User login
Severe hypoglycemia, poor glycemic control fuels fracture risk in older diabetic patients
Patients with type 2 diabetes and poor glycemic control or severe hypoglycemia may be at greater risk for fracture, according to recent research from a Japanese cohort of older men and postmenopausal women.
“The impacts of severe hypoglycemia and poor glycemic control on fractures appeared to be independent,” noted Yuji Komorita, MD, PhD, of the department of medicine and clinical science, Graduate School of Medical Sciences at Kyushu University, and colleagues. “This study suggests that the glycemic target to prevent fractures may be HbA1c <75 mmol/mol, which is far higher than that used to prevent microvascular complications, and higher than that for older adults with type 2 diabetes.”
Dr. Komorita and colleagues performed a prospective analysis of fracture incidence for 2,755 men and 1,951 postmenopausal women with type 2 diabetes in the Fukuoka Diabetes Registry who were mean 66 years old between April 2008 and October 2010. At the start of the study, the researchers assessed patient diabetes duration, previous fracture history, physical activity, alcohol and smoking status, whether patients were treated for diabetic retinopathy with laser photocoagulation, and their history of coronary artery disease or stroke. Patients were followed for a median 5.3 years, during which fractures were assessed through an annual self-administered questionnaire, with the results stratified by glycemic control and hypoglycemia.
Overall, there were 249 men and 413 women who experienced fractures during the study period, with a follow-up rate of 97.6%. In a multivariate analysis, patients with a higher risk of fracture included those with two or more episodes of severe hypoglycemia (hazard ratio, 2.25; 95% confidence interval, 1.57-3.22) and one episode of severe hypoglycemia (HR, 1.57; 95% CI, 1.11-2.20). In patients without severe hypoglycemic episodes, there was an increased risk of fracture in those with baseline hemoglobin A1c (HbA1c) level of 53 to less than 64 mmol/mol (7% to less than 8%; HR, 1.14; 0.94-1.39), 64 to less than 75 mmol/mol (8% to less than 9%; HR, 1.11; 95% CI, 0.86-1.43), and at least 75 mmol/mol (at least 9%; HR, 1.45; 95% CI, 1.06-1.98).
Compared with postmenopausal women, the unadjusted risk of fracture was higher in men with multiple severe hypoglycemic episodes (HR, 3.46; 95% CI, 2.05-5.85) and one episode of hypoglycemia (HR, 2.81; 95% CI, 1.74-4.56). These higher risks in older men persisted after adjustment for age, multivariate factors, and HbA1c.
“The association between severe hypoglycemia, poor glycemic control, and fracture risk at any anatomic site seems to be stronger in men than in postmenopausal women, although the interaction between men and postmenopausal women for fracture risk was not significant,” the researchers said. “The higher incidence rate of fractures in postmenopausal women, compared with men, was attributed to drastic changes in sex hormones after menopause, which may reduce the apparent impacts of hyperglycemia and severe hypoglycemia on postmenopausal women.”
Researchers said they did not consider potential external factors for fracture incidence, nor did they measure incident falls or other markers of bone health, such as bone mineral density and 25-hydroxyvitamin D levels. They also noted among the limitations of the study the self-reported nature of fracture reporting, and the lack of generalizability of the results.
This study was funded in part by grants from The Japan Society for the Promotion of Science KAKENHI from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Junior Scientist Development Grant supported by the Japan Diabetes Society; and the Lilly Research Grant Program for Bone & Mineral Research. The authors reported no relevant conflicts of interest.
SOURCE: Komorita Y et al. Diabet Med. 2019 Sep 25. doi: 10.1111/dme.14142.
Patients with type 2 diabetes and poor glycemic control or severe hypoglycemia may be at greater risk for fracture, according to recent research from a Japanese cohort of older men and postmenopausal women.
“The impacts of severe hypoglycemia and poor glycemic control on fractures appeared to be independent,” noted Yuji Komorita, MD, PhD, of the department of medicine and clinical science, Graduate School of Medical Sciences at Kyushu University, and colleagues. “This study suggests that the glycemic target to prevent fractures may be HbA1c <75 mmol/mol, which is far higher than that used to prevent microvascular complications, and higher than that for older adults with type 2 diabetes.”
Dr. Komorita and colleagues performed a prospective analysis of fracture incidence for 2,755 men and 1,951 postmenopausal women with type 2 diabetes in the Fukuoka Diabetes Registry who were mean 66 years old between April 2008 and October 2010. At the start of the study, the researchers assessed patient diabetes duration, previous fracture history, physical activity, alcohol and smoking status, whether patients were treated for diabetic retinopathy with laser photocoagulation, and their history of coronary artery disease or stroke. Patients were followed for a median 5.3 years, during which fractures were assessed through an annual self-administered questionnaire, with the results stratified by glycemic control and hypoglycemia.
Overall, there were 249 men and 413 women who experienced fractures during the study period, with a follow-up rate of 97.6%. In a multivariate analysis, patients with a higher risk of fracture included those with two or more episodes of severe hypoglycemia (hazard ratio, 2.25; 95% confidence interval, 1.57-3.22) and one episode of severe hypoglycemia (HR, 1.57; 95% CI, 1.11-2.20). In patients without severe hypoglycemic episodes, there was an increased risk of fracture in those with baseline hemoglobin A1c (HbA1c) level of 53 to less than 64 mmol/mol (7% to less than 8%; HR, 1.14; 0.94-1.39), 64 to less than 75 mmol/mol (8% to less than 9%; HR, 1.11; 95% CI, 0.86-1.43), and at least 75 mmol/mol (at least 9%; HR, 1.45; 95% CI, 1.06-1.98).
Compared with postmenopausal women, the unadjusted risk of fracture was higher in men with multiple severe hypoglycemic episodes (HR, 3.46; 95% CI, 2.05-5.85) and one episode of hypoglycemia (HR, 2.81; 95% CI, 1.74-4.56). These higher risks in older men persisted after adjustment for age, multivariate factors, and HbA1c.
“The association between severe hypoglycemia, poor glycemic control, and fracture risk at any anatomic site seems to be stronger in men than in postmenopausal women, although the interaction between men and postmenopausal women for fracture risk was not significant,” the researchers said. “The higher incidence rate of fractures in postmenopausal women, compared with men, was attributed to drastic changes in sex hormones after menopause, which may reduce the apparent impacts of hyperglycemia and severe hypoglycemia on postmenopausal women.”
Researchers said they did not consider potential external factors for fracture incidence, nor did they measure incident falls or other markers of bone health, such as bone mineral density and 25-hydroxyvitamin D levels. They also noted among the limitations of the study the self-reported nature of fracture reporting, and the lack of generalizability of the results.
This study was funded in part by grants from The Japan Society for the Promotion of Science KAKENHI from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Junior Scientist Development Grant supported by the Japan Diabetes Society; and the Lilly Research Grant Program for Bone & Mineral Research. The authors reported no relevant conflicts of interest.
SOURCE: Komorita Y et al. Diabet Med. 2019 Sep 25. doi: 10.1111/dme.14142.
Patients with type 2 diabetes and poor glycemic control or severe hypoglycemia may be at greater risk for fracture, according to recent research from a Japanese cohort of older men and postmenopausal women.
“The impacts of severe hypoglycemia and poor glycemic control on fractures appeared to be independent,” noted Yuji Komorita, MD, PhD, of the department of medicine and clinical science, Graduate School of Medical Sciences at Kyushu University, and colleagues. “This study suggests that the glycemic target to prevent fractures may be HbA1c <75 mmol/mol, which is far higher than that used to prevent microvascular complications, and higher than that for older adults with type 2 diabetes.”
Dr. Komorita and colleagues performed a prospective analysis of fracture incidence for 2,755 men and 1,951 postmenopausal women with type 2 diabetes in the Fukuoka Diabetes Registry who were mean 66 years old between April 2008 and October 2010. At the start of the study, the researchers assessed patient diabetes duration, previous fracture history, physical activity, alcohol and smoking status, whether patients were treated for diabetic retinopathy with laser photocoagulation, and their history of coronary artery disease or stroke. Patients were followed for a median 5.3 years, during which fractures were assessed through an annual self-administered questionnaire, with the results stratified by glycemic control and hypoglycemia.
Overall, there were 249 men and 413 women who experienced fractures during the study period, with a follow-up rate of 97.6%. In a multivariate analysis, patients with a higher risk of fracture included those with two or more episodes of severe hypoglycemia (hazard ratio, 2.25; 95% confidence interval, 1.57-3.22) and one episode of severe hypoglycemia (HR, 1.57; 95% CI, 1.11-2.20). In patients without severe hypoglycemic episodes, there was an increased risk of fracture in those with baseline hemoglobin A1c (HbA1c) level of 53 to less than 64 mmol/mol (7% to less than 8%; HR, 1.14; 0.94-1.39), 64 to less than 75 mmol/mol (8% to less than 9%; HR, 1.11; 95% CI, 0.86-1.43), and at least 75 mmol/mol (at least 9%; HR, 1.45; 95% CI, 1.06-1.98).
Compared with postmenopausal women, the unadjusted risk of fracture was higher in men with multiple severe hypoglycemic episodes (HR, 3.46; 95% CI, 2.05-5.85) and one episode of hypoglycemia (HR, 2.81; 95% CI, 1.74-4.56). These higher risks in older men persisted after adjustment for age, multivariate factors, and HbA1c.
“The association between severe hypoglycemia, poor glycemic control, and fracture risk at any anatomic site seems to be stronger in men than in postmenopausal women, although the interaction between men and postmenopausal women for fracture risk was not significant,” the researchers said. “The higher incidence rate of fractures in postmenopausal women, compared with men, was attributed to drastic changes in sex hormones after menopause, which may reduce the apparent impacts of hyperglycemia and severe hypoglycemia on postmenopausal women.”
Researchers said they did not consider potential external factors for fracture incidence, nor did they measure incident falls or other markers of bone health, such as bone mineral density and 25-hydroxyvitamin D levels. They also noted among the limitations of the study the self-reported nature of fracture reporting, and the lack of generalizability of the results.
This study was funded in part by grants from The Japan Society for the Promotion of Science KAKENHI from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Junior Scientist Development Grant supported by the Japan Diabetes Society; and the Lilly Research Grant Program for Bone & Mineral Research. The authors reported no relevant conflicts of interest.
SOURCE: Komorita Y et al. Diabet Med. 2019 Sep 25. doi: 10.1111/dme.14142.
FROM DIABETIC MEDICINE
Dapagliflozin approved for reducing HF hospitalization in diabetes
The Food And Drug Administration has approved the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin (Farxiga) for reducing the risk of hospitalization for heart failure in adults with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors, according to a statement from AstraZeneca.
The approval was based on results from the DECLARE-TIMI 58 cardiovascular outcomes trial, which evaluated dapagliflozin in more than 17,000 patients with type 2 diabetes and cardiovascular risk factors or cardiovascular disease. They showed that dapagliflozin significantly reduced the risk of the primary composite endpoint of hospitalization for heart failure by 27%, compared with placebo (2.5% vs. 3.3%; HR, 0.73; 95% confidence interval, 0.61-0.88).
The drug is an oral, once-daily SGLT2 inhibitor initially approved as a monotherapy or combination therapy for glycemic control in adults with type 2 diabetes. It has additional benefits of weight loss and reduction in blood pressure in concert with diet and exercise in the same population.
“,” Ruud Dobber, PhD, executive vice president of the company’s biopharmaceuticals business unit, said in the statement. “This is promising news for the 30 million people living with type 2 diabetes in the U.S., as heart failure is one of the earliest cardiovascular complications for them, before heart attack or stroke. [Dapagliflozin] now offers the opportunity for physicians to act sooner and reduce the risk of hospitalization for heart failure.”
In September, the agency granted dapagliflozin a Fast Track designation to reduce the risk of cardiovascular death, or the worsening of heart failure in adults with heart failure with reduced ejection fraction or preserved ejection fraction, based on the phase 3 DAPA-HF and DELIVER trials. It also gave the drug Fast Track designation to delay the progression of renal failure and prevent CV and renal death in patients with chronic kidney disease based on the phase 3 DAPA-CKD trial, the statement noted.
The Food And Drug Administration has approved the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin (Farxiga) for reducing the risk of hospitalization for heart failure in adults with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors, according to a statement from AstraZeneca.
The approval was based on results from the DECLARE-TIMI 58 cardiovascular outcomes trial, which evaluated dapagliflozin in more than 17,000 patients with type 2 diabetes and cardiovascular risk factors or cardiovascular disease. They showed that dapagliflozin significantly reduced the risk of the primary composite endpoint of hospitalization for heart failure by 27%, compared with placebo (2.5% vs. 3.3%; HR, 0.73; 95% confidence interval, 0.61-0.88).
The drug is an oral, once-daily SGLT2 inhibitor initially approved as a monotherapy or combination therapy for glycemic control in adults with type 2 diabetes. It has additional benefits of weight loss and reduction in blood pressure in concert with diet and exercise in the same population.
“,” Ruud Dobber, PhD, executive vice president of the company’s biopharmaceuticals business unit, said in the statement. “This is promising news for the 30 million people living with type 2 diabetes in the U.S., as heart failure is one of the earliest cardiovascular complications for them, before heart attack or stroke. [Dapagliflozin] now offers the opportunity for physicians to act sooner and reduce the risk of hospitalization for heart failure.”
In September, the agency granted dapagliflozin a Fast Track designation to reduce the risk of cardiovascular death, or the worsening of heart failure in adults with heart failure with reduced ejection fraction or preserved ejection fraction, based on the phase 3 DAPA-HF and DELIVER trials. It also gave the drug Fast Track designation to delay the progression of renal failure and prevent CV and renal death in patients with chronic kidney disease based on the phase 3 DAPA-CKD trial, the statement noted.
The Food And Drug Administration has approved the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin (Farxiga) for reducing the risk of hospitalization for heart failure in adults with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors, according to a statement from AstraZeneca.
The approval was based on results from the DECLARE-TIMI 58 cardiovascular outcomes trial, which evaluated dapagliflozin in more than 17,000 patients with type 2 diabetes and cardiovascular risk factors or cardiovascular disease. They showed that dapagliflozin significantly reduced the risk of the primary composite endpoint of hospitalization for heart failure by 27%, compared with placebo (2.5% vs. 3.3%; HR, 0.73; 95% confidence interval, 0.61-0.88).
