User login
Interferon-α Treatment and Depression
About 30% to 50% of patients taking interferon-α (IFN-α), a common treatment for hepatitis C virus (HCV) infection, develop anxiety, depression, or other neuropsychiatric symptoms.
Some research has suggested that IFN-α might induce changes in tryptophan metabolism (lowering brain serotonin) or in glutamine and glutamate levels in the anterior cingulate cortex. But little work has touched on the neuropsychological mechanisms involved in the mood-lowering effects, say researchers from University of Oxford and Warneford Hospital Oxford, in the UK. Interferon-α is known to potently activate the pro-inflammatory cytokine network to produce its antiviral effects. The findings offer “intriguing evidence” indicating that exposure to inflammation by immune system activation may alter affective information processing, leading to depression in some patients.
The researchers conducted a study in 17 patients with HCV infection, measuring changes in emotional processing. They assessed participants’ mood state at baseline and 6 to 8 weeks later after a battery of tests for depression, anxiety, and fatigue. Psychological tasks included facial expression recognition and emotional categorization.
The researchers found significant correlations between pre- and post-IFN-α depressed mood scores. Notably, after IFN-α treatment, patients were more accurate at detecting facial expressions of disgust and paid less attention to the happy faces.
The negative biases in emotional processing were not simply a consequence of depression, the researchers say. It is possible that increased recognition of disgust represents a neuropsychological marker of depressive disorders related to inflammation. It seems conceivable, the researchers note, that effects on disgust recognition represent a complex interplay between inflammatory pathways and neurocircuits, which may in part be modulated by serotonin function.
The connection between disgust recognition and mood disorders has been seen before. Some researchers say it relates to feelings of social rejection, shame, and guilt. These study findings may highlight an effect more specific to inflammatory pathways. If depressive behaviors are regulated by the immune system, the researchers suggest finding out how inflammation plays a part can help define new treatment for infection.
Source:
Cooper CM, Godlewska B, Sharpley AL, Barnes E, Cowen PJ, Harmer CJ. Psychol Med. 2018;48(6):998-1007.
doi: 10.1017/S0033291717002379.
About 30% to 50% of patients taking interferon-α (IFN-α), a common treatment for hepatitis C virus (HCV) infection, develop anxiety, depression, or other neuropsychiatric symptoms.
Some research has suggested that IFN-α might induce changes in tryptophan metabolism (lowering brain serotonin) or in glutamine and glutamate levels in the anterior cingulate cortex. But little work has touched on the neuropsychological mechanisms involved in the mood-lowering effects, say researchers from University of Oxford and Warneford Hospital Oxford, in the UK. Interferon-α is known to potently activate the pro-inflammatory cytokine network to produce its antiviral effects. The findings offer “intriguing evidence” indicating that exposure to inflammation by immune system activation may alter affective information processing, leading to depression in some patients.
The researchers conducted a study in 17 patients with HCV infection, measuring changes in emotional processing. They assessed participants’ mood state at baseline and 6 to 8 weeks later after a battery of tests for depression, anxiety, and fatigue. Psychological tasks included facial expression recognition and emotional categorization.
The researchers found significant correlations between pre- and post-IFN-α depressed mood scores. Notably, after IFN-α treatment, patients were more accurate at detecting facial expressions of disgust and paid less attention to the happy faces.
The negative biases in emotional processing were not simply a consequence of depression, the researchers say. It is possible that increased recognition of disgust represents a neuropsychological marker of depressive disorders related to inflammation. It seems conceivable, the researchers note, that effects on disgust recognition represent a complex interplay between inflammatory pathways and neurocircuits, which may in part be modulated by serotonin function.
The connection between disgust recognition and mood disorders has been seen before. Some researchers say it relates to feelings of social rejection, shame, and guilt. These study findings may highlight an effect more specific to inflammatory pathways. If depressive behaviors are regulated by the immune system, the researchers suggest finding out how inflammation plays a part can help define new treatment for infection.
Source:
Cooper CM, Godlewska B, Sharpley AL, Barnes E, Cowen PJ, Harmer CJ. Psychol Med. 2018;48(6):998-1007.
doi: 10.1017/S0033291717002379.
About 30% to 50% of patients taking interferon-α (IFN-α), a common treatment for hepatitis C virus (HCV) infection, develop anxiety, depression, or other neuropsychiatric symptoms.
Some research has suggested that IFN-α might induce changes in tryptophan metabolism (lowering brain serotonin) or in glutamine and glutamate levels in the anterior cingulate cortex. But little work has touched on the neuropsychological mechanisms involved in the mood-lowering effects, say researchers from University of Oxford and Warneford Hospital Oxford, in the UK. Interferon-α is known to potently activate the pro-inflammatory cytokine network to produce its antiviral effects. The findings offer “intriguing evidence” indicating that exposure to inflammation by immune system activation may alter affective information processing, leading to depression in some patients.
The researchers conducted a study in 17 patients with HCV infection, measuring changes in emotional processing. They assessed participants’ mood state at baseline and 6 to 8 weeks later after a battery of tests for depression, anxiety, and fatigue. Psychological tasks included facial expression recognition and emotional categorization.
The researchers found significant correlations between pre- and post-IFN-α depressed mood scores. Notably, after IFN-α treatment, patients were more accurate at detecting facial expressions of disgust and paid less attention to the happy faces.
The negative biases in emotional processing were not simply a consequence of depression, the researchers say. It is possible that increased recognition of disgust represents a neuropsychological marker of depressive disorders related to inflammation. It seems conceivable, the researchers note, that effects on disgust recognition represent a complex interplay between inflammatory pathways and neurocircuits, which may in part be modulated by serotonin function.
