User login
CD4 Counts Predict Chemo Response in Laryngeal Cancer
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
PHOENIX – Pretreatment CD4 levels predicted response to induction chemotherapy among 97 patients with advanced laryngeal cancer, but not for 66 patients with advanced oropharyngeal cancer, according to a retrospective analysis of data from two clinical trials.
The two groups of head and neck cancer patients were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation, in which tumor response after one cycle of cisplatin and 5-fluorouracil was used to select those who would undergo surgery or definitive chemoradiation (J. Clin. Oncol. 2006;24:593-8 in laryngeal cancer; J. Clin. Oncol. 2008;26:3138-46 in oropharyngeal cancer).
Several lymphocyte subsets were measured before treatment via routine flow cytometry in peripheral blood in the laryngeal cancer patients, but only CD4 (helper cell) levels were significantly associated with chemotherapy response. Both absolute CD4 counts and CD4 percentages were higher among induction chemotherapy responders than nonresponders (P = .006 and P = .04, respectively).
Investigators also saw a trend for responders to have an increased percentage of CD3 cells (P = .13), decreased percentage of CD8 cells (P = .11), and higher CD4/CD8 ratios.
"Host immune parameters are important factors in treatment outcome, and may be useful in identifying subsets of patients with cancers that are responsive to organ-preserving therapy," said Dr. Gregory T. Wolf, who presented the data at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
"It is likely that immunobiology of head and neck cancers differ significantly by tumor site and predisposing factors," added Dr. Wolf, a professor in the department of otolaryngology at the University of Michigan, Ann Arbor.
The median length of follow-up in the two studies was 7.9 years for the patients with laryngeal cancer and 6.6 years for those with cancer of the oropharynx. Disease-free survival was 86% at 3 years and 82% at 5 years for laryngeal cancer, and 78% at 3 years and 76% at 4 years for oropharyngeal cancer. The proportions responding to induction chemotherapy were 75% in the laryngeal cancer trial and 82% in the oropharyngeal cancer study.
In an interview, Dr. Wolf said that having two identical treatment trials provided an opportunity to determine whether correlations of pretreatment CD4 levels with chemoresponse differed by tumor site. When the laryngeal and oropharyngeal cancer patient groups were combined, higher CD4 levels were still associated with response, but this was primarily because of the strong correlation among the larynx cancer patients.
Statistical regression testing determined that for patients with oropharyngeal cancer, CD8 cells were more closely associated with chemotherapy response, but the relationship was not as strong as the strong correlation of CD4 levels among laryngeal cancer patients.
There was a trend toward improved survival by both CD4 percentage (P = .36) and absolute CD4 count (P = .15) in the laryngeal cohort, but not in the oropharyngeal cohort. None of the other lymphocyte subsets predicted survival in either group, Dr. Wolf said.
Results for the oropharyngeal cancer patients were further stratified by human papillomavirus status, and were combined with the laryngeal cancer group. Both lower CD4/CD8 ratio and higher CD8 levels were consistent with better prognosis among patients who were HPV positive (P = .02 and P = .06, respectively).
"We combined the results to get the largest sample size and [to see] if the relationship was independent of tumor site, since the biology of these cancers is so different. It was remarkable that the prediction differed by tumor site, with CD4 cells being predictive for larynx and CD8 cells predictive for oropharynx," Dr. Wolf explained in an interview. This finding likely reflects the major biological differences between these cancers, and is why it was important to also include HPV status, he added.
Dr. Wolf is a consultant for IRX Therapeutics, Inc.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Among laryngeal cancer patients, both absolute and percent CD4 counts were significantly higher among responders to induction chemotherapy than in nonresponders (P = .006 and P = .04, respectively).
Data Source: The data come from a retrospective analysis of head and neck cancer patients who were enrolled in two identical prospective, phase II trials of induction chemotherapy and organ preservation.
Disclosures: Dr. Wolf is a consultant for IRX Therapeutics.
Infrared Imaging Eyes Mucositis After Head & Neck Radiation
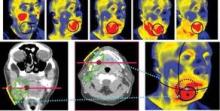
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
PHOENIX – Thermal imaging was able to detect small and early changes in the temperature of mucosal surfaces – a possible predictor of the development of mucositis – among 34 patients who were treated with chemoradiotherapy for locally advanced squamous cell carcinoma of the head and neck.
"Detection of these early changes using sensitive thermal imaging technology would allow identification of patients who will require more intensive supportive care," said Dr. Ezra Cohen, who presented the pilot study at the head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
Radiotherapy-associated mucositis manifests initially as erythematous areas in the treatment field, which are accompanied by an intense inflammatory response histologically. Thus, Dr. Cohen and his associates had hypothesized that patients destined to display severe mucocutaneous toxicity would demonstrate greater alterations in thermal intensity early in therapy, compared with identically treated counterparts who do not subsequently develop the toxicity.
The researchers further hypothesized that they could measure those changes with infrared thermal imaging, a noninvasive technique that allows visualization and quantification of changes in skin or mucosal surface temperature.
The 34 patients (28 male, mean age 58 years) in the pilot study were treated with identical chemoradiotherapy regimens of 5-fluorouracil and hydroxyurea with a median radiation dose of 74 Gy for cancers of the oral cavity or oropharynx.
Using a portable device developed at Argonne National Laboratory in Illinois, the investigators conducted noninvasive baseline and weekly thermal imaging. The device detects infrared light naturally emitted from the skin or mucosal surface and generates an electrical signal, which is amplified and converted into digital data flow that is visualized in color on a monitor.
Grade 3 mucositis based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events v3.0 was observed in 53% of the patients, and dermatitis in 21%. All patients displayed an increase in temperature within the radiation field.
Investigators charted a statistically significant positive association between an early rise in temperature in oral mucous membranes when compared with a reference area and mucositis grade (P = .03). For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis grade, reported Dr. Cohen, codirector of the head and neck cancer program at the University of Chicago.
