User login
Recommending HPV vaccination: How would you grade yourself?
A few weeks ago, a patient asked whether he could get my opinion on something unrelated to his yellow fever vaccine visit: He asked what I thought about the human papillomavirus (HPV) vaccine. His daughter’s primary care physician (PCP) had recommended it, but he “heard that it wasn’t safe.” We had a brief discussion.
My pediatric training days have long since ended, but I was taught never to miss an opportunity to immunize. In this case, it was to help a parent decide to immunize. This type of encounter is not unusual because, as part of preparing persons for international travel, I review their routine immunizations. When documentation of a vaccine is absent, it is pointed out and often remedied after a brief discussion.
Unfortunately, with HPV, too often parents state “my primary care physician said” it was optional, it was not required, or it was never recommended. Some were told to wait until their child was older, and several have safety concerns as did the parent above. I sometimes hear, “it’s not necessary for my child”; this is usually a clue indicating that the issue is more likely about how HPV is transmitted than what HPV vaccine can prevent. Most have welcomed the opportunity to discuss the vaccine, hear about its benefits, and have their questions answered. All leave with HPV information and are directed to websites that provide accurate information. They are referred to their PCP – hopefully to be immunized.
Three vaccines – meningococcal conjugate vaccine (MCV), Tdap, and HPV vaccine – all are recommended for administration at 11-12 years of age. A booster of MCV is recommended at 16 years. However, let’s focus on HPV. In 2007, HPV administration was recommended by the Advisory Committee on Immunization Practices (ACIP) for girls; by 2011, the recommendation was extended to boys. It was a three-dose schedule expected to be completed by age 13 years. In December 2016, a two-dose schedule administered at least 6 months apart was recommended for teens who initiated immunization at less than 15 years. Three doses were still recommended for those initiating HPV after 15 years. This was the only time the number of doses to complete a vaccine series had been decreased based on postlicensure data. So
Vaccine coverage
The National Immunization Survey–Teen (NIS-Teen) monitors vaccine coverage annually amongst adolescents aged 13-17 years. Data are obtained from individuals from every state, as well as the District of Columbia, the U.S. Virgin Islands, and six major urban areas.
According to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2018 Aug 24;67[33]:909-17), HPV vaccination continues to lag behind Tdap and MCV in 2018. Among all adolescents, coverage with one or more doses of HPV was 66%, with up-to-date HPV status in 49%. In contrast, 82% received a dose of MCV, and 89% received a dose of Tdap.
Coverage for receiving one or more doses of HPV among females was 69%, and up-to-date HPV status was 53%; among males, coverage with one or more doses was 63%, and up-to-date HPV status was 44%.
Up-to-date HPV coverage status differed geographically, ranging from 29% in Mississippi to 78% in DC. Overall, eight states and the District of Columbia reported increases in up-to-date status (District of Columbia, Louisiana, Massachusetts, Nebraska, North Carolina, South Carolina, Texas, Vermont, and Virginia). Kudos to Virginia for having the largest increase (20 percentage points).
Coverage also differed between urban and rural areas: one or more doses at 70% vs. 59% and up-to-date status at 52% vs. 42%.
HPV coverage differed by poverty level as well. It was higher for persons living below the poverty level, with one or more doses in 73% and up-to-date status in 54%, compared with persons living at or above poverty level at 63% and 47%, respectively.
HPV-related cancers

The most recent CDC data regarding types of HPV-associated cancers during 2011-2015 suggest that HPV types 16 and 18 account for the majority of cervical (78%) and oropharyngeal (86%) cancers.

Currently, there are more cases of oropharyngeal cancer than cervical, and we have no screening tool for the former.
Safety
Safety has been well documented. Since licensure, no serious safety concerns have been identified, contrary to what has been reported on various social and news media outlets. Yet it remains a concern for many parents who have delayed initiation of vaccine. Efficacy also has been documented in the United States and abroad.
Suggestions for improving HPV immunization coverage
Here are eight suggestions to help you recommend the vaccine and convince hesitant parents of its necessity:
1. Focus on your delivery of the HPV immunization recommendation. Clinician recommendation is the No. 1 reason parents vaccinate. The tone you use and how you make the recommendation can affect how the parent perceives the importance of this vaccine. The following are components of a high-quality recommendation (Academic Pediatrics. 2018;18:S23-S27):
- Routinely recommend vaccine at 11-12 years.
- Recommend vaccine for all preteens, not just those you feel are at risk for infection.
- Recommend the vaccine be given the same day it is discussed.
- Use language that expresses the importance of the HPV vaccine.
2. Use the “announcement or presumptive approach.” You expect the parent to agree with your recommendation. You don’t want to convey that it is an option.
3. Remind parents that immunizing on time means only two doses of HPV.
4. Revisit the topic again during another visit if a parent declines. Data suggest secondary acceptance can be as high as 66%.
5. Consider using a motivational interviewing approach for parents who are very hesitant to vaccinate. Most people want to comply with recommended health interventions.
6. Educate your staff about the importance of HPV vaccine and how it prevents cancer.
7. Determine how well your practice immunizes adolescents. This would be a perfect quality improvement project.
8. Explore “Answering Parents’ Questions” and other resources at www.cdc.gov/hpv to find quick answers to HPV vaccine–related questions .
Why is HPV coverage, a vaccine to prevent cancer, still lagging behind Tdap and MCV? I am as puzzled as others. What I do know is this: Our children will mature and one day become sexually active. They can be exposed to and get infected with HPV, and we can’t predict which ones will not clear the virus and end up developing an HPV-related cancer in the future. At the end of the day, HPV vaccination is cancer prevention.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
A few weeks ago, a patient asked whether he could get my opinion on something unrelated to his yellow fever vaccine visit: He asked what I thought about the human papillomavirus (HPV) vaccine. His daughter’s primary care physician (PCP) had recommended it, but he “heard that it wasn’t safe.” We had a brief discussion.
My pediatric training days have long since ended, but I was taught never to miss an opportunity to immunize. In this case, it was to help a parent decide to immunize. This type of encounter is not unusual because, as part of preparing persons for international travel, I review their routine immunizations. When documentation of a vaccine is absent, it is pointed out and often remedied after a brief discussion.
Unfortunately, with HPV, too often parents state “my primary care physician said” it was optional, it was not required, or it was never recommended. Some were told to wait until their child was older, and several have safety concerns as did the parent above. I sometimes hear, “it’s not necessary for my child”; this is usually a clue indicating that the issue is more likely about how HPV is transmitted than what HPV vaccine can prevent. Most have welcomed the opportunity to discuss the vaccine, hear about its benefits, and have their questions answered. All leave with HPV information and are directed to websites that provide accurate information. They are referred to their PCP – hopefully to be immunized.
Three vaccines – meningococcal conjugate vaccine (MCV), Tdap, and HPV vaccine – all are recommended for administration at 11-12 years of age. A booster of MCV is recommended at 16 years. However, let’s focus on HPV. In 2007, HPV administration was recommended by the Advisory Committee on Immunization Practices (ACIP) for girls; by 2011, the recommendation was extended to boys. It was a three-dose schedule expected to be completed by age 13 years. In December 2016, a two-dose schedule administered at least 6 months apart was recommended for teens who initiated immunization at less than 15 years. Three doses were still recommended for those initiating HPV after 15 years. This was the only time the number of doses to complete a vaccine series had been decreased based on postlicensure data. So
Vaccine coverage
The National Immunization Survey–Teen (NIS-Teen) monitors vaccine coverage annually amongst adolescents aged 13-17 years. Data are obtained from individuals from every state, as well as the District of Columbia, the U.S. Virgin Islands, and six major urban areas.
According to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2018 Aug 24;67[33]:909-17), HPV vaccination continues to lag behind Tdap and MCV in 2018. Among all adolescents, coverage with one or more doses of HPV was 66%, with up-to-date HPV status in 49%. In contrast, 82% received a dose of MCV, and 89% received a dose of Tdap.
Coverage for receiving one or more doses of HPV among females was 69%, and up-to-date HPV status was 53%; among males, coverage with one or more doses was 63%, and up-to-date HPV status was 44%.
Up-to-date HPV coverage status differed geographically, ranging from 29% in Mississippi to 78% in DC. Overall, eight states and the District of Columbia reported increases in up-to-date status (District of Columbia, Louisiana, Massachusetts, Nebraska, North Carolina, South Carolina, Texas, Vermont, and Virginia). Kudos to Virginia for having the largest increase (20 percentage points).
Coverage also differed between urban and rural areas: one or more doses at 70% vs. 59% and up-to-date status at 52% vs. 42%.
HPV coverage differed by poverty level as well. It was higher for persons living below the poverty level, with one or more doses in 73% and up-to-date status in 54%, compared with persons living at or above poverty level at 63% and 47%, respectively.
HPV-related cancers

The most recent CDC data regarding types of HPV-associated cancers during 2011-2015 suggest that HPV types 16 and 18 account for the majority of cervical (78%) and oropharyngeal (86%) cancers.

Currently, there are more cases of oropharyngeal cancer than cervical, and we have no screening tool for the former.
Safety
Safety has been well documented. Since licensure, no serious safety concerns have been identified, contrary to what has been reported on various social and news media outlets. Yet it remains a concern for many parents who have delayed initiation of vaccine. Efficacy also has been documented in the United States and abroad.
Suggestions for improving HPV immunization coverage
Here are eight suggestions to help you recommend the vaccine and convince hesitant parents of its necessity:
1. Focus on your delivery of the HPV immunization recommendation. Clinician recommendation is the No. 1 reason parents vaccinate. The tone you use and how you make the recommendation can affect how the parent perceives the importance of this vaccine. The following are components of a high-quality recommendation (Academic Pediatrics. 2018;18:S23-S27):
- Routinely recommend vaccine at 11-12 years.
- Recommend vaccine for all preteens, not just those you feel are at risk for infection.
- Recommend the vaccine be given the same day it is discussed.
- Use language that expresses the importance of the HPV vaccine.
2. Use the “announcement or presumptive approach.” You expect the parent to agree with your recommendation. You don’t want to convey that it is an option.
3. Remind parents that immunizing on time means only two doses of HPV.
4. Revisit the topic again during another visit if a parent declines. Data suggest secondary acceptance can be as high as 66%.
5. Consider using a motivational interviewing approach for parents who are very hesitant to vaccinate. Most people want to comply with recommended health interventions.
6. Educate your staff about the importance of HPV vaccine and how it prevents cancer.
7. Determine how well your practice immunizes adolescents. This would be a perfect quality improvement project.
8. Explore “Answering Parents’ Questions” and other resources at www.cdc.gov/hpv to find quick answers to HPV vaccine–related questions .
Why is HPV coverage, a vaccine to prevent cancer, still lagging behind Tdap and MCV? I am as puzzled as others. What I do know is this: Our children will mature and one day become sexually active. They can be exposed to and get infected with HPV, and we can’t predict which ones will not clear the virus and end up developing an HPV-related cancer in the future. At the end of the day, HPV vaccination is cancer prevention.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
A few weeks ago, a patient asked whether he could get my opinion on something unrelated to his yellow fever vaccine visit: He asked what I thought about the human papillomavirus (HPV) vaccine. His daughter’s primary care physician (PCP) had recommended it, but he “heard that it wasn’t safe.” We had a brief discussion.
My pediatric training days have long since ended, but I was taught never to miss an opportunity to immunize. In this case, it was to help a parent decide to immunize. This type of encounter is not unusual because, as part of preparing persons for international travel, I review their routine immunizations. When documentation of a vaccine is absent, it is pointed out and often remedied after a brief discussion.
Unfortunately, with HPV, too often parents state “my primary care physician said” it was optional, it was not required, or it was never recommended. Some were told to wait until their child was older, and several have safety concerns as did the parent above. I sometimes hear, “it’s not necessary for my child”; this is usually a clue indicating that the issue is more likely about how HPV is transmitted than what HPV vaccine can prevent. Most have welcomed the opportunity to discuss the vaccine, hear about its benefits, and have their questions answered. All leave with HPV information and are directed to websites that provide accurate information. They are referred to their PCP – hopefully to be immunized.
Three vaccines – meningococcal conjugate vaccine (MCV), Tdap, and HPV vaccine – all are recommended for administration at 11-12 years of age. A booster of MCV is recommended at 16 years. However, let’s focus on HPV. In 2007, HPV administration was recommended by the Advisory Committee on Immunization Practices (ACIP) for girls; by 2011, the recommendation was extended to boys. It was a three-dose schedule expected to be completed by age 13 years. In December 2016, a two-dose schedule administered at least 6 months apart was recommended for teens who initiated immunization at less than 15 years. Three doses were still recommended for those initiating HPV after 15 years. This was the only time the number of doses to complete a vaccine series had been decreased based on postlicensure data. So
Vaccine coverage
The National Immunization Survey–Teen (NIS-Teen) monitors vaccine coverage annually amongst adolescents aged 13-17 years. Data are obtained from individuals from every state, as well as the District of Columbia, the U.S. Virgin Islands, and six major urban areas.
According to the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2018 Aug 24;67[33]:909-17), HPV vaccination continues to lag behind Tdap and MCV in 2018. Among all adolescents, coverage with one or more doses of HPV was 66%, with up-to-date HPV status in 49%. In contrast, 82% received a dose of MCV, and 89% received a dose of Tdap.
Coverage for receiving one or more doses of HPV among females was 69%, and up-to-date HPV status was 53%; among males, coverage with one or more doses was 63%, and up-to-date HPV status was 44%.
Up-to-date HPV coverage status differed geographically, ranging from 29% in Mississippi to 78% in DC. Overall, eight states and the District of Columbia reported increases in up-to-date status (District of Columbia, Louisiana, Massachusetts, Nebraska, North Carolina, South Carolina, Texas, Vermont, and Virginia). Kudos to Virginia for having the largest increase (20 percentage points).