The connection between disgust recognition and mood disorders has been seen before. Some researchers say it relates to feelings of social rejection, shame, and guilt. These study findings may highlight an effect more specific to inflammatory pathways. If depressive behaviors are regulated by the immune system, the researchers suggest finding out how inflammation plays a part can help define new treatment for infection.
Source:
Cooper CM, Godlewska B, Sharpley AL, Barnes E, Cowen PJ, Harmer CJ. Psychol Med. 2018;48(6):998-1007.
doi: 10.1017/S0033291717002379.
Where the latest HCV drug combos fit in
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
MAUI, HAWAII – The addition of the two latest treatment regimens to receive approval for hepatitis C essentially closes the circle on treatment of this disease, Steven L. Flamm, MD, declared at the Gastroenterology Updates, IBD, Liver Disease meeting.
“We now have good options available for all the hepatitis C scenarios you will ever see in your practice,” said Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“We’re already seeing a decline in the number of patients who are listed for liver transplantation with hepatitis C as the indication with UNOS [the United Organ Sharing database],” the gastroenterologist noted, citing a study presented at the 2017 annual meeting of the American Association for the Study of Liver Disease that showed that the proportion of patients who join the transplant wait-list with hepatitis C as their qualifying diagnosis has fallen by 35% since approval of the direct-acting antiviral (DAA) regimens in late 2013.
What’s special about the two newest DAA treatment regimens – sofosbuvir/velpatasvir/voxilaprevir (Vosevi) and glecaprevir/pibrentasvir (Mavyret) – is that they are pangenotypic, they are effective in prior treatment failures, they don’t need to be accompanied by ribavirin, and there is no need for baseline pretreatment resistance-associated substitution testing, Dr. Flamm noted.
“So if you have a patient sitting in front of you with any genotype of hepatitis C infection who has failed on NS5a-inhibitor therapy, you can tell them in general their chance of getting an SVR [sustained viral response] with sofosbuvir/velpatasvir/voxilaprevir is about 97%. And you can give it without worrying about what resistances they might have to begin with,” he said.
His copanelist Norah Terrault, MD, agreed that these two regimens are important additions.
“Glecaprevir/pibrentasvir is the first pangenic 8-week regimen for noncirrhotics. This is a major advance. And now having sofosbuvir/velpatasvir/voxilaprevir for treatment-experienced patients, that’s another strong advance,” commented Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
Dr. Flamm said the biggest remaining challenge in the treatment of hepatitis C is to gain improved access to therapy.
“The public-aid patients make up 30%-35% of patients with hepatitis C in my part of the country, and they still can’t get therapy unless they have cirrhosis. We can’t even treat people who have stage 2 fibrosis if they’re public-aid patients in Illinois. So we can’t achieve the goal of eliminating hepatitis C,” Dr. Flamm said.
He reported having no financial conflicts regarding his presentation.
Very few infants born to HCV-infected mothers receive testing
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
Despite the increasing prevalence of hepatitis C virus (HCV) infection in pregnant women, infants exposed to the disease are screened at a very low rate, Catherine A. Chappell, MD, and her associates wrote in Pediatrics.
During 2006-2014, 87,924 women gave birth at the Magee-Womens Hospital at the University of Pittsburgh Medical Center, of whom 1,043 had HCV. Over this time, the HCV prevalence rate increased 60%, from 1,026 cases per 100,000 women to 1,637 cases per 100,000 women. Women with HCV were more likely to be white, have Medicaid, have opiate use disorder, have other substance use disorders, and be under the age of 30 years.
Infants born to HCV-infected women are significantly more likely to be preterm and of low birth weight.
An additional 32 infants who did not receive well child care did receive HCV testing. A total of nine infants, seven in the well child group and two in the non-well child group, tested positive for HCV.
“Of the infants tested with conclusive results, the HCV transmission rate was 8.4%, with 7.2% having chronic HCV infection,” which is in line with previous reports, according to the researchers.
“Because of the poor rates of pediatric HCV screening described, future researchers should focus on interventions to increase screening in infants who are at risk for perinatal HCV acquisition by including technology to improve the transfer of maternal HCV status to the pediatric record and increase pediatric provider awareness regarding HCV screening guidelines,” the investigators concluded.
SOURCE: Chappell CA et al. Pediatrics. 2018 May 2. doi: 10.1542/peds.2017-3273.
FROM PEDIATRICS
New drugs provide new options in HCC
PHILADELPHIA – Recent approvals and investigations of targeted and immune treatments for advanced hepatocellular carcinoma (HCC) are encouraging, Nikolaos Pyrsopoulos, MD, MBA, said at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
“I am excited, because a few years ago, there was only one [Food and Drug Administration] approved medication,” Dr. Pyrsopoulos, division director for gastroenterology and hepatology at Rutgers New Jersey Medical School, Newark, said in an interview. “We are on the cusp where new compounds not only are being tested, but they are being approved.”
Median overall survival in CELESTIAL was 10.2 months for cabozantinib versus 8.0 for placebo (P = .0049), according to the published report, and investigators also reported significant improvements in progression-free survival and response versus placebo.
“It is very encouraging,” Dr. Pyrsopoulos said of the cabozantinib results in a presentation on advances in HCC that he gave at the conference.
For years, the only FDA-approved treatment for advanced HCC was sorafenib. In the randomized phase 3 SHARP trial, published in the New England Journal of Medicine in 2008, patients receiving the multikinase inhibitor had a median survival of 10.7 months, versus 7.9 months for placebo (P less than .001).
In April 2017, the FDA approved regorafenib for patients with HCC previously treated with sorafenib. In the randomized phase 3 RESORCE trial, published in The Lancet in 2017, median overall survival was 10.6 months for regorafenib-treated patients versus 7.8 months in the placebo group. Investigators reported that regorafenib improved overall survival with a hazard ratio of 0.63 (P less than .0001).
