User login
New Cushing’s guidelines emphasize team approach
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
New clinical practice guidelines for the treatment of Cushing’s syndrome stress coordinated care and patient involvement, and solidify an evidence-based treatment path for surgical and medical treatment options. The Endocrine Society released the guidelines, which were developed in conjunction with the European Society of Endocrinology (J Clin Endocrinol Metab. 2015 Aug;100[8]:2807-2831).
Dr. Lynette Nieman, chair of the task force that developed the guidelines, commented in an interview that the guidelines don’t really contain new or controversial elements, but they do help clarify existing best practices. “This is not a common diagnosis, but it is very important to understand how to handle this disorder,” said Dr. Nieman of the program in reproductive and adult endocrinology at the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md. “Cushing’s syndrome really needs to be treated with a team approach and by expert surgeons and expert endocrinologists,” she said.
In establishing treatment goals, the guidelines emphasize clinically based treatment, only recommending normalization of cortisol levels or action when overt Cushing’s syndrome (CS) and an established diagnosis exist (grade 1 recommendation). “Surgical resection of the causal lesion(s) is generally the first-line approach,” said Dr. Nieman and coauthors (grade 1 recommendation). Medical management of comorbidities and sequelae of hypercortisolism should always accompany any medical or surgical treatment. The guidelines also provide for emergent surgical or medical management of hypercortisolism if life-threatening complications are present (grade 1 recommendation).
Adjunctive management is directed at a patient-centered, multidisciplinary approach to address potential cortisol-dependent comorbidities. These may include hypertension and dyslipidemia, diabetes, electrolyte disturbances, increased infection risk, osteoporosis and deconditioning, and psychiatric illnesses (ungraded best practice recommendation). Additionally, the guidelines recommend perioperative prophylaxis for venous thromboembolism for CS patients (grade 2 recommendation).
For Cushing’s disease (CD), the guidelines recommend excision of ectopic and adrenal lesions, barring contraindications or low likelihood of successful surgery, with unilateral adrenal resection by an experienced adrenal surgeon recommended in benign unilateral disease. Ectopic adrenocorticotropic hormone (ACTH)–secreting tumors should be resected, with local node dissection as appropriate. Transsphenoidal selective adenomectomy is the recommended treatment for CD in adults and children, and should be performed by an experienced pituitary surgeon. Serum sodium should be measured several times during the first 2 weeks after surgery, and free T4 and prolactin by no more than 2 weeks after surgery (all grade 1 recommendations).
The task force recommends an MRI by 3 months after transsphenoidal surgery (ungraded best practice recommendation). When adrenal disorders are bilateral, the task force recommends surgical resection and medical therapy to block aberrant hormone receptors (grade 2 recommendation).
Carrying through the theme of an individualized, patient-centered approach, the task force recommends individualized postoperative management depending on postoperative cortisol levels. Persistent and overt postsurgical hypercortisolism should be treated, while patients with eucortisolism should have serum or salivary cortisol measured late at night. Patients with ACTH-dependent CS should be screened for recurrence of hypercortisolism (all grade 1 recommendations).
Glucocorticoid replacement, when required for hypocortisolemic patients, should be accompanied by appropriate patient education. When patients have an intact adrenal gland remaining, hypothalamic-pituitary-adrenal (HPA) axis recovery should be assessed at follow-up, so glucocorticoids can be stopped when recovery occurs. Other pituitary hormone deficiencies may occur, and care should include assessing the need to treat these deficiencies as well (all grade 1 recommendations).
In the difficult cases where surgery is not possible or does not cure ACTH-dependent CS, shared patient decision making is recommended to choose among the various second-line therapies that may be of benefit (grade 2 recommendation).
Therapy choices may include bilateral adrenalectomy, reserved for occult or metastatic ectopic ACTH secretion, or in an emergency situation where the procedure may be lifesaving (grade 2 recommendation); repeat transsphenoidal surgery when imaging or the clinical picture points to a new lesion or incomplete resection (grade 2 recommendation); radiation therapy or radiosurgery for those who fail transsphenoidal surgery or whose CD recurs, or where mass effect may be of concern (grade 1-2 recommendations; and medical treatment with steroidogenesis inhibitors in limited circumstances (grade 1 recommendation).
Specific medical treatment recommendations include the use of steroidogenesis inhibitors after transsphenoidal surgery for patients with CD or to treat occult or metastatic cases of ectopic ACTH secretion, and as an adjunct in adrenocortical carcinoma (grade 1 recommendation). The task force, in the discussion accompanying the guidelines, lists pros and cons of the various medical choices in order to present a balanced view of medical treatment options, said Dr. Nieman.
The long-term follow-up of individuals with CS should include screening and treating for the comorbidities that may persist even after successful surgery. Follow-up should be lifelong, with each comorbidity followed to resolution and ongoing vigilance for recurrence (except in patients with successfully resected low-attenuation adrenal adenomas – grade 1 recommendation).
In an interview, Dr. Rebecca S. Sippel of the University of Wisconsin–Madison brought an endocrine surgeon’s perspective to the guidelines, agreeing that the document generally reflects accepted practice. She also agreed that the interdisciplinary approach advocated by the task force is critical. “It’s important that discharge planning is done in a systematic way, so there’s systematic follow-up of patients after excision,” she said. She noted that CS patients on her service all receive an endocrine consult while they are inpatients to ensure adequate discharge planning.
Future research directions recommended by Dr. Nieman and the task force coauthors include identification of markers that will “explain the variable clinical effect of steroids among individuals,” with the goal of achieving better quantification of treatment effect and tracking response and remission. Health care–related quality of life is negatively affected by CS even after resolution to eucortisolism in many patients, so the guidelines recommend further research into quality of life and cognitive problems experienced by individuals with CS. Dr. Nieman specifically called for more multisite research, noting that diagnoses of Cushing’s disease and Cushing’s syndrome are rare, and etiologies are varied. “In order to get the numbers we need to do good research, we will need to cooperate,” she said.
All authors of the clinical practice guidelines had financial disclosures; a complete listing of disclosures and the task force’s methodology for resolving conflicts may be found in the downloadable guidelines.
On Twitter @karioakes
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Orbera intragastric balloon approved for weight loss in obese adults
Another endoscopically delivered intragastric balloon indicated as a weight loss aid in obese adults has been approved by the Food and Drug Administration.