The drug is an oral, once-daily SGLT2 inhibitor initially approved as a monotherapy or combination therapy for glycemic control in adults with type 2 diabetes. It has additional benefits of weight loss and reduction in blood pressure in concert with diet and exercise in the same population.
“,” Ruud Dobber, PhD, executive vice president of the company’s biopharmaceuticals business unit, said in the statement. “This is promising news for the 30 million people living with type 2 diabetes in the U.S., as heart failure is one of the earliest cardiovascular complications for them, before heart attack or stroke. [Dapagliflozin] now offers the opportunity for physicians to act sooner and reduce the risk of hospitalization for heart failure.”
In September, the agency granted dapagliflozin a Fast Track designation to reduce the risk of cardiovascular death, or the worsening of heart failure in adults with heart failure with reduced ejection fraction or preserved ejection fraction, based on the phase 3 DAPA-HF and DELIVER trials. It also gave the drug Fast Track designation to delay the progression of renal failure and prevent CV and renal death in patients with chronic kidney disease based on the phase 3 DAPA-CKD trial, the statement noted.
Certain diabetes drugs may thwart dementia
COPENHAGEN – Selected antidiabetes medications appear to blunt the increased risk of dementia associated with type 2 diabetes, according to a Danish national case control registry study.
This benefit applies to the newer antidiabetic agents – specifically, the dipeptidyl peptidase 4 (DPP4) inhibitors, the glucagon-like peptide 1 (GLP1) analogs, and the sodium-glucose transport protein 2 (SGLT2) inhibitors – and metformin as well, Merete Osler, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, neither insulin nor the sulfonylureas showed any signal of a protective effect against development of dementia. In fact, the use of sulfonylureas was associated with a small but statistically significant 7% increased risk, added Dr. Osler, of the University of Copenhagen.
Elsewhere at the meeting, investigators tapped a Swedish national registry to demonstrate that individuals with type 1 diabetes have a sharply reduced risk of developing schizophrenia.
Type 2 diabetes medications and dementia
Dr. Osler and colleagues are among several groups of investigators who have previously shown that patients with type 2 diabetes have an increased risk of dementia.
“This has raised the question of the role of dysregulated glucose metabolism in the development of this neurodegenerative disorder, and the possible effect of antidiabetic medications,” she noted.
To further explore this issue, which links two great ongoing global epidemics, Dr. Osler and coinvestigators conducted a nested case-control study including all 176,250 patients with type 2 diabetes in the comprehensive Danish National Diabetes Register for 1995-2012. The 11,619 patients with type 2 diabetes who received a dementia diagnosis were matched with 46,476 type 2 diabetes patients without dementia. The objective was to determine associations between dementia and ever-use and cumulative dose of antidiabetes drugs, alone and in combination, in logistic regression analyses adjusted for demographics, comorbid conditions, marital status, diabetic complications, and year of dementia diagnosis.
Patients who had ever used metformin had an adjusted 6% reduction in the likelihood of dementia compared with metformin nonusers, a modest but statistically significant difference. Those on a DPP4 inhibitor had a 20% reduction in risk. The GLP1 analogs were associated with a 42% decrease in risk. So were the SGLT2 inhibitors. A dose-response relationship was evident: The higher the cumulative exposure to these agents, the lower the odds of dementia.
Combination therapy is common in type 2 diabetes, so the investigators scrutinized the impact of a variety of multidrug combinations. Combinations including a DPP4 inhibitor or GLP1 analog were also associated with significantly reduced dementia risk.
Records of glycemic control in the form of hemoglobin A1c values were available on only 1,446 type 2 diabetic dementia patients and 4,003 matched controls. An analysis that incorporated this variable showed that the observed anti-dementia effect of selected diabetes drugs was independent of glycemic control, according to Dr. Osler.
The protective effect appeared to extend to both Alzheimer’s disease and vascular dementias, although firm conclusions can’t be drawn on this score because the study was insufficiently powered to address that issue.
Dr. Osler noted that the Danish study confirms a recent Taiwanese study showing an apparent protective effect against dementia for metformin in patients with type 2 diabetes (Aging Dis. 2019 Feb 1;10(1):37-48).
“Ours is the first study on the newer diabetic drugs, so our results need to be confirmed,” she pointed out.
If confirmed, however, it would warrant exploration of these drugs more generally as potential interventions to prevent dementia. That could open a whole new chapter in the remarkable story of the SGLT2 inhibitors, a class of drugs originally developed for treatment of type 2 diabetes but which in major randomized clinical trials later proved to be so effective in the treatment of heart failure that they are now considered cardiology drugs first.
Asked if she thinks these antidiabetes agents have a general neuroprotective effect or, instead, that the observed reduced risk of dementia is a function of patients being treated better early on with modern drugs, the psychiatrist replied, “I think it might be a combination of both, especially because we find different risk estimates between the drugs.”
Dr. Osler reported having no financial conflicts of interest regarding the study, which was funded by the Danish Diabetes Foundation, the Danish Medical Association, and several other foundations.
The full study details were published online shortly before her presentation at ECNP 2019 (Eur J Endocrinol. 2019 Aug 1. pii: EJE-19-0259.R1. doi: 10.1530/EJE-19-0259).
Type 1 diabetes and schizophrenia risk
Kristina Melkersson, MD, PhD, presented a cohort study that utilized Swedish national registries to examine the relationship between type 1 diabetes and schizophrenia. The study comprised 1,745,977 individuals, of whom 10,117 had type 1 diabetes, who were followed for a median of 9.7 and maximum of 18 years from their 13th birthday. During follow-up, 1,280 individuals were diagnosed with schizophrenia and 649 others with schizoaffective disorder. The adjusted risk of schizophrenia was 70% lower in patients with type 1 diabetes. However, there was no difference in the risk of schizoaffective disorder in the type 1 diabetic versus nondiabetic subjects.
The Swedish data confirm the findings of an earlier Finnish national study showing that the risk of schizophrenia is reduced in patients with type 1 diabetes (Arch Gen Psychiatry. 2007 Aug;64(8):894-9). These findings raise the intriguing possibility that autoimmunity somehow figures into the etiology of the psychiatric disorder. Other investigators have previously reported a reduced prevalence of rheumatoid arthritis in patients with schizophrenia, noted Dr. Melkersson of the Karolinska Institute in Stockholm.
She reported having no financial conflicts regarding her study.
SOURCE: Osler M. ECNP Abstract P180. Melkersson K. Abstract 81.
COPENHAGEN – Selected antidiabetes medications appear to blunt the increased risk of dementia associated with type 2 diabetes, according to a Danish national case control registry study.
This benefit applies to the newer antidiabetic agents – specifically, the dipeptidyl peptidase 4 (DPP4) inhibitors, the glucagon-like peptide 1 (GLP1) analogs, and the sodium-glucose transport protein 2 (SGLT2) inhibitors – and metformin as well, Merete Osler, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, neither insulin nor the sulfonylureas showed any signal of a protective effect against development of dementia. In fact, the use of sulfonylureas was associated with a small but statistically significant 7% increased risk, added Dr. Osler, of the University of Copenhagen.
Elsewhere at the meeting, investigators tapped a Swedish national registry to demonstrate that individuals with type 1 diabetes have a sharply reduced risk of developing schizophrenia.
Type 2 diabetes medications and dementia
Dr. Osler and colleagues are among several groups of investigators who have previously shown that patients with type 2 diabetes have an increased risk of dementia.
“This has raised the question of the role of dysregulated glucose metabolism in the development of this neurodegenerative disorder, and the possible effect of antidiabetic medications,” she noted.
To further explore this issue, which links two great ongoing global epidemics, Dr. Osler and coinvestigators conducted a nested case-control study including all 176,250 patients with type 2 diabetes in the comprehensive Danish National Diabetes Register for 1995-2012. The 11,619 patients with type 2 diabetes who received a dementia diagnosis were matched with 46,476 type 2 diabetes patients without dementia. The objective was to determine associations between dementia and ever-use and cumulative dose of antidiabetes drugs, alone and in combination, in logistic regression analyses adjusted for demographics, comorbid conditions, marital status, diabetic complications, and year of dementia diagnosis.
Patients who had ever used metformin had an adjusted 6% reduction in the likelihood of dementia compared with metformin nonusers, a modest but statistically significant difference. Those on a DPP4 inhibitor had a 20% reduction in risk. The GLP1 analogs were associated with a 42% decrease in risk. So were the SGLT2 inhibitors. A dose-response relationship was evident: The higher the cumulative exposure to these agents, the lower the odds of dementia.
Combination therapy is common in type 2 diabetes, so the investigators scrutinized the impact of a variety of multidrug combinations. Combinations including a DPP4 inhibitor or GLP1 analog were also associated with significantly reduced dementia risk.
Records of glycemic control in the form of hemoglobin A1c values were available on only 1,446 type 2 diabetic dementia patients and 4,003 matched controls. An analysis that incorporated this variable showed that the observed anti-dementia effect of selected diabetes drugs was independent of glycemic control, according to Dr. Osler.
The protective effect appeared to extend to both Alzheimer’s disease and vascular dementias, although firm conclusions can’t be drawn on this score because the study was insufficiently powered to address that issue.
Dr. Osler noted that the Danish study confirms a recent Taiwanese study showing an apparent protective effect against dementia for metformin in patients with type 2 diabetes (Aging Dis. 2019 Feb 1;10(1):37-48).
“Ours is the first study on the newer diabetic drugs, so our results need to be confirmed,” she pointed out.
If confirmed, however, it would warrant exploration of these drugs more generally as potential interventions to prevent dementia. That could open a whole new chapter in the remarkable story of the SGLT2 inhibitors, a class of drugs originally developed for treatment of type 2 diabetes but which in major randomized clinical trials later proved to be so effective in the treatment of heart failure that they are now considered cardiology drugs first.
Asked if she thinks these antidiabetes agents have a general neuroprotective effect or, instead, that the observed reduced risk of dementia is a function of patients being treated better early on with modern drugs, the psychiatrist replied, “I think it might be a combination of both, especially because we find different risk estimates between the drugs.”
Dr. Osler reported having no financial conflicts of interest regarding the study, which was funded by the Danish Diabetes Foundation, the Danish Medical Association, and several other foundations.
The full study details were published online shortly before her presentation at ECNP 2019 (Eur J Endocrinol. 2019 Aug 1. pii: EJE-19-0259.R1. doi: 10.1530/EJE-19-0259).
Type 1 diabetes and schizophrenia risk
Kristina Melkersson, MD, PhD, presented a cohort study that utilized Swedish national registries to examine the relationship between type 1 diabetes and schizophrenia. The study comprised 1,745,977 individuals, of whom 10,117 had type 1 diabetes, who were followed for a median of 9.7 and maximum of 18 years from their 13th birthday. During follow-up, 1,280 individuals were diagnosed with schizophrenia and 649 others with schizoaffective disorder. The adjusted risk of schizophrenia was 70% lower in patients with type 1 diabetes. However, there was no difference in the risk of schizoaffective disorder in the type 1 diabetic versus nondiabetic subjects.
The Swedish data confirm the findings of an earlier Finnish national study showing that the risk of schizophrenia is reduced in patients with type 1 diabetes (Arch Gen Psychiatry. 2007 Aug;64(8):894-9). These findings raise the intriguing possibility that autoimmunity somehow figures into the etiology of the psychiatric disorder. Other investigators have previously reported a reduced prevalence of rheumatoid arthritis in patients with schizophrenia, noted Dr. Melkersson of the Karolinska Institute in Stockholm.
She reported having no financial conflicts regarding her study.
SOURCE: Osler M. ECNP Abstract P180. Melkersson K. Abstract 81.
COPENHAGEN – Selected antidiabetes medications appear to blunt the increased risk of dementia associated with type 2 diabetes, according to a Danish national case control registry study.
This benefit applies to the newer antidiabetic agents – specifically, the dipeptidyl peptidase 4 (DPP4) inhibitors, the glucagon-like peptide 1 (GLP1) analogs, and the sodium-glucose transport protein 2 (SGLT2) inhibitors – and metformin as well, Merete Osler, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
In contrast, neither insulin nor the sulfonylureas showed any signal of a protective effect against development of dementia. In fact, the use of sulfonylureas was associated with a small but statistically significant 7% increased risk, added Dr. Osler, of the University of Copenhagen.
Elsewhere at the meeting, investigators tapped a Swedish national registry to demonstrate that individuals with type 1 diabetes have a sharply reduced risk of developing schizophrenia.
Type 2 diabetes medications and dementia
Dr. Osler and colleagues are among several groups of investigators who have previously shown that patients with type 2 diabetes have an increased risk of dementia.
“This has raised the question of the role of dysregulated glucose metabolism in the development of this neurodegenerative disorder, and the possible effect of antidiabetic medications,” she noted.
To further explore this issue, which links two great ongoing global epidemics, Dr. Osler and coinvestigators conducted a nested case-control study including all 176,250 patients with type 2 diabetes in the comprehensive Danish National Diabetes Register for 1995-2012. The 11,619 patients with type 2 diabetes who received a dementia diagnosis were matched with 46,476 type 2 diabetes patients without dementia. The objective was to determine associations between dementia and ever-use and cumulative dose of antidiabetes drugs, alone and in combination, in logistic regression analyses adjusted for demographics, comorbid conditions, marital status, diabetic complications, and year of dementia diagnosis.
Patients who had ever used metformin had an adjusted 6% reduction in the likelihood of dementia compared with metformin nonusers, a modest but statistically significant difference. Those on a DPP4 inhibitor had a 20% reduction in risk. The GLP1 analogs were associated with a 42% decrease in risk. So were the SGLT2 inhibitors. A dose-response relationship was evident: The higher the cumulative exposure to these agents, the lower the odds of dementia.
Combination therapy is common in type 2 diabetes, so the investigators scrutinized the impact of a variety of multidrug combinations. Combinations including a DPP4 inhibitor or GLP1 analog were also associated with significantly reduced dementia risk.
Records of glycemic control in the form of hemoglobin A1c values were available on only 1,446 type 2 diabetic dementia patients and 4,003 matched controls. An analysis that incorporated this variable showed that the observed anti-dementia effect of selected diabetes drugs was independent of glycemic control, according to Dr. Osler.
