User login
Antibiotic before oral surgery spares endocarditis; study validates guidelines
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
The strongest evidence yet to support clinical guidelines that recommend that people at high risk of endocarditis, such as those who’ve had previous episode the disease or who have a prosthetic cardiac valve, should take antibiotics before they have a tooth pulled or other types of oral surgery, comes from a new study that used two methodologies.
But it also pointed out that two-thirds of the time they aren’t getting that type of antibiotic coverage.
The researchers conducted a cohort study of almost 8 million retirees with employer-paid Medicare supplemental prescription benefits and dental benefits, then conducted a case-crossover study of 3,774 people from the cohort who’d been hospitalized with infectious endocarditis (IE) and who had invasive dental procedures. The bottom line is that the study supports the clinical guidelines from the American Heart Association and the European Society of Cardiology that recommend antibiotic prophylaxis (AP) before dental procedures for patients at high-risk of IE.
Likewise, lead author Martin Thornhill, MBBS, BDS, PhD, said in an interview, the findings also suggest that existing guidelines in the United Kingdom, which recommend against AP in these patients, “should be reconsidered.”
Those AHA and ESC guidelines, however, are “based on no good quality evidence,” said Dr. Thornhill, professor of translational research in dentistry at the University of Sheffield (England) School of Clinical Dentistry. “Other studies have looked at this, but we’ve done the largest study that has shown the clear association between invasive dental procedures and subsequent development of infective endocarditis.”
In the entire cohort of 7.95 million patients, 3,774 had cases of IE that required hospitalization. The study defined highest risk of IE as meeting one of these six criteria: a previous case of IE; a prosthetic cardiac valve or a valve repair that used prosthetic material; cyanotic congenital heart disease; palliative shunts or conduits to treat CHD; or a congenital heart defect that had been fully repaired, either by surgery or a transcatheter procedure, with prosthetic material or device – the latter within 6 months of the procedure.
Moderate IE risk included patients who had rheumatic heart disease, nonrheumatic valve disease or congenital valve anomalies—including mitral valve prolapse or aortic stenosis—or hypertrophic cardiomyopathy.
Risk classification and poor compliance
Highest-risk patients had significantly higher rates of IE a month after a dental procedure than lower-risk groups: 467.6 cases per 1 million procedures vs. 24.2 for moderate risk and 3.8 for low or unknown risk. A subanalysis found that the odds of IE were significantly increased for two specific dental procedures: extractions, with an odds ratio of 9.22 (95% confidence interval [CI], 5.54-15.88; P < .0001); and other oral surgical procedures, with an OR of 20.18 (95% CI, 11.22-37.74; P < .0001).
The study also found that 32.6% of the high-risk patients undergoing dental procedures got AP. “Clearly that shows a low level of compliance with the guidelines in the U.S.,” Dr. Thornhill said. “That’s something that needs to be addressed.”
The study was unique in that it used both a population cohort study and the case-crossover study. “It didn’t matter which of the two methods we used; we essentially came to the same result, which I think adds further weight to the findings,” Dr. Thornhill said.
This may be the best evidence to support the guidelines that clinicians may get. While the observational nature of this study has its limitations, conducting a randomized clinical trial to further validate the findings would be “logistically impossible,” he said, in that it would require an “absolutely enormous” cohort and coordination between medical and dental databases covering thousands of lives. An RCT would also require not using AP for some patients. “It’s not ethical to keep somebody off of antibiotic prophylaxis when there’s such a high risk of death and severe outcomes,” Dr. Thornhill said.
Ann Bolger, MD, emeritus professor of medicine at the University of California, San Francisco, and coauthor of an editorial comment on the study, said in an interview that this study is noteworthy not only for its dual methodology, but for the quality of the data that matched patients at high risk for IE with prescription and dental records. “The fact that they were able to have those details in enough granularity that they knew whether a dental procedure was likely to meet the criteria for these more invasive exposures really broke it open from my perspective,” she said.
She called the low compliance rate with AHA guidelines “one of the most sobering points of this,” and said it should put clinicians on notice that they must do more to educate and engage with high-risk patients. “The lines of communication here are somewhat fraught; it’s a little bit of a hot potato,” she said. “It’s a really great communications opportunity to get the provider’s attention back on this. You’re a cardiologist; you have to have this conversation when you see your patient with a prosthetic valve or who’s had endocarditis every time they come in. There’s a whole litany, and it takes 3 minutes, but you have to do it.”
The study received funding from Delta Dental of Michigan Research Committee and Renaissance Health Service Corp., and Dr. Thornhill received support from Delta Dental Research and Data Institute for the study. Dr. Bolger participated in the 2007 and 2021 AHA statements on AP to prevent IE.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
AHA statement outlines symptoms of common heart diseases
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptoms of six common cardiovascular diseases (CVD) – acute coronary syndromes, heart failure, valvular disorders, stroke, rhythm disorders, and peripheral vascular disease – often overlap and may vary over time and by sex, the American Heart Association noted in a new scientific statement.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions,” Corrine Y. Jurgens, PhD, chair of the writing committee, said in a news release.
This scientific statement is a “compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting,” said Dr. Jurgens, associate professor at Connell School of Nursing, Boston College.
The new statement was published online in Circulation.
The writing group noted that measuring CVD symptoms can be challenging because of their subjective nature. Symptoms may go unrecognized or unreported if people don’t think they are important or are related to an existing health condition.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization,” Dr. Jurgens said.
ACS – chest pain and associated symptoms
The writing group noted that chest pain is the most frequently reported symptom of ACS and has often been described as substernal pressure or discomfort and may radiate to the jaw, shoulder, arm, or upper back.
The most common co-occurring symptoms are dyspnea, diaphoresis, unusual fatigue, nausea, and lightheadedness. Women are more likely than men to report additional symptoms outside of chest pain.
As a result, they have often been labeled “atypical.” However, a recent AHA advisory notes that this label may have been caused by the lack of women included in the clinical trials from which the symptom lists were derived.
The writing group said there is a need to “harmonize” ACS symptom measurement in research. The current lack of harmonization of ACS symptom measurement in research hampers growth in cumulative evidence.
“Therefore, little can be done to synthesize salient findings about symptoms across ischemic heart disease/ACS studies and to incorporate evidence-based information about symptoms into treatment guidelines and patient education materials,” they cautioned.
Heart failure
Turning to heart failure (HF), the writing group noted that dyspnea is the classic symptom and a common reason adults seek medical care.
However, early, more subtle symptoms should be recognized. These include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance; insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
Women with HF report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life, compared with men with HF.
“It is important to account for dyspnea heterogeneity in both clinical practice and research by using nuanced measures and probing questions to capture this common and multifaceted symptom,” the writing group said.
“Monitoring symptoms on a spectrum, versus present or not present, with reliable and valid measures may enhance clinical care by identifying more quickly those who may be at risk for poor outcomes, such as lower quality of life, hospitalization, or death,” Dr. Jurgens added.
“Ultimately, we have work to do in terms of determining who needs more frequent monitoring or intervention to avert poor HF outcomes,” she said.
Valvular heart disease
Valvular heart disease is a frequent cause of HF, with symptoms generally indistinguishable from other HF causes. Rheumatic heart disease is still prevalent in low- and middle-income countries but has largely disappeared in high-income countries, with population aging and cardiomyopathies now key drivers of valve disease.
In the absence of acute severe valve dysfunction, patients generally have a prolonged asymptomatic period, followed by a period of progressive symptoms, resulting from the valve lesion itself or secondary myocardial remodeling and dysfunction, the writing group said.
Symptoms of aortic valve disease often differ between men and women. Aortic stenosis is typically silent for years. As stenosis progresses, women report dyspnea and exercise intolerance more often than men. Women are also more likely to be physically frail and to have a higher New York Heart Association class (III/IV) than men. Men are more likely to have chest pain.
“Given the importance of symptom assessment, more work is needed to determine the incremental value of quantitative symptom measurement as an aid to clinical management,” the writing group said.
Stroke
For clinicians, classic stroke symptoms (face drooping, arm weakness, speech difficulty), in addition to nonclassic symptoms, such as partial sensory deficit, dysarthria, vertigo, and diplopia, should be considered for activating a stroke response team, the group says.
A systematic review and meta-analysis revealed that women with stroke were more likely to present with nonfocal symptoms (for example, headache, altered mentality, and coma/stupor) than men, they noted.
To enhance public education about stroke symptoms and to facilitate the diagnosis and treatment of stroke, they say research is needed to better understand the presentation of stroke symptoms by other select demographic characteristics including race and ethnicity, age, and stroke subtype.
Poststroke screening should include assessment for anxiety, depression, fatigue, and pain, the writing group said.
Rhythm disorders
Turning to rhythm disorders, the writing group wrote that cardiac arrhythmias, including atrial fibrillation (AFib), atrial flutter, supraventricular tachycardia, bradyarrhythmia, and ventricular tachycardia, present with common symptoms.
Palpitations are a characteristic symptom of many cardiac arrhythmias. The most common cardiac arrhythmia, AFib, may present with palpitations or less specific symptoms (fatigue, dyspnea, dizziness) that occur with a broad range of rhythm disorders. Chest pain, dizziness, presyncope/syncope, and anxiety occur less frequently in AFib, the group said.
Palpitations are considered the typical symptom presentation for AFib, yet patients with new-onset AFib often present with nonspecific symptoms or no symptoms, they pointed out.
Women and younger individuals with AFib typically present with palpitations, whereas men are more commonly asymptomatic. Older age also increases the likelihood of a nonclassic or asymptomatic presentation of AFib.
Despite non-Hispanic Black individuals being at lower risk for development of AFib, research suggests that Black patients are burdened more with palpitations, dyspnea on exertion, exercise intolerance, dizziness, dyspnea at rest, and chest discomfort, compared with White or Hispanic patients.
Peripheral vascular disease
Classic claudication occurs in roughly one-third of patients with peripheral arterial disease (PAD) and is defined as calf pain that occurs in one or both legs with exertion (walking), does not begin at rest, and resolves within 10 minutes of standing still or rest.
However, non–calf exercise pain is reported more frequently than classic claudication symptoms. Women with PAD are more likely to have nonclassic symptoms or an absence of symptoms.
Assessing symptoms at rest, during exercise, and during recovery can assist with classifying symptoms as ischemic or not, the writing group said.
PAD with symptoms is associated with an increased risk for myocardial infarction and stroke, with men at higher risk than women.
Similar to PAD, peripheral venous disease (PVD) can be symptomatic or asymptomatic. Clinical classification of PVD includes symptoms such as leg pain, aching, fatigue, heaviness, cramping, tightness, restless legs syndrome, and skin irritation.
“Measuring vascular symptoms includes assessing quality of life and activity limitations, as well as the psychological impact of the disease. However, existing measures are often based on the clinician’s appraisal rather than the individual’s self-reported symptoms and severity of symptoms,” Dr. Jurgens commented.
Watch for depression
Finally, the writing group highlighted the importance of depression in cardiac patients, which occurs at about twice the rate, compared with people without any medical condition (10% vs. 5%).
In a prior statement, the AHA said depression should be considered a risk factor for worse outcomes in patients with ACS or CVD diagnosis.
The new statement highlights that people with persistent chest pain, people with HF, as well as stroke survivors and people with PAD commonly have depression and/or anxiety. In addition, cognitive changes after a stroke may affect how and whether symptoms are experienced or noticed.
While symptom relief is an important part of managing CVD, it’s also important to recognize that “factors such as depression and cognitive function may affect symptom detection and reporting,” Dr. Jurgens said.
“Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk,” she added.
The scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Cardiovascular and Stroke Nursing; the Council on Hypertension; and the Stroke Council. The research had no commercial funding. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Early LV recovery after TAVR tied to 5-year mortality
Early improvement of left ventricular ejection fraction (LVEF) after transcatheter aortic valve replacement (TAVR) is associated with improved all-cause and cardiac death at 5 years in patients with severe aortic stenosis and LVEF less than 50%, new research shows.
Further analyses revealed a significant interaction by sex, with the mortality benefit largely in women.
“It’s absolutely fascinating,” senior author Sammy Elmariah, MD, Massachusetts General Hospital, Boston, said of the finding. “We know that women are more likely to have concentric hypertrophy, that they have lesser degrees of fibrosis, and smaller ventricles, and, of course, they’re in general less affected by coronary artery disease and MIs [myocardial infarctions]. All of those things in my mind, at least that’s what I assumed ahead of time, would make it more likely for women’s hearts to recover.”
“But that’s actually not what we found,” he continued. “We didn’t see a difference between the sexes in terms of likelihood of recovery. But what we saw is that the survival benefit, that associates with improvement in EF, was almost completely driven by women. So women really seem to be reaping that benefit in a manner that is unique and very different from what we saw in men.”
Dr. Elmariah noted that the reason for this benefit is unclear but points to the differences in biology for LV remodeling. “Clearly there are several details there that warrant further attention and more research.”
Suzanne J. Baron, MD, director of interventional cardiology research at Lahey Hospital and Medical Center, Burlington, Mass., said in an email that the finding of a substantial long-term survival benefit was “a bit surprising.”
Several studies have suggested that women may derive a greater benefit from TAVR versus surgical aortic valve replacement, and meta-analyses have demonstrated short and intermediate-term survival after TAVR is better in women, compared with in men, she pointed out. However, the mediating mechanism for this finding has never been clearly elucidated.
