User login
ACS NSQIP pilot project IDs risks in older surgical patients
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
AT THE ACS QUALITY AND SAFETY CONFERENCE
Study reveals limits of 4-D CT scanning for parathyroid disease
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point:
Major finding: Compared with cases that showed concordance between the 4-D CT scan and the intraoperative findings, discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02).
Data source: A retrospective analysis of 411 patients with primary hyperparathyroidism who underwent preoperative 4-D CT scans followed by parathyroidectomy.
Disclosures: The researchers reported having no relevant financial disclosures.
Remediation for surgical trainees may lower attrition
Remediation programs and program director attitudes can make the difference in attrition rates among general surgery residents, according to a survey-based study.
A study by the Association of American Medical Colleges, projects a shortage of 29,000 general surgeons by 2030. Some residency programs are taking steps lower program dropout rates, which has been reported as high as 26% in some programs, according to Alexander Schwed, MD, general surgeon at Harbor–University of California, Los Angeles Medical Center.
Dr. Schwed and his colleagues conducted a survey of 21 general surgery residency program directors. In those programs, the overall attrition rate was found to be much lower than expected – 8.8% over a 5-year period (JAMA Surg. 2017 Aug 16. doi: 10.1001/jamasurg.2017.2656).
The survey showed that programs that implemented resident remediation had lower attrition rates, (21.0% vs 6.8%; P less than .001).
“The association between increased use of remediation by residency programs and low rates of resident attrition is novel,” the investigators wrote. “Nevertheless, based on our findings, high-attrition programs could lower their attrition rates through the increased use of resident remediation and increased focus on resident education.”
Both high- and low-attrition programs selected to participate in the study showed relatively similar median numbers of residents, with low-attrition programs reporting a median of 28 participants per year, and high-attrition programs reporting with 35.
Other similarities between low- and high-attrition programs include percentage of female and minority residents, median of 33.3% and 39.8% respectively, and the number of cases performed by first-, second-, and third-year residents.
The other difference between the six low-attrition programs and the five high-attrition programs was the attitude of the program directors regarding their role in the training of residents, according to researchers.
Investigators asked directors a series of questions using a Likert scale with 1 representing “strongly disagree” and 4 representing “strongly agree.”
Program directors from high- and low-attrition programs tended to agree strongly (scoring 3.8 and 3.2, respectively) with the statement that one of their main roles as a program leader was to “redirect residents who should not be surgeons.”
When asked whether “some degree of resident attrition is a necessary phenomenon,” directors from low-attrition programs scored 2.2, while those from high-attrition programs indicated stronger agreement with an overall score of 3.2.
Directors from programs with high dropout rates were also more likely to consider a 6% dropout rate to be too low, compared with directors from low-attrition programs who thought it was too high.
“When we recruit residents, we are very careful to recruit those who seem to buy into our mission, our vision, and our ideals and fit in well with our culture,” said Sharmila Dissanaike, MD, FACS, department of surgery chair at Texas Tech University Health Sciences Center, Lubbock, in an interview. “We emphasize teamwork, collegiality, and an ‘all for one and one for all’ type of mentality.”
This kind of recruitment includes having current residents be a part of the process, Dr. Dissanaike explained, and encouraging current and potential residents to have an informal dinner to get to know one another better.
For the department of surgery at Texas Tech, the collaborative culture combined with a remediation program has resulted in a drop in attrition from 20% down to 7% in recent years, Dr. Dissanaike said. In addition, the current success of her program can be partly attributed to a recent decision to maintain the number of incoming residents at five, she said.*
Larger programs can achieve similar improvement, she noted and the rising demand for surgeons makes it essential to find a solution that incorporates the benefits of both types of programs.
“We need more surgeons, we need more Graduate Medical Education spots, we need more training spots for general surgeons,” said Dr. Dissanaike. “I think within those large programs we need to find ways to structure smaller groups, maybe little pods, to help support residents so they don’t get lost.”
Dr. Schwed and his colleagues expressed concern that institutional barriers, such as the focus on test scores, may impede directors from embracing remediation.
“Greater emphasis on the written and oral General Surgery Qualifying Examination pass rates, which are now publicly posted and used by residency review committees, will likely exert pressure on program directors, who may fear that attempting to remediate a resident with poor medical knowledge may affect their program’s 5-year board pass rates,” the investigators wrote. “Our study suggests that such fears may be unfounded because programs with high levels of remediation and low attrition had similar board pass rates as those with high attrition.”
Dr. Schwed and his coinvestigators acknowledged that the programs studied may not be representative of U.S. residencies and selection bias may have affected the findings.
Researchers reported no relevant financial disclosures.
*Correction, 10/26/17: An earlier version of this article misstated the number of incoming residents in the program.
[email protected]
On Twitter @eaztweets
Remediation programs and program director attitudes can make the difference in attrition rates among general surgery residents, according to a survey-based study.
A study by the Association of American Medical Colleges, projects a shortage of 29,000 general surgeons by 2030. Some residency programs are taking steps lower program dropout rates, which has been reported as high as 26% in some programs, according to Alexander Schwed, MD, general surgeon at Harbor–University of California, Los Angeles Medical Center.
Dr. Schwed and his colleagues conducted a survey of 21 general surgery residency program directors. In those programs, the overall attrition rate was found to be much lower than expected – 8.8% over a 5-year period (JAMA Surg. 2017 Aug 16. doi: 10.1001/jamasurg.2017.2656).
The survey showed that programs that implemented resident remediation had lower attrition rates, (21.0% vs 6.8%; P less than .001).
“The association between increased use of remediation by residency programs and low rates of resident attrition is novel,” the investigators wrote. “Nevertheless, based on our findings, high-attrition programs could lower their attrition rates through the increased use of resident remediation and increased focus on resident education.”
Both high- and low-attrition programs selected to participate in the study showed relatively similar median numbers of residents, with low-attrition programs reporting a median of 28 participants per year, and high-attrition programs reporting with 35.
Other similarities between low- and high-attrition programs include percentage of female and minority residents, median of 33.3% and 39.8% respectively, and the number of cases performed by first-, second-, and third-year residents.
The other difference between the six low-attrition programs and the five high-attrition programs was the attitude of the program directors regarding their role in the training of residents, according to researchers.
Investigators asked directors a series of questions using a Likert scale with 1 representing “strongly disagree” and 4 representing “strongly agree.”
Program directors from high- and low-attrition programs tended to agree strongly (scoring 3.8 and 3.2, respectively) with the statement that one of their main roles as a program leader was to “redirect residents who should not be surgeons.”
When asked whether “some degree of resident attrition is a necessary phenomenon,” directors from low-attrition programs scored 2.2, while those from high-attrition programs indicated stronger agreement with an overall score of 3.2.
Directors from programs with high dropout rates were also more likely to consider a 6% dropout rate to be too low, compared with directors from low-attrition programs who thought it was too high.
“When we recruit residents, we are very careful to recruit those who seem to buy into our mission, our vision, and our ideals and fit in well with our culture,” said Sharmila Dissanaike, MD, FACS, department of surgery chair at Texas Tech University Health Sciences Center, Lubbock, in an interview. “We emphasize teamwork, collegiality, and an ‘all for one and one for all’ type of mentality.”
This kind of recruitment includes having current residents be a part of the process, Dr. Dissanaike explained, and encouraging current and potential residents to have an informal dinner to get to know one another better.
For the department of surgery at Texas Tech, the collaborative culture combined with a remediation program has resulted in a drop in attrition from 20% down to 7% in recent years, Dr. Dissanaike said. In addition, the current success of her program can be partly attributed to a recent decision to maintain the number of incoming residents at five, she said.*
Larger programs can achieve similar improvement, she noted and the rising demand for surgeons makes it essential to find a solution that incorporates the benefits of both types of programs.
“We need more surgeons, we need more Graduate Medical Education spots, we need more training spots for general surgeons,” said Dr. Dissanaike. “I think within those large programs we need to find ways to structure smaller groups, maybe little pods, to help support residents so they don’t get lost.”
Dr. Schwed and his colleagues expressed concern that institutional barriers, such as the focus on test scores, may impede directors from embracing remediation.
“Greater emphasis on the written and oral General Surgery Qualifying Examination pass rates, which are now publicly posted and used by residency review committees, will likely exert pressure on program directors, who may fear that attempting to remediate a resident with poor medical knowledge may affect their program’s 5-year board pass rates,” the investigators wrote. “Our study suggests that such fears may be unfounded because programs with high levels of remediation and low attrition had similar board pass rates as those with high attrition.”
Dr. Schwed and his coinvestigators acknowledged that the programs studied may not be representative of U.S. residencies and selection bias may have affected the findings.
Researchers reported no relevant financial disclosures.
*Correction, 10/26/17: An earlier version of this article misstated the number of incoming residents in the program.
[email protected]
On Twitter @eaztweets
Remediation programs and program director attitudes can make the difference in attrition rates among general surgery residents, according to a survey-based study.
A study by the Association of American Medical Colleges, projects a shortage of 29,000 general surgeons by 2030. Some residency programs are taking steps lower program dropout rates, which has been reported as high as 26% in some programs, according to Alexander Schwed, MD, general surgeon at Harbor–University of California, Los Angeles Medical Center.
Dr. Schwed and his colleagues conducted a survey of 21 general surgery residency program directors. In those programs, the overall attrition rate was found to be much lower than expected – 8.8% over a 5-year period (JAMA Surg. 2017 Aug 16. doi: 10.1001/jamasurg.2017.2656).
The survey showed that programs that implemented resident remediation had lower attrition rates, (21.0% vs 6.8%; P less than .001).
“The association between increased use of remediation by residency programs and low rates of resident attrition is novel,” the investigators wrote. “Nevertheless, based on our findings, high-attrition programs could lower their attrition rates through the increased use of resident remediation and increased focus on resident education.”
Both high- and low-attrition programs selected to participate in the study showed relatively similar median numbers of residents, with low-attrition programs reporting a median of 28 participants per year, and high-attrition programs reporting with 35.