Mucositis and its clinical sequelae are consistently reported as the most clinically significant acute toxicity in the treatment of locally advanced squamous cell carcinoma of the head and neck with chemoradiotherapy, according to Dr. Cohen, who also chaired the meeting. Patient to patient variability in mucositis is related to radiotherapy dosing, fractionation, and volumes, but there also appear to be individual differences in "normal tissue tolerance," even among patients on the same treatment regimen, he said.
"Larger studies with greater dynamic ranges in mucositis scoring are warranted to evaluate whether this tool can help predict which patients would be in need of early intervention to prevent acute complications," he said.
The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: For every 1 C increase in temperature, compared with the reference (temperature near the medial angle of one eye), there was a 0.157 increase in average subsequent mucositis.
Data Source: Data come from a pilot study of functional infrared imaging in 34 patients with locally advanced head and neck cancer who were treated with chemoradiotherapy.
Disclosures: The study was funded by the National Institutes of Health and the University of Chicago Comprehensive Cancer Center. Dr. Cohen and his associates said they had no relevant financial disclosures.
Palliation Trumps PET in Prolonging Head & Neck Cancer Survival
MIAMI BEACH – Using PET scans to diagnose distant metastasis in patients with advanced head and neck squamous cell carcinoma does not significantly prolong life expectancy, compared with other imaging techniques, according to a retrospective study.
Palliative chemotherapy did make a difference, however, significantly increasing life expectancy by 215 days in patients who received it, Dr. Matthew E. Spector and colleagues from the University of Michigan, Ann Arbor, reported at a meeting of the Triological Society.
"Over 90% of patients at University of Michigan have at least one PET scan at some point in their treatment," Dr. Spector said. Increased sensitivity is one reason for such widespread adoption of the imaging technique. "We were wondering, while it may be more sensitive to identify distant metastatic disease, was it changing what we were doing?"
In a retrospective look at 170 patients with such cancers at their institution, researchers found no significant difference in median survival between patients who had a PET scan (168 days) and those who did not (193 days). Determination of any survival difference was a primary aim of the study.
"A lot of studies have looked at PET scans, and we know in up to one-third of cases it may change our decisions," Dr. Spector said. For example, a negative PET scan might mean definitive treatment, whereas a positive PET finding might lead to palliative therapy. However, "no one has looked at the impact of the PET findings on the life expectancy after diagnosis."
All patients in the study had a distant metastasis diagnosis. "We found PET was more likely to diagnose multiple distant metastasis sites [P = .03]," Dr. Spector said. "But there were no differences in life expectancy when comparing PET to the various other imaging modalities like CT or chest x-ray."
Mean patient age was 59 years, and 135 of the patients were men.
Kaplan-Meier survival curves revealed no difference in survival between patients with a single distant metastatic site vs. multiple distant metastatic sites, said Dr. Spector, a head and neck surgery resident at the University of Michigan Health System in Ann Arbor.
The investigators intentionally controlled for chemotherapy use (110 patients, or 65%) in their survival calculations. "Chemotherapy could alter the course of their distant metastasis. Since [survival] was our main outcome measure, we wanted to control for that."
There were no differences in survival by patient age, sex, or site of primary tumor. Primary head and neck tumor sites included the oropharynx in 75 patients, the oral cavity in 40 patients, and the larynx in 36 others. The hypopharynx, nasopharynx, and some cases with unknown primary sites accounted for the remainder.
Dr. Spector and his associates did find a significant difference between the 86% of patients whose distant metastasis was detected during routine follow-up cancer care and the 14% who presented with symptoms. Median survival was 247 days in the routine surveillance group vs. 73 days for patients who might have come into the clinic complaining of chest pain after which subsequent imaging studies revealed a distant metastasis.
"Patients who were symptomatic, as you would imagine, had a worse life expectancy," Dr. Spector said. For the group detected on routine follow-up, the median time to distant metastasis diagnosis was 324 days.
Identification of any factors that did prolong survival was a second aim of the study. For the 85 patients who received palliative chemotherapy, median survival was significantly longer at 285 days, compared with 70 days for those who did not receive it.
Palliative chemotherapy was an independent factor that increased life expectancy, "and should be promoted for patients with these cancers," Dr. Spector said at the meeting, which was sponsored by the Triological Society and the American College of Surgeons. Previous chemotherapy did not alter patient response to palliative chemotherapy.
"Even for patients who were symptomatic at the time of diagnosis of their distant metastasis, palliative chemotherapy was still found to be effective," he added.
By cancer subtype, there was a nonsignificant trend for palliative chemotherapy to prolong survival among patients with primary oropharyngeal cancers (median, 333 days) compared with patients with primary laryngeal cancers (195 days).
Dr. Spector said that he had no relevant disclosures.
MIAMI BEACH – Using PET scans to diagnose distant metastasis in patients with advanced head and neck squamous cell carcinoma does not significantly prolong life expectancy, compared with other imaging techniques, according to a retrospective study.
Palliative chemotherapy did make a difference, however, significantly increasing life expectancy by 215 days in patients who received it, Dr. Matthew E. Spector and colleagues from the University of Michigan, Ann Arbor, reported at a meeting of the Triological Society.
"Over 90% of patients at University of Michigan have at least one PET scan at some point in their treatment," Dr. Spector said. Increased sensitivity is one reason for such widespread adoption of the imaging technique. "We were wondering, while it may be more sensitive to identify distant metastatic disease, was it changing what we were doing?"
In a retrospective look at 170 patients with such cancers at their institution, researchers found no significant difference in median survival between patients who had a PET scan (168 days) and those who did not (193 days). Determination of any survival difference was a primary aim of the study.
"A lot of studies have looked at PET scans, and we know in up to one-third of cases it may change our decisions," Dr. Spector said. For example, a negative PET scan might mean definitive treatment, whereas a positive PET finding might lead to palliative therapy. However, "no one has looked at the impact of the PET findings on the life expectancy after diagnosis."
All patients in the study had a distant metastasis diagnosis. "We found PET was more likely to diagnose multiple distant metastasis sites [P = .03]," Dr. Spector said. "But there were no differences in life expectancy when comparing PET to the various other imaging modalities like CT or chest x-ray."
Mean patient age was 59 years, and 135 of the patients were men.
