User login
TEP inguinal hernia repairs have low incidence of chronic pain
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Chronic pain after total extraperitoneal inguinal hernia repair occurs infrequently in patients, and findings from a study suggest that the means of mesh fixation, permanent or nonpermanant, is not linked to greater risk of this outcome.
Dr. Nihad Gutlic and colleagues from the Skåne University Hospital at University of Lund, Sweden, sought to compare total extraperitoneal inguinal hernia repair (TEP) done with permanent fixture (PF) of mesh vs. nonfixed (NF) or nonpermanent fixation (NPF) and the impact of the means of mesh fixation on chronic pain. Their results were published online in the July issue of Annals of Surgery.
Prospective data were obtained from the Swedish Hernia Registry (SHR) and participants completed the Inguinal Pain Questionnaire (IPQ) and the Short Form-36 (SF-36) to measure health-related quality of life to assess chronic pain. Chronic pain was defined as pain that persisted more than 3 months after surgery.
The study included men aged 30-75 years, consecutively registered in the SHR for TEP repair of a primary groin hernia during January 2005 and May 2009, and the questionnaire was send between February 2010 and May 2010. A minimum follow-up of 6 months was stipulated. The IPQ assessed pain with 19 questions regarding the pain modalities intensity, frequency, duration, influence on daily activities, and testicular pain. Questions concerned “pain right now” and “pain past week” respectively, and answers were given on a 7-grade scale from “no pain” to “pain that could not be ignored – prompt medical advice sought.” Patients were followed for up to 33 months.
A total of 1,110 respondents were analyzed: 325 patients in the PF group and 785 patients in the NPF group (281 with fibrin glue and 504 NF). The PF group had more medial hernias (P < .003) and larger defect sizes (P < .002). There were no differences in the rate of reoperation between the two groups (P < .735).
For the IPQ questionnaire, 7.7% (n = 85) of patients reported having “pain that could not be ignored” in the last week with no difference between the PF group and the NF/NPF groups (P < .462). Of those patients responding, 5.4% reported having “pain right now” (n = 59) with no difference between the two groups (P < .270).
The authors conclude, “that TEP, carried out on men for primary inguinal hernia, is associated with a low frequency of chronic postoperative pain. No difference was seen between permanent and nonpermanent fixation regarding chronic pain.”
The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
FROM ANNALS OF SURGERY
Key clinical point: TEP inguinal hernia repair is associated with a low incidence of chronic pain.
Major finding: Utilizing the IPQ questionnaire, 7.7% of patients reported having “pain that could not be ignored” in the last week with no difference between the two groups (P < .462).
Data source: Prospective data obtained from the Swedish Hernia Registry, IPQ, and SF-36 questionnaires.
Disclosures: The authors declared no conflicts of interest. The study was supported by the Lund (Sweden) University, Region Skåne Research and Development Funds, and the Bard Norden AB and Helge B. Wulffs Foundation.
Risk of major bleeding is decreased when AF patients do not receive bridging anticoagulation
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
FROM 2015 ISTH CONGRESS
Key clinical point: Forgoing bridging anticoagulation in patients with atrial fibrillation is noninferior to perioperative bridging for preventing arterial thromboembolism and decreasing the risk of major bleeding.
Major finding: The incidence of arterial thromboembolism was 0.4% vs. 0.3% in the no-bridging and bridging groups, respectively. The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group.
Data source: A prospective, randomized, placebo-controlled, double-blind trial of 1,884 patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery.
Disclosures: The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
High VTE recurrence risk persists for at least 3 years
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
AT THE 2015 ISTH CONGRESS
Key clinical point: The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Major finding: Active cancer with chemotherapy was the strongest predictor of VTE recurrence (hazard ratio, 2.59).
Data source: Population-based surveillance of 2,989 adults patients.
Disclosures: The National Institutes of Health supported the study.
DDW: Study finds pancreatic cancer misdiagnosis rate at 31%
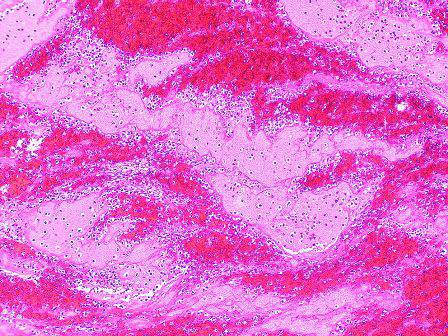
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
AT DDW® 2015
Key clinical point: Pancreatic cancer is often misdiagnosed, and should be considered in patients with vague or atypical symptoms who are referred for a cholecystectomy.
Major finding: About 31% of patients with pancreatic cancer were initially misdiagnosed, most often with a gallbladder disease–related diagnosis.
Data source: A study of 313 patients diagnosed with pancreatic cancer comparing presenting symptoms, the time it took to reach the correct diagnosis, and other features in patients initially misdiagnosed and those who were not misdiagnosed.
Disclosures: Dr. Swords said he had no relevant financial disclosures.
Hospital clinicians commonly work while sick
The vast majority of doctors and other trained medical professionals at a hospital went to work while sick within the past year, even though they realized the risk that decision places on patients, according to a recent study.
In fact, almost 1 in 10 hospital clinicians worked while sick at least five times in the past year, primarily because of staffing concerns or not wanting to let colleagues down, reported Julia Szymczak, Ph.D., and her associates at the Children’s Hospital of Philadelphia (JAMA Pediatr. 2015 July 6 [doi: 10.1001/jamapediatrics.2015.0684]).
“A combination of closed- and open-ended questions illustrated that the decision to work while sick was shaped by systems-level and sociocultural factors that interacted to cause our respondents to work while symptomatic, despite recognizing that this choice may put patients and colleagues at risk,” the authors wrote.
Of 929 surveys sent out, 538 clinicians completed them, which included 280 of 459 physicians (61%) and 256 of 470 advanced-practice clinicians (54.5%). The advanced-practice clinicians included registered nurses, physician assistants, clinical nurse specialists, registered nurse anesthetists, and certified nurse midwives. Of those who responded, 15.7% worked in intensive care, 13.1% in surgery, 12.5% in general pediatrics, and 44.8% in another pediatric subspecialty.
Although 95.3% of respondents believed working while sick put patients at risk, 83.1% reported having done so at least once in the past year. Further, that proportion included 52% of all respondents who reported coming to work sick twice in the past year and 9.3% who worked while ill at least five times in the past year.
Nearly a third of respondents said they would work even if they had diarrhea (30%), while 16% said they would work with a fever, and 55.6% would work with acute respiratory symptoms, including cough, congestion, rhinorrhea, and sore throat.
But doctors were more likely than other professionals to say they would go to work with these symptoms: 38.9% of doctors would work despite diarrhea, compared with 19.9% of advanced-practice clinicians. Doctors and advanced-practice clinicians would also work with acute respiratory symptoms (60% vs. 50.8%, respectively), a fever only (21.8% vs. 9.8%), and fever and chills with body aches (18.6% vs. 10.9%, all P < .03).
Nearly every respondent (98.7%) said they worked despite being sick because they did not want to let their colleagues down, just as almost all of them worried the hospital would not have enough staff (94.9%) or that they would let their patients down (92.5%).
Smaller majorities of respondents also worked because others also work while sick (65%), worried their colleagues would ostracize them (64%) if they didn’t work, were concerned about their patients’ continuity of care (63.8%), had unsupportive leadership (56.2%), or believed they could not be easily replaced (52.6%).
Among the 316 respondents who filled in additional reasons, 64.9% said they had a very hard time finding someone to cover their shift, 61.1% described a strong cultural norm to work unless extremely sick, and 57% expressed uncertainty about what is considered “too sick to work.”
The Centers for Disease Control and Prevention funded the research. The authors reported no disclosures.
