User login
MRI-guided prostate biopsy prevails in PRECISE trial
Here’s welcome news for men of a certain age: New results support a less invasive approach to investigations for suspicion of prostate cancer.
An approach using MRI of the prostate followed by targeted biopsy (TB) in men with images suggesting a high risk beat the conventional approach of using transrectal ultrasound (TRUS)–guided 12-core systematic biopsy.
The results come from the randomized phase 3 PRECISION trial and were published online in JAMA Oncology.
“What the trial showed is that by taking an imaging-first strategy, you could reduce the number of patients needing a biopsy by about 40% and actually find more significant cancer (35% vs. 30%) and reduce the diagnosis of grade group 1 cancers that we don’t want to find by more than half,” lead author Laurence Klotz, CM, MD, of the Sunnybrook Health Sciences Centre in Toronto commented in an interview with this news organization.
These results from the PRECISE trial support and slightly improve upon findings from the European-based PRECISION trial.
The European trial had already provided “compelling evidence in favor of MRI and targeted biopsy,” noted Olivier Rouvière, MD, PhD, from the University of Lyon (France) in an accompanying editorial. But he argued that it was worth duplicating the trial, as “it must not be forgotten that, in science, testing the robustness of an effect and the factors influencing it is are as important as demonstrating this effect in the first place.”
The results from both trials suggest that, instead of replacing TRUS biopsy entirely, MRI results could be used to guide patients to the appropriate diagnostic pathway, Dr. Rouvière commented.
“Using only MRI findings to decide which patients should undergo biopsy is probably insufficient,” he added. “Most likely, MRI findings will be used in conjunction with other biomarkers such as PSA [prostate-specific antigen] density to select, among the patients with positive MRI findings, those who need targeted biopsy (and those who may safely avoid it), and among the patients with negative MRI findings, those who may still deserve systematic biopsy,” he wrote.
Details of PRECISE findings
The Canadian PRECISE study was developed as a noninferiority trial in coordination with the European PRECISION study, but the Canadian version had several additional features. It added risk-based eligibility, systematic follow-up of all patients for 2 years, a repeat MRI in all untreated patients, investigation of fluid- and tissue-based biomarkers in the cohort, and an economic analysis.
PRECISE was conducted in five Canadian academic health sciences centers from January 2017 through November 2019. A total of 453 biopsy-naive men with a clinical suspicion of prostate cancer who were referred for prostate biopsy were enrolled. Of this group, 421 were evaluable per protocol.
The investigators defined clinical suspicion as a 5% or greater chance of grade group 2 or greater prostate cancer. Patients were also required to have serum prostate-specific antigen PSA levels of 20 ng/mL or less and no contraindication to MRI.
The patients randomly assigned to MRI underwent an MRI-targeted biopsy (MRI-TB) only if a lesion with a Prostate Imaging Reporting and Data System (PI-RADS) score of 3 or greater was identified, whereas all men in the other arm of the trial underwent a systematic TRUS-guided 12-core biopsy.
The MRI approach identified more clinically significant cancers. Grade 2 or higher tumors were found in 79 (35%) of 227 men allocated to MRI-TB vs. 67 (30%) of 225 men who underwent TRUS biopsy.
MRI also reduced the need for a biopsy, allowing many men to avoid the associated pain, discomfort, and infection risks. Of 221 men who were randomly assigned to the MRI group, 83 (37%) had a negative MRI result and avoided biopsy. In contrast, all men in the TRUS group had a biopsy.
In addition, MRI was associated with a marked reduction in the diagnosis of clinically insignificant International Society of Urological Pathology (ISUP) grade group 1 cancers (10% with MRI-TB vs. 22% with TRUS). Detection of such early cancers, under conventional protocols, often leads to unnecessary therapies or invasive procedures with significant side effects.
These results led the researchers to conclude that the strategy of MRI followed by MRI-guided biopsy only in men at risk of prostate cancer “offers substantial advantages over an initial systematic biopsy.”
The MRI strategy “results in similar detection rates of clinically significant prostate cancer … while avoiding biopsy in more than one-third of men and reducing the diagnosis of clinically insignificant cancer,” the investigators point out.
The investigators acknowledged that the performance of the MRI-targeted biopsy varied between centers, with differences in both positive MRI rates and target biopsy yields.
“This difference occurred despite the fact that all MRIs were reviewed, and biopsies performed, by experienced radiologists or urologists. This underscores the need for quality control measures to enable the broad application of MRI,” they write.
What’s next?
Dr. Klotz noted that an important addition to PRECISE is the planned follow-up of patients who did not receive treatment on study.
“We know MRI is not perfect, so what happens to the guys who avoid the biopsy? How much at risk are they of having something missed? So the only way to know that really is with long-term follow-up on the patients,” he said in an interview.
In addition to repeating MRI at 2 years, the investigators plan to follow these patients for up to 8 years.
“But certainly, compared to the traditional strategy of systematic biopsy, this looks a lot better,” Dr. Klotz commented.
In his editorial, Dr. Rouvière commented that the intersite variability seen in the study “sounds like a warning to the MRI pathway.”
“Considering that all participating centers were experienced high-volume tertiary centers, the intersite variability is probably much higher among less experienced centers,” he wrote. “Thus, whatever the diagnostic pathway, continuing education and quality insurance programs will become major issues in the future, not only for prostate MRI interpretation, but also for targeted biopsy, which does have a learning curve, even with magnetic resonance and ultrasound fusion systems, and even for systematic biopsy.”
PRECISE was funded by the Ontario Institute of Cancer Research and Prostate Cancer Canada. Dr. Klotz and Dr. Rouvière have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s welcome news for men of a certain age: New results support a less invasive approach to investigations for suspicion of prostate cancer.
An approach using MRI of the prostate followed by targeted biopsy (TB) in men with images suggesting a high risk beat the conventional approach of using transrectal ultrasound (TRUS)–guided 12-core systematic biopsy.
The results come from the randomized phase 3 PRECISION trial and were published online in JAMA Oncology.