The protective effect appeared to extend to both Alzheimer’s disease and vascular dementias, although firm conclusions can’t be drawn on this score because the study was insufficiently powered to address that issue.
Dr. Osler noted that the Danish study confirms a recent Taiwanese study showing an apparent protective effect against dementia for metformin in patients with type 2 diabetes (Aging Dis. 2019 Feb 1;10(1):37-48).
“Ours is the first study on the newer diabetic drugs, so our results need to be confirmed,” she pointed out.
If confirmed, however, it would warrant exploration of these drugs more generally as potential interventions to prevent dementia. That could open a whole new chapter in the remarkable story of the SGLT2 inhibitors, a class of drugs originally developed for treatment of type 2 diabetes but which in major randomized clinical trials later proved to be so effective in the treatment of heart failure that they are now considered cardiology drugs first.
Asked if she thinks these antidiabetes agents have a general neuroprotective effect or, instead, that the observed reduced risk of dementia is a function of patients being treated better early on with modern drugs, the psychiatrist replied, “I think it might be a combination of both, especially because we find different risk estimates between the drugs.”
Dr. Osler reported having no financial conflicts of interest regarding the study, which was funded by the Danish Diabetes Foundation, the Danish Medical Association, and several other foundations.
The full study details were published online shortly before her presentation at ECNP 2019 (Eur J Endocrinol. 2019 Aug 1. pii: EJE-19-0259.R1. doi: 10.1530/EJE-19-0259).
Type 1 diabetes and schizophrenia risk
Kristina Melkersson, MD, PhD, presented a cohort study that utilized Swedish national registries to examine the relationship between type 1 diabetes and schizophrenia. The study comprised 1,745,977 individuals, of whom 10,117 had type 1 diabetes, who were followed for a median of 9.7 and maximum of 18 years from their 13th birthday. During follow-up, 1,280 individuals were diagnosed with schizophrenia and 649 others with schizoaffective disorder. The adjusted risk of schizophrenia was 70% lower in patients with type 1 diabetes. However, there was no difference in the risk of schizoaffective disorder in the type 1 diabetic versus nondiabetic subjects.
The Swedish data confirm the findings of an earlier Finnish national study showing that the risk of schizophrenia is reduced in patients with type 1 diabetes (Arch Gen Psychiatry. 2007 Aug;64(8):894-9). These findings raise the intriguing possibility that autoimmunity somehow figures into the etiology of the psychiatric disorder. Other investigators have previously reported a reduced prevalence of rheumatoid arthritis in patients with schizophrenia, noted Dr. Melkersson of the Karolinska Institute in Stockholm.
She reported having no financial conflicts regarding her study.
SOURCE: Osler M. ECNP Abstract P180. Melkersson K. Abstract 81.
REPORTING FROM ECNP 2019
Eating disorders may add to poor type 2 control, but BMI confounds the issue
Type 2 diabetes patients with binge-eating psychopathology had worse glycemic control than did type 2 diabetes patients without eating disorders, but weight may be a modifying factor, according to a study of 70 outpatients with type 2 diabetes.
“Although the comorbidity of an ED [eating disorder] and T2DM [type 2 diabetes mellitus] has been observed across studies, the impact of this association on the clinical control of diabetes has been less consistent,” wrote Marcello Papelbaum, MD, of the State Institute of Diabetes and Endocrinology, Rio de Janeiro and colleagues.
In an exploratory study published in the Journal of Eating Disorders, the researchers assessed consecutive diabetes patients at a single center. The patients were aged 18-65 years, 77% were women, and 50% were obese. Glycemic control of diabetes was assessed measuring the levels of fasting blood glucose (FBG) and hemoglobin A1c. A total of 14 patients had an eating disorder, and 7 of them had binge eating disorder (BED). The BED patients were combined with three bulimic patients and four patients with subclinical BED and classified as binge-eating related ED.
Although FBG and HbA1c were significantly worse in patients with an eating disorder, compared with patients with normal eating patterns, the significance disappeared when body mass index (BMI) was added to the regression model. “Specifically, normal-BMI individuals exhibited a rate of ED of 8%, contrasted with a 26% prevalence of ED in obese patients,” the authors stated.
The findings were limited by the exploratory study design, small sample size, and lack of controlling for multiple variables, the researchers noted.
However, “although the objective negative clinical impact of an ED on type 2 diabetes control is yet to be confirmed, is possible to speculate that the remission of binge episodes could play a major role in diabetes treatment,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Papelbaum M et al. J Eat Disord. 2019 Sep 6. doi: 10.1186/s40337-019-0260-4.
Type 2 diabetes patients with binge-eating psychopathology had worse glycemic control than did type 2 diabetes patients without eating disorders, but weight may be a modifying factor, according to a study of 70 outpatients with type 2 diabetes.
“Although the comorbidity of an ED [eating disorder] and T2DM [type 2 diabetes mellitus] has been observed across studies, the impact of this association on the clinical control of diabetes has been less consistent,” wrote Marcello Papelbaum, MD, of the State Institute of Diabetes and Endocrinology, Rio de Janeiro and colleagues.
In an exploratory study published in the Journal of Eating Disorders, the researchers assessed consecutive diabetes patients at a single center. The patients were aged 18-65 years, 77% were women, and 50% were obese. Glycemic control of diabetes was assessed measuring the levels of fasting blood glucose (FBG) and hemoglobin A1c. A total of 14 patients had an eating disorder, and 7 of them had binge eating disorder (BED). The BED patients were combined with three bulimic patients and four patients with subclinical BED and classified as binge-eating related ED.
Although FBG and HbA1c were significantly worse in patients with an eating disorder, compared with patients with normal eating patterns, the significance disappeared when body mass index (BMI) was added to the regression model. “Specifically, normal-BMI individuals exhibited a rate of ED of 8%, contrasted with a 26% prevalence of ED in obese patients,” the authors stated.
The findings were limited by the exploratory study design, small sample size, and lack of controlling for multiple variables, the researchers noted.
However, “although the objective negative clinical impact of an ED on type 2 diabetes control is yet to be confirmed, is possible to speculate that the remission of binge episodes could play a major role in diabetes treatment,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Papelbaum M et al. J Eat Disord. 2019 Sep 6. doi: 10.1186/s40337-019-0260-4.
Type 2 diabetes patients with binge-eating psychopathology had worse glycemic control than did type 2 diabetes patients without eating disorders, but weight may be a modifying factor, according to a study of 70 outpatients with type 2 diabetes.
“Although the comorbidity of an ED [eating disorder] and T2DM [type 2 diabetes mellitus] has been observed across studies, the impact of this association on the clinical control of diabetes has been less consistent,” wrote Marcello Papelbaum, MD, of the State Institute of Diabetes and Endocrinology, Rio de Janeiro and colleagues.
In an exploratory study published in the Journal of Eating Disorders, the researchers assessed consecutive diabetes patients at a single center. The patients were aged 18-65 years, 77% were women, and 50% were obese. Glycemic control of diabetes was assessed measuring the levels of fasting blood glucose (FBG) and hemoglobin A1c. A total of 14 patients had an eating disorder, and 7 of them had binge eating disorder (BED). The BED patients were combined with three bulimic patients and four patients with subclinical BED and classified as binge-eating related ED.
Although FBG and HbA1c were significantly worse in patients with an eating disorder, compared with patients with normal eating patterns, the significance disappeared when body mass index (BMI) was added to the regression model. “Specifically, normal-BMI individuals exhibited a rate of ED of 8%, contrasted with a 26% prevalence of ED in obese patients,” the authors stated.
The findings were limited by the exploratory study design, small sample size, and lack of controlling for multiple variables, the researchers noted.
However, “although the objective negative clinical impact of an ED on type 2 diabetes control is yet to be confirmed, is possible to speculate that the remission of binge episodes could play a major role in diabetes treatment,” they said.
The researchers had no financial conflicts to disclose.
SOURCE: Papelbaum M et al. J Eat Disord. 2019 Sep 6. doi: 10.1186/s40337-019-0260-4.
FROM THE JOURNAL OF EATING DISORDERS
Duloxetine ‘sprinkle’ launches for patients with difficulty swallowing
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Obesity ups type 2 diabetes risk far more than lifestyle, genetics
BARCELONA – Obesity, more so than having a poor lifestyle, significantly raised the odds of developing type 2 diabetes, independent of individuals’ genetic susceptibility, according to data from a Danish population-based, case-cohort study.
In fact, having a body mass index (BMI) of more than 30 kg/m2 was linked with a 480% risk of incident type 2 diabetes, compared with being of normal weight (BMI, 18.5-24.9 kg/m2). The 95% confidence interval was 5.16-6.55. Being overweight (BMI, 25-29.9 kg/m2) also carried a 100% increased risk of type 2 diabetes (hazard ratio, 2.37; 95% CI, 2.15-2.62).
Having an unfavorable lifestyle – which was defined as having no or only one of several healthy-living characteristics, from not smoking and moderating alcohol use to eating a well-balanced, nutritious diet and exercising regularly – increased the risk of diabetes by 18%, compared with having a favorable lifestyle (HR, 1.18; 95% CI, 1.06-1.30).
Individuals with a high genetic risk score (GRS) had a 100% increased risk of developing the disease versus those with a low GRS (HR, 2.0; 95% CI, 1.1-1.3).
“High genetic risk, obesity, and [an] unfavorable lifestyle increase the individual-level risk of incident type 2 diabetes,” Hermina Jakupovic and associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes. Their results suggest that “the effect of obesity on type 2 diabetes risk is dominant over other risk factors, highlighting the importance of weight management in type 2 diabetes prevention.”
Ms. Jakupovic, a PhD student at the Novo Nordisk Foundation Center for Basic Metabolic Research at the University of Copenhagen, and coauthors examined data on 9,555 participants of the Diet, Cancer, and Health cohort, a large, prospective study that has been running since the early 1990s.
Around half of the study sample were women and the mean age was 52 years. Just over one-fifth (22.8%) were obese, 43% were overweight, and the remaining 35.2% were of normal weight. A quarter (25.4%) had an unfavorable lifestyle, 40% a favorable lifestyle, and the remainder an “intermediate” lifestyle. Over a follow-up of almost 15 years, nearly half (49.5%) developed type 2 diabetes.
Genetic risk was assessed by a GRS comprising 193 genetic variants known to be strongly associated with type 2 diabetes, Ms. Jakupovic explained, adding that, using the GRS, patients were categorized into being at low (the lowest 20%), intermediate (middle 60%) and high risk (top 20%) of type 2 diabetes.
Considering individuals’ GRS and lifestyle score together showed an increasing risk of developing type 2 diabetes from the low GRS/favorable-lifestyle category (HR, 1.0; reference) upward to the high GRS/unfavorable lifestyle (HR, 2.22; 95% CI, 1.76-2.81).
The Diet, Cancer, and Health cohort is supported by the Danish Cancer Society. The Novo Nordisk Foundation Center for Basic Metabolic Research is an independent research center at the University of Copenhagen partially funded by an unrestricted donation from the Novo Nordisk Foundation. Ms. Jakupovic and associates are funded either directly or indirectly by the Novo Nordisk Foundation.
SOURCE: Jakupovic H et al. EASD 2019, Abstract 376.
BARCELONA – Obesity, more so than having a poor lifestyle, significantly raised the odds of developing type 2 diabetes, independent of individuals’ genetic susceptibility, according to data from a Danish population-based, case-cohort study.
In fact, having a body mass index (BMI) of more than 30 kg/m2 was linked with a 480% risk of incident type 2 diabetes, compared with being of normal weight (BMI, 18.5-24.9 kg/m2). The 95% confidence interval was 5.16-6.55. Being overweight (BMI, 25-29.9 kg/m2) also carried a 100% increased risk of type 2 diabetes (hazard ratio, 2.37; 95% CI, 2.15-2.62).
Having an unfavorable lifestyle – which was defined as having no or only one of several healthy-living characteristics, from not smoking and moderating alcohol use to eating a well-balanced, nutritious diet and exercising regularly – increased the risk of diabetes by 18%, compared with having a favorable lifestyle (HR, 1.18; 95% CI, 1.06-1.30).
Individuals with a high genetic risk score (GRS) had a 100% increased risk of developing the disease versus those with a low GRS (HR, 2.0; 95% CI, 1.1-1.3).
“High genetic risk, obesity, and [an] unfavorable lifestyle increase the individual-level risk of incident type 2 diabetes,” Hermina Jakupovic and associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes. Their results suggest that “the effect of obesity on type 2 diabetes risk is dominant over other risk factors, highlighting the importance of weight management in type 2 diabetes prevention.”
Ms. Jakupovic, a PhD student at the Novo Nordisk Foundation Center for Basic Metabolic Research at the University of Copenhagen, and coauthors examined data on 9,555 participants of the Diet, Cancer, and Health cohort, a large, prospective study that has been running since the early 1990s.
Around half of the study sample were women and the mean age was 52 years. Just over one-fifth (22.8%) were obese, 43% were overweight, and the remaining 35.2% were of normal weight. A quarter (25.4%) had an unfavorable lifestyle, 40% a favorable lifestyle, and the remainder an “intermediate” lifestyle. Over a follow-up of almost 15 years, nearly half (49.5%) developed type 2 diabetes.
Genetic risk was assessed by a GRS comprising 193 genetic variants known to be strongly associated with type 2 diabetes, Ms. Jakupovic explained, adding that, using the GRS, patients were categorized into being at low (the lowest 20%), intermediate (middle 60%) and high risk (top 20%) of type 2 diabetes.
Considering individuals’ GRS and lifestyle score together showed an increasing risk of developing type 2 diabetes from the low GRS/favorable-lifestyle category (HR, 1.0; reference) upward to the high GRS/unfavorable lifestyle (HR, 2.22; 95% CI, 1.76-2.81).
The Diet, Cancer, and Health cohort is supported by the Danish Cancer Society. The Novo Nordisk Foundation Center for Basic Metabolic Research is an independent research center at the University of Copenhagen partially funded by an unrestricted donation from the Novo Nordisk Foundation. Ms. Jakupovic and associates are funded either directly or indirectly by the Novo Nordisk Foundation.
SOURCE: Jakupovic H et al. EASD 2019, Abstract 376.