Dr. Pyrsopoulos noted that a strategy of sorafenib followed by regorafenib would combine two treatments, each of which in clinical trials had a median overall survival approaching 11 months.
“In essence, you have an approximate 2-year survival,” he said.
More agents are under investigation, including lenvatinib, another multikinase inhibitor. In results of a phase 3 randomized trial presented at the 2017 meeting of the American Society of Clinical Oncology, lenvatinib was noninferior to sorafenib in overall survival, with treatment-related adverse effects such as hypertension and diarrhea that were expected based on previous experience with the drug, investigators said.
Cancer immunotherapy is making inroads into HCC. Just a few months after approving regorafenib, the FDA granted approval to nivolumab, a PD-1 inhibitor, for patients with HCC previously treated with sorafenib. The September 2017 approval of this checkpoint inhibitor was based in part on data from the CheckMate-040 trial that included a 14.3% response rate in the 154-patient subgroup of patients who had progressive disease on sorafenib or were intolerant of the treatment.
Dr. Pyrsopoulos highlighted another checkpoint inhibitor, known as BGB-A317, or tislelizumab. In January, BeiGene announced the initiation of a global phase 3 trial of this anti-PD-1 antibody versus sorafenib as first-line treatment of patients with unresectable HCC.
Although cancer immunotherapy holds great promise for HCC and other cancers, the treatments are associated with unique immune-related adverse events (irAEs) including immune-related hepatitis that may require corticosteroid treatment, according to Dr. Pyrsopoulos.
Dr. Pyrsopoulos reported disclosures related to AbbVie, Bayer, Genfit, Gilead Sciences, Hologic, Merck, Prometheus, Shire, and Vital Therapies.
Global Academy for Medical Education and this news organization are owned by the same company.
PHILADELPHIA – Recent approvals and investigations of targeted and immune treatments for advanced hepatocellular carcinoma (HCC) are encouraging, Nikolaos Pyrsopoulos, MD, MBA, said at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
“I am excited, because a few years ago, there was only one [Food and Drug Administration] approved medication,” Dr. Pyrsopoulos, division director for gastroenterology and hepatology at Rutgers New Jersey Medical School, Newark, said in an interview. “We are on the cusp where new compounds not only are being tested, but they are being approved.”
Median overall survival in CELESTIAL was 10.2 months for cabozantinib versus 8.0 for placebo (P = .0049), according to the published report, and investigators also reported significant improvements in progression-free survival and response versus placebo.
“It is very encouraging,” Dr. Pyrsopoulos said of the cabozantinib results in a presentation on advances in HCC that he gave at the conference.
For years, the only FDA-approved treatment for advanced HCC was sorafenib. In the randomized phase 3 SHARP trial, published in the New England Journal of Medicine in 2008, patients receiving the multikinase inhibitor had a median survival of 10.7 months, versus 7.9 months for placebo (P less than .001).
In April 2017, the FDA approved regorafenib for patients with HCC previously treated with sorafenib. In the randomized phase 3 RESORCE trial, published in The Lancet in 2017, median overall survival was 10.6 months for regorafenib-treated patients versus 7.8 months in the placebo group. Investigators reported that regorafenib improved overall survival with a hazard ratio of 0.63 (P less than .0001).
Dr. Pyrsopoulos noted that a strategy of sorafenib followed by regorafenib would combine two treatments, each of which in clinical trials had a median overall survival approaching 11 months.
“In essence, you have an approximate 2-year survival,” he said.
More agents are under investigation, including lenvatinib, another multikinase inhibitor. In results of a phase 3 randomized trial presented at the 2017 meeting of the American Society of Clinical Oncology, lenvatinib was noninferior to sorafenib in overall survival, with treatment-related adverse effects such as hypertension and diarrhea that were expected based on previous experience with the drug, investigators said.
Cancer immunotherapy is making inroads into HCC. Just a few months after approving regorafenib, the FDA granted approval to nivolumab, a PD-1 inhibitor, for patients with HCC previously treated with sorafenib. The September 2017 approval of this checkpoint inhibitor was based in part on data from the CheckMate-040 trial that included a 14.3% response rate in the 154-patient subgroup of patients who had progressive disease on sorafenib or were intolerant of the treatment.
Dr. Pyrsopoulos highlighted another checkpoint inhibitor, known as BGB-A317, or tislelizumab. In January, BeiGene announced the initiation of a global phase 3 trial of this anti-PD-1 antibody versus sorafenib as first-line treatment of patients with unresectable HCC.
Although cancer immunotherapy holds great promise for HCC and other cancers, the treatments are associated with unique immune-related adverse events (irAEs) including immune-related hepatitis that may require corticosteroid treatment, according to Dr. Pyrsopoulos.
Dr. Pyrsopoulos reported disclosures related to AbbVie, Bayer, Genfit, Gilead Sciences, Hologic, Merck, Prometheus, Shire, and Vital Therapies.
Global Academy for Medical Education and this news organization are owned by the same company.
PHILADELPHIA – Recent approvals and investigations of targeted and immune treatments for advanced hepatocellular carcinoma (HCC) are encouraging, Nikolaos Pyrsopoulos, MD, MBA, said at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
“I am excited, because a few years ago, there was only one [Food and Drug Administration] approved medication,” Dr. Pyrsopoulos, division director for gastroenterology and hepatology at Rutgers New Jersey Medical School, Newark, said in an interview. “We are on the cusp where new compounds not only are being tested, but they are being approved.”
Median overall survival in CELESTIAL was 10.2 months for cabozantinib versus 8.0 for placebo (P = .0049), according to the published report, and investigators also reported significant improvements in progression-free survival and response versus placebo.
