User login
Age-Friendly Health Systems and Meeting the Principles of High Reliability Organizations in the VHA
The Veterans Health Administration (VHA) is the largest integrated health care system in the US, providing care to more than 9 million enrolled veterans at 1298 facilities.1 In February 2019, the VHA identified key action steps to become a high reliability organization (HRO), transforming how employees think about patient safety and care quality.2 The VHA is also working toward becoming the largest age-friendly health system in the US to be recognized by the Institute for Healthcare Improvement (IHI) for its commitment to providing care guided by the 4Ms (what matters, medication, mentation, and mobility), causing no harm, and aligning care with what matters to older veterans.3 In this article, we describe how the Age-Friendly Health Systems (AFHS) movement supports the culture shift observed in HROs.
Age-Friendly Veteran Care
By 2060, the US population of adults aged ≥ 65 years is projected to increase to about 95 million.3 In the VHA, nearly half of veteran enrollees are aged ≥ 65 years, necessitating evidence-based models of care, such as the 4Ms, to meet their complex care needs.3 Historically, the VHA has been a leader in caring for older adults, recognizing the value of age-friendly care for veterans.4 In 1975, the VHA established the Geriatric Research, Education, and Clinical Centers (GRECCs) to serve as catalysts for developing, implementing, and refining enduring models of geriatric care.4 For 5 decades, GRECCs have driven innovations related to the 4Ms.
The VHA is well positioned to be a leader in the AFHS movement, building on decades of GRECC innovations and geriatric programs that align with the 4Ms and providing specialized geriatric training for health care professionals to expand age-friendly care to new settings and health systems.4 The AFHS movement organizes the 4Ms into a simple framework for frontline staff, and the VHA has recently begun tracking 4Ms care in the electronic health record (EHR) to facilitate evaluation and continuous improvement.
AFHS use the 4Ms as a framework to be implemented in every care setting, from the emergency department to inpatient units, outpatient settings, and postacute and long-term care. By assessing and acting on each M and practicing the 4Ms collectively, all members of the care team work to improve health outcomes and prevent avoidable harm.5
The 4Ms
What matters, is the driver of this person-centered approach. Any member of the care team may initiate a what matters conversation with the older adult to understand their personal values, health goals, and care preferences. When compared with usual care, care aligned with the older adult’s health priorities has been shown to decrease the use of high-risk medications and reduce treatment burden.6 The VHA has adopted Whole Health principles of care and the Patient Priorities Care approach to identify and support what matters to veterans.7,8
Addressing polypharmacy and identifying and deprescribing potentially inappropriate medications are essential in preventing adverse drug events, drug-drug interactions, and medication nonadherence.9 In the VHA, VIONE (Vital, Important, Optional, Not indicated, Every medication has an indication) is a rapidly expanding medication deprescribing program that exemplifies HRO principles.9 VIONE provides medication management that supports shared decision making, reducing risk and improving patient safety and quality of life.9 As of June 2023, > 600,000 unique veterans have benefited from VIONE, with an average of 2.2 medications deprescribed per patient with an annual cost avoidance of > $100 million.10
Assessing and acting on mentation includes preventing, identifying, and managing depression and dementia in outpatient settings and delirium in hospital and long-term care settings.5 There are many tools and clinical reminders available in the EHR so that interdisciplinary teams can document changes to mentation and identify opportunities for continuous improvement.
Closely aligned with mentation is mobility, with evidence suggesting that regular physical activity reduces the risk of falls (preventing associated complications), maintains physical functioning, and lowers the risk of cognitive impairment and depression.5 Ensuring early, frequent, and safe mobility helps patients achieve better health outcomes and prevent injury.5 Mobility programs within the VHA include the STRIDE program for the inpatient setting and Gerofit for outpatient settings.11,12
HRO Principles
An HRO is a complex environment of care that experiences fewer than anticipated accidents or adverse events by (1) establishing trust among leaders and staff by balancing individual accountability with systems thinking; (2) empowering staff to lead continuous process improvements; and (3) creating an environment where employees feel safe to report harm or near misses, focusing on the reasons errors occur.13 The work of AFHS incorporates HRO principles with an emphasis on 3 elements. First, it involves interactive systems and processes needed to support 4Ms care across care settings. Second, AFHS acknowledge the complexity of age-friendly work and deference to the expertise of interdisciplinary team members. Finally, AFHS are committed to resilience by overcoming failures and challenges to implementation and long-term sustainment as a standard of practice.
Case study
The names and details in this case have been modified to protect patient privacy. It is representative of many Community Living Centers (CLCs) involved in AFHS that work to create a safe, person-centered environment for veterans.
In a CLC team workroom, 2 nurses were discussing a long-term care resident. The nurses approached the attending physician and explained that they were worried about Sgt Johnson, who seemed depressed and sometimes combative. They had noticed a change in his behavior when they helped him clean up after an episode of incontinence and were concerned that he would try to get out of bed on his own and fall. The attending physician thanked them for sharing their concerns. Sgt Johnson was a retired Army veteran who had a long, decorated military career. His chronic health conditions had led to muscle weakness, and he fell and broke a hip before this admission. He had an uneventful hip replacement but was showing signs of depression due to his limited mobility, loss of independence, and inability to live at home without additional support.
The attending physician knocked on the door of his room, sat down next to the bed, and asked, “How are you feeling today?” Sgt Johnson tersely replied, “About the same.” The physician asked, “Sgt Johnson, what matters most to you related to your recovery? What is important to you?” Sgt Johnson responded, “Feeling like a man!” The doctor replied, “So what makes you feel ‘not like a man’?” The Sgt replied, “Having to be cleaned up by the nurses and not being able to use the toilet on my own.” The physician surmised that his decline in physical functioning had a connection to his worsening depression and combativeness and said to the Sgt, “Let’s get the team together and work out a plan to get you strong enough to use a bedside commode by yourself. Let’s make that the first goal in our plan to get you back to using the toilet independently. Can you work with us on that?” He smiled and said, “Sir, yes Sir!”
At the weekly interdisciplinary team meeting, the team discussed Sgt Johnson’s wishes and the nurses’ safety concerns. The physician reported to the team what mattered to the veteran. The nurses arranged for a bedside commode and supplies to be placed in his room, encouraged and assisted him, and provided a privacy screen. The physical therapist continued to support his mobility needs, concentrating on transfers, small steps like standing and turning with a walker to get in position to use the bedside commode, and later the bathroom toilet. The psychologist addressed what matters to Sgt Johnson and his mentation, health goals, and coping strategies. The social worker provided support and counseling for the veteran and his family. The pharmacist checked his medications to be sure that none were affecting his gastrointestinal tract and his ability to move safely and do what matters to him. Knowing what mattered to Sgt Johnson was the driver of the interdisciplinary care plan to provide 4Ms care.
The team worked collaboratively with the veteran to develop and set attainable goals around toileting and regaining his dignity. This improved his overall recovery. As Sgt Johnson became more independent, his mood gradually improved and he began to participate in other activities and interact with other residents on the unit, and he did not experience any falls. By addressing the 4Ms, the interdisciplinary team coordinated efforts to provide high-quality, person-centered care. They built trust with the veteran, shared accountability, and followed HRO principles to keep the veteran safe.
Becoming an Age-Friendly HRO
Becoming an HRO is a dynamic, ever-changing process to maintain high standards, improve care quality, and cause no harm. There are 3 pillars and 5 principles that guide an HRO. The pillars are critical areas of focus and include leadership commitment, culture of safety, and continuous process improvement.14 The first of 5 HRO principles is sensitivity to operations. This is defined as an awareness of how processes and systems impact the entire organization, the downstream impact.15 Focusing on the 4Ms helps develop the capability of frontline staff to provide high-quality care for older adults while ensuring that processes are in place to support the work. The 4Ms provide an efficient way to organize interdisciplinary team meetings, provide warm handoffs using Situation-Background-Assessment-Recommendation, and standardize documentation. Involvement in the AFHS movement improves communication, care quality, and patient and staff satisfaction to meet this HRO principle.15
The second HRO principle, reluctance to simplify, ensures that direct care staff and leaders delve further into issues to find solutions.15 AFHS use the Plan-Do-Study-Act cycle to put the 4Ms into practice; this cycle helps teams test small increments of change, study their performance, and act to ensure that all 4Ms are being practiced as a set. AFHS teams are encouraged to review at least 3 months of data after implementation of the 4Ms, working to find solutions if there are gaps or issues identified.
The third principle, preoccupation with failure, refers to shared attentiveness—being prepared for the unexpected and learning from mistakes.15 The entire AFHS team shares responsibility for providing 4Ms care, where staff are empowered to report any safety concerns or close calls. The fourth principle of deference to expertise includes listening to staff who have the most knowledge for the task at hand, which aligns with the collaborative interdisciplinary teamwork of age-friendly teams.15
The final HRO principle, commitment to resilience, includes continuous learning, interdisciplinary team training, and sharing of lessons learned.15 Although IHI offers 2 levels of AFHS recognition, teams are continuously learning to improve and sustain care beyond level 2, Committed to Care Excellence recognition.16
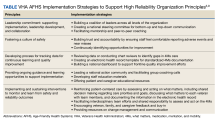
The Table shows the VHA’s AFHS implementation strategies and the HRO principles adapted from the Joint Commission’s High Reliability Health Care Maturity Model and the IHI’s Framework for Safe, Reliable, and Effective Care. The VHA is developing a national dashboard to capture age-friendly processes and health outcome measures that address patient safety and care quality.
Conclusions
AFHS empowers VHA teams to honor veterans’ care preferences and values, supporting their independence, dignity, and quality of life across care settings. The adoption of AFHS brings evidence-based practices to the point of care by addressing common pitfalls in the care of older adults, drawing attention to, and calling for action on inappropriate medication use, physical inactivity, and assessment of the vulnerable brain. The 4Ms also serve as a framework to continuously improve care and cause zero harm, reinforcing HRO pillars and principles across the VHA, and ensuring that older adults reliably receive the evidence-based, high-quality care they deserve.
1. Veterans Health Administration. Providing healthcare for veterans. Updated June 20, 2023. Accessed June 26, 2023. https://www.va.gov/health
2. Veazie S, Peterson K, Bourne D. Evidence brief: implementation of high reliability organization principles. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-199; 2019. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/esp/high-reliability-org.cfm
3. Church K, Munro S, Shaughnessy M, Clancy C. Age-Friendly Health Systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58(suppl 1):5-8. doi:10.1111/1475-6773.14110
4. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
5. Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7-8):469-481. doi:10.1177/0898264321991658
6. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: A nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688-1697. doi:10.1001/jamainternmed.2019.4235
7. US Department of Veterans Affairs. What is whole health? Updated: October 31, 2023. November 30, 2023. https://www.va.gov/wholehealth
8. Patient Priorities Care. Updated 2019. Accessed November 30, 2023. https://patientprioritiescare.org
9. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
10. VA Diffusion Marketplace. VIONE- medication optimization and polypharmacy reduction initiative. Accessed November 30, 2023. https://marketplace.va.gov/innovations/vione
11. US Department of Veterans Affairs, Office of Research and Development. STRIDE program to keep hospitalized veterans mobile. Updated November 6, 2018. Accessed November 30, 2023. https://www.research.va.gov/research_in_action/STRIDE-program-to-keep-hospitalized-Veterans-mobile.cfm
12. US Department of Veterans Affairs, VA Geriatrics and Extended Care. Gerofit: a program promoting exercise and health for older veterans. Updated August 2, 2023. Accessed November 30, 2023. https://www.va.gov/GERIATRICS/pages/gerofit_Home.asp
13. US Department of Veterans Affairs, Health Services Research and Development. VHA’s vision for a high reliability organization. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
14. US Department of Veterans Affairs, Health Services Research and Development. Three HRO evaluation priorities. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-2
15. Oster CA, Deakins S. Practical application of high-reliability principles in healthcare to optimize quality and safety outcomes. J Nurs Adm. 2018;48(1):50-55. doi:10.1097/NNA.0000000000000570
16. Institute for Healthcare Improvement. Age-Friendly Health Systems recognitions. Accessed November 30, 2023. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/Recognition.aspx
The Veterans Health Administration (VHA) is the largest integrated health care system in the US, providing care to more than 9 million enrolled veterans at 1298 facilities.1 In February 2019, the VHA identified key action steps to become a high reliability organization (HRO), transforming how employees think about patient safety and care quality.2 The VHA is also working toward becoming the largest age-friendly health system in the US to be recognized by the Institute for Healthcare Improvement (IHI) for its commitment to providing care guided by the 4Ms (what matters, medication, mentation, and mobility), causing no harm, and aligning care with what matters to older veterans.3 In this article, we describe how the Age-Friendly Health Systems (AFHS) movement supports the culture shift observed in HROs.
Age-Friendly Veteran Care
By 2060, the US population of adults aged ≥ 65 years is projected to increase to about 95 million.3 In the VHA, nearly half of veteran enrollees are aged ≥ 65 years, necessitating evidence-based models of care, such as the 4Ms, to meet their complex care needs.3 Historically, the VHA has been a leader in caring for older adults, recognizing the value of age-friendly care for veterans.4 In 1975, the VHA established the Geriatric Research, Education, and Clinical Centers (GRECCs) to serve as catalysts for developing, implementing, and refining enduring models of geriatric care.4 For 5 decades, GRECCs have driven innovations related to the 4Ms.
