User login
Biofeedback corrects dyssynergic constipation in elderly
SAN ANTONIO – Biofeedback for treatment of dyssynergic constipation is highly effective in the elderly, just as it is in younger patients, Samantha Spilman, MD, reported at the annual meeting of the American College of Gastroenterology.
“I think the main point of this study is that older adults have a profound burden of constipation with dyssynergic defecation, and we propose that biofeedback be given strong consideration as first-line therapy for this population, in whom overall we’re trying to reduce medication use,” said Dr. Spilman, a gastroenterology fellow at the University of California, San Diego.
The prevalence of constipation in older patients is estimated to be up to 40%. Yet few prior studies have scrutinized how well older patients with constipation actually respond to biofeedback. It’s a legitimate question, since biofeedback training involves operant conditioning and requires learning new techniques. For this reason, she and her coinvestigators conducted a retrospective analysis of 58 patients over age 65 referred from the university’s gastrointestinal motility and physiology program to the biofeedback program for treatment of dyssynergic defection. The patients’ mean age was 74 years, with a 9.5-year history of constipation. The oldest patient was 88. Most of the subjects were high school graduates. Thirteen of the 58 carried a diagnosis of irritable bowel syndrome.
Numerous studies have demonstrated that 70%-80% of younger adults with dyssynergic constipation experience marked improvement in response to biofeedback training, which typically utilizes an inflated rectal balloon to simulate retained stool. The key finding in Dr. Spilman’s study was that the elderly patients did comparably well in terms of both self-reported outcomes and objective high-resolution anorectal manometric parameters upon completing an average of three biofeedback sessions.
Mean global bowel satisfaction on a 1-10 scale nearly doubled from 2.77 at baseline to 5.01 with biofeedback. Moreover, 79% of seniors demonstrated resolution of their dyssynergia on high-resolution anorectal manometry performed with sensors in the rectum and anal canal. The proportion of patients who reported a feeling of incomplete evacuation after stooling – a sensation individuals with constipation find highly bothersome – improved from 95% to 24% with biofeedback.
The strongest response in terms of the defecation index was observed in older patients with type 2 dyssynergia, characterized by defective propulsion coupled with a paradoxical contraction of the sphincter muscles during defecation. Their defecation index score, derived by dividing intrarectal pressure by residual intra-anal pressure during simulated defection, showed a robust improvement from 0.307 at baseline to 0.793. Patients with types 1 and 3 dyssynergia showed lesser improvements on this objective measure.
Dr. Spilman noted as a study limitation that baseline cognitive status wasn’t formally assessed, so the investigators don’t know how many of the older patients had minimal cognitive impairment. However, baseline quality of life assessment via the Short Form-36 indicated that patients scored average or above for physical and social functioning as well as emotional well-being.
Dr. Spilman reported having no financial conflicts regarding her study, conducted free of commercial support.
SOURCE: Spilman S. ACG 2019. Abstract 45.
SAN ANTONIO – Biofeedback for treatment of dyssynergic constipation is highly effective in the elderly, just as it is in younger patients, Samantha Spilman, MD, reported at the annual meeting of the American College of Gastroenterology.
“I think the main point of this study is that older adults have a profound burden of constipation with dyssynergic defecation, and we propose that biofeedback be given strong consideration as first-line therapy for this population, in whom overall we’re trying to reduce medication use,” said Dr. Spilman, a gastroenterology fellow at the University of California, San Diego.
The prevalence of constipation in older patients is estimated to be up to 40%. Yet few prior studies have scrutinized how well older patients with constipation actually respond to biofeedback. It’s a legitimate question, since biofeedback training involves operant conditioning and requires learning new techniques. For this reason, she and her coinvestigators conducted a retrospective analysis of 58 patients over age 65 referred from the university’s gastrointestinal motility and physiology program to the biofeedback program for treatment of dyssynergic defection. The patients’ mean age was 74 years, with a 9.5-year history of constipation. The oldest patient was 88. Most of the subjects were high school graduates. Thirteen of the 58 carried a diagnosis of irritable bowel syndrome.
Numerous studies have demonstrated that 70%-80% of younger adults with dyssynergic constipation experience marked improvement in response to biofeedback training, which typically utilizes an inflated rectal balloon to simulate retained stool. The key finding in Dr. Spilman’s study was that the elderly patients did comparably well in terms of both self-reported outcomes and objective high-resolution anorectal manometric parameters upon completing an average of three biofeedback sessions.
Mean global bowel satisfaction on a 1-10 scale nearly doubled from 2.77 at baseline to 5.01 with biofeedback. Moreover, 79% of seniors demonstrated resolution of their dyssynergia on high-resolution anorectal manometry performed with sensors in the rectum and anal canal. The proportion of patients who reported a feeling of incomplete evacuation after stooling – a sensation individuals with constipation find highly bothersome – improved from 95% to 24% with biofeedback.
The strongest response in terms of the defecation index was observed in older patients with type 2 dyssynergia, characterized by defective propulsion coupled with a paradoxical contraction of the sphincter muscles during defecation. Their defecation index score, derived by dividing intrarectal pressure by residual intra-anal pressure during simulated defection, showed a robust improvement from 0.307 at baseline to 0.793. Patients with types 1 and 3 dyssynergia showed lesser improvements on this objective measure.
Dr. Spilman noted as a study limitation that baseline cognitive status wasn’t formally assessed, so the investigators don’t know how many of the older patients had minimal cognitive impairment. However, baseline quality of life assessment via the Short Form-36 indicated that patients scored average or above for physical and social functioning as well as emotional well-being.
Dr. Spilman reported having no financial conflicts regarding her study, conducted free of commercial support.
SOURCE: Spilman S. ACG 2019. Abstract 45.
SAN ANTONIO – Biofeedback for treatment of dyssynergic constipation is highly effective in the elderly, just as it is in younger patients, Samantha Spilman, MD, reported at the annual meeting of the American College of Gastroenterology.
“I think the main point of this study is that older adults have a profound burden of constipation with dyssynergic defecation, and we propose that biofeedback be given strong consideration as first-line therapy for this population, in whom overall we’re trying to reduce medication use,” said Dr. Spilman, a gastroenterology fellow at the University of California, San Diego.
The prevalence of constipation in older patients is estimated to be up to 40%. Yet few prior studies have scrutinized how well older patients with constipation actually respond to biofeedback. It’s a legitimate question, since biofeedback training involves operant conditioning and requires learning new techniques. For this reason, she and her coinvestigators conducted a retrospective analysis of 58 patients over age 65 referred from the university’s gastrointestinal motility and physiology program to the biofeedback program for treatment of dyssynergic defection. The patients’ mean age was 74 years, with a 9.5-year history of constipation. The oldest patient was 88. Most of the subjects were high school graduates. Thirteen of the 58 carried a diagnosis of irritable bowel syndrome.
Numerous studies have demonstrated that 70%-80% of younger adults with dyssynergic constipation experience marked improvement in response to biofeedback training, which typically utilizes an inflated rectal balloon to simulate retained stool. The key finding in Dr. Spilman’s study was that the elderly patients did comparably well in terms of both self-reported outcomes and objective high-resolution anorectal manometric parameters upon completing an average of three biofeedback sessions.
Mean global bowel satisfaction on a 1-10 scale nearly doubled from 2.77 at baseline to 5.01 with biofeedback. Moreover, 79% of seniors demonstrated resolution of their dyssynergia on high-resolution anorectal manometry performed with sensors in the rectum and anal canal. The proportion of patients who reported a feeling of incomplete evacuation after stooling – a sensation individuals with constipation find highly bothersome – improved from 95% to 24% with biofeedback.
The strongest response in terms of the defecation index was observed in older patients with type 2 dyssynergia, characterized by defective propulsion coupled with a paradoxical contraction of the sphincter muscles during defecation. Their defecation index score, derived by dividing intrarectal pressure by residual intra-anal pressure during simulated defection, showed a robust improvement from 0.307 at baseline to 0.793. Patients with types 1 and 3 dyssynergia showed lesser improvements on this objective measure.
Dr. Spilman noted as a study limitation that baseline cognitive status wasn’t formally assessed, so the investigators don’t know how many of the older patients had minimal cognitive impairment. However, baseline quality of life assessment via the Short Form-36 indicated that patients scored average or above for physical and social functioning as well as emotional well-being.
Dr. Spilman reported having no financial conflicts regarding her study, conducted free of commercial support.
SOURCE: Spilman S. ACG 2019. Abstract 45.
REPORTING FROM ACG 2019
Some with mild Crohn’s disease need no treatment
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
Kim L. Isaacs, MD, PhD, said at the annual meeting of the American College of Gastroenterology.
First, it’s essential to establish that a patient truly falls into the mild disease category. And second, during that initial evaluation it’s important to look for the features that signal a high risk of subsequent disease progression.
“Patients with risk factors for disease progression should not be treated as mild Crohn’s disease. These are people that we need to treat perhaps more aggressively up front,” said Dr. Isaacs, professor of medicine and codirector of the Multidisciplinary Center for IBD Research and Treatment at the University of North Carolina, Chapel Hill.
Management of patients with severe Crohn’s disease can be challenging, but Dr. Isaacs finds patients with mild disease flat out “terrifying.”
“The reason I find this situation terrifying is we want to prevent the surgery, the progression from inflammatory disease to more stricturing and penetrating disease. And how can I know that my patient a year from now is not going to be very, very ill and I’ve lost my window to use some of our more potent therapies?” she explained.
Mild Crohn’s disease is characterized clinically by less than 10% weight loss; no fever, tachycardia, or other symptoms of systemic disease; lack of abdominal tenderness; and no signs or symptoms of obstruction. When reading the literature, mild disease is defined by a Crohn’s Disease Activity Index score of 150-220. However, nobody uses that metric outside of research studies; it’s just too cumbersome. More useful in routine clinical practice is the Harvey-Bradshaw Index, where a score of 5-7 indicates mild disease.
Many patients with mild Crohn’s disease will not progress over time. In a recent prospective 29-center European study, just 14% of patients progressed from mild to stricturing and/or penetrating disease within 5 years after diagnosis (Gut. 2018 Jan 23. doi: 10.1136/gutjnl-2017-315568).
Who is likely to progress
Risk factors for disease progression include patients with ileocolonic or perianal disease, smokers, those with inflammatory arthritis or other associated immune-mediated disease, and patients who require corticosteroids in order to maintain remission.
On the other hand, patients with mild Crohn’s disease at low risk for progression have no or only mild symptoms, a limited distribution of bowel inflammation, normal or merely slightly elevated C-reactive protein and/or fecal calprotectin levels, no or only superficial bowel ulceration on colonoscopy, and were diagnosed with inflammatory bowel disease after age 30.
Treatment options
“Our goal in a patient we think is low risk is symptomatic management while avoiding high therapeutic risks in someone we don’t think is going to be progressing,” according to the gastroenterologist.
In patients with mild disease who have symptoms in the ileum or right colon, a good strategy is to induce remission using controlled ileal-release budesonide at 9 mg/day, then follow up with colonoscopy 6-12 months later. The high-dose budesonide regimen has been shown in multiple studies to be more effective than placebo at inducing remission. It’s less effective than conventional oral corticosteroids, but it also causes fewer steroid-related side effects. In fact, the evidence shows that the side effect profile of controlled-release budesonide is no different from that of placebo.
In low-risk, mildly symptomatic patients with diffuse Crohn’s colitis, Dr. Isaacs recommends initial treatment with prednisone and/or sulfasalazine or 5-aminosalicylates. The 5-aminosalicylates aren’t part of most practice guidelines because of conflicting study results. However, a meta-analysis of 22 randomized controlled trials has shown that high-dose mesalamine was 2.29-fold more effective than placebo at inducing remission and is a good option for patients who would rather avoid corticosteroids (Inflamm Bowel Dis. 2017 Mar;23(3):461-72). Prednisone should be tapered after achieving clinical remission. Inability to stop steroids within 6 months after entering remission warrants a switch to maintenance therapy with a biologic or immunomodulatory agent.
Smoking cessation should be a top priority
“I spend a good portion of my time in clinic telling patients, ‘You can do more with stopping smoking than I can do with any of my medications,’ ” Dr. Isaacs said.
Another worthwhile intervention is to check for and correct low serum vitamin D levels. Vitamin D is a potent immunomodulator, and severely low levels below 15 ng/mL are associated with increased risk of Crohn’s disease relapse, more hospitalizations, more active disease activity, and heavier use of corticosteroids than in patients with moderate deficiency in the 15- to 30-ng/mL range (Nutrients. 2019 May 11;11[5]. doi: 10.3390/nu11051059).
Monitoring patients with mild Crohn’s disease
“Monitor closely for mucosal inflammation because if they start to progress, we want to get to them early so they get a good response to their first therapies. If the CRP starts moving up, consider doing something,” she advised.
A CRP above 5 mg/L is associated with a markedly increased risk of relapse. And Spanish investigators have shown in a prospective study of 95 patients in clinical remission for at least 6 months while on a tumor necrosis factor inhibitor that thereafter a fecal calprotein level greater than 300 mcg/g at any point was strongly predictive of relapse within the next 4 months (J Clin Gastroenterol. 2018 Mar;52[3]:229-34). Following a patient with mild Crohn’s disease over time endoscopically, it’s of value to utilize the Simple Endoscopic Score for Crohn’s Disease (SES-CD) to document that in fact the disease is mild. Dr. Isaacs recommended IG-IBD Scores – Calculators in Gastroenterology as “a great site” for assistance in calculating the SES-CD, the Harvey-Bradshaw Index, and a plethora of other inflammatory bowel disease scores.
She reported having no financial conflicts of interest.
REPORTING FROM ACG 2019
UC: Tofacitinib tied to modest, reversible lipid increases, infrequent CV events
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
No clear-cut evidence of vedolizumab effect in retrospective study of primary sclerosing cholangitis
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Bile acid diarrhea guideline highlights data shortage
The Canadian Association of Gastroenterology (CAG) recently co-published a clinical practice guideline for the management of bile acid diarrhea (BAD) in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
Given a minimal evidence base, 16 out of the 17 guideline recommendations are conditional, according to lead author Daniel C. Sadowski, MD, of Royal Alexandra Hospital, Edmonton, Alta., and colleagues. Considering the shortage of high-quality evidence, the panel called for more randomized clinical trials to address current knowledge gaps.
“BAD is an understudied, often underappreciated condition, and questions remain regarding its diagnosis and treatment,” the panelists wrote in Clinical Gastroenterology and Hepatology. “There have been guidelines on the management of chronic diarrhea from the American Gastroenterological Association, and the British Society of Gastroenterology, but diagnosis and management of BAD was not assessed extensively in these publications. The British Society of Gastroenterology updated guidelines on the investigation of chronic diarrhea in adults, published after the consensus meeting, addressed some issues related to BAD.”
For the current guideline, using available evidence and clinical experience, expert panelists from Canada, the United States, and the United Kingdom aimed to “provide a reasonable and practical approach to care for specialists.” The guideline was further reviewed by the CAG Practice Affairs and Clinical Affairs Committees and the CAG Board of Directors.
The guideline first puts BAD in clinical context, noting a chronic diarrhea prevalence rate of approximately 5%. According to the guideline, approximately 1 out of 4 of these patients with chronic diarrhea may have BAD and prevalence of BAD is likely higher among those with other conditions, such as terminal ileal disease.
While BAD may be relatively common, it isn’t necessarily easy to diagnose, the panelists noted.
“The diagnosis of BAD continues to be a challenge, although this may be improved in the future with the general availability of screening serologic tests and other diagnostic tests,” the panelists wrote. “Although a treatment trial with bile acid sequestrants therapy (BAST) often is used, this approach has not been studied adequately, and likely is imprecise, and may lead to both undertreatment and overtreatment.”
