User login
Orchestrated protocols for treating CLABSI decreases hospitalizations
Hospitals and health centers that participate in orchestrated testing protocols for diagnosis and treatment of central line–associated bloodstream infections (CLABSI) have lower rates of hospital admissions, according to a new study published in Pediatrics.
“The purpose of the SLUG Bug (Standardizing Line Care Under Guideline Recommendations) collaborative was to provide potentially better practice recommendations for neonatal health care professionals in care and maintenance of CVCs [central venous catheters] and to prevent CLABSI [central line–associated bloodstream infections],” wrote Dr. Anthony J. Piazza of the department of pediatrics at Emory University, Atlanta, and his colleagues.
The researchers examined 17 health care centers, from which eight test groups were identified and evaluated via orchestrated testing methods. Each center was surveyed to compare CLABSI rates before and after implementation of SLUG Bug protocols, and to determine each center’s compliance rate on procedural aspects such as tubing change, hub care, and sterilization. The measurable target Dr. Piazza and his colleagues had in mind was to lower CLABSI rates by 15% – deemed “a clinically meaningful target” – over the course of 12 months (Pediatrics. 2016 Dec. 22. doi:10.1542/peds.2014-3642).
The mean CLABSI rate across centers declined from 1.333 per 1,000 line-days at baseline to 1.076 per 1,000 line-days at 12 months, a reduction of 19.28%, meeting the benchmark set by the investigators. Furthermore, all but 1 of the 17 centers included in the study recorded a compliance rate of 75% or higher. Of the eight study groups, only two did not see a reduction in CLABSI rates, with changes of 0.512 and 0.444; all other groups saw CLABSI rates decrease anywhere from –0.157 to –1.860.
“The CLABSI Clinical Practice Recommendation is generalizable to other settings in which prolonged CVC use is medically necessary,” the authors wrote, adding that the “results support strong consideration for the use of sterile [tubing change] in conjunction with [hub care] compliance monitoring to further reduce NICU rates of CLABSI.”
The study did not receive any outside funding. Dr. Piazza did not report any relevant financial disclosures, but several coauthors reported potential conflicts of their own.
Hospitals and health centers that participate in orchestrated testing protocols for diagnosis and treatment of central line–associated bloodstream infections (CLABSI) have lower rates of hospital admissions, according to a new study published in Pediatrics.
“The purpose of the SLUG Bug (Standardizing Line Care Under Guideline Recommendations) collaborative was to provide potentially better practice recommendations for neonatal health care professionals in care and maintenance of CVCs [central venous catheters] and to prevent CLABSI [central line–associated bloodstream infections],” wrote Dr. Anthony J. Piazza of the department of pediatrics at Emory University, Atlanta, and his colleagues.
The researchers examined 17 health care centers, from which eight test groups were identified and evaluated via orchestrated testing methods. Each center was surveyed to compare CLABSI rates before and after implementation of SLUG Bug protocols, and to determine each center’s compliance rate on procedural aspects such as tubing change, hub care, and sterilization. The measurable target Dr. Piazza and his colleagues had in mind was to lower CLABSI rates by 15% – deemed “a clinically meaningful target” – over the course of 12 months (Pediatrics. 2016 Dec. 22. doi:10.1542/peds.2014-3642).
The mean CLABSI rate across centers declined from 1.333 per 1,000 line-days at baseline to 1.076 per 1,000 line-days at 12 months, a reduction of 19.28%, meeting the benchmark set by the investigators. Furthermore, all but 1 of the 17 centers included in the study recorded a compliance rate of 75% or higher. Of the eight study groups, only two did not see a reduction in CLABSI rates, with changes of 0.512 and 0.444; all other groups saw CLABSI rates decrease anywhere from –0.157 to –1.860.
“The CLABSI Clinical Practice Recommendation is generalizable to other settings in which prolonged CVC use is medically necessary,” the authors wrote, adding that the “results support strong consideration for the use of sterile [tubing change] in conjunction with [hub care] compliance monitoring to further reduce NICU rates of CLABSI.”
The study did not receive any outside funding. Dr. Piazza did not report any relevant financial disclosures, but several coauthors reported potential conflicts of their own.
Hospitals and health centers that participate in orchestrated testing protocols for diagnosis and treatment of central line–associated bloodstream infections (CLABSI) have lower rates of hospital admissions, according to a new study published in Pediatrics.
“The purpose of the SLUG Bug (Standardizing Line Care Under Guideline Recommendations) collaborative was to provide potentially better practice recommendations for neonatal health care professionals in care and maintenance of CVCs [central venous catheters] and to prevent CLABSI [central line–associated bloodstream infections],” wrote Dr. Anthony J. Piazza of the department of pediatrics at Emory University, Atlanta, and his colleagues.
The researchers examined 17 health care centers, from which eight test groups were identified and evaluated via orchestrated testing methods. Each center was surveyed to compare CLABSI rates before and after implementation of SLUG Bug protocols, and to determine each center’s compliance rate on procedural aspects such as tubing change, hub care, and sterilization. The measurable target Dr. Piazza and his colleagues had in mind was to lower CLABSI rates by 15% – deemed “a clinically meaningful target” – over the course of 12 months (Pediatrics. 2016 Dec. 22. doi:10.1542/peds.2014-3642).
The mean CLABSI rate across centers declined from 1.333 per 1,000 line-days at baseline to 1.076 per 1,000 line-days at 12 months, a reduction of 19.28%, meeting the benchmark set by the investigators. Furthermore, all but 1 of the 17 centers included in the study recorded a compliance rate of 75% or higher. Of the eight study groups, only two did not see a reduction in CLABSI rates, with changes of 0.512 and 0.444; all other groups saw CLABSI rates decrease anywhere from –0.157 to –1.860.
“The CLABSI Clinical Practice Recommendation is generalizable to other settings in which prolonged CVC use is medically necessary,” the authors wrote, adding that the “results support strong consideration for the use of sterile [tubing change] in conjunction with [hub care] compliance monitoring to further reduce NICU rates of CLABSI.”
The study did not receive any outside funding. Dr. Piazza did not report any relevant financial disclosures, but several coauthors reported potential conflicts of their own.
FROM PEDIATRICS
Key clinical point: Multicenter orchestrated testing for central line–associated bloodstream infection (CLABSI) leads to significantly decreased NICU admission rates.
Major finding: CLABSI rates decreased from 1.333 to 1.076 per 1,000 line-days (19.28%), with 16 of 17 centers achieving at least 75% compliance rates.
Data source: Cohort study of 17 hospital centers.
Disclosures: The study received no external funding. Several coauthors reported individual potential conflicts of interest.
Dental, obstetrics, and gynecology residents have highest NSI rate
Needlestick and sharps injuries are most common among dental residents and obstetrics and gynecology residents, according to Dr. Thomas P. Marnejon and his associates.
During the period from 2000 to 2014 at Mercy Health Youngstown (Ohio), 924 residents were trained, and 129 needlestick and sharps injuries (NSIs) were reported. NSIs were most common during the first year of residency, with frequency decreasing with each year. Nearly 31% of dental residents and nearly 29% of ob.gyn. residents reported an NSI. On the low end were transitional medicine residents (3.3%) and family medicine residents (2.7%).
Injuries to the left hand were nearly twice as common as injuries to the right hand, with left index and left middle finger NSIs accounting for more than 36% of all reported NSIs. NSIs were most commonly caused by suture needles, accounting for 43.4% of injuries; scalpel and blood gas syringe injuries also were common.
No source patients had human immunodeficiency virus, but 16 had hepatitis C, and 1 had hepatitis B; however, no seroconversion in residents was reported.
“For new residents, additional procedural skill simulation using sharp instruments may decrease NSI. However, a majority of residents felt comfortable in procedures with instruments causing injury. Despite resident-reported mastery, caution to avoid both overconfidence and decreased attention to NSI risk is warranted,” the investigators noted.