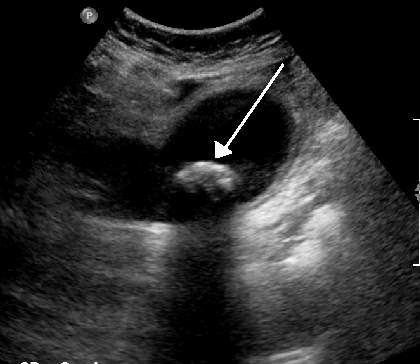
The Orbera intragastric balloon has been approved as a treatment for weight loss, in obese adults, with a body mass index between 30 and 40 kg/m2, the manufacturer, Apollo Endosurgery, announced on Aug. 6. It is intended for obese adults who are considering invasive surgery or for whom invasive surgery is not appropriate, when diet and exercise or pharmaceutical interventions have not worked, the statement said.
During a 20- to 30-minute procedure, the deflated Orbera silicone balloon is placed in the stomach via an endoscopic procedure under a mild sedative, where it is then filled with saline until it is about the size of a grapefruit, according to the company. The patient usually can go home on the same day; the balloon is deflated and removed 6 months later. The company will provide patients with an individualized weight-loss program for patients for 1 year, starting from the time of balloon placement.
The approval of this device follows the approval of the ReShape intragastric balloon for obese adults, for up to 6 months, announced by the FDA on July 28. ReShape was the first such device to be approved in the United States.
The results of the pivotal U.S. 12-month multicenter trial of the Orbera balloon in more than 250 obese adults with a BMI of 30-40 kg/m2 were reported at the Digestive Disease Week meeting in May, by Dr. Barham K. Abu Dayyeh of the Mayo Clinic in Rochester, Minn. For more than 2 years, patients were randomized to a 12-month behavioral modification program, with or without endoscopic placement of the balloon, which was removed at 6 months. Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months.
At 6 months, the mean percent total body weight loss was about 10% in the balloon group, vs. 4% in the control group, a significant difference (P less than .001). In addition, the total body weight loss was significantly higher in the balloon group at 3, 6, 9, and 12 months, and the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P less than .001), he said at the meeting. The majority of excess weight loss achieved at 6 months was also maintained at 12 months.
Serious adverse events were reported in 7% of controls and almost 10% of the balloon group, which included eight early removals for intolerance, one gastric outlet obstruction, one laryngospasm during placement, one case of severe abdominal cramping, and one case of severe dehydration. Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. There were no deaths during the study.
The Orbera balloon has been available in more than 80 countries, according to the manufacturer.
More information is available on the FDA website.
Another endoscopically delivered intragastric balloon indicated as a weight loss aid in obese adults has been approved by the Food and Drug Administration.
The Orbera intragastric balloon has been approved as a treatment for weight loss, in obese adults, with a body mass index between 30 and 40 kg/m2, the manufacturer, Apollo Endosurgery, announced on Aug. 6. It is intended for obese adults who are considering invasive surgery or for whom invasive surgery is not appropriate, when diet and exercise or pharmaceutical interventions have not worked, the statement said.
During a 20- to 30-minute procedure, the deflated Orbera silicone balloon is placed in the stomach via an endoscopic procedure under a mild sedative, where it is then filled with saline until it is about the size of a grapefruit, according to the company. The patient usually can go home on the same day; the balloon is deflated and removed 6 months later. The company will provide patients with an individualized weight-loss program for patients for 1 year, starting from the time of balloon placement.
The approval of this device follows the approval of the ReShape intragastric balloon for obese adults, for up to 6 months, announced by the FDA on July 28. ReShape was the first such device to be approved in the United States.
The results of the pivotal U.S. 12-month multicenter trial of the Orbera balloon in more than 250 obese adults with a BMI of 30-40 kg/m2 were reported at the Digestive Disease Week meeting in May, by Dr. Barham K. Abu Dayyeh of the Mayo Clinic in Rochester, Minn. For more than 2 years, patients were randomized to a 12-month behavioral modification program, with or without endoscopic placement of the balloon, which was removed at 6 months. Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months.
At 6 months, the mean percent total body weight loss was about 10% in the balloon group, vs. 4% in the control group, a significant difference (P less than .001). In addition, the total body weight loss was significantly higher in the balloon group at 3, 6, 9, and 12 months, and the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P less than .001), he said at the meeting. The majority of excess weight loss achieved at 6 months was also maintained at 12 months.
Serious adverse events were reported in 7% of controls and almost 10% of the balloon group, which included eight early removals for intolerance, one gastric outlet obstruction, one laryngospasm during placement, one case of severe abdominal cramping, and one case of severe dehydration. Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. There were no deaths during the study.
The Orbera balloon has been available in more than 80 countries, according to the manufacturer.
More information is available on the FDA website.
Another endoscopically delivered intragastric balloon indicated as a weight loss aid in obese adults has been approved by the Food and Drug Administration.
The Orbera intragastric balloon has been approved as a treatment for weight loss, in obese adults, with a body mass index between 30 and 40 kg/m2, the manufacturer, Apollo Endosurgery, announced on Aug. 6. It is intended for obese adults who are considering invasive surgery or for whom invasive surgery is not appropriate, when diet and exercise or pharmaceutical interventions have not worked, the statement said.
During a 20- to 30-minute procedure, the deflated Orbera silicone balloon is placed in the stomach via an endoscopic procedure under a mild sedative, where it is then filled with saline until it is about the size of a grapefruit, according to the company. The patient usually can go home on the same day; the balloon is deflated and removed 6 months later. The company will provide patients with an individualized weight-loss program for patients for 1 year, starting from the time of balloon placement.
The approval of this device follows the approval of the ReShape intragastric balloon for obese adults, for up to 6 months, announced by the FDA on July 28. ReShape was the first such device to be approved in the United States.
The results of the pivotal U.S. 12-month multicenter trial of the Orbera balloon in more than 250 obese adults with a BMI of 30-40 kg/m2 were reported at the Digestive Disease Week meeting in May, by Dr. Barham K. Abu Dayyeh of the Mayo Clinic in Rochester, Minn. For more than 2 years, patients were randomized to a 12-month behavioral modification program, with or without endoscopic placement of the balloon, which was removed at 6 months. Eighteen patients withdrew before treatment; 215 patients were evaluable at 6 months, 206 at 9 months, and 191 at 12 months.
At 6 months, the mean percent total body weight loss was about 10% in the balloon group, vs. 4% in the control group, a significant difference (P less than .001). In addition, the total body weight loss was significantly higher in the balloon group at 3, 6, 9, and 12 months, and the mean percent of excess weight loss at 6 months was better in the balloon group than in the control group (about 40% vs. 13%; P less than .001), he said at the meeting. The majority of excess weight loss achieved at 6 months was also maintained at 12 months.
