User login
VA cohort study: Individualize SSI prophylaxis based on patient factors
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
The combined use of vancomycin and a beta-lactam antibiotic for prophylaxis against surgical site infections is associated with both benefits and harms, according to findings from a national propensity-score–adjusted retrospective cohort study.
For example, the combination treatment reduced surgical site infections (SSIs) 30 days after cardiac surgical procedures but increased the risk of postoperative acute kidney injury (AKI) in some patients, Westyn Branch-Elliman, MD, of the VA Boston Healthcare System and her colleagues reported online July 10 in PLOS Medicine.
Among cardiac surgery patients, the incidence of surgical site infections was significantly lower for the 6,953 patients treated with both drugs vs. the 12,834 treated with a single agent (0.95% vs. 1.48%), the investigators found (PLOS Med. 2017 Jul 10. doi: 10.1371/journal.pmed.1002340).
SSI benefit with combination therapy
“After controlling for age, diabetes, ASA [American Society of Anesthesiologists] score, mupirocin administration, current smoking status, and preoperative MRSA [methicillin-resistant Staphylococcus aureus] colonization status, receipt of combination antimicrobial prophylaxis was associated with reduced SSI risk following cardiac surgical procedures (adjusted risk ratio, 0.61),” they wrote, noting that, when combination therapy was compared with either of the agents alone, the associations were similar and that no association between SSI reduction and the combination regimen was seen for the other types of surgical procedures assessed.
Secondary analyses showed that, among the cardiac patients, differences in the rates of SSIs were seen based on MRSA status in patients undergoing cardiac surgery. Among MRSA-colonized patients, SSIs occurred in 8 of 346 patients (2.3%) who received combination prophylaxis vs. 4 of 100 patients (4%) who received vancomycin alone (aRR, 0.53), and, among MRSA-negative and MRSA-unknown cardiac surgery patients, SSIs occurred in 58 of 6,607 patients (0.88%) receiving combination prophylaxis and 146 of 10,215 patients (1.4%) receiving a beta-lactam alone (aRR, 0.60).
“Among MRSA-colonized patients undergoing cardiac surgery, the associated absolute risk reduction for SSI was approximately triple that of the absolute risk reduction in MRSA-negative or -unknown patients, with a [number needed to treat] to prevent 1 SSI of 53 for the MRSA-colonized group, compared with 176 for the MRSA-negative or -unknown groups,” they wrote.
The incidence of Clostridium difficile infection was similar in both exposure groups (0.72% and 0.81% with combination and single agent prophylaxis, respectively).
Higher AKI risk with combination therapy
“In contrast, combination versus single prophylaxis was associated with higher relative risk of AKI in the 7-day postoperative period after adjusting for prophylaxis regimen duration, age, diabetes, ASA score, and smoking,” they said.
The rate of AKI was 23.75% among patients receiving combination prophylaxis, compared with 20.79% and 13.93% among those receiving vancomycin alone and a beta-lactam alone, respectively.
Significant associations between absolute risk of AKI and receipt of combination regimens were seen across all types of procedures, the investigators said.
“Overall, the NNH [number needed to harm] to cause one episode of AKI in cardiac surgery patients receiving combination therapy was 22, and, for stage 3 AKI, 167. The NNH associated with one additional episode of any postoperative AKI after receipt of combination therapy was 76 following orthopedic procedures and 25 following vascular surgical procedures,” they said.
The optimal approach for preventing SSIs is unclear. Although the multidisciplinary Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery recommend single agent prophylaxis most often, with a beta-lactam antibiotic, for most surgical procedures, the use of vancomycin alone is a consideration in MRSA-colonized patients and in centers with a high MRSA incidence, and combination prophylaxis with a beta-lactam plus vancomycin is increasing. However, the relative risks and benefit of this strategy have not been carefully studied, the investigators said.
Thus, the investigators used a propensity-adjusted, log-binomial regression model stratified by type of surgical procedure among the cases identified in the Veterans Affairs cohort to assess the association between SSIs and receipt of combination prophylaxis versus single agent prophylaxis.
Though limited by the observational study design and by factors such as a predominantly male and slightly older and more rural population, the findings suggest that “clinicians may need to individualize prophylaxis strategy based on patient-specific factors that influence the risk-versus-benefit equation,” they said, concluding that “future studies are needed to evaluate the utility of MRSA screening protocols for optimizing and individualizing surgical prophylaxis regimen.”
This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated Grant from Merck Pharmaceuticals in 2013.
FROM PLOS MEDICINE
Key clinical point:
Major finding: The SSI incidence was 0.95% vs. 1.48% with combination vs. single agent–therapy in cardiac surgery patients. Acute kidney injuries occurred in 23.75% of all surgery patients receiving combination prophylaxis, compared with 20.79% and 13.93% with vancomycin or a beta-lactam, respectively.
Data source: A retrospective cohort study of more than 70,000 surgical procedures.
Disclosures: This study was funded by Veterans Affairs Health Services Research and Development. Dr. Branch-Elliman reported having no disclosures. One other author, Eli Perencevich, MD, received an investigator initiated grant from Merck Pharmaceuticals in 2013.
Is female genital cosmetic surgery going mainstream?