“What the trial showed is that by taking an imaging-first strategy, you could reduce the number of patients needing a biopsy by about 40% and actually find more significant cancer (35% vs. 30%) and reduce the diagnosis of grade group 1 cancers that we don’t want to find by more than half,” lead author Laurence Klotz, CM, MD, of the Sunnybrook Health Sciences Centre in Toronto commented in an interview with this news organization.
These results from the PRECISE trial support and slightly improve upon findings from the European-based PRECISION trial.
The European trial had already provided “compelling evidence in favor of MRI and targeted biopsy,” noted Olivier Rouvière, MD, PhD, from the University of Lyon (France) in an accompanying editorial. But he argued that it was worth duplicating the trial, as “it must not be forgotten that, in science, testing the robustness of an effect and the factors influencing it is are as important as demonstrating this effect in the first place.”
The results from both trials suggest that, instead of replacing TRUS biopsy entirely, MRI results could be used to guide patients to the appropriate diagnostic pathway, Dr. Rouvière commented.
“Using only MRI findings to decide which patients should undergo biopsy is probably insufficient,” he added. “Most likely, MRI findings will be used in conjunction with other biomarkers such as PSA [prostate-specific antigen] density to select, among the patients with positive MRI findings, those who need targeted biopsy (and those who may safely avoid it), and among the patients with negative MRI findings, those who may still deserve systematic biopsy,” he wrote.
Details of PRECISE findings
The Canadian PRECISE study was developed as a noninferiority trial in coordination with the European PRECISION study, but the Canadian version had several additional features. It added risk-based eligibility, systematic follow-up of all patients for 2 years, a repeat MRI in all untreated patients, investigation of fluid- and tissue-based biomarkers in the cohort, and an economic analysis.
PRECISE was conducted in five Canadian academic health sciences centers from January 2017 through November 2019. A total of 453 biopsy-naive men with a clinical suspicion of prostate cancer who were referred for prostate biopsy were enrolled. Of this group, 421 were evaluable per protocol.
The investigators defined clinical suspicion as a 5% or greater chance of grade group 2 or greater prostate cancer. Patients were also required to have serum prostate-specific antigen PSA levels of 20 ng/mL or less and no contraindication to MRI.
The patients randomly assigned to MRI underwent an MRI-targeted biopsy (MRI-TB) only if a lesion with a Prostate Imaging Reporting and Data System (PI-RADS) score of 3 or greater was identified, whereas all men in the other arm of the trial underwent a systematic TRUS-guided 12-core biopsy.
The MRI approach identified more clinically significant cancers. Grade 2 or higher tumors were found in 79 (35%) of 227 men allocated to MRI-TB vs. 67 (30%) of 225 men who underwent TRUS biopsy.
MRI also reduced the need for a biopsy, allowing many men to avoid the associated pain, discomfort, and infection risks. Of 221 men who were randomly assigned to the MRI group, 83 (37%) had a negative MRI result and avoided biopsy. In contrast, all men in the TRUS group had a biopsy.
In addition, MRI was associated with a marked reduction in the diagnosis of clinically insignificant International Society of Urological Pathology (ISUP) grade group 1 cancers (10% with MRI-TB vs. 22% with TRUS). Detection of such early cancers, under conventional protocols, often leads to unnecessary therapies or invasive procedures with significant side effects.
These results led the researchers to conclude that the strategy of MRI followed by MRI-guided biopsy only in men at risk of prostate cancer “offers substantial advantages over an initial systematic biopsy.”
The MRI strategy “results in similar detection rates of clinically significant prostate cancer … while avoiding biopsy in more than one-third of men and reducing the diagnosis of clinically insignificant cancer,” the investigators point out.
The investigators acknowledged that the performance of the MRI-targeted biopsy varied between centers, with differences in both positive MRI rates and target biopsy yields.
“This difference occurred despite the fact that all MRIs were reviewed, and biopsies performed, by experienced radiologists or urologists. This underscores the need for quality control measures to enable the broad application of MRI,” they write.
What’s next?
Dr. Klotz noted that an important addition to PRECISE is the planned follow-up of patients who did not receive treatment on study.
“We know MRI is not perfect, so what happens to the guys who avoid the biopsy? How much at risk are they of having something missed? So the only way to know that really is with long-term follow-up on the patients,” he said in an interview.
In addition to repeating MRI at 2 years, the investigators plan to follow these patients for up to 8 years.
“But certainly, compared to the traditional strategy of systematic biopsy, this looks a lot better,” Dr. Klotz commented.
In his editorial, Dr. Rouvière commented that the intersite variability seen in the study “sounds like a warning to the MRI pathway.”
“Considering that all participating centers were experienced high-volume tertiary centers, the intersite variability is probably much higher among less experienced centers,” he wrote. “Thus, whatever the diagnostic pathway, continuing education and quality insurance programs will become major issues in the future, not only for prostate MRI interpretation, but also for targeted biopsy, which does have a learning curve, even with magnetic resonance and ultrasound fusion systems, and even for systematic biopsy.”
PRECISE was funded by the Ontario Institute of Cancer Research and Prostate Cancer Canada. Dr. Klotz and Dr. Rouvière have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s welcome news for men of a certain age: New results support a less invasive approach to investigations for suspicion of prostate cancer.
An approach using MRI of the prostate followed by targeted biopsy (TB) in men with images suggesting a high risk beat the conventional approach of using transrectal ultrasound (TRUS)–guided 12-core systematic biopsy.
The results come from the randomized phase 3 PRECISION trial and were published online in JAMA Oncology.
“What the trial showed is that by taking an imaging-first strategy, you could reduce the number of patients needing a biopsy by about 40% and actually find more significant cancer (35% vs. 30%) and reduce the diagnosis of grade group 1 cancers that we don’t want to find by more than half,” lead author Laurence Klotz, CM, MD, of the Sunnybrook Health Sciences Centre in Toronto commented in an interview with this news organization.
