17% had been treated with one systemic agent, 18.9% with two, 15.1% with three, 22.6% with four, and 3.8% with five. The most commonly used agents were cyclosporine (62.3%), methotrexate (47.2%), azathioprine (39.6%), and dupilumab (35.8%).
“The switch in therapy could have been a result of inadequate efficacy or cost reasons because in Singapore patients pay out of pocket for AD treatments,” said Dr. Yew.
Additionally, he offered a caveat on the profile of participants: “Perhaps they were more difficult atopic eczema patients, and therefore, the efficacy [of JAK inhibitors] might be a bit different.”
Clearer skin, less itch
Patients received one of the three study drugs: baricitinib (66%), abrocitinib (21%), and upadacitinib (13%). The distribution was “affected by reimbursement patterns and availability of the drug,” explained Dr. Yew.
They were assessed at weeks 4 and 12. By study end, the proportion of patients who self-reported an improvement in their condition was 100% for upadacitinib, 90% for abrocitinib, and 69% for baricitinib.
Scores on the Investigator Global Assessment (IGA) also improved with treatment. Patients in the baricitinib group saw their mean score fall from 4.0 to 3.0 by week 4, then to 2.0 by week 12. With upadacitinib and abrocitinib, “you can see that there is a nice decrease in IGA responses,” said Dr. Yew, referring to the larger improvement in scores experienced by patients on those two treatments. For patients on upadacitinib, IGA decreased from 3.5 to 2 at 4 weeks, then to 0.5 at 12 weeks, while those taking abrocitinib had their scores drop from 4.0 to 2.0 at 4 weeks, then to 1.0 at 12 weeks.
When it came to itch reduction, the abrocitinib group experienced the biggest reduction, with a median reduction of 5.5 points in itch score. Median reduction in itch score was 4 points for the other two groups. “Oral JAK inhibitors appear to have a good effect on itch response,” said Dr. Yew.
However, the researchers observed no significant reduction in percentage of body surface area affected, the last outcome assessed.
The most commonly reported adverse events were increased creatine kinase levels (11.3% of patients), increased LDL cholesterol levels (9.4%), and herpes zoster (9.4%). Those in the abrocitinib reported a higher number of these adverse events, compared with the other two treatment groups. (There were no herpes zoster cases among those taking baricitinib.)
For herpes zoster, Dr. Yew said “the common recommendation” is to give the inactivated shingles vaccine. “But the problem is that, number one, these patients would have probably failed multiple agents so they probably can’t wait for you to vaccinate before you initiate treatment.”
In addition, people in Singapore have to pay out-of-pocket for the two vaccine doses, “which is probably a month’s worth of medication,” he noted. “So we have a lot of resistance from patients.”
Additionally, Dr. Yew noted that contrary to what has previously been reported in the literature, there were few complaints of acne as a side effect in the Singaporean study population.
Toward greater representation
Dr. Yew pointed out that the study was limited by a few factors: neither the Eczema Area and Severity Index or Scoring of Atopic Dermatitis index data was used, and the study population was small and not representative of the real world.
Still, the new findings contribute to the overall safety and efficacy profile of JAK inhibitors in AD, which has so far been scarce in non-White populations.
“In Western studies, unfortunately, the representation of the population of skin of color or different ethnicities is underrepresented,” said Yousef Binamer, MD, chair of the dermatology department at King Faisal Specialist Hospital, Riyadh, Saudi Arabia, when approached for an independent comment on the results.
“This is now why researchers are looking into specific groups to study them,” which he pointed out, is crucial because “the immunophenotyping of AD is different for each background.”
The incidence and severity of AD tend to be higher in Asian and Middle Eastern populations, for instance, he noted. “It’s very common in Asia, and not so common in very white skin. I did my training in Canada so I see the difference,” said Dr. Binamer. “Asian people tend to be more itchy and have a tendency to scar on pigmentation.” Whereas White people “usually do not have this issue.”
“So I think real-world evidence of JAK inhibitors in the other populations is important,” he said. Studies such as the one conducted in Singapore, as well as the recently reported QUARTZ3 study, which examined the use of the JAK inhibitor ivarmacitinib in 256 Chinese patients with AD, are helping to pave the way.
The study was independently supported. Dr. Yew and Dr. Binamer have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SINGAPORE – conducted in Singapore has found.
“Abrocitinib and upadacitinib surprisingly appeared to have better treatment efficacy compared to baricitinib,” said study lead Yik Weng Yew, MD, PhD, MPH, deputy head of research at Singapore’s National Skin Centre (NSC), who presented the results at the 25th World Congress of Dermatology. “But overall, as a group, I think they show a very good treatment response, as well as a good effect on itch response.”
JAK inhibitors are used to treat a variety of inflammatory diseases including alopecia areata, rheumatoid arthritis, and inflammatory bowel disease. Although treatment for severe eczema was previously limited to topical steroids and oral immunosuppressants, there are now two oral JAK inhibitors – abrocitinib and upadacitinib – approved in 2022 by the Food and Drug Administration for treating AD, which affects up to 2.4% of the global population. (A topical formulation of ruxolitinib, a JAK inhibitor, was approved for AD in 2021.)
The Singapore study is one of the few that have examined the safety and efficacy of JAK inhibitors for treatment of AD in a non-White population.
Chinese population
For the 12-week trial, conducted in 2022, Dr. Yew and associates recruited 35 patients from the NSC. More than half of participants (64%) were men and most (96%) were of Chinese ethnicity. Four of every five patients had previously received systemic agents: 17% had been treated with one systemic agent, 18.9% with two, 15.1% with three, 22.6% with four, and 3.8% with five. The most commonly used agents were cyclosporine (62.3%), methotrexate (47.2%), azathioprine (39.6%), and dupilumab (35.8%).
“The switch in therapy could have been a result of inadequate efficacy or cost reasons because in Singapore patients pay out of pocket for AD treatments,” said Dr. Yew.
Additionally, he offered a caveat on the profile of participants: “Perhaps they were more difficult atopic eczema patients, and therefore, the efficacy [of JAK inhibitors] might be a bit different.”
Clearer skin, less itch
Patients received one of the three study drugs: baricitinib (66%), abrocitinib (21%), and upadacitinib (13%). The distribution was “affected by reimbursement patterns and availability of the drug,” explained Dr. Yew.
They were assessed at weeks 4 and 12. By study end, the proportion of patients who self-reported an improvement in their condition was 100% for upadacitinib, 90% for abrocitinib, and 69% for baricitinib.