Coverage also differed between urban and rural areas: one or more doses at 70% vs. 59% and up-to-date status at 52% vs. 42%.
HPV coverage differed by poverty level as well. It was higher for persons living below the poverty level, with one or more doses in 73% and up-to-date status in 54%, compared with persons living at or above poverty level at 63% and 47%, respectively.
HPV-related cancers

The most recent CDC data regarding types of HPV-associated cancers during 2011-2015 suggest that HPV types 16 and 18 account for the majority of cervical (78%) and oropharyngeal (86%) cancers.

Currently, there are more cases of oropharyngeal cancer than cervical, and we have no screening tool for the former.
Safety
Safety has been well documented. Since licensure, no serious safety concerns have been identified, contrary to what has been reported on various social and news media outlets. Yet it remains a concern for many parents who have delayed initiation of vaccine. Efficacy also has been documented in the United States and abroad.
Suggestions for improving HPV immunization coverage
Here are eight suggestions to help you recommend the vaccine and convince hesitant parents of its necessity:
1. Focus on your delivery of the HPV immunization recommendation. Clinician recommendation is the No. 1 reason parents vaccinate. The tone you use and how you make the recommendation can affect how the parent perceives the importance of this vaccine. The following are components of a high-quality recommendation (Academic Pediatrics. 2018;18:S23-S27):
- Routinely recommend vaccine at 11-12 years.
- Recommend vaccine for all preteens, not just those you feel are at risk for infection.
- Recommend the vaccine be given the same day it is discussed.
- Use language that expresses the importance of the HPV vaccine.
2. Use the “announcement or presumptive approach.” You expect the parent to agree with your recommendation. You don’t want to convey that it is an option.
3. Remind parents that immunizing on time means only two doses of HPV.
4. Revisit the topic again during another visit if a parent declines. Data suggest secondary acceptance can be as high as 66%.
5. Consider using a motivational interviewing approach for parents who are very hesitant to vaccinate. Most people want to comply with recommended health interventions.
6. Educate your staff about the importance of HPV vaccine and how it prevents cancer.
7. Determine how well your practice immunizes adolescents. This would be a perfect quality improvement project.
8. Explore “Answering Parents’ Questions” and other resources at www.cdc.gov/hpv to find quick answers to HPV vaccine–related questions .
Why is HPV coverage, a vaccine to prevent cancer, still lagging behind Tdap and MCV? I am as puzzled as others. What I do know is this: Our children will mature and one day become sexually active. They can be exposed to and get infected with HPV, and we can’t predict which ones will not clear the virus and end up developing an HPV-related cancer in the future. At the end of the day, HPV vaccination is cancer prevention.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
Dramatic response from pembrolizumab in patient with Lynch syndrome
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Pembrolizumab may provide complete tumor regression in patients with mismatch repair deficiency (Lynch syndrome) who have more than one type of cancer.
Major finding: A woman with primary colonic adenocarcinoma and primary intrahepatic cholangiocarcinoma achieved complete regression of both tumor types after pembrolizumab therapy.
Study details: A case study of a 55-year-old woman with Lynch syndrome who had a family history of gastric, uterine, and colon cancer.
Disclosures: Dr. Musher reported receiving compensation from Lokon.
Source: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
Posttherapy HPV DNA a bad omen in cervical cancer
Residual human papillomavirus DNA in plasma following chemoradiation for HPV-positive cervical cancer is not a good sign, investigators warn.
Among 19 women with HPV-positive cervical cancer who underwent definitive chemoradiation (CRT), detectable HPV DNA in plasma at the end of therapy was associated with a significantly lower rate of progression-free survival (PFS), reported Kathy Han, MD, of the Princess Margaret Cancer Center in Toronto, and her colleagues.
“This prospective multicenter study shows that plasma HPV DNA is detectable at end of CRT in a subset of patients with locally advanced cervical cancer and is associated with poor PFS,” they wrote in JCO Precision Oncology.
The investigators also found that HPV DNA testing 3 months after the end of therapy is more accurate than 3-month fluorodeoxyglucose positron emission tomography (FDG-PET) for detecting minimal residual disease.
In a prospective study, the investigators enrolled 23 women with International Federation of Gynecology and Obstetrics stage IB to IVA cervical adenosquamous, adenocarcinoma, or squamous cell carcinoma who were scheduled to undergo CRT. Three of the patients had no detectable HPV DNA on pretreatment cervical swab, and were excluded from the study, and one patient did not complete therapy, leaving 19 patients with detectable plasma HPV DNA for the analysis.
Of these patients, six had detectable DNA at the end of treatment, and of this group, three had metastatic disease at 3 months. In contrast, only 1 of the 13 patients with no detectable DNA at the end of therapy had developed recurrent disease by the data cutoff.
Six of the 13 patients without detectable DNA at the end of treatment had positive 3-month FDG-PET results, but no definite residual disease on either subsequent imaging or clinical exam. Of these six patients, four had undetectable plasma HPV DNA at 3 months.
The accuracy of 3-month plasma HPV DNA for predicting relapse at 18 months was 77%, compared with 60% for 3-month FDG-PET (P = .008).
PFS at 24 months was significantly better for women with undetectable HPV DNA at the end of therapy, at 92% vs. 50% for women with detectable post-treatment HPV DNA (P = .02).
The authors acknowledged that the study was limited by the small sample size and by an 18-month PFS rate (79%) that was higher than expected, which reduced the statistical power to detect significant associations between HPV DNA and outcomes.
“Additional studies are warranted to confirm the prognostic significance of plasma HPV DNA after CRT and to test the clinical utility of plasma HPV DNA for guiding adjuvant/salvage therapy,” they concluded.
SOURCE: Han K et al. JCO Precis Oncol. 2018 Sep 13. doi: 10.1200/PO.18.00152.
Residual human papillomavirus DNA in plasma following chemoradiation for HPV-positive cervical cancer is not a good sign, investigators warn.
Among 19 women with HPV-positive cervical cancer who underwent definitive chemoradiation (CRT), detectable HPV DNA in plasma at the end of therapy was associated with a significantly lower rate of progression-free survival (PFS), reported Kathy Han, MD, of the Princess Margaret Cancer Center in Toronto, and her colleagues.
“This prospective multicenter study shows that plasma HPV DNA is detectable at end of CRT in a subset of patients with locally advanced cervical cancer and is associated with poor PFS,” they wrote in JCO Precision Oncology.
The investigators also found that HPV DNA testing 3 months after the end of therapy is more accurate than 3-month fluorodeoxyglucose positron emission tomography (FDG-PET) for detecting minimal residual disease.
In a prospective study, the investigators enrolled 23 women with International Federation of Gynecology and Obstetrics stage IB to IVA cervical adenosquamous, adenocarcinoma, or squamous cell carcinoma who were scheduled to undergo CRT. Three of the patients had no detectable HPV DNA on pretreatment cervical swab, and were excluded from the study, and one patient did not complete therapy, leaving 19 patients with detectable plasma HPV DNA for the analysis.
Of these patients, six had detectable DNA at the end of treatment, and of this group, three had metastatic disease at 3 months. In contrast, only 1 of the 13 patients with no detectable DNA at the end of therapy had developed recurrent disease by the data cutoff.
Six of the 13 patients without detectable DNA at the end of treatment had positive 3-month FDG-PET results, but no definite residual disease on either subsequent imaging or clinical exam. Of these six patients, four had undetectable plasma HPV DNA at 3 months.
The accuracy of 3-month plasma HPV DNA for predicting relapse at 18 months was 77%, compared with 60% for 3-month FDG-PET (P = .008).
PFS at 24 months was significantly better for women with undetectable HPV DNA at the end of therapy, at 92% vs. 50% for women with detectable post-treatment HPV DNA (P = .02).
The authors acknowledged that the study was limited by the small sample size and by an 18-month PFS rate (79%) that was higher than expected, which reduced the statistical power to detect significant associations between HPV DNA and outcomes.
“Additional studies are warranted to confirm the prognostic significance of plasma HPV DNA after CRT and to test the clinical utility of plasma HPV DNA for guiding adjuvant/salvage therapy,” they concluded.
SOURCE: Han K et al. JCO Precis Oncol. 2018 Sep 13. doi: 10.1200/PO.18.00152.
Residual human papillomavirus DNA in plasma following chemoradiation for HPV-positive cervical cancer is not a good sign, investigators warn.
Among 19 women with HPV-positive cervical cancer who underwent definitive chemoradiation (CRT), detectable HPV DNA in plasma at the end of therapy was associated with a significantly lower rate of progression-free survival (PFS), reported Kathy Han, MD, of the Princess Margaret Cancer Center in Toronto, and her colleagues.
“This prospective multicenter study shows that plasma HPV DNA is detectable at end of CRT in a subset of patients with locally advanced cervical cancer and is associated with poor PFS,” they wrote in JCO Precision Oncology.
The investigators also found that HPV DNA testing 3 months after the end of therapy is more accurate than 3-month fluorodeoxyglucose positron emission tomography (FDG-PET) for detecting minimal residual disease.
In a prospective study, the investigators enrolled 23 women with International Federation of Gynecology and Obstetrics stage IB to IVA cervical adenosquamous, adenocarcinoma, or squamous cell carcinoma who were scheduled to undergo CRT. Three of the patients had no detectable HPV DNA on pretreatment cervical swab, and were excluded from the study, and one patient did not complete therapy, leaving 19 patients with detectable plasma HPV DNA for the analysis.
Of these patients, six had detectable DNA at the end of treatment, and of this group, three had metastatic disease at 3 months. In contrast, only 1 of the 13 patients with no detectable DNA at the end of therapy had developed recurrent disease by the data cutoff.
Six of the 13 patients without detectable DNA at the end of treatment had positive 3-month FDG-PET results, but no definite residual disease on either subsequent imaging or clinical exam. Of these six patients, four had undetectable plasma HPV DNA at 3 months.
The accuracy of 3-month plasma HPV DNA for predicting relapse at 18 months was 77%, compared with 60% for 3-month FDG-PET (P = .008).
PFS at 24 months was significantly better for women with undetectable HPV DNA at the end of therapy, at 92% vs. 50% for women with detectable post-treatment HPV DNA (P = .02).
The authors acknowledged that the study was limited by the small sample size and by an 18-month PFS rate (79%) that was higher than expected, which reduced the statistical power to detect significant associations between HPV DNA and outcomes.
“Additional studies are warranted to confirm the prognostic significance of plasma HPV DNA after CRT and to test the clinical utility of plasma HPV DNA for guiding adjuvant/salvage therapy,” they concluded.
SOURCE: Han K et al. JCO Precis Oncol. 2018 Sep 13. doi: 10.1200/PO.18.00152.
FROM JCO PRECISION ONCOLOGY
Key clinical point: HPV plasma DNA at the end of definitive chemoradiation is prognostic of poor outcomes in women with cervical cancer.
Major finding: PFS rates at 24 months were 92% for women with no detectable HPV DNA at the end of treatment, vs. 50% for women with residual DNA.
Study details: Prospective multicenter study of 19 women with cervical cancer.
Disclosures: The study was supported by a grant from the University of Toronto. Dr. Han reported having no conflicts of interest.
Source: Han K et al. JCO Precis Oncol. 2018 Sep 13. doi: 10.1200/PO.18.00152.
Vaginal intraepithelial neoplasia: What to do when dysplasia persists after hysterectomy
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
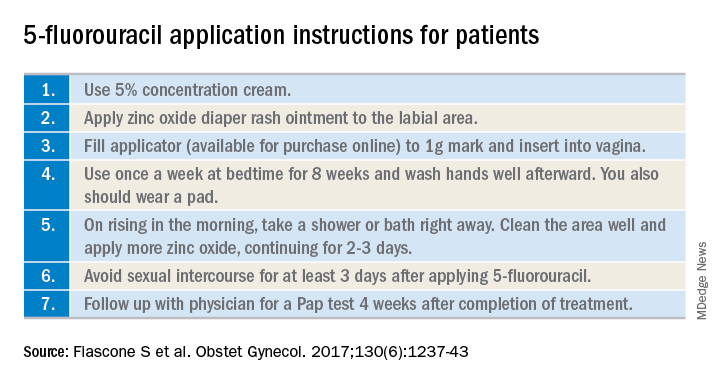
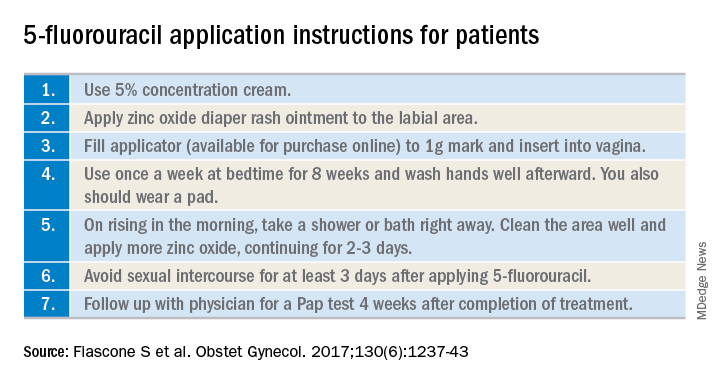
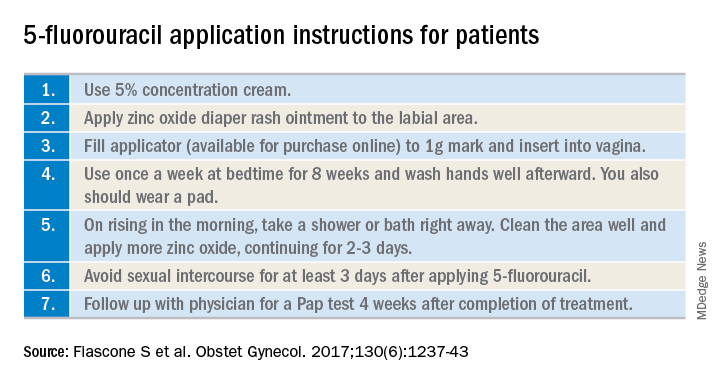
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Pruritus linked to wide variety of cancers
A wide variety of hematologic, dermatologic, and solid organ malignancies are associated with pruritus, a large, single-center, retrospective study suggests.