Serious adverse events were reported in 7% of controls and almost 10% of the balloon group, which included eight early removals for intolerance, one gastric outlet obstruction, one laryngospasm during placement, one case of severe abdominal cramping, and one case of severe dehydration. Early device removals occurred in 22% of patients, 15 for symptoms and 13 at subject request, Dr. Abu Dayyeh said. There were no deaths during the study.
The Orbera balloon has been available in more than 80 countries, according to the manufacturer.
More information is available on the FDA website.
ERAS protocol cuts colorectal surgery morbidity, SSIs
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Through an ERAS protocol, attention to details and small multiple changes can result in dramatic improvements in patient outcomes.
Major finding: After full ERAS implementation, rates of postoperative morbidity and total surgical site infection were reduced 48.7% and 45%, respectively.
Data source: A retrospective analysis of 278 patients undergoing elective colorectal surgery.
Disclosures: The study authors reported having no relevant financial conflicts.
Laparoscopic sleeve gastrectomy: Comorbidity benefits fade with time
Five years after laparoscopic sleeve gastrectomy, patients will have regained, on average, about half of their preop excess weight, according to an Israeli investigation published online Aug. 5 in JAMA Surgery.
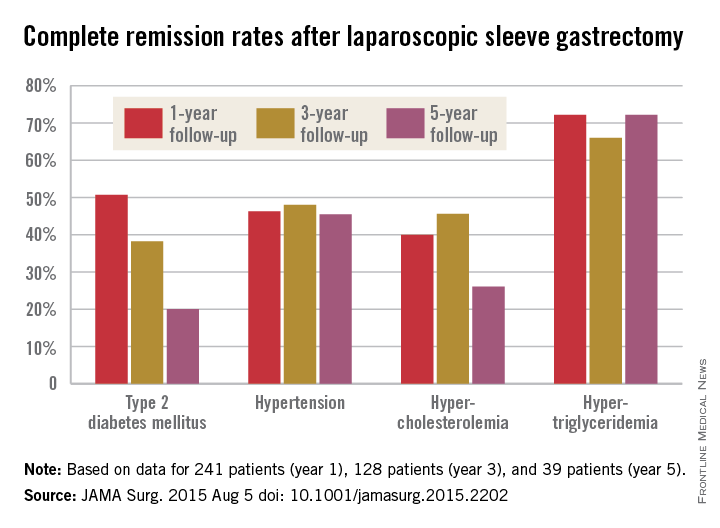
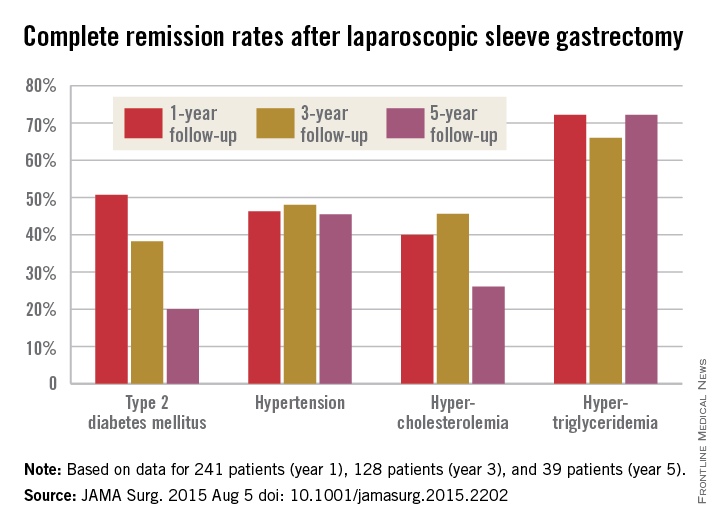
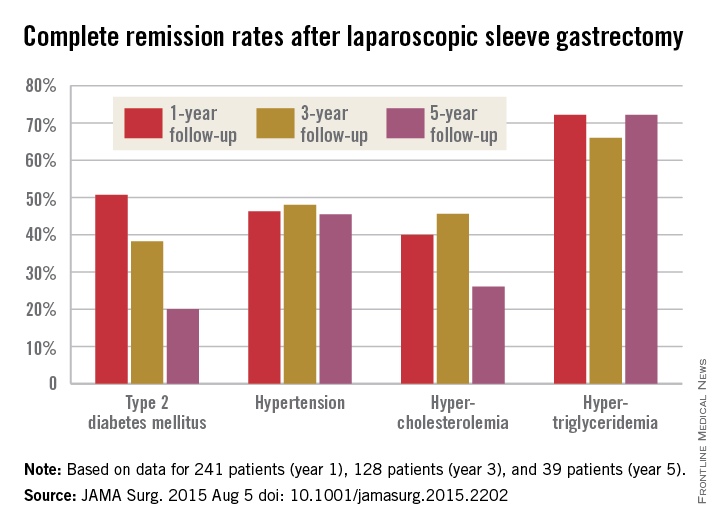
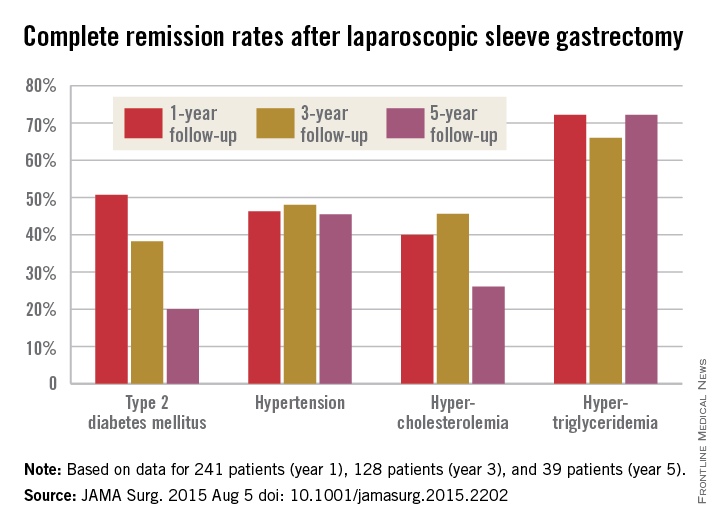
Things went better at first for the 443 patients in the study; at 1 year follow-up, they had lost, on average, 76.8% of their excess weight, but then it started to come back. At 3 years, patients were free of 69.7% of their excess weight, and at 5 years, just 56.1%. The failure rate – the number of patients with a percentage of excess weight loss less than 50% – increased from 13.3% at 1 year to 21.1% at 3 years and 38.5% at 5 years (JAMA Surg. 2015 Aug. 5. doi:10.1001/jamasurg.2015.2202).