Scores on the Investigator Global Assessment (IGA) also improved with treatment. Patients in the baricitinib group saw their mean score fall from 4.0 to 3.0 by week 4, then to 2.0 by week 12. With upadacitinib and abrocitinib, “you can see that there is a nice decrease in IGA responses,” said Dr. Yew, referring to the larger improvement in scores experienced by patients on those two treatments. For patients on upadacitinib, IGA decreased from 3.5 to 2 at 4 weeks, then to 0.5 at 12 weeks, while those taking abrocitinib had their scores drop from 4.0 to 2.0 at 4 weeks, then to 1.0 at 12 weeks.
When it came to itch reduction, the abrocitinib group experienced the biggest reduction, with a median reduction of 5.5 points in itch score. Median reduction in itch score was 4 points for the other two groups. “Oral JAK inhibitors appear to have a good effect on itch response,” said Dr. Yew.
However, the researchers observed no significant reduction in percentage of body surface area affected, the last outcome assessed.
The most commonly reported adverse events were increased creatine kinase levels (11.3% of patients), increased LDL cholesterol levels (9.4%), and herpes zoster (9.4%). Those in the abrocitinib reported a higher number of these adverse events, compared with the other two treatment groups. (There were no herpes zoster cases among those taking baricitinib.)
For herpes zoster, Dr. Yew said “the common recommendation” is to give the inactivated shingles vaccine. “But the problem is that, number one, these patients would have probably failed multiple agents so they probably can’t wait for you to vaccinate before you initiate treatment.”
In addition, people in Singapore have to pay out-of-pocket for the two vaccine doses, “which is probably a month’s worth of medication,” he noted. “So we have a lot of resistance from patients.”
Additionally, Dr. Yew noted that contrary to what has previously been reported in the literature, there were few complaints of acne as a side effect in the Singaporean study population.
Toward greater representation
Dr. Yew pointed out that the study was limited by a few factors: neither the Eczema Area and Severity Index or Scoring of Atopic Dermatitis index data was used, and the study population was small and not representative of the real world.
Still, the new findings contribute to the overall safety and efficacy profile of JAK inhibitors in AD, which has so far been scarce in non-White populations.
“In Western studies, unfortunately, the representation of the population of skin of color or different ethnicities is underrepresented,” said Yousef Binamer, MD, chair of the dermatology department at King Faisal Specialist Hospital, Riyadh, Saudi Arabia, when approached for an independent comment on the results.
“This is now why researchers are looking into specific groups to study them,” which he pointed out, is crucial because “the immunophenotyping of AD is different for each background.”
The incidence and severity of AD tend to be higher in Asian and Middle Eastern populations, for instance, he noted. “It’s very common in Asia, and not so common in very white skin. I did my training in Canada so I see the difference,” said Dr. Binamer. “Asian people tend to be more itchy and have a tendency to scar on pigmentation.” Whereas White people “usually do not have this issue.”
“So I think real-world evidence of JAK inhibitors in the other populations is important,” he said. Studies such as the one conducted in Singapore, as well as the recently reported QUARTZ3 study, which examined the use of the JAK inhibitor ivarmacitinib in 256 Chinese patients with AD, are helping to pave the way.
The study was independently supported. Dr. Yew and Dr. Binamer have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT WCD 2023
Study finds subcutaneous spesolimab reduces flares in patients with GPP
SINGAPORE – presented in a late-breaker session at the World Congress of Dermatology,
In the phase 2b study, patients who received the high-dose regimen (a 600-mg subcutaneous loading dose, then 300-mg SC every 4 weeks) of spesolimab experienced 84% fewer GPP fares over 48 weeks, compared with those on placebo, reported Bruce Strober, MD, PhD, Central Connecticut Dermatology, Cromwell, and clinical professor of dermatology, Yale University, New Haven, Conn. “Additionally, no flares occurred after week 4, and this, in turn, translated into improved patient outcomes.”
GPP is a rare, chronic, systemic neutrophilic skin disease. The resulting flares, characterized by painful pustules all over the body, can lead to sepsis, shock, and other life-threatening complications. “People who have it are considerably burdened by it, so targeted therapy of this disease is incredibly important because it leads to lessened morbidity and, importantly, mortality for these patients,” Dr. Strober said.
“It’s important not only to treat the flares but also to prevent them,” he noted.
The intravenous formulation of spesolimab (Spevigo) was approved for the treatment of GPP flares in adults by the Food and Drug Administration in September 2022. It is now authorized in nearly 40 countries, including Japan, China, and the European Union.
The phase 2 Effisayil 2 study presented at the meeting evaluated the subcutaneous formulation of spesolimab. Data on subcutaneous spesolimab has been submitted to the FDA, and has received breakthrough therapy designation, according to the manufacturer, Boehringer Ingelheim.
Flare prevention
In the study, 123 patients with GPP were randomly assigned 1:1:1:1 to one of four groups: high-dose spesolimab, medium-dose (600-mg SC loading dose, then 300-mg SC every 12 weeks), low-dose (300-mg SC loading dose, then 150-mg SC every 12 weeks), or placebo. In the event of a flare during the randomized treatment period, a patient was administered a single, 900-mg intravenous dose of spesolimab.
Nearly two-thirds of the participants were female and nearly two-thirds were Asian, with a mean age of about 39-43 years.
The mean numbers of GPP flares experienced annually by those in the low-, medium-, and high-dose spesolimab groups were 2.7, 1.9, and 2.4, respectively (2.4% in the placebo group). Fewer than a third had concurrent plaque psoriasis at baseline. Most (48.4%-63.3%) did not have an IL-36RN mutation.
Additionally, the Generalized Pustular Psoriasis Physician Global Assessment total score was 1 in 74.2%-93.5% of participants, and 0 in the remainder.
The primary study endpoint was the time to GPP flare by week 48. The risk of developing a flare among those on high-dose spesolimab was 84% lower, compared with that of those on placebo (hazard ratio, 0.16; 95% confidence interval, 0.05-0.54; P = .0005). No patients on the high dose had a flare after the 4th week of the study.
Similarly, for the secondary endpoint (occurrence of at least one GPP flare by week 48). Dr. Strober and his colleagues reported that high-dose spesolimab was superior to placebo with a risk difference of -39% (95% CI, –0.62 to –0.16; P = .0013). By contrast, the risk differences for the medium- and low-dose spesolimab arms were –0.23 (95% CI, –0.46 to 0.01) and -0.31 (95% CI, –0.54 to –0.08), respectively.