“It is very encouraging,” Dr. Pyrsopoulos said of the cabozantinib results in a presentation on advances in HCC that he gave at the conference.
For years, the only FDA-approved treatment for advanced HCC was sorafenib. In the randomized phase 3 SHARP trial, published in the New England Journal of Medicine in 2008, patients receiving the multikinase inhibitor had a median survival of 10.7 months, versus 7.9 months for placebo (P less than .001).
In April 2017, the FDA approved regorafenib for patients with HCC previously treated with sorafenib. In the randomized phase 3 RESORCE trial, published in The Lancet in 2017, median overall survival was 10.6 months for regorafenib-treated patients versus 7.8 months in the placebo group. Investigators reported that regorafenib improved overall survival with a hazard ratio of 0.63 (P less than .0001).
Dr. Pyrsopoulos noted that a strategy of sorafenib followed by regorafenib would combine two treatments, each of which in clinical trials had a median overall survival approaching 11 months.
“In essence, you have an approximate 2-year survival,” he said.
More agents are under investigation, including lenvatinib, another multikinase inhibitor. In results of a phase 3 randomized trial presented at the 2017 meeting of the American Society of Clinical Oncology, lenvatinib was noninferior to sorafenib in overall survival, with treatment-related adverse effects such as hypertension and diarrhea that were expected based on previous experience with the drug, investigators said.
Cancer immunotherapy is making inroads into HCC. Just a few months after approving regorafenib, the FDA granted approval to nivolumab, a PD-1 inhibitor, for patients with HCC previously treated with sorafenib. The September 2017 approval of this checkpoint inhibitor was based in part on data from the CheckMate-040 trial that included a 14.3% response rate in the 154-patient subgroup of patients who had progressive disease on sorafenib or were intolerant of the treatment.
Dr. Pyrsopoulos highlighted another checkpoint inhibitor, known as BGB-A317, or tislelizumab. In January, BeiGene announced the initiation of a global phase 3 trial of this anti-PD-1 antibody versus sorafenib as first-line treatment of patients with unresectable HCC.
Although cancer immunotherapy holds great promise for HCC and other cancers, the treatments are associated with unique immune-related adverse events (irAEs) including immune-related hepatitis that may require corticosteroid treatment, according to Dr. Pyrsopoulos.
Dr. Pyrsopoulos reported disclosures related to AbbVie, Bayer, Genfit, Gilead Sciences, Hologic, Merck, Prometheus, Shire, and Vital Therapies.
Global Academy for Medical Education and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES
Treatment of HCV in special populations
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
MAUI, HAWAII – Treatment of acute rather than chronic hepatitis C infection is well worth considering in selected circumstances, Norah Terrault, MD, asserted at the Gastroenterology Updates, IBD, Liver Disease meeting.
This is not at present guideline-recommended therapy. Current American Association for the Study of Liver Disease/Infectious Diseases Society of America guidance states that while there is emerging data to support treatment of acute hepatitis C, the evidence isn’t yet sufficiently robust to support a particular regimen or duration. The guidelines currently recommend waiting 6 months to see if the acute infection resolves spontaneously, as happens in a minority of cases, or becomes chronic, at which point it becomes guideline-directed treatment time. But Dr. Terrault believes persuasive evidence to back treatment of acute hepatitis C infection (HCV) is forthcoming, and she noted that the guidelines leave the door ajar by stating, “There are instances wherein a clinician may decide that the benefits of early treatment outweigh waiting for possible spontaneous clearance.”
Treatment of acute HCV
Dr. Terrault deems treatment of acute HCV warranted in circumstances in which there is significant danger of transmission from the acutely infected individual to others. For example, health care providers with a needlestick HCV infection, injecting drug users, and men with acute HCV/HIV coinfection. She also treats acute HCV in patients with underlying chronic liver disease.
“Clearly, I wouldn’t want those individuals to have any worsening of their liver function, so I would treat them acutely,” explained Dr. Terrault, professor of medicine and director of the Viral Hepatitis Center at the University of California, San Francisco.
She cited as particularly impressive the results of the SWIFT-C trial presented by Suzanna Naggie, MD, of Duke University, Durham, N.C., at the 2017 AASLD annual meeting. In this modest-size, National Institutes of Health–sponsored, multicenter study of HIV-infected men with acute HCV coinfection, the sustained viral response (SVR) rate with 8 weeks of ledipasvir/sofosbuvir (Harvoni) was 100%, regardless of their baseline HCV RNA level.
“I think this is remarkable. They cleared virus quite late and yet they went on to achieve HCV eradication. It highlights how little we really know about the treatment of individuals in this phase and that relying on HCV RNA levels may not tell the whole story. I think this is important data to suggest maybe when we treat acute hepatitis C we can use a shorter duration of treatment for that population. There are also other small studies testing 8 weeks of treatment in non–HIV-infected individuals with acute hepatitis C in which they also showed very high SVR rates,” the hepatologist said.
Copanelist Steven L. Flamm, MD, said that when he encounters a patient with acute HCV he, too, is prepared to offer treatment – he finds the available supporting evidence sufficiently compelling – but he often encounters a problem.
“Sometimes I’m blocked by insurance companies because this isn’t officially approved,” noted Dr. Flamm, professor of medicine and chief of the hepatology program at Northwestern University, Chicago.
“You’re right,” Dr. Terrault commented, “we have to make a pretty compelling argument to the insurer as to why we’re treating. But ‘treat to prevent transmission to others’ usually is successful in our hands.”