Kaplan-Meier survival curves revealed no difference in survival between patients with a single distant metastatic site vs. multiple distant metastatic sites, said Dr. Spector, a head and neck surgery resident at the University of Michigan Health System in Ann Arbor.
The investigators intentionally controlled for chemotherapy use (110 patients, or 65%) in their survival calculations. "Chemotherapy could alter the course of their distant metastasis. Since [survival] was our main outcome measure, we wanted to control for that."
There were no differences in survival by patient age, sex, or site of primary tumor. Primary head and neck tumor sites included the oropharynx in 75 patients, the oral cavity in 40 patients, and the larynx in 36 others. The hypopharynx, nasopharynx, and some cases with unknown primary sites accounted for the remainder.
Dr. Spector and his associates did find a significant difference between the 86% of patients whose distant metastasis was detected during routine follow-up cancer care and the 14% who presented with symptoms. Median survival was 247 days in the routine surveillance group vs. 73 days for patients who might have come into the clinic complaining of chest pain after which subsequent imaging studies revealed a distant metastasis.
"Patients who were symptomatic, as you would imagine, had a worse life expectancy," Dr. Spector said. For the group detected on routine follow-up, the median time to distant metastasis diagnosis was 324 days.
Identification of any factors that did prolong survival was a second aim of the study. For the 85 patients who received palliative chemotherapy, median survival was significantly longer at 285 days, compared with 70 days for those who did not receive it.
Palliative chemotherapy was an independent factor that increased life expectancy, "and should be promoted for patients with these cancers," Dr. Spector said at the meeting, which was sponsored by the Triological Society and the American College of Surgeons. Previous chemotherapy did not alter patient response to palliative chemotherapy.
"Even for patients who were symptomatic at the time of diagnosis of their distant metastasis, palliative chemotherapy was still found to be effective," he added.
By cancer subtype, there was a nonsignificant trend for palliative chemotherapy to prolong survival among patients with primary oropharyngeal cancers (median, 333 days) compared with patients with primary laryngeal cancers (195 days).
Dr. Spector said that he had no relevant disclosures.
MIAMI BEACH – Using PET scans to diagnose distant metastasis in patients with advanced head and neck squamous cell carcinoma does not significantly prolong life expectancy, compared with other imaging techniques, according to a retrospective study.
Palliative chemotherapy did make a difference, however, significantly increasing life expectancy by 215 days in patients who received it, Dr. Matthew E. Spector and colleagues from the University of Michigan, Ann Arbor, reported at a meeting of the Triological Society.
"Over 90% of patients at University of Michigan have at least one PET scan at some point in their treatment," Dr. Spector said. Increased sensitivity is one reason for such widespread adoption of the imaging technique. "We were wondering, while it may be more sensitive to identify distant metastatic disease, was it changing what we were doing?"
In a retrospective look at 170 patients with such cancers at their institution, researchers found no significant difference in median survival between patients who had a PET scan (168 days) and those who did not (193 days). Determination of any survival difference was a primary aim of the study.
"A lot of studies have looked at PET scans, and we know in up to one-third of cases it may change our decisions," Dr. Spector said. For example, a negative PET scan might mean definitive treatment, whereas a positive PET finding might lead to palliative therapy. However, "no one has looked at the impact of the PET findings on the life expectancy after diagnosis."
All patients in the study had a distant metastasis diagnosis. "We found PET was more likely to diagnose multiple distant metastasis sites [P = .03]," Dr. Spector said. "But there were no differences in life expectancy when comparing PET to the various other imaging modalities like CT or chest x-ray."
Mean patient age was 59 years, and 135 of the patients were men.
Kaplan-Meier survival curves revealed no difference in survival between patients with a single distant metastatic site vs. multiple distant metastatic sites, said Dr. Spector, a head and neck surgery resident at the University of Michigan Health System in Ann Arbor.
The investigators intentionally controlled for chemotherapy use (110 patients, or 65%) in their survival calculations. "Chemotherapy could alter the course of their distant metastasis. Since [survival] was our main outcome measure, we wanted to control for that."
There were no differences in survival by patient age, sex, or site of primary tumor. Primary head and neck tumor sites included the oropharynx in 75 patients, the oral cavity in 40 patients, and the larynx in 36 others. The hypopharynx, nasopharynx, and some cases with unknown primary sites accounted for the remainder.
Dr. Spector and his associates did find a significant difference between the 86% of patients whose distant metastasis was detected during routine follow-up cancer care and the 14% who presented with symptoms. Median survival was 247 days in the routine surveillance group vs. 73 days for patients who might have come into the clinic complaining of chest pain after which subsequent imaging studies revealed a distant metastasis.
"Patients who were symptomatic, as you would imagine, had a worse life expectancy," Dr. Spector said. For the group detected on routine follow-up, the median time to distant metastasis diagnosis was 324 days.
Identification of any factors that did prolong survival was a second aim of the study. For the 85 patients who received palliative chemotherapy, median survival was significantly longer at 285 days, compared with 70 days for those who did not receive it.
Palliative chemotherapy was an independent factor that increased life expectancy, "and should be promoted for patients with these cancers," Dr. Spector said at the meeting, which was sponsored by the Triological Society and the American College of Surgeons. Previous chemotherapy did not alter patient response to palliative chemotherapy.
"Even for patients who were symptomatic at the time of diagnosis of their distant metastasis, palliative chemotherapy was still found to be effective," he added.
By cancer subtype, there was a nonsignificant trend for palliative chemotherapy to prolong survival among patients with primary oropharyngeal cancers (median, 333 days) compared with patients with primary laryngeal cancers (195 days).
Dr. Spector said that he had no relevant disclosures.
FROM THE TRIOLOGICAL SOCIETY'S COMBINED SECTIONS MEETING
Major Finding: In head and neck cancer patients, median survival was 168 days when distant metastases were detected by PET scan, and 193 days when metastases were detected using other modalities, an insignificant difference.
Data Source: A retrospective study of 170 patients with head and neck cancer diagnosed with distant metastasis at the University of Michigan.
Disclosures: Dr. Spector reported having no relevant financial disclosures.