Instead, the panelists recommended testing for BAD with 75-selenium homocholic acid taurine (SeHCAT) or 7-alpha-hydroxy-4-cholesten-3-one.
After addressing treatable causes of BAD, the guideline recommends initial therapy with cholestyramine or, if this is poorly tolerated, switching to BAST. However, the panelists advised against BAST for patients with resection or ileal Crohn’s disease, for whom other antidiarrheal agents are more suitable. When appropriate, BAST should be given at the lowest effective dose, with periodic trials of on-demand, intermittent administration, the panelists recommended. When BAST is ineffective, the guideline recommends that clinicians review concurrent medications as a possible cause of BAD or reinvestigate.
Concluding the guideline, the panelists emphasized the need for more high-quality research.
“The group recognized that specific, high-certainty evidence was lacking in many areas and recommended further studies that would improve the data available in future methodologic evaluations,” the panelists wrote.
While improving diagnostic accuracy of BAD should be a major goal of such research, progress is currently limited by an integral shortcoming of diagnostic test accuracy (DTA) studies, the panelists wrote.
“The main challenge in conducting DTA studies for BAD is the lack of a widely accepted or universally agreed-upon reference standard because the condition is defined and classified based on pathophysiologic mechanisms and its response to treatment (BAST),” the panelists wrote. “In addition, the index tests (SeHCAT, C4, FGF19, fecal bile acid assay) provide a continuous measure of metabolic function. Hence, DTA studies are not the most appropriate study design.”
“Therefore, one of the research priorities in BAD is for the scientific and clinical communities to agree on a reference standard that best represents BAD (e.g., response to BAST), with full understanding that the reference standard is and likely will be imperfect.”
The guideline was funded by unrestricted grants from Pendopharm and GE Healthcare Canada. The panelists disclosed relationships with AstraZeneca, AbbVie, Merck, Pfizer, and others.
Review the AGA clinical practice guideline on the laboratory evaluation of functional diarrhea and diarrhea-predominan irritable bowel syndrome in adults at https:/www.gastrojournal.org/article/S0016-5085(19)41083-4/fulltext.
SOURCE: Sadowski DC et al. Clin Gastroenterol Hepatol. 2019 Sep 14. doi: 10.1016/j.cgh.2019.08.062.
The Canadian Association of Gastroenterology (CAG) recently co-published a clinical practice guideline for the management of bile acid diarrhea (BAD) in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
Given a minimal evidence base, 16 out of the 17 guideline recommendations are conditional, according to lead author Daniel C. Sadowski, MD, of Royal Alexandra Hospital, Edmonton, Alta., and colleagues. Considering the shortage of high-quality evidence, the panel called for more randomized clinical trials to address current knowledge gaps.
“BAD is an understudied, often underappreciated condition, and questions remain regarding its diagnosis and treatment,” the panelists wrote in Clinical Gastroenterology and Hepatology. “There have been guidelines on the management of chronic diarrhea from the American Gastroenterological Association, and the British Society of Gastroenterology, but diagnosis and management of BAD was not assessed extensively in these publications. The British Society of Gastroenterology updated guidelines on the investigation of chronic diarrhea in adults, published after the consensus meeting, addressed some issues related to BAD.”
For the current guideline, using available evidence and clinical experience, expert panelists from Canada, the United States, and the United Kingdom aimed to “provide a reasonable and practical approach to care for specialists.” The guideline was further reviewed by the CAG Practice Affairs and Clinical Affairs Committees and the CAG Board of Directors.
The guideline first puts BAD in clinical context, noting a chronic diarrhea prevalence rate of approximately 5%. According to the guideline, approximately 1 out of 4 of these patients with chronic diarrhea may have BAD and prevalence of BAD is likely higher among those with other conditions, such as terminal ileal disease.
While BAD may be relatively common, it isn’t necessarily easy to diagnose, the panelists noted.
“The diagnosis of BAD continues to be a challenge, although this may be improved in the future with the general availability of screening serologic tests and other diagnostic tests,” the panelists wrote. “Although a treatment trial with bile acid sequestrants therapy (BAST) often is used, this approach has not been studied adequately, and likely is imprecise, and may lead to both undertreatment and overtreatment.”
Instead, the panelists recommended testing for BAD with 75-selenium homocholic acid taurine (SeHCAT) or 7-alpha-hydroxy-4-cholesten-3-one.
After addressing treatable causes of BAD, the guideline recommends initial therapy with cholestyramine or, if this is poorly tolerated, switching to BAST. However, the panelists advised against BAST for patients with resection or ileal Crohn’s disease, for whom other antidiarrheal agents are more suitable. When appropriate, BAST should be given at the lowest effective dose, with periodic trials of on-demand, intermittent administration, the panelists recommended. When BAST is ineffective, the guideline recommends that clinicians review concurrent medications as a possible cause of BAD or reinvestigate.
Concluding the guideline, the panelists emphasized the need for more high-quality research.
“The group recognized that specific, high-certainty evidence was lacking in many areas and recommended further studies that would improve the data available in future methodologic evaluations,” the panelists wrote.
While improving diagnostic accuracy of BAD should be a major goal of such research, progress is currently limited by an integral shortcoming of diagnostic test accuracy (DTA) studies, the panelists wrote.
“The main challenge in conducting DTA studies for BAD is the lack of a widely accepted or universally agreed-upon reference standard because the condition is defined and classified based on pathophysiologic mechanisms and its response to treatment (BAST),” the panelists wrote. “In addition, the index tests (SeHCAT, C4, FGF19, fecal bile acid assay) provide a continuous measure of metabolic function. Hence, DTA studies are not the most appropriate study design.”
“Therefore, one of the research priorities in BAD is for the scientific and clinical communities to agree on a reference standard that best represents BAD (e.g., response to BAST), with full understanding that the reference standard is and likely will be imperfect.”
The guideline was funded by unrestricted grants from Pendopharm and GE Healthcare Canada. The panelists disclosed relationships with AstraZeneca, AbbVie, Merck, Pfizer, and others.
Review the AGA clinical practice guideline on the laboratory evaluation of functional diarrhea and diarrhea-predominan irritable bowel syndrome in adults at https:/www.gastrojournal.org/article/S0016-5085(19)41083-4/fulltext.
SOURCE: Sadowski DC et al. Clin Gastroenterol Hepatol. 2019 Sep 14. doi: 10.1016/j.cgh.2019.08.062.
The Canadian Association of Gastroenterology (CAG) recently co-published a clinical practice guideline for the management of bile acid diarrhea (BAD) in Clinical Gastroenterology and Hepatology and the Journal of the Canadian Association of Gastroenterology.
Given a minimal evidence base, 16 out of the 17 guideline recommendations are conditional, according to lead author Daniel C. Sadowski, MD, of Royal Alexandra Hospital, Edmonton, Alta., and colleagues. Considering the shortage of high-quality evidence, the panel called for more randomized clinical trials to address current knowledge gaps.
“BAD is an understudied, often underappreciated condition, and questions remain regarding its diagnosis and treatment,” the panelists wrote in Clinical Gastroenterology and Hepatology. “There have been guidelines on the management of chronic diarrhea from the American Gastroenterological Association, and the British Society of Gastroenterology, but diagnosis and management of BAD was not assessed extensively in these publications. The British Society of Gastroenterology updated guidelines on the investigation of chronic diarrhea in adults, published after the consensus meeting, addressed some issues related to BAD.”
For the current guideline, using available evidence and clinical experience, expert panelists from Canada, the United States, and the United Kingdom aimed to “provide a reasonable and practical approach to care for specialists.” The guideline was further reviewed by the CAG Practice Affairs and Clinical Affairs Committees and the CAG Board of Directors.
The guideline first puts BAD in clinical context, noting a chronic diarrhea prevalence rate of approximately 5%. According to the guideline, approximately 1 out of 4 of these patients with chronic diarrhea may have BAD and prevalence of BAD is likely higher among those with other conditions, such as terminal ileal disease.
While BAD may be relatively common, it isn’t necessarily easy to diagnose, the panelists noted.
“The diagnosis of BAD continues to be a challenge, although this may be improved in the future with the general availability of screening serologic tests and other diagnostic tests,” the panelists wrote. “Although a treatment trial with bile acid sequestrants therapy (BAST) often is used, this approach has not been studied adequately, and likely is imprecise, and may lead to both undertreatment and overtreatment.”
Instead, the panelists recommended testing for BAD with 75-selenium homocholic acid taurine (SeHCAT) or 7-alpha-hydroxy-4-cholesten-3-one.
After addressing treatable causes of BAD, the guideline recommends initial therapy with cholestyramine or, if this is poorly tolerated, switching to BAST. However, the panelists advised against BAST for patients with resection or ileal Crohn’s disease, for whom other antidiarrheal agents are more suitable. When appropriate, BAST should be given at the lowest effective dose, with periodic trials of on-demand, intermittent administration, the panelists recommended. When BAST is ineffective, the guideline recommends that clinicians review concurrent medications as a possible cause of BAD or reinvestigate.
Concluding the guideline, the panelists emphasized the need for more high-quality research.
“The group recognized that specific, high-certainty evidence was lacking in many areas and recommended further studies that would improve the data available in future methodologic evaluations,” the panelists wrote.
While improving diagnostic accuracy of BAD should be a major goal of such research, progress is currently limited by an integral shortcoming of diagnostic test accuracy (DTA) studies, the panelists wrote.
“The main challenge in conducting DTA studies for BAD is the lack of a widely accepted or universally agreed-upon reference standard because the condition is defined and classified based on pathophysiologic mechanisms and its response to treatment (BAST),” the panelists wrote. “In addition, the index tests (SeHCAT, C4, FGF19, fecal bile acid assay) provide a continuous measure of metabolic function. Hence, DTA studies are not the most appropriate study design.”
“Therefore, one of the research priorities in BAD is for the scientific and clinical communities to agree on a reference standard that best represents BAD (e.g., response to BAST), with full understanding that the reference standard is and likely will be imperfect.”
The guideline was funded by unrestricted grants from Pendopharm and GE Healthcare Canada. The panelists disclosed relationships with AstraZeneca, AbbVie, Merck, Pfizer, and others.
Review the AGA clinical practice guideline on the laboratory evaluation of functional diarrhea and diarrhea-predominan irritable bowel syndrome in adults at https:/www.gastrojournal.org/article/S0016-5085(19)41083-4/fulltext.
SOURCE: Sadowski DC et al. Clin Gastroenterol Hepatol. 2019 Sep 14. doi: 10.1016/j.cgh.2019.08.062.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The Canadian Association of Gastroenterology recently published a clinical practice guideline for the management of bile acid diarrhea (BAD).
Major finding: BAD occurs in up to 35% of patients with chronic diarrhea or diarrhea-predominant irritable bowel syndrome.
Study details: A clinical practice guideline for the management of BAD.
Disclosures: The guideline was funded by unrestricted grants from Pendopharm and GE Healthcare Canada. The panelists disclosed relationships with AstraZeneca, AbbVie, Merck, Pfizer, and others.
Source: Sadowski DC et al. Clin Gastroenterol Hepatol. 2019 Sep 14. doi: 10.1016/j.cgh.2019.08.062.
Certolizumab safety profile varies widely across indications
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
MADRID – , Andrew Blauvelt, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a comprehensive analysis of safety data from all 49 clinical trials of the tumor necrosis factor inhibitor for its approved indications. The data set included 11,317 patients who received certolizumab for a collective 21,695 person-years in 27 trials in rheumatoid arthritis patients, 5 in psoriasis, 15 for Crohn’s disease, and one trial each for axial spondyloarthritis and psoriatic arthritis.
“It’s not real-world data, but it is a large group of patients [studied] over many years,” noted Dr. Blauvelt, a dermatologist and president of the Oregon Medical Research Center, Portland.
As a renowned authority on psoriasis, he was part of a multidisciplinary expert panel commissioned by UCB to analyze serious adverse events in the complete clinical trials experience involving the company’s tumor necrosis factor inhibitor certolizumab (Cimzia). The panel included experts from rheumatology, gastroenterology, epidemiology, and other disciplines.
The key takeaway: “When you think about the serious side effects of the drug, you have to think about what the indication is, whether the patients are on systemic corticosteroids, and whether they’re heavy or not,” Dr. Blauvelt said.
Take, for example, the risk of serious infections requiring treatment with intravenous antibiotics. The incidence rates ranged from a low of 1.5 per 100 patient-years in psoriasis patients on certolizumab to a high of 5.97 in those with Crohn’s disease, with rates of 3.44 cases per 100 patient-years among rheumatoid arthritis patients and 1.64-1.67 in those with psoriatic arthritis and ankylosing spondylitis, respectively. Patients with Crohn’s disease were 2.22-fold more likely than were those with rheumatoid arthritis to experience a serious infection during their clinical trial experience on certolizumab. In contrast, psoriasis patients had a 52% relative risk reduction and those with psoriatic arthritis were 31% less likely to develop a serious infection compared with those with rheumatoid arthritis.
The explanation for these highly variable serious infection rates lies in part on the huge differences in the concurrent use of systemic corticosteroids with certolizumab across indications. A mere 3.3% of psoriasis patients were also on steroids, compared with 46.2% of rheumatoid arthritis patients, 50.8% of those with ankylosing spondylitis, and about 25% of the Crohn’s disease and psoriatic arthritis patients, he noted.
Advanced age was independently associated with increased risk of serious infections. Patients aged 65 or older were 1.68-fold more likely to experience this event than were those under age 45. And patients whose disease duration was 10 years or more at baseline had a 1.36-fold increased serious infection risk compared with those who had less than a 1-year-long disease history, independent of which disease they had.
The prevalence of baseline obesity varied by indication. The mean body mass index was 30.1 kg/m2 in the psoriasis patients, 29.8 kg/m2 in those with psoriatic arthritis, lowest at 24 kg/m2 in Crohn’s disease patients, and a bit over 27 kg/m2 in those with rheumatoid arthritis or ankylosing spondylitis.
Obesity alone was not an independent risk factor for serious infection in certolizumab-treated patients; however, the combination of a BMI of 30 kg/m2 or more plus systemic corticosteroid use was associated with a greater risk than with steroids alone.
Based upon a multivariate regression analysis adjusted for age, sex, indication, disease duration, use of methotrexate, and prior use of other TNF inhibitors, the investigators calculated that in patients with Crohn’s disease 16.6% of serious infections in patients on certolizumab were attributable to systemic corticosteroid use.
Risks of major adverse cardiovascular events and cancer on certolizumab
The risk of major adverse cardiovascular events (MACE) while on certolizumab ranged from a high of 0.62 MACE events per 100 patient-years in the rheumatoid arthritis population to a low of 0.1 per 100 patient-years in patients treated for Crohn’s disease or ankylosing spondylitis. Psoriasis and psoriatic arthritis patients had MACE rates of 0.27 and 0.54, respectively.
Obesity was independently associated with increased risk of an acute MI and other MACEs. So was advanced age. No surprises there. The investigators calculated that 16.7% of MACEs in patients on certolizumab were attributable to obesity and another 20.9% were attributable to use of systemic corticosteroids.
The incidence rate for all malignancies, including nonmelanoma skin cancer, ranged from a low of 0.46 cases per 100 patient-years in the psoriatic arthritis cohort on certolizumab to a high of 0.93 in those with rheumatoid arthritis, with rates of 0.68, 0.73, and 0.51 in patients with psoriasis, Crohn’s disease, and ankylosing spondylitis, respectively.
Neither systemic corticosteroids, obesity, disease duration, or prior exposure to a TNF inhibitor was linked to increased risk of cancer in patients on certolizumab. The standout risk factor was age: Patients who were 65 or older at baseline were 11.4-fold more likely to develop cancer during participation in their clinical trial than were those younger than 45. Those who were 45 to 65 years old were 4.3-fold more likely to be diagnosed with a malignancy than were those younger than age 45.
