User login
Is acetaminophen really safer than NSAIDs in heart disease?
New research calls into question the assumption that acetaminophen is safer than NSAIDs for patients with known cardiovascular disease (CVD) or CVD risk factors.
The analysis found a significant correlation between the use of acetaminophen and elevated systolic blood pressure.
While acetaminophen may still be safer than NSAIDs from a bleeding risk standpoint, or in patients with known kidney disease, “the gap may not be as large as once thought,” Rahul Gupta, MD, cardiologist with Lehigh Valley Health Network, Allentown, Pa., said in an interview.
“Cautious use is recommended over the long term, especially in patients with pre-existing hypertension or cardiovascular risk factors,” Dr. Gupta said.
The study was presented at the Hypertension Scientific Sessions, San Diego, sponsored by the American Heart Association.
Acetaminophen is one of the most widely used over-the-counter medications, as it is considered a safer medication for long-term use since it lacks the anti-inflammatory effects of NSAIDs, Dr. Gupta explained.
NSAIDs have been known to raise blood pressure, but the effect of acetaminophen in this regard has not been well studied. Observational studies have shown contradictory results in terms of its effect on blood pressure, he noted.
To investigate further, Dr. Gupta and colleagues did a meta-analysis of three studies that compared the effect of acetaminophen (3-4 g/day) versus placebo on systolic and diastolic ambulatory blood pressure in patients with heart disease or hypertension. Together, the studies included 172 adults (mean age, 60 years; 73% male).
They found that patients receiving acetaminophen had significantly higher systolic blood pressure, compared with those receiving placebo (standard mean difference [SMD] = 0.35; 95% confidence interval, 0.08-0.63; P = .01).
Subgroup analysis of the effect on hypertensive patients showed significant change in systolic blood pressure as well (SMD = 0.38; 95% CI, 0.05-0.71; P = .02).
“Interestingly, there was no significant difference in the effect on diastolic blood pressure,” Dr. Gupta commented.
Reached for comment, Timothy S. Anderson, MD, clinical investigator in the Division of General Medicine at Beth Israel Deaconess Medical Center and assistant professor of medicine at the Harvard Medical School, both in Boston, said this is “an interesting and not particularly well-known issue.”
“However, most of the trials look at very high doses of acetaminophen use (for example, six to eight of the 500 mg pills each day) so we don’t really know whether the more common patterns of using one to two acetaminophen pills every once in a while is problematic,” Dr. Anderson told this news organization.
“We also don’t have data showing a direct harm from these medications with regards to strokes or heart attacks or other downstream consequences of high blood pressure. Ideally we would need a head-to-head trial comparing ibuprofen-type medications to acetaminophen-type medications,” Dr. Anderson said.
The study had no specific funding. Dr. Gupta and Dr. Anderson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
New research calls into question the assumption that acetaminophen is safer than NSAIDs for patients with known cardiovascular disease (CVD) or CVD risk factors.
The analysis found a significant correlation between the use of acetaminophen and elevated systolic blood pressure.
While acetaminophen may still be safer than NSAIDs from a bleeding risk standpoint, or in patients with known kidney disease, “the gap may not be as large as once thought,” Rahul Gupta, MD, cardiologist with Lehigh Valley Health Network, Allentown, Pa., said in an interview.
“Cautious use is recommended over the long term, especially in patients with pre-existing hypertension or cardiovascular risk factors,” Dr. Gupta said.
The study was presented at the Hypertension Scientific Sessions, San Diego, sponsored by the American Heart Association.
Acetaminophen is one of the most widely used over-the-counter medications, as it is considered a safer medication for long-term use since it lacks the anti-inflammatory effects of NSAIDs, Dr. Gupta explained.
NSAIDs have been known to raise blood pressure, but the effect of acetaminophen in this regard has not been well studied. Observational studies have shown contradictory results in terms of its effect on blood pressure, he noted.
To investigate further, Dr. Gupta and colleagues did a meta-analysis of three studies that compared the effect of acetaminophen (3-4 g/day) versus placebo on systolic and diastolic ambulatory blood pressure in patients with heart disease or hypertension. Together, the studies included 172 adults (mean age, 60 years; 73% male).
They found that patients receiving acetaminophen had significantly higher systolic blood pressure, compared with those receiving placebo (standard mean difference [SMD] = 0.35; 95% confidence interval, 0.08-0.63; P = .01).
Subgroup analysis of the effect on hypertensive patients showed significant change in systolic blood pressure as well (SMD = 0.38; 95% CI, 0.05-0.71; P = .02).
“Interestingly, there was no significant difference in the effect on diastolic blood pressure,” Dr. Gupta commented.
Reached for comment, Timothy S. Anderson, MD, clinical investigator in the Division of General Medicine at Beth Israel Deaconess Medical Center and assistant professor of medicine at the Harvard Medical School, both in Boston, said this is “an interesting and not particularly well-known issue.”
“However, most of the trials look at very high doses of acetaminophen use (for example, six to eight of the 500 mg pills each day) so we don’t really know whether the more common patterns of using one to two acetaminophen pills every once in a while is problematic,” Dr. Anderson told this news organization.
“We also don’t have data showing a direct harm from these medications with regards to strokes or heart attacks or other downstream consequences of high blood pressure. Ideally we would need a head-to-head trial comparing ibuprofen-type medications to acetaminophen-type medications,” Dr. Anderson said.
The study had no specific funding. Dr. Gupta and Dr. Anderson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
New research calls into question the assumption that acetaminophen is safer than NSAIDs for patients with known cardiovascular disease (CVD) or CVD risk factors.
The analysis found a significant correlation between the use of acetaminophen and elevated systolic blood pressure.
While acetaminophen may still be safer than NSAIDs from a bleeding risk standpoint, or in patients with known kidney disease, “the gap may not be as large as once thought,” Rahul Gupta, MD, cardiologist with Lehigh Valley Health Network, Allentown, Pa., said in an interview.
“Cautious use is recommended over the long term, especially in patients with pre-existing hypertension or cardiovascular risk factors,” Dr. Gupta said.
The study was presented at the Hypertension Scientific Sessions, San Diego, sponsored by the American Heart Association.
Acetaminophen is one of the most widely used over-the-counter medications, as it is considered a safer medication for long-term use since it lacks the anti-inflammatory effects of NSAIDs, Dr. Gupta explained.
NSAIDs have been known to raise blood pressure, but the effect of acetaminophen in this regard has not been well studied. Observational studies have shown contradictory results in terms of its effect on blood pressure, he noted.
To investigate further, Dr. Gupta and colleagues did a meta-analysis of three studies that compared the effect of acetaminophen (3-4 g/day) versus placebo on systolic and diastolic ambulatory blood pressure in patients with heart disease or hypertension. Together, the studies included 172 adults (mean age, 60 years; 73% male).
They found that patients receiving acetaminophen had significantly higher systolic blood pressure, compared with those receiving placebo (standard mean difference [SMD] = 0.35; 95% confidence interval, 0.08-0.63; P = .01).
Subgroup analysis of the effect on hypertensive patients showed significant change in systolic blood pressure as well (SMD = 0.38; 95% CI, 0.05-0.71; P = .02).
“Interestingly, there was no significant difference in the effect on diastolic blood pressure,” Dr. Gupta commented.
Reached for comment, Timothy S. Anderson, MD, clinical investigator in the Division of General Medicine at Beth Israel Deaconess Medical Center and assistant professor of medicine at the Harvard Medical School, both in Boston, said this is “an interesting and not particularly well-known issue.”
“However, most of the trials look at very high doses of acetaminophen use (for example, six to eight of the 500 mg pills each day) so we don’t really know whether the more common patterns of using one to two acetaminophen pills every once in a while is problematic,” Dr. Anderson told this news organization.
“We also don’t have data showing a direct harm from these medications with regards to strokes or heart attacks or other downstream consequences of high blood pressure. Ideally we would need a head-to-head trial comparing ibuprofen-type medications to acetaminophen-type medications,” Dr. Anderson said.
The study had no specific funding. Dr. Gupta and Dr. Anderson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION 2022
Home BP monitoring in older adults falls short of recommendations
Just over 51% of older hypertensive adults regularly check their own blood pressure, compared with 48% of those with blood pressure–related health conditions (BPHCs), based on a 2021 survey of individuals aged 50-80 years.
“Guidelines recommend that patients use self-measured blood pressure monitoring (SBPM) outside the clinic to diagnose and manage hypertension,” but just 61% of respondents with a BPHC and 68% of those with hypertension said that they had received such a recommendation from a physician, nurse, or other health care professional, Melanie V. Springer, MD, and associates said in JAMA Network Open.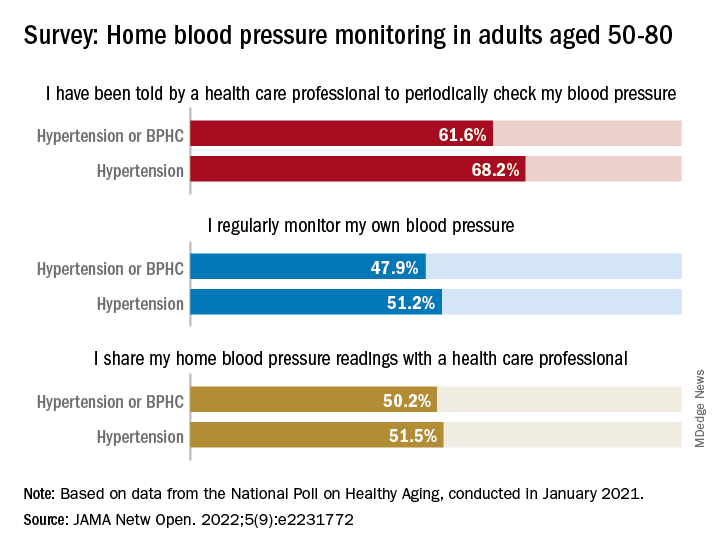
The prevalence of regular monitoring among those with hypertension, 51.2%, does, however, compare favorably with an earlier study showing that 43% of adults aged 18 and older regularly monitored their BP in 2005 and 2008, “which is perhaps associated with our sample’s older age,” said Dr. Springer and associates of the University of Michigan, Ann Arbor.
The current study, they noted, is the first to report “SBPM prevalence in adults ages 50 to 80 years with hypertension or BPHCs, who have a higher risk of adverse outcomes from uncontrolled BP than younger adults.” The analysis is based on data from the National Poll on Healthy Aging, conducted by the University of Michigan in January 2021 and completed by 2,023 individuals.
The frequency of home monitoring varied among adults with BPHCs, as just under 15% reported daily checks and the largest proportion, about 28%, used their device one to three times per month. The results of home monitoring were shared with health care professionals by 50.2% of respondents with a BPHC and by 51.5% of those with hypertension, they said in the research letter.
Home monitoring’s less-than-universal recommendation by providers and use by patients “suggest that protocols should be developed to educate patients about the importance of SBPM and sharing readings with clinicians and the frequency that SBPM should be performed,” Dr. Springer and associates wrote.
The study was funded by AARP, Michigan Medicine, the National Institute of Neurological Disorders and Stroke, and the Department of Veterans Affairs. One investigator has received consulting fees or honoraria from SeeChange Health, HealthMine, the Kaiser Permanente Washington Health Research Institute, the Robert Wood Johnson Foundation, AbilTo, Kansas City Area Life Sciences Institute, American Diabetes Association, Donaghue Foundation, and Luxembourg National Research Fund.
Just over 51% of older hypertensive adults regularly check their own blood pressure, compared with 48% of those with blood pressure–related health conditions (BPHCs), based on a 2021 survey of individuals aged 50-80 years.
“Guidelines recommend that patients use self-measured blood pressure monitoring (SBPM) outside the clinic to diagnose and manage hypertension,” but just 61% of respondents with a BPHC and 68% of those with hypertension said that they had received such a recommendation from a physician, nurse, or other health care professional, Melanie V. Springer, MD, and associates said in JAMA Network Open.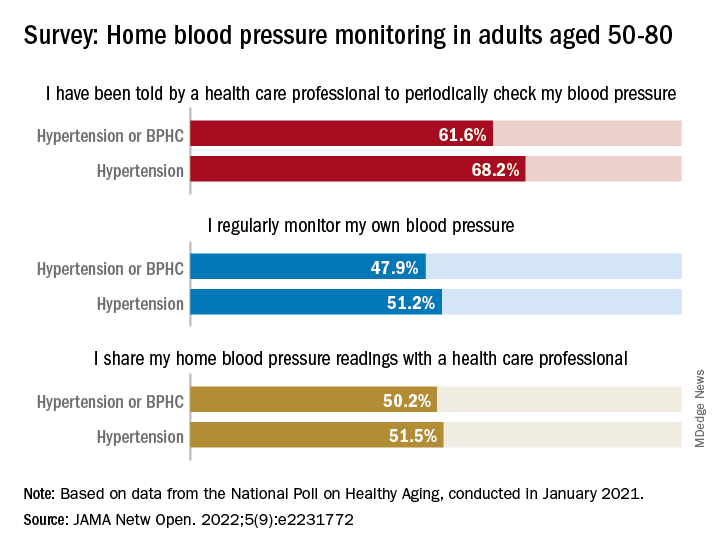
The prevalence of regular monitoring among those with hypertension, 51.2%, does, however, compare favorably with an earlier study showing that 43% of adults aged 18 and older regularly monitored their BP in 2005 and 2008, “which is perhaps associated with our sample’s older age,” said Dr. Springer and associates of the University of Michigan, Ann Arbor.
The current study, they noted, is the first to report “SBPM prevalence in adults ages 50 to 80 years with hypertension or BPHCs, who have a higher risk of adverse outcomes from uncontrolled BP than younger adults.” The analysis is based on data from the National Poll on Healthy Aging, conducted by the University of Michigan in January 2021 and completed by 2,023 individuals.
The frequency of home monitoring varied among adults with BPHCs, as just under 15% reported daily checks and the largest proportion, about 28%, used their device one to three times per month. The results of home monitoring were shared with health care professionals by 50.2% of respondents with a BPHC and by 51.5% of those with hypertension, they said in the research letter.
Home monitoring’s less-than-universal recommendation by providers and use by patients “suggest that protocols should be developed to educate patients about the importance of SBPM and sharing readings with clinicians and the frequency that SBPM should be performed,” Dr. Springer and associates wrote.
The study was funded by AARP, Michigan Medicine, the National Institute of Neurological Disorders and Stroke, and the Department of Veterans Affairs. One investigator has received consulting fees or honoraria from SeeChange Health, HealthMine, the Kaiser Permanente Washington Health Research Institute, the Robert Wood Johnson Foundation, AbilTo, Kansas City Area Life Sciences Institute, American Diabetes Association, Donaghue Foundation, and Luxembourg National Research Fund.
Just over 51% of older hypertensive adults regularly check their own blood pressure, compared with 48% of those with blood pressure–related health conditions (BPHCs), based on a 2021 survey of individuals aged 50-80 years.