“Certainly, the sex differences in LVEF improvement after TAVR observed in this study, which could be related to sex differences in LV remodeling and LV mass regression, may now give us a clue as to why these sex-specific survival differences after TAVR persist,” Dr. Baron said.
More data amassed
Previous research in smaller cohorts with follow-up out to 1 year have shown an association between early LVEF improvement after TAVR and better survival. This includes a 2013 study by the investigators in high-risk patients in PARTNER-1 and a separate 2016 study in patients in the CoreValve extreme and high surgical risk trials.
Now, with longer follow-up amassed, the investigators examined data from 659 high- or intermediate-risk patients with severe stenosis and LVEF less than 50% who underwent transfemoral TAVR in the PARTNER 1, 2, and S3 trials and registries between July 2007 and April 2015.
Their mean age was 82.4 years, 71% were men, and 89.7% were White individuals. During the study period, 55.6% of the cohort died.
As reported in JAMA Cardiology, 32.8% of patients had early LVEF improvement, defined as an increase of at least 10% percentage points at 30 days after TAVR (mean change, 16.4%).
This compares with about 50%-60% of patients in the earlier studies, likely owing to the relatively higher baseline LVEF, especially in the intermediate-risk cohort, the authors suggested.
Independent predictors of lower likelihood of early LVEF improvement were previous MI, diabetes, cancer, higher baseline LVEF, larger LV end-diastolic diameter, and larger aortic valve area (AVA), whereas higher body mass index and higher stroke volume index predicted greater likelihood of LV recovery.
At 5 years, patients with versus without improved early LV improvement had lower risks of all-cause death (50.0% vs. 58.4%; P = .04) and cardiac death (29.5% vs. 38.1%; P = .05).
In multivariable analyses, each 5%-point increase in LVEF after TAVR was associated with a 6% lower risk of all-cause death (hazard ratio [HR], 0.94; P = .04) and 10% lower risk of cardiac death (HR, 0.90; P = .02).
Restricted cubic spline analysis demonstrated an inflection point above a 10% change in LVEF beyond which there was a steep decline in all-cause mortality with increasing degree of LVEF improvement.
There were no significant differences in rehospitalization, New York Heart Association functional class, or Kansas City Cardiomyopathy Questionnaire score at 5 years in patients with and without early LVEF improvement.
“I think what this really gets to is what is the reason behind the LV dysfunction in the first place,” said Dr. Elmariah, soon to be joining the University of California, San Francisco. “We know that TAVR cures aortic stenosis, so if the LV dysfunction is primarily related to the valve itself, hopefully those patients are going to recover.”
On the other hand, if the patient has LV dysfunction because of a prior myocardial infarction or cardiomyopathy and then developed aortic stenosis, “you can treat the aortic stenosis but the heart is still diseased from whatever process was affecting it previously and so it’s not likely to recover in those scenarios,” he added.
The results can be used for counseling patients and highlight the need to optimize goal-directed medical therapy in those with valvular heart disease, Dr. Elmariah suggested.
“Often, patients with aortic stenosis are on miniscule doses of many of the heart failure agents because people are worried about the hemodynamic consequences and they’re worried that patients won’t tolerate these medications,” he said. “But it’s very important for us to aggressively try to treat the heart failure that is affecting these patients in order to hopefully increase the chances that their left ventricles will recover and, hopefully, that they will have improved survival.”
Dr. Baron said that “this study clearly demonstrates that patients with reduced LVEF and severe aortic stenosis can benefit from TAVR and that early improvement in LVEF is an important prognostic marker for this population.”
In Dr. Baron and colleagues’ earlier analysis of 11,000 patients who underwent TAVR as part of the transcatheter valve therapy registry, only low aortic valve gradient but not LV dysfunction was associated with higher adjusted 1-year mortality. Asked about the finding, she noted that patients were evaluated based on LV function at baseline and not for a difference in outcomes based on LVEF improvement after TAVR.
“As such, I think that these two studies are actually complementary,” Dr. Baron said. “Together, they suggest that a low LVEF should not preclude a patient from receiving TAVR and if the patient does experience a 10% increase in LVEF after TAVR, then their 5-year prognosis is improved.”
Dr. Elmariah reports grants from the American Heart Association, National Institutes of Health, Edwards Lifesciences, Medtronic, and Svelte Medical and has received consulting fees from Medtronic and AstraZeneca. Coauthor disclosures are listed in the paper. The PARTNER trials and registries and this analysis were supported by Edwards Lifesciences. Edwards was involved in the design and conduct of the study including collection, management, analysis, and interpretation of the data. Dr. Baron reports receiving research grant funding from Abiomed and Boston Scientific; consulting/medical advisory board fees from Boston Scientific, Shockwave and Biotronik; and speaking honoraria from Medtronic and Zoll.
A version of this article first appeared on Medscape.com.
Early improvement of left ventricular ejection fraction (LVEF) after transcatheter aortic valve replacement (TAVR) is associated with improved all-cause and cardiac death at 5 years in patients with severe aortic stenosis and LVEF less than 50%, new research shows.
Further analyses revealed a significant interaction by sex, with the mortality benefit largely in women.
“It’s absolutely fascinating,” senior author Sammy Elmariah, MD, Massachusetts General Hospital, Boston, said of the finding. “We know that women are more likely to have concentric hypertrophy, that they have lesser degrees of fibrosis, and smaller ventricles, and, of course, they’re in general less affected by coronary artery disease and MIs [myocardial infarctions]. All of those things in my mind, at least that’s what I assumed ahead of time, would make it more likely for women’s hearts to recover.”
“But that’s actually not what we found,” he continued. “We didn’t see a difference between the sexes in terms of likelihood of recovery. But what we saw is that the survival benefit, that associates with improvement in EF, was almost completely driven by women. So women really seem to be reaping that benefit in a manner that is unique and very different from what we saw in men.”
Dr. Elmariah noted that the reason for this benefit is unclear but points to the differences in biology for LV remodeling. “Clearly there are several details there that warrant further attention and more research.”
Suzanne J. Baron, MD, director of interventional cardiology research at Lahey Hospital and Medical Center, Burlington, Mass., said in an email that the finding of a substantial long-term survival benefit was “a bit surprising.”
Several studies have suggested that women may derive a greater benefit from TAVR versus surgical aortic valve replacement, and meta-analyses have demonstrated short and intermediate-term survival after TAVR is better in women, compared with in men, she pointed out. However, the mediating mechanism for this finding has never been clearly elucidated.
“Certainly, the sex differences in LVEF improvement after TAVR observed in this study, which could be related to sex differences in LV remodeling and LV mass regression, may now give us a clue as to why these sex-specific survival differences after TAVR persist,” Dr. Baron said.
More data amassed
Previous research in smaller cohorts with follow-up out to 1 year have shown an association between early LVEF improvement after TAVR and better survival. This includes a 2013 study by the investigators in high-risk patients in PARTNER-1 and a separate 2016 study in patients in the CoreValve extreme and high surgical risk trials.
Now, with longer follow-up amassed, the investigators examined data from 659 high- or intermediate-risk patients with severe stenosis and LVEF less than 50% who underwent transfemoral TAVR in the PARTNER 1, 2, and S3 trials and registries between July 2007 and April 2015.
Their mean age was 82.4 years, 71% were men, and 89.7% were White individuals. During the study period, 55.6% of the cohort died.
As reported in JAMA Cardiology, 32.8% of patients had early LVEF improvement, defined as an increase of at least 10% percentage points at 30 days after TAVR (mean change, 16.4%).
This compares with about 50%-60% of patients in the earlier studies, likely owing to the relatively higher baseline LVEF, especially in the intermediate-risk cohort, the authors suggested.
Independent predictors of lower likelihood of early LVEF improvement were previous MI, diabetes, cancer, higher baseline LVEF, larger LV end-diastolic diameter, and larger aortic valve area (AVA), whereas higher body mass index and higher stroke volume index predicted greater likelihood of LV recovery.
At 5 years, patients with versus without improved early LV improvement had lower risks of all-cause death (50.0% vs. 58.4%; P = .04) and cardiac death (29.5% vs. 38.1%; P = .05).
In multivariable analyses, each 5%-point increase in LVEF after TAVR was associated with a 6% lower risk of all-cause death (hazard ratio [HR], 0.94; P = .04) and 10% lower risk of cardiac death (HR, 0.90; P = .02).
Restricted cubic spline analysis demonstrated an inflection point above a 10% change in LVEF beyond which there was a steep decline in all-cause mortality with increasing degree of LVEF improvement.
There were no significant differences in rehospitalization, New York Heart Association functional class, or Kansas City Cardiomyopathy Questionnaire score at 5 years in patients with and without early LVEF improvement.
“I think what this really gets to is what is the reason behind the LV dysfunction in the first place,” said Dr. Elmariah, soon to be joining the University of California, San Francisco. “We know that TAVR cures aortic stenosis, so if the LV dysfunction is primarily related to the valve itself, hopefully those patients are going to recover.”
On the other hand, if the patient has LV dysfunction because of a prior myocardial infarction or cardiomyopathy and then developed aortic stenosis, “you can treat the aortic stenosis but the heart is still diseased from whatever process was affecting it previously and so it’s not likely to recover in those scenarios,” he added.
The results can be used for counseling patients and highlight the need to optimize goal-directed medical therapy in those with valvular heart disease, Dr. Elmariah suggested.
“Often, patients with aortic stenosis are on miniscule doses of many of the heart failure agents because people are worried about the hemodynamic consequences and they’re worried that patients won’t tolerate these medications,” he said. “But it’s very important for us to aggressively try to treat the heart failure that is affecting these patients in order to hopefully increase the chances that their left ventricles will recover and, hopefully, that they will have improved survival.”
Dr. Baron said that “this study clearly demonstrates that patients with reduced LVEF and severe aortic stenosis can benefit from TAVR and that early improvement in LVEF is an important prognostic marker for this population.”
In Dr. Baron and colleagues’ earlier analysis of 11,000 patients who underwent TAVR as part of the transcatheter valve therapy registry, only low aortic valve gradient but not LV dysfunction was associated with higher adjusted 1-year mortality. Asked about the finding, she noted that patients were evaluated based on LV function at baseline and not for a difference in outcomes based on LVEF improvement after TAVR.
“As such, I think that these two studies are actually complementary,” Dr. Baron said. “Together, they suggest that a low LVEF should not preclude a patient from receiving TAVR and if the patient does experience a 10% increase in LVEF after TAVR, then their 5-year prognosis is improved.”
Dr. Elmariah reports grants from the American Heart Association, National Institutes of Health, Edwards Lifesciences, Medtronic, and Svelte Medical and has received consulting fees from Medtronic and AstraZeneca. Coauthor disclosures are listed in the paper. The PARTNER trials and registries and this analysis were supported by Edwards Lifesciences. Edwards was involved in the design and conduct of the study including collection, management, analysis, and interpretation of the data. Dr. Baron reports receiving research grant funding from Abiomed and Boston Scientific; consulting/medical advisory board fees from Boston Scientific, Shockwave and Biotronik; and speaking honoraria from Medtronic and Zoll.
A version of this article first appeared on Medscape.com.
Early improvement of left ventricular ejection fraction (LVEF) after transcatheter aortic valve replacement (TAVR) is associated with improved all-cause and cardiac death at 5 years in patients with severe aortic stenosis and LVEF less than 50%, new research shows.
Further analyses revealed a significant interaction by sex, with the mortality benefit largely in women.
“It’s absolutely fascinating,” senior author Sammy Elmariah, MD, Massachusetts General Hospital, Boston, said of the finding. “We know that women are more likely to have concentric hypertrophy, that they have lesser degrees of fibrosis, and smaller ventricles, and, of course, they’re in general less affected by coronary artery disease and MIs [myocardial infarctions]. All of those things in my mind, at least that’s what I assumed ahead of time, would make it more likely for women’s hearts to recover.”
“But that’s actually not what we found,” he continued. “We didn’t see a difference between the sexes in terms of likelihood of recovery. But what we saw is that the survival benefit, that associates with improvement in EF, was almost completely driven by women. So women really seem to be reaping that benefit in a manner that is unique and very different from what we saw in men.”
Dr. Elmariah noted that the reason for this benefit is unclear but points to the differences in biology for LV remodeling. “Clearly there are several details there that warrant further attention and more research.”
Suzanne J. Baron, MD, director of interventional cardiology research at Lahey Hospital and Medical Center, Burlington, Mass., said in an email that the finding of a substantial long-term survival benefit was “a bit surprising.”
Several studies have suggested that women may derive a greater benefit from TAVR versus surgical aortic valve replacement, and meta-analyses have demonstrated short and intermediate-term survival after TAVR is better in women, compared with in men, she pointed out. However, the mediating mechanism for this finding has never been clearly elucidated.
“Certainly, the sex differences in LVEF improvement after TAVR observed in this study, which could be related to sex differences in LV remodeling and LV mass regression, may now give us a clue as to why these sex-specific survival differences after TAVR persist,” Dr. Baron said.
More data amassed
Previous research in smaller cohorts with follow-up out to 1 year have shown an association between early LVEF improvement after TAVR and better survival. This includes a 2013 study by the investigators in high-risk patients in PARTNER-1 and a separate 2016 study in patients in the CoreValve extreme and high surgical risk trials.
Now, with longer follow-up amassed, the investigators examined data from 659 high- or intermediate-risk patients with severe stenosis and LVEF less than 50% who underwent transfemoral TAVR in the PARTNER 1, 2, and S3 trials and registries between July 2007 and April 2015.