The safety profile of subcutaneous spesolimab across all three doses was similar to that of placebo, and there was no dose-dependent trend. Reported adverse events (AEs) were mild. There were five (5.4%) AEs leading to discontinuation of the drug in the medium- and high-dose groups, but none in the low-dose group. Overall, there were nine (9.7%) serious AEs reported in the spesolimab groups, and three (10%) in the high-dose group; no deaths occurred on any dose.
Participants most often reported injection-site erythema, reported in 13 (14%) of the patients on spesolimab versus 1 (3.3%) of those on placebo.
“Overall, the study demonstrates that subcutaneous spesolimab is effective at controlling GPP flares, especially at a high dose relative to placebo, and supports subcutaneous spesolimab for the therapy for GPP flare prevention,” Dr. Strober said at the meeting.
Targeting the IL-36 pathway
In a comment, Todd Schlesinger, MD, Clinical Research Center of the Carolinas, Charleston, S.C., who moderated the session, said: “It’s very exciting to be able to have a subcutaneous version of the medication.”
“I think the IL-36 is a great pathway,” he said, referring to the signaling pathway within the immune system that is central to the pathogenesis of GPP and several other autoinflammatory diseases.
However, Dr. Schlesinger said that he would have liked to have seen data on how many patients ended up treated with intravenous spesolimab.
He added that he would like future studies of subcutaneous spesolimab to examine the effect in different populations that vary by parameters such as weight, race, and disease severity. “Just seeing how somebody who’s flaring five times a year and you give them this medication and they’re now flaring once a year – that’s interesting data that we might like to know in the future.”
Other than for preventing GPP flares, spesolimab is being studied for treating other IL-36–mediated skin diseases, such as palmoplantar pustulosis.
The study was funded by Boehringer Ingelheim; both Dr. Strober and Dr. Schlesinger do research and consulting for BI, and receive funding from multiple other pharmaceutical companies.
A version of this article first appeared on Medscape.com.
SINGAPORE – presented in a late-breaker session at the World Congress of Dermatology,
In the phase 2b study, patients who received the high-dose regimen (a 600-mg subcutaneous loading dose, then 300-mg SC every 4 weeks) of spesolimab experienced 84% fewer GPP fares over 48 weeks, compared with those on placebo, reported Bruce Strober, MD, PhD, Central Connecticut Dermatology, Cromwell, and clinical professor of dermatology, Yale University, New Haven, Conn. “Additionally, no flares occurred after week 4, and this, in turn, translated into improved patient outcomes.”
GPP is a rare, chronic, systemic neutrophilic skin disease. The resulting flares, characterized by painful pustules all over the body, can lead to sepsis, shock, and other life-threatening complications. “People who have it are considerably burdened by it, so targeted therapy of this disease is incredibly important because it leads to lessened morbidity and, importantly, mortality for these patients,” Dr. Strober said.
“It’s important not only to treat the flares but also to prevent them,” he noted.
The intravenous formulation of spesolimab (Spevigo) was approved for the treatment of GPP flares in adults by the Food and Drug Administration in September 2022. It is now authorized in nearly 40 countries, including Japan, China, and the European Union.
The phase 2 Effisayil 2 study presented at the meeting evaluated the subcutaneous formulation of spesolimab. Data on subcutaneous spesolimab has been submitted to the FDA, and has received breakthrough therapy designation, according to the manufacturer, Boehringer Ingelheim.
Flare prevention
In the study, 123 patients with GPP were randomly assigned 1:1:1:1 to one of four groups: high-dose spesolimab, medium-dose (600-mg SC loading dose, then 300-mg SC every 12 weeks), low-dose (300-mg SC loading dose, then 150-mg SC every 12 weeks), or placebo. In the event of a flare during the randomized treatment period, a patient was administered a single, 900-mg intravenous dose of spesolimab.
Nearly two-thirds of the participants were female and nearly two-thirds were Asian, with a mean age of about 39-43 years.
The mean numbers of GPP flares experienced annually by those in the low-, medium-, and high-dose spesolimab groups were 2.7, 1.9, and 2.4, respectively (2.4% in the placebo group). Fewer than a third had concurrent plaque psoriasis at baseline. Most (48.4%-63.3%) did not have an IL-36RN mutation.
Additionally, the Generalized Pustular Psoriasis Physician Global Assessment total score was 1 in 74.2%-93.5% of participants, and 0 in the remainder.
The primary study endpoint was the time to GPP flare by week 48. The risk of developing a flare among those on high-dose spesolimab was 84% lower, compared with that of those on placebo (hazard ratio, 0.16; 95% confidence interval, 0.05-0.54; P = .0005). No patients on the high dose had a flare after the 4th week of the study.
Similarly, for the secondary endpoint (occurrence of at least one GPP flare by week 48). Dr. Strober and his colleagues reported that high-dose spesolimab was superior to placebo with a risk difference of -39% (95% CI, –0.62 to –0.16; P = .0013). By contrast, the risk differences for the medium- and low-dose spesolimab arms were –0.23 (95% CI, –0.46 to 0.01) and -0.31 (95% CI, –0.54 to –0.08), respectively.
The safety profile of subcutaneous spesolimab across all three doses was similar to that of placebo, and there was no dose-dependent trend. Reported adverse events (AEs) were mild. There were five (5.4%) AEs leading to discontinuation of the drug in the medium- and high-dose groups, but none in the low-dose group. Overall, there were nine (9.7%) serious AEs reported in the spesolimab groups, and three (10%) in the high-dose group; no deaths occurred on any dose.
Participants most often reported injection-site erythema, reported in 13 (14%) of the patients on spesolimab versus 1 (3.3%) of those on placebo.
“Overall, the study demonstrates that subcutaneous spesolimab is effective at controlling GPP flares, especially at a high dose relative to placebo, and supports subcutaneous spesolimab for the therapy for GPP flare prevention,” Dr. Strober said at the meeting.
Targeting the IL-36 pathway
In a comment, Todd Schlesinger, MD, Clinical Research Center of the Carolinas, Charleston, S.C., who moderated the session, said: “It’s very exciting to be able to have a subcutaneous version of the medication.”
“I think the IL-36 is a great pathway,” he said, referring to the signaling pathway within the immune system that is central to the pathogenesis of GPP and several other autoinflammatory diseases.
However, Dr. Schlesinger said that he would have liked to have seen data on how many patients ended up treated with intravenous spesolimab.
He added that he would like future studies of subcutaneous spesolimab to examine the effect in different populations that vary by parameters such as weight, race, and disease severity. “Just seeing how somebody who’s flaring five times a year and you give them this medication and they’re now flaring once a year – that’s interesting data that we might like to know in the future.”