Head and Neck Cancer Research
Dr. Marshall R. Posner, associate editor of The Oncology Report, discusses research highlights from the Multidisciplinary Head and Neck Cancer Symposium, including the emerging molecular picture of head and neck cancer and the growing awareness of HPV prevalence in the U.S. population.
Keep visiting The Oncology Report for more head and neck cancer news.
Dr. Marshall R. Posner, associate editor of The Oncology Report, discusses research highlights from the Multidisciplinary Head and Neck Cancer Symposium, including the emerging molecular picture of head and neck cancer and the growing awareness of HPV prevalence in the U.S. population.
Keep visiting The Oncology Report for more head and neck cancer news.
Dr. Marshall R. Posner, associate editor of The Oncology Report, discusses research highlights from the Multidisciplinary Head and Neck Cancer Symposium, including the emerging molecular picture of head and neck cancer and the growing awareness of HPV prevalence in the U.S. population.
Keep visiting The Oncology Report for more head and neck cancer news.
Posttransplant Head and Neck Tumors Tallied
MIAMI BEACH – Patients who have undergone solid organ transplantation are at greater risk for subsequent tumor development, and head and neck cancers can be particularly aggressive, according to results of a single-institution study.
Dr. Robert H. Deeb and his associates at Henry Ford Hospital in Detroit studied 3,639 patients who underwent solid organ transplantation between January 1990 and December 2011. By retrospectively searching electronic medical records, they identified 95 people who developed cutaneous, salivary gland, or mucosal malignancies.
They found a 2.1% incidence of cutaneous cancers and a 0.5% incidence of noncutaneous head and neck cancers in this population. Despite a relatively low overall 2.6% incidence, there are reasons for concern, Dr. Deeb said at the Triological Society’s Combined Sections Meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. When cutaneous cancers did occur, they were more aggressive and were associated with shorter 1-year survival rates.
Henry Ford Transplant Institute maintains a noncutaneous tumor registry. This allowed the researchers to compare survival and other factors. Compared with the "nontransplant tumor registry in our institution, we found significantly fewer patients were alive at 1 year," Dr. Deeb said. Specifically, 55% of posttransplant patients with these cancers survived to 1 year, compared with 81% of nontransplant patients. There were no significant differences between groups in terms of age, sex, stage at diagnosis, or 5-year survival.
More than half (52%) of the patients who developed skin cancers had multiple head and neck cutaneous malignancies, pointing to the aggressive nature of these cancers, said Dr. Deeb of the department of otolaryngology–head and neck surgery at Henry Ford Hospital.
"We believe these patients require aggressive screening, treatment, and follow-up," Dr. Deeb said.
Of the 78 cutaneous head and neck cancers, 51% were squamous cell carcinomas, 36% were basal cell carcinomas, and the remaining 13% were other skin cancer types. The cheek and scalp were the most common sites. The patients’ average age was 61 years at the time of diagnosis, and 74% were men. Skin cancer developed a mean 4 years after transplant surgery.
Four patients had a salivary gland cancer and 13 had an upper aerodigestive tract mucosal malignancy. The average patient age in this group was 60 years, and 94% were men. Cancer was diagnosed a mean 66 months post transplantation. All 13 of the mucosal malignancies in the study were squamous cell carcinomas, Dr. Deeb said.
Kidney, liver, and heart were the most commonly transplanted organs among patients who ultimately developed these head and neck malignancies.
Although immunosuppressants are universally prescribed to prevent organ rejection following transplant surgery, the exact mechanism for subsequent cancer development remains unknown, Dr. Deeb said. Loss of immunosurveillance is one possibility; uncontrolled cell proliferation from chronic and low-level antigenic stimulation throughout the body is another. In addition, he said, immunosuppressants might somehow activate oncogenic viruses.
Despite the findings of this study, Dr. Deeb said that the benefits of solid organ transplantation still generally outweigh the risk of subsequent cancer development.
Henry Ford Hospital funded the study. Dr. Deeb said that he had no relevant disclosures.
MIAMI BEACH – Patients who have undergone solid organ transplantation are at greater risk for subsequent tumor development, and head and neck cancers can be particularly aggressive, according to results of a single-institution study.
Dr. Robert H. Deeb and his associates at Henry Ford Hospital in Detroit studied 3,639 patients who underwent solid organ transplantation between January 1990 and December 2011. By retrospectively searching electronic medical records, they identified 95 people who developed cutaneous, salivary gland, or mucosal malignancies.
They found a 2.1% incidence of cutaneous cancers and a 0.5% incidence of noncutaneous head and neck cancers in this population. Despite a relatively low overall 2.6% incidence, there are reasons for concern, Dr. Deeb said at the Triological Society’s Combined Sections Meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. When cutaneous cancers did occur, they were more aggressive and were associated with shorter 1-year survival rates.
Henry Ford Transplant Institute maintains a noncutaneous tumor registry. This allowed the researchers to compare survival and other factors. Compared with the "nontransplant tumor registry in our institution, we found significantly fewer patients were alive at 1 year," Dr. Deeb said. Specifically, 55% of posttransplant patients with these cancers survived to 1 year, compared with 81% of nontransplant patients. There were no significant differences between groups in terms of age, sex, stage at diagnosis, or 5-year survival.
More than half (52%) of the patients who developed skin cancers had multiple head and neck cutaneous malignancies, pointing to the aggressive nature of these cancers, said Dr. Deeb of the department of otolaryngology–head and neck surgery at Henry Ford Hospital.
"We believe these patients require aggressive screening, treatment, and follow-up," Dr. Deeb said.
Of the 78 cutaneous head and neck cancers, 51% were squamous cell carcinomas, 36% were basal cell carcinomas, and the remaining 13% were other skin cancer types. The cheek and scalp were the most common sites. The patients’ average age was 61 years at the time of diagnosis, and 74% were men. Skin cancer developed a mean 4 years after transplant surgery.
Four patients had a salivary gland cancer and 13 had an upper aerodigestive tract mucosal malignancy. The average patient age in this group was 60 years, and 94% were men. Cancer was diagnosed a mean 66 months post transplantation. All 13 of the mucosal malignancies in the study were squamous cell carcinomas, Dr. Deeb said.