The VHA is well positioned to be a leader in the AFHS movement, building on decades of GRECC innovations and geriatric programs that align with the 4Ms and providing specialized geriatric training for health care professionals to expand age-friendly care to new settings and health systems.4 The AFHS movement organizes the 4Ms into a simple framework for frontline staff, and the VHA has recently begun tracking 4Ms care in the electronic health record (EHR) to facilitate evaluation and continuous improvement.
AFHS use the 4Ms as a framework to be implemented in every care setting, from the emergency department to inpatient units, outpatient settings, and postacute and long-term care. By assessing and acting on each M and practicing the 4Ms collectively, all members of the care team work to improve health outcomes and prevent avoidable harm.5
The 4Ms
What matters, is the driver of this person-centered approach. Any member of the care team may initiate a what matters conversation with the older adult to understand their personal values, health goals, and care preferences. When compared with usual care, care aligned with the older adult’s health priorities has been shown to decrease the use of high-risk medications and reduce treatment burden.6 The VHA has adopted Whole Health principles of care and the Patient Priorities Care approach to identify and support what matters to veterans.7,8
Addressing polypharmacy and identifying and deprescribing potentially inappropriate medications are essential in preventing adverse drug events, drug-drug interactions, and medication nonadherence.9 In the VHA, VIONE (Vital, Important, Optional, Not indicated, Every medication has an indication) is a rapidly expanding medication deprescribing program that exemplifies HRO principles.9 VIONE provides medication management that supports shared decision making, reducing risk and improving patient safety and quality of life.9 As of June 2023, > 600,000 unique veterans have benefited from VIONE, with an average of 2.2 medications deprescribed per patient with an annual cost avoidance of > $100 million.10
Assessing and acting on mentation includes preventing, identifying, and managing depression and dementia in outpatient settings and delirium in hospital and long-term care settings.5 There are many tools and clinical reminders available in the EHR so that interdisciplinary teams can document changes to mentation and identify opportunities for continuous improvement.
Closely aligned with mentation is mobility, with evidence suggesting that regular physical activity reduces the risk of falls (preventing associated complications), maintains physical functioning, and lowers the risk of cognitive impairment and depression.5 Ensuring early, frequent, and safe mobility helps patients achieve better health outcomes and prevent injury.5 Mobility programs within the VHA include the STRIDE program for the inpatient setting and Gerofit for outpatient settings.11,12
HRO Principles
An HRO is a complex environment of care that experiences fewer than anticipated accidents or adverse events by (1) establishing trust among leaders and staff by balancing individual accountability with systems thinking; (2) empowering staff to lead continuous process improvements; and (3) creating an environment where employees feel safe to report harm or near misses, focusing on the reasons errors occur.13 The work of AFHS incorporates HRO principles with an emphasis on 3 elements. First, it involves interactive systems and processes needed to support 4Ms care across care settings. Second, AFHS acknowledge the complexity of age-friendly work and deference to the expertise of interdisciplinary team members. Finally, AFHS are committed to resilience by overcoming failures and challenges to implementation and long-term sustainment as a standard of practice.
Case study
The names and details in this case have been modified to protect patient privacy. It is representative of many Community Living Centers (CLCs) involved in AFHS that work to create a safe, person-centered environment for veterans.
In a CLC team workroom, 2 nurses were discussing a long-term care resident. The nurses approached the attending physician and explained that they were worried about Sgt Johnson, who seemed depressed and sometimes combative. They had noticed a change in his behavior when they helped him clean up after an episode of incontinence and were concerned that he would try to get out of bed on his own and fall. The attending physician thanked them for sharing their concerns. Sgt Johnson was a retired Army veteran who had a long, decorated military career. His chronic health conditions had led to muscle weakness, and he fell and broke a hip before this admission. He had an uneventful hip replacement but was showing signs of depression due to his limited mobility, loss of independence, and inability to live at home without additional support.
The attending physician knocked on the door of his room, sat down next to the bed, and asked, “How are you feeling today?” Sgt Johnson tersely replied, “About the same.” The physician asked, “Sgt Johnson, what matters most to you related to your recovery? What is important to you?” Sgt Johnson responded, “Feeling like a man!” The doctor replied, “So what makes you feel ‘not like a man’?” The Sgt replied, “Having to be cleaned up by the nurses and not being able to use the toilet on my own.” The physician surmised that his decline in physical functioning had a connection to his worsening depression and combativeness and said to the Sgt, “Let’s get the team together and work out a plan to get you strong enough to use a bedside commode by yourself. Let’s make that the first goal in our plan to get you back to using the toilet independently. Can you work with us on that?” He smiled and said, “Sir, yes Sir!”
At the weekly interdisciplinary team meeting, the team discussed Sgt Johnson’s wishes and the nurses’ safety concerns. The physician reported to the team what mattered to the veteran. The nurses arranged for a bedside commode and supplies to be placed in his room, encouraged and assisted him, and provided a privacy screen. The physical therapist continued to support his mobility needs, concentrating on transfers, small steps like standing and turning with a walker to get in position to use the bedside commode, and later the bathroom toilet. The psychologist addressed what matters to Sgt Johnson and his mentation, health goals, and coping strategies. The social worker provided support and counseling for the veteran and his family. The pharmacist checked his medications to be sure that none were affecting his gastrointestinal tract and his ability to move safely and do what matters to him. Knowing what mattered to Sgt Johnson was the driver of the interdisciplinary care plan to provide 4Ms care.
The team worked collaboratively with the veteran to develop and set attainable goals around toileting and regaining his dignity. This improved his overall recovery. As Sgt Johnson became more independent, his mood gradually improved and he began to participate in other activities and interact with other residents on the unit, and he did not experience any falls. By addressing the 4Ms, the interdisciplinary team coordinated efforts to provide high-quality, person-centered care. They built trust with the veteran, shared accountability, and followed HRO principles to keep the veteran safe.
Becoming an Age-Friendly HRO
Becoming an HRO is a dynamic, ever-changing process to maintain high standards, improve care quality, and cause no harm. There are 3 pillars and 5 principles that guide an HRO. The pillars are critical areas of focus and include leadership commitment, culture of safety, and continuous process improvement.14 The first of 5 HRO principles is sensitivity to operations. This is defined as an awareness of how processes and systems impact the entire organization, the downstream impact.15 Focusing on the 4Ms helps develop the capability of frontline staff to provide high-quality care for older adults while ensuring that processes are in place to support the work. The 4Ms provide an efficient way to organize interdisciplinary team meetings, provide warm handoffs using Situation-Background-Assessment-Recommendation, and standardize documentation. Involvement in the AFHS movement improves communication, care quality, and patient and staff satisfaction to meet this HRO principle.15
The second HRO principle, reluctance to simplify, ensures that direct care staff and leaders delve further into issues to find solutions.15 AFHS use the Plan-Do-Study-Act cycle to put the 4Ms into practice; this cycle helps teams test small increments of change, study their performance, and act to ensure that all 4Ms are being practiced as a set. AFHS teams are encouraged to review at least 3 months of data after implementation of the 4Ms, working to find solutions if there are gaps or issues identified.
The third principle, preoccupation with failure, refers to shared attentiveness—being prepared for the unexpected and learning from mistakes.15 The entire AFHS team shares responsibility for providing 4Ms care, where staff are empowered to report any safety concerns or close calls. The fourth principle of deference to expertise includes listening to staff who have the most knowledge for the task at hand, which aligns with the collaborative interdisciplinary teamwork of age-friendly teams.15
The final HRO principle, commitment to resilience, includes continuous learning, interdisciplinary team training, and sharing of lessons learned.15 Although IHI offers 2 levels of AFHS recognition, teams are continuously learning to improve and sustain care beyond level 2, Committed to Care Excellence recognition.16
The Table shows the VHA’s AFHS implementation strategies and the HRO principles adapted from the Joint Commission’s High Reliability Health Care Maturity Model and the IHI’s Framework for Safe, Reliable, and Effective Care. The VHA is developing a national dashboard to capture age-friendly processes and health outcome measures that address patient safety and care quality.
Conclusions
AFHS empowers VHA teams to honor veterans’ care preferences and values, supporting their independence, dignity, and quality of life across care settings. The adoption of AFHS brings evidence-based practices to the point of care by addressing common pitfalls in the care of older adults, drawing attention to, and calling for action on inappropriate medication use, physical inactivity, and assessment of the vulnerable brain. The 4Ms also serve as a framework to continuously improve care and cause zero harm, reinforcing HRO pillars and principles across the VHA, and ensuring that older adults reliably receive the evidence-based, high-quality care they deserve.
The Veterans Health Administration (VHA) is the largest integrated health care system in the US, providing care to more than 9 million enrolled veterans at 1298 facilities.1 In February 2019, the VHA identified key action steps to become a high reliability organization (HRO), transforming how employees think about patient safety and care quality.2 The VHA is also working toward becoming the largest age-friendly health system in the US to be recognized by the Institute for Healthcare Improvement (IHI) for its commitment to providing care guided by the 4Ms (what matters, medication, mentation, and mobility), causing no harm, and aligning care with what matters to older veterans.3 In this article, we describe how the Age-Friendly Health Systems (AFHS) movement supports the culture shift observed in HROs.
Age-Friendly Veteran Care
By 2060, the US population of adults aged ≥ 65 years is projected to increase to about 95 million.3 In the VHA, nearly half of veteran enrollees are aged ≥ 65 years, necessitating evidence-based models of care, such as the 4Ms, to meet their complex care needs.3 Historically, the VHA has been a leader in caring for older adults, recognizing the value of age-friendly care for veterans.4 In 1975, the VHA established the Geriatric Research, Education, and Clinical Centers (GRECCs) to serve as catalysts for developing, implementing, and refining enduring models of geriatric care.4 For 5 decades, GRECCs have driven innovations related to the 4Ms.
The VHA is well positioned to be a leader in the AFHS movement, building on decades of GRECC innovations and geriatric programs that align with the 4Ms and providing specialized geriatric training for health care professionals to expand age-friendly care to new settings and health systems.4 The AFHS movement organizes the 4Ms into a simple framework for frontline staff, and the VHA has recently begun tracking 4Ms care in the electronic health record (EHR) to facilitate evaluation and continuous improvement.
AFHS use the 4Ms as a framework to be implemented in every care setting, from the emergency department to inpatient units, outpatient settings, and postacute and long-term care. By assessing and acting on each M and practicing the 4Ms collectively, all members of the care team work to improve health outcomes and prevent avoidable harm.5
The 4Ms
What matters, is the driver of this person-centered approach. Any member of the care team may initiate a what matters conversation with the older adult to understand their personal values, health goals, and care preferences. When compared with usual care, care aligned with the older adult’s health priorities has been shown to decrease the use of high-risk medications and reduce treatment burden.6 The VHA has adopted Whole Health principles of care and the Patient Priorities Care approach to identify and support what matters to veterans.7,8
Addressing polypharmacy and identifying and deprescribing potentially inappropriate medications are essential in preventing adverse drug events, drug-drug interactions, and medication nonadherence.9 In the VHA, VIONE (Vital, Important, Optional, Not indicated, Every medication has an indication) is a rapidly expanding medication deprescribing program that exemplifies HRO principles.9 VIONE provides medication management that supports shared decision making, reducing risk and improving patient safety and quality of life.9 As of June 2023, > 600,000 unique veterans have benefited from VIONE, with an average of 2.2 medications deprescribed per patient with an annual cost avoidance of > $100 million.10
Assessing and acting on mentation includes preventing, identifying, and managing depression and dementia in outpatient settings and delirium in hospital and long-term care settings.5 There are many tools and clinical reminders available in the EHR so that interdisciplinary teams can document changes to mentation and identify opportunities for continuous improvement.
Closely aligned with mentation is mobility, with evidence suggesting that regular physical activity reduces the risk of falls (preventing associated complications), maintains physical functioning, and lowers the risk of cognitive impairment and depression.5 Ensuring early, frequent, and safe mobility helps patients achieve better health outcomes and prevent injury.5 Mobility programs within the VHA include the STRIDE program for the inpatient setting and Gerofit for outpatient settings.11,12
HRO Principles
An HRO is a complex environment of care that experiences fewer than anticipated accidents or adverse events by (1) establishing trust among leaders and staff by balancing individual accountability with systems thinking; (2) empowering staff to lead continuous process improvements; and (3) creating an environment where employees feel safe to report harm or near misses, focusing on the reasons errors occur.13 The work of AFHS incorporates HRO principles with an emphasis on 3 elements. First, it involves interactive systems and processes needed to support 4Ms care across care settings. Second, AFHS acknowledge the complexity of age-friendly work and deference to the expertise of interdisciplinary team members. Finally, AFHS are committed to resilience by overcoming failures and challenges to implementation and long-term sustainment as a standard of practice.
Case study
The names and details in this case have been modified to protect patient privacy. It is representative of many Community Living Centers (CLCs) involved in AFHS that work to create a safe, person-centered environment for veterans.
In a CLC team workroom, 2 nurses were discussing a long-term care resident. The nurses approached the attending physician and explained that they were worried about Sgt Johnson, who seemed depressed and sometimes combative. They had noticed a change in his behavior when they helped him clean up after an episode of incontinence and were concerned that he would try to get out of bed on his own and fall. The attending physician thanked them for sharing their concerns. Sgt Johnson was a retired Army veteran who had a long, decorated military career. His chronic health conditions had led to muscle weakness, and he fell and broke a hip before this admission. He had an uneventful hip replacement but was showing signs of depression due to his limited mobility, loss of independence, and inability to live at home without additional support.