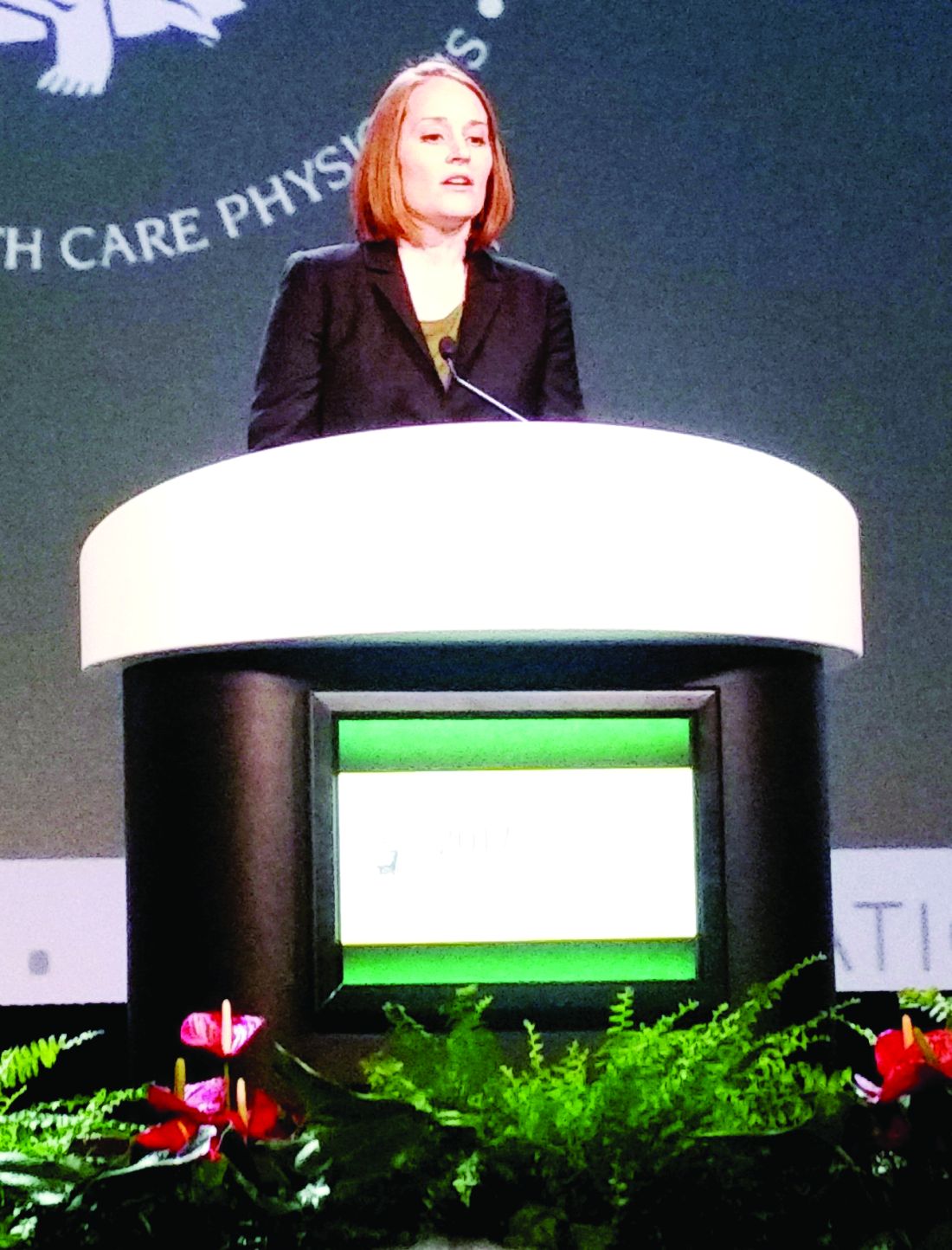
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.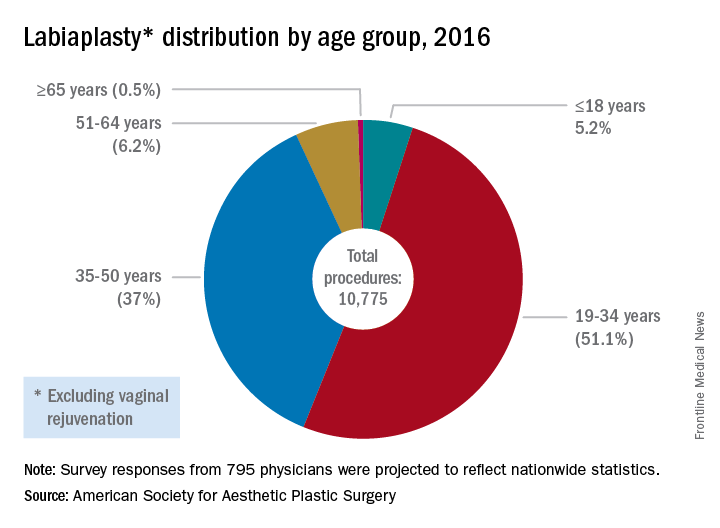
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Experts describe the field of female genital cosmetic surgery as the “Wild West,” but the lack of regulation and consensus has not kept it from exploding in recent years.
More than 10,000 labiaplasties were performed in 2016, a 23% jump over the previous year, and the procedures are offered by more than 35% of all plastic surgeons, according to data from the American Society for Aesthetic Plastic Surgery. As another indicator of increasing attention to the appearance of female genitalia, a 2013 survey of U.S. women revealed that more than 80% performed some sort of pubic hair grooming (JAMA Dermatol. 2016;152[10]:1106-13).
Dr. Iglesia recounted being contacted by a National Gallery of Art staff member, who, when confronted with Gustave Courbet’s L’Origine du Monde, an 1866 below-the-waist portrait of a nude woman, asked, “Is this normal? Do women have this much hair?” Dr. Iglesia said she reassured the staff member that the woman in the portrait did indeed have a normal female Tanner stage IV or V escutcheon. However, she said, social media and other images in the popular press have essentially erased female pubic hair from the public eye, even in explicit imagery that involves female nudity.
“This is an ideal that men and women are seeing in social media, in pornography, and even in the lay press.” And now, she said, “We’re in a new era of sex surgeries, with these ‘nips and tucks’ below the belt.”
Labiaplasty
The combination of a newly-hairless genital region, together with portrayals of adult women with a “Barbie doll” appearance, may contribute to women feeling self-conscious about labia minora protruding beyond the labia majora. Dr. Iglesia, who is section director for female pelvic medicine and reconstructive surgery at MedStar Washington Hospital Center, Washington, D.C., said this is true even though the normal length of labia minora can range from 7 mm to 5 cm.