Kidney, liver, and heart were the most commonly transplanted organs among patients who ultimately developed these head and neck malignancies.
Although immunosuppressants are universally prescribed to prevent organ rejection following transplant surgery, the exact mechanism for subsequent cancer development remains unknown, Dr. Deeb said. Loss of immunosurveillance is one possibility; uncontrolled cell proliferation from chronic and low-level antigenic stimulation throughout the body is another. In addition, he said, immunosuppressants might somehow activate oncogenic viruses.
Despite the findings of this study, Dr. Deeb said that the benefits of solid organ transplantation still generally outweigh the risk of subsequent cancer development.
Henry Ford Hospital funded the study. Dr. Deeb said that he had no relevant disclosures.
MIAMI BEACH – Patients who have undergone solid organ transplantation are at greater risk for subsequent tumor development, and head and neck cancers can be particularly aggressive, according to results of a single-institution study.
Dr. Robert H. Deeb and his associates at Henry Ford Hospital in Detroit studied 3,639 patients who underwent solid organ transplantation between January 1990 and December 2011. By retrospectively searching electronic medical records, they identified 95 people who developed cutaneous, salivary gland, or mucosal malignancies.
They found a 2.1% incidence of cutaneous cancers and a 0.5% incidence of noncutaneous head and neck cancers in this population. Despite a relatively low overall 2.6% incidence, there are reasons for concern, Dr. Deeb said at the Triological Society’s Combined Sections Meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. When cutaneous cancers did occur, they were more aggressive and were associated with shorter 1-year survival rates.
Henry Ford Transplant Institute maintains a noncutaneous tumor registry. This allowed the researchers to compare survival and other factors. Compared with the "nontransplant tumor registry in our institution, we found significantly fewer patients were alive at 1 year," Dr. Deeb said. Specifically, 55% of posttransplant patients with these cancers survived to 1 year, compared with 81% of nontransplant patients. There were no significant differences between groups in terms of age, sex, stage at diagnosis, or 5-year survival.
More than half (52%) of the patients who developed skin cancers had multiple head and neck cutaneous malignancies, pointing to the aggressive nature of these cancers, said Dr. Deeb of the department of otolaryngology–head and neck surgery at Henry Ford Hospital.
"We believe these patients require aggressive screening, treatment, and follow-up," Dr. Deeb said.
Of the 78 cutaneous head and neck cancers, 51% were squamous cell carcinomas, 36% were basal cell carcinomas, and the remaining 13% were other skin cancer types. The cheek and scalp were the most common sites. The patients’ average age was 61 years at the time of diagnosis, and 74% were men. Skin cancer developed a mean 4 years after transplant surgery.
Four patients had a salivary gland cancer and 13 had an upper aerodigestive tract mucosal malignancy. The average patient age in this group was 60 years, and 94% were men. Cancer was diagnosed a mean 66 months post transplantation. All 13 of the mucosal malignancies in the study were squamous cell carcinomas, Dr. Deeb said.
Kidney, liver, and heart were the most commonly transplanted organs among patients who ultimately developed these head and neck malignancies.
Although immunosuppressants are universally prescribed to prevent organ rejection following transplant surgery, the exact mechanism for subsequent cancer development remains unknown, Dr. Deeb said. Loss of immunosurveillance is one possibility; uncontrolled cell proliferation from chronic and low-level antigenic stimulation throughout the body is another. In addition, he said, immunosuppressants might somehow activate oncogenic viruses.
Despite the findings of this study, Dr. Deeb said that the benefits of solid organ transplantation still generally outweigh the risk of subsequent cancer development.
Henry Ford Hospital funded the study. Dr. Deeb said that he had no relevant disclosures.
FROM THE TRIOLOGICAL SOCIETY'S COMBINED SECTIONS MEETING
Major Finding: A total of 95 people who underwent solid organ transplantation over 21 years developed subsequent head and neck cancer, for an incidence of 2.6%.
Data Source: Data are taken from a retrospective study of 3,639 solid organ transplant patients treated at the Henry Ford Hospital since 1990.
Disclosures: Henry Ford Hospital sponsored the study. Dr. Deeb reported having no financial disclosures.
Alcohol Withdrawal Syndrome Worsens Cancer Surgery Outcomes
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
FROM THE TRIOLOGICAL SOCIETY'S COMBINED SECTIONS MEETING
Major Finding: The presence of alcohol withdrawal symptoms was associated with a significantly higher incidence of postoperative complications, 25%, compared with 14% among patients who abused alcohol and 7% for those without alcohol abuse.
Data Source: Data were taken from a retrospective, cross-sectional study of 92,312 ablative procedures for head and neck cancer from the NIS database in 2003-2008.
Disclosures: Dr. Genther reported having no financial disclosures.
Jaw Complications Persist With Head & Neck Cancer Treatment
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
PHOENIX – An analysis of Medicare data for more than 1,800 head and neck cancer patients suggests that jaw complications following radiation treatment may be more common than recognized.
Moreover, intensity-modulated radiation therapy (IMRT) was not associated with significantly lower rates of jaw complications, compared with older radiation techniques, although there was a slight trend in that direction and the interval to developing jaw complications was longer following IMRT, reported Dr. Beth M. Beadle at a head and neck cancer symposium sponsored by the American Society for Radiation Oncology.
In the literature, osteoradionecrosis (ORN), the most severe jaw manifestation resulting from head/neck radiation, was reported on average in 11.8% of patients in 10 studies (total, 3,312 irradiated patients) from the 1930s through the 1960s, said Dr. Beadle, a radiation oncologist at the University of Texas M.D. Anderson Cancer Center, Houston.
With improved technologies, the rate dropped to 5.4%, as documented in 21 studies involving a total of 11,077 patients conducted from the 1970s through the early 1990s. Since 1997, 25 retrospective and prospective studies involving 9,632 patients overall have reported an overall average ORN rate of 3.0%, she said.