The attending physician knocked on the door of his room, sat down next to the bed, and asked, “How are you feeling today?” Sgt Johnson tersely replied, “About the same.” The physician asked, “Sgt Johnson, what matters most to you related to your recovery? What is important to you?” Sgt Johnson responded, “Feeling like a man!” The doctor replied, “So what makes you feel ‘not like a man’?” The Sgt replied, “Having to be cleaned up by the nurses and not being able to use the toilet on my own.” The physician surmised that his decline in physical functioning had a connection to his worsening depression and combativeness and said to the Sgt, “Let’s get the team together and work out a plan to get you strong enough to use a bedside commode by yourself. Let’s make that the first goal in our plan to get you back to using the toilet independently. Can you work with us on that?” He smiled and said, “Sir, yes Sir!”
At the weekly interdisciplinary team meeting, the team discussed Sgt Johnson’s wishes and the nurses’ safety concerns. The physician reported to the team what mattered to the veteran. The nurses arranged for a bedside commode and supplies to be placed in his room, encouraged and assisted him, and provided a privacy screen. The physical therapist continued to support his mobility needs, concentrating on transfers, small steps like standing and turning with a walker to get in position to use the bedside commode, and later the bathroom toilet. The psychologist addressed what matters to Sgt Johnson and his mentation, health goals, and coping strategies. The social worker provided support and counseling for the veteran and his family. The pharmacist checked his medications to be sure that none were affecting his gastrointestinal tract and his ability to move safely and do what matters to him. Knowing what mattered to Sgt Johnson was the driver of the interdisciplinary care plan to provide 4Ms care.
The team worked collaboratively with the veteran to develop and set attainable goals around toileting and regaining his dignity. This improved his overall recovery. As Sgt Johnson became more independent, his mood gradually improved and he began to participate in other activities and interact with other residents on the unit, and he did not experience any falls. By addressing the 4Ms, the interdisciplinary team coordinated efforts to provide high-quality, person-centered care. They built trust with the veteran, shared accountability, and followed HRO principles to keep the veteran safe.
Becoming an Age-Friendly HRO
Becoming an HRO is a dynamic, ever-changing process to maintain high standards, improve care quality, and cause no harm. There are 3 pillars and 5 principles that guide an HRO. The pillars are critical areas of focus and include leadership commitment, culture of safety, and continuous process improvement.14 The first of 5 HRO principles is sensitivity to operations. This is defined as an awareness of how processes and systems impact the entire organization, the downstream impact.15 Focusing on the 4Ms helps develop the capability of frontline staff to provide high-quality care for older adults while ensuring that processes are in place to support the work. The 4Ms provide an efficient way to organize interdisciplinary team meetings, provide warm handoffs using Situation-Background-Assessment-Recommendation, and standardize documentation. Involvement in the AFHS movement improves communication, care quality, and patient and staff satisfaction to meet this HRO principle.15
The second HRO principle, reluctance to simplify, ensures that direct care staff and leaders delve further into issues to find solutions.15 AFHS use the Plan-Do-Study-Act cycle to put the 4Ms into practice; this cycle helps teams test small increments of change, study their performance, and act to ensure that all 4Ms are being practiced as a set. AFHS teams are encouraged to review at least 3 months of data after implementation of the 4Ms, working to find solutions if there are gaps or issues identified.
The third principle, preoccupation with failure, refers to shared attentiveness—being prepared for the unexpected and learning from mistakes.15 The entire AFHS team shares responsibility for providing 4Ms care, where staff are empowered to report any safety concerns or close calls. The fourth principle of deference to expertise includes listening to staff who have the most knowledge for the task at hand, which aligns with the collaborative interdisciplinary teamwork of age-friendly teams.15
The final HRO principle, commitment to resilience, includes continuous learning, interdisciplinary team training, and sharing of lessons learned.15 Although IHI offers 2 levels of AFHS recognition, teams are continuously learning to improve and sustain care beyond level 2, Committed to Care Excellence recognition.16
The Table shows the VHA’s AFHS implementation strategies and the HRO principles adapted from the Joint Commission’s High Reliability Health Care Maturity Model and the IHI’s Framework for Safe, Reliable, and Effective Care. The VHA is developing a national dashboard to capture age-friendly processes and health outcome measures that address patient safety and care quality.
Conclusions
AFHS empowers VHA teams to honor veterans’ care preferences and values, supporting their independence, dignity, and quality of life across care settings. The adoption of AFHS brings evidence-based practices to the point of care by addressing common pitfalls in the care of older adults, drawing attention to, and calling for action on inappropriate medication use, physical inactivity, and assessment of the vulnerable brain. The 4Ms also serve as a framework to continuously improve care and cause zero harm, reinforcing HRO pillars and principles across the VHA, and ensuring that older adults reliably receive the evidence-based, high-quality care they deserve.
1. Veterans Health Administration. Providing healthcare for veterans. Updated June 20, 2023. Accessed June 26, 2023. https://www.va.gov/health
2. Veazie S, Peterson K, Bourne D. Evidence brief: implementation of high reliability organization principles. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-199; 2019. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/esp/high-reliability-org.cfm
3. Church K, Munro S, Shaughnessy M, Clancy C. Age-Friendly Health Systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58(suppl 1):5-8. doi:10.1111/1475-6773.14110
4. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
5. Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7-8):469-481. doi:10.1177/0898264321991658
6. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: A nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688-1697. doi:10.1001/jamainternmed.2019.4235
7. US Department of Veterans Affairs. What is whole health? Updated: October 31, 2023. November 30, 2023. https://www.va.gov/wholehealth
8. Patient Priorities Care. Updated 2019. Accessed November 30, 2023. https://patientprioritiescare.org
9. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
10. VA Diffusion Marketplace. VIONE- medication optimization and polypharmacy reduction initiative. Accessed November 30, 2023. https://marketplace.va.gov/innovations/vione
11. US Department of Veterans Affairs, Office of Research and Development. STRIDE program to keep hospitalized veterans mobile. Updated November 6, 2018. Accessed November 30, 2023. https://www.research.va.gov/research_in_action/STRIDE-program-to-keep-hospitalized-Veterans-mobile.cfm
12. US Department of Veterans Affairs, VA Geriatrics and Extended Care. Gerofit: a program promoting exercise and health for older veterans. Updated August 2, 2023. Accessed November 30, 2023. https://www.va.gov/GERIATRICS/pages/gerofit_Home.asp
13. US Department of Veterans Affairs, Health Services Research and Development. VHA’s vision for a high reliability organization. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
14. US Department of Veterans Affairs, Health Services Research and Development. Three HRO evaluation priorities. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-2
15. Oster CA, Deakins S. Practical application of high-reliability principles in healthcare to optimize quality and safety outcomes. J Nurs Adm. 2018;48(1):50-55. doi:10.1097/NNA.0000000000000570
16. Institute for Healthcare Improvement. Age-Friendly Health Systems recognitions. Accessed November 30, 2023. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/Recognition.aspx
1. Veterans Health Administration. Providing healthcare for veterans. Updated June 20, 2023. Accessed June 26, 2023. https://www.va.gov/health
2. Veazie S, Peterson K, Bourne D. Evidence brief: implementation of high reliability organization principles. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-199; 2019. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/esp/high-reliability-org.cfm
3. Church K, Munro S, Shaughnessy M, Clancy C. Age-Friendly Health Systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58(suppl 1):5-8. doi:10.1111/1475-6773.14110
4. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
5. Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7-8):469-481. doi:10.1177/0898264321991658
6. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: A nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688-1697. doi:10.1001/jamainternmed.2019.4235
7. US Department of Veterans Affairs. What is whole health? Updated: October 31, 2023. November 30, 2023. https://www.va.gov/wholehealth
8. Patient Priorities Care. Updated 2019. Accessed November 30, 2023. https://patientprioritiescare.org
9. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
10. VA Diffusion Marketplace. VIONE- medication optimization and polypharmacy reduction initiative. Accessed November 30, 2023. https://marketplace.va.gov/innovations/vione
11. US Department of Veterans Affairs, Office of Research and Development. STRIDE program to keep hospitalized veterans mobile. Updated November 6, 2018. Accessed November 30, 2023. https://www.research.va.gov/research_in_action/STRIDE-program-to-keep-hospitalized-Veterans-mobile.cfm
12. US Department of Veterans Affairs, VA Geriatrics and Extended Care. Gerofit: a program promoting exercise and health for older veterans. Updated August 2, 2023. Accessed November 30, 2023. https://www.va.gov/GERIATRICS/pages/gerofit_Home.asp
13. US Department of Veterans Affairs, Health Services Research and Development. VHA’s vision for a high reliability organization. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-1
14. US Department of Veterans Affairs, Health Services Research and Development. Three HRO evaluation priorities. Updated August 14, 2020. Accessed November 30, 2023. https://www.hsrd.research.va.gov/publications/forum/summer20/default.cfm?ForumMenu=summer20-2
15. Oster CA, Deakins S. Practical application of high-reliability principles in healthcare to optimize quality and safety outcomes. J Nurs Adm. 2018;48(1):50-55. doi:10.1097/NNA.0000000000000570
16. Institute for Healthcare Improvement. Age-Friendly Health Systems recognitions. Accessed November 30, 2023. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/Recognition.aspx
JAMA Internal Medicine Editor Recaps 2023’s High-Impact Research
Harvard Medical School’s Sharon K. Inouye, MD, MPH, is editor in chief of JAMA Internal Medicine and a leading voice in American gerontology. We asked her to choose five of the influential journal’s most impactful studies from 2023 and highlight important take-home messages for internists and their colleagues.
Q: One of the studies you chose suggests that the antiviral nirmatrelvir (Paxlovid) can ward off long COVID. Could you recap the findings?
A: Researchers followed a group of more than 280,000 Department of Veterans Affairs patients who were seen in 2022, had a positive COVID test, and had at least one risk factor for severe COVID. They focused on those who survived to 30 days after their COVID infection and compared those who received the drug within the first 5 days of a positive test with an equivalent control group.
They found that 13 long COVID symptoms were all significantly less common (relative risk = 0.74) in those who received nirmatrelvir. This was true no matter whether they’d ever had a COVID vaccination.
Q: How should this research affect clinical practice?
A: You can’t generalize from this to everyone because, of course, not everyone was included in this study. But it is highly suggestive that this drug is very effective for preventing long COVID.
Nirmatrelvir was touted as being able to shorten duration of illness and prevent hospitalization. But if you were low risk or you were already well into your COVID course, it wasn’t like rush, rush, rush to the doctor to get it.
This changes that equation because we know long COVID is such a huge issue. The vast majority of doctors who work with COVID patients and know this are now being more aggressive about prescribing it.
Q: What about patients whom the CDC considers to be at less risk — people with up-to-date vaccinations who are under 50 with mild-to-moderate COVID and no higher-risk medical conditions? Should they take nirmatrelvir?
A: The evidence is not 100% in yet. A study like this one needs to be repeated and include younger people without any risk factors to see if we see the same thing. So it’s a personal choice, and a personal calculus needs to be done. A lot of people are making that choice [to take the drug], and it can be a rational decision.
Q: You also chose a study that links high thyroid hormone levels to higher rates of dementia. What did it reveal?
A: This study looks at patients who had thyrotoxicosis — a thyroid level that’s too high — from hormone produced endogenously, and exogenously. Researchers tracked almost 66,000 patients aged 65 and older and found that thyrotoxicosis from all causes, whether it was endogenous or exogenous, was linked to an increased risk of dementia in a dose-response relationship (adjusted hazard ratio = 1.39).
Q: Is there a clinical take-home message here?
A: When we start patients on thyroid medication, they don’t always get reassessed on a regular basis. Given this finding, a TSH [thyroid-stimulating hormone] level is indicated during the annual wellness check that patients on Medicare can get every year.
Q: Is TSH measured as part of routine blood tests?
A: No it’s not. It has to be ordered. I think that’s why we’re seeing this problem to begin with — because it’s not something we all have awareness about. I wasn’t aware myself that mildly high levels of thyroid could increase the risk of cognitive impairment. Certainly, I’m going to be much more aware in my practice.
Q: You also picked a study about silicosis in workers who are exposed to dust when they make engineered stone countertops, also known as quartz countertops. What were the findings?
A: Silicosis is a very serious lung condition that develops from exposure to crystalline silica. Essentially, sand gets inhaled into the lungs. Workers can be exposed when they’re making engineered stone countertops, the most popular countertops now in the United States.
This study is based on statewide surveys from 2019 to 2022 that the California Department of Public Health does routinely. They gathered cases of silicosis and found 52 — all men with an average age of 45. All but one were Latino immigrants, and most either had no insurance or very poor insurance.
Q: The study found that “diagnosis was delayed in 58%, with 38% presenting with advanced disease (progressive massive fibrosis), and 19% died.” What does that tell you?
A: It’s a very serious condition. Once it gets to the advanced stage, it will just continue to progress, and the person will die. That’s why it’s so important to know that it’s absolutely preventable.
Q: Is there a message here for internists?
A: If you treat a lot of immigrants or work in an area where there are a lot of industrial workers, you’re going to want to have a very high suspicion about it. If you see an atypical pattern on the chest x-ray or via diffusion scoring, have a low threshold for getting a pulmonary function test.
Doctors need to be aware and diagnose this very quickly. When patients present, you can pull them out of that work environment or put mitigation systems into place.
Q: California regulators were expected to put emergency rules into place in late December to protect workers. Did this study play a role in focusing attention on the problem?
A: This article, along with a commentary and podcast that we put out, really helped with advocacy to improve health and safety for workers at stone-cutting and fabrication shops.