Their mean age was 82.4 years, 71% were men, and 89.7% were White individuals. During the study period, 55.6% of the cohort died.
As reported in JAMA Cardiology, 32.8% of patients had early LVEF improvement, defined as an increase of at least 10% percentage points at 30 days after TAVR (mean change, 16.4%).
This compares with about 50%-60% of patients in the earlier studies, likely owing to the relatively higher baseline LVEF, especially in the intermediate-risk cohort, the authors suggested.
Independent predictors of lower likelihood of early LVEF improvement were previous MI, diabetes, cancer, higher baseline LVEF, larger LV end-diastolic diameter, and larger aortic valve area (AVA), whereas higher body mass index and higher stroke volume index predicted greater likelihood of LV recovery.
At 5 years, patients with versus without improved early LV improvement had lower risks of all-cause death (50.0% vs. 58.4%; P = .04) and cardiac death (29.5% vs. 38.1%; P = .05).
In multivariable analyses, each 5%-point increase in LVEF after TAVR was associated with a 6% lower risk of all-cause death (hazard ratio [HR], 0.94; P = .04) and 10% lower risk of cardiac death (HR, 0.90; P = .02).
Restricted cubic spline analysis demonstrated an inflection point above a 10% change in LVEF beyond which there was a steep decline in all-cause mortality with increasing degree of LVEF improvement.
There were no significant differences in rehospitalization, New York Heart Association functional class, or Kansas City Cardiomyopathy Questionnaire score at 5 years in patients with and without early LVEF improvement.
“I think what this really gets to is what is the reason behind the LV dysfunction in the first place,” said Dr. Elmariah, soon to be joining the University of California, San Francisco. “We know that TAVR cures aortic stenosis, so if the LV dysfunction is primarily related to the valve itself, hopefully those patients are going to recover.”
On the other hand, if the patient has LV dysfunction because of a prior myocardial infarction or cardiomyopathy and then developed aortic stenosis, “you can treat the aortic stenosis but the heart is still diseased from whatever process was affecting it previously and so it’s not likely to recover in those scenarios,” he added.
The results can be used for counseling patients and highlight the need to optimize goal-directed medical therapy in those with valvular heart disease, Dr. Elmariah suggested.
“Often, patients with aortic stenosis are on miniscule doses of many of the heart failure agents because people are worried about the hemodynamic consequences and they’re worried that patients won’t tolerate these medications,” he said. “But it’s very important for us to aggressively try to treat the heart failure that is affecting these patients in order to hopefully increase the chances that their left ventricles will recover and, hopefully, that they will have improved survival.”
Dr. Baron said that “this study clearly demonstrates that patients with reduced LVEF and severe aortic stenosis can benefit from TAVR and that early improvement in LVEF is an important prognostic marker for this population.”
In Dr. Baron and colleagues’ earlier analysis of 11,000 patients who underwent TAVR as part of the transcatheter valve therapy registry, only low aortic valve gradient but not LV dysfunction was associated with higher adjusted 1-year mortality. Asked about the finding, she noted that patients were evaluated based on LV function at baseline and not for a difference in outcomes based on LVEF improvement after TAVR.
“As such, I think that these two studies are actually complementary,” Dr. Baron said. “Together, they suggest that a low LVEF should not preclude a patient from receiving TAVR and if the patient does experience a 10% increase in LVEF after TAVR, then their 5-year prognosis is improved.”
Dr. Elmariah reports grants from the American Heart Association, National Institutes of Health, Edwards Lifesciences, Medtronic, and Svelte Medical and has received consulting fees from Medtronic and AstraZeneca. Coauthor disclosures are listed in the paper. The PARTNER trials and registries and this analysis were supported by Edwards Lifesciences. Edwards was involved in the design and conduct of the study including collection, management, analysis, and interpretation of the data. Dr. Baron reports receiving research grant funding from Abiomed and Boston Scientific; consulting/medical advisory board fees from Boston Scientific, Shockwave and Biotronik; and speaking honoraria from Medtronic and Zoll.
A version of this article first appeared on Medscape.com.
More evidence salt substitutes lower risk of CVD and death
Dietary salt substitutes not only lower blood pressure but also have a clear impact on hard clinical endpoints, lowering the risk of myocardial infarction (MI), stroke, and death from all causes and cardiovascular disease (CVD), a meta-analysis shows.
The blood pressure–mediated protective effects of salt substitutes on CVD and death are likely to apply to the roughly 1.28 billion people around the world who have high blood pressure, the researchers say.
“These findings are unlikely to reflect the play of chance and support the adoption of salt substitutes in clinical practice and public health policy as a strategy to reduce dietary sodium intake, increase dietary potassium intake, lower blood pressure, and prevent major cardiovascular events,” they write.
The study was published online in Heart.
Strong support for landmark study
In salt substitutes, a proportion of sodium chloride is replaced with potassium chloride. They are known to help lower blood pressure, but less is known about their impact on hard clinical endpoints, Maoyi Tian, PhD, with Harbin Medical University, China, and the George Institute for Global Health, Sydney, and colleagues note in their article.
In the landmark Salt Substitute and Stroke Study (SSaSS), salt substitutes cut the risk of MI, stroke, and early death, as reported previously by this news organization.
But SSaSS was conducted in China, and it was unclear whether these benefits would apply to people in other parts of the world.
To investigate, Dr. Tian and colleagues pooled data from 21 relevant parallel-group, step-wedge, or cluster randomized controlled trials published through August 2021, with 31,949 participants. The trials were conducted in Europe, the Western Pacific Region, the Americas, and South East Asia and reported the effect of a salt substitute on blood pressure or clinical outcomes.
A meta-analysis of blood pressure data from 19 trials that included 29,528 participants showed that salt substitutes lowered systolic blood pressure (SBP) by 4.61 mm Hg (95% confidence interval, −6.07 to −3.14) and diastolic blood pressure (DBP) by 1.61 mm Hg (95% CI, −2.42 to −0.79).
The proportion of sodium chloride in the salt substitutes varied from 33% to 75%; the proportion of potassium ranged from 25% to 65%.
Each 10% lower proportion of sodium chloride in the salt substitute was associated with a 1.53 mm Hg (95% CI, −3.02 to −0.03; P = .045) greater reduction in SBP and a 0.95 mm Hg (95% CI, −1.78 to −0.12; P = .025) greater reduction in DBP.
Reductions in blood pressure appeared consistent, irrespective of country, age, sex, history of high blood pressure, weight, baseline blood pressure, and baseline levels of urinary sodium and potassium.
Clear benefit on hard outcomes
Pooled data on clinical outcomes from five trials that included 24,306 participants, mostly from the SSaSS, showed clear protective effects of salt substitutes on total mortality (risk ratio, 0.89; 95% CI, 0.85-0.94), CV mortality (RR, 0.87; 95% CI, 0.81-0.94), and CV events (RR, 0.89; 95% CI, 0.85-0.94).
Dr. Tian and colleagues say that “broader population use of salt substitute is supported by the absence of any detectable adverse effect of salt substitutes on hyperkalemia in this review.”
They note, however, that all of the trials took “pragmatic steps to exclude participants at elevated risk of hyperkalemia, seeking to exclude those with chronic kidney disease or using medications that elevate serum potassium.”
Offering perspective on the study, Harlan Krumholz, MD, with Yale New Haven Hospital and Yale School of Medicine, both in New Haven, Conn., said it provides “useful information by bringing together the trial evidence on salt substitutes. The evidence is dominated by the SSaSS, but the others add context.”
Dr. Krumholz said that at this point, he thinks salt substitutes “could be included in recommendations to patients.”
“SSaSS was conducted in villages in China, so that is where the evidence is strongest and most relevant, but this is a low-cost and seemingly safe strategy that could be tried by anyone without contraindications, such as kidney disease or taking a potassium-sparing medication or potassium supplement,” Dr. Krumholz told this news organization.
Johanna Contreras, MD, heart failure and transplant cardiologist at the Mount Sinai Hospital, New York, agrees that in the absence of contraindications, salt substitutes should be recommended.
“Americans put salt on everything and don’t even think about it. The salt substitutes are very helpful,” Dr. Contreras said in an interview.
“People who don’t have high blood pressure should limit salt intake, because what we have seen is that if you have high blood pressure in your family – even if you don’t have high blood pressure in your 20s or 30s – you’re likely to develop high blood pressure,” Dr. Contreras said.
“Therefore, it’s wise early on to start protecting yourself and using low salt and salt substitutes,” she added.
The study had no specific funding. Dr. Tian, Dr. Krumholz, and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dietary salt substitutes not only lower blood pressure but also have a clear impact on hard clinical endpoints, lowering the risk of myocardial infarction (MI), stroke, and death from all causes and cardiovascular disease (CVD), a meta-analysis shows.
The blood pressure–mediated protective effects of salt substitutes on CVD and death are likely to apply to the roughly 1.28 billion people around the world who have high blood pressure, the researchers say.
“These findings are unlikely to reflect the play of chance and support the adoption of salt substitutes in clinical practice and public health policy as a strategy to reduce dietary sodium intake, increase dietary potassium intake, lower blood pressure, and prevent major cardiovascular events,” they write.
The study was published online in Heart.
Strong support for landmark study
In salt substitutes, a proportion of sodium chloride is replaced with potassium chloride. They are known to help lower blood pressure, but less is known about their impact on hard clinical endpoints, Maoyi Tian, PhD, with Harbin Medical University, China, and the George Institute for Global Health, Sydney, and colleagues note in their article.
In the landmark Salt Substitute and Stroke Study (SSaSS), salt substitutes cut the risk of MI, stroke, and early death, as reported previously by this news organization.
But SSaSS was conducted in China, and it was unclear whether these benefits would apply to people in other parts of the world.
To investigate, Dr. Tian and colleagues pooled data from 21 relevant parallel-group, step-wedge, or cluster randomized controlled trials published through August 2021, with 31,949 participants. The trials were conducted in Europe, the Western Pacific Region, the Americas, and South East Asia and reported the effect of a salt substitute on blood pressure or clinical outcomes.
A meta-analysis of blood pressure data from 19 trials that included 29,528 participants showed that salt substitutes lowered systolic blood pressure (SBP) by 4.61 mm Hg (95% confidence interval, −6.07 to −3.14) and diastolic blood pressure (DBP) by 1.61 mm Hg (95% CI, −2.42 to −0.79).
The proportion of sodium chloride in the salt substitutes varied from 33% to 75%; the proportion of potassium ranged from 25% to 65%.
Each 10% lower proportion of sodium chloride in the salt substitute was associated with a 1.53 mm Hg (95% CI, −3.02 to −0.03; P = .045) greater reduction in SBP and a 0.95 mm Hg (95% CI, −1.78 to −0.12; P = .025) greater reduction in DBP.
Reductions in blood pressure appeared consistent, irrespective of country, age, sex, history of high blood pressure, weight, baseline blood pressure, and baseline levels of urinary sodium and potassium.
Clear benefit on hard outcomes
Pooled data on clinical outcomes from five trials that included 24,306 participants, mostly from the SSaSS, showed clear protective effects of salt substitutes on total mortality (risk ratio, 0.89; 95% CI, 0.85-0.94), CV mortality (RR, 0.87; 95% CI, 0.81-0.94), and CV events (RR, 0.89; 95% CI, 0.85-0.94).
Dr. Tian and colleagues say that “broader population use of salt substitute is supported by the absence of any detectable adverse effect of salt substitutes on hyperkalemia in this review.”
They note, however, that all of the trials took “pragmatic steps to exclude participants at elevated risk of hyperkalemia, seeking to exclude those with chronic kidney disease or using medications that elevate serum potassium.”
Offering perspective on the study, Harlan Krumholz, MD, with Yale New Haven Hospital and Yale School of Medicine, both in New Haven, Conn., said it provides “useful information by bringing together the trial evidence on salt substitutes. The evidence is dominated by the SSaSS, but the others add context.”
Dr. Krumholz said that at this point, he thinks salt substitutes “could be included in recommendations to patients.”
“SSaSS was conducted in villages in China, so that is where the evidence is strongest and most relevant, but this is a low-cost and seemingly safe strategy that could be tried by anyone without contraindications, such as kidney disease or taking a potassium-sparing medication or potassium supplement,” Dr. Krumholz told this news organization.
Johanna Contreras, MD, heart failure and transplant cardiologist at the Mount Sinai Hospital, New York, agrees that in the absence of contraindications, salt substitutes should be recommended.
“Americans put salt on everything and don’t even think about it. The salt substitutes are very helpful,” Dr. Contreras said in an interview.
“People who don’t have high blood pressure should limit salt intake, because what we have seen is that if you have high blood pressure in your family – even if you don’t have high blood pressure in your 20s or 30s – you’re likely to develop high blood pressure,” Dr. Contreras said.
“Therefore, it’s wise early on to start protecting yourself and using low salt and salt substitutes,” she added.
The study had no specific funding. Dr. Tian, Dr. Krumholz, and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dietary salt substitutes not only lower blood pressure but also have a clear impact on hard clinical endpoints, lowering the risk of myocardial infarction (MI), stroke, and death from all causes and cardiovascular disease (CVD), a meta-analysis shows.
The blood pressure–mediated protective effects of salt substitutes on CVD and death are likely to apply to the roughly 1.28 billion people around the world who have high blood pressure, the researchers say.
