User login
Critical Access for Veterans Bill Would Undermine VA Care
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
The Critical Access for Veterans Care Act, S.1868, introduced in May by Senators Kevin Cramer (R-ND) and Tim Sheehy (R-MT), would fundamentally reshape how veterans living in rural communities access private health care. The legislation establishes a new paradigm impacting veterans enrolled in US Department of Veterans Affairs (VA) health care who reside within 35 miles of any Centers for Medicare & Medicaid Services-designated Critical Access Hospital (CAH) or affiliated clinic. The bill would allow veterans unprecedented autonomy to self-refer directly to these facilities.
However, despite its seemingly straightforward title, the bill will not expedite care delivery, reduce travel burdens, or enhance network critical care capacity for veterans living in rural areas. Instead, the bill would further privatize veteran health care delivery by permitting veterans within this geographic radius to independently pursue care at CAHs and clinics without prior authorization. The legislation would establish a parallel referral system that erodes the Veterans Community Care Program (VCCP) eligibility determinations that were meticulously developed under the VA MISSION Act of 2018.
Some lawmakers have repeatedly pushed to eliminate VA's authorization role in the past 6 years, seeking to grant unrestricted private sector access to various veteran populations, particularly those requiring mental health services. Sponsors of the current bill are explicitly pursuing this same objective, characterizing VA authorization as an “unnecessary roadblock” that should be removed. However, this characterization misrepresents the actual function and value of the authorization process.
Over the past 6 years, provisions in the VA MISSION Act and other laws for predetermining veteran eligibility for private care have provided veterans with broad access while maintaining oversight and accountability. Enrolled veterans may receive comprehensive emergency medical and psychiatric care at any health care facility, including CAHs. They are guaranteed unrestricted walk-in urgent care access anywhere in the country. Veterans can also obtain outpatient and inpatient services through VCCP clinicians when they meet the following established access criteria: VA facilities exceed 30-minute travel times for primary and mental health services or 60 minutes for specialty care, or when appointment wait times surpass 20 days for primary/mental health care or 28 days for specialty services. Nearly half of covered veterans used this option in FY2023.
This bill does more than upend the established paradigm of VCCP eligibility requirements: it also eliminates the critical function of utilization review and accountability. Its passage would establish a dangerous precedent. By eliminating drive time and wait time eligibility standards and simultaneously removing VA’s ability to manage use, the bill generates powerful political momentum to extend identical provisions to all enrolled veterans. Furthermore, this legislation could specifically precipitate the downsizing or closure of VA community-based outpatient clinics (CBOCs) in areas served by CAHs. North Dakota, for example, operates 5 CBOCs that could be affected. Veterans who live in rural areas within the standard 30- to 60-minute drive time of a CBOC and can secure appointments within the established 20- to 28-day timeframes would no longer be subject to the same eligibility criteria that govern all covered veterans.
The Veterans Healthcare Policy Institute (VHPI) has serious reservations about legislation that eliminates VA's indispensable authorization and referral functions for supplemental private care. Founded in 2016, the VHPI is a nonprofit, nonpartisan organization dedicated to analyzing health care, disability compensation, and benefits for US veterans and their families. It provides fact-based research to educate the public and improve care quality both within and outside the VA.
New initiatives threaten to drastically reduce veterans' health and disability benefits through staff cuts and service reductions that will limit access to earned benefits and life-sustaining health care. Attacks against the VA also threaten to erode the training that produces new cohorts of health professionals, dramatically exacerbating the nation’s already dire shortages of physicians, nurses, psychologists and social workers.
VHPI’s coverage of Veterans Health Administration downsizing within rural health care provides important context. Starting with a comprehensive 15-page white paper published in 2024, VHPI has consistently highlighted how veterans living in rural communities face the same health care access challenges as all rural Americans—living in regions with severe shortages of health care facilities, professionals, and support staff. Lawmakers who assume veterans living in rural areas will experience shorter wait times and drive distances through private sector care fundamentally misunderstand these systemic issues
VHPI is committed to rigorously scrutinize policies that may compromise high quality care for veterans, especially those living in rural areas. The organization recently examined the flawed assumptions underlying these misguided policies. On August 12, VHPI released an in-depth analysis of private sector clinicians’ capacity to care for veterans in across all 50 states titled “Veterans’ Health Care Choice—Myth or Reality? A State- by- State Reality Check of the False Promise of VA Privatization.” This analysis revealed that, in most states, and in all rural states, the private sector system was struggling to meet even the basic needs of non-veterans. As one long time VA expert stated, to imagine that the system could absorb an influx of millions of veterans – particularly when new cuts to Medicaid and other healthcare funding are implemented, is “delusional.”
Russell Lemle and Suzanne Gordon are senior policy analysts at the Veterans Healthcare Policy Institute. Suzanne Gordon is author of Wounds of War.
VA To Lose 30K Positions Via Attrition, No RIFs Planned
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
The initial plan to reduce the US Department of Veterans Affairs (VA) workforce by 15%—roughly 83,000 employees—has been revised. The VA announced that it expected to reduce its workforce by 30,000 positions through normal attrition, early retirements, and resignations by the end of fiscal year 2025, “eliminating the need for a large-scale reduction-in-force.” Most of the positions will not be replaced due to the federal hiring freeze, which has been extended for 3 months.
“Since March, we’ve been conducting a holistic review of the department centered on reducing bureaucracy and improving services to Veterans,” VA Secretary Doug Collins said in a press release. “A department-wide RIF is off the table, but that doesn’t mean we’re done improving VA.”
About 17,000 VA employees have left their jobs as of June 1. From now and Sept. 30, the department expects another reduction of nearly 12,000. Pete Kasperowicz, a VA spokesperson, said there would not be any reductions beyond the 30,000 planned.
The VA says it has multiple safeguards in place to ensure the reductions do not impact veteran care or benefits. All VA mission-critical positions are exempt from the voluntary early retirement authority and deferred resignation program, and > 350,000 positions are exempt from the federal hiring freeze.
The release noted several other improvements regarding VA performance in 2025, among them that the disability claims backlog has been reduced by 30% and a record 2 million disability claims have been processed by June. More than 60,000 VA employees have also returned to the office, according to the release.
“As a result of our efforts, VA is headed in the right direction – both in terms of staff levels and customer service,” Collins said. “Our review has resulted in a host of new ideas for better serving Veterans that we will continue to pursue.”
OIG Report Reveals Lapses in VA Retention and Recruitment Process
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
The Veterans Health Administration (VHA) paid about $828 million in recruitment and retention incentives from 2020 to 2023, but the process for providing an estimated $340.9 million of that was not “effectively governed” according to a recent US Department of Veterans Affairs (VA) Office of Inspector General (OIG) investigation.
About one-third of incentives were missing forms or signatures, or lacked sufficient justification, for the payments to about 130,000 VHA employees. In the report, the OIG notes the VHA has faced “long-standing challenges related to occupational shortages,” adding that a shortage occupation designation does not mean there are actual shortages at a facility.
“Most shortage occupations continue to experience annual net growth and are not critically understaffed in most facilities,” the report says.
More than 85% of incentive monies in 2022 and 2023 were paid to employees in occupations on staffing shortage lists. OIG estimated the VHA paid incentives to 38,800 employees (about 30%) where the award justification could not be verified or was insufficient.
Amplified by the COVID-19 pandemic and the PACT Act, the need to recruit and retain employees peaked in 2021, when record numbers of health care workers left their jobs. An October 2021 survey of 1000 medical professionals found nearly 1 in 5 health care workers quit during the pandemic, with most citing stress and burnout, and an additional 31% were considering quitting. When the PACT Act was signed into law in August 2022, it created thousands of newly benefits-eligible veterans.
In May 2022, the VA reported it needed to hire 52,000 employees annually for the next 5 years to keep up. In response, the VA released a 10-step plan to support recruitment and retention, focusing on raising wages when possible and finding other incentives when it wasn’t (ie, relocation bonuses or greater flexibility for remote work). The OIG report acknowledged the pandemic exacerbated VHA’s recruitment and retention challenges.
By 2024, the VA had not only reduced employee turnover by 20% over the prior 2 years, but had also exceeded its hiring goals. The VHA workforce grew by 7.4% in fiscal year 2023, its highest rate of growth in > 15 years.
VA officials must retain the documentation for incentives for 6 years so the process can be reconstructed if necessary. However, the OIG report noted “numerous instances” where documentation couldn’t be produced and therefore could not determine whether the incentives complied with policy.
The report also identified 28 employees who received retention incentive payments long after their award period had expired. The VA paid about $4.6 million for incentives that should have been terminated. The VA reported that it is pursuing debt collection for 27 of the 28 employees.
Only if the “identified weaknesses” are addressed will the VHA have assurance that incentives are being used effectively, the OIG said. Its recommendations included enforcing quality control checks and establishing accountability measures. The OIG also recommended establishing oversight procedures to review retention incentives annually, recertify them if appropriate, or terminate them.
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
The US House Appropriations Committee approved a $453 billion budget to fund the US Department of Veterans (VA), military construction, and other programs in 2026 by a 36-27 vote. The bill includes $34 billion proposed for community care programs, an increase of > 50% from 2025 community care funding levels.
The discretionary funding would also send $2.5 billion to the VA electronic health records modernization program. Mandatory spending includes $53 billion for the Toxic Exposures Fund, which supports benefits and health care costs associated with the PACT Act.
Although VA budget bills are typically bipartisan in nature, this bill passed by a much narrower margin than is typical. Rep. Debbie Wasserman Schultz (D-FL), ranking member of the Military Construction, Veterans Affairs and Related Agencies Appropriations Subcommittee, said the bill “diverts far too many resources away from the vital, VA-based care that veterans consistently tell us they want, and it pushes them into pricier, subpar corporate hospitals.”
Committee Democrats offered dozens of amendments. All amendments were rejected except for a modification that would block staff reductions at the Veterans Crisis Line and other VA suicide prevention programs.
The bill now moves to the full House of Representatives for consideration. House leaders have not yet announced when that vote will take place; the House is in recess the week of June 16, 2025.
The committee also released the Fiscal Year 2026 Military Construction, Veterans Affairs, and Related Agencies Bill, which would spend > $83 million, a 22% increase over the 2025.
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
2026 VA Budget Bill Narrowly Passed by House Appropriations Committee
VA to Allow Veteran Referrals to Community Care Without Second Review
VA to Allow Veteran Referrals to Community Care Without Second Review
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
Veterans enrolled in the US Department of Veterans Affairs (VA) who have been referred to Community Care no longer need a second review from a VA clinician according to a new policy. The provision implements language from the Senator Elizabeth Dole 21st Century Veterans Healthcare and Benefits Improvement Act. VA officials hope that it will speed up access to community care.
The move expands on the 2019 MISSION Act, which allows eligible veterans to access health care from non-VA clinicians that is paid for by the VA when it is in their “best medical interest.” Those decisions, however, were not considered final until reviewed by a second VA doctor.
The Dole Act prohibits VA administrators from overriding a VA doctor’s referral for a patient to receive outside care. According to the law, the ban on administrative review will remain in place for 2 years, after which the VA must report on its effects to Congress. The VA announced it would begin training employees to ensure the community care referral process is followed in compliance with the Dole Act.
Analysis from the Veterans Healthcare Policy Institute claims the best medical interest criterion “is to be considered when a veteran's health and/or well-being would be compromised if they were not able to be seen in the community for the requested clinical service.”
During a March hearing, Rep. Julia Brownley (D-CA), ranking Democrat on the House Veterans’ Affairs subcommittee on health, said any veteran who seeks residential treatment should get it, but noted the VA has not developed a fee schedule for community treatment centers. In at least 1 case, she said, the department was charged up to $6000 a day for 1 patient. Brownley also noted that the VA doesn't track the timeliness or quality of medical care in community residential treatment facilities.
“We have no way of knowing the level of treatment or support they are getting,” she said. “We must find a balance between community care and VA direct care. In my opinion, we have not found that balance when it comes to residential rehabilitation treatment facilities.”
At the same hearing, chair of the House Veterans Affairs health subcommittee Rep. Mariannette Miller-Meeks (R-IA) said more change is needed—specifically to ensure that veterans also can access private residential substance abuse treatment centers. Some, she said, “are told they cannot access community care unless a VA facility fails to meet a 20-day threshold—forcing them to wait, even when immediate, alternative options exist."
The House of Representatives passed H.R. 1969, the No Wrong Door for Veterans Act, in May, which expands the VA suicide prevention grant program. However, the Senate has yet to take up the legislation. “I’ve seen firsthand how difficult it can be for veterans in crisis to navigate a complicated system when every second counts,” Miller-Meeks said. “The No Wrong Door for Veterans Act ensures that our heroes are never turned away or left without help. It streamlines access, strengthens coordination, and reaffirms our promise to those who served.”
VA to Allow Veteran Referrals to Community Care Without Second Review
VA to Allow Veteran Referrals to Community Care Without Second Review
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Community-based organizations that provide suicide-prevention services can now access about $52.5 million in US Department of Veterans Affairs (VA) grants. The grant is part of the 3-year Staff Sergeant Fox Suicide Prevention Grant Program, which honors Parker Gordon Fox, a sniper instructor at the U.S. Army Infantry School at Fort Benning, Georgia, who died by suicide in 2020. In consecutive Congressional hearings, lawmakers called for the reauthorization of the program to address gaps in VA care.
“It has been a game-changer for so many veterans,” Sen. Richard Blumenthal (D-CT) said.
The money provides or coordinates primarily nonclinical suicide prevention services, including outreach and linkage to VA and community resources. Services also may include baseline mental health screenings, case management and peer support, education on suicide risk, VA benefits assistance, and emergency clinical services.
Since its inception in 2022, the program has awarded $157.5 million to 95 organizations in 43 states, US territories, and tribal lands. Speaking before the House Committee on Veterans’ Affairs on May 15, VA Secretary Doug Collins praised the Fox program for bringing “different voices into the conversation,” but added it wasn’t enough. He noted that the veteran suicide rate has not changed since 2008, despite the VA annually spending $588 million on suicide prevention over the past few years.
In an op-ed, Russell Lemle, a senior policy analyst at the Veterans Healthcare Policy Institute, disputed Collins' characterization of veteran suicides. Between 2008 and 2022 (the last year for which complete data is available), US deaths by suicide increased 37% while the number of veteran deaths by suicide fell 2%. “This data collection was the single best part of the program,” he argued, calling for reauthorization to continue requiring data-targeted solutions.
According to a 2024 VA interim report on the Fox grant program, grantees had completed > 16,590 outreach contacts and engaged 3204 participants as of September 30, 2023. An additional 864 individuals were onboarding at the time of the report.
The current version of the grant program requires grantees to use validated tools, including the VA Data Collection Tool, and other assessments furnished by VA to determine the effectiveness of the suicide prevention services. They must also provide each participant with a satisfaction survey and submit periodic and annual financial and performance reports.
Despite the Trump administration’s cuts and cancellations to the federal workforce and federal programs, Collins told the Senate committee he is firmly on the side of working with community-based organizations like the Fox grant program to broaden the VA’s reach: “I want to use grants and programs like [the Fox grant program] to reach out beyond the scope of where we’re currently reaching, to say how can we actually touch the veteran that’s not being touched right now by these programs,” Collins said. “We’ve got to do better at using the grants, using our programs to go outside the normal bubble and use others to help get the word out.”
Grant applications are due in July and VA will choose awardees in September. Organizations can apply for grants worth up to $750,000 and may apply to renew awards from year to year throughout the length of the program.
Suicide Prevention Grant Program Reauthorized
Suicide Prevention Grant Program Reauthorized
Collins Lays Out Plans to Reduce VA by 15% in Congressional Hearings
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
US Department of Veterans Affairs (VA) Secretary Doug Collins testified in US House of Representatives and US Senate committees hearings that bringing staff numbers down to fiscal year 2019 figures was simply a goal: “Our goal, as we look at it, as everything goes forward, is a 15% decrease,” he told the senators. “It’s a goal. You have to start somewhere.”
“It’s a process we’re going through and I’m not going to work out a process in front of a committee or anywhere else,” Collins testified in the Senate on May 6, adding that it would be “incompetence” or “malpractice” to do so before time. “[When] we’re doing something as large as we are in an organization as sensitive on this Hill, it would not be right for us to do that in public. It would not be right for us to just come out and say here’s everything that we got and then have everybody scared because in the end it may not be the final decision.”
“We’re going to come to the best possible decision we can for the veterans in this country so they can have a VA system that actually works,” Collins argued in the Senate. “The VA’s been an issue for a long time. We’re trying to not make it an issue anymore.”
Collins later told a House committee on May 15 that VA was conducting a thorough review of department structure and staffing across the enterpise. "Our goal is to increase productivity and efficiency and to eliminate waste and bureaucracy improving health care delivery and benefits to our veterans. We are going to maintain VA essential jobs like doctors and nurses and claims processors" but eliminate positions it deemed "nonmission-critical" and consolidating areas of "overlap and waste."
Senate ranking member Richard Blumenthal (D-CT) and Chairman Jerry Moran (R-KS) both placed an emphasis on accountability for responsible resizing at the hearing.
“The department is at a critical juncture,” Moran said. “Perhaps that’s always true, and I want to hear from you that the changes under way at the VA are backed by data, informed by veteran demand, focused on improving outcomes for men and women the VA serves, and will be carried out in close coordination with this committee, as well as with veterans, VA staff, and veteran organizations.” Moran stressed that cutting should be about right-sizing, done carefully, and while treating people “with gratitude and respect.”
Blumenthal was more direct in his criticism of the approach: “You cannot slash and trash the VA without eliminating those essential positions which provide access and availability of health care. It simply cannot be done,” he told Collins.
In response, Collins replied, “You have stated on several occasions already that I am saying we are going to fire 83,000 employees. That is wrong.” Collins insisted that the VA was “looking at a goal of how many employees we have and how many employees that are actually working in the front line taking care. I have doctors and nurses right now that do not see patients. Is that helping veteran health care?”
Collins defended the actions of the VA and spoke about challenges he was “constantly fighting” in the early weeks of his tenure. “We’ve been hit by a barrage of false rumors, innuendo, disinformation, speculation implying firing doctors and nurses, and forcing staff to work in closets and showers and that there’s chaos in the department, none of which have been backed up. Why? Because we canceled some contracts that worked for the VA that we should be doing in-house and we let go of less than one half of one percent of nonmission critical employees.”
The Trump Administration offered federal employees the option of resigning, which purportedly will go toward meeting the 15% target. NPR reported that VA employees have since shared data showing that 11,273 agency employees nationwide have applied for deferred resignation. Most of those employees are nurses (about 1300), medical support assistants (about 800), and social workers (about 300).
Collins stressed that the aim of restructuring was to protect veterans’ health care. By getting rid of DEI initiatives, the VA saved $14 million, which he said was redirected to veterans with disabilities who need prosthetics.
Sen. Bernie Sanders (D-VT) addressed concerns about the existing shortage of clinicians at the VA, asking Collins what he was doing to bring in more doctors, nurses, and social workers. In addition to moving doctors and nurses from nonpatient care to patient care, Collins said, he planned to work with Congress to make salaries more competitive.
But money and adding more employees are not always the solution, Collins said. For example, he said, the VA has been spending $588 million a year veteran suicide research, its top clinical priority. Yet, he said there has not been a significant decrease in veteran suicide rates since 2008.
The most recent VA suicide report, released in 2024, indicates suicide rates have remained steady since 2001. However, in 2022, the number of suicides among veterans (6407) was actually lower than in 12 of the previous 14 years.
According to media reports, congressional lawmakers, and union officials, Veteran Crisis Line (VCL) staff were among the 2400 probationary employees fired in February. In a Feb. 20 video, Collins accused Democrats of spreading lies and insisted no one who answered the phone was fired.
Later, in a letter to senators, Collins admitted that 24 VCL support staff were “erroneously” sent termination notices. The firings were later reversed, Collins said, and all VCL employees had been reinstated at the same position they previously held. “Ensuring the VCL is always accessible 24/7 is one of the department’s top priorities,” Collins insisted.
Collins shared his approval of keeping and expanding VA programs and studies on psychedelic treatments for patients with posttraumatic stress disorder and traumatic brain injury. He also spoke to the proposed 2026 budget calling for a $5.4 billion increase for the VA. If approved, that money would be targeted for medical care and homelessness.
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Collins Lays Out Plans to Reduce VA by 15% in Senate Hearing
Multiagent AI Systems in Health Care: Envisioning Next-Generation Intelligence
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Artificial intelligence (AI) is rapidly evolving, with large language models (LLMs) marking a significant milestone in processing and generating human-like responses to natural language prompts. However, this advancement only signals the beginning of a more profound transformation in AI capabilities. The development of AI agents represents a new paradigm at the forefront of this evolution.
BACKGROUND
AI agents represent a leap forward from traditional LLM applications. While definitions may vary slightly among technology developers, the core concept remains: these agents are autonomous software entities designed to interact with their environment, make independent decisions, and execute tasks based on predefined goals.1-3 What sets AI agents apart is their combination of sophisticated components within structured architectures. At their core, AI agents incorporate an LLM for response generation, which is augmented by a suite of tools to optimize workflow and complete tasks, memory capabilities for personalized interactions, and autonomous reasoning. This combination allows AI agents to plan, create subtasks, gather information, and learn iteratively from their own experiences or other AI agents.
The true potential of this technology becomes apparent when multiple AI agents collaborate within multiagent AI systems. This concept introduces a new level of flexibility and capability in tackling complex tasks. Autogen, CrewAI, and LangChain offer various agent network configurations, including hierarchical, sequential, conditional, or even parallel task execution.4-6 This adaptability opens up a world of possibilities across various industries, but perhaps nowhere is the potential impact more exciting and profound than in health care.
AI agents in health care present an opportunity to revolutionize patient care, streamline administrative processes, and support complex clinical decision-making. This review examines 3 scenarios that illustrate the impact of AI agents in health care: a hypothetical sepsis management system, chronic disease management, and hospital patient flow optimization. This article will provide a detailed look at the technical implementation challenges, including the integration with existing health care IT systems, data privacy considerations, and the crucial role of explainable AI in maintaining trust and transparency.
It is challenging to implement AI agents in health care. Concerns include ensuring data quality and mitigating bias, seamlessly integrating these systems into existing clinical workflows, and navigating the complex ethical considerations that arise when deploying autonomous systems in health care. The integration with Internet of Things (IoT) devices for real-time patient data monitoring and the development of more sophisticated natural language interfaces to enhance future human-AI collaboration.
The adoption of AI agents in health care is only beginning, and it promises to be transformative. As AI continues to evolve, a comprehensive understanding of its applications, limitations, and ethical considerations is essential. This report provides a comprehensive overview of the current state, potential applications, and future directions of AI agents in health care, offering insights valuable to researchers, clinicians, and policymakers.
MultiAgent AI architecture
Sepsis Management
Despite advancements in broad-spectrum antibiotics, imaging, and life support systems, mortality rates associated with sepsis remain high. The complexity of optimizing care in clinical settings has hindered progress in managing sepsis. Previous attempts to develop predictive sepsis models have proven challenging.7 This report proposes a multiagent AI system designed to enhance comprehensive patient monitoring and care through coordinated AI-driven interventions.
Data Collection and Integration Agent. Powered by a controlled vocabulary to specify all data, the primary function for the data collection and integration agent is to clean, transform, and organize patient data from structured and unstructured sources. This agent prepares succinct summaries of consultant notes and formats data for human and machine consumption. All numerical data are presented graphically, including relevant historical data trends. The agent also digitally captures all orders in a structured format using a specified controlled vocabulary. This structured data feed supports the output of other agents, including documentation, treatment planning, and risk stratification, while also supplying the data structures for future training.
Diagnostic Agent. Critical illness is characterized by multiple abnormalities across a wide array of tests, ranging from plain chest X-ray, computed tomography (CT), blood cell composition, plasma chemistry, and microscopic evaluation of specimens. Additionally, life support parameters provide insights into disease severity and can inform management recommendations. These data offer a wide array of visual and numerical data to be used as input for computation, recommendation, and further training. For example, to evaluate fluid overload on chest X-rays or tissue histopathology slides, an AI agent can leverage deep learning models such as convolutional neural networks and vision transformers to analyze images like radiographs and histopathology slides.8,9 Recurrent neural networks or transformer models process sequential data like time-series vital signs. The agent also implements ensemble methods that combine multiple machine learning algorithms to enhance diagnostic accuracy.
Risk Stratification Agent. This assesses severity and predicts potential outcomes. Morbidity and mortality risks are calculated using an established scoring system and individualized based on the history of other agents’ conditional patients. These are presented graphically, with major risk factors highlighted for explainability.
Treatment Recommendation Agent. Using a reinforcement learning framework supplemented by up-to-date clinical guidelines, this system leverages historical data structured with standardized vocabulary to analyze patients with similar clinical features. Training is also conducted on the patient’s physiological data. All recommendations are presented via a dedicated user interface in a readable format, along with recommendations for editable, orderable items, references, and full-text snippets from previous research. Stop rules end computing if confidence in recommendations is too broad or no clear pathway can be computed with certainty, prompting human mitigation.
Resource Management Agent. This agent coordinates hospital resources using constraint programming techniques for optimal resource allocation, uses queueing theory models to predict and manage patient flow, and implements genetic algorithms for complex scheduling problems.10,11
Monitoring and Alert Agent. By tracking patients’ progress and alerting staff to changes, this agent uses anomaly detection algorithms to identify unusual patterns in patient data and implement time-series forecasting models, such as autoregressive integrated moving average and prophet, to predict future patient states. The agent also uses stream-processing techniques for real-time data analysis.12,13
Documentation and Reporting Agent. This agent maintains comprehensive medical records and generates reports. It employs advanced natural language processing techniques for automated report generation, uses advanced LLMs fine-tuned on medical corpora for narrative creation, and implements information-retrieval techniques to efficiently query patient records.
CLINICAL CASE STUDIES
To illustrate the functionality of a multiagent system, this report examines its application for managing sepsis. The data collection and integration agent continuously aggregates patient data from various sources, normalizing and timestamping it for consistent processing. The diagnostic agent analyzes this integrated data in real time, applying sepsis criteria and utilizing a deep learning model trained on a large sepsis dataset to detect subtle patterns.
The risk stratification agent calculates severity scores, such as the Sepsis-related Organ Failure Assessment (SOFA), quick SOFA (qSOFA), and Acute Physiology and Chronic Health Evaluation II, upon detecting a possible sepsis case.14 It predicts the likelihood of specific outcomes and estimates the potential trajectory of the patient’s condition for the next 24 to 48 hours. Based on this assessment, the treatment recommendation agent suggests an initial treatment plan, including appropriate antibiotics, fluid resuscitation protocols, and vasopressor recommendations, recommendations when indicated.
Concurrently, the resource management agent checks the availability of necessary resources and prioritizes allocation based on the severity. The monitoring agent tracks the patient’s response to interventions in real time, alerting the care team to any concerning changes or lack of expected improvement. Throughout this process, the documentation agent ensures that all actions, responses, and outcomes are meticulously recorded in a structured format and generates real-time updates for the patient’s electronic health record (EHR) and preparing summary reports for handoffs between care teams.
Administrative Workflow Support
Modern health care operations are resource-intensive, requiring coordination of advanced imaging, procedures, laboratory testing, and professional consultations.15 AI-powered health care administrative workflow systems are revolutionizing how medical facilities coordinate patient care. For patients with chronic cough, these systems seamlessly integrate scheduling, imaging, diagnostics, and follow-up care into a cohesive process that reduces administrative burden while improving patient outcomes. Through an intuitive interface and automated assistance, health care practitioners (HCPs) can track patient progress from initial consultation through diagnosis and treatment.
The process begins when an HCP enters a patient into the system, which triggers an automated CT scan scheduling system. The system considers factors like urgency, facility availability, and patient preferences to suggest optimal appointment times. Once imaging is complete, AI agents analyze the radiology reports, extract key findings, and generate structured summaries that highlight critical information such as “mild bronchial wall thickening with patchy ground-glass opacities” or “findings consistent with chronic bronchitis.”
Based on these findings, the system automatically generates evidence-based recommendations for follow-up care, such as pulmonology consultations or follow-up imaging in 3 months. These recommendations are presented to the ordering clinician, along with suggested appointment slots for specialist consultations. The system then manages the coordination of multiple appointments, ensuring each step in the patient’s care plan is properly sequenced and scheduled.
The entire process is monitored through a comprehensive dashboard that provides real-time updates on patient status, appointment schedules, and clinical recommendations. HCPs can track which patients require immediate attention, view upcoming appointments, and monitor the progress of ongoing care plans.