Q: You were impressed by another study about airborne dangers, this one linking air pollution to dementia. What did researchers discover?
A: [This analysis] of more than 27,000 people in the Health and Retirement Study, a respected and rich database, found that exposure to air pollution was associated with greater rates of dementia — an increase of about 8% a year. Exposure to agricultural emissions and wildfire smoke were most robustly associated with a greater risk of dementia.
Q: How are these findings important, especially in light of the unhealthy air spawned by recent wildfires in the United States and Canada?
A: Studies like this will make it even more compelling that we are better prepared for air quality issues.
I grew up in Los Angeles, where smog and pollution were very big issues. I was constantly hearing about various mitigation strategies that were going into place. But after I moved to the East Coast, I almost never heard about prevention.
Now, I’m hoping we can keep this topic in the national conversation.
Q: You also highlighted a systematic review of the use of restraints in the emergency department. Why did you choose this research?
A: At JAMA Internal Medicine, we’re really focused on ways we can address health disparities and raise awareness of potential unconscious bias.
This review looked at 10 studies that included more than 2.5 million patient encounters, including 24,000 incidents of physical restraint use. They found that the overall rate of use of restraints was low at below 1%.
But when they are used, Black patients were 1.3 times more likely to be restrained than White patients.
Q: What’s the message here?
A: This is an important start to recognizing these differences and then changing our behavior. Perhaps restraints don’t need to be used as often in light of evidence, for example, of increased rates of misdiagnosis of psychosis in the Black population.
Q: How should physicians change their approach to restraints?
A: Restraints are not to be used to control disruption — wild behavior or verbal outbursts. They’re for when someone is a danger to themselves or others.
Dr. Inouye has no conflicts of interest.
Harvard Medical School’s Sharon K. Inouye, MD, MPH, is editor in chief of JAMA Internal Medicine and a leading voice in American gerontology. We asked her to choose five of the influential journal’s most impactful studies from 2023 and highlight important take-home messages for internists and their colleagues.
Q: One of the studies you chose suggests that the antiviral nirmatrelvir (Paxlovid) can ward off long COVID. Could you recap the findings?
A: Researchers followed a group of more than 280,000 Department of Veterans Affairs patients who were seen in 2022, had a positive COVID test, and had at least one risk factor for severe COVID. They focused on those who survived to 30 days after their COVID infection and compared those who received the drug within the first 5 days of a positive test with an equivalent control group.
They found that 13 long COVID symptoms were all significantly less common (relative risk = 0.74) in those who received nirmatrelvir. This was true no matter whether they’d ever had a COVID vaccination.
Q: How should this research affect clinical practice?
A: You can’t generalize from this to everyone because, of course, not everyone was included in this study. But it is highly suggestive that this drug is very effective for preventing long COVID.
Nirmatrelvir was touted as being able to shorten duration of illness and prevent hospitalization. But if you were low risk or you were already well into your COVID course, it wasn’t like rush, rush, rush to the doctor to get it.
This changes that equation because we know long COVID is such a huge issue. The vast majority of doctors who work with COVID patients and know this are now being more aggressive about prescribing it.
Q: What about patients whom the CDC considers to be at less risk — people with up-to-date vaccinations who are under 50 with mild-to-moderate COVID and no higher-risk medical conditions? Should they take nirmatrelvir?
A: The evidence is not 100% in yet. A study like this one needs to be repeated and include younger people without any risk factors to see if we see the same thing. So it’s a personal choice, and a personal calculus needs to be done. A lot of people are making that choice [to take the drug], and it can be a rational decision.
Q: You also chose a study that links high thyroid hormone levels to higher rates of dementia. What did it reveal?
A: This study looks at patients who had thyrotoxicosis — a thyroid level that’s too high — from hormone produced endogenously, and exogenously. Researchers tracked almost 66,000 patients aged 65 and older and found that thyrotoxicosis from all causes, whether it was endogenous or exogenous, was linked to an increased risk of dementia in a dose-response relationship (adjusted hazard ratio = 1.39).
Q: Is there a clinical take-home message here?
A: When we start patients on thyroid medication, they don’t always get reassessed on a regular basis. Given this finding, a TSH [thyroid-stimulating hormone] level is indicated during the annual wellness check that patients on Medicare can get every year.
Q: Is TSH measured as part of routine blood tests?
A: No it’s not. It has to be ordered. I think that’s why we’re seeing this problem to begin with — because it’s not something we all have awareness about. I wasn’t aware myself that mildly high levels of thyroid could increase the risk of cognitive impairment. Certainly, I’m going to be much more aware in my practice.
Q: You also picked a study about silicosis in workers who are exposed to dust when they make engineered stone countertops, also known as quartz countertops. What were the findings?
A: Silicosis is a very serious lung condition that develops from exposure to crystalline silica. Essentially, sand gets inhaled into the lungs. Workers can be exposed when they’re making engineered stone countertops, the most popular countertops now in the United States.
This study is based on statewide surveys from 2019 to 2022 that the California Department of Public Health does routinely. They gathered cases of silicosis and found 52 — all men with an average age of 45. All but one were Latino immigrants, and most either had no insurance or very poor insurance.
Q: The study found that “diagnosis was delayed in 58%, with 38% presenting with advanced disease (progressive massive fibrosis), and 19% died.” What does that tell you?
A: It’s a very serious condition. Once it gets to the advanced stage, it will just continue to progress, and the person will die. That’s why it’s so important to know that it’s absolutely preventable.
Q: Is there a message here for internists?
A: If you treat a lot of immigrants or work in an area where there are a lot of industrial workers, you’re going to want to have a very high suspicion about it. If you see an atypical pattern on the chest x-ray or via diffusion scoring, have a low threshold for getting a pulmonary function test.
Doctors need to be aware and diagnose this very quickly. When patients present, you can pull them out of that work environment or put mitigation systems into place.
Q: California regulators were expected to put emergency rules into place in late December to protect workers. Did this study play a role in focusing attention on the problem?
A: This article, along with a commentary and podcast that we put out, really helped with advocacy to improve health and safety for workers at stone-cutting and fabrication shops.
Q: You were impressed by another study about airborne dangers, this one linking air pollution to dementia. What did researchers discover?
A: [This analysis] of more than 27,000 people in the Health and Retirement Study, a respected and rich database, found that exposure to air pollution was associated with greater rates of dementia — an increase of about 8% a year. Exposure to agricultural emissions and wildfire smoke were most robustly associated with a greater risk of dementia.
Q: How are these findings important, especially in light of the unhealthy air spawned by recent wildfires in the United States and Canada?
A: Studies like this will make it even more compelling that we are better prepared for air quality issues.
I grew up in Los Angeles, where smog and pollution were very big issues. I was constantly hearing about various mitigation strategies that were going into place. But after I moved to the East Coast, I almost never heard about prevention.
Now, I’m hoping we can keep this topic in the national conversation.
Q: You also highlighted a systematic review of the use of restraints in the emergency department. Why did you choose this research?
A: At JAMA Internal Medicine, we’re really focused on ways we can address health disparities and raise awareness of potential unconscious bias.
This review looked at 10 studies that included more than 2.5 million patient encounters, including 24,000 incidents of physical restraint use. They found that the overall rate of use of restraints was low at below 1%.
But when they are used, Black patients were 1.3 times more likely to be restrained than White patients.
Q: What’s the message here?
A: This is an important start to recognizing these differences and then changing our behavior. Perhaps restraints don’t need to be used as often in light of evidence, for example, of increased rates of misdiagnosis of psychosis in the Black population.
Q: How should physicians change their approach to restraints?
A: Restraints are not to be used to control disruption — wild behavior or verbal outbursts. They’re for when someone is a danger to themselves or others.
Dr. Inouye has no conflicts of interest.
Harvard Medical School’s Sharon K. Inouye, MD, MPH, is editor in chief of JAMA Internal Medicine and a leading voice in American gerontology. We asked her to choose five of the influential journal’s most impactful studies from 2023 and highlight important take-home messages for internists and their colleagues.
Q: One of the studies you chose suggests that the antiviral nirmatrelvir (Paxlovid) can ward off long COVID. Could you recap the findings?
A: Researchers followed a group of more than 280,000 Department of Veterans Affairs patients who were seen in 2022, had a positive COVID test, and had at least one risk factor for severe COVID. They focused on those who survived to 30 days after their COVID infection and compared those who received the drug within the first 5 days of a positive test with an equivalent control group.
They found that 13 long COVID symptoms were all significantly less common (relative risk = 0.74) in those who received nirmatrelvir. This was true no matter whether they’d ever had a COVID vaccination.
Q: How should this research affect clinical practice?
A: You can’t generalize from this to everyone because, of course, not everyone was included in this study. But it is highly suggestive that this drug is very effective for preventing long COVID.
Nirmatrelvir was touted as being able to shorten duration of illness and prevent hospitalization. But if you were low risk or you were already well into your COVID course, it wasn’t like rush, rush, rush to the doctor to get it.
This changes that equation because we know long COVID is such a huge issue. The vast majority of doctors who work with COVID patients and know this are now being more aggressive about prescribing it.
Q: What about patients whom the CDC considers to be at less risk — people with up-to-date vaccinations who are under 50 with mild-to-moderate COVID and no higher-risk medical conditions? Should they take nirmatrelvir?
A: The evidence is not 100% in yet. A study like this one needs to be repeated and include younger people without any risk factors to see if we see the same thing. So it’s a personal choice, and a personal calculus needs to be done. A lot of people are making that choice [to take the drug], and it can be a rational decision.
Q: You also chose a study that links high thyroid hormone levels to higher rates of dementia. What did it reveal?
A: This study looks at patients who had thyrotoxicosis — a thyroid level that’s too high — from hormone produced endogenously, and exogenously. Researchers tracked almost 66,000 patients aged 65 and older and found that thyrotoxicosis from all causes, whether it was endogenous or exogenous, was linked to an increased risk of dementia in a dose-response relationship (adjusted hazard ratio = 1.39).
Q: Is there a clinical take-home message here?
A: When we start patients on thyroid medication, they don’t always get reassessed on a regular basis. Given this finding, a TSH [thyroid-stimulating hormone] level is indicated during the annual wellness check that patients on Medicare can get every year.
Q: Is TSH measured as part of routine blood tests?
A: No it’s not. It has to be ordered. I think that’s why we’re seeing this problem to begin with — because it’s not something we all have awareness about. I wasn’t aware myself that mildly high levels of thyroid could increase the risk of cognitive impairment. Certainly, I’m going to be much more aware in my practice.
Q: You also picked a study about silicosis in workers who are exposed to dust when they make engineered stone countertops, also known as quartz countertops. What were the findings?
A: Silicosis is a very serious lung condition that develops from exposure to crystalline silica. Essentially, sand gets inhaled into the lungs. Workers can be exposed when they’re making engineered stone countertops, the most popular countertops now in the United States.
This study is based on statewide surveys from 2019 to 2022 that the California Department of Public Health does routinely. They gathered cases of silicosis and found 52 — all men with an average age of 45. All but one were Latino immigrants, and most either had no insurance or very poor insurance.
Q: The study found that “diagnosis was delayed in 58%, with 38% presenting with advanced disease (progressive massive fibrosis), and 19% died.” What does that tell you?
A: It’s a very serious condition. Once it gets to the advanced stage, it will just continue to progress, and the person will die. That’s why it’s so important to know that it’s absolutely preventable.
Q: Is there a message here for internists?
A: If you treat a lot of immigrants or work in an area where there are a lot of industrial workers, you’re going to want to have a very high suspicion about it. If you see an atypical pattern on the chest x-ray or via diffusion scoring, have a low threshold for getting a pulmonary function test.
Doctors need to be aware and diagnose this very quickly. When patients present, you can pull them out of that work environment or put mitigation systems into place.
Q: California regulators were expected to put emergency rules into place in late December to protect workers. Did this study play a role in focusing attention on the problem?
A: This article, along with a commentary and podcast that we put out, really helped with advocacy to improve health and safety for workers at stone-cutting and fabrication shops.
Q: You were impressed by another study about airborne dangers, this one linking air pollution to dementia. What did researchers discover?
A: [This analysis] of more than 27,000 people in the Health and Retirement Study, a respected and rich database, found that exposure to air pollution was associated with greater rates of dementia — an increase of about 8% a year. Exposure to agricultural emissions and wildfire smoke were most robustly associated with a greater risk of dementia.
Q: How are these findings important, especially in light of the unhealthy air spawned by recent wildfires in the United States and Canada?
A: Studies like this will make it even more compelling that we are better prepared for air quality issues.
I grew up in Los Angeles, where smog and pollution were very big issues. I was constantly hearing about various mitigation strategies that were going into place. But after I moved to the East Coast, I almost never heard about prevention.
Now, I’m hoping we can keep this topic in the national conversation.
Q: You also highlighted a systematic review of the use of restraints in the emergency department. Why did you choose this research?
A: At JAMA Internal Medicine, we’re really focused on ways we can address health disparities and raise awareness of potential unconscious bias.
This review looked at 10 studies that included more than 2.5 million patient encounters, including 24,000 incidents of physical restraint use. They found that the overall rate of use of restraints was low at below 1%.
But when they are used, Black patients were 1.3 times more likely to be restrained than White patients.
Q: What’s the message here?
A: This is an important start to recognizing these differences and then changing our behavior. Perhaps restraints don’t need to be used as often in light of evidence, for example, of increased rates of misdiagnosis of psychosis in the Black population.