For centuries, a guiding principle for health care workers has been primum non nocere, or first do no harm. However, health care workers do exactly that when they work with patients while ill themselves with contagious infections. Even common but untreatable infectious like enterovirus and respiratory syncytial virus can prove deadly to immunocompromised patients.
The propensity to work while ill is influenced by cultural trends. In past years, many ill physicians worked even to the point of receiving intravenous fluids while on the job; working while sick was regarded as a badge of courage. Dr. Szymczak and colleagues identified as an issue the absence of an effective sick relief system that has sufficient flexibility to “staff up” during high rates of health care worker illness. Sick relief systems and policies need to be clear regarding when health care workers should stay away from work, how patient coverage will be ensured, and the availability of and access to paid sick leave.
Determining what constitutes being too sick to work is complicated and lacks a sufficient evidence base. Using a system that bases work restrictions on the presence of key symptoms may add clarity and enable health care workers to recognize when they need to stay home.
Creating a safer and more equitable system of sick leave for health care workers requires a culture change in many institutions to decrease the stigma – internal and external – associated with health care worker illness. Identifying solutions to prioritize patient safety must factor in workforce demands and variability in patient census and emphasize flexibility. Strong administrative and physician leadership and creativity are essential to support appropriate sick leave and ensure adequate staffing. Hospital leadership must ensure that the culture supports a paid sick leave policy that is adequate and nonpunitive.
These comments are selected from an accompanying editorial (JAMA Pediatr. 2015 July 6 [doi:10.1001/jamapediatrics.2015.0994]), written by Dr. Jeffrey R. Starke of the department of pediatrics at Baylor College of Medicine in Houston, and Dr. Mary Anne Jackson of the division of infectious diseases at Children’s Mercy Hospital, University of Missouri–Kansas City. Dr. Starke and Dr. Jackson reported no disclosures.
For centuries, a guiding principle for health care workers has been primum non nocere, or first do no harm. However, health care workers do exactly that when they work with patients while ill themselves with contagious infections. Even common but untreatable infectious like enterovirus and respiratory syncytial virus can prove deadly to immunocompromised patients.
The propensity to work while ill is influenced by cultural trends. In past years, many ill physicians worked even to the point of receiving intravenous fluids while on the job; working while sick was regarded as a badge of courage. Dr. Szymczak and colleagues identified as an issue the absence of an effective sick relief system that has sufficient flexibility to “staff up” during high rates of health care worker illness. Sick relief systems and policies need to be clear regarding when health care workers should stay away from work, how patient coverage will be ensured, and the availability of and access to paid sick leave.
Determining what constitutes being too sick to work is complicated and lacks a sufficient evidence base. Using a system that bases work restrictions on the presence of key symptoms may add clarity and enable health care workers to recognize when they need to stay home.
Creating a safer and more equitable system of sick leave for health care workers requires a culture change in many institutions to decrease the stigma – internal and external – associated with health care worker illness. Identifying solutions to prioritize patient safety must factor in workforce demands and variability in patient census and emphasize flexibility. Strong administrative and physician leadership and creativity are essential to support appropriate sick leave and ensure adequate staffing. Hospital leadership must ensure that the culture supports a paid sick leave policy that is adequate and nonpunitive.
These comments are selected from an accompanying editorial (JAMA Pediatr. 2015 July 6 [doi:10.1001/jamapediatrics.2015.0994]), written by Dr. Jeffrey R. Starke of the department of pediatrics at Baylor College of Medicine in Houston, and Dr. Mary Anne Jackson of the division of infectious diseases at Children’s Mercy Hospital, University of Missouri–Kansas City. Dr. Starke and Dr. Jackson reported no disclosures.
For centuries, a guiding principle for health care workers has been primum non nocere, or first do no harm. However, health care workers do exactly that when they work with patients while ill themselves with contagious infections. Even common but untreatable infectious like enterovirus and respiratory syncytial virus can prove deadly to immunocompromised patients.
The propensity to work while ill is influenced by cultural trends. In past years, many ill physicians worked even to the point of receiving intravenous fluids while on the job; working while sick was regarded as a badge of courage. Dr. Szymczak and colleagues identified as an issue the absence of an effective sick relief system that has sufficient flexibility to “staff up” during high rates of health care worker illness. Sick relief systems and policies need to be clear regarding when health care workers should stay away from work, how patient coverage will be ensured, and the availability of and access to paid sick leave.
Determining what constitutes being too sick to work is complicated and lacks a sufficient evidence base. Using a system that bases work restrictions on the presence of key symptoms may add clarity and enable health care workers to recognize when they need to stay home.
Creating a safer and more equitable system of sick leave for health care workers requires a culture change in many institutions to decrease the stigma – internal and external – associated with health care worker illness. Identifying solutions to prioritize patient safety must factor in workforce demands and variability in patient census and emphasize flexibility. Strong administrative and physician leadership and creativity are essential to support appropriate sick leave and ensure adequate staffing. Hospital leadership must ensure that the culture supports a paid sick leave policy that is adequate and nonpunitive.
These comments are selected from an accompanying editorial (JAMA Pediatr. 2015 July 6 [doi:10.1001/jamapediatrics.2015.0994]), written by Dr. Jeffrey R. Starke of the department of pediatrics at Baylor College of Medicine in Houston, and Dr. Mary Anne Jackson of the division of infectious diseases at Children’s Mercy Hospital, University of Missouri–Kansas City. Dr. Starke and Dr. Jackson reported no disclosures.
The vast majority of doctors and other trained medical professionals at a hospital went to work while sick within the past year, even though they realized the risk that decision places on patients, according to a recent study.
In fact, almost 1 in 10 hospital clinicians worked while sick at least five times in the past year, primarily because of staffing concerns or not wanting to let colleagues down, reported Julia Szymczak, Ph.D., and her associates at the Children’s Hospital of Philadelphia (JAMA Pediatr. 2015 July 6 [doi: 10.1001/jamapediatrics.2015.0684]).
“A combination of closed- and open-ended questions illustrated that the decision to work while sick was shaped by systems-level and sociocultural factors that interacted to cause our respondents to work while symptomatic, despite recognizing that this choice may put patients and colleagues at risk,” the authors wrote.
Of 929 surveys sent out, 538 clinicians completed them, which included 280 of 459 physicians (61%) and 256 of 470 advanced-practice clinicians (54.5%). The advanced-practice clinicians included registered nurses, physician assistants, clinical nurse specialists, registered nurse anesthetists, and certified nurse midwives. Of those who responded, 15.7% worked in intensive care, 13.1% in surgery, 12.5% in general pediatrics, and 44.8% in another pediatric subspecialty.
Although 95.3% of respondents believed working while sick put patients at risk, 83.1% reported having done so at least once in the past year. Further, that proportion included 52% of all respondents who reported coming to work sick twice in the past year and 9.3% who worked while ill at least five times in the past year.
Nearly a third of respondents said they would work even if they had diarrhea (30%), while 16% said they would work with a fever, and 55.6% would work with acute respiratory symptoms, including cough, congestion, rhinorrhea, and sore throat.
But doctors were more likely than other professionals to say they would go to work with these symptoms: 38.9% of doctors would work despite diarrhea, compared with 19.9% of advanced-practice clinicians. Doctors and advanced-practice clinicians would also work with acute respiratory symptoms (60% vs. 50.8%, respectively), a fever only (21.8% vs. 9.8%), and fever and chills with body aches (18.6% vs. 10.9%, all P < .03).
Nearly every respondent (98.7%) said they worked despite being sick because they did not want to let their colleagues down, just as almost all of them worried the hospital would not have enough staff (94.9%) or that they would let their patients down (92.5%).
Smaller majorities of respondents also worked because others also work while sick (65%), worried their colleagues would ostracize them (64%) if they didn’t work, were concerned about their patients’ continuity of care (63.8%), had unsupportive leadership (56.2%), or believed they could not be easily replaced (52.6%).