Multiagent AI Operation Optimization
Hospitals are complex entities that must function at different scales and respond in an agile, timely manner at all hours, deploying staff at various positions.16 A system of AI agents can receive signals from sensors monitoring foot traffic in the emergency department and trauma unit, as well as the availability of operating room staff, equipment, and intensive care unit beds. Smart sensors enable this monitoring through IoT networks. These networks benefit from advances in adaptive and consensus networking algorithms, along with recent advances in bioengineering and biocomputing.17
For example, in the case of imaging for suspected abdominal obstruction, an AI agent tasked with scheduling CTs could time the patient’s arrival based on acuity. Another AI agent could alert staff transporting the patient to the CT appointment, with the next location contingent on a clinical decision to proceed to the operating room. Yet another AI agent could summarize radiology interpretations and alert the surgery and anesthesia teams to a potential case, while others could notify operating room staff of equipment needs or reserve a bed. In this paradigm, AI agents facilitate more precise and timely communication between multiple staff members.
TECHNICAL IMPLEMENTATION
Large Language Models
Each agent uses a different LLM optimized for its specific task. For example, the diagnostic agent uses an LLM pretrained on a large corpus of biomedical literature and fine-tuned on a dataset of confirmed sepsis cases and their presentations.18 It implements few-shot learning techniques to adapt to rare or atypical presentations. The treatment recommendation agent also uses an LLM, employing a retrieval-augmented generation approach to access the latest clinical guidelines during inference. The documentation agent uses another advanced language model, fine-tuned on a large corpus of high-quality medical documentation, implementing controlled text generation techniques and utilizing a separate smaller model for real-time error checking and correction.
Interagent Quality Control
Agents learn from their own experience and the experience of other agents. They are equipped with user-defined rule-based and model-based systems for quality assurance, with clear stopping rules for human involvement and mitigation.
Sophisticated quality control measures bolster the system’s reliability, including ensemble techniques for result comparison, redundancy for critical tasks, and automatic human review for disagreements above a certain threshold. Each agent provides a calibrated confidence score with its output, used to weigh inputs in downstream tasks and trigger additional checks for low-confidence outputs.
A dedicated quality control agent monitors output from all agents, employing both supervised and unsupervised anomaly detection techniques. Feedback loops allow agents to evaluate the quality and utility of information received from other agents. The system implements a multiarmed bandit approach to dynamically adjust the influence of different agents based on their performance and periodically retrains agent models using federated learning techniques.19
Electronic Health Record Integration
Seamless EHR integration is crucial for practical implementation. The system has secure application programming interface access to various EHR platforms, implements OAuth 2.0 for authentication, and use HTTPS with perfect forward secrecy for all communications.20 It works with HL7 FHIR to ensure interoperability and uses SNOMED CT for clinical terminology to ensure semantic interoperability across different EHRs.21,22
The system implements a multilevel approval system for write-backs to EHRs, with different thresholds based on the information’s criticality. It uses digital signatures to ensure the integrity and nonrepudiation of AI-generated entries and implements blockchain technology to create an immutable and distributed ledger of all AI system actions.23
Decision Transparency
To ensure transparency in decision-making processes, the system applies techniques (eg, local interpretable model-agnostic explanations and Shapley additive explanations) to provide insights into agent decision-making processes.24-26 It provides customized visualizations for different stakeholders and allows users to explore alternative decision paths through what-if scenario modeling.27
The system provides calibrated confidence indicators for each recommendation or decision, implementing a novel confidence calibration agent that continuously monitors and adjusts confidence scores based on observed outcomes.
Continuous Learning and Adaptation
The system employs several techniques to remain current with evolving medical knowledge. Federated learning includes information from diverse datasets across multiple institutions without compromising patient privacy.28 A/B testing is used to safely deploy and compare new agent versions in controlled settings, implementing multiarmed bandit algorithms to efficiently explore new models while minimizing potential negative impacts. Human-in-the-loop learning and active learning techniques are used to incorporate feedback from HCPs and efficiently solicit expert input on the most informative data.29
CLINICAL IMPLICATIONS
The implementation of multiagent AI systems in health care has several potential benefits: enhanced diagnostic accuracy, personalized treatment, improved efficiency, continuous monitoring, and resource optimization. A recent review of AI sepsis predictive models exhibited superior results to standard clinical scoring methods like qSOFA.30 In oncology, such systems can result in more tailored treatments, enhancing outcomes.31 The implementation of an ambient dictation system can improve workflow and prevent HCP burnout.32
ETHICAL CONSIDERATIONS AND AI OVERSIGHT
Integrating AI agents into health care raises significant ethical considerations that must be carefully addressed to ensure equitable and effective care delivery. One primary concern involves cultural and linguistic competency, as AI systems may struggle with cultural nuances, idioms, and context-specific communication patterns. This becomes particularly challenging in regions with diverse ethnic populations or immigrant communities, where medical terminology may not have direct translations and cultural beliefs significantly influence health care decisions. AI systems also may inherit and amplify existing biases in health care delivery, whether through HCP bias reflected in training data, patient bias affecting acceptance of AI-assisted care, or demographic underrepresentation during system development.
AI agents present unique opportunities for improving health care access and outcomes through community engagement, though such initiatives require thoughtful implementation. Predictive analytics can identify high-risk individuals within communities who may benefit from preventive care, while analysis of social determinants of health can enable more targeted interventions. However, these capabilities must be balanced with privacy concerns and the risk of surveillance, particularly in communities that distrust health care institutions. The potential for AI to bridge health care gaps must be weighed against the need to maintain cultural sensitivity and community trust.
The governance and oversight of health care AI systems requires a multistakeholder approach with clear lines of responsibility and accountability. This includes involvement from government health care agencies, professional medical associations, ethics boards, and independent auditors, all working together to establish and enforce standards while monitoring system performance and addressing potential biases. Health care organizations must maintain transparent policies about AI use, implement regular monitoring and evaluation protocols, and establish precise mechanisms for patient feedback and grievance resolution. Ongoing assessment and adjustment of these systems, informed by community feedback and outcomes data, will be crucial for their ethical implementation, ensuring that AI agents complement, rather than replace, human judgment and cultural sensitivity.
FUTURE DIRECTIONS
Despite the potential benefits, implementing multiagent AI systems in health care faces significant challenges that require careful consideration. Beyond the fundamental issues such as data quality and bias mitigation, health care organizations struggle with fragmented systems, inconsistent data formats, and varying quality. Technical infrastructure requirements are substantial, particularly in rural or underserved areas that lack robust networks and cybersecurity. HCPs already face significant cognitive load and time pressures, making integrating AI agents into existing workflows particularly challenging. There is also the critical issue of transparency and interpretability, as health care decisions require clear reasoning and accountability that many black-box AI systems struggle to provide.
The legal landscape introduces another layer of complexity, particularly regarding liability, consent, and privacy questions. When AI agents contribute to medical decisions, establishing clear lines of responsibility becomes crucial. There are also serious concerns about algorithmic fairness and the potential for AI systems to perpetuate or amplify existing inequities. The cost of implementation remains a significant barrier, requiring substantial investment in technology, training, and ongoing maintenance while ensuring resources are not diverted from direct patient care. Moreover, HCPs may resist adoption due to concerns about job security, loss of autonomy, or skepticism about AI capabilities while paradoxically facing risks of overreliance on AI systems that could lead to the degradation of human clinical skills.
Addressing these challenges requires a multifaceted approach that combines technical solutions with organizational and policy changes. Health care organizations must implement rigorous data validation processes and interoperability standards while developing hybrid models that balance sophisticated AI capabilities with interpretable techniques. Extensive research and iterative design processes, with direct input from HCPs, are essential for successful integration. Establishing independent ethics boards to oversee system development and deployment, conducting multicenter randomized controlled trials, and creating clear regulatory frameworks will ensure safe and effective implementation. Success will ultimately depend on ongoing collaboration between technology developers, HCPs, policymakers, and patients, maintaining a steady focus on improving patient care and outcomes while carefully navigating the complex challenges of AI integration in health care.33-35
As multiagent AI systems in health care evolve, several exciting directions emerge. These include the integration of IoT and wearable devices, the development of more sophisticated natural language interfaces, and applying these systems to predictive maintenance of medical equipment.
CONCLUSIONS
The advent of multiagent AI systems in health care represents a paradigm shift in the approach to patient care, clinical decision making, and health care management. While these systems offer immense potential to transform health care delivery, their development and implementation must be guided by rigorous scientific validation, ethical considerations, and a patient-centered approach. The ultimate goal remains clear: harnessing the power of AI to improve patient outcomes, enhance the efficiency of health care delivery, and ultimately advance the health and well-being of patients.
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5
Amazon Web Services, Inc. What are AI agents? Agents in artificial intelligence explained. Accessed April 7, 2025. https://aws.amazon.com/what-is/ai-agents/
Gutowska A. What are AI agents? IBM. Accessed April 7, 2025. https://www.ibm.com/think/topics/ai-agents
Agent AI. Microsoft Research. Accessed April 7, 2025. https://www.microsoft.com/en-us/research/project/agent-ai
Microsoft. AutoGen. Accessed April 7, 2025. https://microsoft.github.io/autogen/
Crew AI. The Leading Multi-Agent Platform. CrewAI. Accessed April 7, 2025. https://www.crewai.com/
LangChain. Accessed April 7, 2025. https://www.langchain.com/
Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065-1070. doi:10.1001/jamainternmed.2021.2626
Willemink MJ, Roth HR, Sandfort V. Toward foundational deep learning models for medical imaging in the new era of transformer networks. Radiol Artif Intell. 2022;4(6):e210284. doi:10.1148/ryai.210284
Waqas A, Bui MM, Glassy EF, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255
Moreno-Carrillo A, Arenas LMÁ, Fonseca JA, Caicedo CA, Tovar SV, Muñoz-Velandia OM. Application of queuing theory to optimize the triage process in a tertiary emergency care (“ER”) department. J Emerg Trauma Shock. 2019;12(4):268-273. doi:10.4103/JETS.JETS_42_19
Pongcharoen P, Hicks C, Braiden PM, Stewardson DJ. Determining optimum genetic algorithm parameters for scheduling the manufacturing and assembly of complex products. Int J Prod Econ. 2002;78(3):311-322. doi:10.1016/S0925-5273(02)00104-4
Sardar I, Akbar MA, Leiva V, Alsanad A, Mishra P. Machine learning and automatic ARIMA/Prophet models-based forecasting of COVID-19: methodology, evaluation, and case study in SAARC countries. Stoch Environ Res Risk Assess. 2023;37(1):345-359. doi:10.1007/s00477-022-02307-x
Samosir J, Indrawan-Santiago M, Haghighi PD. An evaluation of data stream processing systems for data driven applications. Procedia Comput Sci. 2016;80:439-449. doi:10.1016/j.procs.2016.05.322
Asmarawati TP, Suryantoro SD, Rosyid AN, et al. Predictive value of sequential organ failure assessment, quick sequential organ failure assessment, acute physiology and chronic health evaluation II, and new early warning signs scores estimate mortality of COVID-19 patients requiring intensive care unit. Indian J Crit Care Med. 2022;26(4):466-473. doi:10.5005/jp-journals-10071-24170
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. doi:10.1186/s12913-018-2994-0
Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
Kouchaki S, Ding X, Sanei S. AI- and IoT-enabled solutions for healthcare. Sensors. 2024;24(8):2607. doi:10.3390/s24082607
Saab K, Tu T, Weng WH, et al. Capabilities of Gemini Models in Medicine. arXiv. doi:10.48550/arXiv.2404.18416
Villar SS, Bowden J, Wason J. Multi-armed bandit models for the optimal design of clinical trials: benefits and challenges. Stat Sci. 2015;30(2):199-215. doi:10.1214/14-STS504
Auth0. What is OAuth 2.0. Accessed April 7, 2025. https://auth0.com/intro-to-iam/what-is-oauth-2
HL7. Welcome to FHIR. Updated March 26, 2025. Accessed April 7, 2025. https://www.hl7.org/fhir/
SNOMED International. Accessed April 7, 2025. https://www.snomed.org
Hasselgren A, Kralevska K, Gligoroski D, Pedersen SA, Faxvaag A. Blockchain in healthcare and health sciences—a scoping review. Int J Med Inf. 2020;134:104040. doi:10.1016/j.ijmedinf.2019.104040
Ribeiro MT, Singh S, Guestrin C. “Why Should I Trust You?”: Explaining the predictions of any classifier. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. 2016:1135-1144. doi:10.1145/2939672.2939778
Ekanayake IU, Meddage DPP, Rathnayake U. A novel approach to explain the black-box nature of machine learning in compressive strength predictions of concrete using Shapley additive explanations (SHAP). Case Stud Constr Mater. 2022;16:e01059. doi:10.1016/j.cscm.2022.e01059
Alabi RO, Elmusrati M, Leivo I, Almangush A, Mäkitie AA. Machine learning explainability in nasopharyngeal cancer survival using LIME and SHAP. Sci Rep. 2023;13(1):8984. doi:10.1038/s41598-023-35795-0
Otto E, Culakova E, Meng S, et al. Overview of sankey flow diagrams: focusing on symptom trajectories in older adults with advanced cancer. J Geriatr Oncol. 2022;13(5):742-746. doi:10.1016/j.jgo.2021.12.017
Fereidooni H, Marchal S, Miettinen M, et al. SAFELearn: secure aggregation for private federated learning. In: 2021 IEEE security and privacy workshops (SPW). 2021:56-62. doi:10.1109/SPW53761.2021.00017
Linton DL, Pangle WM, Wyatt KH, Powell KN, Sherwood RE. Identifying key features of effective active learning: the effects of writing and peer discussion. Life Sci Educ. 2014;13(3):469-477. doi:10.1187/cbe.13-12-0242
Yang HS. Machine learning for sepsis prediction: prospects and challenges. Clin Chem. 2024;70(3):465-467. doi:10.1093/clinchem/hvae006
Liao J, Li X, Gan Y, et al. Artificial intelligence assists precision medicine in cancer treatment. Front Oncol. 2023;12. doi:10.3389/fonc.2022.998222
Tierney AA, Gayre G, Hoberman B, et al. Ambient artificial intelligence scribes to alleviate the burden of clinical documentation. NEJM Catal. 2024;5(3):CAT.23.0404. doi:10.1056/CAT.23.0404
Borkowski AA, Jakey CE, Thomas LB, Viswanadhan N, Mastorides SM. Establishing a hospital artificial intelligence committee to improve patient care. Fed Pract. 2022;39(8):334-336. doi:10.12788/fp.0299
Isaacks DB, Borkowski AA. Implementing trustworthy AI in VA high reliability health care organizations. Fed Pract.2024;41(2):40-43. doi:10.12788/fp.0454
Han R, Acosta JN, Shakeri Z, Ioannidis JPA, Topol EJ, Rajpurkar P. Randomized controlled trials evaluating artificial intelligence in clinical practice: a scoping review. Lancet Digit Health. 2024;6(5):e367-e373. doi:10.1016/S2589-7500(24)00047-5
Community Care Radiation Oncology Cost Calculations for a VA Medical Center
Community Care Radiation Oncology Cost Calculations for a VA Medical Center
William Kissick’s description of health care’s iron triangle in 1994 still resonates. Access, quality, and cost will always come at the expense of the others.1 In 2018, Congress passed the VA MISSION Act, allowing patients to pursue community care options for extended waits (> 28 days) or longer distance drive times of > 60 minutes for specialty care services, such as radiation oncology. According to Albanese et al, the VA MISSION Act sought to address gaps in care for veterans living in rural and underserved areas.2 The Veterans Health Administration (VHA) continues to increase community care spending, with a 13.8% increase in fiscal year 2024 and an expected cost of > $40 billion for 2025.3 One could argue this pays for access for remote patients and quality when services are unavailable, making it a direct application of the iron triangle.
The VA MISSION Act also bolstered the expansion of existing community care department staff to expediently facilitate and coordinate care and payments.2 Cost management and monitoring have become critical in predicting future staff requirements, maintaining functionality, and ensuring patients receive optimal care. The VHA purchases care through partner networks and defines these bundled health care services as standard episodes of care (SEOCs), which are “clinically related health care services for a specific unique illness or medical condition… over a defined period of time.”4 Medicare publishes its rates quarterly, and outpatient procedure pricing is readily available online.5 Along these same lines, the US Department of Veterans Affairs (VA) publishes a current list of available procedures and associated Current Procedure Technology (CPT) codes that are covered under its VA fee schedule for community care.
Unique challenges persist when using this system to accurately account for radiation oncology expenditures. This study was based on the current practices at the Richard L. Roudebush VA Medical Center (RLRVAMC), a large 1a hospital. A detailed analysis reveals the contemporaneous cost of radiation oncology cancer care from October 1, 2021, through February 1, 2024, highlights the challenges in SEOC definition and duration, communication issues between RLRVAMC and purchase partners, inconsistencies in billing, erroneous payments, and difficulty of cost categorization.
METHODS
Community care radiation oncology-related costs were examined from October 1, 2021, to February 1, 2024 for RLRVAMC, 6 months prior to billing data extraction. Figure 1 shows a simple radiation oncology patient pathway with consultation or visit, simulation and planning, and treatment, with codes used to check billing. It illustrates the expected relationships between the VHA (radiation oncology, primary, and specialty care) and community care (clinicians and radiation oncology treatment sites).
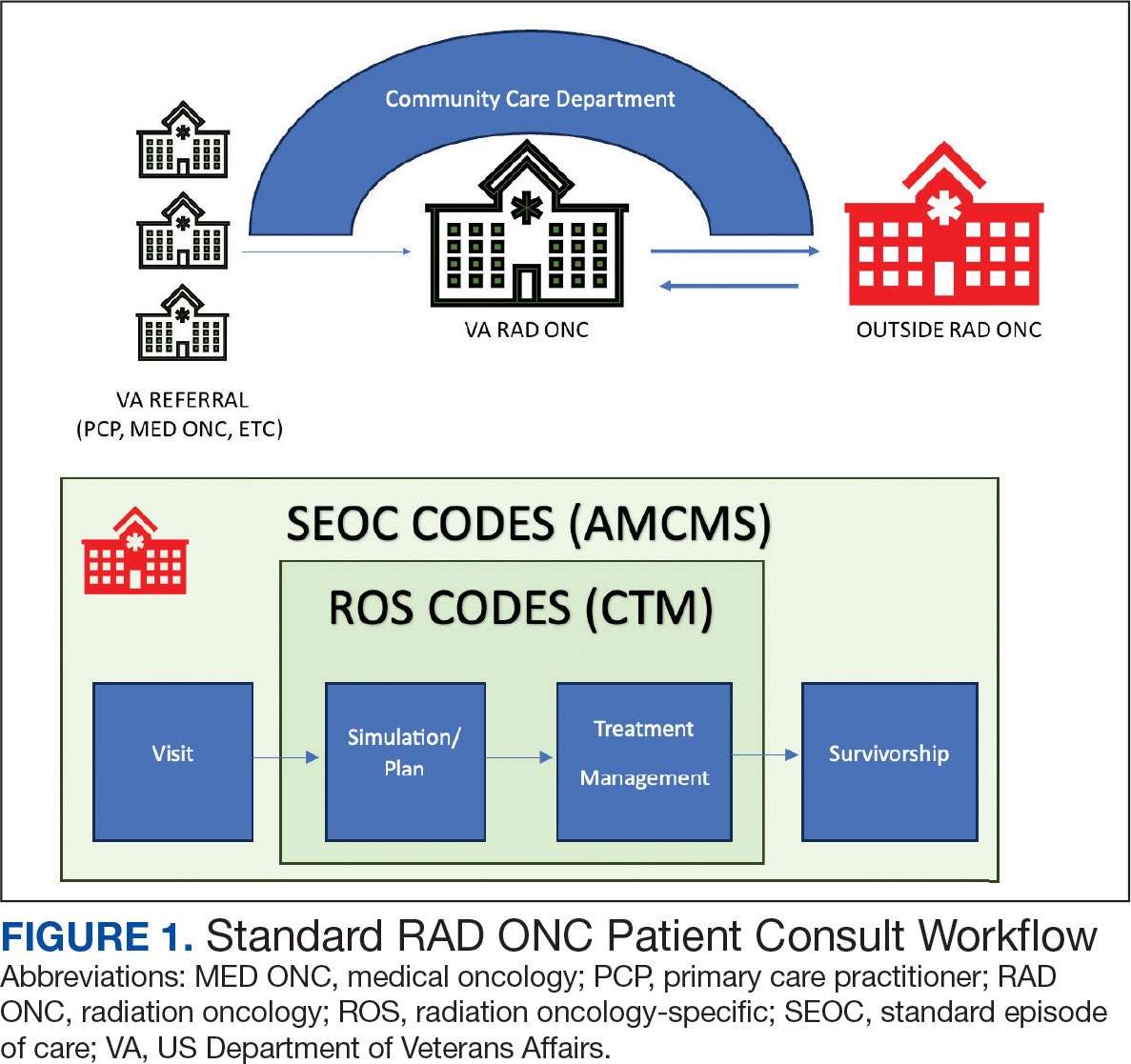
VHA standard operating procedures for a patient requesting community-based radiation oncology care require a board-certified radiation oncologist at RLRVAMC to review and approve the outside care request. Community care radiation oncology consultation data were accessed from the VA Corporate Data Warehouse (CDW) using Pyramid Analytics (V25.2). Nurses, physicians, and community care staff can add comments, forward consultations to other services, and mark them as complete or discontinued, when appropriate. Consultations not completed within 91 days are automatically discontinued. All community care requests from 2018 through 2024 were extracted; analysis began April 1, 2021, 6 months prior to the cost evaluation date of October 1, 2021.
An approved consultation is reviewed for eligibility by a nurse in the community care department and assigned an authorization number (a VA prefix followed by 12 digits). Billing codes are approved and organized by the community care networks, and all procedure codes should be captured and labeled under this number. The VAMC Community Care department obtains initial correspondence from the treating clinicians. Subsequent records from the treating radiation oncologist are expected to be scanned into the electronic health record and made accessible via the VA Joint Legacy Viewer (JLV) and Computerized Patient Record System (CPRS).
Radiation Oncology SEOC
The start date of the radiation oncology SEOC is determined by the community care nurse based on guidance established by the VA. It can be manually backdated or delayed, but current practice is to start at first visit or procedure code entry after approval from the VAMC Radiation Oncology department. Approved CPT codes from SEOC versions between October 1, 2021, and February 1, 2024, are in eAppendix 1 (available at doi:10.12788/fp.0585). These generally include 10 types of encounters, about 115 different laboratory tests, 115 imaging studies, 25 simulation and planning procedures, and 115 radiation treatment codes. The radiation oncology SEOCs during the study period had an approval duration of 180 days. Advanced Medical Cost Management Solutions software (AMCMS) is the VHA data analytics platform for community care medical service costs. AMCMS includes all individual CPT codes billed by specific radiation oncology SEOC versions. Data are refreshed monthly, and all charges were extracted on September 12, 2024, > 6 months after the final evaluated service date to allow for complete billing returns.6
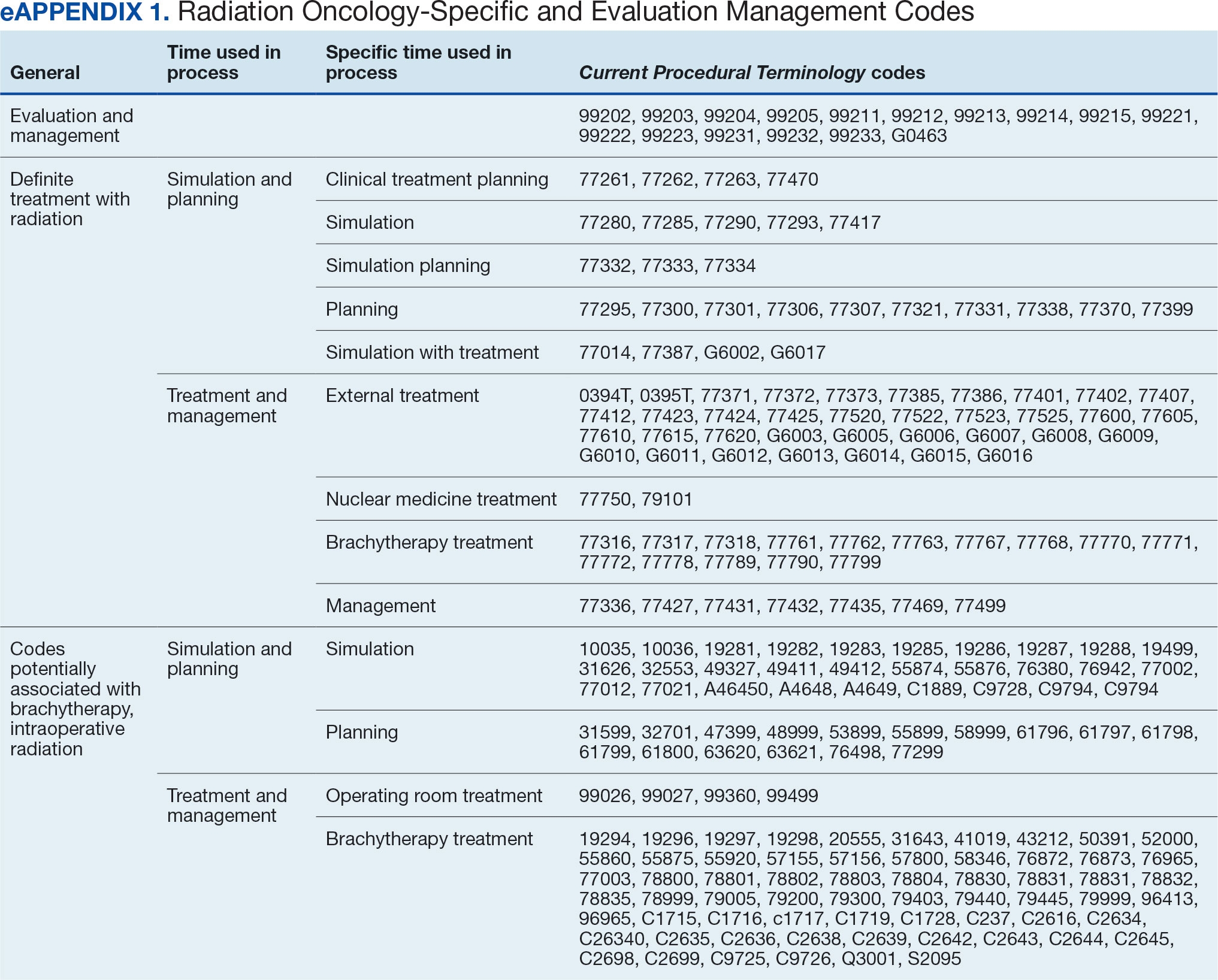
Radiation Oncology-Specific Costs
The VA Close to Me (CTM) program was used to find 84 specific radiation oncology CPT codes, nearly all within the 77.XXX or G6.XXX series, which included all radiation oncology-specific (ROS) codes (except visits accrued during consultation and return appointments). ROS costs are those that could not be performed by any other service and include procedures related to radiation oncology simulation, treatment planning, treatment delivery (with or without image guidance), and physician or physicist management. All ROS costs should be included in a patient’s radiation oncology SEOC. Other costs that may accompany operating room or brachytherapy administration did not follow a 77.XXX or G6.XXX pattern but were included in total radiation therapy operating costs.
Data obtained from AMCMS and CTM included patient name and identifier; CPT billed amount; CPT paid amount; dates of service; number of claims; International Classification of Diseases, Tenth Revision (ICD) diagnosis; and VA authorization numbers. Only CTM listed code modifiers. Only items categorized as paid were included in the analysis. Charges associated with discontinued consultations that had accrued costs also were included. Codes that were not directly related to ROS were separately characterized as other and further subcategorized.
Deep Dive Categorization
All scanned documents tagged to the community consultation were accessed and evaluated for completeness by a radiation oncologist (RS). The presence or absence of consultation notes and treatment summaries was evaluated based on necessity (ie, not needed for continuation of care or treatment was not given). In the absence of a specific completion summary or follow-up note detailing the treatment modality, number of fractions, and treatment sites, available documentation, including clinical notes and billing information, was used. Radical or curative therapies were identified as courses expected to eradicate disease, including stereotactic ablative radiotherapy to the brain, lung, liver, and other organs. Palliative therapies included whole-brain radiotherapy or other low-dose treatments. If the patient received the intended course, this was categorized as full. If incomplete, it was considered partial.
Billing Deviations
The complete document review allowed for close evaluation of paid therapy and identification of gaps in billing (eg, charges not found in extracted data that should have occurred) for external beam radiotherapy patients. Conversely, extra charges, such as an additional weekly treatment management charge (CPT code 77427), would be noted. Patients were expected to have the number of treatments specified in the summary, a clinical treatment planning code, and weekly treatment management notes from physicians and physicists every 5 fractions. Consultations and follow-up visits were expected to have 1 visit code; CPT codes 99205 and 99215, respectively, were used to estimate costs in their absence.