Q: How should physicians change their approach to restraints?
A: Restraints are not to be used to control disruption — wild behavior or verbal outbursts. They’re for when someone is a danger to themselves or others.
Dr. Inouye has no conflicts of interest.
Older Adults Want Medicare, Insurance to Cover Obesity Drugs
Weight-loss drugs should be covered by Medicare and by other health insurance, according to a poll of US adults aged 50-80 years.
Among more than 2600 polled, 83% say that health insurance should cover prescription weight-loss drugs that have been approved by the US Food and Drug Administration (FDA), and 76% say Medicare should cover such drugs. However, only 30% would be willing to pay higher Medicare premiums to have these medications covered.
Among the 27% of respondents who say they are overweight, 63% are interested in taking such medications, as are 45% of those with diabetes, regardless of weight.
The University of Michigan (U-M) National Poll on Healthy Aging was published online on December 13, 2023.
High Awareness
The findings come at a time when injectable glucagon-like peptide 1 receptor agonists (GLP-1 RAs), such as Ozempic, Wegovy, Zepbound, and Mounjaro, are receiving a lot of public attention, the university noted.
Overall, 64% of survey respondents had heard of at least one prescription medication used for weight management.
By brand name, 61% had heard of Ozempic, approved for the treatment of type 2 diabetes but prescribed off label for weight loss; 18% had heard of Wegovy; and 13% had heard of the anorexiant drug phentermine .
Very few respondents (3% for each) had heard of the GLP-1 RA Saxenda, Qsymia (phentermine plus the anticonvulsant topiramate ), and the opiate antagonist Contrave.
Zepbound, the obesity -specific form of the diabetes drug Mounjaro, received FDA approval after the poll was taken and was not included in survey questions.
Among respondents who had heard of at least one prescription medication used for weight management, 58% had heard about them through the news (eg, TV, magazines, newspapers) and 53% had heard about them from an advertisement on TV, the Internet, or radio. Only 11% heard about them from their healthcare providers.
Respondents more likely to be interested in taking a prescription medication for weight management included women, those aged 50-64 years, Black persons, Hispanic persons, those with household incomes of less than $60,000 annually, those with lower levels of education, those in fair or poor physical or mental health, and those with a health problem or disability limiting their daily activities.
Spotty Coverage
The GLP-1 RAs can cost more than $12,000 a year for people who pay out of pocket, the university noted.
A Medicare Part D law passed in 2003 prohibits Medicare from covering medications for weight loss, although currently it can cover such drugs to help people with type 2 diabetes manage their weight.
Medicaid covers the cost of antiobesity drugs in some states.
Most private plans and the Veterans Health Administration cover them, but with restrictions due to high monthly costs for the newer medications.
The American Medical Association recently called on insurers to cover evidence-based weight-loss medications.
The strong demand for these medications, including for off-label purposes by people willing to pay full price, has created major shortages, the university noted.
“As these medications grow in awareness and use, and insurers make decisions about coverage, it’s crucial for patients who have obesity or diabetes, or who are overweight with other health problems, to talk with their healthcare providers about their options,” said poll director Jeffrey Kullgren, MD, MPH, MS, a primary care physician at the VA Ann Arbor Healthcare System and associate professor of internal medicine at U-M.
Other weight-management strategies that respondents think should be covered by health insurance include sessions with a registered dietitian or nutritionist (85%); weight-loss surgery (73%); gym or fitness facility memberships (65%); apps or online programs to track diet, exercise, and/or behavior change (58%); and sessions with a personal trainer (53%).
The randomly selected nationally representative household survey of 2657 adults was conducted from July 17 to August 7, 2023, by NORC at the University of Chicago for the U-M Institute for Healthcare Policy and Innovation. The sample was subsequently weighted to reflect population figures from the US Census Bureau. The completion rate was 50% among those contacted to participate. The margin of error is ±1 to 5 percentage points for questions asked of the full sample and higher among subgroups.
The poll is based at the U-M Institute for Healthcare Policy and Innovation and supported by AARP and Michigan Medicine, the University of Michigan’s academic medical center.
A version of this article appeared on Medscape.com.
Weight-loss drugs should be covered by Medicare and by other health insurance, according to a poll of US adults aged 50-80 years.
Among more than 2600 polled, 83% say that health insurance should cover prescription weight-loss drugs that have been approved by the US Food and Drug Administration (FDA), and 76% say Medicare should cover such drugs. However, only 30% would be willing to pay higher Medicare premiums to have these medications covered.
Among the 27% of respondents who say they are overweight, 63% are interested in taking such medications, as are 45% of those with diabetes, regardless of weight.
The University of Michigan (U-M) National Poll on Healthy Aging was published online on December 13, 2023.
High Awareness
The findings come at a time when injectable glucagon-like peptide 1 receptor agonists (GLP-1 RAs), such as Ozempic, Wegovy, Zepbound, and Mounjaro, are receiving a lot of public attention, the university noted.
Overall, 64% of survey respondents had heard of at least one prescription medication used for weight management.
By brand name, 61% had heard of Ozempic, approved for the treatment of type 2 diabetes but prescribed off label for weight loss; 18% had heard of Wegovy; and 13% had heard of the anorexiant drug phentermine .
Very few respondents (3% for each) had heard of the GLP-1 RA Saxenda, Qsymia (phentermine plus the anticonvulsant topiramate ), and the opiate antagonist Contrave.
Zepbound, the obesity -specific form of the diabetes drug Mounjaro, received FDA approval after the poll was taken and was not included in survey questions.
Among respondents who had heard of at least one prescription medication used for weight management, 58% had heard about them through the news (eg, TV, magazines, newspapers) and 53% had heard about them from an advertisement on TV, the Internet, or radio. Only 11% heard about them from their healthcare providers.
Respondents more likely to be interested in taking a prescription medication for weight management included women, those aged 50-64 years, Black persons, Hispanic persons, those with household incomes of less than $60,000 annually, those with lower levels of education, those in fair or poor physical or mental health, and those with a health problem or disability limiting their daily activities.
Spotty Coverage
The GLP-1 RAs can cost more than $12,000 a year for people who pay out of pocket, the university noted.
A Medicare Part D law passed in 2003 prohibits Medicare from covering medications for weight loss, although currently it can cover such drugs to help people with type 2 diabetes manage their weight.
Medicaid covers the cost of antiobesity drugs in some states.
Most private plans and the Veterans Health Administration cover them, but with restrictions due to high monthly costs for the newer medications.
The American Medical Association recently called on insurers to cover evidence-based weight-loss medications.
The strong demand for these medications, including for off-label purposes by people willing to pay full price, has created major shortages, the university noted.
“As these medications grow in awareness and use, and insurers make decisions about coverage, it’s crucial for patients who have obesity or diabetes, or who are overweight with other health problems, to talk with their healthcare providers about their options,” said poll director Jeffrey Kullgren, MD, MPH, MS, a primary care physician at the VA Ann Arbor Healthcare System and associate professor of internal medicine at U-M.
Other weight-management strategies that respondents think should be covered by health insurance include sessions with a registered dietitian or nutritionist (85%); weight-loss surgery (73%); gym or fitness facility memberships (65%); apps or online programs to track diet, exercise, and/or behavior change (58%); and sessions with a personal trainer (53%).
The randomly selected nationally representative household survey of 2657 adults was conducted from July 17 to August 7, 2023, by NORC at the University of Chicago for the U-M Institute for Healthcare Policy and Innovation. The sample was subsequently weighted to reflect population figures from the US Census Bureau. The completion rate was 50% among those contacted to participate. The margin of error is ±1 to 5 percentage points for questions asked of the full sample and higher among subgroups.
The poll is based at the U-M Institute for Healthcare Policy and Innovation and supported by AARP and Michigan Medicine, the University of Michigan’s academic medical center.
A version of this article appeared on Medscape.com.
Weight-loss drugs should be covered by Medicare and by other health insurance, according to a poll of US adults aged 50-80 years.
Among more than 2600 polled, 83% say that health insurance should cover prescription weight-loss drugs that have been approved by the US Food and Drug Administration (FDA), and 76% say Medicare should cover such drugs. However, only 30% would be willing to pay higher Medicare premiums to have these medications covered.
Among the 27% of respondents who say they are overweight, 63% are interested in taking such medications, as are 45% of those with diabetes, regardless of weight.
The University of Michigan (U-M) National Poll on Healthy Aging was published online on December 13, 2023.
High Awareness
The findings come at a time when injectable glucagon-like peptide 1 receptor agonists (GLP-1 RAs), such as Ozempic, Wegovy, Zepbound, and Mounjaro, are receiving a lot of public attention, the university noted.
Overall, 64% of survey respondents had heard of at least one prescription medication used for weight management.
By brand name, 61% had heard of Ozempic, approved for the treatment of type 2 diabetes but prescribed off label for weight loss; 18% had heard of Wegovy; and 13% had heard of the anorexiant drug phentermine .
Very few respondents (3% for each) had heard of the GLP-1 RA Saxenda, Qsymia (phentermine plus the anticonvulsant topiramate ), and the opiate antagonist Contrave.
Zepbound, the obesity -specific form of the diabetes drug Mounjaro, received FDA approval after the poll was taken and was not included in survey questions.
Among respondents who had heard of at least one prescription medication used for weight management, 58% had heard about them through the news (eg, TV, magazines, newspapers) and 53% had heard about them from an advertisement on TV, the Internet, or radio. Only 11% heard about them from their healthcare providers.
Respondents more likely to be interested in taking a prescription medication for weight management included women, those aged 50-64 years, Black persons, Hispanic persons, those with household incomes of less than $60,000 annually, those with lower levels of education, those in fair or poor physical or mental health, and those with a health problem or disability limiting their daily activities.
Spotty Coverage
The GLP-1 RAs can cost more than $12,000 a year for people who pay out of pocket, the university noted.
A Medicare Part D law passed in 2003 prohibits Medicare from covering medications for weight loss, although currently it can cover such drugs to help people with type 2 diabetes manage their weight.
Medicaid covers the cost of antiobesity drugs in some states.
Most private plans and the Veterans Health Administration cover them, but with restrictions due to high monthly costs for the newer medications.
The American Medical Association recently called on insurers to cover evidence-based weight-loss medications.
The strong demand for these medications, including for off-label purposes by people willing to pay full price, has created major shortages, the university noted.
“As these medications grow in awareness and use, and insurers make decisions about coverage, it’s crucial for patients who have obesity or diabetes, or who are overweight with other health problems, to talk with their healthcare providers about their options,” said poll director Jeffrey Kullgren, MD, MPH, MS, a primary care physician at the VA Ann Arbor Healthcare System and associate professor of internal medicine at U-M.
Other weight-management strategies that respondents think should be covered by health insurance include sessions with a registered dietitian or nutritionist (85%); weight-loss surgery (73%); gym or fitness facility memberships (65%); apps or online programs to track diet, exercise, and/or behavior change (58%); and sessions with a personal trainer (53%).
The randomly selected nationally representative household survey of 2657 adults was conducted from July 17 to August 7, 2023, by NORC at the University of Chicago for the U-M Institute for Healthcare Policy and Innovation. The sample was subsequently weighted to reflect population figures from the US Census Bureau. The completion rate was 50% among those contacted to participate. The margin of error is ±1 to 5 percentage points for questions asked of the full sample and higher among subgroups.
The poll is based at the U-M Institute for Healthcare Policy and Innovation and supported by AARP and Michigan Medicine, the University of Michigan’s academic medical center.
A version of this article appeared on Medscape.com.
New Insights, New Standards: How 2023 Changed Care for Internists
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
The past year brought major changes in preventive standards for anxiety, HIV, and RSV along with new guidelines for the treatment of atrial fibrillation. For insight into the effect on internal medicine, we turned to Sarah Candler, MD, MPH, a Houston internist who specializes in the care of high-risk older adults.
Q: Which new prevention guidelines had the most impact on you over the past year?
A: I’m a primary care doctor, and most of the internal medicine updates that are interesting to me focus on how we can keep people from getting sick in the first place. That’s especially important in light of the fact that we had a decrease in life expectancy of 2 years [it finally rose slightly in 2022] and widening of the gender gap in life expectancy for men and women.
I’m excited to see new recommendations from the U.S. Preventive Services Task Force, including a new one about using PREP [pre-exposure prophylaxis] to preventively treat anyone who’s at risk for getting HIV. That’s a big one because it’s one of the first times that we’ve identified at-risk groups for screening based on social risk factors, not gender, age, or genetics.
The new recommendation is PREP for anyone who’s at risk for getting HIV because they have a partner with HIV, had an sexually transmitted infection in the last 6 months, or a history of inconsistent or no condom use with partners with unknown HIV status.
PREP therapy is something that most primary care physicians can either do or learn how to do pretty easily. But the treatment does require maintenance and monitoring.
Q: How firm is this recommendation?
A: The task force gives different grades for their recommendations based on how strong the evidence is. For the guidelines about PREP, they give a grade of A. That means this is top of the class: You should definitely do this.
Q: What are the best strategies to ask patients personal questions about their sex lives in order to evaluate their risk?
A: A lot of internal medicine physicians are getting pretty good at this. We see it as part of our job just the same way as we asked things like, “How often are you walking?” and “Have you been feeling down?”
There’s no one right way to have a conversation like that. But it’s key to say, as I do to my patients, that “I’m not here to judge anything. I am truly here to gather information and make recommendations to you as a partner in your care.”
Q: What other guidelines made an impact in 2023?