These results from the PRECISE trial support and slightly improve upon findings from the European-based PRECISION trial.
The European trial had already provided “compelling evidence in favor of MRI and targeted biopsy,” noted Olivier Rouvière, MD, PhD, from the University of Lyon (France) in an accompanying editorial. But he argued that it was worth duplicating the trial, as “it must not be forgotten that, in science, testing the robustness of an effect and the factors influencing it is are as important as demonstrating this effect in the first place.”
The results from both trials suggest that, instead of replacing TRUS biopsy entirely, MRI results could be used to guide patients to the appropriate diagnostic pathway, Dr. Rouvière commented.
“Using only MRI findings to decide which patients should undergo biopsy is probably insufficient,” he added. “Most likely, MRI findings will be used in conjunction with other biomarkers such as PSA [prostate-specific antigen] density to select, among the patients with positive MRI findings, those who need targeted biopsy (and those who may safely avoid it), and among the patients with negative MRI findings, those who may still deserve systematic biopsy,” he wrote.
Details of PRECISE findings
The Canadian PRECISE study was developed as a noninferiority trial in coordination with the European PRECISION study, but the Canadian version had several additional features. It added risk-based eligibility, systematic follow-up of all patients for 2 years, a repeat MRI in all untreated patients, investigation of fluid- and tissue-based biomarkers in the cohort, and an economic analysis.
PRECISE was conducted in five Canadian academic health sciences centers from January 2017 through November 2019. A total of 453 biopsy-naive men with a clinical suspicion of prostate cancer who were referred for prostate biopsy were enrolled. Of this group, 421 were evaluable per protocol.
The investigators defined clinical suspicion as a 5% or greater chance of grade group 2 or greater prostate cancer. Patients were also required to have serum prostate-specific antigen PSA levels of 20 ng/mL or less and no contraindication to MRI.
The patients randomly assigned to MRI underwent an MRI-targeted biopsy (MRI-TB) only if a lesion with a Prostate Imaging Reporting and Data System (PI-RADS) score of 3 or greater was identified, whereas all men in the other arm of the trial underwent a systematic TRUS-guided 12-core biopsy.
The MRI approach identified more clinically significant cancers. Grade 2 or higher tumors were found in 79 (35%) of 227 men allocated to MRI-TB vs. 67 (30%) of 225 men who underwent TRUS biopsy.
MRI also reduced the need for a biopsy, allowing many men to avoid the associated pain, discomfort, and infection risks. Of 221 men who were randomly assigned to the MRI group, 83 (37%) had a negative MRI result and avoided biopsy. In contrast, all men in the TRUS group had a biopsy.
In addition, MRI was associated with a marked reduction in the diagnosis of clinically insignificant International Society of Urological Pathology (ISUP) grade group 1 cancers (10% with MRI-TB vs. 22% with TRUS). Detection of such early cancers, under conventional protocols, often leads to unnecessary therapies or invasive procedures with significant side effects.
These results led the researchers to conclude that the strategy of MRI followed by MRI-guided biopsy only in men at risk of prostate cancer “offers substantial advantages over an initial systematic biopsy.”
The MRI strategy “results in similar detection rates of clinically significant prostate cancer … while avoiding biopsy in more than one-third of men and reducing the diagnosis of clinically insignificant cancer,” the investigators point out.
The investigators acknowledged that the performance of the MRI-targeted biopsy varied between centers, with differences in both positive MRI rates and target biopsy yields.
“This difference occurred despite the fact that all MRIs were reviewed, and biopsies performed, by experienced radiologists or urologists. This underscores the need for quality control measures to enable the broad application of MRI,” they write.
What’s next?
Dr. Klotz noted that an important addition to PRECISE is the planned follow-up of patients who did not receive treatment on study.
“We know MRI is not perfect, so what happens to the guys who avoid the biopsy? How much at risk are they of having something missed? So the only way to know that really is with long-term follow-up on the patients,” he said in an interview.
In addition to repeating MRI at 2 years, the investigators plan to follow these patients for up to 8 years.
“But certainly, compared to the traditional strategy of systematic biopsy, this looks a lot better,” Dr. Klotz commented.
In his editorial, Dr. Rouvière commented that the intersite variability seen in the study “sounds like a warning to the MRI pathway.”
“Considering that all participating centers were experienced high-volume tertiary centers, the intersite variability is probably much higher among less experienced centers,” he wrote. “Thus, whatever the diagnostic pathway, continuing education and quality insurance programs will become major issues in the future, not only for prostate MRI interpretation, but also for targeted biopsy, which does have a learning curve, even with magnetic resonance and ultrasound fusion systems, and even for systematic biopsy.”
PRECISE was funded by the Ontario Institute of Cancer Research and Prostate Cancer Canada. Dr. Klotz and Dr. Rouvière have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CXR-Net: An AI-based diagnostic tool for COVID-19
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
FROM AACR: COVID-19 AND CANCER 2021
Asymptomatic screening for COVID-19 in cancer patients still debated
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
FROM AACR: COVID-19 AND CANCER 2021
Managing cancer outpatients during the pandemic: Tips from MSKCC
“We’ve tried a lot of new things to ensure optimal care for our patients,” said Tiffany A. Traina, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “We need to effectively utilize all resources at our disposal to keep in touch with our patients during this time.”
Dr. Traina described the approach to outpatient management used at MSKCC during a presentation at the AACR Virtual Meeting: COVID-19 and Cancer.
Four guiding principles
MSKCC has established four guiding principles on how to manage cancer patients during the pandemic: openness, safety, technology, and staffing.
Openness ensures that decisions are guided by clinical priorities to provide optimal patient care and allow for prioritization of clinical research and education, Dr. Traina said.
The safety of patients and staff is of the utmost importance, she added. To ensure safety in the context of outpatient care, several operational levers were developed, including COVID surge planning, universal masking and personal protective equipment guidelines, remote work, clinical levers, and new dashboards and communications.
Dr. Traina said data analytics and dashboards have been key technological tools used to support evidence-based decision-making and deliver care remotely for patients during the pandemic.