BARCELONA – Obesity, more so than having a poor lifestyle, significantly raised the odds of developing type 2 diabetes, independent of individuals’ genetic susceptibility, according to data from a Danish population-based, case-cohort study.
In fact, having a body mass index (BMI) of more than 30 kg/m2 was linked with a 480% risk of incident type 2 diabetes, compared with being of normal weight (BMI, 18.5-24.9 kg/m2). The 95% confidence interval was 5.16-6.55. Being overweight (BMI, 25-29.9 kg/m2) also carried a 100% increased risk of type 2 diabetes (hazard ratio, 2.37; 95% CI, 2.15-2.62).
Having an unfavorable lifestyle – which was defined as having no or only one of several healthy-living characteristics, from not smoking and moderating alcohol use to eating a well-balanced, nutritious diet and exercising regularly – increased the risk of diabetes by 18%, compared with having a favorable lifestyle (HR, 1.18; 95% CI, 1.06-1.30).
Individuals with a high genetic risk score (GRS) had a 100% increased risk of developing the disease versus those with a low GRS (HR, 2.0; 95% CI, 1.1-1.3).
“High genetic risk, obesity, and [an] unfavorable lifestyle increase the individual-level risk of incident type 2 diabetes,” Hermina Jakupovic and associates reported in a poster presentation at the annual meeting of the European Association for the Study of Diabetes. Their results suggest that “the effect of obesity on type 2 diabetes risk is dominant over other risk factors, highlighting the importance of weight management in type 2 diabetes prevention.”
Ms. Jakupovic, a PhD student at the Novo Nordisk Foundation Center for Basic Metabolic Research at the University of Copenhagen, and coauthors examined data on 9,555 participants of the Diet, Cancer, and Health cohort, a large, prospective study that has been running since the early 1990s.
Around half of the study sample were women and the mean age was 52 years. Just over one-fifth (22.8%) were obese, 43% were overweight, and the remaining 35.2% were of normal weight. A quarter (25.4%) had an unfavorable lifestyle, 40% a favorable lifestyle, and the remainder an “intermediate” lifestyle. Over a follow-up of almost 15 years, nearly half (49.5%) developed type 2 diabetes.
Genetic risk was assessed by a GRS comprising 193 genetic variants known to be strongly associated with type 2 diabetes, Ms. Jakupovic explained, adding that, using the GRS, patients were categorized into being at low (the lowest 20%), intermediate (middle 60%) and high risk (top 20%) of type 2 diabetes.
Considering individuals’ GRS and lifestyle score together showed an increasing risk of developing type 2 diabetes from the low GRS/favorable-lifestyle category (HR, 1.0; reference) upward to the high GRS/unfavorable lifestyle (HR, 2.22; 95% CI, 1.76-2.81).
The Diet, Cancer, and Health cohort is supported by the Danish Cancer Society. The Novo Nordisk Foundation Center for Basic Metabolic Research is an independent research center at the University of Copenhagen partially funded by an unrestricted donation from the Novo Nordisk Foundation. Ms. Jakupovic and associates are funded either directly or indirectly by the Novo Nordisk Foundation.
SOURCE: Jakupovic H et al. EASD 2019, Abstract 376.
REPORTING FROM EASD 2019
Closed-loop delivery system increases time in target glucose range
Patients with type 1 diabetes who used a closed-loop insulin delivery system spent a greater percentage of time in their target blood glucose range, compared with patients using a sensor-augmented insulin pump.
The significant, between-group, mean-adjusted difference of 11 percentage points between the two groups translated into the closed-loop patients spending an additional 2.6 hr/day in the target range of 70-180 mg/dL, Susan A. Brown, MD, and colleagues wrote in the New England Journal of Medicine.
Most of the benefit occurred in the early morning hours, at 5 am, when 89% of patients using the closed-loop system remained in the target range, compared with 62% of those using the pump system, said Dr. Brown of the University of Virginia, Charlottesville, and colleagues.
The randomized study comprised 168 patients with a mean age of 33 years, although the age range was wide (14-71 years). The patients had a mean disease duration of 16 years. Their baseline glycated hemoglobin level ranged between 5.4% and 10.6%. At enrollment, 79% of patients used insulin pumps, and 21% used multiple daily insulin injections; 70% were using continuous glucose monitoring, of whom 86% were using pumps. Patients in both groups had follow-up visits at 2, 6, 13, and 26 weeks.
There were no dropouts in this study – 100% of clinical and telephone follow-ups were completed.
During the 6-month trial, the mean percentage of time spent in the glucose target range rose from 61% at baseline to 71% in the closed-loop group, but remained unchanged at 59% in the pump group. The difference became apparent very early in the study and remained consistent over its course.
“The mean percentage of time that the glucose level was in the target range was 70% in the closed-loop group and 59% in the control [pump] group during the daytime (6 a.m. to midnight) and 76% and 59%, respectively, during the nighttime (midnight to 6 am) ... and the greatest differences in the mean glucose level occurred at 5 a.m. and 6 a.m. [139 mg/dL in the closed-loop group vs. 166 mg/dL in the control group at both time points]. This diurnal pattern is a result of the increased aggressiveness of the algorithm to meet a lower glucose target during the second half of the night,” the authors noted.
The closed-loop system was also better than the pump system on all secondary endpoints, including the following:
- Glycated hemoglobin at 26 weeks: mean difference, –0.33 percentage points.
- Percentage of time with glucose higher than 180 mg/dL: mean difference, –10 percentage points (a difference of 2.4 hr/day).
- Percentage of time with glucose less than 70 mg/dL: mean difference, –0.88 percentage points (a difference of 13 min/day).
The other secondary endpoints – mean glucose level and mean glycated hemoglobin level – were also significantly better in those using the closed-loop system.
The benefits “consistently favored the closed-loop system across a broad range of baseline characteristics, including age, sex, body mass index, income, educational level, insulin pump or infection use, previous use of continuous glucose monitor, and glycated hemoglobin,” the authors said.
There were 17 adverse events in 16 patients in the closed-loop group, and 2 events in 2 patients in the pump group, but no incidents of severe hypoglycemia. One person in the closed-loop system experienced ketoacidosis because of a failure in the pump infusion set. There were 13 hyperglycemic or ketosis episodes in 12 patients in the closed-loop group, and 2 in 2 patients the pump group, but none of them met the criteria for diabetic ketoacidosis. All of these episodes were deemed related to infusion set failures.
There were three serious adverse events in the closed-loop group, and none related to the device. Blood ketones exceeding 1 mmol/L occurred in 11 closed-loop patients and 8 pump patients.
The results should be interpreted with consideration of potential group bias, the authors noted. “In our trial, 70% of the patients were using a continuous glucose monitor, and 79% were using an insulin pump at the time of enrollment, percentages that are substantially higher than the reported usage in the general population of type 1 diabetes. These data may reflect an interest in and willingness to use a closed-loop system among patients who were already using devices as part of diabetes management.”
Dr. Brown reported receiving grant support from Tandem Diabetes Care, Dexcom, and Roche Diagnostics. Other authors reported a range of support from numerous pharmaceutical and medical technology companies. Several reported patents on diabetes-related devices.
SOURCE: Brown SA et al. New Engl J Med. 2019 Oct 16. doi: 10.1056/NEJMoa1907863.
Patients with type 1 diabetes who used a closed-loop insulin delivery system spent a greater percentage of time in their target blood glucose range, compared with patients using a sensor-augmented insulin pump.
The significant, between-group, mean-adjusted difference of 11 percentage points between the two groups translated into the closed-loop patients spending an additional 2.6 hr/day in the target range of 70-180 mg/dL, Susan A. Brown, MD, and colleagues wrote in the New England Journal of Medicine.
Most of the benefit occurred in the early morning hours, at 5 am, when 89% of patients using the closed-loop system remained in the target range, compared with 62% of those using the pump system, said Dr. Brown of the University of Virginia, Charlottesville, and colleagues.
The randomized study comprised 168 patients with a mean age of 33 years, although the age range was wide (14-71 years). The patients had a mean disease duration of 16 years. Their baseline glycated hemoglobin level ranged between 5.4% and 10.6%. At enrollment, 79% of patients used insulin pumps, and 21% used multiple daily insulin injections; 70% were using continuous glucose monitoring, of whom 86% were using pumps. Patients in both groups had follow-up visits at 2, 6, 13, and 26 weeks.
There were no dropouts in this study – 100% of clinical and telephone follow-ups were completed.
During the 6-month trial, the mean percentage of time spent in the glucose target range rose from 61% at baseline to 71% in the closed-loop group, but remained unchanged at 59% in the pump group. The difference became apparent very early in the study and remained consistent over its course.
“The mean percentage of time that the glucose level was in the target range was 70% in the closed-loop group and 59% in the control [pump] group during the daytime (6 a.m. to midnight) and 76% and 59%, respectively, during the nighttime (midnight to 6 am) ... and the greatest differences in the mean glucose level occurred at 5 a.m. and 6 a.m. [139 mg/dL in the closed-loop group vs. 166 mg/dL in the control group at both time points]. This diurnal pattern is a result of the increased aggressiveness of the algorithm to meet a lower glucose target during the second half of the night,” the authors noted.
The closed-loop system was also better than the pump system on all secondary endpoints, including the following:
- Glycated hemoglobin at 26 weeks: mean difference, –0.33 percentage points.
- Percentage of time with glucose higher than 180 mg/dL: mean difference, –10 percentage points (a difference of 2.4 hr/day).
- Percentage of time with glucose less than 70 mg/dL: mean difference, –0.88 percentage points (a difference of 13 min/day).
The other secondary endpoints – mean glucose level and mean glycated hemoglobin level – were also significantly better in those using the closed-loop system.
The benefits “consistently favored the closed-loop system across a broad range of baseline characteristics, including age, sex, body mass index, income, educational level, insulin pump or infection use, previous use of continuous glucose monitor, and glycated hemoglobin,” the authors said.
There were 17 adverse events in 16 patients in the closed-loop group, and 2 events in 2 patients in the pump group, but no incidents of severe hypoglycemia. One person in the closed-loop system experienced ketoacidosis because of a failure in the pump infusion set. There were 13 hyperglycemic or ketosis episodes in 12 patients in the closed-loop group, and 2 in 2 patients the pump group, but none of them met the criteria for diabetic ketoacidosis. All of these episodes were deemed related to infusion set failures.
There were three serious adverse events in the closed-loop group, and none related to the device. Blood ketones exceeding 1 mmol/L occurred in 11 closed-loop patients and 8 pump patients.
The results should be interpreted with consideration of potential group bias, the authors noted. “In our trial, 70% of the patients were using a continuous glucose monitor, and 79% were using an insulin pump at the time of enrollment, percentages that are substantially higher than the reported usage in the general population of type 1 diabetes. These data may reflect an interest in and willingness to use a closed-loop system among patients who were already using devices as part of diabetes management.”
Dr. Brown reported receiving grant support from Tandem Diabetes Care, Dexcom, and Roche Diagnostics. Other authors reported a range of support from numerous pharmaceutical and medical technology companies. Several reported patents on diabetes-related devices.
SOURCE: Brown SA et al. New Engl J Med. 2019 Oct 16. doi: 10.1056/NEJMoa1907863.
Patients with type 1 diabetes who used a closed-loop insulin delivery system spent a greater percentage of time in their target blood glucose range, compared with patients using a sensor-augmented insulin pump.
The significant, between-group, mean-adjusted difference of 11 percentage points between the two groups translated into the closed-loop patients spending an additional 2.6 hr/day in the target range of 70-180 mg/dL, Susan A. Brown, MD, and colleagues wrote in the New England Journal of Medicine.
Most of the benefit occurred in the early morning hours, at 5 am, when 89% of patients using the closed-loop system remained in the target range, compared with 62% of those using the pump system, said Dr. Brown of the University of Virginia, Charlottesville, and colleagues.
The randomized study comprised 168 patients with a mean age of 33 years, although the age range was wide (14-71 years). The patients had a mean disease duration of 16 years. Their baseline glycated hemoglobin level ranged between 5.4% and 10.6%. At enrollment, 79% of patients used insulin pumps, and 21% used multiple daily insulin injections; 70% were using continuous glucose monitoring, of whom 86% were using pumps. Patients in both groups had follow-up visits at 2, 6, 13, and 26 weeks.
There were no dropouts in this study – 100% of clinical and telephone follow-ups were completed.
During the 6-month trial, the mean percentage of time spent in the glucose target range rose from 61% at baseline to 71% in the closed-loop group, but remained unchanged at 59% in the pump group. The difference became apparent very early in the study and remained consistent over its course.
“The mean percentage of time that the glucose level was in the target range was 70% in the closed-loop group and 59% in the control [pump] group during the daytime (6 a.m. to midnight) and 76% and 59%, respectively, during the nighttime (midnight to 6 am) ... and the greatest differences in the mean glucose level occurred at 5 a.m. and 6 a.m. [139 mg/dL in the closed-loop group vs. 166 mg/dL in the control group at both time points]. This diurnal pattern is a result of the increased aggressiveness of the algorithm to meet a lower glucose target during the second half of the night,” the authors noted.
The closed-loop system was also better than the pump system on all secondary endpoints, including the following:
- Glycated hemoglobin at 26 weeks: mean difference, –0.33 percentage points.
- Percentage of time with glucose higher than 180 mg/dL: mean difference, –10 percentage points (a difference of 2.4 hr/day).
- Percentage of time with glucose less than 70 mg/dL: mean difference, –0.88 percentage points (a difference of 13 min/day).
The other secondary endpoints – mean glucose level and mean glycated hemoglobin level – were also significantly better in those using the closed-loop system.
The benefits “consistently favored the closed-loop system across a broad range of baseline characteristics, including age, sex, body mass index, income, educational level, insulin pump or infection use, previous use of continuous glucose monitor, and glycated hemoglobin,” the authors said.
There were 17 adverse events in 16 patients in the closed-loop group, and 2 events in 2 patients in the pump group, but no incidents of severe hypoglycemia. One person in the closed-loop system experienced ketoacidosis because of a failure in the pump infusion set. There were 13 hyperglycemic or ketosis episodes in 12 patients in the closed-loop group, and 2 in 2 patients the pump group, but none of them met the criteria for diabetic ketoacidosis. All of these episodes were deemed related to infusion set failures.