A: The U.S. Preventive Services Task Force made a recommendation to screen adults aged 18-64 for anxiety, and this guidance got a B grade. [The task force said there’s not enough evidence to support routine anxiety screening in adults 65 and older.]
The new recommendations is a sign that we’re doing a better job at making treatment of those diseases more acceptable. This is also another example of the medical community recognizing that internal medicine physicians are pretty good at identifying and treating mental health.
Q: How do you figure out whether to treat depression/anxiety yourself or refer patients to specialists?
A: As a primary care physician, I feel comfortable diagnosing and managing some mental health disease in my own practice. There are FDA-approved medications for both anxiety and depression that are easily managed by a primary care physician.
And there’s something to the therapeutic relationship, to naming and identifying these conditions with your patients. Some patients feel a bit of relief just knowing that they have a diagnosis.
Q: What should internists know about the new CDC guidelines that promote discussing RSV vaccines with patients who are over 60?
A: The vaccines are recommended for folks who have underlying conditions like lung disease or heart disease. Those are the ones who end up getting really, really sick. There are two adult vaccines that are available, and there’s not a preference for one over the other.
The vaccines are both protein-based, like the old-school versions of vaccines, not the mRNA vaccines that we’ve all been hearing more about through COVID. Anybody who’s reluctant to take an mRNA vaccine can rest assured that the RSV is not protein-based. And they are single-dose vaccines, which is helpful.
Q: What else should internists know about that was new in 2023?
A: I’m super excited about how cardiologists are thinking about atrial fibrillation. In 2023, the American College of Cardiology and the American Heart Association came up with a giant overhaul of how they look at atrial fibrillation. They classify it in stages and allows us to think about stopping it before it starts.
They’re talking about something they’re calling preclinical or subclinical atrial fibrillation, which you may detect on wearables like somebody’s watch or another tool used to monitor heart rate or exercise. It might be the first harbinger that there’s something wrong with the heart rate, and they may not even have symptoms of it. [A 2023 study in The New England Journal of Medicine linked the anticoagulant apixaban, or Eliquis, to a 37% lower risk of stroke and systemic embolism rates in older patients with subclinical atrial fibrillation but an 80% higher risk of major bleeding vs. aspirin therapy.]
And they’re now recommending early rhythm control.
Q: What does early rhythm control mean for patients and physicians?
A: For the longest time, we have thought about atrial fibrillation treatment in terms of rate control and not worrying too much about the rhythm. But now we recognize that it’s actually really important that we get the rhythm under control because physical changes to the heart can lead to permanent damage.
So now they’re recommending catheter ablation as first-line therapy in some patients as a class 1 recommendation because heart function is already decreased. Improving the ability of the heart to beat with a regular rhythm can lead to improvement of function. This was unheard of even 5 years ago.
Q: Should internists be more willing to refer patients with atrial fibrillation to cardiologists?
A: Yes, I think so. One of the biggest changes for me is that I am going to refer new diagnoses of atrial fibrillation to a cardiologist. And I’m going to ask patients if they have wearable devices because sometimes those things might tell me about something like subclinical atrial fibrillation.
Q: There’s also detailed data about atrial fibrillation risk factors, which include older age, smoking, sedentary lifestyle, alcohol use, diabetes, height, obesity, diabetes, and others. Is this information useful?
A: It’s a really great tool to have in the arsenal because it helps me have shared decision-making conversations with my patients in a way that’s much more convincing. A patient might say, “Why do you care if I drink so much? My liver levels are fine.” And I can say, “It’s going to be a risk factor for having problems with your heart.”
For better or worse, people really take the heart very seriously, I am an internal medicine physician, so I love all the organs equally. But man, people get pretty scared when you tell them something can affect their heart. So when I talk to patients about their risk factors, it’s going to really be helpful that I can remind them of the impact that some of these lifestyle behaviors can have on their heart health.
Dr. Candler has no disclosures.
Light therapy a beacon of hope for Alzheimer’s?
TOPLINE:
Light therapy leads to significant improvement in several sleep measures and helps alleviate depression and agitation in patients with Alzheimer’s disease (AD), a meta-analysis of 15 high-quality trials shows.
METHODOLOGY:
- This meta-analysis included 15 randomized controlled trials involving 598 patients with mild to moderate AD.
- The included trials were written in English, published between 2005 and 2022, and performed in seven countries. A fixed-effects model was used for data analysis.
TAKEAWAY:
- Light therapy significantly improved sleep efficiency (mean difference [MD], −2.42; P < .00001), increased interdaily stability (MD, −0.04; P < .00001), and reduced intradaily variability (MD, −0.04; P < .00001), indicating better sleep quality.
- Light therapy reduced agitation (MD, −3.97; P < .00001), depression (MD, −2.55; P < .00001), and caregiver burden (MD, −3.57; P < .00001).
- Light therapy also had a significant advantage over usual care in reducing the severity of psychobehavioral symptoms as assessed by the Neuropsychiatric Inventory (MD, −3.07; P < .00001).
- Light therapy had no statistically significant effect on improving cognitive function as measured by the Mini-Mental State Examination.
IN PRACTICE:
“These findings, combined with its low side-effects, suggest the role of light therapy as a promising treatment for AD. Although light therapy has fewer side effects than pharmacological treatment, adverse behavioral outcomes in patients due to bright light exposure should be considered,” the authors wrote.
SOURCE:
The study by Lili Zang and colleagues from Weifang Medical University School of Nursing, Shandong Province, China, was published online on December 6, 2023, in PLOS One.
LIMITATIONS:
The types and degrees of dementia in the included studies were inconsistent, potentially affecting the outcome indicators. Some articles did not clearly describe their randomization and allocation concealment methods, indicating possible bias in these studies.
DISCLOSURES:
The study was supported by the Natural Science Foundation of Shandong Province, China. The authors declared no competing interests.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
Light therapy leads to significant improvement in several sleep measures and helps alleviate depression and agitation in patients with Alzheimer’s disease (AD), a meta-analysis of 15 high-quality trials shows.
METHODOLOGY:
- This meta-analysis included 15 randomized controlled trials involving 598 patients with mild to moderate AD.
- The included trials were written in English, published between 2005 and 2022, and performed in seven countries. A fixed-effects model was used for data analysis.
TAKEAWAY:
- Light therapy significantly improved sleep efficiency (mean difference [MD], −2.42; P < .00001), increased interdaily stability (MD, −0.04; P < .00001), and reduced intradaily variability (MD, −0.04; P < .00001), indicating better sleep quality.
- Light therapy reduced agitation (MD, −3.97; P < .00001), depression (MD, −2.55; P < .00001), and caregiver burden (MD, −3.57; P < .00001).
- Light therapy also had a significant advantage over usual care in reducing the severity of psychobehavioral symptoms as assessed by the Neuropsychiatric Inventory (MD, −3.07; P < .00001).
- Light therapy had no statistically significant effect on improving cognitive function as measured by the Mini-Mental State Examination.
IN PRACTICE:
“These findings, combined with its low side-effects, suggest the role of light therapy as a promising treatment for AD. Although light therapy has fewer side effects than pharmacological treatment, adverse behavioral outcomes in patients due to bright light exposure should be considered,” the authors wrote.
SOURCE:
The study by Lili Zang and colleagues from Weifang Medical University School of Nursing, Shandong Province, China, was published online on December 6, 2023, in PLOS One.
LIMITATIONS:
The types and degrees of dementia in the included studies were inconsistent, potentially affecting the outcome indicators. Some articles did not clearly describe their randomization and allocation concealment methods, indicating possible bias in these studies.
DISCLOSURES:
The study was supported by the Natural Science Foundation of Shandong Province, China. The authors declared no competing interests.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
Light therapy leads to significant improvement in several sleep measures and helps alleviate depression and agitation in patients with Alzheimer’s disease (AD), a meta-analysis of 15 high-quality trials shows.
METHODOLOGY:
- This meta-analysis included 15 randomized controlled trials involving 598 patients with mild to moderate AD.
- The included trials were written in English, published between 2005 and 2022, and performed in seven countries. A fixed-effects model was used for data analysis.
TAKEAWAY:
- Light therapy significantly improved sleep efficiency (mean difference [MD], −2.42; P < .00001), increased interdaily stability (MD, −0.04; P < .00001), and reduced intradaily variability (MD, −0.04; P < .00001), indicating better sleep quality.
- Light therapy reduced agitation (MD, −3.97; P < .00001), depression (MD, −2.55; P < .00001), and caregiver burden (MD, −3.57; P < .00001).
- Light therapy also had a significant advantage over usual care in reducing the severity of psychobehavioral symptoms as assessed by the Neuropsychiatric Inventory (MD, −3.07; P < .00001).
- Light therapy had no statistically significant effect on improving cognitive function as measured by the Mini-Mental State Examination.
IN PRACTICE:
“These findings, combined with its low side-effects, suggest the role of light therapy as a promising treatment for AD. Although light therapy has fewer side effects than pharmacological treatment, adverse behavioral outcomes in patients due to bright light exposure should be considered,” the authors wrote.
SOURCE:
The study by Lili Zang and colleagues from Weifang Medical University School of Nursing, Shandong Province, China, was published online on December 6, 2023, in PLOS One.
LIMITATIONS:
The types and degrees of dementia in the included studies were inconsistent, potentially affecting the outcome indicators. Some articles did not clearly describe their randomization and allocation concealment methods, indicating possible bias in these studies.
DISCLOSURES:
The study was supported by the Natural Science Foundation of Shandong Province, China. The authors declared no competing interests.
Megan Brooks has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Exercise plan cost-effective in post-stroke cognitive rehab
A multicomponent exercise program that includes strength, aerobic, agility, and balance training exercises is cost-effective and results in improved cognition among stroke survivors, compared with a balance and tone control group, according to a new analysis.
On the other hand, a program consisting of cognitive and social enrichment activities that includes memory, brain training, and group social games entailed higher costs, compared with the balance and tone group, which included stretches, deep breathing and relaxation techniques, posture education, and core control exercises.
“Cognitive impairment is experienced in approximately one-third of stroke survivors,” study author Jennifer Davis, PhD, a Canada research chair in applied health economics and assistant professor of management at the University of British Columbia in Kelowna, said in an interview.
“The economic evaluation of the exercise intervention demonstrated that the multicomponent exercise program provided good value for the money when comparing costs and cognitive outcomes,” she said. However, “impacts on health-related quality of life were not observed.”
The study was published online November 30 in JAMA Network Open.
Comparing Three Approaches
Despite improved care, patients with stroke often face challenges with physical function, cognitive abilities, and quality of life, the authors wrote. Among older adults, in particular, cognitive deficits remain prevalent and are associated with increased risks for dementia, mortality, and increased burdens for patients, caregivers, and health systems.
Numerous interventions have shown promise for post-stroke cognitive rehabilitation, including exercise and cognitive training, the authors wrote. Research hasn’t indicated which programs offer the most efficient or cost-effective options, however.
Dr. Davis and colleagues conducted an economic evaluation alongside the Vitality study, a three-group randomized clinical trial that examined the efficacy of improving cognitive function among patients with chronic stroke through a multicomponent exercise program, cognitive and social enrichment activities, or a control group with balance and tone activities.
The economic evaluation team included a cost-effectiveness analysis (based on incremental cost per cognitive function change) and a cost-utility analysis (incremental cost per quality-adjusted life-year [QALY] gained). The researchers used a cost-effectiveness threshold of CAD $50,000 (Canadian dollars) per QALY for the cost-utility analysis, which was based on precedent treatment in Canada.
The clinical trial included 120 community-dwelling adults aged 55 years and older who had a stroke at least 12 months before the study. Based in the Vancouver metropolitan area, participants were randomly assigned to twice-weekly, 60-minute classes led by trained instructors for 26 weeks. The mean age was 71 years, and 62% of participants were men.
Exercise Effective
Overall, the balance and tone control group had the lowest delivery cost at CAD $777 per person, followed by CAD $1090 per person for the exercise group and CAD $1492 per person for the cognitive and social enrichment group.
After the 6-month intervention, the mean cognitive scores were –0.192 for the exercise group, –0.184 for the cognitive and social enrichment group, and –0.171 for the balance and tone group, indicating better cognitive function across all three groups.
In the cost-effectiveness analysis, the exercise intervention was costlier but more effective than the control group, with an incremental cost-effectiveness ratio (ICER) of CAD –$8823.
In the cost-utility analysis, the exercise intervention was cost saving (less costly and more effective), compared with the control group, with an ICER of CAD –$3381 per QALY gained at the end of the intervention and an ICER of CAD –$154,198 per QALY gained at the end of the 12-month follow-up period. The cognitive and social enrichment program was more costly and more effective than the control group, with an ICER of CAD $101,687 per QALY gained at the end of the intervention and an ICER of CAD $331,306 per QALY gained at the end of the follow-up period.
In additional analyses, the exercise group had the lowest healthcare resource utilization due to lower healthcare costs for physician visits and lab tests.
“This study provides initial data that suggests multicomponent exercise may be a cost-effective solution for combating cognitive decline among stroke survivors,” said Dr. Davis.
Overall, exercise was cost-effective for improving cognitive function but not quality of life among participants. The clinical trial was powered to detect changes in cognitive function rather than quality of life, so it lacked statistical power to detect differences in quality of life, said Dr. Davis.
Exercise programs and cognitive and social enrichment programs show promise for improving cognitive function after stroke, the authors wrote, though future research should focus on optimizing cost-effectiveness and enhancing health-related quality of life.