Other than for preventing GPP flares, spesolimab is being studied for treating other IL-36–mediated skin diseases, such as palmoplantar pustulosis.
The study was funded by Boehringer Ingelheim; both Dr. Strober and Dr. Schlesinger do research and consulting for BI, and receive funding from multiple other pharmaceutical companies.
A version of this article first appeared on Medscape.com.
SINGAPORE – presented in a late-breaker session at the World Congress of Dermatology,
In the phase 2b study, patients who received the high-dose regimen (a 600-mg subcutaneous loading dose, then 300-mg SC every 4 weeks) of spesolimab experienced 84% fewer GPP fares over 48 weeks, compared with those on placebo, reported Bruce Strober, MD, PhD, Central Connecticut Dermatology, Cromwell, and clinical professor of dermatology, Yale University, New Haven, Conn. “Additionally, no flares occurred after week 4, and this, in turn, translated into improved patient outcomes.”
GPP is a rare, chronic, systemic neutrophilic skin disease. The resulting flares, characterized by painful pustules all over the body, can lead to sepsis, shock, and other life-threatening complications. “People who have it are considerably burdened by it, so targeted therapy of this disease is incredibly important because it leads to lessened morbidity and, importantly, mortality for these patients,” Dr. Strober said.
“It’s important not only to treat the flares but also to prevent them,” he noted.
The intravenous formulation of spesolimab (Spevigo) was approved for the treatment of GPP flares in adults by the Food and Drug Administration in September 2022. It is now authorized in nearly 40 countries, including Japan, China, and the European Union.
The phase 2 Effisayil 2 study presented at the meeting evaluated the subcutaneous formulation of spesolimab. Data on subcutaneous spesolimab has been submitted to the FDA, and has received breakthrough therapy designation, according to the manufacturer, Boehringer Ingelheim.
Flare prevention
In the study, 123 patients with GPP were randomly assigned 1:1:1:1 to one of four groups: high-dose spesolimab, medium-dose (600-mg SC loading dose, then 300-mg SC every 12 weeks), low-dose (300-mg SC loading dose, then 150-mg SC every 12 weeks), or placebo. In the event of a flare during the randomized treatment period, a patient was administered a single, 900-mg intravenous dose of spesolimab.
Nearly two-thirds of the participants were female and nearly two-thirds were Asian, with a mean age of about 39-43 years.
The mean numbers of GPP flares experienced annually by those in the low-, medium-, and high-dose spesolimab groups were 2.7, 1.9, and 2.4, respectively (2.4% in the placebo group). Fewer than a third had concurrent plaque psoriasis at baseline. Most (48.4%-63.3%) did not have an IL-36RN mutation.
Additionally, the Generalized Pustular Psoriasis Physician Global Assessment total score was 1 in 74.2%-93.5% of participants, and 0 in the remainder.
The primary study endpoint was the time to GPP flare by week 48. The risk of developing a flare among those on high-dose spesolimab was 84% lower, compared with that of those on placebo (hazard ratio, 0.16; 95% confidence interval, 0.05-0.54; P = .0005). No patients on the high dose had a flare after the 4th week of the study.
Similarly, for the secondary endpoint (occurrence of at least one GPP flare by week 48). Dr. Strober and his colleagues reported that high-dose spesolimab was superior to placebo with a risk difference of -39% (95% CI, –0.62 to –0.16; P = .0013). By contrast, the risk differences for the medium- and low-dose spesolimab arms were –0.23 (95% CI, –0.46 to 0.01) and -0.31 (95% CI, –0.54 to –0.08), respectively.
The safety profile of subcutaneous spesolimab across all three doses was similar to that of placebo, and there was no dose-dependent trend. Reported adverse events (AEs) were mild. There were five (5.4%) AEs leading to discontinuation of the drug in the medium- and high-dose groups, but none in the low-dose group. Overall, there were nine (9.7%) serious AEs reported in the spesolimab groups, and three (10%) in the high-dose group; no deaths occurred on any dose.
Participants most often reported injection-site erythema, reported in 13 (14%) of the patients on spesolimab versus 1 (3.3%) of those on placebo.
“Overall, the study demonstrates that subcutaneous spesolimab is effective at controlling GPP flares, especially at a high dose relative to placebo, and supports subcutaneous spesolimab for the therapy for GPP flare prevention,” Dr. Strober said at the meeting.
Targeting the IL-36 pathway
In a comment, Todd Schlesinger, MD, Clinical Research Center of the Carolinas, Charleston, S.C., who moderated the session, said: “It’s very exciting to be able to have a subcutaneous version of the medication.”
“I think the IL-36 is a great pathway,” he said, referring to the signaling pathway within the immune system that is central to the pathogenesis of GPP and several other autoinflammatory diseases.
However, Dr. Schlesinger said that he would have liked to have seen data on how many patients ended up treated with intravenous spesolimab.
He added that he would like future studies of subcutaneous spesolimab to examine the effect in different populations that vary by parameters such as weight, race, and disease severity. “Just seeing how somebody who’s flaring five times a year and you give them this medication and they’re now flaring once a year – that’s interesting data that we might like to know in the future.”
Other than for preventing GPP flares, spesolimab is being studied for treating other IL-36–mediated skin diseases, such as palmoplantar pustulosis.
The study was funded by Boehringer Ingelheim; both Dr. Strober and Dr. Schlesinger do research and consulting for BI, and receive funding from multiple other pharmaceutical companies.
A version of this article first appeared on Medscape.com.
AT WCD 2023
Focal plaques and finger swelling

Well-demarcated symmetrical scaly plaques and dactylitis are consistent with psoriasis and psoriatic arthritis (PsA). Even in the absence of significant skin disease, a patient like this should be evaluated by Rheumatology for initiation of disease-modifying antirheumatic drugs (DMARDs).
Psoriatic arthritis manifests as a peripheral arthritis affecting the small joints of the wrists and hands, pain at the insertion of tendons and ligaments (enthesitis), or as axial arthritis. This variable presentation and the lack of specific serological marker can make diagnosis challenging. Associated symptoms beyond the musculoskeletal system include uveitis, inflammatory bowel disease, and cutaneous psoriasis.1 In contrast to osteoarthritis, PsA symptoms are often worse in the morning and improve over the course of the day. Patients with a history of psoriasis on the skin have about a 10% chance of developing PsA, with increased rates in patients who have more widespread plaques and patients with psoriasis at a young age.2 Although not pathognomonic for PsA, pitting of the fingernails may reflect episodic enthesitis in the extensor tendons of the fingers.3 Radiographs of the hands in severe cases may demonstrate narrowing of the proximal portion of the distal or proximal interphalangeal joints with a cup-like concavity of the distal half of the joint.
