User login
Researchers examine learning curve for gender-affirming vaginoplasty
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
FROM SGS 2020
Identifying ovarian malignancy is not so easy
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
When an ovarian mass is anticipated or known, following evaluation of a patient’s history and physician examination, imaging via transvaginal and often abdominal ultrasound is the very next step. This evaluation likely will include both gray-scale and color Doppler examination. The initial concern always must be to identify ovarian malignancy.
Despite morphological scoring systems as well as the use of Doppler ultrasonography, there remains a lack of agreement and acceptance. In a 2008 multicenter study, Timmerman and colleagues evaluated 1,066 patients with 1,233 persistent adnexal tumors via transvaginal grayscale and Doppler ultrasound; 73% were benign tumors, and 27% were malignant tumors. Information on 42 gray-scale ultrasound variables and 6 Doppler variables was collected and evaluated to determine which variables had the highest positive predictive value for a malignant tumor and for a benign mass (Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365).
Five simple rules were selected that best predict malignancy (M-rules), as follows:
- Irregular solid tumor.
- Ascites.
- At least four papillary projections.
- Irregular multilocular-solid tumor with a greatest diameter greater than or equal to 10 cm.
- Very high color content on Doppler exam.
The following five simple rules suggested that a mass is benign (B-rules):
- Unilocular cyst.
- Largest solid component less than 7 mm.
- Acoustic shadows.
- Smooth multilocular tumor less than 10 cm.
- No detectable blood flow with Doppler exam.
Unfortunately, despite a sensitivity of 93% and specificity of 90%, and a positive and negative predictive value of 80% and 97%, these 10 simple rules were applicable to only 76% of tumors.
To assist those of us who are not gynecologic oncologists and who are often faced with having to determine whether surgery is recommended, I have elicited the expertise of Jubilee Brown, MD, professor and associate director of gynecologic oncology at the Levine Cancer Institute, Carolinas HealthCare System, in Charlotte, N.C., and the current president of the AAGL, to lead us in a review of evaluating an ovarian mass.
Dr. Miller is professor of obstetrics & gynecology in the department of clinical sciences, Rosalind Franklin University, North Chicago, Ill., and director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, both in Illinois. Email him at [email protected].
How to evaluate a suspicious ovarian mass
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Ovarian masses are common in women of all ages. It is important not to miss even one ovarian cancer, but we must also identify masses that will resolve on their own over time to avoid overtreatment. These concurrent goals of excluding malignancy while not overtreating patients are the basis for management of the pelvic mass. Additionally, fertility preservation is important when surgery is performed in a reproductive-aged woman.
An ovarian mass may be anything from a simple functional or physiologic cyst to an endometrioma to an epithelial carcinoma, a germ-cell tumor, or a stromal tumor (the latter three of which may metastasize). Across the general population, women have a 5%-10% lifetime risk of needing surgery for a suspected ovarian mass and a 1.4% (1 in 70) risk that this mass is cancerous. The majority of ovarian cysts or masses therefore are benign.
A thorough history – including family history – and physical examination with appropriate laboratory testing and directed imaging are important first steps for the ob.gyn. Fortunately, we have guidelines and criteria governing not only when observation or surgery is warranted but also when patients should be referred to a gynecologic oncologist. By following these guidelines,1 we are able to achieve the best outcomes.
Transvaginal ultrasound
A 2007 groundbreaking study led by Barbara Goff, MD, demonstrated that there are warning signs for ovarian cancer – symptoms that are significantly associated with malignancy. Dr. Goff and her coinvestigators evaluated the charts of hundreds of patients, including about 150 with ovarian cancer, and found that pelvic/abdominal pressure or pain, bloating, increase in abdominal size, and difficulty eating or feeling full were significantly and independently associated with cancer if these symptoms were present for less than a year and occurred at least 12 times per month.2
A pelvic examination is an integral part of evaluating every patient who has such concerns. That said, pelvic exams have limited ability to identify adnexal masses, especially in women who are obese – and that’s where imaging becomes especially important.
Masses generally can be considered simple or complex based on their appearance. A simple cyst is fluid-filled with thin, smooth walls and the absence of solid components or septations; it is significantly more likely to resolve on its own and is less likely to imply malignancy than a complex cyst, especially in a premenopausal woman. A complex cyst is multiseptated and/or solid – possibly with papillary projections – and is more concerning, especially if there is increased, new vascularity. Making this distinction helps us determine the risk of malignancy.
Transvaginal ultrasound (TVUS) is the preferred method for imaging, and our threshold for obtaining a TVUS should be very low. Women who have symptoms or concerns that can’t be attributed to a particular condition, and women in whom a mass can be palpated (even if asymptomatic) should have a TVUS. The imaging modality is cost effective and well tolerated by patients, does not expose the patient to ionizing radiation, and should generally be considered first-line imaging.3,4
Size is not predictive of malignancy, but it is important for determining whether surgery is warranted. In our experience, a mass of 8-10 cm or larger on TVUS is at risk of torsion and is unlikely to resolve on its own, even in a premenopausal woman. While large masses generally require surgery, patients of any age who have simple cysts smaller than 8-10 cm generally can be followed with serial exams and ultrasound; spontaneous regression is common.
Doppler ultrasonography is useful for evaluating blood flow in and around an ovarian mass and can be helpful for confirming suspected characteristics of a mass.
Recent studies from the radiology community have looked at the utility of the resistive index – a measure of the impedance and velocity of blood flow – as a predictor of ovarian malignancy. However, we caution against using Doppler to determine whether a mass is benign or malignant, or to determine the necessity of surgery. An abnormal ovary may have what is considered to be a normal resistive index, and the resistive index of a normal ovary may fall within the abnormal range. Doppler flow can be helpful, but it must be combined with other predictive features, like solid components with flow or papillary projections within a cyst, to define a decision about surgery.4,5
Magnetic resonance imaging can be useful in differentiating a fibroid from an ovarian mass, and a CT scan can be helpful in looking for disseminated disease when ovarian cancer is suspected based on ultrasound imaging, physical and history, and serum markers. A CT is useful, for instance, in a patient whose ovary is distended with ascites or who has upper abdominal complaints and a complex cyst. CT, PET, and MRI are not recommended in the initial evaluation of an ovarian mass.
The utility of serum biomarkers
Cancer antigen 125 (CA-125) testing may be helpful – in combination with other findings – for decision-making regarding the likelihood of malignancy and the need to refer patients. CA-125 is like Doppler in that a normal CA-125 cannot eliminate the possibility of cancer, and an abnormal CA-125 does not in and of itself imply malignancy. It’s far from a perfect cancer screening test.
CA-125 is a protein associated with epithelial ovarian malignancies, the type of ovarian cancer most commonly seen in postmenopausal women with genetic predispositions. Its specificity and positive predictive value are much higher in postmenopausal women than in average-risk premenopausal women (those without a family history or a known mutation that predisposes them to ovarian cancer). Levels of the marker are elevated in association with many nonmalignant conditions in premenopausal women – endometriosis, fibroids, and various inflammatory conditions, for instance – so the marker’s utility in this population is limited.
For women who have a family history of ovarian cancer or a known breast cancer gene 1 (BRCA1) or BRCA2 mutation, there are some data that suggest that monitoring with CA-125 measurements and TVUS may be a good approach to following patients prior to the age at which risk-reducing surgery can best be performed.
In an adolescent girl or a woman of reproductive age, we think less about epithelial cancer and more about germ-cell and stromal tumors. When a solid mass is palpated or visualized on imaging, we therefore will utilize a different set of markers; alpha-fetoprotein, L-lactate dehydrogenase, and beta-HCG, for instance, have much higher specificity than CA-125 does for germ-cell tumors in this age group and may be helpful in the evaluation. Similarly, in cases of a very large mass resembling a mucinous tumor, a carcinoembryonic antigen may be helpful.
A number of proprietary profiling technologies have been developed to determine the risk of a diagnosed mass being malignant. For instance, the OVA1 assay looks at five serum markers and scores the results, and the Risk of Ovarian Malignancy Algorithm (ROMA) combines the results of three serum markers with menopausal status into a numerical score. Both have Food and Drug Administration approval for use in women in whom surgery has been deemed necessary. These panels can be fairly predictive of risk and may be helpful – especially in rural areas – in determining which women should be referred to a gynecologic oncologist for surgery.
It is important to appreciate that an ovarian cyst or mass should never be biopsied or aspirated lest a malignant tumor confined to one ovary be potentially spread to the peritoneum.
Referral to a gynecologic oncologist
Postmenopausal women with a CA-125 greater than 35 U/mL should be referred, as should postmenopausal women with ascites, those with a nodular or fixed pelvic mass, and those with suspected abdominal or distant metastases (per a CT scan, for instance).
In premenopausal women, ascites, a nodular or fixed mass, and evidence of metastases also are reasons for referral to a gynecologic oncologist. CA-125, again, is much more likely to be elevated for reasons other than malignancy and therefore is not as strong a driver for referral as in postmenopausal women. Patients with markedly elevated levels, however, should probably be referred – particularly when other clinical factors also suggest the need for consultation. While there is no evidence-based threshold for CA-125 in premenopausal women, a CA-125 greater than 200 U/mL is a good cutoff for referral.
For any patient, family history of breast and/or ovarian cancer – especially in a first-degree relative – raises the risk of malignancy and should figure prominently into decision-making regarding referral. Criteria for referral are among the points discussed in the ACOG 2016 Practice Bulletin on Evaluation and Management of Adnexal Masses.1
A note on BRCA mutations
As the American College of Obstetricians and Gynecologists says in its practice bulletin, the most important personal risk factor for ovarian cancer is a strong family history of breast or ovarian cancer. Women with such a family history can undergo genetic testing for BRCA mutations and have the opportunity to prevent ovarian cancers when mutations are detected. This simple blood test can save lives.
A modeling study we recently completed – not yet published – shows that it actually would be cost effective to do population screening with BRCA testing performed on every woman at age 30 years.
According to the National Cancer Institute website (last review: 2018), it is estimated that about 44% of women who inherit a BRCA1 mutation, and about 17% of those who inherit a BRAC2 mutation, will develop ovarian cancer by the age of 80 years. By identifying those mutations, women may undergo risk-reducing surgery at designated ages after childbearing is complete and bring their risk down to under 5%.
An international take on managing adnexal masses
- Pelvic ultrasound should include the transvaginal approach. Use Doppler imaging as indicated.