Find the full research letter in JAMA Internal Medicine (2015 Dec 7. doi: 10.1001/jamainternmed.2015.6828).
Needlestick and sharps injuries are most common among dental residents and obstetrics and gynecology residents, according to Dr. Thomas P. Marnejon and his associates.
During the period from 2000 to 2014 at Mercy Health Youngstown (Ohio), 924 residents were trained, and 129 needlestick and sharps injuries (NSIs) were reported. NSIs were most common during the first year of residency, with frequency decreasing with each year. Nearly 31% of dental residents and nearly 29% of ob.gyn. residents reported an NSI. On the low end were transitional medicine residents (3.3%) and family medicine residents (2.7%).
Injuries to the left hand were nearly twice as common as injuries to the right hand, with left index and left middle finger NSIs accounting for more than 36% of all reported NSIs. NSIs were most commonly caused by suture needles, accounting for 43.4% of injuries; scalpel and blood gas syringe injuries also were common.
No source patients had human immunodeficiency virus, but 16 had hepatitis C, and 1 had hepatitis B; however, no seroconversion in residents was reported.
“For new residents, additional procedural skill simulation using sharp instruments may decrease NSI. However, a majority of residents felt comfortable in procedures with instruments causing injury. Despite resident-reported mastery, caution to avoid both overconfidence and decreased attention to NSI risk is warranted,” the investigators noted.
Find the full research letter in JAMA Internal Medicine (2015 Dec 7. doi: 10.1001/jamainternmed.2015.6828).
Needlestick and sharps injuries are most common among dental residents and obstetrics and gynecology residents, according to Dr. Thomas P. Marnejon and his associates.
During the period from 2000 to 2014 at Mercy Health Youngstown (Ohio), 924 residents were trained, and 129 needlestick and sharps injuries (NSIs) were reported. NSIs were most common during the first year of residency, with frequency decreasing with each year. Nearly 31% of dental residents and nearly 29% of ob.gyn. residents reported an NSI. On the low end were transitional medicine residents (3.3%) and family medicine residents (2.7%).
Injuries to the left hand were nearly twice as common as injuries to the right hand, with left index and left middle finger NSIs accounting for more than 36% of all reported NSIs. NSIs were most commonly caused by suture needles, accounting for 43.4% of injuries; scalpel and blood gas syringe injuries also were common.
No source patients had human immunodeficiency virus, but 16 had hepatitis C, and 1 had hepatitis B; however, no seroconversion in residents was reported.
“For new residents, additional procedural skill simulation using sharp instruments may decrease NSI. However, a majority of residents felt comfortable in procedures with instruments causing injury. Despite resident-reported mastery, caution to avoid both overconfidence and decreased attention to NSI risk is warranted,” the investigators noted.
Find the full research letter in JAMA Internal Medicine (2015 Dec 7. doi: 10.1001/jamainternmed.2015.6828).
FROM JAMA INTERNAL MEDICINE
Minority of U.S. hospitals mandate flu vaccination
Less than 50% of U.S. hospitals require health care workers to receive annual flu shots, according to a survey study with responses from nearly 500 facilities.
The study, published online in Infection Control & Hospital Epidemiology (2015 Nov 27. doi: 10.1017/ice.2015.277), also found that only 1.3% of U.S. Veterans Affairs hospitals mandate flu shots, despite no law preventing them from doing so.
Dr. M. Todd Greene of the University of Michigan, Ann Arbor, and the Veterans Affairs/University of Michigan Patient Safety Enhancement Program, led the study, which asked hospital infection specialists to report on their institutions’ policies regarding annual vaccines, the stated reasons behind these policies, and other efforts to promote vaccination or discourage nonvaccination in 2013. Only 42.7% of respondents from 386 non-VA hospitals said their institutions required universal vaccination of personnel. However, many reported policies promoting uptake and/or mandating declination forms and face masks for personnel who opted out.
Among non-VA hospitals without mandatory vaccination, 22% said their administrations were unwilling to require it, while another 22% said vaccination was “strongly recommended” or otherwise promoted, and 21% said face masks and signed declination forms were mandatory for nonvaccinated personnel. Union concerns were cited by 8% as a reason vaccination was not required. In the VA system, meanwhile, 57% of hospitals without mandatory vaccination cited federal agency status as a reason, and more than a quarter cited union issues.
Dr. Greene and colleagues noted that while the VA does not have a national vaccination requirement, individual hospitals are free to determine their own policies. The Veterans Hospital Administration estimates vaccine uptake among workers at its hospitals to be only 55% in recent flu seasons, while a recent study by the Centers for Disease Control and Prevention found that overall about 77% of U.S. health care workers in diverse clinical settings received flu shots in 2014-2015, and that those settings with vaccination requirements saw 96% of personnel covered.
Dr. Greene and colleagues’ study was funded by the Blue Cross Blue Shield of Michigan Foundation, the Department of Veterans Affairs, and the National Center for Patient Safety. None of its authors disclosed conflicts of interest.
Less than 50% of U.S. hospitals require health care workers to receive annual flu shots, according to a survey study with responses from nearly 500 facilities.
The study, published online in Infection Control & Hospital Epidemiology (2015 Nov 27. doi: 10.1017/ice.2015.277), also found that only 1.3% of U.S. Veterans Affairs hospitals mandate flu shots, despite no law preventing them from doing so.
Dr. M. Todd Greene of the University of Michigan, Ann Arbor, and the Veterans Affairs/University of Michigan Patient Safety Enhancement Program, led the study, which asked hospital infection specialists to report on their institutions’ policies regarding annual vaccines, the stated reasons behind these policies, and other efforts to promote vaccination or discourage nonvaccination in 2013. Only 42.7% of respondents from 386 non-VA hospitals said their institutions required universal vaccination of personnel. However, many reported policies promoting uptake and/or mandating declination forms and face masks for personnel who opted out.
Among non-VA hospitals without mandatory vaccination, 22% said their administrations were unwilling to require it, while another 22% said vaccination was “strongly recommended” or otherwise promoted, and 21% said face masks and signed declination forms were mandatory for nonvaccinated personnel. Union concerns were cited by 8% as a reason vaccination was not required. In the VA system, meanwhile, 57% of hospitals without mandatory vaccination cited federal agency status as a reason, and more than a quarter cited union issues.
Dr. Greene and colleagues noted that while the VA does not have a national vaccination requirement, individual hospitals are free to determine their own policies. The Veterans Hospital Administration estimates vaccine uptake among workers at its hospitals to be only 55% in recent flu seasons, while a recent study by the Centers for Disease Control and Prevention found that overall about 77% of U.S. health care workers in diverse clinical settings received flu shots in 2014-2015, and that those settings with vaccination requirements saw 96% of personnel covered.
Dr. Greene and colleagues’ study was funded by the Blue Cross Blue Shield of Michigan Foundation, the Department of Veterans Affairs, and the National Center for Patient Safety. None of its authors disclosed conflicts of interest.
Less than 50% of U.S. hospitals require health care workers to receive annual flu shots, according to a survey study with responses from nearly 500 facilities.
The study, published online in Infection Control & Hospital Epidemiology (2015 Nov 27. doi: 10.1017/ice.2015.277), also found that only 1.3% of U.S. Veterans Affairs hospitals mandate flu shots, despite no law preventing them from doing so.
Dr. M. Todd Greene of the University of Michigan, Ann Arbor, and the Veterans Affairs/University of Michigan Patient Safety Enhancement Program, led the study, which asked hospital infection specialists to report on their institutions’ policies regarding annual vaccines, the stated reasons behind these policies, and other efforts to promote vaccination or discourage nonvaccination in 2013. Only 42.7% of respondents from 386 non-VA hospitals said their institutions required universal vaccination of personnel. However, many reported policies promoting uptake and/or mandating declination forms and face masks for personnel who opted out.