There were three serious adverse events in the closed-loop group, and none related to the device. Blood ketones exceeding 1 mmol/L occurred in 11 closed-loop patients and 8 pump patients.
The results should be interpreted with consideration of potential group bias, the authors noted. “In our trial, 70% of the patients were using a continuous glucose monitor, and 79% were using an insulin pump at the time of enrollment, percentages that are substantially higher than the reported usage in the general population of type 1 diabetes. These data may reflect an interest in and willingness to use a closed-loop system among patients who were already using devices as part of diabetes management.”
Dr. Brown reported receiving grant support from Tandem Diabetes Care, Dexcom, and Roche Diagnostics. Other authors reported a range of support from numerous pharmaceutical and medical technology companies. Several reported patents on diabetes-related devices.
SOURCE: Brown SA et al. New Engl J Med. 2019 Oct 16. doi: 10.1056/NEJMoa1907863.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Clinical Pharmacists Improve Patient Outcomes and Expand Access to Care
The US is in the midst of a chronic disease crisis. According to the latest published data available, 60% of Americans have at least 1 chronic condition, and 42% have ≥ 2 chronic conditions.1 Estimates by the Health Resources and Services Administration (HRSA) indicate a current shortfall of 13 800 primary care physicians and a projected escalation of that shortage to be between 14 800 and 49 300 physicians by the year 2030.2
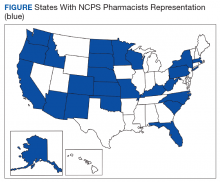
The US Public Health Service (USPHS) has used pharmacists since 1930 to provide direct patient care to underserved and vulnerable populations. Clinical pharmacists currently serve in direct patient care roles within the Indian Health Service (IHS), Federal Bureau of Prisons (BOP), Immigration and Customs Enforcement (ICE), and the United States Coast Guard (USCG) in many states (Figure). These pharmacists play a vital role in improving access to care and delivering quality care by managing acute and chronic diseases in collaborative practice settings and pharmacist-managed clinics.
It has previously been reported that in the face of physician shortages and growing demand for primary health care providers, pharmacists are well-equipped and motivated to meet this demand.3 A review of the previous 2 years of outcomes reported by clinical pharmacists certified through the USPHS National Clinical Pharmacy Specialist (NCPS) Committee are presented to demonstrate the impact of pharmacists in advancing the health of the populations they serve and to showcase a model for ameliorating the ongoing physician shortage.
Background
The USPHS NCPS Committee serves to promote uniform competency among clinical pharmacists by establishing national standards for protocols, collaborative practice agreements (CPAs), credentialing and privileging of pharmacists, and by collecting, reviewing, and publishing health care outcomes. The committee, whose constituents include pharmacist and physician subject matter experts from across USPHS agencies, reviews applications and protocols and certifies pharmacists (civilian and uniformed) to recognize an advanced scope of practice in managing various diseases and optimizing medication therapy. NCPScertified pharmacists manage a wide spectrum of diseases, including coagulopathy, asthma, diabetes mellitus (DM), hepatitis C, HIV, hypertension, pain, seizure disorders, and tobacco use disorders.
Clinical pharmacists practicing chronic disease management establish a clinical service in collaboration with 1 or more physicians, physician assistants, or nurse practitioners. In this collaborative practice, the health care practitioner(s) refer patients to be managed by a pharmacist for specific medical needs, such as anticoagulation management, or for holistic medication- focused care (eg, cardiovascular risk reduction, DM management, HIV, hepatitis, or mental health). The pharmacist may order and interpret laboratory tests, check vital signs, perform a limited physical examination, and gather other pertinent information from the patient and the medical record in order to provide the best possible care to the patient.
Medications may be started, stopped, or adjusted, education is provided, and therapeutic lifestyle interventions may be recommended. The pharmacist-run clinic provides the patient more frequent interaction with a health care professional (pharmacist) and focused disease management. As a result, pharmacists increase access to care and allow the medical team to handle a larger panel of patients as the practitioner delegates specified diseases to the pharmacist- managed clinic(s). The number of NCPS-certified pharmacists grew 46% from 2012 (n = 230) to 2017 (n = 336), reflecting an evolution of pharmacists’ practice to better meet the need of patients across the nation.
Methods
The NCPS Committee requires NCPS pharmacists to report data annually from all patients referred for pharmacist management for specific diseases in which they have been certified. The data reflect the patient’s clinical outcome goal status at the time of referral as well as the same status at the end of the reporting period or on release from the pharmacist-run clinic. These data describe the impact prescribing pharmacists have on patients reaching clinical outcome goals acting as the team member specializing in the medication selection and dosing aspect of care.
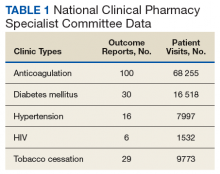
These records were reviewed for the fiscal year (FY) periods of October 1, 2015 to September 30, 2016 (FY 2016) and October 1, 2016 to September 30, 2017 (FY 2017). A systematic review of submitted reports resulted in 181 reports that included all requested data points for the disease as published here for FYs 2016 and 2017. These include 66 reports from FY 2016 and 115 reports from FY 2017; they cover 76 BOP and IHS facilities located across 24 states. Table 1 shows the number of outcome reports collected from 104 075 patient visits in pharmacist-run clinics in FYs 2016 and 2017.
Results
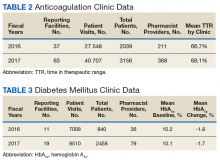
The following tables represent the standardized outcomes collected by NCPS-certified pharmacists providing direct patient care. Patients on anticoagulants (eg, warfarin) require special monitoring and education for drug interactions and adverse effects. NCPS-certified pharmacists were able to achieve a mean patient time in therapeutic range (TTR) of 67.6% (regardless of indication) over the 2 years (calculated per each facility by Rosendaal method of linear interpolation then combined in a weighted average per visit). The TTR produced by NCPS-certified pharmacists are consistent with Chest Guidelines and Expert Panel Report suggesting that TTR should be between 65% and 70%.4 Table 2 shows data from 100 reports with 68 255 patient visits for anticoagulation management.
DM management can be complex and time-intensive. NCPS data indicate pharmacist intervention resulted in a mean decrease in hemoglobin A1c (HbA1c) of 1.8% from a baseline of 10.2% (decrease calculated per each facility then combined by weighted average per visit). Table 3 shows data from 30 reports with 16 518 patient visits for DM care.
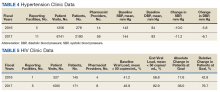
In addition to diet and exercise, medication management plays a vital role in managing hypertension. Patients managed by an NCPS-certified pharmacist experienced a mean decrease in blood pressure from 144/83 to 133/77, putting them in goal for both systolic and diastolic ranges (decrease calculated per each facility then combined by weighted average per visit). Table 4 shows data from 16 reports and 7997 patient visits for treatment of hypertension.
HIV viral suppression is vital in order to best manage patients with HIV and reduce the risk of transmission. Pharmacistled clinics have shown a 32.9% absolute improvement in patients at goal (viral load < 50 copies/mL), from a mean baseline of 46.0% to a mean final assessment of 71.6% of patients at goal (combined by weighted average visits). Table 5 shows data from 6 reports covering 1532 patient encounters for management of HIV.
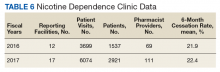
Nicotine dependence includes the use of cigarettes, cigars, pipe tobacco, chewing tobacco, and vaping products containing nicotine. NCPS-certified pharmacists have successfully helped patients improve their chance of quitting, with a 6-month quit rate of 22.2% (quit rate calculated per each facility then combined by weighted average by visits), which is higher than the national average of 9.4% as reported by the Centers for Disease and Control and Prevention. 5 Table 6 shows 29 reports covering 9773 patient visits for treatment of nicotine dependence.
Discussion
These data demonstrate the ability of advanced practice pharmacists in multiple locations within the federal sector to improve targeted clinical outcomes in patients with varying diseases. These results are strengthened by their varied origins as well as the improvements observed across the board. Limitations include the general lack of a comparable dataset, manual method of selfreporting by the individual facilities, and the relatively limited array of diseases reported. Although NCPS-certified pharmacists are currently providing care for patients with hepatitis C, asthma, seizure, pain and other diseases not reported here, there are insufficient data collected for FYs 2016 and 2017 to merit inclusion within this report.
Pharmacists are trusted, readily available medication experts. In a clinical role, NCPS-certified pharmacists have increased access to primary care services and demonstrated beneficial impact on important health outcomes as exhibited by the data reported above. Clinical pharmacy is a growing field, and NCPS has displayed continual growth in both the number of NCPS-certified pharmacists and the number of patient encounters performed by these providers. As more pharmacists in all settings collaborate with medical providers to offer high-quality clinical care, these providers will have more opportunity to delegate disease management. Continued reporting of clinical pharmacy outcomes is expected to increase confidence in pharmacists as primary care providers, increase utilization of pharmacy clinical services, and assist in easing the burden of primary care provider shortages across our nation.
Although these outcomes indicate demonstrable benefit in patient-centered outcomes, the need for ongoing assessment and continued improvement is not obviated. Future efforts may benefit from a comparison of alternative approaches to better facilitate the establishment of best practices. Alignment of clinical outcomes with the Centers for Medicare and Medicaid Services (CMS) Electronic Clinical Quality Measures, where applicable, also may prove beneficial by automating the reporting process and thereby decreasing the burden of reporting as well as providing an avenue for standard comparison across multiple populations. Clinical pharmacy interventions have positive outcomes based on the NCPS model, and the NCPS Committee invites other clinical settings to report outcomes data with which to compare.
Conclusion
The NCPS Committee has documented positive outcomes of clinical pharmacy intervention and anticipates growth of the pharmacy profession as additional states and health systems recognize the capacity of the pharmacist to provide high-quality, multidisciplinary patient care. Clinical pharmacists are prepared to address critical health care needs as the US continues to face a PCP shortage.2 The NCPS Committee challenges those participating in clinical pharmacy practice to report outcomes to amplify this body of evidence.
Acknowledgments
NCPS-certified pharmacists provided the outcomes detailed in this report. For document review and edits: Federal Bureau of Prison Publication Review Workgroup; RADM Ty Bingham, USPHS; CAPT Cindy Gunderson, USPHS; CAPT Kevin Brooks, USPHS.
1. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Santa Monica, CA: Rand Corp; 2017.
2. Dall T, West T, Chakrabarti R, Reynolds R, Iacobucci W. The complexities of physician supply and demand: projections from 2016 to 2030, 2018 update. Association of American Medical Colleges. March 2018.
3. Giberson S, Yoder S, Lee MP. Improving patient and health system outcomes through advanced pharmacy practice. A report to the U.S. Surgeon General 2011. https://www .accp.com/docs/positions/misc/improving_patient_and _health_system_outcomes.pdf. Updated December 2011. Accessed September 11, 2019.
4. Lip G, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation. CHEST guideline and Expert Panel Report. Chest. 2018;154(5):1121-1201.
5. Babb S, Marlarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457-1464.
The US is in the midst of a chronic disease crisis. According to the latest published data available, 60% of Americans have at least 1 chronic condition, and 42% have ≥ 2 chronic conditions.1 Estimates by the Health Resources and Services Administration (HRSA) indicate a current shortfall of 13 800 primary care physicians and a projected escalation of that shortage to be between 14 800 and 49 300 physicians by the year 2030.2
The US Public Health Service (USPHS) has used pharmacists since 1930 to provide direct patient care to underserved and vulnerable populations. Clinical pharmacists currently serve in direct patient care roles within the Indian Health Service (IHS), Federal Bureau of Prisons (BOP), Immigration and Customs Enforcement (ICE), and the United States Coast Guard (USCG) in many states (Figure). These pharmacists play a vital role in improving access to care and delivering quality care by managing acute and chronic diseases in collaborative practice settings and pharmacist-managed clinics.
It has previously been reported that in the face of physician shortages and growing demand for primary health care providers, pharmacists are well-equipped and motivated to meet this demand.3 A review of the previous 2 years of outcomes reported by clinical pharmacists certified through the USPHS National Clinical Pharmacy Specialist (NCPS) Committee are presented to demonstrate the impact of pharmacists in advancing the health of the populations they serve and to showcase a model for ameliorating the ongoing physician shortage.
Background
The USPHS NCPS Committee serves to promote uniform competency among clinical pharmacists by establishing national standards for protocols, collaborative practice agreements (CPAs), credentialing and privileging of pharmacists, and by collecting, reviewing, and publishing health care outcomes. The committee, whose constituents include pharmacist and physician subject matter experts from across USPHS agencies, reviews applications and protocols and certifies pharmacists (civilian and uniformed) to recognize an advanced scope of practice in managing various diseases and optimizing medication therapy. NCPScertified pharmacists manage a wide spectrum of diseases, including coagulopathy, asthma, diabetes mellitus (DM), hepatitis C, HIV, hypertension, pain, seizure disorders, and tobacco use disorders.
Clinical pharmacists practicing chronic disease management establish a clinical service in collaboration with 1 or more physicians, physician assistants, or nurse practitioners. In this collaborative practice, the health care practitioner(s) refer patients to be managed by a pharmacist for specific medical needs, such as anticoagulation management, or for holistic medication- focused care (eg, cardiovascular risk reduction, DM management, HIV, hepatitis, or mental health). The pharmacist may order and interpret laboratory tests, check vital signs, perform a limited physical examination, and gather other pertinent information from the patient and the medical record in order to provide the best possible care to the patient.
Medications may be started, stopped, or adjusted, education is provided, and therapeutic lifestyle interventions may be recommended. The pharmacist-run clinic provides the patient more frequent interaction with a health care professional (pharmacist) and focused disease management. As a result, pharmacists increase access to care and allow the medical team to handle a larger panel of patients as the practitioner delegates specified diseases to the pharmacist- managed clinic(s). The number of NCPS-certified pharmacists grew 46% from 2012 (n = 230) to 2017 (n = 336), reflecting an evolution of pharmacists’ practice to better meet the need of patients across the nation.
Methods
The NCPS Committee requires NCPS pharmacists to report data annually from all patients referred for pharmacist management for specific diseases in which they have been certified. The data reflect the patient’s clinical outcome goal status at the time of referral as well as the same status at the end of the reporting period or on release from the pharmacist-run clinic. These data describe the impact prescribing pharmacists have on patients reaching clinical outcome goals acting as the team member specializing in the medication selection and dosing aspect of care.