HCV in patients with end-stage renal disease
The product labeling for sofosbuvir (Sovaldi) says the drug’s safety and efficacy haven’t been established in patients with severe renal impairment or end-stage renal disease. However, a small multicenter study presented at the 2017 AASLD meeting demonstrated that 12 weeks of ledipasvir/sofosbuvir achieved a 100% SVR rate in patients with genotype 1 HCV and severe renal impairment, including some on dialysis, with no clinically meaningful change in estimated glomerular filtration rate or any signal of cardiac arrhythmia.
“The serum drug levels went up significantly, but reassuringly they saw no meaningful safety signals,” according to Dr. Terrault. “This, I think, is initial reassuring information that we were all very much waiting for.”
Still, as the AASLD/IDSA guidelines point out, ledipasvir/sofosbuvir is not a recommended option for HCV treatment in end-stage renal disease.
“In general, I think glecapravir/pibrentasvir [Mavyret] has become the go-to drug for patients who have renal dysfunction because it’s a pangenic regimen, it doesn’t require use of sofosbuvir, and there’s no dose adjustment. But I would say you could encounter situations where you might want to use sofosbuvir, and for me that situation is typically those direct-acting, antiviral-experienced patients who have failed other therapies and you really need to use sofosbuvir/velpatasvir/voxilaprevir [Vosevi] as your last or rescue therapy,” the hepatologist continued.
HCV in liver transplant recipients
“In the years before the direct-acting antivirals, treating transplant patients was always very challenging,” Dr. Terrault recalled. “They had very low response rates to therapy. That’s all gone away. Now we can say that liver transplant recipients who require treatment have response rates that are the same as in individuals who have not had a transplant. These patients are now being treated earlier and earlier after their transplant because you can do it safely.”
She pointed to a study presented at the 2017 AASLD meeting by Kosh Agarwal, MD, of Kings College London. It involved 79 adults with recurrent genotypes 1-4 HCV infection post–liver transplant who were treated with sofosbuvir/velpatasvir (Epclusa) for 12 weeks with a total SVR rate of 96%.
“The nice thing about sofosbuvir/velpatasvir is there are no drug-drug interactions with immunosuppressive drugs. Now it’s very easy to take care of these patients. The SVR rates are excellent,” Dr. Terrault observed.
The other combination that’s been studied specifically in liver transplant recipients, and in kidney transplant recipients as well, is glecapravir/pibrentasvir. In the MAGELLAN-2 study of 100 such patients with genotypes 1-6 HCV, the SVR rate was 99% with no drug-related adverse events leading to discontinuation.
Persons who inject drugs
The Centers for Disease Control and Prevention and the World Health Organization want HCV eradicated by 2030. If that’s going to happen, physicians will have to become more comfortable treating the disease in injectable drug users, a population with a high prevalence of HCV. Several studies have now shown that very high SVR rates can be achieved with direct-acting antiviral regimens as short as 8 weeks in these individuals, even if they are concurrently injecting drugs.
“There is increasing evidence that we should be doing more treatment in persons who inject drugs. Many of these individuals have very early disease and their response rates are excellent,” according to Dr. Terrault.
Moreover, their reinfection rates “are not outrageous,” she said: 1% or less in individuals who stopped injecting drugs decades prior to anti-HCV treatment, 5%-10% over the course of 3-5 years in those who continue injecting drugs after achieving SVR, and about 2% in those on methadone substitution therapy.
“These are very acceptable levels of reinfection if our goal is to move toward elimination of hepatitis C in this population,” she said.
She reported having no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM GUILD 2018
Hep B therapy: Indefinite or FINITE for e-negative patients?
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
LAS VEGAS – Current guidelines recommend indefinite continuation of antiviral therapy in chronic hepatitis B patients who are hepatitis B e-antigen (HBeAg)-negative. But emerging data suggest that this may not always be the case.
“It’s very provocative data, though not at the guideline level,” W. Ray Kim, MD, said in a presentation at the inaugural Perspectives in Digestive Diseases meeting held by Global Academy for Medical Education.
“There are patients who really have begged to go off treatment because they are sick of taking the medication for year after year after year,” said Dr. Kim, professor of medicine, gastroenterology and hepatology, Stanford (Calif.) University.
In light of new data, taking them off medication might be “something to consider” in noncirrhotic patients if they are completely suppressed, have normal ALT, and have a low level of quantitative hepatitis B surface antigen (HBsAg), Dr. Kim told attendees.
The most current Association for the Advancement of the Study of Liver Diseases guidelines state that unless there is a competing rationale, antiviral therapy should be continued indefinitely for noncirrhotic adults with HBeAg‐negative immune‐active chronic hepatitis B.
They do also say that treatment discontinuation “may be considered” for individuals with proven loss of HBsAg. “However, there is currently insufficient evidence to definitively guide treatment decisions for such persons,” the guidelines say.
Evidence has emerged since those guideline statements were written. Most recently, German investigators published results of the FINITE study showing some long-term responses after stopping tenofovir disoproxil fumarate (TDF) in noncirrhotic, HBeAg-negative patients.
In that prospective, controlled study, 62% of patients who stopped TDF therapy (n = 13) stayed off therapy to week 144 of treatment follow-up. Four of the patients achieved HBsAg loss, and median HBsAg change was –0.59log10IU/mL vs. 0.21log10IU/mL in patients who stayed on TDF therapy.
Investigators said that result demonstrated the potential of stopping long-term TDF treatment and seeing either HBsAg loss or sustained virologic response.
Before that, a retrospective study from investigators in Taiwan showed that age plus level of HBsAg were associated with HBV relapse after entecavir treatment in HBeAg-negative patients. According to investigators, those results suggested HBsAg levels could be used to guide timing of entecavir cessation.
If antiviral therapy is stopped in an HBeAg-negative patient, that patient should be monitored every 3 month for a year for recurrent viremia, ALT flares, and hepatic decompensation, Dr. Kim said at the meeting.