- Although simple ovarian cysts are not precursor lesions to a malignant ovarian cancer, perform a high-quality examination to make sure there are no solid/papillary structures before classifying a cyst as a simple cyst. The risk of progression to malignancy is extremely low, but some follow-up is prudent.
- The most accurate method of characterizing an ovarian mass currently is real-time pattern recognition sonography in the hands of an experienced imager.
- Pattern recognition sonography or a risk model such as the International Ovarian Tumor Analysis (IOTA) Simple Rules can be used to initially characterize an ovarian mass.
- When an ovarian lesion is classified as benign, the patient may be followed conservatively, or if indicated, surgery can be performed by a general gynecologist.
- Serial sonography can be beneficial, but there are limited prospective data to support an exact interval and duration.
- Fewer surgical interventions may result in an increase in sonographic surveillance.
- When an ovarian lesion is considered indeterminate on initial sonography, and after appropriate clinical evaluation, a “second-step” evaluation may include referral to an expert sonologist, serial sonography, application of established risk-prediction models, correlation with serum biomarkers, correlation with MRI, or referral to a gynecologic oncologist for further evaluation.
From the First International Consensus Report on Adnexal Masses: Management Recommendations
Source: Glanc P et al. J Ultrasound Med. 2017 May;36(5):849-63.
Dr. Brown reported that she had received an earlier grant from Aspira Labs, the company that developed the OVA1 assay. Dr. Miller reported that he has no relevant financial disclosures.
References
1. Obstet Gynecol. 2016 Nov. doi: 10.1097/AOG.0000000000001768.
2. Cancer. 2007 Jan 15. doi: 10.1002/cncr.22371.
3. Clin Obstet Gynecol. 2015 Mar. doi: 10.1097/GRF.0000000000000083.
4. Ultrasound Q. 2013 Mar. doi: 10.1097/RUQ.0b013e3182814d9b.
5. Ultrasound Obstet Gynecol. 2008 Jun. doi: 10.1002/uog.5365.
Patients may prefer retrograde-fill voiding trials after pelvic floor surgery
Voiding trials after female pelvic floor surgery may detect similar rates of voiding dysfunction regardless of whether voiding occurs spontaneously or after the bladder is retrograde-filled with saline, according to a randomized study.
Nevertheless, patients may prefer the more common retrograde-fill approach.
In the study of 109 patients, those who underwent retrograde fill reported significantly greater satisfaction with their method of voiding evaluation, compared with patients whose voiding trials occurred spontaneously. The increased satisfaction could relate to the fact that retrograde-fill trials take less time, study investigator Patrick Popiel, MD, of Yale University, New Haven, Conn., suggested at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. The exact reasons are unclear, however.
Voiding trials help identify patients who cannot sufficiently empty their bladder after surgery. Prior research has indicated that the incidence of voiding dysfunction after pelvic floor surgery is about 25%-35%. “Patients with voiding dysfunction are generally managed with an indwelling Foley catheter or clean intermittent self-catheterization,” Dr. Popiel said. “Catheterization increases the risk of urinary tract infection, increases anxiety, and decreases patient satisfaction. A large proportion of patients who are discharged home with a Foley catheter state that the catheter was the worst aspect of their experience.”
Dr. Popiel and colleagues conducted a randomized, prospective study to examine the rate of failed voiding trials that necessitate discharge home with an indwelling Foley catheter using spontaneous and retrograde-fill approaches. The study included women who required a voiding trial after surgery for pelvic organ prolapse or urinary incontinence. Patients who required prolonged catheterization after surgery, such as those with a urinary tract infection, bowel injury, or large amount of blood loss, were excluded.
Researchers analyzed data from 55 patients who were randomly assigned to the retrograde-fill group and 54 patients who were randomly assigned to the spontaneous trial group.
In the spontaneous group, patients were required to void at least 150 mL at one time within 6 hours of catheter removal to successfully complete the voiding trial.
In the retrograde-fill group, the bladder was filled in the postanesthesia care unit with 300 mL of saline or until the maximum volume tolerated by the patient (not exceeding 300 mL ) was reached. Patients in this group had to void at least 150 mL or 50% of the instilled volume at one time within 60 minutes of catheter removal to pass the trial.
The researchers documented postvoid residual (PVR) but did not use this measure to determine voiding function.
The baseline demographics of the two groups were similar, although prior hysterectomy was more common in the retrograde-fill group than in the spontaneous group (32.7% vs. 14.8%). The average age was 58.5 years in the retrograde-fill group and 61 years in the spontaneous group.
“There was no significant difference in our primary outcome,” Dr. Popiel said. “There was a 12.7% rate of failed voiding trial in the retrograde group versus 7.7% in the spontaneous group.”
No patients had urinary retention after initially passing their voiding trial. Force of stream did not differ between groups, and about 15% in each group had a postoperative urinary tract infection.
The study demonstrates that voiding assessment based on a spontaneous minimum void of 150 mL is safe and has similar pass rates, compared with the more commonly performed retrograde void trial, Dr. Popiel said. “If the voided amount is at least 150 mL, PVR is not critical to obtain. The study adds to the body of literature that supports less stringent criteria for evaluating voiding function and can limit postoperative urinary recatheterization.”
The investigators allowed patients with PVRs as high as 575 mL to return home without an alternative way to empty the bladder, C. Sage Claydon, MD, a urogynecologist who was not involved in the study, noted during a discussion after the presentation. In all, 6 patients who met the passing criteria for the spontaneous voiding trial had a PVR greater than 200 mL, with volumes ranging from 205-575 mL.
The patients received standardized counseling about postoperative voiding problems, said Dr. Popiel. “This is similar to the work done by Ingber et al. from 2011, where patients who reached a certain force of stream, greater than 5 out of 10, were discharged home regardless of PVR.”
Dr. Popiel had no relevant disclosures. Two coinvestigators disclosed ties to BlossomMed, Renovia, and ArmadaHealth.
SOURCE: Popiel P et al. SGS 2020, Abstract 14.
Voiding trials after female pelvic floor surgery may detect similar rates of voiding dysfunction regardless of whether voiding occurs spontaneously or after the bladder is retrograde-filled with saline, according to a randomized study.
Nevertheless, patients may prefer the more common retrograde-fill approach.
In the study of 109 patients, those who underwent retrograde fill reported significantly greater satisfaction with their method of voiding evaluation, compared with patients whose voiding trials occurred spontaneously. The increased satisfaction could relate to the fact that retrograde-fill trials take less time, study investigator Patrick Popiel, MD, of Yale University, New Haven, Conn., suggested at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. The exact reasons are unclear, however.
Voiding trials help identify patients who cannot sufficiently empty their bladder after surgery. Prior research has indicated that the incidence of voiding dysfunction after pelvic floor surgery is about 25%-35%. “Patients with voiding dysfunction are generally managed with an indwelling Foley catheter or clean intermittent self-catheterization,” Dr. Popiel said. “Catheterization increases the risk of urinary tract infection, increases anxiety, and decreases patient satisfaction. A large proportion of patients who are discharged home with a Foley catheter state that the catheter was the worst aspect of their experience.”
Dr. Popiel and colleagues conducted a randomized, prospective study to examine the rate of failed voiding trials that necessitate discharge home with an indwelling Foley catheter using spontaneous and retrograde-fill approaches. The study included women who required a voiding trial after surgery for pelvic organ prolapse or urinary incontinence. Patients who required prolonged catheterization after surgery, such as those with a urinary tract infection, bowel injury, or large amount of blood loss, were excluded.
Researchers analyzed data from 55 patients who were randomly assigned to the retrograde-fill group and 54 patients who were randomly assigned to the spontaneous trial group.
In the spontaneous group, patients were required to void at least 150 mL at one time within 6 hours of catheter removal to successfully complete the voiding trial.
In the retrograde-fill group, the bladder was filled in the postanesthesia care unit with 300 mL of saline or until the maximum volume tolerated by the patient (not exceeding 300 mL ) was reached. Patients in this group had to void at least 150 mL or 50% of the instilled volume at one time within 60 minutes of catheter removal to pass the trial.
The researchers documented postvoid residual (PVR) but did not use this measure to determine voiding function.
The baseline demographics of the two groups were similar, although prior hysterectomy was more common in the retrograde-fill group than in the spontaneous group (32.7% vs. 14.8%). The average age was 58.5 years in the retrograde-fill group and 61 years in the spontaneous group.
“There was no significant difference in our primary outcome,” Dr. Popiel said. “There was a 12.7% rate of failed voiding trial in the retrograde group versus 7.7% in the spontaneous group.”
No patients had urinary retention after initially passing their voiding trial. Force of stream did not differ between groups, and about 15% in each group had a postoperative urinary tract infection.
The study demonstrates that voiding assessment based on a spontaneous minimum void of 150 mL is safe and has similar pass rates, compared with the more commonly performed retrograde void trial, Dr. Popiel said. “If the voided amount is at least 150 mL, PVR is not critical to obtain. The study adds to the body of literature that supports less stringent criteria for evaluating voiding function and can limit postoperative urinary recatheterization.”
The investigators allowed patients with PVRs as high as 575 mL to return home without an alternative way to empty the bladder, C. Sage Claydon, MD, a urogynecologist who was not involved in the study, noted during a discussion after the presentation. In all, 6 patients who met the passing criteria for the spontaneous voiding trial had a PVR greater than 200 mL, with volumes ranging from 205-575 mL.
The patients received standardized counseling about postoperative voiding problems, said Dr. Popiel. “This is similar to the work done by Ingber et al. from 2011, where patients who reached a certain force of stream, greater than 5 out of 10, were discharged home regardless of PVR.”
Dr. Popiel had no relevant disclosures. Two coinvestigators disclosed ties to BlossomMed, Renovia, and ArmadaHealth.
SOURCE: Popiel P et al. SGS 2020, Abstract 14.
Voiding trials after female pelvic floor surgery may detect similar rates of voiding dysfunction regardless of whether voiding occurs spontaneously or after the bladder is retrograde-filled with saline, according to a randomized study.
Nevertheless, patients may prefer the more common retrograde-fill approach.
In the study of 109 patients, those who underwent retrograde fill reported significantly greater satisfaction with their method of voiding evaluation, compared with patients whose voiding trials occurred spontaneously. The increased satisfaction could relate to the fact that retrograde-fill trials take less time, study investigator Patrick Popiel, MD, of Yale University, New Haven, Conn., suggested at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. The exact reasons are unclear, however.