Among the 316 respondents who filled in additional reasons, 64.9% said they had a very hard time finding someone to cover their shift, 61.1% described a strong cultural norm to work unless extremely sick, and 57% expressed uncertainty about what is considered “too sick to work.”
The Centers for Disease Control and Prevention funded the research. The authors reported no disclosures.
The vast majority of doctors and other trained medical professionals at a hospital went to work while sick within the past year, even though they realized the risk that decision places on patients, according to a recent study.
In fact, almost 1 in 10 hospital clinicians worked while sick at least five times in the past year, primarily because of staffing concerns or not wanting to let colleagues down, reported Julia Szymczak, Ph.D., and her associates at the Children’s Hospital of Philadelphia (JAMA Pediatr. 2015 July 6 [doi: 10.1001/jamapediatrics.2015.0684]).
“A combination of closed- and open-ended questions illustrated that the decision to work while sick was shaped by systems-level and sociocultural factors that interacted to cause our respondents to work while symptomatic, despite recognizing that this choice may put patients and colleagues at risk,” the authors wrote.
Of 929 surveys sent out, 538 clinicians completed them, which included 280 of 459 physicians (61%) and 256 of 470 advanced-practice clinicians (54.5%). The advanced-practice clinicians included registered nurses, physician assistants, clinical nurse specialists, registered nurse anesthetists, and certified nurse midwives. Of those who responded, 15.7% worked in intensive care, 13.1% in surgery, 12.5% in general pediatrics, and 44.8% in another pediatric subspecialty.
Although 95.3% of respondents believed working while sick put patients at risk, 83.1% reported having done so at least once in the past year. Further, that proportion included 52% of all respondents who reported coming to work sick twice in the past year and 9.3% who worked while ill at least five times in the past year.
Nearly a third of respondents said they would work even if they had diarrhea (30%), while 16% said they would work with a fever, and 55.6% would work with acute respiratory symptoms, including cough, congestion, rhinorrhea, and sore throat.
But doctors were more likely than other professionals to say they would go to work with these symptoms: 38.9% of doctors would work despite diarrhea, compared with 19.9% of advanced-practice clinicians. Doctors and advanced-practice clinicians would also work with acute respiratory symptoms (60% vs. 50.8%, respectively), a fever only (21.8% vs. 9.8%), and fever and chills with body aches (18.6% vs. 10.9%, all P < .03).
Nearly every respondent (98.7%) said they worked despite being sick because they did not want to let their colleagues down, just as almost all of them worried the hospital would not have enough staff (94.9%) or that they would let their patients down (92.5%).
Smaller majorities of respondents also worked because others also work while sick (65%), worried their colleagues would ostracize them (64%) if they didn’t work, were concerned about their patients’ continuity of care (63.8%), had unsupportive leadership (56.2%), or believed they could not be easily replaced (52.6%).
Among the 316 respondents who filled in additional reasons, 64.9% said they had a very hard time finding someone to cover their shift, 61.1% described a strong cultural norm to work unless extremely sick, and 57% expressed uncertainty about what is considered “too sick to work.”
The Centers for Disease Control and Prevention funded the research. The authors reported no disclosures.
FROM PEDIATRICS
Key clinical point: A majority of hospital doctors and other clinicians work while sick.
Major finding: 83.1% of doctors and advanced-practice clinicians worked while ill at least once in the past year; 95.3% recognized the risk to patients and colleagues.
Data source: The findings are based on a cross-sectional, anonymous survey of 280 attending physicians and 256 advanced-practice clinicians at the Children’s Hospital of Philadelphia from January 2014 to March 2014.
Disclosures: The research was funded by the Centers for Disease Control and Prevention. The authors reported no disclosures.
DDW: LINX device beneficial, safe for GERD
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
AT DDW 2015
Key clinical point: A magnetic device designed to augment the lower esophageal sphincter is a surgical option that can be expected to provide long-term control of reflux symptoms in patients with GERD.
Major finding: Improvements 5 years after treatment with the Linx Reflux Management System include a drop from 60% experiencing regurgitation to 1%, and two-third of patients no longer taking PPIs.
Data source: The multicenter, prospective study evaluated the long-term safety and efficacy of the device over 5 years in 100 patients with GERD, who served as their own controls; 85 were included in the 5-year follow-up.
Disclosures: The study was funded by the device manufacturer, Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
Bariatric surgery beats lifestyle changes alone for type 2 diabetes
Among obese patients who underwent bariatric surgery 40% achieved at least partial remission of type 2 diabetes mellitus, compared with no patients who underwent a nonsurgical lifestyle intervention program, investigators reported online July 1 in JAMA Surgery.
The randomized clinical trial of 61 patients offers “further important evidence that at longer-term follow-up of 3 years, surgical treatments, including Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding, are superior to lifestyle intervention alone for the remission of type 2 diabetes mellitus in obese individuals, including those with a body mass index (BMI) between 30 and 35 [kg/m2],” said Dr. Anita Courcoulas at the University of Pittsburgh Medical Center and her associates. But further studies will be needed to explore exactly how bariatric surgery affects diabetes and the effect of these procedures on the microvascular and macrovascular complications of diabetes, the investigators added (JAMA Surg. 2015 July 1 [doi:10.1001/jamasurg.2015.1534]).
Several studies have reported major improvements in type 2 diabetes mellitus (T2DM) after bariatric surgery, but did not assess long-term efficacy or safety compared with lifestyle and medical management, the researchers noted. To fill that gap, they randomized obese middle-aged adults with T2DM to either an intensive lifestyle weight loss program for 1 year followed by a 2-year low-level lifestyle intervention program, or to Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB) followed by the low-level lifestyle intervention program during years 2 and 3.
After 3 years, 40% of RYGB patients and 29% of LAGB patients were fully or partially remitted, compared with none of the control group (P = .004), the investigators reported. The bariatric surgery groups did not significantly differ in terms of complete remission, but 65% of RYGB patients and 33% of LAGB patients were able to stop all insulin and oral diabetes medications, compared with none of the control group (P < .001). Also, RYGB patients lost an average of 25% of their baseline body weight, compared with 15% for LAGB (P = .0002) and only 5.7% for the lifestyle-only control group (P < .0001).
At baseline, patients averaged 100.5 kg (standard deviation, 13.7 kg) in body weight, mean hemoglobin A1c level was 7.8% (standard deviation, 1.9%), average fasting plasma glucose level was 171.3 (72.5) mg per dL, the investigators said. “One important aspect of this study was that more than 40% of the sample were individuals with class I obesity (BMI ≥ 30), for whom data in the literature are largely lacking,” they added. Adverse events were uncommon after the first year, but RYGB was linked to significant drops in lean muscle and bone mass that will need further study, they noted.
The National Institutes of Health and the University of Pittsburgh Medical Center funded the study. Dr. Courcoulas reported research support from Nutrisystem, J&J Ethicon, and Covidien, and consulting relationships with Ethicon and Apollo Endosurgery. Two coauthors reported relationships with the Obesity Society/Nutrisystem, Jawbone/BodyMedia, and Weight Watchers. The other investigators declared no conflicts of interest.
We should consider the use of bariatric (metabolic) surgery in all severely obese patients with type 2 diabetes mellitus and start a mass treatment, similar to what was done with coronary artery bypass graft more than 50 years ago.
[The study findings are] reminiscent of the Swedish Obesity Study, a nonrandomized study of 1,658 obese patients who underwent bariatric surgery and 1,771 obese matched controls. None of these participants had diabetes mellitus at baseline. After 15 years, T2DM developed in 6.8 cases per 1,000 person-years and 28.4 cases per 1,000 person-years, respectively (P < .001). The effect of surgery was influenced by the presence of impaired fasting glucose, but not by body mass index. It was concluded that surgery appeared to be more efficient than the control [lifestyle intervention] in the prevention of T2DM.