“Guidelines recommend that patients use self-measured blood pressure monitoring (SBPM) outside the clinic to diagnose and manage hypertension,” but just 61% of respondents with a BPHC and 68% of those with hypertension said that they had received such a recommendation from a physician, nurse, or other health care professional, Melanie V. Springer, MD, and associates said in JAMA Network Open.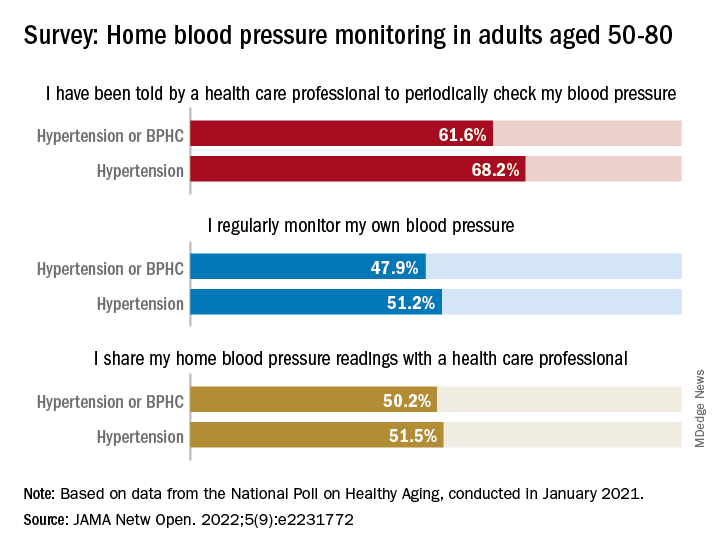
The prevalence of regular monitoring among those with hypertension, 51.2%, does, however, compare favorably with an earlier study showing that 43% of adults aged 18 and older regularly monitored their BP in 2005 and 2008, “which is perhaps associated with our sample’s older age,” said Dr. Springer and associates of the University of Michigan, Ann Arbor.
The current study, they noted, is the first to report “SBPM prevalence in adults ages 50 to 80 years with hypertension or BPHCs, who have a higher risk of adverse outcomes from uncontrolled BP than younger adults.” The analysis is based on data from the National Poll on Healthy Aging, conducted by the University of Michigan in January 2021 and completed by 2,023 individuals.
The frequency of home monitoring varied among adults with BPHCs, as just under 15% reported daily checks and the largest proportion, about 28%, used their device one to three times per month. The results of home monitoring were shared with health care professionals by 50.2% of respondents with a BPHC and by 51.5% of those with hypertension, they said in the research letter.
Home monitoring’s less-than-universal recommendation by providers and use by patients “suggest that protocols should be developed to educate patients about the importance of SBPM and sharing readings with clinicians and the frequency that SBPM should be performed,” Dr. Springer and associates wrote.
The study was funded by AARP, Michigan Medicine, the National Institute of Neurological Disorders and Stroke, and the Department of Veterans Affairs. One investigator has received consulting fees or honoraria from SeeChange Health, HealthMine, the Kaiser Permanente Washington Health Research Institute, the Robert Wood Johnson Foundation, AbilTo, Kansas City Area Life Sciences Institute, American Diabetes Association, Donaghue Foundation, and Luxembourg National Research Fund.
FROM JAMA NETWORK OPEN
Continuous cuffless monitoring may fuel lifestyle change to lower BP
Wearing a cuffless device on the wrist to continuously monitor blood pressure was associated with a significantly lower systolic BP at 6 months among hypertensive adults, real-world results from Europe show.
“We don’t know what they did to reduce their blood pressure,” Jay Shah, MD, Division of Cardiology, Mayo Clinic Arizona, Phoenix, told this news organization.
“The idea is that because they were exposed to their data on a continual basis, that may have prompted them to do something that led to an improvement in their blood pressure, whether it be exercise more, go to their doctor, or change their medication,” said Dr. Shah, who is also chief medical officer for Aktiia.
Dr. Shah presented the study at the Hypertension Scientific Sessions, San Diego.
Empowering data
The study used the Aktiia 24/7 BP monitor; Atkiia funded the trial. The monitor passively and continually monitors BP values from photoplethysmography signals collected via optical sensors at the wrist.
After initial individualized calibration using a cuff-based reference, BP measurements are displayed on a smartphone app, allowing users to consistently monitor their own BP for long periods of time.
Aktiia received CE mark in Europe in January 2021 and is currently under review by the U.S. Food and Drug Administration.
Dr. Shah and colleagues analyzed systolic BP (SBP) trends among 838 real-world Aktiia users in Europe (age 57 ± 11 years; 14% women) who consistently used the monitor for 6 months.
Altogether, they had data on 375 (± 287) app interactions, 3,646 (± 1,417) cuffless readings per user, and 9 (± 7) cuff readings per user.
Traditional cuff SBP averages were calculated monthly and compared with the SBP average of the first month. A t-test analysis was used to detect the difference in SBP between the first and successive months.
On the basis of the mean SBP calculated over 6 months, 136 participants were hypertensive (SBP > 140 mm Hg) and the rest had SBP less than 140 mm Hg.
Hypertensive users saw a statistically significant reduction in SBP of –3.2 mm Hg (95% CI, –0.70 to –5.59; P < .02), beginning at 3 months of continual cuffless BP monitoring, which was sustained through 6 months.
Among users with SBP less than 140 mm Hg, the mean SBP remained unchanged.
“The magnitude of improvement might look modest, but even a 5 mm Hg reduction in systolic BP correlates to a 10% decrease in cardiovascular risk,” Dr. Shah told this news organization.
He noted that “one of the major hurdles is that people may not be aware they have high blood pressure because they don’t feel it. And with a regular cuff, they’ll only see that number when they actually check their blood pressure, which is extremely rare, even for people who have hypertension.”
“Having the ability to show someone their continual blood pressure picture really empowers them to do something to make changes and to be aware, [as well as] to be a more active participant in their health,” Dr. Shah said.
He said that a good analogy is diabetes management, which has transitioned from single finger-stick glucose monitoring to continuous glucose monitoring that provides a complete 24/7 picture of glucose levels.
Transforming technology
Offering perspective on the study, Harlan Krumholz, MD, SM, with Yale New Haven Hospital and Yale School of Medicine, New Haven, Conn., said that having an accurate, affordable, unobtrusive cuffless continuous BP monitor would “transform” BP management.
“This could unlock an era of precision BP management with empowerment of patients to view and act on their numbers,” Dr. Krumholz said in an interview.
“We need data to be confident in the devices – and then research to best leverage the streams of information – and strategies to optimize its use in practice,” Dr. Krumholz added.
“Like any new innovation, we need to mitigate risks and monitor for unintended adverse consequences, but I am bullish on the future of cuffless continuous BP monitors,” Dr. Krumholz said.
Dr. Krumholz said that he “applauds Aktiia for doing studies that assess the effect of the information they are producing on BP over time. We need to know that new approaches not only generate valid information but that they can improve health.”
Ready for prime time?
In June, the European Society of Hypertension issued a statement noting that cuffless BP measurement is a fast-growing and promising field with considerable potential for improving hypertension awareness, management, and control, but because the accuracy of these new devices has not yet been validated, they are not yet suitable for clinical use.
Also providing perspective, Stephen Juraschek, MD, PhD, research director, Hypertension Center of Excellence at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston, said that “there is a lot of interest in cuffless BP monitors due to their ease of measurement, comfort, and ability to obtain BP measurements in multiple settings and environments, and this study showed that the monitoring improved BP over time.”
“It is believed that the increased awareness and feedback may promote healthier behaviors aimed at lowering BP. However, this result should not be conflated with the accuracy of these monitors,” Dr. Juraschek cautioned.
He also noted that there is still no formally approved validation protocol by the Association for the Advancement of Medical Instrumentation.
“While a number of cuffless devices are cleared by the FDA through its 510k mechanism (that is, demonstration of device equivalence), there is no formal stamp of approval or attestation that the measurements are accurate,” Dr. Juraschek said in an interview.
In his view, “more work is needed to understand the validity of these devices. For now, validated, cuff-based home devices are recommended for BP measurement at home, while further work is done to determine the accuracy of these cuffless technologies.”
The study was funded by Aktiia. Dr. Shah is an employee of the company. Dr. Krumholz has no relevant disclosures. Dr. Juraschek is a member of the Validate BP review committee and the AAMI sphygmomanometer committee.
A version of this article first appeared on Medscape.com.
Wearing a cuffless device on the wrist to continuously monitor blood pressure was associated with a significantly lower systolic BP at 6 months among hypertensive adults, real-world results from Europe show.
“We don’t know what they did to reduce their blood pressure,” Jay Shah, MD, Division of Cardiology, Mayo Clinic Arizona, Phoenix, told this news organization.
“The idea is that because they were exposed to their data on a continual basis, that may have prompted them to do something that led to an improvement in their blood pressure, whether it be exercise more, go to their doctor, or change their medication,” said Dr. Shah, who is also chief medical officer for Aktiia.
Dr. Shah presented the study at the Hypertension Scientific Sessions, San Diego.
Empowering data
The study used the Aktiia 24/7 BP monitor; Atkiia funded the trial. The monitor passively and continually monitors BP values from photoplethysmography signals collected via optical sensors at the wrist.
After initial individualized calibration using a cuff-based reference, BP measurements are displayed on a smartphone app, allowing users to consistently monitor their own BP for long periods of time.
Aktiia received CE mark in Europe in January 2021 and is currently under review by the U.S. Food and Drug Administration.
Dr. Shah and colleagues analyzed systolic BP (SBP) trends among 838 real-world Aktiia users in Europe (age 57 ± 11 years; 14% women) who consistently used the monitor for 6 months.
Altogether, they had data on 375 (± 287) app interactions, 3,646 (± 1,417) cuffless readings per user, and 9 (± 7) cuff readings per user.
Traditional cuff SBP averages were calculated monthly and compared with the SBP average of the first month. A t-test analysis was used to detect the difference in SBP between the first and successive months.
On the basis of the mean SBP calculated over 6 months, 136 participants were hypertensive (SBP > 140 mm Hg) and the rest had SBP less than 140 mm Hg.
Hypertensive users saw a statistically significant reduction in SBP of –3.2 mm Hg (95% CI, –0.70 to –5.59; P < .02), beginning at 3 months of continual cuffless BP monitoring, which was sustained through 6 months.
Among users with SBP less than 140 mm Hg, the mean SBP remained unchanged.
“The magnitude of improvement might look modest, but even a 5 mm Hg reduction in systolic BP correlates to a 10% decrease in cardiovascular risk,” Dr. Shah told this news organization.
He noted that “one of the major hurdles is that people may not be aware they have high blood pressure because they don’t feel it. And with a regular cuff, they’ll only see that number when they actually check their blood pressure, which is extremely rare, even for people who have hypertension.”
“Having the ability to show someone their continual blood pressure picture really empowers them to do something to make changes and to be aware, [as well as] to be a more active participant in their health,” Dr. Shah said.
He said that a good analogy is diabetes management, which has transitioned from single finger-stick glucose monitoring to continuous glucose monitoring that provides a complete 24/7 picture of glucose levels.
Transforming technology
Offering perspective on the study, Harlan Krumholz, MD, SM, with Yale New Haven Hospital and Yale School of Medicine, New Haven, Conn., said that having an accurate, affordable, unobtrusive cuffless continuous BP monitor would “transform” BP management.
“This could unlock an era of precision BP management with empowerment of patients to view and act on their numbers,” Dr. Krumholz said in an interview.
“We need data to be confident in the devices – and then research to best leverage the streams of information – and strategies to optimize its use in practice,” Dr. Krumholz added.
“Like any new innovation, we need to mitigate risks and monitor for unintended adverse consequences, but I am bullish on the future of cuffless continuous BP monitors,” Dr. Krumholz said.
Dr. Krumholz said that he “applauds Aktiia for doing studies that assess the effect of the information they are producing on BP over time. We need to know that new approaches not only generate valid information but that they can improve health.”
Ready for prime time?
In June, the European Society of Hypertension issued a statement noting that cuffless BP measurement is a fast-growing and promising field with considerable potential for improving hypertension awareness, management, and control, but because the accuracy of these new devices has not yet been validated, they are not yet suitable for clinical use.
Also providing perspective, Stephen Juraschek, MD, PhD, research director, Hypertension Center of Excellence at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston, said that “there is a lot of interest in cuffless BP monitors due to their ease of measurement, comfort, and ability to obtain BP measurements in multiple settings and environments, and this study showed that the monitoring improved BP over time.”
“It is believed that the increased awareness and feedback may promote healthier behaviors aimed at lowering BP. However, this result should not be conflated with the accuracy of these monitors,” Dr. Juraschek cautioned.
He also noted that there is still no formally approved validation protocol by the Association for the Advancement of Medical Instrumentation.
“While a number of cuffless devices are cleared by the FDA through its 510k mechanism (that is, demonstration of device equivalence), there is no formal stamp of approval or attestation that the measurements are accurate,” Dr. Juraschek said in an interview.
In his view, “more work is needed to understand the validity of these devices. For now, validated, cuff-based home devices are recommended for BP measurement at home, while further work is done to determine the accuracy of these cuffless technologies.”
The study was funded by Aktiia. Dr. Shah is an employee of the company. Dr. Krumholz has no relevant disclosures. Dr. Juraschek is a member of the Validate BP review committee and the AAMI sphygmomanometer committee.
A version of this article first appeared on Medscape.com.
Wearing a cuffless device on the wrist to continuously monitor blood pressure was associated with a significantly lower systolic BP at 6 months among hypertensive adults, real-world results from Europe show.
“We don’t know what they did to reduce their blood pressure,” Jay Shah, MD, Division of Cardiology, Mayo Clinic Arizona, Phoenix, told this news organization.
“The idea is that because they were exposed to their data on a continual basis, that may have prompted them to do something that led to an improvement in their blood pressure, whether it be exercise more, go to their doctor, or change their medication,” said Dr. Shah, who is also chief medical officer for Aktiia.
Dr. Shah presented the study at the Hypertension Scientific Sessions, San Diego.
Empowering data
The study used the Aktiia 24/7 BP monitor; Atkiia funded the trial. The monitor passively and continually monitors BP values from photoplethysmography signals collected via optical sensors at the wrist.
After initial individualized calibration using a cuff-based reference, BP measurements are displayed on a smartphone app, allowing users to consistently monitor their own BP for long periods of time.
Aktiia received CE mark in Europe in January 2021 and is currently under review by the U.S. Food and Drug Administration.
Dr. Shah and colleagues analyzed systolic BP (SBP) trends among 838 real-world Aktiia users in Europe (age 57 ± 11 years; 14% women) who consistently used the monitor for 6 months.
Altogether, they had data on 375 (± 287) app interactions, 3,646 (± 1,417) cuffless readings per user, and 9 (± 7) cuff readings per user.
Traditional cuff SBP averages were calculated monthly and compared with the SBP average of the first month. A t-test analysis was used to detect the difference in SBP between the first and successive months.
On the basis of the mean SBP calculated over 6 months, 136 participants were hypertensive (SBP > 140 mm Hg) and the rest had SBP less than 140 mm Hg.
Hypertensive users saw a statistically significant reduction in SBP of –3.2 mm Hg (95% CI, –0.70 to –5.59; P < .02), beginning at 3 months of continual cuffless BP monitoring, which was sustained through 6 months.
Among users with SBP less than 140 mm Hg, the mean SBP remained unchanged.
“The magnitude of improvement might look modest, but even a 5 mm Hg reduction in systolic BP correlates to a 10% decrease in cardiovascular risk,” Dr. Shah told this news organization.
He noted that “one of the major hurdles is that people may not be aware they have high blood pressure because they don’t feel it. And with a regular cuff, they’ll only see that number when they actually check their blood pressure, which is extremely rare, even for people who have hypertension.”
“Having the ability to show someone their continual blood pressure picture really empowers them to do something to make changes and to be aware, [as well as] to be a more active participant in their health,” Dr. Shah said.
He said that a good analogy is diabetes management, which has transitioned from single finger-stick glucose monitoring to continuous glucose monitoring that provides a complete 24/7 picture of glucose levels.