That’s where labiaplasty comes in. The procedure, which can be performed with conventional surgical techniques or with a laser, is sometimes done for functional reasons.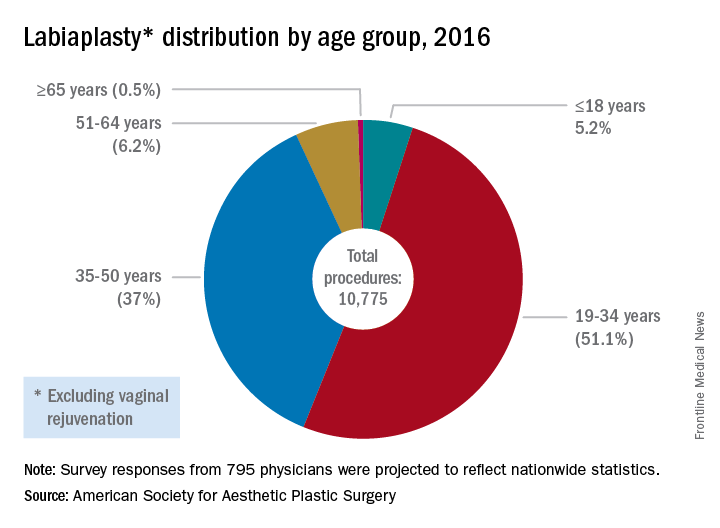
The waters are murkier when labiaplasty is performed for cosmetic reasons, to get that “Barbie doll” look, with some offices advertising the procedure as “designer lips,” Dr. Iglesia said.
In 2007, ACOG issued a committee opinion expressing concern about the lack of data and sometimes deceptive marketing practices surrounding a number of cosmetic vaginal surgeries (Obstet Gynecol 2007;110:737–8). The policy was reaffirmed in 2017.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/is-it-appropriate-to-perform-gynecologic-procedures-such-as-labiaplasty-for-cosmetic-reasons?iframe=1"}]Similarly, the Society of Obstetricians and Gynaecologists of Canada issued a 2013 statement about labiaplasty and other female genital cosmetic surgeries saying that “there is little evidence to support any of the female genital cosmetic surgeries in terms of improvement to sexual satisfaction or self-images. Physicians choosing to proceed with these cosmetic procedures should not promote these surgeries for the enhancement of sexual function and advertising of female genital cosmetic surgical procedures should be avoided.”
However, Mickey Karram, MD, who is director of the urogynecology program at Christ Hospital, Cincinnatti, said that informed consent is the key to dealing appropriately with these procedures.
“If a patient is physically bothered from a cosmetic standpoint that her labia are larger than she thinks they should be, and they are bothering her, is it appropriate or inappropriate to potentially discuss with her a labiaplasty?” Dr. Karram said at the ACOG meeting. For the patient who understands the risk and is also clear that the procedure is not medically necessary, he said he “feels strongly” that labiaplasty should be an option.
Fractional laser
The introduction of the fractional laser to gynecology is also adding to the debate about the appropriate integration of gynecologic procedures that may have nonmedical uses, such as vaginal “tightening.” Used primarily intravaginally, these devices have shallow penetration and are meant to stimulate collagen, proteoglycan, and hyaluronic acid synthesis with minimal tissue damage and downtime. One such device, the MonaLisa Touch, is marketed in the United States by Cynosure.
These energy sources hold great promise for the genitourinary syndrome of menopause (GSM) and other conditions, Dr. Karram said. “Many of these energy sources are being promoted for actual disease states, like vulvovaginal atrophy and lichen sclerosus,” he said.
Dr. Iglesia is not so sure: “This is not the fountain of youth.” She pointed out that the vasculature and innervation of the vagina and vulva are complex, with the outer one-eighth of the vagina being much more highly innervated. Laser treatment with a shallow penetration depth may not get at all of the issues that contribute to GSM.
“Is marketing ahead of the science? I would say yes,” she said. “There’s too much hype about this curing vaginal dryness and making your sex life better.”
Dr. Zahn also urged caution with the use of this technology. “The data are very limited, but, despite this, it’s become a very popular and highly-advertised approach. We need larger studies and more longitudinal data. This is especially true since one of the proposed ways this device works is by stimulating fibrosis. In every other body system, fibrosis stimulation may result in scarring. We have no idea if this is the case with this device. If it is, its application could result in worsening of bodily function, especially in regard to dyspareunia,” he said. “We clearly need more data.”
In 2016, ACOG issued a position statement about the fractional carbon dioxide and yttrium-aluminum-garnet laser systems that had received clearance from the Food and Drug Administration. The statement advised both ob.gyns. and patients that “this technology is, in fact, neither approved nor cleared by the FDA for the specific indication of treating vulvovaginal atrophy.”
Both Dr. Karram and Dr. Iglesia are investigators in an ongoing randomized, placebo- and sham-controlled trial comparing vaginal estrogen and laser therapy used both in conjunction and singly.
‘No-go’ procedures
Though Dr. Karram and Dr. Iglesia disagree on whether cosmetic labiaplasty is appropriate, they were in agreement that certain procedures are so untested, or have such potential risk with no proven benefit, that they should not be performed at all. The procedures on both physicians’ “no-go” lists included clitoral unhooding, G-spot amplification, “revirginification” in any form, vulval recontouring with autologous fat, and the so-called “O-shot,” injections of platelet-rich plasma that are touted as augmenting the sexual experience.
What’s to be done?
There is also agreement that a lack of common terminology is a significant problem. Step one, Dr. Karram said, is doing away with the term vaginal rejuvenation. “This is a terrible term. … There’s no real definition for this term.” He called for a multidisciplinary working group that would bring together gynecologists, plastic surgeons, and dermatologists to begin the work of terminology standardization.