Voiding trials help identify patients who cannot sufficiently empty their bladder after surgery. Prior research has indicated that the incidence of voiding dysfunction after pelvic floor surgery is about 25%-35%. “Patients with voiding dysfunction are generally managed with an indwelling Foley catheter or clean intermittent self-catheterization,” Dr. Popiel said. “Catheterization increases the risk of urinary tract infection, increases anxiety, and decreases patient satisfaction. A large proportion of patients who are discharged home with a Foley catheter state that the catheter was the worst aspect of their experience.”
Dr. Popiel and colleagues conducted a randomized, prospective study to examine the rate of failed voiding trials that necessitate discharge home with an indwelling Foley catheter using spontaneous and retrograde-fill approaches. The study included women who required a voiding trial after surgery for pelvic organ prolapse or urinary incontinence. Patients who required prolonged catheterization after surgery, such as those with a urinary tract infection, bowel injury, or large amount of blood loss, were excluded.
Researchers analyzed data from 55 patients who were randomly assigned to the retrograde-fill group and 54 patients who were randomly assigned to the spontaneous trial group.
In the spontaneous group, patients were required to void at least 150 mL at one time within 6 hours of catheter removal to successfully complete the voiding trial.
In the retrograde-fill group, the bladder was filled in the postanesthesia care unit with 300 mL of saline or until the maximum volume tolerated by the patient (not exceeding 300 mL ) was reached. Patients in this group had to void at least 150 mL or 50% of the instilled volume at one time within 60 minutes of catheter removal to pass the trial.
The researchers documented postvoid residual (PVR) but did not use this measure to determine voiding function.
The baseline demographics of the two groups were similar, although prior hysterectomy was more common in the retrograde-fill group than in the spontaneous group (32.7% vs. 14.8%). The average age was 58.5 years in the retrograde-fill group and 61 years in the spontaneous group.
“There was no significant difference in our primary outcome,” Dr. Popiel said. “There was a 12.7% rate of failed voiding trial in the retrograde group versus 7.7% in the spontaneous group.”
No patients had urinary retention after initially passing their voiding trial. Force of stream did not differ between groups, and about 15% in each group had a postoperative urinary tract infection.
The study demonstrates that voiding assessment based on a spontaneous minimum void of 150 mL is safe and has similar pass rates, compared with the more commonly performed retrograde void trial, Dr. Popiel said. “If the voided amount is at least 150 mL, PVR is not critical to obtain. The study adds to the body of literature that supports less stringent criteria for evaluating voiding function and can limit postoperative urinary recatheterization.”
The investigators allowed patients with PVRs as high as 575 mL to return home without an alternative way to empty the bladder, C. Sage Claydon, MD, a urogynecologist who was not involved in the study, noted during a discussion after the presentation. In all, 6 patients who met the passing criteria for the spontaneous voiding trial had a PVR greater than 200 mL, with volumes ranging from 205-575 mL.
The patients received standardized counseling about postoperative voiding problems, said Dr. Popiel. “This is similar to the work done by Ingber et al. from 2011, where patients who reached a certain force of stream, greater than 5 out of 10, were discharged home regardless of PVR.”
Dr. Popiel had no relevant disclosures. Two coinvestigators disclosed ties to BlossomMed, Renovia, and ArmadaHealth.
SOURCE: Popiel P et al. SGS 2020, Abstract 14.
FROM SGS 2020
Molecular developments in treatment of UPSC
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
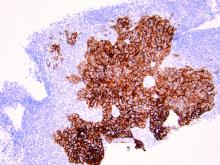
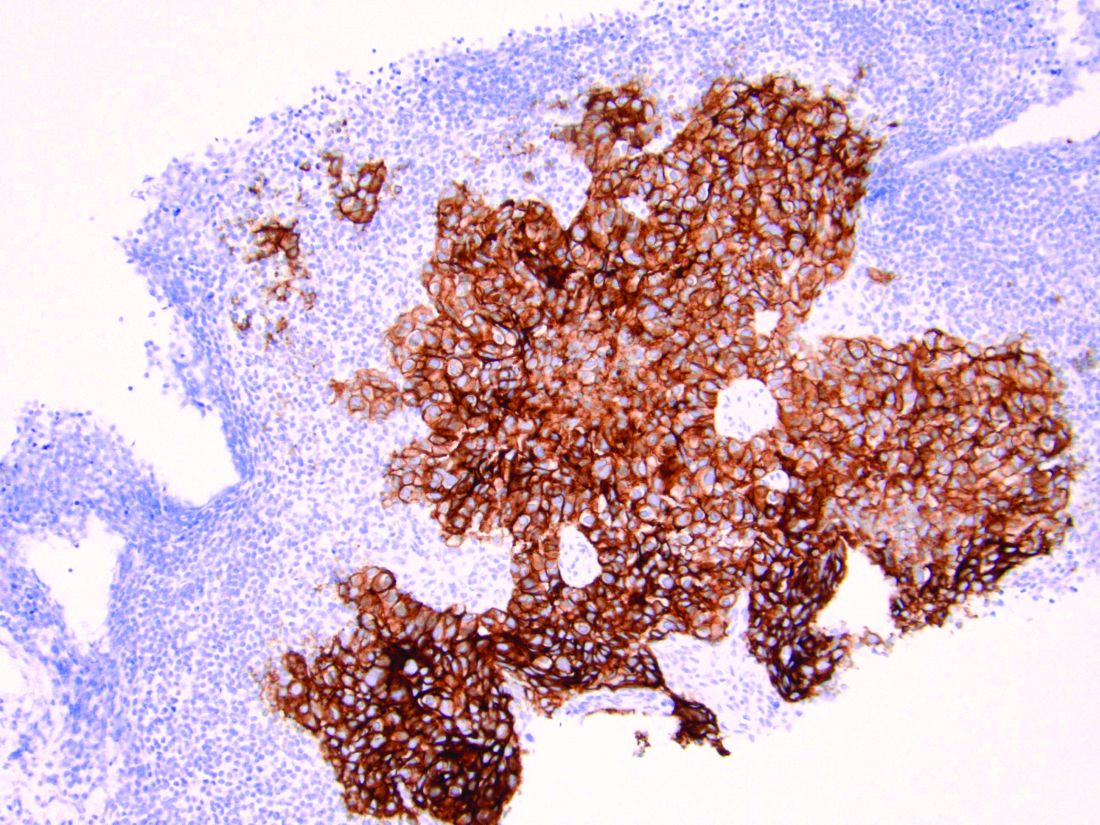
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
Uterine papillary serous carcinoma (UPSC) is an infrequent but deadly form of endometrial cancer comprising 10% of cases but contributing 40% of deaths from the disease. Recurrence rates are high for this disease. Five-year survival is 55% for all patients and only 70% for stage I disease.1 Patterns of recurrence tend to be distant (extrapelvic and extraabdominal) as frequently as they are localized to the pelvis, and metastases and recurrences are unrelated to the extent of uterine disease (such as myometrial invasion). It is for these reasons that the recommended course of adjuvant therapy for this disease is systemic therapy (typically six doses of carboplatin and paclitaxel chemotherapy) with consideration for radiation to the vagina or pelvis to consolidate pelvic and vaginal control.2 This differs from early-stage high/intermediate–risk endometrioid adenocarcinomas, for which adjuvant chemotherapy has not been found to be helpful.
Because of the lower incidence of UPSC, it frequently has been studied alongside endometrioid cell types in clinical trials which explore novel adjuvant therapies. However, UPSC is biologically distinct from endometrioid endometrial cancers, which likely results in inferior clinical responses to conventional interventions. Fortunately we are beginning to better understand UPSC at a molecular level, and advancements are being made in the targeted therapies for these patients that are unique, compared with those applied to other cancer subtypes.
As discussed above, UPSC is a particularly aggressive form of uterine cancer. Histologically it is characterized by a precursor lesion of endometrial glandular dysplasia progressing to endometrial intraepithelial neoplasia (EIC). Histologically it presents with a highly atypical slit-like glandular configuration, which appears similar to serous carcinomas of the fallopian tube and ovary. Molecularly these tumors commonly manifest mutations in tumor protein p53 (TP53) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), which are both genes associated with oncogenic potential.1 While most UPSC tumors have loss of expression in hormone receptors such as estrogen and progesterone, 25%-30% of cases overexpress the tyrosine kinase receptor human epidermal growth factor receptor 2 (HER2).3-5 This has proven to provide an exciting target for therapeutic interventions.
A target for therapeutic intervention
HER2 is a transmembrane receptor which, when activated, signals complex downstream pathways responsible for cellular proliferation, dedifferentiation, and metastasis. In a recent multi-institutional analysis of early-stage UPSC, HER2 overexpression was identified among 25% of cases.4 Approximately 30% of cases of advanced disease manifest overexpression of this biomarker.5 HER2 overexpression (HER2-positive status) is significantly associated with higher rates of recurrence and mortality, even among patients treated with conventional therapies.3 Thus HER2-positive status is obviously an indicator of particularly aggressive disease.
Fortunately this particular biomarker is one for which we have established and developing therapeutics. The humanized monoclonal antibody, trastuzumab, has been highly effective in improving survival for HER2-positive breast cancer.6 More recently, it was studied in a phase 2 trial with carboplatin and paclitaxel chemotherapy for advanced or recurrent HER2-positive UPSC.5 This trial showed that the addition of this targeted therapy to conventional chemotherapy improved recurrence-free survival from 8 months to 12 months, and improved overall survival from 24.4 months to 29.6 months.5
One discovery leads to another treatment
This discovery led to the approval of trastuzumab to be used in addition to chemotherapy for advanced or recurrent disease.2 The most significant effects appear to be among those who have not received prior therapies, with a doubling of progression-free survival among these patients, and a more modest response among patients treated for recurrent, mostly pretreated disease.
Work currently is underway to explore an array of antibody or small-molecule blockades of HER2 in addition to vaccines against the protein or treatment with conjugate compounds in which an antibody to HER2 is paired with a cytotoxic drug able to be internalized into HER2-expressing cells.7 This represents a form of personalized medicine referred to as biomarker-driven targeted therapy, in which therapies are prescribed based on the expression of specific molecular markers (such as HER2 expression) typically in combination with other clinical markers such as surgical staging results, race, age, etc. These approaches can be very effective strategies in rare tumor subtypes with distinct molecular and clinical behaviors.