Costs were based on Medicare rates as of January 1 of the year in which they were accrued. 7-10 Duplicates were charges with the same code, date, billed quantity, and paid amounts for a given patient. These would always be considered erroneous. Medicare treatment costs for procedures such as intensity modulated radiotherapy (CPT code 77385 or 77386) are available on the Medicare website. When reviewing locality deviations for 77427, there was a maximum of 33% increase in Medicare rates. Therefore, for treatment codes, one would expect the range to be at least the Medicare rate and maximally 33% higher. These rates are negotiated with insurance companies, but this range was used for the purpose of reviewing and adjusting large data sets.
RESULTS
Since 2018, > 500 community care consults have been placed by radiation oncology for treatment in the community, with more following implementation of the VA MISSION Act. Use of radiation oncology community care services annually increased during the study period for this facility (Table 1, Figure 2). Of the 325 community care consults placed from October 1, 2021, to February 1, 2024, 248 radiation oncology SEOCs were recorded with charges for 181 patients (range, 1-5 SEOCs). Long drive time was the rationale for > 97% of patients directed to community care (Supplemental materials, available at doi:10.12788/fp.0585). Based on AMCMS data, $22.2 million was billed and $2.7 million was paid (20%) for 8747 CPT codes. Each community care interval cost the VA a median (range) of $5000 ($8-$168,000 (Figure 3).
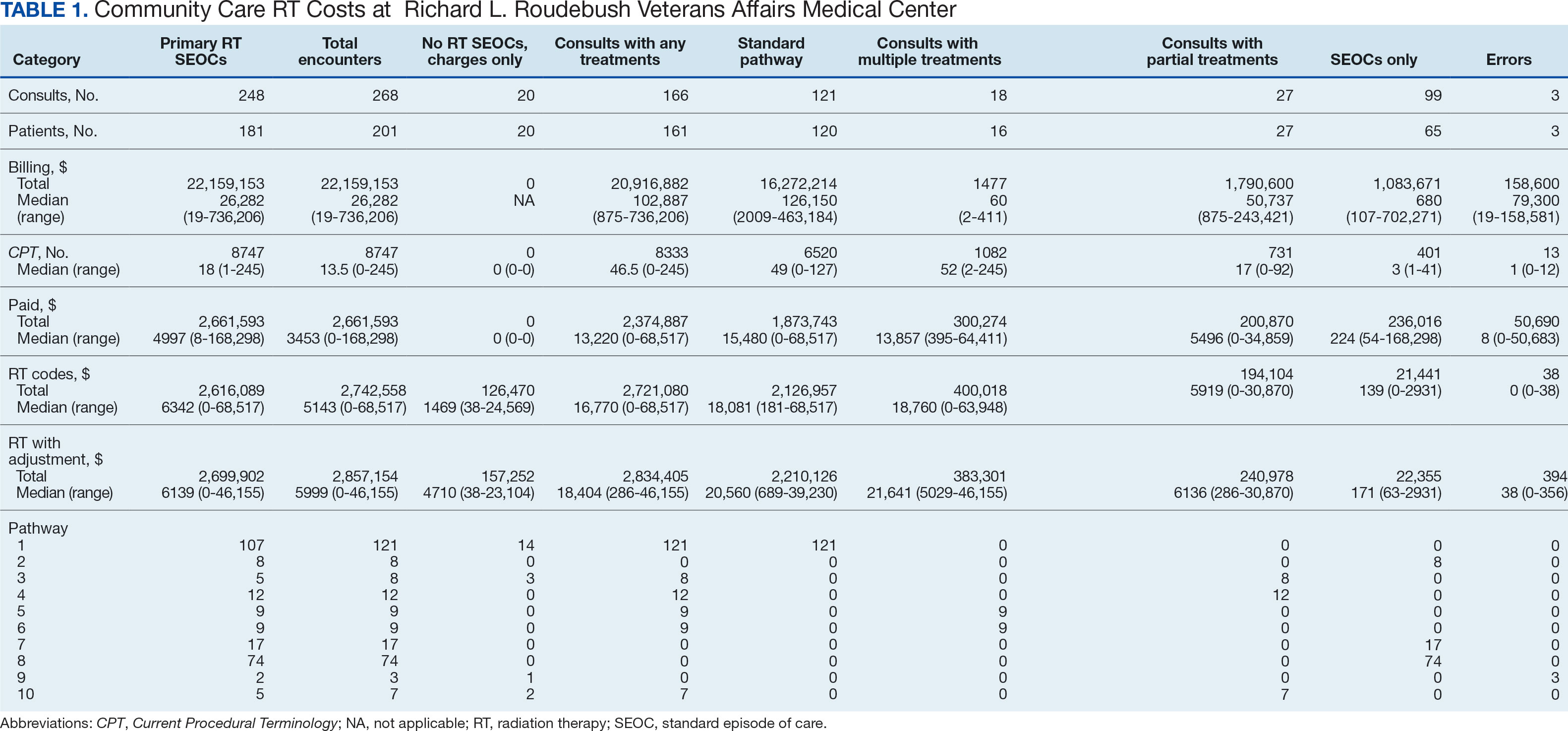
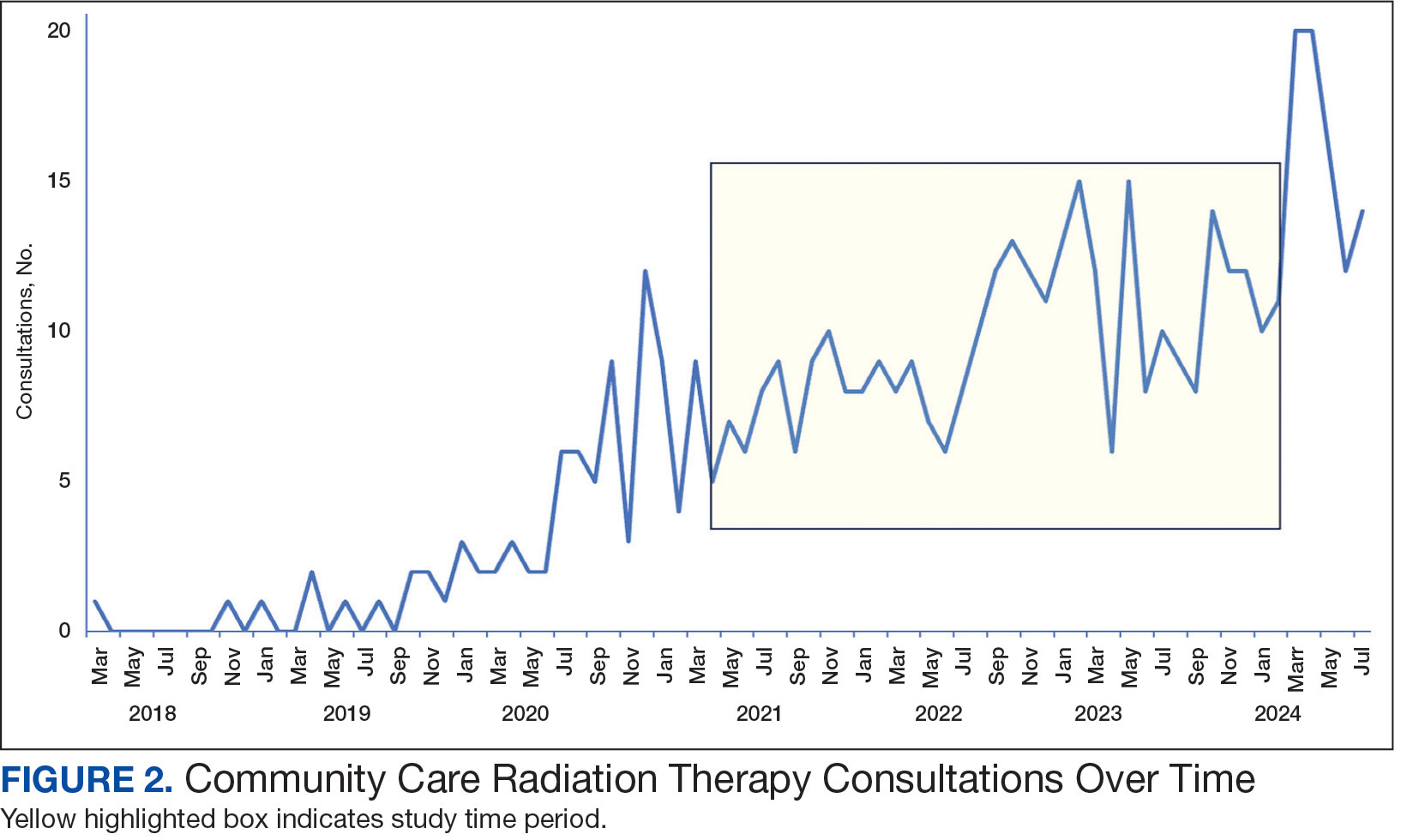
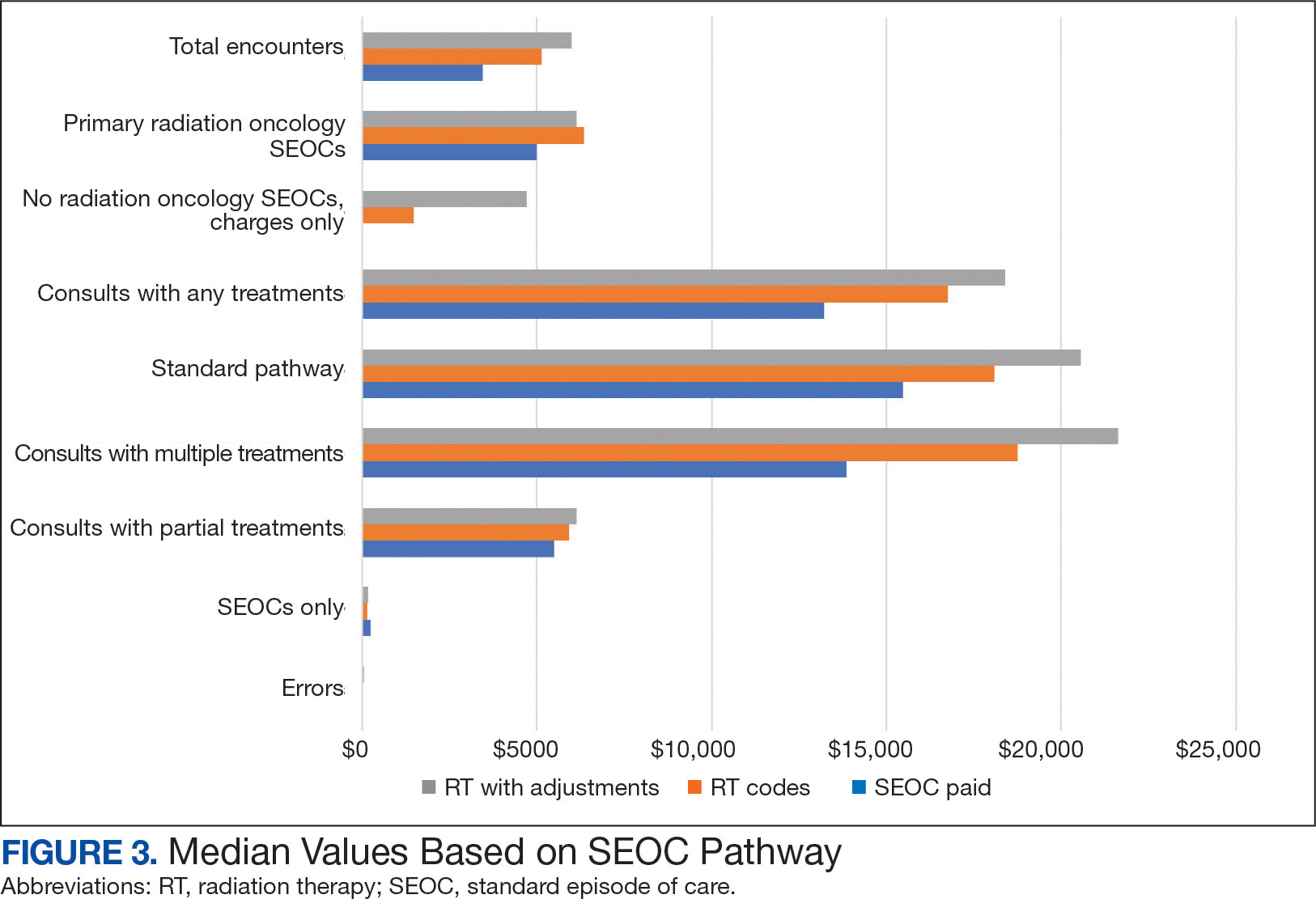
After reviewing ROS charges extracted from CTM, 20 additional patients had radiation oncology charges but did not have a radiation oncology SEOC for 268 episodes of care for 201 unique patients. In addition to the 20 patients who did not have a SEOC, 42 nonradiation oncology SEOCs contained 1148 radiation oncology codes, corresponding to almost $500,000 paid. Additional charges of about $416,000, which included biologic agents (eg, durvalumab, nivolumab), procedures (eg, mastectomies), and ambulance rides were inappropriately added to radiation oncology SEOCs.
While 77% of consultations were scanned into CPRS and JLV, only 54% of completion summaries were available with an estimated $115,000 in additional costs. The total adjusted costs was about $2.9 million. Almost 37% of SEOCs were for visits only. For the 166 SEOCs where patients received any radiation treatment or planning, the median cost was $18,000. Differences in SEOC pathways are shown in Figure 4. One hundred twenty-one SEOCs (45%) followed the standard pathway, with median SEOC costs of $15,500; when corrected for radiation-specific costs, the median cost increased to $18,000. When adjusted for billing irregularities, the median cost was $20,600. Ninety-nine SEOCs (37%) were for consultation/ follow-up visits only, with a median cost of $220. When omitting shared scans and nonradiation therapy costs and correcting for billing gaps, the median cost decreased to $170. A median of $9200 was paid per patient, with $12,900 for radiation therapy-specific costs and $13,300 adjusted for billing deviations. Narrowing to the 106 patients who received full, radical courses, the median SEOC, ROS, and adjusted radiation therapy costs increased to $19,400, $22,200, and $22,900, respectively (Table 2, Figure 5). Seventy-one SEOCs (26%) had already seen a radiation oncologist before the VA radiation oncology department was aware, and 49 SEOCs (18%) had retroactive approvals (Supplemental materials available at doi:10.12788/fp.0585).
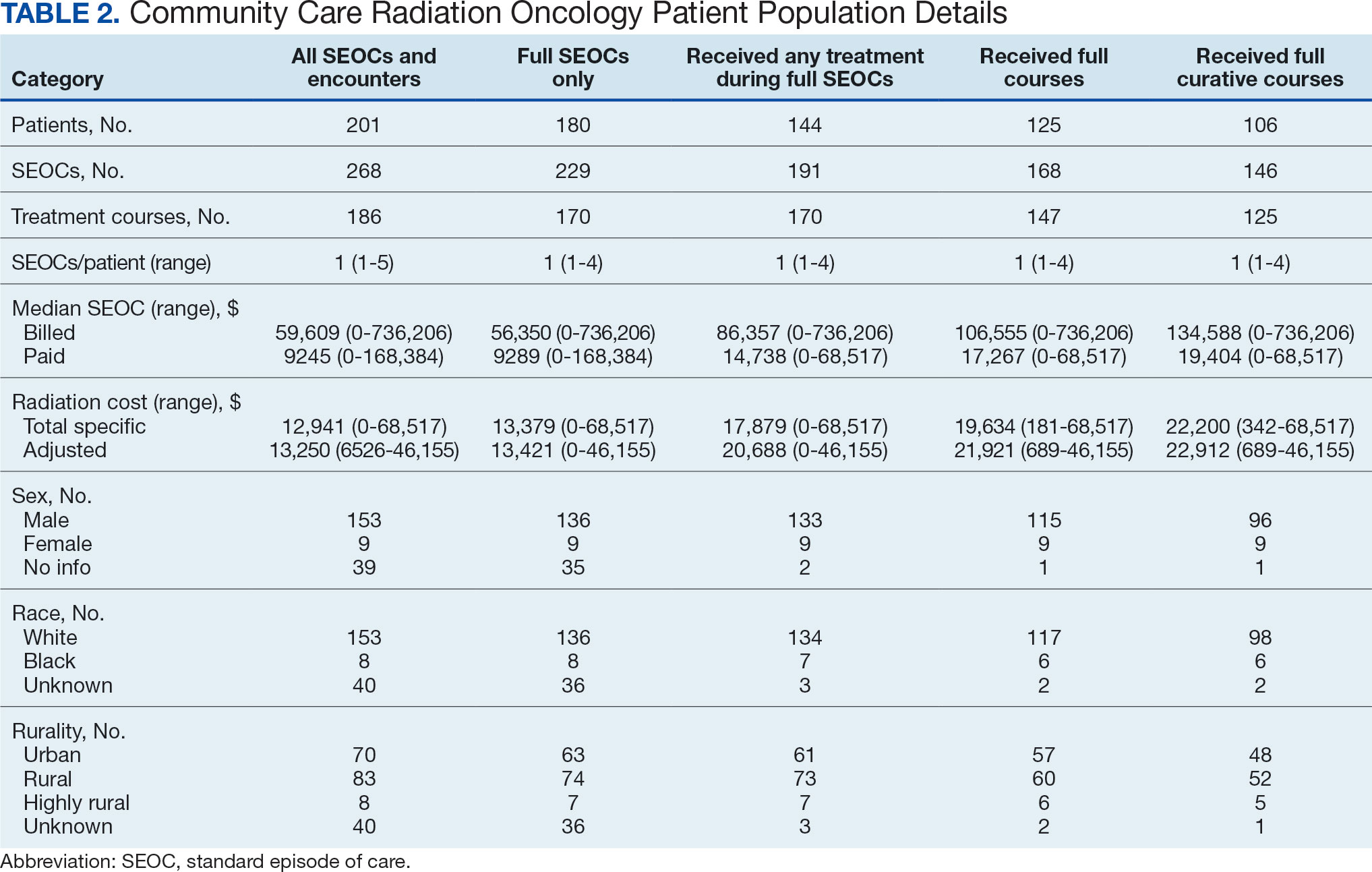
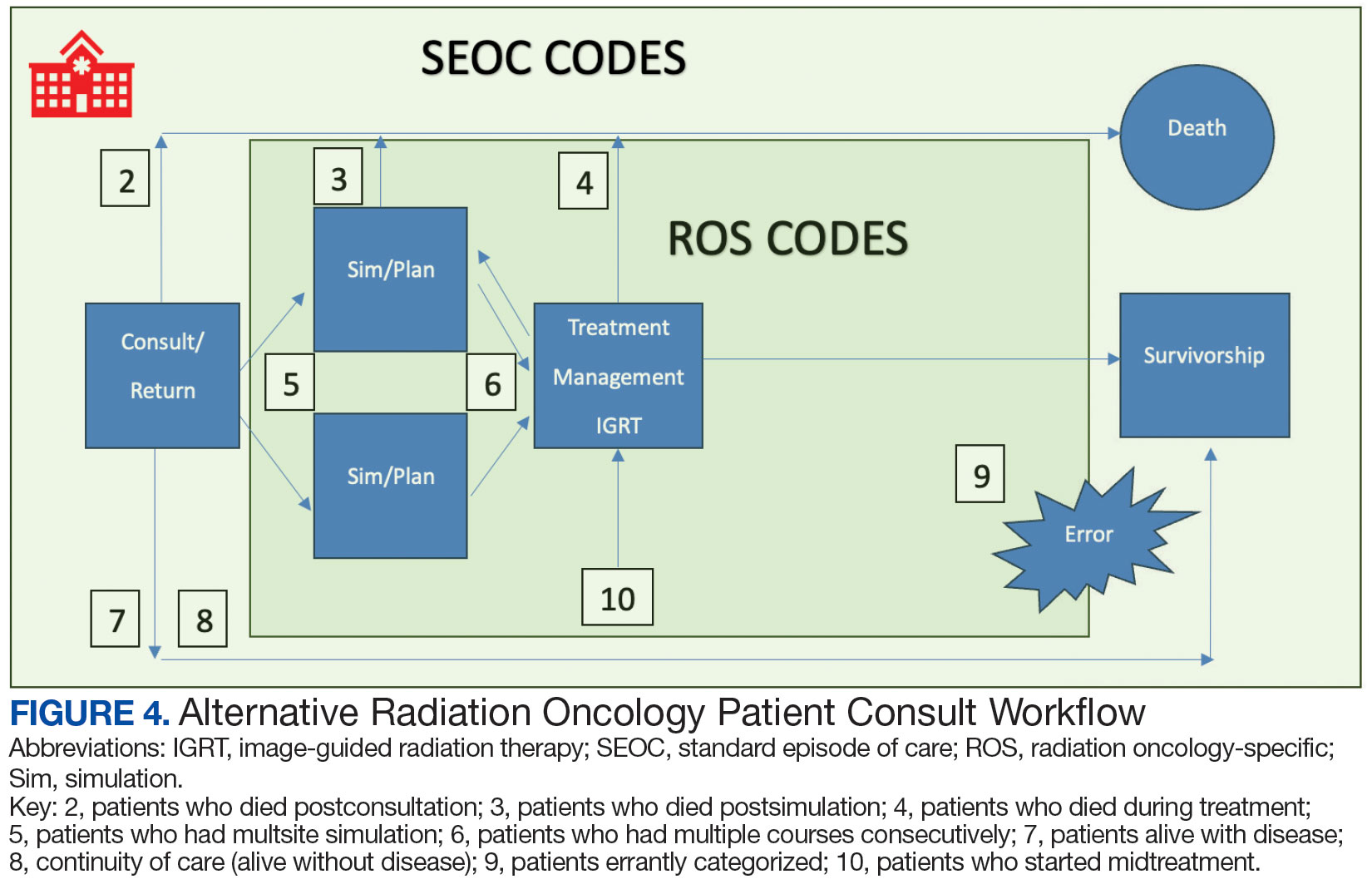
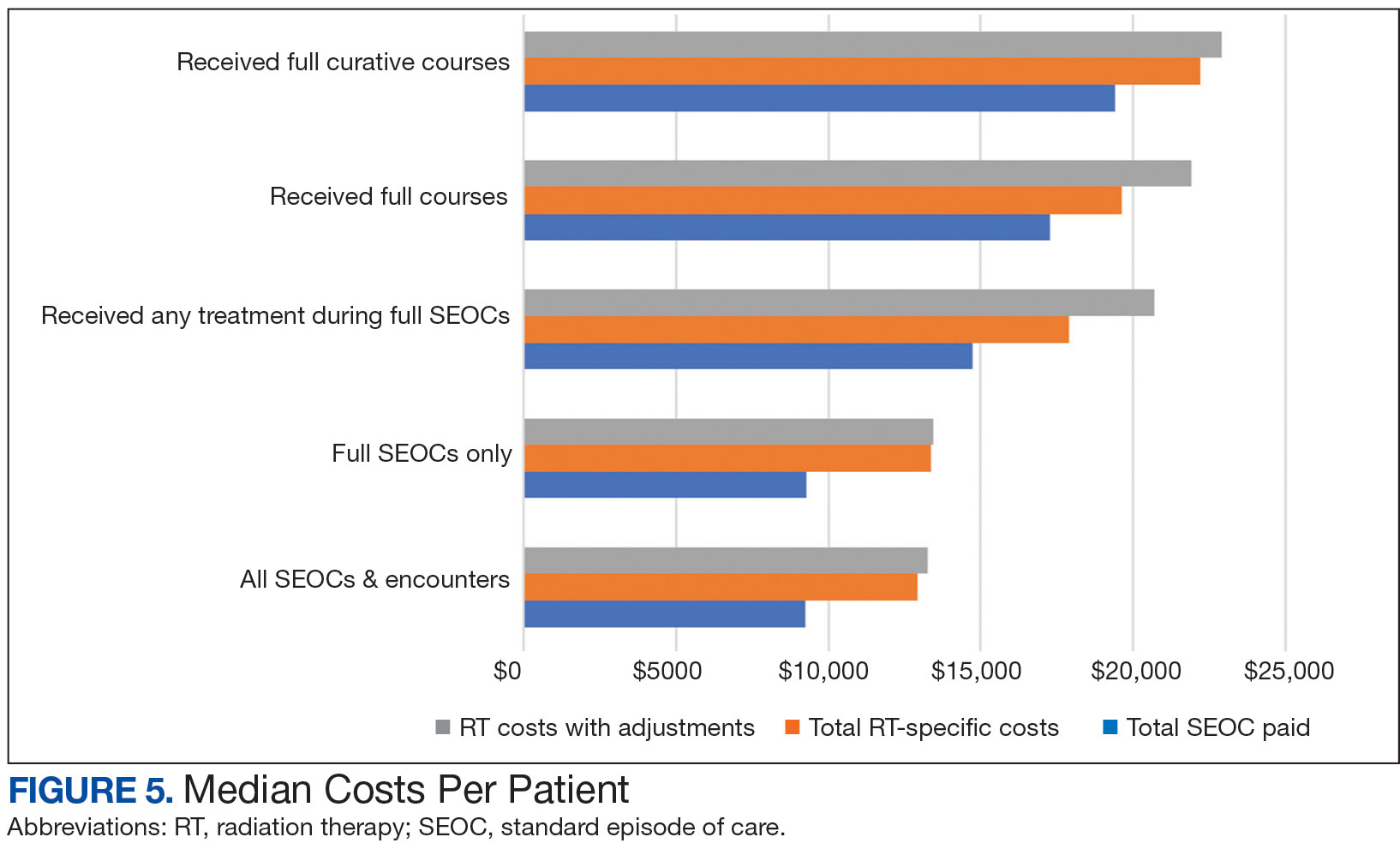
Every consultation charge was reviewed. A typical patient following the standard pathway (eAppendix 2, available at doi:10.12788/ fp.0585) exhibited a predictable pattern of consultation payment, simulation and planning, multiple radiation treatments interspersed with treatment management visits and a cone-down phase, and finishing with a follow-up visit. A less predictable case with excess CPT codes, gaps in charges, and an additional unexpected palliative course is shown in eAppendix 3 (available at doi:10.12788/fp.0585). Gaps occurred in 42% of SEOCs with missed bills costing as much as $12,000. For example, a patient with lung cancer had a treatment summary note for lung cancer after completion that showed the patient received 30 fractions of 2 Gy, a typical course. Only 10 treatment codes and 3 of 6 weekly treatment management codes were available. There was a gap of 20 volumetric modulated arc therapy treatments, 3 physics weekly status checks, 3 physician managements notes, and a computed tomography simulation charge.
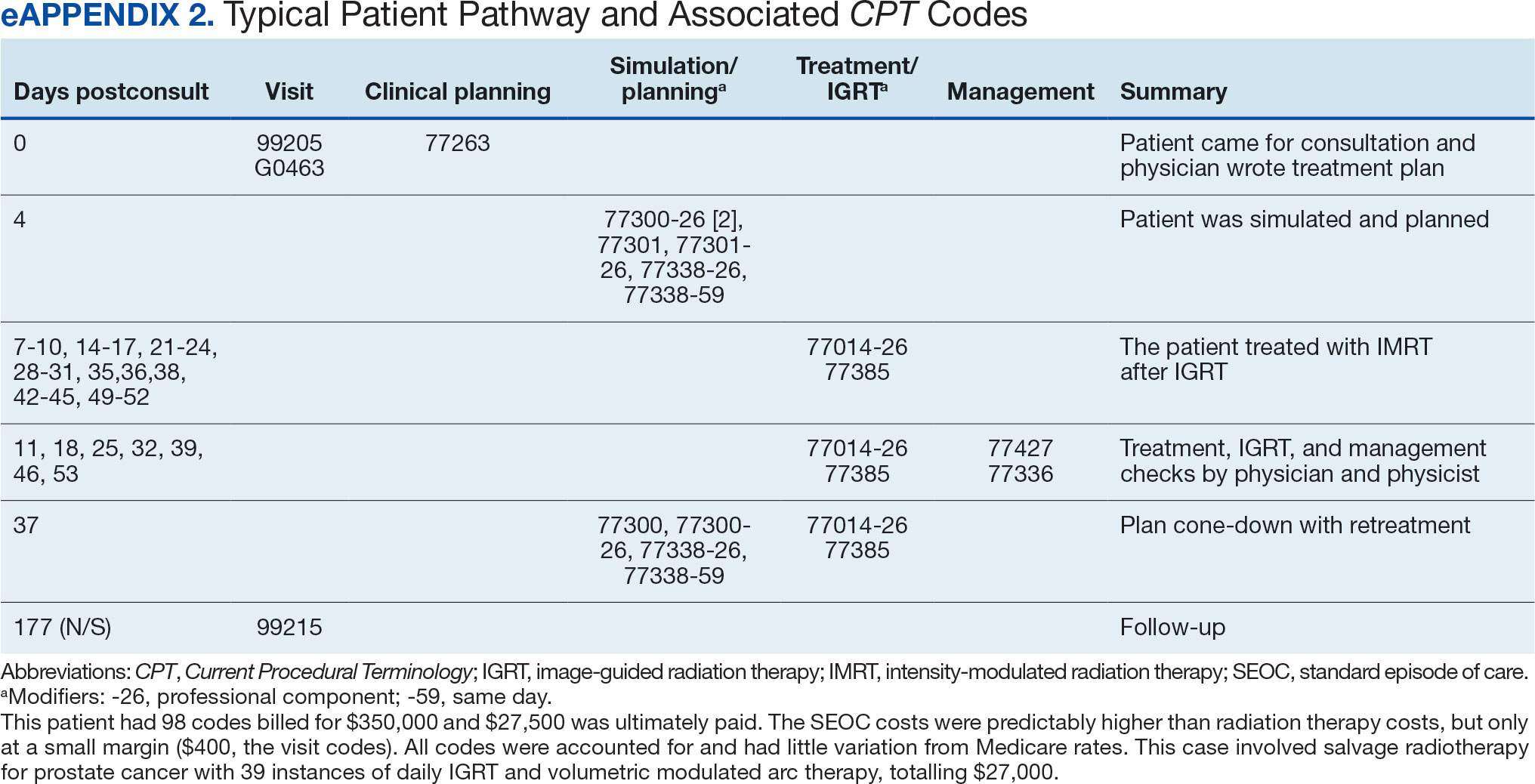

Between AMCMS and CTM, 10,005 CPT codes were evaluated; 1255 (12.5%) were unique to AMCMS (either related to the radiation oncology course, such as Evaluation and Management CPT codes or “other” unrelated codes) while 1158 (11.6%) were unique to CTM. Of the 7592 CPT codes shared between AMCMS and CTM, there was a discrepancy in 135 (1.8%); all were duplicates (CTM showed double payment while AMCMS showed $0 paid). The total CPT code costs came to $3.2 million with $560,000 unique to SEOCs and $500,000 unique to CTM. Treatment codes were the most common (33%) as shown in Table 3 and accounted for 55% of the cost ($1.8 million). About 700 CPT codes were considered “other,” typically for biologic therapeutic agents (Table 4 and eAppendix 4, available at doi:10.12788/fp.0585).