From there, he proposed that the group develop a classification system that clarifies whether procedures are being done for cosmetic reasons, to enhance the sexual experience, or to address a specific disease state. Finally, he said, the group should recommend standardized outcome metrics that can be used to study the various interventions.
Dr. Zahn applauded this notion. “It’s a great point. I agree that multiple disciplines should be involved in examining outcomes, statistics, and criteria for evaluating procedures.”
And gynecologists should be leading this effort, Dr. Karram suggested. “Who knows this anatomy the best? We do.” He added, “If it’s going to be addressed, it should be addressed by us.”
But, Dr. Iglesia said she worries about vulnerable populations, such as adolescents and cancer survivors, who may undergo surgeries, for which the benefits may not outweigh the potential risks. For labiaplasty and laser resurfacing techniques, there have been a small number of studies on outcomes and patient satisfaction that have generally been conducted at single centers with no comparison arms and limited follow-up, she said.
“I also am concerned about pain, scarring, altered sensation, painful sex that could develop, wound complications, and what happens over time,” especially when these procedures may be performed on adolescents or women in their 20s or 30s who may later go on to have children, Dr. Iglesia said.
The question, she said, is not just whether gynecologists are better equipped than plastic surgeons or dermatologists to be performing female genital cosmetic surgery, “but should we be doing this at all?”
Dr. Zahn emphasized the need for evidence to guide decision making. “There has to be data that there is benefit and that the benefit outweighs the potential harm. There is no data on most cosmetic gynecologic procedures. If there are no data, they shouldn’t be done because we would not have the information necessary to appropriately counsel patients,” he said.
Dr. Karram has a financial relationship with Cynosure, which markets the MonaLisa Touch system in the United States. Dr. Iglesia reported that she had no relevant financial disclosures. Dr. Zahn is employed by ACOG.
[email protected]
On Twitter @karioakes
Postcesarean outpatient opioid needs predicted by inpatient use
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
[email protected]
On Twitter @karioakes
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
[email protected]
On Twitter @karioakes
SAN DIEGO – The amount of pain medication a women requires in the hospital after a cesarean delivery was an accurate predictor of postdischarge needs, and could provide guidance to tailor home prescriptions, reducing the amount of unused opioids left after recovery, according to a new study.
Jenna Emerson, MD, and her colleagues also found that more than half of the opioid medications prescribed for home postcesarean use went untaken, and that one in five women used no opioid medication after leaving the hospital.
The prospective cohort study, one of two awarded the Donald F. Richardson Prize at the meeting, looked at how much opioid medication was used by women while they were inpatients, and also asked women to keep track of how much medication they used at home, to see if one could predict the other.
The pilot study enrolled 100 women who had a postdelivery inpatient stay of less than 8 days, who spoke English, and who had given birth to a live viable infant. The study’s statistical analysis looked for relationships not only between inpatient and outpatient use of opioids, but also between patient characteristics and level of opioid use in the hospital and at home.
A total of 76 women completed follow-up, said Dr. Emerson, who is a fourth-year ob.gyn. resident at Brown University, Providence, R.I. One patient was excluded because she was on high opioid doses for addiction treatment before delivery, and her postdelivery opioid requirements represented a clear outlier in the data.
The investigators used medical record data to determine opioid requirements as inpatients after cesarean delivery. For standardization of different strengths of opioids, use was expressed by using Mean Morphine Equivalents (MME). Baseline patient demographic characteristics and comorbidities were also obtained from medical record review.
Patients were asked to track their home opioid use for 2 weeks postdischarge, and also received a follow-up phone call at the end of their first 2 weeks at home.
Inpatient opioid use was divided into tertiles according to low (less than 40 MME), medium (41-70 MME), and high (greater than 70 MME) use. Overall, the group’s mean opioid use in the final 24 hours before discharge was 59 MME, an amount Dr. Emerson said was equivalent to about eight tablets of oxycodone/acetaminophen or 12 tablets of hydrocodone/acetaminophen.
Most patients (89%) went home with a prescription for oxycodone/acetaminophen, and the mean number of pills prescribed per patient was 35. For the original group of 100 patients, this meant that prescriptions were written for 3,150 oxycodone/acetaminophen tablets, 162 hydrocodone/acetaminophen tablets, and 139 oxycodone tablets.
Home use over the first 2 weeks postdischarge was a mean 126 MME, or the equivalent of about 17 oxycodone/acetaminophen tablets. A total of 39% of women reported they had used less than half of their opioid medication; 21% had used all or required more opioids, and 20% had used at least half of their opioids. One in five patients (20%) had not taken a single opioid tablet after discharge from the hospital, and only 2 of the 75 women were still using opioids at the time of the 2-week follow-up call, Dr. Emerson said.
This means there was a total of 1,538 tablets of unused prescription opioid medication left in the homes of the 75 women included in the final analysis, Dr. Emerson said.
When the investigators compared inpatient and outpatient opioid use, they found that 26 women (34.7%) had been in the lowest tertile of inpatient opioid use. These women also had the lowest mean MME at home, using 53 MME in the first 2 weeks post discharge. The middle tertile for inpatient use used a mean 111 MME at home, while the highest used 195 MME (analysis of variance P less than .001).
Higher outpatient opioid use was seen in patients with a history of psychiatric comorbidities (MME 172 vs. 103 for no psychiatric comorbidities; P = .046). Other factors associated with numerically higher use that did not reach statistical significance included breastfeeding status (MME 197 for no breastfeeding, 112 for breastfeeding; P = .068) and insurance status (MME 154 for public, 95 for private; P = .058).
Patients’ mean age was 30.3 years; 63% of participants were Caucasian, 5% were black, and 19% identified their ethnicity as Hispanic. Patients were about evenly divided between having public and private insurance, and most (72%) had some post-high school education. Just 5% had a prior history of drug use or abuse, and about half (49%) were having a repeat cesarean delivery. Three quarters were breastfeeding their infants.