Even before stopping, “there are a number of factors to consider, including biological relapse, flare, hepatic decompensation,” he said.
On the other hand, there is the burden of continued therapy, financial concerns of continuing treatment due not only to medication costs but also long-term monitoring, as well as patient and provider preference, he noted in his presentation.
Global Academy and this news organization are owned by the same parent company.
Dr. Kim reported serving as a consultant to Gilead.
EXPERT ANALYSIS FROM PERSPECTIVES IN DIGESTIVE DISEASES
DAAs open up organ donation from HCV patients
BOSTON – There was no sign of HCV infection more than a year after 10 patients at Johns Hopkins University, Baltimore, received kidneys from HCV-infected donors.
The patients were treated with prophylactic direct-acting antivirals (DAAs) before and after the procedure. Low levels of hepatitis C RNA were detected shortly after transplant in five patients, but it became undetectable within a week. None of the patients developed any clinical signs of chronic hepatitis C infection, and the transplanted kidneys functioned well.
The number of organs from HCV–infected people is on the rise because of the opioid epidemic. Organ donations from drug overdoses used to be rare, but about 10% of transplanted organs are now from an overdose death, and about 30% of people who overdose have HCV. “These are young people who could donate hearts, lungs, and kidneys, and their parents and families want them to be able to make that gift of life,” said lead investigator Christine Durand, MD, of Johns Hopkins University, Baltimore.
DAAs make that possible because they cure HCV. “If the success of these transplants continues, it could pave the way for other hepatitis C–positive organs, including hearts and livers, to be transplanted as well,” Dr. Durand and her colleagues said in a press release from Johns Hopkins.
The 10 patients were over age 50 years, with a mean age of 71 years, and had been on the kidney transplant list for an average of 4 months. The HCV-positive donors were 13-50 years old with no evidence of kidney disease (Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871)..
Each recipient received a dose of grazoprevir/elbasvir (Zepatier) before transplant and stayed on the medication daily for 12 weeks postop. Three patients also took a daily dose of sofosbuvir (Sovaldi) because of the strain of HCV in the donor kidney. Maybe 8 weeks of treatment, or even 4, is enough, Dr. Durand said at the Conference on Retroviruses and Opportunistic Infections.
“I am thrilled to report that at 1 year post transplant 10 out of 10 of these recipients are HCV free, and they are doing very well. Prophylactic treatment may mean that more individuals can receive transplants from hepatitis C–infected donors without transmission of infection. The use of organs from infected donors can help everyone on the transplant list by shortening wait times and shortening the wait list,” she said.
“I’m not surprised by the results of the study because these DAAs are highly effective, but I was surprised by how willing patients were to sign up for the study. They said it was a no-brainer. In our region, if you need a kidney, you are going to wait for up to 5 years, and you may die while you are waiting. If you can accept a hepatitis C–positive donor organ, you will get transplanted in a matter of weeks,” she said.
“I hope providers tell their patients with HCV that they can register as organ donors,” she said.
The work is being supported primarily by Merck Sharp & Dohme. Dr. Durand is an advisor to Bristol-Meyers Squibb, Gilead Sciences, and Merck Pharmaceuticals and has research funding from the companies.
SOURCE: Durand CM et al. Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871.
BOSTON – There was no sign of HCV infection more than a year after 10 patients at Johns Hopkins University, Baltimore, received kidneys from HCV-infected donors.
The patients were treated with prophylactic direct-acting antivirals (DAAs) before and after the procedure. Low levels of hepatitis C RNA were detected shortly after transplant in five patients, but it became undetectable within a week. None of the patients developed any clinical signs of chronic hepatitis C infection, and the transplanted kidneys functioned well.
The number of organs from HCV–infected people is on the rise because of the opioid epidemic. Organ donations from drug overdoses used to be rare, but about 10% of transplanted organs are now from an overdose death, and about 30% of people who overdose have HCV. “These are young people who could donate hearts, lungs, and kidneys, and their parents and families want them to be able to make that gift of life,” said lead investigator Christine Durand, MD, of Johns Hopkins University, Baltimore.
DAAs make that possible because they cure HCV. “If the success of these transplants continues, it could pave the way for other hepatitis C–positive organs, including hearts and livers, to be transplanted as well,” Dr. Durand and her colleagues said in a press release from Johns Hopkins.
The 10 patients were over age 50 years, with a mean age of 71 years, and had been on the kidney transplant list for an average of 4 months. The HCV-positive donors were 13-50 years old with no evidence of kidney disease (Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871)..
Each recipient received a dose of grazoprevir/elbasvir (Zepatier) before transplant and stayed on the medication daily for 12 weeks postop. Three patients also took a daily dose of sofosbuvir (Sovaldi) because of the strain of HCV in the donor kidney. Maybe 8 weeks of treatment, or even 4, is enough, Dr. Durand said at the Conference on Retroviruses and Opportunistic Infections.
“I am thrilled to report that at 1 year post transplant 10 out of 10 of these recipients are HCV free, and they are doing very well. Prophylactic treatment may mean that more individuals can receive transplants from hepatitis C–infected donors without transmission of infection. The use of organs from infected donors can help everyone on the transplant list by shortening wait times and shortening the wait list,” she said.
“I’m not surprised by the results of the study because these DAAs are highly effective, but I was surprised by how willing patients were to sign up for the study. They said it was a no-brainer. In our region, if you need a kidney, you are going to wait for up to 5 years, and you may die while you are waiting. If you can accept a hepatitis C–positive donor organ, you will get transplanted in a matter of weeks,” she said.
“I hope providers tell their patients with HCV that they can register as organ donors,” she said.
The work is being supported primarily by Merck Sharp & Dohme. Dr. Durand is an advisor to Bristol-Meyers Squibb, Gilead Sciences, and Merck Pharmaceuticals and has research funding from the companies.