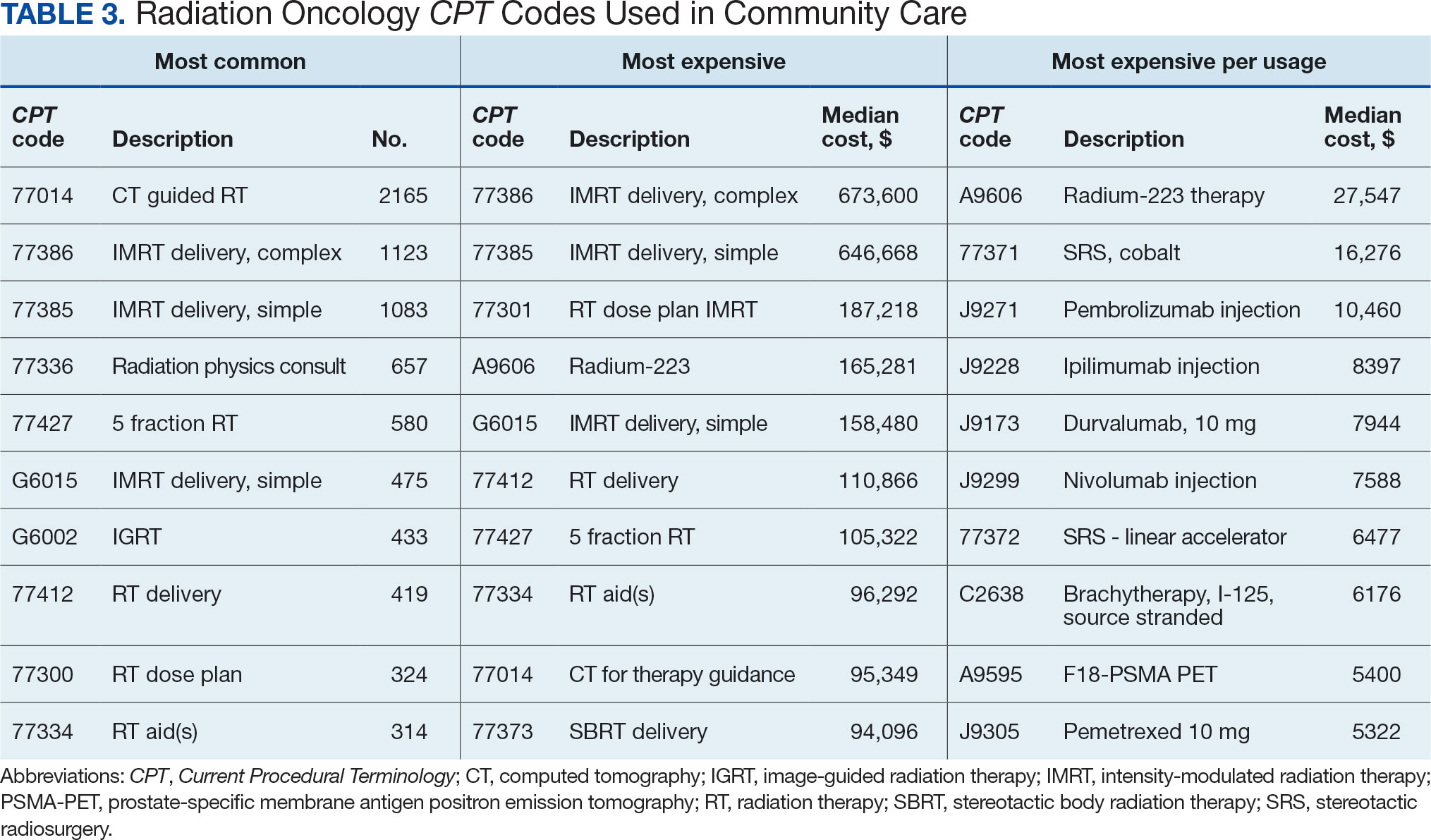
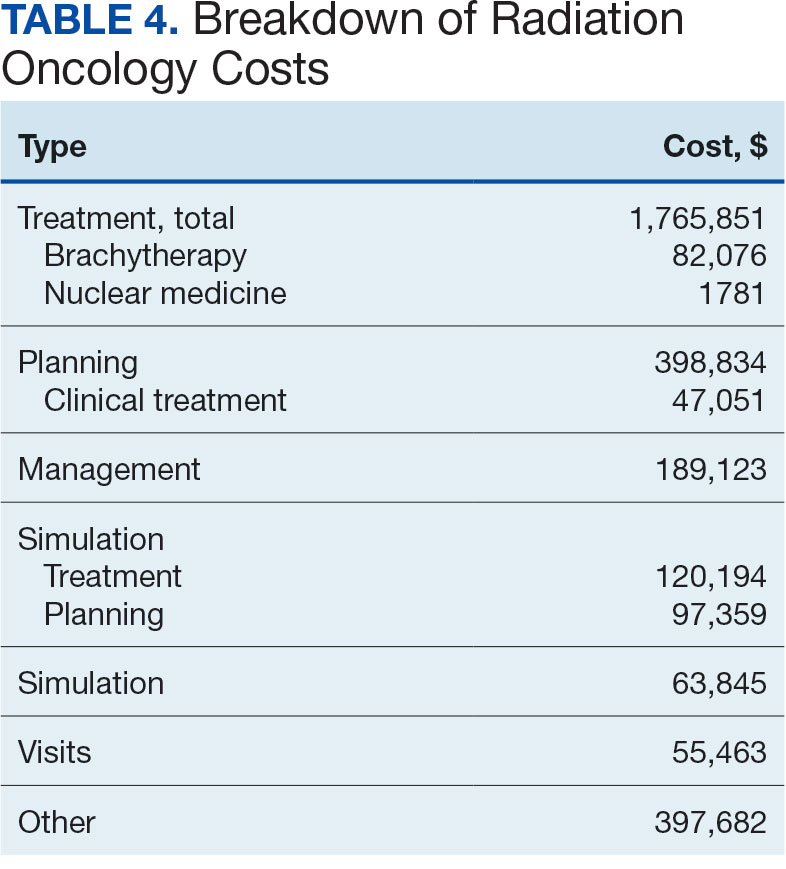

DISCUSSION
The current method of reporting radiation oncology costs used by VA is insufficient and misleading. Better data are needed to summarize purchased care costs to guide decisions about community care at the VA. Investigations into whether the extra costs for quality care (ie, expensive capital equipment, specialized staff, mandatory accreditations) are worthwhile if omitted at other facilities patients choose for their health care needs. No study has defined specialty care-specific costs by evaluating billing receipts from the CDW to answer the question. Kenamond et al highlight the need for radiation oncology for rural patients.11 Drive time was cited as the reason for community care referral for 97% of veterans, many of whom lived in rural locations. Of patients with rurality information who enrolled in community care, 57% came from rural or highly rural counties, and this ratio held for those who received full curative therapies. An executive administrator relying on AMCMS reports would see a median SEOC cost of $5000, but without ROS knowledge in coding, the administrator would miss many additional costs. For example, 2 patients who each had 5 SEOCs during the evaluated period, incurred a total cost of only $1800.
Additionally, an administrator could include miscategorized costs with significant ramifications. The 2 most expensive SEOCs were not typical radiation oncology treatments. A patient undergoing radium-223 dichloride therapy incurred charges exceeding $165,000, contributing disproportionately to the overall median cost analysis; this would normally be administered by the nuclear medicine department. Immunotherapy and chemotherapy are uniformly overseen by medical oncology services, but drug administration codes were still found in radiation oncology SEOCs. A patient (whose SEOC was discontinued but accrued charges) had an electrocardiogram interpretation for $8 as the SEOC cost; 3 other SEOCs continued to incur costs after being discontinued. There were 24 empty SEOCs for patients that had consults to the community, and 2 had notes stating treatment had been delivered yet there was no ROS costs or SEOC costs. Of the 268 encounters, 43% had some sort of billing irregularities (ie, missing treatment costs) that would be unlikely for a private practice to omit; it would be much more likely that the CDW miscategorized the payment despite confirmation of the 2 retrieval systems.
It would be inadvisable to make staffing decisions or forecast costs based on current SEOC reports without specialized curation. A simple yet effective improvement to the cost attribution process would be to restrict the analysis to encounters containing primary radiation treatment codes. This targeted approach allows more accurate identification of patients actively receiving radiation oncology treatment, while excluding those seen solely for consultations or follow-up visits. Implementing this refinement leads to a substantial increase in the median payment—from $5000 to $13,000—without requiring additional coding or data processing, thereby enhancing the accuracy of cost estimates with minimal effort.
Clarifying radiation oncology service costs requires addressing the time frame and services included, given laxity and interpretation of the SEOCs. VA community care departments have streamlined the reimbursement process at the expense of medical cost organization and accuracy; 86% of VA practitioners reported that ≥ 1 potential community health care partners had refused to work with the VA because of payment delays.12 Payments are contingent on correspondence from outside practices for community work. For radiation oncology, this includes the consultation but also critical radiation-related details of treatment, which were omitted nearly half the time. SEOC approval forms have many costly laboratory tests, imaging, and procedures that have little to do with radiation oncology cancer treatments but may be used in the workup and staging process; this creates noise when calculating radiation oncology fiscal cost.
The presumption that an episode of care equates to a completed radiation therapy course is incorrect; this occurs less than half of the time. An episode often refers to a return visit, or conversely, multiple treatment courses. As the patients’ medical homes are their VHA primary care practitioners, it would be particularly challenging to care for the patients without full treatment information, especially if adverse effects from therapy were to arise. As a tertiary specialty, radiation oncology does not seek out patients and are sent consultations from medical oncology, surgical, and medical oncologic specialties. Timesensitive processes such as workup, staging, and diagnosis often occur in parallel. This analysis revealed that patients see outside radiation oncologists prior to the VA. There are ≥ 100 patients who had radiation oncology codes without a radiation oncology SEOC or community care consultation, and in many cases, the consultation was placed after the patient was seen.
Given the lack of uniformity and standardization of patient traffic, the typical and expected pathways were insufficient to find the costs. Too many opportunities for errors and incorrect categorization of costs meant a different method would be necessary. Starting at the inception of the community care consult, only 1 diagnosis code can be entered. For patients with multiple diagnoses, one would not be able to tell what was treated without chart access. Radiation oncology consults come from primary and specialty care practitioners and nurses throughout the VA. Oftentimes, the referral would be solicited by the community radiation oncology clinic, diagnosing community specialty (ie, urology for a patient with prostate cancer), or indirectly from the patient through primary care. Many cases were retroactively approved as the veteran had already been consulted by the community care radiation oncologist. If the patient is drive-time eligible, it would be unlikely that they would leave and choose to return to the VA. There is no way for a facility VA service chief or administrator to mitigate VA community costs of care, especially as shown by the miscategorization of several codes. Database challenges exacerbate the issue: 1 patient changed her first and last name during this time frame, and 2 patients had the same name but different social security numbers. In order to strictly find costs between 2 discrete timepoints, 39 (15%) SEOCs were split and incomplete, and 6 SEOCs contained charges for 2 different patients. This was corrected, and all inadvertent charges were cancelled. Only 1 ICD code is allowed per community care consultation, so an investigation is required to find costs for patients with multiple sites of disease. Additionally, 5 of the patients marked for drive time were actually patients who received Gamma Knife and brachytherapy, services not available at the VA.
Hanks et al first attempted to calculate cost of radiation oncology services. External beam prostate cancer radiotherapy at 3 suburban California centers cost $6750 ($20,503 inflation adjusted) per patient before October 1984 and $5600 ($17,010 inflation adjusted) afterwards.13 According to the American Society for Radiation Oncology, Advocacy Radiation Oncology Case Rate Program Curative radiation courses should cost $20,000 to $30,000 and palliative courses should cost $10,000 to $15,000. These costs are consistent with totals demonstrated in this analysis and similar to the inflation-adjusted Hanks et al figures. Preliminary findings suggest that radiation treatment constituted more than half of the total expenditures, with a notable $4 million increase in adjusted cost compared to the Medicare rates, indicating significant variation. Direct comparisons with Medicaid or commercial payer rates remain unexplored.
Future Directions
During the study period, 201 patients received 186 courses of radiation therapy in the community, while 1014 patients were treated in-house for a total of 833 courses. A forthcoming analysis will directly compare the cost of in-house care with that of communitybased treatment, specifically breaking down expenditure differences by diagnosis. Future research should investigate strategies to align reimbursement with quality metrics, including the potential role of tertiary accreditation in incentivizing high-value care. Additional work is also warranted to assess patient out-ofpocket expenses across care settings and to benchmark VA reimbursement against Medicare, Medicaid, and private insurance rates. In any case, with the increasing possibility of fewer fractions for treatments such as stereotactic radiotherapy or palliative care therapy, there is a clear financial incentive to treat as frequently as allowed despite equal clinical outcomes.
CONCLUSIONS
Veterans increasingly choose to receive care closer to home if the option is available. In the VA iron triangle, cost comes at the expense of access but quantifying this has proved elusive in the cost accounting model currently used at the VA.1 The inclusion of all charges loosely associated with SEOCs significantly impairs the ability to conduct meaningful cost analyses. The current VA methodology not only introduces substantial noise into the data but also leads to a marked underestimation of the true cost of care delivered in community settings. Such misrepresentation risks driving policy decisions that could inappropriately reduce or eliminate in-house radiation oncology services. Categorizing costs effectively in the VA could assist in making managerial and administrative decisions and would prevent damaging service lines based on misleading or incorrect data. A system which differentiates between patients who have received any treatment codes vs those who have not would increase accuracy.
- Kissick W. Medicine’s Dilemmas: Infinite Needs Versus Finite Resources. 1st ed. Yale University Press; 1994.
- Albanese AP, Bope ET, Sanders KM, Bowman M. The VA MISSION Act of 2018: a potential game changer for rural GME expansion and veteran health care. J Rural Health. 2020;36(1):133-136. doi:10.1111/jrh.12360
- Office of Management and Budget (US). Budget of the United States Government, Fiscal Year 2025. Washington, DC: US Government Publishing Office; 2024. Available from: US Department of Veterans Affairs FY 2025 Budget Submission: Budget in Brief.
- US Department of Veterans Affairs. Veteran care claims. Accessed April 3, 2025. https://www.va.gov/COMMUNITYCARE/revenue-ops/Veteran-Care-Claims.asp
- US Centers for Medicare and Medicaid Services. Accessed April 3, 2025. Procedure price lookup https://www.medicare.gov/procedure-price-lookup
- US Department of Veterans Affairs. WellHive -Enterprise. Accessed April 3, 2025. https://department.va.gov/privacy/wp-content/uploads/sites/5/2023/05/FY23WellHiveEnterprisePIA.pdf
- US Centers for Medicare and Medicaid Services. RVU21a physician fee schedule, January 2021 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu21a
- US Centers for Medicare and Medicaid Services. RVU22a physician fee schedule, January 2022 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu22a
- US Centers for Medicare and Medicaid Services. RVU23a physician fee schedule, January 2023 release. Accessed April 3, 2025. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-relative-value-files/rvu23a
- US Centers for Medicare and Medicaid Services. RVU23a Medicare Physician Fee Schedule rates effective January 1, 2024, through March 8, 2024. Accessed on April 3, 2025. https://www.cms.gov/medicare/payment/fee-schedules/physician/pfs-relative-value-files/rvu24a
- Kenamond MC, Mourad WF, Randall ME, Kaushal A. No oncology patient left behind: challenges and solutions in rural radiation oncology. Lancet Reg Health Am. 2022;13:100289. doi:10.1016/j.lana.2022.100289
- Mattocks KM, Kroll-Desrosiers A, Kinney R, Elwy AR, Cunningham KJ, Mengeling MA. Understanding VA’s use of and relationships with community care providers under the MISSION Act. Med Care. 2021;59(Suppl 3):S252-S258. doi:10.1097/MLR.0000000000001545
- Hanks GE, Dunlap K. A comparison of the cost of various treatment methods for early cancer of the prostate. Int J Radiat Oncol Biol Phys. 1986;12(10):1879-1881. doi:10.1016/0360-3016(86)90334-2
- American Society of Radiation Oncology. Radiation oncology case rate program (ROCR). Accessed April 3, 2025. https://www.astro.org/advocacy/key-issues-8f3e5a3b76643265ee93287d79c4fc40/rocr
William Kissick’s description of health care’s iron triangle in 1994 still resonates. Access, quality, and cost will always come at the expense of the others.1 In 2018, Congress passed the VA MISSION Act, allowing patients to pursue community care options for extended waits (> 28 days) or longer distance drive times of > 60 minutes for specialty care services, such as radiation oncology. According to Albanese et al, the VA MISSION Act sought to address gaps in care for veterans living in rural and underserved areas.2 The Veterans Health Administration (VHA) continues to increase community care spending, with a 13.8% increase in fiscal year 2024 and an expected cost of > $40 billion for 2025.3 One could argue this pays for access for remote patients and quality when services are unavailable, making it a direct application of the iron triangle.
The VA MISSION Act also bolstered the expansion of existing community care department staff to expediently facilitate and coordinate care and payments.2 Cost management and monitoring have become critical in predicting future staff requirements, maintaining functionality, and ensuring patients receive optimal care. The VHA purchases care through partner networks and defines these bundled health care services as standard episodes of care (SEOCs), which are “clinically related health care services for a specific unique illness or medical condition… over a defined period of time.”4 Medicare publishes its rates quarterly, and outpatient procedure pricing is readily available online.5 Along these same lines, the US Department of Veterans Affairs (VA) publishes a current list of available procedures and associated Current Procedure Technology (CPT) codes that are covered under its VA fee schedule for community care.
Unique challenges persist when using this system to accurately account for radiation oncology expenditures. This study was based on the current practices at the Richard L. Roudebush VA Medical Center (RLRVAMC), a large 1a hospital. A detailed analysis reveals the contemporaneous cost of radiation oncology cancer care from October 1, 2021, through February 1, 2024, highlights the challenges in SEOC definition and duration, communication issues between RLRVAMC and purchase partners, inconsistencies in billing, erroneous payments, and difficulty of cost categorization.
METHODS
Community care radiation oncology-related costs were examined from October 1, 2021, to February 1, 2024 for RLRVAMC, 6 months prior to billing data extraction. Figure 1 shows a simple radiation oncology patient pathway with consultation or visit, simulation and planning, and treatment, with codes used to check billing. It illustrates the expected relationships between the VHA (radiation oncology, primary, and specialty care) and community care (clinicians and radiation oncology treatment sites).
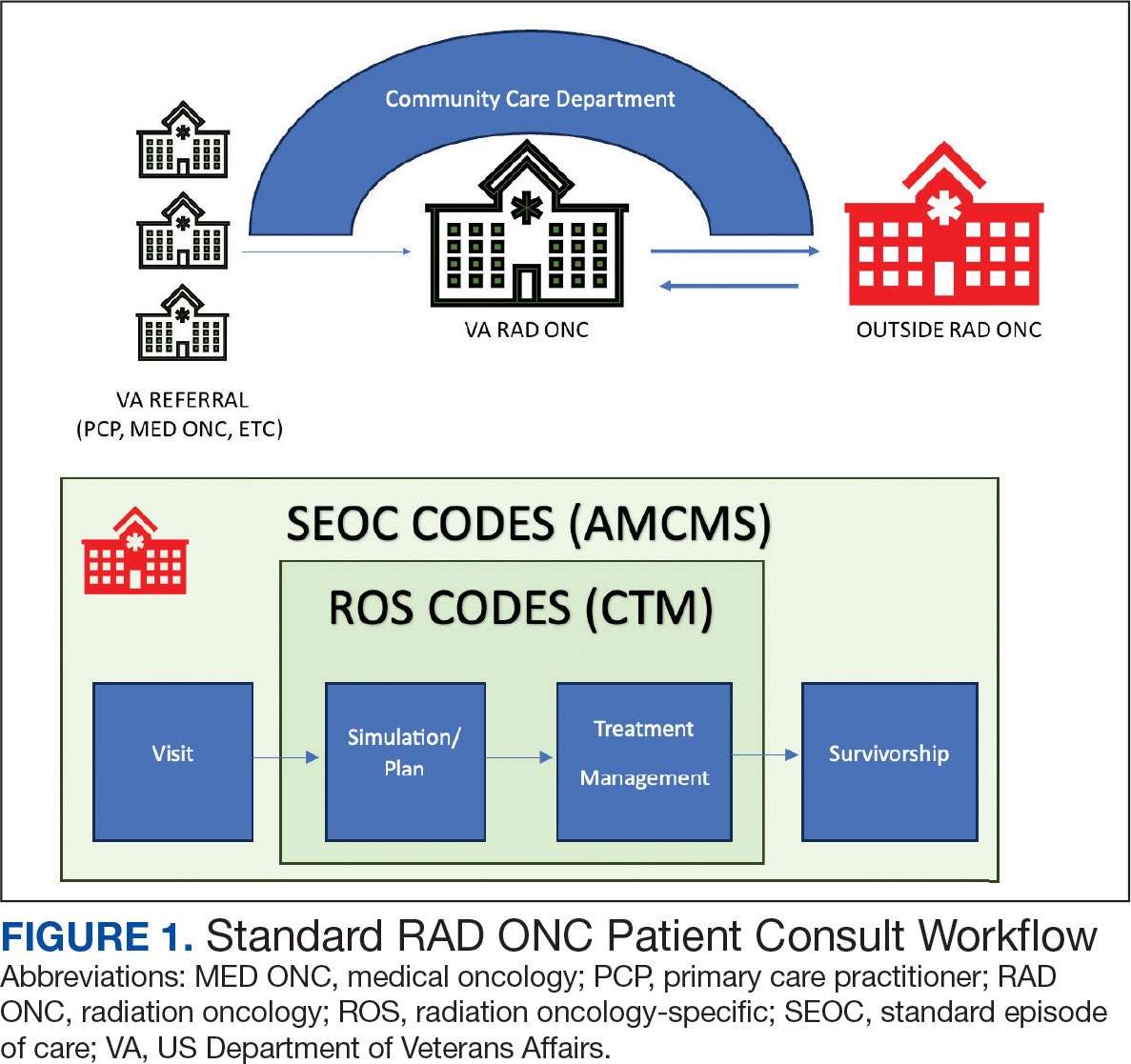
VHA standard operating procedures for a patient requesting community-based radiation oncology care require a board-certified radiation oncologist at RLRVAMC to review and approve the outside care request. Community care radiation oncology consultation data were accessed from the VA Corporate Data Warehouse (CDW) using Pyramid Analytics (V25.2). Nurses, physicians, and community care staff can add comments, forward consultations to other services, and mark them as complete or discontinued, when appropriate. Consultations not completed within 91 days are automatically discontinued. All community care requests from 2018 through 2024 were extracted; analysis began April 1, 2021, 6 months prior to the cost evaluation date of October 1, 2021.
An approved consultation is reviewed for eligibility by a nurse in the community care department and assigned an authorization number (a VA prefix followed by 12 digits). Billing codes are approved and organized by the community care networks, and all procedure codes should be captured and labeled under this number. The VAMC Community Care department obtains initial correspondence from the treating clinicians. Subsequent records from the treating radiation oncologist are expected to be scanned into the electronic health record and made accessible via the VA Joint Legacy Viewer (JLV) and Computerized Patient Record System (CPRS).
Radiation Oncology SEOC
The start date of the radiation oncology SEOC is determined by the community care nurse based on guidance established by the VA. It can be manually backdated or delayed, but current practice is to start at first visit or procedure code entry after approval from the VAMC Radiation Oncology department. Approved CPT codes from SEOC versions between October 1, 2021, and February 1, 2024, are in eAppendix 1 (available at doi:10.12788/fp.0585). These generally include 10 types of encounters, about 115 different laboratory tests, 115 imaging studies, 25 simulation and planning procedures, and 115 radiation treatment codes. The radiation oncology SEOCs during the study period had an approval duration of 180 days. Advanced Medical Cost Management Solutions software (AMCMS) is the VHA data analytics platform for community care medical service costs. AMCMS includes all individual CPT codes billed by specific radiation oncology SEOC versions. Data are refreshed monthly, and all charges were extracted on September 12, 2024, > 6 months after the final evaluated service date to allow for complete billing returns.6
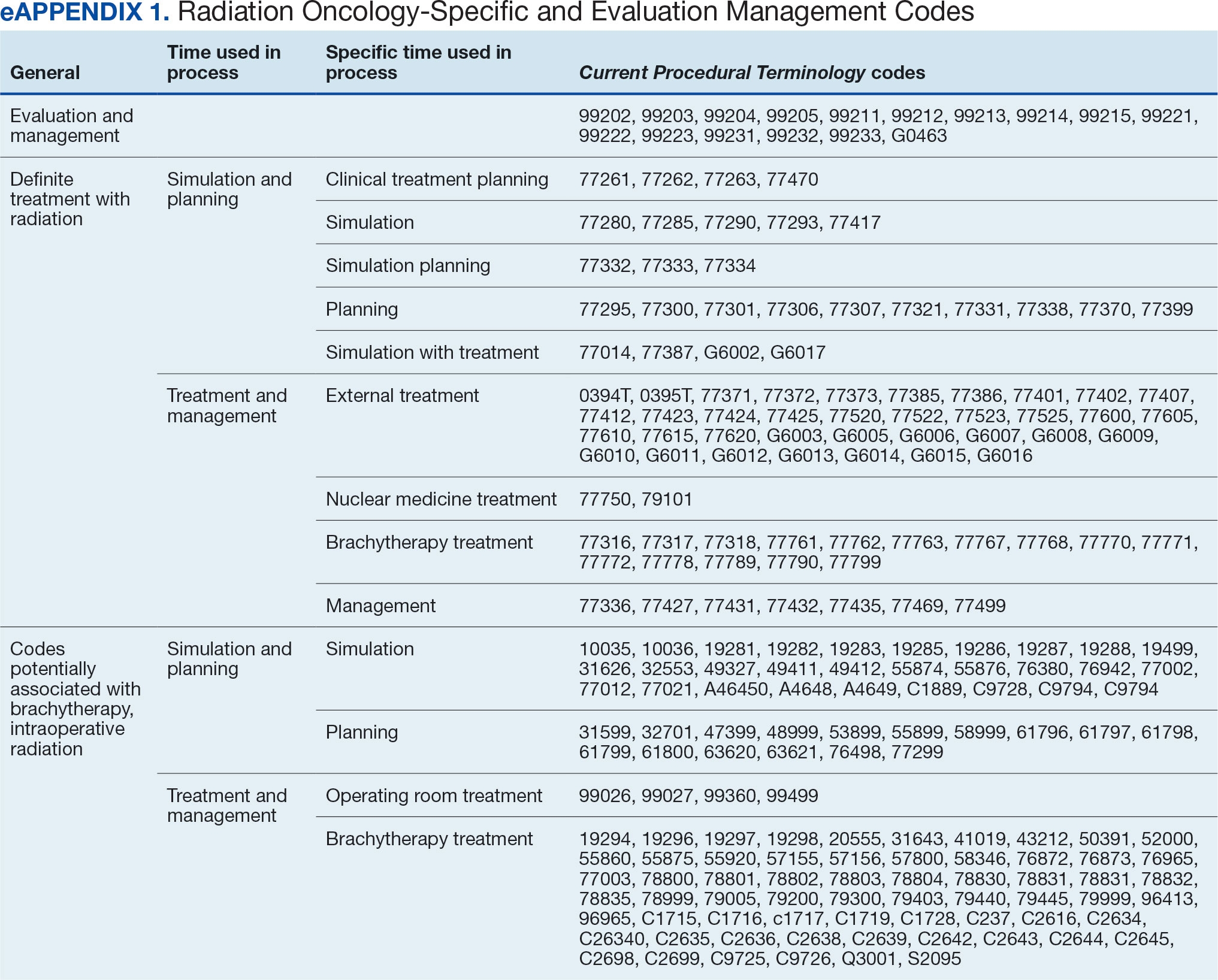
Radiation Oncology-Specific Costs
The VA Close to Me (CTM) program was used to find 84 specific radiation oncology CPT codes, nearly all within the 77.XXX or G6.XXX series, which included all radiation oncology-specific (ROS) codes (except visits accrued during consultation and return appointments). ROS costs are those that could not be performed by any other service and include procedures related to radiation oncology simulation, treatment planning, treatment delivery (with or without image guidance), and physician or physicist management. All ROS costs should be included in a patient’s radiation oncology SEOC. Other costs that may accompany operating room or brachytherapy administration did not follow a 77.XXX or G6.XXX pattern but were included in total radiation therapy operating costs.