Of note, concomitant use of methotrexate was associated with a statistically significant 28% reduction in malignancy risk.
Dr. Blauvelt reported serving as a consultant to and receiving research funding from UCB, the study sponsor, as well as more than two dozen other pharmaceutical companies.
SOURCE: Blauvelt A. EADV Congress, Abstract FC04.06.
REPORTING FROM THE EADV CONGRESS
Geriatric IBD hospitalization carries steep inpatient mortality
SAN ANTONIO – Jeffrey Schwartz, MD, reported at the annual meeting of the American College of Gastroenterology.

The magnitude of the age-related increased risk highlighted in this large national study was strikingly larger than the differential inpatient mortality between geriatric and nongeriatric patients hospitalized for conditions other than inflammatory bowel disease (IBD). It’s a finding that reveals a major unmet need for improved systems of care for elderly hospitalized IBD patients, according to Dr. Schwartz, an internal medicine resident at Beth Israel Deaconess Medical Center, Boston.
“Given the high prevalence of IBD patients that require inpatient admission, as well as the rapidly aging nature of the U.S. population, it’s our hope that this study will provide some insight to drive efforts to improve standardized guideline-directed therapy and propose interventions to help close what I think is a very important gap in clinical care,” he said.
It’s well established that a second peak of IBD diagnoses occurs in 50- to 70-year-olds. At present, roughly 30% of all individuals carrying the diagnosis of IBD are over age 65, and with the graying of the baby-boomer population, this proportion is climbing.
Dr. Schwartz presented a study of the National Inpatient Sample for 2016, which is a representative sample comprising 20% of all U.S. hospital discharges for that year, the most recent year for which the data are available. The study population included all 71,040 patients hospitalized for acute management of Crohn’s disease or its immediate complications, of whom 10,095 were aged over age 75 years, as well as the 35,950 patients hospitalized for ulcerative colitis, 8,285 of whom were over 75.
Inpatient mortality occurred in 1.5% of the geriatric admissions, compared with 0.2% of nongeriatric admissions for Crohn’s disease. Similarly, the inpatient mortality rate in geriatric patients with ulcerative colitis was 1.0% versus 0.1% in patients under age 75 hospitalized for ulcerative colitis.
There are lots of reasons why the management of geriatric patients with IBD is particularly challenging, Dr. Schwartz noted. They have a higher burden of comorbid conditions, worse nutritional status, and increased risks of infection and cancer. In a regression analysis that attempted to control for such confounders using the Elixhauser mortality index, the nongeriatric Crohn’s disease patients were an adjusted 75% less likely to die in the hospital than those who were older. Nongeriatric ulcerative colitis patients were 81% less likely to die than geriatric patients with the disease. In contrast, nongeriatric patients admitted for reasons other than IBD had only an adjusted 50% lower risk of inpatient mortality than those who were older than 75.
Of note, in this analysis adjusted for confounders, there was no difference between geriatric and nongeriatric IBD patients in terms of resource utilization as reflected in average length of stay and hospital charges, Dr. Schwartz continued.
Asked if he could shed light on any specific complications that drove the age-related disparity in inpatient mortality in the IBD population, the physician replied that he and his coinvestigators were thwarted in their effort to do so because the inpatient mortality of 1.0%-1.5% was so low that further breakdown as to causes of death would have been statistically unreliable. It might be possible to do so successfully by combining several years of National Inpatient Sample data. That being said, it’s reasonable to hypothesize that cardiovascular complications are an important contributor, he added.
Dr. Schwartz reported having no financial conflicts regarding his study, conducted free of commercial support.
SAN ANTONIO – Jeffrey Schwartz, MD, reported at the annual meeting of the American College of Gastroenterology.

The magnitude of the age-related increased risk highlighted in this large national study was strikingly larger than the differential inpatient mortality between geriatric and nongeriatric patients hospitalized for conditions other than inflammatory bowel disease (IBD). It’s a finding that reveals a major unmet need for improved systems of care for elderly hospitalized IBD patients, according to Dr. Schwartz, an internal medicine resident at Beth Israel Deaconess Medical Center, Boston.
“Given the high prevalence of IBD patients that require inpatient admission, as well as the rapidly aging nature of the U.S. population, it’s our hope that this study will provide some insight to drive efforts to improve standardized guideline-directed therapy and propose interventions to help close what I think is a very important gap in clinical care,” he said.
It’s well established that a second peak of IBD diagnoses occurs in 50- to 70-year-olds. At present, roughly 30% of all individuals carrying the diagnosis of IBD are over age 65, and with the graying of the baby-boomer population, this proportion is climbing.
Dr. Schwartz presented a study of the National Inpatient Sample for 2016, which is a representative sample comprising 20% of all U.S. hospital discharges for that year, the most recent year for which the data are available. The study population included all 71,040 patients hospitalized for acute management of Crohn’s disease or its immediate complications, of whom 10,095 were aged over age 75 years, as well as the 35,950 patients hospitalized for ulcerative colitis, 8,285 of whom were over 75.
Inpatient mortality occurred in 1.5% of the geriatric admissions, compared with 0.2% of nongeriatric admissions for Crohn’s disease. Similarly, the inpatient mortality rate in geriatric patients with ulcerative colitis was 1.0% versus 0.1% in patients under age 75 hospitalized for ulcerative colitis.
There are lots of reasons why the management of geriatric patients with IBD is particularly challenging, Dr. Schwartz noted. They have a higher burden of comorbid conditions, worse nutritional status, and increased risks of infection and cancer. In a regression analysis that attempted to control for such confounders using the Elixhauser mortality index, the nongeriatric Crohn’s disease patients were an adjusted 75% less likely to die in the hospital than those who were older. Nongeriatric ulcerative colitis patients were 81% less likely to die than geriatric patients with the disease. In contrast, nongeriatric patients admitted for reasons other than IBD had only an adjusted 50% lower risk of inpatient mortality than those who were older than 75.
Of note, in this analysis adjusted for confounders, there was no difference between geriatric and nongeriatric IBD patients in terms of resource utilization as reflected in average length of stay and hospital charges, Dr. Schwartz continued.
Asked if he could shed light on any specific complications that drove the age-related disparity in inpatient mortality in the IBD population, the physician replied that he and his coinvestigators were thwarted in their effort to do so because the inpatient mortality of 1.0%-1.5% was so low that further breakdown as to causes of death would have been statistically unreliable. It might be possible to do so successfully by combining several years of National Inpatient Sample data. That being said, it’s reasonable to hypothesize that cardiovascular complications are an important contributor, he added.
Dr. Schwartz reported having no financial conflicts regarding his study, conducted free of commercial support.
SAN ANTONIO – Jeffrey Schwartz, MD, reported at the annual meeting of the American College of Gastroenterology.

The magnitude of the age-related increased risk highlighted in this large national study was strikingly larger than the differential inpatient mortality between geriatric and nongeriatric patients hospitalized for conditions other than inflammatory bowel disease (IBD). It’s a finding that reveals a major unmet need for improved systems of care for elderly hospitalized IBD patients, according to Dr. Schwartz, an internal medicine resident at Beth Israel Deaconess Medical Center, Boston.
“Given the high prevalence of IBD patients that require inpatient admission, as well as the rapidly aging nature of the U.S. population, it’s our hope that this study will provide some insight to drive efforts to improve standardized guideline-directed therapy and propose interventions to help close what I think is a very important gap in clinical care,” he said.
It’s well established that a second peak of IBD diagnoses occurs in 50- to 70-year-olds. At present, roughly 30% of all individuals carrying the diagnosis of IBD are over age 65, and with the graying of the baby-boomer population, this proportion is climbing.
Dr. Schwartz presented a study of the National Inpatient Sample for 2016, which is a representative sample comprising 20% of all U.S. hospital discharges for that year, the most recent year for which the data are available. The study population included all 71,040 patients hospitalized for acute management of Crohn’s disease or its immediate complications, of whom 10,095 were aged over age 75 years, as well as the 35,950 patients hospitalized for ulcerative colitis, 8,285 of whom were over 75.
Inpatient mortality occurred in 1.5% of the geriatric admissions, compared with 0.2% of nongeriatric admissions for Crohn’s disease. Similarly, the inpatient mortality rate in geriatric patients with ulcerative colitis was 1.0% versus 0.1% in patients under age 75 hospitalized for ulcerative colitis.
There are lots of reasons why the management of geriatric patients with IBD is particularly challenging, Dr. Schwartz noted. They have a higher burden of comorbid conditions, worse nutritional status, and increased risks of infection and cancer. In a regression analysis that attempted to control for such confounders using the Elixhauser mortality index, the nongeriatric Crohn’s disease patients were an adjusted 75% less likely to die in the hospital than those who were older. Nongeriatric ulcerative colitis patients were 81% less likely to die than geriatric patients with the disease. In contrast, nongeriatric patients admitted for reasons other than IBD had only an adjusted 50% lower risk of inpatient mortality than those who were older than 75.
Of note, in this analysis adjusted for confounders, there was no difference between geriatric and nongeriatric IBD patients in terms of resource utilization as reflected in average length of stay and hospital charges, Dr. Schwartz continued.
Asked if he could shed light on any specific complications that drove the age-related disparity in inpatient mortality in the IBD population, the physician replied that he and his coinvestigators were thwarted in their effort to do so because the inpatient mortality of 1.0%-1.5% was so low that further breakdown as to causes of death would have been statistically unreliable. It might be possible to do so successfully by combining several years of National Inpatient Sample data. That being said, it’s reasonable to hypothesize that cardiovascular complications are an important contributor, he added.
Dr. Schwartz reported having no financial conflicts regarding his study, conducted free of commercial support.
REPORTING FROM ACG 2019
Key clinical point: A major unmet need exists for better guideline-directed management of geriatric patients hospitalized for inflammatory bowel disease.
Major finding: The inpatient mortality rate among patients aged over age 75 years hospitalized for management of inflammatory bowel disease is four to five times higher than in those who are younger.
Study details: This was a retrospective analysis of all 106,990 hospital admissions for management of inflammatory bowel disease included in the 2016 National Inpatient Sample.
Disclosures: The presenter reported having no financial conflicts regarding his study, conducted free of commercial support.
Source: Schwartz J. ACG 2019, Abstract 42.
Clinicians ask FDA for continued ‘discretion’ to do fecal transplants
Attendees at a public meeting on Nov. 4 gave the US Food and Drug Administration conflicting views on whether the agency should continue to allow a relatively loose regulatory environment for fecal microbiota transplants (FMT) – debating the limits of “enforcement discretion” the FDA now has in place.
The question is especially relevant as use of the procedure is growing, while safety data are not being rigorously collected in all cases. The death of an immunocompromised FMT patient earlier in 2018 from an invasive bacterial infection caused by drug-resistant Escherichia coli, as reported by Medscape Medical News, is seen by some as an example of the consequences of a loose policy.
Still, the American Gastroenterological Association (AGA) presented new, unpublished follow-up data at the meeting that showed that the majority of FMT patients in a national registry had no adverse events.
Some companies developing FMT-based products argued at the meeting that the agency should impose stricter requirements, while stool banks and clinicians offering the therapy outside of clinical trials said that the current policy – in place since 2013 – in which the FDA has exercised “enforcement discretion,” should be allowed to continue.
“Enforcement discretion has been successful in enabling and overcoming key barriers to access to treatment,” said Majdi Osman, MD, clinical program director at OpenBiome, a nonprofit stool bank based in Cambridge, Mass. Dr. Osman said that 98% of the U.S. population now lives within a 2-hour drive of an FMT provider.
Amanda Kabage, a researcher and donor program coordinator for the Microbiota Therapeutics program at the University of Minnesota in Minneapolis, and herself a former recipient of FMT, said she was in favor of continuing the FDA policy.
“If enforcement discretion were to go away, patients far sicker than I was will not have access. They’ll get sicker and they will die,” Ms. Kabage said.
But, she added, the FDA had missed an opportunity by not insisting on collecting outcomes and safety data. Minnesota has established a patient registry to do just that, and physicians cannot administer FMT unless they agree to participate, she said. In response, FDA panelists noted that the agency cannot mandate data collection under an enforcement policy.
Lee Jones, founder and chief executive officer of Rebiotix/Ferring, a biotech company focused on the development of microbiome-based therapeutics, argued for tighter restrictions, however, claiming that increased access – and the FDA policy – had led to a fourfold decrease in enrollment since the company began study of its lead FMT product, RBX2660, in 2013.
“We’re dealing with an orphan indication and the patients were hard to come by to begin with,” she said at the meeting. “Enforcement discretion has slowed our clinical development and delayed patient access to FDA-approved therapies by over 2 years.”
An investigator at the University of Texas Health Science Center at Houston, Herbert DuPont, MD, who has administered FMT and is conducting a trial for Rebiotix, said his center wanted the FDA policy to continue “allowing multiple groups to perform FMT for recurrent [Clostridium difficile], because of the incredible public health need.”
But, he added, “We’re very concerned about industry and ability to do clinical trials.”
Those trials are important, Dr. DuPont said. “I think we have to address very actively how industry can move these products through,” he said, “because all of us want to remove the F from FMT,” by isolating the necessary elements of the process while not having the risk sometimes associated with human stool.
Policy slow to evolve
“I’m frustrated that it’s taken over 6 years and three draft guidances to get us this far,” Christian John Lillis, executive director of the Peggy Lillis Foundation – a group dedicated to creating awareness about the dangers of C. difficile – said at the meeting.
Mr. Lillis said that probably several thousand deaths had been prevented through increased FMT access, but that it was time to create a concrete policy that advanced the therapy.
The FDA guidance issued in 2013 allowed physicians to provide FMT for recurrent or refractory C. difficile infection without filing an investigational new drug (IND) application.
Clinicians must obtain informed consent that includes a discussion of the risks, and a statement that FMT is investigational. In March 2016, the agency issued revised draft guidance that it was aiming to require stool banks to apply for INDs, as reported by Medscape Medical News.
OpenBiome has flourished under the current policy. It has provided more than 50,000 treatments to 1,200 hospitals and clinics, and has provided FMT for 49 clinical trials and for 16 single patients who received INDs, Dr. Osman said.
But requiring INDs for all centers is a bad idea, he said. “IND requirements are insurmountable for most health centers,” Dr. Osman said, noting that most of the FMT material OpenBiome produces is sent to community-based physicians.
“These requirements would likely mean restrictions in access for stool bank–provided FMT and potentially pushing patients to physician-directed FMT or discouraging physicians from using FMT at all,” he said.
Stacy Kahn, MD, FMT director at Boston Children’s Hospital in Massachusetts, said that having ready access from a stool bank was crucial.
“Universal donor FMT is much easier, much faster and much more cost effective than what we can do as clinicians,” she said.
New safety and efficacy data
One unpublished study showed that 75% of patients treated since 2011 had a sustained cure, noted Colleen Kelly, MD, a Brown University professor of medicine and principal investigator for the National Institutes of Health–funded national FMT registry (although the data in this study were not from the FMT registry).
The study, which was a collaboration between the Alpert Medical School of Brown University, Brigham and Women’s Hospital, and Indiana University School of Medicine, attempted follow-up on 533 patients; 208 were successfully contacted, and an additional 55 had died, none due to FMT.
Dr. Kelly also presented data from the FMT National Registry showing that at 1 month posttransplant, two (1%) of 253 patients had an infection possibly related to FMT; one with Bacteroides fragilis and one with enteropathogenic E. coli. Seven hospitalizations were deemed related or possibly related to FMT, including two recurrences of C. difficile.
At 6 months posttransplant, 8 (5%) of 152 patients had a serious infection, and 23 patients reported a diagnosis of a new condition, primarily diarrhea-predominant irritable bowel syndrome, which is common post FMT, said Dr. Kelly, who presented the data on behalf of AGA, which administers the registry.