“These findings are unlikely to reflect the play of chance and support the adoption of salt substitutes in clinical practice and public health policy as a strategy to reduce dietary sodium intake, increase dietary potassium intake, lower blood pressure, and prevent major cardiovascular events,” they write.
The study was published online in Heart.
Strong support for landmark study
In salt substitutes, a proportion of sodium chloride is replaced with potassium chloride. They are known to help lower blood pressure, but less is known about their impact on hard clinical endpoints, Maoyi Tian, PhD, with Harbin Medical University, China, and the George Institute for Global Health, Sydney, and colleagues note in their article.
In the landmark Salt Substitute and Stroke Study (SSaSS), salt substitutes cut the risk of MI, stroke, and early death, as reported previously by this news organization.
But SSaSS was conducted in China, and it was unclear whether these benefits would apply to people in other parts of the world.
To investigate, Dr. Tian and colleagues pooled data from 21 relevant parallel-group, step-wedge, or cluster randomized controlled trials published through August 2021, with 31,949 participants. The trials were conducted in Europe, the Western Pacific Region, the Americas, and South East Asia and reported the effect of a salt substitute on blood pressure or clinical outcomes.
A meta-analysis of blood pressure data from 19 trials that included 29,528 participants showed that salt substitutes lowered systolic blood pressure (SBP) by 4.61 mm Hg (95% confidence interval, −6.07 to −3.14) and diastolic blood pressure (DBP) by 1.61 mm Hg (95% CI, −2.42 to −0.79).
The proportion of sodium chloride in the salt substitutes varied from 33% to 75%; the proportion of potassium ranged from 25% to 65%.
Each 10% lower proportion of sodium chloride in the salt substitute was associated with a 1.53 mm Hg (95% CI, −3.02 to −0.03; P = .045) greater reduction in SBP and a 0.95 mm Hg (95% CI, −1.78 to −0.12; P = .025) greater reduction in DBP.
Reductions in blood pressure appeared consistent, irrespective of country, age, sex, history of high blood pressure, weight, baseline blood pressure, and baseline levels of urinary sodium and potassium.
Clear benefit on hard outcomes
Pooled data on clinical outcomes from five trials that included 24,306 participants, mostly from the SSaSS, showed clear protective effects of salt substitutes on total mortality (risk ratio, 0.89; 95% CI, 0.85-0.94), CV mortality (RR, 0.87; 95% CI, 0.81-0.94), and CV events (RR, 0.89; 95% CI, 0.85-0.94).
Dr. Tian and colleagues say that “broader population use of salt substitute is supported by the absence of any detectable adverse effect of salt substitutes on hyperkalemia in this review.”
They note, however, that all of the trials took “pragmatic steps to exclude participants at elevated risk of hyperkalemia, seeking to exclude those with chronic kidney disease or using medications that elevate serum potassium.”
Offering perspective on the study, Harlan Krumholz, MD, with Yale New Haven Hospital and Yale School of Medicine, both in New Haven, Conn., said it provides “useful information by bringing together the trial evidence on salt substitutes. The evidence is dominated by the SSaSS, but the others add context.”
Dr. Krumholz said that at this point, he thinks salt substitutes “could be included in recommendations to patients.”
“SSaSS was conducted in villages in China, so that is where the evidence is strongest and most relevant, but this is a low-cost and seemingly safe strategy that could be tried by anyone without contraindications, such as kidney disease or taking a potassium-sparing medication or potassium supplement,” Dr. Krumholz told this news organization.
Johanna Contreras, MD, heart failure and transplant cardiologist at the Mount Sinai Hospital, New York, agrees that in the absence of contraindications, salt substitutes should be recommended.
“Americans put salt on everything and don’t even think about it. The salt substitutes are very helpful,” Dr. Contreras said in an interview.
“People who don’t have high blood pressure should limit salt intake, because what we have seen is that if you have high blood pressure in your family – even if you don’t have high blood pressure in your 20s or 30s – you’re likely to develop high blood pressure,” Dr. Contreras said.
“Therefore, it’s wise early on to start protecting yourself and using low salt and salt substitutes,” she added.
The study had no specific funding. Dr. Tian, Dr. Krumholz, and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social isolation, loneliness tied to death, MI, stroke: AHA
People who are socially isolated or lonely have an increased risk for myocardial infarction, stroke, and death, independent of other factors, the American Heart Association concludes in a new scientific statement.
More than 4 decades of research have “clearly demonstrated that social isolation and loneliness are both associated with adverse health outcomes,” writing group chair Crystal Wiley Cené, MD, University of California San Diego Health, said in a news release.
“Given the prevalence of social disconnectedness across the United States, the public health impact is quite significant,” Dr. Cené added.
The writing group says more research is needed to develop, implement, and test interventions to improve cardiovascular (CV) and brain health in people who are socially isolated or lonely.
The scientific statement was published online in the Journal of the American Heart Association.
Common and potentially deadly
Social isolation is defined as having infrequent in-person contact with people and loneliness is when a person feels he or she is alone or has less connection with others than desired.
It’s estimated that one-quarter of community-dwelling Americans 65 years and older are socially isolated, with even more experiencing loneliness.
The problem is not limited to older adults, however. Research suggests that younger adults also experience social isolation and loneliness, which might be attributed to more social media use and less frequent in-person activities.
Dr. Cené and colleagues reviewed observational and intervention research on social isolation published through July 2021 to examine the impact of social isolation and loneliness on CV and brain health.
The evidence is most consistent for a direct association between social isolation, loneliness, and death from coronary heart disease (CHD) and stroke, they reported.
For example, one meta-analysis of 19 studies showed that social isolation and loneliness increase the risk for CHD by 29%; most of these studies focused on acute MI and/or CHD death as the measure of CHD.
A meta-analysis of eight longitudinal observational studies showed social isolation and loneliness were associated with a 32% increased risk for stroke, after adjustment for age, sex, and socioeconomic status.
The literature also suggests social isolation and loneliness are associated with worse prognoses in adults with existing CHD or history of stroke.
One systematic review showed that socially isolated people with CHD had a two- to threefold increase in illness and death over 6 years, independent of cardiac risk factors.
Other research suggests that socially isolated adults with three or fewer social contacts per month have a 40% increased risk for recurrent stroke or MI.
There are fewer and less robust data on the association between social isolation and loneliness with heart failure (HF), dementia, and cognitive impairment, the writing group noted.
It’s also unclear whether actually being isolated (social isolation) or feeling isolated (loneliness) matters most for cardiovascular and brain health, because only a few studies have examined both in the same sample, they pointed out.
However, a study published in Neurology in June showed that older adults who reported feeling socially isolated had worse cognitive function at baseline than did those who did not report social isolation, and were 26% more likely to have dementia at follow-up, as reported by this news organization.
Urgent need for interventions
“There is an urgent need to develop, implement, and evaluate programs and strategies to reduce the negative effects of social isolation and loneliness on cardiovascular and brain health, particularly for at-risk populations,” Dr. Cené said in the news release.
She encourages clinicians to ask patients about their social life and whether they are satisfied with their level of interactions with friends and family, and to be prepared to refer patients who are socially isolated or lonely, especially those with a history of CHD or stroke, to community resources to help them connect with others.
Fitness programs and recreational activities at senior centers, as well as interventions that address negative thoughts of self-worth and other negative thinking, have shown promise in reducing isolation and loneliness, the writing group said.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Social Determinants of Health Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Stroke Council.
This research had no commercial funding. Members of the writing group have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who are socially isolated or lonely have an increased risk for myocardial infarction, stroke, and death, independent of other factors, the American Heart Association concludes in a new scientific statement.
More than 4 decades of research have “clearly demonstrated that social isolation and loneliness are both associated with adverse health outcomes,” writing group chair Crystal Wiley Cené, MD, University of California San Diego Health, said in a news release.
“Given the prevalence of social disconnectedness across the United States, the public health impact is quite significant,” Dr. Cené added.
The writing group says more research is needed to develop, implement, and test interventions to improve cardiovascular (CV) and brain health in people who are socially isolated or lonely.
The scientific statement was published online in the Journal of the American Heart Association.
Common and potentially deadly
Social isolation is defined as having infrequent in-person contact with people and loneliness is when a person feels he or she is alone or has less connection with others than desired.
It’s estimated that one-quarter of community-dwelling Americans 65 years and older are socially isolated, with even more experiencing loneliness.
The problem is not limited to older adults, however. Research suggests that younger adults also experience social isolation and loneliness, which might be attributed to more social media use and less frequent in-person activities.
Dr. Cené and colleagues reviewed observational and intervention research on social isolation published through July 2021 to examine the impact of social isolation and loneliness on CV and brain health.
The evidence is most consistent for a direct association between social isolation, loneliness, and death from coronary heart disease (CHD) and stroke, they reported.
For example, one meta-analysis of 19 studies showed that social isolation and loneliness increase the risk for CHD by 29%; most of these studies focused on acute MI and/or CHD death as the measure of CHD.
A meta-analysis of eight longitudinal observational studies showed social isolation and loneliness were associated with a 32% increased risk for stroke, after adjustment for age, sex, and socioeconomic status.
The literature also suggests social isolation and loneliness are associated with worse prognoses in adults with existing CHD or history of stroke.
One systematic review showed that socially isolated people with CHD had a two- to threefold increase in illness and death over 6 years, independent of cardiac risk factors.
Other research suggests that socially isolated adults with three or fewer social contacts per month have a 40% increased risk for recurrent stroke or MI.
There are fewer and less robust data on the association between social isolation and loneliness with heart failure (HF), dementia, and cognitive impairment, the writing group noted.
It’s also unclear whether actually being isolated (social isolation) or feeling isolated (loneliness) matters most for cardiovascular and brain health, because only a few studies have examined both in the same sample, they pointed out.
However, a study published in Neurology in June showed that older adults who reported feeling socially isolated had worse cognitive function at baseline than did those who did not report social isolation, and were 26% more likely to have dementia at follow-up, as reported by this news organization.
Urgent need for interventions
“There is an urgent need to develop, implement, and evaluate programs and strategies to reduce the negative effects of social isolation and loneliness on cardiovascular and brain health, particularly for at-risk populations,” Dr. Cené said in the news release.
She encourages clinicians to ask patients about their social life and whether they are satisfied with their level of interactions with friends and family, and to be prepared to refer patients who are socially isolated or lonely, especially those with a history of CHD or stroke, to community resources to help them connect with others.
Fitness programs and recreational activities at senior centers, as well as interventions that address negative thoughts of self-worth and other negative thinking, have shown promise in reducing isolation and loneliness, the writing group said.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Social Determinants of Health Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Stroke Council.
This research had no commercial funding. Members of the writing group have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who are socially isolated or lonely have an increased risk for myocardial infarction, stroke, and death, independent of other factors, the American Heart Association concludes in a new scientific statement.
More than 4 decades of research have “clearly demonstrated that social isolation and loneliness are both associated with adverse health outcomes,” writing group chair Crystal Wiley Cené, MD, University of California San Diego Health, said in a news release.
“Given the prevalence of social disconnectedness across the United States, the public health impact is quite significant,” Dr. Cené added.
The writing group says more research is needed to develop, implement, and test interventions to improve cardiovascular (CV) and brain health in people who are socially isolated or lonely.
The scientific statement was published online in the Journal of the American Heart Association.
Common and potentially deadly
Social isolation is defined as having infrequent in-person contact with people and loneliness is when a person feels he or she is alone or has less connection with others than desired.
It’s estimated that one-quarter of community-dwelling Americans 65 years and older are socially isolated, with even more experiencing loneliness.
The problem is not limited to older adults, however. Research suggests that younger adults also experience social isolation and loneliness, which might be attributed to more social media use and less frequent in-person activities.
Dr. Cené and colleagues reviewed observational and intervention research on social isolation published through July 2021 to examine the impact of social isolation and loneliness on CV and brain health.
The evidence is most consistent for a direct association between social isolation, loneliness, and death from coronary heart disease (CHD) and stroke, they reported.
For example, one meta-analysis of 19 studies showed that social isolation and loneliness increase the risk for CHD by 29%; most of these studies focused on acute MI and/or CHD death as the measure of CHD.
A meta-analysis of eight longitudinal observational studies showed social isolation and loneliness were associated with a 32% increased risk for stroke, after adjustment for age, sex, and socioeconomic status.
The literature also suggests social isolation and loneliness are associated with worse prognoses in adults with existing CHD or history of stroke.
One systematic review showed that socially isolated people with CHD had a two- to threefold increase in illness and death over 6 years, independent of cardiac risk factors.
Other research suggests that socially isolated adults with three or fewer social contacts per month have a 40% increased risk for recurrent stroke or MI.
There are fewer and less robust data on the association between social isolation and loneliness with heart failure (HF), dementia, and cognitive impairment, the writing group noted.
It’s also unclear whether actually being isolated (social isolation) or feeling isolated (loneliness) matters most for cardiovascular and brain health, because only a few studies have examined both in the same sample, they pointed out.
However, a study published in Neurology in June showed that older adults who reported feeling socially isolated had worse cognitive function at baseline than did those who did not report social isolation, and were 26% more likely to have dementia at follow-up, as reported by this news organization.
Urgent need for interventions
“There is an urgent need to develop, implement, and evaluate programs and strategies to reduce the negative effects of social isolation and loneliness on cardiovascular and brain health, particularly for at-risk populations,” Dr. Cené said in the news release.