In the Look AHEAD clinical trial, an intensive lifestyle intervention for weight loss was examined to determine the impact on cardiovascular events. The trial was stopped early based on a futility analysis. … Similarly, the TODAY clinical trial on adolescents with recent-onset T2DM demonstrated no benefits of intensive lifestyle intervention.
If surgery is more successful for these patients, which surgery should be done? It has been shown that malabsorption is better than restriction. … In a randomized clinical trial [of] severely obese patients with T2DM, at 2 years, diabetic remission occurred in none of the medical therapy patients versus 75% of the gastric bypass group and 95% of the biliary pancreatic diversion group (P < .001).
Dr. Michael Gagner is at Florida International University in Miami. He reported receiving honoraria from Ethicon, Covidien, Fore, MID, Olympus, and Boehringer Laboratories, and equity from Transenterix. These remarks are based on his accompanying editorial (JAMA Surg. 2015 July 1 [doi: 10.1001/jamasurg.2015.1542]).
We should consider the use of bariatric (metabolic) surgery in all severely obese patients with type 2 diabetes mellitus and start a mass treatment, similar to what was done with coronary artery bypass graft more than 50 years ago.
[The study findings are] reminiscent of the Swedish Obesity Study, a nonrandomized study of 1,658 obese patients who underwent bariatric surgery and 1,771 obese matched controls. None of these participants had diabetes mellitus at baseline. After 15 years, T2DM developed in 6.8 cases per 1,000 person-years and 28.4 cases per 1,000 person-years, respectively (P < .001). The effect of surgery was influenced by the presence of impaired fasting glucose, but not by body mass index. It was concluded that surgery appeared to be more efficient than the control [lifestyle intervention] in the prevention of T2DM.
In the Look AHEAD clinical trial, an intensive lifestyle intervention for weight loss was examined to determine the impact on cardiovascular events. The trial was stopped early based on a futility analysis. … Similarly, the TODAY clinical trial on adolescents with recent-onset T2DM demonstrated no benefits of intensive lifestyle intervention.
If surgery is more successful for these patients, which surgery should be done? It has been shown that malabsorption is better than restriction. … In a randomized clinical trial [of] severely obese patients with T2DM, at 2 years, diabetic remission occurred in none of the medical therapy patients versus 75% of the gastric bypass group and 95% of the biliary pancreatic diversion group (P < .001).
Dr. Michael Gagner is at Florida International University in Miami. He reported receiving honoraria from Ethicon, Covidien, Fore, MID, Olympus, and Boehringer Laboratories, and equity from Transenterix. These remarks are based on his accompanying editorial (JAMA Surg. 2015 July 1 [doi: 10.1001/jamasurg.2015.1542]).
We should consider the use of bariatric (metabolic) surgery in all severely obese patients with type 2 diabetes mellitus and start a mass treatment, similar to what was done with coronary artery bypass graft more than 50 years ago.
[The study findings are] reminiscent of the Swedish Obesity Study, a nonrandomized study of 1,658 obese patients who underwent bariatric surgery and 1,771 obese matched controls. None of these participants had diabetes mellitus at baseline. After 15 years, T2DM developed in 6.8 cases per 1,000 person-years and 28.4 cases per 1,000 person-years, respectively (P < .001). The effect of surgery was influenced by the presence of impaired fasting glucose, but not by body mass index. It was concluded that surgery appeared to be more efficient than the control [lifestyle intervention] in the prevention of T2DM.
In the Look AHEAD clinical trial, an intensive lifestyle intervention for weight loss was examined to determine the impact on cardiovascular events. The trial was stopped early based on a futility analysis. … Similarly, the TODAY clinical trial on adolescents with recent-onset T2DM demonstrated no benefits of intensive lifestyle intervention.
If surgery is more successful for these patients, which surgery should be done? It has been shown that malabsorption is better than restriction. … In a randomized clinical trial [of] severely obese patients with T2DM, at 2 years, diabetic remission occurred in none of the medical therapy patients versus 75% of the gastric bypass group and 95% of the biliary pancreatic diversion group (P < .001).
Dr. Michael Gagner is at Florida International University in Miami. He reported receiving honoraria from Ethicon, Covidien, Fore, MID, Olympus, and Boehringer Laboratories, and equity from Transenterix. These remarks are based on his accompanying editorial (JAMA Surg. 2015 July 1 [doi: 10.1001/jamasurg.2015.1542]).
Among obese patients who underwent bariatric surgery 40% achieved at least partial remission of type 2 diabetes mellitus, compared with no patients who underwent a nonsurgical lifestyle intervention program, investigators reported online July 1 in JAMA Surgery.
The randomized clinical trial of 61 patients offers “further important evidence that at longer-term follow-up of 3 years, surgical treatments, including Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding, are superior to lifestyle intervention alone for the remission of type 2 diabetes mellitus in obese individuals, including those with a body mass index (BMI) between 30 and 35 [kg/m2],” said Dr. Anita Courcoulas at the University of Pittsburgh Medical Center and her associates. But further studies will be needed to explore exactly how bariatric surgery affects diabetes and the effect of these procedures on the microvascular and macrovascular complications of diabetes, the investigators added (JAMA Surg. 2015 July 1 [doi:10.1001/jamasurg.2015.1534]).
Several studies have reported major improvements in type 2 diabetes mellitus (T2DM) after bariatric surgery, but did not assess long-term efficacy or safety compared with lifestyle and medical management, the researchers noted. To fill that gap, they randomized obese middle-aged adults with T2DM to either an intensive lifestyle weight loss program for 1 year followed by a 2-year low-level lifestyle intervention program, or to Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB) followed by the low-level lifestyle intervention program during years 2 and 3.
After 3 years, 40% of RYGB patients and 29% of LAGB patients were fully or partially remitted, compared with none of the control group (P = .004), the investigators reported. The bariatric surgery groups did not significantly differ in terms of complete remission, but 65% of RYGB patients and 33% of LAGB patients were able to stop all insulin and oral diabetes medications, compared with none of the control group (P < .001). Also, RYGB patients lost an average of 25% of their baseline body weight, compared with 15% for LAGB (P = .0002) and only 5.7% for the lifestyle-only control group (P < .0001).
At baseline, patients averaged 100.5 kg (standard deviation, 13.7 kg) in body weight, mean hemoglobin A1c level was 7.8% (standard deviation, 1.9%), average fasting plasma glucose level was 171.3 (72.5) mg per dL, the investigators said. “One important aspect of this study was that more than 40% of the sample were individuals with class I obesity (BMI ≥ 30), for whom data in the literature are largely lacking,” they added. Adverse events were uncommon after the first year, but RYGB was linked to significant drops in lean muscle and bone mass that will need further study, they noted.
The National Institutes of Health and the University of Pittsburgh Medical Center funded the study. Dr. Courcoulas reported research support from Nutrisystem, J&J Ethicon, and Covidien, and consulting relationships with Ethicon and Apollo Endosurgery. Two coauthors reported relationships with the Obesity Society/Nutrisystem, Jawbone/BodyMedia, and Weight Watchers. The other investigators declared no conflicts of interest.
Among obese patients who underwent bariatric surgery 40% achieved at least partial remission of type 2 diabetes mellitus, compared with no patients who underwent a nonsurgical lifestyle intervention program, investigators reported online July 1 in JAMA Surgery.
The randomized clinical trial of 61 patients offers “further important evidence that at longer-term follow-up of 3 years, surgical treatments, including Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding, are superior to lifestyle intervention alone for the remission of type 2 diabetes mellitus in obese individuals, including those with a body mass index (BMI) between 30 and 35 [kg/m2],” said Dr. Anita Courcoulas at the University of Pittsburgh Medical Center and her associates. But further studies will be needed to explore exactly how bariatric surgery affects diabetes and the effect of these procedures on the microvascular and macrovascular complications of diabetes, the investigators added (JAMA Surg. 2015 July 1 [doi:10.1001/jamasurg.2015.1534]).