Other similarities between low- and high-attrition programs include percentage of female and minority residents, median of 33.3% and 39.8% respectively, and the number of cases performed by first-, second-, and third-year residents.
The other difference between the six low-attrition programs and the five high-attrition programs was the attitude of the program directors regarding their role in the training of residents, according to researchers.
Investigators asked directors a series of questions using a Likert scale with 1 representing “strongly disagree” and 4 representing “strongly agree.”
Program directors from high- and low-attrition programs tended to agree strongly (scoring 3.8 and 3.2, respectively) with the statement that one of their main roles as a program leader was to “redirect residents who should not be surgeons.”
When asked whether “some degree of resident attrition is a necessary phenomenon,” directors from low-attrition programs scored 2.2, while those from high-attrition programs indicated stronger agreement with an overall score of 3.2.
Directors from programs with high dropout rates were also more likely to consider a 6% dropout rate to be too low, compared with directors from low-attrition programs who thought it was too high.
“When we recruit residents, we are very careful to recruit those who seem to buy into our mission, our vision, and our ideals and fit in well with our culture,” said Sharmila Dissanaike, MD, FACS, department of surgery chair at Texas Tech University Health Sciences Center, Lubbock, in an interview. “We emphasize teamwork, collegiality, and an ‘all for one and one for all’ type of mentality.”
This kind of recruitment includes having current residents be a part of the process, Dr. Dissanaike explained, and encouraging current and potential residents to have an informal dinner to get to know one another better.
For the department of surgery at Texas Tech, the collaborative culture combined with a remediation program has resulted in a drop in attrition from 20% down to 7% in recent years, Dr. Dissanaike said. In addition, the current success of her program can be partly attributed to a recent decision to maintain the number of incoming residents at five, she said.*
Larger programs can achieve similar improvement, she noted and the rising demand for surgeons makes it essential to find a solution that incorporates the benefits of both types of programs.
“We need more surgeons, we need more Graduate Medical Education spots, we need more training spots for general surgeons,” said Dr. Dissanaike. “I think within those large programs we need to find ways to structure smaller groups, maybe little pods, to help support residents so they don’t get lost.”
Dr. Schwed and his colleagues expressed concern that institutional barriers, such as the focus on test scores, may impede directors from embracing remediation.
“Greater emphasis on the written and oral General Surgery Qualifying Examination pass rates, which are now publicly posted and used by residency review committees, will likely exert pressure on program directors, who may fear that attempting to remediate a resident with poor medical knowledge may affect their program’s 5-year board pass rates,” the investigators wrote. “Our study suggests that such fears may be unfounded because programs with high levels of remediation and low attrition had similar board pass rates as those with high attrition.”
Dr. Schwed and his coinvestigators acknowledged that the programs studied may not be representative of U.S. residencies and selection bias may have affected the findings.
Researchers reported no relevant financial disclosures.
*Correction, 10/26/17: An earlier version of this article misstated the number of incoming residents in the program.
[email protected]
On Twitter @eaztweets
FROM JAMA SURGERY
Key clinical point:
Major finding: Of the 21 programs surveyed, there was an average attrition rate of 8.8% over 5 years.
Data source: Survey of 21 general surgery residency program directors between July 2010 and June 2015.
Disclosures: Investigators report no relevant financial disclosures.
Sodium fusidate noninferior to linezolid for acute skin infections
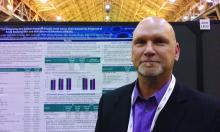
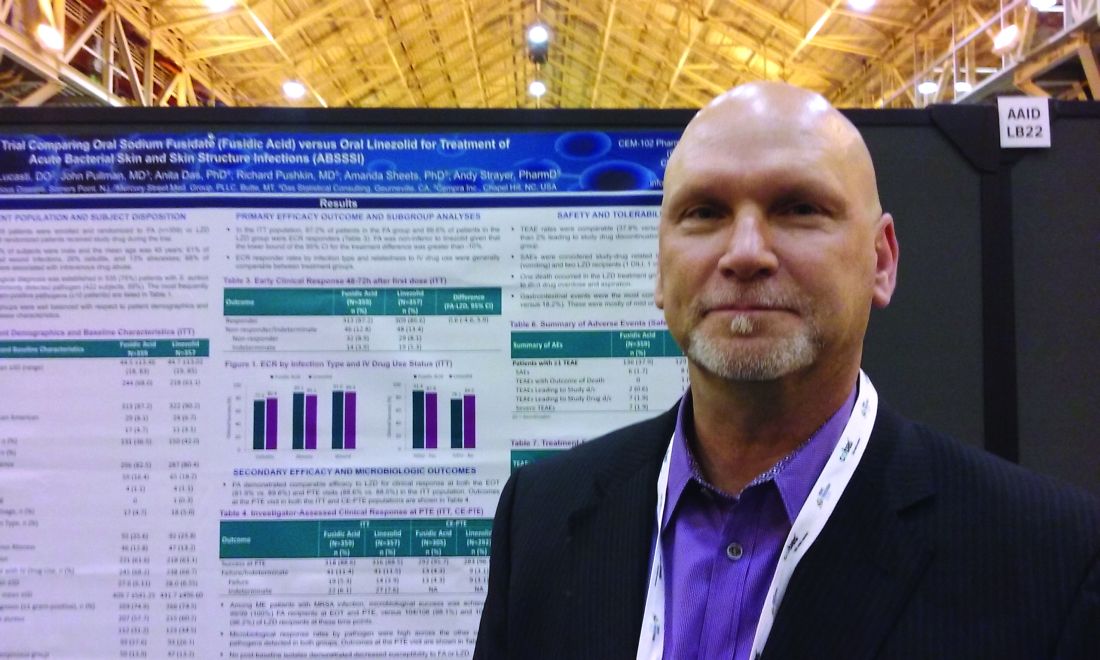
NEW ORLEANS – An oral antibiotic in development in the United States, fusidic acid (oral formulation, sodium fusidate) was noninferior to linezolid based on early clinical response in a randomized, double-blind, multicenter trial of 716 people with acute bacterial skin and skin structure infections (ABSSSI), including cellulitis, wound infection, and major cutaneous abscesses.
Early clinical response was defined as a 20% or greater reduction from baseline in the surface area of redness, edema, or induration at 48-72 hours after starting treatment with the study drugs. In an intent-to-treat analysis, 87.2% of patients randomized to fusidic acid and 86.6% of the linezolid group met this primary endpoint of the phase 3 study.
“Fusidic acid showed similar efficacy and comparable safety” that persisted through treatment, said Andy Strayer, PharmD, vice president of clinical programs at Cempra Pharmaceuticals, which is developing sodium fusidate as an oral agent to treat ABSSSI patients in the United States. Leo Pharmaceuticals has marketed sodium fusidate outside the United States in various formulations for decades.
Fusidic acid has potent activity against gram-positive aerobic organisms, including methicillin-resistant Staphylococcus aureus (MRSA). “Strikingly, fusidic acid showed 100% success in patients with MRSA in the microbiologically evaluable population at the end of treatment and posttherapy evaluation time points,” Dr. Strayer said at the annual meeting of the American Society for Microbiology. “Fusidic acid may offer an important oral therapy alternative for MRSA infection.”
“Fusidic acid, a drug long used in other parts of the world, has been demonstrated in this first phase 3 trial, to be a potential new option for the treatment of MRSA skin and skin structure infections in the U.S.,” said Carrie Cardenas, MD, lead study author and a principal investigator at eStudySite, San Diego, and an internist in private practice in La Mesa, California.
There was a microbiological diagnosis established in 75% of patients. S. aureus was the most commonly detected pathogen (422 patients; 59%), and the study included 235 patients diagnosed with MRSA infection.
About two-thirds, 65%, of participants were men. Mean age was 45 years. Infections were classified as wounds in 61%, cellulitis in 26%, and abscess in 13%. Notably, 68% of the recruited participants had ABSSSI associated with intravenous drug use, a “sometimes overlooked consequence of the ongoing epidemic of IV drug use in the U.S.,” Dr. Strayer said.
In terms of safety, treatment-emergent adverse event rates were comparable between the two groups (37.9% with fusidic acid versus 36.1% with linezolid). Gastrointestinal events were the most common adverse events, 22.8% versus 18.2%, respectively.
“Considering complicated skin infections are one of the most rapidly growing reasons for hospitalizations and emergency department visits each year, we anticipate that fusidic acid, if approved, may help clinicians decrease the length of inpatient stay or avoid hospitalization altogether,” Dr. Strayer said.
Cempra sponsored the study. Dr. Strayer is a Cempra employee and shareholder. Dr. Carrie Cardenas is a principal investigator at eStudySite, San Diego, and performs research for Cempra, Paratek, Debiopharm, Motif, Durata, MicuRx, Bristol-Myers Squibb, and Bayer.
NEW ORLEANS – An oral antibiotic in development in the United States, fusidic acid (oral formulation, sodium fusidate) was noninferior to linezolid based on early clinical response in a randomized, double-blind, multicenter trial of 716 people with acute bacterial skin and skin structure infections (ABSSSI), including cellulitis, wound infection, and major cutaneous abscesses.
Early clinical response was defined as a 20% or greater reduction from baseline in the surface area of redness, edema, or induration at 48-72 hours after starting treatment with the study drugs. In an intent-to-treat analysis, 87.2% of patients randomized to fusidic acid and 86.6% of the linezolid group met this primary endpoint of the phase 3 study.
“Fusidic acid showed similar efficacy and comparable safety” that persisted through treatment, said Andy Strayer, PharmD, vice president of clinical programs at Cempra Pharmaceuticals, which is developing sodium fusidate as an oral agent to treat ABSSSI patients in the United States. Leo Pharmaceuticals has marketed sodium fusidate outside the United States in various formulations for decades.
