User login
ESC: Statins reduce postoperative noncardiac surgery event rates
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
LONDON – Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days by 17% when compared with no statin use in a large, international observational study.
Results of the prospective VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation) study showed that the primary composite endpoint of all-cause mortality, myocardial injury after noncardiac surgery (MINS), or stroke at 30 days was 11.8% in a propensity-matched cohort of patients, 2,845 of whom were treated with a statin and 4,492 who were not. The relative risk (RR) for this composite endpoint was 0.83 favoring the use of preoperative statins, with a 95% confidence interval (CI) of 0.73-0.95 and a P value of .007.
Perioperative statin vs. no statin use also cut all-cause mortality by 42% (RR, 0.58; 95% CI, 0.40-0.83; P = .003), cardiovascular mortality by 58% (RR, 0.42; 95% CI, 0.23-0.76; P = .004), and MINS by 14% (RR, 0.86; 95% CI, 0.73-0.98; P = .002).
“These study results are hypothesis generating at most,” emphasized Dr. Otavio Berwanger, who presented the findings at the annual congress of the European Society of Cardiology while they were simultaneously published online (Eur Heart J. 2015 Sept. 1. doi: 10.1093/eurheartj/ehv456).
“It is true that, in this large representative cohort of contemporary patients, statins were associated with lower event rates,” added Dr. Berwanger of Hospital do Coração in São Paulo, Brazil, and “together with the previous body of evidence, statins appear to be an interesting and attractive intervention to reduce postoperative events.” A large-scale, randomized trial is needed, however, to answer the question of whether statins should be used preoperatively to prevent postoperative events in noncardiac surgery patients.
Over a 4-year period that started in August 2007, more than 15,000 individuals aged 45 years or older who were undergoing a variety of noncardiac surgical procedures that required regional or a general anesthetic and at least an overnight stay in the hospital were recruited at 12 centers in eight countries in North and South America, Africa, Asia, Australia, and Europe.
One of the objectives of the study was to examine the use of perioperative statins on cardiovascular events at 30 days, and to do this, the VISION investigators identified the patients who had received a statin in the 7 days prior to surgery and then used propensity matching to form a control group of patients that had not received a statin in the week before surgery.
Just under half of the propensity-matched population was male, with an average age of nearly 69 years. Around 70% of the population had hypertension, 9%-10% had a prior stroke, and 13% had active cancer. Surgeries were urgent in about 2% and emergent in 8%. Around a quarter had undergone orthopedic procedures, and 4% were vascular surgeries. Overall, 36% of surgeries were classified as low risk and 39% as other.
One of the limitations of the study, however, is that, despite the propensity matching, there were some variables that remained different between the two groups, with higher rates of coronary artery disease (20% vs. 14%), peripheral vascular disease (8% vs. 5%), diabetes (30% vs. 25%), and preoperative use of aspirin (25% vs. 19%) and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (53% vs. 48%) in the statin- versus nonstatin-treated patients.
Other limitations are that these data are observational and the use of statins could be just a surrogate for unmeasured confounders that relate to prognosis. Information on the type and dosing of statins also was not obtained, and there was no information collected on potential liver or muscle function side effects.
Nevertheless, the VISION investigators noted in the published paper that the results are consistent with those from other observational studies and prior small-scale, randomized trials and so do add important information. They noted that these data were collected prospectively in a broader range of patients and types of surgeries than has been reported previously. In addition, patients were recruited from several countries and were actively monitored for outcomes and events were centrally adjudicated. VISION is also the only study to report on the effects of statins on MINS.
“Another message from our results is that the use of long-term statins is sub-optimal in high cardiovascular risk patients, who should be on long-term lipid-lowering therapy independently of surgery,” the VISION investigators wrote in their report.
The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
AT THE ESC CONGRESS 2015
Key clinical point: Statin therapy, given the week before a host of noncardiac surgical procedures, reduced the postoperative risk for death and cardiac complications at 30 days, but the findings are hypothesis generating and need validation in a randomized controlled clinical trial.
Major finding: The primary composite outcome (all-cause mortality, myocardial injury after noncardiac surgery, or stroke at 30 days) was 11.8% overall in the propensity-matched cohort, with a 17% relative risk reduction favoring the use of statin versus no statin (P = .007).