Staffing resources have also shifted to support demand at different health system locations.
Screening, cohorting, and telemedicine
One measure MSKCC adopted is the MSK Engage Questionnaire, a COVID-19 screening questionnaire assigned to every patient with a scheduled outpatient visit. After completing the questionnaire, patients receive a response denoting whether they need to come into the outpatient setting.
On the staffing side, clinic coordinators prepare appointments accordingly, based on the risk level for each patient.
“We also try to cohort COVID-positive patients into particular areas within the outpatient setting,” Dr. Traina explained. “In addition, we control flow through ambulatory care locations by having separate patient entrances and use other tools to make flow as efficient as possible.”
On the technology side, interactive dashboards are being used to model traffic through different buildings.
“These data and analytics are useful for operational engineering, answering questions such as (1) Are there backups in chemotherapy? and (2) Are patients seeing one particular physician?” Dr. Traina explained. “One important key takeaway is the importance of frequently communicating simple messages through multiple mechanisms, including signage, websites, and dedicated resources.”
Other key technological measures are leveraging telemedicine to convert inpatient appointments to a virtual setting, as well as developing and deploying a system for centralized outpatient follow-up of COVID-19-positive patients.
“We saw a 3,000% increase in telemedicine utilization from February 2020 to June 2020,” Dr. Traina reported. “In a given month, we have approximately 230,000 outpatient visits, and a substantial proportion of these are now done via telemedicine.”
Dr. Traina also noted that multiple organizations have released guidelines addressing when to resume anticancer therapy in patients who have been COVID-19 positive. Adherence is important, as unnecessary COVID-19 testing may delay cancer therapy and is not recommended.
During a live discussion, Louis P. Voigt, MD, of MSKCC, said Dr. Traina’s presentation provided “a lot of good ideas for other institutions who may be facing similar challenges.”
Dr. Traina and Dr. Voigt disclosed no conflicts of interest. No funding sources were reported.
“We’ve tried a lot of new things to ensure optimal care for our patients,” said Tiffany A. Traina, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “We need to effectively utilize all resources at our disposal to keep in touch with our patients during this time.”
Dr. Traina described the approach to outpatient management used at MSKCC during a presentation at the AACR Virtual Meeting: COVID-19 and Cancer.
Four guiding principles
MSKCC has established four guiding principles on how to manage cancer patients during the pandemic: openness, safety, technology, and staffing.
Openness ensures that decisions are guided by clinical priorities to provide optimal patient care and allow for prioritization of clinical research and education, Dr. Traina said.
The safety of patients and staff is of the utmost importance, she added. To ensure safety in the context of outpatient care, several operational levers were developed, including COVID surge planning, universal masking and personal protective equipment guidelines, remote work, clinical levers, and new dashboards and communications.
Dr. Traina said data analytics and dashboards have been key technological tools used to support evidence-based decision-making and deliver care remotely for patients during the pandemic.
Staffing resources have also shifted to support demand at different health system locations.
Screening, cohorting, and telemedicine
One measure MSKCC adopted is the MSK Engage Questionnaire, a COVID-19 screening questionnaire assigned to every patient with a scheduled outpatient visit. After completing the questionnaire, patients receive a response denoting whether they need to come into the outpatient setting.
On the staffing side, clinic coordinators prepare appointments accordingly, based on the risk level for each patient.
“We also try to cohort COVID-positive patients into particular areas within the outpatient setting,” Dr. Traina explained. “In addition, we control flow through ambulatory care locations by having separate patient entrances and use other tools to make flow as efficient as possible.”
On the technology side, interactive dashboards are being used to model traffic through different buildings.
“These data and analytics are useful for operational engineering, answering questions such as (1) Are there backups in chemotherapy? and (2) Are patients seeing one particular physician?” Dr. Traina explained. “One important key takeaway is the importance of frequently communicating simple messages through multiple mechanisms, including signage, websites, and dedicated resources.”
Other key technological measures are leveraging telemedicine to convert inpatient appointments to a virtual setting, as well as developing and deploying a system for centralized outpatient follow-up of COVID-19-positive patients.
“We saw a 3,000% increase in telemedicine utilization from February 2020 to June 2020,” Dr. Traina reported. “In a given month, we have approximately 230,000 outpatient visits, and a substantial proportion of these are now done via telemedicine.”
Dr. Traina also noted that multiple organizations have released guidelines addressing when to resume anticancer therapy in patients who have been COVID-19 positive. Adherence is important, as unnecessary COVID-19 testing may delay cancer therapy and is not recommended.
During a live discussion, Louis P. Voigt, MD, of MSKCC, said Dr. Traina’s presentation provided “a lot of good ideas for other institutions who may be facing similar challenges.”
Dr. Traina and Dr. Voigt disclosed no conflicts of interest. No funding sources were reported.
“We’ve tried a lot of new things to ensure optimal care for our patients,” said Tiffany A. Traina, MD, of Memorial Sloan Kettering Cancer Center (MSKCC) in New York. “We need to effectively utilize all resources at our disposal to keep in touch with our patients during this time.”
Dr. Traina described the approach to outpatient management used at MSKCC during a presentation at the AACR Virtual Meeting: COVID-19 and Cancer.
Four guiding principles
MSKCC has established four guiding principles on how to manage cancer patients during the pandemic: openness, safety, technology, and staffing.
Openness ensures that decisions are guided by clinical priorities to provide optimal patient care and allow for prioritization of clinical research and education, Dr. Traina said.
The safety of patients and staff is of the utmost importance, she added. To ensure safety in the context of outpatient care, several operational levers were developed, including COVID surge planning, universal masking and personal protective equipment guidelines, remote work, clinical levers, and new dashboards and communications.
Dr. Traina said data analytics and dashboards have been key technological tools used to support evidence-based decision-making and deliver care remotely for patients during the pandemic.
Staffing resources have also shifted to support demand at different health system locations.