Fusidic acid has potent activity against gram-positive aerobic organisms, including methicillin-resistant Staphylococcus aureus (MRSA). “Strikingly, fusidic acid showed 100% success in patients with MRSA in the microbiologically evaluable population at the end of treatment and posttherapy evaluation time points,” Dr. Strayer said at the annual meeting of the American Society for Microbiology. “Fusidic acid may offer an important oral therapy alternative for MRSA infection.”
“Fusidic acid, a drug long used in other parts of the world, has been demonstrated in this first phase 3 trial, to be a potential new option for the treatment of MRSA skin and skin structure infections in the U.S.,” said Carrie Cardenas, MD, lead study author and a principal investigator at eStudySite, San Diego, and an internist in private practice in La Mesa, California.
There was a microbiological diagnosis established in 75% of patients. S. aureus was the most commonly detected pathogen (422 patients; 59%), and the study included 235 patients diagnosed with MRSA infection.
About two-thirds, 65%, of participants were men. Mean age was 45 years. Infections were classified as wounds in 61%, cellulitis in 26%, and abscess in 13%. Notably, 68% of the recruited participants had ABSSSI associated with intravenous drug use, a “sometimes overlooked consequence of the ongoing epidemic of IV drug use in the U.S.,” Dr. Strayer said.
In terms of safety, treatment-emergent adverse event rates were comparable between the two groups (37.9% with fusidic acid versus 36.1% with linezolid). Gastrointestinal events were the most common adverse events, 22.8% versus 18.2%, respectively.
“Considering complicated skin infections are one of the most rapidly growing reasons for hospitalizations and emergency department visits each year, we anticipate that fusidic acid, if approved, may help clinicians decrease the length of inpatient stay or avoid hospitalization altogether,” Dr. Strayer said.
Cempra sponsored the study. Dr. Strayer is a Cempra employee and shareholder. Dr. Carrie Cardenas is a principal investigator at eStudySite, San Diego, and performs research for Cempra, Paratek, Debiopharm, Motif, Durata, MicuRx, Bristol-Myers Squibb, and Bayer.
NEW ORLEANS – An oral antibiotic in development in the United States, fusidic acid (oral formulation, sodium fusidate) was noninferior to linezolid based on early clinical response in a randomized, double-blind, multicenter trial of 716 people with acute bacterial skin and skin structure infections (ABSSSI), including cellulitis, wound infection, and major cutaneous abscesses.
Early clinical response was defined as a 20% or greater reduction from baseline in the surface area of redness, edema, or induration at 48-72 hours after starting treatment with the study drugs. In an intent-to-treat analysis, 87.2% of patients randomized to fusidic acid and 86.6% of the linezolid group met this primary endpoint of the phase 3 study.
“Fusidic acid showed similar efficacy and comparable safety” that persisted through treatment, said Andy Strayer, PharmD, vice president of clinical programs at Cempra Pharmaceuticals, which is developing sodium fusidate as an oral agent to treat ABSSSI patients in the United States. Leo Pharmaceuticals has marketed sodium fusidate outside the United States in various formulations for decades.
Fusidic acid has potent activity against gram-positive aerobic organisms, including methicillin-resistant Staphylococcus aureus (MRSA). “Strikingly, fusidic acid showed 100% success in patients with MRSA in the microbiologically evaluable population at the end of treatment and posttherapy evaluation time points,” Dr. Strayer said at the annual meeting of the American Society for Microbiology. “Fusidic acid may offer an important oral therapy alternative for MRSA infection.”
“Fusidic acid, a drug long used in other parts of the world, has been demonstrated in this first phase 3 trial, to be a potential new option for the treatment of MRSA skin and skin structure infections in the U.S.,” said Carrie Cardenas, MD, lead study author and a principal investigator at eStudySite, San Diego, and an internist in private practice in La Mesa, California.
There was a microbiological diagnosis established in 75% of patients. S. aureus was the most commonly detected pathogen (422 patients; 59%), and the study included 235 patients diagnosed with MRSA infection.
About two-thirds, 65%, of participants were men. Mean age was 45 years. Infections were classified as wounds in 61%, cellulitis in 26%, and abscess in 13%. Notably, 68% of the recruited participants had ABSSSI associated with intravenous drug use, a “sometimes overlooked consequence of the ongoing epidemic of IV drug use in the U.S.,” Dr. Strayer said.
In terms of safety, treatment-emergent adverse event rates were comparable between the two groups (37.9% with fusidic acid versus 36.1% with linezolid). Gastrointestinal events were the most common adverse events, 22.8% versus 18.2%, respectively.
“Considering complicated skin infections are one of the most rapidly growing reasons for hospitalizations and emergency department visits each year, we anticipate that fusidic acid, if approved, may help clinicians decrease the length of inpatient stay or avoid hospitalization altogether,” Dr. Strayer said.
Cempra sponsored the study. Dr. Strayer is a Cempra employee and shareholder. Dr. Carrie Cardenas is a principal investigator at eStudySite, San Diego, and performs research for Cempra, Paratek, Debiopharm, Motif, Durata, MicuRx, Bristol-Myers Squibb, and Bayer.
AT ASM MICROBE 2017
Key clinical point: Sodium fusidate, active as fusidic acid, showed noninferiority to linezolid for early clinical response in ABSSI patients.
Major finding: 87.2% of patients given sodium fusidate and 86.6% of those receiving linezolid achieved an early clinical response.
Data source: Randomized, controlled, double-blind, phase 3 study with 716 participants.
Disclosures: Cempra sponsored the study. Dr. Carrier Cardenas is a researcher for Cempra, Paratek, Debiopharm, Motif, Durata, MicuRx, Bristol-Myers Squibb, and Bayer. Dr. Strayer is a Cempra employee and shareholder.
VIDEO: Study highlights risks of postponing cholecystectomy
Almost half of patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) did not undergo cholecystectomy (CCY) within the next 60 days according to the results of a large, retrospective cohort study reported in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2017.05.048).
“Although early and delayed CCY equally reduce the risk of subsequent recurrent biliary events, patients are at 10-fold higher risk of a recurrent biliary event while waiting for a delayed CCY, compared with patients who underwent early CCY,” wrote Robert J. Huang, MD, and his associates of Stanford (Calif.) University Medical Center. Delayed CCY is cost effective, but that benefit must be weighed against the risk of loss to follow-up, especially if patients have “little or no health insurance,” they said.
Source: American Gastroenterological Association
Gallstone disease affects up to 15% of adults in developed societies, including about 20-25 million Americans. Yearly costs of treatment tally at more than $6.2 billion and have risen by more than 20% in 3 decades, according to multiple studies. Approximately 20% of patients with gallstone disease have choledocholithiasis, mainly because gallstones can pass from the gallbladder into the common bile duct. After undergoing ERCP, such patients are typically referred for CCY, but there are no “societal guidelines” on timing the referral, the researchers said. Practice patterns remain “largely institution based and may be subject to the vagaries of surgeon availability and other institutional resource constraints.” One prior study linked a median 7-week wait time for CCY with a 20% rate of recurrent biliary events. To evaluate large-scale practice patterns, the researchers studied 4,516 patients who had undergone ERCP for choledocholithiasis in California (during 2009-2011), New York (during 2011-2013), and Florida (during 2012-2014) and calculated timing and rates of subsequent CCY, recurrent biliary events, and deaths. Patients were followed for up to 365 days after ERCP.
Of the 4,516 patients studied, 1,859 (41.2%) patients underwent CCY during their index hospital admission (early CCY). Of the 2,657 (58.8%) patients who were discharged without CCY, only 491 (18%) had a planned CCY within 60 days (delayed CCY), 350 (71.3%) of which were done in an outpatient setting. Of the patients in the study, 2,168 (48.0%) did not have a CCY (no CCY) during their index visit or within 60 days. Over 365 days of follow-up, 10% of patients who did not have a CCY had recurrent biliary events, compared with 1.3% of patients who underwent early or delayed CCY. The risk of recurrent biliary events for patients who underwent early or delayed CCY was about 88% lower than if they had had no CCY within 60 days of ERCP (P less than .001 for each comparison). Performing CCY during index admission cut the risk of recurrent biliary events occurring within 60 days by 92%, compared with delayed or no CCY (P less than .001).
In all, 15 (0.7%) patients who did not undergo CCY died after subsequent hospitalization for a recurrent biliary event, compared with 1 patient who underwent early CCY (0.1%; P less than .001). There were no deaths associated with recurrent biliary events in the delayed-CCY group. Rates of all-cause mortality over 365 days were 3.1% in the no-CCY group, 0.6% in the early-CCY group, and 0% in the delayed-CCY group. Thus, cumulative death rates were about seven times higher among patients who did not undergo CCY compared with those who did (P less than .001).
Patients who did not undergo CCY tended to be older than delayed- and early-CCY patients (mean ages 66 years, 58 years, and 52 years, respectively). No-CCY patients also tended to have more comorbidities. Nonetheless, having an early CCY retained a “robust” protective effect against recurrent biliary events after accounting for age, sex, comorbidities, stent placement, facility volume, and state of residence. Even after researchers adjusted for those factors, the protective effect of early CCY dropped by less than 5% (from 92% to about 87%), the investigators said.
They also noted that the overall cohort averaged 60 years of age and that 64% were female, which is consistent with the epidemiology of biliary stone disease. Just over half were non-Hispanic whites. Medicare was the single largest primary payer (46%), followed by private insurance (28%) and Medicaid (16%).
“A strategy of delayed CCY performed on an outpatient basis was least costly,” the researchers said. “Performance of early CCY was inversely associated with low facility volume. Hispanic race, Asian race, Medicaid insurance, and no insurance associated inversely with performance of delayed CCY.”
Funders included a seed grant from the Stanford division of gastroenterology and hepatology and the National Institutes of Health. The investigators had no conflicts of interest.
Almost half of patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) did not undergo cholecystectomy (CCY) within the next 60 days according to the results of a large, retrospective cohort study reported in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2017.05.048).