Data source: The VISION study is an international, prospective, observational study of more than 15,000 patients who underwent noncardiac surgery between 2007 and 2011.
Disclosures: The study was funded by Hamilton Health Sciences Corp. at McMaster University. Dr. Berwanger disclosed receiving research contracts from AstraZeneca, Bayer Healthcare, Amgen, Boehringer-Ingelheim, Pfizer, and Roche Diagnostics.
Burning the midnight oil does not impact surgical outcomes
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
Attending physicians who work through the wee hours of the night do not have measurably different short-term outcomes for elective surgeries performed the next day, according to a population-based, matched-control study published online Aug. 26.
The primary composite outcome of death, readmission, or complications within 30 days occurred in 22.2% of patients undergoing elective daytime surgery by an attending who treated patients from midnight to 7 a.m. and in 22.4% of those undergoing the same procedure by the same attending, but after a night when no clinical work had been performed (P = .66).
There was no significant between-group difference in the primary outcome in adjusted analyses (adjusted odds ratio, 0.99; P = .65).
Secondary outcomes also were similar between the postmidnight and control groups: death within 30 days (both 1.1%), readmission within 30 days (6.6% vs. 7.1%), complications within 30 days (18.1% vs. 18.2%), median length of stay (both 3 days), and median duration of surgery (both 2.6 hours).
“These data suggest that calls for broad-based policy shifts in duty hours and practices of attending surgeons may not be necessary at this time,” wrote surgical oncologist Dr. Anand Govindarajan of Mount Sinai Hospital, Toronto, and his associates (N Engl J Med. 2015;373:845-53. doi: 10.1056/NEJMsa1415994).
The current study addresses a gap in the literature on the effects of sleep deprivation and may help inform policy discussions on this issue, the authors suggested.
Most studies of physicians suggesting that sleep deprivation may affect mood, cognition, and psycho-motor function have focused on medical trainees, but few studies have examined the effects of sleep deprivation in attending physicians and the results have been conflicting.
A 2009 single-center study prompted calls for policy-level changes regarding sleep deprivation in surgeons after showing a higher rate of complications for procedures performed by attending physicians with sleep opportunities of less than 6 hours (JAMA. 2009 Oct 14;302[14]:1565-72), but the findings have not been replicated by other groups, Dr. Govindarajan and his associates observed.
In the current study, a small but significant increase in complications was observed in the subset of patients whose physician had performed two or more procedures the night before (adjusted OR, 1.14; P = .05). Importantly, this isolated finding was from a post-hoc subgroup analysis and may be the result of random error, they suggested.
Further, three a priori analyses found no significant difference in outcomes after stratification for academic vs. nonacademic center, physician age, or type of procedure.
The current study involved 38,978 patients who underwent 1 of 12 elective daytime procedures performed by 1,448 physicians at 147 hospitals in Ontario. Patients undergoing procedures performed by a physician who had treated patients from midnight to 7 a.m. were matched in a 1:1 ratio to patients undergoing the same procedure by the same physician on a day when the physician had not treated patients after midnight.
The physicians had been in practice for a median of 20 years, and 40.6% of procedures were performed at academic institutions. Physicians who treated patients after midnight performed a mean of 1.25 procedures during that time.
The elective procedures (cholecystectomy, gastric bypass, colon resection, coronary artery bypass grafting, coronary angioplasty, knee replacement, hip replacement, hip fracture repair, hysterectomy, spinal surgery, craniotomy, and lung resection) were all performed on weekdays.
The investigators selected procedures that varied in duration and were associated with a range of complication rates because sleep studies have suggested that tasks requiring longer periods of concentration may be more affected by sleep deprivation.
“The broad scope of the study enhances its generalizability, a particularly relevant consideration if policy changes are being contemplated with respect to duty hours,” Dr. Govindarajan and his associates noted.
Other strengths of the study are the matched study groups and sufficiently sized cohorts and event rates to provide adequate power to show clinically meaningful differences.
Limitations of the study are the inability to quantify the number of hours that a physician was deprived of sleep and to determine whether there was a difference in outcomes between daytime procedures performed later in the day and those performed earlier in the day or whether procedures may have been postponed till later in the day because of substantial sleep deprivation. “However, given the constraints of operating room schedules in Ontario, it would not usually be feasible to postpone an operation until later in the day on short notice,” the investigators wrote.
Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
On Twitter @pwendl
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The risks of adverse outcomes of elective daytime surgical procedures were similar whether or not the attending physician had provided medical care the previous night.
Major finding: The primary composite endpoint was similar between the postmidnight and control groups (22.2% vs. 22.4%; P = .66).
Data source: Population-based, retrospective, matched cohort study in 38,978 patients.
Disclosures: Dr. Govindarajan reported grant support from the Canadian Institutes for Health Research and the University of Toronto Dean’s Fund while conducting the study.
Scoring tool points to postop ventilator dependence
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
CHICAGO – A new preoperative risk scoring tool may help identify patients at high risk for requiring mechanical ventilation for more than 48 hours in the 30 days after surgery, a study suggests.
The risk score is based on seven measures: whether patients have had a small bowel procedure, have had an esophageal procedure, are current smokers, have severe chronic obstructive pulmonary disease, have hypoalbuminemia, are older than age 60 years, or have signs of systemic inflammatory response syndrome or sepsis.
The score was validated via the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) database to identify patients who underwent nonemergent general or vascular surgery at Thomas Jefferson University Hospital between 2006 and 2013, Dr. Adam P. Johnson, study coauthor, reported at the ACS/NSQIP National Conference.
The risk score assigned 1 point each for a small bowel procedure, current smoking, severe chronic obstructive pulmonary disease, and hypoalbuminemia (less than 3.5 mg/dL); 2 points each for age over 60 years and signs of systemic inflammatory response syndrome or sepsis; and 3 points for esophageal procedures. Total risk scores ranged from 0 to 7 points for the population.
The median score was 2 for patients who did not need a ventilator after surgery and 3 for those who did, Dr. Johnson said.
Notably, patients with a risk score of more than 3 comprised the 20%-30% of patients who experienced 60%-70% of adverse events. A cutoff value of 3 identified the top 20% of patients at highest risk for ventilator dependence, with a ventilator dependence rate of 5.4% (P less than .01).
The risk factors and scoring system are specific to Thomas Jefferson University Hospital, where many patients with advanced gastrointestinal malignancies are treated. However, other institutions should be able to use the methodology and framework to identify ventilator risk factors in their own patients, Dr. Johnson suggested.
Future steps include evaluating how the risk tool performs when compared with risk scores derived from national datasets, automating the best performing risk score, and using the score in the preadmission testing of every patient undergoing elective general surgery or vascular operations. Once identified, high-risk patients would then be entered into an aggressive pre-, intra-, and postoperative pulmonary optimization pathway.
“The pathway might be resource intensive for all patients, but we might be able to hone in and use it more effectively for patients at greatest risk,” Dr. Johnson said in a statement.
Although ventilator dependence occurs in only about 1-3% of patients, the consequences are nonetheless significant, increasing mortality and health care costs, said Dr. Scott W. Cowan, senior study author and Jefferson’s NSQIP Surgeon Champion.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A preoperative risk score can help identify patients at highest risk for postoperative ventilator dependence.
Major finding: A risk score greater than 3 identified the top 20%-30% of patients experiencing 60%-70% of postop ventilator dependence events.
Data source: Retrospective analysis of 7,473 elective general and vascular surgical patients.
Disclosures: The authors reported having no financial disclosures.
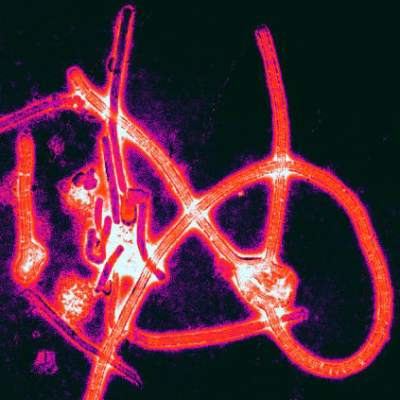
Postexposure prophylaxis may prevent Ebola disease development
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
A small group of health care workers at intermediate or high risk of developing Ebola virus disease after exposure to the virus did not develop the disease after being treated with postexposure prophylaxis, according to Dr. Michael Jacobs and his associates.