As previously mentioned, the targeting of HER2 overexpression with trastuzumab has been shown to be highly effective in the treatment of HER2-positive breast cancers where even patients with early-stage disease receive a multimodal therapy approach including antibody, chemotherapy, surgical, and often radiation treatments.6 We are moving towards a similar multimodal comprehensive treatment strategy for UPSC. If it is as successful as it is in breast cancer, it will be long overdue, and desperately necessary given the poor prognosis of this disease for all stages because of the inadequacies of current treatments strategies.
Routine testing of UPSC for HER2 expression is now a part of routine molecular substaging of uterine cancers in the same way we have embraced testing for microsatellite instability and hormone-receptor status. While a diagnosis of HER2 overexpression in UPSC portends a poor prognosis, patients can be reassured that treatment strategies exist that can target this malignant mechanism in advanced disease and more are under further development for early-stage disease.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Curr Opin Obstet Gynecol. 2010 Feb. doi: 10.1097/GCO.0b013e328334d8a3.
2. National Comprehensive Cancer Network. Uterine Neoplasms (version 2.2020).
3. Cancer 2005 Oct 1. doi: 10.1002/cncr.21308.
4. Gynecol Oncol 2020 doi: 10.1016/j.ygyno.2020.07.016.
5. J Clin Oncol 2018. doi: 10.1200/JCO.2017.76.5966.
6. N Engl J Med 2011. doi: 10.1056/NEJMoa0910383.
7. Discov Med. 2016 Apr;21(116):293-303.
New uterine compression technique controls postpartum hemorrhage
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
FROM OBSTETRICS & GYNECOLOGY
Does stirrup choice influence vaginal surgery outcome?
according to the first randomized controlled trial comparing both types of lithotomy stirrups.
“Participants positioned in candy cane stirrups had greater hip abduction than those positioned in boot stirrups, which could provide a rationale for our findings,” suggested Ankita Gupta, MD, MPH, of the University of Louisville (Ky.), and colleagues. Their report is in Obstetrics & Gynecology.
But one expert questions this interpretation, calling it a major limitation of the study.
“The only difference between the two arms of the study is associated with the angles between the femurs,” said Rosanne M. Kho, MD, a gynecologic surgeon at Cleveland Clinic, who was not involved in the study. “The difference of the angles at the femur is not inherent to the type of stirrup but in the method in which the patients were positioned using the two different types of stirrups,” she said. “The same wide angle between the femurs can be attained with the boot stirrups if the patient is not positioned properly. To determine if the same benefit in physical function is achieved with a lesser angle between the femur, the investigators should use only one type of stirrup (whether the candy cane or the boot stirrups) and change only the angles of the femur.”
The study was a single-masked, randomized controlled trial of women undergoing vaginal surgery at the University of Louisville’s division of urogynecology between March 2018 and Oct. 2019. Surgeries included any combination of vaginal hysterectomy, vaginal vault suspension (uterosacral or sacrospinous ligament fixation), vaginectomy (partial or total), mid-urethral slings, or other surgeries such as urethral diverticulectomy, fistula repair, or mesh excision.
Among the 138 women included in the intention-to-treat analysis, 72 were randomized to candy cane, and 66 to boot (Yellofin) stirrups. They were positioned in the assigned stirrup by the attending surgeon, with assistance from the surgical team, after administration of anesthesia and were not informed of their allocation until the end of the study at 6 weeks post surgery.
On day 1 post surgery, a 100-point visual analog scale (VAS) questionnaire was administered for pain in the lower back, hips, buttocks, thighs, knees, calves, and feet, followed by a series of questionnaires at 6 weeks post surgery, including the PROMIS (Patient-Reported Outcomes Measurement Information System) forms on physical function, pain intensity, and pain interference, as well as the Pelvic Floor Disability Index (PFDI-20) and the Patient Global Impression of Improvement forms.
While the authors acknowledged that neurologic injuries following vaginal surgery are rare, and therefore difficult to measure, physical function is a “prudent” alternative measurement.
Although the study was designed to compare lithotomy stirrups, patient positioning also was measured. Once the patient was anesthetized, the surgeon used a goniometer to measure flexion at the hip and knee joints, the angle of abduction and external rotation at the hip. The “angle between the femurs” was measured by placing the fulcrum of the goniometer at the anal opening.
While the angles of flexion at the hips and knees were similar between groups, the study found a significant difference between groups in the angle between the femurs (mean ± standard deviation, 88.7 ± 13.4 candy cane vs. 77.2 ± 13.3 boot, P < .01).
In addition, the primary outcome, change in physical function based on the PROMIS physical function shortform-20a, was significantly different between the two groups: While subjects in the candy cane group demonstrated a decline of 1.9 in mean physical function score at 6 weeks compared to baseline, those in the boot stirrup group showed an increase of 1.9 from baseline. The mean 6-week postoperative scores were 45.8 versus 49.8 for the candy cane and boot stirrup groups respectively (P < .01).
Although it was “well executed by a well-respected group of vaginal surgeons at a major academic institution,” the study has other limitations, noted Dr. Kho.
“Though the measurements were obtained with the goniometer at the beginning of the surgery, it does not appear that a repeat measurement was performed at the end of the case. Is it possible that positioning could have shifted and resulted in further change in the angle of the femur/hip/knees compared to the beginning of the surgery?” she asked.
In addition, “compared to the candy canes, the boot stirrup has bulky boots that could limit opportunities for bedside assistants who were standing next to the primary surgeon to lean against the patient’s thighs during the surgery. Were there measures done to ensure that assistants were not leaning against the [candy cane] patients?”
In terms of the 6-week outcome measure, Dr. Kho suggested PROMIS outcomes measured at 2 weeks and at 4 or 6 weeks “would have provided greater insight to the study question.
“The authors acknowledge that neuropathies due to patient positioning manifest soon after surgery and tend to be transient. Incidence of neuropathy is extremely low in both groups and is equivalent. Factors that could impair quick return to normal activity as a result of the neuromuscular effects due to patient positioning should have been measured earlier,” she suggested.
Finally, Dr. Kho noted that the authors “fail to provide any likely rationale for the impaired physical function measured at 6 weeks that can be attributed to the difference in the angles at the femur. The findings of decreased physical function at 6 weeks in the candy cane group may be incidental, and may be different if measured at an earlier time (which would be more pertinent for this study) or at a later time such as 3 months.”
Individual authors acknowledged personal funds from Society of Gynecologic Surgeons, Elsevier publishing, RBI Medical, and AMAG Pharmaceuticals. Dr. Kho had no relevant financial disclosures.
SOURCE: Gupta A et al. Obstet Gynecol. 2020 July 8. doi: 10.1097/AOG.0000000000003954.
according to the first randomized controlled trial comparing both types of lithotomy stirrups.
“Participants positioned in candy cane stirrups had greater hip abduction than those positioned in boot stirrups, which could provide a rationale for our findings,” suggested Ankita Gupta, MD, MPH, of the University of Louisville (Ky.), and colleagues. Their report is in Obstetrics & Gynecology.
But one expert questions this interpretation, calling it a major limitation of the study.
“The only difference between the two arms of the study is associated with the angles between the femurs,” said Rosanne M. Kho, MD, a gynecologic surgeon at Cleveland Clinic, who was not involved in the study. “The difference of the angles at the femur is not inherent to the type of stirrup but in the method in which the patients were positioned using the two different types of stirrups,” she said. “The same wide angle between the femurs can be attained with the boot stirrups if the patient is not positioned properly. To determine if the same benefit in physical function is achieved with a lesser angle between the femur, the investigators should use only one type of stirrup (whether the candy cane or the boot stirrups) and change only the angles of the femur.”
The study was a single-masked, randomized controlled trial of women undergoing vaginal surgery at the University of Louisville’s division of urogynecology between March 2018 and Oct. 2019. Surgeries included any combination of vaginal hysterectomy, vaginal vault suspension (uterosacral or sacrospinous ligament fixation), vaginectomy (partial or total), mid-urethral slings, or other surgeries such as urethral diverticulectomy, fistula repair, or mesh excision.
Among the 138 women included in the intention-to-treat analysis, 72 were randomized to candy cane, and 66 to boot (Yellofin) stirrups. They were positioned in the assigned stirrup by the attending surgeon, with assistance from the surgical team, after administration of anesthesia and were not informed of their allocation until the end of the study at 6 weeks post surgery.
On day 1 post surgery, a 100-point visual analog scale (VAS) questionnaire was administered for pain in the lower back, hips, buttocks, thighs, knees, calves, and feet, followed by a series of questionnaires at 6 weeks post surgery, including the PROMIS (Patient-Reported Outcomes Measurement Information System) forms on physical function, pain intensity, and pain interference, as well as the Pelvic Floor Disability Index (PFDI-20) and the Patient Global Impression of Improvement forms.
While the authors acknowledged that neurologic injuries following vaginal surgery are rare, and therefore difficult to measure, physical function is a “prudent” alternative measurement.
Although the study was designed to compare lithotomy stirrups, patient positioning also was measured. Once the patient was anesthetized, the surgeon used a goniometer to measure flexion at the hip and knee joints, the angle of abduction and external rotation at the hip. The “angle between the femurs” was measured by placing the fulcrum of the goniometer at the anal opening.
While the angles of flexion at the hips and knees were similar between groups, the study found a significant difference between groups in the angle between the femurs (mean ± standard deviation, 88.7 ± 13.4 candy cane vs. 77.2 ± 13.3 boot, P < .01).
In addition, the primary outcome, change in physical function based on the PROMIS physical function shortform-20a, was significantly different between the two groups: While subjects in the candy cane group demonstrated a decline of 1.9 in mean physical function score at 6 weeks compared to baseline, those in the boot stirrup group showed an increase of 1.9 from baseline. The mean 6-week postoperative scores were 45.8 versus 49.8 for the candy cane and boot stirrup groups respectively (P < .01).
Although it was “well executed by a well-respected group of vaginal surgeons at a major academic institution,” the study has other limitations, noted Dr. Kho.
“Though the measurements were obtained with the goniometer at the beginning of the surgery, it does not appear that a repeat measurement was performed at the end of the case. Is it possible that positioning could have shifted and resulted in further change in the angle of the femur/hip/knees compared to the beginning of the surgery?” she asked.