Several studies have reported major improvements in type 2 diabetes mellitus (T2DM) after bariatric surgery, but did not assess long-term efficacy or safety compared with lifestyle and medical management, the researchers noted. To fill that gap, they randomized obese middle-aged adults with T2DM to either an intensive lifestyle weight loss program for 1 year followed by a 2-year low-level lifestyle intervention program, or to Roux-en-Y gastric bypass (RYGB) or laparoscopic adjustable gastric banding (LAGB) followed by the low-level lifestyle intervention program during years 2 and 3.
After 3 years, 40% of RYGB patients and 29% of LAGB patients were fully or partially remitted, compared with none of the control group (P = .004), the investigators reported. The bariatric surgery groups did not significantly differ in terms of complete remission, but 65% of RYGB patients and 33% of LAGB patients were able to stop all insulin and oral diabetes medications, compared with none of the control group (P < .001). Also, RYGB patients lost an average of 25% of their baseline body weight, compared with 15% for LAGB (P = .0002) and only 5.7% for the lifestyle-only control group (P < .0001).
At baseline, patients averaged 100.5 kg (standard deviation, 13.7 kg) in body weight, mean hemoglobin A1c level was 7.8% (standard deviation, 1.9%), average fasting plasma glucose level was 171.3 (72.5) mg per dL, the investigators said. “One important aspect of this study was that more than 40% of the sample were individuals with class I obesity (BMI ≥ 30), for whom data in the literature are largely lacking,” they added. Adverse events were uncommon after the first year, but RYGB was linked to significant drops in lean muscle and bone mass that will need further study, they noted.
The National Institutes of Health and the University of Pittsburgh Medical Center funded the study. Dr. Courcoulas reported research support from Nutrisystem, J&J Ethicon, and Covidien, and consulting relationships with Ethicon and Apollo Endosurgery. Two coauthors reported relationships with the Obesity Society/Nutrisystem, Jawbone/BodyMedia, and Weight Watchers. The other investigators declared no conflicts of interest.
FROM JAMA SURGERY
Key clinical point: Bariatric surgery, especially Roux-en-Y gastric bypass, led to significant improvements in type 2 diabetes mellitus, compared with lifestyle changes alone.
Major finding: At year 3, 40% of RYGB patients and 29% of LAGB patients were fully or partially remitted, compared with none of the nonsurgical control group (P = .004).
Data source: Randomized, parallel-group clinical trial of 61 obese adults with type 2 diabetes mellitus.
Disclosures: The National Institutes of Health and the University of Pittsburgh Medical Center funded the study. Dr. Courcoulas reported research support from Nutrisystem, J&J Ethicon, and Covidien, and consulting relationships with Ethicon and Apollo Endosurgery. Two coauthors reported relationships with the Obesity Society/Nutrisystem, Jawbone/BodyMedia, and Weight Watchers. The other investigators declared no conflicts of interest.
Cefazolin ranks sixth as cause of drug-induced liver injury
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A single dose of cefazolin can cause drug-induced liver injury (DILI), and the agent is implicated more often than previously thought.
Major finding: Cefazolin ranked sixth among causes of DILI, and signs and symptoms began 1-3 weeks after initial exposure.
Data source: Registry-based study of 1,212 cases of DILI.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
Commentary: Molecular marker testing for diagnosis and prognosis – Where are we really?
An emerging market of molecular markers for thyroid cancer diagnostic and prognostic evaluation challenges current medical and surgical management; however, here is a strong word of caution; Unless the markers have been tested in the context of clinical and surgical management their true efficacy has not been accurately assessed.
We must always ask two questions before ordering these tests that can cost more than $3,000: 1) Does the use of a molecular test add any additional information that would otherwise change our recommendations; in other words, is the clinical information already known enough for appropriate clinical decision making? 2) What is the basis upon which recommendations for its use have been made; in other words, how were the studies conducted and interpreted? Are they valid?
By way of background, the gene expression clarifier (GEC) Afirma is marketed as a diagnostic tool for the differential diagnosis of indeterminate thyroid cytology (atypical cells of undetermined significance or follicular neoplasm, Bethesda categories III and IV, respectively).
Most importantly, it has been tested and is marketed as a negative predictor only. It is also only useful if used in the appropriate setting and if the test result is negative; a positive Afirma test can tell us only that the nodule is indeterminate, something, by definition, already determined by fine needle aspiration (FNA). Furthermore, any study examining its efficacy must be conducted within the context of clinical scenarios. For example, for a patient with an indeterminate lesion and a symptomatic multinodular goiter, neither a negative nor positive Afirma result would have any impact on surgical decision making and yet would have cost the patient more than $3,000. The latter patient simply needs a thyroidectomy. A patient who has a nodule that is approaching 4 cm or is increasing in size or a patient who has undergone several FNAs, ultrasounds, and endocrinology consultations similarly would likely choose surgery regardless of the GEC test result.
The only scenario in which Afirma testing is useful is in a patient with otherwise no indications for surgery except an indeterminate FNA; for instance for a patient with an asymptomatic < 4cm, stable, single nodule. In this scenario only a negative result could be helpful and would obviate the need for surgical intervention. One also must ask what is the likelihood of the patient undergoing repeat FNA, having repeat indeterminate cytology and repeat Afirma testing over the ensuing years and at what point should we consider these costs prohibitive compared with the patient undergoing a thyroidectomy instead?
Similar concerns exist with regard to somatic mutation panels, the most commonly marketed and used being Asuragen. The mutation panel consists of Ras and BRAF mutation and RET/PTC and PAX8/PPAR-gamma chromosomal rearrangement analyses. Importantly, the expanding literature on molecular markers for thyroid cancer, however, has lost track of a vast body of literature that reports Ras mutations present in up to 30% of benign thyroid nodules; RET/PTC in 24% and PAX8/PPAR-gamma in 14%, dramatically challenging the validity of the panel purported to accurately identify thyroid malignancy. We know that BRAF mutation is exclusively found in papillary thyroid cancer, but generally a BRAF-positive tumor is one in which a cytological diagnosis is already clear; it is either suspicious or definitively malignant on FNA. One might suggest that these aforementioned markers might indicate a harbinger of malignancy or identify a precancerous lesion; however, there is no study that supports this theory. Furthermore, it is important to note that even among pathology experts the diagnoses of follicular adenoma, follicular cancer, and follicular variant of papillary thyroid cancer have significant and documented inter- and intra- observer variability, thus challenging the gold standard upon which these markers have been tested.
With regard to BRAF, Ras, RET/PTC and PAX8/PPAR-gamma as prognostic markers there are many considerations, the least of which includes the differential diagnosis of follicular lesions addressed above and the known presence of these abnormalities in benign tumors. The majority of studies to date have conducted only univariate analyses without consideration of the clinical variables already available to us to make needed clinical decisions. In order to examine the usefulness of any marker panel a multivariable study is required, incorporating the available clinical variables such as size, lymph node metastases, and extra-thyroidal extension. For instance, the majority of studies examining the presence of lymph node metastases in BRAF-negative vs. BRAF-positive tumors were almost uniformly conducted on patients in whom routine lymph node dissection was not performed, thereby skewing the results. Only patients with suspicious nodes underwent a lymph node dissection; thus for those patients who had no suspicious nodes there was no information about their nodal status. Furthermore, several studies that included patients who underwent routine lymph node dissections and, importantly, included patients who underwent prophylactic dissections for whom a marker would be most useful, did not find that BRAF mutation was associated with aggressive features, including the presence of lymph node metastases. The same can be stated for a panel that includes Ras, RET/PTC, & PAX8/PPAR-gamma. “Follicular variant of papillary thyroid cancer and follicular cancer” will more likely harbor Ras and PAX8/PPAR-gamma mutations and will, by definition, include some tumors that would be considered benign by other pathologists.