Screening, cohorting, and telemedicine
One measure MSKCC adopted is the MSK Engage Questionnaire, a COVID-19 screening questionnaire assigned to every patient with a scheduled outpatient visit. After completing the questionnaire, patients receive a response denoting whether they need to come into the outpatient setting.
On the staffing side, clinic coordinators prepare appointments accordingly, based on the risk level for each patient.
“We also try to cohort COVID-positive patients into particular areas within the outpatient setting,” Dr. Traina explained. “In addition, we control flow through ambulatory care locations by having separate patient entrances and use other tools to make flow as efficient as possible.”
On the technology side, interactive dashboards are being used to model traffic through different buildings.
“These data and analytics are useful for operational engineering, answering questions such as (1) Are there backups in chemotherapy? and (2) Are patients seeing one particular physician?” Dr. Traina explained. “One important key takeaway is the importance of frequently communicating simple messages through multiple mechanisms, including signage, websites, and dedicated resources.”
Other key technological measures are leveraging telemedicine to convert inpatient appointments to a virtual setting, as well as developing and deploying a system for centralized outpatient follow-up of COVID-19-positive patients.
“We saw a 3,000% increase in telemedicine utilization from February 2020 to June 2020,” Dr. Traina reported. “In a given month, we have approximately 230,000 outpatient visits, and a substantial proportion of these are now done via telemedicine.”
Dr. Traina also noted that multiple organizations have released guidelines addressing when to resume anticancer therapy in patients who have been COVID-19 positive. Adherence is important, as unnecessary COVID-19 testing may delay cancer therapy and is not recommended.
During a live discussion, Louis P. Voigt, MD, of MSKCC, said Dr. Traina’s presentation provided “a lot of good ideas for other institutions who may be facing similar challenges.”
Dr. Traina and Dr. Voigt disclosed no conflicts of interest. No funding sources were reported.
FROM AACR: COVID-19 AND CANCER 2021
Aspirin linked to reduced bladder, breast cancer mortality
However, the treatment – particularly with frequency of at least three times a week – is associated with reductions in mortality in bladder cancer and breast cancer, new observational research shows.
“The results presented here add to the accumulating evidence that aspirin may improve survival for some cancers,” the authors write in their cohort study that uses data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. The new research was published online Jan. 15 in JAMA Network Open.
“Although prior research has been most heavily concentrated in gastrointestinal cancers, our analysis extends the advantages associated with aspirin use to other cancers, such as bladder and breast cancers,” they explained.
In commenting on the study, John J. McNeil, MBBS, PhD, head of the department of epidemiology and preventive medicine at Monash University in Melbourne, said the findings, though intriguing, are not necessarily conclusive.
“The data was derived from a very large and well-conducted study,” Dr. McNeil, who has led other research on aspirin use and the elderly, said in an interview.
“But these conclusions were drawn from the observational component of the study and therefore potentially confounded by other characteristics that differentiate aspirin users from nonusers.”
Aspirin/cancer research in older people lacking
With well-known reports of decreased risks of heart disease, stroke, cancer – particularly gastrointestinal cancers – and all-cause mortality, as many as 25%-50% of adults in the U.S. report taking aspirin daily or every other day.
However, evidence of the benefits relating to cancer, specifically in older people, has been inconsistent, with one recent notable study, the randomized, double-blind ASPREE trial, showing no effect of aspirin on cancer incidence, but a higher mortality rate in elderly patients randomly assigned to aspirin for primary prevention.
To further investigate the effects in older patients, first author Holli A. Loomans-Kropp, PhD, and colleagues with the National Cancer Institute evaluated data on patients who were either 65 years or older at baseline or who had reached aged 65 during follow-up in the PLCO Cancer Screening Trial, which had enrollment from 1993 to 2001.
The authors identified 139,896 individuals with a mean age at baseline of 66.4 years; about half were women and 88.5% were non-Hispanic White.
Follow-up took place until the time of death, December 2014 for those who consented to follow-up, or December 2009 for those who refused consent to follow-up. The authors reported that there were 32,580 incident cancers, including 5.4% bladder, 14% breast, 1% esophageal, 1.2% gastric, 2.7% pancreatic, and 2.2% uterine cancers.
The study showed no association between aspirin use and the incidence of any of the cancer types included in the study among those over age 65.
However, further multivariate analysis of survival showed that, with follow-up adjusted to until the time of death, Dec. 31, 2015, or earlier refusal to consent, the use of aspirin at least three times per week was associated with reduced mortality in those with bladder (hazard ratio, 0.67) and breast (HR, 0.75) cancers, whereas no significant associations were observed with esophageal, gastric, pancreatic, or uterine cancer.
A similar association of any aspirin use (less than three times per week) with bladder (HR, 0.75) and breast (HR, 0.79) cancer survival was observed, the authors noted.
“These results may indicate that, for some cancer types, any aspirin use may be advantageous; however, greater benefit may be observed with increased frequency of use,” the authors wrote.
Mechanism speculation focuses on COX-2 pathway
Theories of the mechanisms behind a potential benefit of aspirin for those with bladder cancer include that urothelial cancer has increased RNA and protein expression of cyclooxygenase-2 (COX-2) and urinary prostaglandin E2, “suggesting up-regulation of the COX-2 pathway during cancer progression,” the authors wrote.
In breast cancer, a similar elevated expression of COX-2 has been shown to predict disease outcomes, including progression and decreased survival.
“This may be partly due to the mechanistic interplay between angiogenesis, cell proliferation, apoptosis, and inflammatory processes,” the authors noted.
The study isn’t the first to show a benefit specifically with bladder cancer; other studies include recent research (J Urol. 2018 Nov;200[5]:1014-21) showing that daily aspirin use among patients with bladder cancer was associated with increased 5-year survival following radical cystectomy, the authors noted.
Dr. McNeil noted that the new findings from the U.S. researchers, particularly regarding bladder cancer, are of interest. “The reduction in mortality from breast cancer is modest, but the reduction in mortality from bladder cancer was more impressive,” he said.