SOURCE: Durand CM et al. Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871.
BOSTON – There was no sign of HCV infection more than a year after 10 patients at Johns Hopkins University, Baltimore, received kidneys from HCV-infected donors.
The patients were treated with prophylactic direct-acting antivirals (DAAs) before and after the procedure. Low levels of hepatitis C RNA were detected shortly after transplant in five patients, but it became undetectable within a week. None of the patients developed any clinical signs of chronic hepatitis C infection, and the transplanted kidneys functioned well.
The number of organs from HCV–infected people is on the rise because of the opioid epidemic. Organ donations from drug overdoses used to be rare, but about 10% of transplanted organs are now from an overdose death, and about 30% of people who overdose have HCV. “These are young people who could donate hearts, lungs, and kidneys, and their parents and families want them to be able to make that gift of life,” said lead investigator Christine Durand, MD, of Johns Hopkins University, Baltimore.
DAAs make that possible because they cure HCV. “If the success of these transplants continues, it could pave the way for other hepatitis C–positive organs, including hearts and livers, to be transplanted as well,” Dr. Durand and her colleagues said in a press release from Johns Hopkins.
The 10 patients were over age 50 years, with a mean age of 71 years, and had been on the kidney transplant list for an average of 4 months. The HCV-positive donors were 13-50 years old with no evidence of kidney disease (Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871)..
Each recipient received a dose of grazoprevir/elbasvir (Zepatier) before transplant and stayed on the medication daily for 12 weeks postop. Three patients also took a daily dose of sofosbuvir (Sovaldi) because of the strain of HCV in the donor kidney. Maybe 8 weeks of treatment, or even 4, is enough, Dr. Durand said at the Conference on Retroviruses and Opportunistic Infections.
“I am thrilled to report that at 1 year post transplant 10 out of 10 of these recipients are HCV free, and they are doing very well. Prophylactic treatment may mean that more individuals can receive transplants from hepatitis C–infected donors without transmission of infection. The use of organs from infected donors can help everyone on the transplant list by shortening wait times and shortening the wait list,” she said.
“I’m not surprised by the results of the study because these DAAs are highly effective, but I was surprised by how willing patients were to sign up for the study. They said it was a no-brainer. In our region, if you need a kidney, you are going to wait for up to 5 years, and you may die while you are waiting. If you can accept a hepatitis C–positive donor organ, you will get transplanted in a matter of weeks,” she said.