For the current study, data were taken from the SEER (Surveillance, Epidemiology, and End Results) database for Medicare beneficiaries. Patients who were diagnosed with oral cancers in 1999-2007 were identified using SEER, ICD-9, and CPT codes. Primary tumor sites included those of the lip, tongue, floor of mouth, gum, tonsil, oropharynx, and other oral cavity and pharynx.
Of 1,848 patients overall, 16.1% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion. Of those, 256 patients had ICD-9 diagnostic codes that included those for osteonecrosis of jaw (733.45), osteomyelitis of jaw (526.4), and other diseases of the jaws, including inflammatory conditions, alveolitis, and periradicular pathology (all 526.x).
Some 41 patients (3.8% of the total) had CPT procedure codes, including drainage of abscess (41800), alveolectomy (41830), operations on facial bones or joints with concurrent ORN diagnosis (76.3), or hyperbaric oxygen therapy (99183), and 30 patients (1.6% of the total) had both a diagnostic and a procedural ORN code, Dr. Beadle said.
The percentage of patients who required intervention for ORN (3.8%) is more consistent with the overall ORN rates from the literature, suggesting that most previous studies have captured only the more severe osteoradionecrosis, which is usually defined as that requiring a procedure, she explained.
In univariate analysis, female sex, not receiving chemotherapy, and a lower number of comorbidities on the Charlson Comorbidity Index were the only factors significantly associated with all jaw complications.
Receipt of IMRT was not a significant predictor, although there was a trend. Patients who received IMRT differed significantly from non-IMRT patients in several ways, however, including their younger age and their greater likelihood to be male, to have advanced-stage disease, to have received definitive vs. adjuvant treatment, to have received chemotherapy, and to have fewer comorbidities.
Although IMRT per se did not predict jaw complications, there was a longer time interval between treatment and the development of jaw complications among the patients who received IMRT (462 days vs. 386 days for the non-IMRT patient).
In response to questions from the audience, Dr. Beadle said that it wasn’t clear why jaw complications would be more common among patients who did not receive chemotherapy, but it might be that those patients received higher doses of radiation. As for the sex difference, she suggested it may be that women have better follow-up care, or it might relate to either osteoporosis or use of bisphosphonates. Her group is investigating those possibilities.
Dr. Beadle stated that she has no disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Of a total 1,848 patients with oral cancers, 16% (297) had at least one osteoradionecrosis code within 90 days of radiation therapy completion.
Data source: Data were taken from the SEER database for Medicare beneficiaries.
Disclosures: Dr. Beadle reported having no financial disclosures.
Toxicity Drives Costly Head and Neck Cancer Readmissions
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
PHOENIX – Unplanned hospitalizations due to toxicities associated with head and neck cancer treatment were a source of substantial cost in a retrospective chart review of 141 patients treated at a single cancer center during 2007-2011.
Much of the increased cost was among patients who underwent docetaxel plus cisplatin and fluorouracil induction chemotherapy (TPF) plus chemoradiotherapy.
"In recent years, induction chemotherapy has been increasingly incorporated into multimodality regimens for selected patients with locally advanced primary squamous cell carcinoma of the head and neck (HNSCC) ... Although efficacious (N. Engl. J. Med. 2007;357:1705-15), TPF has the potential for toxicities [that] may lead to unplanned admissions during treatment. Concurrent use of chemotherapy with radiation is well documented to intensify therapeutic effect and toxicity," Dr. Regan D. Rostorfer and his associates said in a poster.
Symptoms leading to the unplanned readmissions during induction chemotherapy (27 readmissions, 18 patients) included dehydration (in 13 of the 27 readmissions), infection (8), diarrhea (6), nausea/vomiting (5), pain (4), and mucositis (3).
A range of strategies can be used to avoid readmissions and thereby reduce these costs, including careful patient selection, use of prophylactic antimicrobials, standardized use of growth factor support, post-treatment support with outpatient intravenous fluids, integration of home health care services, early gastrostomy-tube placement, use of long-acting antiemetics during treatment, and frequent outpatient office visits during treatment, Dr. Rostorfer and his associates said.
"A number of initiatives are ongoing at our center in efforts to decrease readmission rates during combined modality treatment. Further studies are planned to assess the impact of these measures on readmission rates, and impact on costs of care," the investigators said in their poster.
In an interview, Dr. Rostorfer said the study was initially intended to simply to gather statistics about readmission for head/neck cancer treatment-related toxicity, since there were no published data on it.
"We decided to look at data from our own institution, simply to see how frequently patients were readmitted, and the reason for readmission. More recently, costs have become an issue at almost every hospital in the country, so we decided to look at the excess costs associated with these unplanned admissions, as well.
The investigators reviewed charts for 91 randomly assigned patients with locally advanced primary HNSCC who received treatment with concurrent chemoradiotherapy, and for another 50 patients who received induction TPF chemotherapy followed by chemoradiation. The oropharynx was the most common cancer site, in 24 of the induction group (48%) and 59 of the concurrent group (65%).
A total of 19 induction patients (38%) required unplanned readmission, with 8 requiring more than one. Median length of stay for those total 27 unplanned stays was 6 days (range 1-25). In the concurrent group, 47 patients required unplanned readmission (52%), with 19 requiring more than one. That group had a total 77 unplanned readmissions, with a median stay of 7.8 days (1-65).
Total costs of admissions in the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay – elective admission for chemotherapy – was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, which did not have planned hospitalizations, the cost per unplanned stay was $69,460, said Dr. Rostorfer, medical oncology and hematology chief fellow at MD Anderson Cancer Center Orlando, and his associates.
"Obviously this was a small, retrospective review, but the numbers can be quite alarming. We have begun to implement measures to reduce the numbers of readmission, so hopefully to reduce the cost associated with care. We will see the difference it makes."
Dr. Rostorfer stated that he has no disclosures.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: Total costs of all admissions for the induction group were $3,368,583 for the planned admissions and $1,777,136 for the unplanned admissions. The median cost per planned hospital stay, that is, the elective admission for chemotherapy, was $32,276. In contrast, the cost per unplanned hospital stay was $42,390. For the concurrent group, the cost per unplanned stay was $69,460.
Data Source: The findings come from a retrospective chart review of 141 patients with locally advanced head and neck cancer seen at a single center.