“Although early and delayed CCY equally reduce the risk of subsequent recurrent biliary events, patients are at 10-fold higher risk of a recurrent biliary event while waiting for a delayed CCY, compared with patients who underwent early CCY,” wrote Robert J. Huang, MD, and his associates of Stanford (Calif.) University Medical Center. Delayed CCY is cost effective, but that benefit must be weighed against the risk of loss to follow-up, especially if patients have “little or no health insurance,” they said.
Source: American Gastroenterological Association
Gallstone disease affects up to 15% of adults in developed societies, including about 20-25 million Americans. Yearly costs of treatment tally at more than $6.2 billion and have risen by more than 20% in 3 decades, according to multiple studies. Approximately 20% of patients with gallstone disease have choledocholithiasis, mainly because gallstones can pass from the gallbladder into the common bile duct. After undergoing ERCP, such patients are typically referred for CCY, but there are no “societal guidelines” on timing the referral, the researchers said. Practice patterns remain “largely institution based and may be subject to the vagaries of surgeon availability and other institutional resource constraints.” One prior study linked a median 7-week wait time for CCY with a 20% rate of recurrent biliary events. To evaluate large-scale practice patterns, the researchers studied 4,516 patients who had undergone ERCP for choledocholithiasis in California (during 2009-2011), New York (during 2011-2013), and Florida (during 2012-2014) and calculated timing and rates of subsequent CCY, recurrent biliary events, and deaths. Patients were followed for up to 365 days after ERCP.
Of the 4,516 patients studied, 1,859 (41.2%) patients underwent CCY during their index hospital admission (early CCY). Of the 2,657 (58.8%) patients who were discharged without CCY, only 491 (18%) had a planned CCY within 60 days (delayed CCY), 350 (71.3%) of which were done in an outpatient setting. Of the patients in the study, 2,168 (48.0%) did not have a CCY (no CCY) during their index visit or within 60 days. Over 365 days of follow-up, 10% of patients who did not have a CCY had recurrent biliary events, compared with 1.3% of patients who underwent early or delayed CCY. The risk of recurrent biliary events for patients who underwent early or delayed CCY was about 88% lower than if they had had no CCY within 60 days of ERCP (P less than .001 for each comparison). Performing CCY during index admission cut the risk of recurrent biliary events occurring within 60 days by 92%, compared with delayed or no CCY (P less than .001).
In all, 15 (0.7%) patients who did not undergo CCY died after subsequent hospitalization for a recurrent biliary event, compared with 1 patient who underwent early CCY (0.1%; P less than .001). There were no deaths associated with recurrent biliary events in the delayed-CCY group. Rates of all-cause mortality over 365 days were 3.1% in the no-CCY group, 0.6% in the early-CCY group, and 0% in the delayed-CCY group. Thus, cumulative death rates were about seven times higher among patients who did not undergo CCY compared with those who did (P less than .001).
Patients who did not undergo CCY tended to be older than delayed- and early-CCY patients (mean ages 66 years, 58 years, and 52 years, respectively). No-CCY patients also tended to have more comorbidities. Nonetheless, having an early CCY retained a “robust” protective effect against recurrent biliary events after accounting for age, sex, comorbidities, stent placement, facility volume, and state of residence. Even after researchers adjusted for those factors, the protective effect of early CCY dropped by less than 5% (from 92% to about 87%), the investigators said.
They also noted that the overall cohort averaged 60 years of age and that 64% were female, which is consistent with the epidemiology of biliary stone disease. Just over half were non-Hispanic whites. Medicare was the single largest primary payer (46%), followed by private insurance (28%) and Medicaid (16%).
“A strategy of delayed CCY performed on an outpatient basis was least costly,” the researchers said. “Performance of early CCY was inversely associated with low facility volume. Hispanic race, Asian race, Medicaid insurance, and no insurance associated inversely with performance of delayed CCY.”
Funders included a seed grant from the Stanford division of gastroenterology and hepatology and the National Institutes of Health. The investigators had no conflicts of interest.
Almost half of patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) did not undergo cholecystectomy (CCY) within the next 60 days according to the results of a large, retrospective cohort study reported in the September issue of Gastroenterology (doi: 10.1053/j.gastro.2017.05.048).
“Although early and delayed CCY equally reduce the risk of subsequent recurrent biliary events, patients are at 10-fold higher risk of a recurrent biliary event while waiting for a delayed CCY, compared with patients who underwent early CCY,” wrote Robert J. Huang, MD, and his associates of Stanford (Calif.) University Medical Center. Delayed CCY is cost effective, but that benefit must be weighed against the risk of loss to follow-up, especially if patients have “little or no health insurance,” they said.
Source: American Gastroenterological Association
Gallstone disease affects up to 15% of adults in developed societies, including about 20-25 million Americans. Yearly costs of treatment tally at more than $6.2 billion and have risen by more than 20% in 3 decades, according to multiple studies. Approximately 20% of patients with gallstone disease have choledocholithiasis, mainly because gallstones can pass from the gallbladder into the common bile duct. After undergoing ERCP, such patients are typically referred for CCY, but there are no “societal guidelines” on timing the referral, the researchers said. Practice patterns remain “largely institution based and may be subject to the vagaries of surgeon availability and other institutional resource constraints.” One prior study linked a median 7-week wait time for CCY with a 20% rate of recurrent biliary events. To evaluate large-scale practice patterns, the researchers studied 4,516 patients who had undergone ERCP for choledocholithiasis in California (during 2009-2011), New York (during 2011-2013), and Florida (during 2012-2014) and calculated timing and rates of subsequent CCY, recurrent biliary events, and deaths. Patients were followed for up to 365 days after ERCP.
Of the 4,516 patients studied, 1,859 (41.2%) patients underwent CCY during their index hospital admission (early CCY). Of the 2,657 (58.8%) patients who were discharged without CCY, only 491 (18%) had a planned CCY within 60 days (delayed CCY), 350 (71.3%) of which were done in an outpatient setting. Of the patients in the study, 2,168 (48.0%) did not have a CCY (no CCY) during their index visit or within 60 days. Over 365 days of follow-up, 10% of patients who did not have a CCY had recurrent biliary events, compared with 1.3% of patients who underwent early or delayed CCY. The risk of recurrent biliary events for patients who underwent early or delayed CCY was about 88% lower than if they had had no CCY within 60 days of ERCP (P less than .001 for each comparison). Performing CCY during index admission cut the risk of recurrent biliary events occurring within 60 days by 92%, compared with delayed or no CCY (P less than .001).
In all, 15 (0.7%) patients who did not undergo CCY died after subsequent hospitalization for a recurrent biliary event, compared with 1 patient who underwent early CCY (0.1%; P less than .001). There were no deaths associated with recurrent biliary events in the delayed-CCY group. Rates of all-cause mortality over 365 days were 3.1% in the no-CCY group, 0.6% in the early-CCY group, and 0% in the delayed-CCY group. Thus, cumulative death rates were about seven times higher among patients who did not undergo CCY compared with those who did (P less than .001).
Patients who did not undergo CCY tended to be older than delayed- and early-CCY patients (mean ages 66 years, 58 years, and 52 years, respectively). No-CCY patients also tended to have more comorbidities. Nonetheless, having an early CCY retained a “robust” protective effect against recurrent biliary events after accounting for age, sex, comorbidities, stent placement, facility volume, and state of residence. Even after researchers adjusted for those factors, the protective effect of early CCY dropped by less than 5% (from 92% to about 87%), the investigators said.
They also noted that the overall cohort averaged 60 years of age and that 64% were female, which is consistent with the epidemiology of biliary stone disease. Just over half were non-Hispanic whites. Medicare was the single largest primary payer (46%), followed by private insurance (28%) and Medicaid (16%).
“A strategy of delayed CCY performed on an outpatient basis was least costly,” the researchers said. “Performance of early CCY was inversely associated with low facility volume. Hispanic race, Asian race, Medicaid insurance, and no insurance associated inversely with performance of delayed CCY.”
Funders included a seed grant from the Stanford division of gastroenterology and hepatology and the National Institutes of Health. The investigators had no conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Almost half of patients who underwent endoscopic retrograde cholangiopancreatography (ERCP) did not undergo cholecystectomy within 60 days.
Major finding: A total of 48% had no cholecystectomy within 60 days. Performing cholecystectomy during index admission cut the risk of recurrent biliary events within 60 days by 92%, compared with delayed or no cholecystectomy (P less than .001).
Data source: A multistate, retrospective study of 4,516 patients hospitalized with choledocholithiasis.
Disclosures: Funders included a Stanford division of gastroenterology and hepatology divisional seed grant and the National Institutes of Health. The investigators had no conflicts of interest.
Adding cefepime to vancomycin improved MRSA bacteremia outcomes
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: Median duration of MRSA bacteremia was 4 days with combination therapy, versus 6 days with vancomycin alone.
Data source: A retrospective, single-center comparison of 109 patients treated with either vancomycin plus cefepime or vancomycin alone.
Disclosures: Safana M. Atwan had no relevant financial disclosures.
Surgeon, primary care collaboration needed to catch hyperparathyroidism
A report from the University of Alabama at Birmingham provides further evidence that hyperparathyroidism is often missed in the United States health care system.
Investigators reviewed the electronic health records for 682,704 patients at the university from 2011 to 2015 and identified hypercalcemia (serum calcium greater than 10.5 mg/dL) – usually the first indication of disease – in 10,432 patients. The next step should have been a parathyroid hormone (PTH) measurement, but PTH was measured in only 3,200 patients (31%), and it usually took multiple abnormal calcium levels before PTH was checked, reported Courtney Balentine, MD, and her colleagues at the University of Alabama at Birmingham.
In addition, 592 of 2,666 patients (22%) with both elevated calcium and PTH levels were referred to surgeons for a parathyroidectomy consult, although parathyroidectomy is a low-risk outpatient procedure that cures up to 95% of patients, and surgeons are best suited to discuss the risks and benefits of the procedure with patients, investigators said (Ann Surg. 2017 Jul 3. doi: 10.1097/SLA.0000000000002370).