There is an emerging market for molecular markers for thyroid cancer diagnosis and prognosis, but many of the studies driving this market are lacking in scientific rigor with regard to design and interpretation of results. Furthermore, the use of the marker panel requires scrutiny of its true impact on clinical management as well as its cost-effectiveness. GEC provides a negative predictor of malignancy and should be used to obviate surgery only; if the patient requires surgery its use provides no added information. BRAF is specific for thyroid cancer diagnosis, but is often not required as FNA evaluation in BRAF-positive tumors is usually already suspicious or malignant. Finally, molecular marker panels for thyroid cancer prognosis may be promising, but scrutiny for true accuracy and true clinical impact is necessary in order to make logical and useful recommendations for our patients.
Dr. Zeiger is professor of surgery, oncology, cellular, and molecular medicine, associate vice chair for faculty development, and associate dean for postdoctoral affairs at Johns Hopkins University in Baltimore. Dr. Zeiger consults for Interpace Diagnostics.
An emerging market of molecular markers for thyroid cancer diagnostic and prognostic evaluation challenges current medical and surgical management; however, here is a strong word of caution; Unless the markers have been tested in the context of clinical and surgical management their true efficacy has not been accurately assessed.
We must always ask two questions before ordering these tests that can cost more than $3,000: 1) Does the use of a molecular test add any additional information that would otherwise change our recommendations; in other words, is the clinical information already known enough for appropriate clinical decision making? 2) What is the basis upon which recommendations for its use have been made; in other words, how were the studies conducted and interpreted? Are they valid?
By way of background, the gene expression clarifier (GEC) Afirma is marketed as a diagnostic tool for the differential diagnosis of indeterminate thyroid cytology (atypical cells of undetermined significance or follicular neoplasm, Bethesda categories III and IV, respectively).
Most importantly, it has been tested and is marketed as a negative predictor only. It is also only useful if used in the appropriate setting and if the test result is negative; a positive Afirma test can tell us only that the nodule is indeterminate, something, by definition, already determined by fine needle aspiration (FNA). Furthermore, any study examining its efficacy must be conducted within the context of clinical scenarios. For example, for a patient with an indeterminate lesion and a symptomatic multinodular goiter, neither a negative nor positive Afirma result would have any impact on surgical decision making and yet would have cost the patient more than $3,000. The latter patient simply needs a thyroidectomy. A patient who has a nodule that is approaching 4 cm or is increasing in size or a patient who has undergone several FNAs, ultrasounds, and endocrinology consultations similarly would likely choose surgery regardless of the GEC test result.
The only scenario in which Afirma testing is useful is in a patient with otherwise no indications for surgery except an indeterminate FNA; for instance for a patient with an asymptomatic < 4cm, stable, single nodule. In this scenario only a negative result could be helpful and would obviate the need for surgical intervention. One also must ask what is the likelihood of the patient undergoing repeat FNA, having repeat indeterminate cytology and repeat Afirma testing over the ensuing years and at what point should we consider these costs prohibitive compared with the patient undergoing a thyroidectomy instead?
Similar concerns exist with regard to somatic mutation panels, the most commonly marketed and used being Asuragen. The mutation panel consists of Ras and BRAF mutation and RET/PTC and PAX8/PPAR-gamma chromosomal rearrangement analyses. Importantly, the expanding literature on molecular markers for thyroid cancer, however, has lost track of a vast body of literature that reports Ras mutations present in up to 30% of benign thyroid nodules; RET/PTC in 24% and PAX8/PPAR-gamma in 14%, dramatically challenging the validity of the panel purported to accurately identify thyroid malignancy. We know that BRAF mutation is exclusively found in papillary thyroid cancer, but generally a BRAF-positive tumor is one in which a cytological diagnosis is already clear; it is either suspicious or definitively malignant on FNA. One might suggest that these aforementioned markers might indicate a harbinger of malignancy or identify a precancerous lesion; however, there is no study that supports this theory. Furthermore, it is important to note that even among pathology experts the diagnoses of follicular adenoma, follicular cancer, and follicular variant of papillary thyroid cancer have significant and documented inter- and intra- observer variability, thus challenging the gold standard upon which these markers have been tested.
With regard to BRAF, Ras, RET/PTC and PAX8/PPAR-gamma as prognostic markers there are many considerations, the least of which includes the differential diagnosis of follicular lesions addressed above and the known presence of these abnormalities in benign tumors. The majority of studies to date have conducted only univariate analyses without consideration of the clinical variables already available to us to make needed clinical decisions. In order to examine the usefulness of any marker panel a multivariable study is required, incorporating the available clinical variables such as size, lymph node metastases, and extra-thyroidal extension. For instance, the majority of studies examining the presence of lymph node metastases in BRAF-negative vs. BRAF-positive tumors were almost uniformly conducted on patients in whom routine lymph node dissection was not performed, thereby skewing the results. Only patients with suspicious nodes underwent a lymph node dissection; thus for those patients who had no suspicious nodes there was no information about their nodal status. Furthermore, several studies that included patients who underwent routine lymph node dissections and, importantly, included patients who underwent prophylactic dissections for whom a marker would be most useful, did not find that BRAF mutation was associated with aggressive features, including the presence of lymph node metastases. The same can be stated for a panel that includes Ras, RET/PTC, & PAX8/PPAR-gamma. “Follicular variant of papillary thyroid cancer and follicular cancer” will more likely harbor Ras and PAX8/PPAR-gamma mutations and will, by definition, include some tumors that would be considered benign by other pathologists.
There is an emerging market for molecular markers for thyroid cancer diagnosis and prognosis, but many of the studies driving this market are lacking in scientific rigor with regard to design and interpretation of results. Furthermore, the use of the marker panel requires scrutiny of its true impact on clinical management as well as its cost-effectiveness. GEC provides a negative predictor of malignancy and should be used to obviate surgery only; if the patient requires surgery its use provides no added information. BRAF is specific for thyroid cancer diagnosis, but is often not required as FNA evaluation in BRAF-positive tumors is usually already suspicious or malignant. Finally, molecular marker panels for thyroid cancer prognosis may be promising, but scrutiny for true accuracy and true clinical impact is necessary in order to make logical and useful recommendations for our patients.
Dr. Zeiger is professor of surgery, oncology, cellular, and molecular medicine, associate vice chair for faculty development, and associate dean for postdoctoral affairs at Johns Hopkins University in Baltimore. Dr. Zeiger consults for Interpace Diagnostics.
An emerging market of molecular markers for thyroid cancer diagnostic and prognostic evaluation challenges current medical and surgical management; however, here is a strong word of caution; Unless the markers have been tested in the context of clinical and surgical management their true efficacy has not been accurately assessed.
We must always ask two questions before ordering these tests that can cost more than $3,000: 1) Does the use of a molecular test add any additional information that would otherwise change our recommendations; in other words, is the clinical information already known enough for appropriate clinical decision making? 2) What is the basis upon which recommendations for its use have been made; in other words, how were the studies conducted and interpreted? Are they valid?
By way of background, the gene expression clarifier (GEC) Afirma is marketed as a diagnostic tool for the differential diagnosis of indeterminate thyroid cytology (atypical cells of undetermined significance or follicular neoplasm, Bethesda categories III and IV, respectively).