Transforming technology
Offering perspective on the study, Harlan Krumholz, MD, SM, with Yale New Haven Hospital and Yale School of Medicine, New Haven, Conn., said that having an accurate, affordable, unobtrusive cuffless continuous BP monitor would “transform” BP management.
“This could unlock an era of precision BP management with empowerment of patients to view and act on their numbers,” Dr. Krumholz said in an interview.
“We need data to be confident in the devices – and then research to best leverage the streams of information – and strategies to optimize its use in practice,” Dr. Krumholz added.
“Like any new innovation, we need to mitigate risks and monitor for unintended adverse consequences, but I am bullish on the future of cuffless continuous BP monitors,” Dr. Krumholz said.
Dr. Krumholz said that he “applauds Aktiia for doing studies that assess the effect of the information they are producing on BP over time. We need to know that new approaches not only generate valid information but that they can improve health.”
Ready for prime time?
In June, the European Society of Hypertension issued a statement noting that cuffless BP measurement is a fast-growing and promising field with considerable potential for improving hypertension awareness, management, and control, but because the accuracy of these new devices has not yet been validated, they are not yet suitable for clinical use.
Also providing perspective, Stephen Juraschek, MD, PhD, research director, Hypertension Center of Excellence at Healthcare Associates, Beth Israel Deaconess Medical Center, Boston, said that “there is a lot of interest in cuffless BP monitors due to their ease of measurement, comfort, and ability to obtain BP measurements in multiple settings and environments, and this study showed that the monitoring improved BP over time.”
“It is believed that the increased awareness and feedback may promote healthier behaviors aimed at lowering BP. However, this result should not be conflated with the accuracy of these monitors,” Dr. Juraschek cautioned.
He also noted that there is still no formally approved validation protocol by the Association for the Advancement of Medical Instrumentation.
“While a number of cuffless devices are cleared by the FDA through its 510k mechanism (that is, demonstration of device equivalence), there is no formal stamp of approval or attestation that the measurements are accurate,” Dr. Juraschek said in an interview.
In his view, “more work is needed to understand the validity of these devices. For now, validated, cuff-based home devices are recommended for BP measurement at home, while further work is done to determine the accuracy of these cuffless technologies.”
The study was funded by Aktiia. Dr. Shah is an employee of the company. Dr. Krumholz has no relevant disclosures. Dr. Juraschek is a member of the Validate BP review committee and the AAMI sphygmomanometer committee.
A version of this article first appeared on Medscape.com.
FROM AHA HYPERTENSION 2022
Ultrasonic renal denervation passes 2-month test in uncontrolled HTN: RADIANCE II
Systolic blood pressure went down safely and consistently 2 months after renal denervation achieved by ultrasound ablation in patients with uncontrolled, mild to moderate hypertension (HTN) in a key sham-controlled test of the balloon-equipped catheter.
The BP reductions were significant almost regardless of how they were measured – at home, in the office, during the day, at night, or over 24 hours – and weren’t dependent on baseline BP levels.
The 224-patient RADIANCE II Pivotal Study follows two earlier successful sham-controlled trials that used the same renal denervation catheter in other types of patients with HTN. They were RADIANCE-HTN SOLO, which entered patients with mild to moderate HTN not taking medication, and RADIANCE-HTN TRIO, which included patients with HTN despite fixed-dose, single-pill, triple-antihypertensive therapy.
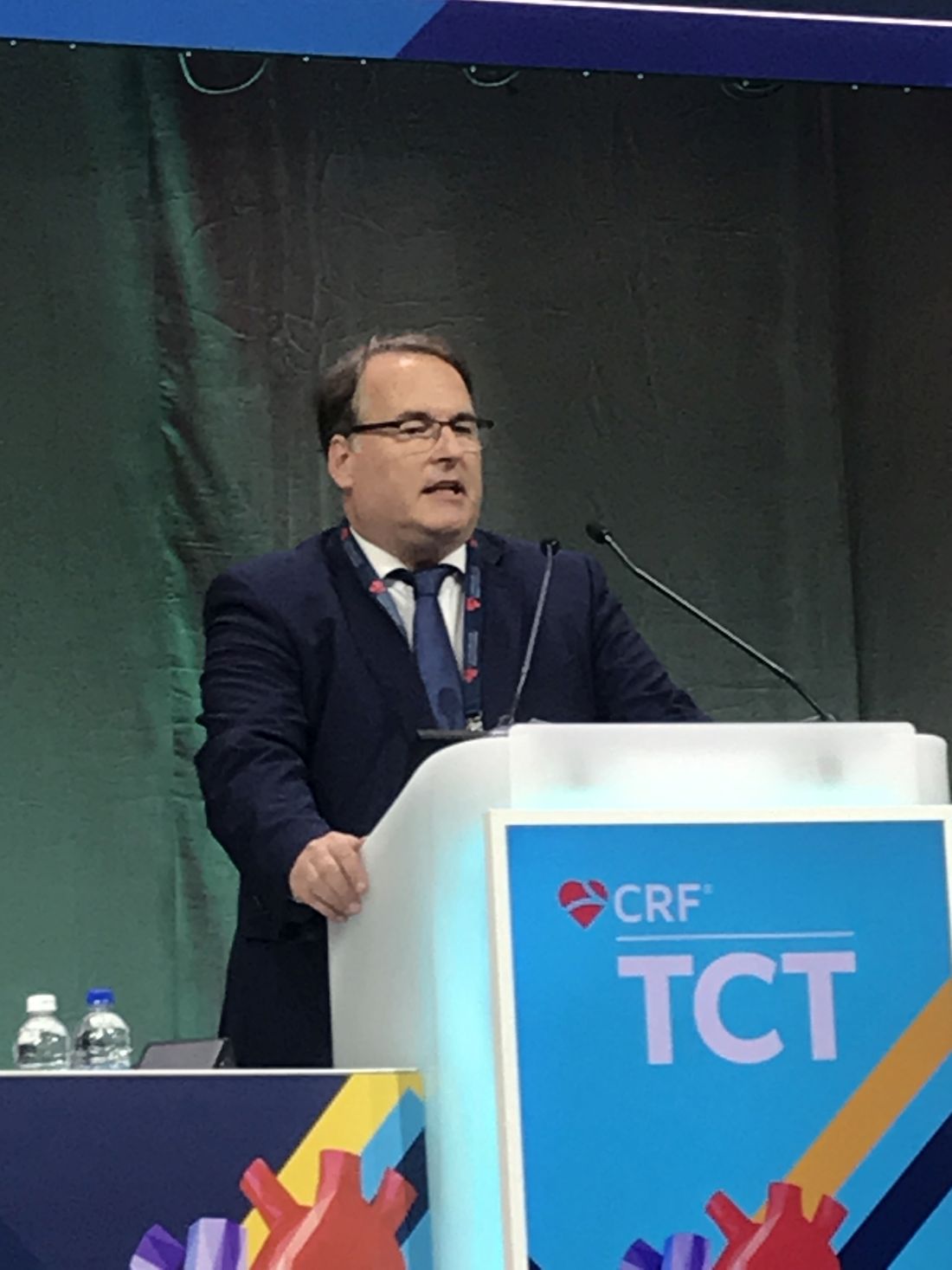
The consistent results of all three trials suggest that the ultrasound renal denervation (uRDN) technique “lowers blood pressure across the spectrum of hypertension,” concluded co–principal investigator Ajay J. Kirtane, MD, SM, Columbia University Irving Medical Center, New York–Presbyterian Hospital, when presenting RADIANCE II at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
RADIANCE II, the largest of the three studies, met its prespecified primary efficacy endpoint of change in daytime ambulatory systolic BP at 2 months by showing a significant 6.3–mm Hg greater reduction in the uRDN group, compared with the sham-control group. There were no major adverse events at 30 days in either group.
The trial was similarly successful for the secondary endpoints of change in systolic BP measured in various other settings, including over 24 hours. Reductions after uRDN averaged 5-7 mm Hg greater than in the control group.
Sparse top-line results of the RADIANCE II pivotal trial were announced in July by the study’s sponsor, ReCor Medical.
Dr. Kirtane stressed in an interview that uRDN and likely any form of HTN renal denervation therapy is not a substitute for standard management. “This is really for patients in whom you’ve made best efforts to do the traditional things – lifestyle modification, medications, all of that – and yet they’re still uncontrolled.” At that point, assuming denervation therapy is available in practice, “it would be something to potentially consider.”
As a panelist after Dr. Kirtane’s formal presentation of RADIANCE II at the conference, Naomi D. Fisher, MD, who was a RADIANCE-HTN TRIO investigator, described how the treatment’s perceived intended patient population evolved over time.
“We all began with the idea that we were going to treat patients with resistant hypertension, that was going to be the first target. We have learned that those patients are far fewer than we thought,” said Dr. Fisher, who directs the hypertension service at Brigham and Women’s Hospital, Boston.
Initial estimates were that such patients with the resistant form, “meaning they require more than three drugs to control their blood pressure,” would represent 15%-20% of patients with HTN.
“We learned from our TRIO data that if you give these patients one single combined pill, lo and behold, many of them become controlled,” she said. “There is so much nonadherence out there in the world, about 50% of our patients aren’t taking their pills. It’s a hard and true fact.”
Exclude patients who aren’t adherent and “our true resistance population becomes minuscule. So, I don’t think that’s going to be the main population” for renal denervation therapy.
More likely, she said, it would be “patients who are uncontrolled and unable to take their medications. So that is going to include nonadherence, intolerance. It’s a very large category of patients. And the priorities can be stacked in favor of those who have higher cardiovascular risk.”
RADIANCE II can show the persistence of uRDN’s BP-lowering effect only out to 2 months so far, but the effect’s durability based on the RADIANCE program’s combined experience appears to be at least 2 years, Dr. Kirtane said in an interview.
“The RADIANCE II pivotal trial is a powerful, well-designed study attesting to the efficacy of renal denervation in BP lowering,” Franz H. Messerli, MD, Swiss Cardiovascular Center, University Hospital Bern, said in an interview.
The trial “shows the well-known unpredictability of antihypertensive response. We cannot predict who responds to renal denervation and who does not, and who even has a paradoxical increase in BP,” Dr. Messerli, an international hypertension expert not associated with the trial, said in an interview.
“As long as we cannot predict the antihypertensive response to renal denervation therapy, potential synergism/antagonism with drug therapy remains an educated guess,” he said.
“Hypertension is a disease that lasts years and decades. As impressive as RADIANCE II’s 2-month snapshot is, I look forward to similar or better BP data 12 and 24 months after renal denervation,” Dr. Messerli added.
RADIANCE II entered patients with mild to moderate uncontrolled HTN, that is, a systolic BP at least 140/90 mm Hg and less than 180/120 mm Hg, who were receiving no more than two antihypertensive medications. They could have no history of cardiovascular or cerebrovascular events or uncontrolled diabetes, and their estimated glomerular filtration rate (eGFR) had to be at least 40 mL/min per 1.73 m2.
After a 4-week drug washout period, patients who were clinically stable with an ambulatory BP of at least 135/85 mm Hg and less than 170/105 mm Hg underwent CT and renal angiography. Then, the 224 patients still anatomically eligible for the procedure were randomly assigned 2:1 to uRDN or a sham-control procedure: 150 and 74 patients, respectively.
At 2 months, daytime ambulatory systolic BP on average fell 7.9 mm Hg in the uRDN group and 1.8 mm Hg in the sham-control group, for a drop that was steeper by 6.3 mm Hg (P < .0001) after uRDN.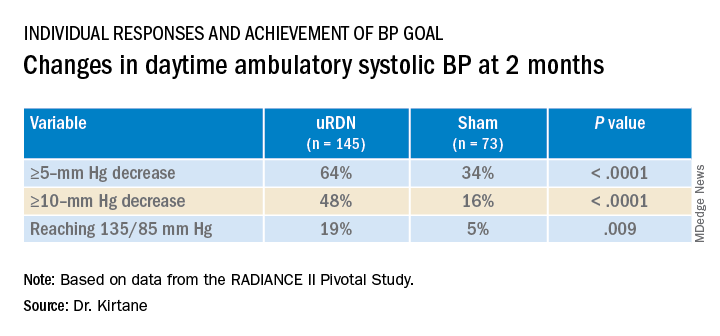
Also in the uRDN group, there was a 6.2–mm Hg larger decrease in 24-hour ambulatory systolic BP (P < .0001), a 5.8–mm Hg greater decline in nighttime ambulatory systolic BP (P < .0004), a 7.6–mm Hg steeper drop in mean home systolic BP (P < .0001), and 5.4 mm Hg more of a decrease in office-based systolic BP (P = .0035).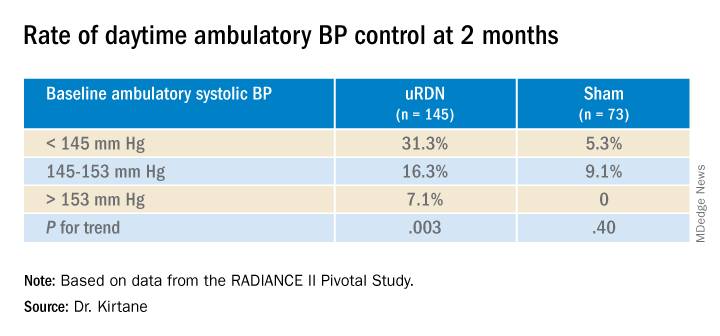
No significant differences were seen in subgroup analyses by sex, age, higher versus lower baseline systolic pressures, high versus low baseline eGFR, degree of abdominal obesity, U.S. versus European site, or whether patients entered before or during the COVID pandemic
Regulators have been accepting change in systolic BP as a surrogate for clinical endpoints in trials of antihypertensive therapy, whether pharmacologic or interventional, under consideration for approval. “That’s why safety endpoints are important to investigate” in these clinical trials, especially for invasive therapies like renal denervation, Dr. Kirtane observed.
That said, “in the longer-term follow-ups of the renal denervation therapies that are out there, including this one, there does not appear to be an appreciable decline in glomerular filtration rate, or any adverse safety signals that we see to date,” Dr. Kirtane said in an interview. “But we know that these are low-frequency events, so we have to be very vigilant, and we can’t get complacent about it.”
In RADIANCE II, there were zero adverse events within 30 days in both groups; the endpoint included death, new myocardial infarction, renal artery complications requiring invasive intervention, and hospitalization for major cardiovascular or hemodynamic-related events. Nor were there instances of new-onset renal artery stenosis greater than 70% documented by imaging at 6 months.
The ReCor uRDN catheter uses ultrasound energy to disrupt renal nerve signaling, a technology thought to deliver safer “burns,” compared with other renal denervation catheter technologies. It features an axially stabilizing balloon that transmits ultrasound energy – two to three sonications, each lasting 7 seconds, Dr. Kirtane said – outward through the arterial wall. The design is intended to ensure consistently circumferential ablation. Circulating saline within the balloon, Kirtane noted, directly cools the adjacent vessel wall to help it avoid thermal damage.
Dr. Kirtane reported receiving institutional funding from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CSI, Philips, ReCor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, Shockwave Medical, and Merck; consulting for IMDS; and receiving travel and meal expenses from Medtronic, Boston Scientific, Abbott Vascular, CSI, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron. Dr. Fisher disclosed receiving honoraria or fees for consulting or serving on a speaker’s bureau for Medtronic, ReCor Medical, and Aktiia and receiving grant support or holding research contracts for Recor Medical and Aktiia. Dr. Messerli disclosed receiving honoraria from Medtronic, Menarini, Krka, and Ipca.
A version of this article first appeared on Medscape.com.