Blacks with pruritus had a higher odds ratio of hematologic malignancies, among others, while whites had higher likelihood of liver, gastrointestinal, respiratory and gynecologic cancers, results of the study show.
The results by race help address a gap in the literature, according to Shawn G. Kwatra, MD, of Johns Hopkins University, Baltimore, and his coinvestigators.
“Little is known about the association between pruritus and malignancy among different ethnic groups,” Dr. Kwatra and his coauthors wrote in the Journal of the American Academy of Dermatology.
The study shows a stronger association with more types of malignancies than has been reported previously, according to the investigators.
“The main difference is that prior studies focused on diagnosis of malignancy after the onset of pruritus, while our study includes malignancies diagnosed on or after pruritus onset,” they wrote.
Retrospective data for the study, which came from the Johns Hopkins Health System, included 16,925 patients aged 18 years or older who presented with itching or pruritus between April 4, 2013 and Dec. 31, 2017.
Of those 16,925 patients, 2,903 were also diagnosed with a concomitant malignancy during that time period. Compared with patients with no itching diagnosis during that time period, the pruritus patients more likely to have a concomitant malignancy, with an OR of 5.76 (95% confidence interval, 5.53-6.00), Dr. Kwatra and his colleagues found.
Malignancies most strongly associated with pruritus included those of the skin, liver, gallbladder and biliary tract, and hematopoietic system.
Among hematologic malignancies, pruritus was most strongly linked to myeloid leukemia and primary cutaneous lymphoma, while among skin cancers, squamous cell carcinoma was most strongly linked.
Whites had higher odds of any malignancy versus blacks, according to investigators, with ORs of 6.12 (95% CI, 5.81-6.46) and 5.61 (95% CI, 5.21-6.04), respectively.
Blacks with pruritus had higher ORs for hematologic and soft tissue malignancies including those of the muscle, fat, and peripheral nerve, investigators said, while whites had higher ORs for skin and liver malignancies.
The investigators also looked at the prevalence of skin eruptions in patients with pruritus and malignancy. “Eruption is variable by malignancy type and points to differing underlying mechanisms of pruritus,” they reported.
The highest rates of skin eruption were in patients with myeloid leukemia at 66%, followed by bone cancers at 58%, lymphocytic leukemia at 57%, multiple myeloma at 53%, and bronchus at 53%. The lowest rates of skin eruption were in patients with gallbladder and biliary tract, colon, pancreas, and liver malignancies.
Dr. Kwatra reported that he is an advisory board member for Menlo Therapeutics and Trevi Therapeutics.
SOURCE: Kwatra SG et al. J Am Acad Dermatol. 2018 Sep 11. doi: 10.1016/j.jaad.2018.08.044.
A wide variety of hematologic, dermatologic, and solid organ malignancies are associated with pruritus, a large, single-center, retrospective study suggests.
Blacks with pruritus had a higher odds ratio of hematologic malignancies, among others, while whites had higher likelihood of liver, gastrointestinal, respiratory and gynecologic cancers, results of the study show.
The results by race help address a gap in the literature, according to Shawn G. Kwatra, MD, of Johns Hopkins University, Baltimore, and his coinvestigators.
“Little is known about the association between pruritus and malignancy among different ethnic groups,” Dr. Kwatra and his coauthors wrote in the Journal of the American Academy of Dermatology.
The study shows a stronger association with more types of malignancies than has been reported previously, according to the investigators.
“The main difference is that prior studies focused on diagnosis of malignancy after the onset of pruritus, while our study includes malignancies diagnosed on or after pruritus onset,” they wrote.
Retrospective data for the study, which came from the Johns Hopkins Health System, included 16,925 patients aged 18 years or older who presented with itching or pruritus between April 4, 2013 and Dec. 31, 2017.
Of those 16,925 patients, 2,903 were also diagnosed with a concomitant malignancy during that time period. Compared with patients with no itching diagnosis during that time period, the pruritus patients more likely to have a concomitant malignancy, with an OR of 5.76 (95% confidence interval, 5.53-6.00), Dr. Kwatra and his colleagues found.
Malignancies most strongly associated with pruritus included those of the skin, liver, gallbladder and biliary tract, and hematopoietic system.
Among hematologic malignancies, pruritus was most strongly linked to myeloid leukemia and primary cutaneous lymphoma, while among skin cancers, squamous cell carcinoma was most strongly linked.
Whites had higher odds of any malignancy versus blacks, according to investigators, with ORs of 6.12 (95% CI, 5.81-6.46) and 5.61 (95% CI, 5.21-6.04), respectively.
Blacks with pruritus had higher ORs for hematologic and soft tissue malignancies including those of the muscle, fat, and peripheral nerve, investigators said, while whites had higher ORs for skin and liver malignancies.
The investigators also looked at the prevalence of skin eruptions in patients with pruritus and malignancy. “Eruption is variable by malignancy type and points to differing underlying mechanisms of pruritus,” they reported.
The highest rates of skin eruption were in patients with myeloid leukemia at 66%, followed by bone cancers at 58%, lymphocytic leukemia at 57%, multiple myeloma at 53%, and bronchus at 53%. The lowest rates of skin eruption were in patients with gallbladder and biliary tract, colon, pancreas, and liver malignancies.
Dr. Kwatra reported that he is an advisory board member for Menlo Therapeutics and Trevi Therapeutics.
SOURCE: Kwatra SG et al. J Am Acad Dermatol. 2018 Sep 11. doi: 10.1016/j.jaad.2018.08.044.
A wide variety of hematologic, dermatologic, and solid organ malignancies are associated with pruritus, a large, single-center, retrospective study suggests.
Blacks with pruritus had a higher odds ratio of hematologic malignancies, among others, while whites had higher likelihood of liver, gastrointestinal, respiratory and gynecologic cancers, results of the study show.
The results by race help address a gap in the literature, according to Shawn G. Kwatra, MD, of Johns Hopkins University, Baltimore, and his coinvestigators.
“Little is known about the association between pruritus and malignancy among different ethnic groups,” Dr. Kwatra and his coauthors wrote in the Journal of the American Academy of Dermatology.
The study shows a stronger association with more types of malignancies than has been reported previously, according to the investigators.
“The main difference is that prior studies focused on diagnosis of malignancy after the onset of pruritus, while our study includes malignancies diagnosed on or after pruritus onset,” they wrote.
Retrospective data for the study, which came from the Johns Hopkins Health System, included 16,925 patients aged 18 years or older who presented with itching or pruritus between April 4, 2013 and Dec. 31, 2017.
Of those 16,925 patients, 2,903 were also diagnosed with a concomitant malignancy during that time period. Compared with patients with no itching diagnosis during that time period, the pruritus patients more likely to have a concomitant malignancy, with an OR of 5.76 (95% confidence interval, 5.53-6.00), Dr. Kwatra and his colleagues found.
Malignancies most strongly associated with pruritus included those of the skin, liver, gallbladder and biliary tract, and hematopoietic system.
Among hematologic malignancies, pruritus was most strongly linked to myeloid leukemia and primary cutaneous lymphoma, while among skin cancers, squamous cell carcinoma was most strongly linked.
Whites had higher odds of any malignancy versus blacks, according to investigators, with ORs of 6.12 (95% CI, 5.81-6.46) and 5.61 (95% CI, 5.21-6.04), respectively.
Blacks with pruritus had higher ORs for hematologic and soft tissue malignancies including those of the muscle, fat, and peripheral nerve, investigators said, while whites had higher ORs for skin and liver malignancies.
The investigators also looked at the prevalence of skin eruptions in patients with pruritus and malignancy. “Eruption is variable by malignancy type and points to differing underlying mechanisms of pruritus,” they reported.
The highest rates of skin eruption were in patients with myeloid leukemia at 66%, followed by bone cancers at 58%, lymphocytic leukemia at 57%, multiple myeloma at 53%, and bronchus at 53%. The lowest rates of skin eruption were in patients with gallbladder and biliary tract, colon, pancreas, and liver malignancies.
Dr. Kwatra reported that he is an advisory board member for Menlo Therapeutics and Trevi Therapeutics.
SOURCE: Kwatra SG et al. J Am Acad Dermatol. 2018 Sep 11. doi: 10.1016/j.jaad.2018.08.044.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point:
Major finding: Blacks with pruritus had higher odds ratios for hematologic and soft tissue malignancies, while whites had higher ORs for skin and liver malignancies.
Study details: A retrospective study of 16,925 adults with itching or pruritus seen at a tertiary care center.
Disclosures: Dr. Kwatra reported serving as an advisory board member for Menlo Therapeutics and Trevi Therapeutics.
Source: Kwatra SG et al. J Am Acad Dermatol. 2018 Sep 11. doi: 10.1016/j.jaad.2018.08.044.
FILM: Rave review for indocyanine green in lymphatic mapping
Green is just as good – make that better – than blue at identifying sentinel lymph nodes in women with cervical and uterine cancers, results of the multicenter FILM (Fluorescence Imaging for Lymphatic Mapping) study indicate.
Among 176 patients randomly assigned to first have lymphatic mapping with indocyanine green fluorescent dye visualized with near infrared imaging followed by isosulfan blue dye visualized with white light, or the two modalities in the reverse order, indocyanine green identified 50% more lymph nodes in both modified intention-to-treat and per-protocol analyses, reported Michael Frumovitz, MD, from the University of Texas MD Anderson Cancer Center in Houston and colleagues.
“Indocyanine green dye with near-infrared imaging identified significantly more sentinel nodes and more bilateral sentinel nodes than did isosulfan blue dye. It also identified all sentinel nodes with metastatic disease, whereas isosulfan blue dye missed a large proportion of them,” they wrote in the Lancet Oncology.
The FILM study was designed to determine whether fluorescent indocyanine green dye would be noninferior to isosulfan blue dye for accurately identifying sentinel lymph nodes in patients with cancer.
Although several single-center retrospective studies have reported on the use of interstitial injection of indocyanine green for lymphatic mapping in various solid tumors, including uterine and cervical cancers, there were no published studies comparing indocyanine green mapping to isosulfan blue mapping, the standard of care, the authors noted.
They enrolled 180 women aged 18 or older with clinical stage I endometrial or cervical cancers who were undergoing curative surgery and randomly assigned them as described above to have lymphatic mapping with each of the imaging modalities assigned in random order.
The patients but not the operators were masked as to the order of randomization.
Of the 180 patients enrolled, 176 received the intervention, and 13 of these patients were excluded because of major protocol violations, leaving 163 for a per-protocol analysis.
In the per-protocol analysis, 517 sentinel nodes were identified in the 163 patients, and of these, 478 (92%) were confirmed to be lymph nodes on pathological examination. This sample included 219 of 238 nodes identified with both blue and green dyes, all seven nodes revealed by blue dye alone, and 252 of 265 nodes identified by only green dye. Seven sentinel lymph nodes that were not identified by either dye were removed because they were enlarged or appeared suspicious on visual inspection.
In total, green dye identified 97% of lymph nodes in the per-protocol population, and blue dye identified 47%, an absolute difference of 50% (P less than .0001).
In the modified intention-to-treat population, which included all 176 patients randomized and treated, 545 nodes were identified, and 513 (94%) were confirmed to be lymph nodes on pathology. In this sample, 229 (92%) of 248 nodes showed both blue and green, nine nodes were blue only, and 266 (95%) of 279 were green only. Nine sentinel lymph nodes that were not revealed by either blue or green were removed for appearing suspicious or enlarged visually.
In total, in the modified-ITT analysis, 495 of 513 (96%) nodes were identified with the green dye and 238 (46%) were identified with the blue dye, again for an absolute difference of 50% (P less than .0001).
Based on the results of the study, the green dye’s maker, Novadaq Technologies, is submitting an application to the Food and Drug Administration for on-label use of interstitial injection of indocyanine green combined with near-infrared imaging for lymphatic mapping.
The study was funded by Novadaq. Dr. Frumovitz reported grants from Novadaq/Stryker during the conduct of the study, as well as personal fees; grants from Navidea; personal fees from Johnson & Johnson; and personal fees from Genentech outside the submitted work. The other authors declared no competing interests.
SOURCE: Frumovitz M et al. Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30448-0.
In endometrial cancer, the site of injection is still debated; intracervical injection is simple and effective, but hysteroscopic peritumoral injection of the tracer might lead to increased detection of para-aortic sentinel lymph nodes. A combination of pericervical and hysteroscopic peritumoral injection could be useful in selected cases with a higher incidence, such as poorly differentiated carcinomas, or metastasis to isolated para-aortic lymph nodes. The oncologic significance of low-volume metastasis to sentinel lymph nodes and the role of systematic lymphadenectomy in patients with positive sentinel lymph nodes still remain unclear.
In cervical cancer, preliminary data from the LACC trial (NCT00614211) of long-term outcomes of different surgical methods need to be integrated with sentinel lymph node mapping. These data show a detrimental oncologic effect of a minimally invasive approach. If the LACC data are confirmed, two options might be considered: minimally invasive sentinel lymph node mapping as triage to an open radical hysterectomy or the adoption of dedicated near-infrared technology hardware for open surgery.
Through its user-friendliness and effectiveness, indocyanine green is enabling surgeons to transition from systematic lymphadenectomy to sentinel lymph node biopsy. After all, innovation is not only about new technologies, it is also about changing how people think about alternative treatment approaches.