Conventional DMARDs (such as methotrexate and azathioprine) and biologic DMARDs (including TNF-alpha inhibitors, IL-17 inhibitors, IL-23 inhibitors) are first-line treatments and can stop or slow the progression of disease but will not reverse existing damage. For this reason, it is important to promptly start DMARD therapy after the diagnosis has been established.4
This patient was initiated on adalimumab 40 mg subcutaneously every other week. Her pain improved after 2 months of therapy and her skin plaques almost entirely resolved at 6 months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Rida MA, Chandran V. Challenges in the clinical diagnosis of psoriatic arthritis. Clin Immunol. 2020;214:108390. doi: 10.1016/j.clim.2020.108390
2. Ogdie A, Gelfand JM. Clinical risk factors for the development of psoriatic arthritis among patients with psoriasis: a review of available evidence. Curr Rheumatol Rep. 2015;17:64. doi: 10.1007/s11926-015-0540-1
3. Elliott A, Pendleton A, Wright G, et al. The relationship between the nail and systemic enthesitis in psoriatic arthritis. Rheumatol Adv Pract. 2021;5:rkab088. doi: 10.1093/rap/rkab088
4. Coates LC, Soriano ER, Corp N, et al. GRAPPA treatment recommendations domain subcommittees. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18:465-479. doi: 10.1038/s41584-022-00798-0

Well-demarcated symmetrical scaly plaques and dactylitis are consistent with psoriasis and psoriatic arthritis (PsA). Even in the absence of significant skin disease, a patient like this should be evaluated by Rheumatology for initiation of disease-modifying antirheumatic drugs (DMARDs).
Psoriatic arthritis manifests as a peripheral arthritis affecting the small joints of the wrists and hands, pain at the insertion of tendons and ligaments (enthesitis), or as axial arthritis. This variable presentation and the lack of specific serological marker can make diagnosis challenging. Associated symptoms beyond the musculoskeletal system include uveitis, inflammatory bowel disease, and cutaneous psoriasis.1 In contrast to osteoarthritis, PsA symptoms are often worse in the morning and improve over the course of the day. Patients with a history of psoriasis on the skin have about a 10% chance of developing PsA, with increased rates in patients who have more widespread plaques and patients with psoriasis at a young age.2 Although not pathognomonic for PsA, pitting of the fingernails may reflect episodic enthesitis in the extensor tendons of the fingers.3 Radiographs of the hands in severe cases may demonstrate narrowing of the proximal portion of the distal or proximal interphalangeal joints with a cup-like concavity of the distal half of the joint.
Conventional DMARDs (such as methotrexate and azathioprine) and biologic DMARDs (including TNF-alpha inhibitors, IL-17 inhibitors, IL-23 inhibitors) are first-line treatments and can stop or slow the progression of disease but will not reverse existing damage. For this reason, it is important to promptly start DMARD therapy after the diagnosis has been established.4
This patient was initiated on adalimumab 40 mg subcutaneously every other week. Her pain improved after 2 months of therapy and her skin plaques almost entirely resolved at 6 months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

Well-demarcated symmetrical scaly plaques and dactylitis are consistent with psoriasis and psoriatic arthritis (PsA). Even in the absence of significant skin disease, a patient like this should be evaluated by Rheumatology for initiation of disease-modifying antirheumatic drugs (DMARDs).
Psoriatic arthritis manifests as a peripheral arthritis affecting the small joints of the wrists and hands, pain at the insertion of tendons and ligaments (enthesitis), or as axial arthritis. This variable presentation and the lack of specific serological marker can make diagnosis challenging. Associated symptoms beyond the musculoskeletal system include uveitis, inflammatory bowel disease, and cutaneous psoriasis.1 In contrast to osteoarthritis, PsA symptoms are often worse in the morning and improve over the course of the day. Patients with a history of psoriasis on the skin have about a 10% chance of developing PsA, with increased rates in patients who have more widespread plaques and patients with psoriasis at a young age.2 Although not pathognomonic for PsA, pitting of the fingernails may reflect episodic enthesitis in the extensor tendons of the fingers.3 Radiographs of the hands in severe cases may demonstrate narrowing of the proximal portion of the distal or proximal interphalangeal joints with a cup-like concavity of the distal half of the joint.
Conventional DMARDs (such as methotrexate and azathioprine) and biologic DMARDs (including TNF-alpha inhibitors, IL-17 inhibitors, IL-23 inhibitors) are first-line treatments and can stop or slow the progression of disease but will not reverse existing damage. For this reason, it is important to promptly start DMARD therapy after the diagnosis has been established.4
This patient was initiated on adalimumab 40 mg subcutaneously every other week. Her pain improved after 2 months of therapy and her skin plaques almost entirely resolved at 6 months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Rida MA, Chandran V. Challenges in the clinical diagnosis of psoriatic arthritis. Clin Immunol. 2020;214:108390. doi: 10.1016/j.clim.2020.108390
2. Ogdie A, Gelfand JM. Clinical risk factors for the development of psoriatic arthritis among patients with psoriasis: a review of available evidence. Curr Rheumatol Rep. 2015;17:64. doi: 10.1007/s11926-015-0540-1
3. Elliott A, Pendleton A, Wright G, et al. The relationship between the nail and systemic enthesitis in psoriatic arthritis. Rheumatol Adv Pract. 2021;5:rkab088. doi: 10.1093/rap/rkab088
4. Coates LC, Soriano ER, Corp N, et al. GRAPPA treatment recommendations domain subcommittees. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18:465-479. doi: 10.1038/s41584-022-00798-0
1. Rida MA, Chandran V. Challenges in the clinical diagnosis of psoriatic arthritis. Clin Immunol. 2020;214:108390. doi: 10.1016/j.clim.2020.108390
2. Ogdie A, Gelfand JM. Clinical risk factors for the development of psoriatic arthritis among patients with psoriasis: a review of available evidence. Curr Rheumatol Rep. 2015;17:64. doi: 10.1007/s11926-015-0540-1
3. Elliott A, Pendleton A, Wright G, et al. The relationship between the nail and systemic enthesitis in psoriatic arthritis. Rheumatol Adv Pract. 2021;5:rkab088. doi: 10.1093/rap/rkab088
4. Coates LC, Soriano ER, Corp N, et al. GRAPPA treatment recommendations domain subcommittees. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18:465-479. doi: 10.1038/s41584-022-00798-0
FDA adds safety-related information to its dermal filler webpage
On July 6, the .