Systolic blood pressure went down safely and consistently 2 months after renal denervation achieved by ultrasound ablation in patients with uncontrolled, mild to moderate hypertension (HTN) in a key sham-controlled test of the balloon-equipped catheter.
The BP reductions were significant almost regardless of how they were measured – at home, in the office, during the day, at night, or over 24 hours – and weren’t dependent on baseline BP levels.
The 224-patient RADIANCE II Pivotal Study follows two earlier successful sham-controlled trials that used the same renal denervation catheter in other types of patients with HTN. They were RADIANCE-HTN SOLO, which entered patients with mild to moderate HTN not taking medication, and RADIANCE-HTN TRIO, which included patients with HTN despite fixed-dose, single-pill, triple-antihypertensive therapy.
The consistent results of all three trials suggest that the ultrasound renal denervation (uRDN) technique “lowers blood pressure across the spectrum of hypertension,” concluded co–principal investigator Ajay J. Kirtane, MD, SM, Columbia University Irving Medical Center, New York–Presbyterian Hospital, when presenting RADIANCE II at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
RADIANCE II, the largest of the three studies, met its prespecified primary efficacy endpoint of change in daytime ambulatory systolic BP at 2 months by showing a significant 6.3–mm Hg greater reduction in the uRDN group, compared with the sham-control group. There were no major adverse events at 30 days in either group.
The trial was similarly successful for the secondary endpoints of change in systolic BP measured in various other settings, including over 24 hours. Reductions after uRDN averaged 5-7 mm Hg greater than in the control group.
Sparse top-line results of the RADIANCE II pivotal trial were announced in July by the study’s sponsor, ReCor Medical.
Dr. Kirtane stressed in an interview that uRDN and likely any form of HTN renal denervation therapy is not a substitute for standard management. “This is really for patients in whom you’ve made best efforts to do the traditional things – lifestyle modification, medications, all of that – and yet they’re still uncontrolled.” At that point, assuming denervation therapy is available in practice, “it would be something to potentially consider.”
As a panelist after Dr. Kirtane’s formal presentation of RADIANCE II at the conference, Naomi D. Fisher, MD, who was a RADIANCE-HTN TRIO investigator, described how the treatment’s perceived intended patient population evolved over time.
“We all began with the idea that we were going to treat patients with resistant hypertension, that was going to be the first target. We have learned that those patients are far fewer than we thought,” said Dr. Fisher, who directs the hypertension service at Brigham and Women’s Hospital, Boston.
Initial estimates were that such patients with the resistant form, “meaning they require more than three drugs to control their blood pressure,” would represent 15%-20% of patients with HTN.
“We learned from our TRIO data that if you give these patients one single combined pill, lo and behold, many of them become controlled,” she said. “There is so much nonadherence out there in the world, about 50% of our patients aren’t taking their pills. It’s a hard and true fact.”
Exclude patients who aren’t adherent and “our true resistance population becomes minuscule. So, I don’t think that’s going to be the main population” for renal denervation therapy.
More likely, she said, it would be “patients who are uncontrolled and unable to take their medications. So that is going to include nonadherence, intolerance. It’s a very large category of patients. And the priorities can be stacked in favor of those who have higher cardiovascular risk.”
RADIANCE II can show the persistence of uRDN’s BP-lowering effect only out to 2 months so far, but the effect’s durability based on the RADIANCE program’s combined experience appears to be at least 2 years, Dr. Kirtane said in an interview.
“The RADIANCE II pivotal trial is a powerful, well-designed study attesting to the efficacy of renal denervation in BP lowering,” Franz H. Messerli, MD, Swiss Cardiovascular Center, University Hospital Bern, said in an interview.
The trial “shows the well-known unpredictability of antihypertensive response. We cannot predict who responds to renal denervation and who does not, and who even has a paradoxical increase in BP,” Dr. Messerli, an international hypertension expert not associated with the trial, said in an interview.
“As long as we cannot predict the antihypertensive response to renal denervation therapy, potential synergism/antagonism with drug therapy remains an educated guess,” he said.
“Hypertension is a disease that lasts years and decades. As impressive as RADIANCE II’s 2-month snapshot is, I look forward to similar or better BP data 12 and 24 months after renal denervation,” Dr. Messerli added.
RADIANCE II entered patients with mild to moderate uncontrolled HTN, that is, a systolic BP at least 140/90 mm Hg and less than 180/120 mm Hg, who were receiving no more than two antihypertensive medications. They could have no history of cardiovascular or cerebrovascular events or uncontrolled diabetes, and their estimated glomerular filtration rate (eGFR) had to be at least 40 mL/min per 1.73 m2.
After a 4-week drug washout period, patients who were clinically stable with an ambulatory BP of at least 135/85 mm Hg and less than 170/105 mm Hg underwent CT and renal angiography. Then, the 224 patients still anatomically eligible for the procedure were randomly assigned 2:1 to uRDN or a sham-control procedure: 150 and 74 patients, respectively.
At 2 months, daytime ambulatory systolic BP on average fell 7.9 mm Hg in the uRDN group and 1.8 mm Hg in the sham-control group, for a drop that was steeper by 6.3 mm Hg (P < .0001) after uRDN.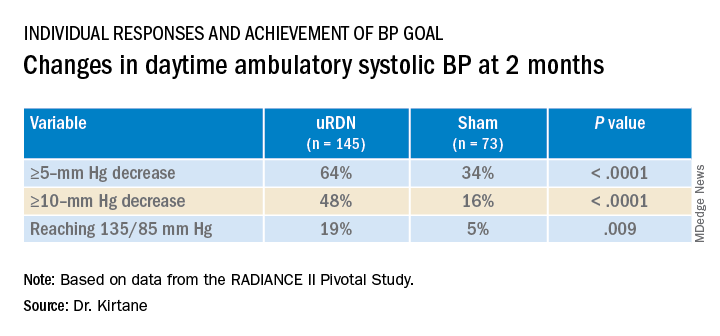
Also in the uRDN group, there was a 6.2–mm Hg larger decrease in 24-hour ambulatory systolic BP (P < .0001), a 5.8–mm Hg greater decline in nighttime ambulatory systolic BP (P < .0004), a 7.6–mm Hg steeper drop in mean home systolic BP (P < .0001), and 5.4 mm Hg more of a decrease in office-based systolic BP (P = .0035).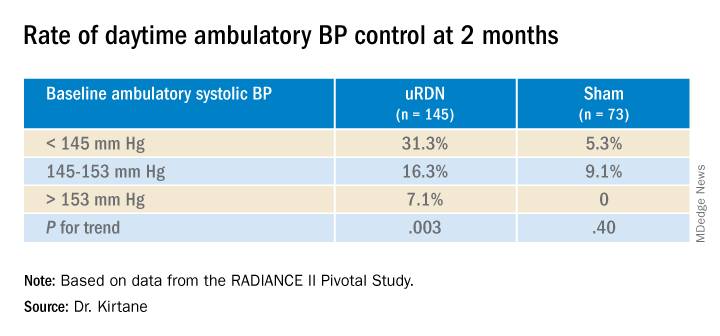
No significant differences were seen in subgroup analyses by sex, age, higher versus lower baseline systolic pressures, high versus low baseline eGFR, degree of abdominal obesity, U.S. versus European site, or whether patients entered before or during the COVID pandemic
Regulators have been accepting change in systolic BP as a surrogate for clinical endpoints in trials of antihypertensive therapy, whether pharmacologic or interventional, under consideration for approval. “That’s why safety endpoints are important to investigate” in these clinical trials, especially for invasive therapies like renal denervation, Dr. Kirtane observed.
That said, “in the longer-term follow-ups of the renal denervation therapies that are out there, including this one, there does not appear to be an appreciable decline in glomerular filtration rate, or any adverse safety signals that we see to date,” Dr. Kirtane said in an interview. “But we know that these are low-frequency events, so we have to be very vigilant, and we can’t get complacent about it.”
In RADIANCE II, there were zero adverse events within 30 days in both groups; the endpoint included death, new myocardial infarction, renal artery complications requiring invasive intervention, and hospitalization for major cardiovascular or hemodynamic-related events. Nor were there instances of new-onset renal artery stenosis greater than 70% documented by imaging at 6 months.
The ReCor uRDN catheter uses ultrasound energy to disrupt renal nerve signaling, a technology thought to deliver safer “burns,” compared with other renal denervation catheter technologies. It features an axially stabilizing balloon that transmits ultrasound energy – two to three sonications, each lasting 7 seconds, Dr. Kirtane said – outward through the arterial wall. The design is intended to ensure consistently circumferential ablation. Circulating saline within the balloon, Kirtane noted, directly cools the adjacent vessel wall to help it avoid thermal damage.
Dr. Kirtane reported receiving institutional funding from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CSI, Philips, ReCor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, Shockwave Medical, and Merck; consulting for IMDS; and receiving travel and meal expenses from Medtronic, Boston Scientific, Abbott Vascular, CSI, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron. Dr. Fisher disclosed receiving honoraria or fees for consulting or serving on a speaker’s bureau for Medtronic, ReCor Medical, and Aktiia and receiving grant support or holding research contracts for Recor Medical and Aktiia. Dr. Messerli disclosed receiving honoraria from Medtronic, Menarini, Krka, and Ipca.
A version of this article first appeared on Medscape.com.
Systolic blood pressure went down safely and consistently 2 months after renal denervation achieved by ultrasound ablation in patients with uncontrolled, mild to moderate hypertension (HTN) in a key sham-controlled test of the balloon-equipped catheter.
The BP reductions were significant almost regardless of how they were measured – at home, in the office, during the day, at night, or over 24 hours – and weren’t dependent on baseline BP levels.
The 224-patient RADIANCE II Pivotal Study follows two earlier successful sham-controlled trials that used the same renal denervation catheter in other types of patients with HTN. They were RADIANCE-HTN SOLO, which entered patients with mild to moderate HTN not taking medication, and RADIANCE-HTN TRIO, which included patients with HTN despite fixed-dose, single-pill, triple-antihypertensive therapy.
The consistent results of all three trials suggest that the ultrasound renal denervation (uRDN) technique “lowers blood pressure across the spectrum of hypertension,” concluded co–principal investigator Ajay J. Kirtane, MD, SM, Columbia University Irving Medical Center, New York–Presbyterian Hospital, when presenting RADIANCE II at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
RADIANCE II, the largest of the three studies, met its prespecified primary efficacy endpoint of change in daytime ambulatory systolic BP at 2 months by showing a significant 6.3–mm Hg greater reduction in the uRDN group, compared with the sham-control group. There were no major adverse events at 30 days in either group.
The trial was similarly successful for the secondary endpoints of change in systolic BP measured in various other settings, including over 24 hours. Reductions after uRDN averaged 5-7 mm Hg greater than in the control group.
Sparse top-line results of the RADIANCE II pivotal trial were announced in July by the study’s sponsor, ReCor Medical.
Dr. Kirtane stressed in an interview that uRDN and likely any form of HTN renal denervation therapy is not a substitute for standard management. “This is really for patients in whom you’ve made best efforts to do the traditional things – lifestyle modification, medications, all of that – and yet they’re still uncontrolled.” At that point, assuming denervation therapy is available in practice, “it would be something to potentially consider.”
As a panelist after Dr. Kirtane’s formal presentation of RADIANCE II at the conference, Naomi D. Fisher, MD, who was a RADIANCE-HTN TRIO investigator, described how the treatment’s perceived intended patient population evolved over time.
“We all began with the idea that we were going to treat patients with resistant hypertension, that was going to be the first target. We have learned that those patients are far fewer than we thought,” said Dr. Fisher, who directs the hypertension service at Brigham and Women’s Hospital, Boston.
Initial estimates were that such patients with the resistant form, “meaning they require more than three drugs to control their blood pressure,” would represent 15%-20% of patients with HTN.
“We learned from our TRIO data that if you give these patients one single combined pill, lo and behold, many of them become controlled,” she said. “There is so much nonadherence out there in the world, about 50% of our patients aren’t taking their pills. It’s a hard and true fact.”
Exclude patients who aren’t adherent and “our true resistance population becomes minuscule. So, I don’t think that’s going to be the main population” for renal denervation therapy.
More likely, she said, it would be “patients who are uncontrolled and unable to take their medications. So that is going to include nonadherence, intolerance. It’s a very large category of patients. And the priorities can be stacked in favor of those who have higher cardiovascular risk.”
RADIANCE II can show the persistence of uRDN’s BP-lowering effect only out to 2 months so far, but the effect’s durability based on the RADIANCE program’s combined experience appears to be at least 2 years, Dr. Kirtane said in an interview.
“The RADIANCE II pivotal trial is a powerful, well-designed study attesting to the efficacy of renal denervation in BP lowering,” Franz H. Messerli, MD, Swiss Cardiovascular Center, University Hospital Bern, said in an interview.
The trial “shows the well-known unpredictability of antihypertensive response. We cannot predict who responds to renal denervation and who does not, and who even has a paradoxical increase in BP,” Dr. Messerli, an international hypertension expert not associated with the trial, said in an interview.
“As long as we cannot predict the antihypertensive response to renal denervation therapy, potential synergism/antagonism with drug therapy remains an educated guess,” he said.
“Hypertension is a disease that lasts years and decades. As impressive as RADIANCE II’s 2-month snapshot is, I look forward to similar or better BP data 12 and 24 months after renal denervation,” Dr. Messerli added.
RADIANCE II entered patients with mild to moderate uncontrolled HTN, that is, a systolic BP at least 140/90 mm Hg and less than 180/120 mm Hg, who were receiving no more than two antihypertensive medications. They could have no history of cardiovascular or cerebrovascular events or uncontrolled diabetes, and their estimated glomerular filtration rate (eGFR) had to be at least 40 mL/min per 1.73 m2.
After a 4-week drug washout period, patients who were clinically stable with an ambulatory BP of at least 135/85 mm Hg and less than 170/105 mm Hg underwent CT and renal angiography. Then, the 224 patients still anatomically eligible for the procedure were randomly assigned 2:1 to uRDN or a sham-control procedure: 150 and 74 patients, respectively.
At 2 months, daytime ambulatory systolic BP on average fell 7.9 mm Hg in the uRDN group and 1.8 mm Hg in the sham-control group, for a drop that was steeper by 6.3 mm Hg (P < .0001) after uRDN.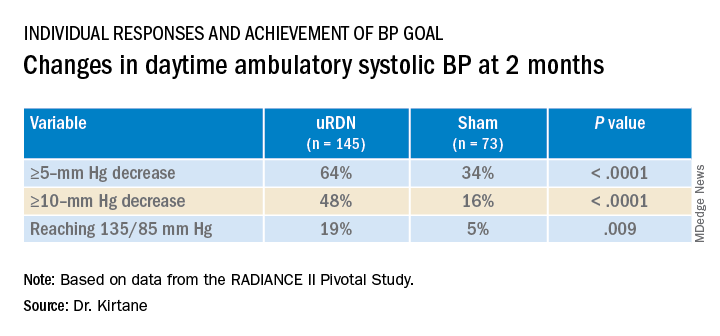
Also in the uRDN group, there was a 6.2–mm Hg larger decrease in 24-hour ambulatory systolic BP (P < .0001), a 5.8–mm Hg greater decline in nighttime ambulatory systolic BP (P < .0004), a 7.6–mm Hg steeper drop in mean home systolic BP (P < .0001), and 5.4 mm Hg more of a decrease in office-based systolic BP (P = .0035).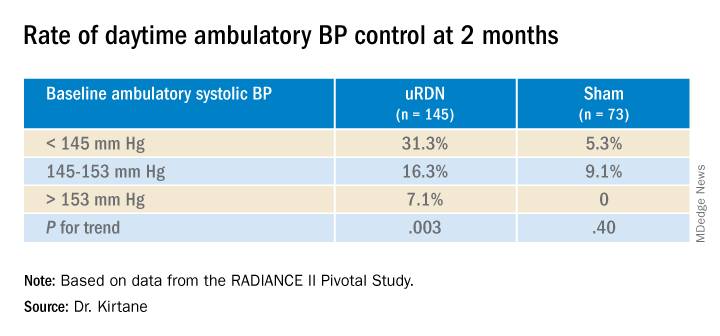
No significant differences were seen in subgroup analyses by sex, age, higher versus lower baseline systolic pressures, high versus low baseline eGFR, degree of abdominal obesity, U.S. versus European site, or whether patients entered before or during the COVID pandemic
Regulators have been accepting change in systolic BP as a surrogate for clinical endpoints in trials of antihypertensive therapy, whether pharmacologic or interventional, under consideration for approval. “That’s why safety endpoints are important to investigate” in these clinical trials, especially for invasive therapies like renal denervation, Dr. Kirtane observed.