The AGA supports a continuation of the enforcement discretion as a means to maintain patient access where the evidence supports the use of FMT, but the group does not back use of FMT outside medical supervision, Dr. Kelly said.
This article originally appeared on Medscape. For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Attendees at a public meeting on Nov. 4 gave the US Food and Drug Administration conflicting views on whether the agency should continue to allow a relatively loose regulatory environment for fecal microbiota transplants (FMT) – debating the limits of “enforcement discretion” the FDA now has in place.
The question is especially relevant as use of the procedure is growing, while safety data are not being rigorously collected in all cases. The death of an immunocompromised FMT patient earlier in 2018 from an invasive bacterial infection caused by drug-resistant Escherichia coli, as reported by Medscape Medical News, is seen by some as an example of the consequences of a loose policy.
Still, the American Gastroenterological Association (AGA) presented new, unpublished follow-up data at the meeting that showed that the majority of FMT patients in a national registry had no adverse events.
Some companies developing FMT-based products argued at the meeting that the agency should impose stricter requirements, while stool banks and clinicians offering the therapy outside of clinical trials said that the current policy – in place since 2013 – in which the FDA has exercised “enforcement discretion,” should be allowed to continue.
“Enforcement discretion has been successful in enabling and overcoming key barriers to access to treatment,” said Majdi Osman, MD, clinical program director at OpenBiome, a nonprofit stool bank based in Cambridge, Mass. Dr. Osman said that 98% of the U.S. population now lives within a 2-hour drive of an FMT provider.
Amanda Kabage, a researcher and donor program coordinator for the Microbiota Therapeutics program at the University of Minnesota in Minneapolis, and herself a former recipient of FMT, said she was in favor of continuing the FDA policy.
“If enforcement discretion were to go away, patients far sicker than I was will not have access. They’ll get sicker and they will die,” Ms. Kabage said.
But, she added, the FDA had missed an opportunity by not insisting on collecting outcomes and safety data. Minnesota has established a patient registry to do just that, and physicians cannot administer FMT unless they agree to participate, she said. In response, FDA panelists noted that the agency cannot mandate data collection under an enforcement policy.
Lee Jones, founder and chief executive officer of Rebiotix/Ferring, a biotech company focused on the development of microbiome-based therapeutics, argued for tighter restrictions, however, claiming that increased access – and the FDA policy – had led to a fourfold decrease in enrollment since the company began study of its lead FMT product, RBX2660, in 2013.
“We’re dealing with an orphan indication and the patients were hard to come by to begin with,” she said at the meeting. “Enforcement discretion has slowed our clinical development and delayed patient access to FDA-approved therapies by over 2 years.”
An investigator at the University of Texas Health Science Center at Houston, Herbert DuPont, MD, who has administered FMT and is conducting a trial for Rebiotix, said his center wanted the FDA policy to continue “allowing multiple groups to perform FMT for recurrent [Clostridium difficile], because of the incredible public health need.”
But, he added, “We’re very concerned about industry and ability to do clinical trials.”
Those trials are important, Dr. DuPont said. “I think we have to address very actively how industry can move these products through,” he said, “because all of us want to remove the F from FMT,” by isolating the necessary elements of the process while not having the risk sometimes associated with human stool.
Policy slow to evolve
“I’m frustrated that it’s taken over 6 years and three draft guidances to get us this far,” Christian John Lillis, executive director of the Peggy Lillis Foundation – a group dedicated to creating awareness about the dangers of C. difficile – said at the meeting.
Mr. Lillis said that probably several thousand deaths had been prevented through increased FMT access, but that it was time to create a concrete policy that advanced the therapy.
The FDA guidance issued in 2013 allowed physicians to provide FMT for recurrent or refractory C. difficile infection without filing an investigational new drug (IND) application.
Clinicians must obtain informed consent that includes a discussion of the risks, and a statement that FMT is investigational. In March 2016, the agency issued revised draft guidance that it was aiming to require stool banks to apply for INDs, as reported by Medscape Medical News.
OpenBiome has flourished under the current policy. It has provided more than 50,000 treatments to 1,200 hospitals and clinics, and has provided FMT for 49 clinical trials and for 16 single patients who received INDs, Dr. Osman said.
But requiring INDs for all centers is a bad idea, he said. “IND requirements are insurmountable for most health centers,” Dr. Osman said, noting that most of the FMT material OpenBiome produces is sent to community-based physicians.
“These requirements would likely mean restrictions in access for stool bank–provided FMT and potentially pushing patients to physician-directed FMT or discouraging physicians from using FMT at all,” he said.
Stacy Kahn, MD, FMT director at Boston Children’s Hospital in Massachusetts, said that having ready access from a stool bank was crucial.
“Universal donor FMT is much easier, much faster and much more cost effective than what we can do as clinicians,” she said.
New safety and efficacy data
One unpublished study showed that 75% of patients treated since 2011 had a sustained cure, noted Colleen Kelly, MD, a Brown University professor of medicine and principal investigator for the National Institutes of Health–funded national FMT registry (although the data in this study were not from the FMT registry).
The study, which was a collaboration between the Alpert Medical School of Brown University, Brigham and Women’s Hospital, and Indiana University School of Medicine, attempted follow-up on 533 patients; 208 were successfully contacted, and an additional 55 had died, none due to FMT.
Dr. Kelly also presented data from the FMT National Registry showing that at 1 month posttransplant, two (1%) of 253 patients had an infection possibly related to FMT; one with Bacteroides fragilis and one with enteropathogenic E. coli. Seven hospitalizations were deemed related or possibly related to FMT, including two recurrences of C. difficile.
At 6 months posttransplant, 8 (5%) of 152 patients had a serious infection, and 23 patients reported a diagnosis of a new condition, primarily diarrhea-predominant irritable bowel syndrome, which is common post FMT, said Dr. Kelly, who presented the data on behalf of AGA, which administers the registry.
The AGA supports a continuation of the enforcement discretion as a means to maintain patient access where the evidence supports the use of FMT, but the group does not back use of FMT outside medical supervision, Dr. Kelly said.
This article originally appeared on Medscape. For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Attendees at a public meeting on Nov. 4 gave the US Food and Drug Administration conflicting views on whether the agency should continue to allow a relatively loose regulatory environment for fecal microbiota transplants (FMT) – debating the limits of “enforcement discretion” the FDA now has in place.
The question is especially relevant as use of the procedure is growing, while safety data are not being rigorously collected in all cases. The death of an immunocompromised FMT patient earlier in 2018 from an invasive bacterial infection caused by drug-resistant Escherichia coli, as reported by Medscape Medical News, is seen by some as an example of the consequences of a loose policy.
Still, the American Gastroenterological Association (AGA) presented new, unpublished follow-up data at the meeting that showed that the majority of FMT patients in a national registry had no adverse events.
Some companies developing FMT-based products argued at the meeting that the agency should impose stricter requirements, while stool banks and clinicians offering the therapy outside of clinical trials said that the current policy – in place since 2013 – in which the FDA has exercised “enforcement discretion,” should be allowed to continue.
“Enforcement discretion has been successful in enabling and overcoming key barriers to access to treatment,” said Majdi Osman, MD, clinical program director at OpenBiome, a nonprofit stool bank based in Cambridge, Mass. Dr. Osman said that 98% of the U.S. population now lives within a 2-hour drive of an FMT provider.
Amanda Kabage, a researcher and donor program coordinator for the Microbiota Therapeutics program at the University of Minnesota in Minneapolis, and herself a former recipient of FMT, said she was in favor of continuing the FDA policy.
“If enforcement discretion were to go away, patients far sicker than I was will not have access. They’ll get sicker and they will die,” Ms. Kabage said.
But, she added, the FDA had missed an opportunity by not insisting on collecting outcomes and safety data. Minnesota has established a patient registry to do just that, and physicians cannot administer FMT unless they agree to participate, she said. In response, FDA panelists noted that the agency cannot mandate data collection under an enforcement policy.
Lee Jones, founder and chief executive officer of Rebiotix/Ferring, a biotech company focused on the development of microbiome-based therapeutics, argued for tighter restrictions, however, claiming that increased access – and the FDA policy – had led to a fourfold decrease in enrollment since the company began study of its lead FMT product, RBX2660, in 2013.
“We’re dealing with an orphan indication and the patients were hard to come by to begin with,” she said at the meeting. “Enforcement discretion has slowed our clinical development and delayed patient access to FDA-approved therapies by over 2 years.”
An investigator at the University of Texas Health Science Center at Houston, Herbert DuPont, MD, who has administered FMT and is conducting a trial for Rebiotix, said his center wanted the FDA policy to continue “allowing multiple groups to perform FMT for recurrent [Clostridium difficile], because of the incredible public health need.”
But, he added, “We’re very concerned about industry and ability to do clinical trials.”
Those trials are important, Dr. DuPont said. “I think we have to address very actively how industry can move these products through,” he said, “because all of us want to remove the F from FMT,” by isolating the necessary elements of the process while not having the risk sometimes associated with human stool.
Policy slow to evolve
“I’m frustrated that it’s taken over 6 years and three draft guidances to get us this far,” Christian John Lillis, executive director of the Peggy Lillis Foundation – a group dedicated to creating awareness about the dangers of C. difficile – said at the meeting.
Mr. Lillis said that probably several thousand deaths had been prevented through increased FMT access, but that it was time to create a concrete policy that advanced the therapy.
The FDA guidance issued in 2013 allowed physicians to provide FMT for recurrent or refractory C. difficile infection without filing an investigational new drug (IND) application.
Clinicians must obtain informed consent that includes a discussion of the risks, and a statement that FMT is investigational. In March 2016, the agency issued revised draft guidance that it was aiming to require stool banks to apply for INDs, as reported by Medscape Medical News.
OpenBiome has flourished under the current policy. It has provided more than 50,000 treatments to 1,200 hospitals and clinics, and has provided FMT for 49 clinical trials and for 16 single patients who received INDs, Dr. Osman said.
But requiring INDs for all centers is a bad idea, he said. “IND requirements are insurmountable for most health centers,” Dr. Osman said, noting that most of the FMT material OpenBiome produces is sent to community-based physicians.
“These requirements would likely mean restrictions in access for stool bank–provided FMT and potentially pushing patients to physician-directed FMT or discouraging physicians from using FMT at all,” he said.
Stacy Kahn, MD, FMT director at Boston Children’s Hospital in Massachusetts, said that having ready access from a stool bank was crucial.
“Universal donor FMT is much easier, much faster and much more cost effective than what we can do as clinicians,” she said.
New safety and efficacy data
One unpublished study showed that 75% of patients treated since 2011 had a sustained cure, noted Colleen Kelly, MD, a Brown University professor of medicine and principal investigator for the National Institutes of Health–funded national FMT registry (although the data in this study were not from the FMT registry).
The study, which was a collaboration between the Alpert Medical School of Brown University, Brigham and Women’s Hospital, and Indiana University School of Medicine, attempted follow-up on 533 patients; 208 were successfully contacted, and an additional 55 had died, none due to FMT.
Dr. Kelly also presented data from the FMT National Registry showing that at 1 month posttransplant, two (1%) of 253 patients had an infection possibly related to FMT; one with Bacteroides fragilis and one with enteropathogenic E. coli. Seven hospitalizations were deemed related or possibly related to FMT, including two recurrences of C. difficile.
At 6 months posttransplant, 8 (5%) of 152 patients had a serious infection, and 23 patients reported a diagnosis of a new condition, primarily diarrhea-predominant irritable bowel syndrome, which is common post FMT, said Dr. Kelly, who presented the data on behalf of AGA, which administers the registry.
The AGA supports a continuation of the enforcement discretion as a means to maintain patient access where the evidence supports the use of FMT, but the group does not back use of FMT outside medical supervision, Dr. Kelly said.
This article originally appeared on Medscape. For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Management of the hospitalized ulcerative colitis patient: A primer for the initial approach to care for the practicing gastroenterologist
Introduction
Inpatient management of acute ulcerative colitis (UC) flares can be challenging because of the multiple patient and disease-related factors influencing therapeutic decision making. The clinical course during the first 24-72 hours of the hospitalization will likely guide the decision between rescue medical and surgical therapy. Using available evidence from clinical practice guidelines, we present a day-by-day guide to managing most hospitalized UC patients.
Day 0 – The emergency department (ED)
When an UC patient presents to the ED for evaluation, the initial assessments should focus on the acuity and severity of the flare. Key clinical features of disease severity include the presence of fever, tachycardia, hypotension, or weight loss in addition to worsened gastrointestinal symptoms of stool frequency relative to baseline, rectal bleeding, and abdominal pain. Acute severe ulcerative colitis (ASUC) is often defined using the modified Truelove and Witts criteria.1 A patient meets criteria for ASUC if they have at least six bloody stools per day and at least one sign of systemic toxicity, such as heart rate greater than 90 bpm, temperature at or above 37.8° C, hemoglobin level below 10.5 g/dL, or elevated inflammatory markers.
Initial laboratory assessments should include complete blood counts to identify anemia, potential superimposed infection, or toxicity and a comprehensive metabolic profile to evaluate for dehydration, electrolyte abnormalities, hepatic injury or hypoalbuminemia (an important predictor of surgery), as well as assessment of response to treatment and readmission.2,3 An evaluation at admission of C-reactive protein (CRP) is crucial because changes from the initial value will determine steroid response and predict need for surgical intervention or rescue therapy. A baseline fecal calprotectin can serve as a noninvasive marker that can be followed after discharge to monitor response to therapy.
Clostridioides difficile infection (CDI) must be ruled out in all patients presenting with ASUC regardless of history of antibiotic use or prior negative testing. Concomitant UC and CDI are associated with a four- to sixfold increased risk of in-hospital mortality and a two- to sixfold increased risk of bowel surgery.4-6 Immunoassay testing is inexpensive and fast with a high specificity but has low sensitivity; nucleic acid amplification testing with polymerase chain reaction has a high sensitivity and specificity.7 Knowing which testing algorithm the hospital lab uses helps guide interpretation of results.
For patients meeting criteria for ASUC, obtaining at least an abdominal x-ray is important to assess for colonic dilation to further stratify the patient by risk. Colonic dilation, defined as a transverse colon diameter greater than 5.5 cm, places the patient in the category of fulminant colitis and colorectal surgical consultation should be obtained.8 A CT scan is often ordered first because it can provide a rapid assessment of intra-abdominal processes but is not routinely needed unless hemodynamic instability, an acute abdomen, or markedly abnormal laboratory testing (specifically white blood cell count with bandemia) is present as these can be indicators of toxic megacolon or perforation.8-10
Day 1 – Assess disease severity and assemble the team
Obtaining a thorough clinical history is essential to classify disease severity and identify potential triggers for the acute exacerbation. Potential triggers may include infections, new medications, recent antibiotic use, recent travel, sick contacts, or cessation of treatments. Standard questions include asking about the timing of onset of symptoms, bowel movements during a 24-hour period, and particularly the presence of nocturnal bowel movements. If patients report bloody stools, inquire how often they see blood relative to the total number of bowel movements. The presence and nature of abdominal pain should be elicited, particularly changes in abdominal pain and comparison with previous disease flares. These clinical parameters are used to assess response to treatment; therefore, ask patients to keep a log of their stool frequency, consistency, rectal urgency, and bleeding each day to report to the team during daily rounds.