Data obtained from AMCMS and CTM included patient name and identifier; CPT billed amount; CPT paid amount; dates of service; number of claims; International Classification of Diseases, Tenth Revision (ICD) diagnosis; and VA authorization numbers. Only CTM listed code modifiers. Only items categorized as paid were included in the analysis. Charges associated with discontinued consultations that had accrued costs also were included. Codes that were not directly related to ROS were separately characterized as other and further subcategorized.
Deep Dive Categorization
All scanned documents tagged to the community consultation were accessed and evaluated for completeness by a radiation oncologist (RS). The presence or absence of consultation notes and treatment summaries was evaluated based on necessity (ie, not needed for continuation of care or treatment was not given). In the absence of a specific completion summary or follow-up note detailing the treatment modality, number of fractions, and treatment sites, available documentation, including clinical notes and billing information, was used. Radical or curative therapies were identified as courses expected to eradicate disease, including stereotactic ablative radiotherapy to the brain, lung, liver, and other organs. Palliative therapies included whole-brain radiotherapy or other low-dose treatments. If the patient received the intended course, this was categorized as full. If incomplete, it was considered partial.
Billing Deviations
The complete document review allowed for close evaluation of paid therapy and identification of gaps in billing (eg, charges not found in extracted data that should have occurred) for external beam radiotherapy patients. Conversely, extra charges, such as an additional weekly treatment management charge (CPT code 77427), would be noted. Patients were expected to have the number of treatments specified in the summary, a clinical treatment planning code, and weekly treatment management notes from physicians and physicists every 5 fractions. Consultations and follow-up visits were expected to have 1 visit code; CPT codes 99205 and 99215, respectively, were used to estimate costs in their absence.
Costs were based on Medicare rates as of January 1 of the year in which they were accrued. 7-10 Duplicates were charges with the same code, date, billed quantity, and paid amounts for a given patient. These would always be considered erroneous. Medicare treatment costs for procedures such as intensity modulated radiotherapy (CPT code 77385 or 77386) are available on the Medicare website. When reviewing locality deviations for 77427, there was a maximum of 33% increase in Medicare rates. Therefore, for treatment codes, one would expect the range to be at least the Medicare rate and maximally 33% higher. These rates are negotiated with insurance companies, but this range was used for the purpose of reviewing and adjusting large data sets.
RESULTS
Since 2018, > 500 community care consults have been placed by radiation oncology for treatment in the community, with more following implementation of the VA MISSION Act. Use of radiation oncology community care services annually increased during the study period for this facility (Table 1, Figure 2). Of the 325 community care consults placed from October 1, 2021, to February 1, 2024, 248 radiation oncology SEOCs were recorded with charges for 181 patients (range, 1-5 SEOCs). Long drive time was the rationale for > 97% of patients directed to community care (Supplemental materials, available at doi:10.12788/fp.0585). Based on AMCMS data, $22.2 million was billed and $2.7 million was paid (20%) for 8747 CPT codes. Each community care interval cost the VA a median (range) of $5000 ($8-$168,000 (Figure 3).
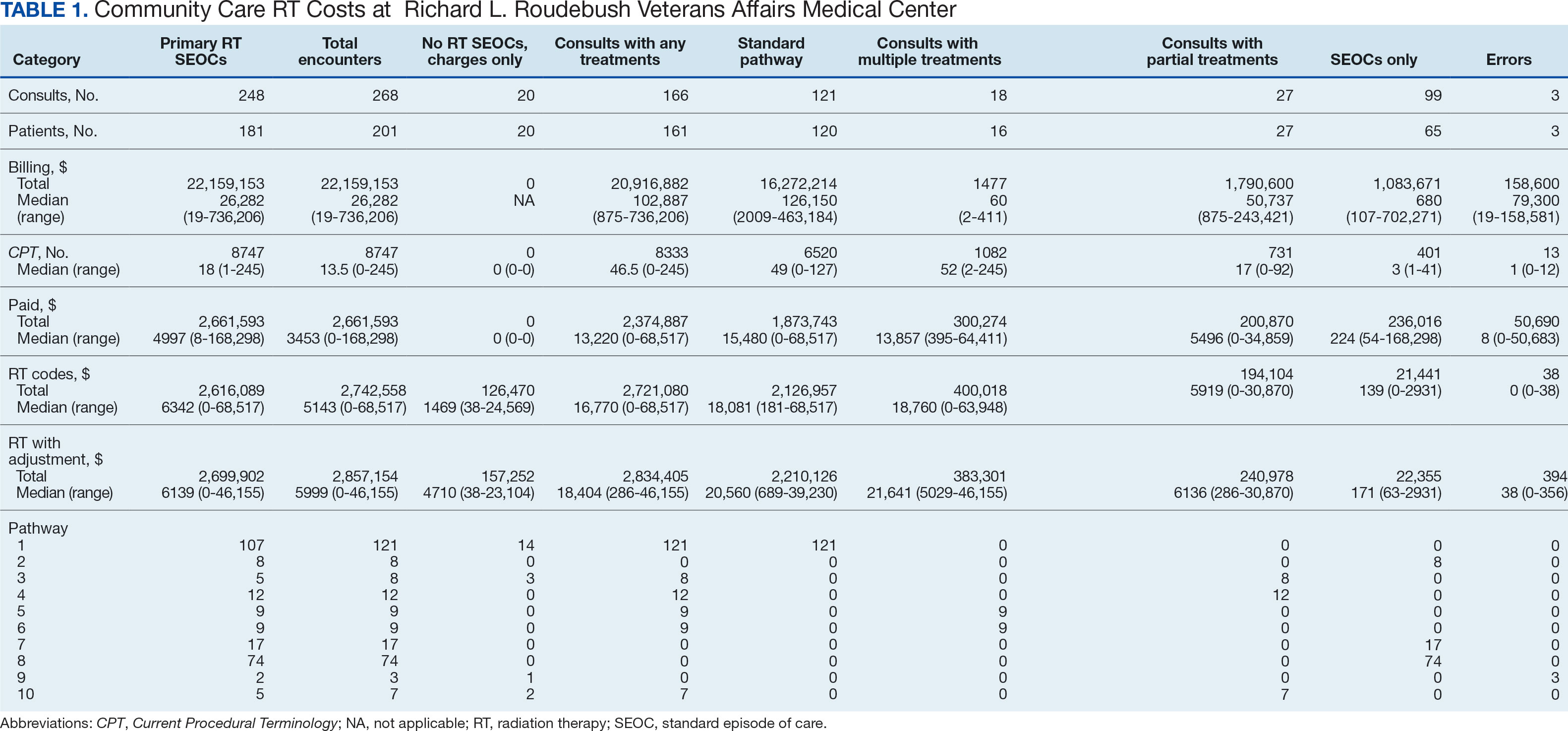
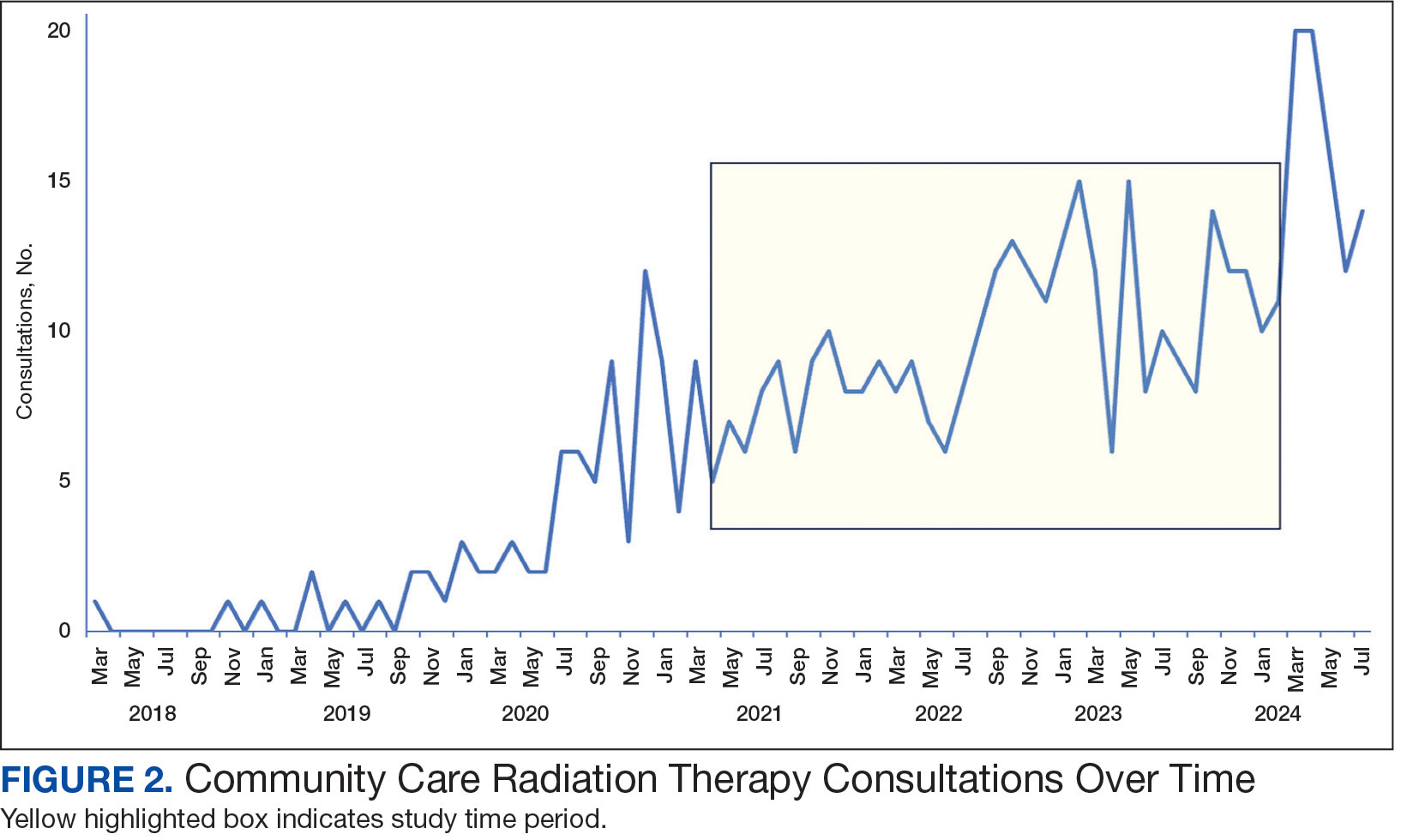
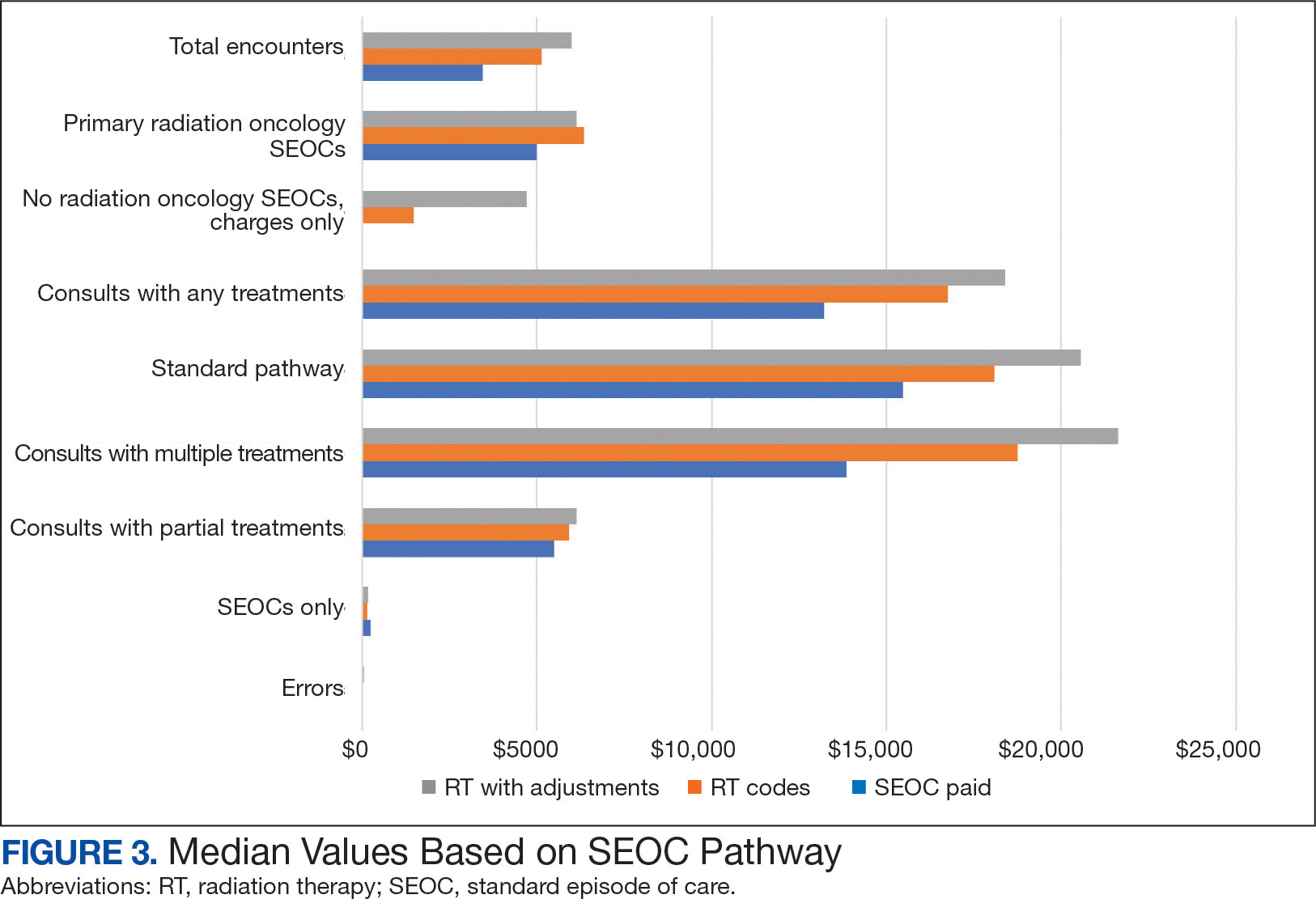
After reviewing ROS charges extracted from CTM, 20 additional patients had radiation oncology charges but did not have a radiation oncology SEOC for 268 episodes of care for 201 unique patients. In addition to the 20 patients who did not have a SEOC, 42 nonradiation oncology SEOCs contained 1148 radiation oncology codes, corresponding to almost $500,000 paid. Additional charges of about $416,000, which included biologic agents (eg, durvalumab, nivolumab), procedures (eg, mastectomies), and ambulance rides were inappropriately added to radiation oncology SEOCs.
While 77% of consultations were scanned into CPRS and JLV, only 54% of completion summaries were available with an estimated $115,000 in additional costs. The total adjusted costs was about $2.9 million. Almost 37% of SEOCs were for visits only. For the 166 SEOCs where patients received any radiation treatment or planning, the median cost was $18,000. Differences in SEOC pathways are shown in Figure 4. One hundred twenty-one SEOCs (45%) followed the standard pathway, with median SEOC costs of $15,500; when corrected for radiation-specific costs, the median cost increased to $18,000. When adjusted for billing irregularities, the median cost was $20,600. Ninety-nine SEOCs (37%) were for consultation/ follow-up visits only, with a median cost of $220. When omitting shared scans and nonradiation therapy costs and correcting for billing gaps, the median cost decreased to $170. A median of $9200 was paid per patient, with $12,900 for radiation therapy-specific costs and $13,300 adjusted for billing deviations. Narrowing to the 106 patients who received full, radical courses, the median SEOC, ROS, and adjusted radiation therapy costs increased to $19,400, $22,200, and $22,900, respectively (Table 2, Figure 5). Seventy-one SEOCs (26%) had already seen a radiation oncologist before the VA radiation oncology department was aware, and 49 SEOCs (18%) had retroactive approvals (Supplemental materials available at doi:10.12788/fp.0585).
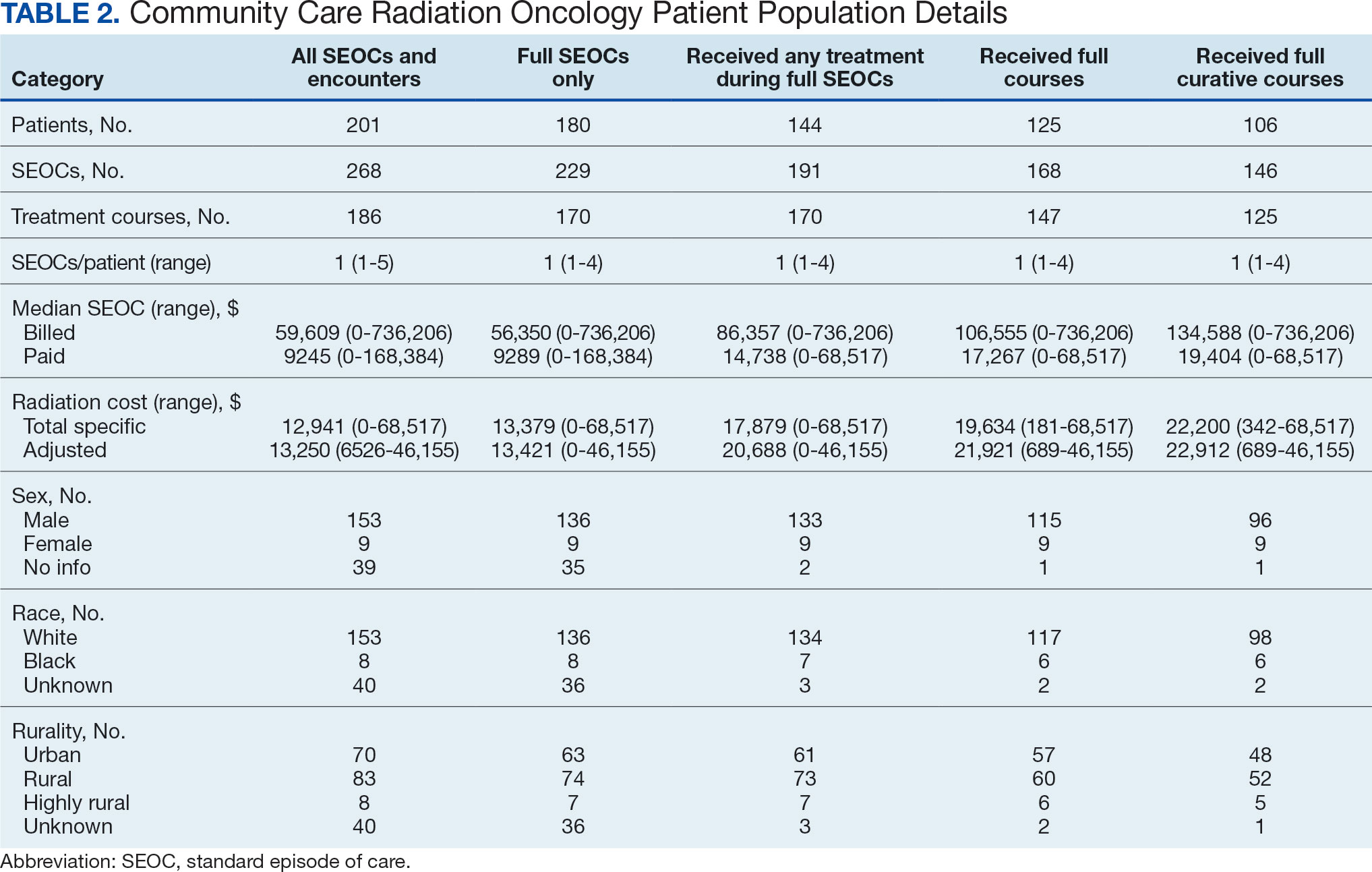
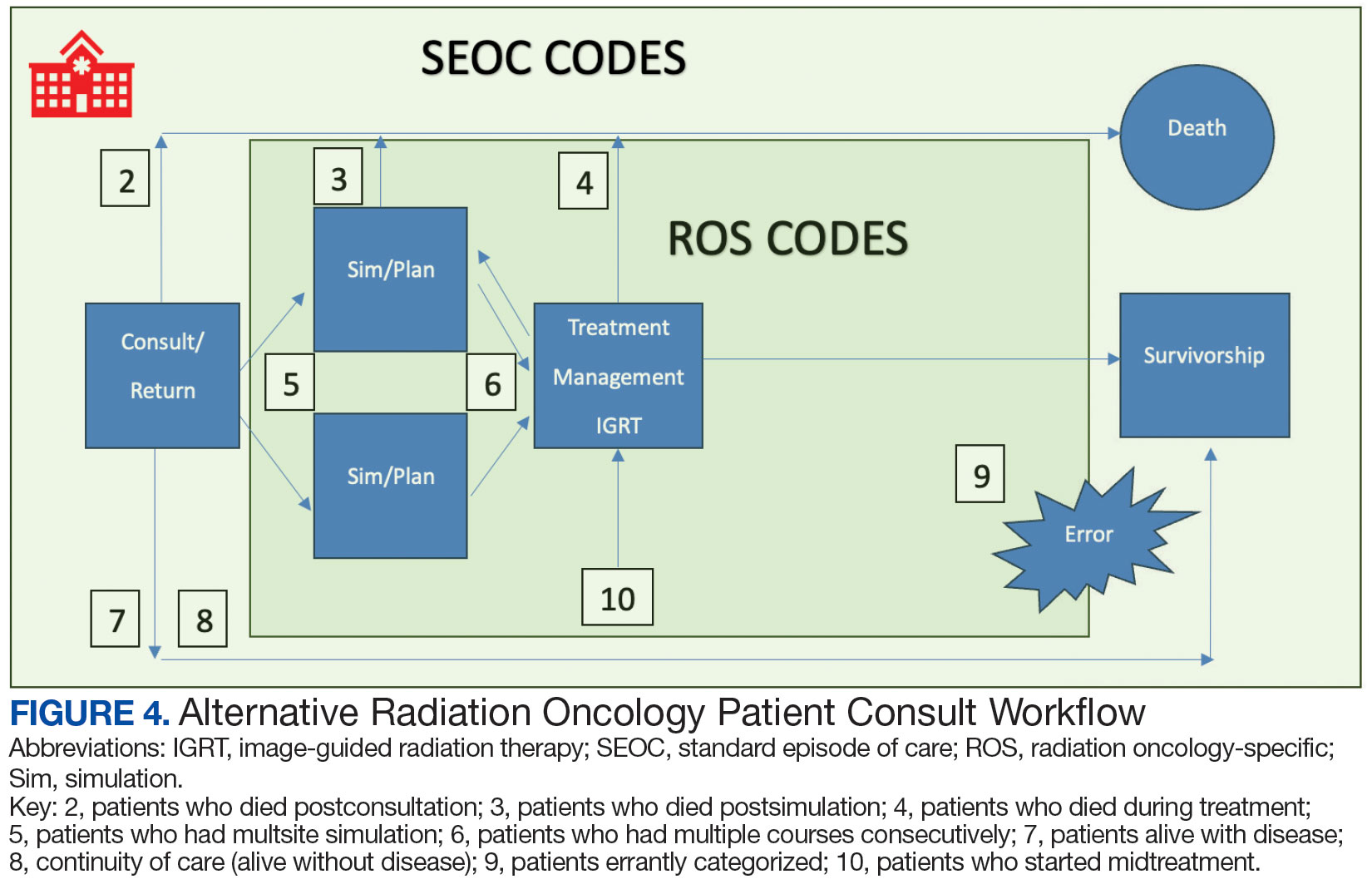
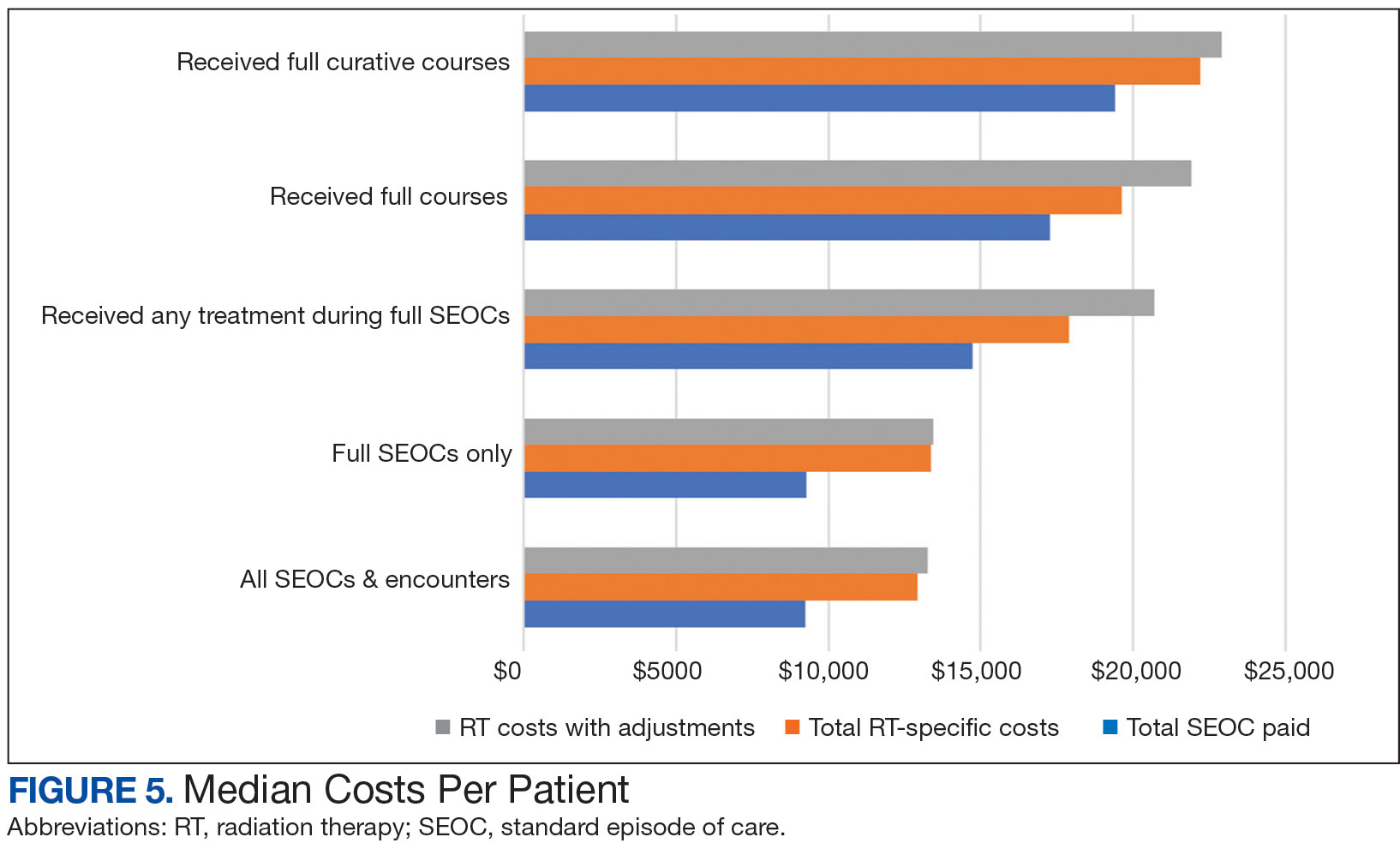
Every consultation charge was reviewed. A typical patient following the standard pathway (eAppendix 2, available at doi:10.12788/ fp.0585) exhibited a predictable pattern of consultation payment, simulation and planning, multiple radiation treatments interspersed with treatment management visits and a cone-down phase, and finishing with a follow-up visit. A less predictable case with excess CPT codes, gaps in charges, and an additional unexpected palliative course is shown in eAppendix 3 (available at doi:10.12788/fp.0585). Gaps occurred in 42% of SEOCs with missed bills costing as much as $12,000. For example, a patient with lung cancer had a treatment summary note for lung cancer after completion that showed the patient received 30 fractions of 2 Gy, a typical course. Only 10 treatment codes and 3 of 6 weekly treatment management codes were available. There was a gap of 20 volumetric modulated arc therapy treatments, 3 physics weekly status checks, 3 physician managements notes, and a computed tomography simulation charge.