Among non-VA hospitals without mandatory vaccination, 22% said their administrations were unwilling to require it, while another 22% said vaccination was “strongly recommended” or otherwise promoted, and 21% said face masks and signed declination forms were mandatory for nonvaccinated personnel. Union concerns were cited by 8% as a reason vaccination was not required. In the VA system, meanwhile, 57% of hospitals without mandatory vaccination cited federal agency status as a reason, and more than a quarter cited union issues.
Dr. Greene and colleagues noted that while the VA does not have a national vaccination requirement, individual hospitals are free to determine their own policies. The Veterans Hospital Administration estimates vaccine uptake among workers at its hospitals to be only 55% in recent flu seasons, while a recent study by the Centers for Disease Control and Prevention found that overall about 77% of U.S. health care workers in diverse clinical settings received flu shots in 2014-2015, and that those settings with vaccination requirements saw 96% of personnel covered.
Dr. Greene and colleagues’ study was funded by the Blue Cross Blue Shield of Michigan Foundation, the Department of Veterans Affairs, and the National Center for Patient Safety. None of its authors disclosed conflicts of interest.
FROM INFECTION CONTROL & HOSPITAL EPIDEMIOLOGY
Key clinical point: Despite evidence that mandatory influenza vaccination policies result in high coverage, fewer than half of U.S. hospitals, and very few VA hospitals, require workers to be vaccinated.
Major finding: 42.7% of non-VA hospitals and only 1.3% of VA hospitals required all health care workers to receive flu shots in 2013.
Data source: A survey of infection control specialists at 571 non-VA hospitals (71% responding, n = 403) and 126 VA hospitals (63% responding, n = 80) in 2013.
Disclosures: Blue Cross Blue Shield of Michigan Foundation, the Department of Veterans Affairs, and the National Center for Patient Safety funded the study, and authors reported no conflicts of interest.
IDWEEK: Cefazolin beats ceftriaxone for MSSA bacteremia treatment
SAN DIEGO – Veteran patients treated with ceftriaxone for methicillin-susceptible Staphylococcus aureus bacteremia were more likely to have treatment failure, compared with those who received cefazolin, a retrospective observational study found.
“To date, no study has specifically evaluated cefazolin versus ceftriaxone for MSSA bacteremia,” Dustin Carr, Pharm.D., said at an annual scientific meeting on infectious diseases. “The main design of this study was to inform our current site and give us additional antimicrobial stewardship opportunities to ensure appropriate selection, dosing, route, and duration.”
In a study conducted during Dr. Carr’s residency training at Louis Stokes Cleveland VA Medical Center, he and his colleagues retrospectively evaluated veteran patients with MSSA bacteremia from January 2009 to August 2014 who received at least 14 days of parenteral cefazolin or ceftriaxone. The use of concomitant anti-staphylococcal agents were excluded, as were patients with polymicrobial infections and those who received empiric antibiotics greater than 72 hours after cultures were finalized. Dr. Carr noted that infectious diseases clinicians are consulted for all cases of MSSA bacteremia at the Louis Stokes Cleveland VA Medical Center, which accounts for about 25% of all outpatient parenteral antimicrobial therapy cases.
Treatment failure was defined as unplanned extension of parenteral antimicrobial therapy, failure to complete a course of parenteral therapy, relapse or recurrence of infection within 90 days, addition of suppressive oral antimicrobial therapy, readmission or unanticipated surgical intervention within 90 days, and being lost to follow-up. Secondary outcomes were relapse and recurrence within 90 days of treatment, overall 90-day mortality, rate of Clostridium difficile infection within 90 days, adverse drug reactions, and cost of IV antimicrobials. The researchers used logistic regression to assess variables of treatment failure.
Dr. Carr, who is currently an infectious diseases specialty resident at Wake Forest Baptist Health, Winston-Salem, N.C., reported results from 71 patients: 38 who received cefazolin (the cefazolin group) and 33 who received ceftriaxone (the ceftriaxone group). Patients in the cefazolin group were more likely to be on dialysis, compared with those in the ceftriaxone group (24% vs. 0%, respectively; P = .003) and they were more likely to have a prosthesis (53% vs. 24%; P = .015).
The researchers observed no significant differences in the comorbidities between the two groups, but there was more IV drug use in the cefazolin group (13% vs. 0%). The primary source of infection did not differ between the groups, but SSTIs were more likely to be treated with ceftriaxone, compared with cefazolin (33% vs. 8%; P = .086).
Dr. Carr reported that 28.9% of patients in the cefazolin group experienced a treatment failure, compared with 54.5% of those in the ceftriaxone group, a difference that was statistically significant (P = .029). There were no significant differences in the rate of most secondary outcomes between the two groups, with the exception of cost and loss to follow-up. The mean cost of IV therapy per patient was $746.51 in the cefazolin group, compared with $60.30 in the ceftriaxone group, while 5.3% of patients in the cefazolin group were lost to follow-up, compared with 12.1% in the ceftriaxone group.
By setting of outpatient parenteral antibiotic therapy, treatment failure occurred most often in the community skilled nursing facility setting (71%), followed by home settings (41%) and the VA long-term care facility attached to Louis Stokes Cleveland VA Medical Center (17%).
On logistic regression, the only significant predictors of treatment failure among all patients were duration of IV therapy (OR 1.05; P = .015), having heart failure (OR 7.93; P less than .001), as well as being treated in an outside community skilled nursing facility, compared with being treated at the long-term care setting attached to Louis Stokes Cleveland VA Medical Center (P = .008).
Dr. Carr acknowledged certain limitations of the study, including its retrospective design and the fact that it lacked data on antimicrobial susceptibilities and minimum inhibitory concentrations. Other limitations, he said, were that patients were allowed to receive cefazolin prior to ceftriaxone use and that there were low frequencies of secondary outcomes.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
SAN DIEGO – Veteran patients treated with ceftriaxone for methicillin-susceptible Staphylococcus aureus bacteremia were more likely to have treatment failure, compared with those who received cefazolin, a retrospective observational study found.
“To date, no study has specifically evaluated cefazolin versus ceftriaxone for MSSA bacteremia,” Dustin Carr, Pharm.D., said at an annual scientific meeting on infectious diseases. “The main design of this study was to inform our current site and give us additional antimicrobial stewardship opportunities to ensure appropriate selection, dosing, route, and duration.”
In a study conducted during Dr. Carr’s residency training at Louis Stokes Cleveland VA Medical Center, he and his colleagues retrospectively evaluated veteran patients with MSSA bacteremia from January 2009 to August 2014 who received at least 14 days of parenteral cefazolin or ceftriaxone. The use of concomitant anti-staphylococcal agents were excluded, as were patients with polymicrobial infections and those who received empiric antibiotics greater than 72 hours after cultures were finalized. Dr. Carr noted that infectious diseases clinicians are consulted for all cases of MSSA bacteremia at the Louis Stokes Cleveland VA Medical Center, which accounts for about 25% of all outpatient parenteral antimicrobial therapy cases.
Treatment failure was defined as unplanned extension of parenteral antimicrobial therapy, failure to complete a course of parenteral therapy, relapse or recurrence of infection within 90 days, addition of suppressive oral antimicrobial therapy, readmission or unanticipated surgical intervention within 90 days, and being lost to follow-up. Secondary outcomes were relapse and recurrence within 90 days of treatment, overall 90-day mortality, rate of Clostridium difficile infection within 90 days, adverse drug reactions, and cost of IV antimicrobials. The researchers used logistic regression to assess variables of treatment failure.
Dr. Carr, who is currently an infectious diseases specialty resident at Wake Forest Baptist Health, Winston-Salem, N.C., reported results from 71 patients: 38 who received cefazolin (the cefazolin group) and 33 who received ceftriaxone (the ceftriaxone group). Patients in the cefazolin group were more likely to be on dialysis, compared with those in the ceftriaxone group (24% vs. 0%, respectively; P = .003) and they were more likely to have a prosthesis (53% vs. 24%; P = .015).