Unused opioid prescriptions are a significant contributor to the pool of opioids available for diversion and recent work has shown that up to 23% of opioids prescribed are used for “nonmedical” purposes, Dr. Emerson said. Since cesarean deliveries are the most commonly performed major surgery in the United States, the opportunity to reduce the number of opioids available for diversion is significant, she said.
“Opioid prescription use after cesarean delivery should be tailored to patient needs,” she said, calling for larger studies to validate and expand on the findings.
Dr. Emerson reported having no outside sources of funding and no relevant financial disclosures.
[email protected]
On Twitter @karioakes
AT ACOG 2017
Key clinical point:
Major finding: Inpatient opioid use by tertile was highly associated with outpatient opioid use by tertile (P less than .001).
Data source: A prospective cohort study of 75 women with cesarean deliveries of live viable infants.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Avoid hysterectomy in POP repairs
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
SAN ANTONIO – The Systematic Review Group of the Society of Gynecologic Surgeons is suggesting uterine preservation, when not contraindicated, for most pelvic organ prolapse repairs to decrease mesh erosion, operating room time, and blood loss.
The advice is based on a review of 94 original studies, including 12 randomized controlled trials (RCTs) and 41 nonrandomized comparative studies, winnowed down to the strongest work from an original review of 7,324 abstracts through January 2017.
Short-term prolapse outcomes – 12-30 months in most of the studies – “are usually not clinically significant due to uterine preservation,” with the one exception of vaginal hysterectomy with native tissue reconstruction, which the group recommended over laparoscopic sacrohysteropexy, Kate Meriwether, MD, a gynecologic surgeon at the University of Louisville, Ky., said at the annual scientific meeting of the Society of Gynecologic Surgeons.
Hysterectomy for prolapse surgery is common: More than 74,000 hysterectomies are done in the United States each year with prolapse as the main indication. Even so, it’s not always necessary to take out the uterus, and perhaps more than a third of women would prefer to keep theirs, Dr. Meriwether said, speaking on behalf of the SGS Systematic Review Group.
The recommendations from the Systematic Review Group must be sent to the SGS board and the full membership before they can be approved as guidelines.*
The Review Group made a grade A recommendation for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, meaning it was based on high-quality evidence. The rest of the advice came in the form of suggestions, based on moderate grade B evidence, often nonrandomized comparative studies and case reviews.
The Review Group suggested uterine preservation during laparoscopic native tissue prolapse repair to reduce operating room (OR) time and blood loss, and preserve vaginal length, based on four nonrandomized comparison studies using various approaches, with a total of 446 women and up to 3 years’ follow-up. There might be a higher risk of apical recurrence without hysterectomy, but without worsening of prolapse symptoms.
The Review Group also suggested uterine preservation in transvaginal mesh reconstruction for prolapse, based on four RCTs and nine comparison studies with 1,381 women and up to 30 months’ follow-up. The studies found a decreased risk of mesh erosion, reoperating for mesh erosion, blood loss, and postop bleeding, and improved posterior and apical Pelvic Organ Prolapse Quantification scores when women keep their uterus.
However, “the patient should be counseled that there may be increased de novo stress incontinence, overactive bladder,” postop constipation, and shorter vaginal length, Dr. Meriwether said.
Also, “we suggest preservation of the uterus in transvaginal apical native tissue repair of prolapse, as it does not worsen any outcomes and slightly reduces OR time and estimated blood loss,” based on 13 studies, including four RCTs, and a total of 1,449 women followed for up to 26 months, she said.
The Review Group also came out in favor of the Manchester procedure, when available, over vaginal hysterectomy with native tissue suspension, based on one RCT and five nonrandomized studies involving 1,126 women and up to 61 months’ follow-up. The Manchester procedure pushed back the time to prolapse reoperation 9 months in one study, and also decreased transfusions, OR time, and blood loss. It also better preserved perineal length.
The group suggested uterine preservation when considering mesh sacrocolpopexy versus mesh sacrohysteropexy, to reduce mesh erosion, OR time, blood loss, hospital stay, and surgery costs, although there might be a slight worsening of Pelvic Floor Distress Inventory and Pelvic Floor Impact scores. The advice was based on nine nonrandomized comparison studies involving 745 women followed for up to 39 months. There was no difference in prolapse resolution between the two techniques.
The one grade A recommendation, for vaginal hysterectomy with native tissue reconstruction over laparoscopic sacrohysteropexy, was based on two RCTs with 182 women followed for up to 12 months.
Hysterectomy in those studies significantly reduced the risk of repeat surgery for prolapse and urinary symptoms, shortened OR time, and improved quality of life scores. However, the benefits came at the cost of slightly shorter vaginal length, worse Pelvic Organ Prolapse Quantification point C scores, greater blood loss, and up to a day longer spent in the hospital.
Dr. Meriwether reported having no relevant financial disclosures.
*Correction, 6/8/2017: An earlier version of this story misstated the status of the Systematic Review Group's recommendations. The recommendations have not been approved as official SGS guidelines. Also, the meeting sponsor information was updated.
Predicting extraction of an intact uterus in robotic-assisted laparoscopic hysterectomy
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Investigators at the University of Tennessee, Chattanooga, have come up with a simple scoring system to predict if an intact uterus can be delivered vaginally during laparoscopic hysterectomy.
Age greater than 50 years counts as 1 point and uterine length greater than 11 cm, height greater than 8 cm, and width greater than 6.9 cm each count for 3 points. A score of 4 or higher suggests the need for an alternative to vaginal extraction, they reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
The team reviewed 367 robotic-assisted total laparoscopic hysterectomies. An intact uterus was able to be extracted vaginally in 265 cases (72%); minilaparotomy was used for the rest. Uterine length, height, and width were documented from pathology reports. The scoring system correctly classified 94.6% of the cases. Sensitivity was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Factoring in parity, uterine weight, body mass index, procedure indications, tobacco use, and comorbidities did not statistically influence the predictive power.