Along with a list of common reactions such as bruising, redness, swelling, and pain, the webpage now includes language to inform the public and health care providers about reports of delayed-onset inflammation that have been reported to occur near the dermal filler treatment site following viral or bacterial illnesses or infections, vaccinations, or dental procedures. According to an FDA spokesperson, the update is based on several sources of information, including postmarketing data from adverse event–reporting databases, such as the Manufacturer and User Facility Device Experience (MAUDE) for devices and the Vaccine Adverse Event Reporting System (VAERS) for vaccines, published literature, and recommendations from federal agencies and professional societies.
“More specifically, the site was updated to include certain risks of using dermal fillers such as swelling and bruising as well as some less common risks such as inflammation – swelling or redness near the dermal filler injection site – following viral or bacterial illnesses or infections, vaccinations, or dental procedures,” the spokesperson said.
The announcement about the update also states that “typically, the reported inflammation is responsive to treatment or resolves on its own.”
Other less common risks from dermal filler use listed on the website include bumps in or under the skin (nodules or granulomas) that may need to be treated with injections, oral antibiotics, or surgical removal; infection; open or draining wounds; a sore at the injection site; allergic reactions; or necrosis.
Meanwhile, rare risks from dermal filler use that have been reported to the FDA include severe allergic reactions (anaphylactic shock) that require immediate emergency medical assistance; migration (movement of filler material from the site of injection); leakage or rupture of the filler material at the injection site or through the skin (which may result from a tissue reaction or an infection); the formation of permanent hard nodules; and injury to the blood supply after an unintentional injection into a blood vessel, resulting in necrosis, vision abnormalities (including blindness), or stroke.
Lawrence J. Green, MD, of the department of dermatology at George Washington University, Washington, who was asked to comment about the FDA update on dermal fillers, said that the agency “is doing its job by making consumers aware of all possible complications [common and uncommon], as it does when it creates a package insert for a medication. Fortunately, however, comprehensive reviews published in the peer-reviewed dermatology literature show delayed inflammation to be a very rare event. So, while it is important for dermatologists during informed consent – prior to filler – to discuss that redness and/or nodules after infection/vaccinations, etc. are possible, it is important to add that based on the data, they are also highly unlikely.”
Sue Ellen Cox, MD, a dermatologist who practices in Chapel Hill, N.C., said that she was glad to see separate sections of recommendations geared to patients and health care providers. For example, the website recommends that patients seek a physician in the field of dermatology or plastic surgery to perform procedures that use dermal fillers. “These are not procedures to be done in an unsupervised spa setting,” said Dr. Cox, a past president of the American Society for Dermatologic Surgery and one of the task force authors of recommendations on preventing and treating adverse events of injectable fillers.
“It also makes the point of using products that are acquired from FDA-approved manufacturers, not products sold online or bootlegged from other countries. Finally, it goes into detail about the importance of in-depth knowledge of anatomy, which is crucial for safe injections and reviews potential complications such as intravascular events and hypersensitivity reactions. The administering physician should have extensive knowledge regarding how to treat any potential problems that arise.”
Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies. Dr. Cox disclosed that she has been a clinical investigator for many injectable companies including AbbVie, Galderma, Revance, and Chroma.
Health care professionals, patients, and others can report adverse events related to dermal fillers and other medical devices to the FDA at 800-FDA-1088 or on the MAUDE website.
On July 6, the .
Along with a list of common reactions such as bruising, redness, swelling, and pain, the webpage now includes language to inform the public and health care providers about reports of delayed-onset inflammation that have been reported to occur near the dermal filler treatment site following viral or bacterial illnesses or infections, vaccinations, or dental procedures. According to an FDA spokesperson, the update is based on several sources of information, including postmarketing data from adverse event–reporting databases, such as the Manufacturer and User Facility Device Experience (MAUDE) for devices and the Vaccine Adverse Event Reporting System (VAERS) for vaccines, published literature, and recommendations from federal agencies and professional societies.
“More specifically, the site was updated to include certain risks of using dermal fillers such as swelling and bruising as well as some less common risks such as inflammation – swelling or redness near the dermal filler injection site – following viral or bacterial illnesses or infections, vaccinations, or dental procedures,” the spokesperson said.
The announcement about the update also states that “typically, the reported inflammation is responsive to treatment or resolves on its own.”
Other less common risks from dermal filler use listed on the website include bumps in or under the skin (nodules or granulomas) that may need to be treated with injections, oral antibiotics, or surgical removal; infection; open or draining wounds; a sore at the injection site; allergic reactions; or necrosis.
Meanwhile, rare risks from dermal filler use that have been reported to the FDA include severe allergic reactions (anaphylactic shock) that require immediate emergency medical assistance; migration (movement of filler material from the site of injection); leakage or rupture of the filler material at the injection site or through the skin (which may result from a tissue reaction or an infection); the formation of permanent hard nodules; and injury to the blood supply after an unintentional injection into a blood vessel, resulting in necrosis, vision abnormalities (including blindness), or stroke.
Lawrence J. Green, MD, of the department of dermatology at George Washington University, Washington, who was asked to comment about the FDA update on dermal fillers, said that the agency “is doing its job by making consumers aware of all possible complications [common and uncommon], as it does when it creates a package insert for a medication. Fortunately, however, comprehensive reviews published in the peer-reviewed dermatology literature show delayed inflammation to be a very rare event. So, while it is important for dermatologists during informed consent – prior to filler – to discuss that redness and/or nodules after infection/vaccinations, etc. are possible, it is important to add that based on the data, they are also highly unlikely.”
Sue Ellen Cox, MD, a dermatologist who practices in Chapel Hill, N.C., said that she was glad to see separate sections of recommendations geared to patients and health care providers. For example, the website recommends that patients seek a physician in the field of dermatology or plastic surgery to perform procedures that use dermal fillers. “These are not procedures to be done in an unsupervised spa setting,” said Dr. Cox, a past president of the American Society for Dermatologic Surgery and one of the task force authors of recommendations on preventing and treating adverse events of injectable fillers.
“It also makes the point of using products that are acquired from FDA-approved manufacturers, not products sold online or bootlegged from other countries. Finally, it goes into detail about the importance of in-depth knowledge of anatomy, which is crucial for safe injections and reviews potential complications such as intravascular events and hypersensitivity reactions. The administering physician should have extensive knowledge regarding how to treat any potential problems that arise.”
Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies. Dr. Cox disclosed that she has been a clinical investigator for many injectable companies including AbbVie, Galderma, Revance, and Chroma.