“I hope providers tell their patients with HCV that they can register as organ donors,” she said.
The work is being supported primarily by Merck Sharp & Dohme. Dr. Durand is an advisor to Bristol-Meyers Squibb, Gilead Sciences, and Merck Pharmaceuticals and has research funding from the companies.
SOURCE: Durand CM et al. Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871.
REPORTING FROM CROI
Key clinical point: HCV may soon no longer bar organ donation.
Major finding: There was no sign of HCV infection more than a year after 10 patients at Johns Hopkins University, Baltimore, received kidneys from HCV-infected donors.
Study details: Open-label nonrandomized trial.
Disclosures: The work is being supported primarily by Merck Sharp & Dohme. The study lead is an advisor to Bristol-Meyers Squibb, Gilead Sciences, and Merck Pharmaceuticals, and has research funding from the companies.
Source: Durand CM et al. Ann Intern Med. 2018 Mar 6. doi: 10.7326/M17-2871.
Fibrosis-related genes are dysregulated in HCV-induced liver disease
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
FROM GENE
New point-of-care HCV assay shows promise for developing world
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
FROM GUT
Life and health are not even across the U.S.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.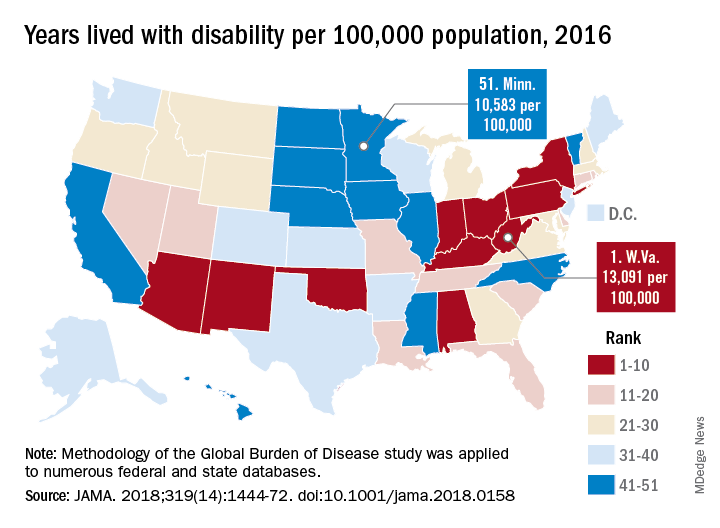
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
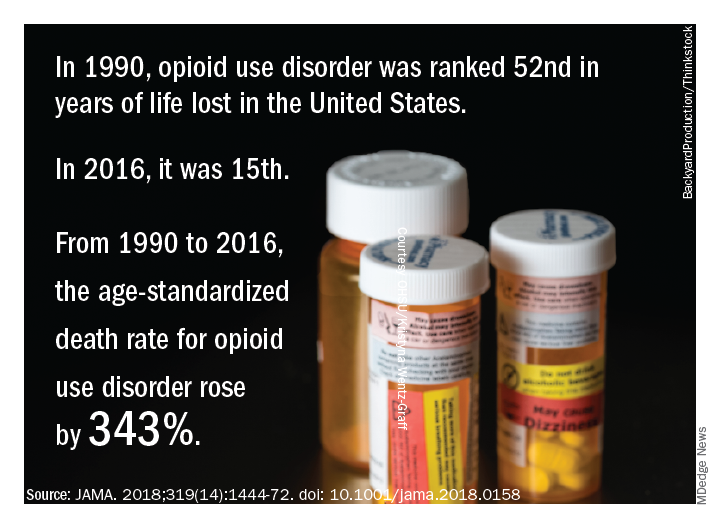
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.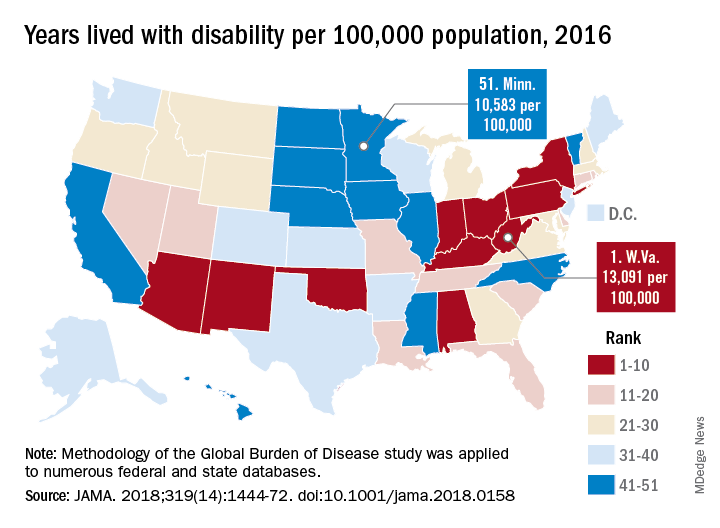
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
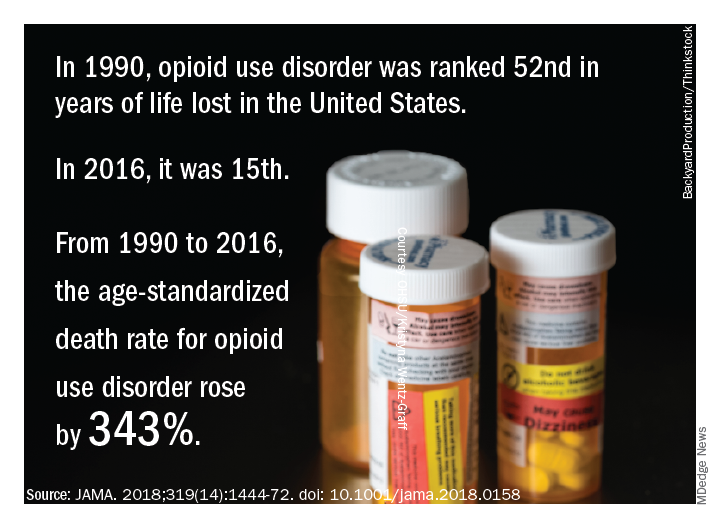
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.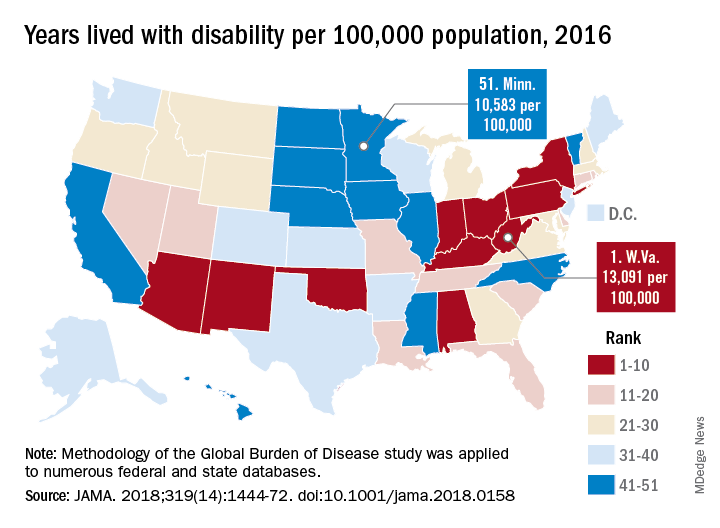
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
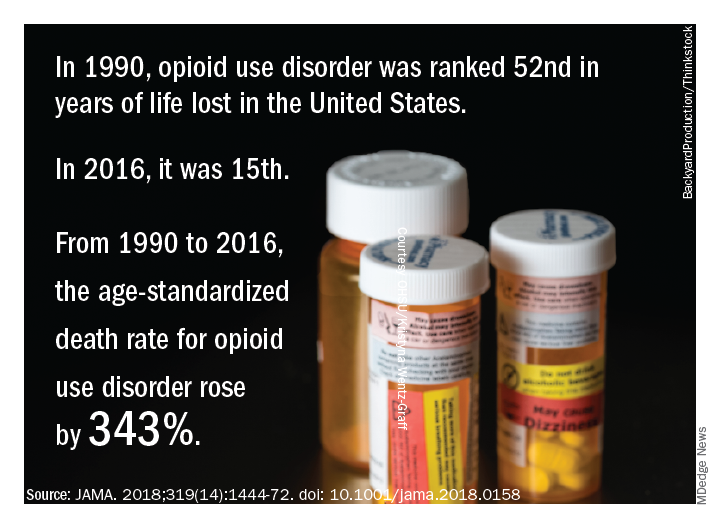
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
FROM JAMA
Key clinical point: While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors.
Major finding: Life expectancy ranged from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, and previously decreasing death rates for adults have reversed in 19 states.
Study details: A U.S. state-level analysis of results from the Global Burden of Disease (GBD) study illustrating trends in diseases, injuries, risk factors, and deaths from 1990 to 2016.
Disclosures: The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Study authors reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
Source: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-1472.