Gynecologic surgeons “are trying to get specimens out intact” and want to know ahead of time if it’s possible, Dr. Mohling said. “I wanted to create a model that was very reproducible.”
The general benchmark for vaginal delivery of an intact uterus is size below 12 weeks pregnancy, but the University of Tennessee model is more precise, according to Dr. Mohling. “I’ve added this to my counseling,” she said.
There was no external funding for the work and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The sensitivity of the scoring system was 85.3%, specificity was 98.1%, positive predictive value was 94.57%, and negative predictive value was 94.55%.
Data source: Single-center review of 367 robotic total laparoscopic hysterectomies during 2012-2015.
Disclosures: There was no external funding for the work, and the investigators reported having no relevant financial disclosures.
Confirmatory blood typing unnecessary for closed prolapse repairs
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
A lot of people automatically order type and screen for vaginal prolapse repairs, but we really need to rethink that if there aren’t risk factors that warrant it. I defer to the anesthesiologists because they are the ones who usually want this, but most of the time we screen but don’t use the results. There’s room to improve clinical practice here.
Robert Gutman, MD, is a gynecologic surgeon in Washington, D.C., and the program chair for the 2017 Society of Gynecologic Surgeons annual scientific meeting. He wasn’t involved in the studies presented.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – It was safe to skip preoperative blood type and antibody screening before vaginal and robotic apical prolapse surgeries at the University of North Carolina, Chapel Hill, so long as the women didn’t have hemorrhage risk factors.
The rate of blood transfusions was 0.5% for both the 204 women who had vaginal repairs and the 203 women who underwent robotic repairs; the rate of positive antibody tests was 1.6%. Given the 0.4% risk of transfusion reactions in unscreened women, the investigators calculated that the risk of serious transfusion reactions was 1 in 50,000 with closed vaginal prolapse repairs.
“The bottom line for us is that the risk in this situation is very low, even if preop type and screens are not performed, and women hemorrhage. This information provides insight to answer our key clinical question, which was if we should continue to order preop type and screens,” lead investigator Taylor Brueseke, MD, an ob.gyn. fellow at the University of North Carolina, Chapel Hill, said at the annual scientific meeting of the Society of Gynecologic Surgeons.
That question has been on the minds of gynecologic surgeons, and it’s probably never been parsed out before by route of surgery. The American College of Pathologists recommends two blood type and antibody screens from separate venipunctures before surgery. Often, the second, confirmatory test means that women have to come in even earlier on the morning of surgery and deal with another painful blood draw. It also adds a few hundred dollars to the bill.
Every surgeon needs to draw their own line between risks and benefits, Dr. Brueseke said, but it seems reasonable in many cases to skip the second screening for closed repairs. Even if a woman has a transfusion reaction, “it doesn’t mean that the patient is going to die. It’s something that you can deal with,” he said.
However, the team reached a different conclusion for women who undergo open abdominal repairs. Among the 201 cases they reviewed, 10.5% had a transfusion, which translated to a transfusion reaction risk of 1 in 2,645 for unscreened women undergoing open apical prolapse surgery. The higher hemorrhage rate was probably due to concomitant Burch procedures and other open incontinence operations.
For abdominal cases, and for women who have had prior transfusions, surgeries, or anticoagulation, “consider type and screen,” Dr. Brueseke said at the meeting.
In a separate study presented at the conference, more than 50,000 pelvic floor disorder surgeries in the National Surgery Quality Improvement Program database further defined the hemorrhage risk.
Investigators at Ohio State University, Columbus, found that the overall incidence of blood transfusions was low at 1.26%, but open abdominal procedures again increased the risk. Other factors associated with an increased risk of blood transfusion included preoperative hematocrit less than 30%, an American Society of Anesthesiologists physical status score of 3 or higher, concomitant hysterectomy, body mass index below 18.5 kg/m2, age less than 30 and over 65 years, and a history of bleeding disorders.
In the UNC study, the median Pelvic Organ Prolapse Quantification was stage III. Patients with bleeding disorders, anticoagulant use, or combined surgery with other services were excluded.
There was no industry funding for the two studies, and the investigators reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: Given the 0.4% risk of transfusion reactions in unscreened women, the risk of serious transfusion reactions was 1 in 50,000 women with closed apical prolapse repairs.
Data source: A review of more than 600 cases of apical prolapse surgery at a single center.
Disclosures: There was no industry funding, and the investigators reported having no relevant financial disclosures.
Long-term durability low for nonmesh vaginal prolapse repair
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – At 5-year follow-up, outcomes were slightly better on most measures for transvaginal uterosacral ligament suspension versus transvaginal sacrospinous ligament fixation for apical prolapse, but the differences were not statistically significant, according to the first randomized trial to compare the two techniques.
Quality of life improvements were durable, but the overall 5-year success rate – defined as the absence of descent of the vaginal apex more than one-third into the vagina; anterior or posterior vaginal wall descent beyond the hymen; bothersome vaginal bulge symptoms; and further treatment for prolapse – was 39% in the 109 women randomized to bilateral uterosacral ligament suspension (ULS) and 30% in the 109 women randomized to unilateral sacrospinous ligament fixation (SSLF).
But there was a notable finding in the study. If women failed to meet all the requirements for success at any one visit, they were classified as surgical failures. However, many who missed the mark at one visit met all the requirements for success on other visits, including their last follow-up.
“We don’t think as surgeons that a bulge comes and goes on a yearly basis, but people actually moved in and out of success and failure over time, and that’s new,” Dr. Jelovsek said. “We just don’t understand the dynamic variables of anatomic prolapse, because no one’s looked at it. The assumption of ‘once a failure, always a failure’ may underestimate success rates.”