Underdiagnosis and treatment of hyperparathyroidism can lead to fractures, kidney stones, depression, cognitive impairment, hypertension, stroke, and myocardial infarction.
The investigators plan to meet with primary care doctors to hear how they think the problem should be addressed. Alerts and automatic referrals are also being considered for the EHR. “The combination of systems changes and stakeholder engagement is more likely to succeed than focusing on one component to the exclusion of others,” Dr. Balentine and colleagues said.
The issue could be that primary care physicians are just too overwhelmed to notice or be concerned about an isolated abnormal calcium level in an otherwise routine assessment. Or perhaps they assume surgeons come into play only if there are kidney stones, bone changes, or other obvious signs of trouble, they said.
The team has started to look at charts to get a better understanding of what’s going wrong. “I have been a little bit flabbergasted by how many excuses there are for either not checking a PTH or not referring once the diagnosis is there. … ‘This patient probably would not benefit from the surgery; the risk is too high; he or she does not want X, Y, or Z.’ I think if they just refer [patients to surgeons] to have the conversation, we might very well agree with them, but at least we [could] have the conversation with the patient, and I think [that] would make more sense,” Dr. Balentine said in a transcript of a question and answer session that was published with the report.
“Indeed, the recent American Association of Endocrine Surgery guidelines emphasize the importance of referring patients to surgical experts for discussion of treatment options,” the investigators said in the report.
It’s possible that elevated calcium and PTH levels were evaluated and treated at other institutions and so were not captured by the analysis. “Our mean follow-up was 16 months, however, which suggests that most patients were seen in the UAB system long enough to undergo appropriate evaluation and referral.” Also, patients with “two or more abnormal calcium values had similarly low rates of surgical referral, which suggests that loss to follow-up is unlikely to explain our findings,” they said.
The mean age of the cohort was 54 years; 56% of the patients were white, and 61% were women.
The work was supported by the Agency for Healthcare Research and Quality. The authors reported no conflicts of interest.
A report from the University of Alabama at Birmingham provides further evidence that hyperparathyroidism is often missed in the United States health care system.
Investigators reviewed the electronic health records for 682,704 patients at the university from 2011 to 2015 and identified hypercalcemia (serum calcium greater than 10.5 mg/dL) – usually the first indication of disease – in 10,432 patients. The next step should have been a parathyroid hormone (PTH) measurement, but PTH was measured in only 3,200 patients (31%), and it usually took multiple abnormal calcium levels before PTH was checked, reported Courtney Balentine, MD, and her colleagues at the University of Alabama at Birmingham.
In addition, 592 of 2,666 patients (22%) with both elevated calcium and PTH levels were referred to surgeons for a parathyroidectomy consult, although parathyroidectomy is a low-risk outpatient procedure that cures up to 95% of patients, and surgeons are best suited to discuss the risks and benefits of the procedure with patients, investigators said (Ann Surg. 2017 Jul 3. doi: 10.1097/SLA.0000000000002370).
Underdiagnosis and treatment of hyperparathyroidism can lead to fractures, kidney stones, depression, cognitive impairment, hypertension, stroke, and myocardial infarction.
The investigators plan to meet with primary care doctors to hear how they think the problem should be addressed. Alerts and automatic referrals are also being considered for the EHR. “The combination of systems changes and stakeholder engagement is more likely to succeed than focusing on one component to the exclusion of others,” Dr. Balentine and colleagues said.
The issue could be that primary care physicians are just too overwhelmed to notice or be concerned about an isolated abnormal calcium level in an otherwise routine assessment. Or perhaps they assume surgeons come into play only if there are kidney stones, bone changes, or other obvious signs of trouble, they said.
The team has started to look at charts to get a better understanding of what’s going wrong. “I have been a little bit flabbergasted by how many excuses there are for either not checking a PTH or not referring once the diagnosis is there. … ‘This patient probably would not benefit from the surgery; the risk is too high; he or she does not want X, Y, or Z.’ I think if they just refer [patients to surgeons] to have the conversation, we might very well agree with them, but at least we [could] have the conversation with the patient, and I think [that] would make more sense,” Dr. Balentine said in a transcript of a question and answer session that was published with the report.
“Indeed, the recent American Association of Endocrine Surgery guidelines emphasize the importance of referring patients to surgical experts for discussion of treatment options,” the investigators said in the report.
It’s possible that elevated calcium and PTH levels were evaluated and treated at other institutions and so were not captured by the analysis. “Our mean follow-up was 16 months, however, which suggests that most patients were seen in the UAB system long enough to undergo appropriate evaluation and referral.” Also, patients with “two or more abnormal calcium values had similarly low rates of surgical referral, which suggests that loss to follow-up is unlikely to explain our findings,” they said.
The mean age of the cohort was 54 years; 56% of the patients were white, and 61% were women.
The work was supported by the Agency for Healthcare Research and Quality. The authors reported no conflicts of interest.
A report from the University of Alabama at Birmingham provides further evidence that hyperparathyroidism is often missed in the United States health care system.
Investigators reviewed the electronic health records for 682,704 patients at the university from 2011 to 2015 and identified hypercalcemia (serum calcium greater than 10.5 mg/dL) – usually the first indication of disease – in 10,432 patients. The next step should have been a parathyroid hormone (PTH) measurement, but PTH was measured in only 3,200 patients (31%), and it usually took multiple abnormal calcium levels before PTH was checked, reported Courtney Balentine, MD, and her colleagues at the University of Alabama at Birmingham.
In addition, 592 of 2,666 patients (22%) with both elevated calcium and PTH levels were referred to surgeons for a parathyroidectomy consult, although parathyroidectomy is a low-risk outpatient procedure that cures up to 95% of patients, and surgeons are best suited to discuss the risks and benefits of the procedure with patients, investigators said (Ann Surg. 2017 Jul 3. doi: 10.1097/SLA.0000000000002370).
Underdiagnosis and treatment of hyperparathyroidism can lead to fractures, kidney stones, depression, cognitive impairment, hypertension, stroke, and myocardial infarction.
The investigators plan to meet with primary care doctors to hear how they think the problem should be addressed. Alerts and automatic referrals are also being considered for the EHR. “The combination of systems changes and stakeholder engagement is more likely to succeed than focusing on one component to the exclusion of others,” Dr. Balentine and colleagues said.
The issue could be that primary care physicians are just too overwhelmed to notice or be concerned about an isolated abnormal calcium level in an otherwise routine assessment. Or perhaps they assume surgeons come into play only if there are kidney stones, bone changes, or other obvious signs of trouble, they said.
The team has started to look at charts to get a better understanding of what’s going wrong. “I have been a little bit flabbergasted by how many excuses there are for either not checking a PTH or not referring once the diagnosis is there. … ‘This patient probably would not benefit from the surgery; the risk is too high; he or she does not want X, Y, or Z.’ I think if they just refer [patients to surgeons] to have the conversation, we might very well agree with them, but at least we [could] have the conversation with the patient, and I think [that] would make more sense,” Dr. Balentine said in a transcript of a question and answer session that was published with the report.
“Indeed, the recent American Association of Endocrine Surgery guidelines emphasize the importance of referring patients to surgical experts for discussion of treatment options,” the investigators said in the report.
It’s possible that elevated calcium and PTH levels were evaluated and treated at other institutions and so were not captured by the analysis. “Our mean follow-up was 16 months, however, which suggests that most patients were seen in the UAB system long enough to undergo appropriate evaluation and referral.” Also, patients with “two or more abnormal calcium values had similarly low rates of surgical referral, which suggests that loss to follow-up is unlikely to explain our findings,” they said.
The mean age of the cohort was 54 years; 56% of the patients were white, and 61% were women.
The work was supported by the Agency for Healthcare Research and Quality. The authors reported no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point:
Major finding: Just 31% of patients with a finding of hypercalcemia went on to have their parathyroid hormone levels checked.
Data source: Electronic health record review of 682,704 patients at a large American university.
Disclosures: The work was supported by the Agency for Healthcare Research and Quality. The authors reported no conflicts of interest.
Point/Counterpoint: Is intraoperative drain placement essential during pancreatectomy?
Yes, placing drains is essential.
It’s important to look at the evidence in the literature, starting with a randomized controlled trial of 179 patients from 2001 that showed no reduction in death or complication rate associated with use of surgical intraperitoneal closed suction drainage (Ann. Surg. 2001;234:487-94). Interestingly, even though this study showed there was no benefit to using drains, they address the use of closed suction drainage. The investigators were not claiming all drains are unnecessary.
Why drain placement? The argument for drains includes evacuation of blood, pancreatic juice, bile, and chyle. In addition, assessing drainage can act as a warning sign for anastomotic leak or hemorrhage, so patients can potentially avoid additional interventions.
A study from University of Tokyo researchers found three drains were more effective than one. In addition, the investigators argued against early removal, pointing out that the risk for infection associated with drains only increased after day 10. The researchers were not only in favor of drains but in favor of multiple drains (World J Surg. 2016;40:1226-35).
A multicenter, randomized prospective trial conducted in the United States compared 68 patients with drains to 69 others without during pancreaticoduodenectomy. They reported an increase in the frequency and severity of complications when drains were omitted, including the number of grade 2 or greater complications. Furthermore, the safety monitoring board stopped the study early because mortality among patients in the drain group was 3%, compared with 12% in the no-drain group. (Ann. Surg. 2014:259:605-12).
Another set of researchers in Germany conducted a prospective, randomized study that favored omission of drains. However, a closer look at demographics shows that about one-fourth of participants had chronic pancreatitis, which is associated with a low risk of fistula (Ann Surg. 2016;263:440-9). In addition, they found no significant difference in fistula rates between patients who underwent pancreaticojejunostomy or pancreaticoduodenectomy. Interestingly, the authors noted that surgeons were reluctant to omit drains in many situations, even in a clinical trial context.