That said, “in the longer-term follow-ups of the renal denervation therapies that are out there, including this one, there does not appear to be an appreciable decline in glomerular filtration rate, or any adverse safety signals that we see to date,” Dr. Kirtane said in an interview. “But we know that these are low-frequency events, so we have to be very vigilant, and we can’t get complacent about it.”
In RADIANCE II, there were zero adverse events within 30 days in both groups; the endpoint included death, new myocardial infarction, renal artery complications requiring invasive intervention, and hospitalization for major cardiovascular or hemodynamic-related events. Nor were there instances of new-onset renal artery stenosis greater than 70% documented by imaging at 6 months.
The ReCor uRDN catheter uses ultrasound energy to disrupt renal nerve signaling, a technology thought to deliver safer “burns,” compared with other renal denervation catheter technologies. It features an axially stabilizing balloon that transmits ultrasound energy – two to three sonications, each lasting 7 seconds, Dr. Kirtane said – outward through the arterial wall. The design is intended to ensure consistently circumferential ablation. Circulating saline within the balloon, Kirtane noted, directly cools the adjacent vessel wall to help it avoid thermal damage.
Dr. Kirtane reported receiving institutional funding from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CSI, Philips, ReCor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, Shockwave Medical, and Merck; consulting for IMDS; and receiving travel and meal expenses from Medtronic, Boston Scientific, Abbott Vascular, CSI, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron. Dr. Fisher disclosed receiving honoraria or fees for consulting or serving on a speaker’s bureau for Medtronic, ReCor Medical, and Aktiia and receiving grant support or holding research contracts for Recor Medical and Aktiia. Dr. Messerli disclosed receiving honoraria from Medtronic, Menarini, Krka, and Ipca.
A version of this article first appeared on Medscape.com.
FROM TCT 2022
Fourth-gen transcatheter mitral valve shows clinical, procedural improvements
The design improvements introduced in the fourth-generation device for transcatheter mitral valve repair, called the MitraClip G4 (Abbott), appears to yield better outcomes than previous iterations, according to a multinational postapproval study with more than 1,000 patients.
Not least, the 1.3% all-cause mortality at 30 days in this series, called EXPAND G4, “is the lowest that has been reported to date,” reported Ralph Stephan von Bardeleben, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
The evidence of relative advantages was based on comparisons with historical data and a similar study of the previous-generation device. That previous study, called EXPAND, evaluated the MitraClip NTR and ETR systems.
Device times shorter with new device
“There were shorter device times with MitraClip G4,” said Dr. von Bardeleben, referring to a more than 10-minute advantage over the previous generation device (35 minutes in EXPAND G4 vs. 46 min in EXPAND). Although the reduction in overall median procedure time was more modest (77 vs. 80 minutes), Dr. von Bardeleben said these are “the shortest device and procedural times reported to date.”
He also reported what appeared to be incremental advantages across multiple other endpoints, such as procedural success (96.2% vs. 95.8%) and a reduction in the mean clip rate (1.4 vs. 1.5).
Compared with historical outcomes with other devices employed in transcatheter edge-to-edge repair (TEER) of mitral valves, Dr. von Bardeleben contended that the results support the premise that the MitraClip G4 system is a meaningful advance by incorporating such features as an expanded choice of clip sizes, a greater coaptation area, and a more advanced gripper actuation for leaflet grasping.
Over 90% achieve MR 1+
Not least, it appears to increase the proportion of patients who achieve a mitral regurgitation grade of 1+ (MR1+) or lower, which is increasingly recognized as the goal of TEER, said Dr. von Bardeleben, head of the Centre of Structure Heart Disease Interventions, Heart Valve Centre, Mainz, Germany.
He said the rates of 91% achieving MR1+ or less and 98% achieved 2+ or lower compare favorably with most other series and exceeds levels achieved with surgery.
Dr. von Bardeleben also contended that, because of its design features, the MitraClip G4 “expands the spectrum of TEER-suitable patients.” He noted that 5% of the patients in this real-world series had a high risk of stenosis owing to such issues as severe annular or leaflet calcification and another 5% had factors that would predict inadequate MR reduction, such as Barlow’s disease, bi-leaflet prolapse, and severe leaflet degeneration.
The 1,164 patients in EXPAND G4 were enrolled from sites in the United States, Europe, Canada, and Japan. For the key outcome measure of procedural success, echocardiograms were assessed by an independent core laboratory. Of the 1,164 patients enrolled, 1,044 (91%) had complete follow-up data at 30 days.
The procedural success rates were reflected in improvements in New York Heart Association (NYHA) functional classes and in the Kansas City Cardiomyopathy Questionnaire (KCCQ), a quality of life instrument. Prior to treatment, 69% were in NYHA class III or greater. Following treatment, the proportion was 17% (P < .0001). The 18-point improvement in the KCCQ was characterized by Dr. von Bardeleben as “both clinically and statistically significant [P < .0001].”
There were no strokes in this series, and the 30-day incidence of myocardial infarction was 0.2%. The proportion requiring cardiovascular surgery within 30 days was less than 1%. The rate of bleeding episodes, all of which were nonserious, was 7%.
The “EXPAND G4 study confirms the safety and effectiveness of the next generation MitraClip G4 system,” according to Dr. von Bardeleben, and it did so “in a contemporary real-world setting.”
Outcome data characterized as ‘excellent’
Several invited panelists participating in a discussion following the presentation agreed.
“These results are excellent,” said Raj Makkar, MD, associate director of interventional technologies at Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles. While he was impressed with the fact that only 2% missed the primary endpoint of MR 2+ or lower, he indicated that the 91% achieving MR 1+ or lower might be an even more apt signal that newer-generation devices are improving.
This was echoed by other panelists who appeared to form a general consensus over the premise that the target in TEER should no longer be MR 2+ for most patients.
“We should now be aiming for MR grade of 0-1,” stated panelist Stephan Windecker, MD, chairman, department of cardiology, University of Bern (Switzerland). He indicated that this goal is increasingly reasonable given the advances in device design and greater operator experience.
Dr. von Bardeleben reported financial relationships with Abbott Vascular, Edwards Lifesciences, Medtronic, and Neochord. Dr. Makkar reported financial relationships with Abbott Vascular, Cordis, Edwards Lifesciences, and Medtronic. Dr. Windecker reported financial relationships with more than 30 pharmaceutical companies, including Abbott Vascular, which manufactures MitraClip G4.
The design improvements introduced in the fourth-generation device for transcatheter mitral valve repair, called the MitraClip G4 (Abbott), appears to yield better outcomes than previous iterations, according to a multinational postapproval study with more than 1,000 patients.
Not least, the 1.3% all-cause mortality at 30 days in this series, called EXPAND G4, “is the lowest that has been reported to date,” reported Ralph Stephan von Bardeleben, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
The evidence of relative advantages was based on comparisons with historical data and a similar study of the previous-generation device. That previous study, called EXPAND, evaluated the MitraClip NTR and ETR systems.
Device times shorter with new device
“There were shorter device times with MitraClip G4,” said Dr. von Bardeleben, referring to a more than 10-minute advantage over the previous generation device (35 minutes in EXPAND G4 vs. 46 min in EXPAND). Although the reduction in overall median procedure time was more modest (77 vs. 80 minutes), Dr. von Bardeleben said these are “the shortest device and procedural times reported to date.”
He also reported what appeared to be incremental advantages across multiple other endpoints, such as procedural success (96.2% vs. 95.8%) and a reduction in the mean clip rate (1.4 vs. 1.5).
Compared with historical outcomes with other devices employed in transcatheter edge-to-edge repair (TEER) of mitral valves, Dr. von Bardeleben contended that the results support the premise that the MitraClip G4 system is a meaningful advance by incorporating such features as an expanded choice of clip sizes, a greater coaptation area, and a more advanced gripper actuation for leaflet grasping.
Over 90% achieve MR 1+
Not least, it appears to increase the proportion of patients who achieve a mitral regurgitation grade of 1+ (MR1+) or lower, which is increasingly recognized as the goal of TEER, said Dr. von Bardeleben, head of the Centre of Structure Heart Disease Interventions, Heart Valve Centre, Mainz, Germany.
He said the rates of 91% achieving MR1+ or less and 98% achieved 2+ or lower compare favorably with most other series and exceeds levels achieved with surgery.
Dr. von Bardeleben also contended that, because of its design features, the MitraClip G4 “expands the spectrum of TEER-suitable patients.” He noted that 5% of the patients in this real-world series had a high risk of stenosis owing to such issues as severe annular or leaflet calcification and another 5% had factors that would predict inadequate MR reduction, such as Barlow’s disease, bi-leaflet prolapse, and severe leaflet degeneration.
The 1,164 patients in EXPAND G4 were enrolled from sites in the United States, Europe, Canada, and Japan. For the key outcome measure of procedural success, echocardiograms were assessed by an independent core laboratory. Of the 1,164 patients enrolled, 1,044 (91%) had complete follow-up data at 30 days.
The procedural success rates were reflected in improvements in New York Heart Association (NYHA) functional classes and in the Kansas City Cardiomyopathy Questionnaire (KCCQ), a quality of life instrument. Prior to treatment, 69% were in NYHA class III or greater. Following treatment, the proportion was 17% (P < .0001). The 18-point improvement in the KCCQ was characterized by Dr. von Bardeleben as “both clinically and statistically significant [P < .0001].”
There were no strokes in this series, and the 30-day incidence of myocardial infarction was 0.2%. The proportion requiring cardiovascular surgery within 30 days was less than 1%. The rate of bleeding episodes, all of which were nonserious, was 7%.
The “EXPAND G4 study confirms the safety and effectiveness of the next generation MitraClip G4 system,” according to Dr. von Bardeleben, and it did so “in a contemporary real-world setting.”
Outcome data characterized as ‘excellent’
Several invited panelists participating in a discussion following the presentation agreed.
“These results are excellent,” said Raj Makkar, MD, associate director of interventional technologies at Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles. While he was impressed with the fact that only 2% missed the primary endpoint of MR 2+ or lower, he indicated that the 91% achieving MR 1+ or lower might be an even more apt signal that newer-generation devices are improving.
This was echoed by other panelists who appeared to form a general consensus over the premise that the target in TEER should no longer be MR 2+ for most patients.
“We should now be aiming for MR grade of 0-1,” stated panelist Stephan Windecker, MD, chairman, department of cardiology, University of Bern (Switzerland). He indicated that this goal is increasingly reasonable given the advances in device design and greater operator experience.
Dr. von Bardeleben reported financial relationships with Abbott Vascular, Edwards Lifesciences, Medtronic, and Neochord. Dr. Makkar reported financial relationships with Abbott Vascular, Cordis, Edwards Lifesciences, and Medtronic. Dr. Windecker reported financial relationships with more than 30 pharmaceutical companies, including Abbott Vascular, which manufactures MitraClip G4.
The design improvements introduced in the fourth-generation device for transcatheter mitral valve repair, called the MitraClip G4 (Abbott), appears to yield better outcomes than previous iterations, according to a multinational postapproval study with more than 1,000 patients.
Not least, the 1.3% all-cause mortality at 30 days in this series, called EXPAND G4, “is the lowest that has been reported to date,” reported Ralph Stephan von Bardeleben, MD, at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
The evidence of relative advantages was based on comparisons with historical data and a similar study of the previous-generation device. That previous study, called EXPAND, evaluated the MitraClip NTR and ETR systems.
Device times shorter with new device
“There were shorter device times with MitraClip G4,” said Dr. von Bardeleben, referring to a more than 10-minute advantage over the previous generation device (35 minutes in EXPAND G4 vs. 46 min in EXPAND). Although the reduction in overall median procedure time was more modest (77 vs. 80 minutes), Dr. von Bardeleben said these are “the shortest device and procedural times reported to date.”
He also reported what appeared to be incremental advantages across multiple other endpoints, such as procedural success (96.2% vs. 95.8%) and a reduction in the mean clip rate (1.4 vs. 1.5).
Compared with historical outcomes with other devices employed in transcatheter edge-to-edge repair (TEER) of mitral valves, Dr. von Bardeleben contended that the results support the premise that the MitraClip G4 system is a meaningful advance by incorporating such features as an expanded choice of clip sizes, a greater coaptation area, and a more advanced gripper actuation for leaflet grasping.
Over 90% achieve MR 1+
Not least, it appears to increase the proportion of patients who achieve a mitral regurgitation grade of 1+ (MR1+) or lower, which is increasingly recognized as the goal of TEER, said Dr. von Bardeleben, head of the Centre of Structure Heart Disease Interventions, Heart Valve Centre, Mainz, Germany.
He said the rates of 91% achieving MR1+ or less and 98% achieved 2+ or lower compare favorably with most other series and exceeds levels achieved with surgery.
Dr. von Bardeleben also contended that, because of its design features, the MitraClip G4 “expands the spectrum of TEER-suitable patients.” He noted that 5% of the patients in this real-world series had a high risk of stenosis owing to such issues as severe annular or leaflet calcification and another 5% had factors that would predict inadequate MR reduction, such as Barlow’s disease, bi-leaflet prolapse, and severe leaflet degeneration.
The 1,164 patients in EXPAND G4 were enrolled from sites in the United States, Europe, Canada, and Japan. For the key outcome measure of procedural success, echocardiograms were assessed by an independent core laboratory. Of the 1,164 patients enrolled, 1,044 (91%) had complete follow-up data at 30 days.
The procedural success rates were reflected in improvements in New York Heart Association (NYHA) functional classes and in the Kansas City Cardiomyopathy Questionnaire (KCCQ), a quality of life instrument. Prior to treatment, 69% were in NYHA class III or greater. Following treatment, the proportion was 17% (P < .0001). The 18-point improvement in the KCCQ was characterized by Dr. von Bardeleben as “both clinically and statistically significant [P < .0001].”
There were no strokes in this series, and the 30-day incidence of myocardial infarction was 0.2%. The proportion requiring cardiovascular surgery within 30 days was less than 1%. The rate of bleeding episodes, all of which were nonserious, was 7%.
The “EXPAND G4 study confirms the safety and effectiveness of the next generation MitraClip G4 system,” according to Dr. von Bardeleben, and it did so “in a contemporary real-world setting.”
Outcome data characterized as ‘excellent’
Several invited panelists participating in a discussion following the presentation agreed.
“These results are excellent,” said Raj Makkar, MD, associate director of interventional technologies at Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles. While he was impressed with the fact that only 2% missed the primary endpoint of MR 2+ or lower, he indicated that the 91% achieving MR 1+ or lower might be an even more apt signal that newer-generation devices are improving.