Maria Luisa Gasparri, MD, Michael D. Mueller, MD, and Andrea Papadia, MD, are with the department of obstetrics and gynecology, University Hospital of Bern and University of Bern, Switzerland. Their remarks are adapted and condensed from an editorial accompanying the study (Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30514-X.) The authors declared no competing financial interests.
In endometrial cancer, the site of injection is still debated; intracervical injection is simple and effective, but hysteroscopic peritumoral injection of the tracer might lead to increased detection of para-aortic sentinel lymph nodes. A combination of pericervical and hysteroscopic peritumoral injection could be useful in selected cases with a higher incidence, such as poorly differentiated carcinomas, or metastasis to isolated para-aortic lymph nodes. The oncologic significance of low-volume metastasis to sentinel lymph nodes and the role of systematic lymphadenectomy in patients with positive sentinel lymph nodes still remain unclear.
In cervical cancer, preliminary data from the LACC trial (NCT00614211) of long-term outcomes of different surgical methods need to be integrated with sentinel lymph node mapping. These data show a detrimental oncologic effect of a minimally invasive approach. If the LACC data are confirmed, two options might be considered: minimally invasive sentinel lymph node mapping as triage to an open radical hysterectomy or the adoption of dedicated near-infrared technology hardware for open surgery.
Through its user-friendliness and effectiveness, indocyanine green is enabling surgeons to transition from systematic lymphadenectomy to sentinel lymph node biopsy. After all, innovation is not only about new technologies, it is also about changing how people think about alternative treatment approaches.
Maria Luisa Gasparri, MD, Michael D. Mueller, MD, and Andrea Papadia, MD, are with the department of obstetrics and gynecology, University Hospital of Bern and University of Bern, Switzerland. Their remarks are adapted and condensed from an editorial accompanying the study (Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30514-X.) The authors declared no competing financial interests.
In endometrial cancer, the site of injection is still debated; intracervical injection is simple and effective, but hysteroscopic peritumoral injection of the tracer might lead to increased detection of para-aortic sentinel lymph nodes. A combination of pericervical and hysteroscopic peritumoral injection could be useful in selected cases with a higher incidence, such as poorly differentiated carcinomas, or metastasis to isolated para-aortic lymph nodes. The oncologic significance of low-volume metastasis to sentinel lymph nodes and the role of systematic lymphadenectomy in patients with positive sentinel lymph nodes still remain unclear.
In cervical cancer, preliminary data from the LACC trial (NCT00614211) of long-term outcomes of different surgical methods need to be integrated with sentinel lymph node mapping. These data show a detrimental oncologic effect of a minimally invasive approach. If the LACC data are confirmed, two options might be considered: minimally invasive sentinel lymph node mapping as triage to an open radical hysterectomy or the adoption of dedicated near-infrared technology hardware for open surgery.
Through its user-friendliness and effectiveness, indocyanine green is enabling surgeons to transition from systematic lymphadenectomy to sentinel lymph node biopsy. After all, innovation is not only about new technologies, it is also about changing how people think about alternative treatment approaches.
Maria Luisa Gasparri, MD, Michael D. Mueller, MD, and Andrea Papadia, MD, are with the department of obstetrics and gynecology, University Hospital of Bern and University of Bern, Switzerland. Their remarks are adapted and condensed from an editorial accompanying the study (Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30514-X.) The authors declared no competing financial interests.
Green is just as good – make that better – than blue at identifying sentinel lymph nodes in women with cervical and uterine cancers, results of the multicenter FILM (Fluorescence Imaging for Lymphatic Mapping) study indicate.
Among 176 patients randomly assigned to first have lymphatic mapping with indocyanine green fluorescent dye visualized with near infrared imaging followed by isosulfan blue dye visualized with white light, or the two modalities in the reverse order, indocyanine green identified 50% more lymph nodes in both modified intention-to-treat and per-protocol analyses, reported Michael Frumovitz, MD, from the University of Texas MD Anderson Cancer Center in Houston and colleagues.
“Indocyanine green dye with near-infrared imaging identified significantly more sentinel nodes and more bilateral sentinel nodes than did isosulfan blue dye. It also identified all sentinel nodes with metastatic disease, whereas isosulfan blue dye missed a large proportion of them,” they wrote in the Lancet Oncology.
The FILM study was designed to determine whether fluorescent indocyanine green dye would be noninferior to isosulfan blue dye for accurately identifying sentinel lymph nodes in patients with cancer.
Although several single-center retrospective studies have reported on the use of interstitial injection of indocyanine green for lymphatic mapping in various solid tumors, including uterine and cervical cancers, there were no published studies comparing indocyanine green mapping to isosulfan blue mapping, the standard of care, the authors noted.
They enrolled 180 women aged 18 or older with clinical stage I endometrial or cervical cancers who were undergoing curative surgery and randomly assigned them as described above to have lymphatic mapping with each of the imaging modalities assigned in random order.
The patients but not the operators were masked as to the order of randomization.
Of the 180 patients enrolled, 176 received the intervention, and 13 of these patients were excluded because of major protocol violations, leaving 163 for a per-protocol analysis.
In the per-protocol analysis, 517 sentinel nodes were identified in the 163 patients, and of these, 478 (92%) were confirmed to be lymph nodes on pathological examination. This sample included 219 of 238 nodes identified with both blue and green dyes, all seven nodes revealed by blue dye alone, and 252 of 265 nodes identified by only green dye. Seven sentinel lymph nodes that were not identified by either dye were removed because they were enlarged or appeared suspicious on visual inspection.
In total, green dye identified 97% of lymph nodes in the per-protocol population, and blue dye identified 47%, an absolute difference of 50% (P less than .0001).
In the modified intention-to-treat population, which included all 176 patients randomized and treated, 545 nodes were identified, and 513 (94%) were confirmed to be lymph nodes on pathology. In this sample, 229 (92%) of 248 nodes showed both blue and green, nine nodes were blue only, and 266 (95%) of 279 were green only. Nine sentinel lymph nodes that were not revealed by either blue or green were removed for appearing suspicious or enlarged visually.
In total, in the modified-ITT analysis, 495 of 513 (96%) nodes were identified with the green dye and 238 (46%) were identified with the blue dye, again for an absolute difference of 50% (P less than .0001).
Based on the results of the study, the green dye’s maker, Novadaq Technologies, is submitting an application to the Food and Drug Administration for on-label use of interstitial injection of indocyanine green combined with near-infrared imaging for lymphatic mapping.
The study was funded by Novadaq. Dr. Frumovitz reported grants from Novadaq/Stryker during the conduct of the study, as well as personal fees; grants from Navidea; personal fees from Johnson & Johnson; and personal fees from Genentech outside the submitted work. The other authors declared no competing interests.
SOURCE: Frumovitz M et al. Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30448-0.
Green is just as good – make that better – than blue at identifying sentinel lymph nodes in women with cervical and uterine cancers, results of the multicenter FILM (Fluorescence Imaging for Lymphatic Mapping) study indicate.
Among 176 patients randomly assigned to first have lymphatic mapping with indocyanine green fluorescent dye visualized with near infrared imaging followed by isosulfan blue dye visualized with white light, or the two modalities in the reverse order, indocyanine green identified 50% more lymph nodes in both modified intention-to-treat and per-protocol analyses, reported Michael Frumovitz, MD, from the University of Texas MD Anderson Cancer Center in Houston and colleagues.
“Indocyanine green dye with near-infrared imaging identified significantly more sentinel nodes and more bilateral sentinel nodes than did isosulfan blue dye. It also identified all sentinel nodes with metastatic disease, whereas isosulfan blue dye missed a large proportion of them,” they wrote in the Lancet Oncology.
The FILM study was designed to determine whether fluorescent indocyanine green dye would be noninferior to isosulfan blue dye for accurately identifying sentinel lymph nodes in patients with cancer.
Although several single-center retrospective studies have reported on the use of interstitial injection of indocyanine green for lymphatic mapping in various solid tumors, including uterine and cervical cancers, there were no published studies comparing indocyanine green mapping to isosulfan blue mapping, the standard of care, the authors noted.
They enrolled 180 women aged 18 or older with clinical stage I endometrial or cervical cancers who were undergoing curative surgery and randomly assigned them as described above to have lymphatic mapping with each of the imaging modalities assigned in random order.
The patients but not the operators were masked as to the order of randomization.
Of the 180 patients enrolled, 176 received the intervention, and 13 of these patients were excluded because of major protocol violations, leaving 163 for a per-protocol analysis.
In the per-protocol analysis, 517 sentinel nodes were identified in the 163 patients, and of these, 478 (92%) were confirmed to be lymph nodes on pathological examination. This sample included 219 of 238 nodes identified with both blue and green dyes, all seven nodes revealed by blue dye alone, and 252 of 265 nodes identified by only green dye. Seven sentinel lymph nodes that were not identified by either dye were removed because they were enlarged or appeared suspicious on visual inspection.
In total, green dye identified 97% of lymph nodes in the per-protocol population, and blue dye identified 47%, an absolute difference of 50% (P less than .0001).
In the modified intention-to-treat population, which included all 176 patients randomized and treated, 545 nodes were identified, and 513 (94%) were confirmed to be lymph nodes on pathology. In this sample, 229 (92%) of 248 nodes showed both blue and green, nine nodes were blue only, and 266 (95%) of 279 were green only. Nine sentinel lymph nodes that were not revealed by either blue or green were removed for appearing suspicious or enlarged visually.
In total, in the modified-ITT analysis, 495 of 513 (96%) nodes were identified with the green dye and 238 (46%) were identified with the blue dye, again for an absolute difference of 50% (P less than .0001).
Based on the results of the study, the green dye’s maker, Novadaq Technologies, is submitting an application to the Food and Drug Administration for on-label use of interstitial injection of indocyanine green combined with near-infrared imaging for lymphatic mapping.
The study was funded by Novadaq. Dr. Frumovitz reported grants from Novadaq/Stryker during the conduct of the study, as well as personal fees; grants from Navidea; personal fees from Johnson & Johnson; and personal fees from Genentech outside the submitted work. The other authors declared no competing interests.
SOURCE: Frumovitz M et al. Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30448-0.
FROM LANCET ONCOLOGY
Key clinical point: Fluorescent indocyanine green dye with near-infrared visualization was superior to isosulfan blue dye at identifying lymph nodes in patients with early-stage cervical and endometrial cancers.
Major finding: Indocyanine green identified 50% more lymph nodes than isosulfan blue, the standard of care.
Study details: Randomized, phase 3, within-patient, noninferiority trial in 176 women with clinical stage I endometrial or cervical cancers.
Disclosures: The study was funded by Novadaq. Dr. Frumovitz reported grants from Novadaq/Stryker during the conduct of the study, as well as personal fees; grants from Navidea, personal fees from Johnson & Johnson; and personal fees from Genentech outside the submitted work. The other authors declared no competing interests.
Source: Frumovitz M et al. Lancet Oncol. 2018 Aug 21. doi: 10.1016/S1470-2045(18)30448-0.
Cervical cancer screening recommendations vary by age and risk
Screen women for cervical cancer with basic cytology starting at age 21 years, and consider adding high-risk human papillomavirus (hrHPV) testing alone or with cytology for women aged 30 years and older, the U.S. Preventive Services Task Force recommended in an updated statement on cervical cancer screening .
The statement, accompanying evidence report, and a modeling study were published online in JAMA.
Cervical cancer deaths in the United States have declined from 2.8 deaths per 100,000 women in 2000 to 2.3 deaths per 100,000 women in 2015 because of the adoption of widespread screening, according to Susan J. Curry, PhD., of the University of Iowa, Iowa City, and her colleagues in the USPSTF (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
Based on the latest evidence and the modeling study, the USPSTF gives an A recommendation to screening women aged 21-29 years for cervical cancer every 3 years with cervical cytology alone. The task force also gives an A to screening women aged 30-65 years every 5 years with either hrHPV testing alone or in combination with cytology.
The task force recommends against screening (D recommendation) for women younger than 21 years, older than 65 years with a history of screening and low cervical cancer risk, and women who have had hysterectomies with removal of the cervix and no history of cervical cancer risk.
To update the previous recommendations issued in 2012, the task force reviewed the latest evidence and commissioned a modeling study to help determine the best screening strategies in terms of age, screening intervals, and risks vs. benefits.
In the model, researchers assessed 19 strategies for cervical cancer screening based on a hypothetical cohort of women who began screening at 21 years of age.
Overall, the different strategies were similar in effectiveness, but primary hrHPV testing and alternative cotesting were slightly more effective: Cervical cancer deaths ranged from 0.23 to 0.29 deaths per 1,000 women in strategies involving hrHPV testing or cotesting, vs. 0.30 to 0.76 deaths per 1,000 women for strategies based on the current guidelines.
In addition, switching the age of hrHPV testing from 25 years to 30 years and using a 5-year screening interval showed the most effectiveness in terms of risks vs. harms, wrote Jane K. Kim, PhD, of Harvard University, Boston, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872). “Switching from cytology to 5-year primary hrHPV testing at age 30 years (strategy 14) was associated with a ratio of 640 colposcopies per cancer case averted; earlier switch ages required a greater number of colposcopies per cancer case averted.”
The recommendations also were supported by an evidence report including eight randomized, controlled trials of 410,556 women, five cohort studies of 402,615 women, and a meta-analysis of individual participant data including 176,464 women.
The evidence report sought to address the benefits and harms of cervical cancer screening using hrHPV screening alone as the primary screening method or paired with cytology (cotesting), compared with primary screening using cytology alone.
Overall, both hrHPV and hrHPV plus cytology were associated with higher rates of false-positives and colposcopy compared with cytology alone, “which could lead to more treatments with potential harms,” wrote Joy Melnikow, MD, of the University of California, Davis, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400.