She encourages clinicians to ask patients about their social life and whether they are satisfied with their level of interactions with friends and family, and to be prepared to refer patients who are socially isolated or lonely, especially those with a history of CHD or stroke, to community resources to help them connect with others.
Fitness programs and recreational activities at senior centers, as well as interventions that address negative thoughts of self-worth and other negative thinking, have shown promise in reducing isolation and loneliness, the writing group said.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Social Determinants of Health Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Quality of Care and Outcomes Research; the Prevention Science Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Stroke Council.
This research had no commercial funding. Members of the writing group have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Omecamtiv mecarbil fails to improve exercise capacity in HFrEF
Treatment with the novel agent omecamtiv mecarbil did not improve exercise capacity in people with chronic heart failure with reduced ejection fraction (HFrEF), in the METEORIC-HF trial.
The double-blind, phase 3 study failed to achieve its primary endpoint of change in peak oxygen uptake (VO2) after 20 weeks of treatment with omecamtiv mecarbil, compared with placebo.
There also was no benefit on secondary measures of total workload, ventilatory efficiency, and daily physical activity, according to results presented earlier this year at ACC 2022 and formally published this month in JAMA.
“These findings do not support the use of omecamtiv mecarbil for treatment of HFrEF for improvement of exercise capacity,” lead author Gregory D. Lewis, MD, Massachusetts General Hospital, Boston, and colleagues conclude in the paper.
Researchers had hoped that the oral selective myosin activator would prove useful in this subset of patients, having previously shown in the GALACTIC-HF trial to provide a significant improvement in heart failure (HF) events and cardiovascular death.
A prespecified subgroup analysis from that trial also found that HF patients with the lowest ejection fraction derived the greatest relative benefit from omecamtiv mecarbil.
“The lack of effect of omecamtiv mecarbil on exercise performance is inconsistent with its known mechanism of action of directly enhancing ventricular performance and reducing the risk of cardiovascular events,” Dr. Lewis and colleagues observe.
The drug’s novel mechanism of action, direct activation of myosin, contrasts with that of currently available inotropic agents, such as dobutamine or milrinone. It is not yet approved by the U.S. Food and Drug Administration but is scheduled for an advisory committee meeting on Dec. 13, 2022, and has been assigned a Prescription Drug User Fee Act date of Feb. 28, 2023.
METEORIC-HF randomly assigned 276 patients with New York Heart Association class II or III symptoms and a left ventricular ejection fraction of 35% or less to omecamtiv mecarbil (n = 185) or placebo (n = 91), given orally twice daily at a dose of 25 mg, 37.5 mg, or 50 mg based on target plasma levels for 20 weeks, on top of guideline-directed medical therapy.
The patients’ median age was 64 years and 15% were women. The median ejection fraction was 28% and median baseline peak VO2 was 14.2 mL/kg per minute in the omecamtiv mecarbil group and 15.0 mL/kg per minute in the control group.
At 20 weeks, the mean change in peak VO2 in the omecamtiv mecarbil group was –0.24 mL/kg per minute and 0.21 mL/kg per minute in the placebo group (95% confidence interval, –1.02-0.13; P = .13).
For the secondary outcomes, the change in workload achieved on stress testing declined in the omecamtiv mecarbil group (–3.8 vs. 1.6). The drug had a neutral effect on minute ventilation relative to carbon dioxide production throughout exercise (0.28 vs. –0.14 VE/VCO2 slope) and average total daily activity units, measured over 2 weeks by accelerometer (–0.2 vs. –0.5).
The authors suggest that “one possible explanation for discordance between clinical events in a long-term follow-up study and exercise capacity improvement is that cardiac performance was not exclusively responsible for limiting exercise capacity in trial participants with HFrEF who were stable and very well treated with both pharmacologic and device HFrEF therapy.”
In an accompanying editorial, Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas, writes that another possible explanation is that participants in METEORIC-HF had less severe heart failure, compared with participants in GALACTIC-HF, and so were less likely to benefit from omecamtiv mecarbil.
METEORIC-HF excluded participants who had a HF hospitalization that required intravenous diuretics in the preceding 3 months, whereas 25% of participants in GALACTIC-HF were inpatients for decompensated HF and 36% had a HF hospitalization within the preceding 3 months.
Another plausible explanation for the differing results is that a therapy that improves long-term clinical outcomes may not improve exercise capacity, Dr. Drazner writes. “The available data are persuasive to suggest this may be the case.”
Some pharmacologic therapies, such as flosequinan, improved exercise capacity in patients with HF yet increased long-term mortality, he noted. Several medications that have a class I recommendation in the 2022 Heart Failure Guideline for the treatment of HFrEF also have not been shown to improve exercise capacity, as measured by peak VO2 or by 6-minute walk distance.
In this context, Dr. Drazner said he doesn’t anticipate the METEORIC-HF findings to derail FDA approval. However, should the drug be approved, clinicians will have increasingly complex decisions to make about which therapies should be prescribed to which patients.
“Some clinicians may contemplate using omecamtiv mecarbil either in the subgroup of patients with very low ejection fractions or more severe disease, believing this strategy will maximize the benefits of this therapy, but those approaches should be pursued with caution given they are predicated on subgroup and post hoc analyses, respectively,” he wrote.
Dr. Drazner concludes that medications known to improve survival in patients with HFrEF are used at “disappointingly low rates and suboptimal doses in the United States. Implementation strategies to improve use of such therapies are needed, and those efforts should be prioritized before adoption of therapies that reduce morbidity but not cardiovascular mortality.”
The study was sponsored by Amgen and Cytokinetics. Dr. Lewis reports financial relationships with the National Institutes of Health, American Heart Association, Amgen, Cytokinetics, Applied Therapeutics, AstraZeneca, SoniVie, Pfizer, Merck, Boehringer Ingelheim, Novartis, American Regent, Cyclerion, MyoKardia, Novo Nordisk, and UpToDate. Dr. Drazner reports being a member of the writing committee of the 2022 Heart Failure guidelines; and that he is supported by the James M. Wooten Chair in Cardiology at the University of Texas Southwestern Medical Center, which was a clinical site in METEORIC-HF. However, Dr. Drazner was not a study investigator in the trial.
A version of this article first appeared on Medscape.com.
Treatment with the novel agent omecamtiv mecarbil did not improve exercise capacity in people with chronic heart failure with reduced ejection fraction (HFrEF), in the METEORIC-HF trial.
The double-blind, phase 3 study failed to achieve its primary endpoint of change in peak oxygen uptake (VO2) after 20 weeks of treatment with omecamtiv mecarbil, compared with placebo.
There also was no benefit on secondary measures of total workload, ventilatory efficiency, and daily physical activity, according to results presented earlier this year at ACC 2022 and formally published this month in JAMA.
“These findings do not support the use of omecamtiv mecarbil for treatment of HFrEF for improvement of exercise capacity,” lead author Gregory D. Lewis, MD, Massachusetts General Hospital, Boston, and colleagues conclude in the paper.
Researchers had hoped that the oral selective myosin activator would prove useful in this subset of patients, having previously shown in the GALACTIC-HF trial to provide a significant improvement in heart failure (HF) events and cardiovascular death.
A prespecified subgroup analysis from that trial also found that HF patients with the lowest ejection fraction derived the greatest relative benefit from omecamtiv mecarbil.
“The lack of effect of omecamtiv mecarbil on exercise performance is inconsistent with its known mechanism of action of directly enhancing ventricular performance and reducing the risk of cardiovascular events,” Dr. Lewis and colleagues observe.
The drug’s novel mechanism of action, direct activation of myosin, contrasts with that of currently available inotropic agents, such as dobutamine or milrinone. It is not yet approved by the U.S. Food and Drug Administration but is scheduled for an advisory committee meeting on Dec. 13, 2022, and has been assigned a Prescription Drug User Fee Act date of Feb. 28, 2023.
METEORIC-HF randomly assigned 276 patients with New York Heart Association class II or III symptoms and a left ventricular ejection fraction of 35% or less to omecamtiv mecarbil (n = 185) or placebo (n = 91), given orally twice daily at a dose of 25 mg, 37.5 mg, or 50 mg based on target plasma levels for 20 weeks, on top of guideline-directed medical therapy.
The patients’ median age was 64 years and 15% were women. The median ejection fraction was 28% and median baseline peak VO2 was 14.2 mL/kg per minute in the omecamtiv mecarbil group and 15.0 mL/kg per minute in the control group.
At 20 weeks, the mean change in peak VO2 in the omecamtiv mecarbil group was –0.24 mL/kg per minute and 0.21 mL/kg per minute in the placebo group (95% confidence interval, –1.02-0.13; P = .13).
For the secondary outcomes, the change in workload achieved on stress testing declined in the omecamtiv mecarbil group (–3.8 vs. 1.6). The drug had a neutral effect on minute ventilation relative to carbon dioxide production throughout exercise (0.28 vs. –0.14 VE/VCO2 slope) and average total daily activity units, measured over 2 weeks by accelerometer (–0.2 vs. –0.5).
The authors suggest that “one possible explanation for discordance between clinical events in a long-term follow-up study and exercise capacity improvement is that cardiac performance was not exclusively responsible for limiting exercise capacity in trial participants with HFrEF who were stable and very well treated with both pharmacologic and device HFrEF therapy.”
In an accompanying editorial, Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas, writes that another possible explanation is that participants in METEORIC-HF had less severe heart failure, compared with participants in GALACTIC-HF, and so were less likely to benefit from omecamtiv mecarbil.
METEORIC-HF excluded participants who had a HF hospitalization that required intravenous diuretics in the preceding 3 months, whereas 25% of participants in GALACTIC-HF were inpatients for decompensated HF and 36% had a HF hospitalization within the preceding 3 months.
Another plausible explanation for the differing results is that a therapy that improves long-term clinical outcomes may not improve exercise capacity, Dr. Drazner writes. “The available data are persuasive to suggest this may be the case.”
Some pharmacologic therapies, such as flosequinan, improved exercise capacity in patients with HF yet increased long-term mortality, he noted. Several medications that have a class I recommendation in the 2022 Heart Failure Guideline for the treatment of HFrEF also have not been shown to improve exercise capacity, as measured by peak VO2 or by 6-minute walk distance.
In this context, Dr. Drazner said he doesn’t anticipate the METEORIC-HF findings to derail FDA approval. However, should the drug be approved, clinicians will have increasingly complex decisions to make about which therapies should be prescribed to which patients.
“Some clinicians may contemplate using omecamtiv mecarbil either in the subgroup of patients with very low ejection fractions or more severe disease, believing this strategy will maximize the benefits of this therapy, but those approaches should be pursued with caution given they are predicated on subgroup and post hoc analyses, respectively,” he wrote.
Dr. Drazner concludes that medications known to improve survival in patients with HFrEF are used at “disappointingly low rates and suboptimal doses in the United States. Implementation strategies to improve use of such therapies are needed, and those efforts should be prioritized before adoption of therapies that reduce morbidity but not cardiovascular mortality.”
The study was sponsored by Amgen and Cytokinetics. Dr. Lewis reports financial relationships with the National Institutes of Health, American Heart Association, Amgen, Cytokinetics, Applied Therapeutics, AstraZeneca, SoniVie, Pfizer, Merck, Boehringer Ingelheim, Novartis, American Regent, Cyclerion, MyoKardia, Novo Nordisk, and UpToDate. Dr. Drazner reports being a member of the writing committee of the 2022 Heart Failure guidelines; and that he is supported by the James M. Wooten Chair in Cardiology at the University of Texas Southwestern Medical Center, which was a clinical site in METEORIC-HF. However, Dr. Drazner was not a study investigator in the trial.
A version of this article first appeared on Medscape.com.
Treatment with the novel agent omecamtiv mecarbil did not improve exercise capacity in people with chronic heart failure with reduced ejection fraction (HFrEF), in the METEORIC-HF trial.
The double-blind, phase 3 study failed to achieve its primary endpoint of change in peak oxygen uptake (VO2) after 20 weeks of treatment with omecamtiv mecarbil, compared with placebo.
There also was no benefit on secondary measures of total workload, ventilatory efficiency, and daily physical activity, according to results presented earlier this year at ACC 2022 and formally published this month in JAMA.
“These findings do not support the use of omecamtiv mecarbil for treatment of HFrEF for improvement of exercise capacity,” lead author Gregory D. Lewis, MD, Massachusetts General Hospital, Boston, and colleagues conclude in the paper.
Researchers had hoped that the oral selective myosin activator would prove useful in this subset of patients, having previously shown in the GALACTIC-HF trial to provide a significant improvement in heart failure (HF) events and cardiovascular death.
A prespecified subgroup analysis from that trial also found that HF patients with the lowest ejection fraction derived the greatest relative benefit from omecamtiv mecarbil.
“The lack of effect of omecamtiv mecarbil on exercise performance is inconsistent with its known mechanism of action of directly enhancing ventricular performance and reducing the risk of cardiovascular events,” Dr. Lewis and colleagues observe.
The drug’s novel mechanism of action, direct activation of myosin, contrasts with that of currently available inotropic agents, such as dobutamine or milrinone. It is not yet approved by the U.S. Food and Drug Administration but is scheduled for an advisory committee meeting on Dec. 13, 2022, and has been assigned a Prescription Drug User Fee Act date of Feb. 28, 2023.