Of eight health care workers evacuated to the United Kingdom between January and March 2015 and assessed using an Ebola risk calculator, four were deemed to be at intermediate or high risk for developing Ebola virus disease (EVD) and were started on postexposure prophylaxis (PEP) using oral favipiravir over 10 days. In addition, two of the four also were treated with monoclonal antibodies to Ebola glycoproteins. The favipiravir, administered in high dosages, was tolerated well by the four patients, the investigators reported in Lancet Infectious Diseases.
The second half of the eight-person study group had a low risk of EVD after assessment, and patients in this group were watched carefully, receiving no other form of treatment. No EVD developed in this low-risk group.
It cannot be known “whether or not PEP prevented the onset of Ebola virus disease in any of these individuals. However, two individuals had very high risk of Ebola virus transmission, and these are the first reported cases of transcutaneous, hollow-bore needlestick injuries contaminated with fresh blood that have not resulted in Ebola virus transmission,” noted Dr. Jacobs of the department of infection at Royal Free London NHS Foundation Trust and his associates.
In a related comment, Dr. Mark J. Mulligan and Dr. Paul N. Siebert said, “A needed next step is the development of a consensus risk determination algorithm devised by an expert panel, drawing on all available evidence, endorsed by health organizations, and disseminated to the field. The algorithm could be accompanied by a chart abstraction and case report form to standardize and organize data gathering.”
Dr. Mulligan and Dr. Siebert of the division of infectious diseases at Emory University in Atlanta added, “These data for recognized exposures in health care workers could be collated and analyzed in an international registry.”
Find the full study here: Lancet Infect Dis. 2015 Aug 26. doi: 10.1016/S1473-3099(15)00228-5.
Evidence-based practices can cut breast cancer costs
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
HOUSTON – There are at least three evidence-based practices for reducing the costs of locoregional therapy for early breast cancer without compromising the quality of care, according to Dr. Rachel Adams Greenup of the department of surgery at Duke University Medical Center, in Durham, North Carolina.
Management of axilla per the ACOSOG Z0011 study, adherence to joint Society of Surgical Oncology/American Society of Radiation Oncology (SSO/ASTRO) margin guidelines, and alternative radiation regimens following lumpectomy can all cut costs without compromsing quality of care, she said at the annual Society of Surgical Oncology Symposium.
The results of ACOSOG Z0011, published in 2010, were universally acknowledged to be practice changing. They showed that for women undergoing lumpectomy and radiation therapy for T1-2 invasive breast cancer and positive sentinel lymph node biopsy, completion axiallary dissection did not improve either disease-free or overall survival (DFS/OS). There were low rates of locoregional recurrence regardless of whether patients received axillary node dissection.
The potential savings from eliminating the routine practice of axillary dissection were estimated to be a 64% reduction in inpatient days, and an 18% decrease in perioperative costs.
The SSO/ASTRO margin guidelines, published in 2014, were developed by a multidisciplinary panel based on a meta-analysis of 33 studies involving more than 28,000 patients. The guidelines note that positive surgical margins are associated with a 2-fold increase in ipsilateral breast tumor recurrence, with “no ink on tumor” sufficient for a negative margin. The guidelines say that further margin width resections do not decrease same-breast recurrences.
In a related analysis of the cost implications, Dr. Greenup and colleagues noted that there are wide variations in clinical practice, and that 20% of women with close but negative margins were re-excised needlessly. Eliminating 25,000 unnecessary re-excisions annually would save $31 million dollars. These savings do not include cost reductions from an estimated 8% to 12% reduction in conversions to mastectomy that would be avoided, the authors calculated.
The costs of radiation following lumpectomy correlate directly with the number of delivered radiation fractions or treatment sessions, and also with the technique. Alternatives to standard radiation schedules include the following:
Per-patient costs for each of these options in 2011 ranged from $0 for no radiation, as in CALGB 9343, to $5342 for APBI, $9122 for HF-WBI, and $13m358 for conventionally fractionated WBI.
Dr Greenup and colleagues looked at data on 43,247 women in the National Cancer Data Base with T1-T2, NO invasive breast cancers treated with lumpectomy, and compared the actual costs of treatment with the evidence-based alternative. They found that 26% of patients were treated with the least cost-effective radiation, while nearly all of the remaining patients received more expensive radiation than necessary. If every patient were treated with the most cost-effective approach, there would be an estimated 39% reduction in costs, translating into a saving of $164 million over a single year, they reported in an abstract presented at the 2014 San Antonio Breast Cancer Symposium.