The researchers observed no significant differences in the comorbidities between the two groups, but there was more IV drug use in the cefazolin group (13% vs. 0%). The primary source of infection did not differ between the groups, but SSTIs were more likely to be treated with ceftriaxone, compared with cefazolin (33% vs. 8%; P = .086).
Dr. Carr reported that 28.9% of patients in the cefazolin group experienced a treatment failure, compared with 54.5% of those in the ceftriaxone group, a difference that was statistically significant (P = .029). There were no significant differences in the rate of most secondary outcomes between the two groups, with the exception of cost and loss to follow-up. The mean cost of IV therapy per patient was $746.51 in the cefazolin group, compared with $60.30 in the ceftriaxone group, while 5.3% of patients in the cefazolin group were lost to follow-up, compared with 12.1% in the ceftriaxone group.
By setting of outpatient parenteral antibiotic therapy, treatment failure occurred most often in the community skilled nursing facility setting (71%), followed by home settings (41%) and the VA long-term care facility attached to Louis Stokes Cleveland VA Medical Center (17%).
On logistic regression, the only significant predictors of treatment failure among all patients were duration of IV therapy (OR 1.05; P = .015), having heart failure (OR 7.93; P less than .001), as well as being treated in an outside community skilled nursing facility, compared with being treated at the long-term care setting attached to Louis Stokes Cleveland VA Medical Center (P = .008).
Dr. Carr acknowledged certain limitations of the study, including its retrospective design and the fact that it lacked data on antimicrobial susceptibilities and minimum inhibitory concentrations. Other limitations, he said, were that patients were allowed to receive cefazolin prior to ceftriaxone use and that there were low frequencies of secondary outcomes.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
SAN DIEGO – Veteran patients treated with ceftriaxone for methicillin-susceptible Staphylococcus aureus bacteremia were more likely to have treatment failure, compared with those who received cefazolin, a retrospective observational study found.
“To date, no study has specifically evaluated cefazolin versus ceftriaxone for MSSA bacteremia,” Dustin Carr, Pharm.D., said at an annual scientific meeting on infectious diseases. “The main design of this study was to inform our current site and give us additional antimicrobial stewardship opportunities to ensure appropriate selection, dosing, route, and duration.”
In a study conducted during Dr. Carr’s residency training at Louis Stokes Cleveland VA Medical Center, he and his colleagues retrospectively evaluated veteran patients with MSSA bacteremia from January 2009 to August 2014 who received at least 14 days of parenteral cefazolin or ceftriaxone. The use of concomitant anti-staphylococcal agents were excluded, as were patients with polymicrobial infections and those who received empiric antibiotics greater than 72 hours after cultures were finalized. Dr. Carr noted that infectious diseases clinicians are consulted for all cases of MSSA bacteremia at the Louis Stokes Cleveland VA Medical Center, which accounts for about 25% of all outpatient parenteral antimicrobial therapy cases.
Treatment failure was defined as unplanned extension of parenteral antimicrobial therapy, failure to complete a course of parenteral therapy, relapse or recurrence of infection within 90 days, addition of suppressive oral antimicrobial therapy, readmission or unanticipated surgical intervention within 90 days, and being lost to follow-up. Secondary outcomes were relapse and recurrence within 90 days of treatment, overall 90-day mortality, rate of Clostridium difficile infection within 90 days, adverse drug reactions, and cost of IV antimicrobials. The researchers used logistic regression to assess variables of treatment failure.
Dr. Carr, who is currently an infectious diseases specialty resident at Wake Forest Baptist Health, Winston-Salem, N.C., reported results from 71 patients: 38 who received cefazolin (the cefazolin group) and 33 who received ceftriaxone (the ceftriaxone group). Patients in the cefazolin group were more likely to be on dialysis, compared with those in the ceftriaxone group (24% vs. 0%, respectively; P = .003) and they were more likely to have a prosthesis (53% vs. 24%; P = .015).
The researchers observed no significant differences in the comorbidities between the two groups, but there was more IV drug use in the cefazolin group (13% vs. 0%). The primary source of infection did not differ between the groups, but SSTIs were more likely to be treated with ceftriaxone, compared with cefazolin (33% vs. 8%; P = .086).
Dr. Carr reported that 28.9% of patients in the cefazolin group experienced a treatment failure, compared with 54.5% of those in the ceftriaxone group, a difference that was statistically significant (P = .029). There were no significant differences in the rate of most secondary outcomes between the two groups, with the exception of cost and loss to follow-up. The mean cost of IV therapy per patient was $746.51 in the cefazolin group, compared with $60.30 in the ceftriaxone group, while 5.3% of patients in the cefazolin group were lost to follow-up, compared with 12.1% in the ceftriaxone group.
By setting of outpatient parenteral antibiotic therapy, treatment failure occurred most often in the community skilled nursing facility setting (71%), followed by home settings (41%) and the VA long-term care facility attached to Louis Stokes Cleveland VA Medical Center (17%).
On logistic regression, the only significant predictors of treatment failure among all patients were duration of IV therapy (OR 1.05; P = .015), having heart failure (OR 7.93; P less than .001), as well as being treated in an outside community skilled nursing facility, compared with being treated at the long-term care setting attached to Louis Stokes Cleveland VA Medical Center (P = .008).
Dr. Carr acknowledged certain limitations of the study, including its retrospective design and the fact that it lacked data on antimicrobial susceptibilities and minimum inhibitory concentrations. Other limitations, he said, were that patients were allowed to receive cefazolin prior to ceftriaxone use and that there were low frequencies of secondary outcomes.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
AT IDWEEK 2015
Key clinical point: In a veteran population, ceftriaxone had a higher rate of treatment failure than did cefazolin for parenteral treatment of MSSA infection.
Major finding: More than one-fourth of patients in the cefazolin group (28.9%) experienced a treatment failure, compared with 54.5% of those in the ceftriaxone group (P = .029).
Data source: A retrospective, observational analysis of 71patients with MSSA bacteremia who received at least 14 days of parenteral cefazolin or ceftriaxone.
Disclosures: The researchers reported having no financial disclosures.
Antibiotic-resistant bacteria uncommon in nursing homes, but better testing needed
A low incidence of antibiotic-resistant Enterobacteriaceae bacteria was found in a study of Rhode Island nursing home residents admitted to acute care facilities, but researchers said a better understanding of risk factors associated with carriage of carbapenem-resistant gram-negative bacteria among nursing home patients is needed.
Dr. Cheston B. Cunha of the division of infectious diseases at Rhode Island Hospital in Providence and colleagues investigated the prevalence of carbapenem-resistant Enterobacteriaceae (CRE) and carbapenemase-producing Enterobacteriaceae (CPE) in fecal samples of asymptomatic nursing home residents during hospitalization. Their results were published online in the American Journal of Infection Control (2015 Nov 24. doi: 10.1016/j.ajic.2015.09.019)
The researchers conducted a point prevalence survey of 500 hospitalizations of nursing home residents admitted to two Providence, R.I., hospitals. Risk factors associated with CRE carriage were determined by a case-control study. They obtained cultures on 404 patients with 96 readmissions for a total of 500 rectal swabs. The study population consisted of 40% men with a mean age of 80 years.
In total, 23 patients with 30 isolates (4.6%) grew carbapenem resistant or carbapenemase-producing gram-negative bacteria. Of those, seven isolates (1.4%) were CPE or CRE with two isolates (0.4%) that were Citrobacter freundii that contained Klebsiella pneumoniae carbapenemase.
On univariate analysis the researchers found the use of a gastrostomy tube was associated with fecal carriage of CRE (P = .4).
“We found seven CRE-CPE [isolates] among 500 hospital admissions from local nursing homes; however, only two, both C. freundii isolates, contained potentially transmissible carbapenem-resistance genes,” the authors said, noting that the results suggest that in their region, the levels of CPE and CRE carriage are low in nursing home patients.