Disclosures: Dr. Rostorfer reported having no financial disclosures.
IMRT Provides Better QOL in Head and Neck Cancers
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
PHOENIX – Intensity-modulated radiotherapy is more expensive than 3-D–conformal radiotherapy is and has not been shown to improve standard outcomes in patients with head and neck cancer. But it results in better quality of life.
These findings from two studies presented at the Multidisciplinary Head and Neck Cancer Symposium raise the question: Does improved quality of life justify the greater expense of intensity modulated radiotherapy (IMRT), which has been rapidly adopted for the treatment of head and neck cancer?
Because IMRT spares surrounding tissues, it reduces the likelihood of developing xerostomia, noted Dr. Nathan C. Sheets, who presented data on billing charges associated with IMRT, compared with 3-D–conformal radiotherapy (CRT). IMRT is reimbursed at a substantially higher level than CRT, however, and it is unclear how to assess this cost relative to other aspects of care in this population, said Dr. Sheets, a radiation oncology resident at the University of North Carolina, Chapel Hill.
A separate study presented by Dr. Allen M. Chen compared quality of life in patients who received IMRT vs. CRT. "There’s very little data to suggest IMRT is better than non-IMRT using traditional end points. But the question is: How do you define ‘better’?" said Dr. Chen, director of the radiation oncology residency training program at the University of California, Davis in Sacramento.
"IMRT might not particularly involve better cure rates, but it could make a difference in terms of other end points, such as quality of life, which we all know is very important to patients," he said.
Gap Ranges from $5,000 to $6,000
The cost study analyzed data for 184 patients who had received definitive radiation therapy for head and neck squamous cell cancer at the University of North Carolina at Chapel Hill during 2000-2009 and for whom billing records were available.
The median year of treatment was 2004 for 89 patients treated with CRT, and 2007 for 95 IMRT patients, reflecting the shift to use of IMRT over time. The majority of patients – 87% of CRT and 94% of IMRT – received concurrent chemotherapy. More IMRT patients received positron emission tomography (PET) scans at any point (69% vs. 37%).
Over 36 months’ follow-up, locoregional control was nearly identical for the two patient groups (P = .73). Mean total costs, from the time of diagnosis through the first year of follow-up, were considerably higher for IMRT, at $50,502 vs. $38,977 for CRT. Outpatient costs accounted for the bulk of the difference ($35,418 IMRT vs. $22,696 CRT), whereas inpatient costs were similar, Dr. Sheets reported.
Multivariate analysis showed that factors associated with increased cost of radiotherapy included IMRT, recurrent disease, comorbidities, non-white race, and use of positron-emission scanning. After adjustment for inflation, each of these factors, including IMRT, independently increased the total cost by approximately $5,000-$6000. (Treatment failure was much more expensive, contributing about $14,274 to the total cost.)
Dr. Sheets ended his presentation with the question, "Do the benefits of IMRT outweigh the costs?"
QOL Improves Over 2 Years’ Follow-up
Dr. Chen’s quality of life study addressed that question. The study used the University of Washington Quality of Life instrument (UW-QOL), a previously validated, self-administered questionnaire given to patients returning for follow-up after completion of radiation therapy for head and neck cancer. The University of California, Davis, routinely uses the measure in clinical practice.
Scores on the UW-QOL were retrospectively reviewed for 155 patients with squamous cell carcinomas of the head and neck requiring bilateral neck irradiation for locally advanced disease. Only patients who were clinically without evidence of recurrent disease and with at least 2 years of follow-up were included in the analysis. Definitive radiation therapy was given to 82 patients (53%), while 73 (47%) underwent postoperative treatment.
IMRT was used in 84 patients (54%), with inclusion of the low neck in an extended field. The remaining 71 patients (46%) were treated with 3-D–CRT using opposed lateral fields matched to a low anterior neck field. Concurrent chemotherapy was administered with radiation therapy for 73 patients (47%).
The mean global quality of life scores for the IMRT patients were 67.5 at 1 year and 80.1 at 2 years, compared with 55.4 and 57.0, respectively, for the CRT patients (P less than .001). At 1 year after completion of radiation therapy, the proportion of patients who rated their global quality of life as "very good" or "outstanding" 51% of the IMRT patients, compared with 41% of those treated with CRT (P = .11).
Those numbers became statistically significant at 2 years, with "very good" or "outstanding" quality of life reported by 73% of the IMRT patients and 49% of the CRT group (P less than .001). At last follow-up, 80% of patients treated by IMRT reported that their health-related quality of life was "much better" or "somewhat better," compared with the month before developing cancer, compared with 61% among patients treated by 3-D–CRT (P less than .001).
On multivariate analysis accounting for gender, age, radiation intent (definitive vs. postoperative), radiation dose, T stage, primary site, use of concurrent chemotherapy, and neck dissection, the use of IMRT was the only variable independently associated with improved quality of life (P = .01).
In 1- and 2-year analyses of factors contributing to the difference in UW-QOL score, only "saliva" was found to be significantly different between IMRT and CRT (P less than .001) for both time points. Other examined factors that did not affect the score included pain, appearance, activity, recreation, chewing, swallowing, speech, mood, and anxiety.
"Treatments for dry mouth are fairly primitive and ineffective at present, so preventing dry mouth is so critical. It’s a huge problem. Imagine not being able to make any saliva. And, there are health consequences with respect to things like oral hygiene and dental caries. There’s a cost associated with chronic dry mouth," Dr. Chen said in the interview.
Increased Cost Not That Big
The increase in cost with IMRT isn’t that big, Dr. Bhisham Chera, the principal investigator for the cost study and a radiation oncologist at the University of North Carolina said in an interview.
"On average, it was about $5,000-$6,000 more total," he said. "It is more expensive, but what was shocking to me is that it wasn’t much more expensive as some therapies – like newer chemotherapy drugs, compared to older ones, where there’s a hundred thousand dollar difference in cost and the survival improvement is only a few months."