This was echoed by other panelists who appeared to form a general consensus over the premise that the target in TEER should no longer be MR 2+ for most patients.
“We should now be aiming for MR grade of 0-1,” stated panelist Stephan Windecker, MD, chairman, department of cardiology, University of Bern (Switzerland). He indicated that this goal is increasingly reasonable given the advances in device design and greater operator experience.
Dr. von Bardeleben reported financial relationships with Abbott Vascular, Edwards Lifesciences, Medtronic, and Neochord. Dr. Makkar reported financial relationships with Abbott Vascular, Cordis, Edwards Lifesciences, and Medtronic. Dr. Windecker reported financial relationships with more than 30 pharmaceutical companies, including Abbott Vascular, which manufactures MitraClip G4.
FROM TCT 2022
Cumulative blood pressure load: A better predictor of CV events?
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
Cumulative systolic blood pressure load, which can be calculated from serial blood pressure measurements, may provide better prediction of major cardiovascular events, compared with traditional blood pressure measures, a new study suggests.
“Our results suggest that cumulative blood pressure load is an independent predictor of cardiovascular events and should be used in future cardiovascular risk prediction algorithms,” the authors, led by Nelson Wang, MD, George Institute for Global Health, Sydney, conclude.
The study was published online in the Journal of the American College of Cardiology.
The researchers explain that the management of hypertension has traditionally centered around blood pressure measurements taken at a single timepoint, with adequate control defined as those measurements being below a predefined target threshold.
However, this approach fails to recognize blood pressure as a continuous measure that fluctuates over time and does not acknowledge that the most recently recorded measurement may not reflect previous blood pressure control.
More recently, studies have defined the time a patient spends below blood pressure target, or TIme at TaRgEt (TITRE), as a novel marker of cardiovascular risk that is independent of mean blood pressure.
Although TITRE has the added advantage of incorporating duration of control, it is unable to characterize the magnitude of blood pressure elevation, the researchers note.
They point out that an optimal measure as a risk factor for cardiovascular disease would account for both the magnitude and duration of elevated blood pressure.
Such a measure is cumulative blood pressure load, defined as the area under the curve (AUC) expressed in units of mm Hg by time.
The only prior study of this measure was small and retrospective and calculated cumulative blood pressure load from ambulatory blood pressure monitoring estimated over a short (24-hour) period.
Therefore, the aim of the current study was to estimate the association between cumulative systolic blood pressure load over a longer period (24 months) and subsequent major cardiovascular events.
To do this, the researchers conducted a post-hoc analysis of 9,338 patients with type 2 diabetes in the ADVANCE-ON study.
Cumulative systolic blood pressure load was defined as the AUC for systolic blood pressure values above 130 mm Hg divided by the AUC for all measured systolic blood pressure values over a 24-month exposure period.
Over a median 7.6 years of follow-up, 1,469 major cardiovascular events, 1,615 deaths, and 660 cardiovascular deaths occurred.
Results showed that each one standard deviation increase in cumulative systolic blood pressure load was associated with a 14% increase in major cardiovascular events, a 13% increase in all-cause mortality, and a 21% increase in cardiovascular death.
Cumulative systolic blood pressure load outperformed mean systolic blood pressure, time-below-target, and visit-to-visit systolic blood pressure variability for the prediction of cardiovascular events and death and also discriminated risk and reclassified more patients’ risk correctly than the other measures.
“Small improvements in risk prediction can have a major impact when scaled up across large high-risk populations. Furthermore, cumulative systolic pressure load may also prove useful to inform the design of future clinical trials,” the researchers say.
Although the present study only assessed cumulative systolic blood pressure load over 24 months, clinicians should recognize the importance of this measure over a lifetime, they note.
“This approach emphasizes the importance of early blood pressure–lowering interventions to reduce the cumulative systolic blood pressure load that each individual experiences over their lifetime,” they conclude.
The researchers suggest that, based on these results, cumulative systolic blood pressure load and visit-to-visit systolic blood pressure variability “should be used in conjunction in future cardiovascular risk prediction algorithms.”
In an accompanying editorial, Donald Lloyd-Jones, MD, Northwestern Feinberg School of Medicine, Chicago, says that before routinely adopting these new measures, several additional questions need to be addressed.
He notes that many patients in the current study already had cardiovascular disease, and it is not known whether the benefit was consistent among those with and without cardiovascular disease. In addition, longer term data using blood pressure measurements in the real-world clinical setting would be desirable, as well as information on whether these new measures add incremental value to existing risk prediction equations.
“Certainly, the next guidelines should reconsider all types of blood pressure measures, and other potential predictors, to optimize risk estimation and identification of patients with greatest net benefit from risk-reducing therapies,” Dr. Lloyd-Jones comments.
“Ultimately, clinicians should leverage as much information on their patients as possible to understand their blood pressure–related cardiovascular risk, to identify those who may be more likely have occult or emerging subclinical target organ damage, and to identify those who may have particular net benefit from earlier or more intensive treatment,” he concludes.
“These opportunities are more readily available with integration of data that allow for visualization of longer-term blood pressure patterns and incorporation of home monitoring and ambulatory monitoring data to monitor out-of-office blood pressure levels and control.”
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Should patients stand for office BP readings?
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests.
Combining three standing and three seated BP measurements in the same visit may lead to a “quicker diagnosis and save people a trip back to the office,” Wanpen Vongpatanasin, MD, professor of internal medicine and director of the hypertension section, cardiology division, UT Southwestern Medical Center, Dallas, said in an interview.
The study was presented at the Hypertension Scientific Sessions, sponsored by the American Heart Association.
Practice changing?
Clinical guidelines recommend office BP be taken in a seated position for most patients.
However, research has suggested that the sensitivity of seated office BP in diagnosing hypertension is about 50%, with high specificity around 90% during a single visit, Dr. Vongpatanasin explained.
At the follow-up visit, however, the second office BP yielded higher sensitivity to 80% but specificity fell to 55%. Nevertheless, the accuracy of standing BP measurements for diagnosing hypertension has not been investigated.
In a cross-sectional study, Dr. Vongpatanasin and colleagues determined the accuracy of both seated and standing BP for diagnosing hypertension in a single visit in 125 healthy adults who had not had a previous diagnosis of hypertension and were not taking any BP medications. The cohort had a mean age of 49 years, 62% were women, and 24% were Black.
During each office visit, seated BP was measured three times, then standing BP was measured three times using an automated and validated device.
Average seated BP was 123/76 mm Hg and average standing BP was 126/80 mm Hg.
Of the 125 participants, 42 (34%) had hypertension, defined as 24-hour ambulatory systolic/diastolic BP (SBP/DBP) of ≥ 125/75 mm Hg.
The sensitivity and specificity of seated SBP for hypertension was 43% and 92%, respectively.
“Interestingly, with standing SBP, sensitivity was improved to 74% and specificity dropped to 65% – which is okay; you will have to confirm a positive test anyway and when screening for a common disease you’d rather have a high sensitivity rather than low sensitivity to pick it up in this case,” Dr. Vongpatanasin said.
The area under receiver operating characteristic curve (AUROC) of standing SBP was significantly higher than seated SBP (Bayes factor [BF] = 11.8) when hypertension was defined as 24-hour SBP ≥ 125 mm Hg.
Similarly, when hypertension was defined as 24-hour DBP ≥ 75 mm Hg or daytime DBP ≥ 80 mm Hg, the AUROC of standing DBP was higher than seated DBP (all BF > 3).
The addition of standing to seated BP improved detection of hypertension compared with seated BP alone based on 24-hour SBP/DBP ≥ 125/75 mm Hg or daytime SBP/DBP ≥ 130/80 mm Hg (all BF > 3).
“In our hypertension clinic, we always measure both seated and standing BP in all of our patients,” John Giacona, PA-C, a PhD candidate at UT Southwestern Medical Center and coauthor of the study, told this news organization,
Multiple readings most important
Reached for comment, Johanna Contreras, MD, a cardiologist at Mount Sinai Hospital in New York, noted that diagnosing hypertension is “difficult” and she agrees that multiple readings are important.
“I usually take at least two readings in two different visits before I tell the patient they have high blood pressure,” Dr. Contreras said in an interview.
Dr. Contreras said she takes blood pressure both seated and standing.
“I’m not sure standing versus seated makes a big difference. However, when the patient first comes into the office, it is really important to let them rest and calm down before taking the blood pressure,” she said.
The study had no commercial funding. The authors and Dr. Contreras have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION 2022
Dietary change tops for reducing CVD risk in stage 1 hypertension
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Healthy lifestyle changes to reduce systolic blood pressure to below 130 mm Hg may prevent 26,000 heart attacks and strokes and reduce health care costs over the next 10 years, a new simulation study suggests.
Among the various lifestyle changes, adopting the Dietary Approaches to Stop Hypertension diet, known as the DASH diet, may have the greatest impact for young and middle-aged adults with stage 1 hypertension.
“This research reveals that we should look to feasible ways our food system could make healthy eating the default option,” Kendra Sims, PhD, MPH, postdoctoral fellow at University of California, San Francisco, told this news organization.
“Above all, it means collaborating with the patient about nourishing choices that fit best into their culture and lifestyle,” Dr. Sims said.
Be proactive
“What is important is that people not wait until they have hypertension to start thinking about healthful diets,” commented Taylor Wallace, PhD, department of nutrition and food studies, George Mason University, Fairfax, Va., who was not involved in the study.
“It’s all about prevention in my mind. Whether you are hypertensive or are perfectly healthy, the DASH diet or any other dietary pattern that emphasizes consumption of fruits, vegetables, whole grains, lean meats, seafood, nuts/seeds, and low/non-fat dairy and decreased intake of saturated fats, added sugars, and sodium is a good idea,” Dr. Wallace said in an interview.
The study was presented at the American Heart Association Hypertension Scientific Sessions 2022 in San Diego.
Dr. Sims and colleagues used U.S. statistics from multiple sources to simulate CVD events, mortality, and health care costs between 2018 and 2027 in adults aged 35-64 years with untreated stage 1 hypertension, defined as systolic BP of 130 to 139 mm Hg.
The researchers estimate that 8.8 million U.S. adults (5.5 million women) aged 35-64 years have untreated stage 1 hypertension and would be recommended for lifestyle change, such as physical activity, weight loss, moderating alcohol intake, and adoption of the DASH diet.
Controlling blood pressure to less than 130 mm Hg in this population could prevent 26,000 CVD events, avoid 2,900 deaths, and lead to $1.6 billion saved in associated health care costs, the researchers calculate.
The largest benefit would come from adoption of the DASH diet, with an estimated 15,000 CVD events prevented among men and 11,000 among women.
Even small changes can help
“Young and middle-aged adults with stage 1 hypertension aren’t as low risk as you – or even your doctor – might think,” Dr. Sims told this news organization.
“Millions of working-aged people are walking around with elevated blood pressure, which is symptomless but is also a leading preventable cause of disability and death. Most do not follow the recommended DASH diet,” Dr. Sims said.
“Unfortunately, the availability and affordability of healthy food sources does not easily allow people to follow the DASH diet,” Dr. Sims adds in a conference news release.
“Clinicians should consider whether their patients live in food deserts or places with limited walkability. Health counseling should include addressing these specific challenges to blood pressure control,” Dr. Sims says.
Dr. Wallace noted that diet changes don’t have to be drastic.
“Honestly, just increasing fruit and vegetable intake has been shown to displace calories from saturated fats, added sugars, and sodium,” he told this news organization.
“It’s hard for people to stick to ‘diets’ long-term, so shifting toward healthier dietary patterns without having to read a book on the DASH diet or count calories and carbs seems like a more practical solution for the general population, although I have no issues with the DASH diet and think it is a great dietary pattern for heart health,” Dr. Wallace said.
The study had no funding. Dr. Sims reports no relevant financial relationships. Dr. Wallace is principal and CEO of Think Healthy Group; chief food and nutrition scientist with Produce for Better Health Foundation; editor, Journal of Dietary Supplements; deputy editor, Journal of the American College of Nutrition; nutrition section editor, Annals of Medicine; and advisory board member with Forbes Health.
A version of this article first appeared on Medscape.com.
Lack of exercise linked to small heart, HFpEF
Chronic lack of exercise – dubbed “exercise deficiency” – is associated with cardiac atrophy, reduced cardiac output and chamber size, and diminished cardiorespiratory fitness (CRF) in a subgroup of patients with heart failure with preserved ejection fraction (HFpEF), researchers say.
Increasing the physical activity levels of these sedentary individuals could be an effective preventive strategy, particularly for those who are younger and middle-aged, they suggest.
Thinking of HFpEF as an exercise deficiency syndrome leading to a small heart “flies in the face of decades of cardiovascular teaching, because traditionally, we’ve thought of heart failure as the big floppy heart,” Andre La Gerche, MBBS, PhD, of the Baker Heart and Diabetes Institute, Melbourne, told this news organization.
“While it is true that some people with HFpEF have thick, stiff hearts, we propose that another subset has a normal heart, except it’s small because it’s been underexercised,” he said.
The article, published online as part of a Focus Seminar series in the Journal of the American College of Cardiology, has “gone viral on social media,” Jason C. Kovacic, MBBS, PhD, of the Victor Chang Cardiac Research Institute, Darlinghurst, Australia, told this news organization.
Dr. Kovacic is a JACC section editor and the coordinating and senior author of the series, which covers other issues surrounding physical activity, both in athletes and the general public.
‘Coin-dropping moment’
To support their hypothesis that HFpEF is an exercise deficiency in certain patients, Dr. La Gerche and colleagues conducted a literature review that highlights the following points:
- There is a strong association between physical activity and both CRF and heart function.
- Exercise deficiency is a major risk factor for HFpEF in a subset of patients.
- Increasing physical activity is associated with greater cardiac mass, stroke volumes, cardiac output, and peak oxygen consumption.
- Physical inactivity leads to loss of heart muscle, reduced output and chamber size, and less ability to improve cardiac performance with exercise.
- Aging results in a smaller, stiffer heart; however, this effect is mitigated by regular exercise.
- Individuals who are sedentary throughout life cannot attenuate age-related reductions in heart size and have increasing chamber stiffness.
“When we explain it, it’s like a coin-dropping moment, because it’s actually a really simple concept,” Dr. La Gerche said. “A small heart has a small stroke volume. A patient with a small heart with a maximal stroke volume of 60 mL can generate a cardiac output of 9 L/min at a heart rate of 150 beats/min during exercise – an output that just isn’t enough. It’s like trying to drive a truck with a 50cc motorbike engine.”
“Plus,” Dr. La Gerche added, “exercise deficiency also sets the stage for comorbidities such as obesity, diabetes, and high blood pressure, all of which can ultimately lead to HFpEF.”
Considering HFpEF as an exercise deficiency syndrome has two clinical implications, Dr. La Gerche said. “First, it helps us understand the condition and diagnose more cases. For example, I think practitioners will start to recognize that breathlessness in some of their patients is associated with a small heart.”
“Second,” he said, “if it’s an exercise deficiency syndrome, the treatment is exercise. For most people, that means exercising regularly before the age of 60 to prevent HFpEF, because studies have found that after the age of 60, the heart is a bit fixed and harder to remodel. That doesn’t mean you shouldn’t try after 60 or that you won’t get benefit. But the real sweet spot is in middle age and younger.”
The bigger picture
The JACC Focus Seminar series starts with an article that underscores the benefits of regular physical activity. “The key is getting our patients to meet the guidelines: 150 to 300 minutes of moderate intensity exercise per week, or 75 to 250 minutes of vigorous activity per week,” Dr. Kovacic emphasized.