In addition, hrHPV testing yielded higher rates of positive cervical intraepithelial neoplasia, compared with cytology alone as initial screening.
However, further research is needed to address the impact of any cervical cancer screening strategies in populations with limited access to health care and screening, the researchers noted.
The updated USPSTF recommendations are largely in line with those issued by leading women’s health organizations including the American College of Obstetricians and Gynecologists, ASCCP, and the Society for Gynecologic Oncology, according to a joint statement.
“With a number of screening options now available, the new guidelines emphasize the importance of the patient-provider shared decision-making process to assist women in making an informed choice about which screening method is most suitable for them,” according to the statement, “However, more importantly, there needs to be a continued effort to ensure all women are adequately screened because a significant number of women in the country are not. It’s also essential for women to have access to all of the tests and that they are appropriately covered by insurance companies.
“We hope the USPSTF recommendations foster more discussions between patients and providers about cervical cancer screening, promote opportunities for patient education on the benefits and safety of HPV vaccination for cervical cancer prevention and encourage providers to offer HPV vaccines in their offices,” the statement noted.
The USPSTF research was funded by the Agency for Healthcare Research and Quality. The researchers for the modeling report were supported in part by a National Cancer Institute grant. The researchers had no relevant financial conflicts to disclose.
SOURCES: Kim J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872; Melnikow J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400; Curry S et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
In 2016, the Society for Gynecologic Oncology (SGO) recommended screening with the newly approved hrHPV test for women aged 25 years and older, with rescreening 3 years later if the test was negative, George F. Sawaya, MD, wrote in an accompanying editorial published in JAMA Internal Medicine. The new recommendations from the U.S. Preventive Services Task Force do not endorse a single triage strategy, and do not consider costs, he said.
“Although the USPSTF sets the standard for evidence-based recommendations and acknowledges the critical value of high-quality evidence in making recommendations, it might reasonably be asked, where is the evidence of value in cervical cancer screening?” Dr. Sawaya wrote.
The updated USPSTF recommendations differ from the SGO recommendation by changing the starting age for hrHPV testing to 30 years from 25, and rescreening at 5-year intervals.
“The USPSTF recommendation that HPV testing not begin until age 30 years seems prudent,” Dr. Sawaya said, in light of the evidence report and modeling analysis of harms and benefits. He noted that the evidence reviewed by the task force showed that HPV testing and cotesting resulting in a small amount of life-years gained compared with no testing, but with the trade-off of more follow-up tests and colposcopies.
“From the perspective of society, it has been proposed that cost-effectiveness analyses be an essential part of the guideline process,” Dr. Sawaya noted. “To assist in policy decisions that many professional societies will soon face, a study that I am leading is seeking to use cost-effectiveness analyses to determine the range of reasonable options for cervical cancer screening. Such analyses may inform future screening recommendations.”
Dr. Sawaya is affiliated with the University of California, San Francisco. These comments are taken from an editorial accompanying USPSTF recommendations on cervical cancer screening (JAMA Intern Med. 2018 Aug 21. doi: 10.1001/jamainternmed.2018.4282). He disclosed serving as the principal investigator of a National Cancer Institute study on cost-effectiveness analyses to determine reasonable options for cervical cancer screening. He also served as a member of the U.S. Preventive Services Task Force from 2004 to 2008.
In 2016, the Society for Gynecologic Oncology (SGO) recommended screening with the newly approved hrHPV test for women aged 25 years and older, with rescreening 3 years later if the test was negative, George F. Sawaya, MD, wrote in an accompanying editorial published in JAMA Internal Medicine. The new recommendations from the U.S. Preventive Services Task Force do not endorse a single triage strategy, and do not consider costs, he said.
“Although the USPSTF sets the standard for evidence-based recommendations and acknowledges the critical value of high-quality evidence in making recommendations, it might reasonably be asked, where is the evidence of value in cervical cancer screening?” Dr. Sawaya wrote.
The updated USPSTF recommendations differ from the SGO recommendation by changing the starting age for hrHPV testing to 30 years from 25, and rescreening at 5-year intervals.
“The USPSTF recommendation that HPV testing not begin until age 30 years seems prudent,” Dr. Sawaya said, in light of the evidence report and modeling analysis of harms and benefits. He noted that the evidence reviewed by the task force showed that HPV testing and cotesting resulting in a small amount of life-years gained compared with no testing, but with the trade-off of more follow-up tests and colposcopies.
“From the perspective of society, it has been proposed that cost-effectiveness analyses be an essential part of the guideline process,” Dr. Sawaya noted. “To assist in policy decisions that many professional societies will soon face, a study that I am leading is seeking to use cost-effectiveness analyses to determine the range of reasonable options for cervical cancer screening. Such analyses may inform future screening recommendations.”
Dr. Sawaya is affiliated with the University of California, San Francisco. These comments are taken from an editorial accompanying USPSTF recommendations on cervical cancer screening (JAMA Intern Med. 2018 Aug 21. doi: 10.1001/jamainternmed.2018.4282). He disclosed serving as the principal investigator of a National Cancer Institute study on cost-effectiveness analyses to determine reasonable options for cervical cancer screening. He also served as a member of the U.S. Preventive Services Task Force from 2004 to 2008.
In 2016, the Society for Gynecologic Oncology (SGO) recommended screening with the newly approved hrHPV test for women aged 25 years and older, with rescreening 3 years later if the test was negative, George F. Sawaya, MD, wrote in an accompanying editorial published in JAMA Internal Medicine. The new recommendations from the U.S. Preventive Services Task Force do not endorse a single triage strategy, and do not consider costs, he said.
“Although the USPSTF sets the standard for evidence-based recommendations and acknowledges the critical value of high-quality evidence in making recommendations, it might reasonably be asked, where is the evidence of value in cervical cancer screening?” Dr. Sawaya wrote.
The updated USPSTF recommendations differ from the SGO recommendation by changing the starting age for hrHPV testing to 30 years from 25, and rescreening at 5-year intervals.
“The USPSTF recommendation that HPV testing not begin until age 30 years seems prudent,” Dr. Sawaya said, in light of the evidence report and modeling analysis of harms and benefits. He noted that the evidence reviewed by the task force showed that HPV testing and cotesting resulting in a small amount of life-years gained compared with no testing, but with the trade-off of more follow-up tests and colposcopies.
“From the perspective of society, it has been proposed that cost-effectiveness analyses be an essential part of the guideline process,” Dr. Sawaya noted. “To assist in policy decisions that many professional societies will soon face, a study that I am leading is seeking to use cost-effectiveness analyses to determine the range of reasonable options for cervical cancer screening. Such analyses may inform future screening recommendations.”
Dr. Sawaya is affiliated with the University of California, San Francisco. These comments are taken from an editorial accompanying USPSTF recommendations on cervical cancer screening (JAMA Intern Med. 2018 Aug 21. doi: 10.1001/jamainternmed.2018.4282). He disclosed serving as the principal investigator of a National Cancer Institute study on cost-effectiveness analyses to determine reasonable options for cervical cancer screening. He also served as a member of the U.S. Preventive Services Task Force from 2004 to 2008.
Screen women for cervical cancer with basic cytology starting at age 21 years, and consider adding high-risk human papillomavirus (hrHPV) testing alone or with cytology for women aged 30 years and older, the U.S. Preventive Services Task Force recommended in an updated statement on cervical cancer screening .
The statement, accompanying evidence report, and a modeling study were published online in JAMA.
Cervical cancer deaths in the United States have declined from 2.8 deaths per 100,000 women in 2000 to 2.3 deaths per 100,000 women in 2015 because of the adoption of widespread screening, according to Susan J. Curry, PhD., of the University of Iowa, Iowa City, and her colleagues in the USPSTF (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
Based on the latest evidence and the modeling study, the USPSTF gives an A recommendation to screening women aged 21-29 years for cervical cancer every 3 years with cervical cytology alone. The task force also gives an A to screening women aged 30-65 years every 5 years with either hrHPV testing alone or in combination with cytology.
The task force recommends against screening (D recommendation) for women younger than 21 years, older than 65 years with a history of screening and low cervical cancer risk, and women who have had hysterectomies with removal of the cervix and no history of cervical cancer risk.
To update the previous recommendations issued in 2012, the task force reviewed the latest evidence and commissioned a modeling study to help determine the best screening strategies in terms of age, screening intervals, and risks vs. benefits.
In the model, researchers assessed 19 strategies for cervical cancer screening based on a hypothetical cohort of women who began screening at 21 years of age.
Overall, the different strategies were similar in effectiveness, but primary hrHPV testing and alternative cotesting were slightly more effective: Cervical cancer deaths ranged from 0.23 to 0.29 deaths per 1,000 women in strategies involving hrHPV testing or cotesting, vs. 0.30 to 0.76 deaths per 1,000 women for strategies based on the current guidelines.
In addition, switching the age of hrHPV testing from 25 years to 30 years and using a 5-year screening interval showed the most effectiveness in terms of risks vs. harms, wrote Jane K. Kim, PhD, of Harvard University, Boston, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872). “Switching from cytology to 5-year primary hrHPV testing at age 30 years (strategy 14) was associated with a ratio of 640 colposcopies per cancer case averted; earlier switch ages required a greater number of colposcopies per cancer case averted.”
The recommendations also were supported by an evidence report including eight randomized, controlled trials of 410,556 women, five cohort studies of 402,615 women, and a meta-analysis of individual participant data including 176,464 women.
The evidence report sought to address the benefits and harms of cervical cancer screening using hrHPV screening alone as the primary screening method or paired with cytology (cotesting), compared with primary screening using cytology alone.
Overall, both hrHPV and hrHPV plus cytology were associated with higher rates of false-positives and colposcopy compared with cytology alone, “which could lead to more treatments with potential harms,” wrote Joy Melnikow, MD, of the University of California, Davis, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400.
In addition, hrHPV testing yielded higher rates of positive cervical intraepithelial neoplasia, compared with cytology alone as initial screening.
However, further research is needed to address the impact of any cervical cancer screening strategies in populations with limited access to health care and screening, the researchers noted.
The updated USPSTF recommendations are largely in line with those issued by leading women’s health organizations including the American College of Obstetricians and Gynecologists, ASCCP, and the Society for Gynecologic Oncology, according to a joint statement.
“With a number of screening options now available, the new guidelines emphasize the importance of the patient-provider shared decision-making process to assist women in making an informed choice about which screening method is most suitable for them,” according to the statement, “However, more importantly, there needs to be a continued effort to ensure all women are adequately screened because a significant number of women in the country are not. It’s also essential for women to have access to all of the tests and that they are appropriately covered by insurance companies.
“We hope the USPSTF recommendations foster more discussions between patients and providers about cervical cancer screening, promote opportunities for patient education on the benefits and safety of HPV vaccination for cervical cancer prevention and encourage providers to offer HPV vaccines in their offices,” the statement noted.
The USPSTF research was funded by the Agency for Healthcare Research and Quality. The researchers for the modeling report were supported in part by a National Cancer Institute grant. The researchers had no relevant financial conflicts to disclose.
SOURCES: Kim J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872; Melnikow J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400; Curry S et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
Screen women for cervical cancer with basic cytology starting at age 21 years, and consider adding high-risk human papillomavirus (hrHPV) testing alone or with cytology for women aged 30 years and older, the U.S. Preventive Services Task Force recommended in an updated statement on cervical cancer screening .
The statement, accompanying evidence report, and a modeling study were published online in JAMA.
Cervical cancer deaths in the United States have declined from 2.8 deaths per 100,000 women in 2000 to 2.3 deaths per 100,000 women in 2015 because of the adoption of widespread screening, according to Susan J. Curry, PhD., of the University of Iowa, Iowa City, and her colleagues in the USPSTF (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
Based on the latest evidence and the modeling study, the USPSTF gives an A recommendation to screening women aged 21-29 years for cervical cancer every 3 years with cervical cytology alone. The task force also gives an A to screening women aged 30-65 years every 5 years with either hrHPV testing alone or in combination with cytology.
The task force recommends against screening (D recommendation) for women younger than 21 years, older than 65 years with a history of screening and low cervical cancer risk, and women who have had hysterectomies with removal of the cervix and no history of cervical cancer risk.
To update the previous recommendations issued in 2012, the task force reviewed the latest evidence and commissioned a modeling study to help determine the best screening strategies in terms of age, screening intervals, and risks vs. benefits.
In the model, researchers assessed 19 strategies for cervical cancer screening based on a hypothetical cohort of women who began screening at 21 years of age.
Overall, the different strategies were similar in effectiveness, but primary hrHPV testing and alternative cotesting were slightly more effective: Cervical cancer deaths ranged from 0.23 to 0.29 deaths per 1,000 women in strategies involving hrHPV testing or cotesting, vs. 0.30 to 0.76 deaths per 1,000 women for strategies based on the current guidelines.
In addition, switching the age of hrHPV testing from 25 years to 30 years and using a 5-year screening interval showed the most effectiveness in terms of risks vs. harms, wrote Jane K. Kim, PhD, of Harvard University, Boston, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872). “Switching from cytology to 5-year primary hrHPV testing at age 30 years (strategy 14) was associated with a ratio of 640 colposcopies per cancer case averted; earlier switch ages required a greater number of colposcopies per cancer case averted.”
The recommendations also were supported by an evidence report including eight randomized, controlled trials of 410,556 women, five cohort studies of 402,615 women, and a meta-analysis of individual participant data including 176,464 women.
The evidence report sought to address the benefits and harms of cervical cancer screening using hrHPV screening alone as the primary screening method or paired with cytology (cotesting), compared with primary screening using cytology alone.
Overall, both hrHPV and hrHPV plus cytology were associated with higher rates of false-positives and colposcopy compared with cytology alone, “which could lead to more treatments with potential harms,” wrote Joy Melnikow, MD, of the University of California, Davis, and her colleagues (JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400.