METEORIC-HF randomly assigned 276 patients with New York Heart Association class II or III symptoms and a left ventricular ejection fraction of 35% or less to omecamtiv mecarbil (n = 185) or placebo (n = 91), given orally twice daily at a dose of 25 mg, 37.5 mg, or 50 mg based on target plasma levels for 20 weeks, on top of guideline-directed medical therapy.
The patients’ median age was 64 years and 15% were women. The median ejection fraction was 28% and median baseline peak VO2 was 14.2 mL/kg per minute in the omecamtiv mecarbil group and 15.0 mL/kg per minute in the control group.
At 20 weeks, the mean change in peak VO2 in the omecamtiv mecarbil group was –0.24 mL/kg per minute and 0.21 mL/kg per minute in the placebo group (95% confidence interval, –1.02-0.13; P = .13).
For the secondary outcomes, the change in workload achieved on stress testing declined in the omecamtiv mecarbil group (–3.8 vs. 1.6). The drug had a neutral effect on minute ventilation relative to carbon dioxide production throughout exercise (0.28 vs. –0.14 VE/VCO2 slope) and average total daily activity units, measured over 2 weeks by accelerometer (–0.2 vs. –0.5).
The authors suggest that “one possible explanation for discordance between clinical events in a long-term follow-up study and exercise capacity improvement is that cardiac performance was not exclusively responsible for limiting exercise capacity in trial participants with HFrEF who were stable and very well treated with both pharmacologic and device HFrEF therapy.”
In an accompanying editorial, Mark H. Drazner, MD, MSc, University of Texas Southwestern Medical Center, Dallas, writes that another possible explanation is that participants in METEORIC-HF had less severe heart failure, compared with participants in GALACTIC-HF, and so were less likely to benefit from omecamtiv mecarbil.
METEORIC-HF excluded participants who had a HF hospitalization that required intravenous diuretics in the preceding 3 months, whereas 25% of participants in GALACTIC-HF were inpatients for decompensated HF and 36% had a HF hospitalization within the preceding 3 months.
Another plausible explanation for the differing results is that a therapy that improves long-term clinical outcomes may not improve exercise capacity, Dr. Drazner writes. “The available data are persuasive to suggest this may be the case.”
Some pharmacologic therapies, such as flosequinan, improved exercise capacity in patients with HF yet increased long-term mortality, he noted. Several medications that have a class I recommendation in the 2022 Heart Failure Guideline for the treatment of HFrEF also have not been shown to improve exercise capacity, as measured by peak VO2 or by 6-minute walk distance.
In this context, Dr. Drazner said he doesn’t anticipate the METEORIC-HF findings to derail FDA approval. However, should the drug be approved, clinicians will have increasingly complex decisions to make about which therapies should be prescribed to which patients.
“Some clinicians may contemplate using omecamtiv mecarbil either in the subgroup of patients with very low ejection fractions or more severe disease, believing this strategy will maximize the benefits of this therapy, but those approaches should be pursued with caution given they are predicated on subgroup and post hoc analyses, respectively,” he wrote.
Dr. Drazner concludes that medications known to improve survival in patients with HFrEF are used at “disappointingly low rates and suboptimal doses in the United States. Implementation strategies to improve use of such therapies are needed, and those efforts should be prioritized before adoption of therapies that reduce morbidity but not cardiovascular mortality.”
The study was sponsored by Amgen and Cytokinetics. Dr. Lewis reports financial relationships with the National Institutes of Health, American Heart Association, Amgen, Cytokinetics, Applied Therapeutics, AstraZeneca, SoniVie, Pfizer, Merck, Boehringer Ingelheim, Novartis, American Regent, Cyclerion, MyoKardia, Novo Nordisk, and UpToDate. Dr. Drazner reports being a member of the writing committee of the 2022 Heart Failure guidelines; and that he is supported by the James M. Wooten Chair in Cardiology at the University of Texas Southwestern Medical Center, which was a clinical site in METEORIC-HF. However, Dr. Drazner was not a study investigator in the trial.
A version of this article first appeared on Medscape.com.
‘Staggering’ CVD rise projected in U.S., especially in minorities
A new analysis projects steep increases by 2060 in the prevalence of cardiovascular (CV) risk factors and disease that will disproportionately affect non-White populations who have limited access to health care.
The study by Reza Mohebi, MD, Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues was published in the Journal of the American College of Cardiology.
“Even though several assumptions underlie these projections, the importance of this work cannot be overestimated,” Andreas P. Kalogeropoulos, MD, MPH, PhD, and Javed Butler, MD, MPH, MBA, wrote in an accompanying editorial. “The absolute numbers are staggering.”
From 2025 to 2060, the number of people with any one of four CV risk factors – type 2 diabetes, hypertension, dyslipidemia, and obesity – is projected to increase by 15.4 million, to 34.7 million.
And the number of people with of any one of four CV disease types – ischemic heart disease, heart failure, MI, and stroke – is projected to increase by 3.2 million, to 6.8 million.
Although the model predicts that the prevalence of CV risk factors will gradually decrease among White Americans, the highest prevalence of CV risk factors will be among the White population because of its overall size.
Conversely, the projected prevalence of CV risk factors is expected to increase in Black, Hispanic, Asian, and other race/ethnicity populations.
In parallel, the prevalence of CV disease is projected to decrease in the White population and increase among all other race/ethnicities, particularly in the Black and Hispanic populations.
“Our results project a worrisome increase with a particularly ominous increase in risk factors and disease in our most vulnerable patients, including Blacks and Hispanics,” senior author James L. Januzzi Jr., MD, summarized in a video issued by the society.
“The steep rise in CV risk factors and disease reflects the generally higher prevalence in populations projected to increase in the United States, owing to immigration and growth, including Black or Hispanic individuals,” Dr. Januzzi, also from Massachusetts General and Harvard, said in an interview.
“The disproportionate size of the risk is expected in a sense, as minority populations are disproportionately disadvantaged with respect to their health care,” he said. “But whether it is expected or not, the increase in projected prevalence is, nonetheless, concerning and a call to action.”
This study identifies “areas of opportunity for change in the U.S. health care system,” he continued. “Business as usual will result in us encountering a huge number of individuals with CV risk factors and diseases.”
The results from the current analysis assume there will be no modification in health care policies or changes in access to care for at-risk populations, Dr. Mohebi and colleagues noted.
To “stem the rising tide of CV disease in at-risk individuals,” would require strategies such as “emphasis on education regarding CV risk factors, improving access to quality healthcare, and facilitating lower-cost access to effective therapies for treatment of CV risk factors,” according to the researchers.
“Such advances need to be applied in a more equitable way throughout the United States, however,” they cautioned.
Census plus NHANES data
The researchers used 2020 U.S. census data and projected growth and 2013-2018 U.S. National Health and Nutrition Survey data to estimate the number of people with CV risk factors and CV disease from 2025 to 2060.
The estimates are based on a growing population and a fixed frequency.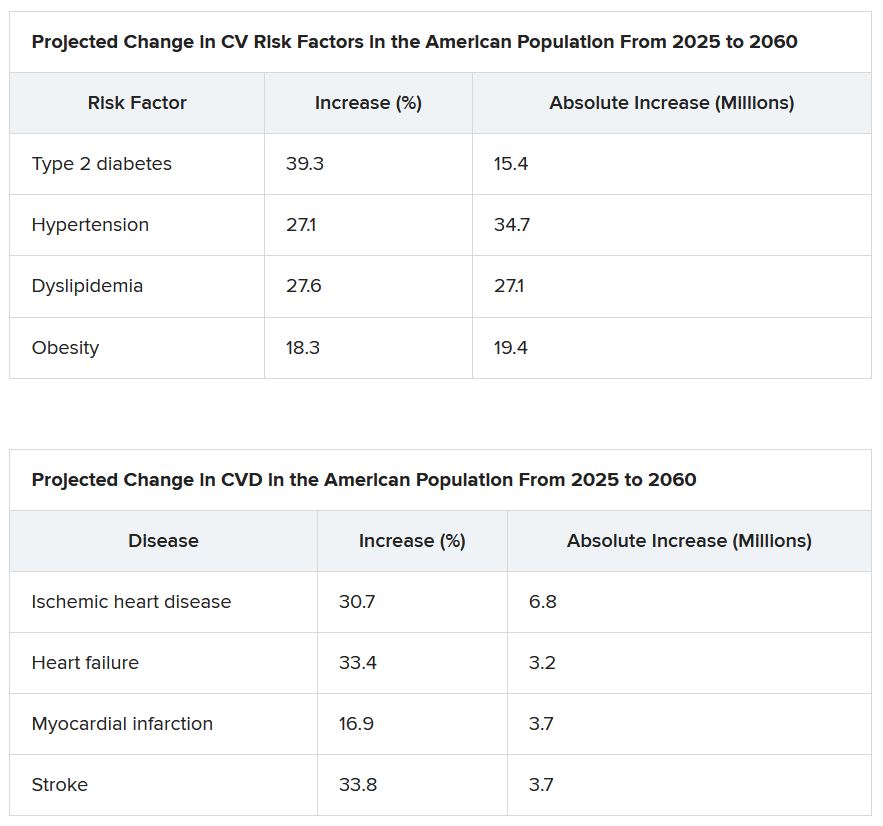
The projected changes in CV risk factors and disease over time were similar in men and women.
The researchers acknowledge that study limitations include the assumption that the prevalence patterns for CV risk factors and disease will be stable.
“To the extent the frequency of risk factors and disease are not likely to remain static, that assumption may reduce the accuracy of the projections,” Dr. Januzzi said. “However, we would point out that the goals of our analysis were to set general trends, and not to seek to project exact figures.”
Also, they did not take into account the effect of COVID-19. CV diseases were also based on self-report and CV risk factors could have been underestimated in minority populations that do not access health care.
Changing demographic landscape
It is “striking” that the numbers of non-White individuals with CV risk factors is projected to surpass the number of White individuals over time, and the number of non-White individuals with CV disease will be almost as many as White individuals by the year 2060, the editorialists noted.
“From a policy perspective, this means that unless appropriate, targeted action is taken, disparities in the burden of cardiovascular disease are only going to be exacerbated over time,” wrote Dr. Kalogeropoulos, from Stony Brook (N.Y.) University, and Dr. Butler, from Baylor College of Medicine, Dallas.
“On the positive side,” they continued, “the absolute increase in the percent prevalence of cardiovascular risk factors and conditions is projected to lie within a manageable range,” assuming that specific prevention policies are implemented.
“This is an opportunity for professional societies, including the cardiovascular care community, to re-evaluate priorities and strategies, for both training and practice, to best match the growing demands of a changing demographic landscape in the United States,” Dr. Kalogeropoulos and Dr. Butler concluded.
Dr. Mohebi is supported by the Barry Fellowship. Dr. Januzzi is supported by the Hutter Family Professorship; is a Trustee of the American College of Cardiology; is a board member of Imbria Pharmaceuticals; has received grant support from Abbott Diagnostics, Applied Therapeutics, Innolife, and Novartis; has received consulting income from Abbott Diagnostics, Boehringer Ingelheim, Janssen, Novartis, and Roche Diagnostics; and participates in clinical endpoint committees/data safety monitoring boards for AbbVie, Siemens, Takeda, and Vifor. Dr. Kalogeropoulos has received research funding from the National Heart, Lung, and Blood Institute; the American Heart Association; and the Centers for Disease Control and Prevention. Dr. Butler has been a consultant for numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
A new analysis projects steep increases by 2060 in the prevalence of cardiovascular (CV) risk factors and disease that will disproportionately affect non-White populations who have limited access to health care.
The study by Reza Mohebi, MD, Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues was published in the Journal of the American College of Cardiology.
“Even though several assumptions underlie these projections, the importance of this work cannot be overestimated,” Andreas P. Kalogeropoulos, MD, MPH, PhD, and Javed Butler, MD, MPH, MBA, wrote in an accompanying editorial. “The absolute numbers are staggering.”
From 2025 to 2060, the number of people with any one of four CV risk factors – type 2 diabetes, hypertension, dyslipidemia, and obesity – is projected to increase by 15.4 million, to 34.7 million.
And the number of people with of any one of four CV disease types – ischemic heart disease, heart failure, MI, and stroke – is projected to increase by 3.2 million, to 6.8 million.
Although the model predicts that the prevalence of CV risk factors will gradually decrease among White Americans, the highest prevalence of CV risk factors will be among the White population because of its overall size.
Conversely, the projected prevalence of CV risk factors is expected to increase in Black, Hispanic, Asian, and other race/ethnicity populations.
In parallel, the prevalence of CV disease is projected to decrease in the White population and increase among all other race/ethnicities, particularly in the Black and Hispanic populations.
“Our results project a worrisome increase with a particularly ominous increase in risk factors and disease in our most vulnerable patients, including Blacks and Hispanics,” senior author James L. Januzzi Jr., MD, summarized in a video issued by the society.
“The steep rise in CV risk factors and disease reflects the generally higher prevalence in populations projected to increase in the United States, owing to immigration and growth, including Black or Hispanic individuals,” Dr. Januzzi, also from Massachusetts General and Harvard, said in an interview.
“The disproportionate size of the risk is expected in a sense, as minority populations are disproportionately disadvantaged with respect to their health care,” he said. “But whether it is expected or not, the increase in projected prevalence is, nonetheless, concerning and a call to action.”
This study identifies “areas of opportunity for change in the U.S. health care system,” he continued. “Business as usual will result in us encountering a huge number of individuals with CV risk factors and diseases.”