For patients with ASUC, a full colonoscopy is rarely indicated in the inpatient setting because it is unlikely to change management and poses a risk of perforation.11 However, a sigmoidoscopy within the first 24 hours of admission will provide useful information about the endoscopic disease activity, particularly if features such as deep or well-like ulcers, large mucosal abrasions, or extensive loss of the mucosal layer are present because these are predictors of colectomy.8 Tissue biopsies can exclude cytomegalovirus (CMV) infection, an important consideration for patients on immunosuppression including corticosteroids.12-16
Venous thromboembolism (VTE) prophylaxis is extremely important for hospitalized inflammatory bowel disease (IBD) patients. At baseline, IBD patients have a threefold higher risk of VTE than do non-IBD patients, which increases to approximately sixfold during flares.17 Pharmacologic VTE prophylaxis is recommended for all hospitalized IBD patients, even those with rectal bleeding. This may seem counterintuitive in the setting of “GI bleeding,” so it is important to counsel both patients and team members regarding VTE risks and the role of the prophylactic regimen to ensure adherence. Mechanical VTE prophylaxis can be used in patients with severe bleeding and hemodynamic instability until pharmacologic VTE prophylaxis can be safely initiated.17
Narcotics should be used sparingly for hospitalized IBD patients. Narcotic use is associated with greater likelihood of subsequent IBD hospitalizations, ED visits, and higher costs of health care for patients with IBD.18 Heavy use of opiates, defined as continuous use for more than 30 days at a dose exceeding 50 mg morphine per day or equivalent, was strongly associated with an increased overall mortality in IBD patients.19 Opiates also slow bowel motility and precipitate toxic megacolon, along with any other agent that slows bowel motility, such as anticholinergic medications.8 These agents may also mask bowel frequency symptoms that would otherwise indicate a failure of medical therapy. Similarly, use of NSAIDS should also be avoided because these have been associated with disease relapse and escalating intestinal inflammation.20
Once disease severity has been determined, intravenous corticosteroid therapy may be initiated, ideally once CDI and CMV have been excluded. The recommended dosing of intravenous corticosteroids is methylprednisolone 20 mg IV every 8 hours or equivalent. There is no evidence to support additional benefit for doses exceeding these amounts.8 Prior to starting parenteral corticosteroids, it is important to keep in mind the possible need for rescue therapy during the admission. Recommended testing includes hepatitis B surface antigen and antibody, hepatitis B core antibody and tuberculosis testing if there is no documented negative testing within the past 6-12 months. These labs should be drawn prior to steroid treatment to avoid delays in care and indeterminate results. Finally, a lipid profile is recommended for patients who may be cyclosporine candidates pending response to intravenous corticosteroids. Unless the patient has been admitted with a bowel obstruction, which should raise the suspicion that the diagnosis is actually Crohn’s disease, enteral feeding is preferred for UC patients even if they may have significant food aversion. The early involvement of a registered dietitian is valuable to guide dietary choices and recommend appropriate enteral nutrition supplements. During acute flares, patients may find a low-residue diet to be less stimulating to their gut while their acute flare is being treated. Electrolyte abnormalities should be repleted and consistently monitored during the hospitalization. Providing parenteral intravenous iron for anemic patients will expedite correction of the anemia alongside treatment of the underlying UC.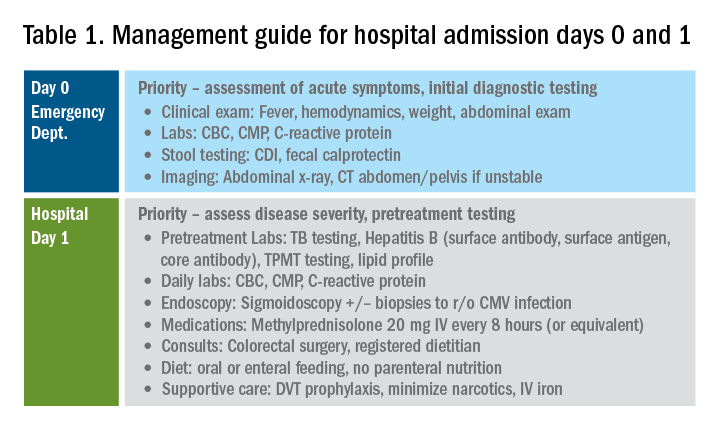
Most UC patients admitted to the hospital will require a multidisciplinary approach with gastroenterologists, surgeons, radiologists, dietitians, and case coordinators/social workers, among others. It is essential to assemble the team, especially the surgeons, earlier during the hospitalization rather than later. It is especially important to discuss the role of the surgeon in the management of UC and explain why the surgeon is being consulted in the context of the patient’s acute presentation. Being transparent about the parameters the GI team are monitoring to determine if and when surgery is the most appropriate and safe approach will improve patients’ acceptance of the surgical team’s role in their care. Specific indications for surgery in ASUC include toxic megacolon, colonic perforation, severe refractory hemorrhage, and failure to respond to medical therapy (Table 1).8
Day 3 – Assessing response to corticosteroids
In addition to daily symptom assessments, a careful abdominal exam should be performed every day with the understanding that steroids (and also narcotics) may mask perforation or pain. Any abrupt decrease or cessation of bowel movements, increasing abdominal distention, or a sudden increase in abdominal pain or tenderness may require abdominal imaging to ensure no interim perforation or severe colonic dilation has occurred while receiving steroid therapy. In these circumstances, the addition of broad spectrum intravenous antibiotics should be considered, particularly if hemodynamic instability (such as tachycardia) is present.
Patients should be assessed for response to intravenous steroid therapy after 3 days of treatment. A meaningful response to corticosteroids is present if the patient has had more than 50% improvement in symptoms, particularly rectal bleeding and stool frequency. A more than 75% improvement in CRP should also be noted from admission to day 3 with an overall trend of improvement.2,21 Additionally, patients should be afebrile, require minimal to no narcotic usage, tolerating oral intake, and be ambulatory. If the patient has met all these parameters, it is reasonable to transition to oral corticosteroids, such as prednisone 40-60 mg daily after a course of 3-5 days of intravenous corticosteroids. Ideally, patients should be observed for 24-48 hours in the hospital after transitioning to oral corticosteroids to make sure that symptoms do not worsen with the switch.
Patients with more than eight bowel movements per day, CRP greater than 4.5 g/dL, deep ulcers on endoscopy, or albumin less than 3.0 g/dL have a higher likelihood of failing intravenous corticosteroid therapy, and these patients should be prepared for rescue therapy.2,21 A patient has failed intravenous corticosteroids by day 3 if they have sustained fever in the absence of an infection, continued CRP elevation or lack of CRP decrease, or ongoing high stool frequency, bleeding, and pain with less than 50% improvement from baseline on admission.8 In the setting of nonresponse to intravenous corticosteroids, it is prudent to involve colorectal surgery to discuss colectomy as an option of equal merit to medical salvage therapies such as infliximab or cyclosporine.
Infliximab is the most readily available rescue therapy for steroid-refractory patients and has been shown to increase colectomy-free survival in patients with ASUC.8 However, patients with the same predictors for intravenous steroid failures (low albumin, high CRP, and/or deep ulcers on endoscopy) are also at the highest risk for infliximab nonresponse. These factors are important to discuss with the patients and colorectal surgery teams when providing the options of treatment strategy, particularly with medication dosing. ASUC with more severe disease biochemically (low albumin, elevated CRP, possibly bandemia) benefit from a higher dose of infliximab at 10 mg/kg, given the likelihood of increased drug clearance in this situation.22,23
From a practical standpoint, it is important to confirm the patient’s insurance status prior to medication administration to make sure therapy can be continued after hospital discharge. Early involvement of the social workers and case coordinators is key to ensuring timely administration of the next dose of treatment. Patients who receive infliximab rescue therapy should be monitored for an additional 1-2 days after administration to ensure they are responding to this therapy with continued monitoring of CRP and symptoms during this period. If there is no response at this point, an additional dose of infliximab may be considered but surgery should not be delayed if there is no meaningful response after the first dose.
Another option for intravenous corticosteroid nonresponders is intravenous cyclosporine because treatment failure rates for cyclosporine and infliximab were similar in head-to-head studies.24 However, patient selection is key to successful utilization of this agent. Unlike infliximab, cyclosporine is primarily an induction agent for steroid nonresponders rather than a maintenance strategy. Therefore, in patients in whom cyclosporine is being considered, thiopurines or vedolizumab are potential options for maintenance therapy. If the patient has poor renal function, low cholesterol, advanced age, significant comorbidities, or a history of nonadherence to therapy, cyclosporine should not be given. Additionally, clinical experience with intravenous cyclosporine administration and monitoring both during inpatient and outpatient care settings should be factored into the decision making for infliximab versus cyclosporine.8
Day 5 and beyond – Discharge planning
Patients who have responded to the initial intravenous steroid course by hospital day 5 should have successfully transitioned to oral steroids with plans to start an appropriate steroid-sparing therapy shortly after discharge. Treatment planning should commence prior to discharge and should be communicated with the outpatient GI team to ensure a smooth transition to the ambulatory care setting, primarily to begin insurance authorizations as soon as possible. If the patient has had a meaningful response to infliximab rescue therapy (improvement by more than 50% in bowel frequency, amount of blood, abdominal pain), discharge planning needs to prioritize obtaining authorization for the second dose within 2 weeks of the initial infusion. These patients are high risk for readmission, and close outpatient follow-up by the ambulatory GI care team is necessary to help direct the tapering of steroids and monitor response to treatment.
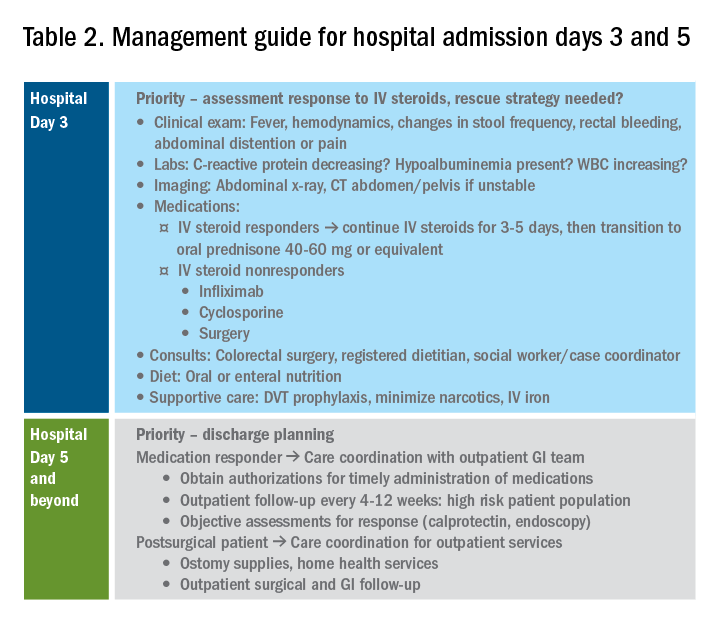
If the patient has not responded to intravenous steroid therapy, infliximab, or cyclosporine by day 5-7, then surgery should be strongly considered. Delaying surgery may worsen outcomes as patients become more malnourished, anemic, and continue to receive intravenous steroids. Additional preoperative optimization may be required depending on the patient’s course up to this point (Table 2).
Summary
The cornerstones of inpatient UC management center on a thorough initial evaluation including imaging and endoscopy as appropriate, establishment of baseline parameters, and daily assessment of response to therapy through a combination of patient-reported outcomes and biomarkers of inflammation. With this strategy in mind, practitioners and care teams can manage these complex patients using a consistent strategy focusing on multidisciplinary, evidence-based care.
References
1. Truelove SC et al. Br Med J. 1955 Oct 23;2(4947):1041-8.
2. Ho GT et al. Aliment Pharmacol Ther. 2004 May 15;19(10):1079-87.
3. Tinsley A et al. Scand J Gastroenterol. 2015;50(9):1103-9.
4. Issa M et al. Clin Gastroenterol Hepatol. 2007 Mar;5(3):345-51.
5. Ananthakrishnan AN et al. Gut. 2008 Feb;57(2):205-10.
6. Negron ME et al. Am J Gastroenterol. 2016 May;111(5):691-704.
7. Taylor KN et al. Gynecol Oncol. 2017 Feb;144(2):428-37.
8. Rubin DT et al. Am J Gastroenterol. 2019 Mar;114(3):384-413.
9. Jalan KN et al. Gastroenterology. 1969 Jul;57(1):68-82.
10. Gan SI et al. Am J Gastroenterol. 2003 Nov;98(11):2363-71.
11. Makkar R et al. Gastroenterol Hepatol (N Y). 2013 Sep;9(9):573-83.
12. Hindryckx P et al. Nat Rev Gastroenterol Hepatol. 2016 Nov;13(11):654-64.
13. Yerushalmy-Feler A et al. Curr Infect Dis Rep. 2019 Feb 15;21(2):5.
14. Shukla T et al. J Clin Gastroenterol. 2017 May/Jun;51(5):394-401.
15. McCurdy JD et al. Clin Gastroenterol Hepatol. 2015 Jan;13(1):131-7; quiz e7.
16. Cottone M et al. Am J Gastroenterol. 2001 Mar;96(3):773-5.
17. Nguyen GC et al. Gastroenterology. 2014 Mar;146(3):835-48 e6.
18. Limsrivilai J et al. Clin Gastroenterol Hepatol. 2017 Mar;15(3):385-92 e2.
19. Targownik LE et al. Am J Gastroenterol. 2014 Oct;109(10):1613-20.
20. Takeuchi K et al. Clin Gastroenterol Hepatol. 2006 Feb;4(2):196-202.
21. Travis SP et al. Gut. 1996 Jun;38(6):905-10.
22. Syal G et al. Mo1891 - Gastroenterology. 2018;154:S841.
23. Ungar B et al. Aliment Pharmacol Ther. 2016 Jun;43(12):1293-9.
24. Laharie D et al. Lancet 2012 Dec 1;380(9857):1909-15.
Dr. Chiplunker is an advanced inflammatory bowel disease fellow; Dr. Ha is associate professor of medicine at the Inflammatory Bowel Disease Center at Cedars-Sinai Medical Center, Los Angeles.
Introduction
Inpatient management of acute ulcerative colitis (UC) flares can be challenging because of the multiple patient and disease-related factors influencing therapeutic decision making. The clinical course during the first 24-72 hours of the hospitalization will likely guide the decision between rescue medical and surgical therapy. Using available evidence from clinical practice guidelines, we present a day-by-day guide to managing most hospitalized UC patients.
Day 0 – The emergency department (ED)
When an UC patient presents to the ED for evaluation, the initial assessments should focus on the acuity and severity of the flare. Key clinical features of disease severity include the presence of fever, tachycardia, hypotension, or weight loss in addition to worsened gastrointestinal symptoms of stool frequency relative to baseline, rectal bleeding, and abdominal pain. Acute severe ulcerative colitis (ASUC) is often defined using the modified Truelove and Witts criteria.1 A patient meets criteria for ASUC if they have at least six bloody stools per day and at least one sign of systemic toxicity, such as heart rate greater than 90 bpm, temperature at or above 37.8° C, hemoglobin level below 10.5 g/dL, or elevated inflammatory markers.
Initial laboratory assessments should include complete blood counts to identify anemia, potential superimposed infection, or toxicity and a comprehensive metabolic profile to evaluate for dehydration, electrolyte abnormalities, hepatic injury or hypoalbuminemia (an important predictor of surgery), as well as assessment of response to treatment and readmission.2,3 An evaluation at admission of C-reactive protein (CRP) is crucial because changes from the initial value will determine steroid response and predict need for surgical intervention or rescue therapy. A baseline fecal calprotectin can serve as a noninvasive marker that can be followed after discharge to monitor response to therapy.
Clostridioides difficile infection (CDI) must be ruled out in all patients presenting with ASUC regardless of history of antibiotic use or prior negative testing. Concomitant UC and CDI are associated with a four- to sixfold increased risk of in-hospital mortality and a two- to sixfold increased risk of bowel surgery.4-6 Immunoassay testing is inexpensive and fast with a high specificity but has low sensitivity; nucleic acid amplification testing with polymerase chain reaction has a high sensitivity and specificity.7 Knowing which testing algorithm the hospital lab uses helps guide interpretation of results.