In addition, hrHPV testing yielded higher rates of positive cervical intraepithelial neoplasia, compared with cytology alone as initial screening.
However, further research is needed to address the impact of any cervical cancer screening strategies in populations with limited access to health care and screening, the researchers noted.
The updated USPSTF recommendations are largely in line with those issued by leading women’s health organizations including the American College of Obstetricians and Gynecologists, ASCCP, and the Society for Gynecologic Oncology, according to a joint statement.
“With a number of screening options now available, the new guidelines emphasize the importance of the patient-provider shared decision-making process to assist women in making an informed choice about which screening method is most suitable for them,” according to the statement, “However, more importantly, there needs to be a continued effort to ensure all women are adequately screened because a significant number of women in the country are not. It’s also essential for women to have access to all of the tests and that they are appropriately covered by insurance companies.
“We hope the USPSTF recommendations foster more discussions between patients and providers about cervical cancer screening, promote opportunities for patient education on the benefits and safety of HPV vaccination for cervical cancer prevention and encourage providers to offer HPV vaccines in their offices,” the statement noted.
The USPSTF research was funded by the Agency for Healthcare Research and Quality. The researchers for the modeling report were supported in part by a National Cancer Institute grant. The researchers had no relevant financial conflicts to disclose.
SOURCES: Kim J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2017.19872; Melnikow J et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10400; Curry S et al. JAMA. 2018 Aug 21. doi: 10.1001/jama.2018.10897.
FROM JAMA
First-ever gestational trophoblastic neoplasia guidelines published
The National Comprehensive Cancer Network (NCCN) has issued its first-ever clinical practice guidelines for the treatment of gestational trophoblastic neoplasia (GTN), a rare, serious complication of pregnancy that can often be cured, but can have devastating consequences if mismanaged or if treatment is needlessly delayed.
David Mutch, MD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, who heads the NCCN Clinical Practice Guidelines in Oncology Committee for GTN, explained the critical importance of the GTN guidelines.
“It’s a rare disease, people weren’t that familiar with it, and they often are patients treated with single-agent therapy when they should be treated with multi-agent therapy,” he said in an interview.
“There wasn’t a clear understanding of what to do except by those people who treated these patients regularly. The only thing most people knew was that it was very chemosensitive and should be curable, but it’s only curable if you follow the appropriate algorithms,” he continued.
The algorithms he referred to were established by a handful of centers with expertise and experience in diagnosing and treating these rare conditions, including noninvasive hydatidiform mole, invasive mole, and choriocarcinoma, the most aggressive form of GTN.
Neil Horowitz, MD, director of clinical research in gynecologic oncology at the Dana-Farber Cancer Institute in Boston, works with colleagues in one of those referral centers, the New England Trophoblastic Disease Center, and is familiar with the new guidelines. As with other rare malignancies, there are data to suggest that patients with GTN who are treated in centers of excellence with higher patient volumes have better outcomes than do similar patients treated in a community setting, he said in an interview.
Placental origins
GTNs arise from placental rather than maternal tissue. They most commonly present with vaginal bleeding and a rapidly enlarging uterus, and may be accompanied by pelvic pain or pressure, anemia, severe nausea/vomiting (hyperemesis gravidarum), hyperthyroidism, or early-pregnancy preeclampsia.
The overall reported incidence of GTN in the United States, including hydatidiform mole, is approximately 110 to 120 per 100,000 pregnancies, and the reported incidence of choriocarcinoma is about 2 to 7 per 100,000, according to the National Cancer Institute.
The GTN guidelines provide evidence-based recommendations about optimal approaches to GTN in all of its known forms. For example, the section on noninvasive hydatidiform mole recommends the tests that should be routinely performed during workup, followed by surgery with either suction, dilation and curettage – preferably under ultrasound guidance – or hysterectomy for women who are older or who do not wish to preserve fertility.
The guidelines also specify steps that should be taken for diagnosis and staging of GTN as well as risk-based therapeutic approaches.
For example, the guidelines recommend therapy with either methotrexate alone or alternating with leucovorin, or dactinomycin alone for patients with confirmed low risk GTN, defined as a prognostic score less than 7.
The prognostic scoring index, also included in the guidelines, considers risk factors such as age, prior pregnancies, interval from an index pregnancy, pretreatment human chorionic gonadotropin (hCG) levels, site and number of metastases, largest tumor size, and previous chemotherapy failure.
For patients with high-risk GTN, defined as FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stages II-III with a prognostic score of 7 or greater, or FIGO stage IV, chemotherapy with the EMA/CO regimen is recommended. This aggressive regimen consists of etoposide, methotrexate, dactinomycin (the “EMA “component) plus cyclophosphamide and vincristine (the “CO” component).
“In my mind, the most important part of the guidelines is reiterating how the diagnosis of GTN should be made, and importantly, how the score should be calculated so that women are put in the appropriate low-risk or high-risk category, so they get the right treatment,” Dr. Horowitz said.
Reassuring insurers
Dr. Mutch said that he and his colleagues in GTN centers sometimes treat patients with intermediate or high-risk disease who were started on single-agent therapy or suboptimal therapies and present with advanced, drug-resistant disease.
“These guidelines were established so that people could see exactly what needs to be done when,” he said.
The guidelines also are critical for convincing third-party payers about the need for specific treatments, he added.
“I had a high-risk patient who needed EMA/CO, and the insurance company said ‘well, there’s no NCCN guidelines – we won’t approve it.’ So then I had to wait 3 days while it went through peer review. Meanwhile, the tumor doubled in size, and then the nurse who was reviewing it declined the ‘CO’ part, so that was delayed a week, and it really jeopardized this patient’s survival,” Dr. Mutch said.
The guidelines also include recommendations for patients with special clinical situations, such as women with clinical responses to EMA/CO who continue to have plateauing low levels of hCG or have a re-elevation of hCG levels after having a complete response to EMA/CO.
There are also specific recommendations for treatment of two even rarer intermediate trophoblastic tumor types: placental-site trophoblastic tumor and epithelioid trophoblastic tumor.
The guidelines are supported by the NCCN. Dr. Mutch reported consulting/advisory board participation for Clovis. Dr. Horowitz reported having no relationships to disclose.
SOURCE: Gestational Trophoblastic Neoplasia. NCCN.org, Version 1.2019, published Aug. 9, 2018.
The National Comprehensive Cancer Network (NCCN) has issued its first-ever clinical practice guidelines for the treatment of gestational trophoblastic neoplasia (GTN), a rare, serious complication of pregnancy that can often be cured, but can have devastating consequences if mismanaged or if treatment is needlessly delayed.
David Mutch, MD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, who heads the NCCN Clinical Practice Guidelines in Oncology Committee for GTN, explained the critical importance of the GTN guidelines.
“It’s a rare disease, people weren’t that familiar with it, and they often are patients treated with single-agent therapy when they should be treated with multi-agent therapy,” he said in an interview.
“There wasn’t a clear understanding of what to do except by those people who treated these patients regularly. The only thing most people knew was that it was very chemosensitive and should be curable, but it’s only curable if you follow the appropriate algorithms,” he continued.
The algorithms he referred to were established by a handful of centers with expertise and experience in diagnosing and treating these rare conditions, including noninvasive hydatidiform mole, invasive mole, and choriocarcinoma, the most aggressive form of GTN.
Neil Horowitz, MD, director of clinical research in gynecologic oncology at the Dana-Farber Cancer Institute in Boston, works with colleagues in one of those referral centers, the New England Trophoblastic Disease Center, and is familiar with the new guidelines. As with other rare malignancies, there are data to suggest that patients with GTN who are treated in centers of excellence with higher patient volumes have better outcomes than do similar patients treated in a community setting, he said in an interview.
Placental origins
GTNs arise from placental rather than maternal tissue. They most commonly present with vaginal bleeding and a rapidly enlarging uterus, and may be accompanied by pelvic pain or pressure, anemia, severe nausea/vomiting (hyperemesis gravidarum), hyperthyroidism, or early-pregnancy preeclampsia.
The overall reported incidence of GTN in the United States, including hydatidiform mole, is approximately 110 to 120 per 100,000 pregnancies, and the reported incidence of choriocarcinoma is about 2 to 7 per 100,000, according to the National Cancer Institute.
The GTN guidelines provide evidence-based recommendations about optimal approaches to GTN in all of its known forms. For example, the section on noninvasive hydatidiform mole recommends the tests that should be routinely performed during workup, followed by surgery with either suction, dilation and curettage – preferably under ultrasound guidance – or hysterectomy for women who are older or who do not wish to preserve fertility.
The guidelines also specify steps that should be taken for diagnosis and staging of GTN as well as risk-based therapeutic approaches.
For example, the guidelines recommend therapy with either methotrexate alone or alternating with leucovorin, or dactinomycin alone for patients with confirmed low risk GTN, defined as a prognostic score less than 7.
The prognostic scoring index, also included in the guidelines, considers risk factors such as age, prior pregnancies, interval from an index pregnancy, pretreatment human chorionic gonadotropin (hCG) levels, site and number of metastases, largest tumor size, and previous chemotherapy failure.
For patients with high-risk GTN, defined as FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stages II-III with a prognostic score of 7 or greater, or FIGO stage IV, chemotherapy with the EMA/CO regimen is recommended. This aggressive regimen consists of etoposide, methotrexate, dactinomycin (the “EMA “component) plus cyclophosphamide and vincristine (the “CO” component).
“In my mind, the most important part of the guidelines is reiterating how the diagnosis of GTN should be made, and importantly, how the score should be calculated so that women are put in the appropriate low-risk or high-risk category, so they get the right treatment,” Dr. Horowitz said.
Reassuring insurers
Dr. Mutch said that he and his colleagues in GTN centers sometimes treat patients with intermediate or high-risk disease who were started on single-agent therapy or suboptimal therapies and present with advanced, drug-resistant disease.
“These guidelines were established so that people could see exactly what needs to be done when,” he said.
The guidelines also are critical for convincing third-party payers about the need for specific treatments, he added.
“I had a high-risk patient who needed EMA/CO, and the insurance company said ‘well, there’s no NCCN guidelines – we won’t approve it.’ So then I had to wait 3 days while it went through peer review. Meanwhile, the tumor doubled in size, and then the nurse who was reviewing it declined the ‘CO’ part, so that was delayed a week, and it really jeopardized this patient’s survival,” Dr. Mutch said.
The guidelines also include recommendations for patients with special clinical situations, such as women with clinical responses to EMA/CO who continue to have plateauing low levels of hCG or have a re-elevation of hCG levels after having a complete response to EMA/CO.
There are also specific recommendations for treatment of two even rarer intermediate trophoblastic tumor types: placental-site trophoblastic tumor and epithelioid trophoblastic tumor.
The guidelines are supported by the NCCN. Dr. Mutch reported consulting/advisory board participation for Clovis. Dr. Horowitz reported having no relationships to disclose.
SOURCE: Gestational Trophoblastic Neoplasia. NCCN.org, Version 1.2019, published Aug. 9, 2018.
The National Comprehensive Cancer Network (NCCN) has issued its first-ever clinical practice guidelines for the treatment of gestational trophoblastic neoplasia (GTN), a rare, serious complication of pregnancy that can often be cured, but can have devastating consequences if mismanaged or if treatment is needlessly delayed.
David Mutch, MD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, who heads the NCCN Clinical Practice Guidelines in Oncology Committee for GTN, explained the critical importance of the GTN guidelines.
“It’s a rare disease, people weren’t that familiar with it, and they often are patients treated with single-agent therapy when they should be treated with multi-agent therapy,” he said in an interview.
“There wasn’t a clear understanding of what to do except by those people who treated these patients regularly. The only thing most people knew was that it was very chemosensitive and should be curable, but it’s only curable if you follow the appropriate algorithms,” he continued.
The algorithms he referred to were established by a handful of centers with expertise and experience in diagnosing and treating these rare conditions, including noninvasive hydatidiform mole, invasive mole, and choriocarcinoma, the most aggressive form of GTN.
Neil Horowitz, MD, director of clinical research in gynecologic oncology at the Dana-Farber Cancer Institute in Boston, works with colleagues in one of those referral centers, the New England Trophoblastic Disease Center, and is familiar with the new guidelines. As with other rare malignancies, there are data to suggest that patients with GTN who are treated in centers of excellence with higher patient volumes have better outcomes than do similar patients treated in a community setting, he said in an interview.
Placental origins
GTNs arise from placental rather than maternal tissue. They most commonly present with vaginal bleeding and a rapidly enlarging uterus, and may be accompanied by pelvic pain or pressure, anemia, severe nausea/vomiting (hyperemesis gravidarum), hyperthyroidism, or early-pregnancy preeclampsia.
The overall reported incidence of GTN in the United States, including hydatidiform mole, is approximately 110 to 120 per 100,000 pregnancies, and the reported incidence of choriocarcinoma is about 2 to 7 per 100,000, according to the National Cancer Institute.
The GTN guidelines provide evidence-based recommendations about optimal approaches to GTN in all of its known forms. For example, the section on noninvasive hydatidiform mole recommends the tests that should be routinely performed during workup, followed by surgery with either suction, dilation and curettage – preferably under ultrasound guidance – or hysterectomy for women who are older or who do not wish to preserve fertility.
The guidelines also specify steps that should be taken for diagnosis and staging of GTN as well as risk-based therapeutic approaches.
For example, the guidelines recommend therapy with either methotrexate alone or alternating with leucovorin, or dactinomycin alone for patients with confirmed low risk GTN, defined as a prognostic score less than 7.
The prognostic scoring index, also included in the guidelines, considers risk factors such as age, prior pregnancies, interval from an index pregnancy, pretreatment human chorionic gonadotropin (hCG) levels, site and number of metastases, largest tumor size, and previous chemotherapy failure.