Nonetheless, using that approach in the study, the investigators found that the anatomic success was 54% in the ULS and 38% in the SSLF groups at 5 years, and 37% of women in the ULS group reported bothersome vaginal bulge symptoms, versus 42% of women with SSLF. A total of 12% of women with ULS and 8% of women with SSLF had undergone POP retreatment at 5 years, either by pessary or secondary surgery but, again, the differences were not statistically significant.
Of the 145 anatomic failures in the study, 41% were stage 3 or 4.
Quality of life improvements, assessed annually by phone, “were maintained over 5 years despite progressive increases in surgical failure rates over time,” with about a 70-point improvement in the Pelvic Organ Prolapse Distress Inventory and similar gains in other measures in both groups, Dr. Jelovsek reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
There were no between-group differences in suture exposure (about 25% in both groups) or sling erosion (about 3%) at 5 years.
There was a difference in granulation tissue: 28.9% with ULS and 18.8% with SSLF (odds ratio with ULS, 1.9; 95% confidence interval 1-3.7). The majority of adverse events occurred within 2 years of surgery.
Early pelvic floor muscle training made no difference in outcomes for the women randomized to it.
The women in the study had stage 2-4 prolapse at baseline. In addition to vaginal suspension surgery, they had vaginal hysterectomies if there was uterine prolapse, and all the women had concomitant retropubic midurethral sling surgery for stress incontinence.
At 2 years, composite success rates were about 60% in both groups (JAMA. 2014 Mar 12;311[10]:1023-34).
The study didn’t identify risk factors for failure, but they would be helpful to know, Dr. Jelovsek said. High-risk women might benefit from a more durable mesh repair. For now at least, “most women say the risk” of pain and other serious mesh complications “completely outweighs the bulge symptoms,” he said.
The trial, an extension of OPTIMAL (Operations and Pelvic Muscle Training in the Management of Apical Support Loss), was conducted at nine U.S. centers in the Pelvic Floor Disorders Network, which is funded by the National Institutes of Health. Dr. Jelovsek reported having no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
Key clinical point:
Major finding: The overall 5-year success rate was 39% in women randomized to bilateral uterosacral ligament suspension and 30% in women randomized to unilateral sacrospinous ligament fixation.
Data source: The first randomized trial to compare the two commonly used techniques was conducted among 218 women at nine U.S. centers in the Pelvic Floor Disorders Network.
Disclosures: The Pelvic Floor Disorders Network is funded by the National Institutes of Health. The lead investigator reported having no relevant financial disclosures.
Don’t shy away from vaginal salpingectomy
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Surgeons at Houston Methodist Hospital reported a 75% success rate in removing both fallopian tubes during vaginal hysterectomy in a study presented at the annual scientific meeting of the Society of Gynecologic Surgeons.
Serous ovarian carcinoma is now thought to arise from the distal fallopian tube, and it’s estimated that salpingectomy prevents diagnosis of ovarian cancer in 1 in 225 women and death from ovarian cancer in 1 in 450 women. The American Congress of Obstetricians and Gynecologists recommends that surgeons and patients “discuss the potential benefits of the removal of the fallopian tubes” during hysterectomy in women not having an oophorectomy.
The findings from the Houston team show that “it’s feasible in most cases, with very little risk,” said Danielle Antosh, MD, lead investigator and director of the Center for Restorative Pelvic Medicine at Houston Methodist Urogynecology Associates.
“People are doing laparoscopic hysterectomies or robotic hysterectomies” to get at the fallopian tubes, “but they shouldn’t be deterred from trying to remove the fallopian tubes vaginally,” Dr. Antosh said at the SGS 2017 meeting. When women are having a vaginal hysterectomy, “why not try to remove the fallopian tubes? It’s something I would definitely consider counseling your patients about.”
Dr. Antosh said that residents should be taught how to perform salpingectomy during vaginal hysterectomy. “I think it is definitely feasible for residents to do.” Technically, “it’s a lot easier than removing the ovaries” vaginally, she said.
The 70 women in the study were undergoing vaginal hysterectomies by attending physicians for benign reasons, mostly uterine prolapse, followed by heavy menstrual flow and fibroids. In total, 52 (75%) had successful concomitant bilateral vaginal salpingectomies, and 7 additional women had one tube removed. Success was more likely with increasing parity and a history of prolapse. Most of the failures were because the tubes were too high in the pelvis or there were adhesions from prior adnexal surgery. Even with prior adnexal surgery, however, the success rate was 50%.
Vaginal salpingectomy added a mean of 11 minutes to surgery and a mean of 5 mL blood loss. There were no complications reported from including salpingectomy with vaginal hysterectomy. The study wasn’t powered to detect an impact on menopause symptoms, but there was a decrease in menopause symptoms at 16 week follow-up in the salpingectomy group, perhaps related to less sexual dysfunction and urinary incontinence.
The mean age in the study was 51 years, and mean body mass index was 27 kg/m2. There were no malignancies found on tubal pathology.
Five women were transferred to an abdominal approach because of a large uterus or discovery of ovarian pathology. None were transferred for the purpose of salpingectomy.
There was no external funding for the study, and the investigators reported no relevant financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: Three-quarters of women undergoing vaginal hysterectomy for benign reasons had successful concomitant bilateral vaginal salpingectomy.
Data source: A single-center, observational study among 70 women undergoing vaginal hysterectomy for benign reasons.
Disclosures: There was no external funding and the investigators reported no relevant financial disclosures.
Study supports NCCN recommendations on risk-reducing salpingo-oophorectomy
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
NATIONAL HARBOR, MD – A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy (RRSO) between ages 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations, Lydia Usha, MD, said at the annual meeting of the Society of Gynecologic Oncology.
The average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations, said Dr. Usha of Rush Medical College, Chicago. When appropriate, delaying RRSO “avoids the psychosocial and medical complications of premature menopause,” she said.