For patients meeting criteria for ASUC, obtaining at least an abdominal x-ray is important to assess for colonic dilation to further stratify the patient by risk. Colonic dilation, defined as a transverse colon diameter greater than 5.5 cm, places the patient in the category of fulminant colitis and colorectal surgical consultation should be obtained.8 A CT scan is often ordered first because it can provide a rapid assessment of intra-abdominal processes but is not routinely needed unless hemodynamic instability, an acute abdomen, or markedly abnormal laboratory testing (specifically white blood cell count with bandemia) is present as these can be indicators of toxic megacolon or perforation.8-10
Day 1 – Assess disease severity and assemble the team
Obtaining a thorough clinical history is essential to classify disease severity and identify potential triggers for the acute exacerbation. Potential triggers may include infections, new medications, recent antibiotic use, recent travel, sick contacts, or cessation of treatments. Standard questions include asking about the timing of onset of symptoms, bowel movements during a 24-hour period, and particularly the presence of nocturnal bowel movements. If patients report bloody stools, inquire how often they see blood relative to the total number of bowel movements. The presence and nature of abdominal pain should be elicited, particularly changes in abdominal pain and comparison with previous disease flares. These clinical parameters are used to assess response to treatment; therefore, ask patients to keep a log of their stool frequency, consistency, rectal urgency, and bleeding each day to report to the team during daily rounds.
For patients with ASUC, a full colonoscopy is rarely indicated in the inpatient setting because it is unlikely to change management and poses a risk of perforation.11 However, a sigmoidoscopy within the first 24 hours of admission will provide useful information about the endoscopic disease activity, particularly if features such as deep or well-like ulcers, large mucosal abrasions, or extensive loss of the mucosal layer are present because these are predictors of colectomy.8 Tissue biopsies can exclude cytomegalovirus (CMV) infection, an important consideration for patients on immunosuppression including corticosteroids.12-16
Venous thromboembolism (VTE) prophylaxis is extremely important for hospitalized inflammatory bowel disease (IBD) patients. At baseline, IBD patients have a threefold higher risk of VTE than do non-IBD patients, which increases to approximately sixfold during flares.17 Pharmacologic VTE prophylaxis is recommended for all hospitalized IBD patients, even those with rectal bleeding. This may seem counterintuitive in the setting of “GI bleeding,” so it is important to counsel both patients and team members regarding VTE risks and the role of the prophylactic regimen to ensure adherence. Mechanical VTE prophylaxis can be used in patients with severe bleeding and hemodynamic instability until pharmacologic VTE prophylaxis can be safely initiated.17
Narcotics should be used sparingly for hospitalized IBD patients. Narcotic use is associated with greater likelihood of subsequent IBD hospitalizations, ED visits, and higher costs of health care for patients with IBD.18 Heavy use of opiates, defined as continuous use for more than 30 days at a dose exceeding 50 mg morphine per day or equivalent, was strongly associated with an increased overall mortality in IBD patients.19 Opiates also slow bowel motility and precipitate toxic megacolon, along with any other agent that slows bowel motility, such as anticholinergic medications.8 These agents may also mask bowel frequency symptoms that would otherwise indicate a failure of medical therapy. Similarly, use of NSAIDS should also be avoided because these have been associated with disease relapse and escalating intestinal inflammation.20
Once disease severity has been determined, intravenous corticosteroid therapy may be initiated, ideally once CDI and CMV have been excluded. The recommended dosing of intravenous corticosteroids is methylprednisolone 20 mg IV every 8 hours or equivalent. There is no evidence to support additional benefit for doses exceeding these amounts.8 Prior to starting parenteral corticosteroids, it is important to keep in mind the possible need for rescue therapy during the admission. Recommended testing includes hepatitis B surface antigen and antibody, hepatitis B core antibody and tuberculosis testing if there is no documented negative testing within the past 6-12 months. These labs should be drawn prior to steroid treatment to avoid delays in care and indeterminate results. Finally, a lipid profile is recommended for patients who may be cyclosporine candidates pending response to intravenous corticosteroids. Unless the patient has been admitted with a bowel obstruction, which should raise the suspicion that the diagnosis is actually Crohn’s disease, enteral feeding is preferred for UC patients even if they may have significant food aversion. The early involvement of a registered dietitian is valuable to guide dietary choices and recommend appropriate enteral nutrition supplements. During acute flares, patients may find a low-residue diet to be less stimulating to their gut while their acute flare is being treated. Electrolyte abnormalities should be repleted and consistently monitored during the hospitalization. Providing parenteral intravenous iron for anemic patients will expedite correction of the anemia alongside treatment of the underlying UC.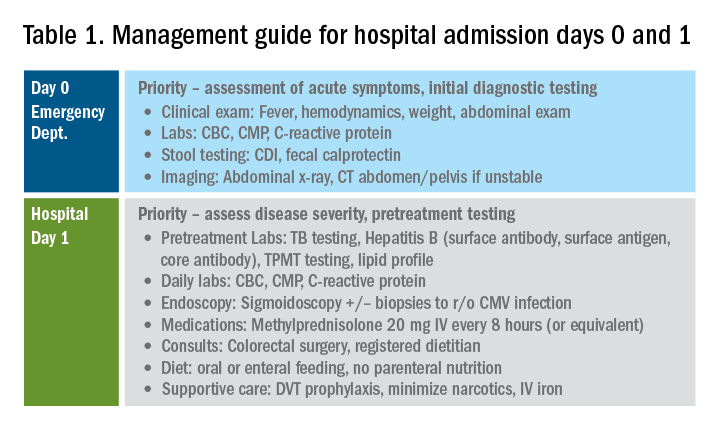
Most UC patients admitted to the hospital will require a multidisciplinary approach with gastroenterologists, surgeons, radiologists, dietitians, and case coordinators/social workers, among others. It is essential to assemble the team, especially the surgeons, earlier during the hospitalization rather than later. It is especially important to discuss the role of the surgeon in the management of UC and explain why the surgeon is being consulted in the context of the patient’s acute presentation. Being transparent about the parameters the GI team are monitoring to determine if and when surgery is the most appropriate and safe approach will improve patients’ acceptance of the surgical team’s role in their care. Specific indications for surgery in ASUC include toxic megacolon, colonic perforation, severe refractory hemorrhage, and failure to respond to medical therapy (Table 1).8
Day 3 – Assessing response to corticosteroids
In addition to daily symptom assessments, a careful abdominal exam should be performed every day with the understanding that steroids (and also narcotics) may mask perforation or pain. Any abrupt decrease or cessation of bowel movements, increasing abdominal distention, or a sudden increase in abdominal pain or tenderness may require abdominal imaging to ensure no interim perforation or severe colonic dilation has occurred while receiving steroid therapy. In these circumstances, the addition of broad spectrum intravenous antibiotics should be considered, particularly if hemodynamic instability (such as tachycardia) is present.
Patients should be assessed for response to intravenous steroid therapy after 3 days of treatment. A meaningful response to corticosteroids is present if the patient has had more than 50% improvement in symptoms, particularly rectal bleeding and stool frequency. A more than 75% improvement in CRP should also be noted from admission to day 3 with an overall trend of improvement.2,21 Additionally, patients should be afebrile, require minimal to no narcotic usage, tolerating oral intake, and be ambulatory. If the patient has met all these parameters, it is reasonable to transition to oral corticosteroids, such as prednisone 40-60 mg daily after a course of 3-5 days of intravenous corticosteroids. Ideally, patients should be observed for 24-48 hours in the hospital after transitioning to oral corticosteroids to make sure that symptoms do not worsen with the switch.
Patients with more than eight bowel movements per day, CRP greater than 4.5 g/dL, deep ulcers on endoscopy, or albumin less than 3.0 g/dL have a higher likelihood of failing intravenous corticosteroid therapy, and these patients should be prepared for rescue therapy.2,21 A patient has failed intravenous corticosteroids by day 3 if they have sustained fever in the absence of an infection, continued CRP elevation or lack of CRP decrease, or ongoing high stool frequency, bleeding, and pain with less than 50% improvement from baseline on admission.8 In the setting of nonresponse to intravenous corticosteroids, it is prudent to involve colorectal surgery to discuss colectomy as an option of equal merit to medical salvage therapies such as infliximab or cyclosporine.
Infliximab is the most readily available rescue therapy for steroid-refractory patients and has been shown to increase colectomy-free survival in patients with ASUC.8 However, patients with the same predictors for intravenous steroid failures (low albumin, high CRP, and/or deep ulcers on endoscopy) are also at the highest risk for infliximab nonresponse. These factors are important to discuss with the patients and colorectal surgery teams when providing the options of treatment strategy, particularly with medication dosing. ASUC with more severe disease biochemically (low albumin, elevated CRP, possibly bandemia) benefit from a higher dose of infliximab at 10 mg/kg, given the likelihood of increased drug clearance in this situation.22,23
From a practical standpoint, it is important to confirm the patient’s insurance status prior to medication administration to make sure therapy can be continued after hospital discharge. Early involvement of the social workers and case coordinators is key to ensuring timely administration of the next dose of treatment. Patients who receive infliximab rescue therapy should be monitored for an additional 1-2 days after administration to ensure they are responding to this therapy with continued monitoring of CRP and symptoms during this period. If there is no response at this point, an additional dose of infliximab may be considered but surgery should not be delayed if there is no meaningful response after the first dose.
Another option for intravenous corticosteroid nonresponders is intravenous cyclosporine because treatment failure rates for cyclosporine and infliximab were similar in head-to-head studies.24 However, patient selection is key to successful utilization of this agent. Unlike infliximab, cyclosporine is primarily an induction agent for steroid nonresponders rather than a maintenance strategy. Therefore, in patients in whom cyclosporine is being considered, thiopurines or vedolizumab are potential options for maintenance therapy. If the patient has poor renal function, low cholesterol, advanced age, significant comorbidities, or a history of nonadherence to therapy, cyclosporine should not be given. Additionally, clinical experience with intravenous cyclosporine administration and monitoring both during inpatient and outpatient care settings should be factored into the decision making for infliximab versus cyclosporine.8
Day 5 and beyond – Discharge planning
Patients who have responded to the initial intravenous steroid course by hospital day 5 should have successfully transitioned to oral steroids with plans to start an appropriate steroid-sparing therapy shortly after discharge. Treatment planning should commence prior to discharge and should be communicated with the outpatient GI team to ensure a smooth transition to the ambulatory care setting, primarily to begin insurance authorizations as soon as possible. If the patient has had a meaningful response to infliximab rescue therapy (improvement by more than 50% in bowel frequency, amount of blood, abdominal pain), discharge planning needs to prioritize obtaining authorization for the second dose within 2 weeks of the initial infusion. These patients are high risk for readmission, and close outpatient follow-up by the ambulatory GI care team is necessary to help direct the tapering of steroids and monitor response to treatment.
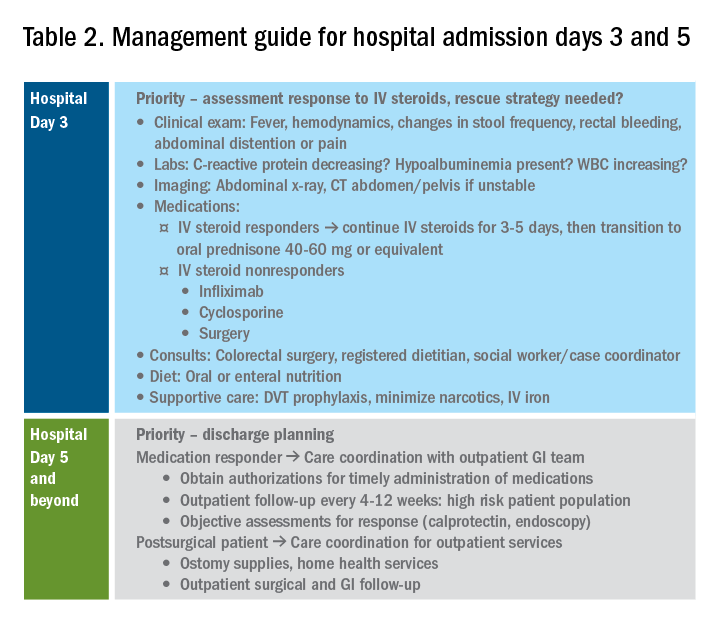
If the patient has not responded to intravenous steroid therapy, infliximab, or cyclosporine by day 5-7, then surgery should be strongly considered. Delaying surgery may worsen outcomes as patients become more malnourished, anemic, and continue to receive intravenous steroids. Additional preoperative optimization may be required depending on the patient’s course up to this point (Table 2).
Summary
The cornerstones of inpatient UC management center on a thorough initial evaluation including imaging and endoscopy as appropriate, establishment of baseline parameters, and daily assessment of response to therapy through a combination of patient-reported outcomes and biomarkers of inflammation. With this strategy in mind, practitioners and care teams can manage these complex patients using a consistent strategy focusing on multidisciplinary, evidence-based care.
References
1. Truelove SC et al. Br Med J. 1955 Oct 23;2(4947):1041-8.
2. Ho GT et al. Aliment Pharmacol Ther. 2004 May 15;19(10):1079-87.
3. Tinsley A et al. Scand J Gastroenterol. 2015;50(9):1103-9.
4. Issa M et al. Clin Gastroenterol Hepatol. 2007 Mar;5(3):345-51.
5. Ananthakrishnan AN et al. Gut. 2008 Feb;57(2):205-10.
6. Negron ME et al. Am J Gastroenterol. 2016 May;111(5):691-704.
7. Taylor KN et al. Gynecol Oncol. 2017 Feb;144(2):428-37.
8. Rubin DT et al. Am J Gastroenterol. 2019 Mar;114(3):384-413.
9. Jalan KN et al. Gastroenterology. 1969 Jul;57(1):68-82.
10. Gan SI et al. Am J Gastroenterol. 2003 Nov;98(11):2363-71.
11. Makkar R et al. Gastroenterol Hepatol (N Y). 2013 Sep;9(9):573-83.
12. Hindryckx P et al. Nat Rev Gastroenterol Hepatol. 2016 Nov;13(11):654-64.
13. Yerushalmy-Feler A et al. Curr Infect Dis Rep. 2019 Feb 15;21(2):5.
14. Shukla T et al. J Clin Gastroenterol. 2017 May/Jun;51(5):394-401.
15. McCurdy JD et al. Clin Gastroenterol Hepatol. 2015 Jan;13(1):131-7; quiz e7.
16. Cottone M et al. Am J Gastroenterol. 2001 Mar;96(3):773-5.
17. Nguyen GC et al. Gastroenterology. 2014 Mar;146(3):835-48 e6.
18. Limsrivilai J et al. Clin Gastroenterol Hepatol. 2017 Mar;15(3):385-92 e2.
19. Targownik LE et al. Am J Gastroenterol. 2014 Oct;109(10):1613-20.
20. Takeuchi K et al. Clin Gastroenterol Hepatol. 2006 Feb;4(2):196-202.
21. Travis SP et al. Gut. 1996 Jun;38(6):905-10.
22. Syal G et al. Mo1891 - Gastroenterology. 2018;154:S841.
23. Ungar B et al. Aliment Pharmacol Ther. 2016 Jun;43(12):1293-9.
24. Laharie D et al. Lancet 2012 Dec 1;380(9857):1909-15.
Dr. Chiplunker is an advanced inflammatory bowel disease fellow; Dr. Ha is associate professor of medicine at the Inflammatory Bowel Disease Center at Cedars-Sinai Medical Center, Los Angeles.