Health care professionals, patients, and others can report adverse events related to dermal fillers and other medical devices to the FDA at 800-FDA-1088 or on the MAUDE website.
On July 6, the .
Along with a list of common reactions such as bruising, redness, swelling, and pain, the webpage now includes language to inform the public and health care providers about reports of delayed-onset inflammation that have been reported to occur near the dermal filler treatment site following viral or bacterial illnesses or infections, vaccinations, or dental procedures. According to an FDA spokesperson, the update is based on several sources of information, including postmarketing data from adverse event–reporting databases, such as the Manufacturer and User Facility Device Experience (MAUDE) for devices and the Vaccine Adverse Event Reporting System (VAERS) for vaccines, published literature, and recommendations from federal agencies and professional societies.
“More specifically, the site was updated to include certain risks of using dermal fillers such as swelling and bruising as well as some less common risks such as inflammation – swelling or redness near the dermal filler injection site – following viral or bacterial illnesses or infections, vaccinations, or dental procedures,” the spokesperson said.
The announcement about the update also states that “typically, the reported inflammation is responsive to treatment or resolves on its own.”
Other less common risks from dermal filler use listed on the website include bumps in or under the skin (nodules or granulomas) that may need to be treated with injections, oral antibiotics, or surgical removal; infection; open or draining wounds; a sore at the injection site; allergic reactions; or necrosis.
Meanwhile, rare risks from dermal filler use that have been reported to the FDA include severe allergic reactions (anaphylactic shock) that require immediate emergency medical assistance; migration (movement of filler material from the site of injection); leakage or rupture of the filler material at the injection site or through the skin (which may result from a tissue reaction or an infection); the formation of permanent hard nodules; and injury to the blood supply after an unintentional injection into a blood vessel, resulting in necrosis, vision abnormalities (including blindness), or stroke.
Lawrence J. Green, MD, of the department of dermatology at George Washington University, Washington, who was asked to comment about the FDA update on dermal fillers, said that the agency “is doing its job by making consumers aware of all possible complications [common and uncommon], as it does when it creates a package insert for a medication. Fortunately, however, comprehensive reviews published in the peer-reviewed dermatology literature show delayed inflammation to be a very rare event. So, while it is important for dermatologists during informed consent – prior to filler – to discuss that redness and/or nodules after infection/vaccinations, etc. are possible, it is important to add that based on the data, they are also highly unlikely.”
Sue Ellen Cox, MD, a dermatologist who practices in Chapel Hill, N.C., said that she was glad to see separate sections of recommendations geared to patients and health care providers. For example, the website recommends that patients seek a physician in the field of dermatology or plastic surgery to perform procedures that use dermal fillers. “These are not procedures to be done in an unsupervised spa setting,” said Dr. Cox, a past president of the American Society for Dermatologic Surgery and one of the task force authors of recommendations on preventing and treating adverse events of injectable fillers.
“It also makes the point of using products that are acquired from FDA-approved manufacturers, not products sold online or bootlegged from other countries. Finally, it goes into detail about the importance of in-depth knowledge of anatomy, which is crucial for safe injections and reviews potential complications such as intravascular events and hypersensitivity reactions. The administering physician should have extensive knowledge regarding how to treat any potential problems that arise.”
Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies. Dr. Cox disclosed that she has been a clinical investigator for many injectable companies including AbbVie, Galderma, Revance, and Chroma.
Health care professionals, patients, and others can report adverse events related to dermal fillers and other medical devices to the FDA at 800-FDA-1088 or on the MAUDE website.
Necessary Updates to Skin Cancer Risk Stratification
1. Powers JG, Patel NA, Powers EA, Mayer JE, Stricklin GP, Geller AC. Skin cancer
risk factors and preventative behaviors among United States military veterans deployed to Iraq and Afghanistan. J Invest Dermatol. 2015;135:2871-2873.
2. Balci S, Ayaz L, Gorur A, Yildirim Yaroglu H, Akbayir S, Dogruer Unal N, Bulut B,
Tursen U, Tamer L. microRNA profiling for early detection of nonmelanoma skin cancer. Clin Exp Dermatol. 2016;41(4):346-51. doi:10.1111/ced.12736
3. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
4. Agbai ON, Buster K, Sanchez M, Hernandez C, Kundu RV, Chiu M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748-62.
5. Chou SE, Gaysynsky A, Trivedi N, Vanderpool R. Using social media for health: national data from HINTS 2019. Journ of Health Comm. 2019;26(3):184-193. doi:10.1080/10810730.2021.
6. Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279-82.
7. Dennis LK, et al. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Annals of Epidem. 2008;18(8):614-627. doi:10.1016/j.annepidem.2008.
8. Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomar Prev. 2014;23(6):1080-1089.
9. 2020 Demographics Profile of the military community. US Department of Defense. 2020:iv. Accessed November 15, 2022. 2020 Demographics Profile of the Military Community (militaryonesource.mil)
10. Apalla Z, Lallas A, Sotiriou E, Lazaridou E, Ioannides D. Epidemiological trends in skin cancer. Dermatol Pract Concept. 2017;7:1-6.
11. Basch CH, Hillyer GC. Skin cancer on Instagram: implications for adolescents and young adults. Int J Adolesc Med Health. 2022;34(3). doi:10.1515/ijamh-2019-0218
1. Powers JG, Patel NA, Powers EA, Mayer JE, Stricklin GP, Geller AC. Skin cancer
risk factors and preventative behaviors among United States military veterans deployed to Iraq and Afghanistan. J Invest Dermatol. 2015;135:2871-2873.
2. Balci S, Ayaz L, Gorur A, Yildirim Yaroglu H, Akbayir S, Dogruer Unal N, Bulut B,
Tursen U, Tamer L. microRNA profiling for early detection of nonmelanoma skin cancer. Clin Exp Dermatol. 2016;41(4):346-51. doi:10.1111/ced.12736
3. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
4. Agbai ON, Buster K, Sanchez M, Hernandez C, Kundu RV, Chiu M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748-62.
5. Chou SE, Gaysynsky A, Trivedi N, Vanderpool R. Using social media for health: national data from HINTS 2019. Journ of Health Comm. 2019;26(3):184-193. doi:10.1080/10810730.2021.
6. Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279-82.
7. Dennis LK, et al. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Annals of Epidem. 2008;18(8):614-627. doi:10.1016/j.annepidem.2008.
8. Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomar Prev. 2014;23(6):1080-1089.