In addition, “compared to the candy canes, the boot stirrup has bulky boots that could limit opportunities for bedside assistants who were standing next to the primary surgeon to lean against the patient’s thighs during the surgery. Were there measures done to ensure that assistants were not leaning against the [candy cane] patients?”
In terms of the 6-week outcome measure, Dr. Kho suggested PROMIS outcomes measured at 2 weeks and at 4 or 6 weeks “would have provided greater insight to the study question.
“The authors acknowledge that neuropathies due to patient positioning manifest soon after surgery and tend to be transient. Incidence of neuropathy is extremely low in both groups and is equivalent. Factors that could impair quick return to normal activity as a result of the neuromuscular effects due to patient positioning should have been measured earlier,” she suggested.
Finally, Dr. Kho noted that the authors “fail to provide any likely rationale for the impaired physical function measured at 6 weeks that can be attributed to the difference in the angles at the femur. The findings of decreased physical function at 6 weeks in the candy cane group may be incidental, and may be different if measured at an earlier time (which would be more pertinent for this study) or at a later time such as 3 months.”
Individual authors acknowledged personal funds from Society of Gynecologic Surgeons, Elsevier publishing, RBI Medical, and AMAG Pharmaceuticals. Dr. Kho had no relevant financial disclosures.
SOURCE: Gupta A et al. Obstet Gynecol. 2020 July 8. doi: 10.1097/AOG.0000000000003954.
according to the first randomized controlled trial comparing both types of lithotomy stirrups.
“Participants positioned in candy cane stirrups had greater hip abduction than those positioned in boot stirrups, which could provide a rationale for our findings,” suggested Ankita Gupta, MD, MPH, of the University of Louisville (Ky.), and colleagues. Their report is in Obstetrics & Gynecology.
But one expert questions this interpretation, calling it a major limitation of the study.
“The only difference between the two arms of the study is associated with the angles between the femurs,” said Rosanne M. Kho, MD, a gynecologic surgeon at Cleveland Clinic, who was not involved in the study. “The difference of the angles at the femur is not inherent to the type of stirrup but in the method in which the patients were positioned using the two different types of stirrups,” she said. “The same wide angle between the femurs can be attained with the boot stirrups if the patient is not positioned properly. To determine if the same benefit in physical function is achieved with a lesser angle between the femur, the investigators should use only one type of stirrup (whether the candy cane or the boot stirrups) and change only the angles of the femur.”
The study was a single-masked, randomized controlled trial of women undergoing vaginal surgery at the University of Louisville’s division of urogynecology between March 2018 and Oct. 2019. Surgeries included any combination of vaginal hysterectomy, vaginal vault suspension (uterosacral or sacrospinous ligament fixation), vaginectomy (partial or total), mid-urethral slings, or other surgeries such as urethral diverticulectomy, fistula repair, or mesh excision.
Among the 138 women included in the intention-to-treat analysis, 72 were randomized to candy cane, and 66 to boot (Yellofin) stirrups. They were positioned in the assigned stirrup by the attending surgeon, with assistance from the surgical team, after administration of anesthesia and were not informed of their allocation until the end of the study at 6 weeks post surgery.
On day 1 post surgery, a 100-point visual analog scale (VAS) questionnaire was administered for pain in the lower back, hips, buttocks, thighs, knees, calves, and feet, followed by a series of questionnaires at 6 weeks post surgery, including the PROMIS (Patient-Reported Outcomes Measurement Information System) forms on physical function, pain intensity, and pain interference, as well as the Pelvic Floor Disability Index (PFDI-20) and the Patient Global Impression of Improvement forms.
While the authors acknowledged that neurologic injuries following vaginal surgery are rare, and therefore difficult to measure, physical function is a “prudent” alternative measurement.
Although the study was designed to compare lithotomy stirrups, patient positioning also was measured. Once the patient was anesthetized, the surgeon used a goniometer to measure flexion at the hip and knee joints, the angle of abduction and external rotation at the hip. The “angle between the femurs” was measured by placing the fulcrum of the goniometer at the anal opening.
While the angles of flexion at the hips and knees were similar between groups, the study found a significant difference between groups in the angle between the femurs (mean ± standard deviation, 88.7 ± 13.4 candy cane vs. 77.2 ± 13.3 boot, P < .01).
In addition, the primary outcome, change in physical function based on the PROMIS physical function shortform-20a, was significantly different between the two groups: While subjects in the candy cane group demonstrated a decline of 1.9 in mean physical function score at 6 weeks compared to baseline, those in the boot stirrup group showed an increase of 1.9 from baseline. The mean 6-week postoperative scores were 45.8 versus 49.8 for the candy cane and boot stirrup groups respectively (P < .01).
Although it was “well executed by a well-respected group of vaginal surgeons at a major academic institution,” the study has other limitations, noted Dr. Kho.
“Though the measurements were obtained with the goniometer at the beginning of the surgery, it does not appear that a repeat measurement was performed at the end of the case. Is it possible that positioning could have shifted and resulted in further change in the angle of the femur/hip/knees compared to the beginning of the surgery?” she asked.
In addition, “compared to the candy canes, the boot stirrup has bulky boots that could limit opportunities for bedside assistants who were standing next to the primary surgeon to lean against the patient’s thighs during the surgery. Were there measures done to ensure that assistants were not leaning against the [candy cane] patients?”
In terms of the 6-week outcome measure, Dr. Kho suggested PROMIS outcomes measured at 2 weeks and at 4 or 6 weeks “would have provided greater insight to the study question.
“The authors acknowledge that neuropathies due to patient positioning manifest soon after surgery and tend to be transient. Incidence of neuropathy is extremely low in both groups and is equivalent. Factors that could impair quick return to normal activity as a result of the neuromuscular effects due to patient positioning should have been measured earlier,” she suggested.
Finally, Dr. Kho noted that the authors “fail to provide any likely rationale for the impaired physical function measured at 6 weeks that can be attributed to the difference in the angles at the femur. The findings of decreased physical function at 6 weeks in the candy cane group may be incidental, and may be different if measured at an earlier time (which would be more pertinent for this study) or at a later time such as 3 months.”
Individual authors acknowledged personal funds from Society of Gynecologic Surgeons, Elsevier publishing, RBI Medical, and AMAG Pharmaceuticals. Dr. Kho had no relevant financial disclosures.
SOURCE: Gupta A et al. Obstet Gynecol. 2020 July 8. doi: 10.1097/AOG.0000000000003954.
FROM OBSTETRICS & GYNECOLOGY
Postpartum tubal ligation safe in obese women
Women with a high body mass index who request tubal ligation immediately post partum face no increased risk of complications, compared with normal-weight woman, according to a large, single-institution, retrospective study.
“Our study underscores the overall safety of postpartum tubal ligation among overweight and obese women,” John J. Byrne, MD, MPH, and colleagues at the University of Texas, Dallas, reported in Obstetrics & Gynecology.
“Even among women in the highest BMI category, this procedure is safe and effective,” they noted, despite previous studies identifying body mass index (BMI) higher than 40 kg/m2 “as a significant barrier to this procedure.”
“For the woman who is appropriately counseled and desires permanent contraception, BMI should not impede her access to the procedure,” Dr. Byrne and associates said.
The study included 3,670 women undergoing postpartum tubal ligation after a vaginal delivery between August 2015 and March 2019 at Parkland Hospital, which is operated by the Dallas County Hospital District.
The method used was the Parkland-type tubal ligation – a bilateral midsegment partial salpingectomy performed through a 2-3 cm infraumbilical incision. Women were excluded if they were planning additional surgery, such as ovarian cyst removal or hernia repair at the same time.
Comparing a composite outcome of surgical complications and subsequent pregnancies over a 5-year follow-up, the study found no differences across all maternal BMI categories, which were stratified as: underweight or normal weight (BMI, 24.9 or lower), overweight (25-29.9), class I obesity (30-34.9), class II obesity (35-39.9), and class III obesity (40 or higher).
A full breakdown of the composite morbidity included “blood transfusion, aborted procedure, intraoperative complications (bleeding requiring additional surgery, extension of incision), anesthetic complication (high spinal, bronchospasm, postdural puncture headaches requiring blood patch, and allergic reaction to anesthetic), postoperative complication (deep wound infection, venous thromboembolism, ileus, small bowel obstruction, acute intestinal herniation, peritonitis), return to operating room, incomplete transection of fallopian tube, and subsequent pregnancy,” they reported.
Among the study subjects, the mean BMI was 32.2, with 263 being underweight or normal weight at the time of admission, 1,044 being overweight, 1,371 having class I obesity, 689 having class II obesity, 303 having class III obesity, and 11 patients classified as supermorbidly obese (a BMI of 50 or higher).
Overall, “composite morbidity occurred in 49 (1.3%) women and was not significantly different across BMI categories (P = .07),” noted the authors.
More specifically, there were 19 (1.5%) composite morbidity events in the nonobese cohort and 30 (1.3%) in the obese cohort. “Even among women who had undergone prior abdominal surgery, there was no association of BMI with the rate of procedural complication,” Dr. Byrne and associates added.
The subsequent pregnancy rate was 1.63 per 1,000 procedures performed, which is “significantly lower than previously reported estimates,” they noted. In total, there were six subsequent pregnancies in the cohort: three full term, two ectopic, and one of unknown location.
“Although there was variability in operative time in all BMI categories, this is likely not clinically relevant as the range in operative time overlapped across groups,” reported the authors. “Other surgical metrics, such as estimated blood loss and length of hospitalization after tubal ligation, were found to be no different between BMI categories.”
Their findings “can be generalized to other tubal ligation forms, such as modified Pomeroy and even possibly salpingectomy, if the minilaparotomy incision is the same,” Dr. Byrne and colleagues suggested.
“This innovative study adds an important practical perspective to the literature on postpartum permanent contraception – a finding that should be reassuring for obstetrician/gynecologists,” commented Eve Espey, MD MPH, who was not involved in the research.
“Women with high BMI are significantly less likely to receive desired postvaginal delivery tubal ligation, compared to lower-BMI women, as documented in several prior studies,” said Dr. Espey, who is professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“Although those studies did not explore the reasons for nonfulfillment, intuitively concerns about complications or inability to complete the procedure are the most likely explanations,” she added.