Considering Additional Benefits
Commenting on the study, Alan Tam, MD, a physiatrist at the Toronto Rehabilitation Institute’s Brain Rehabilitation Program, said, “The authors show that within the timeframe of their analysis, there is a trend to cost-effectiveness for the cognitive intervention being offered.” Dr. Tam did not participate in the research.
“However, the finding is not robust, as less than 50% of their simulations would meet their acceptability level they have defined,” he said. “Given that most of the cost of the intervention is up front, but the benefits are likely lifelong, potentially taking the 12-month analysis to a lifetime analysis would show more significant findings.”
Dr. Tam researches factors associated with brain injury rehabilitation and has explored the cost-effectiveness of a high-intensity outpatient stroke rehabilitation program.
“Presenting this type of work is important,” he said. “While there are interventions that do not meet our definition of statistical significance, especially in the rehabilitation world, there can still be a benefit for patients and health systems.”
The primary study was funded by the Canadian Institutes of Health Research (CIHR) and the Jack Brown and Family Alzheimer Research Foundation Society. Dr. Davis reported receiving grants from the CIHR and Michael Smith Health Research BC during the conduct of the study. Dr. Tam reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
A multicomponent exercise program that includes strength, aerobic, agility, and balance training exercises is cost-effective and results in improved cognition among stroke survivors, compared with a balance and tone control group, according to a new analysis.
On the other hand, a program consisting of cognitive and social enrichment activities that includes memory, brain training, and group social games entailed higher costs, compared with the balance and tone group, which included stretches, deep breathing and relaxation techniques, posture education, and core control exercises.
“Cognitive impairment is experienced in approximately one-third of stroke survivors,” study author Jennifer Davis, PhD, a Canada research chair in applied health economics and assistant professor of management at the University of British Columbia in Kelowna, said in an interview.
“The economic evaluation of the exercise intervention demonstrated that the multicomponent exercise program provided good value for the money when comparing costs and cognitive outcomes,” she said. However, “impacts on health-related quality of life were not observed.”
The study was published online November 30 in JAMA Network Open.
Comparing Three Approaches
Despite improved care, patients with stroke often face challenges with physical function, cognitive abilities, and quality of life, the authors wrote. Among older adults, in particular, cognitive deficits remain prevalent and are associated with increased risks for dementia, mortality, and increased burdens for patients, caregivers, and health systems.
Numerous interventions have shown promise for post-stroke cognitive rehabilitation, including exercise and cognitive training, the authors wrote. Research hasn’t indicated which programs offer the most efficient or cost-effective options, however.
Dr. Davis and colleagues conducted an economic evaluation alongside the Vitality study, a three-group randomized clinical trial that examined the efficacy of improving cognitive function among patients with chronic stroke through a multicomponent exercise program, cognitive and social enrichment activities, or a control group with balance and tone activities.
The economic evaluation team included a cost-effectiveness analysis (based on incremental cost per cognitive function change) and a cost-utility analysis (incremental cost per quality-adjusted life-year [QALY] gained). The researchers used a cost-effectiveness threshold of CAD $50,000 (Canadian dollars) per QALY for the cost-utility analysis, which was based on precedent treatment in Canada.
The clinical trial included 120 community-dwelling adults aged 55 years and older who had a stroke at least 12 months before the study. Based in the Vancouver metropolitan area, participants were randomly assigned to twice-weekly, 60-minute classes led by trained instructors for 26 weeks. The mean age was 71 years, and 62% of participants were men.
Exercise Effective
Overall, the balance and tone control group had the lowest delivery cost at CAD $777 per person, followed by CAD $1090 per person for the exercise group and CAD $1492 per person for the cognitive and social enrichment group.
After the 6-month intervention, the mean cognitive scores were –0.192 for the exercise group, –0.184 for the cognitive and social enrichment group, and –0.171 for the balance and tone group, indicating better cognitive function across all three groups.
In the cost-effectiveness analysis, the exercise intervention was costlier but more effective than the control group, with an incremental cost-effectiveness ratio (ICER) of CAD –$8823.
In the cost-utility analysis, the exercise intervention was cost saving (less costly and more effective), compared with the control group, with an ICER of CAD –$3381 per QALY gained at the end of the intervention and an ICER of CAD –$154,198 per QALY gained at the end of the 12-month follow-up period. The cognitive and social enrichment program was more costly and more effective than the control group, with an ICER of CAD $101,687 per QALY gained at the end of the intervention and an ICER of CAD $331,306 per QALY gained at the end of the follow-up period.
In additional analyses, the exercise group had the lowest healthcare resource utilization due to lower healthcare costs for physician visits and lab tests.
“This study provides initial data that suggests multicomponent exercise may be a cost-effective solution for combating cognitive decline among stroke survivors,” said Dr. Davis.
Overall, exercise was cost-effective for improving cognitive function but not quality of life among participants. The clinical trial was powered to detect changes in cognitive function rather than quality of life, so it lacked statistical power to detect differences in quality of life, said Dr. Davis.
Exercise programs and cognitive and social enrichment programs show promise for improving cognitive function after stroke, the authors wrote, though future research should focus on optimizing cost-effectiveness and enhancing health-related quality of life.
Considering Additional Benefits
Commenting on the study, Alan Tam, MD, a physiatrist at the Toronto Rehabilitation Institute’s Brain Rehabilitation Program, said, “The authors show that within the timeframe of their analysis, there is a trend to cost-effectiveness for the cognitive intervention being offered.” Dr. Tam did not participate in the research.
“However, the finding is not robust, as less than 50% of their simulations would meet their acceptability level they have defined,” he said. “Given that most of the cost of the intervention is up front, but the benefits are likely lifelong, potentially taking the 12-month analysis to a lifetime analysis would show more significant findings.”
Dr. Tam researches factors associated with brain injury rehabilitation and has explored the cost-effectiveness of a high-intensity outpatient stroke rehabilitation program.
“Presenting this type of work is important,” he said. “While there are interventions that do not meet our definition of statistical significance, especially in the rehabilitation world, there can still be a benefit for patients and health systems.”
The primary study was funded by the Canadian Institutes of Health Research (CIHR) and the Jack Brown and Family Alzheimer Research Foundation Society. Dr. Davis reported receiving grants from the CIHR and Michael Smith Health Research BC during the conduct of the study. Dr. Tam reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
A multicomponent exercise program that includes strength, aerobic, agility, and balance training exercises is cost-effective and results in improved cognition among stroke survivors, compared with a balance and tone control group, according to a new analysis.
On the other hand, a program consisting of cognitive and social enrichment activities that includes memory, brain training, and group social games entailed higher costs, compared with the balance and tone group, which included stretches, deep breathing and relaxation techniques, posture education, and core control exercises.
“Cognitive impairment is experienced in approximately one-third of stroke survivors,” study author Jennifer Davis, PhD, a Canada research chair in applied health economics and assistant professor of management at the University of British Columbia in Kelowna, said in an interview.
“The economic evaluation of the exercise intervention demonstrated that the multicomponent exercise program provided good value for the money when comparing costs and cognitive outcomes,” she said. However, “impacts on health-related quality of life were not observed.”
The study was published online November 30 in JAMA Network Open.
Comparing Three Approaches
Despite improved care, patients with stroke often face challenges with physical function, cognitive abilities, and quality of life, the authors wrote. Among older adults, in particular, cognitive deficits remain prevalent and are associated with increased risks for dementia, mortality, and increased burdens for patients, caregivers, and health systems.
Numerous interventions have shown promise for post-stroke cognitive rehabilitation, including exercise and cognitive training, the authors wrote. Research hasn’t indicated which programs offer the most efficient or cost-effective options, however.
Dr. Davis and colleagues conducted an economic evaluation alongside the Vitality study, a three-group randomized clinical trial that examined the efficacy of improving cognitive function among patients with chronic stroke through a multicomponent exercise program, cognitive and social enrichment activities, or a control group with balance and tone activities.
The economic evaluation team included a cost-effectiveness analysis (based on incremental cost per cognitive function change) and a cost-utility analysis (incremental cost per quality-adjusted life-year [QALY] gained). The researchers used a cost-effectiveness threshold of CAD $50,000 (Canadian dollars) per QALY for the cost-utility analysis, which was based on precedent treatment in Canada.
The clinical trial included 120 community-dwelling adults aged 55 years and older who had a stroke at least 12 months before the study. Based in the Vancouver metropolitan area, participants were randomly assigned to twice-weekly, 60-minute classes led by trained instructors for 26 weeks. The mean age was 71 years, and 62% of participants were men.
Exercise Effective
Overall, the balance and tone control group had the lowest delivery cost at CAD $777 per person, followed by CAD $1090 per person for the exercise group and CAD $1492 per person for the cognitive and social enrichment group.
After the 6-month intervention, the mean cognitive scores were –0.192 for the exercise group, –0.184 for the cognitive and social enrichment group, and –0.171 for the balance and tone group, indicating better cognitive function across all three groups.
In the cost-effectiveness analysis, the exercise intervention was costlier but more effective than the control group, with an incremental cost-effectiveness ratio (ICER) of CAD –$8823.
In the cost-utility analysis, the exercise intervention was cost saving (less costly and more effective), compared with the control group, with an ICER of CAD –$3381 per QALY gained at the end of the intervention and an ICER of CAD –$154,198 per QALY gained at the end of the 12-month follow-up period. The cognitive and social enrichment program was more costly and more effective than the control group, with an ICER of CAD $101,687 per QALY gained at the end of the intervention and an ICER of CAD $331,306 per QALY gained at the end of the follow-up period.
In additional analyses, the exercise group had the lowest healthcare resource utilization due to lower healthcare costs for physician visits and lab tests.
“This study provides initial data that suggests multicomponent exercise may be a cost-effective solution for combating cognitive decline among stroke survivors,” said Dr. Davis.
Overall, exercise was cost-effective for improving cognitive function but not quality of life among participants. The clinical trial was powered to detect changes in cognitive function rather than quality of life, so it lacked statistical power to detect differences in quality of life, said Dr. Davis.
Exercise programs and cognitive and social enrichment programs show promise for improving cognitive function after stroke, the authors wrote, though future research should focus on optimizing cost-effectiveness and enhancing health-related quality of life.
Considering Additional Benefits
Commenting on the study, Alan Tam, MD, a physiatrist at the Toronto Rehabilitation Institute’s Brain Rehabilitation Program, said, “The authors show that within the timeframe of their analysis, there is a trend to cost-effectiveness for the cognitive intervention being offered.” Dr. Tam did not participate in the research.
“However, the finding is not robust, as less than 50% of their simulations would meet their acceptability level they have defined,” he said. “Given that most of the cost of the intervention is up front, but the benefits are likely lifelong, potentially taking the 12-month analysis to a lifetime analysis would show more significant findings.”
Dr. Tam researches factors associated with brain injury rehabilitation and has explored the cost-effectiveness of a high-intensity outpatient stroke rehabilitation program.
“Presenting this type of work is important,” he said. “While there are interventions that do not meet our definition of statistical significance, especially in the rehabilitation world, there can still be a benefit for patients and health systems.”
The primary study was funded by the Canadian Institutes of Health Research (CIHR) and the Jack Brown and Family Alzheimer Research Foundation Society. Dr. Davis reported receiving grants from the CIHR and Michael Smith Health Research BC during the conduct of the study. Dr. Tam reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Food insecurity a dementia risk factor?
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Patients with Parkinson’s at elevated risk for suicidal thoughts, behavior
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alzheimer’s blood test coming within 5 years, UK group pledges
Alzheimer’s Research UK, the Alzheimer’s Society, and the National Institute for Health and Care Research (NIHR) are collaborating and leading AD researchers to bring a diagnostic blood test to the UK’s National Health Service (NHS).
“Dementia affects around 900,000 people in the UK today, and that number is expected to rise to 1.4 million by 2040. It is the UK’s biggest killer,” Fiona Carragher, with the Alzheimer’s Society, said during a media briefing announcing the project.
Yet, many people face a very long wait of up to 2-4 years to get a dementia diagnosis, and many cases remain undiagnosed, she noted.
A chief reason is lack of access to specialized diagnostic testing. Currently, only 2% of people in the United Kingdom have access to advanced diagnostic tests such as PET scans and lumbar punctures owing to limited availability.
“Getting an early and accurate diagnosis is the pivotal first step to getting help today and unlocking hope for the future” and blood biomarkers provide a “real opportunity to disrupt the diagnostic paradigm,” Ms. Carragher said. It also offers greater opportunities to participate in research and clinical trials, she added.
Attitude shift
Susan Kohlhaas, PhD, with Alzheimer’s Research UK, noted that attitudes toward dementia diagnosis have changed in the past few years. The days when people may have not wanted to know if they have dementia are gone.
Data from the latest wave of the Alzheimer’s Research UK Dementia Attitudes Monitor survey show that 9 in 10 people would seek a diagnosis from their provider. “That’s been driven by awareness of treatments and things that people can proactively do to try and slow disease progression,” Dr. Kohlhaas said.
“As new treatments for dementia become available there will to be a surge in people seeking a diagnosis. At the moment, we don’t have adequate infrastructure to cope with that demand,” Dr. Kohlhaas added.
She noted that blood tests are starting to show their potential as an effective part of the diagnosis and are widely used in research.
“In some cases, they are similar in sensitivity to gold-standard PET scans and lumbar punctures, and they’re less expensive and potentially more scalable on the NHS. What we need to do over the next several years is to understand how they fit into the clinical pathway,” Dr. Kohlhaas said.
The project will involve working with leading dementia researchers to pilot the implementation of potential blood tests in the NHS that can give an early and accurate diagnose of dementia.