“However, given the fact that this finding is observational data and was a sole finding among multiple comparisons, it must be seen as suggestive rather than proven.”
Regarding possible mechanisms, Dr. McNeil added that, like the bulk of the prior research, many questions remain.
“There have been many suggestions about ways that aspirin might work at a molecular and cellular level, but no firm consensus has been reached.”
The study authors and Dr. McNeil disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the treatment – particularly with frequency of at least three times a week – is associated with reductions in mortality in bladder cancer and breast cancer, new observational research shows.
“The results presented here add to the accumulating evidence that aspirin may improve survival for some cancers,” the authors write in their cohort study that uses data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. The new research was published online Jan. 15 in JAMA Network Open.
“Although prior research has been most heavily concentrated in gastrointestinal cancers, our analysis extends the advantages associated with aspirin use to other cancers, such as bladder and breast cancers,” they explained.
In commenting on the study, John J. McNeil, MBBS, PhD, head of the department of epidemiology and preventive medicine at Monash University in Melbourne, said the findings, though intriguing, are not necessarily conclusive.
“The data was derived from a very large and well-conducted study,” Dr. McNeil, who has led other research on aspirin use and the elderly, said in an interview.
“But these conclusions were drawn from the observational component of the study and therefore potentially confounded by other characteristics that differentiate aspirin users from nonusers.”
Aspirin/cancer research in older people lacking
With well-known reports of decreased risks of heart disease, stroke, cancer – particularly gastrointestinal cancers – and all-cause mortality, as many as 25%-50% of adults in the U.S. report taking aspirin daily or every other day.
However, evidence of the benefits relating to cancer, specifically in older people, has been inconsistent, with one recent notable study, the randomized, double-blind ASPREE trial, showing no effect of aspirin on cancer incidence, but a higher mortality rate in elderly patients randomly assigned to aspirin for primary prevention.
To further investigate the effects in older patients, first author Holli A. Loomans-Kropp, PhD, and colleagues with the National Cancer Institute evaluated data on patients who were either 65 years or older at baseline or who had reached aged 65 during follow-up in the PLCO Cancer Screening Trial, which had enrollment from 1993 to 2001.
The authors identified 139,896 individuals with a mean age at baseline of 66.4 years; about half were women and 88.5% were non-Hispanic White.
Follow-up took place until the time of death, December 2014 for those who consented to follow-up, or December 2009 for those who refused consent to follow-up. The authors reported that there were 32,580 incident cancers, including 5.4% bladder, 14% breast, 1% esophageal, 1.2% gastric, 2.7% pancreatic, and 2.2% uterine cancers.
The study showed no association between aspirin use and the incidence of any of the cancer types included in the study among those over age 65.
However, further multivariate analysis of survival showed that, with follow-up adjusted to until the time of death, Dec. 31, 2015, or earlier refusal to consent, the use of aspirin at least three times per week was associated with reduced mortality in those with bladder (hazard ratio, 0.67) and breast (HR, 0.75) cancers, whereas no significant associations were observed with esophageal, gastric, pancreatic, or uterine cancer.
A similar association of any aspirin use (less than three times per week) with bladder (HR, 0.75) and breast (HR, 0.79) cancer survival was observed, the authors noted.
“These results may indicate that, for some cancer types, any aspirin use may be advantageous; however, greater benefit may be observed with increased frequency of use,” the authors wrote.
Mechanism speculation focuses on COX-2 pathway
Theories of the mechanisms behind a potential benefit of aspirin for those with bladder cancer include that urothelial cancer has increased RNA and protein expression of cyclooxygenase-2 (COX-2) and urinary prostaglandin E2, “suggesting up-regulation of the COX-2 pathway during cancer progression,” the authors wrote.
In breast cancer, a similar elevated expression of COX-2 has been shown to predict disease outcomes, including progression and decreased survival.
“This may be partly due to the mechanistic interplay between angiogenesis, cell proliferation, apoptosis, and inflammatory processes,” the authors noted.
The study isn’t the first to show a benefit specifically with bladder cancer; other studies include recent research (J Urol. 2018 Nov;200[5]:1014-21) showing that daily aspirin use among patients with bladder cancer was associated with increased 5-year survival following radical cystectomy, the authors noted.
Dr. McNeil noted that the new findings from the U.S. researchers, particularly regarding bladder cancer, are of interest. “The reduction in mortality from breast cancer is modest, but the reduction in mortality from bladder cancer was more impressive,” he said.
“However, given the fact that this finding is observational data and was a sole finding among multiple comparisons, it must be seen as suggestive rather than proven.”
Regarding possible mechanisms, Dr. McNeil added that, like the bulk of the prior research, many questions remain.
“There have been many suggestions about ways that aspirin might work at a molecular and cellular level, but no firm consensus has been reached.”
The study authors and Dr. McNeil disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
However, the treatment – particularly with frequency of at least three times a week – is associated with reductions in mortality in bladder cancer and breast cancer, new observational research shows.
“The results presented here add to the accumulating evidence that aspirin may improve survival for some cancers,” the authors write in their cohort study that uses data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. The new research was published online Jan. 15 in JAMA Network Open.
“Although prior research has been most heavily concentrated in gastrointestinal cancers, our analysis extends the advantages associated with aspirin use to other cancers, such as bladder and breast cancers,” they explained.
In commenting on the study, John J. McNeil, MBBS, PhD, head of the department of epidemiology and preventive medicine at Monash University in Melbourne, said the findings, though intriguing, are not necessarily conclusive.
“The data was derived from a very large and well-conducted study,” Dr. McNeil, who has led other research on aspirin use and the elderly, said in an interview.
“But these conclusions were drawn from the observational component of the study and therefore potentially confounded by other characteristics that differentiate aspirin users from nonusers.”
Aspirin/cancer research in older people lacking
With well-known reports of decreased risks of heart disease, stroke, cancer – particularly gastrointestinal cancers – and all-cause mortality, as many as 25%-50% of adults in the U.S. report taking aspirin daily or every other day.