These records were reviewed for the fiscal year (FY) periods of October 1, 2015 to September 30, 2016 (FY 2016) and October 1, 2016 to September 30, 2017 (FY 2017). A systematic review of submitted reports resulted in 181 reports that included all requested data points for the disease as published here for FYs 2016 and 2017. These include 66 reports from FY 2016 and 115 reports from FY 2017; they cover 76 BOP and IHS facilities located across 24 states. Table 1 shows the number of outcome reports collected from 104 075 patient visits in pharmacist-run clinics in FYs 2016 and 2017.
Results
The following tables represent the standardized outcomes collected by NCPS-certified pharmacists providing direct patient care. Patients on anticoagulants (eg, warfarin) require special monitoring and education for drug interactions and adverse effects. NCPS-certified pharmacists were able to achieve a mean patient time in therapeutic range (TTR) of 67.6% (regardless of indication) over the 2 years (calculated per each facility by Rosendaal method of linear interpolation then combined in a weighted average per visit). The TTR produced by NCPS-certified pharmacists are consistent with Chest Guidelines and Expert Panel Report suggesting that TTR should be between 65% and 70%.4 Table 2 shows data from 100 reports with 68 255 patient visits for anticoagulation management.
DM management can be complex and time-intensive. NCPS data indicate pharmacist intervention resulted in a mean decrease in hemoglobin A1c (HbA1c) of 1.8% from a baseline of 10.2% (decrease calculated per each facility then combined by weighted average per visit). Table 3 shows data from 30 reports with 16 518 patient visits for DM care.
In addition to diet and exercise, medication management plays a vital role in managing hypertension. Patients managed by an NCPS-certified pharmacist experienced a mean decrease in blood pressure from 144/83 to 133/77, putting them in goal for both systolic and diastolic ranges (decrease calculated per each facility then combined by weighted average per visit). Table 4 shows data from 16 reports and 7997 patient visits for treatment of hypertension.
HIV viral suppression is vital in order to best manage patients with HIV and reduce the risk of transmission. Pharmacistled clinics have shown a 32.9% absolute improvement in patients at goal (viral load < 50 copies/mL), from a mean baseline of 46.0% to a mean final assessment of 71.6% of patients at goal (combined by weighted average visits). Table 5 shows data from 6 reports covering 1532 patient encounters for management of HIV.
Nicotine dependence includes the use of cigarettes, cigars, pipe tobacco, chewing tobacco, and vaping products containing nicotine. NCPS-certified pharmacists have successfully helped patients improve their chance of quitting, with a 6-month quit rate of 22.2% (quit rate calculated per each facility then combined by weighted average by visits), which is higher than the national average of 9.4% as reported by the Centers for Disease and Control and Prevention. 5 Table 6 shows 29 reports covering 9773 patient visits for treatment of nicotine dependence.
Discussion
These data demonstrate the ability of advanced practice pharmacists in multiple locations within the federal sector to improve targeted clinical outcomes in patients with varying diseases. These results are strengthened by their varied origins as well as the improvements observed across the board. Limitations include the general lack of a comparable dataset, manual method of selfreporting by the individual facilities, and the relatively limited array of diseases reported. Although NCPS-certified pharmacists are currently providing care for patients with hepatitis C, asthma, seizure, pain and other diseases not reported here, there are insufficient data collected for FYs 2016 and 2017 to merit inclusion within this report.
Pharmacists are trusted, readily available medication experts. In a clinical role, NCPS-certified pharmacists have increased access to primary care services and demonstrated beneficial impact on important health outcomes as exhibited by the data reported above. Clinical pharmacy is a growing field, and NCPS has displayed continual growth in both the number of NCPS-certified pharmacists and the number of patient encounters performed by these providers. As more pharmacists in all settings collaborate with medical providers to offer high-quality clinical care, these providers will have more opportunity to delegate disease management. Continued reporting of clinical pharmacy outcomes is expected to increase confidence in pharmacists as primary care providers, increase utilization of pharmacy clinical services, and assist in easing the burden of primary care provider shortages across our nation.
Although these outcomes indicate demonstrable benefit in patient-centered outcomes, the need for ongoing assessment and continued improvement is not obviated. Future efforts may benefit from a comparison of alternative approaches to better facilitate the establishment of best practices. Alignment of clinical outcomes with the Centers for Medicare and Medicaid Services (CMS) Electronic Clinical Quality Measures, where applicable, also may prove beneficial by automating the reporting process and thereby decreasing the burden of reporting as well as providing an avenue for standard comparison across multiple populations. Clinical pharmacy interventions have positive outcomes based on the NCPS model, and the NCPS Committee invites other clinical settings to report outcomes data with which to compare.
Conclusion
The NCPS Committee has documented positive outcomes of clinical pharmacy intervention and anticipates growth of the pharmacy profession as additional states and health systems recognize the capacity of the pharmacist to provide high-quality, multidisciplinary patient care. Clinical pharmacists are prepared to address critical health care needs as the US continues to face a PCP shortage.2 The NCPS Committee challenges those participating in clinical pharmacy practice to report outcomes to amplify this body of evidence.
Acknowledgments
NCPS-certified pharmacists provided the outcomes detailed in this report. For document review and edits: Federal Bureau of Prison Publication Review Workgroup; RADM Ty Bingham, USPHS; CAPT Cindy Gunderson, USPHS; CAPT Kevin Brooks, USPHS.
The US is in the midst of a chronic disease crisis. According to the latest published data available, 60% of Americans have at least 1 chronic condition, and 42% have ≥ 2 chronic conditions.1 Estimates by the Health Resources and Services Administration (HRSA) indicate a current shortfall of 13 800 primary care physicians and a projected escalation of that shortage to be between 14 800 and 49 300 physicians by the year 2030.2
The US Public Health Service (USPHS) has used pharmacists since 1930 to provide direct patient care to underserved and vulnerable populations. Clinical pharmacists currently serve in direct patient care roles within the Indian Health Service (IHS), Federal Bureau of Prisons (BOP), Immigration and Customs Enforcement (ICE), and the United States Coast Guard (USCG) in many states (Figure). These pharmacists play a vital role in improving access to care and delivering quality care by managing acute and chronic diseases in collaborative practice settings and pharmacist-managed clinics.
It has previously been reported that in the face of physician shortages and growing demand for primary health care providers, pharmacists are well-equipped and motivated to meet this demand.3 A review of the previous 2 years of outcomes reported by clinical pharmacists certified through the USPHS National Clinical Pharmacy Specialist (NCPS) Committee are presented to demonstrate the impact of pharmacists in advancing the health of the populations they serve and to showcase a model for ameliorating the ongoing physician shortage.
Background
The USPHS NCPS Committee serves to promote uniform competency among clinical pharmacists by establishing national standards for protocols, collaborative practice agreements (CPAs), credentialing and privileging of pharmacists, and by collecting, reviewing, and publishing health care outcomes. The committee, whose constituents include pharmacist and physician subject matter experts from across USPHS agencies, reviews applications and protocols and certifies pharmacists (civilian and uniformed) to recognize an advanced scope of practice in managing various diseases and optimizing medication therapy. NCPScertified pharmacists manage a wide spectrum of diseases, including coagulopathy, asthma, diabetes mellitus (DM), hepatitis C, HIV, hypertension, pain, seizure disorders, and tobacco use disorders.
Clinical pharmacists practicing chronic disease management establish a clinical service in collaboration with 1 or more physicians, physician assistants, or nurse practitioners. In this collaborative practice, the health care practitioner(s) refer patients to be managed by a pharmacist for specific medical needs, such as anticoagulation management, or for holistic medication- focused care (eg, cardiovascular risk reduction, DM management, HIV, hepatitis, or mental health). The pharmacist may order and interpret laboratory tests, check vital signs, perform a limited physical examination, and gather other pertinent information from the patient and the medical record in order to provide the best possible care to the patient.
Medications may be started, stopped, or adjusted, education is provided, and therapeutic lifestyle interventions may be recommended. The pharmacist-run clinic provides the patient more frequent interaction with a health care professional (pharmacist) and focused disease management. As a result, pharmacists increase access to care and allow the medical team to handle a larger panel of patients as the practitioner delegates specified diseases to the pharmacist- managed clinic(s). The number of NCPS-certified pharmacists grew 46% from 2012 (n = 230) to 2017 (n = 336), reflecting an evolution of pharmacists’ practice to better meet the need of patients across the nation.
Methods
The NCPS Committee requires NCPS pharmacists to report data annually from all patients referred for pharmacist management for specific diseases in which they have been certified. The data reflect the patient’s clinical outcome goal status at the time of referral as well as the same status at the end of the reporting period or on release from the pharmacist-run clinic. These data describe the impact prescribing pharmacists have on patients reaching clinical outcome goals acting as the team member specializing in the medication selection and dosing aspect of care.
These records were reviewed for the fiscal year (FY) periods of October 1, 2015 to September 30, 2016 (FY 2016) and October 1, 2016 to September 30, 2017 (FY 2017). A systematic review of submitted reports resulted in 181 reports that included all requested data points for the disease as published here for FYs 2016 and 2017. These include 66 reports from FY 2016 and 115 reports from FY 2017; they cover 76 BOP and IHS facilities located across 24 states. Table 1 shows the number of outcome reports collected from 104 075 patient visits in pharmacist-run clinics in FYs 2016 and 2017.
Results
The following tables represent the standardized outcomes collected by NCPS-certified pharmacists providing direct patient care. Patients on anticoagulants (eg, warfarin) require special monitoring and education for drug interactions and adverse effects. NCPS-certified pharmacists were able to achieve a mean patient time in therapeutic range (TTR) of 67.6% (regardless of indication) over the 2 years (calculated per each facility by Rosendaal method of linear interpolation then combined in a weighted average per visit). The TTR produced by NCPS-certified pharmacists are consistent with Chest Guidelines and Expert Panel Report suggesting that TTR should be between 65% and 70%.4 Table 2 shows data from 100 reports with 68 255 patient visits for anticoagulation management.
DM management can be complex and time-intensive. NCPS data indicate pharmacist intervention resulted in a mean decrease in hemoglobin A1c (HbA1c) of 1.8% from a baseline of 10.2% (decrease calculated per each facility then combined by weighted average per visit). Table 3 shows data from 30 reports with 16 518 patient visits for DM care.
In addition to diet and exercise, medication management plays a vital role in managing hypertension. Patients managed by an NCPS-certified pharmacist experienced a mean decrease in blood pressure from 144/83 to 133/77, putting them in goal for both systolic and diastolic ranges (decrease calculated per each facility then combined by weighted average per visit). Table 4 shows data from 16 reports and 7997 patient visits for treatment of hypertension.
HIV viral suppression is vital in order to best manage patients with HIV and reduce the risk of transmission. Pharmacistled clinics have shown a 32.9% absolute improvement in patients at goal (viral load < 50 copies/mL), from a mean baseline of 46.0% to a mean final assessment of 71.6% of patients at goal (combined by weighted average visits). Table 5 shows data from 6 reports covering 1532 patient encounters for management of HIV.
Nicotine dependence includes the use of cigarettes, cigars, pipe tobacco, chewing tobacco, and vaping products containing nicotine. NCPS-certified pharmacists have successfully helped patients improve their chance of quitting, with a 6-month quit rate of 22.2% (quit rate calculated per each facility then combined by weighted average by visits), which is higher than the national average of 9.4% as reported by the Centers for Disease and Control and Prevention. 5 Table 6 shows 29 reports covering 9773 patient visits for treatment of nicotine dependence.
Discussion
These data demonstrate the ability of advanced practice pharmacists in multiple locations within the federal sector to improve targeted clinical outcomes in patients with varying diseases. These results are strengthened by their varied origins as well as the improvements observed across the board. Limitations include the general lack of a comparable dataset, manual method of selfreporting by the individual facilities, and the relatively limited array of diseases reported. Although NCPS-certified pharmacists are currently providing care for patients with hepatitis C, asthma, seizure, pain and other diseases not reported here, there are insufficient data collected for FYs 2016 and 2017 to merit inclusion within this report.
Pharmacists are trusted, readily available medication experts. In a clinical role, NCPS-certified pharmacists have increased access to primary care services and demonstrated beneficial impact on important health outcomes as exhibited by the data reported above. Clinical pharmacy is a growing field, and NCPS has displayed continual growth in both the number of NCPS-certified pharmacists and the number of patient encounters performed by these providers. As more pharmacists in all settings collaborate with medical providers to offer high-quality clinical care, these providers will have more opportunity to delegate disease management. Continued reporting of clinical pharmacy outcomes is expected to increase confidence in pharmacists as primary care providers, increase utilization of pharmacy clinical services, and assist in easing the burden of primary care provider shortages across our nation.
Although these outcomes indicate demonstrable benefit in patient-centered outcomes, the need for ongoing assessment and continued improvement is not obviated. Future efforts may benefit from a comparison of alternative approaches to better facilitate the establishment of best practices. Alignment of clinical outcomes with the Centers for Medicare and Medicaid Services (CMS) Electronic Clinical Quality Measures, where applicable, also may prove beneficial by automating the reporting process and thereby decreasing the burden of reporting as well as providing an avenue for standard comparison across multiple populations. Clinical pharmacy interventions have positive outcomes based on the NCPS model, and the NCPS Committee invites other clinical settings to report outcomes data with which to compare.
Conclusion
The NCPS Committee has documented positive outcomes of clinical pharmacy intervention and anticipates growth of the pharmacy profession as additional states and health systems recognize the capacity of the pharmacist to provide high-quality, multidisciplinary patient care. Clinical pharmacists are prepared to address critical health care needs as the US continues to face a PCP shortage.2 The NCPS Committee challenges those participating in clinical pharmacy practice to report outcomes to amplify this body of evidence.
Acknowledgments
NCPS-certified pharmacists provided the outcomes detailed in this report. For document review and edits: Federal Bureau of Prison Publication Review Workgroup; RADM Ty Bingham, USPHS; CAPT Cindy Gunderson, USPHS; CAPT Kevin Brooks, USPHS.
1. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Santa Monica, CA: Rand Corp; 2017.