“We can’t make decisions based on cost alone, and value is certainly more important, but clinical trials, moving forward, should incorporate cost information. There is an opportunity to have small changes in clinical practice have the potential to make dramatic reductions in health care spending, and there are lots of opportunities in early stage breast cancer to practice evidence-based care while reducing health care spending,” Dr. Greenup concluded.
Dr. Greenup reported having no relevant financial disclosures.
EXPERT ANALYSIS AT SSO 2015
More octogenarians muscling through emergent surgeries
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
CHICAGO – An increasing number of octogenarians are undergoing emergent surgeries, but the mortality associated with these procedures has not changed significantly, a national ACS/NSQIP analysis found.
From 2005 to 2012, overall mortality among 5,016 octogenarians actually decreased slightly from 8.8% to 7.3%. This reduction was driven by declining death rates for appendectomy from 6.7% to 2.4%, ventral hernia repair from 11% to 4%, and cholecystectomy from 5% to 3%.
Only octogenarians undergoing a Hartmann’s procedure were more likely to die over the 7-year study period, increasing from 14.3% to 21.7%, Dr. Busayo Irojah, of Wellspan Health York (Pa.) Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
In all, 1,440 patients, mean age 84 years, underwent appendectomy (35% open; 65% laparoscopic), 1,252 cholecystectomy (34% open; 66% laparoscopic), 1,197 ventral (umbilical/inguinal) hernia repair (96% open; 4% laparoscopic), and 1,127 Hartmann’s procedure.
Mortality was lower for laparoscopic than for open procedures; appendectomy (2.1% vs. 4.2%; P = .024), cholecystectomy (3.1% vs. 11.6%; P less than .0001), and hernia repair (1.9% vs. 5.8%; P = .22), Dr. Irojah reported.
In multivariate analysis that adjusted for 31 variables including patient characteristics, medical comorbidities, and hospital characteristics, significant predictors of mortality were: sepsis (Odds ratio, 2.5; P less than .01), DNR status (OR, 2.4; P less than .001), previous cardiac surgery (OR, 2.3; P = .003), postoperative renal failure (OR, 2.6; P = .03), poor functional health status (OR, 4.5; P less than .001), and disseminated cancer (OR 6.5; P = .01).
Super elders
Poor functional status was also a strong predictor of morbidity and mortality in the “super elderly” following cholecystectomy in a separate analysis, also led by Dr. Irojah.
The study involved 1,017 patients, aged 90 years and older, who underwent cholecystectomy from 2005 to 2012 in the ACS/NSQIP database. Of these cases, 78% were laparoscopic, 22% open, 80% emergent, and 20% elective.
Mortality was three times higher for an open than a laparoscopic procedure (12.2% vs. 3.8%; P less than .01) and twice as high for emergent than elective cases (10% vs. 4.5%; P less than .01).
In multivariate analysis that adjusted for 25 variables, significant independent predictors of mortality were: preoperative total dependence vs. functional independence (OR, 12.75), postoperative acute renal failure (OR 19.46), postoperative myocardial infarction (OR 71.16), and an open approach (OR, 5.44; all P values less than .00).
“Mortality following both elective and emergent cholecystectomy in patients ninety and over is higher than the general population; hence preoperative optimization is essential and nonoperative management might be reasonable in high-risk patients,” Dr. Irojah observed.
The odds of a complication were double for super elders undergoing open cholecystectomy (OR, 2.4; P less than .01) and at least four times higher for those with poor preoperative functional health status (OR, 4.2; P less than .01), undergoing emergency surgery (OR 4.3; P = .03), or who were Hispanic (OR 4.9; P less than .01), Dr. Irojah reported.
An outpatient procedure, however, was protective for morbidity (OR, 0.39: P = .03) in multivariate analysis adjusted for 13 variables.
“We are trying to educate primary care in our area on the need to avoid emergency operation and preemptively assess for elective operation. Secondarily, we are discussing palliative care with families of elderly higher-risk patients,” senior author and colleague Dr. Vanita Ahuja said in an interview.
The study authors reported having no disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
OR-focused effort cuts catheter use, surgical UTIs
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
CHICAGO – A novel effort to change the prevailing culture toward overuse of catheters in surgical patients appears to be paying off for one Midwestern hospital.