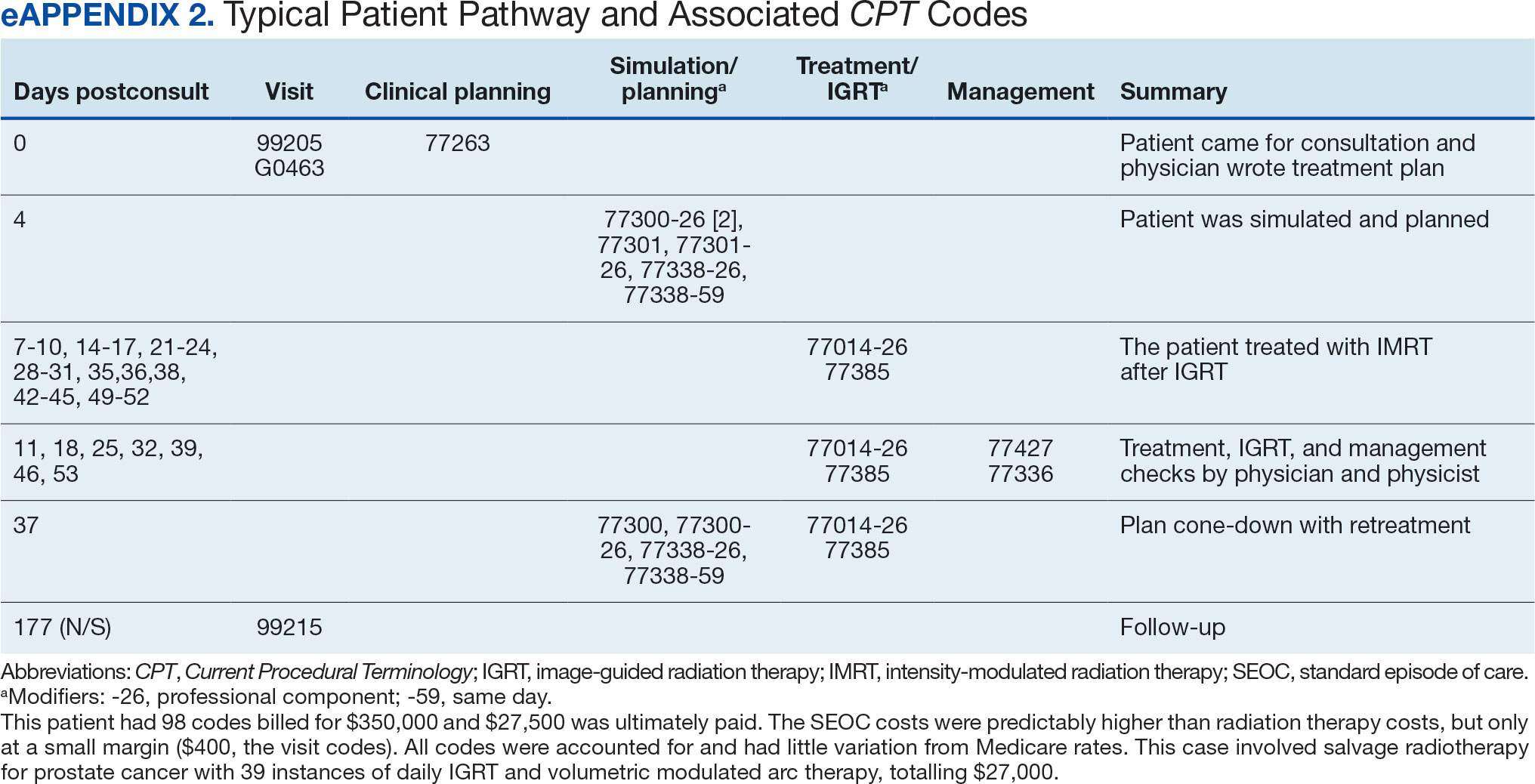

Between AMCMS and CTM, 10,005 CPT codes were evaluated; 1255 (12.5%) were unique to AMCMS (either related to the radiation oncology course, such as Evaluation and Management CPT codes or “other” unrelated codes) while 1158 (11.6%) were unique to CTM. Of the 7592 CPT codes shared between AMCMS and CTM, there was a discrepancy in 135 (1.8%); all were duplicates (CTM showed double payment while AMCMS showed $0 paid). The total CPT code costs came to $3.2 million with $560,000 unique to SEOCs and $500,000 unique to CTM. Treatment codes were the most common (33%) as shown in Table 3 and accounted for 55% of the cost ($1.8 million). About 700 CPT codes were considered “other,” typically for biologic therapeutic agents (Table 4 and eAppendix 4, available at doi:10.12788/fp.0585).
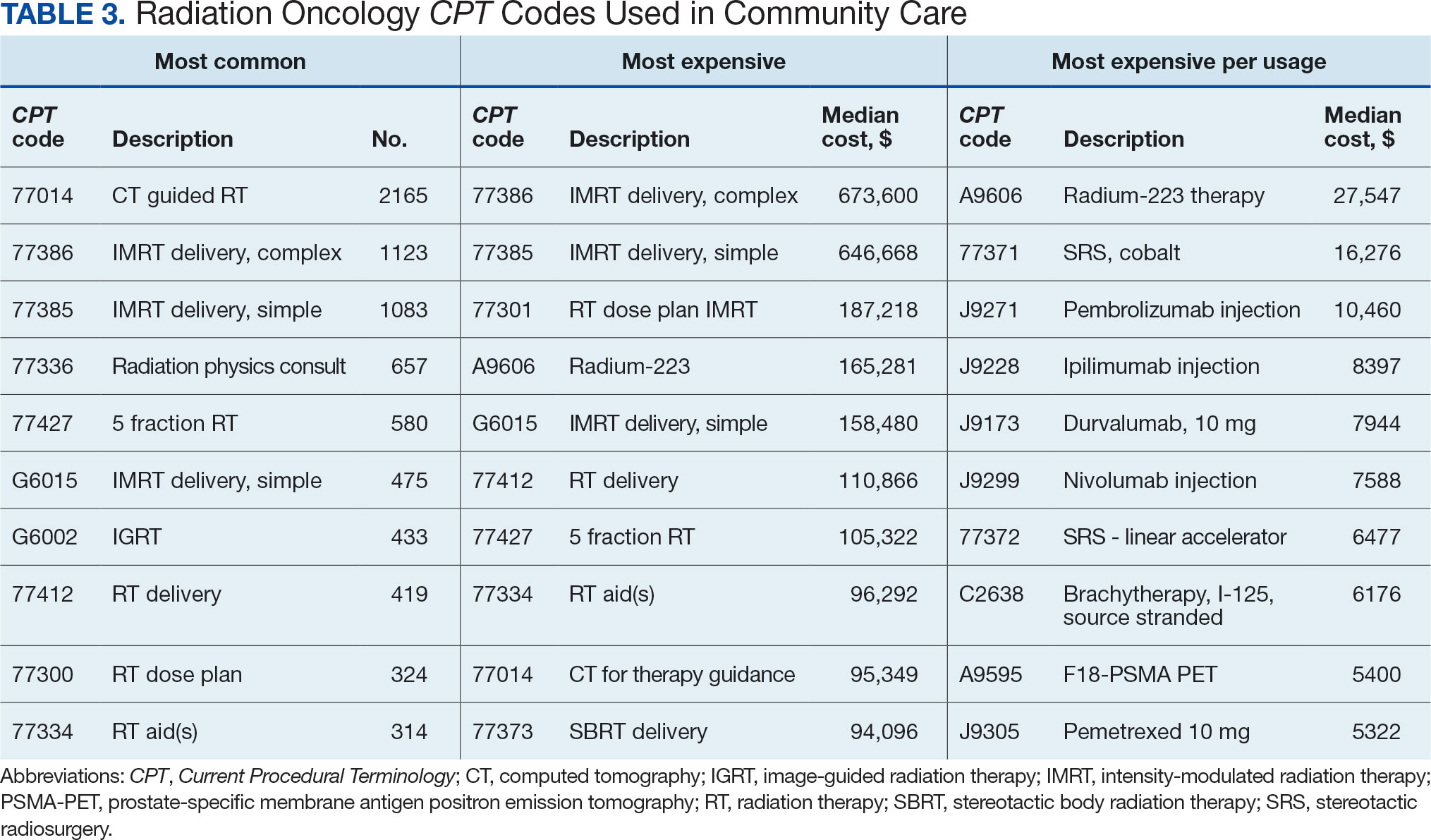
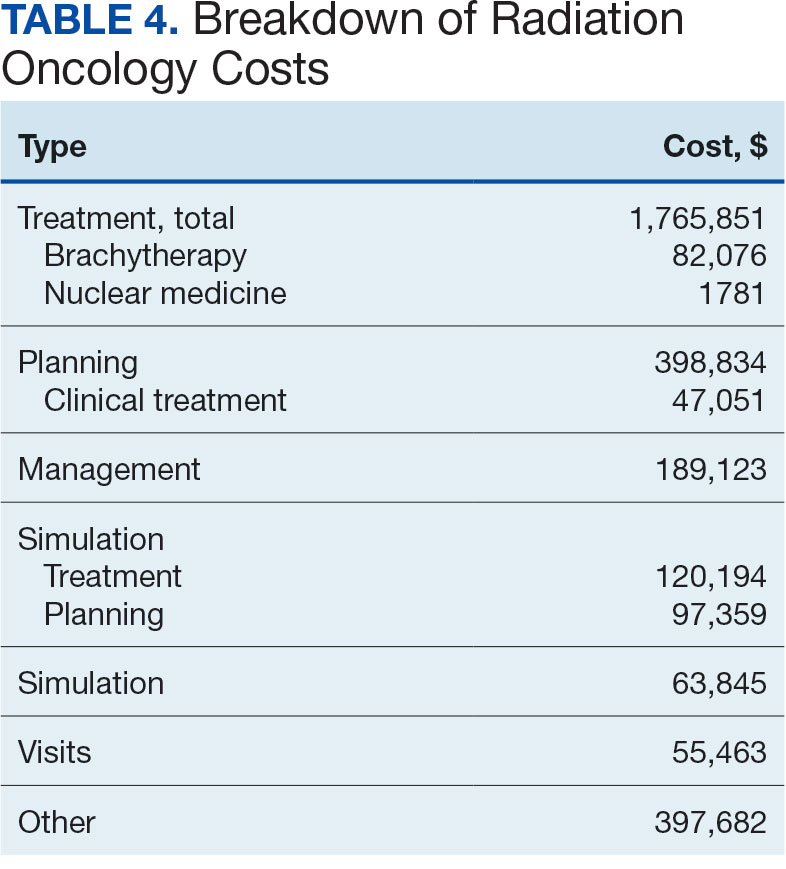

DISCUSSION
The current method of reporting radiation oncology costs used by VA is insufficient and misleading. Better data are needed to summarize purchased care costs to guide decisions about community care at the VA. Investigations into whether the extra costs for quality care (ie, expensive capital equipment, specialized staff, mandatory accreditations) are worthwhile if omitted at other facilities patients choose for their health care needs. No study has defined specialty care-specific costs by evaluating billing receipts from the CDW to answer the question. Kenamond et al highlight the need for radiation oncology for rural patients.11 Drive time was cited as the reason for community care referral for 97% of veterans, many of whom lived in rural locations. Of patients with rurality information who enrolled in community care, 57% came from rural or highly rural counties, and this ratio held for those who received full curative therapies. An executive administrator relying on AMCMS reports would see a median SEOC cost of $5000, but without ROS knowledge in coding, the administrator would miss many additional costs. For example, 2 patients who each had 5 SEOCs during the evaluated period, incurred a total cost of only $1800.
Additionally, an administrator could include miscategorized costs with significant ramifications. The 2 most expensive SEOCs were not typical radiation oncology treatments. A patient undergoing radium-223 dichloride therapy incurred charges exceeding $165,000, contributing disproportionately to the overall median cost analysis; this would normally be administered by the nuclear medicine department. Immunotherapy and chemotherapy are uniformly overseen by medical oncology services, but drug administration codes were still found in radiation oncology SEOCs. A patient (whose SEOC was discontinued but accrued charges) had an electrocardiogram interpretation for $8 as the SEOC cost; 3 other SEOCs continued to incur costs after being discontinued. There were 24 empty SEOCs for patients that had consults to the community, and 2 had notes stating treatment had been delivered yet there was no ROS costs or SEOC costs. Of the 268 encounters, 43% had some sort of billing irregularities (ie, missing treatment costs) that would be unlikely for a private practice to omit; it would be much more likely that the CDW miscategorized the payment despite confirmation of the 2 retrieval systems.
It would be inadvisable to make staffing decisions or forecast costs based on current SEOC reports without specialized curation. A simple yet effective improvement to the cost attribution process would be to restrict the analysis to encounters containing primary radiation treatment codes. This targeted approach allows more accurate identification of patients actively receiving radiation oncology treatment, while excluding those seen solely for consultations or follow-up visits. Implementing this refinement leads to a substantial increase in the median payment—from $5000 to $13,000—without requiring additional coding or data processing, thereby enhancing the accuracy of cost estimates with minimal effort.
Clarifying radiation oncology service costs requires addressing the time frame and services included, given laxity and interpretation of the SEOCs. VA community care departments have streamlined the reimbursement process at the expense of medical cost organization and accuracy; 86% of VA practitioners reported that ≥ 1 potential community health care partners had refused to work with the VA because of payment delays.12 Payments are contingent on correspondence from outside practices for community work. For radiation oncology, this includes the consultation but also critical radiation-related details of treatment, which were omitted nearly half the time. SEOC approval forms have many costly laboratory tests, imaging, and procedures that have little to do with radiation oncology cancer treatments but may be used in the workup and staging process; this creates noise when calculating radiation oncology fiscal cost.
The presumption that an episode of care equates to a completed radiation therapy course is incorrect; this occurs less than half of the time. An episode often refers to a return visit, or conversely, multiple treatment courses. As the patients’ medical homes are their VHA primary care practitioners, it would be particularly challenging to care for the patients without full treatment information, especially if adverse effects from therapy were to arise. As a tertiary specialty, radiation oncology does not seek out patients and are sent consultations from medical oncology, surgical, and medical oncologic specialties. Timesensitive processes such as workup, staging, and diagnosis often occur in parallel. This analysis revealed that patients see outside radiation oncologists prior to the VA. There are ≥ 100 patients who had radiation oncology codes without a radiation oncology SEOC or community care consultation, and in many cases, the consultation was placed after the patient was seen.
Given the lack of uniformity and standardization of patient traffic, the typical and expected pathways were insufficient to find the costs. Too many opportunities for errors and incorrect categorization of costs meant a different method would be necessary. Starting at the inception of the community care consult, only 1 diagnosis code can be entered. For patients with multiple diagnoses, one would not be able to tell what was treated without chart access. Radiation oncology consults come from primary and specialty care practitioners and nurses throughout the VA. Oftentimes, the referral would be solicited by the community radiation oncology clinic, diagnosing community specialty (ie, urology for a patient with prostate cancer), or indirectly from the patient through primary care. Many cases were retroactively approved as the veteran had already been consulted by the community care radiation oncologist. If the patient is drive-time eligible, it would be unlikely that they would leave and choose to return to the VA. There is no way for a facility VA service chief or administrator to mitigate VA community costs of care, especially as shown by the miscategorization of several codes. Database challenges exacerbate the issue: 1 patient changed her first and last name during this time frame, and 2 patients had the same name but different social security numbers. In order to strictly find costs between 2 discrete timepoints, 39 (15%) SEOCs were split and incomplete, and 6 SEOCs contained charges for 2 different patients. This was corrected, and all inadvertent charges were cancelled. Only 1 ICD code is allowed per community care consultation, so an investigation is required to find costs for patients with multiple sites of disease. Additionally, 5 of the patients marked for drive time were actually patients who received Gamma Knife and brachytherapy, services not available at the VA.
Hanks et al first attempted to calculate cost of radiation oncology services. External beam prostate cancer radiotherapy at 3 suburban California centers cost $6750 ($20,503 inflation adjusted) per patient before October 1984 and $5600 ($17,010 inflation adjusted) afterwards.13 According to the American Society for Radiation Oncology, Advocacy Radiation Oncology Case Rate Program Curative radiation courses should cost $20,000 to $30,000 and palliative courses should cost $10,000 to $15,000. These costs are consistent with totals demonstrated in this analysis and similar to the inflation-adjusted Hanks et al figures. Preliminary findings suggest that radiation treatment constituted more than half of the total expenditures, with a notable $4 million increase in adjusted cost compared to the Medicare rates, indicating significant variation. Direct comparisons with Medicaid or commercial payer rates remain unexplored.
Future Directions
During the study period, 201 patients received 186 courses of radiation therapy in the community, while 1014 patients were treated in-house for a total of 833 courses. A forthcoming analysis will directly compare the cost of in-house care with that of communitybased treatment, specifically breaking down expenditure differences by diagnosis. Future research should investigate strategies to align reimbursement with quality metrics, including the potential role of tertiary accreditation in incentivizing high-value care. Additional work is also warranted to assess patient out-ofpocket expenses across care settings and to benchmark VA reimbursement against Medicare, Medicaid, and private insurance rates. In any case, with the increasing possibility of fewer fractions for treatments such as stereotactic radiotherapy or palliative care therapy, there is a clear financial incentive to treat as frequently as allowed despite equal clinical outcomes.
CONCLUSIONS
Veterans increasingly choose to receive care closer to home if the option is available. In the VA iron triangle, cost comes at the expense of access but quantifying this has proved elusive in the cost accounting model currently used at the VA.1 The inclusion of all charges loosely associated with SEOCs significantly impairs the ability to conduct meaningful cost analyses. The current VA methodology not only introduces substantial noise into the data but also leads to a marked underestimation of the true cost of care delivered in community settings. Such misrepresentation risks driving policy decisions that could inappropriately reduce or eliminate in-house radiation oncology services. Categorizing costs effectively in the VA could assist in making managerial and administrative decisions and would prevent damaging service lines based on misleading or incorrect data. A system which differentiates between patients who have received any treatment codes vs those who have not would increase accuracy.
William Kissick’s description of health care’s iron triangle in 1994 still resonates. Access, quality, and cost will always come at the expense of the others.1 In 2018, Congress passed the VA MISSION Act, allowing patients to pursue community care options for extended waits (> 28 days) or longer distance drive times of > 60 minutes for specialty care services, such as radiation oncology. According to Albanese et al, the VA MISSION Act sought to address gaps in care for veterans living in rural and underserved areas.2 The Veterans Health Administration (VHA) continues to increase community care spending, with a 13.8% increase in fiscal year 2024 and an expected cost of > $40 billion for 2025.3 One could argue this pays for access for remote patients and quality when services are unavailable, making it a direct application of the iron triangle.
The VA MISSION Act also bolstered the expansion of existing community care department staff to expediently facilitate and coordinate care and payments.2 Cost management and monitoring have become critical in predicting future staff requirements, maintaining functionality, and ensuring patients receive optimal care. The VHA purchases care through partner networks and defines these bundled health care services as standard episodes of care (SEOCs), which are “clinically related health care services for a specific unique illness or medical condition… over a defined period of time.”4 Medicare publishes its rates quarterly, and outpatient procedure pricing is readily available online.5 Along these same lines, the US Department of Veterans Affairs (VA) publishes a current list of available procedures and associated Current Procedure Technology (CPT) codes that are covered under its VA fee schedule for community care.
Unique challenges persist when using this system to accurately account for radiation oncology expenditures. This study was based on the current practices at the Richard L. Roudebush VA Medical Center (RLRVAMC), a large 1a hospital. A detailed analysis reveals the contemporaneous cost of radiation oncology cancer care from October 1, 2021, through February 1, 2024, highlights the challenges in SEOC definition and duration, communication issues between RLRVAMC and purchase partners, inconsistencies in billing, erroneous payments, and difficulty of cost categorization.
METHODS
Community care radiation oncology-related costs were examined from October 1, 2021, to February 1, 2024 for RLRVAMC, 6 months prior to billing data extraction. Figure 1 shows a simple radiation oncology patient pathway with consultation or visit, simulation and planning, and treatment, with codes used to check billing. It illustrates the expected relationships between the VHA (radiation oncology, primary, and specialty care) and community care (clinicians and radiation oncology treatment sites).
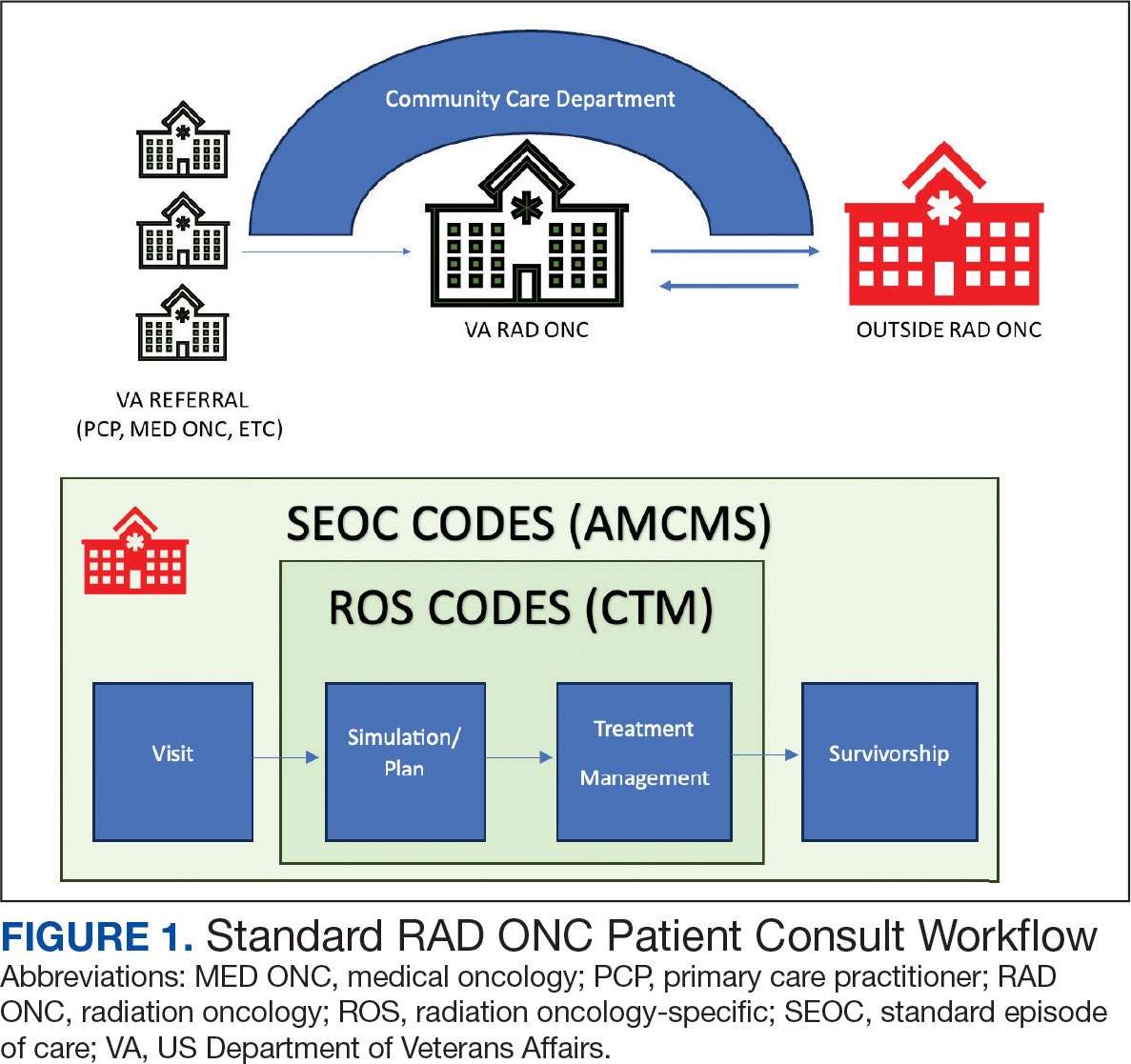
VHA standard operating procedures for a patient requesting community-based radiation oncology care require a board-certified radiation oncologist at RLRVAMC to review and approve the outside care request. Community care radiation oncology consultation data were accessed from the VA Corporate Data Warehouse (CDW) using Pyramid Analytics (V25.2). Nurses, physicians, and community care staff can add comments, forward consultations to other services, and mark them as complete or discontinued, when appropriate. Consultations not completed within 91 days are automatically discontinued. All community care requests from 2018 through 2024 were extracted; analysis began April 1, 2021, 6 months prior to the cost evaluation date of October 1, 2021.
An approved consultation is reviewed for eligibility by a nurse in the community care department and assigned an authorization number (a VA prefix followed by 12 digits). Billing codes are approved and organized by the community care networks, and all procedure codes should be captured and labeled under this number. The VAMC Community Care department obtains initial correspondence from the treating clinicians. Subsequent records from the treating radiation oncologist are expected to be scanned into the electronic health record and made accessible via the VA Joint Legacy Viewer (JLV) and Computerized Patient Record System (CPRS).
Radiation Oncology SEOC
The start date of the radiation oncology SEOC is determined by the community care nurse based on guidance established by the VA. It can be manually backdated or delayed, but current practice is to start at first visit or procedure code entry after approval from the VAMC Radiation Oncology department. Approved CPT codes from SEOC versions between October 1, 2021, and February 1, 2024, are in eAppendix 1 (available at doi:10.12788/fp.0585). These generally include 10 types of encounters, about 115 different laboratory tests, 115 imaging studies, 25 simulation and planning procedures, and 115 radiation treatment codes. The radiation oncology SEOCs during the study period had an approval duration of 180 days. Advanced Medical Cost Management Solutions software (AMCMS) is the VHA data analytics platform for community care medical service costs. AMCMS includes all individual CPT codes billed by specific radiation oncology SEOC versions. Data are refreshed monthly, and all charges were extracted on September 12, 2024, > 6 months after the final evaluated service date to allow for complete billing returns.6
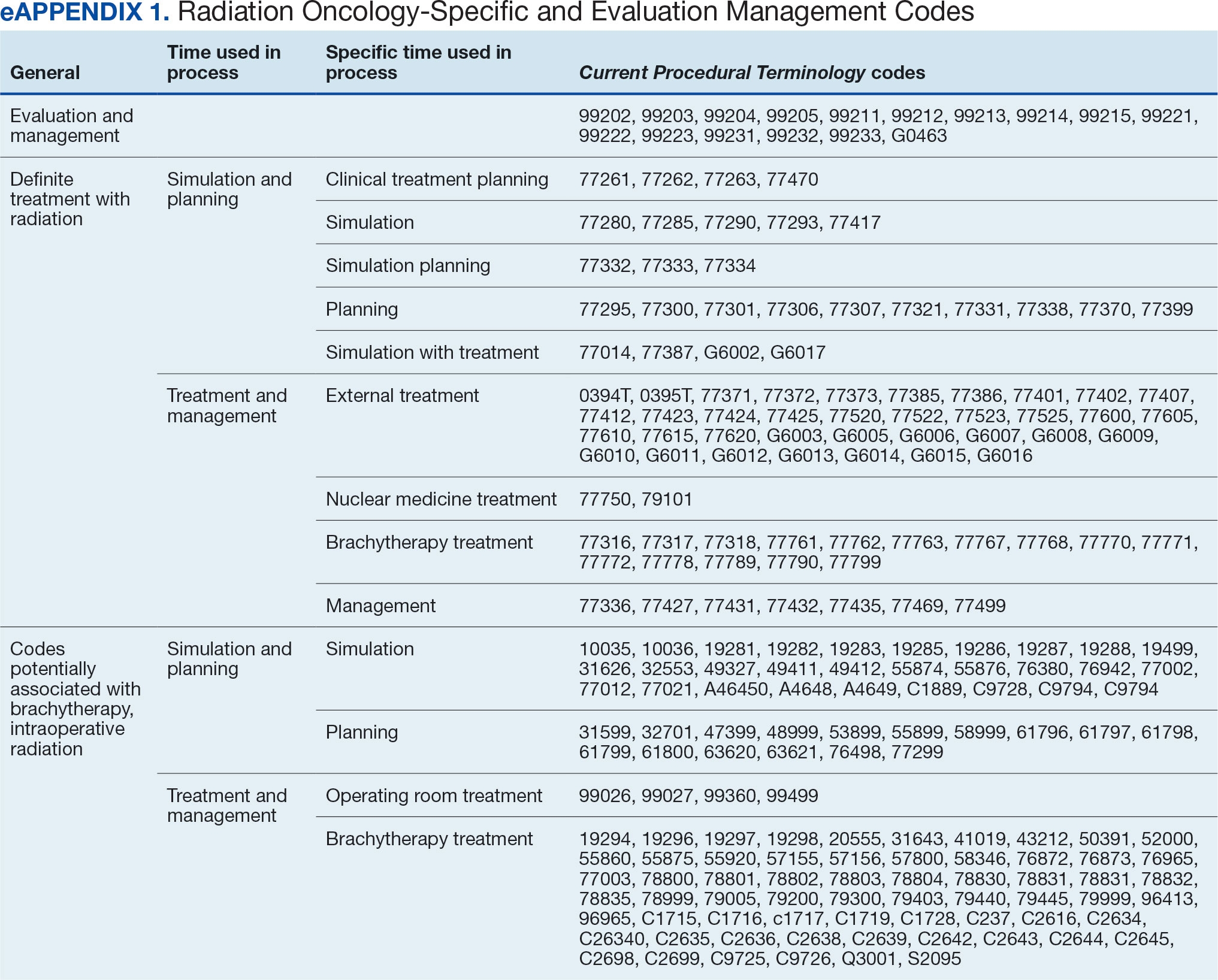
Radiation Oncology-Specific Costs
The VA Close to Me (CTM) program was used to find 84 specific radiation oncology CPT codes, nearly all within the 77.XXX or G6.XXX series, which included all radiation oncology-specific (ROS) codes (except visits accrued during consultation and return appointments). ROS costs are those that could not be performed by any other service and include procedures related to radiation oncology simulation, treatment planning, treatment delivery (with or without image guidance), and physician or physicist management. All ROS costs should be included in a patient’s radiation oncology SEOC. Other costs that may accompany operating room or brachytherapy administration did not follow a 77.XXX or G6.XXX pattern but were included in total radiation therapy operating costs.