Most importantly, it has been tested and is marketed as a negative predictor only. It is also only useful if used in the appropriate setting and if the test result is negative; a positive Afirma test can tell us only that the nodule is indeterminate, something, by definition, already determined by fine needle aspiration (FNA). Furthermore, any study examining its efficacy must be conducted within the context of clinical scenarios. For example, for a patient with an indeterminate lesion and a symptomatic multinodular goiter, neither a negative nor positive Afirma result would have any impact on surgical decision making and yet would have cost the patient more than $3,000. The latter patient simply needs a thyroidectomy. A patient who has a nodule that is approaching 4 cm or is increasing in size or a patient who has undergone several FNAs, ultrasounds, and endocrinology consultations similarly would likely choose surgery regardless of the GEC test result.
The only scenario in which Afirma testing is useful is in a patient with otherwise no indications for surgery except an indeterminate FNA; for instance for a patient with an asymptomatic < 4cm, stable, single nodule. In this scenario only a negative result could be helpful and would obviate the need for surgical intervention. One also must ask what is the likelihood of the patient undergoing repeat FNA, having repeat indeterminate cytology and repeat Afirma testing over the ensuing years and at what point should we consider these costs prohibitive compared with the patient undergoing a thyroidectomy instead?
Similar concerns exist with regard to somatic mutation panels, the most commonly marketed and used being Asuragen. The mutation panel consists of Ras and BRAF mutation and RET/PTC and PAX8/PPAR-gamma chromosomal rearrangement analyses. Importantly, the expanding literature on molecular markers for thyroid cancer, however, has lost track of a vast body of literature that reports Ras mutations present in up to 30% of benign thyroid nodules; RET/PTC in 24% and PAX8/PPAR-gamma in 14%, dramatically challenging the validity of the panel purported to accurately identify thyroid malignancy. We know that BRAF mutation is exclusively found in papillary thyroid cancer, but generally a BRAF-positive tumor is one in which a cytological diagnosis is already clear; it is either suspicious or definitively malignant on FNA. One might suggest that these aforementioned markers might indicate a harbinger of malignancy or identify a precancerous lesion; however, there is no study that supports this theory. Furthermore, it is important to note that even among pathology experts the diagnoses of follicular adenoma, follicular cancer, and follicular variant of papillary thyroid cancer have significant and documented inter- and intra- observer variability, thus challenging the gold standard upon which these markers have been tested.
With regard to BRAF, Ras, RET/PTC and PAX8/PPAR-gamma as prognostic markers there are many considerations, the least of which includes the differential diagnosis of follicular lesions addressed above and the known presence of these abnormalities in benign tumors. The majority of studies to date have conducted only univariate analyses without consideration of the clinical variables already available to us to make needed clinical decisions. In order to examine the usefulness of any marker panel a multivariable study is required, incorporating the available clinical variables such as size, lymph node metastases, and extra-thyroidal extension. For instance, the majority of studies examining the presence of lymph node metastases in BRAF-negative vs. BRAF-positive tumors were almost uniformly conducted on patients in whom routine lymph node dissection was not performed, thereby skewing the results. Only patients with suspicious nodes underwent a lymph node dissection; thus for those patients who had no suspicious nodes there was no information about their nodal status. Furthermore, several studies that included patients who underwent routine lymph node dissections and, importantly, included patients who underwent prophylactic dissections for whom a marker would be most useful, did not find that BRAF mutation was associated with aggressive features, including the presence of lymph node metastases. The same can be stated for a panel that includes Ras, RET/PTC, & PAX8/PPAR-gamma. “Follicular variant of papillary thyroid cancer and follicular cancer” will more likely harbor Ras and PAX8/PPAR-gamma mutations and will, by definition, include some tumors that would be considered benign by other pathologists.
There is an emerging market for molecular markers for thyroid cancer diagnosis and prognosis, but many of the studies driving this market are lacking in scientific rigor with regard to design and interpretation of results. Furthermore, the use of the marker panel requires scrutiny of its true impact on clinical management as well as its cost-effectiveness. GEC provides a negative predictor of malignancy and should be used to obviate surgery only; if the patient requires surgery its use provides no added information. BRAF is specific for thyroid cancer diagnosis, but is often not required as FNA evaluation in BRAF-positive tumors is usually already suspicious or malignant. Finally, molecular marker panels for thyroid cancer prognosis may be promising, but scrutiny for true accuracy and true clinical impact is necessary in order to make logical and useful recommendations for our patients.
Dr. Zeiger is professor of surgery, oncology, cellular, and molecular medicine, associate vice chair for faculty development, and associate dean for postdoctoral affairs at Johns Hopkins University in Baltimore. Dr. Zeiger consults for Interpace Diagnostics.
Surgical bleeding risk ‘remarkable’ with platelet disorders
VIENNA – Inherited platelet function disorders are associated with a significant bleeding risk during surgery, a retrospective, multicenter study shows.
“The frequency of excessive bleeding assessed by one of three criteria at surgery is pretty remarkable because we had rates ranging from 13% to about 19% depending on the assessment criteria,” Dr. Paolo Gresele said at the annual congress of the European Hematology Association.
Any excessive bleeding by any criteria took place in about 23% of patients.
Although conventionally considered rare, inherited platelet function disorders (IPFD) are more frequent than previously thought, and recent advances in their diagnosis have expanded the forms and number of reported patients.
Only a handful of case reports or small case series have evaluated the bleeding risk associated with surgery in patients with IPFD. As a result, the exact bleeding risk and most appropriate management options in IPFD are not known, Dr. Gresele of University of Perugia (Italy) said.
He reported on a retrospective study involving patients with IPFD enrolled at 42 centers from 16 countries. The median age of the 205 patients was 35 years, and 56% were women; 89 had Glanzmann thrombasthenia, 46 had primary secretion defect, 14 had combined alpha-delta granule deficiency, 11 had Hermansky-Pudlak syndrome, 9 had gray platelet syndrome, and 36 had other forms of IPFD.
Data were collected from 389 procedures, of which 54.5% were surgeries, 30% were dental procedures, and 15.5% were invasive procedures. The most frequent surgeries were otolaryngologic, abdominal, orthopedic, gynecologic, urologic, and dermatologic.
The frequency of excessive bleeding at surgery was about 19.7% by the Bleeding Academic Research Consortium (BARC) bleeding classification, 17% by subjective evaluation by the surgeon or patient, and 13% based on duration of bleeding at surgery of at least 6 or more hours, Dr. Gresele said.
The World Health Organization (WHO) bleeding scale before surgery was quite predictive of excessive bleeding at surgery, with patients at grade 3 and 4 having an odds ratio for excessive bleeding of 9.22 and 28, respectively, compared with patients at grade 0, he said.
Somewhat unexpectedly, the most serious bleeders based on a BARC of at least 2 or more at surgery were patients with Hermansky-Pudlak syndrome, Glanzmann thrombasthenia, and gray platelet syndrome. Those with primary secretion defect and combined alpha-delta granule deficiency had a relatively low risk of bleeding at surgery, he said.
The procedures associated with more excessive bleeding were urologic surgery, gynecologic surgery, and abdominal surgery.
Preparation for surgery was made in 82% of procedures and included prophylactic platelet transfusions in 38.5%, desmopressin (DDAVP) in about 19%, antifibrinolytic agents in about 12%, factor VIIa in less than 10%, and other interventions such as cryoprecipitate, fibrinogen, fresh frozen plasma, intravenous immunoglobulin, suture, and local hemostatic agent in less than 5%.
Generally all measures had a good ability to prevent excessive bleeding, bringing rates down to about 20% or less, Dr. Gresele said. The two exceptions were no prophylaxis and “other” interventions, where the bleeding rate reached a high of about 45% for the latter. In contrast, bleeding risk was significantly reduced when any prophylaxis (odds ratio, 0.38) or DDAVP (OR, 0.24) were used.
In 87 cases, however, emergency treatment for excessive bleeding was required, he said. Platelet transfusions were the most common treatment, given in roughly half of patients, followed by antifibrinolytic agents. The success rate was about 80% for all measures, except for “other” interventions, which had a success rate of about 65%.