The story was similar for obesity-related comorbidities; early gains eroded with time. Complete remission of diabetes, for instance, was maintained by 50.7% of patients at 1 year, 38.2% at 3 years, and just 20.0% at 5 years. Likewise, a drop in LDL cholesterol from baseline was significant at years 1 and 3, but not 5. Meanwhile, laparoscopic sleeve gastrectomy (LSG) didn’t significantly improve total cholesterol over baseline, and triglyceride improvements began to fade after year 1.
“In our opinion, the presence of obesity-related comorbidities should play a major role when choosing the appropriate procedure for a specific patient. For example, performing an operation that yields a low resolution rate of hyperlipidemia translates into lifelong medical treatment in a young patient with significant hyperlipidemia. In that case, a malabsorptive procedure might be more beneficial than LSG. If the recurrence of obesity is known to be followed by the remittance of an existing comorbidity in a specific procedure, an alternative procedure should be considered. The weight loss durability failure of almost 40% at 5 years of follow-up of LSG should be one of the deciding factors in such cases,” said senior investigator and bariatric surgeon Dr. Andrei Keidar of Beilinson Hospital in Petah Tikva, Israel, and his colleagues.
LSG is becoming more popular in part because it’s easier to learn and less disruptive than gastric bypass, but there are not enough data on long-term outcomes; the investigators sought to fill the gaps.
The average age in the study was 42.2 years; mean body mass index was 43.9 kg/m2, and mean preop excess weight was 51.2 kg. The majority of subjects were women. The operations were performed from 2006 to 2013, and there was considerable loss to follow-up during the project.
Baseline triglycerides followed overall trends with a drop from a mean of 155.2 mg/dL to 106.3 mg/dL at year 1, followed by a tick upward to 107.2 mg/dL at year 3 and 126.4 mg/dL at year 5.
The mean preop HDL cholesterol of 46.7 mg/dL rose to 52.8 mg/dL at year 1 and remained at about that level at 5 years. Improvements in hypertension were fairly durable, as well, with remission in 46.3% of patients at 1 year, 48.0% at 3 years, and 45.5% at 5 years.
“Surprisingly, our results showed that none of the changes in obesity-related comorbidity status correlated with” the amount of “excess weight prior to the surgery,” the investigators noted.
The authors didn’t compare LSG to other bariatric surgeries, but did note that in 2012, the American Society for Metabolic and Bariatric Surgery found that short-term weight loss and improvement in comorbidities was better with LSG than with Roux-en-Y gastric bypass (RYGB) and laparoscopic adjustable gastric bypass. On the other hand, RYGB has been found to beat LSG on lipid fraction improvements and short term control of type 2 diabetes.
The investigators had no disclosures.
Laparoscopic sleeve gastrectomy [has evolved] very quickly during the last several years into the dominant procedure in use despite a complete void of information about the longer-term effects. [The investigators try] to address this ... but clearly raise more issues than they can answer.

|
Dr. Anita P. Courcoulas |
It is unclear whether current studies will address critical questions about the long-term outcomes of bariatric surgery, including the sustainability of weight loss and comorbidity control and long-term complication rates. The answers will likely be generated over time not only by ... large-scale efforts but also by thoughtful inference that will be made through pooled analyses of data like that from [this study] and from many other disparate randomized and nonrandomized studies of bariatric surgery. It will take time, patience, and a willingness to avoid a rush to judgment. In the meantime, clinicians and prospective patients will need to discuss and weigh the evidence in a dynamic exchange driven not always by final conclusions but by the most current available data.
Dr. Anita Courcoulas is professor of surgery and chief of the section of minimally invasive bariatric and general surgery at the University of Pittsburgh. She reported receiving grants from Nutrisystem, Ethicon, and Covidien and serving as a project consultant for Ethicon and Apollo Endosurgery. She made her comments in an editorial that accompanied the study.
Laparoscopic sleeve gastrectomy [has evolved] very quickly during the last several years into the dominant procedure in use despite a complete void of information about the longer-term effects. [The investigators try] to address this ... but clearly raise more issues than they can answer.

|
Dr. Anita P. Courcoulas |
It is unclear whether current studies will address critical questions about the long-term outcomes of bariatric surgery, including the sustainability of weight loss and comorbidity control and long-term complication rates. The answers will likely be generated over time not only by ... large-scale efforts but also by thoughtful inference that will be made through pooled analyses of data like that from [this study] and from many other disparate randomized and nonrandomized studies of bariatric surgery. It will take time, patience, and a willingness to avoid a rush to judgment. In the meantime, clinicians and prospective patients will need to discuss and weigh the evidence in a dynamic exchange driven not always by final conclusions but by the most current available data.
Dr. Anita Courcoulas is professor of surgery and chief of the section of minimally invasive bariatric and general surgery at the University of Pittsburgh. She reported receiving grants from Nutrisystem, Ethicon, and Covidien and serving as a project consultant for Ethicon and Apollo Endosurgery. She made her comments in an editorial that accompanied the study.
Laparoscopic sleeve gastrectomy [has evolved] very quickly during the last several years into the dominant procedure in use despite a complete void of information about the longer-term effects. [The investigators try] to address this ... but clearly raise more issues than they can answer.

|
Dr. Anita P. Courcoulas |
It is unclear whether current studies will address critical questions about the long-term outcomes of bariatric surgery, including the sustainability of weight loss and comorbidity control and long-term complication rates. The answers will likely be generated over time not only by ... large-scale efforts but also by thoughtful inference that will be made through pooled analyses of data like that from [this study] and from many other disparate randomized and nonrandomized studies of bariatric surgery. It will take time, patience, and a willingness to avoid a rush to judgment. In the meantime, clinicians and prospective patients will need to discuss and weigh the evidence in a dynamic exchange driven not always by final conclusions but by the most current available data.
Dr. Anita Courcoulas is professor of surgery and chief of the section of minimally invasive bariatric and general surgery at the University of Pittsburgh. She reported receiving grants from Nutrisystem, Ethicon, and Covidien and serving as a project consultant for Ethicon and Apollo Endosurgery. She made her comments in an editorial that accompanied the study.
Five years after laparoscopic sleeve gastrectomy, patients will have regained, on average, about half of their preop excess weight, according to an Israeli investigation published online Aug. 5 in JAMA Surgery.
Things went better at first for the 443 patients in the study; at 1 year follow-up, they had lost, on average, 76.8% of their excess weight, but then it started to come back. At 3 years, patients were free of 69.7% of their excess weight, and at 5 years, just 56.1%. The failure rate – the number of patients with a percentage of excess weight loss less than 50% – increased from 13.3% at 1 year to 21.1% at 3 years and 38.5% at 5 years (JAMA Surg. 2015 Aug. 5. doi:10.1001/jamasurg.2015.2202).