“Although this study is limited by its retrospective nature, the smaller number of women in the highest BMI category, and lack of information on patients with unfulfilled requests for tubal ligation, it is overall well designed and should serve to encourage physicians to proceed with postvaginal delivery tubal ligation in patients across all BMI categories,” Dr. Espey concluded.
The study received no external funding; Dr. Byrne and associates reported no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News editorial advisory board, and said she has no relevant financial disclosures.
SOURCE: Byrne JJ et al. Obstet Gynecol. 2020;136:342-8.
Women with a high body mass index who request tubal ligation immediately post partum face no increased risk of complications, compared with normal-weight woman, according to a large, single-institution, retrospective study.
“Our study underscores the overall safety of postpartum tubal ligation among overweight and obese women,” John J. Byrne, MD, MPH, and colleagues at the University of Texas, Dallas, reported in Obstetrics & Gynecology.
“Even among women in the highest BMI category, this procedure is safe and effective,” they noted, despite previous studies identifying body mass index (BMI) higher than 40 kg/m2 “as a significant barrier to this procedure.”
“For the woman who is appropriately counseled and desires permanent contraception, BMI should not impede her access to the procedure,” Dr. Byrne and associates said.
The study included 3,670 women undergoing postpartum tubal ligation after a vaginal delivery between August 2015 and March 2019 at Parkland Hospital, which is operated by the Dallas County Hospital District.
The method used was the Parkland-type tubal ligation – a bilateral midsegment partial salpingectomy performed through a 2-3 cm infraumbilical incision. Women were excluded if they were planning additional surgery, such as ovarian cyst removal or hernia repair at the same time.
Comparing a composite outcome of surgical complications and subsequent pregnancies over a 5-year follow-up, the study found no differences across all maternal BMI categories, which were stratified as: underweight or normal weight (BMI, 24.9 or lower), overweight (25-29.9), class I obesity (30-34.9), class II obesity (35-39.9), and class III obesity (40 or higher).
A full breakdown of the composite morbidity included “blood transfusion, aborted procedure, intraoperative complications (bleeding requiring additional surgery, extension of incision), anesthetic complication (high spinal, bronchospasm, postdural puncture headaches requiring blood patch, and allergic reaction to anesthetic), postoperative complication (deep wound infection, venous thromboembolism, ileus, small bowel obstruction, acute intestinal herniation, peritonitis), return to operating room, incomplete transection of fallopian tube, and subsequent pregnancy,” they reported.
Among the study subjects, the mean BMI was 32.2, with 263 being underweight or normal weight at the time of admission, 1,044 being overweight, 1,371 having class I obesity, 689 having class II obesity, 303 having class III obesity, and 11 patients classified as supermorbidly obese (a BMI of 50 or higher).
Overall, “composite morbidity occurred in 49 (1.3%) women and was not significantly different across BMI categories (P = .07),” noted the authors.
More specifically, there were 19 (1.5%) composite morbidity events in the nonobese cohort and 30 (1.3%) in the obese cohort. “Even among women who had undergone prior abdominal surgery, there was no association of BMI with the rate of procedural complication,” Dr. Byrne and associates added.
The subsequent pregnancy rate was 1.63 per 1,000 procedures performed, which is “significantly lower than previously reported estimates,” they noted. In total, there were six subsequent pregnancies in the cohort: three full term, two ectopic, and one of unknown location.
“Although there was variability in operative time in all BMI categories, this is likely not clinically relevant as the range in operative time overlapped across groups,” reported the authors. “Other surgical metrics, such as estimated blood loss and length of hospitalization after tubal ligation, were found to be no different between BMI categories.”
Their findings “can be generalized to other tubal ligation forms, such as modified Pomeroy and even possibly salpingectomy, if the minilaparotomy incision is the same,” Dr. Byrne and colleagues suggested.
“This innovative study adds an important practical perspective to the literature on postpartum permanent contraception – a finding that should be reassuring for obstetrician/gynecologists,” commented Eve Espey, MD MPH, who was not involved in the research.
“Women with high BMI are significantly less likely to receive desired postvaginal delivery tubal ligation, compared to lower-BMI women, as documented in several prior studies,” said Dr. Espey, who is professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“Although those studies did not explore the reasons for nonfulfillment, intuitively concerns about complications or inability to complete the procedure are the most likely explanations,” she added.
“Although this study is limited by its retrospective nature, the smaller number of women in the highest BMI category, and lack of information on patients with unfulfilled requests for tubal ligation, it is overall well designed and should serve to encourage physicians to proceed with postvaginal delivery tubal ligation in patients across all BMI categories,” Dr. Espey concluded.
The study received no external funding; Dr. Byrne and associates reported no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News editorial advisory board, and said she has no relevant financial disclosures.
SOURCE: Byrne JJ et al. Obstet Gynecol. 2020;136:342-8.
Women with a high body mass index who request tubal ligation immediately post partum face no increased risk of complications, compared with normal-weight woman, according to a large, single-institution, retrospective study.
“Our study underscores the overall safety of postpartum tubal ligation among overweight and obese women,” John J. Byrne, MD, MPH, and colleagues at the University of Texas, Dallas, reported in Obstetrics & Gynecology.
“Even among women in the highest BMI category, this procedure is safe and effective,” they noted, despite previous studies identifying body mass index (BMI) higher than 40 kg/m2 “as a significant barrier to this procedure.”
“For the woman who is appropriately counseled and desires permanent contraception, BMI should not impede her access to the procedure,” Dr. Byrne and associates said.
The study included 3,670 women undergoing postpartum tubal ligation after a vaginal delivery between August 2015 and March 2019 at Parkland Hospital, which is operated by the Dallas County Hospital District.
The method used was the Parkland-type tubal ligation – a bilateral midsegment partial salpingectomy performed through a 2-3 cm infraumbilical incision. Women were excluded if they were planning additional surgery, such as ovarian cyst removal or hernia repair at the same time.
Comparing a composite outcome of surgical complications and subsequent pregnancies over a 5-year follow-up, the study found no differences across all maternal BMI categories, which were stratified as: underweight or normal weight (BMI, 24.9 or lower), overweight (25-29.9), class I obesity (30-34.9), class II obesity (35-39.9), and class III obesity (40 or higher).
A full breakdown of the composite morbidity included “blood transfusion, aborted procedure, intraoperative complications (bleeding requiring additional surgery, extension of incision), anesthetic complication (high spinal, bronchospasm, postdural puncture headaches requiring blood patch, and allergic reaction to anesthetic), postoperative complication (deep wound infection, venous thromboembolism, ileus, small bowel obstruction, acute intestinal herniation, peritonitis), return to operating room, incomplete transection of fallopian tube, and subsequent pregnancy,” they reported.
Among the study subjects, the mean BMI was 32.2, with 263 being underweight or normal weight at the time of admission, 1,044 being overweight, 1,371 having class I obesity, 689 having class II obesity, 303 having class III obesity, and 11 patients classified as supermorbidly obese (a BMI of 50 or higher).
Overall, “composite morbidity occurred in 49 (1.3%) women and was not significantly different across BMI categories (P = .07),” noted the authors.
More specifically, there were 19 (1.5%) composite morbidity events in the nonobese cohort and 30 (1.3%) in the obese cohort. “Even among women who had undergone prior abdominal surgery, there was no association of BMI with the rate of procedural complication,” Dr. Byrne and associates added.
The subsequent pregnancy rate was 1.63 per 1,000 procedures performed, which is “significantly lower than previously reported estimates,” they noted. In total, there were six subsequent pregnancies in the cohort: three full term, two ectopic, and one of unknown location.
“Although there was variability in operative time in all BMI categories, this is likely not clinically relevant as the range in operative time overlapped across groups,” reported the authors. “Other surgical metrics, such as estimated blood loss and length of hospitalization after tubal ligation, were found to be no different between BMI categories.”
Their findings “can be generalized to other tubal ligation forms, such as modified Pomeroy and even possibly salpingectomy, if the minilaparotomy incision is the same,” Dr. Byrne and colleagues suggested.
“This innovative study adds an important practical perspective to the literature on postpartum permanent contraception – a finding that should be reassuring for obstetrician/gynecologists,” commented Eve Espey, MD MPH, who was not involved in the research.
“Women with high BMI are significantly less likely to receive desired postvaginal delivery tubal ligation, compared to lower-BMI women, as documented in several prior studies,” said Dr. Espey, who is professor and chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque.
“Although those studies did not explore the reasons for nonfulfillment, intuitively concerns about complications or inability to complete the procedure are the most likely explanations,” she added.
“Although this study is limited by its retrospective nature, the smaller number of women in the highest BMI category, and lack of information on patients with unfulfilled requests for tubal ligation, it is overall well designed and should serve to encourage physicians to proceed with postvaginal delivery tubal ligation in patients across all BMI categories,” Dr. Espey concluded.
The study received no external funding; Dr. Byrne and associates reported no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News editorial advisory board, and said she has no relevant financial disclosures.
SOURCE: Byrne JJ et al. Obstet Gynecol. 2020;136:342-8.
FROM OBSTETRICS & GYNECOLOGY
How often does risk-reducing salpingo-oophorectomy identify cancer?
Among women with BRCA mutations who underwent risk-reducing bilateral salpingo-oophorectomy, the procedure led to a cancer diagnosis in 3%, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Of 269 patients, 8 (3%) received a cancer diagnosis. In five cases, the cancer was diagnosed on final pathology, and three had immediate conversion to staging.
The data suggest that gynecologists as well as gynecologic oncologists may perform the procedure, but gynecologists may be less likely to obtain pelvic washings in accordance with guidelines for this indication.
said study author Coralee Toal, MD, of UPMC Magee-Womans Hospital in Pittsburgh. “It is often a diagnosis that is found at the time of pathology, so the initial procedure would not have been changed either way.”
Still, doctors who perform the procedure should follow recommended practices such as obtaining pelvic washings and identifying patients for the procedure within target age ranges, Dr. Toal said.
BRCA1 and BRCA2 mutations confer an increased risk of ovarian and breast cancer, but there is no effective form of ovarian cancer screening. Women with a known mutation may have a bilateral salpingo-oophorectomy to reduce the risk of cancer. The recommended age range for the procedure is 35-40 years for women with BRCA1 mutations and 40-45 years for women with BRCA2 mutations.
When the procedure is performed for this indication, various recommendations apply that may differ from those when the procedure is performed under different circumstances.