“Yes, we can give a statin to lower cholesterol. Yes, we can give a blood pressure medication to lower blood pressure. But when you prescribe exercise, you impact patients’ blood pressure, their cholesterol, their weight, their sense of well-being,” he said. “It cuts across so many different aspects of people’s lives that it’s important to underscore the value of exercise to everybody.”
That includes physicians, he affirmed. “It behooves all physicians to be leading by example. I would encourage those who are overweight or aren’t exercising as much as they should be to make the time to be healthy and to exercise. If you don’t, then bad health will force you to make the time to deal with bad health issues.”
Other articles in the series deal with the athlete’s heart. Christopher Semsarian, MBBS, PhD, MPH, University of Sydney, and colleagues discuss emerging data on hypertrophic cardiomyopathy and other genetic cardiovascular diseases, with the conclusion that it is probably okay for more athletes with these conditions to participate in recreational and competitive sports than was previously thought – another paradigm shift, according to Dr. Kovacic.
The final article addresses some of the challenges and controversies related to the athlete’s heart, including whether extreme exercise is associated with vulnerability to atrial fibrillation and other arrhythmias, and the impact of gender on the cardiac response to exercise, which can’t be determined now because of a paucity of data on women in sports.
Overall, Dr. Kovacic said, the series makes for “compelling” reading that should encourage readers to embark on their own studies to add to the data and support exercise prescription across the board.
No commercial funding or relevant conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Chronic lack of exercise – dubbed “exercise deficiency” – is associated with cardiac atrophy, reduced cardiac output and chamber size, and diminished cardiorespiratory fitness (CRF) in a subgroup of patients with heart failure with preserved ejection fraction (HFpEF), researchers say.
Increasing the physical activity levels of these sedentary individuals could be an effective preventive strategy, particularly for those who are younger and middle-aged, they suggest.
Thinking of HFpEF as an exercise deficiency syndrome leading to a small heart “flies in the face of decades of cardiovascular teaching, because traditionally, we’ve thought of heart failure as the big floppy heart,” Andre La Gerche, MBBS, PhD, of the Baker Heart and Diabetes Institute, Melbourne, told this news organization.
“While it is true that some people with HFpEF have thick, stiff hearts, we propose that another subset has a normal heart, except it’s small because it’s been underexercised,” he said.
The article, published online as part of a Focus Seminar series in the Journal of the American College of Cardiology, has “gone viral on social media,” Jason C. Kovacic, MBBS, PhD, of the Victor Chang Cardiac Research Institute, Darlinghurst, Australia, told this news organization.
Dr. Kovacic is a JACC section editor and the coordinating and senior author of the series, which covers other issues surrounding physical activity, both in athletes and the general public.
‘Coin-dropping moment’
To support their hypothesis that HFpEF is an exercise deficiency in certain patients, Dr. La Gerche and colleagues conducted a literature review that highlights the following points:
- There is a strong association between physical activity and both CRF and heart function.
- Exercise deficiency is a major risk factor for HFpEF in a subset of patients.
- Increasing physical activity is associated with greater cardiac mass, stroke volumes, cardiac output, and peak oxygen consumption.
- Physical inactivity leads to loss of heart muscle, reduced output and chamber size, and less ability to improve cardiac performance with exercise.
- Aging results in a smaller, stiffer heart; however, this effect is mitigated by regular exercise.
- Individuals who are sedentary throughout life cannot attenuate age-related reductions in heart size and have increasing chamber stiffness.
“When we explain it, it’s like a coin-dropping moment, because it’s actually a really simple concept,” Dr. La Gerche said. “A small heart has a small stroke volume. A patient with a small heart with a maximal stroke volume of 60 mL can generate a cardiac output of 9 L/min at a heart rate of 150 beats/min during exercise – an output that just isn’t enough. It’s like trying to drive a truck with a 50cc motorbike engine.”
“Plus,” Dr. La Gerche added, “exercise deficiency also sets the stage for comorbidities such as obesity, diabetes, and high blood pressure, all of which can ultimately lead to HFpEF.”
Considering HFpEF as an exercise deficiency syndrome has two clinical implications, Dr. La Gerche said. “First, it helps us understand the condition and diagnose more cases. For example, I think practitioners will start to recognize that breathlessness in some of their patients is associated with a small heart.”
“Second,” he said, “if it’s an exercise deficiency syndrome, the treatment is exercise. For most people, that means exercising regularly before the age of 60 to prevent HFpEF, because studies have found that after the age of 60, the heart is a bit fixed and harder to remodel. That doesn’t mean you shouldn’t try after 60 or that you won’t get benefit. But the real sweet spot is in middle age and younger.”
The bigger picture
The JACC Focus Seminar series starts with an article that underscores the benefits of regular physical activity. “The key is getting our patients to meet the guidelines: 150 to 300 minutes of moderate intensity exercise per week, or 75 to 250 minutes of vigorous activity per week,” Dr. Kovacic emphasized.
“Yes, we can give a statin to lower cholesterol. Yes, we can give a blood pressure medication to lower blood pressure. But when you prescribe exercise, you impact patients’ blood pressure, their cholesterol, their weight, their sense of well-being,” he said. “It cuts across so many different aspects of people’s lives that it’s important to underscore the value of exercise to everybody.”
That includes physicians, he affirmed. “It behooves all physicians to be leading by example. I would encourage those who are overweight or aren’t exercising as much as they should be to make the time to be healthy and to exercise. If you don’t, then bad health will force you to make the time to deal with bad health issues.”
Other articles in the series deal with the athlete’s heart. Christopher Semsarian, MBBS, PhD, MPH, University of Sydney, and colleagues discuss emerging data on hypertrophic cardiomyopathy and other genetic cardiovascular diseases, with the conclusion that it is probably okay for more athletes with these conditions to participate in recreational and competitive sports than was previously thought – another paradigm shift, according to Dr. Kovacic.
The final article addresses some of the challenges and controversies related to the athlete’s heart, including whether extreme exercise is associated with vulnerability to atrial fibrillation and other arrhythmias, and the impact of gender on the cardiac response to exercise, which can’t be determined now because of a paucity of data on women in sports.
Overall, Dr. Kovacic said, the series makes for “compelling” reading that should encourage readers to embark on their own studies to add to the data and support exercise prescription across the board.
No commercial funding or relevant conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Chronic lack of exercise – dubbed “exercise deficiency” – is associated with cardiac atrophy, reduced cardiac output and chamber size, and diminished cardiorespiratory fitness (CRF) in a subgroup of patients with heart failure with preserved ejection fraction (HFpEF), researchers say.
Increasing the physical activity levels of these sedentary individuals could be an effective preventive strategy, particularly for those who are younger and middle-aged, they suggest.
Thinking of HFpEF as an exercise deficiency syndrome leading to a small heart “flies in the face of decades of cardiovascular teaching, because traditionally, we’ve thought of heart failure as the big floppy heart,” Andre La Gerche, MBBS, PhD, of the Baker Heart and Diabetes Institute, Melbourne, told this news organization.
“While it is true that some people with HFpEF have thick, stiff hearts, we propose that another subset has a normal heart, except it’s small because it’s been underexercised,” he said.
The article, published online as part of a Focus Seminar series in the Journal of the American College of Cardiology, has “gone viral on social media,” Jason C. Kovacic, MBBS, PhD, of the Victor Chang Cardiac Research Institute, Darlinghurst, Australia, told this news organization.
Dr. Kovacic is a JACC section editor and the coordinating and senior author of the series, which covers other issues surrounding physical activity, both in athletes and the general public.
‘Coin-dropping moment’
To support their hypothesis that HFpEF is an exercise deficiency in certain patients, Dr. La Gerche and colleagues conducted a literature review that highlights the following points:
- There is a strong association between physical activity and both CRF and heart function.
- Exercise deficiency is a major risk factor for HFpEF in a subset of patients.
- Increasing physical activity is associated with greater cardiac mass, stroke volumes, cardiac output, and peak oxygen consumption.
- Physical inactivity leads to loss of heart muscle, reduced output and chamber size, and less ability to improve cardiac performance with exercise.
- Aging results in a smaller, stiffer heart; however, this effect is mitigated by regular exercise.
- Individuals who are sedentary throughout life cannot attenuate age-related reductions in heart size and have increasing chamber stiffness.
“When we explain it, it’s like a coin-dropping moment, because it’s actually a really simple concept,” Dr. La Gerche said. “A small heart has a small stroke volume. A patient with a small heart with a maximal stroke volume of 60 mL can generate a cardiac output of 9 L/min at a heart rate of 150 beats/min during exercise – an output that just isn’t enough. It’s like trying to drive a truck with a 50cc motorbike engine.”
“Plus,” Dr. La Gerche added, “exercise deficiency also sets the stage for comorbidities such as obesity, diabetes, and high blood pressure, all of which can ultimately lead to HFpEF.”
Considering HFpEF as an exercise deficiency syndrome has two clinical implications, Dr. La Gerche said. “First, it helps us understand the condition and diagnose more cases. For example, I think practitioners will start to recognize that breathlessness in some of their patients is associated with a small heart.”
“Second,” he said, “if it’s an exercise deficiency syndrome, the treatment is exercise. For most people, that means exercising regularly before the age of 60 to prevent HFpEF, because studies have found that after the age of 60, the heart is a bit fixed and harder to remodel. That doesn’t mean you shouldn’t try after 60 or that you won’t get benefit. But the real sweet spot is in middle age and younger.”
The bigger picture
The JACC Focus Seminar series starts with an article that underscores the benefits of regular physical activity. “The key is getting our patients to meet the guidelines: 150 to 300 minutes of moderate intensity exercise per week, or 75 to 250 minutes of vigorous activity per week,” Dr. Kovacic emphasized.
“Yes, we can give a statin to lower cholesterol. Yes, we can give a blood pressure medication to lower blood pressure. But when you prescribe exercise, you impact patients’ blood pressure, their cholesterol, their weight, their sense of well-being,” he said. “It cuts across so many different aspects of people’s lives that it’s important to underscore the value of exercise to everybody.”
That includes physicians, he affirmed. “It behooves all physicians to be leading by example. I would encourage those who are overweight or aren’t exercising as much as they should be to make the time to be healthy and to exercise. If you don’t, then bad health will force you to make the time to deal with bad health issues.”
Other articles in the series deal with the athlete’s heart. Christopher Semsarian, MBBS, PhD, MPH, University of Sydney, and colleagues discuss emerging data on hypertrophic cardiomyopathy and other genetic cardiovascular diseases, with the conclusion that it is probably okay for more athletes with these conditions to participate in recreational and competitive sports than was previously thought – another paradigm shift, according to Dr. Kovacic.
The final article addresses some of the challenges and controversies related to the athlete’s heart, including whether extreme exercise is associated with vulnerability to atrial fibrillation and other arrhythmias, and the impact of gender on the cardiac response to exercise, which can’t be determined now because of a paucity of data on women in sports.
Overall, Dr. Kovacic said, the series makes for “compelling” reading that should encourage readers to embark on their own studies to add to the data and support exercise prescription across the board.
No commercial funding or relevant conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
‘Spectacular’ polypill results also puzzle docs
But results from the SECURE trial, published in the New England Journal of Medicine, also raise questions.
How do the polypills reduce cardiovascular problems? And will they ever be available in the United States?
Questions about how they work center on a mystery in the trial data: the polypill – containing aspirin, an angiotensin-converting enzyme (ACE) inhibitor, and a statin – apparently conferred substantial cardiovascular protection while producing average blood pressure and lipid levels that were virtually the same as with usual care.
As to when polypills will be available, the answer may hinge on whether companies, government agencies, or philanthropic foundations come to see making and paying for such treatments – combinations of typically inexpensive generic drugs in a single pill for the sake of convenience and greater adherence – as financially worthwhile.
A matter of adherence?
In the SECURE trial, presented late August at the annual congress of the European Society of Cardiology, Barcelona, investigators randomly assigned 2,499 patients with an MI in the previous 6 months to receive usual care or a polypill.
Patients in the usual-care group typically received the same types of treatments included the polypill, only taken separately. Different versions of the polypill were available to allow for titration to tolerated doses of the component medications: aspirin (100 mg), ramipril (2.5, 5, or 10 mg), and atorvastatin (20 mg or 40 mg).
Researchers used the Morisky Medication Adherence Scale to gauge participants’ adherence to their medication regimen and found the polypill group was more adherent. Patients who received the polypill were more likely to have a high level of adherence at 6 months (70.6% vs. 62.7%) and 24 months (74.1% vs. 63.2%), they reported. (The Morisky tool is the subject of some controversy because of aggressive licensing tactics of its creator.)
The primary endpoint of cardiovascular death, MI, stroke, or urgent revascularization was significantly less likely in the polypill group during a median of 3 years of follow-up (hazard ratio, 0.76; P = .02).
“A primary-outcome event occurred in 118 of 1,237 patients (9.5%) in the polypill group and in 156 of 1,229 (12.7%) in the usual-care group,” the researchers report.
“Probably, adherence is the most important reason of how this works,” Valentin Fuster, MD, physician-in-chief at Mount Sinai Hospital, New York, who led the study, said at ESC 2022.
Still, some clinicians were left scratching their heads by the lack of difference between treatment groups in average blood pressure and levels of low-density lipoprotein (LDL) cholesterol.
In the group that received the polypill, average systolic and diastolic blood pressure at 24 months were 135.2 mmHg and 74.8 mmHg, respectively. In the group that received usual care, those values were 135.5 mmHg and 74.9 mmHg, respectively.
Likewise, “no substantial differences were found in LDL-cholesterol levels over time between the groups, with a mean value at 24 months of 67.7 mg/dL in the polypill group and 67.2 mg/dL in the usual-care group,” according to the researchers.
One explanation for the findings is that greater adherence led to beneficial effects that were not reflected in lipid and blood pressure measurements, the investigators said. Alternatively, the open-label trial design could have led to different health behaviors between groups, they suggested.
Martha Gulati, MD, director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles, said she loves the idea of polypills. But she wonders about the lack of difference in blood pressure and lipids in SECURE.
Dr. Gulati said she sees in practice how medication adherence and measurements of blood pressure and lipids typically go hand in hand.
When a patient initially responds to a medication, but then their LDL cholesterol goes up later, “my first question is, ‘Are you still taking your medication or how frequently are you taking it?’” Dr. Gulati said in an interview. “And I get all kinds of answers.”
“If you are more adherent, why wouldn’t your LDL actually be lower, and why wouldn’t your blood pressure be lower?” she asked.
Can the results be replicated?
Ethan J. Weiss, MD, a cardiologist and volunteer associate clinical professor of medicine at the University of California, San Francisco, said the SECURE results are “spectacular,” but the seeming disconnect with the biomarker measurements “doesn’t make for a clean story.”
“It just seems like if you are making an argument that this is a way to improve compliance ... you would see some evidence of improved compliance objectively” in the biomarker readings, Dr. Weiss said.
Trying to understand how the polypill worked requires more imagination. “Or it makes you just say, ‘Who cares what the mechanism is?’ These people did a lot better, full stop, and that’s all that matters,” he said.
Dr. Weiss said he expects some degree of replication of the results may be needed before practice changes.
To Steven E. Nissen, MD, chief academic officer of the Heart and Vascular Institute at Cleveland Clinic, the results “don’t make any sense.”
“If they got the same results on the biomarkers that the pill was designed to intervene upon, why are the [primary outcome] results different? It’s completely unexplained,” Dr. Nissen said.
In general, Dr. Nissen has not been an advocate of the polypill approach in higher-income countries.