9. 2020 Demographics Profile of the military community. US Department of Defense. 2020:iv. Accessed November 15, 2022. 2020 Demographics Profile of the Military Community (militaryonesource.mil)
10. Apalla Z, Lallas A, Sotiriou E, Lazaridou E, Ioannides D. Epidemiological trends in skin cancer. Dermatol Pract Concept. 2017;7:1-6.
11. Basch CH, Hillyer GC. Skin cancer on Instagram: implications for adolescents and young adults. Int J Adolesc Med Health. 2022;34(3). doi:10.1515/ijamh-2019-0218
1. Powers JG, Patel NA, Powers EA, Mayer JE, Stricklin GP, Geller AC. Skin cancer
risk factors and preventative behaviors among United States military veterans deployed to Iraq and Afghanistan. J Invest Dermatol. 2015;135:2871-2873.
2. Balci S, Ayaz L, Gorur A, Yildirim Yaroglu H, Akbayir S, Dogruer Unal N, Bulut B,
Tursen U, Tamer L. microRNA profiling for early detection of nonmelanoma skin cancer. Clin Exp Dermatol. 2016;41(4):346-51. doi:10.1111/ced.12736
3. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
4. Agbai ON, Buster K, Sanchez M, Hernandez C, Kundu RV, Chiu M, et al. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748-62.
5. Chou SE, Gaysynsky A, Trivedi N, Vanderpool R. Using social media for health: national data from HINTS 2019. Journ of Health Comm. 2019;26(3):184-193. doi:10.1080/10810730.2021.
6. Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279-82.
7. Dennis LK, et al. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Annals of Epidem. 2008;18(8):614-627. doi:10.1016/j.annepidem.2008.
8. Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomar Prev. 2014;23(6):1080-1089.
9. 2020 Demographics Profile of the military community. US Department of Defense. 2020:iv. Accessed November 15, 2022. 2020 Demographics Profile of the Military Community (militaryonesource.mil)
10. Apalla Z, Lallas A, Sotiriou E, Lazaridou E, Ioannides D. Epidemiological trends in skin cancer. Dermatol Pract Concept. 2017;7:1-6.
11. Basch CH, Hillyer GC. Skin cancer on Instagram: implications for adolescents and young adults. Int J Adolesc Med Health. 2022;34(3). doi:10.1515/ijamh-2019-0218
Nails falling off in a 3-year-old

When the nails peel off from the proximal nail folds, the clinical term is onychomadesis and it is important to ask about recent infections or severe metabolic stressors. In children and adults, onychomadesis on multiple fingers may occur after infections and has been associated with hand-foot-mouth disease caused by common viral infections—especially strains of coxsackievirus.1
Because shed nails show evidence of viral infection, one hypothesis for their peeling off is that the tissue of the nail matrix is infected, leading to metabolic changes. As the nail matrix returns to normal function, a new nail is made and ultimately will replace the nail that has come off. In healthy US adults, fingernails grow 3.47 mm per month on average while toenails grow 1.62 mm per month on average.2
Sometimes it’s hard to elicit a history of a very mild viral illness weeks or months after it has resolved. Asking specifically about mouth ulcers may help. If there is a history of a viral illness, no specific work-up or treatment is necessary. Patients may be reassured that nails will improve over several months without lasting effects.
In this case, the patient and her family were given reassurance and the nails returned to normal within a few months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Kim EJ, Park HS, Yoon HS, et al. Four cases of onychomadesis after hand-foot-mouth disease. Ann Dermatol. 2014;26:777-778. doi: 10.5021/ad.2014.26.6.777
2. Yaemsiri S, Hou N, Slining MM, et al. Growth rate of human fingernails and toenails in healthy American young adults. J Eur Acad Dermatol Venereol. 2010;24:420-423. doi: 10.1111/j.1468-3083.2009.03426.x

When the nails peel off from the proximal nail folds, the clinical term is onychomadesis and it is important to ask about recent infections or severe metabolic stressors. In children and adults, onychomadesis on multiple fingers may occur after infections and has been associated with hand-foot-mouth disease caused by common viral infections—especially strains of coxsackievirus.1
Because shed nails show evidence of viral infection, one hypothesis for their peeling off is that the tissue of the nail matrix is infected, leading to metabolic changes. As the nail matrix returns to normal function, a new nail is made and ultimately will replace the nail that has come off. In healthy US adults, fingernails grow 3.47 mm per month on average while toenails grow 1.62 mm per month on average.2
Sometimes it’s hard to elicit a history of a very mild viral illness weeks or months after it has resolved. Asking specifically about mouth ulcers may help. If there is a history of a viral illness, no specific work-up or treatment is necessary. Patients may be reassured that nails will improve over several months without lasting effects.
In this case, the patient and her family were given reassurance and the nails returned to normal within a few months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

When the nails peel off from the proximal nail folds, the clinical term is onychomadesis and it is important to ask about recent infections or severe metabolic stressors. In children and adults, onychomadesis on multiple fingers may occur after infections and has been associated with hand-foot-mouth disease caused by common viral infections—especially strains of coxsackievirus.1
Because shed nails show evidence of viral infection, one hypothesis for their peeling off is that the tissue of the nail matrix is infected, leading to metabolic changes. As the nail matrix returns to normal function, a new nail is made and ultimately will replace the nail that has come off. In healthy US adults, fingernails grow 3.47 mm per month on average while toenails grow 1.62 mm per month on average.2
Sometimes it’s hard to elicit a history of a very mild viral illness weeks or months after it has resolved. Asking specifically about mouth ulcers may help. If there is a history of a viral illness, no specific work-up or treatment is necessary. Patients may be reassured that nails will improve over several months without lasting effects.
In this case, the patient and her family were given reassurance and the nails returned to normal within a few months.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Kim EJ, Park HS, Yoon HS, et al. Four cases of onychomadesis after hand-foot-mouth disease. Ann Dermatol. 2014;26:777-778. doi: 10.5021/ad.2014.26.6.777
2. Yaemsiri S, Hou N, Slining MM, et al. Growth rate of human fingernails and toenails in healthy American young adults. J Eur Acad Dermatol Venereol. 2010;24:420-423. doi: 10.1111/j.1468-3083.2009.03426.x
1. Kim EJ, Park HS, Yoon HS, et al. Four cases of onychomadesis after hand-foot-mouth disease. Ann Dermatol. 2014;26:777-778. doi: 10.5021/ad.2014.26.6.777
2. Yaemsiri S, Hou N, Slining MM, et al. Growth rate of human fingernails and toenails in healthy American young adults. J Eur Acad Dermatol Venereol. 2010;24:420-423. doi: 10.1111/j.1468-3083.2009.03426.x