Furthermore, the investigators suggested that antibiotic resistance is likely promoted by overtreatment with antibiotics, with nursing home residents being at risk for transmission of multidrug-resistant bacteria. “Active infection with CRE and CPE is associated with a high mortality; therefore, efforts to control their spread is of paramount importance,” the authors wrote.
Several limitations of the study were highlighted, including its retrospective design, that it was underpowered to assess risk factors, and that the study population may have been a sicker group of patients because only hospitalized patients were included.
Coauthor Fred C. Tenover, Ph.D., reported employment by Cepheid, and coauthor Ryan Chan reported employment by Cepheid and GeneWeave Biosciences.
A low incidence of antibiotic-resistant Enterobacteriaceae bacteria was found in a study of Rhode Island nursing home residents admitted to acute care facilities, but researchers said a better understanding of risk factors associated with carriage of carbapenem-resistant gram-negative bacteria among nursing home patients is needed.
Dr. Cheston B. Cunha of the division of infectious diseases at Rhode Island Hospital in Providence and colleagues investigated the prevalence of carbapenem-resistant Enterobacteriaceae (CRE) and carbapenemase-producing Enterobacteriaceae (CPE) in fecal samples of asymptomatic nursing home residents during hospitalization. Their results were published online in the American Journal of Infection Control (2015 Nov 24. doi: 10.1016/j.ajic.2015.09.019)
The researchers conducted a point prevalence survey of 500 hospitalizations of nursing home residents admitted to two Providence, R.I., hospitals. Risk factors associated with CRE carriage were determined by a case-control study. They obtained cultures on 404 patients with 96 readmissions for a total of 500 rectal swabs. The study population consisted of 40% men with a mean age of 80 years.
In total, 23 patients with 30 isolates (4.6%) grew carbapenem resistant or carbapenemase-producing gram-negative bacteria. Of those, seven isolates (1.4%) were CPE or CRE with two isolates (0.4%) that were Citrobacter freundii that contained Klebsiella pneumoniae carbapenemase.
On univariate analysis the researchers found the use of a gastrostomy tube was associated with fecal carriage of CRE (P = .4).
“We found seven CRE-CPE [isolates] among 500 hospital admissions from local nursing homes; however, only two, both C. freundii isolates, contained potentially transmissible carbapenem-resistance genes,” the authors said, noting that the results suggest that in their region, the levels of CPE and CRE carriage are low in nursing home patients.
Furthermore, the investigators suggested that antibiotic resistance is likely promoted by overtreatment with antibiotics, with nursing home residents being at risk for transmission of multidrug-resistant bacteria. “Active infection with CRE and CPE is associated with a high mortality; therefore, efforts to control their spread is of paramount importance,” the authors wrote.
Several limitations of the study were highlighted, including its retrospective design, that it was underpowered to assess risk factors, and that the study population may have been a sicker group of patients because only hospitalized patients were included.
Coauthor Fred C. Tenover, Ph.D., reported employment by Cepheid, and coauthor Ryan Chan reported employment by Cepheid and GeneWeave Biosciences.
A low incidence of antibiotic-resistant Enterobacteriaceae bacteria was found in a study of Rhode Island nursing home residents admitted to acute care facilities, but researchers said a better understanding of risk factors associated with carriage of carbapenem-resistant gram-negative bacteria among nursing home patients is needed.
Dr. Cheston B. Cunha of the division of infectious diseases at Rhode Island Hospital in Providence and colleagues investigated the prevalence of carbapenem-resistant Enterobacteriaceae (CRE) and carbapenemase-producing Enterobacteriaceae (CPE) in fecal samples of asymptomatic nursing home residents during hospitalization. Their results were published online in the American Journal of Infection Control (2015 Nov 24. doi: 10.1016/j.ajic.2015.09.019)
The researchers conducted a point prevalence survey of 500 hospitalizations of nursing home residents admitted to two Providence, R.I., hospitals. Risk factors associated with CRE carriage were determined by a case-control study. They obtained cultures on 404 patients with 96 readmissions for a total of 500 rectal swabs. The study population consisted of 40% men with a mean age of 80 years.
In total, 23 patients with 30 isolates (4.6%) grew carbapenem resistant or carbapenemase-producing gram-negative bacteria. Of those, seven isolates (1.4%) were CPE or CRE with two isolates (0.4%) that were Citrobacter freundii that contained Klebsiella pneumoniae carbapenemase.
On univariate analysis the researchers found the use of a gastrostomy tube was associated with fecal carriage of CRE (P = .4).
“We found seven CRE-CPE [isolates] among 500 hospital admissions from local nursing homes; however, only two, both C. freundii isolates, contained potentially transmissible carbapenem-resistance genes,” the authors said, noting that the results suggest that in their region, the levels of CPE and CRE carriage are low in nursing home patients.
Furthermore, the investigators suggested that antibiotic resistance is likely promoted by overtreatment with antibiotics, with nursing home residents being at risk for transmission of multidrug-resistant bacteria. “Active infection with CRE and CPE is associated with a high mortality; therefore, efforts to control their spread is of paramount importance,” the authors wrote.
Several limitations of the study were highlighted, including its retrospective design, that it was underpowered to assess risk factors, and that the study population may have been a sicker group of patients because only hospitalized patients were included.
Coauthor Fred C. Tenover, Ph.D., reported employment by Cepheid, and coauthor Ryan Chan reported employment by Cepheid and GeneWeave Biosciences.
FROM AMERICAN JOURNAL OF INFECTION CONTROL
Key clinical point: A study of antibiotic-resistant Enterobacteriaceae in Rhode Island nursing home residents admitted to acute care facilities found a low incidence of the bacteria.
Major finding: In total, 4.6% of study subjects grew carbapenem-resistant or carbapenemase-producing gram-negative bacteria, and 1.4% of the isolates were CPE or CRE.
Data source: A point prevalence survey of 500 hospitalizations of nursing home residents and a case-control study to assess risk factors associated with CRE.
Disclosures: Coauthor Fred C. Tenover, Ph.D., reported employment by Cepheid and coauthor Ryan Chan reported employment by Cepheid and GeneWeave Biosciences.
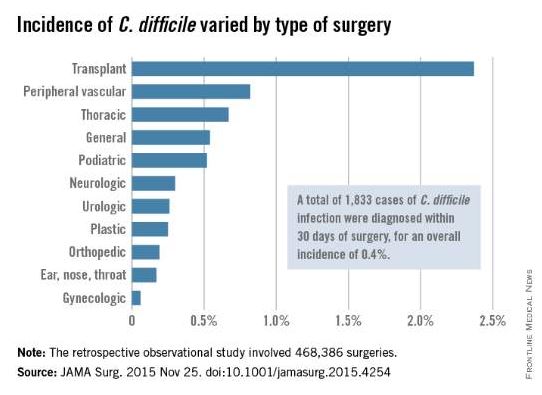
Postop C. diff infection associated with presurgical antibiotics
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
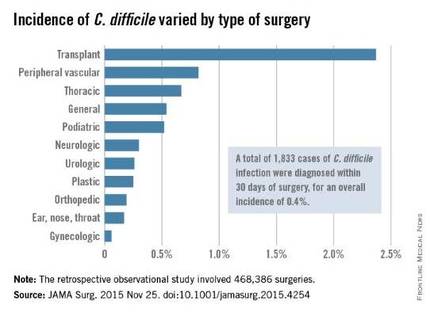
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
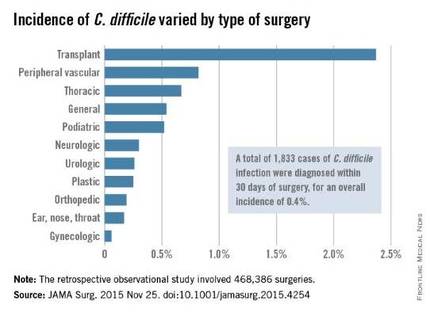
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
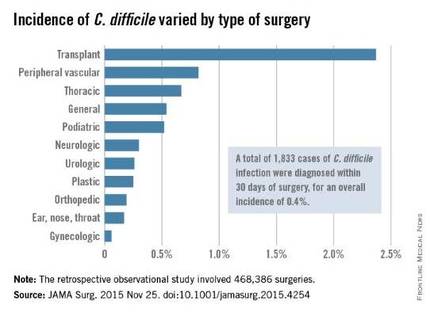
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point: A hospital’s rate of postoperative C. difficile infection is related to the number of preoperative antibiotics patients took and the complexity of their surgeries.