The goal was to decrease catheter utilization by 5%, but 6 months after implementation, the number of catheters placed per day in the operating room in surgeries lasting less than 3 hours declined 9% (mean 14.2/day vs. 12.9/day) and overall catheter utilization in these short cases by 12% (mean 23.7% vs. 20.6%).
Removal of catheters in the OR after surgery decreased by 15% (18.3% vs. 21%), Dr. Anthony D. Yang, of Northwestern Memorial Hospital, reported at the American College of Surgeons (ACS)/National Surgical Quality Improvement Program (NSQIP) National Conference.
Catheter-associated urinary tract infection (CAUTI) rates before the intervention put the Chicago-based hospital in the bottom 10% of ACS NSQIP hospitals.
Post-intervention, the number of CAUTIs in patients whose catheters were inserted in the OR declined 89% from a mean of 2.75 to 0.3 per month. In 4 out of 6 post-intervention months, no CAUTIs were reported, Dr. Yang observed.
Efforts to improve CAUTIs typically focus on removing catheters in surgical patients promptly after transfer to the floor, but the assembled multidisciplinary team chose the less-studied approach of decreasing overall utilization of catheters in the OR.
Using the DMAIC (Define, Measure, Analyze, Improve and Control) method of process improvement, the team identified and instituted two major interventions. First, all catheters have to be inserted with a two-person technique to identify previously unnoticed breaks in sterile technique. Second, OR staff routinely address the necessity for catheters with the surgical team at the beginning of the procedure and with the attending surgeon in the OR before the end of surgery in all cases.
To help change culture, educational programs were instituted with all perioperative services staff and house-staff physicians in all surgical departments, awareness was raised about the project and its justification, and the intervention was mandated to permit tracking.
A total of 465 catheters were inserted in the OR in cases less than 3 hours in the month prior to the intervention, compared with 391, 348, 409, 387, 382, and 427, respectively, in the first six months after the intervention, team leader Dr. Yang, with the hospital’s department of surgery and surgical oncology, said.
Adherence to the two-person sterile technique for OR catheter placement was 80% in the first month, reached 100% for the second and third months, but dropped to around 70% for months four through six. Data for the latter months was fed back to OR staff with encouragement to redouble efforts and increase compliance. It’s thought the problem is actually with documentation because at the time, the fields to document two-person technique in the electronic medical record were not required to be filled in before closing the file, he said.
Compliance with catheter status with the attending surgeon at sign-out was 88% in the first month, dipped slightly in months 2 and 3, and reached and has been maintained at about 85% in months 4 through 6.
“With any intervention it is expected to see periodic decreases in performance,” Dr. Yang said in an interview. “This is why using the DMAIC method becomes important, because the Control part of the methodology calls for continuously monitoring for drops in performance and includes a plan to respond to them. In our plan, the Control plan was to feedback data to the OR staff as the initial step.”
Future steps are to utilize the hospital’s Enterprise Data Warehouse report for monthly performance audits to identify any problem areas, develop a detailed Control plan and consensus criteria for catheter insertion in short cases, and to continue to provide feedback data to relevant stakeholders.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: An OR-focused multidisciplinary effort decreased catheter use in the operating room and catheter-associated UTIs.
Major finding: Catheter utilization in short cases declined 9% and surgical CAUTI by 89%.
Data source: Observational analysis of 2,809 surgical catheters placed.
Disclosures: The authors reported having no financial disclosures.
Longer hospitalization after bariatric surgery ups readmission risk
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Patients who stayed in hospital for at least 3 days after bariatric surgery were up to four times as likely to be readmitted as were patients who were discharged within a day, according to a study in the August issue of Surgery.
Short length of stay (LOS) after bariatric surgery might not be a risk factor for readmission as long as clinical decisions reflect the individual needs of patients, said Alex W. Lois of the Medical College of Wisconsin, and his associates.
“The goal of a program or response to this study should not be to strive to discharge all patients in 1 day or less – the key is to discharge the right patients in the right circumstances in 1 day when feasible,” the researchers said.
Fast-tracking patients after laparoscopic bariatric surgery is controversial. Some papers have described successful programs, while others have described increased risk of morbidity or mortality without careful patient selection, the researchers noted. “Although discharge in 1 day or less is certainly possible, median duration of stay is closer to 2 days for most patients,” they noted (Surgery. 2015 Aug;158[2]:501-7).