However, evidence of the benefits relating to cancer, specifically in older people, has been inconsistent, with one recent notable study, the randomized, double-blind ASPREE trial, showing no effect of aspirin on cancer incidence, but a higher mortality rate in elderly patients randomly assigned to aspirin for primary prevention.
To further investigate the effects in older patients, first author Holli A. Loomans-Kropp, PhD, and colleagues with the National Cancer Institute evaluated data on patients who were either 65 years or older at baseline or who had reached aged 65 during follow-up in the PLCO Cancer Screening Trial, which had enrollment from 1993 to 2001.
The authors identified 139,896 individuals with a mean age at baseline of 66.4 years; about half were women and 88.5% were non-Hispanic White.
Follow-up took place until the time of death, December 2014 for those who consented to follow-up, or December 2009 for those who refused consent to follow-up. The authors reported that there were 32,580 incident cancers, including 5.4% bladder, 14% breast, 1% esophageal, 1.2% gastric, 2.7% pancreatic, and 2.2% uterine cancers.
The study showed no association between aspirin use and the incidence of any of the cancer types included in the study among those over age 65.
However, further multivariate analysis of survival showed that, with follow-up adjusted to until the time of death, Dec. 31, 2015, or earlier refusal to consent, the use of aspirin at least three times per week was associated with reduced mortality in those with bladder (hazard ratio, 0.67) and breast (HR, 0.75) cancers, whereas no significant associations were observed with esophageal, gastric, pancreatic, or uterine cancer.
A similar association of any aspirin use (less than three times per week) with bladder (HR, 0.75) and breast (HR, 0.79) cancer survival was observed, the authors noted.
“These results may indicate that, for some cancer types, any aspirin use may be advantageous; however, greater benefit may be observed with increased frequency of use,” the authors wrote.
Mechanism speculation focuses on COX-2 pathway
Theories of the mechanisms behind a potential benefit of aspirin for those with bladder cancer include that urothelial cancer has increased RNA and protein expression of cyclooxygenase-2 (COX-2) and urinary prostaglandin E2, “suggesting up-regulation of the COX-2 pathway during cancer progression,” the authors wrote.
In breast cancer, a similar elevated expression of COX-2 has been shown to predict disease outcomes, including progression and decreased survival.
“This may be partly due to the mechanistic interplay between angiogenesis, cell proliferation, apoptosis, and inflammatory processes,” the authors noted.
The study isn’t the first to show a benefit specifically with bladder cancer; other studies include recent research (J Urol. 2018 Nov;200[5]:1014-21) showing that daily aspirin use among patients with bladder cancer was associated with increased 5-year survival following radical cystectomy, the authors noted.
Dr. McNeil noted that the new findings from the U.S. researchers, particularly regarding bladder cancer, are of interest. “The reduction in mortality from breast cancer is modest, but the reduction in mortality from bladder cancer was more impressive,” he said.
“However, given the fact that this finding is observational data and was a sole finding among multiple comparisons, it must be seen as suggestive rather than proven.”
Regarding possible mechanisms, Dr. McNeil added that, like the bulk of the prior research, many questions remain.
“There have been many suggestions about ways that aspirin might work at a molecular and cellular level, but no firm consensus has been reached.”
The study authors and Dr. McNeil disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 vaccination in cancer patients: NCCN outlines priorities
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Model predicts acute kidney injury in cancer patients a month in advance
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
FROM AACR: AI, DIAGNOSIS, AND IMAGING 2021
PCPs play a small part in low-value care spending
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.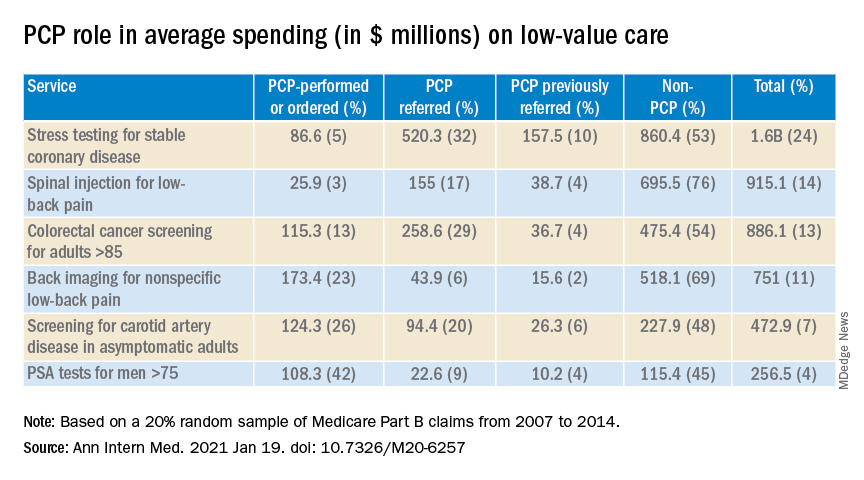
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.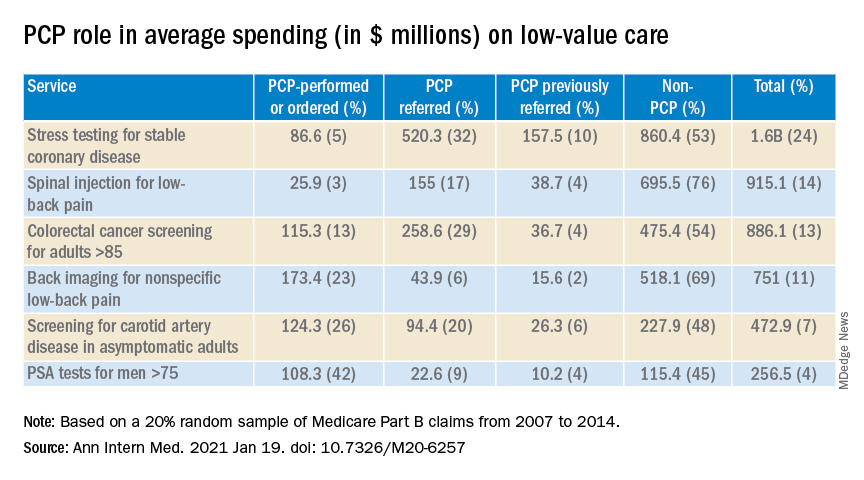
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a brief report published online Jan. 18 in Annals of Internal Medicine.