For patients with high-risk GTN, defined as FIGO (Fédération Internationale de Gynécologie et d’Obstétrique) stages II-III with a prognostic score of 7 or greater, or FIGO stage IV, chemotherapy with the EMA/CO regimen is recommended. This aggressive regimen consists of etoposide, methotrexate, dactinomycin (the “EMA “component) plus cyclophosphamide and vincristine (the “CO” component).
“In my mind, the most important part of the guidelines is reiterating how the diagnosis of GTN should be made, and importantly, how the score should be calculated so that women are put in the appropriate low-risk or high-risk category, so they get the right treatment,” Dr. Horowitz said.
Reassuring insurers
Dr. Mutch said that he and his colleagues in GTN centers sometimes treat patients with intermediate or high-risk disease who were started on single-agent therapy or suboptimal therapies and present with advanced, drug-resistant disease.
“These guidelines were established so that people could see exactly what needs to be done when,” he said.
The guidelines also are critical for convincing third-party payers about the need for specific treatments, he added.
“I had a high-risk patient who needed EMA/CO, and the insurance company said ‘well, there’s no NCCN guidelines – we won’t approve it.’ So then I had to wait 3 days while it went through peer review. Meanwhile, the tumor doubled in size, and then the nurse who was reviewing it declined the ‘CO’ part, so that was delayed a week, and it really jeopardized this patient’s survival,” Dr. Mutch said.
The guidelines also include recommendations for patients with special clinical situations, such as women with clinical responses to EMA/CO who continue to have plateauing low levels of hCG or have a re-elevation of hCG levels after having a complete response to EMA/CO.
There are also specific recommendations for treatment of two even rarer intermediate trophoblastic tumor types: placental-site trophoblastic tumor and epithelioid trophoblastic tumor.
The guidelines are supported by the NCCN. Dr. Mutch reported consulting/advisory board participation for Clovis. Dr. Horowitz reported having no relationships to disclose.
SOURCE: Gestational Trophoblastic Neoplasia. NCCN.org, Version 1.2019, published Aug. 9, 2018.
Key clinical point: Gestational trophoblastic neoplasia (GTN) is a complication of pregnancy involving rare placental derived tumors that are generally curable with appropriate therapy, best delivered at a center of excellence.
Major finding: National Comprehensive Cancer Network Guidelines specify risk-based therapy for GTN based on staging and prognostic indicators.
Study details: Evidence-based guidelines issued by the National Comprehensive Cancer Network.
Disclosures: The guidelines are supported by the NCCN. Dr. Mutch reported consulting/advisory board participation for Clovis. Dr. Horowitz reported having no disclosures to report.
Source: Gestational Trophoblastic Neoplasia. NCCN.org, Version 1.2019, published Aug. 9, 2018.
VEGF inhibitor shows promise in platinum resistant/refractory ovarian cancer
Combining the vascular endothelial growth factor (VEGF) receptor–targeting tyrosine kinase inhibitor apatinib with oral etoposide in people with platinum resistant or refractory ovarian cancer has shown promising efficacy and manageable toxicity in a Phase 2 study.
Angiogenesis was a “hallmark” process in cancer, and antiangiogenic therapy, including anti-VEGF antibodies and multireceptor tyrosine kinase inhibitors, has been shown to be an attractive therapeutic strategy for ovarian cancer.
“Increasing evidence suggests that the combination of antiangiogenic therapy and single-agent chemotherapy improves the outcome of platinum-resistant ovarian cancer,” Chun-Yan Lan, MD, of the Collaborative Innovation Center for Cancer Medicine at Sun Yat-sen University Cancer Center in Guangzhou, China, and colleagues wrote in Lancet Oncology.
The investigators chose apatinib because it has shown encouraging antitumor activities and tolerable toxicities in several malignant tumors and was available in mainland China, they said.
The single-arm prospective study enrolled 35 women aged 18-70 years with heavily pretreated ovarian cancer that was refractory to platinum (defined as progression during the initial platinum-based treatment) or resistant to platinum (defined as progression within 6 months after the last platinum treatment).
Women were treated with apatinib at an initial dose of 500 mg once daily on a continuous basis and with oral etoposide at a dose of 50 mg once daily on days 1-14 of a 21-day cycle. Oral etoposide was administered for a maximum of six cycles. Dose modifications, including dose interruptions, were allowed in order to manage adverse events.
Treatment was continued until disease progression, patient withdrawal, or unacceptable toxic effects. The primary endpoint of the study was the proportion of patients achieving an objective response according to Response Evaluation Criteria in Solid Tumors (RECIST). The study authors analyzed efficacy data using three populations: intention-to-treat, per-protocol, and safety populations.
Results showed that 19 of 35 patients achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%) in an intention-to-treat analysis. In the per-protocol population, 19 of 31 patients (61%; 95% CI, 42.2%-78.2%) achieved an objective response.
Median progression-free survival was 8.1 months (interquartile range, 4.3-14.6; 95% CI, 2.8-13.4), and the median duration of response was 7.4 months (IQR, 4.0-13.0; 95% CI, 2.3-12.0).
The most common grade 3 or 4 adverse events reported were neutropenia (n = 17), fatigue (n = 11), anemia n = 10), and mucositis (n = 8). Serious adverse events were reported in two patients who were admitted to the hospital.
Dose reductions were required in 82% (n = 28) of 34 patients on apatinib and 77% (n = 26) for etoposide. The authors said they would suggest future studies use a lower starting dose of apatinib and give etoposide for 10 days rather than 14.
“Our study showed that the combination therapy of apatinib with oral etoposide shows promising efficacy and manageable toxicities in patients with platinum-resistant or platinum-refractory recurrent ovarian cancer and further study in phase 3 trials is warranted,” the study authors concluded.
They said that a strength of their study was that both apatinib and oral etoposide were able to be given orally without the need for hospital admission or an infusion pump, factors that could improve adherence and cost effectiveness for patients.
However, they noted that one limitation was that it was a single-arm study with no control group, which meant the selection bias could not be ruled out.
Source: Lan CY et al. Lancet Oncol. 2018 Aug 3. doi: 10.1016/ S1470-2045(18)30349-8.
In the study by Chun-Yan Lan and colleagues, an “impressive” number of patients in the intention to treat analysis achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%). Given that the response to standard cytotoxic therapies in ovarian cancer is reported to be between 0-30%, the combination of apatinib with etoposide should be studied further.
The median progression-free survival of 8.1 months indicates the responses observed are durable, particularly against the backdrop of survival rates seen in other studies, such as 6.7 months in AURELIA and 6.4 months in MITO 11. However, the dangers of comparing results across trials when patient populations are different should be acknowledged.
The levels of neutropenia and anemia and fatigue seen in study participants is acceptable, but the grade 3 or 4 mucositis in 8 of 34 patients is of concern given the need for patients to take oral medications long term.
It is noteworthy that the number of patients requiring a dose reduction of apatinib was high – at 82% of patients, with 76% needing a dose reduction of etoposide. Although the authors do suggest that future studies should use a lower starting dose. Further studies should also include patient reported outcomes in order to ensure that the convenience of this combination of apatinib with etoposide is not at the expense of toxicity.
These comments were excerpted from an accompanying commentary (Lancet Oncol. 2018 Aug 3. doi: 10.1016/S1470-2045[18]30444-3) by Charlie Gourley, MD, of University of Edinburgh, U.K.
In the study by Chun-Yan Lan and colleagues, an “impressive” number of patients in the intention to treat analysis achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%). Given that the response to standard cytotoxic therapies in ovarian cancer is reported to be between 0-30%, the combination of apatinib with etoposide should be studied further.
The median progression-free survival of 8.1 months indicates the responses observed are durable, particularly against the backdrop of survival rates seen in other studies, such as 6.7 months in AURELIA and 6.4 months in MITO 11. However, the dangers of comparing results across trials when patient populations are different should be acknowledged.
The levels of neutropenia and anemia and fatigue seen in study participants is acceptable, but the grade 3 or 4 mucositis in 8 of 34 patients is of concern given the need for patients to take oral medications long term.
It is noteworthy that the number of patients requiring a dose reduction of apatinib was high – at 82% of patients, with 76% needing a dose reduction of etoposide. Although the authors do suggest that future studies should use a lower starting dose. Further studies should also include patient reported outcomes in order to ensure that the convenience of this combination of apatinib with etoposide is not at the expense of toxicity.
These comments were excerpted from an accompanying commentary (Lancet Oncol. 2018 Aug 3. doi: 10.1016/S1470-2045[18]30444-3) by Charlie Gourley, MD, of University of Edinburgh, U.K.
In the study by Chun-Yan Lan and colleagues, an “impressive” number of patients in the intention to treat analysis achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%). Given that the response to standard cytotoxic therapies in ovarian cancer is reported to be between 0-30%, the combination of apatinib with etoposide should be studied further.
The median progression-free survival of 8.1 months indicates the responses observed are durable, particularly against the backdrop of survival rates seen in other studies, such as 6.7 months in AURELIA and 6.4 months in MITO 11. However, the dangers of comparing results across trials when patient populations are different should be acknowledged.
The levels of neutropenia and anemia and fatigue seen in study participants is acceptable, but the grade 3 or 4 mucositis in 8 of 34 patients is of concern given the need for patients to take oral medications long term.
It is noteworthy that the number of patients requiring a dose reduction of apatinib was high – at 82% of patients, with 76% needing a dose reduction of etoposide. Although the authors do suggest that future studies should use a lower starting dose. Further studies should also include patient reported outcomes in order to ensure that the convenience of this combination of apatinib with etoposide is not at the expense of toxicity.
These comments were excerpted from an accompanying commentary (Lancet Oncol. 2018 Aug 3. doi: 10.1016/S1470-2045[18]30444-3) by Charlie Gourley, MD, of University of Edinburgh, U.K.
Combining the vascular endothelial growth factor (VEGF) receptor–targeting tyrosine kinase inhibitor apatinib with oral etoposide in people with platinum resistant or refractory ovarian cancer has shown promising efficacy and manageable toxicity in a Phase 2 study.
Angiogenesis was a “hallmark” process in cancer, and antiangiogenic therapy, including anti-VEGF antibodies and multireceptor tyrosine kinase inhibitors, has been shown to be an attractive therapeutic strategy for ovarian cancer.
“Increasing evidence suggests that the combination of antiangiogenic therapy and single-agent chemotherapy improves the outcome of platinum-resistant ovarian cancer,” Chun-Yan Lan, MD, of the Collaborative Innovation Center for Cancer Medicine at Sun Yat-sen University Cancer Center in Guangzhou, China, and colleagues wrote in Lancet Oncology.
The investigators chose apatinib because it has shown encouraging antitumor activities and tolerable toxicities in several malignant tumors and was available in mainland China, they said.
The single-arm prospective study enrolled 35 women aged 18-70 years with heavily pretreated ovarian cancer that was refractory to platinum (defined as progression during the initial platinum-based treatment) or resistant to platinum (defined as progression within 6 months after the last platinum treatment).
Women were treated with apatinib at an initial dose of 500 mg once daily on a continuous basis and with oral etoposide at a dose of 50 mg once daily on days 1-14 of a 21-day cycle. Oral etoposide was administered for a maximum of six cycles. Dose modifications, including dose interruptions, were allowed in order to manage adverse events.
Treatment was continued until disease progression, patient withdrawal, or unacceptable toxic effects. The primary endpoint of the study was the proportion of patients achieving an objective response according to Response Evaluation Criteria in Solid Tumors (RECIST). The study authors analyzed efficacy data using three populations: intention-to-treat, per-protocol, and safety populations.
Results showed that 19 of 35 patients achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%) in an intention-to-treat analysis. In the per-protocol population, 19 of 31 patients (61%; 95% CI, 42.2%-78.2%) achieved an objective response.
Median progression-free survival was 8.1 months (interquartile range, 4.3-14.6; 95% CI, 2.8-13.4), and the median duration of response was 7.4 months (IQR, 4.0-13.0; 95% CI, 2.3-12.0).
The most common grade 3 or 4 adverse events reported were neutropenia (n = 17), fatigue (n = 11), anemia n = 10), and mucositis (n = 8). Serious adverse events were reported in two patients who were admitted to the hospital.
Dose reductions were required in 82% (n = 28) of 34 patients on apatinib and 77% (n = 26) for etoposide. The authors said they would suggest future studies use a lower starting dose of apatinib and give etoposide for 10 days rather than 14.
“Our study showed that the combination therapy of apatinib with oral etoposide shows promising efficacy and manageable toxicities in patients with platinum-resistant or platinum-refractory recurrent ovarian cancer and further study in phase 3 trials is warranted,” the study authors concluded.
They said that a strength of their study was that both apatinib and oral etoposide were able to be given orally without the need for hospital admission or an infusion pump, factors that could improve adherence and cost effectiveness for patients.
However, they noted that one limitation was that it was a single-arm study with no control group, which meant the selection bias could not be ruled out.
Source: Lan CY et al. Lancet Oncol. 2018 Aug 3. doi: 10.1016/ S1470-2045(18)30349-8.
Combining the vascular endothelial growth factor (VEGF) receptor–targeting tyrosine kinase inhibitor apatinib with oral etoposide in people with platinum resistant or refractory ovarian cancer has shown promising efficacy and manageable toxicity in a Phase 2 study.
Angiogenesis was a “hallmark” process in cancer, and antiangiogenic therapy, including anti-VEGF antibodies and multireceptor tyrosine kinase inhibitors, has been shown to be an attractive therapeutic strategy for ovarian cancer.
“Increasing evidence suggests that the combination of antiangiogenic therapy and single-agent chemotherapy improves the outcome of platinum-resistant ovarian cancer,” Chun-Yan Lan, MD, of the Collaborative Innovation Center for Cancer Medicine at Sun Yat-sen University Cancer Center in Guangzhou, China, and colleagues wrote in Lancet Oncology.