The results from the current analysis assume there will be no modification in health care policies or changes in access to care for at-risk populations, Dr. Mohebi and colleagues noted.
To “stem the rising tide of CV disease in at-risk individuals,” would require strategies such as “emphasis on education regarding CV risk factors, improving access to quality healthcare, and facilitating lower-cost access to effective therapies for treatment of CV risk factors,” according to the researchers.
“Such advances need to be applied in a more equitable way throughout the United States, however,” they cautioned.
Census plus NHANES data
The researchers used 2020 U.S. census data and projected growth and 2013-2018 U.S. National Health and Nutrition Survey data to estimate the number of people with CV risk factors and CV disease from 2025 to 2060.
The estimates are based on a growing population and a fixed frequency.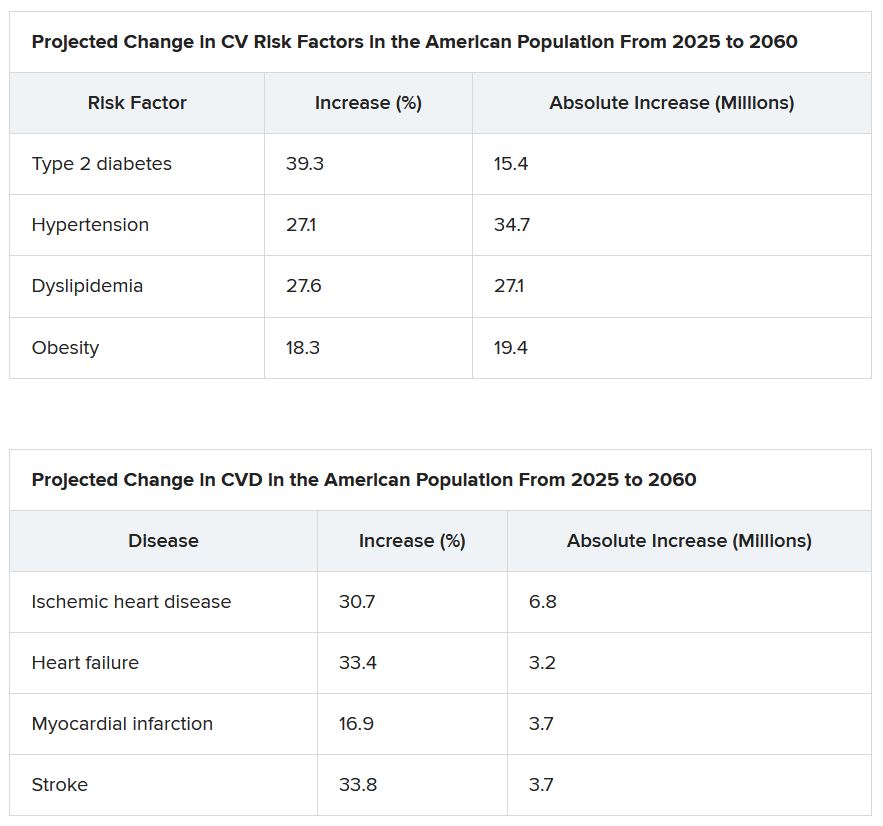
The projected changes in CV risk factors and disease over time were similar in men and women.
The researchers acknowledge that study limitations include the assumption that the prevalence patterns for CV risk factors and disease will be stable.
“To the extent the frequency of risk factors and disease are not likely to remain static, that assumption may reduce the accuracy of the projections,” Dr. Januzzi said. “However, we would point out that the goals of our analysis were to set general trends, and not to seek to project exact figures.”
Also, they did not take into account the effect of COVID-19. CV diseases were also based on self-report and CV risk factors could have been underestimated in minority populations that do not access health care.
Changing demographic landscape
It is “striking” that the numbers of non-White individuals with CV risk factors is projected to surpass the number of White individuals over time, and the number of non-White individuals with CV disease will be almost as many as White individuals by the year 2060, the editorialists noted.
“From a policy perspective, this means that unless appropriate, targeted action is taken, disparities in the burden of cardiovascular disease are only going to be exacerbated over time,” wrote Dr. Kalogeropoulos, from Stony Brook (N.Y.) University, and Dr. Butler, from Baylor College of Medicine, Dallas.
“On the positive side,” they continued, “the absolute increase in the percent prevalence of cardiovascular risk factors and conditions is projected to lie within a manageable range,” assuming that specific prevention policies are implemented.
“This is an opportunity for professional societies, including the cardiovascular care community, to re-evaluate priorities and strategies, for both training and practice, to best match the growing demands of a changing demographic landscape in the United States,” Dr. Kalogeropoulos and Dr. Butler concluded.
Dr. Mohebi is supported by the Barry Fellowship. Dr. Januzzi is supported by the Hutter Family Professorship; is a Trustee of the American College of Cardiology; is a board member of Imbria Pharmaceuticals; has received grant support from Abbott Diagnostics, Applied Therapeutics, Innolife, and Novartis; has received consulting income from Abbott Diagnostics, Boehringer Ingelheim, Janssen, Novartis, and Roche Diagnostics; and participates in clinical endpoint committees/data safety monitoring boards for AbbVie, Siemens, Takeda, and Vifor. Dr. Kalogeropoulos has received research funding from the National Heart, Lung, and Blood Institute; the American Heart Association; and the Centers for Disease Control and Prevention. Dr. Butler has been a consultant for numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
A new analysis projects steep increases by 2060 in the prevalence of cardiovascular (CV) risk factors and disease that will disproportionately affect non-White populations who have limited access to health care.
The study by Reza Mohebi, MD, Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues was published in the Journal of the American College of Cardiology.
“Even though several assumptions underlie these projections, the importance of this work cannot be overestimated,” Andreas P. Kalogeropoulos, MD, MPH, PhD, and Javed Butler, MD, MPH, MBA, wrote in an accompanying editorial. “The absolute numbers are staggering.”
From 2025 to 2060, the number of people with any one of four CV risk factors – type 2 diabetes, hypertension, dyslipidemia, and obesity – is projected to increase by 15.4 million, to 34.7 million.
And the number of people with of any one of four CV disease types – ischemic heart disease, heart failure, MI, and stroke – is projected to increase by 3.2 million, to 6.8 million.
Although the model predicts that the prevalence of CV risk factors will gradually decrease among White Americans, the highest prevalence of CV risk factors will be among the White population because of its overall size.
Conversely, the projected prevalence of CV risk factors is expected to increase in Black, Hispanic, Asian, and other race/ethnicity populations.
In parallel, the prevalence of CV disease is projected to decrease in the White population and increase among all other race/ethnicities, particularly in the Black and Hispanic populations.
“Our results project a worrisome increase with a particularly ominous increase in risk factors and disease in our most vulnerable patients, including Blacks and Hispanics,” senior author James L. Januzzi Jr., MD, summarized in a video issued by the society.
“The steep rise in CV risk factors and disease reflects the generally higher prevalence in populations projected to increase in the United States, owing to immigration and growth, including Black or Hispanic individuals,” Dr. Januzzi, also from Massachusetts General and Harvard, said in an interview.
“The disproportionate size of the risk is expected in a sense, as minority populations are disproportionately disadvantaged with respect to their health care,” he said. “But whether it is expected or not, the increase in projected prevalence is, nonetheless, concerning and a call to action.”
This study identifies “areas of opportunity for change in the U.S. health care system,” he continued. “Business as usual will result in us encountering a huge number of individuals with CV risk factors and diseases.”
The results from the current analysis assume there will be no modification in health care policies or changes in access to care for at-risk populations, Dr. Mohebi and colleagues noted.
To “stem the rising tide of CV disease in at-risk individuals,” would require strategies such as “emphasis on education regarding CV risk factors, improving access to quality healthcare, and facilitating lower-cost access to effective therapies for treatment of CV risk factors,” according to the researchers.
“Such advances need to be applied in a more equitable way throughout the United States, however,” they cautioned.
Census plus NHANES data
The researchers used 2020 U.S. census data and projected growth and 2013-2018 U.S. National Health and Nutrition Survey data to estimate the number of people with CV risk factors and CV disease from 2025 to 2060.
The estimates are based on a growing population and a fixed frequency.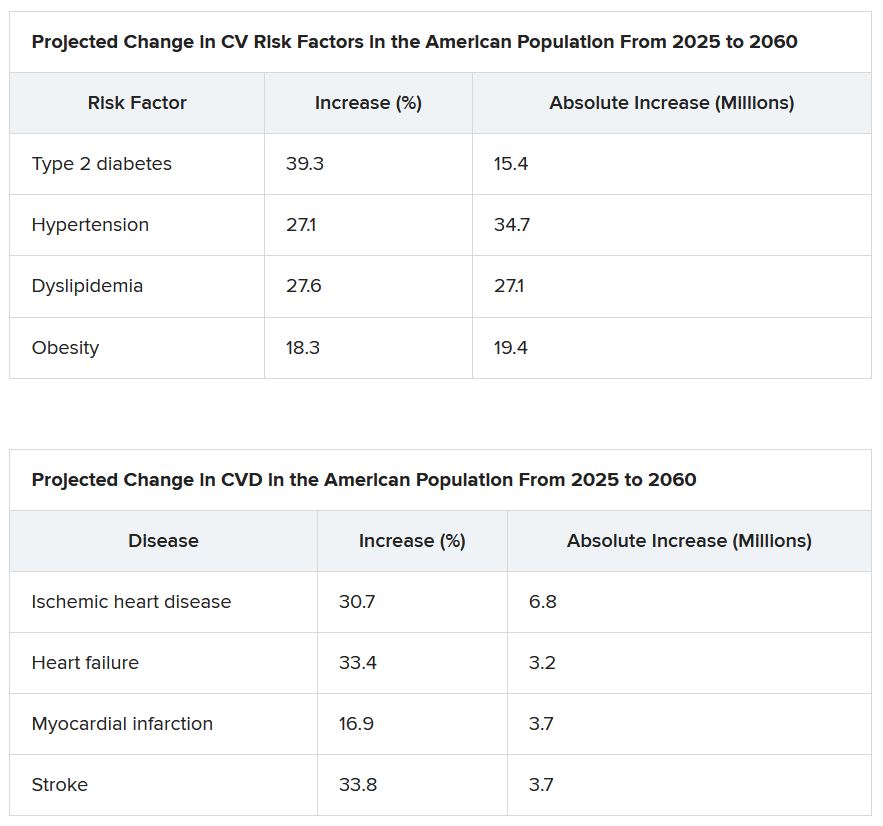
The projected changes in CV risk factors and disease over time were similar in men and women.
The researchers acknowledge that study limitations include the assumption that the prevalence patterns for CV risk factors and disease will be stable.
“To the extent the frequency of risk factors and disease are not likely to remain static, that assumption may reduce the accuracy of the projections,” Dr. Januzzi said. “However, we would point out that the goals of our analysis were to set general trends, and not to seek to project exact figures.”
Also, they did not take into account the effect of COVID-19. CV diseases were also based on self-report and CV risk factors could have been underestimated in minority populations that do not access health care.
Changing demographic landscape
It is “striking” that the numbers of non-White individuals with CV risk factors is projected to surpass the number of White individuals over time, and the number of non-White individuals with CV disease will be almost as many as White individuals by the year 2060, the editorialists noted.
“From a policy perspective, this means that unless appropriate, targeted action is taken, disparities in the burden of cardiovascular disease are only going to be exacerbated over time,” wrote Dr. Kalogeropoulos, from Stony Brook (N.Y.) University, and Dr. Butler, from Baylor College of Medicine, Dallas.
“On the positive side,” they continued, “the absolute increase in the percent prevalence of cardiovascular risk factors and conditions is projected to lie within a manageable range,” assuming that specific prevention policies are implemented.
“This is an opportunity for professional societies, including the cardiovascular care community, to re-evaluate priorities and strategies, for both training and practice, to best match the growing demands of a changing demographic landscape in the United States,” Dr. Kalogeropoulos and Dr. Butler concluded.
Dr. Mohebi is supported by the Barry Fellowship. Dr. Januzzi is supported by the Hutter Family Professorship; is a Trustee of the American College of Cardiology; is a board member of Imbria Pharmaceuticals; has received grant support from Abbott Diagnostics, Applied Therapeutics, Innolife, and Novartis; has received consulting income from Abbott Diagnostics, Boehringer Ingelheim, Janssen, Novartis, and Roche Diagnostics; and participates in clinical endpoint committees/data safety monitoring boards for AbbVie, Siemens, Takeda, and Vifor. Dr. Kalogeropoulos has received research funding from the National Heart, Lung, and Blood Institute; the American Heart Association; and the Centers for Disease Control and Prevention. Dr. Butler has been a consultant for numerous pharmaceutical companies.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AMERICAN COLLEGE OF CARDIOLOGY
Topline results for novel drug in ATTR amyloidosis with cardiomyopathy
The RNA interference (RNAi) therapeutic patisiran (Onpattro, Alnylam Pharmaceuticals) led to statistically significant improvement in functional capacity and quality of life in adults with transthyretin-mediated (ATTR) amyloidosis with cardiomyopathy in the phase 3 APOLLO-B study, according to topline results released Aug. 3.
“We are thrilled that APOLLO-B successfully met all its major objectives, which we believe for the first time validates the hypothesis that TTR silencing by an RNAi therapeutic can be an effective approach for treating the cardiomyopathy of ATTR amyloidosis,” Pushkal Garg, MD, Alnylam chief medical officer, said in a news release.