Data obtained from AMCMS and CTM included patient name and identifier; CPT billed amount; CPT paid amount; dates of service; number of claims; International Classification of Diseases, Tenth Revision (ICD) diagnosis; and VA authorization numbers. Only CTM listed code modifiers. Only items categorized as paid were included in the analysis. Charges associated with discontinued consultations that had accrued costs also were included. Codes that were not directly related to ROS were separately characterized as other and further subcategorized.
Deep Dive Categorization
All scanned documents tagged to the community consultation were accessed and evaluated for completeness by a radiation oncologist (RS). The presence or absence of consultation notes and treatment summaries was evaluated based on necessity (ie, not needed for continuation of care or treatment was not given). In the absence of a specific completion summary or follow-up note detailing the treatment modality, number of fractions, and treatment sites, available documentation, including clinical notes and billing information, was used. Radical or curative therapies were identified as courses expected to eradicate disease, including stereotactic ablative radiotherapy to the brain, lung, liver, and other organs. Palliative therapies included whole-brain radiotherapy or other low-dose treatments. If the patient received the intended course, this was categorized as full. If incomplete, it was considered partial.
Billing Deviations
The complete document review allowed for close evaluation of paid therapy and identification of gaps in billing (eg, charges not found in extracted data that should have occurred) for external beam radiotherapy patients. Conversely, extra charges, such as an additional weekly treatment management charge (CPT code 77427), would be noted. Patients were expected to have the number of treatments specified in the summary, a clinical treatment planning code, and weekly treatment management notes from physicians and physicists every 5 fractions. Consultations and follow-up visits were expected to have 1 visit code; CPT codes 99205 and 99215, respectively, were used to estimate costs in their absence.
Costs were based on Medicare rates as of January 1 of the year in which they were accrued. 7-10 Duplicates were charges with the same code, date, billed quantity, and paid amounts for a given patient. These would always be considered erroneous. Medicare treatment costs for procedures such as intensity modulated radiotherapy (CPT code 77385 or 77386) are available on the Medicare website. When reviewing locality deviations for 77427, there was a maximum of 33% increase in Medicare rates. Therefore, for treatment codes, one would expect the range to be at least the Medicare rate and maximally 33% higher. These rates are negotiated with insurance companies, but this range was used for the purpose of reviewing and adjusting large data sets.
RESULTS
Since 2018, > 500 community care consults have been placed by radiation oncology for treatment in the community, with more following implementation of the VA MISSION Act. Use of radiation oncology community care services annually increased during the study period for this facility (Table 1, Figure 2). Of the 325 community care consults placed from October 1, 2021, to February 1, 2024, 248 radiation oncology SEOCs were recorded with charges for 181 patients (range, 1-5 SEOCs). Long drive time was the rationale for > 97% of patients directed to community care (Supplemental materials, available at doi:10.12788/fp.0585). Based on AMCMS data, $22.2 million was billed and $2.7 million was paid (20%) for 8747 CPT codes. Each community care interval cost the VA a median (range) of $5000 ($8-$168,000 (Figure 3).
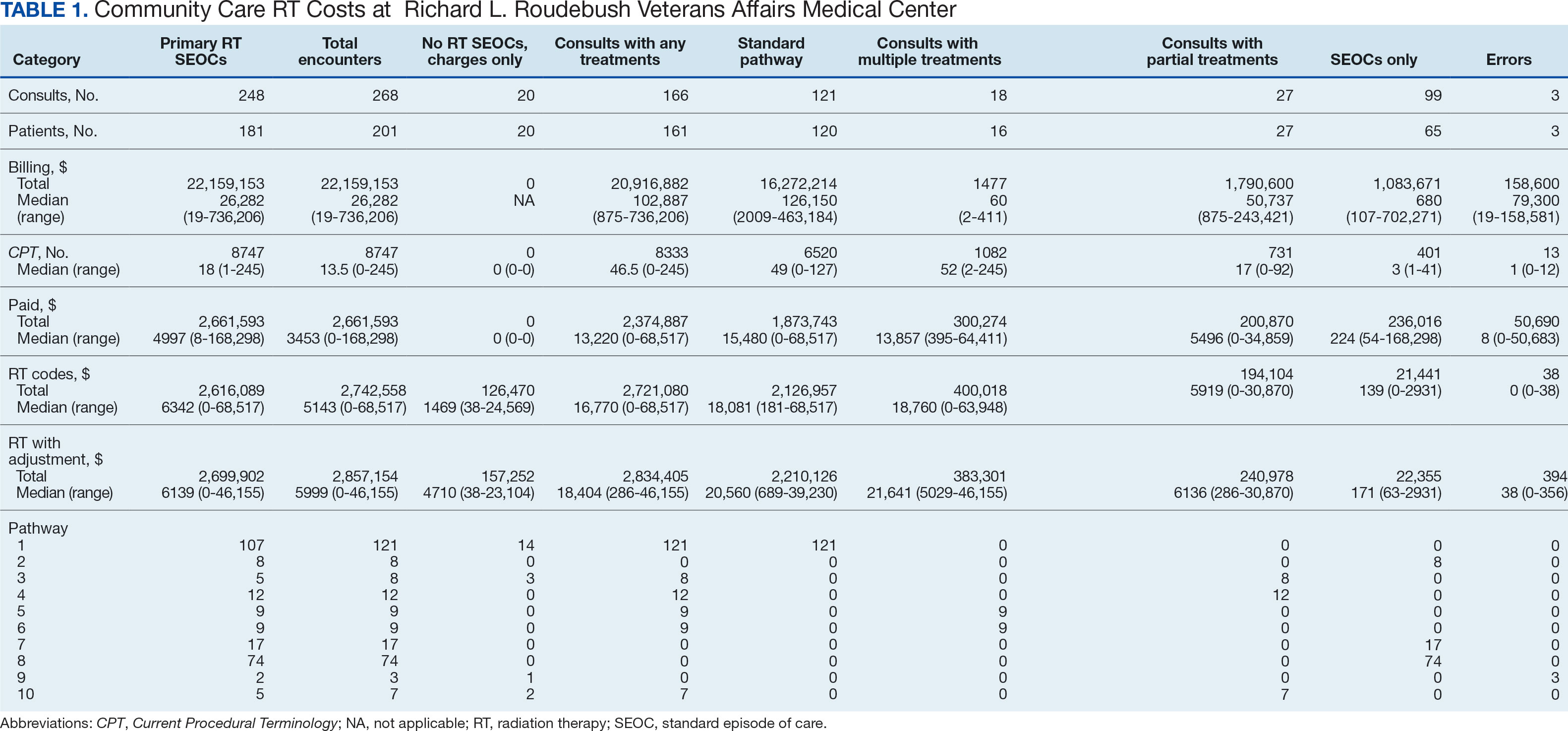
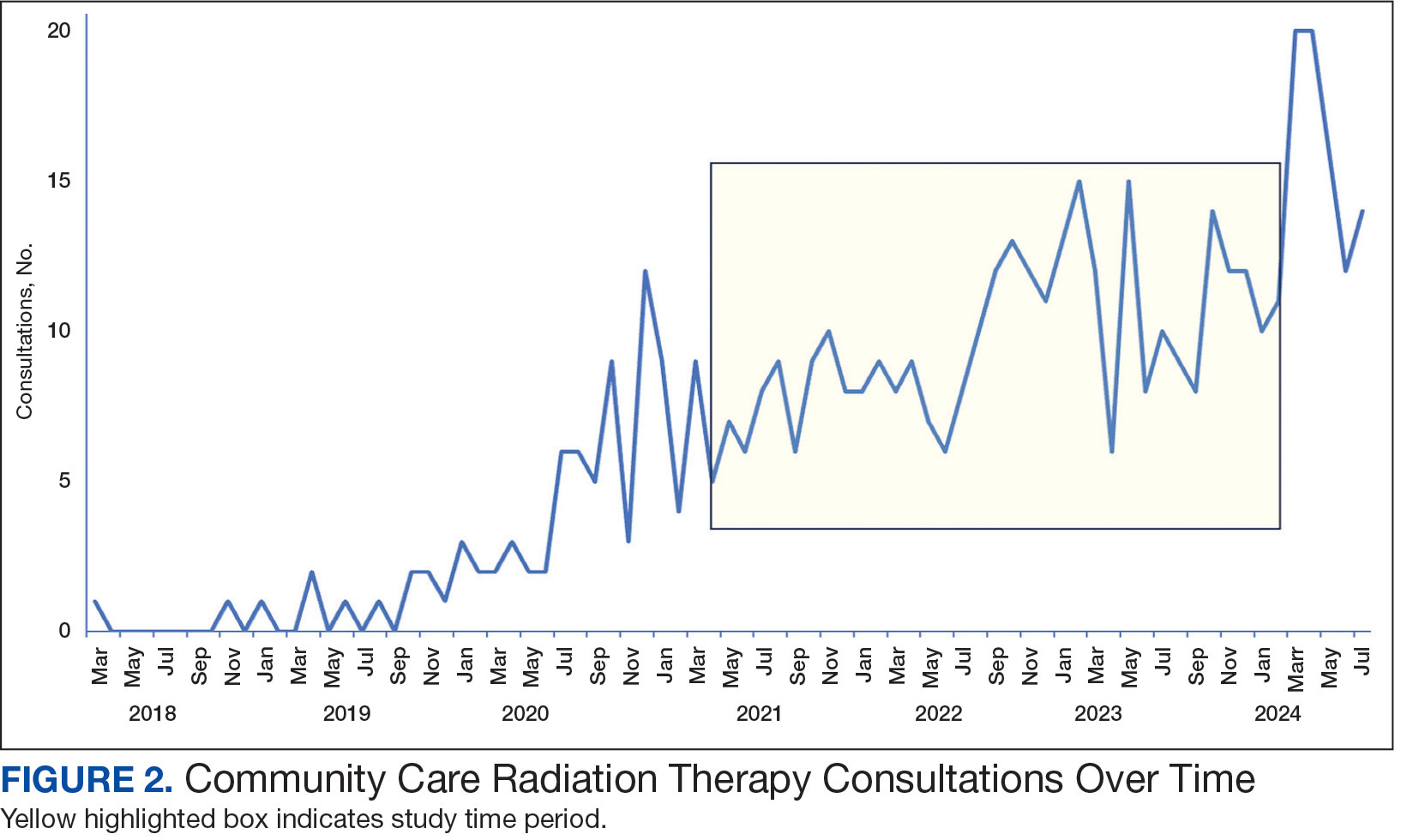
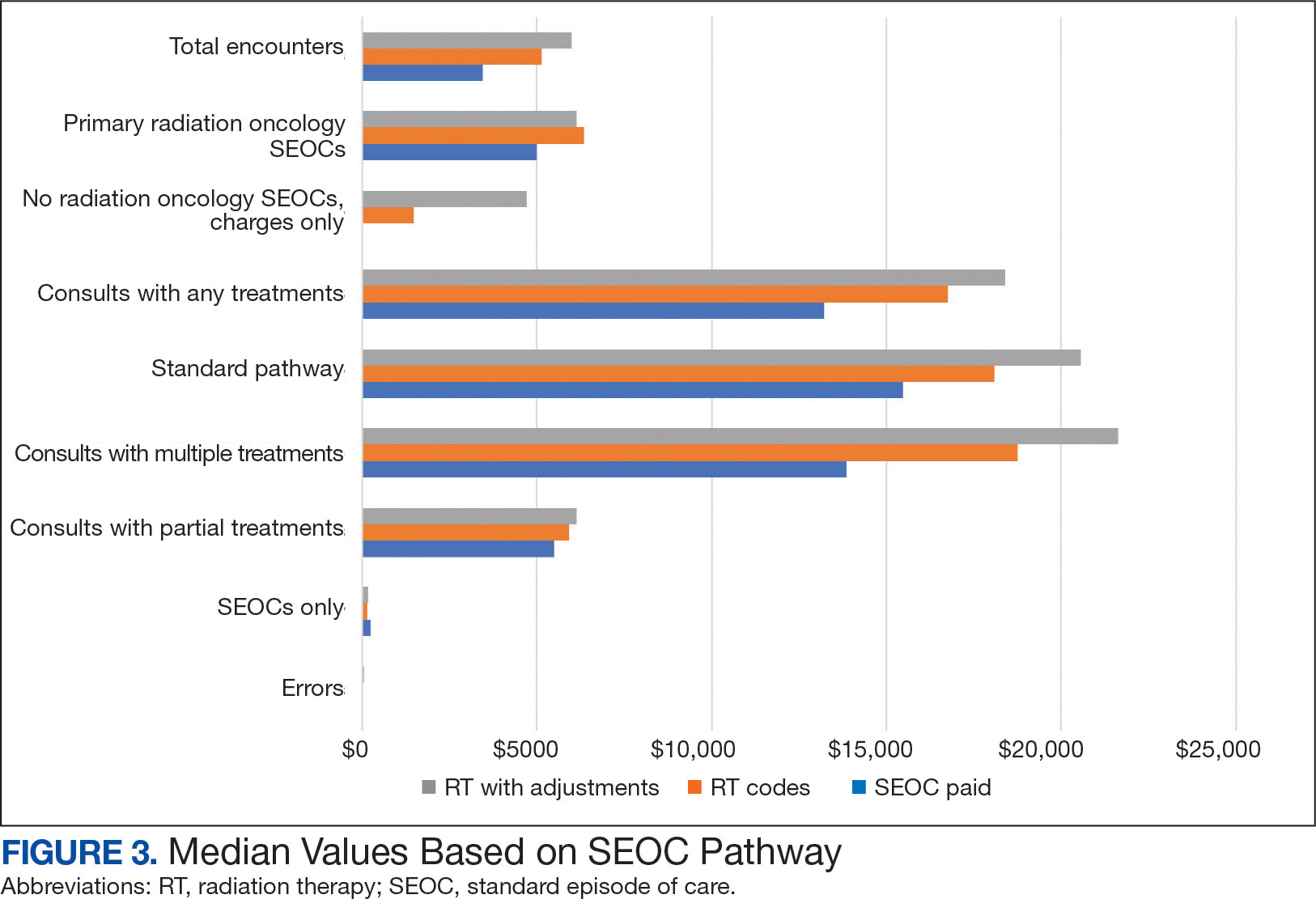
After reviewing ROS charges extracted from CTM, 20 additional patients had radiation oncology charges but did not have a radiation oncology SEOC for 268 episodes of care for 201 unique patients. In addition to the 20 patients who did not have a SEOC, 42 nonradiation oncology SEOCs contained 1148 radiation oncology codes, corresponding to almost $500,000 paid. Additional charges of about $416,000, which included biologic agents (eg, durvalumab, nivolumab), procedures (eg, mastectomies), and ambulance rides were inappropriately added to radiation oncology SEOCs.
While 77% of consultations were scanned into CPRS and JLV, only 54% of completion summaries were available with an estimated $115,000 in additional costs. The total adjusted costs was about $2.9 million. Almost 37% of SEOCs were for visits only. For the 166 SEOCs where patients received any radiation treatment or planning, the median cost was $18,000. Differences in SEOC pathways are shown in Figure 4. One hundred twenty-one SEOCs (45%) followed the standard pathway, with median SEOC costs of $15,500; when corrected for radiation-specific costs, the median cost increased to $18,000. When adjusted for billing irregularities, the median cost was $20,600. Ninety-nine SEOCs (37%) were for consultation/ follow-up visits only, with a median cost of $220. When omitting shared scans and nonradiation therapy costs and correcting for billing gaps, the median cost decreased to $170. A median of $9200 was paid per patient, with $12,900 for radiation therapy-specific costs and $13,300 adjusted for billing deviations. Narrowing to the 106 patients who received full, radical courses, the median SEOC, ROS, and adjusted radiation therapy costs increased to $19,400, $22,200, and $22,900, respectively (Table 2, Figure 5). Seventy-one SEOCs (26%) had already seen a radiation oncologist before the VA radiation oncology department was aware, and 49 SEOCs (18%) had retroactive approvals (Supplemental materials available at doi:10.12788/fp.0585).
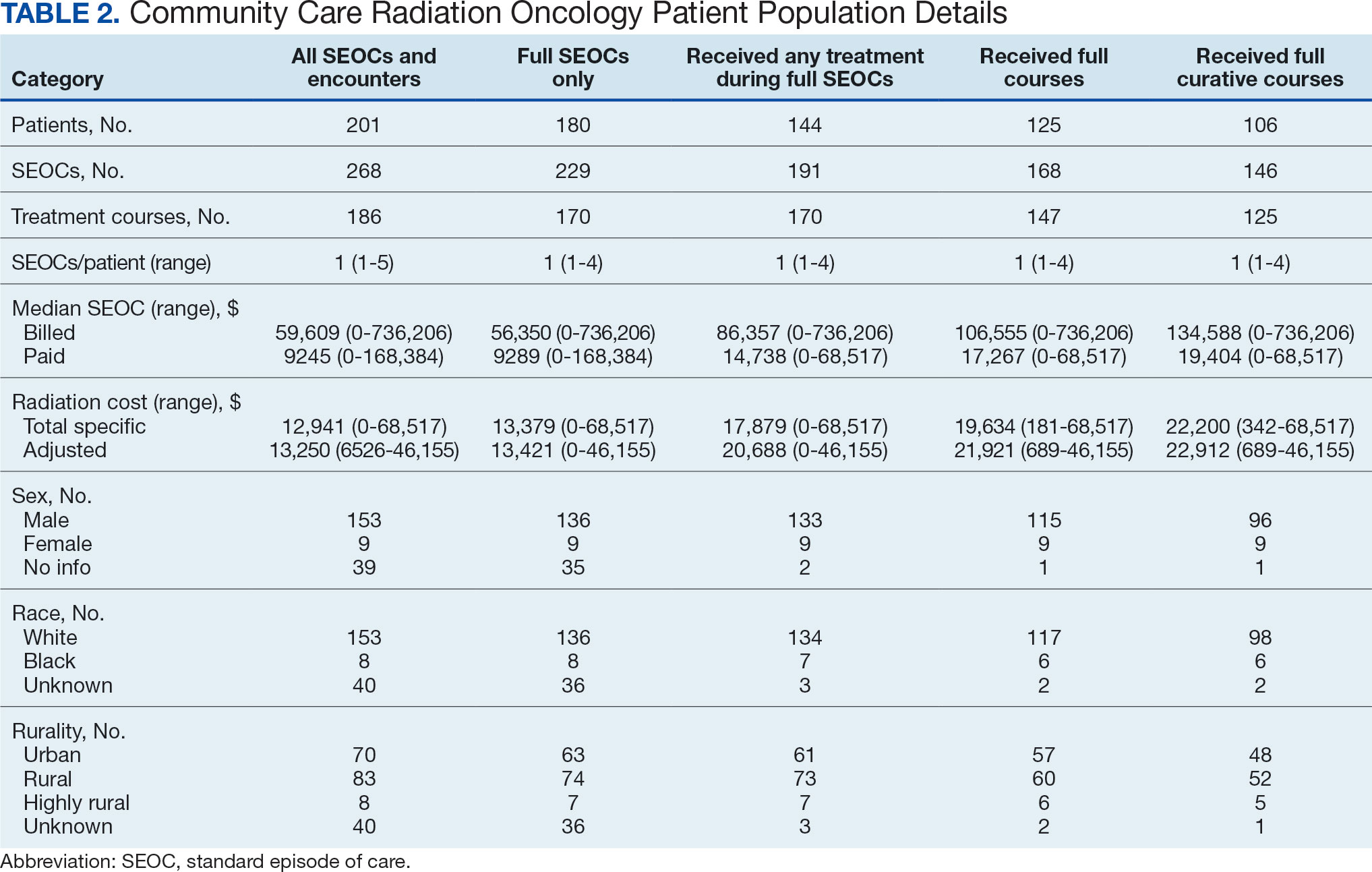
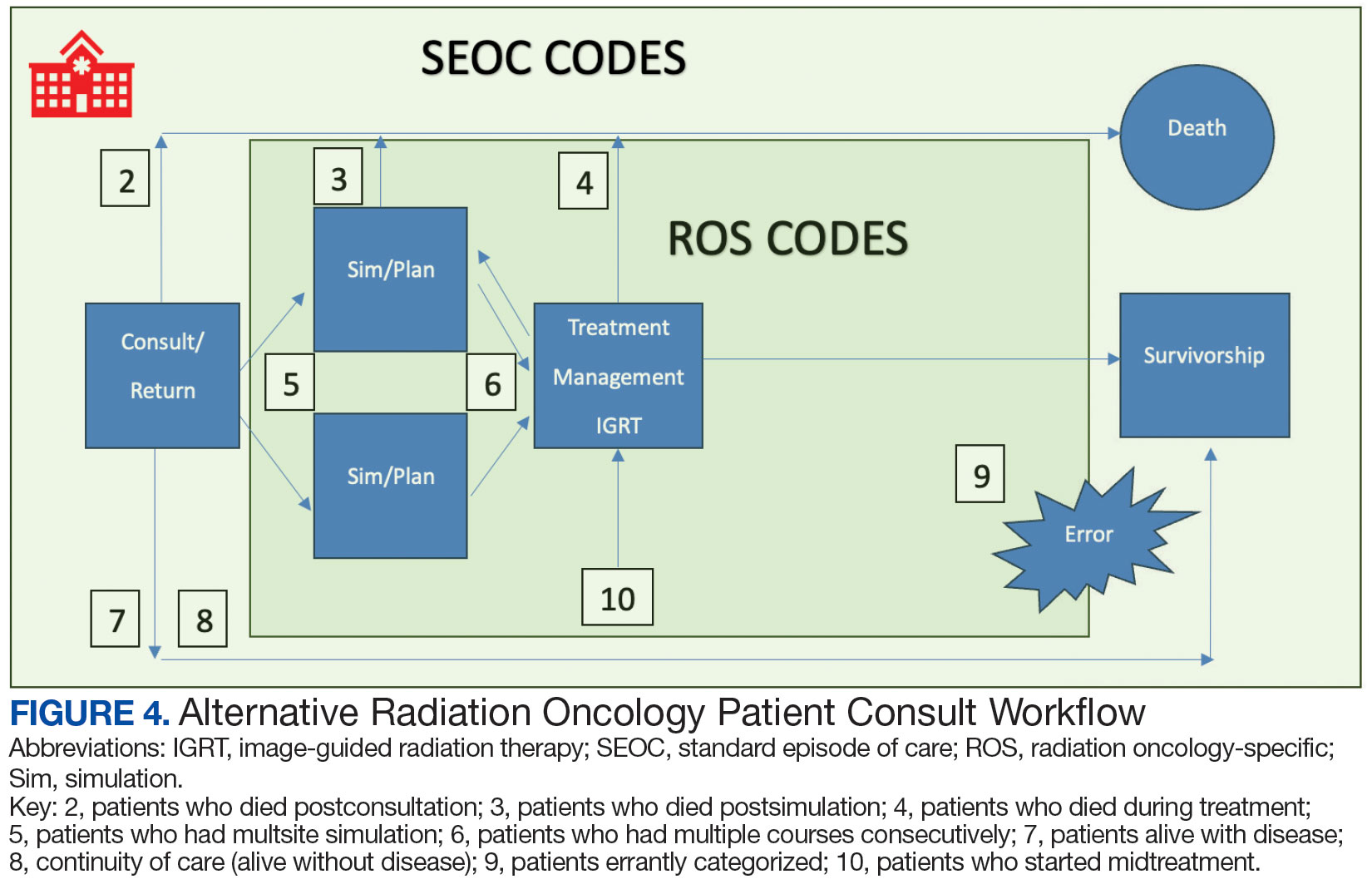
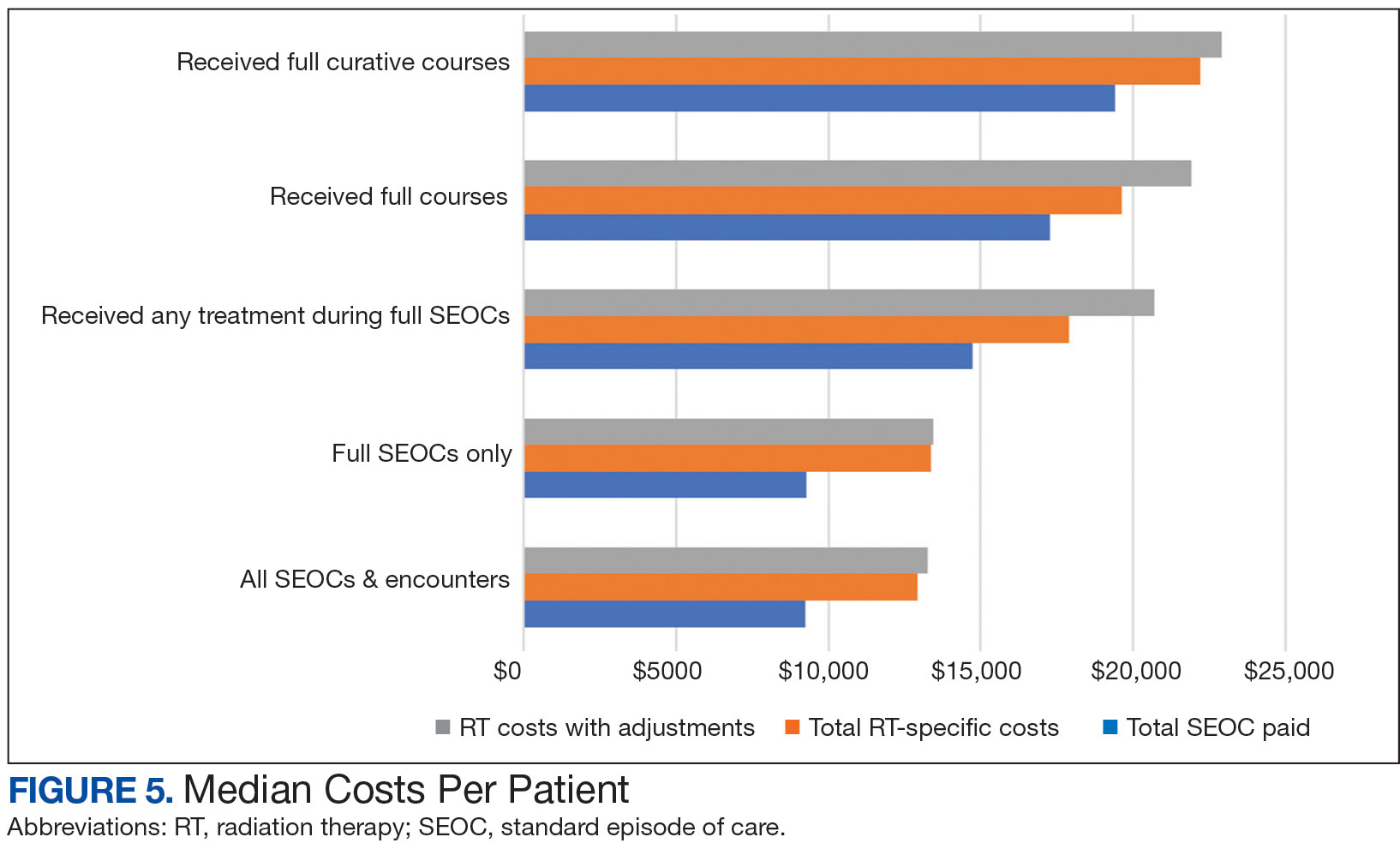
Every consultation charge was reviewed. A typical patient following the standard pathway (eAppendix 2, available at doi:10.12788/ fp.0585) exhibited a predictable pattern of consultation payment, simulation and planning, multiple radiation treatments interspersed with treatment management visits and a cone-down phase, and finishing with a follow-up visit. A less predictable case with excess CPT codes, gaps in charges, and an additional unexpected palliative course is shown in eAppendix 3 (available at doi:10.12788/fp.0585). Gaps occurred in 42% of SEOCs with missed bills costing as much as $12,000. For example, a patient with lung cancer had a treatment summary note for lung cancer after completion that showed the patient received 30 fractions of 2 Gy, a typical course. Only 10 treatment codes and 3 of 6 weekly treatment management codes were available. There was a gap of 20 volumetric modulated arc therapy treatments, 3 physics weekly status checks, 3 physician managements notes, and a computed tomography simulation charge.