2. Dall T, West T, Chakrabarti R, Reynolds R, Iacobucci W. The complexities of physician supply and demand: projections from 2016 to 2030, 2018 update. Association of American Medical Colleges. March 2018.
3. Giberson S, Yoder S, Lee MP. Improving patient and health system outcomes through advanced pharmacy practice. A report to the U.S. Surgeon General 2011. https://www .accp.com/docs/positions/misc/improving_patient_and _health_system_outcomes.pdf. Updated December 2011. Accessed September 11, 2019.
4. Lip G, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation. CHEST guideline and Expert Panel Report. Chest. 2018;154(5):1121-1201.
5. Babb S, Marlarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457-1464.
1. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Santa Monica, CA: Rand Corp; 2017.
2. Dall T, West T, Chakrabarti R, Reynolds R, Iacobucci W. The complexities of physician supply and demand: projections from 2016 to 2030, 2018 update. Association of American Medical Colleges. March 2018.
3. Giberson S, Yoder S, Lee MP. Improving patient and health system outcomes through advanced pharmacy practice. A report to the U.S. Surgeon General 2011. https://www .accp.com/docs/positions/misc/improving_patient_and _health_system_outcomes.pdf. Updated December 2011. Accessed September 11, 2019.
4. Lip G, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation. CHEST guideline and Expert Panel Report. Chest. 2018;154(5):1121-1201.
5. Babb S, Marlarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457-1464.
Liraglutide ‘option’ for treating pediatric type 2 diabetes
BARCELONA – The glucagon-like peptide-1 receptor agonist (GLP-1 RA) liraglutide added onto metformin with or without basal insulin effectively reduced hemoglobin A1c and fasting plasma glucose levels in children with type 2 diabetes in the 52-week ELLIPSE study.
The primary endpoint of the trial, which was the mean change in HbA1c from baseline to 26 weeks, was met, with a greater percentage point decrease with liraglutide (Victoza) than placebo (–0.64 vs. +0.42), with an estimated treatment difference of –1.06 percentage points (P less than .001). At the end of the study, the percentage point changes were –0.50 and +0.80, with a between-group difference of –1.30 in favor of liraglutide.
“Those of us working in pediatric practice are seeing an increasing demand for our clinical services in children with type 2 diabetes,” study investigator Timothy Barrett, PhD, MBBS, observed at the annual meeting of the European Association for the Study of Diabetes. This reflects the increasing prevalence of type 2 diabetes in this age group and is most likely linked to the rising rates of obesity and overweight that have been reported widely in young people in recent years, he added.
“Unfortunately, we look with envy upon our adult physician colleagues, and the range of treatments they have available to treat type 2 diabetes in adults.” In pediatrics, the only licensed treatments that have been available until recently were metformin and insulin, with the latter being an “illogical treatment to treat those with obesity-related diabetes.” The study’s findings, however, support liraglutide as another option to consider, said Dr. Barrett, a pediatric endocrinologist and professor of pediatrics and child health based at the University of Birmingham, England.
“Liraglutide at doses of up to 1.8 mg/day when added to metformin, and basal insulin if required, does seem to offer an additional treatment option for children and young people with type 2 diabetes who require improved glycemic control after they’ve reached a maximum dose of metformin,” he said.
ELLIPSE (Evaluation of Liraglutide in Pediatrics with Diabetes) was a multicenter, randomized, parallel group, placebo-controlled trial to assess the efficacy and safety of liraglutide as an add-on treatment to metformin, with or without basal insulin, in 134 overweight or obese children and adolescents (aged 10-17) with type 2 diabetes.
For inclusion, patients had to be able to complete the trial before their 18th birthday, and have an HbA1c of at least 7% if being treated with diet and exercise, or 6.5% or higher if already being treated with metformin, with or without insulin. Body mass index had to be above the 85the percentile for their age and sex.
Of 307 children and adolescents screened at 84 centers in 25 countries, 135 were randomized and 134 were treated between 2012 and 2018. Screening took place over a period of 2 weeks, after which time those eligible for the trial underwent a 3- to 4-week period where their dose of metformin was titrated if needed followed by an 8-week maintenance period. Only after that was randomization to liraglutide or placebo done, with the GLP-1R started at a subcutaneous dose of 0.6 mg and titrated up to 1.2 or 1.8 mg over 3 days to achieve a fasting plasma glucose (FPG) of less than 6.1 mmol/L (110 mg/dL). However, not all patients were escalated to the top dose, Dr. Barrett noted.
The mean age of patients in the trial was 14.5 years; about 60% of patients were female. The duration of diabetes was about 1.9 years and the average body weight and BMI a respective 91 kg and 33 kg/m2.
Over the course of the study, FPG fell by 1.06 mmol/L at week 26 and 1.03 mmol/L at week 52 in the liraglutide group but rose in the placebo group by 0.80 and 0.78 mmol/L, respectively. The estimated treatment difference was –1.88 (P = .002) and –1.81 at 26 an 52 weeks, respectively.
What was “a really gratifying to see,” said Dr. Barrett, was that the proportion of children and young people achieving a glycemic target of an HbA1c of less than 7% by the end of the double-blind treatment period was significantly higher in the liraglutide than placebo group, at 63.7% and 36.5%, respectively.
Most of the adverse effects seen in the study were gastrointestinal symptoms, including nausea, vomiting, and diarrhea, in about 20% of liraglutide-treated patients, compared with roughly 10% of placebo-treated patients. “This is really reflected in the adult studies as well, and many of these were thankfully transient.”
As for hypoglycemia, Dr. Barrett reported that there was a higher rate in liraglutide- than placebo-treated patients (45.5% vs. 25% for any event), although there were no severe episodes in the liraglutide group and one in the placebo group. Almost a third (31%) of hypoglycemic episodes were asymptomatic, versus 17.6% for the placebo group.
“This is the first successfully completed phase 3 trial showing efficacy of a noninsulin agent, in this case, for children who do not get managed solely on metformin monotherapy,” Dr. Barrett said.
The Food and Drug Administration has approved liraglutide for use in pediatric patients 10 years or older with type 2 diabetes, based in part on results of the ELLIPSE results, Novo Nordisk announced in June. The trial results were published prior to the EASD meeting (Tamborlane WV et al. N Engl J Med. 2019 Aug 15;381:637-46).
Novo Nordisk initiated and funded the trial, and most of the investigators reported receiving funds from the company outside the submitted work. Dr Barrett disclosed being a consultant to and/or receiving honoraria from AstraZeneca, Novo Nordisk and Servier.
SOURCE: Barrett T et al. EASD 2019. Abstract 84.
BARCELONA – The glucagon-like peptide-1 receptor agonist (GLP-1 RA) liraglutide added onto metformin with or without basal insulin effectively reduced hemoglobin A1c and fasting plasma glucose levels in children with type 2 diabetes in the 52-week ELLIPSE study.
The primary endpoint of the trial, which was the mean change in HbA1c from baseline to 26 weeks, was met, with a greater percentage point decrease with liraglutide (Victoza) than placebo (–0.64 vs. +0.42), with an estimated treatment difference of –1.06 percentage points (P less than .001). At the end of the study, the percentage point changes were –0.50 and +0.80, with a between-group difference of –1.30 in favor of liraglutide.
“Those of us working in pediatric practice are seeing an increasing demand for our clinical services in children with type 2 diabetes,” study investigator Timothy Barrett, PhD, MBBS, observed at the annual meeting of the European Association for the Study of Diabetes. This reflects the increasing prevalence of type 2 diabetes in this age group and is most likely linked to the rising rates of obesity and overweight that have been reported widely in young people in recent years, he added.
“Unfortunately, we look with envy upon our adult physician colleagues, and the range of treatments they have available to treat type 2 diabetes in adults.” In pediatrics, the only licensed treatments that have been available until recently were metformin and insulin, with the latter being an “illogical treatment to treat those with obesity-related diabetes.” The study’s findings, however, support liraglutide as another option to consider, said Dr. Barrett, a pediatric endocrinologist and professor of pediatrics and child health based at the University of Birmingham, England.
“Liraglutide at doses of up to 1.8 mg/day when added to metformin, and basal insulin if required, does seem to offer an additional treatment option for children and young people with type 2 diabetes who require improved glycemic control after they’ve reached a maximum dose of metformin,” he said.
ELLIPSE (Evaluation of Liraglutide in Pediatrics with Diabetes) was a multicenter, randomized, parallel group, placebo-controlled trial to assess the efficacy and safety of liraglutide as an add-on treatment to metformin, with or without basal insulin, in 134 overweight or obese children and adolescents (aged 10-17) with type 2 diabetes.
For inclusion, patients had to be able to complete the trial before their 18th birthday, and have an HbA1c of at least 7% if being treated with diet and exercise, or 6.5% or higher if already being treated with metformin, with or without insulin. Body mass index had to be above the 85the percentile for their age and sex.
Of 307 children and adolescents screened at 84 centers in 25 countries, 135 were randomized and 134 were treated between 2012 and 2018. Screening took place over a period of 2 weeks, after which time those eligible for the trial underwent a 3- to 4-week period where their dose of metformin was titrated if needed followed by an 8-week maintenance period. Only after that was randomization to liraglutide or placebo done, with the GLP-1R started at a subcutaneous dose of 0.6 mg and titrated up to 1.2 or 1.8 mg over 3 days to achieve a fasting plasma glucose (FPG) of less than 6.1 mmol/L (110 mg/dL). However, not all patients were escalated to the top dose, Dr. Barrett noted.
The mean age of patients in the trial was 14.5 years; about 60% of patients were female. The duration of diabetes was about 1.9 years and the average body weight and BMI a respective 91 kg and 33 kg/m2.
Over the course of the study, FPG fell by 1.06 mmol/L at week 26 and 1.03 mmol/L at week 52 in the liraglutide group but rose in the placebo group by 0.80 and 0.78 mmol/L, respectively. The estimated treatment difference was –1.88 (P = .002) and –1.81 at 26 an 52 weeks, respectively.
What was “a really gratifying to see,” said Dr. Barrett, was that the proportion of children and young people achieving a glycemic target of an HbA1c of less than 7% by the end of the double-blind treatment period was significantly higher in the liraglutide than placebo group, at 63.7% and 36.5%, respectively.
Most of the adverse effects seen in the study were gastrointestinal symptoms, including nausea, vomiting, and diarrhea, in about 20% of liraglutide-treated patients, compared with roughly 10% of placebo-treated patients. “This is really reflected in the adult studies as well, and many of these were thankfully transient.”
As for hypoglycemia, Dr. Barrett reported that there was a higher rate in liraglutide- than placebo-treated patients (45.5% vs. 25% for any event), although there were no severe episodes in the liraglutide group and one in the placebo group. Almost a third (31%) of hypoglycemic episodes were asymptomatic, versus 17.6% for the placebo group.
“This is the first successfully completed phase 3 trial showing efficacy of a noninsulin agent, in this case, for children who do not get managed solely on metformin monotherapy,” Dr. Barrett said.
The Food and Drug Administration has approved liraglutide for use in pediatric patients 10 years or older with type 2 diabetes, based in part on results of the ELLIPSE results, Novo Nordisk announced in June. The trial results were published prior to the EASD meeting (Tamborlane WV et al. N Engl J Med. 2019 Aug 15;381:637-46).
Novo Nordisk initiated and funded the trial, and most of the investigators reported receiving funds from the company outside the submitted work. Dr Barrett disclosed being a consultant to and/or receiving honoraria from AstraZeneca, Novo Nordisk and Servier.
SOURCE: Barrett T et al. EASD 2019. Abstract 84.
BARCELONA – The glucagon-like peptide-1 receptor agonist (GLP-1 RA) liraglutide added onto metformin with or without basal insulin effectively reduced hemoglobin A1c and fasting plasma glucose levels in children with type 2 diabetes in the 52-week ELLIPSE study.
The primary endpoint of the trial, which was the mean change in HbA1c from baseline to 26 weeks, was met, with a greater percentage point decrease with liraglutide (Victoza) than placebo (–0.64 vs. +0.42), with an estimated treatment difference of –1.06 percentage points (P less than .001). At the end of the study, the percentage point changes were –0.50 and +0.80, with a between-group difference of –1.30 in favor of liraglutide.
“Those of us working in pediatric practice are seeing an increasing demand for our clinical services in children with type 2 diabetes,” study investigator Timothy Barrett, PhD, MBBS, observed at the annual meeting of the European Association for the Study of Diabetes. This reflects the increasing prevalence of type 2 diabetes in this age group and is most likely linked to the rising rates of obesity and overweight that have been reported widely in young people in recent years, he added.
“Unfortunately, we look with envy upon our adult physician colleagues, and the range of treatments they have available to treat type 2 diabetes in adults.” In pediatrics, the only licensed treatments that have been available until recently were metformin and insulin, with the latter being an “illogical treatment to treat those with obesity-related diabetes.” The study’s findings, however, support liraglutide as another option to consider, said Dr. Barrett, a pediatric endocrinologist and professor of pediatrics and child health based at the University of Birmingham, England.
“Liraglutide at doses of up to 1.8 mg/day when added to metformin, and basal insulin if required, does seem to offer an additional treatment option for children and young people with type 2 diabetes who require improved glycemic control after they’ve reached a maximum dose of metformin,” he said.
ELLIPSE (Evaluation of Liraglutide in Pediatrics with Diabetes) was a multicenter, randomized, parallel group, placebo-controlled trial to assess the efficacy and safety of liraglutide as an add-on treatment to metformin, with or without basal insulin, in 134 overweight or obese children and adolescents (aged 10-17) with type 2 diabetes.
For inclusion, patients had to be able to complete the trial before their 18th birthday, and have an HbA1c of at least 7% if being treated with diet and exercise, or 6.5% or higher if already being treated with metformin, with or without insulin. Body mass index had to be above the 85the percentile for their age and sex.
Of 307 children and adolescents screened at 84 centers in 25 countries, 135 were randomized and 134 were treated between 2012 and 2018. Screening took place over a period of 2 weeks, after which time those eligible for the trial underwent a 3- to 4-week period where their dose of metformin was titrated if needed followed by an 8-week maintenance period. Only after that was randomization to liraglutide or placebo done, with the GLP-1R started at a subcutaneous dose of 0.6 mg and titrated up to 1.2 or 1.8 mg over 3 days to achieve a fasting plasma glucose (FPG) of less than 6.1 mmol/L (110 mg/dL). However, not all patients were escalated to the top dose, Dr. Barrett noted.