During risk-reducing bilateral salpingo-oophorectomy, the surgeon should thoroughly evaluate the abdominal cavity, obtain pelvic washings for cytology, remove at least 2 cm of the infundibulopelvic ligament, and divide the fallopian tube at the uterine cornua.
To assess the incidence of occult ovarian cancer at the time of risk-reducing bilateral salpingo-oophorectomy and surgeon adherence to recommended practices, Dr. Toal and colleagues performed a retrospective chart review.
They included patients who had a known BRCA mutation and underwent a risk-reducing bilateral salpingo-oophorectomy between July 2007 and September 2018. They excluded patients who had a suspicious adnexal mass before the procedure but not a known diagnosis, as well as patients with another malignancy or genetic syndrome.
The researchers evaluated adherence to recommendations by reviewing operative reports.
In all, they reviewed data from 269 patients. In 220 cases, a gynecologic oncologist performed the procedure, and in 49 cases a gynecologist performed the procedure.
Patients tended to be older than would be expected, said Dr. Toal. Patients with BRCA1 mutations had an average age of 46 years, and patients with BRCA2 mutations had an average age of 49 years.
Patients who received a cancer diagnosis were significantly older on average, compared with the other patients: 58 years versus 48 years.
Pelvic washings were performed during 95% of the procedures performed by a gynecologic oncologist, compared with 63% of the procedures performed by a gynecologist. In addition, patients who had the procedure performed by a gynecologist were significantly older than those who had the procedure performed by a gynecologic oncologist (49 vs. 47 years).
Miles Murphy, MD, president of the Society of Gynecologic Surgeons, asked how doctors should weigh the possibility of risk-reducing oophorectomy at the time of benign hysterectomy in patients without a family history of female cancer.
It could be that genetic testing would be appropriate for some of those patients, Dr. Toal said. It is “important to take a thorough family history to make sure that you are identifying anybody who may benefit from genetic counseling and genetic testing, where you might identify an otherwise not known mutation prior to an otherwise benign or routine surgery,” Dr. Toal said. “Then you would have the opportunity to perform this.”
For patients without known mutations, however, “we do know the benefit of ovaries remaining in situ ... including cardiac health,” she said. “You have to remember that people can die of a broken hip as well. The risk of osteoporosis and those things is not zero and in fact may be much higher than their ovarian cancer risk.”
One of the study authors is a surgeon educator for Covidien and Medtronic.
SOURCE: Newcomb LK et al. SGS 2020, Abstract 18.
Among women with BRCA mutations who underwent risk-reducing bilateral salpingo-oophorectomy, the procedure led to a cancer diagnosis in 3%, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Of 269 patients, 8 (3%) received a cancer diagnosis. In five cases, the cancer was diagnosed on final pathology, and three had immediate conversion to staging.
The data suggest that gynecologists as well as gynecologic oncologists may perform the procedure, but gynecologists may be less likely to obtain pelvic washings in accordance with guidelines for this indication.
said study author Coralee Toal, MD, of UPMC Magee-Womans Hospital in Pittsburgh. “It is often a diagnosis that is found at the time of pathology, so the initial procedure would not have been changed either way.”
Still, doctors who perform the procedure should follow recommended practices such as obtaining pelvic washings and identifying patients for the procedure within target age ranges, Dr. Toal said.
BRCA1 and BRCA2 mutations confer an increased risk of ovarian and breast cancer, but there is no effective form of ovarian cancer screening. Women with a known mutation may have a bilateral salpingo-oophorectomy to reduce the risk of cancer. The recommended age range for the procedure is 35-40 years for women with BRCA1 mutations and 40-45 years for women with BRCA2 mutations.
When the procedure is performed for this indication, various recommendations apply that may differ from those when the procedure is performed under different circumstances.
During risk-reducing bilateral salpingo-oophorectomy, the surgeon should thoroughly evaluate the abdominal cavity, obtain pelvic washings for cytology, remove at least 2 cm of the infundibulopelvic ligament, and divide the fallopian tube at the uterine cornua.
To assess the incidence of occult ovarian cancer at the time of risk-reducing bilateral salpingo-oophorectomy and surgeon adherence to recommended practices, Dr. Toal and colleagues performed a retrospective chart review.
They included patients who had a known BRCA mutation and underwent a risk-reducing bilateral salpingo-oophorectomy between July 2007 and September 2018. They excluded patients who had a suspicious adnexal mass before the procedure but not a known diagnosis, as well as patients with another malignancy or genetic syndrome.
The researchers evaluated adherence to recommendations by reviewing operative reports.
In all, they reviewed data from 269 patients. In 220 cases, a gynecologic oncologist performed the procedure, and in 49 cases a gynecologist performed the procedure.
Patients tended to be older than would be expected, said Dr. Toal. Patients with BRCA1 mutations had an average age of 46 years, and patients with BRCA2 mutations had an average age of 49 years.
Patients who received a cancer diagnosis were significantly older on average, compared with the other patients: 58 years versus 48 years.
Pelvic washings were performed during 95% of the procedures performed by a gynecologic oncologist, compared with 63% of the procedures performed by a gynecologist. In addition, patients who had the procedure performed by a gynecologist were significantly older than those who had the procedure performed by a gynecologic oncologist (49 vs. 47 years).
Miles Murphy, MD, president of the Society of Gynecologic Surgeons, asked how doctors should weigh the possibility of risk-reducing oophorectomy at the time of benign hysterectomy in patients without a family history of female cancer.
It could be that genetic testing would be appropriate for some of those patients, Dr. Toal said. It is “important to take a thorough family history to make sure that you are identifying anybody who may benefit from genetic counseling and genetic testing, where you might identify an otherwise not known mutation prior to an otherwise benign or routine surgery,” Dr. Toal said. “Then you would have the opportunity to perform this.”
For patients without known mutations, however, “we do know the benefit of ovaries remaining in situ ... including cardiac health,” she said. “You have to remember that people can die of a broken hip as well. The risk of osteoporosis and those things is not zero and in fact may be much higher than their ovarian cancer risk.”
One of the study authors is a surgeon educator for Covidien and Medtronic.
SOURCE: Newcomb LK et al. SGS 2020, Abstract 18.
Among women with BRCA mutations who underwent risk-reducing bilateral salpingo-oophorectomy, the procedure led to a cancer diagnosis in 3%, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Of 269 patients, 8 (3%) received a cancer diagnosis. In five cases, the cancer was diagnosed on final pathology, and three had immediate conversion to staging.
The data suggest that gynecologists as well as gynecologic oncologists may perform the procedure, but gynecologists may be less likely to obtain pelvic washings in accordance with guidelines for this indication.
said study author Coralee Toal, MD, of UPMC Magee-Womans Hospital in Pittsburgh. “It is often a diagnosis that is found at the time of pathology, so the initial procedure would not have been changed either way.”
Still, doctors who perform the procedure should follow recommended practices such as obtaining pelvic washings and identifying patients for the procedure within target age ranges, Dr. Toal said.
BRCA1 and BRCA2 mutations confer an increased risk of ovarian and breast cancer, but there is no effective form of ovarian cancer screening. Women with a known mutation may have a bilateral salpingo-oophorectomy to reduce the risk of cancer. The recommended age range for the procedure is 35-40 years for women with BRCA1 mutations and 40-45 years for women with BRCA2 mutations.
When the procedure is performed for this indication, various recommendations apply that may differ from those when the procedure is performed under different circumstances.
During risk-reducing bilateral salpingo-oophorectomy, the surgeon should thoroughly evaluate the abdominal cavity, obtain pelvic washings for cytology, remove at least 2 cm of the infundibulopelvic ligament, and divide the fallopian tube at the uterine cornua.
To assess the incidence of occult ovarian cancer at the time of risk-reducing bilateral salpingo-oophorectomy and surgeon adherence to recommended practices, Dr. Toal and colleagues performed a retrospective chart review.
They included patients who had a known BRCA mutation and underwent a risk-reducing bilateral salpingo-oophorectomy between July 2007 and September 2018. They excluded patients who had a suspicious adnexal mass before the procedure but not a known diagnosis, as well as patients with another malignancy or genetic syndrome.
The researchers evaluated adherence to recommendations by reviewing operative reports.
In all, they reviewed data from 269 patients. In 220 cases, a gynecologic oncologist performed the procedure, and in 49 cases a gynecologist performed the procedure.
Patients tended to be older than would be expected, said Dr. Toal. Patients with BRCA1 mutations had an average age of 46 years, and patients with BRCA2 mutations had an average age of 49 years.
Patients who received a cancer diagnosis were significantly older on average, compared with the other patients: 58 years versus 48 years.
Pelvic washings were performed during 95% of the procedures performed by a gynecologic oncologist, compared with 63% of the procedures performed by a gynecologist. In addition, patients who had the procedure performed by a gynecologist were significantly older than those who had the procedure performed by a gynecologic oncologist (49 vs. 47 years).
Miles Murphy, MD, president of the Society of Gynecologic Surgeons, asked how doctors should weigh the possibility of risk-reducing oophorectomy at the time of benign hysterectomy in patients without a family history of female cancer.
It could be that genetic testing would be appropriate for some of those patients, Dr. Toal said. It is “important to take a thorough family history to make sure that you are identifying anybody who may benefit from genetic counseling and genetic testing, where you might identify an otherwise not known mutation prior to an otherwise benign or routine surgery,” Dr. Toal said. “Then you would have the opportunity to perform this.”
For patients without known mutations, however, “we do know the benefit of ovaries remaining in situ ... including cardiac health,” she said. “You have to remember that people can die of a broken hip as well. The risk of osteoporosis and those things is not zero and in fact may be much higher than their ovarian cancer risk.”
One of the study authors is a surgeon educator for Covidien and Medtronic.
SOURCE: Newcomb LK et al. SGS 2020, Abstract 18.
FROM SGS 2020
Range of interventions reduces likelihood of infection after hysterectomy
Improving hand hygiene, optimizing antibiotic order sets, and removing catheters sooner were among the interventions associated with a decreased risk of infections after hysterectomy, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
“Implementation of said study author Shitanshu Uppal, MBBS, an ob.gyn. specializing in gynecologic oncology at the University of Michigan in Ann Arbor.
To assess the impact of quality improvement efforts on infectious morbidity after hysterectomy, Dr. Uppal and colleagues analyzed data from 1,867 hysterectomies performed between Oct. 8, 2015, and Oct. 7, 2018. Patients were at least 18 years old, younger than 90 years old, and underwent hysterectomy via any route at the University of Michigan Medical Center Hospital.