The story was similar for obesity-related comorbidities; early gains eroded with time. Complete remission of diabetes, for instance, was maintained by 50.7% of patients at 1 year, 38.2% at 3 years, and just 20.0% at 5 years. Likewise, a drop in LDL cholesterol from baseline was significant at years 1 and 3, but not 5. Meanwhile, laparoscopic sleeve gastrectomy (LSG) didn’t significantly improve total cholesterol over baseline, and triglyceride improvements began to fade after year 1.
“In our opinion, the presence of obesity-related comorbidities should play a major role when choosing the appropriate procedure for a specific patient. For example, performing an operation that yields a low resolution rate of hyperlipidemia translates into lifelong medical treatment in a young patient with significant hyperlipidemia. In that case, a malabsorptive procedure might be more beneficial than LSG. If the recurrence of obesity is known to be followed by the remittance of an existing comorbidity in a specific procedure, an alternative procedure should be considered. The weight loss durability failure of almost 40% at 5 years of follow-up of LSG should be one of the deciding factors in such cases,” said senior investigator and bariatric surgeon Dr. Andrei Keidar of Beilinson Hospital in Petah Tikva, Israel, and his colleagues.
LSG is becoming more popular in part because it’s easier to learn and less disruptive than gastric bypass, but there are not enough data on long-term outcomes; the investigators sought to fill the gaps.
The average age in the study was 42.2 years; mean body mass index was 43.9 kg/m2, and mean preop excess weight was 51.2 kg. The majority of subjects were women. The operations were performed from 2006 to 2013, and there was considerable loss to follow-up during the project.
Baseline triglycerides followed overall trends with a drop from a mean of 155.2 mg/dL to 106.3 mg/dL at year 1, followed by a tick upward to 107.2 mg/dL at year 3 and 126.4 mg/dL at year 5.
The mean preop HDL cholesterol of 46.7 mg/dL rose to 52.8 mg/dL at year 1 and remained at about that level at 5 years. Improvements in hypertension were fairly durable, as well, with remission in 46.3% of patients at 1 year, 48.0% at 3 years, and 45.5% at 5 years.
“Surprisingly, our results showed that none of the changes in obesity-related comorbidity status correlated with” the amount of “excess weight prior to the surgery,” the investigators noted.
The authors didn’t compare LSG to other bariatric surgeries, but did note that in 2012, the American Society for Metabolic and Bariatric Surgery found that short-term weight loss and improvement in comorbidities was better with LSG than with Roux-en-Y gastric bypass (RYGB) and laparoscopic adjustable gastric bypass. On the other hand, RYGB has been found to beat LSG on lipid fraction improvements and short term control of type 2 diabetes.
The investigators had no disclosures.
Five years after laparoscopic sleeve gastrectomy, patients will have regained, on average, about half of their preop excess weight, according to an Israeli investigation published online Aug. 5 in JAMA Surgery.
Things went better at first for the 443 patients in the study; at 1 year follow-up, they had lost, on average, 76.8% of their excess weight, but then it started to come back. At 3 years, patients were free of 69.7% of their excess weight, and at 5 years, just 56.1%. The failure rate – the number of patients with a percentage of excess weight loss less than 50% – increased from 13.3% at 1 year to 21.1% at 3 years and 38.5% at 5 years (JAMA Surg. 2015 Aug. 5. doi:10.1001/jamasurg.2015.2202).
The story was similar for obesity-related comorbidities; early gains eroded with time. Complete remission of diabetes, for instance, was maintained by 50.7% of patients at 1 year, 38.2% at 3 years, and just 20.0% at 5 years. Likewise, a drop in LDL cholesterol from baseline was significant at years 1 and 3, but not 5. Meanwhile, laparoscopic sleeve gastrectomy (LSG) didn’t significantly improve total cholesterol over baseline, and triglyceride improvements began to fade after year 1.
“In our opinion, the presence of obesity-related comorbidities should play a major role when choosing the appropriate procedure for a specific patient. For example, performing an operation that yields a low resolution rate of hyperlipidemia translates into lifelong medical treatment in a young patient with significant hyperlipidemia. In that case, a malabsorptive procedure might be more beneficial than LSG. If the recurrence of obesity is known to be followed by the remittance of an existing comorbidity in a specific procedure, an alternative procedure should be considered. The weight loss durability failure of almost 40% at 5 years of follow-up of LSG should be one of the deciding factors in such cases,” said senior investigator and bariatric surgeon Dr. Andrei Keidar of Beilinson Hospital in Petah Tikva, Israel, and his colleagues.
LSG is becoming more popular in part because it’s easier to learn and less disruptive than gastric bypass, but there are not enough data on long-term outcomes; the investigators sought to fill the gaps.
The average age in the study was 42.2 years; mean body mass index was 43.9 kg/m2, and mean preop excess weight was 51.2 kg. The majority of subjects were women. The operations were performed from 2006 to 2013, and there was considerable loss to follow-up during the project.
Baseline triglycerides followed overall trends with a drop from a mean of 155.2 mg/dL to 106.3 mg/dL at year 1, followed by a tick upward to 107.2 mg/dL at year 3 and 126.4 mg/dL at year 5.
The mean preop HDL cholesterol of 46.7 mg/dL rose to 52.8 mg/dL at year 1 and remained at about that level at 5 years. Improvements in hypertension were fairly durable, as well, with remission in 46.3% of patients at 1 year, 48.0% at 3 years, and 45.5% at 5 years.
“Surprisingly, our results showed that none of the changes in obesity-related comorbidity status correlated with” the amount of “excess weight prior to the surgery,” the investigators noted.
The authors didn’t compare LSG to other bariatric surgeries, but did note that in 2012, the American Society for Metabolic and Bariatric Surgery found that short-term weight loss and improvement in comorbidities was better with LSG than with Roux-en-Y gastric bypass (RYGB) and laparoscopic adjustable gastric bypass. On the other hand, RYGB has been found to beat LSG on lipid fraction improvements and short term control of type 2 diabetes.
The investigators had no disclosures.
FROM JAMA SURGERY
Key clinical point: Laparoscopic sleeve gastrectomy (LSG) might not be the best surgical choice for bariatric patients with significant hyperlipidemia.
Major finding: One year after LSG, patients lost, on average, 76.8% of their excess weight. At 3 years, patients were free of 69.7% of their excess weight, and at 5 years, just 56.1%.
Data source: Retrospective study of 443 Israeli laparoscopic sleeve gastrectomies.
Disclosures: The investigators had no disclosures.