Furthermore, a systematic review of nine studies with nearly 3,000 patients suggests it is still necessary to place abdominal drains during pancreatic resection, researchers at the Medical College of Xi’an Jiaotong University in China reported (World J Gastroenterol. 2015;21:5719-34). The authors cited a significant increase in morbidity among patients in whom drains were omitted (odds ratio, 2.39).
Perhaps the cleverest way to address this controversy with drains during pancreatic resection comes from researchers at the University of Pennsylvania. They looked at surgical risk factors to gain a more nuanced view. They used the Fistula Risk Score (FRS) to stratify patients and re-examined the outcomes of the multicenter U.S. study I cited earlier that was stopped early because of differences in mortality rates. The University of Pennsylvania research found that FRS correlated well with outcomes, suggesting its use as a mitigation strategy in patients at moderate to high risk for developing clinically relevant postoperative pancreatic fistula (J Gastrointest Surg. 2015;19:21-30). In other words, they suggest routine prophylactic drainage for patients at moderate to high risk but also suggest that there may be no need for prophylactic drainage for negligible to low risk patients.
I would like to conclude that drains appear essential in many cases, including for moderate to higher risk patients. We need to tailor our practices as surgeons regarding placement of drains during pancreatectomy or pancreaticoduodenectomy. Our goal remains to create opportunities for prolonged survival and better quality of life for our patients.
Dr. Dervenis is head of the Department of Surgical Oncology at the Metropolitan Hospital in Athens, Greece. He is also chair of the hepato-pancreato-biliary surgical unit. He reported no disclosures.
No, drain placement is not always necessary.
Drain placement is not essential during all pancreatectomies. The practice is so historically entrenched in our specialty that I need you to check your dogma at the door and take a look at the data with an open mind.
There are many, many retrospective studies that examine drainage versus no drainage. All of these studies have shown the same thing: There is no difference in many outcomes, including mortality. There may be a difference in terms of complicated, postoperative fistulae, which are difficult to manage in patients who have drains.
Another prospective randomized trial from Germany compared the reintervention rate, an endpoint I like, among 439 patients (Ann Surg. 2016;264:528-37). There was no statistically significant difference between the drain or no drain groups, further suggesting that drains are not essential in all cases.
We also need to take a closer look at the study Dr. Dervenis cited (Ann Surg. 2014:259:605-12). It’s true this trial was stopped early because of a higher mortality rate of 12% in the no drain group, but the difference was not statistically significant (P = .097). There was no difference in the fistula rate.
When you look at these data, there are a couple of conclusions you can reach. One conclusion is that a trial of 130 people designed for 750 found something uniquely different that had never been reported in any retrospective series, including one by the study’s senior author that demonstrated drains are essential (HPB [Oxford]. 2011;13:503-10). Another conclusion is that drains are not needed, and there is a very good chance this is a false positive finding. Look at the reasons the 10 participants died. I’m not sure a drain would have helped some of the patients without them, and some of the patients who had drains still died.
A study looking at practice at my institution, MSKCC, shows that drains are still used about half the time, indicating they are not essential. (Ann. Surg. 2013 Dec;258[6]:1051-8). Drains were more commonly used for pancreaticoduodenectomy and when the surgeon thought there might be a problem, such as a soft gland, difficult time in the OR, or a small pancreatic duct.
If you look at these data, this pans out in every retrospective study I’ve seen comparing drain versus no drain – the patients with drains tend to have higher morbidity. Among the 1,122 resection patients in the MSKCC study, those without operative drains had significantly lower rates of grade 3 complications and overall morbidity and fewer readmissions and lower rates of grade 3 or higher pancreatic fistula. Mortality and reintervention rates were no different.
I also looked at our most recent data, between 2010 and 2015. Now we are using intraoperative drains even less often. They are not considered essential at this point.
There are multiple retrospective and well-designed prospective, randomized trials that show no benefit to routine drainage following pancreatectomy. Acceptance of randomized clinical data is slow, particularly when it flies in the face of what you were taught by your mentors over the past 40 or 50 years. I encourage you to look at these data carefully and utilize them in your practice.
Dr. Allen is associate director for clinical programs at David M. Rubenstein Center for Pancreatic Cancer Research and the Murray F. Brennan chair in surgery at Memorial Sloan-Kettering Cancer Center in New York City. He reported no disclosures.
Yes, placing drains is essential.
It’s important to look at the evidence in the literature, starting with a randomized controlled trial of 179 patients from 2001 that showed no reduction in death or complication rate associated with use of surgical intraperitoneal closed suction drainage (Ann. Surg. 2001;234:487-94). Interestingly, even though this study showed there was no benefit to using drains, they address the use of closed suction drainage. The investigators were not claiming all drains are unnecessary.
Why drain placement? The argument for drains includes evacuation of blood, pancreatic juice, bile, and chyle. In addition, assessing drainage can act as a warning sign for anastomotic leak or hemorrhage, so patients can potentially avoid additional interventions.
A study from University of Tokyo researchers found three drains were more effective than one. In addition, the investigators argued against early removal, pointing out that the risk for infection associated with drains only increased after day 10. The researchers were not only in favor of drains but in favor of multiple drains (World J Surg. 2016;40:1226-35).
A multicenter, randomized prospective trial conducted in the United States compared 68 patients with drains to 69 others without during pancreaticoduodenectomy. They reported an increase in the frequency and severity of complications when drains were omitted, including the number of grade 2 or greater complications. Furthermore, the safety monitoring board stopped the study early because mortality among patients in the drain group was 3%, compared with 12% in the no-drain group. (Ann. Surg. 2014:259:605-12).
Another set of researchers in Germany conducted a prospective, randomized study that favored omission of drains. However, a closer look at demographics shows that about one-fourth of participants had chronic pancreatitis, which is associated with a low risk of fistula (Ann Surg. 2016;263:440-9). In addition, they found no significant difference in fistula rates between patients who underwent pancreaticojejunostomy or pancreaticoduodenectomy. Interestingly, the authors noted that surgeons were reluctant to omit drains in many situations, even in a clinical trial context.
Furthermore, a systematic review of nine studies with nearly 3,000 patients suggests it is still necessary to place abdominal drains during pancreatic resection, researchers at the Medical College of Xi’an Jiaotong University in China reported (World J Gastroenterol. 2015;21:5719-34). The authors cited a significant increase in morbidity among patients in whom drains were omitted (odds ratio, 2.39).
Perhaps the cleverest way to address this controversy with drains during pancreatic resection comes from researchers at the University of Pennsylvania. They looked at surgical risk factors to gain a more nuanced view. They used the Fistula Risk Score (FRS) to stratify patients and re-examined the outcomes of the multicenter U.S. study I cited earlier that was stopped early because of differences in mortality rates. The University of Pennsylvania research found that FRS correlated well with outcomes, suggesting its use as a mitigation strategy in patients at moderate to high risk for developing clinically relevant postoperative pancreatic fistula (J Gastrointest Surg. 2015;19:21-30). In other words, they suggest routine prophylactic drainage for patients at moderate to high risk but also suggest that there may be no need for prophylactic drainage for negligible to low risk patients.
I would like to conclude that drains appear essential in many cases, including for moderate to higher risk patients. We need to tailor our practices as surgeons regarding placement of drains during pancreatectomy or pancreaticoduodenectomy. Our goal remains to create opportunities for prolonged survival and better quality of life for our patients.
Dr. Dervenis is head of the Department of Surgical Oncology at the Metropolitan Hospital in Athens, Greece. He is also chair of the hepato-pancreato-biliary surgical unit. He reported no disclosures.
No, drain placement is not always necessary.
Drain placement is not essential during all pancreatectomies. The practice is so historically entrenched in our specialty that I need you to check your dogma at the door and take a look at the data with an open mind.
There are many, many retrospective studies that examine drainage versus no drainage. All of these studies have shown the same thing: There is no difference in many outcomes, including mortality. There may be a difference in terms of complicated, postoperative fistulae, which are difficult to manage in patients who have drains.
Another prospective randomized trial from Germany compared the reintervention rate, an endpoint I like, among 439 patients (Ann Surg. 2016;264:528-37). There was no statistically significant difference between the drain or no drain groups, further suggesting that drains are not essential in all cases.
We also need to take a closer look at the study Dr. Dervenis cited (Ann Surg. 2014:259:605-12). It’s true this trial was stopped early because of a higher mortality rate of 12% in the no drain group, but the difference was not statistically significant (P = .097). There was no difference in the fistula rate.
When you look at these data, there are a couple of conclusions you can reach. One conclusion is that a trial of 130 people designed for 750 found something uniquely different that had never been reported in any retrospective series, including one by the study’s senior author that demonstrated drains are essential (HPB [Oxford]. 2011;13:503-10). Another conclusion is that drains are not needed, and there is a very good chance this is a false positive finding. Look at the reasons the 10 participants died. I’m not sure a drain would have helped some of the patients without them, and some of the patients who had drains still died.
A study looking at practice at my institution, MSKCC, shows that drains are still used about half the time, indicating they are not essential. (Ann. Surg. 2013 Dec;258[6]:1051-8). Drains were more commonly used for pancreaticoduodenectomy and when the surgeon thought there might be a problem, such as a soft gland, difficult time in the OR, or a small pancreatic duct.
If you look at these data, this pans out in every retrospective study I’ve seen comparing drain versus no drain – the patients with drains tend to have higher morbidity. Among the 1,122 resection patients in the MSKCC study, those without operative drains had significantly lower rates of grade 3 complications and overall morbidity and fewer readmissions and lower rates of grade 3 or higher pancreatic fistula. Mortality and reintervention rates were no different.
I also looked at our most recent data, between 2010 and 2015. Now we are using intraoperative drains even less often. They are not considered essential at this point.
There are multiple retrospective and well-designed prospective, randomized trials that show no benefit to routine drainage following pancreatectomy. Acceptance of randomized clinical data is slow, particularly when it flies in the face of what you were taught by your mentors over the past 40 or 50 years. I encourage you to look at these data carefully and utilize them in your practice.