Among all women, mutation prevalence was 0.3% for BRIP1, 0.1% for RAD51C and RAD51D, 1.2% for BRCA1, and 1.3% for BRCA2 mutations, Dr. Usha reported. Among 18,719 women who had a personal history of ovarian cancer, the most common mutation was BRCA1 (3.5%), followed by BRCA2 (2.7%). In contrast, the combined prevalence of BRIP1, RAD51C, and RAD51D mutations among cancer patients was only 1.6%.
Cancer prevalence was highest among women who had mutations of RAD51C (22%), followed by RAD51D (19%), BRCA1 and BRIP1 (16% in each case), and BRCA2 (11%). Thus, while BRIP1 and RAD51D mutations were uncommon, their presence signified an ovarian cancer risk that was similar to that with BRCA1 mutations, and a greater risk than with BRCA2, Dr. Usha said.
The average ages for ovarian cancer diagnosis were 64 years for BRIP1, 61 years for RAD51C, 60 years for BRCA2, 56 years for RAD51C, and 54 years for BRCA1. “More than 80% of women with ovarian cancer who had a mutation in BRIP1, RAD51C, or BRCA2 were diagnosed after age 50,” Dr. Usha noted. These findings support considering RRSO closer to age 45 years for RAD51D mutation carriers and closer to age 50 years for women with pathogenic variants of BRIP1, added discussant Kari Ring, MD, of the University of Virginia, Charlottesville.
Mutation type did not significantly correlate with ethnicity or type of ovarian cancer, Dr. Usha noted. “Collectively, these findings may aid clinical decisions about the medical management of women with mutations in these genes,” she said. “Our data may also assist with reproductive decisions, such as age of childbearing.”
Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Key clinical point: A large hereditary cancer study supports National Comprehensive Cancer Network guidance to consider risk-reducing salpingo-oophorectomy between age 45 and 50 years for women with BRIP1, RAD51C, or RAD51D mutations.
Major finding: Average ages for an ovarian cancer diagnosis were 56 years for women with RAD51D mutations, 61 years for RAD51C mutations, and 64 years for BRIP1 mutations.
Data source: Analyses of a 25-gene hereditary panel performed in 345,667 women.
Disclosures: Dr. Usha did not report external funding sources, but disclosed travel expenses from Myriad Genetics.
Laparoscopic and abdominal hysterectomy yield equivalent survival
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
This study adds to a growing body of literature that suggests laparoscopic hysterectomy is not only safe, but also the preferred modality of hysterectomy for women with endometrial cancer.
Despite the clear benefits of laparoscopic hysterectomy, the findings from the LACE trial should be interpreted in the context of the study design. Importantly, patients randomized to the study represent a highly select group of women with endometrial cancer. The study entry criteria involved a low-risk population of women with stage I tumors of endometrioid histology with a uterine size of less than 10 weeks’ gestation. In practice, laparoscopic hysterectomy is now routinely used for women with nonendometrioid histologies and in those with more advanced disease.
The LACE trial reported by Janda et al. provides confirmation that laparoscopic hysterectomy is a safe and effective treatment modality for women with early-stage endometrial cancer. The favorable short-term outcomes along with equivalent oncological outcomes make laparoscopic hysterectomy the preferred surgical modality in this setting. Even though the road to defining the benefits of laparoscopic hysterectomy has been long, efforts to promote the procedure for women with endometrial cancer should now be a priority.
Jason D. Wright, MD, is at the Herbert Irving Comprehensive Cancer Center and the department of ob.gyn. at Columbia University, New York. He reported having no relevant financial disclosures. These comments are excerpted from an accompanying editorial (JAMA 2017;317[12]:1215-6).
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
Laparoscopic hysterectomy yields equivalent disease-free and overall survival at 4.5 years, compared with abdominal hysterectomy in stage I endometrial cancer, according to a report published online March 28 in JAMA.
Several short-term advantages with the laparoscopic approach have been well documented, including less pain, less morbidity, better quality of life, decreased risk of surgery-related adverse events, and cost savings. But until now, no large international trial has demonstrated that longer-term survival outcomes are at least as good with laparoscopic as with open abdominal hysterectomy in this patient population, reported Monika Janda, PhD, of Queensland University of Technology, Brisbane (Australia) and her colleagues.
They conducted the Laparoscopic Approach to Cancer of the Endometrium (LACE) trial, a randomized equivalence study involving 760 women treated at 20 medical centers in Australia, New Zealand, and Hong Kong during 2005-2010. The women were followed for a median of 4.5 years.
All of the women had histologically confirmed stage I adenocarcinoma of the endometrium. A total of 407 patients were randomly assigned to undergo total laparoscopic hysterectomy and 353 patients to undergo total abdominal hysterectomy. Medical comorbidities were equally distributed between the two study groups, and there were no significant between-group differences in tumor type, histologic grade, number of involved lymph nodes, or adjuvant treatments.
Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy, meeting the criteria for equivalence. Overall survival at 4.5 years was 92.0% and 92.4%, respectively. Cancer recurred near the operative site in 3% of each group and at a regional or distant site in 2% or less of each group. Causes of death also were similar between the two study groups, with 56% of all deaths attributed to endometrial cancer (JAMA. 2017;317[12]:1224-33).
Of note, two patients who underwent laparoscopic surgery developed port-site metastases and two patients who underwent abdominal surgery developed metastases at the site of the abdominal wound.
The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and numerous others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.
FROM JAMA
Key clinical point:
Major finding: Disease-free survival at 4.5 years was 81.6% with laparoscopic hysterectomy and 81.3% with abdominal hysterectomy.
Data source: An international, randomized, phase III equivalence trial involving 760 women treated with total abdominal or total laparoscopic hysterectomy.
Disclosures: The study was funded by Cancer Councils in Australia, the National Health and Medical Research Council, Cancer Australia, QLD Health, and others. Dr. Janda reported having no relevant financial disclosures; one of her coauthors reported ties to the O.R. Company, SurgicalPerformance Pty, and Covidien.