CDC: Coordinated strategy will curb resistant infections
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
Key clinical point: A coordinated U.S. strategy is needed to stem the tide of antibiotic-resistant and health care–associated infections.
Major finding: A coordinated 5-year approach would prevent more than 600,000 infections and save more than 37,000 lives in the United States.
Data source: Centers for Disease Control and Prevention Vital Signs report modeling coordinated strategies to combat antibiotic resistant and health care–associated infections.
Disclosures: The study was sponsored by the Centers for Disease Control and Prevention, with assistance from Emerging Infectious Programs participants, the Agency for Healthcare Research and Quality, University of Pittsburgh Center for Simulation and Modeling, and the VA Salt Lake City Health Care System.
FDA approves ReShape intragastric balloon device for weight loss
The first intragastric balloon–based device designed to help obese people lose weight has been approved by the Food and Drug Administration, providing a treatment option that is less invasive than bariatric surgery and gastric banding.
The FDA approved the ReShape Integrated Dual Balloon System on July 28, for “weight reduction when used in conjunction with diet and exercise, in obese patients with a body mass index (BMI) of 30 kg/m2-40 kg/m2 and one or more obesity-related comorbid conditions,” in adults who have not been able to lose weight with diet and exercise alone, according to the agency’s approval letter. Laparoscopic gastric banding is indicated for patients with a BMI of at least 40 kg/m2 (or at least 30 kg/m2 in people with one or more obesity-related comorbidities) and bariatric surgery is usually recommended for patients with a BMI of at least 40 kg/m2 (or at least 35 kg/m2 in people with at least one obesity-related comorbidity).
The ReShape device is made up of two attached balloons that are placed in the stomach through a minimally invasive endoscopic procedure, where they are filled with about 2 cups of saline and methylene blue dye, under mild sedation; the balloons are sealed with mineral oil and left in place for up to 6 months. If a balloon ruptures, the dye appears in the urine. When it is time to remove the balloons, they are deflated then removed using another endoscopic procedure.
The device was evaluated in a pivotal study at eight U.S. sites of over 300 mostly female obese patients whose mean age was about 44 years; their mean weight was about 209-213 pounds, and their mean BMI was about 35 kg/m2; 187 received the device and 139 had the endoscopy only. All participants were on a medically managed diet and exercise program. At 6 months, those in the device group had lost a mean of about 24% of their weight, vs. a mean of about 11% among controls, a statistically significant difference (P = .0041). Those who had lost weight at 6 months “maintained 60% of this weight loss through 48 weeks of follow-up,” according to the FDA.
After placement of the device, common adverse events were vomiting, nausea, and abdominal pain, but most symptoms resolved within 30 days, according to the FDA. The development of gastric ulcerations is described as the “most worrisome” device-related risk, but “there were no unanticipated adverse device effects, no deaths, no intestinal obstructions, and no gastric perforations” in the study.
Among the 265 patients who received the device (those initially enrolled in the pivotal trial plus 78 who were in the control group and opted to receive the device after the first 6 months), 20 (7.5%) experienced severe adverse events; vomiting was the most common, in 4.5%. Serious events included gastric ulcers in two patients (0.8%) at 19 and at 97 days after the device was placed; in both cases, the device was removed. Almost 15% of those who received the device had to have it removed because of an adverse event. The rate of gastric ulcers after a minor change was made to the device was 10%; and the rate of balloon deflations without migration was 6%.
The FDA summary of the approval refers to the “marginal benefit of weight loss” among those in the treatment group, compared with controls, but adds that the decision to approve the device “is based in part on the limited options available to patients with mild to moderate obesity who have failed other means for conservative weight loss.” While the effectiveness of the device is better than what would be expected with diet and exercise or pharmacologic therapy,” it is “substantially less than what would be expected with gastric banding or other surgical interventions.” The list of contraindications includes previous gastrointestinal surgery “with sequelae,” such as an obstruction or adhesions; previous bariatric surgery; any GI inflammatory disease, severe coagulopathy; and women who are pregnant or breastfeeding.
“The company plans to make the ReShape procedure available to patients first in select markets, as physicians and allied health professionals are trained in the procedure and support program to optimize patient outcome,” according to the company’s statement announcing approval.
The ReShape device has been available in Europe since 2007.
Information posted by the FDA, including labeling for professionals, is available at www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfTopic/pma/pma.cfm?num=P140012.
The first intragastric balloon–based device designed to help obese people lose weight has been approved by the Food and Drug Administration, providing a treatment option that is less invasive than bariatric surgery and gastric banding.
The FDA approved the ReShape Integrated Dual Balloon System on July 28, for “weight reduction when used in conjunction with diet and exercise, in obese patients with a body mass index (BMI) of 30 kg/m2-40 kg/m2 and one or more obesity-related comorbid conditions,” in adults who have not been able to lose weight with diet and exercise alone, according to the agency’s approval letter. Laparoscopic gastric banding is indicated for patients with a BMI of at least 40 kg/m2 (or at least 30 kg/m2 in people with one or more obesity-related comorbidities) and bariatric surgery is usually recommended for patients with a BMI of at least 40 kg/m2 (or at least 35 kg/m2 in people with at least one obesity-related comorbidity).
The ReShape device is made up of two attached balloons that are placed in the stomach through a minimally invasive endoscopic procedure, where they are filled with about 2 cups of saline and methylene blue dye, under mild sedation; the balloons are sealed with mineral oil and left in place for up to 6 months. If a balloon ruptures, the dye appears in the urine. When it is time to remove the balloons, they are deflated then removed using another endoscopic procedure.
The device was evaluated in a pivotal study at eight U.S. sites of over 300 mostly female obese patients whose mean age was about 44 years; their mean weight was about 209-213 pounds, and their mean BMI was about 35 kg/m2; 187 received the device and 139 had the endoscopy only. All participants were on a medically managed diet and exercise program. At 6 months, those in the device group had lost a mean of about 24% of their weight, vs. a mean of about 11% among controls, a statistically significant difference (P = .0041). Those who had lost weight at 6 months “maintained 60% of this weight loss through 48 weeks of follow-up,” according to the FDA.
After placement of the device, common adverse events were vomiting, nausea, and abdominal pain, but most symptoms resolved within 30 days, according to the FDA. The development of gastric ulcerations is described as the “most worrisome” device-related risk, but “there were no unanticipated adverse device effects, no deaths, no intestinal obstructions, and no gastric perforations” in the study.