The mean age of patients in the trial was 14.5 years; about 60% of patients were female. The duration of diabetes was about 1.9 years and the average body weight and BMI a respective 91 kg and 33 kg/m2.
Over the course of the study, FPG fell by 1.06 mmol/L at week 26 and 1.03 mmol/L at week 52 in the liraglutide group but rose in the placebo group by 0.80 and 0.78 mmol/L, respectively. The estimated treatment difference was –1.88 (P = .002) and –1.81 at 26 an 52 weeks, respectively.
What was “a really gratifying to see,” said Dr. Barrett, was that the proportion of children and young people achieving a glycemic target of an HbA1c of less than 7% by the end of the double-blind treatment period was significantly higher in the liraglutide than placebo group, at 63.7% and 36.5%, respectively.
Most of the adverse effects seen in the study were gastrointestinal symptoms, including nausea, vomiting, and diarrhea, in about 20% of liraglutide-treated patients, compared with roughly 10% of placebo-treated patients. “This is really reflected in the adult studies as well, and many of these were thankfully transient.”
As for hypoglycemia, Dr. Barrett reported that there was a higher rate in liraglutide- than placebo-treated patients (45.5% vs. 25% for any event), although there were no severe episodes in the liraglutide group and one in the placebo group. Almost a third (31%) of hypoglycemic episodes were asymptomatic, versus 17.6% for the placebo group.
“This is the first successfully completed phase 3 trial showing efficacy of a noninsulin agent, in this case, for children who do not get managed solely on metformin monotherapy,” Dr. Barrett said.
The Food and Drug Administration has approved liraglutide for use in pediatric patients 10 years or older with type 2 diabetes, based in part on results of the ELLIPSE results, Novo Nordisk announced in June. The trial results were published prior to the EASD meeting (Tamborlane WV et al. N Engl J Med. 2019 Aug 15;381:637-46).
Novo Nordisk initiated and funded the trial, and most of the investigators reported receiving funds from the company outside the submitted work. Dr Barrett disclosed being a consultant to and/or receiving honoraria from AstraZeneca, Novo Nordisk and Servier.
SOURCE: Barrett T et al. EASD 2019. Abstract 84.
REPORTING FROM EASD 2019
Smoking, inactivity most powerful post-MI lifestyle risk factors
PARIS – All lifestyle-related cardiovascular risk factors aren’t equal in power when it comes to secondary prevention after a first acute MI, according to a massive Swedish registry study.
Insufficient physical activity and current smoking were consistently the strongest risk factors for all-cause mortality, major adverse cardiovascular events, and other key adverse outcomes in an analysis from the SWEDEHEART registry. The study included 65,002 patients discharged after a first MI and 325,010 age- and sex-matched controls with no prior MI followed for a median of 5.5 years and maximum of 12, Emil Hagstrom, MD, PhD, reported at the annual congress of the European Society of Cardiology.
Strongest lifestyle risk factors
The study examined the long-term relative importance of control of six major lifestyle risk factors for secondary cardiovascular prevention: current smoking, insufficient physical activity, blood pressure of 140/90 mm Hg or more, obesity, a fasting blood glucose of at least 126 mg/dL, and an LDL cholesterol of 70 mg/dL or more. Notably, two risk factors that physicians often emphasize in working with their patients with known coronary heart disease – an elevated LDL cholesterol and obesity – barely moved the needle. Out of the six risk factors scrutinized, those two consistently showed the weakest association with long-term risk of adverse outcomes. Occupying the middle ground in terms of predictive strength were hypertension and elevated blood glucose, according to Dr. Hagstrom, a cardiologist at Uppsala (Sweden) University.
Risk factor status was assessed 6-10 weeks post MI. Insufficient physical activity was defined as not engaging in at least 30 minutes of moderate-intensity exercise on at least 5 days per week. And when Dr. Hagstrom recalculated the risk of adverse outcomes using an LDL cholesterol threshold of 55 mg/dL rather than using 70 mg/dL, as recommended in new ESC secondary prevention guidelines released during the congress, the study results remained unchanged.
Cumulative effects
A key SWEDEHEART finding underscoring the importance of lifestyle in secondary prevention was that a linear stepwise relationship existed between the number of risk factors at target levels and the risk of all of the various adverse outcomes assessed, including stroke and heart failure hospitalization as well as all-cause mortality, cardiovascular mortality, and major bleeding.
Moreover, patients with none of the six risk factors outside of target when assessed after their MI had the same risks of all-cause mortality, cardiovascular mortality, and stroke as the matched controls.
For example, in an analysis adjusted for comorbid cancer, chronic obstructive pulmonary disease, and dementia, post-MI patients with zero risk factors had the same long-term risk of cardiovascular mortality as controls without a history of MI at baseline. With one risk factor not at target, a patient had a 41% increased risk compared with controls, a statistically significant difference. With two out-of-whack risk factors, the risk climbed to 102%. With three, 185%. With four risk factors not at target, the all-cause mortality risk jumped to 291%. And patients with more than four of the six risk factors not at target had a 409% greater risk of all-cause mortality than controls who had never had a heart attack.
When Dr. Hagstrom stratified subjects by age at baseline – up to 55, 56-64, 65-70, and 70-75 years – he discovered that, regardless of age, patients with zero risk factors had the same risk of all-cause mortality and other adverse outcomes as controls. However, when risk factors were present, younger patients consistently had a higher risk of all adverse outcomes than older patients with the same number of risk factors. When asked for an explanation of this phenomenon, Dr. Hagstrom noted that younger patients with multiple risk factors have a longer time to be exposed to and accumulate risk.
Follow-up of the study cohort will continue for years to come, the cardiologist promised.
At an ESC congress highlights session that closed out the meeting, Eva Prescott, MD, put the SWEDEHEART study at the top of her list of important developments in preventive cardiology arising from the congress.
“This is an excellent national registry I think we’re all envious of,” commented Dr. Prescott, a cardiologist at Copenhagen University. “The conclusion of this registry-based data, I think, is that lifestyle really remains at the core of prevention of cardiovascular events still today.”
The SWEDEHEART study analysis was funded free of commercial support. Dr. Hagstrom reported serving as a consultant to or receiving speakers’ fees from Amgen, AstraZeneca, Bayer, Novo Nordisk, and Sanofi.
PARIS – All lifestyle-related cardiovascular risk factors aren’t equal in power when it comes to secondary prevention after a first acute MI, according to a massive Swedish registry study.
Insufficient physical activity and current smoking were consistently the strongest risk factors for all-cause mortality, major adverse cardiovascular events, and other key adverse outcomes in an analysis from the SWEDEHEART registry. The study included 65,002 patients discharged after a first MI and 325,010 age- and sex-matched controls with no prior MI followed for a median of 5.5 years and maximum of 12, Emil Hagstrom, MD, PhD, reported at the annual congress of the European Society of Cardiology.
Strongest lifestyle risk factors
The study examined the long-term relative importance of control of six major lifestyle risk factors for secondary cardiovascular prevention: current smoking, insufficient physical activity, blood pressure of 140/90 mm Hg or more, obesity, a fasting blood glucose of at least 126 mg/dL, and an LDL cholesterol of 70 mg/dL or more. Notably, two risk factors that physicians often emphasize in working with their patients with known coronary heart disease – an elevated LDL cholesterol and obesity – barely moved the needle. Out of the six risk factors scrutinized, those two consistently showed the weakest association with long-term risk of adverse outcomes. Occupying the middle ground in terms of predictive strength were hypertension and elevated blood glucose, according to Dr. Hagstrom, a cardiologist at Uppsala (Sweden) University.
Risk factor status was assessed 6-10 weeks post MI. Insufficient physical activity was defined as not engaging in at least 30 minutes of moderate-intensity exercise on at least 5 days per week. And when Dr. Hagstrom recalculated the risk of adverse outcomes using an LDL cholesterol threshold of 55 mg/dL rather than using 70 mg/dL, as recommended in new ESC secondary prevention guidelines released during the congress, the study results remained unchanged.
Cumulative effects
A key SWEDEHEART finding underscoring the importance of lifestyle in secondary prevention was that a linear stepwise relationship existed between the number of risk factors at target levels and the risk of all of the various adverse outcomes assessed, including stroke and heart failure hospitalization as well as all-cause mortality, cardiovascular mortality, and major bleeding.
Moreover, patients with none of the six risk factors outside of target when assessed after their MI had the same risks of all-cause mortality, cardiovascular mortality, and stroke as the matched controls.
For example, in an analysis adjusted for comorbid cancer, chronic obstructive pulmonary disease, and dementia, post-MI patients with zero risk factors had the same long-term risk of cardiovascular mortality as controls without a history of MI at baseline. With one risk factor not at target, a patient had a 41% increased risk compared with controls, a statistically significant difference. With two out-of-whack risk factors, the risk climbed to 102%. With three, 185%. With four risk factors not at target, the all-cause mortality risk jumped to 291%. And patients with more than four of the six risk factors not at target had a 409% greater risk of all-cause mortality than controls who had never had a heart attack.
When Dr. Hagstrom stratified subjects by age at baseline – up to 55, 56-64, 65-70, and 70-75 years – he discovered that, regardless of age, patients with zero risk factors had the same risk of all-cause mortality and other adverse outcomes as controls. However, when risk factors were present, younger patients consistently had a higher risk of all adverse outcomes than older patients with the same number of risk factors. When asked for an explanation of this phenomenon, Dr. Hagstrom noted that younger patients with multiple risk factors have a longer time to be exposed to and accumulate risk.
Follow-up of the study cohort will continue for years to come, the cardiologist promised.
At an ESC congress highlights session that closed out the meeting, Eva Prescott, MD, put the SWEDEHEART study at the top of her list of important developments in preventive cardiology arising from the congress.
“This is an excellent national registry I think we’re all envious of,” commented Dr. Prescott, a cardiologist at Copenhagen University. “The conclusion of this registry-based data, I think, is that lifestyle really remains at the core of prevention of cardiovascular events still today.”
The SWEDEHEART study analysis was funded free of commercial support. Dr. Hagstrom reported serving as a consultant to or receiving speakers’ fees from Amgen, AstraZeneca, Bayer, Novo Nordisk, and Sanofi.
PARIS – All lifestyle-related cardiovascular risk factors aren’t equal in power when it comes to secondary prevention after a first acute MI, according to a massive Swedish registry study.
Insufficient physical activity and current smoking were consistently the strongest risk factors for all-cause mortality, major adverse cardiovascular events, and other key adverse outcomes in an analysis from the SWEDEHEART registry. The study included 65,002 patients discharged after a first MI and 325,010 age- and sex-matched controls with no prior MI followed for a median of 5.5 years and maximum of 12, Emil Hagstrom, MD, PhD, reported at the annual congress of the European Society of Cardiology.
Strongest lifestyle risk factors
The study examined the long-term relative importance of control of six major lifestyle risk factors for secondary cardiovascular prevention: current smoking, insufficient physical activity, blood pressure of 140/90 mm Hg or more, obesity, a fasting blood glucose of at least 126 mg/dL, and an LDL cholesterol of 70 mg/dL or more. Notably, two risk factors that physicians often emphasize in working with their patients with known coronary heart disease – an elevated LDL cholesterol and obesity – barely moved the needle. Out of the six risk factors scrutinized, those two consistently showed the weakest association with long-term risk of adverse outcomes. Occupying the middle ground in terms of predictive strength were hypertension and elevated blood glucose, according to Dr. Hagstrom, a cardiologist at Uppsala (Sweden) University.
Risk factor status was assessed 6-10 weeks post MI. Insufficient physical activity was defined as not engaging in at least 30 minutes of moderate-intensity exercise on at least 5 days per week. And when Dr. Hagstrom recalculated the risk of adverse outcomes using an LDL cholesterol threshold of 55 mg/dL rather than using 70 mg/dL, as recommended in new ESC secondary prevention guidelines released during the congress, the study results remained unchanged.
Cumulative effects
A key SWEDEHEART finding underscoring the importance of lifestyle in secondary prevention was that a linear stepwise relationship existed between the number of risk factors at target levels and the risk of all of the various adverse outcomes assessed, including stroke and heart failure hospitalization as well as all-cause mortality, cardiovascular mortality, and major bleeding.
Moreover, patients with none of the six risk factors outside of target when assessed after their MI had the same risks of all-cause mortality, cardiovascular mortality, and stroke as the matched controls.
For example, in an analysis adjusted for comorbid cancer, chronic obstructive pulmonary disease, and dementia, post-MI patients with zero risk factors had the same long-term risk of cardiovascular mortality as controls without a history of MI at baseline. With one risk factor not at target, a patient had a 41% increased risk compared with controls, a statistically significant difference. With two out-of-whack risk factors, the risk climbed to 102%. With three, 185%. With four risk factors not at target, the all-cause mortality risk jumped to 291%. And patients with more than four of the six risk factors not at target had a 409% greater risk of all-cause mortality than controls who had never had a heart attack.
When Dr. Hagstrom stratified subjects by age at baseline – up to 55, 56-64, 65-70, and 70-75 years – he discovered that, regardless of age, patients with zero risk factors had the same risk of all-cause mortality and other adverse outcomes as controls. However, when risk factors were present, younger patients consistently had a higher risk of all adverse outcomes than older patients with the same number of risk factors. When asked for an explanation of this phenomenon, Dr. Hagstrom noted that younger patients with multiple risk factors have a longer time to be exposed to and accumulate risk.
Follow-up of the study cohort will continue for years to come, the cardiologist promised.
At an ESC congress highlights session that closed out the meeting, Eva Prescott, MD, put the SWEDEHEART study at the top of her list of important developments in preventive cardiology arising from the congress.
“This is an excellent national registry I think we’re all envious of,” commented Dr. Prescott, a cardiologist at Copenhagen University. “The conclusion of this registry-based data, I think, is that lifestyle really remains at the core of prevention of cardiovascular events still today.”
The SWEDEHEART study analysis was funded free of commercial support. Dr. Hagstrom reported serving as a consultant to or receiving speakers’ fees from Amgen, AstraZeneca, Bayer, Novo Nordisk, and Sanofi.
REPORTING FROM THE ESC CONGRESS 2019