The Food and Drug Administration approved patisiran in 2018 for polyneuropathy caused by hereditary ATTR in adults on the basis of results of the APOLLO phase 3 trial, as reported by this news organization.
APOLLO-B enrolled 360 adults with ATTR amyloidosis (hereditary or wild-type) with cardiomyopathy at 69 centers in 21 countries. Half were randomly allocated to 0.3 mg/kg of patisiran or placebo administered intravenously every 3 weeks for 12 months.
The study met the primary endpoint of a statistically significant improvement from baseline in the 6-minute walk test at 12 months compared with placebo (P = .0162), the company said.
The study also met the first secondary endpoint of a statistically significant improvement from baseline in quality of life compared with placebo, as measured by the Kansas City Cardiomyopathy Questionnaire (P = .0397).
The patisiran and placebo groups had similar frequencies of adverse events (91% and 94%, respectively) and serious adverse events (34% and 35%, respectively).
“ATTR amyloidosis with cardiomyopathy is an increasingly recognized cause of heart failure, affecting greater than 250,000 patients around the world. These patients have limited treatment options, and disease progression is common. As such, we are encouraged to see the potential of patisiran to improve the functional capacity and quality of life of patients living with this fatal, multisystem disease,” Dr. Garg said in the release.
Full results from APOLLO-B will be presented at a late-breaker session at the 18th International Symposium on Amyloidosis in September in Heidelberg, Germany.
Based on these results, the company plans to file a supplementary new drug application (sNDA) for patisiran for this indication with the FDA later this year, the release noted.
A version of this article first appeared on Medscape.com.
The RNA interference (RNAi) therapeutic patisiran (Onpattro, Alnylam Pharmaceuticals) led to statistically significant improvement in functional capacity and quality of life in adults with transthyretin-mediated (ATTR) amyloidosis with cardiomyopathy in the phase 3 APOLLO-B study, according to topline results released Aug. 3.
“We are thrilled that APOLLO-B successfully met all its major objectives, which we believe for the first time validates the hypothesis that TTR silencing by an RNAi therapeutic can be an effective approach for treating the cardiomyopathy of ATTR amyloidosis,” Pushkal Garg, MD, Alnylam chief medical officer, said in a news release.
The Food and Drug Administration approved patisiran in 2018 for polyneuropathy caused by hereditary ATTR in adults on the basis of results of the APOLLO phase 3 trial, as reported by this news organization.
APOLLO-B enrolled 360 adults with ATTR amyloidosis (hereditary or wild-type) with cardiomyopathy at 69 centers in 21 countries. Half were randomly allocated to 0.3 mg/kg of patisiran or placebo administered intravenously every 3 weeks for 12 months.
The study met the primary endpoint of a statistically significant improvement from baseline in the 6-minute walk test at 12 months compared with placebo (P = .0162), the company said.
The study also met the first secondary endpoint of a statistically significant improvement from baseline in quality of life compared with placebo, as measured by the Kansas City Cardiomyopathy Questionnaire (P = .0397).
The patisiran and placebo groups had similar frequencies of adverse events (91% and 94%, respectively) and serious adverse events (34% and 35%, respectively).
“ATTR amyloidosis with cardiomyopathy is an increasingly recognized cause of heart failure, affecting greater than 250,000 patients around the world. These patients have limited treatment options, and disease progression is common. As such, we are encouraged to see the potential of patisiran to improve the functional capacity and quality of life of patients living with this fatal, multisystem disease,” Dr. Garg said in the release.
Full results from APOLLO-B will be presented at a late-breaker session at the 18th International Symposium on Amyloidosis in September in Heidelberg, Germany.
Based on these results, the company plans to file a supplementary new drug application (sNDA) for patisiran for this indication with the FDA later this year, the release noted.
A version of this article first appeared on Medscape.com.
The RNA interference (RNAi) therapeutic patisiran (Onpattro, Alnylam Pharmaceuticals) led to statistically significant improvement in functional capacity and quality of life in adults with transthyretin-mediated (ATTR) amyloidosis with cardiomyopathy in the phase 3 APOLLO-B study, according to topline results released Aug. 3.
“We are thrilled that APOLLO-B successfully met all its major objectives, which we believe for the first time validates the hypothesis that TTR silencing by an RNAi therapeutic can be an effective approach for treating the cardiomyopathy of ATTR amyloidosis,” Pushkal Garg, MD, Alnylam chief medical officer, said in a news release.
The Food and Drug Administration approved patisiran in 2018 for polyneuropathy caused by hereditary ATTR in adults on the basis of results of the APOLLO phase 3 trial, as reported by this news organization.
APOLLO-B enrolled 360 adults with ATTR amyloidosis (hereditary or wild-type) with cardiomyopathy at 69 centers in 21 countries. Half were randomly allocated to 0.3 mg/kg of patisiran or placebo administered intravenously every 3 weeks for 12 months.
The study met the primary endpoint of a statistically significant improvement from baseline in the 6-minute walk test at 12 months compared with placebo (P = .0162), the company said.
The study also met the first secondary endpoint of a statistically significant improvement from baseline in quality of life compared with placebo, as measured by the Kansas City Cardiomyopathy Questionnaire (P = .0397).
The patisiran and placebo groups had similar frequencies of adverse events (91% and 94%, respectively) and serious adverse events (34% and 35%, respectively).
“ATTR amyloidosis with cardiomyopathy is an increasingly recognized cause of heart failure, affecting greater than 250,000 patients around the world. These patients have limited treatment options, and disease progression is common. As such, we are encouraged to see the potential of patisiran to improve the functional capacity and quality of life of patients living with this fatal, multisystem disease,” Dr. Garg said in the release.
Full results from APOLLO-B will be presented at a late-breaker session at the 18th International Symposium on Amyloidosis in September in Heidelberg, Germany.
Based on these results, the company plans to file a supplementary new drug application (sNDA) for patisiran for this indication with the FDA later this year, the release noted.
A version of this article first appeared on Medscape.com.
Do ICDs still ‘work’ in primary prevention given today’s recommended HF meds?
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Contemporary guidelines highly recommend patients with heart failure with reduced ejection fraction (HFrEF) be on all four drug classes that together have shown clinical clout, including improved survival, in major randomized trials.
Although many such patients don’t receive all four drug classes, the more that are prescribed to those with primary-prevention implantable defibrillators (ICD), the better their odds of survival, a new analysis suggests.
The cohort study of almost 5,000 patients with HFrEF and such devices saw their all-cause mortality risk improve stepwise with each additional prescription they were given toward the full quadruple drug combo at the core of modern HFrEF guideline-directed medical therapy (GDMT). The four classes are sodium-glucose cotransporter 2 inhibitors, beta-blockers, mineralocorticoid receptor antagonists (MRA), and renin-angiotensin system (RAS) inhibitors.
That inverse relation between risk and number of GDMT medications held whether patients had solo-ICD or defibrillating cardiac resynchronization therapy (CRT-D) implants, and were independent of device-implantation year and comorbidities, regardless of HFrEF etiology.
“If anybody had doubts about really pushing forward as much of these guideline-directed medical therapies as the patient tolerates, these data confirm that, by doing so, we definitely do better than with two medications or one medication,” Samir Saba, MD, University of Pittsburgh Medical Center, said in an interview.
The analysis begs an old and challenging question: Do primary-prevention ICDs confer clinically important survival gains over those provided by increasingly life-preserving recommended HFrEF medical therapy?
Given the study’s incremental survival bumps with each added GDMT med, “one ought to consider whether ICD therapy can still have an impact on overall survival in this population,” proposes a report published online in JACC Clinical Electrophysiology, with Dr. Saba as senior author.
In the adjusted analysis, the 2-year risk for death from any cause in HFrEF patients with primary-prevention devices fell 36% in those with ICDs and 30% in those with CRT-D devices for each added prescribed GDMT drug, from none up to either three or four such agents (P < .001 in both cases).
Only so much can be made of nonrandomized study results, Saba observed in an interview. But they are enough to justify asking whether primary-prevention ICDs are “still valuable” in HFrEF given current GDMT. One interpretation of the study, the published report noted, is that contemporary GDMT improves HFrEF survival so much that it eclipses any such benefit from a primary-prevention ICD.
Both defibrillators and the four core drug therapies boost survival in such cases, “so the fundamental question is, are they additive. Do we save more lives by having a defibrillator on top of the medications, or is it overlapping?” Dr. Saba asked. “We don’t know the answer.”
For now, at least, the findings could reassure clinicians as they consider whether to recommended a primary-prevention ICD when there might be reasons not to, as long there is full GDMT on board, “especially what we today define as quadruple guideline-directed medical therapy.”
Recently announced North American guidelines defining an HFrEF quadruple regimen prefer – beyond a beta-blocker, MRA, and SGLT2 inhibitor – that the selected RAS inhibitor be sacubitril/valsartan (Entresto, Novartis), with ACE inhibitors or angiotensin-receptor blockers (ARBs) as a substitute, if needed.
Nearly identical European guidelines on HFrEF quad therapy, unveiled in 2021, include but do not necessarily prefer sacubitril/valsartan over ACE inhibitors as the RAS inhibitor of choice.
GDMT a moving target
Primary-prevention defibrillators entered practice at a time when expected background GDMT consisted of beta-blockers and either ACE inhibitors or ARBs, the current report notes. In practice, many patients receive the devices without both drug classes optimally on board. Moreover, many who otherwise meet guidelines for such ICDs won’t tolerate the kind of maximally tolerated GDMT used in the major primary-prevention device trials.
Yet current guidelines give such devices a class I recommendation, based on the highest level of evidence, in HFrEF patients who remain symptomatic despite quad GDMT, observed Gregg C. Fonarow, MD, University of California Los Angeles Medical Center.
The current analysis “further reinforces the importance of providing all four foundational GDMTs” to all eligible HFrEF patients without contraindications who can tolerate them, he said in an interview. Such quad therapy “is associated with incremental 1-year survival advantages” in patients with primary-prevention devices. And in the major trials, “there were reductions in sudden deaths, as well as progressive heart failure deaths.”
But the current study also suggests that in practice “very few patients can actually get to all four drugs on GDMT,” Roderick Tung, MD, University of Arizona, Phoenix, said in an interview. Optimized GDMT in randomized trials probably represents the best-case scenario. “There is a difference between randomized data and real-world data, which is why we need both.”
And it asserts that “the more GDMT you’re on, the better you do,” he said. “But does that obviate the need for an ICD? I think that’s not clear,” in part because of potential confounding in the analysis. For example, patients who can take all four agents tend to be less sick than those who cannot.
“The ones who can get up to four are preselected, because they’re healthier,” Dr. Tung said. “There are real limitations – such as metabolic disturbances, acute kidney injury and cardiorenal syndrome, and hypotension – that actually make it difficult to initiate and titrate these medications.”
Indeed, the major primary-prevention ICD trials usually excluded the sickest patients with the most comorbidities, Dr. Saba observed, which raises issues about their relevance to clinical practice. But his group’s study controlled for many potential confounders by adjusting for, among other things, Elixhauser comorbidity score, ejection fraction, type of cardiomyopathy, and year of device implantation.
“We tried to level the playing field that way, to see if – despite all of this adjustment – the incremental number of heart failure medicines stills make a difference,” Dr. Saba said. “And our results suggest that yes, they still do.”
GDMT coverage in the real world
The analysis of patients with HFrEF involved 3,210 with ICD-only implants and 1,762 with CRT-D devices for primary prevention at a major medical center from 2010 to 2021. Of the total, 5% had not been prescribed any of the four GDMT agents, 20% had been prescribed only one, 52% were prescribed two, and 23% were prescribed three or four. Only 113 patients had been prescribed SGLT2 inhibitors, which have only recently been indicated for HFrEF.
Adjusted hazard ratios for death from any cause at 2 years for each added GDMT drug (P < .001 in each case), were 0.64 (95% confidence interval, 0.56-0.74) for ICD recipients, 0.70 (95% CI, 0.58-0.86) for those with a CRT-D device, 0.70 (95% CI, 0.60-0.81) for those with ischemic cardiomyopathy, and 0.61 (95% CI, 0.51-0.73) for patients with nonischemic disease.
The results “raise questions rather than answers,” Dr. Saba said. “At some point, someone will need to take patients who are optimized on their heart failure medications and then randomize them to defibrillator versus no defibrillator to see whether there is still an additive impact.”
Current best evidence suggests that primary-prevention ICDs in patients with guideline-based indications confer benefits that far outweigh any risks. But if the major primary-prevention ICD trials were to be repeated in patients on contemporary quad-therapy GDMT, Dr. Tung said, “would the benefit of ICD be attenuated? I think most of us believe it likely would.”
Still, he said, a background of modern GDMT could potentially “optimize” such trials by attenuating mortality from heart failure progression and thereby expanding the proportion of deaths that are arrhythmic, “which the defibrillator can prevent.”
Dr. Saba discloses receiving research support from Boston Scientific and Abbott; and serving on advisory boards for Medtronic and Boston Scientific. The other authors reported no relevant relationships. Dr. Tung has disclosed receiving speaker fees from Abbott and Boston Scientific. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
FROM JACC CLINICAL ELECTROPHYSIOLOGY
‘Striking’ disparities in CVD deaths persist across COVID waves
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MAYO CLINIC PROCEEDINGS