Among the 265 patients who received the device (those initially enrolled in the pivotal trial plus 78 who were in the control group and opted to receive the device after the first 6 months), 20 (7.5%) experienced severe adverse events; vomiting was the most common, in 4.5%. Serious events included gastric ulcers in two patients (0.8%) at 19 and at 97 days after the device was placed; in both cases, the device was removed. Almost 15% of those who received the device had to have it removed because of an adverse event. The rate of gastric ulcers after a minor change was made to the device was 10%; and the rate of balloon deflations without migration was 6%.
The FDA summary of the approval refers to the “marginal benefit of weight loss” among those in the treatment group, compared with controls, but adds that the decision to approve the device “is based in part on the limited options available to patients with mild to moderate obesity who have failed other means for conservative weight loss.” While the effectiveness of the device is better than what would be expected with diet and exercise or pharmacologic therapy,” it is “substantially less than what would be expected with gastric banding or other surgical interventions.” The list of contraindications includes previous gastrointestinal surgery “with sequelae,” such as an obstruction or adhesions; previous bariatric surgery; any GI inflammatory disease, severe coagulopathy; and women who are pregnant or breastfeeding.
“The company plans to make the ReShape procedure available to patients first in select markets, as physicians and allied health professionals are trained in the procedure and support program to optimize patient outcome,” according to the company’s statement announcing approval.
The ReShape device has been available in Europe since 2007.
Information posted by the FDA, including labeling for professionals, is available at www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfTopic/pma/pma.cfm?num=P140012.
The first intragastric balloon–based device designed to help obese people lose weight has been approved by the Food and Drug Administration, providing a treatment option that is less invasive than bariatric surgery and gastric banding.
The FDA approved the ReShape Integrated Dual Balloon System on July 28, for “weight reduction when used in conjunction with diet and exercise, in obese patients with a body mass index (BMI) of 30 kg/m2-40 kg/m2 and one or more obesity-related comorbid conditions,” in adults who have not been able to lose weight with diet and exercise alone, according to the agency’s approval letter. Laparoscopic gastric banding is indicated for patients with a BMI of at least 40 kg/m2 (or at least 30 kg/m2 in people with one or more obesity-related comorbidities) and bariatric surgery is usually recommended for patients with a BMI of at least 40 kg/m2 (or at least 35 kg/m2 in people with at least one obesity-related comorbidity).
The ReShape device is made up of two attached balloons that are placed in the stomach through a minimally invasive endoscopic procedure, where they are filled with about 2 cups of saline and methylene blue dye, under mild sedation; the balloons are sealed with mineral oil and left in place for up to 6 months. If a balloon ruptures, the dye appears in the urine. When it is time to remove the balloons, they are deflated then removed using another endoscopic procedure.
The device was evaluated in a pivotal study at eight U.S. sites of over 300 mostly female obese patients whose mean age was about 44 years; their mean weight was about 209-213 pounds, and their mean BMI was about 35 kg/m2; 187 received the device and 139 had the endoscopy only. All participants were on a medically managed diet and exercise program. At 6 months, those in the device group had lost a mean of about 24% of their weight, vs. a mean of about 11% among controls, a statistically significant difference (P = .0041). Those who had lost weight at 6 months “maintained 60% of this weight loss through 48 weeks of follow-up,” according to the FDA.
After placement of the device, common adverse events were vomiting, nausea, and abdominal pain, but most symptoms resolved within 30 days, according to the FDA. The development of gastric ulcerations is described as the “most worrisome” device-related risk, but “there were no unanticipated adverse device effects, no deaths, no intestinal obstructions, and no gastric perforations” in the study.
Among the 265 patients who received the device (those initially enrolled in the pivotal trial plus 78 who were in the control group and opted to receive the device after the first 6 months), 20 (7.5%) experienced severe adverse events; vomiting was the most common, in 4.5%. Serious events included gastric ulcers in two patients (0.8%) at 19 and at 97 days after the device was placed; in both cases, the device was removed. Almost 15% of those who received the device had to have it removed because of an adverse event. The rate of gastric ulcers after a minor change was made to the device was 10%; and the rate of balloon deflations without migration was 6%.
The FDA summary of the approval refers to the “marginal benefit of weight loss” among those in the treatment group, compared with controls, but adds that the decision to approve the device “is based in part on the limited options available to patients with mild to moderate obesity who have failed other means for conservative weight loss.” While the effectiveness of the device is better than what would be expected with diet and exercise or pharmacologic therapy,” it is “substantially less than what would be expected with gastric banding or other surgical interventions.” The list of contraindications includes previous gastrointestinal surgery “with sequelae,” such as an obstruction or adhesions; previous bariatric surgery; any GI inflammatory disease, severe coagulopathy; and women who are pregnant or breastfeeding.
“The company plans to make the ReShape procedure available to patients first in select markets, as physicians and allied health professionals are trained in the procedure and support program to optimize patient outcome,” according to the company’s statement announcing approval.
The ReShape device has been available in Europe since 2007.
Information posted by the FDA, including labeling for professionals, is available at www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfTopic/pma/pma.cfm?num=P140012.
VIDEO: Postoperative cognitive decline hits women hardest
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
AT AAIC 2015
Surgical follow-up after ED cholelithiasis episode cuts long-term costs, complications
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
FROM JOURNAL OF SURGICAL RESEARCH
Key clinical point: Surgical follow-up after a patient presents at the ED with symptomatic cholelithiasis is critical in reducing ED visits, complications, and costs for gallbladder disease.
Major finding: Of those patients who did not have elective surgery, 37.1% had repeat visits to the ED for gallstone symptoms, 17.7% of which had two or more additional ED visits, and over half of those additional visits resulted in CT or ultrasound imaging.
Data source: A single-center study of 71 patients presenting to the emergency department with symptomatic cholelithiasis and followed for up to 2 years.
Disclosures: The investigators had no relevant disclosures.
Moderate THST was most effective at treating thyroid cancer
Moderate thyroid hormone suppression therapy (THST) is associated with the best outcomes for patients with all stages of thyroid cancer, according to a prospective analysis of a multi-institutional registry published in the Journal of Clinical Endocrinology & Metabolism.
The researchers examined the outcomes of initial treatment for 4,941 patients with differentiated thyroid cancer (DTC), according to registry data from the National Thyroid Cancer Treatment Cooperative Study Group. The treatments included total/near total thyroidectomy (T/NTT), postoperative radioactive iodine-131 (131I), and THST. The median duration between treatment and follow-up for a patient was 6 years, with follow-up information available for all but 94 (1.9%) of the patients in the cohort.