“Treatment of excessive bleeding is made mostly with platelet transfusions or antifibrinolytic agents and is able to stop bleeding in many, but not all cases,” Dr. Gresele concluded.
On Twitter @pwendl
VIENNA – Inherited platelet function disorders are associated with a significant bleeding risk during surgery, a retrospective, multicenter study shows.
“The frequency of excessive bleeding assessed by one of three criteria at surgery is pretty remarkable because we had rates ranging from 13% to about 19% depending on the assessment criteria,” Dr. Paolo Gresele said at the annual congress of the European Hematology Association.
Any excessive bleeding by any criteria took place in about 23% of patients.
Although conventionally considered rare, inherited platelet function disorders (IPFD) are more frequent than previously thought, and recent advances in their diagnosis have expanded the forms and number of reported patients.
Only a handful of case reports or small case series have evaluated the bleeding risk associated with surgery in patients with IPFD. As a result, the exact bleeding risk and most appropriate management options in IPFD are not known, Dr. Gresele of University of Perugia (Italy) said.
He reported on a retrospective study involving patients with IPFD enrolled at 42 centers from 16 countries. The median age of the 205 patients was 35 years, and 56% were women; 89 had Glanzmann thrombasthenia, 46 had primary secretion defect, 14 had combined alpha-delta granule deficiency, 11 had Hermansky-Pudlak syndrome, 9 had gray platelet syndrome, and 36 had other forms of IPFD.
Data were collected from 389 procedures, of which 54.5% were surgeries, 30% were dental procedures, and 15.5% were invasive procedures. The most frequent surgeries were otolaryngologic, abdominal, orthopedic, gynecologic, urologic, and dermatologic.
The frequency of excessive bleeding at surgery was about 19.7% by the Bleeding Academic Research Consortium (BARC) bleeding classification, 17% by subjective evaluation by the surgeon or patient, and 13% based on duration of bleeding at surgery of at least 6 or more hours, Dr. Gresele said.
The World Health Organization (WHO) bleeding scale before surgery was quite predictive of excessive bleeding at surgery, with patients at grade 3 and 4 having an odds ratio for excessive bleeding of 9.22 and 28, respectively, compared with patients at grade 0, he said.
Somewhat unexpectedly, the most serious bleeders based on a BARC of at least 2 or more at surgery were patients with Hermansky-Pudlak syndrome, Glanzmann thrombasthenia, and gray platelet syndrome. Those with primary secretion defect and combined alpha-delta granule deficiency had a relatively low risk of bleeding at surgery, he said.
The procedures associated with more excessive bleeding were urologic surgery, gynecologic surgery, and abdominal surgery.
Preparation for surgery was made in 82% of procedures and included prophylactic platelet transfusions in 38.5%, desmopressin (DDAVP) in about 19%, antifibrinolytic agents in about 12%, factor VIIa in less than 10%, and other interventions such as cryoprecipitate, fibrinogen, fresh frozen plasma, intravenous immunoglobulin, suture, and local hemostatic agent in less than 5%.
Generally all measures had a good ability to prevent excessive bleeding, bringing rates down to about 20% or less, Dr. Gresele said. The two exceptions were no prophylaxis and “other” interventions, where the bleeding rate reached a high of about 45% for the latter. In contrast, bleeding risk was significantly reduced when any prophylaxis (odds ratio, 0.38) or DDAVP (OR, 0.24) were used.
In 87 cases, however, emergency treatment for excessive bleeding was required, he said. Platelet transfusions were the most common treatment, given in roughly half of patients, followed by antifibrinolytic agents. The success rate was about 80% for all measures, except for “other” interventions, which had a success rate of about 65%.
“Treatment of excessive bleeding is made mostly with platelet transfusions or antifibrinolytic agents and is able to stop bleeding in many, but not all cases,” Dr. Gresele concluded.
On Twitter @pwendl
VIENNA – Inherited platelet function disorders are associated with a significant bleeding risk during surgery, a retrospective, multicenter study shows.
“The frequency of excessive bleeding assessed by one of three criteria at surgery is pretty remarkable because we had rates ranging from 13% to about 19% depending on the assessment criteria,” Dr. Paolo Gresele said at the annual congress of the European Hematology Association.
Any excessive bleeding by any criteria took place in about 23% of patients.
Although conventionally considered rare, inherited platelet function disorders (IPFD) are more frequent than previously thought, and recent advances in their diagnosis have expanded the forms and number of reported patients.
Only a handful of case reports or small case series have evaluated the bleeding risk associated with surgery in patients with IPFD. As a result, the exact bleeding risk and most appropriate management options in IPFD are not known, Dr. Gresele of University of Perugia (Italy) said.
He reported on a retrospective study involving patients with IPFD enrolled at 42 centers from 16 countries. The median age of the 205 patients was 35 years, and 56% were women; 89 had Glanzmann thrombasthenia, 46 had primary secretion defect, 14 had combined alpha-delta granule deficiency, 11 had Hermansky-Pudlak syndrome, 9 had gray platelet syndrome, and 36 had other forms of IPFD.
Data were collected from 389 procedures, of which 54.5% were surgeries, 30% were dental procedures, and 15.5% were invasive procedures. The most frequent surgeries were otolaryngologic, abdominal, orthopedic, gynecologic, urologic, and dermatologic.
The frequency of excessive bleeding at surgery was about 19.7% by the Bleeding Academic Research Consortium (BARC) bleeding classification, 17% by subjective evaluation by the surgeon or patient, and 13% based on duration of bleeding at surgery of at least 6 or more hours, Dr. Gresele said.
The World Health Organization (WHO) bleeding scale before surgery was quite predictive of excessive bleeding at surgery, with patients at grade 3 and 4 having an odds ratio for excessive bleeding of 9.22 and 28, respectively, compared with patients at grade 0, he said.
Somewhat unexpectedly, the most serious bleeders based on a BARC of at least 2 or more at surgery were patients with Hermansky-Pudlak syndrome, Glanzmann thrombasthenia, and gray platelet syndrome. Those with primary secretion defect and combined alpha-delta granule deficiency had a relatively low risk of bleeding at surgery, he said.
The procedures associated with more excessive bleeding were urologic surgery, gynecologic surgery, and abdominal surgery.
Preparation for surgery was made in 82% of procedures and included prophylactic platelet transfusions in 38.5%, desmopressin (DDAVP) in about 19%, antifibrinolytic agents in about 12%, factor VIIa in less than 10%, and other interventions such as cryoprecipitate, fibrinogen, fresh frozen plasma, intravenous immunoglobulin, suture, and local hemostatic agent in less than 5%.
Generally all measures had a good ability to prevent excessive bleeding, bringing rates down to about 20% or less, Dr. Gresele said. The two exceptions were no prophylaxis and “other” interventions, where the bleeding rate reached a high of about 45% for the latter. In contrast, bleeding risk was significantly reduced when any prophylaxis (odds ratio, 0.38) or DDAVP (OR, 0.24) were used.
In 87 cases, however, emergency treatment for excessive bleeding was required, he said. Platelet transfusions were the most common treatment, given in roughly half of patients, followed by antifibrinolytic agents. The success rate was about 80% for all measures, except for “other” interventions, which had a success rate of about 65%.
“Treatment of excessive bleeding is made mostly with platelet transfusions or antifibrinolytic agents and is able to stop bleeding in many, but not all cases,” Dr. Gresele concluded.
On Twitter @pwendl
AT THE EHA CONGRESS
Key clinical point: Inherited platelet function disorders are associated with a significant surgical bleeding risk.
Major finding: The frequency of excessive bleeding ranged from about 13% to about 19%.
Data source: Retrospective, multicenter study in 205 patients with inherited platelet function disorders and 389 procedures.
Disclosures: Dr. Gesele reported no financial disclosures.