Interventions to reduce infections included the use of cefazolin as a preferred antibiotic, the addition of metronidazole to first-generation cephalosporins for antibiotic prophylaxis, subcuticular closure of open incisions, and earlier removal of Foley catheters. In addition, the institution evaluated and shared information about doctors’ hand hygiene, implemented enhanced recovery after surgery (ERAS) protocols, and held periodic meetings with doctors to discuss efforts to reduce infections. Most interventions were implemented by November 2017.
The primary outcome was overall infection rate in the 30 days after surgery for each of the 3 years included the study. Infections included superficial surgical site infections, deep infections, Clostridium difficile infections, and urinary tract infections, among others.
Patients’ baseline clinical characteristics did not differ during the 3 years studied. Length of stay decreased, which may be attributed to increased use of ERAS protocols and institution of same-day discharge in laparoscopic cases, Dr. Uppal said. The rate of malignancy on final pathology decreased from 29% in year 1 to 23% in year 3. The rate of laparoscopic surgery increased from 55% to 64%.
Infectious morbidity rates decreased from 7% in year 1 (47 infections per 644 cases) to 4% in year 3 (22 infections per 616 cases).
“We saw a reduction in infection rate in all categories,” said Dr. Uppal. “However, the reduction in urinary tract infection as well as superficial surgical site infection was most pronounced.”
After adjustment for the route of surgery, body mass index, age, malignancy on final pathology, modality of surgery, and comorbidities, performance of hysterectomy in year 3 was independently predictive of lower rates of infectious morbidity by 56%.
In addition, the standardized incidence ratio for surgical site infection as reported by the Centers for Medicare & Medicaid Services decreased. In December 2016, Michigan Medicine’s ratio was 1.057. At the end of 2018, the projected ratio was 0.243.
The interventions started on different dates, and “we are unable to conclude, from all the implemented interventions, which one worked,” Dr. Uppal noted.
“I hope the elements from this quality improvement initiative will become the standard of care in order to benefit our patients,” said Amy Park, MD, section head of female pelvic medicine and reconstructive surgery at Cleveland Clinic.
In addition, the study “pertains to one of CMS’s major programs to reduce and prevent health care-associated infections,” Dr. Park said at the virtual meeting. Several CMS quality indicators in 2020 relate to gynecologic surgery, including postoperative wound dehiscence rate, catheter-related UTI rate, and surgical site infection related to hysterectomy. The CMS will reduce hospital payments to institutions in the worst performing quartile for hospital-acquired infection scores by 1%.
Dr. Uppal advised that hospitals need four things to achieve similar results: a commitment from the team and leadership to reduce infections; patience; making it easy for doctors to implement the new interventions; and periodic feedback.
The process may be tedious but worth it in the end, he said.
Dr. Uppal disclosed salary support from Blue Cross Blue Shield of Michigan. A coauthor disclosed salary support from the company plus royalties from UpToDate. Dr. Park disclosed speaking for Allergan and royalties from UpToDate.
SOURCE: Uppal S et al. SGS 2020, Abstract 16.
Improving hand hygiene, optimizing antibiotic order sets, and removing catheters sooner were among the interventions associated with a decreased risk of infections after hysterectomy, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
“Implementation of said study author Shitanshu Uppal, MBBS, an ob.gyn. specializing in gynecologic oncology at the University of Michigan in Ann Arbor.
To assess the impact of quality improvement efforts on infectious morbidity after hysterectomy, Dr. Uppal and colleagues analyzed data from 1,867 hysterectomies performed between Oct. 8, 2015, and Oct. 7, 2018. Patients were at least 18 years old, younger than 90 years old, and underwent hysterectomy via any route at the University of Michigan Medical Center Hospital.
Interventions to reduce infections included the use of cefazolin as a preferred antibiotic, the addition of metronidazole to first-generation cephalosporins for antibiotic prophylaxis, subcuticular closure of open incisions, and earlier removal of Foley catheters. In addition, the institution evaluated and shared information about doctors’ hand hygiene, implemented enhanced recovery after surgery (ERAS) protocols, and held periodic meetings with doctors to discuss efforts to reduce infections. Most interventions were implemented by November 2017.
The primary outcome was overall infection rate in the 30 days after surgery for each of the 3 years included the study. Infections included superficial surgical site infections, deep infections, Clostridium difficile infections, and urinary tract infections, among others.
Patients’ baseline clinical characteristics did not differ during the 3 years studied. Length of stay decreased, which may be attributed to increased use of ERAS protocols and institution of same-day discharge in laparoscopic cases, Dr. Uppal said. The rate of malignancy on final pathology decreased from 29% in year 1 to 23% in year 3. The rate of laparoscopic surgery increased from 55% to 64%.
Infectious morbidity rates decreased from 7% in year 1 (47 infections per 644 cases) to 4% in year 3 (22 infections per 616 cases).
“We saw a reduction in infection rate in all categories,” said Dr. Uppal. “However, the reduction in urinary tract infection as well as superficial surgical site infection was most pronounced.”
After adjustment for the route of surgery, body mass index, age, malignancy on final pathology, modality of surgery, and comorbidities, performance of hysterectomy in year 3 was independently predictive of lower rates of infectious morbidity by 56%.
In addition, the standardized incidence ratio for surgical site infection as reported by the Centers for Medicare & Medicaid Services decreased. In December 2016, Michigan Medicine’s ratio was 1.057. At the end of 2018, the projected ratio was 0.243.
The interventions started on different dates, and “we are unable to conclude, from all the implemented interventions, which one worked,” Dr. Uppal noted.
“I hope the elements from this quality improvement initiative will become the standard of care in order to benefit our patients,” said Amy Park, MD, section head of female pelvic medicine and reconstructive surgery at Cleveland Clinic.
In addition, the study “pertains to one of CMS’s major programs to reduce and prevent health care-associated infections,” Dr. Park said at the virtual meeting. Several CMS quality indicators in 2020 relate to gynecologic surgery, including postoperative wound dehiscence rate, catheter-related UTI rate, and surgical site infection related to hysterectomy. The CMS will reduce hospital payments to institutions in the worst performing quartile for hospital-acquired infection scores by 1%.
Dr. Uppal advised that hospitals need four things to achieve similar results: a commitment from the team and leadership to reduce infections; patience; making it easy for doctors to implement the new interventions; and periodic feedback.
The process may be tedious but worth it in the end, he said.
Dr. Uppal disclosed salary support from Blue Cross Blue Shield of Michigan. A coauthor disclosed salary support from the company plus royalties from UpToDate. Dr. Park disclosed speaking for Allergan and royalties from UpToDate.
SOURCE: Uppal S et al. SGS 2020, Abstract 16.
Improving hand hygiene, optimizing antibiotic order sets, and removing catheters sooner were among the interventions associated with a decreased risk of infections after hysterectomy, according to research presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
“Implementation of said study author Shitanshu Uppal, MBBS, an ob.gyn. specializing in gynecologic oncology at the University of Michigan in Ann Arbor.
To assess the impact of quality improvement efforts on infectious morbidity after hysterectomy, Dr. Uppal and colleagues analyzed data from 1,867 hysterectomies performed between Oct. 8, 2015, and Oct. 7, 2018. Patients were at least 18 years old, younger than 90 years old, and underwent hysterectomy via any route at the University of Michigan Medical Center Hospital.
Interventions to reduce infections included the use of cefazolin as a preferred antibiotic, the addition of metronidazole to first-generation cephalosporins for antibiotic prophylaxis, subcuticular closure of open incisions, and earlier removal of Foley catheters. In addition, the institution evaluated and shared information about doctors’ hand hygiene, implemented enhanced recovery after surgery (ERAS) protocols, and held periodic meetings with doctors to discuss efforts to reduce infections. Most interventions were implemented by November 2017.
The primary outcome was overall infection rate in the 30 days after surgery for each of the 3 years included the study. Infections included superficial surgical site infections, deep infections, Clostridium difficile infections, and urinary tract infections, among others.
Patients’ baseline clinical characteristics did not differ during the 3 years studied. Length of stay decreased, which may be attributed to increased use of ERAS protocols and institution of same-day discharge in laparoscopic cases, Dr. Uppal said. The rate of malignancy on final pathology decreased from 29% in year 1 to 23% in year 3. The rate of laparoscopic surgery increased from 55% to 64%.
Infectious morbidity rates decreased from 7% in year 1 (47 infections per 644 cases) to 4% in year 3 (22 infections per 616 cases).
“We saw a reduction in infection rate in all categories,” said Dr. Uppal. “However, the reduction in urinary tract infection as well as superficial surgical site infection was most pronounced.”
After adjustment for the route of surgery, body mass index, age, malignancy on final pathology, modality of surgery, and comorbidities, performance of hysterectomy in year 3 was independently predictive of lower rates of infectious morbidity by 56%.
In addition, the standardized incidence ratio for surgical site infection as reported by the Centers for Medicare & Medicaid Services decreased. In December 2016, Michigan Medicine’s ratio was 1.057. At the end of 2018, the projected ratio was 0.243.
The interventions started on different dates, and “we are unable to conclude, from all the implemented interventions, which one worked,” Dr. Uppal noted.
“I hope the elements from this quality improvement initiative will become the standard of care in order to benefit our patients,” said Amy Park, MD, section head of female pelvic medicine and reconstructive surgery at Cleveland Clinic.
In addition, the study “pertains to one of CMS’s major programs to reduce and prevent health care-associated infections,” Dr. Park said at the virtual meeting. Several CMS quality indicators in 2020 relate to gynecologic surgery, including postoperative wound dehiscence rate, catheter-related UTI rate, and surgical site infection related to hysterectomy. The CMS will reduce hospital payments to institutions in the worst performing quartile for hospital-acquired infection scores by 1%.
Dr. Uppal advised that hospitals need four things to achieve similar results: a commitment from the team and leadership to reduce infections; patience; making it easy for doctors to implement the new interventions; and periodic feedback.
The process may be tedious but worth it in the end, he said.
Dr. Uppal disclosed salary support from Blue Cross Blue Shield of Michigan. A coauthor disclosed salary support from the company plus royalties from UpToDate. Dr. Park disclosed speaking for Allergan and royalties from UpToDate.
SOURCE: Uppal S et al. SGS 2020, Abstract 16.
FROM SGS 2020