Introduction
Inpatient management of acute ulcerative colitis (UC) flares can be challenging because of the multiple patient and disease-related factors influencing therapeutic decision making. The clinical course during the first 24-72 hours of the hospitalization will likely guide the decision between rescue medical and surgical therapy. Using available evidence from clinical practice guidelines, we present a day-by-day guide to managing most hospitalized UC patients.
Day 0 – The emergency department (ED)
When an UC patient presents to the ED for evaluation, the initial assessments should focus on the acuity and severity of the flare. Key clinical features of disease severity include the presence of fever, tachycardia, hypotension, or weight loss in addition to worsened gastrointestinal symptoms of stool frequency relative to baseline, rectal bleeding, and abdominal pain. Acute severe ulcerative colitis (ASUC) is often defined using the modified Truelove and Witts criteria.1 A patient meets criteria for ASUC if they have at least six bloody stools per day and at least one sign of systemic toxicity, such as heart rate greater than 90 bpm, temperature at or above 37.8° C, hemoglobin level below 10.5 g/dL, or elevated inflammatory markers.
Initial laboratory assessments should include complete blood counts to identify anemia, potential superimposed infection, or toxicity and a comprehensive metabolic profile to evaluate for dehydration, electrolyte abnormalities, hepatic injury or hypoalbuminemia (an important predictor of surgery), as well as assessment of response to treatment and readmission.2,3 An evaluation at admission of C-reactive protein (CRP) is crucial because changes from the initial value will determine steroid response and predict need for surgical intervention or rescue therapy. A baseline fecal calprotectin can serve as a noninvasive marker that can be followed after discharge to monitor response to therapy.
Clostridioides difficile infection (CDI) must be ruled out in all patients presenting with ASUC regardless of history of antibiotic use or prior negative testing. Concomitant UC and CDI are associated with a four- to sixfold increased risk of in-hospital mortality and a two- to sixfold increased risk of bowel surgery.4-6 Immunoassay testing is inexpensive and fast with a high specificity but has low sensitivity; nucleic acid amplification testing with polymerase chain reaction has a high sensitivity and specificity.7 Knowing which testing algorithm the hospital lab uses helps guide interpretation of results.
For patients meeting criteria for ASUC, obtaining at least an abdominal x-ray is important to assess for colonic dilation to further stratify the patient by risk. Colonic dilation, defined as a transverse colon diameter greater than 5.5 cm, places the patient in the category of fulminant colitis and colorectal surgical consultation should be obtained.8 A CT scan is often ordered first because it can provide a rapid assessment of intra-abdominal processes but is not routinely needed unless hemodynamic instability, an acute abdomen, or markedly abnormal laboratory testing (specifically white blood cell count with bandemia) is present as these can be indicators of toxic megacolon or perforation.8-10
Day 1 – Assess disease severity and assemble the team
Obtaining a thorough clinical history is essential to classify disease severity and identify potential triggers for the acute exacerbation. Potential triggers may include infections, new medications, recent antibiotic use, recent travel, sick contacts, or cessation of treatments. Standard questions include asking about the timing of onset of symptoms, bowel movements during a 24-hour period, and particularly the presence of nocturnal bowel movements. If patients report bloody stools, inquire how often they see blood relative to the total number of bowel movements. The presence and nature of abdominal pain should be elicited, particularly changes in abdominal pain and comparison with previous disease flares. These clinical parameters are used to assess response to treatment; therefore, ask patients to keep a log of their stool frequency, consistency, rectal urgency, and bleeding each day to report to the team during daily rounds.
For patients with ASUC, a full colonoscopy is rarely indicated in the inpatient setting because it is unlikely to change management and poses a risk of perforation.11 However, a sigmoidoscopy within the first 24 hours of admission will provide useful information about the endoscopic disease activity, particularly if features such as deep or well-like ulcers, large mucosal abrasions, or extensive loss of the mucosal layer are present because these are predictors of colectomy.8 Tissue biopsies can exclude cytomegalovirus (CMV) infection, an important consideration for patients on immunosuppression including corticosteroids.12-16
Venous thromboembolism (VTE) prophylaxis is extremely important for hospitalized inflammatory bowel disease (IBD) patients. At baseline, IBD patients have a threefold higher risk of VTE than do non-IBD patients, which increases to approximately sixfold during flares.17 Pharmacologic VTE prophylaxis is recommended for all hospitalized IBD patients, even those with rectal bleeding. This may seem counterintuitive in the setting of “GI bleeding,” so it is important to counsel both patients and team members regarding VTE risks and the role of the prophylactic regimen to ensure adherence. Mechanical VTE prophylaxis can be used in patients with severe bleeding and hemodynamic instability until pharmacologic VTE prophylaxis can be safely initiated.17
Narcotics should be used sparingly for hospitalized IBD patients. Narcotic use is associated with greater likelihood of subsequent IBD hospitalizations, ED visits, and higher costs of health care for patients with IBD.18 Heavy use of opiates, defined as continuous use for more than 30 days at a dose exceeding 50 mg morphine per day or equivalent, was strongly associated with an increased overall mortality in IBD patients.19 Opiates also slow bowel motility and precipitate toxic megacolon, along with any other agent that slows bowel motility, such as anticholinergic medications.8 These agents may also mask bowel frequency symptoms that would otherwise indicate a failure of medical therapy. Similarly, use of NSAIDS should also be avoided because these have been associated with disease relapse and escalating intestinal inflammation.20
Once disease severity has been determined, intravenous corticosteroid therapy may be initiated, ideally once CDI and CMV have been excluded. The recommended dosing of intravenous corticosteroids is methylprednisolone 20 mg IV every 8 hours or equivalent. There is no evidence to support additional benefit for doses exceeding these amounts.8 Prior to starting parenteral corticosteroids, it is important to keep in mind the possible need for rescue therapy during the admission. Recommended testing includes hepatitis B surface antigen and antibody, hepatitis B core antibody and tuberculosis testing if there is no documented negative testing within the past 6-12 months. These labs should be drawn prior to steroid treatment to avoid delays in care and indeterminate results. Finally, a lipid profile is recommended for patients who may be cyclosporine candidates pending response to intravenous corticosteroids. Unless the patient has been admitted with a bowel obstruction, which should raise the suspicion that the diagnosis is actually Crohn’s disease, enteral feeding is preferred for UC patients even if they may have significant food aversion. The early involvement of a registered dietitian is valuable to guide dietary choices and recommend appropriate enteral nutrition supplements. During acute flares, patients may find a low-residue diet to be less stimulating to their gut while their acute flare is being treated. Electrolyte abnormalities should be repleted and consistently monitored during the hospitalization. Providing parenteral intravenous iron for anemic patients will expedite correction of the anemia alongside treatment of the underlying UC.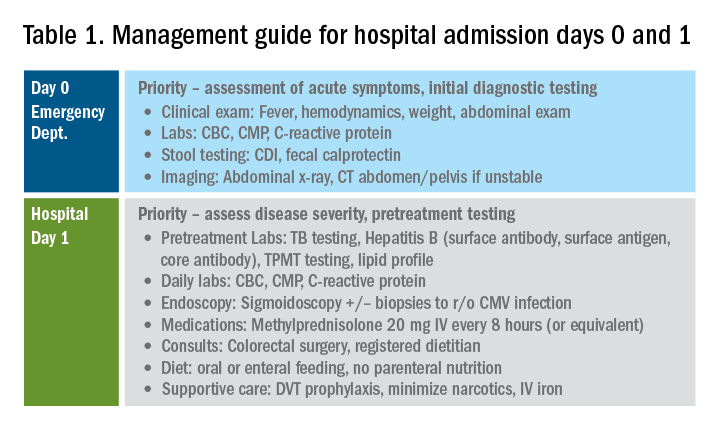
Most UC patients admitted to the hospital will require a multidisciplinary approach with gastroenterologists, surgeons, radiologists, dietitians, and case coordinators/social workers, among others. It is essential to assemble the team, especially the surgeons, earlier during the hospitalization rather than later. It is especially important to discuss the role of the surgeon in the management of UC and explain why the surgeon is being consulted in the context of the patient’s acute presentation. Being transparent about the parameters the GI team are monitoring to determine if and when surgery is the most appropriate and safe approach will improve patients’ acceptance of the surgical team’s role in their care. Specific indications for surgery in ASUC include toxic megacolon, colonic perforation, severe refractory hemorrhage, and failure to respond to medical therapy (Table 1).8
Day 3 – Assessing response to corticosteroids
In addition to daily symptom assessments, a careful abdominal exam should be performed every day with the understanding that steroids (and also narcotics) may mask perforation or pain. Any abrupt decrease or cessation of bowel movements, increasing abdominal distention, or a sudden increase in abdominal pain or tenderness may require abdominal imaging to ensure no interim perforation or severe colonic dilation has occurred while receiving steroid therapy. In these circumstances, the addition of broad spectrum intravenous antibiotics should be considered, particularly if hemodynamic instability (such as tachycardia) is present.
Patients should be assessed for response to intravenous steroid therapy after 3 days of treatment. A meaningful response to corticosteroids is present if the patient has had more than 50% improvement in symptoms, particularly rectal bleeding and stool frequency. A more than 75% improvement in CRP should also be noted from admission to day 3 with an overall trend of improvement.2,21 Additionally, patients should be afebrile, require minimal to no narcotic usage, tolerating oral intake, and be ambulatory. If the patient has met all these parameters, it is reasonable to transition to oral corticosteroids, such as prednisone 40-60 mg daily after a course of 3-5 days of intravenous corticosteroids. Ideally, patients should be observed for 24-48 hours in the hospital after transitioning to oral corticosteroids to make sure that symptoms do not worsen with the switch.
Patients with more than eight bowel movements per day, CRP greater than 4.5 g/dL, deep ulcers on endoscopy, or albumin less than 3.0 g/dL have a higher likelihood of failing intravenous corticosteroid therapy, and these patients should be prepared for rescue therapy.2,21 A patient has failed intravenous corticosteroids by day 3 if they have sustained fever in the absence of an infection, continued CRP elevation or lack of CRP decrease, or ongoing high stool frequency, bleeding, and pain with less than 50% improvement from baseline on admission.8 In the setting of nonresponse to intravenous corticosteroids, it is prudent to involve colorectal surgery to discuss colectomy as an option of equal merit to medical salvage therapies such as infliximab or cyclosporine.
Infliximab is the most readily available rescue therapy for steroid-refractory patients and has been shown to increase colectomy-free survival in patients with ASUC.8 However, patients with the same predictors for intravenous steroid failures (low albumin, high CRP, and/or deep ulcers on endoscopy) are also at the highest risk for infliximab nonresponse. These factors are important to discuss with the patients and colorectal surgery teams when providing the options of treatment strategy, particularly with medication dosing. ASUC with more severe disease biochemically (low albumin, elevated CRP, possibly bandemia) benefit from a higher dose of infliximab at 10 mg/kg, given the likelihood of increased drug clearance in this situation.22,23
From a practical standpoint, it is important to confirm the patient’s insurance status prior to medication administration to make sure therapy can be continued after hospital discharge. Early involvement of the social workers and case coordinators is key to ensuring timely administration of the next dose of treatment. Patients who receive infliximab rescue therapy should be monitored for an additional 1-2 days after administration to ensure they are responding to this therapy with continued monitoring of CRP and symptoms during this period. If there is no response at this point, an additional dose of infliximab may be considered but surgery should not be delayed if there is no meaningful response after the first dose.
Another option for intravenous corticosteroid nonresponders is intravenous cyclosporine because treatment failure rates for cyclosporine and infliximab were similar in head-to-head studies.24 However, patient selection is key to successful utilization of this agent. Unlike infliximab, cyclosporine is primarily an induction agent for steroid nonresponders rather than a maintenance strategy. Therefore, in patients in whom cyclosporine is being considered, thiopurines or vedolizumab are potential options for maintenance therapy. If the patient has poor renal function, low cholesterol, advanced age, significant comorbidities, or a history of nonadherence to therapy, cyclosporine should not be given. Additionally, clinical experience with intravenous cyclosporine administration and monitoring both during inpatient and outpatient care settings should be factored into the decision making for infliximab versus cyclosporine.8
Day 5 and beyond – Discharge planning
Patients who have responded to the initial intravenous steroid course by hospital day 5 should have successfully transitioned to oral steroids with plans to start an appropriate steroid-sparing therapy shortly after discharge. Treatment planning should commence prior to discharge and should be communicated with the outpatient GI team to ensure a smooth transition to the ambulatory care setting, primarily to begin insurance authorizations as soon as possible. If the patient has had a meaningful response to infliximab rescue therapy (improvement by more than 50% in bowel frequency, amount of blood, abdominal pain), discharge planning needs to prioritize obtaining authorization for the second dose within 2 weeks of the initial infusion. These patients are high risk for readmission, and close outpatient follow-up by the ambulatory GI care team is necessary to help direct the tapering of steroids and monitor response to treatment.
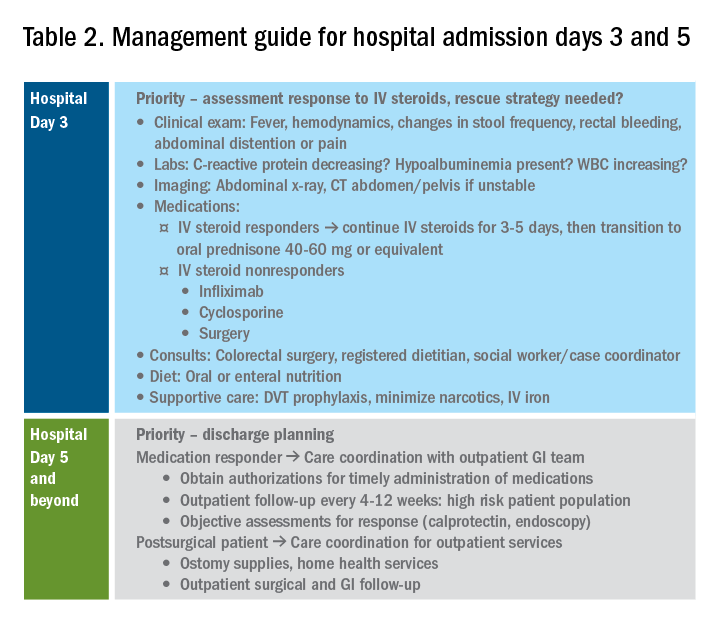
If the patient has not responded to intravenous steroid therapy, infliximab, or cyclosporine by day 5-7, then surgery should be strongly considered. Delaying surgery may worsen outcomes as patients become more malnourished, anemic, and continue to receive intravenous steroids. Additional preoperative optimization may be required depending on the patient’s course up to this point (Table 2).
Summary
The cornerstones of inpatient UC management center on a thorough initial evaluation including imaging and endoscopy as appropriate, establishment of baseline parameters, and daily assessment of response to therapy through a combination of patient-reported outcomes and biomarkers of inflammation. With this strategy in mind, practitioners and care teams can manage these complex patients using a consistent strategy focusing on multidisciplinary, evidence-based care.