“Medicine is all about customization of therapy,” he said. “Not everybody needs blood pressure lowering. Not everybody needs the same intensity of LDL reduction. We spend much of our lives seeing patients and treating their blood pressure, and if it doesn’t come down adequately, giving them a higher dose or adding another agent.”
Polypills might be reasonable for primary prevention in countries where people have less access to health care resources, he added. In such settings, a low-cost, simple treatment strategy might have benefit.
But Dr. Nissen still doesn’t see a role for a polypill in secondary prevention.
“I think we have to take a step back, take a deep breath, and look very carefully at the science and try to understand whether this, in fact, is sensible,” he said. “We may need another study to see if this can be replicated.”
For Dhruv S. Kazi, MD, the results of the SECURE trial offer an opportunity to rekindle conversations about the use of polypills for cardiovascular protection. These conversations and studies have been taking place for nearly two decades.
Dr. Kazi, associate director of the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center, Boston, has used models to study the expected cost-effectiveness of polypills in various countries.
Although polypills can improve patients’ adherence to their prescribed medications, Dr. Kazi and colleagues have found that treatment gaps are “often at the physician level,” with many patients not prescribed all of the medications from which they could benefit.
Availability of polypills could help address those gaps. At the same time, many patients, even those with higher incomes, may have a strong preference for taking a single pill.
Dr. Kazi’s research also shows that a polypill approach may be more economically attractive as countries develop because successful treatment averts cardiovascular events that are costlier to treat.
“In the United States, in order for this to work, we would need a polypill that is both available widely but also affordable,” Dr. Kazi said. “It is going to require a visionary mover” to make that happen.
That could include philanthropic foundations. But it could also be a business opportunity for a company like Barcelona-based Ferrer, which provided the polypills for the SECURE trial.
The clinical and economic evidence in support of polypills has been compelling, Dr. Kazi said: “We have to get on with the business of implementing something that is effective and has the potential to greatly improve population health at scale.”
The SECURE trial was funded by the European Union Horizon 2020 program and coordinated by the Spanish National Center for Cardiovascular Research (CNIC). Ferrer International provided the polypill that was used in the trial. CNIC receives royalties for sales of the polypill from Ferrer. Dr. Weiss is starting a biotech company unrelated to this area of research.
A version of this article first appeared on Medscape.com.
But results from the SECURE trial, published in the New England Journal of Medicine, also raise questions.
How do the polypills reduce cardiovascular problems? And will they ever be available in the United States?
Questions about how they work center on a mystery in the trial data: the polypill – containing aspirin, an angiotensin-converting enzyme (ACE) inhibitor, and a statin – apparently conferred substantial cardiovascular protection while producing average blood pressure and lipid levels that were virtually the same as with usual care.
As to when polypills will be available, the answer may hinge on whether companies, government agencies, or philanthropic foundations come to see making and paying for such treatments – combinations of typically inexpensive generic drugs in a single pill for the sake of convenience and greater adherence – as financially worthwhile.
A matter of adherence?
In the SECURE trial, presented late August at the annual congress of the European Society of Cardiology, Barcelona, investigators randomly assigned 2,499 patients with an MI in the previous 6 months to receive usual care or a polypill.
Patients in the usual-care group typically received the same types of treatments included the polypill, only taken separately. Different versions of the polypill were available to allow for titration to tolerated doses of the component medications: aspirin (100 mg), ramipril (2.5, 5, or 10 mg), and atorvastatin (20 mg or 40 mg).
Researchers used the Morisky Medication Adherence Scale to gauge participants’ adherence to their medication regimen and found the polypill group was more adherent. Patients who received the polypill were more likely to have a high level of adherence at 6 months (70.6% vs. 62.7%) and 24 months (74.1% vs. 63.2%), they reported. (The Morisky tool is the subject of some controversy because of aggressive licensing tactics of its creator.)
The primary endpoint of cardiovascular death, MI, stroke, or urgent revascularization was significantly less likely in the polypill group during a median of 3 years of follow-up (hazard ratio, 0.76; P = .02).
“A primary-outcome event occurred in 118 of 1,237 patients (9.5%) in the polypill group and in 156 of 1,229 (12.7%) in the usual-care group,” the researchers report.
“Probably, adherence is the most important reason of how this works,” Valentin Fuster, MD, physician-in-chief at Mount Sinai Hospital, New York, who led the study, said at ESC 2022.
Still, some clinicians were left scratching their heads by the lack of difference between treatment groups in average blood pressure and levels of low-density lipoprotein (LDL) cholesterol.
In the group that received the polypill, average systolic and diastolic blood pressure at 24 months were 135.2 mmHg and 74.8 mmHg, respectively. In the group that received usual care, those values were 135.5 mmHg and 74.9 mmHg, respectively.
Likewise, “no substantial differences were found in LDL-cholesterol levels over time between the groups, with a mean value at 24 months of 67.7 mg/dL in the polypill group and 67.2 mg/dL in the usual-care group,” according to the researchers.
One explanation for the findings is that greater adherence led to beneficial effects that were not reflected in lipid and blood pressure measurements, the investigators said. Alternatively, the open-label trial design could have led to different health behaviors between groups, they suggested.
Martha Gulati, MD, director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles, said she loves the idea of polypills. But she wonders about the lack of difference in blood pressure and lipids in SECURE.
Dr. Gulati said she sees in practice how medication adherence and measurements of blood pressure and lipids typically go hand in hand.
When a patient initially responds to a medication, but then their LDL cholesterol goes up later, “my first question is, ‘Are you still taking your medication or how frequently are you taking it?’” Dr. Gulati said in an interview. “And I get all kinds of answers.”
“If you are more adherent, why wouldn’t your LDL actually be lower, and why wouldn’t your blood pressure be lower?” she asked.
Can the results be replicated?
Ethan J. Weiss, MD, a cardiologist and volunteer associate clinical professor of medicine at the University of California, San Francisco, said the SECURE results are “spectacular,” but the seeming disconnect with the biomarker measurements “doesn’t make for a clean story.”
“It just seems like if you are making an argument that this is a way to improve compliance ... you would see some evidence of improved compliance objectively” in the biomarker readings, Dr. Weiss said.
Trying to understand how the polypill worked requires more imagination. “Or it makes you just say, ‘Who cares what the mechanism is?’ These people did a lot better, full stop, and that’s all that matters,” he said.
Dr. Weiss said he expects some degree of replication of the results may be needed before practice changes.
To Steven E. Nissen, MD, chief academic officer of the Heart and Vascular Institute at Cleveland Clinic, the results “don’t make any sense.”
“If they got the same results on the biomarkers that the pill was designed to intervene upon, why are the [primary outcome] results different? It’s completely unexplained,” Dr. Nissen said.
In general, Dr. Nissen has not been an advocate of the polypill approach in higher-income countries.
“Medicine is all about customization of therapy,” he said. “Not everybody needs blood pressure lowering. Not everybody needs the same intensity of LDL reduction. We spend much of our lives seeing patients and treating their blood pressure, and if it doesn’t come down adequately, giving them a higher dose or adding another agent.”
Polypills might be reasonable for primary prevention in countries where people have less access to health care resources, he added. In such settings, a low-cost, simple treatment strategy might have benefit.
But Dr. Nissen still doesn’t see a role for a polypill in secondary prevention.
“I think we have to take a step back, take a deep breath, and look very carefully at the science and try to understand whether this, in fact, is sensible,” he said. “We may need another study to see if this can be replicated.”
For Dhruv S. Kazi, MD, the results of the SECURE trial offer an opportunity to rekindle conversations about the use of polypills for cardiovascular protection. These conversations and studies have been taking place for nearly two decades.
Dr. Kazi, associate director of the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center, Boston, has used models to study the expected cost-effectiveness of polypills in various countries.
Although polypills can improve patients’ adherence to their prescribed medications, Dr. Kazi and colleagues have found that treatment gaps are “often at the physician level,” with many patients not prescribed all of the medications from which they could benefit.
Availability of polypills could help address those gaps. At the same time, many patients, even those with higher incomes, may have a strong preference for taking a single pill.
Dr. Kazi’s research also shows that a polypill approach may be more economically attractive as countries develop because successful treatment averts cardiovascular events that are costlier to treat.
“In the United States, in order for this to work, we would need a polypill that is both available widely but also affordable,” Dr. Kazi said. “It is going to require a visionary mover” to make that happen.
That could include philanthropic foundations. But it could also be a business opportunity for a company like Barcelona-based Ferrer, which provided the polypills for the SECURE trial.
The clinical and economic evidence in support of polypills has been compelling, Dr. Kazi said: “We have to get on with the business of implementing something that is effective and has the potential to greatly improve population health at scale.”
The SECURE trial was funded by the European Union Horizon 2020 program and coordinated by the Spanish National Center for Cardiovascular Research (CNIC). Ferrer International provided the polypill that was used in the trial. CNIC receives royalties for sales of the polypill from Ferrer. Dr. Weiss is starting a biotech company unrelated to this area of research.
A version of this article first appeared on Medscape.com.
But results from the SECURE trial, published in the New England Journal of Medicine, also raise questions.
How do the polypills reduce cardiovascular problems? And will they ever be available in the United States?
Questions about how they work center on a mystery in the trial data: the polypill – containing aspirin, an angiotensin-converting enzyme (ACE) inhibitor, and a statin – apparently conferred substantial cardiovascular protection while producing average blood pressure and lipid levels that were virtually the same as with usual care.
As to when polypills will be available, the answer may hinge on whether companies, government agencies, or philanthropic foundations come to see making and paying for such treatments – combinations of typically inexpensive generic drugs in a single pill for the sake of convenience and greater adherence – as financially worthwhile.
A matter of adherence?
In the SECURE trial, presented late August at the annual congress of the European Society of Cardiology, Barcelona, investigators randomly assigned 2,499 patients with an MI in the previous 6 months to receive usual care or a polypill.
Patients in the usual-care group typically received the same types of treatments included the polypill, only taken separately. Different versions of the polypill were available to allow for titration to tolerated doses of the component medications: aspirin (100 mg), ramipril (2.5, 5, or 10 mg), and atorvastatin (20 mg or 40 mg).
Researchers used the Morisky Medication Adherence Scale to gauge participants’ adherence to their medication regimen and found the polypill group was more adherent. Patients who received the polypill were more likely to have a high level of adherence at 6 months (70.6% vs. 62.7%) and 24 months (74.1% vs. 63.2%), they reported. (The Morisky tool is the subject of some controversy because of aggressive licensing tactics of its creator.)
The primary endpoint of cardiovascular death, MI, stroke, or urgent revascularization was significantly less likely in the polypill group during a median of 3 years of follow-up (hazard ratio, 0.76; P = .02).
“A primary-outcome event occurred in 118 of 1,237 patients (9.5%) in the polypill group and in 156 of 1,229 (12.7%) in the usual-care group,” the researchers report.
“Probably, adherence is the most important reason of how this works,” Valentin Fuster, MD, physician-in-chief at Mount Sinai Hospital, New York, who led the study, said at ESC 2022.
Still, some clinicians were left scratching their heads by the lack of difference between treatment groups in average blood pressure and levels of low-density lipoprotein (LDL) cholesterol.
In the group that received the polypill, average systolic and diastolic blood pressure at 24 months were 135.2 mmHg and 74.8 mmHg, respectively. In the group that received usual care, those values were 135.5 mmHg and 74.9 mmHg, respectively.
Likewise, “no substantial differences were found in LDL-cholesterol levels over time between the groups, with a mean value at 24 months of 67.7 mg/dL in the polypill group and 67.2 mg/dL in the usual-care group,” according to the researchers.
One explanation for the findings is that greater adherence led to beneficial effects that were not reflected in lipid and blood pressure measurements, the investigators said. Alternatively, the open-label trial design could have led to different health behaviors between groups, they suggested.
Martha Gulati, MD, director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles, said she loves the idea of polypills. But she wonders about the lack of difference in blood pressure and lipids in SECURE.
Dr. Gulati said she sees in practice how medication adherence and measurements of blood pressure and lipids typically go hand in hand.
When a patient initially responds to a medication, but then their LDL cholesterol goes up later, “my first question is, ‘Are you still taking your medication or how frequently are you taking it?’” Dr. Gulati said in an interview. “And I get all kinds of answers.”
“If you are more adherent, why wouldn’t your LDL actually be lower, and why wouldn’t your blood pressure be lower?” she asked.
Can the results be replicated?
Ethan J. Weiss, MD, a cardiologist and volunteer associate clinical professor of medicine at the University of California, San Francisco, said the SECURE results are “spectacular,” but the seeming disconnect with the biomarker measurements “doesn’t make for a clean story.”
“It just seems like if you are making an argument that this is a way to improve compliance ... you would see some evidence of improved compliance objectively” in the biomarker readings, Dr. Weiss said.
Trying to understand how the polypill worked requires more imagination. “Or it makes you just say, ‘Who cares what the mechanism is?’ These people did a lot better, full stop, and that’s all that matters,” he said.
Dr. Weiss said he expects some degree of replication of the results may be needed before practice changes.
To Steven E. Nissen, MD, chief academic officer of the Heart and Vascular Institute at Cleveland Clinic, the results “don’t make any sense.”
“If they got the same results on the biomarkers that the pill was designed to intervene upon, why are the [primary outcome] results different? It’s completely unexplained,” Dr. Nissen said.
In general, Dr. Nissen has not been an advocate of the polypill approach in higher-income countries.
“Medicine is all about customization of therapy,” he said. “Not everybody needs blood pressure lowering. Not everybody needs the same intensity of LDL reduction. We spend much of our lives seeing patients and treating their blood pressure, and if it doesn’t come down adequately, giving them a higher dose or adding another agent.”
Polypills might be reasonable for primary prevention in countries where people have less access to health care resources, he added. In such settings, a low-cost, simple treatment strategy might have benefit.
But Dr. Nissen still doesn’t see a role for a polypill in secondary prevention.
“I think we have to take a step back, take a deep breath, and look very carefully at the science and try to understand whether this, in fact, is sensible,” he said. “We may need another study to see if this can be replicated.”
For Dhruv S. Kazi, MD, the results of the SECURE trial offer an opportunity to rekindle conversations about the use of polypills for cardiovascular protection. These conversations and studies have been taking place for nearly two decades.
Dr. Kazi, associate director of the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center, Boston, has used models to study the expected cost-effectiveness of polypills in various countries.
Although polypills can improve patients’ adherence to their prescribed medications, Dr. Kazi and colleagues have found that treatment gaps are “often at the physician level,” with many patients not prescribed all of the medications from which they could benefit.
Availability of polypills could help address those gaps. At the same time, many patients, even those with higher incomes, may have a strong preference for taking a single pill.
Dr. Kazi’s research also shows that a polypill approach may be more economically attractive as countries develop because successful treatment averts cardiovascular events that are costlier to treat.
“In the United States, in order for this to work, we would need a polypill that is both available widely but also affordable,” Dr. Kazi said. “It is going to require a visionary mover” to make that happen.
That could include philanthropic foundations. But it could also be a business opportunity for a company like Barcelona-based Ferrer, which provided the polypills for the SECURE trial.
The clinical and economic evidence in support of polypills has been compelling, Dr. Kazi said: “We have to get on with the business of implementing something that is effective and has the potential to greatly improve population health at scale.”
The SECURE trial was funded by the European Union Horizon 2020 program and coordinated by the Spanish National Center for Cardiovascular Research (CNIC). Ferrer International provided the polypill that was used in the trial. CNIC receives royalties for sales of the polypill from Ferrer. Dr. Weiss is starting a biotech company unrelated to this area of research.
A version of this article first appeared on Medscape.com.