Overall improvement was noted in stage III patients who received 131I (risk ratio, 0.66; P = .04) and stage IV patients who received both T/NTT and 131I (RR, 0.66; P = .049). In all stages, moderate THST was associated with significantly improved overall survival (RR stages I-IV: 0.13, 0.09, 0.13, and 0.33, respectively) and disease-free survival (DFS) (RR stages I-III: 0.52, 0.40, and 0.18, respectively); no additional survival benefit was achieved with more aggressive THST, even when distant metastatic disease was diagnosed during follow-up.
Lower initial stage and moderate THST were independent predictors of improved overall survival during follow-up years 1-3.
Consistent with previous research, this study also showed that T/NTT followed by 131I is associated with benefit in high-risk, but not low-risk patients.
“We report for the first time, in multivariate analysis of primary treatments for DTC, across all stages, only THST was associated with both improved stage-adjusted OS and DFS,” noted Dr. Aubrey A. Carhill and his colleagues.
“This analysis of the larger, more mature registry database extends and refines earlier observations regarding the impact of initial therapies on patient outcomes and further justifies the need for prospective, long-term, controlled studies,” the researchers noted.
Read the full study in the Journal of Clinical Endocrinology & Metabolism (doi:10.1210/JC.2015-1346).
Moderate thyroid hormone suppression therapy (THST) is associated with the best outcomes for patients with all stages of thyroid cancer, according to a prospective analysis of a multi-institutional registry published in the Journal of Clinical Endocrinology & Metabolism.
The researchers examined the outcomes of initial treatment for 4,941 patients with differentiated thyroid cancer (DTC), according to registry data from the National Thyroid Cancer Treatment Cooperative Study Group. The treatments included total/near total thyroidectomy (T/NTT), postoperative radioactive iodine-131 (131I), and THST. The median duration between treatment and follow-up for a patient was 6 years, with follow-up information available for all but 94 (1.9%) of the patients in the cohort.
Overall improvement was noted in stage III patients who received 131I (risk ratio, 0.66; P = .04) and stage IV patients who received both T/NTT and 131I (RR, 0.66; P = .049). In all stages, moderate THST was associated with significantly improved overall survival (RR stages I-IV: 0.13, 0.09, 0.13, and 0.33, respectively) and disease-free survival (DFS) (RR stages I-III: 0.52, 0.40, and 0.18, respectively); no additional survival benefit was achieved with more aggressive THST, even when distant metastatic disease was diagnosed during follow-up.
Lower initial stage and moderate THST were independent predictors of improved overall survival during follow-up years 1-3.
Consistent with previous research, this study also showed that T/NTT followed by 131I is associated with benefit in high-risk, but not low-risk patients.
“We report for the first time, in multivariate analysis of primary treatments for DTC, across all stages, only THST was associated with both improved stage-adjusted OS and DFS,” noted Dr. Aubrey A. Carhill and his colleagues.
“This analysis of the larger, more mature registry database extends and refines earlier observations regarding the impact of initial therapies on patient outcomes and further justifies the need for prospective, long-term, controlled studies,” the researchers noted.
Read the full study in the Journal of Clinical Endocrinology & Metabolism (doi:10.1210/JC.2015-1346).
Moderate thyroid hormone suppression therapy (THST) is associated with the best outcomes for patients with all stages of thyroid cancer, according to a prospective analysis of a multi-institutional registry published in the Journal of Clinical Endocrinology & Metabolism.
The researchers examined the outcomes of initial treatment for 4,941 patients with differentiated thyroid cancer (DTC), according to registry data from the National Thyroid Cancer Treatment Cooperative Study Group. The treatments included total/near total thyroidectomy (T/NTT), postoperative radioactive iodine-131 (131I), and THST. The median duration between treatment and follow-up for a patient was 6 years, with follow-up information available for all but 94 (1.9%) of the patients in the cohort.
Overall improvement was noted in stage III patients who received 131I (risk ratio, 0.66; P = .04) and stage IV patients who received both T/NTT and 131I (RR, 0.66; P = .049). In all stages, moderate THST was associated with significantly improved overall survival (RR stages I-IV: 0.13, 0.09, 0.13, and 0.33, respectively) and disease-free survival (DFS) (RR stages I-III: 0.52, 0.40, and 0.18, respectively); no additional survival benefit was achieved with more aggressive THST, even when distant metastatic disease was diagnosed during follow-up.
Lower initial stage and moderate THST were independent predictors of improved overall survival during follow-up years 1-3.
Consistent with previous research, this study also showed that T/NTT followed by 131I is associated with benefit in high-risk, but not low-risk patients.
“We report for the first time, in multivariate analysis of primary treatments for DTC, across all stages, only THST was associated with both improved stage-adjusted OS and DFS,” noted Dr. Aubrey A. Carhill and his colleagues.
“This analysis of the larger, more mature registry database extends and refines earlier observations regarding the impact of initial therapies on patient outcomes and further justifies the need for prospective, long-term, controlled studies,” the researchers noted.
Read the full study in the Journal of Clinical Endocrinology & Metabolism (doi:10.1210/JC.2015-1346).
Elevated IL-6 linked to complications after major abdominal surgery
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
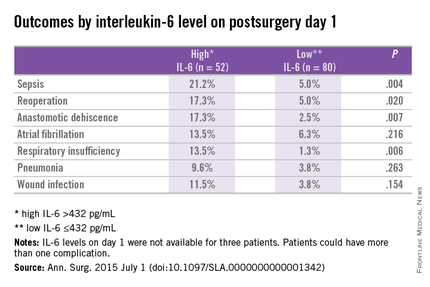
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
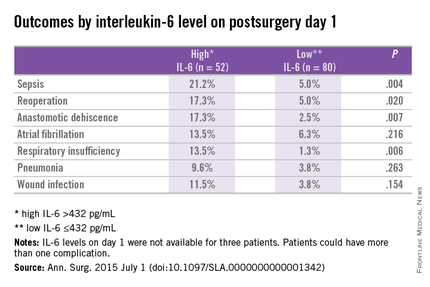
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
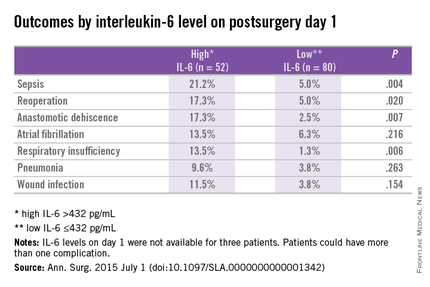
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Postoperative complications after major abdominal surgery are associated with elevated IL-6.
Major finding: Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (P < .02).
Data source: Prospective cohort study at a single center using data from the Myocardial Injury and Postoperative Complications after major abdominal surgery (MICOLON) study.
Disclosures: The authors reported no conflicts of interest.