The project, which kicks off in January 2024, will receive £5 million ($6.13 million) awarded by the UK Postcode Dream Fund. Specific details regarding the leadership team, participating centers, and specific blood biomarker tests to be trialed will be announced then.
Ms. Carragher and Dr. Kohlhaas reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Alzheimer’s Research UK, the Alzheimer’s Society, and the National Institute for Health and Care Research (NIHR) are collaborating and leading AD researchers to bring a diagnostic blood test to the UK’s National Health Service (NHS).
“Dementia affects around 900,000 people in the UK today, and that number is expected to rise to 1.4 million by 2040. It is the UK’s biggest killer,” Fiona Carragher, with the Alzheimer’s Society, said during a media briefing announcing the project.
Yet, many people face a very long wait of up to 2-4 years to get a dementia diagnosis, and many cases remain undiagnosed, she noted.
A chief reason is lack of access to specialized diagnostic testing. Currently, only 2% of people in the United Kingdom have access to advanced diagnostic tests such as PET scans and lumbar punctures owing to limited availability.
“Getting an early and accurate diagnosis is the pivotal first step to getting help today and unlocking hope for the future” and blood biomarkers provide a “real opportunity to disrupt the diagnostic paradigm,” Ms. Carragher said. It also offers greater opportunities to participate in research and clinical trials, she added.
Attitude shift
Susan Kohlhaas, PhD, with Alzheimer’s Research UK, noted that attitudes toward dementia diagnosis have changed in the past few years. The days when people may have not wanted to know if they have dementia are gone.
Data from the latest wave of the Alzheimer’s Research UK Dementia Attitudes Monitor survey show that 9 in 10 people would seek a diagnosis from their provider. “That’s been driven by awareness of treatments and things that people can proactively do to try and slow disease progression,” Dr. Kohlhaas said.
“As new treatments for dementia become available there will to be a surge in people seeking a diagnosis. At the moment, we don’t have adequate infrastructure to cope with that demand,” Dr. Kohlhaas added.
She noted that blood tests are starting to show their potential as an effective part of the diagnosis and are widely used in research.
“In some cases, they are similar in sensitivity to gold-standard PET scans and lumbar punctures, and they’re less expensive and potentially more scalable on the NHS. What we need to do over the next several years is to understand how they fit into the clinical pathway,” Dr. Kohlhaas said.
The project will involve working with leading dementia researchers to pilot the implementation of potential blood tests in the NHS that can give an early and accurate diagnose of dementia.
The project, which kicks off in January 2024, will receive £5 million ($6.13 million) awarded by the UK Postcode Dream Fund. Specific details regarding the leadership team, participating centers, and specific blood biomarker tests to be trialed will be announced then.
Ms. Carragher and Dr. Kohlhaas reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Alzheimer’s Research UK, the Alzheimer’s Society, and the National Institute for Health and Care Research (NIHR) are collaborating and leading AD researchers to bring a diagnostic blood test to the UK’s National Health Service (NHS).
“Dementia affects around 900,000 people in the UK today, and that number is expected to rise to 1.4 million by 2040. It is the UK’s biggest killer,” Fiona Carragher, with the Alzheimer’s Society, said during a media briefing announcing the project.
Yet, many people face a very long wait of up to 2-4 years to get a dementia diagnosis, and many cases remain undiagnosed, she noted.
A chief reason is lack of access to specialized diagnostic testing. Currently, only 2% of people in the United Kingdom have access to advanced diagnostic tests such as PET scans and lumbar punctures owing to limited availability.
“Getting an early and accurate diagnosis is the pivotal first step to getting help today and unlocking hope for the future” and blood biomarkers provide a “real opportunity to disrupt the diagnostic paradigm,” Ms. Carragher said. It also offers greater opportunities to participate in research and clinical trials, she added.
Attitude shift
Susan Kohlhaas, PhD, with Alzheimer’s Research UK, noted that attitudes toward dementia diagnosis have changed in the past few years. The days when people may have not wanted to know if they have dementia are gone.
Data from the latest wave of the Alzheimer’s Research UK Dementia Attitudes Monitor survey show that 9 in 10 people would seek a diagnosis from their provider. “That’s been driven by awareness of treatments and things that people can proactively do to try and slow disease progression,” Dr. Kohlhaas said.
“As new treatments for dementia become available there will to be a surge in people seeking a diagnosis. At the moment, we don’t have adequate infrastructure to cope with that demand,” Dr. Kohlhaas added.
She noted that blood tests are starting to show their potential as an effective part of the diagnosis and are widely used in research.
“In some cases, they are similar in sensitivity to gold-standard PET scans and lumbar punctures, and they’re less expensive and potentially more scalable on the NHS. What we need to do over the next several years is to understand how they fit into the clinical pathway,” Dr. Kohlhaas said.
The project will involve working with leading dementia researchers to pilot the implementation of potential blood tests in the NHS that can give an early and accurate diagnose of dementia.
The project, which kicks off in January 2024, will receive £5 million ($6.13 million) awarded by the UK Postcode Dream Fund. Specific details regarding the leadership team, participating centers, and specific blood biomarker tests to be trialed will be announced then.
Ms. Carragher and Dr. Kohlhaas reported no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Pandemic tied to a 50% drop in memory, executive function in older adults
TOPLINE:
This was attributed to an increase in known dementia risk factors, including increased alcohol use and a more sedentary lifestyle. This trend persisted into the second year of the pandemic, after social restrictions had eased.
METHODOLOGY:
- In total, 3,140 participants (54% women; mean age, 68 years) in the PROTECT study, a longitudinal aging study in the United Kingdom, completed annual cognitive assessments and self-reported questionnaires related to mental health and lifestyle.
- Investigators analyzed cognition across three time periods: during the year before the pandemic (March 2019 to February 2020), during pandemic year 1 (March 2020 to February 2021), and pandemic year 2 (March 2021 to February 2022).
- Investigators conducted a subanalysis on those with mild cognitive impairment and those with a history of COVID-19 (n = 752).
TAKEAWAY:
- During the first year of the pandemic, when there were societal lockdowns totaling 6 months, significant worsening of executive function and working memory was seen across the entire cohort (effect sizes, 0.15 and 0.51, respectively), in people with mild cognitive impairment (effect sizes, 0.13 and 0.40, respectively), and in those with a previous history of COVID-19 (effect sizes, 0.24 and 0.46, respectively).
- Worsening of working memory was sustained across the whole cohort in the second year of the pandemic after lockdowns were lifted (effect size, 0.47).
- Even after investigators removed data on people with mild cognitive impairment and COVID-19, the decline in executive function (effect size, 0.15; P < .0001) and working memory (effect size, 0.53; P < .0001) persisted.
- Cognitive decline was significantly associated with known risk factors for dementia, such as reduced exercise (P = .0049) and increased alcohol use (P = .049), across the whole cohort, as well as depression (P = .011) in those with a history of COVID-19 and loneliness (P = .0038) in those with mild cognitive impairment.
IN PRACTICE:
Investigators noted that these data add to existing knowledge of long-standing health consequences of COVID-19, especially for older people with memory problems. “On the positive note, there is evidence that lifestyle changes and improved health management can positively influence mental functioning,” study coauthor Dag Aarsland, MD, PhD, professor of old age psychiatry at the Institute of Psychiatry, Psychology & Neuroscience of King’s College London, said in a press release. “The current study underlines the importance of careful monitoring of people at risk during major events such as the pandemic.”
SOURCE:
The study was led by Anne Corbett, PhD, of University of Exeter, and was published online in The Lancet Healthy Longevity. The research was funded by the National Institute for Health and Care Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London and the NIHR Exeter Biomedical Research Centre.
LIMITATIONS:
The study relied on self-reported data. In addition, the PROTECT cohort is self-selected and may skew toward participants with higher education levels.
DISCLOSURES:
Dr. Corbett reported receiving funding from the NIHR and grants from Synexus, reMYND, and Novo Nordisk. Other disclosures are noted in the original article.
A version of this article appeared on Medscape.com.
TOPLINE:
This was attributed to an increase in known dementia risk factors, including increased alcohol use and a more sedentary lifestyle. This trend persisted into the second year of the pandemic, after social restrictions had eased.
METHODOLOGY:
- In total, 3,140 participants (54% women; mean age, 68 years) in the PROTECT study, a longitudinal aging study in the United Kingdom, completed annual cognitive assessments and self-reported questionnaires related to mental health and lifestyle.
- Investigators analyzed cognition across three time periods: during the year before the pandemic (March 2019 to February 2020), during pandemic year 1 (March 2020 to February 2021), and pandemic year 2 (March 2021 to February 2022).
- Investigators conducted a subanalysis on those with mild cognitive impairment and those with a history of COVID-19 (n = 752).
TAKEAWAY:
- During the first year of the pandemic, when there were societal lockdowns totaling 6 months, significant worsening of executive function and working memory was seen across the entire cohort (effect sizes, 0.15 and 0.51, respectively), in people with mild cognitive impairment (effect sizes, 0.13 and 0.40, respectively), and in those with a previous history of COVID-19 (effect sizes, 0.24 and 0.46, respectively).
- Worsening of working memory was sustained across the whole cohort in the second year of the pandemic after lockdowns were lifted (effect size, 0.47).
- Even after investigators removed data on people with mild cognitive impairment and COVID-19, the decline in executive function (effect size, 0.15; P < .0001) and working memory (effect size, 0.53; P < .0001) persisted.
- Cognitive decline was significantly associated with known risk factors for dementia, such as reduced exercise (P = .0049) and increased alcohol use (P = .049), across the whole cohort, as well as depression (P = .011) in those with a history of COVID-19 and loneliness (P = .0038) in those with mild cognitive impairment.
IN PRACTICE:
Investigators noted that these data add to existing knowledge of long-standing health consequences of COVID-19, especially for older people with memory problems. “On the positive note, there is evidence that lifestyle changes and improved health management can positively influence mental functioning,” study coauthor Dag Aarsland, MD, PhD, professor of old age psychiatry at the Institute of Psychiatry, Psychology & Neuroscience of King’s College London, said in a press release. “The current study underlines the importance of careful monitoring of people at risk during major events such as the pandemic.”
SOURCE:
The study was led by Anne Corbett, PhD, of University of Exeter, and was published online in The Lancet Healthy Longevity. The research was funded by the National Institute for Health and Care Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London and the NIHR Exeter Biomedical Research Centre.
LIMITATIONS:
The study relied on self-reported data. In addition, the PROTECT cohort is self-selected and may skew toward participants with higher education levels.
DISCLOSURES:
Dr. Corbett reported receiving funding from the NIHR and grants from Synexus, reMYND, and Novo Nordisk. Other disclosures are noted in the original article.
A version of this article appeared on Medscape.com.
TOPLINE:
This was attributed to an increase in known dementia risk factors, including increased alcohol use and a more sedentary lifestyle. This trend persisted into the second year of the pandemic, after social restrictions had eased.
METHODOLOGY:
- In total, 3,140 participants (54% women; mean age, 68 years) in the PROTECT study, a longitudinal aging study in the United Kingdom, completed annual cognitive assessments and self-reported questionnaires related to mental health and lifestyle.
- Investigators analyzed cognition across three time periods: during the year before the pandemic (March 2019 to February 2020), during pandemic year 1 (March 2020 to February 2021), and pandemic year 2 (March 2021 to February 2022).
- Investigators conducted a subanalysis on those with mild cognitive impairment and those with a history of COVID-19 (n = 752).
TAKEAWAY:
- During the first year of the pandemic, when there were societal lockdowns totaling 6 months, significant worsening of executive function and working memory was seen across the entire cohort (effect sizes, 0.15 and 0.51, respectively), in people with mild cognitive impairment (effect sizes, 0.13 and 0.40, respectively), and in those with a previous history of COVID-19 (effect sizes, 0.24 and 0.46, respectively).
- Worsening of working memory was sustained across the whole cohort in the second year of the pandemic after lockdowns were lifted (effect size, 0.47).
- Even after investigators removed data on people with mild cognitive impairment and COVID-19, the decline in executive function (effect size, 0.15; P < .0001) and working memory (effect size, 0.53; P < .0001) persisted.
- Cognitive decline was significantly associated with known risk factors for dementia, such as reduced exercise (P = .0049) and increased alcohol use (P = .049), across the whole cohort, as well as depression (P = .011) in those with a history of COVID-19 and loneliness (P = .0038) in those with mild cognitive impairment.
IN PRACTICE:
Investigators noted that these data add to existing knowledge of long-standing health consequences of COVID-19, especially for older people with memory problems. “On the positive note, there is evidence that lifestyle changes and improved health management can positively influence mental functioning,” study coauthor Dag Aarsland, MD, PhD, professor of old age psychiatry at the Institute of Psychiatry, Psychology & Neuroscience of King’s College London, said in a press release. “The current study underlines the importance of careful monitoring of people at risk during major events such as the pandemic.”
SOURCE:
The study was led by Anne Corbett, PhD, of University of Exeter, and was published online in The Lancet Healthy Longevity. The research was funded by the National Institute for Health and Care Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London and the NIHR Exeter Biomedical Research Centre.
LIMITATIONS:
The study relied on self-reported data. In addition, the PROTECT cohort is self-selected and may skew toward participants with higher education levels.
DISCLOSURES:
Dr. Corbett reported receiving funding from the NIHR and grants from Synexus, reMYND, and Novo Nordisk. Other disclosures are noted in the original article.
A version of this article appeared on Medscape.com.