To examine the risks of fast-tracking bariatric surgery patients, the researchers performed a multicenter database analysis of 95,294 such patients who were treated from January 2009 to December 2013. The average age of the patients was 44 years, and more than three-quarters were female. Most procedures were laparoscopic Roux en-Y gastric bypass (LRYGB) surgeries, the investigators noted.
In all, 5,423 patients (5.7%) were readmitted before the end of the study period, and 83 (0.1%) died, said the investigators. Patients with 3-day and more than 3-day LOS after bariatric surgery had double and quadruple the risk of readmission, compared with patients with 1-day LOS, respectively (P less than .001 for both). Other significant predictors of readmission included LRYGB surgery, increased postoperative complications, and more comorbidities at initial admission, they said.
Preventing readmissions is not always realistic, the researchers emphasized. “Not all readmissions are avoidable. Not all readmissions represent poor quality care, either,” they said. “The decision to readmit a patient who was recently discharged is often the best option for appropriate care.” They pointed to a recent analysis of Medicare patients that found that low readmission rates after pancreaticoduodenectomy were linked with the highest rates of mortality.
But hospitals that are able to efficiently discharge bariatric surgery patients also might have other attributes that prevent readmissions but were not discernable from the study database, the investigators said. “Patients who are successfully discharged earlier also may be different than those who ultimately stay longer,” they noted. “In addition to prolonged duration of stay, complications, gastric bypass, and increased number of comorbidities also are associated with an increased risk of readmission. Targeted interventions for patients with specific risk factors for readmission may be an effective strategy for reducing readmissions after bariatric surgery.”
The study did not examine care protocols and pathways, which can affect readmission rates, and the database included administrative billing records, which differ from clinical databases when calculating readmissions. “Clinical databases like the National Surgical Quality Improvement Program more accurately capture these data,” said the researchers. “[But] regardless of these shortcomings, we believe that the size of the dataset (nearly 100,000 bariatric surgery patients) provides significant statistical power for evaluating the relationship between duration of stay and readmission rates.” Future analyses of the NSQIP dataset or the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program could further study risk factors and preventive strategies, they noted.
The Medical College of Wisconsin and the National Institutes of Health supported the study. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
FROM SURGERY
Key clinical point: Short length of hospital stay after bariatric surgery was not a risk factor for readmission.
Major finding: Patients who were hospitalized for 3 days and longer were two to four times as likely to be readmitted than were patients with 1-day stays (P less than .001 for both).
Data source: Multicenter database analysis of postoperative outcomes for 95,294 bariatric surgery patients.
Disclosures: The Medical College of Wisconsin and the National Institutes of Health supported the research. Two coauthors disclosed consulting relationships with the University HealthSystem Consortium and Torax Medical.
Cut to the chase: Admitting patients with ASBO directly to surgical service
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Patients who needed surgery for suspected adhesive small bowel obstruction had shorter hospital stays and lower costs if they went straight to surgical services instead of medical hospital services.
Major finding: ASBO patients requiring surgery who were admitted to the medical hospitalist service had longer median hospital stays, compared with those admitted to the surgical service (9.57 days vs. 6.99 days) and higher median charges ($38,800 vs. $30,100).
Data source: Data from 555 consecutive admissions with presumed adhesive small bowel obstruction from 2008 to 2012.
Disclosures: The study authors had no relevant financial conflicts.
For diabetic patients, LRYGB safety comparable to other common procedures
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
CHICAGO – Laparoscopic Roux-en-Y gastric bypass (LRYGB) in diabetic patients has comparable short-term morbidity and mortality with other common surgical procedures and may circumvent the need for many of them, a NSQIP database analysis shows.
Thirty-day mortality for LRYGB was 3 per 1,000 patients, or approximately one-tenth that of coronary artery bypass graft (0.3% vs. 2.8%).
“This is significant to us moving forward from the point of meeting patients earlier on in their life and approaching the idea of bariatric surgery because the earlier intervention of bariatric surgery, which may have the chance of curing their diabetes, may eliminate the need for higher-risk procedures such as a cardiac bypass down the road,” study author Dr. Matthew Davis said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Similarly, total knee arthroplasty had a complication rate nearly five times that of LRYGB (16.7% vs. 3.4%) and comparable mortality (both 0.3%).