Dr. Allen is associate director for clinical programs at David M. Rubenstein Center for Pancreatic Cancer Research and the Murray F. Brennan chair in surgery at Memorial Sloan-Kettering Cancer Center in New York City. He reported no disclosures.
Yes, placing drains is essential.
It’s important to look at the evidence in the literature, starting with a randomized controlled trial of 179 patients from 2001 that showed no reduction in death or complication rate associated with use of surgical intraperitoneal closed suction drainage (Ann. Surg. 2001;234:487-94). Interestingly, even though this study showed there was no benefit to using drains, they address the use of closed suction drainage. The investigators were not claiming all drains are unnecessary.
Why drain placement? The argument for drains includes evacuation of blood, pancreatic juice, bile, and chyle. In addition, assessing drainage can act as a warning sign for anastomotic leak or hemorrhage, so patients can potentially avoid additional interventions.
A study from University of Tokyo researchers found three drains were more effective than one. In addition, the investigators argued against early removal, pointing out that the risk for infection associated with drains only increased after day 10. The researchers were not only in favor of drains but in favor of multiple drains (World J Surg. 2016;40:1226-35).
A multicenter, randomized prospective trial conducted in the United States compared 68 patients with drains to 69 others without during pancreaticoduodenectomy. They reported an increase in the frequency and severity of complications when drains were omitted, including the number of grade 2 or greater complications. Furthermore, the safety monitoring board stopped the study early because mortality among patients in the drain group was 3%, compared with 12% in the no-drain group. (Ann. Surg. 2014:259:605-12).
Another set of researchers in Germany conducted a prospective, randomized study that favored omission of drains. However, a closer look at demographics shows that about one-fourth of participants had chronic pancreatitis, which is associated with a low risk of fistula (Ann Surg. 2016;263:440-9). In addition, they found no significant difference in fistula rates between patients who underwent pancreaticojejunostomy or pancreaticoduodenectomy. Interestingly, the authors noted that surgeons were reluctant to omit drains in many situations, even in a clinical trial context.
Furthermore, a systematic review of nine studies with nearly 3,000 patients suggests it is still necessary to place abdominal drains during pancreatic resection, researchers at the Medical College of Xi’an Jiaotong University in China reported (World J Gastroenterol. 2015;21:5719-34). The authors cited a significant increase in morbidity among patients in whom drains were omitted (odds ratio, 2.39).
Perhaps the cleverest way to address this controversy with drains during pancreatic resection comes from researchers at the University of Pennsylvania. They looked at surgical risk factors to gain a more nuanced view. They used the Fistula Risk Score (FRS) to stratify patients and re-examined the outcomes of the multicenter U.S. study I cited earlier that was stopped early because of differences in mortality rates. The University of Pennsylvania research found that FRS correlated well with outcomes, suggesting its use as a mitigation strategy in patients at moderate to high risk for developing clinically relevant postoperative pancreatic fistula (J Gastrointest Surg. 2015;19:21-30). In other words, they suggest routine prophylactic drainage for patients at moderate to high risk but also suggest that there may be no need for prophylactic drainage for negligible to low risk patients.
I would like to conclude that drains appear essential in many cases, including for moderate to higher risk patients. We need to tailor our practices as surgeons regarding placement of drains during pancreatectomy or pancreaticoduodenectomy. Our goal remains to create opportunities for prolonged survival and better quality of life for our patients.
Dr. Dervenis is head of the Department of Surgical Oncology at the Metropolitan Hospital in Athens, Greece. He is also chair of the hepato-pancreato-biliary surgical unit. He reported no disclosures.
No, drain placement is not always necessary.
Drain placement is not essential during all pancreatectomies. The practice is so historically entrenched in our specialty that I need you to check your dogma at the door and take a look at the data with an open mind.
There are many, many retrospective studies that examine drainage versus no drainage. All of these studies have shown the same thing: There is no difference in many outcomes, including mortality. There may be a difference in terms of complicated, postoperative fistulae, which are difficult to manage in patients who have drains.
Another prospective randomized trial from Germany compared the reintervention rate, an endpoint I like, among 439 patients (Ann Surg. 2016;264:528-37). There was no statistically significant difference between the drain or no drain groups, further suggesting that drains are not essential in all cases.
We also need to take a closer look at the study Dr. Dervenis cited (Ann Surg. 2014:259:605-12). It’s true this trial was stopped early because of a higher mortality rate of 12% in the no drain group, but the difference was not statistically significant (P = .097). There was no difference in the fistula rate.
When you look at these data, there are a couple of conclusions you can reach. One conclusion is that a trial of 130 people designed for 750 found something uniquely different that had never been reported in any retrospective series, including one by the study’s senior author that demonstrated drains are essential (HPB [Oxford]. 2011;13:503-10). Another conclusion is that drains are not needed, and there is a very good chance this is a false positive finding. Look at the reasons the 10 participants died. I’m not sure a drain would have helped some of the patients without them, and some of the patients who had drains still died.
A study looking at practice at my institution, MSKCC, shows that drains are still used about half the time, indicating they are not essential. (Ann. Surg. 2013 Dec;258[6]:1051-8). Drains were more commonly used for pancreaticoduodenectomy and when the surgeon thought there might be a problem, such as a soft gland, difficult time in the OR, or a small pancreatic duct.
If you look at these data, this pans out in every retrospective study I’ve seen comparing drain versus no drain – the patients with drains tend to have higher morbidity. Among the 1,122 resection patients in the MSKCC study, those without operative drains had significantly lower rates of grade 3 complications and overall morbidity and fewer readmissions and lower rates of grade 3 or higher pancreatic fistula. Mortality and reintervention rates were no different.
I also looked at our most recent data, between 2010 and 2015. Now we are using intraoperative drains even less often. They are not considered essential at this point.
There are multiple retrospective and well-designed prospective, randomized trials that show no benefit to routine drainage following pancreatectomy. Acceptance of randomized clinical data is slow, particularly when it flies in the face of what you were taught by your mentors over the past 40 or 50 years. I encourage you to look at these data carefully and utilize them in your practice.
Dr. Allen is associate director for clinical programs at David M. Rubenstein Center for Pancreatic Cancer Research and the Murray F. Brennan chair in surgery at Memorial Sloan-Kettering Cancer Center in New York City. He reported no disclosures.
Idarucizumab reversed dabigatran completely and rapidly in study
One IV 5-g dose of idarucizumab completely, rapidly, and safely reversed the anticoagulant effect of dabigatran, according to final results for 503 patients in the multicenter, prospective, open-label, uncontrolled RE-VERSE AD study.
Uncontrolled bleeding stopped a median of 2.5 hours after 134 patients received idarucizumab. In a separate group of 202 patients, 197 were able to undergo urgent procedures after a median of 1.6 hours, Charles V. Pollack Jr., MD, and his associates reported at the International Society on Thrombosis and Haemostasis congress. The report was simultaneously published in the New England Journal of Medicine.
Idarucizumab was specifically developed to reverse the anticoagulant effect of dabigatran. Many countries have already licensed the humanized monoclonal antibody fragment based on interim results for the first 90 patients enrolled in the Reversal Effects of Idarucizumab on Active Dabigatran (RE-VERSE AD) study (NCT02104947), noted Dr. Pollack, of Thomas Jefferson University, Philadelphia.
The final RE-VERSE AD cohort included 301 patients with uncontrolled gastrointestinal, intracranial, or trauma-related bleeding and 202 patients who needed urgent procedures. Participants from both groups typically were white, in their late 70s (age range, 21-96 years), and receiving 110 mg (75-150 mg) dabigatran twice daily. The primary endpoint was maximum percentage reversal within 4 hours after patients received idarucizumab, based on diluted thrombin time and ecarin clotting time.
The median maximum percentage reversal of dabigatran was 100% (95% confidence interval, 100% to 100%) in more than 98% of patients, and the effect usually lasted 24 hours. Among patients who underwent procedures, intraprocedural hemostasis was considered normal in 93% of cases, mildly abnormal in 5% of cases, and moderately abnormal in 2% of cases, the researchers noted. Seven patients received another dose of idarucizumab after developing recurrent or postoperative bleeding.
A total of 24 patients had an adjudicated thrombotic event within 30 days after receiving idarucizumab. These events included pulmonary embolism, systemic embolism, ischemic stroke, deep vein thrombosis, and myocardial infarction. The fact that many patients did not restart anticoagulation could have contributed to these thrombotic events, the researchers asserted. They noted that idarucizumab had no procoagulant activity in studies of animals and healthy human volunteers.
About 19% of patients in both groups died within 90 days. “Patients enrolled in this study were elderly, had numerous coexisting conditions, and presented with serious index events, such as intracranial hemorrhage, multiple trauma, sepsis, acute abdomen, or open fracture,” the investigators wrote. “Most of the deaths that occurred within 5 days after enrollment appeared to be related to the severity of the index event or to coexisting conditions, such as respiratory failure or multiple organ failure, whereas deaths that occurred after 30 days were more likely to be independent events or related to coexisting conditions.”
Boehringer Ingelheim Pharmaceuticals provided funding. Dr. Pollack disclosed grant support from Boehringer Ingelheim during the course of the study and ties to Daiichi Sankyo, Portola, CSL Behring, Bristol-Myers Squibb/Pfizer, Janssen Pharma, and AstraZeneca. Eighteen coinvestigators also disclosed ties to Boehringer Ingelheim and a number of other pharmaceutical companies. Two coinvestigators had no relevant financial disclosures.
One IV 5-g dose of idarucizumab completely, rapidly, and safely reversed the anticoagulant effect of dabigatran, according to final results for 503 patients in the multicenter, prospective, open-label, uncontrolled RE-VERSE AD study.