However, one expert said there are better ways to curb low-value care than focusing on which specialties are guilty of the practice.
Analyzing a 20% random sample of Medicare Part B claims, Aaron Baum, PhD, with the Icahn School of Medicine at Mount Sinai, New York, and colleagues found that the services primary care physicians performed or ordered made up on average 8.3% of the low-value care their patients received (interquartile range, 3.9%-15.1%; 95th percentile, 35.6%) and their referrals made up 15.4% (IQR, 6.3%-26.4%; 95th percentile, 44.6%).
By specialty, cardiology had the worst record with 27% of all spending on low-value services ($1.8 billion) attributed to that specialty. Yet, of the 25 highest-spending specialties in the report, 12 of them were associated with 1% or less than 1% each of all low-value spending, indicating the waste was widely distributed.
Dr. Baum said in an interview that though there are some PCPs guilty of high spending on low-value services, overall, most primary care physicians’ low-value services add up to only 0.3% of Part B spending. He noted that Part B spending is about one-third of all Medicare spending.
Primary care is often thought to be at the core of care management and spending and PCPs are often seen as the gatekeepers, but this analysis suggests that efforts to make big differences in curtailing low-value spending might be more effective elsewhere.
“There’s only so much spending you can reduce by changing primary care physicians’ services that they directly perform,” Dr. Baum said.
Low-value care is costly, can be harmful
Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, said in an interview that the report adds confirmation to previous research that has consistently shown low-value care is “extremely common, very costly, and provided by primary care providers and specialists alike.” He noted that it can also be harmful.
“The math is simple,” he said. “If we want to improve coverage and lower patient costs for essential services like visits, diagnostic tests, and drugs, we have to reduce spending on those services that do not make Americans any healthier.”
The study ranked 31 clinical services judged to be low value by physician societies, Medicare and clinical guidelines, and their use among beneficiaries enrolled between 2007 and 2014. Here’s how the top six low-value services compare.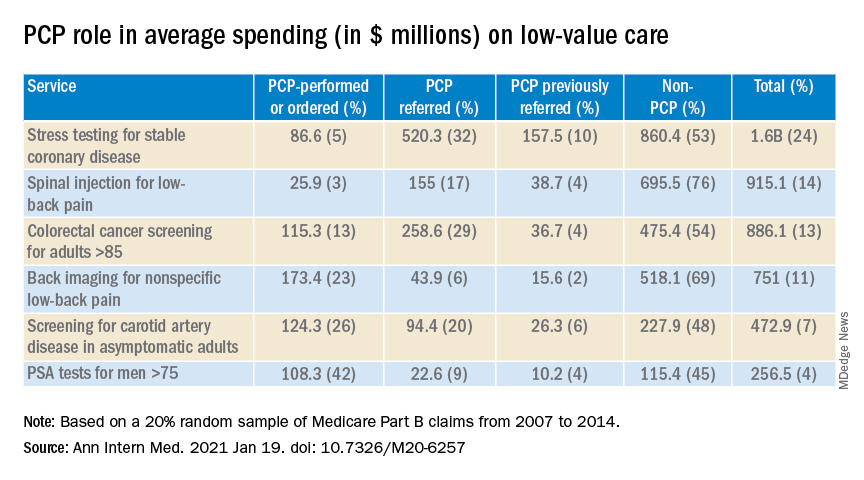
Dr. Fendrick said a weakness of the paper is the years of the data (2007-2014). Some of the criteria around low-value care have changed since then. The age that a prostate-specific antigen test becomes low-value is now 70 years, for instance, instead of 75. He added that some of the figures attributed to non-PCP providers appear out of date.
Dr. Fendrick said, “I understand that there are Medicare patients who end up at a gastroenterologist or surgeon’s office to get colorectal cancer screening, but it would be very hard for me to believe that half of stress tests and over half of colon cancer screening over [age] 85 [years] and half of PSA for people over 75 did not have some type of referring clinicians involved. I certainly don’t think that would be the case in 2020-2021.”
Dr. Baum said those years were the latest years available for the data points needed for this analysis, but he and his colleagues were working to update the data for future publication.
Dr. Fendrick said not much has changed in recent years in terms of waste on low-value care, even with campaigns such as Choosing Wisely dedicated to identifying low-value services or procedures in each specialty.
“I believe there’s not a particular group of clinicians one way or the other who are actually doing any better now than they were 7 years ago,” he said. He would rather focus less on which specialties are associated with the most low-value care and more on the underlying policies that encourage low-value care.
“If you’re going to get paid for doing a stress test and get paid nothing or significantly less if you don’t, the incentives are in the wrong direction,” he said.
Dr. Fendrick said the pandemic era provides an opportunity to eliminate low-value care because use of those services has dropped drastically as resources have been diverted to COVID-19 patients and many services have been delayed or canceled.
He said he has been pushing an approach that providers should be paid more after the pandemic “to do the things we want them to do.”
As an example, he said, instead of paying $886 million on colonoscopies for people over the age of 85, “why don’t we put a policy in place that would make it better for patients by lowering cost sharing and better for providers by paying them more to do the service on the people who need it as opposed to the people who don’t?”
The research was funded by the American Board of Family Medicine Foundation. Dr. Baum and a coauthor reported receiving personal fees from American Board of Family Medicine Foundation during the conduct of the study. Another coauthor reported receiving personal fees from Collective Health, HealthRight 360, PLOS Medicine, and the New England Journal of Medicine, outside the submitted work. Dr. Fendrick disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Family physicians can help achieve national goals on STIs
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.
U.S. cancer death rates drop for second year in a row
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.