"We think the incremental increase in cost is justified because of the improvement in dry mouth. If you really compare it to other therapies such as using transperineal prostatectomy vs. robotic prostatectomy or cisplatin vs. cetuximab chemotherapy, the cost difference is vastly greater," he added. "Here, the incremental difference is not that much. It is more expensive, but it’s not astronomically more expensive."
Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
A HEAD AND NECK CANCER SYMPOSIUM SPONSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: IMRT was about $5,000-$6,000 more expensive than was 3-D–CRT. But 73% of IMRT patients reported very good or outstanding quality of life at 2 years vs. 49% of CRT patients (P less than .001).
Data Source: Investigators presented separate retrospective studies comparing IMRT with 3D-CRT in head and neck cancers at their institutions.
Disclosures: Dr. Sheets, Dr. Chen, and Dr. Chera all stated that they had no disclosures.
Cisplatin Aids Survival of High-Risk Head and Neck Cancer
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
PHOENIX – Adding chemotherapy to radiotherapy improved 10-year survival of resectable head and neck carcinomas among high-risk patients who had microscopically involved resection margins and/or extracapsular spread of disease – but not in high-risk patients who only had tumor in multiple lymph nodes.
The findings come from a long-term update and unplanned subset analysis of 410 evaluable patients from the RTOG (Radiation Therapy Oncology Group) 9501 phase III study, which previously showed no overall survival advantage from the addition of cisplatin chemotherapy to radiation.
The new data are "good news," according to lead author Dr. Jay Cooper, director of Maimonides Cancer Center in Brooklyn, N.Y.
"We now can eradicate some advanced head and neck tumors that we couldn’t before by adding chemotherapy to radiation therapy. At the same time, we can spare other patients who would not do better with the addition of chemotherapy from its side effects," he said at a head and neck cancer symposium sponsored by the American Society for Radiation Therapy.
The RTOG 9501 study randomized 459 patients with high-risk, resected head and neck cancers to receive either radiation therapy of 60 Gy in 6 weeks (RT), or identical radiotherapy plus cisplatin at 100 mg/m2 IV on days 1, 22, and 43 (RT+CT).
When reported at a median follow-up of 45.9 months, the locoregional control rate was significantly higher in the combined-therapy group than in the group given radiotherapy alone (hazard ratio for locoregional recurrence, 0.61); disease-free survival was significantly longer with combined therapy (HR for disease or death, 0.78), but overall survival was not (HR for death, 0.84). Moreover, four patients who received combination therapy died as a result of treatment (N. Engl. J. Med. 2004;350:1937-44).
In the current updated analysis conducted 10 years post treatment, none of the primary outcomes differed significantly between the two groups. The evaluable population comprised 208 patients who received RT and 202 given RT+CT. For patients treated by RT vs. RT+CT, the rates were, respectively, 28.8% vs. 22.3% (P = .10) for locoregional failure, 19.1% vs. 20.1% (P = .25) for disease-free survival, and 27.0% vs. 29.1% (P = .31) for overall survival.
In a subset analysis that had not been performed previously, however, statistically significant differences appeared within the 242 patients who had microscopically involved resection margins and/or extracapsular spread of disease. In this group, 115 patients received RT and 127 were given RT+CT. Locoregional failure occurred in 33.1% of the CT group vs. 21.0% of those treated with RT+CT (P = .02). The disease-free survival rate was 12.3% vs. 18.4% (P = .05), and the overall survival rate was 19.6% vs. 27.1% (P = .07), with both end points favoring RT+CT.
That left 168 patients who did not have involved margins or extracapsular extension and were included in the trial solely because they had multiple involved nodes. In this group, 93 received RT and 75 RT+CT, with no significant difference in long-term outcomes.
There was a trend in improved cause-specific survival with RT+CT for patients whose death resulted from head and neck cancer, but more deaths not due to the study cancer were observed in patients treated with concurrent cisplatin. This is a hypothesis-generating finding that needs to be investigated in future trials, Dr. Cooper noted.
In an interview, he explained that the rationale for looking specifically at the patients with microscopically involved resection margins and/or extracapsular spread came from a previous analysis of the raw data from the RTOG trial combined with those of a concurrently published study conducted by the EORTC (European Organisation for Research and Treatment of Cancer).
Although the design of the EORTC 22931 study was similar, the outcome was different. Of a total 167 patients who had been randomized to RT or RT+CT, the rate of progression-free survival at a median follow-up of 60 months was significantly higher in the combined-therapy group than in the group given radiotherapy alone (P = .04) (N. Engl. J. Med. 2004;350:1945-52).
When the data from RTOG and EORTC were combined, it became clear that the main reason for the difference in outcome was in the different entry criteria for the two trials, and that extracapsular extension (ECE) and/or microscopically involved surgical margins were the only risk factors for which the impact of adjuvant chemotherapy-enhanced radiation therapy was significant in both trials (Head Neck 2005;27:843-50).
"What we learned from that analysis is that the patients who got on one of the trials but wouldn’t have qualified for the other trial were not getting much benefit from the study regimen, whereas those who qualified for either study – due to having involved margins and/or extracapsular extension – did better with chemotherapy on all three measures.
"These results were highly significant. But more importantly, the data suggested a subgroup where the big bang for the buck was," Dr. Cooper said in the interview.
The findings don’t mean that the patients who did not benefit are not "high risk," Dr. Cooper said. "Would they benefit from other chemotherapy? We don’t know. Would they benefit from different drugs or different regimens? Maybe. But we can now fairly comfortably say that in both the short and long run, if patients are high risk only because of involved lymph nodes, don’t treat them with this combination, and spare them the toxicity."
Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.
FROM A HEAD AND NECK CANCER SYMPOSIUM SPONOSORED BY THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY
Major Finding: At 10 years post treatment, the overall survival rate was higher when cisplatin was added to adjuvant radiotherapy in patients who had microscopically involved resection margins and/or extracapsular spread of disease (27.1% vs. 19.6% with RT alone; P = .07).
Data Source: The data come from an unplanned analysis of 410 patients in the randomized phase III RTOG 9501.
Disclosures: Dr. Cooper stated that he has no disclosures, as did nine coauthors. One additional coauthor is an employee of Lilly USA.