Major finding: Patients who had taken three or more preoperative antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics.
Data source: A retrospective observational study involving 468,386 surgeries at 134 VA medical centers during a 4-year period.
Disclosures: This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
ACR: Don’t be fooled by contaminated synovial fluid
SAN FRANCISCO – Hold off on surgery in patients with presumed septic arthritis if they’re not otherwise too sick and their cultures don’t grow out a pathogenic organism within 48 hours.
The reason is because those patients are likely to have synovial fluid that was contaminated during collection, not a true joint infection.
The advice comes from investigators at Beth Israel Deaconess Medical Center, Boston, who compared 425 monoarticular septic arthritis cases with 25 cases that turned out to be false positives due to synovial fluid contamination; most of the false positives got antibiotics, and three (12%) had joint operations that they did not need.
“Rushing off to the operating room isn’t” always warranted. “You can suspect contamination if patients have milder disease manifestations and cultures grow late,” said investigator Dr. Robert H. Shmerling, clinical chief of Beth Israel’s division of rheumatology.
The findings help determine when – and when not – to be aggressive with patients who present with what looks to be septic arthritis. “No one’s ever really looked at this before,” he said at the annual meeting of the American College of Rheumatology.
“These are very different sorts of patients. Look at the full range of clinical characteristics and lab values, not just the synovial fluid tap. If contamination is suspected, you can wait until the cultures come back or possibly do serial taps before going to the operating room,” said coinvestigator Clara Zhu, a medical student at Boston University.
Patients with true joint infections had higher mean peripheral polymorphonuclear neutrophil percentages (78% vs. 68% in false positives) and synovial fluid polymorphonuclear cell percentages (88% vs. 74% in false positives). True cases also had substantially higher mean synovial fluid white blood cell counts (88,000 vs. 29,000).
Unlike true cases, contaminated synovial fluid took about 4 days to grow out a positive culture, and the most common organisms by far were coagulase-negative staphylococci, typically normal skin bacteria.
Patients with contaminated fluid also tended to be older (71 vs. 59 years), with fewer prior admissions. They were far less likely to have had recent joint procedures and histories of septic arthritis but were more likely to have synovial fluid crystals, as in gout. False positives also left the hospital sooner (7 vs. 11 days) and were less likely to be readmitted within 2 months. They were also less likely to present with fever (19% vs. 37%) but not significantly so.
This “study suggests that contaminated synovial fluid is found in up to 6% of patients with suspected septic arthritis and positive synovial fluid or synovial biopsy cultures. We recommend a conservative approach for patients with ... mild disease manifestations and no growth of pathogenic organisms within the first 48 hours,” the investigators concluded.
The authors have no disclosures, and there was no outside funding for the work.
SAN FRANCISCO – Hold off on surgery in patients with presumed septic arthritis if they’re not otherwise too sick and their cultures don’t grow out a pathogenic organism within 48 hours.
The reason is because those patients are likely to have synovial fluid that was contaminated during collection, not a true joint infection.
The advice comes from investigators at Beth Israel Deaconess Medical Center, Boston, who compared 425 monoarticular septic arthritis cases with 25 cases that turned out to be false positives due to synovial fluid contamination; most of the false positives got antibiotics, and three (12%) had joint operations that they did not need.
“Rushing off to the operating room isn’t” always warranted. “You can suspect contamination if patients have milder disease manifestations and cultures grow late,” said investigator Dr. Robert H. Shmerling, clinical chief of Beth Israel’s division of rheumatology.
The findings help determine when – and when not – to be aggressive with patients who present with what looks to be septic arthritis. “No one’s ever really looked at this before,” he said at the annual meeting of the American College of Rheumatology.
“These are very different sorts of patients. Look at the full range of clinical characteristics and lab values, not just the synovial fluid tap. If contamination is suspected, you can wait until the cultures come back or possibly do serial taps before going to the operating room,” said coinvestigator Clara Zhu, a medical student at Boston University.
Patients with true joint infections had higher mean peripheral polymorphonuclear neutrophil percentages (78% vs. 68% in false positives) and synovial fluid polymorphonuclear cell percentages (88% vs. 74% in false positives). True cases also had substantially higher mean synovial fluid white blood cell counts (88,000 vs. 29,000).
Unlike true cases, contaminated synovial fluid took about 4 days to grow out a positive culture, and the most common organisms by far were coagulase-negative staphylococci, typically normal skin bacteria.
Patients with contaminated fluid also tended to be older (71 vs. 59 years), with fewer prior admissions. They were far less likely to have had recent joint procedures and histories of septic arthritis but were more likely to have synovial fluid crystals, as in gout. False positives also left the hospital sooner (7 vs. 11 days) and were less likely to be readmitted within 2 months. They were also less likely to present with fever (19% vs. 37%) but not significantly so.
This “study suggests that contaminated synovial fluid is found in up to 6% of patients with suspected septic arthritis and positive synovial fluid or synovial biopsy cultures. We recommend a conservative approach for patients with ... mild disease manifestations and no growth of pathogenic organisms within the first 48 hours,” the investigators concluded.
The authors have no disclosures, and there was no outside funding for the work.
SAN FRANCISCO – Hold off on surgery in patients with presumed septic arthritis if they’re not otherwise too sick and their cultures don’t grow out a pathogenic organism within 48 hours.
The reason is because those patients are likely to have synovial fluid that was contaminated during collection, not a true joint infection.
The advice comes from investigators at Beth Israel Deaconess Medical Center, Boston, who compared 425 monoarticular septic arthritis cases with 25 cases that turned out to be false positives due to synovial fluid contamination; most of the false positives got antibiotics, and three (12%) had joint operations that they did not need.
“Rushing off to the operating room isn’t” always warranted. “You can suspect contamination if patients have milder disease manifestations and cultures grow late,” said investigator Dr. Robert H. Shmerling, clinical chief of Beth Israel’s division of rheumatology.
The findings help determine when – and when not – to be aggressive with patients who present with what looks to be septic arthritis. “No one’s ever really looked at this before,” he said at the annual meeting of the American College of Rheumatology.
“These are very different sorts of patients. Look at the full range of clinical characteristics and lab values, not just the synovial fluid tap. If contamination is suspected, you can wait until the cultures come back or possibly do serial taps before going to the operating room,” said coinvestigator Clara Zhu, a medical student at Boston University.
Patients with true joint infections had higher mean peripheral polymorphonuclear neutrophil percentages (78% vs. 68% in false positives) and synovial fluid polymorphonuclear cell percentages (88% vs. 74% in false positives). True cases also had substantially higher mean synovial fluid white blood cell counts (88,000 vs. 29,000).
Unlike true cases, contaminated synovial fluid took about 4 days to grow out a positive culture, and the most common organisms by far were coagulase-negative staphylococci, typically normal skin bacteria.
Patients with contaminated fluid also tended to be older (71 vs. 59 years), with fewer prior admissions. They were far less likely to have had recent joint procedures and histories of septic arthritis but were more likely to have synovial fluid crystals, as in gout. False positives also left the hospital sooner (7 vs. 11 days) and were less likely to be readmitted within 2 months. They were also less likely to present with fever (19% vs. 37%) but not significantly so.