The investigators chose apatinib because it has shown encouraging antitumor activities and tolerable toxicities in several malignant tumors and was available in mainland China, they said.
The single-arm prospective study enrolled 35 women aged 18-70 years with heavily pretreated ovarian cancer that was refractory to platinum (defined as progression during the initial platinum-based treatment) or resistant to platinum (defined as progression within 6 months after the last platinum treatment).
Women were treated with apatinib at an initial dose of 500 mg once daily on a continuous basis and with oral etoposide at a dose of 50 mg once daily on days 1-14 of a 21-day cycle. Oral etoposide was administered for a maximum of six cycles. Dose modifications, including dose interruptions, were allowed in order to manage adverse events.
Treatment was continued until disease progression, patient withdrawal, or unacceptable toxic effects. The primary endpoint of the study was the proportion of patients achieving an objective response according to Response Evaluation Criteria in Solid Tumors (RECIST). The study authors analyzed efficacy data using three populations: intention-to-treat, per-protocol, and safety populations.
Results showed that 19 of 35 patients achieved an objective response (54%; 95% confidence interval, 36.6%-71.2%) in an intention-to-treat analysis. In the per-protocol population, 19 of 31 patients (61%; 95% CI, 42.2%-78.2%) achieved an objective response.
Median progression-free survival was 8.1 months (interquartile range, 4.3-14.6; 95% CI, 2.8-13.4), and the median duration of response was 7.4 months (IQR, 4.0-13.0; 95% CI, 2.3-12.0).
The most common grade 3 or 4 adverse events reported were neutropenia (n = 17), fatigue (n = 11), anemia n = 10), and mucositis (n = 8). Serious adverse events were reported in two patients who were admitted to the hospital.
Dose reductions were required in 82% (n = 28) of 34 patients on apatinib and 77% (n = 26) for etoposide. The authors said they would suggest future studies use a lower starting dose of apatinib and give etoposide for 10 days rather than 14.
“Our study showed that the combination therapy of apatinib with oral etoposide shows promising efficacy and manageable toxicities in patients with platinum-resistant or platinum-refractory recurrent ovarian cancer and further study in phase 3 trials is warranted,” the study authors concluded.
They said that a strength of their study was that both apatinib and oral etoposide were able to be given orally without the need for hospital admission or an infusion pump, factors that could improve adherence and cost effectiveness for patients.
However, they noted that one limitation was that it was a single-arm study with no control group, which meant the selection bias could not be ruled out.
Source: Lan CY et al. Lancet Oncol. 2018 Aug 3. doi: 10.1016/ S1470-2045(18)30349-8.
FROM LANCET ONCOLOGY
Key clinical point: The VEGF receptor tyrosine kinase inhibitor apatinib in combination with oral etoposide in people with platinum resistant or refractory ovarian cancer has shown promising efficacy and manageable toxicity.
Major finding: Nineteen of 35 patients with heavily pretreated ovarian cancer refractory or resistant to platinum achieved an objective response (54%; 95% CI 36.6-71.2) in an intention-to-treat analysis.
Study details: A single arm prospective phase 2 study of 35 women aged 18-70 years with heavily pretreated platinum resistant or refractory ovarian cancer.
Disclosures: Jiangsu Hengrui Pharmaceuticals discounted apatinib to patients enrolled in the study.
Source: Lan CY et al. Lancet Oncol. 2018 Aug 3. doi: 10.1016/ S1470-2045(18)30349-8.
Phase 2 trial: Dendritic cell vaccine maintenance prolongs PFS in EOC
CHICAGO – who have undergone primary debulking surgery, according to interim findings from a randomized, phase 2, open-label trial.
Of 99 patients enrolled in the international, multicenter trial between November 2013 and March 2016, 92 received at least one dose of therapy and had a postbaseline endpoint assessment (the modified intention-to-treat population). Median progression-free survival was 18.3 months in the 31 patients who received autologous dendritic cell vaccine (DCVAC) given concomitantly with chemotherapy (group A), 24.3 months in the 30 patients who received DCVAC given sequentially as maintenance therapy after chemotherapy (group B), and 18.6 months in the 31 controls who received chemotherapy alone (group C), Lukas Rob, MD, reported at the annual meeting of the American Society of Clinical Oncology.
“When DCVAC was administered as maintenance [therapy] after the chemotherapy, the time to disease progression was prolonged by almost 6 months. Based on the hazard ratio, there was a 57% decrease in the hazard of progression in favor of arm B,” said Dr. Rob, of University Hospital Kralovske Vinohrady, Prague.
Compared with group C, progression-free survival hazard ratios were 0.64 and 0.43 in the modified intention-to-treat population in groups A and B, respectively, he said.
“These results are statistically significant and the clinical benefit is even more significant in patients who received more doses of DCVAC,” he added, explaining that the hazard ratios for patients in groups A and B who received at least eight doses of DCVAC and/or three cycles of chemotherapy (the per protocol population, including 87 patients) were 1.01 and 0.32, respectively.
Although the overall survival data in this study is immature, there is “a strong trend in favor of DCVAC in the maintenance treatment arm,” he said.
Study participants had FIGO stage III epithelial ovarian cancer (EOC) and a performance status score of 0-2. All had undergone primary debulking surgery and had less than 1 cm maximal residuum and no prior systemic therapy. Patients were randomized up to 6 weeks after surgery. Chemotherapy in all three groups included six cycles of carboplatin and paclitaxel, and DCVAC was given at doses of 1 x 107 dendritic cells per dose for a planned 10 doses.
Most patients with EOC – about 70% of those with stage III/IV disease – relapse after optimal debulking surgery and chemotherapy.
“There is no doubt that we need a new treatment modality,” he said. Because autologous DCVAC can present tumor antigens to elicit a durable immune response, he and his colleagues hypothesized that adding DCVAC to chemotherapy could improve outcomes – either when used concomitantly to target tumor-induced immune suppression and allowing for partial recovery of the immune system after each cycle, or when used sequentially as maintenance therapy, as minimal tumor burden after chemotherapy would provide optimal conditions for immune stimulation and the immune system would be fully recovered after completing cytotoxic therapy.
The treatments in this study were well tolerated; no grade 3 or greater adverse events were related solely to DCVAC, and the vaccine did not worsen the side effects of chemotherapy, Dr. Rob said.
The findings suggested that sequential DCVAC after chemotherapy in patients with EOC is a promising maintenance treatment option that can delay disease progression, he concluded, noting that “due to the excellent result in the maintenance arm we decided ... to enroll more patients in arms B and C to increase the power of this study.”
Additionally, a phase 3 trial is planned and enrollment should begin in early 2019, he said.
Dr. Rob reported having no disclosures.
SOURCE: Rob L et al. ASCO 2018, Abstract 5509.
CHICAGO – who have undergone primary debulking surgery, according to interim findings from a randomized, phase 2, open-label trial.
Of 99 patients enrolled in the international, multicenter trial between November 2013 and March 2016, 92 received at least one dose of therapy and had a postbaseline endpoint assessment (the modified intention-to-treat population). Median progression-free survival was 18.3 months in the 31 patients who received autologous dendritic cell vaccine (DCVAC) given concomitantly with chemotherapy (group A), 24.3 months in the 30 patients who received DCVAC given sequentially as maintenance therapy after chemotherapy (group B), and 18.6 months in the 31 controls who received chemotherapy alone (group C), Lukas Rob, MD, reported at the annual meeting of the American Society of Clinical Oncology.
“When DCVAC was administered as maintenance [therapy] after the chemotherapy, the time to disease progression was prolonged by almost 6 months. Based on the hazard ratio, there was a 57% decrease in the hazard of progression in favor of arm B,” said Dr. Rob, of University Hospital Kralovske Vinohrady, Prague.
Compared with group C, progression-free survival hazard ratios were 0.64 and 0.43 in the modified intention-to-treat population in groups A and B, respectively, he said.
“These results are statistically significant and the clinical benefit is even more significant in patients who received more doses of DCVAC,” he added, explaining that the hazard ratios for patients in groups A and B who received at least eight doses of DCVAC and/or three cycles of chemotherapy (the per protocol population, including 87 patients) were 1.01 and 0.32, respectively.
Although the overall survival data in this study is immature, there is “a strong trend in favor of DCVAC in the maintenance treatment arm,” he said.
Study participants had FIGO stage III epithelial ovarian cancer (EOC) and a performance status score of 0-2. All had undergone primary debulking surgery and had less than 1 cm maximal residuum and no prior systemic therapy. Patients were randomized up to 6 weeks after surgery. Chemotherapy in all three groups included six cycles of carboplatin and paclitaxel, and DCVAC was given at doses of 1 x 107 dendritic cells per dose for a planned 10 doses.
Most patients with EOC – about 70% of those with stage III/IV disease – relapse after optimal debulking surgery and chemotherapy.
“There is no doubt that we need a new treatment modality,” he said. Because autologous DCVAC can present tumor antigens to elicit a durable immune response, he and his colleagues hypothesized that adding DCVAC to chemotherapy could improve outcomes – either when used concomitantly to target tumor-induced immune suppression and allowing for partial recovery of the immune system after each cycle, or when used sequentially as maintenance therapy, as minimal tumor burden after chemotherapy would provide optimal conditions for immune stimulation and the immune system would be fully recovered after completing cytotoxic therapy.
The treatments in this study were well tolerated; no grade 3 or greater adverse events were related solely to DCVAC, and the vaccine did not worsen the side effects of chemotherapy, Dr. Rob said.
The findings suggested that sequential DCVAC after chemotherapy in patients with EOC is a promising maintenance treatment option that can delay disease progression, he concluded, noting that “due to the excellent result in the maintenance arm we decided ... to enroll more patients in arms B and C to increase the power of this study.”
Additionally, a phase 3 trial is planned and enrollment should begin in early 2019, he said.
Dr. Rob reported having no disclosures.
SOURCE: Rob L et al. ASCO 2018, Abstract 5509.
CHICAGO – who have undergone primary debulking surgery, according to interim findings from a randomized, phase 2, open-label trial.
Of 99 patients enrolled in the international, multicenter trial between November 2013 and March 2016, 92 received at least one dose of therapy and had a postbaseline endpoint assessment (the modified intention-to-treat population). Median progression-free survival was 18.3 months in the 31 patients who received autologous dendritic cell vaccine (DCVAC) given concomitantly with chemotherapy (group A), 24.3 months in the 30 patients who received DCVAC given sequentially as maintenance therapy after chemotherapy (group B), and 18.6 months in the 31 controls who received chemotherapy alone (group C), Lukas Rob, MD, reported at the annual meeting of the American Society of Clinical Oncology.
“When DCVAC was administered as maintenance [therapy] after the chemotherapy, the time to disease progression was prolonged by almost 6 months. Based on the hazard ratio, there was a 57% decrease in the hazard of progression in favor of arm B,” said Dr. Rob, of University Hospital Kralovske Vinohrady, Prague.
Compared with group C, progression-free survival hazard ratios were 0.64 and 0.43 in the modified intention-to-treat population in groups A and B, respectively, he said.
“These results are statistically significant and the clinical benefit is even more significant in patients who received more doses of DCVAC,” he added, explaining that the hazard ratios for patients in groups A and B who received at least eight doses of DCVAC and/or three cycles of chemotherapy (the per protocol population, including 87 patients) were 1.01 and 0.32, respectively.
Although the overall survival data in this study is immature, there is “a strong trend in favor of DCVAC in the maintenance treatment arm,” he said.
Study participants had FIGO stage III epithelial ovarian cancer (EOC) and a performance status score of 0-2. All had undergone primary debulking surgery and had less than 1 cm maximal residuum and no prior systemic therapy. Patients were randomized up to 6 weeks after surgery. Chemotherapy in all three groups included six cycles of carboplatin and paclitaxel, and DCVAC was given at doses of 1 x 107 dendritic cells per dose for a planned 10 doses.
Most patients with EOC – about 70% of those with stage III/IV disease – relapse after optimal debulking surgery and chemotherapy.
“There is no doubt that we need a new treatment modality,” he said. Because autologous DCVAC can present tumor antigens to elicit a durable immune response, he and his colleagues hypothesized that adding DCVAC to chemotherapy could improve outcomes – either when used concomitantly to target tumor-induced immune suppression and allowing for partial recovery of the immune system after each cycle, or when used sequentially as maintenance therapy, as minimal tumor burden after chemotherapy would provide optimal conditions for immune stimulation and the immune system would be fully recovered after completing cytotoxic therapy.
The treatments in this study were well tolerated; no grade 3 or greater adverse events were related solely to DCVAC, and the vaccine did not worsen the side effects of chemotherapy, Dr. Rob said.
The findings suggested that sequential DCVAC after chemotherapy in patients with EOC is a promising maintenance treatment option that can delay disease progression, he concluded, noting that “due to the excellent result in the maintenance arm we decided ... to enroll more patients in arms B and C to increase the power of this study.”
Additionally, a phase 3 trial is planned and enrollment should begin in early 2019, he said.
Dr. Rob reported having no disclosures.
SOURCE: Rob L et al. ASCO 2018, Abstract 5509.
REPORTING FROM ASCO 2018
Key clinical point: Dendritic cell vaccine maintenance improves progression-free survival in patients with epithelial ovarian carcinoma who have undergone primary debulking surgery.
Major finding: DCVAC maintenance after chemotherapy prolonged progression-free survival by almost 6 months (hazard ratio, 0.43 vs. chemotherapy alone).
Study details: A randomized, phase 2, open-label trial including 99 patients.
Disclosures: Dr. Rob reported having no disclosures.
Source: Rob L et al. ASCO 2018, Abstract 5509.