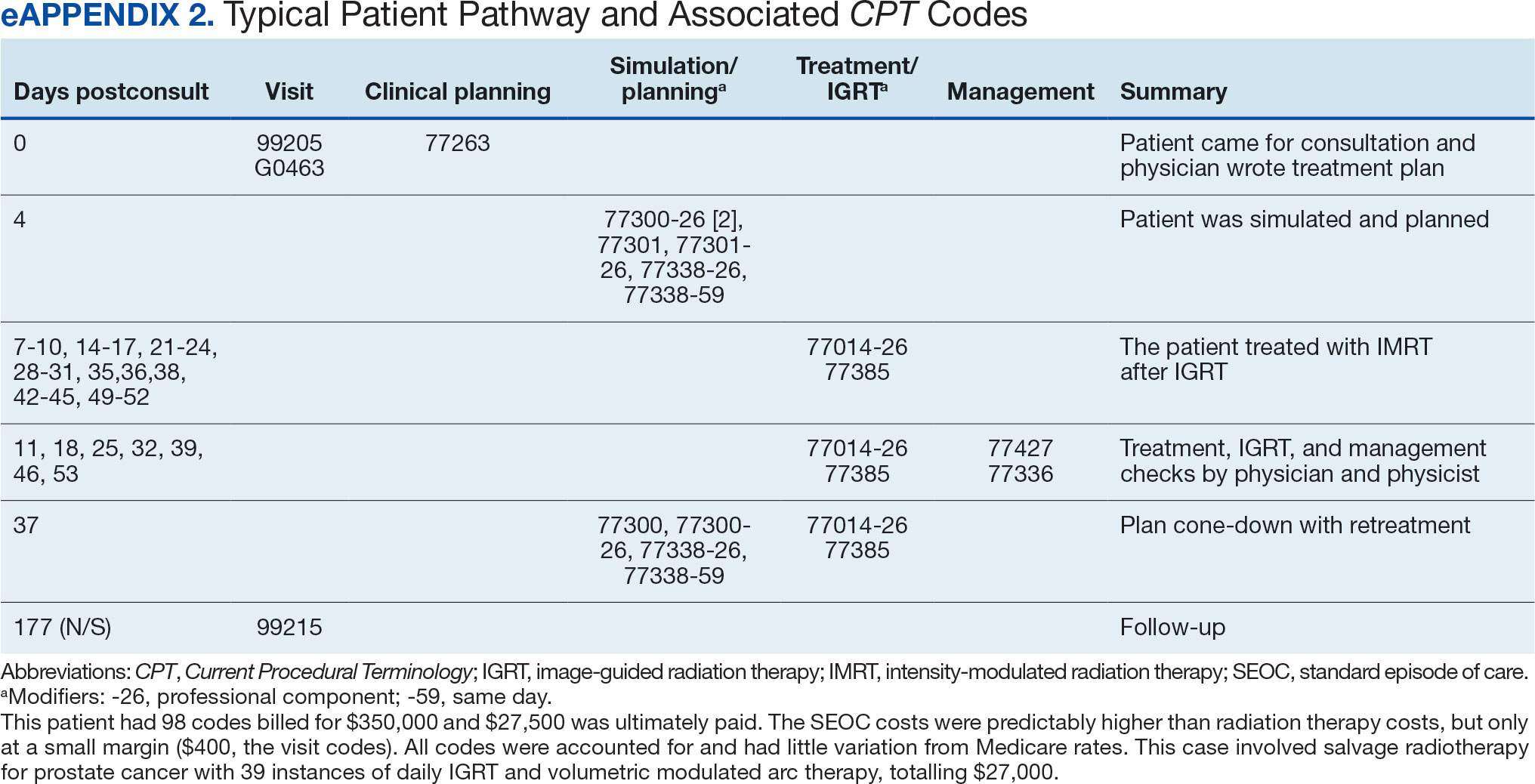

Between AMCMS and CTM, 10,005 CPT codes were evaluated; 1255 (12.5%) were unique to AMCMS (either related to the radiation oncology course, such as Evaluation and Management CPT codes or “other” unrelated codes) while 1158 (11.6%) were unique to CTM. Of the 7592 CPT codes shared between AMCMS and CTM, there was a discrepancy in 135 (1.8%); all were duplicates (CTM showed double payment while AMCMS showed $0 paid). The total CPT code costs came to $3.2 million with $560,000 unique to SEOCs and $500,000 unique to CTM. Treatment codes were the most common (33%) as shown in Table 3 and accounted for 55% of the cost ($1.8 million). About 700 CPT codes were considered “other,” typically for biologic therapeutic agents (Table 4 and eAppendix 4, available at doi:10.12788/fp.0585).
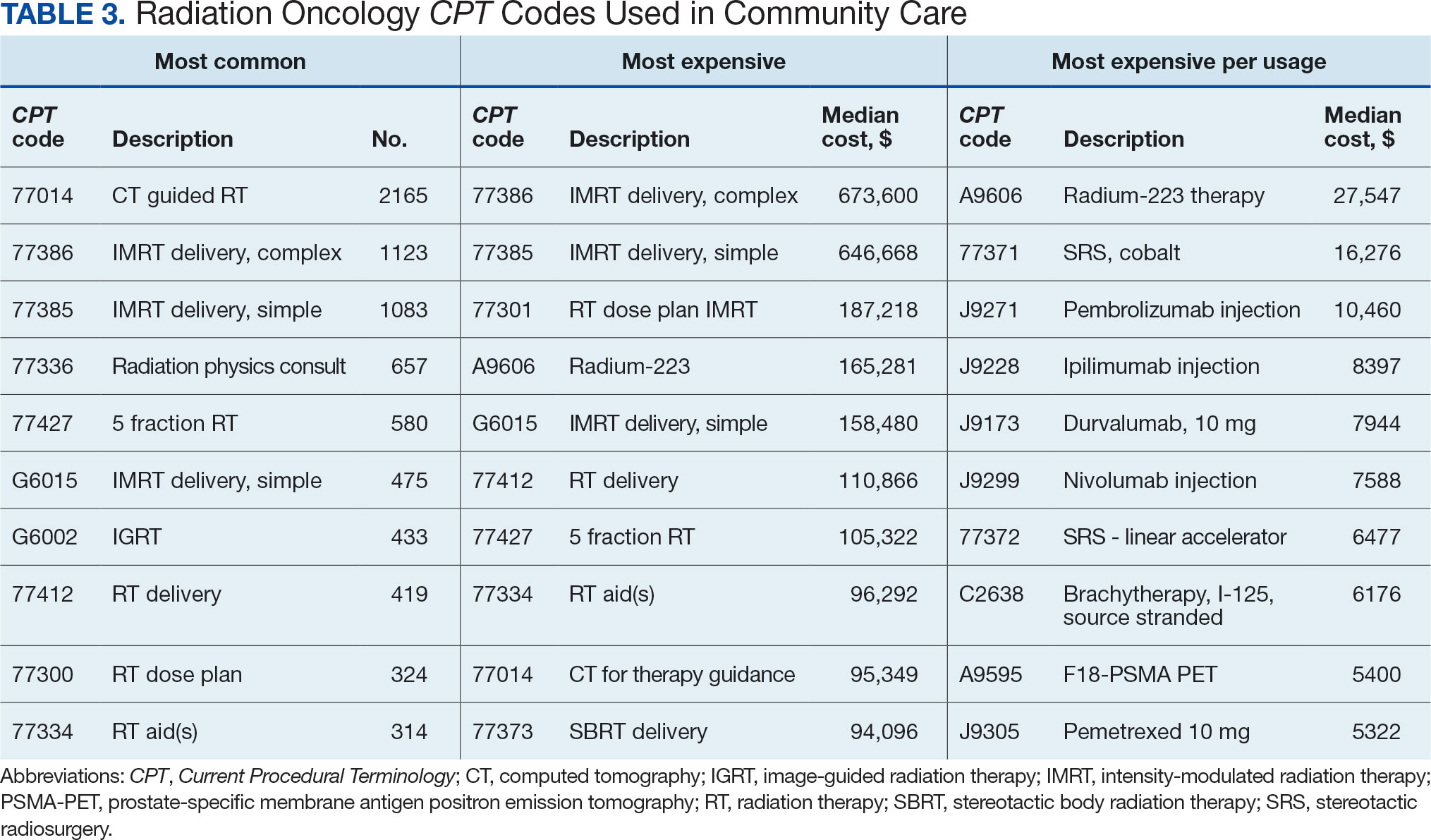
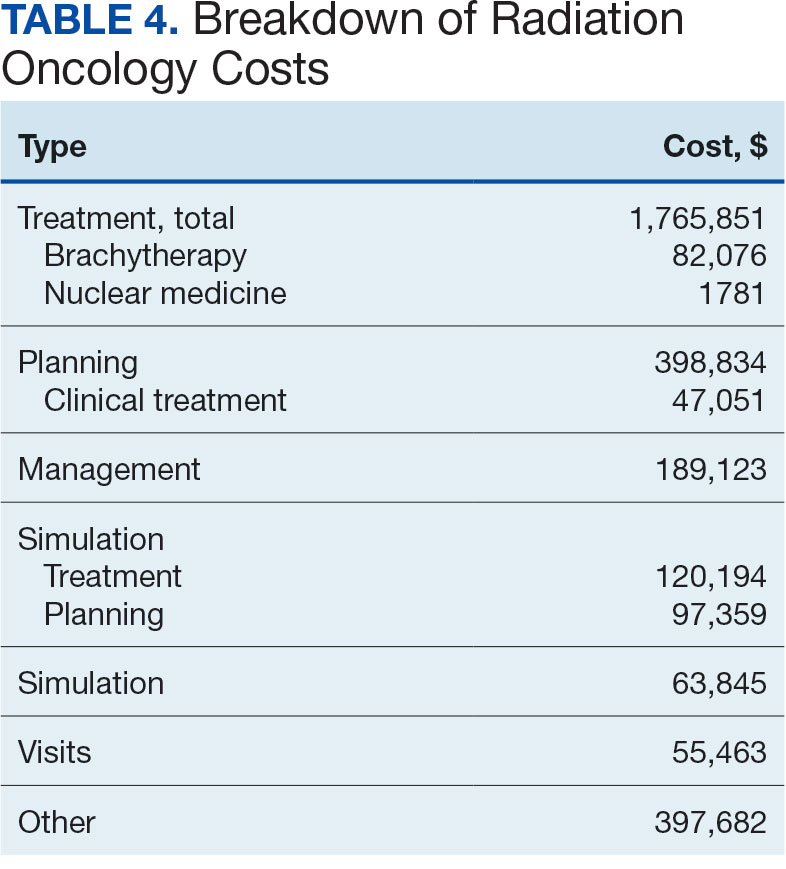

DISCUSSION
The current method of reporting radiation oncology costs used by VA is insufficient and misleading. Better data are needed to summarize purchased care costs to guide decisions about community care at the VA. Investigations into whether the extra costs for quality care (ie, expensive capital equipment, specialized staff, mandatory accreditations) are worthwhile if omitted at other facilities patients choose for their health care needs. No study has defined specialty care-specific costs by evaluating billing receipts from the CDW to answer the question. Kenamond et al highlight the need for radiation oncology for rural patients.11 Drive time was cited as the reason for community care referral for 97% of veterans, many of whom lived in rural locations. Of patients with rurality information who enrolled in community care, 57% came from rural or highly rural counties, and this ratio held for those who received full curative therapies. An executive administrator relying on AMCMS reports would see a median SEOC cost of $5000, but without ROS knowledge in coding, the administrator would miss many additional costs. For example, 2 patients who each had 5 SEOCs during the evaluated period, incurred a total cost of only $1800.
Additionally, an administrator could include miscategorized costs with significant ramifications. The 2 most expensive SEOCs were not typical radiation oncology treatments. A patient undergoing radium-223 dichloride therapy incurred charges exceeding $165,000, contributing disproportionately to the overall median cost analysis; this would normally be administered by the nuclear medicine department. Immunotherapy and chemotherapy are uniformly overseen by medical oncology services, but drug administration codes were still found in radiation oncology SEOCs. A patient (whose SEOC was discontinued but accrued charges) had an electrocardiogram interpretation for $8 as the SEOC cost; 3 other SEOCs continued to incur costs after being discontinued. There were 24 empty SEOCs for patients that had consults to the community, and 2 had notes stating treatment had been delivered yet there was no ROS costs or SEOC costs. Of the 268 encounters, 43% had some sort of billing irregularities (ie, missing treatment costs) that would be unlikely for a private practice to omit; it would be much more likely that the CDW miscategorized the payment despite confirmation of the 2 retrieval systems.
It would be inadvisable to make staffing decisions or forecast costs based on current SEOC reports without specialized curation. A simple yet effective improvement to the cost attribution process would be to restrict the analysis to encounters containing primary radiation treatment codes. This targeted approach allows more accurate identification of patients actively receiving radiation oncology treatment, while excluding those seen solely for consultations or follow-up visits. Implementing this refinement leads to a substantial increase in the median payment—from $5000 to $13,000—without requiring additional coding or data processing, thereby enhancing the accuracy of cost estimates with minimal effort.
Clarifying radiation oncology service costs requires addressing the time frame and services included, given laxity and interpretation of the SEOCs. VA community care departments have streamlined the reimbursement process at the expense of medical cost organization and accuracy; 86% of VA practitioners reported that ≥ 1 potential community health care partners had refused to work with the VA because of payment delays.12 Payments are contingent on correspondence from outside practices for community work. For radiation oncology, this includes the consultation but also critical radiation-related details of treatment, which were omitted nearly half the time. SEOC approval forms have many costly laboratory tests, imaging, and procedures that have little to do with radiation oncology cancer treatments but may be used in the workup and staging process; this creates noise when calculating radiation oncology fiscal cost.
The presumption that an episode of care equates to a completed radiation therapy course is incorrect; this occurs less than half of the time. An episode often refers to a return visit, or conversely, multiple treatment courses. As the patients’ medical homes are their VHA primary care practitioners, it would be particularly challenging to care for the patients without full treatment information, especially if adverse effects from therapy were to arise. As a tertiary specialty, radiation oncology does not seek out patients and are sent consultations from medical oncology, surgical, and medical oncologic specialties. Timesensitive processes such as workup, staging, and diagnosis often occur in parallel. This analysis revealed that patients see outside radiation oncologists prior to the VA. There are ≥ 100 patients who had radiation oncology codes without a radiation oncology SEOC or community care consultation, and in many cases, the consultation was placed after the patient was seen.
Given the lack of uniformity and standardization of patient traffic, the typical and expected pathways were insufficient to find the costs. Too many opportunities for errors and incorrect categorization of costs meant a different method would be necessary. Starting at the inception of the community care consult, only 1 diagnosis code can be entered. For patients with multiple diagnoses, one would not be able to tell what was treated without chart access. Radiation oncology consults come from primary and specialty care practitioners and nurses throughout the VA. Oftentimes, the referral would be solicited by the community radiation oncology clinic, diagnosing community specialty (ie, urology for a patient with prostate cancer), or indirectly from the patient through primary care. Many cases were retroactively approved as the veteran had already been consulted by the community care radiation oncologist. If the patient is drive-time eligible, it would be unlikely that they would leave and choose to return to the VA. There is no way for a facility VA service chief or administrator to mitigate VA community costs of care, especially as shown by the miscategorization of several codes. Database challenges exacerbate the issue: 1 patient changed her first and last name during this time frame, and 2 patients had the same name but different social security numbers. In order to strictly find costs between 2 discrete timepoints, 39 (15%) SEOCs were split and incomplete, and 6 SEOCs contained charges for 2 different patients. This was corrected, and all inadvertent charges were cancelled. Only 1 ICD code is allowed per community care consultation, so an investigation is required to find costs for patients with multiple sites of disease. Additionally, 5 of the patients marked for drive time were actually patients who received Gamma Knife and brachytherapy, services not available at the VA.
Hanks et al first attempted to calculate cost of radiation oncology services. External beam prostate cancer radiotherapy at 3 suburban California centers cost $6750 ($20,503 inflation adjusted) per patient before October 1984 and $5600 ($17,010 inflation adjusted) afterwards.13 According to the American Society for Radiation Oncology, Advocacy Radiation Oncology Case Rate Program Curative radiation courses should cost $20,000 to $30,000 and palliative courses should cost $10,000 to $15,000. These costs are consistent with totals demonstrated in this analysis and similar to the inflation-adjusted Hanks et al figures. Preliminary findings suggest that radiation treatment constituted more than half of the total expenditures, with a notable $4 million increase in adjusted cost compared to the Medicare rates, indicating significant variation. Direct comparisons with Medicaid or commercial payer rates remain unexplored.
Future Directions
During the study period, 201 patients received 186 courses of radiation therapy in the community, while 1014 patients were treated in-house for a total of 833 courses. A forthcoming analysis will directly compare the cost of in-house care with that of communitybased treatment, specifically breaking down expenditure differences by diagnosis. Future research should investigate strategies to align reimbursement with quality metrics, including the potential role of tertiary accreditation in incentivizing high-value care. Additional work is also warranted to assess patient out-ofpocket expenses across care settings and to benchmark VA reimbursement against Medicare, Medicaid, and private insurance rates. In any case, with the increasing possibility of fewer fractions for treatments such as stereotactic radiotherapy or palliative care therapy, there is a clear financial incentive to treat as frequently as allowed despite equal clinical outcomes.
CONCLUSIONS
Veterans increasingly choose to receive care closer to home if the option is available. In the VA iron triangle, cost comes at the expense of access but quantifying this has proved elusive in the cost accounting model currently used at the VA.1 The inclusion of all charges loosely associated with SEOCs significantly impairs the ability to conduct meaningful cost analyses. The current VA methodology not only introduces substantial noise into the data but also leads to a marked underestimation of the true cost of care delivered in community settings. Such misrepresentation risks driving policy decisions that could inappropriately reduce or eliminate in-house radiation oncology services. Categorizing costs effectively in the VA could assist in making managerial and administrative decisions and would prevent damaging service lines based on misleading or incorrect data. A system which differentiates between patients who have received any treatment codes vs those who have not would increase accuracy.
- Kissick W. Medicine’s Dilemmas: Infinite Needs Versus Finite Resources. 1st ed. Yale University Press; 1994.
- Albanese AP, Bope ET, Sanders KM, Bowman M. The VA MISSION Act of 2018: a potential game changer for rural GME expansion and veteran health care. J Rural Health. 2020;36(1):133-136. doi:10.1111/jrh.12360
- Office of Management and Budget (US). Budget of the United States Government, Fiscal Year 2025. Washington, DC: US Government Publishing Office; 2024. Available from: US Department of Veterans Affairs FY 2025 Budget Submission: Budget in Brief.
- US Department of Veterans Affairs. Veteran care claims. Accessed April 3, 2025. https://www.va.gov/COMMUNITYCARE/revenue-ops/Veteran-Care-Claims.asp
- US Centers for Medicare and Medicaid Services. Accessed April 3, 2025. Procedure price lookup https://www.medicare.gov/procedure-price-lookup
- US Department of Veterans Affairs. WellHive -Enterprise. Accessed April 3, 2025. https://department.va.gov/privacy/wp-content/uploads/sites/5/2023/05/FY23WellHiveEnterprisePIA.pdf
- US Centers for Medicare and Medicaid Services. RVU21a physician fee schedule, January 2021 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu21a
- US Centers for Medicare and Medicaid Services. RVU22a physician fee schedule, January 2022 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu22a
- US Centers for Medicare and Medicaid Services. RVU23a physician fee schedule, January 2023 release. Accessed April 3, 2025. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-relative-value-files/rvu23a
- US Centers for Medicare and Medicaid Services. RVU23a Medicare Physician Fee Schedule rates effective January 1, 2024, through March 8, 2024. Accessed on April 3, 2025. https://www.cms.gov/medicare/payment/fee-schedules/physician/pfs-relative-value-files/rvu24a
- Kenamond MC, Mourad WF, Randall ME, Kaushal A. No oncology patient left behind: challenges and solutions in rural radiation oncology. Lancet Reg Health Am. 2022;13:100289. doi:10.1016/j.lana.2022.100289
- Mattocks KM, Kroll-Desrosiers A, Kinney R, Elwy AR, Cunningham KJ, Mengeling MA. Understanding VA’s use of and relationships with community care providers under the MISSION Act. Med Care. 2021;59(Suppl 3):S252-S258. doi:10.1097/MLR.0000000000001545
- Hanks GE, Dunlap K. A comparison of the cost of various treatment methods for early cancer of the prostate. Int J Radiat Oncol Biol Phys. 1986;12(10):1879-1881. doi:10.1016/0360-3016(86)90334-2
- American Society of Radiation Oncology. Radiation oncology case rate program (ROCR). Accessed April 3, 2025. https://www.astro.org/advocacy/key-issues-8f3e5a3b76643265ee93287d79c4fc40/rocr
- Kissick W. Medicine’s Dilemmas: Infinite Needs Versus Finite Resources. 1st ed. Yale University Press; 1994.
- Albanese AP, Bope ET, Sanders KM, Bowman M. The VA MISSION Act of 2018: a potential game changer for rural GME expansion and veteran health care. J Rural Health. 2020;36(1):133-136. doi:10.1111/jrh.12360
- Office of Management and Budget (US). Budget of the United States Government, Fiscal Year 2025. Washington, DC: US Government Publishing Office; 2024. Available from: US Department of Veterans Affairs FY 2025 Budget Submission: Budget in Brief.
- US Department of Veterans Affairs. Veteran care claims. Accessed April 3, 2025. https://www.va.gov/COMMUNITYCARE/revenue-ops/Veteran-Care-Claims.asp
- US Centers for Medicare and Medicaid Services. Accessed April 3, 2025. Procedure price lookup https://www.medicare.gov/procedure-price-lookup
- US Department of Veterans Affairs. WellHive -Enterprise. Accessed April 3, 2025. https://department.va.gov/privacy/wp-content/uploads/sites/5/2023/05/FY23WellHiveEnterprisePIA.pdf
- US Centers for Medicare and Medicaid Services. RVU21a physician fee schedule, January 2021 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu21a
- US Centers for Medicare and Medicaid Services. RVU22a physician fee schedule, January 2022 release. Accessed April 3, 2025. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu22a
- US Centers for Medicare and Medicaid Services. RVU23a physician fee schedule, January 2023 release. Accessed April 3, 2025. https://www.cms.gov/medicare/medicare-fee-service-payment/physicianfeesched/pfs-relative-value-files/rvu23a
- US Centers for Medicare and Medicaid Services. RVU23a Medicare Physician Fee Schedule rates effective January 1, 2024, through March 8, 2024. Accessed on April 3, 2025. https://www.cms.gov/medicare/payment/fee-schedules/physician/pfs-relative-value-files/rvu24a
- Kenamond MC, Mourad WF, Randall ME, Kaushal A. No oncology patient left behind: challenges and solutions in rural radiation oncology. Lancet Reg Health Am. 2022;13:100289. doi:10.1016/j.lana.2022.100289
- Mattocks KM, Kroll-Desrosiers A, Kinney R, Elwy AR, Cunningham KJ, Mengeling MA. Understanding VA’s use of and relationships with community care providers under the MISSION Act. Med Care. 2021;59(Suppl 3):S252-S258. doi:10.1097/MLR.0000000000001545
- Hanks GE, Dunlap K. A comparison of the cost of various treatment methods for early cancer of the prostate. Int J Radiat Oncol Biol Phys. 1986;12(10):1879-1881. doi:10.1016/0360-3016(86)90334-2
- American Society of Radiation Oncology. Radiation oncology case rate program (ROCR). Accessed April 3, 2025. https://www.astro.org/advocacy/key-issues-8f3e5a3b76643265ee93287d79c4fc40/rocr
Community Care Radiation Oncology Cost Calculations for a VA Medical Center
Community Care Radiation Oncology Cost Calculations for a VA Medical Center
Clinicians Should Have Private Spaces for Telehealth According to VA Memo
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”
US Department of Veterans Affairs (VA) officials are insisting that when remote telehealth clinicians return to an office setting, they must have private workspaces “that foster trusted, confidential, and therapeutic relationships with veterans,” according to an April internal memo reported on by NPR.
The return-to-office mandate followed a Trump Administration executive order in February indicated that mental health clinicians at the US Department of Veterans Affairs (VA) must physically return to their workplace by May 5. For some, the deadline came as early as April 14; however, that order, like many others, may now be being revised or reconsidered due to concerns that have been raised. Many mental health clinicians were hired specifically to work remotely. They worried there would simply not be enough space for them, particularly to provide confidential counseling.
Millions of veterans use telehealth to access VA care. More than 98% of VA mental health clinicians have conducted ≥ 1 video visit to screen and treat patients for anxiety, depression, posttraumatic stress disorder, and more. Telehealth has been particularly important for veterans living in rural communities.
The April VA memo stipulated that “spaces used to deliver synchronous telehealth services should offer the same level of privacy and therapeutic environment applicable to an in-person visit in the same space.”
Therapists, patients, advocacy groups, and lawmakers have expressed concern about the potential impacts the policy change could have on patient care for veterans and, above all, about what it could mean for privacy. On Mar. 27, the American Psychological Association issued a statement noting that the change “resulted in providers being asked to conduct sensitive therapy sessions in open office environments, cubicles, or shared spaces that fail to meet basic confidentiality and privacy requirements for the delivery of mental health care services.”
Twenty Democrats in the House of Representatives sent a letter to VA Secretary Doug Collins expressing concern with the return to office policy. According to the letter a VA social worker supervisor reported managing their caseload while sharing a 100 ft2 shower space with another supervisor. It also reported that Clinical Resource Hub employees were being told to report to buildings where federal employees from other agencies work. “We have heard from countless stakeholders, veterans, and Department of Veterans Affairs (VA) employees that by carrying out President Trump’s blanket return-to-office policy your administration is damaging veteran and employee trust in VA, disrupting and impeding veterans’ access to care, and creating untenable and inefficient conditions for both veterans and the VA workforce,” the letter stated.
“This is a clear violation of veterans’ privacy and VA’s obligation to protect veterans’ private health information, and risks violation of the Health Insurance Portability and Accountability Act (HIPAA),” the letter added.
The lawmakers noted that, as of March 10, the VA was exempting Veterans Crisis Line workers, most of whom had been working remotely for the past 5 years, responding to more than 10 million calls, texts, and chats. That move, they said, indicated “that you understand there will be negative impacts to veterans’ care due to the return-to-office order and that these must be mitigated.”
VA spokesperson Peter Kasperowicz called the privacy concerns “nonsensical” and blamed “fear mongering from the media.” The VA, he said, “is no longer a place where the status quo for employees is to simply phone it in from home.” He also claimed that “the small number of employees who are desperate to avoid returning to the office will do more to drive away staff and patients than VA’s commonsense return-to-office policy ever will.”
VA care, he said, would continue uninterrupted and the “VA will ensure that employees have a workspace that is appropriate for the work they do.”