This “study suggests that contaminated synovial fluid is found in up to 6% of patients with suspected septic arthritis and positive synovial fluid or synovial biopsy cultures. We recommend a conservative approach for patients with ... mild disease manifestations and no growth of pathogenic organisms within the first 48 hours,” the investigators concluded.
The authors have no disclosures, and there was no outside funding for the work.
AT THE ACR ANNUAL MEETING
Key clinical point: It’s probably not really septic arthritis if patients have mild disease manifestations and slow-growing synovial fluid cultures.
Major finding: True cases of septic arthritis had substantially higher mean synovial fluid white blood cell counts than did false-positive cases (88,000 vs. 29,000).
Data source: Review of 450 patients with presumed septic arthritis.
Disclosures: The authors have no disclosures, and there was no outside funding for the work.
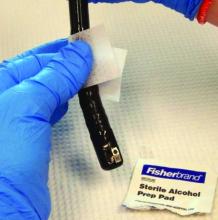
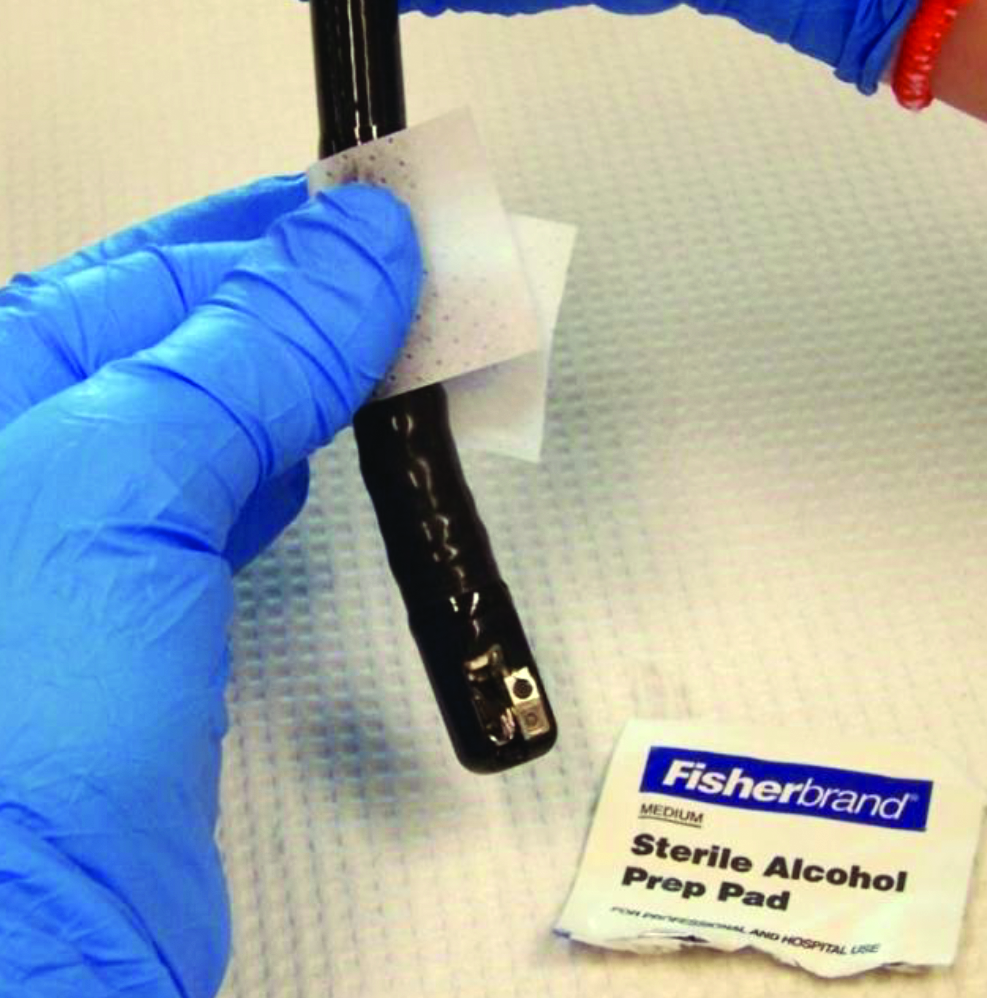
Duodenoscopes often cultured high-concern organisms
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
AT IDWEEK 2015
Key clinical point: High-concern organisms often contaminated duodenoscopes after ERCP.
Major finding: Investigators cultured these bacteria from 92% of duodenoscopes immediately after ERCP, and from 17% of scopes after reprocessing.
Data source: Cultures of 12 duodenoscopes immediately after ERCP and again after reprocessing, and surveillance cultures of 11 stored duodenoscopes.
Disclosures: Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
Impact of health care–associated meningitis or ventriculitis spotlighted
SAN DIEGO – Health care–associated meningitis or ventriculitis continues to occur despite well established preventive methods and is associated with significant morbidity and mortality, a long-term analysis at two hospitals showed.
“Health care–associated meningitis or ventriculitis remains challenging for providers in terms of diagnosis, treatment, and prevention,” Dr. Chanunya Srihawan said at an annual scientific meeting on infectious diseases. “Even though there are a lot of well described methods to minimize the risk of infection, we still see patients with health care–associated meningitis or ventriculitis in the hospital, and most of them have a poor outcome.”
Dr. Srihawan, of the division of infectious diseases in the department of internal medicine at the University of Texas, Houston, and her associates set out to describe the clinical characteristics of patients with health care–associated meningitis or ventriculitis, and to identify risk factors associated with clinical outcomes. They examined data from adult and pediatric patients with a diagnosis of health care–associated meningitis or ventriculitis based on the 2015 Centers for Disease Control and Prevention/National Healthcare Safety Network surveillance definition who were treated at two large tertiary care hospitals in Houston from July 2003 to November 2014.
Patients were prospectively identified by infection control clinicians and by screening of all cerebrospinal fluid samples sent to a central laboratory. The researchers collected patient information on demographics, clinical presentations, laboratory results, imaging studies, treatments, and clinical outcomes. They used Pearson chi-square and Fischer’s exact test for bivariate analysis between baseline variables and outcomes, followed by logistic regression analysis with bootstrap.
Dr. Srihawan reported results from 166 adult and 49 pediatric patients. The median age of patients was 45 years, 45% were white, 26% were Hispanic, 20% were African American, and the remainder were from other ethnic groups. The two most common indications for neurosurgical intervention were hemorrhage (49%) and hydrocephalus (48%), followed by trauma (18%), and brain tumor (11%). The top three neurological signs and symptoms reported were headache (48%), changes in mental status (41%), and nausea/vomiting (39%), followed by focal neurological deficits (33%), neck stiffness (19%), seizures (10%), and photophobia (6%). Nearly three quarters of patients (71%) were admitted to the ICU and 43% received mechanical ventilation for a median of 9 days.
A positive cerebrospinal fluid culture was observed in 106 patients (49%), with the majority of the etiologies being Staphylococcus and Gram-negative rods. An adverse clinical outcome occurred in 167 patients (78%) and was defined as death in 20 patients (9%), persistent vegetative state in 31 patients (14%), severe disability in 77 patients (36%), and moderate disability in 39 patients (18%).
Baseline variables associated with adverse clinical outcomes included age 45 years or older (odds ratio, 11.39), CNS bleeding (OR, 4.37), abnormal neurological exam (OR, 6.51), ICU admission (OR, 5.81), and use of mechanical ventilation (OR, 12.59; P less than .001 for all comparisons). Use of a ventriculoperitoneal shunt was found to be a protective variable (OR, 0.17), which, Dr. Srihawan said, could be explained by the fact most patients who received a ventriculoperitoneal shunt were children who had fewer comorbidities “and tended to be less sick.”