“Being that morbid obesity, or obesity in general, is a significant risk factor for osteoarthritis, which is the number-one indication for total knee [arthroplasty], again, we can potentially perform one surgery to eliminate the need for a further surgery that does show to have a higher complication rate,” he said.
Five randomized controlled trials have shown the remarkable effects of bariatric surgery on type 2 diabetes mellitus, including better glycemic control, cardiovascular risk factor modification, and the potential for long-term remission. The safety profile of metabolic diabetes surgery, however, has been a matter of concern among patients and physicians, said Dr. Davis of the Bariatric & Metabolic Institute at the Cleveland Clinic.
To explore short-term metabolic diabetes surgery outcomes, the investigators used the American College of Surgeons’ NSQIP dataset to identify 16,509 diabetic patients who underwent LRYGB from January 2007 to December 2012 and compare them with patients undergoing seven other common surgical procedures: coronary artery bypass graft (n = 2,868), infrainguinal bypass (n = 10,454), laparoscopic partial colectomy (n = 5,511), laparoscopic cholecystectomy (n = 15,306), laparoscopic appendectomy (n = 4,537), laparoscopic hysterectomy (n = 2,309), and total knee arthroplasty (n = 9,184).
Patients undergoing open or revisional bariatric surgery were excluded. Also excluded were sleeve gastrectomy cases because data were not available for the entire study period and gastric banding because its effect on diabetes is not as significant as gastric bypass, he said.
One-third (37.4%) of patients used insulin, 79% had hypertension, and 71.5% were women. The average body mass index was 46.5 kg/m2 and the average age was 50 years.
The 30-day composite complication rate was defined as the presence of any of nine postoperative adverse events: stroke, myocardial infarction, pulmonary embolism, acute renal failure, septic shock, deep vein thrombosis, pneumonia, sepsis, and need for transfusion.
The most frequent adverse event with LRYGB was need for transfusion, which occurred in 1.22% of patients, Dr. Davis said. Rates for the other eight complications in ascending order were: stroke (0.05%), MI (0.16%), pulmonary embolism (0.22%), acute renal failure (0.22%), septic shock (0.30%), deep vein thrombosis (0.36%), pneumonia (0.66%), and sepsis (0.81%).
The 30-day complication rate for LRYGB was comparable with that for laparoscopic cholecystectomy (3.7%) and laparoscopic hysterectomy. Complication rates were significantly higher, however, for CABG (46.6%), infrainguinal bypass (23.6%), laparoscopic partial colectomy (12%), laparoscopic appendectomy (4.5%), and total knee arthroplasty (16.7%), according to Dr. Davis.
Among LRYGB patients, the mean length of stay was 2.6 days, and 6.7% were readmitted, 2.5% underwent reoperation, and 0.3% died.
In contrast, the average length of stay was 6 days for laparoscopic partial colectomy, with readmission, reoperation, and mortality rates of 9.4%, 3.8%, and 1.8%, respectively.
“Compared with laparoscopic colectomy, gastric bypass superseded in all categories with morbidity and mortality,” he said.
Limitations of the study were the lack of information on sleeve gastrectomy and long-term safety outcomes, and nonsimilar baseline characteristics for comparator groups.
Session comoderator Dr. Konstantin Umanskiy of the University of Chicago said that the results highlight the dramatic improvements achieved in bariatric surgery through centers of excellence and could serve to invigorate efforts to bring this model to colorectal surgery. An initiative by the 144-member Consortium for Optimizing the Surgical Treatment of Rectal Cancer (OSTRICH) to establish a U.S. Rectal Cancer Centers of Excellence program was endorsed last year by the American College of Surgeons and the Commission on Cancer.
The investigators and Dr. Umanskiy reported having no conflicts of interest.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Laparoscopic Roux-en-Y gastric bypass in patients with diabetes is as safe as other common procedures.
Major finding: At 30 days, LRYGB mortality was 0.3% and the composite complication rate was 3.4%.
Data source: Retrospective study in 16,509 diabetic patients who underwent Roux-en-Y gastric bypass and 50,169 patients who had other surgical procedures.
Disclosures: The investigators and Dr. Umanskiy reported having no conflicts of interest.