Uncontrolled bleeding stopped a median of 2.5 hours after 134 patients received idarucizumab. In a separate group of 202 patients, 197 were able to undergo urgent procedures after a median of 1.6 hours, Charles V. Pollack Jr., MD, and his associates reported at the International Society on Thrombosis and Haemostasis congress. The report was simultaneously published in the New England Journal of Medicine.
Idarucizumab was specifically developed to reverse the anticoagulant effect of dabigatran. Many countries have already licensed the humanized monoclonal antibody fragment based on interim results for the first 90 patients enrolled in the Reversal Effects of Idarucizumab on Active Dabigatran (RE-VERSE AD) study (NCT02104947), noted Dr. Pollack, of Thomas Jefferson University, Philadelphia.
The final RE-VERSE AD cohort included 301 patients with uncontrolled gastrointestinal, intracranial, or trauma-related bleeding and 202 patients who needed urgent procedures. Participants from both groups typically were white, in their late 70s (age range, 21-96 years), and receiving 110 mg (75-150 mg) dabigatran twice daily. The primary endpoint was maximum percentage reversal within 4 hours after patients received idarucizumab, based on diluted thrombin time and ecarin clotting time.
The median maximum percentage reversal of dabigatran was 100% (95% confidence interval, 100% to 100%) in more than 98% of patients, and the effect usually lasted 24 hours. Among patients who underwent procedures, intraprocedural hemostasis was considered normal in 93% of cases, mildly abnormal in 5% of cases, and moderately abnormal in 2% of cases, the researchers noted. Seven patients received another dose of idarucizumab after developing recurrent or postoperative bleeding.
A total of 24 patients had an adjudicated thrombotic event within 30 days after receiving idarucizumab. These events included pulmonary embolism, systemic embolism, ischemic stroke, deep vein thrombosis, and myocardial infarction. The fact that many patients did not restart anticoagulation could have contributed to these thrombotic events, the researchers asserted. They noted that idarucizumab had no procoagulant activity in studies of animals and healthy human volunteers.
About 19% of patients in both groups died within 90 days. “Patients enrolled in this study were elderly, had numerous coexisting conditions, and presented with serious index events, such as intracranial hemorrhage, multiple trauma, sepsis, acute abdomen, or open fracture,” the investigators wrote. “Most of the deaths that occurred within 5 days after enrollment appeared to be related to the severity of the index event or to coexisting conditions, such as respiratory failure or multiple organ failure, whereas deaths that occurred after 30 days were more likely to be independent events or related to coexisting conditions.”
Boehringer Ingelheim Pharmaceuticals provided funding. Dr. Pollack disclosed grant support from Boehringer Ingelheim during the course of the study and ties to Daiichi Sankyo, Portola, CSL Behring, Bristol-Myers Squibb/Pfizer, Janssen Pharma, and AstraZeneca. Eighteen coinvestigators also disclosed ties to Boehringer Ingelheim and a number of other pharmaceutical companies. Two coinvestigators had no relevant financial disclosures.
One IV 5-g dose of idarucizumab completely, rapidly, and safely reversed the anticoagulant effect of dabigatran, according to final results for 503 patients in the multicenter, prospective, open-label, uncontrolled RE-VERSE AD study.
Uncontrolled bleeding stopped a median of 2.5 hours after 134 patients received idarucizumab. In a separate group of 202 patients, 197 were able to undergo urgent procedures after a median of 1.6 hours, Charles V. Pollack Jr., MD, and his associates reported at the International Society on Thrombosis and Haemostasis congress. The report was simultaneously published in the New England Journal of Medicine.
Idarucizumab was specifically developed to reverse the anticoagulant effect of dabigatran. Many countries have already licensed the humanized monoclonal antibody fragment based on interim results for the first 90 patients enrolled in the Reversal Effects of Idarucizumab on Active Dabigatran (RE-VERSE AD) study (NCT02104947), noted Dr. Pollack, of Thomas Jefferson University, Philadelphia.
The final RE-VERSE AD cohort included 301 patients with uncontrolled gastrointestinal, intracranial, or trauma-related bleeding and 202 patients who needed urgent procedures. Participants from both groups typically were white, in their late 70s (age range, 21-96 years), and receiving 110 mg (75-150 mg) dabigatran twice daily. The primary endpoint was maximum percentage reversal within 4 hours after patients received idarucizumab, based on diluted thrombin time and ecarin clotting time.
The median maximum percentage reversal of dabigatran was 100% (95% confidence interval, 100% to 100%) in more than 98% of patients, and the effect usually lasted 24 hours. Among patients who underwent procedures, intraprocedural hemostasis was considered normal in 93% of cases, mildly abnormal in 5% of cases, and moderately abnormal in 2% of cases, the researchers noted. Seven patients received another dose of idarucizumab after developing recurrent or postoperative bleeding.
A total of 24 patients had an adjudicated thrombotic event within 30 days after receiving idarucizumab. These events included pulmonary embolism, systemic embolism, ischemic stroke, deep vein thrombosis, and myocardial infarction. The fact that many patients did not restart anticoagulation could have contributed to these thrombotic events, the researchers asserted. They noted that idarucizumab had no procoagulant activity in studies of animals and healthy human volunteers.
About 19% of patients in both groups died within 90 days. “Patients enrolled in this study were elderly, had numerous coexisting conditions, and presented with serious index events, such as intracranial hemorrhage, multiple trauma, sepsis, acute abdomen, or open fracture,” the investigators wrote. “Most of the deaths that occurred within 5 days after enrollment appeared to be related to the severity of the index event or to coexisting conditions, such as respiratory failure or multiple organ failure, whereas deaths that occurred after 30 days were more likely to be independent events or related to coexisting conditions.”
Boehringer Ingelheim Pharmaceuticals provided funding. Dr. Pollack disclosed grant support from Boehringer Ingelheim during the course of the study and ties to Daiichi Sankyo, Portola, CSL Behring, Bristol-Myers Squibb/Pfizer, Janssen Pharma, and AstraZeneca. Eighteen coinvestigators also disclosed ties to Boehringer Ingelheim and a number of other pharmaceutical companies. Two coinvestigators had no relevant financial disclosures.
FROM 2017 ISTH CONGRESS
Key clinical point:
Major finding: Uncontrolled bleeding stopped a median of 2.5 hours after 134 patients received idarucizumab. In a separate group, 197 patients were able to undergo urgent procedures after a median of 1.6 hours.
Data source: A multicenter, prospective, open-label study of 503 patients (RE-VERSE AD).
Disclosures: Boehringer Ingelheim Pharmaceuticals provided funding. Dr. Pollack disclosed grant support from Boehringer Ingelheim during the course of the study and ties to Daiichi Sankyo, Portola, CSL Behring, BMS/Pfizer, Janssen Pharma, and AstraZeneca. Eighteen coinvestigators disclosed ties to Boehringer Ingelheim and a number of other pharmaceutical companies. Two coinvestigators had no relevant financial disclosures.
Massive blood transfusions increase risk with CRS/HIPEC
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
Massive allogenic blood transfusion during cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC) increased the risk of major complications and reduced overall survival in a review of 936 cases at St. George Hospital near Sydney, Australia.
CRS/HIPEC is a long, complex procedure for peritoneal carcinomatosis, pseudomyxoma peritonei, peritoneal mesothelioma, and other abdominal cancers. The abdomen is opened, the cancer is debulked as much as possible, and the cavity is filled with heated chemotherapy drugs. Because CRS/HIPEC often requires multivisceral resection and dissection in multiple abdominal regions, up to 77% of patients require intraoperative transfusions, and up to 37% require massive allogenic blood transfusions (MABT) with five or more units.
Blood transfusions are known to be associated with poorer cancer surgery outcomes, but their effect in CRS/HIPEC hasn’t been much studied, which is “surprising given the extent to which blood products are used in” the procedure, said investigators led by Akshat Saxena, MD, a surgeon at St. George Hospital (J Gastrointest Surg. 2017 May 30. doi: 10.1007/s11605-017-3444-8).
Based on their findings, the researchers concluded that “there is a real need to evaluate new strategies to reduce the rate of MABT during CRS/HIPEC.”
The procedures in the study were performed from 1996 to 2016. The in-hospital mortality rate was 0.3% in patients who did not have MABT but 4.4% among the 337 patients (36%) who did. Even after adjusting for confounders on multivariate analysis, including the fact that MABT patients had more extensive disease and longer surgeries, MABT significantly increased the risk of in-hospital mortality (relative risk, 7.72; P = .021). In patients requiring MABT had a 5-year survival of 5%. In patients not requiring MABT, 5-year survival was at 36%. The difference remained significant on multivariate analysis.
MABT patients also had twice the risk of life-threatening complications and complications requiring surgical, endoscopic, or radiological intervention (62% versus 30%; RR, 2.05; P less than .001). MABT patients were more likely to stay in the ICU for 4 or more days and in the hospital for 28 or more days.
Worse overall survival with MABT was driven at least in part by patients who had CRS/HIPEC for colorectal cancer peritoneal carcinomatosis and pseudomyxoma peritonei. MABT did not seem to contribute to lower survival in patients who had the procedure for appendiceal or ovarian cancer. “It seems that the impact of long-term immunomodulation induced by blood transfusion” – the suspected mechanism through which transfusions cause problems – “varies according to the disease subtype. This warrants further investigation,” the investigators said.
Several strategies have been tried to reduce the need for transfusions during CRS/HIPEC. The study team previously reported that preemptive clotting factor replacement helps. Others have had success with preemptive tranexamic acid and cryoprecipitate to address low serum fibrinogen levels during CRS/HIPEC. “Further evaluation of both these strategies is warranted,” the researchers said.
Funding source and disclosure information were not included in the study report.
FROM THE JOURNAL OF GASTROINTESTINAL SURGERY
Key clinical point:
Major finding: Even after adjusting for confounders, MABT significantly increased the risk of in-hospital mortality (RR, 7.72; P = .021).
Data source: A single institution review of 936 cases.
Disclosures: Funding source and disclosure information were not included in the study report.