After logistic regression, only three variables remained significantly associated with adverse clinical outcomes: age 45 years or older (OR, 6.47), abnormal neurological exam (OR, 3.04), and use of mechanical ventilation (OR, 5.34).
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
SAN DIEGO – Health care–associated meningitis or ventriculitis continues to occur despite well established preventive methods and is associated with significant morbidity and mortality, a long-term analysis at two hospitals showed.
“Health care–associated meningitis or ventriculitis remains challenging for providers in terms of diagnosis, treatment, and prevention,” Dr. Chanunya Srihawan said at an annual scientific meeting on infectious diseases. “Even though there are a lot of well described methods to minimize the risk of infection, we still see patients with health care–associated meningitis or ventriculitis in the hospital, and most of them have a poor outcome.”
Dr. Srihawan, of the division of infectious diseases in the department of internal medicine at the University of Texas, Houston, and her associates set out to describe the clinical characteristics of patients with health care–associated meningitis or ventriculitis, and to identify risk factors associated with clinical outcomes. They examined data from adult and pediatric patients with a diagnosis of health care–associated meningitis or ventriculitis based on the 2015 Centers for Disease Control and Prevention/National Healthcare Safety Network surveillance definition who were treated at two large tertiary care hospitals in Houston from July 2003 to November 2014.
Patients were prospectively identified by infection control clinicians and by screening of all cerebrospinal fluid samples sent to a central laboratory. The researchers collected patient information on demographics, clinical presentations, laboratory results, imaging studies, treatments, and clinical outcomes. They used Pearson chi-square and Fischer’s exact test for bivariate analysis between baseline variables and outcomes, followed by logistic regression analysis with bootstrap.
Dr. Srihawan reported results from 166 adult and 49 pediatric patients. The median age of patients was 45 years, 45% were white, 26% were Hispanic, 20% were African American, and the remainder were from other ethnic groups. The two most common indications for neurosurgical intervention were hemorrhage (49%) and hydrocephalus (48%), followed by trauma (18%), and brain tumor (11%). The top three neurological signs and symptoms reported were headache (48%), changes in mental status (41%), and nausea/vomiting (39%), followed by focal neurological deficits (33%), neck stiffness (19%), seizures (10%), and photophobia (6%). Nearly three quarters of patients (71%) were admitted to the ICU and 43% received mechanical ventilation for a median of 9 days.
A positive cerebrospinal fluid culture was observed in 106 patients (49%), with the majority of the etiologies being Staphylococcus and Gram-negative rods. An adverse clinical outcome occurred in 167 patients (78%) and was defined as death in 20 patients (9%), persistent vegetative state in 31 patients (14%), severe disability in 77 patients (36%), and moderate disability in 39 patients (18%).
Baseline variables associated with adverse clinical outcomes included age 45 years or older (odds ratio, 11.39), CNS bleeding (OR, 4.37), abnormal neurological exam (OR, 6.51), ICU admission (OR, 5.81), and use of mechanical ventilation (OR, 12.59; P less than .001 for all comparisons). Use of a ventriculoperitoneal shunt was found to be a protective variable (OR, 0.17), which, Dr. Srihawan said, could be explained by the fact most patients who received a ventriculoperitoneal shunt were children who had fewer comorbidities “and tended to be less sick.”
After logistic regression, only three variables remained significantly associated with adverse clinical outcomes: age 45 years or older (OR, 6.47), abnormal neurological exam (OR, 3.04), and use of mechanical ventilation (OR, 5.34).
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
SAN DIEGO – Health care–associated meningitis or ventriculitis continues to occur despite well established preventive methods and is associated with significant morbidity and mortality, a long-term analysis at two hospitals showed.
“Health care–associated meningitis or ventriculitis remains challenging for providers in terms of diagnosis, treatment, and prevention,” Dr. Chanunya Srihawan said at an annual scientific meeting on infectious diseases. “Even though there are a lot of well described methods to minimize the risk of infection, we still see patients with health care–associated meningitis or ventriculitis in the hospital, and most of them have a poor outcome.”
Dr. Srihawan, of the division of infectious diseases in the department of internal medicine at the University of Texas, Houston, and her associates set out to describe the clinical characteristics of patients with health care–associated meningitis or ventriculitis, and to identify risk factors associated with clinical outcomes. They examined data from adult and pediatric patients with a diagnosis of health care–associated meningitis or ventriculitis based on the 2015 Centers for Disease Control and Prevention/National Healthcare Safety Network surveillance definition who were treated at two large tertiary care hospitals in Houston from July 2003 to November 2014.
Patients were prospectively identified by infection control clinicians and by screening of all cerebrospinal fluid samples sent to a central laboratory. The researchers collected patient information on demographics, clinical presentations, laboratory results, imaging studies, treatments, and clinical outcomes. They used Pearson chi-square and Fischer’s exact test for bivariate analysis between baseline variables and outcomes, followed by logistic regression analysis with bootstrap.
Dr. Srihawan reported results from 166 adult and 49 pediatric patients. The median age of patients was 45 years, 45% were white, 26% were Hispanic, 20% were African American, and the remainder were from other ethnic groups. The two most common indications for neurosurgical intervention were hemorrhage (49%) and hydrocephalus (48%), followed by trauma (18%), and brain tumor (11%). The top three neurological signs and symptoms reported were headache (48%), changes in mental status (41%), and nausea/vomiting (39%), followed by focal neurological deficits (33%), neck stiffness (19%), seizures (10%), and photophobia (6%). Nearly three quarters of patients (71%) were admitted to the ICU and 43% received mechanical ventilation for a median of 9 days.
A positive cerebrospinal fluid culture was observed in 106 patients (49%), with the majority of the etiologies being Staphylococcus and Gram-negative rods. An adverse clinical outcome occurred in 167 patients (78%) and was defined as death in 20 patients (9%), persistent vegetative state in 31 patients (14%), severe disability in 77 patients (36%), and moderate disability in 39 patients (18%).
Baseline variables associated with adverse clinical outcomes included age 45 years or older (odds ratio, 11.39), CNS bleeding (OR, 4.37), abnormal neurological exam (OR, 6.51), ICU admission (OR, 5.81), and use of mechanical ventilation (OR, 12.59; P less than .001 for all comparisons). Use of a ventriculoperitoneal shunt was found to be a protective variable (OR, 0.17), which, Dr. Srihawan said, could be explained by the fact most patients who received a ventriculoperitoneal shunt were children who had fewer comorbidities “and tended to be less sick.”
After logistic regression, only three variables remained significantly associated with adverse clinical outcomes: age 45 years or older (OR, 6.47), abnormal neurological exam (OR, 3.04), and use of mechanical ventilation (OR, 5.34).
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported having no financial disclosures.
AT IDWEEK 2015
Key clinical point: The majority of patients treated for health care–associated meningitis or ventriculitis had an adverse outcome.
Major finding: An adverse clinical outcome occurred in 78% of patients treated for health care–associated meningitis or ventriculitis.
Data source: An analysis of 215 adult and pediatric patients with a diagnosis of health care–associated meningitis or ventriculitis who were treated at two large tertiary care hospitals in Houston from July 2003 to November 2014.
Disclosures: The researchers reported having no financial disclosures.
VIDEO: Gut microbiota may predict C. diff treatment response
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HONOLULU – Could gut microbiota be a better predictor than clinical factors of a patient’s response to treatment for Clostridium difficile infection?
In a study of 88 patients with C. difficile, the overall treatment failure rate was 12.5% – but clinical factors such as age, sex, ongoing antibiotic exposure, and hospitalization status failed to predict which patients wouldn’t respond to treatment.
So, “we aimed to identify if there are any gut microbiota signatures to predict treatment response and treatment failure,” explained the study’s lead author, Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn.
In an interview at the annual meeting of the American College of Gastroenterology, Dr. Khanna discussed the study results and why gut microbiota may be an effective predictor of treatment responders and nonresponders.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At ACG 2015