References
1. Truelove SC et al. Br Med J. 1955 Oct 23;2(4947):1041-8.
2. Ho GT et al. Aliment Pharmacol Ther. 2004 May 15;19(10):1079-87.
3. Tinsley A et al. Scand J Gastroenterol. 2015;50(9):1103-9.
4. Issa M et al. Clin Gastroenterol Hepatol. 2007 Mar;5(3):345-51.
5. Ananthakrishnan AN et al. Gut. 2008 Feb;57(2):205-10.
6. Negron ME et al. Am J Gastroenterol. 2016 May;111(5):691-704.
7. Taylor KN et al. Gynecol Oncol. 2017 Feb;144(2):428-37.
8. Rubin DT et al. Am J Gastroenterol. 2019 Mar;114(3):384-413.
9. Jalan KN et al. Gastroenterology. 1969 Jul;57(1):68-82.
10. Gan SI et al. Am J Gastroenterol. 2003 Nov;98(11):2363-71.
11. Makkar R et al. Gastroenterol Hepatol (N Y). 2013 Sep;9(9):573-83.
12. Hindryckx P et al. Nat Rev Gastroenterol Hepatol. 2016 Nov;13(11):654-64.
13. Yerushalmy-Feler A et al. Curr Infect Dis Rep. 2019 Feb 15;21(2):5.
14. Shukla T et al. J Clin Gastroenterol. 2017 May/Jun;51(5):394-401.
15. McCurdy JD et al. Clin Gastroenterol Hepatol. 2015 Jan;13(1):131-7; quiz e7.
16. Cottone M et al. Am J Gastroenterol. 2001 Mar;96(3):773-5.
17. Nguyen GC et al. Gastroenterology. 2014 Mar;146(3):835-48 e6.
18. Limsrivilai J et al. Clin Gastroenterol Hepatol. 2017 Mar;15(3):385-92 e2.
19. Targownik LE et al. Am J Gastroenterol. 2014 Oct;109(10):1613-20.
20. Takeuchi K et al. Clin Gastroenterol Hepatol. 2006 Feb;4(2):196-202.
21. Travis SP et al. Gut. 1996 Jun;38(6):905-10.
22. Syal G et al. Mo1891 - Gastroenterology. 2018;154:S841.
23. Ungar B et al. Aliment Pharmacol Ther. 2016 Jun;43(12):1293-9.
24. Laharie D et al. Lancet 2012 Dec 1;380(9857):1909-15.
Dr. Chiplunker is an advanced inflammatory bowel disease fellow; Dr. Ha is associate professor of medicine at the Inflammatory Bowel Disease Center at Cedars-Sinai Medical Center, Los Angeles.
A sepsis death linked to fecal microbiota transplantation
Two cases of bacteremia have been described in two patients who received fecal microbiota transplants from the same donor.
Writing in the New England Journal of Medicine, researchers reported the two case studies of extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli bacteremia, one of which ended in the death of the patient. These cases were previously announced by the Food and Drug Administration in a June 2019 safety alert.
Zachariah DeFilipp, MD, from Massachusetts General Hospital at Harvard Medical School, Boston, and coauthors wrote that fecal microbiota transplantation is rarely associated with complications. Placebo-controlled trials and a systematic review have found similar rates of complications in immunocompromised and immunocompetent recipients. Only four cases of gram-negative bacteremia previously have been reported, and in three of these, there was a plausible alternative explanation for the bacteremia.
In this paper, both patients received fecal microbiota transplantation via frozen oral capsules containing donor stool. These capsules were prepared prior to the implementation of screening for ESBL-producing organisms at the institution, and were not retrospectively tested since this expanded donor screening.
The first patient was a 69-year-old man with liver cirrhosis attributed to hepatitis C infection who was enrolled in a trial of fecal microbiota transplantation via oral capsules to treat hepatic encephalopathy. The first sign of the adverse event was a fever and cough, which developed 17 days after the final dose of 15 capsules. He was treated for pneumonia but failed to improve after 2 days, at which time gram-negative rods were discovered in blood cultures taken at the initial presentation.
After admission and further treatment, blood cultures were found to have ESBL-producing E. coli, and after further treatment, the patient was clinically stable. A stool sample taken after treatment was negative for ESBL-producing E. coli.
The second case study was a 73-year-old man with therapy-related myelodysplastic syndrome who was undergoing allogeneic hematopoietic stem cell transplantation and was receiving fecal microbiota transplantation via oral capsule as part of a phase 2 trial.
Eight days after the last dose of oral capsules, and 5 days after the stem-cell infusion, the man developed a fever, chills, febrile neutropenia and showed altered mental status. He was treated with cefepime but developed hypoxia and labored breathing later that evening, which prompted clinicians to intubate and begin mechanical ventilation.
His blood culture results showed gram-negative rods, and meropenem was added to his antibiotic regimen. However, the patient’s condition worsened, and he died of severe sepsis 2 days later with blood cultures confirmed as positive for ESBL-producing E. coli.
A follow-up investigation revealed that both patients received stool from the same donor. Each lot of three capsules from that donor was found to contain ESBL-producing E. coli with a resistance pattern similar to that seen in the two recipients.
Twenty-two patients had received capsules from this donor. Researchers contacted all the recipients and offered them stool screening for ESBL-producing E. coli. Twelve underwent testing, which found that five had samples that grew on ESBL-producing E. coli–selective medium.
The remaining seven patients who had follow-up testing were receiving treatment for recurrent or refractory Clostridioides difficile infection, and four of these grew samples on the selective medium.
“When FMT is successful, the recipient’s metagenomic burden of antimicrobial resistance genes mimics that of the donor,” the authors wrote. “Although we cannot conclusively attribute positive screening results for ESBL-producing organisms in other asymptomatic recipients to FMT, the rates of positive tests are, in our opinion, unexpectedly high and probably represent transmission through FMT.”
The authors said the donor had no risk factors for carriage of multidrug-resistant organism and had previously donated fecal material before the introduction of routine screening for ESBL-producing organisms.
However, they noted that both patients had risk factors for bacteremia, namely advanced cirrhosis and allogeneic hematopoietic stem cell transplantation and they also received oral antibiotics around the time of the fecal microbiota transplantation.
“Despite the infectious complications reported here, the benefits of FMT should be balanced with the associated risks when considering treatment options for patients with recurrent or refractory C. difficile infection,” the authors wrote. “Ongoing assessment of the risks and benefit of FMT research is needed, as are continuing efforts to improve donor screening to limit transmission of microorganisms that could lead to adverse infectious events.”
The American Gastroenterological Association FMT National Registry is a critical effort to track short- and long-term patient outcomes and potential risks associated with FMT. The registry's goal is to track 4,000 patients for 10 years. If you perform FMT, please contribute to this important initiative. Learn more at www.gastro.org/FMTRegistry.
The study was supported by a grant from the American College of Gastroenterology. Three authors declared personal fees and grants from the medical sector outside the submitted work, and two were attached to a diagnostics company involved in the study.
SOURCE: DeFilipp Z et al. N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMoa1910437.
* This story was updated on Oct. 31, 2019.
Fecal microbiota transplantation could have therapeutic utility in a range of conditions in which primary dysbiosis is suspected, but this study shows the procedure may carry risks that only become apparent after treatment. Improved screening of donors and fecal material could reduce the risks of infections by known agents. However, new pathogens may not be recognized until after they have been transplanted into a new host.
The benefits and risks of fecal microbiota transplantation must be balanced, but up to now the complications have been infrequent and the benefits have clearly outweighed the risks.
Martin J. Blaser, MD, is from Rutgers University in New Brunswick, N.J. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMe1913807). Dr. Blaser declared personal fees and stock options from the medical sector unrelated to the work.
Fecal microbiota transplantation could have therapeutic utility in a range of conditions in which primary dysbiosis is suspected, but this study shows the procedure may carry risks that only become apparent after treatment. Improved screening of donors and fecal material could reduce the risks of infections by known agents. However, new pathogens may not be recognized until after they have been transplanted into a new host.
The benefits and risks of fecal microbiota transplantation must be balanced, but up to now the complications have been infrequent and the benefits have clearly outweighed the risks.
Martin J. Blaser, MD, is from Rutgers University in New Brunswick, N.J. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMe1913807). Dr. Blaser declared personal fees and stock options from the medical sector unrelated to the work.
Fecal microbiota transplantation could have therapeutic utility in a range of conditions in which primary dysbiosis is suspected, but this study shows the procedure may carry risks that only become apparent after treatment. Improved screening of donors and fecal material could reduce the risks of infections by known agents. However, new pathogens may not be recognized until after they have been transplanted into a new host.
The benefits and risks of fecal microbiota transplantation must be balanced, but up to now the complications have been infrequent and the benefits have clearly outweighed the risks.
Martin J. Blaser, MD, is from Rutgers University in New Brunswick, N.J. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMe1913807). Dr. Blaser declared personal fees and stock options from the medical sector unrelated to the work.
Two cases of bacteremia have been described in two patients who received fecal microbiota transplants from the same donor.
Writing in the New England Journal of Medicine, researchers reported the two case studies of extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli bacteremia, one of which ended in the death of the patient. These cases were previously announced by the Food and Drug Administration in a June 2019 safety alert.
Zachariah DeFilipp, MD, from Massachusetts General Hospital at Harvard Medical School, Boston, and coauthors wrote that fecal microbiota transplantation is rarely associated with complications. Placebo-controlled trials and a systematic review have found similar rates of complications in immunocompromised and immunocompetent recipients. Only four cases of gram-negative bacteremia previously have been reported, and in three of these, there was a plausible alternative explanation for the bacteremia.
In this paper, both patients received fecal microbiota transplantation via frozen oral capsules containing donor stool. These capsules were prepared prior to the implementation of screening for ESBL-producing organisms at the institution, and were not retrospectively tested since this expanded donor screening.
The first patient was a 69-year-old man with liver cirrhosis attributed to hepatitis C infection who was enrolled in a trial of fecal microbiota transplantation via oral capsules to treat hepatic encephalopathy. The first sign of the adverse event was a fever and cough, which developed 17 days after the final dose of 15 capsules. He was treated for pneumonia but failed to improve after 2 days, at which time gram-negative rods were discovered in blood cultures taken at the initial presentation.
After admission and further treatment, blood cultures were found to have ESBL-producing E. coli, and after further treatment, the patient was clinically stable. A stool sample taken after treatment was negative for ESBL-producing E. coli.
The second case study was a 73-year-old man with therapy-related myelodysplastic syndrome who was undergoing allogeneic hematopoietic stem cell transplantation and was receiving fecal microbiota transplantation via oral capsule as part of a phase 2 trial.
Eight days after the last dose of oral capsules, and 5 days after the stem-cell infusion, the man developed a fever, chills, febrile neutropenia and showed altered mental status. He was treated with cefepime but developed hypoxia and labored breathing later that evening, which prompted clinicians to intubate and begin mechanical ventilation.
His blood culture results showed gram-negative rods, and meropenem was added to his antibiotic regimen. However, the patient’s condition worsened, and he died of severe sepsis 2 days later with blood cultures confirmed as positive for ESBL-producing E. coli.
A follow-up investigation revealed that both patients received stool from the same donor. Each lot of three capsules from that donor was found to contain ESBL-producing E. coli with a resistance pattern similar to that seen in the two recipients.
Twenty-two patients had received capsules from this donor. Researchers contacted all the recipients and offered them stool screening for ESBL-producing E. coli. Twelve underwent testing, which found that five had samples that grew on ESBL-producing E. coli–selective medium.
The remaining seven patients who had follow-up testing were receiving treatment for recurrent or refractory Clostridioides difficile infection, and four of these grew samples on the selective medium.
“When FMT is successful, the recipient’s metagenomic burden of antimicrobial resistance genes mimics that of the donor,” the authors wrote. “Although we cannot conclusively attribute positive screening results for ESBL-producing organisms in other asymptomatic recipients to FMT, the rates of positive tests are, in our opinion, unexpectedly high and probably represent transmission through FMT.”
The authors said the donor had no risk factors for carriage of multidrug-resistant organism and had previously donated fecal material before the introduction of routine screening for ESBL-producing organisms.
However, they noted that both patients had risk factors for bacteremia, namely advanced cirrhosis and allogeneic hematopoietic stem cell transplantation and they also received oral antibiotics around the time of the fecal microbiota transplantation.
“Despite the infectious complications reported here, the benefits of FMT should be balanced with the associated risks when considering treatment options for patients with recurrent or refractory C. difficile infection,” the authors wrote. “Ongoing assessment of the risks and benefit of FMT research is needed, as are continuing efforts to improve donor screening to limit transmission of microorganisms that could lead to adverse infectious events.”
The American Gastroenterological Association FMT National Registry is a critical effort to track short- and long-term patient outcomes and potential risks associated with FMT. The registry's goal is to track 4,000 patients for 10 years. If you perform FMT, please contribute to this important initiative. Learn more at www.gastro.org/FMTRegistry.
The study was supported by a grant from the American College of Gastroenterology. Three authors declared personal fees and grants from the medical sector outside the submitted work, and two were attached to a diagnostics company involved in the study.
SOURCE: DeFilipp Z et al. N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMoa1910437.
* This story was updated on Oct. 31, 2019.
Two cases of bacteremia have been described in two patients who received fecal microbiota transplants from the same donor.
Writing in the New England Journal of Medicine, researchers reported the two case studies of extended-spectrum beta-lactamase (ESBL)–producing Escherichia coli bacteremia, one of which ended in the death of the patient. These cases were previously announced by the Food and Drug Administration in a June 2019 safety alert.
Zachariah DeFilipp, MD, from Massachusetts General Hospital at Harvard Medical School, Boston, and coauthors wrote that fecal microbiota transplantation is rarely associated with complications. Placebo-controlled trials and a systematic review have found similar rates of complications in immunocompromised and immunocompetent recipients. Only four cases of gram-negative bacteremia previously have been reported, and in three of these, there was a plausible alternative explanation for the bacteremia.
In this paper, both patients received fecal microbiota transplantation via frozen oral capsules containing donor stool. These capsules were prepared prior to the implementation of screening for ESBL-producing organisms at the institution, and were not retrospectively tested since this expanded donor screening.
The first patient was a 69-year-old man with liver cirrhosis attributed to hepatitis C infection who was enrolled in a trial of fecal microbiota transplantation via oral capsules to treat hepatic encephalopathy. The first sign of the adverse event was a fever and cough, which developed 17 days after the final dose of 15 capsules. He was treated for pneumonia but failed to improve after 2 days, at which time gram-negative rods were discovered in blood cultures taken at the initial presentation.
After admission and further treatment, blood cultures were found to have ESBL-producing E. coli, and after further treatment, the patient was clinically stable. A stool sample taken after treatment was negative for ESBL-producing E. coli.
The second case study was a 73-year-old man with therapy-related myelodysplastic syndrome who was undergoing allogeneic hematopoietic stem cell transplantation and was receiving fecal microbiota transplantation via oral capsule as part of a phase 2 trial.
Eight days after the last dose of oral capsules, and 5 days after the stem-cell infusion, the man developed a fever, chills, febrile neutropenia and showed altered mental status. He was treated with cefepime but developed hypoxia and labored breathing later that evening, which prompted clinicians to intubate and begin mechanical ventilation.
His blood culture results showed gram-negative rods, and meropenem was added to his antibiotic regimen. However, the patient’s condition worsened, and he died of severe sepsis 2 days later with blood cultures confirmed as positive for ESBL-producing E. coli.
A follow-up investigation revealed that both patients received stool from the same donor. Each lot of three capsules from that donor was found to contain ESBL-producing E. coli with a resistance pattern similar to that seen in the two recipients.
Twenty-two patients had received capsules from this donor. Researchers contacted all the recipients and offered them stool screening for ESBL-producing E. coli. Twelve underwent testing, which found that five had samples that grew on ESBL-producing E. coli–selective medium.
The remaining seven patients who had follow-up testing were receiving treatment for recurrent or refractory Clostridioides difficile infection, and four of these grew samples on the selective medium.
“When FMT is successful, the recipient’s metagenomic burden of antimicrobial resistance genes mimics that of the donor,” the authors wrote. “Although we cannot conclusively attribute positive screening results for ESBL-producing organisms in other asymptomatic recipients to FMT, the rates of positive tests are, in our opinion, unexpectedly high and probably represent transmission through FMT.”
The authors said the donor had no risk factors for carriage of multidrug-resistant organism and had previously donated fecal material before the introduction of routine screening for ESBL-producing organisms.
However, they noted that both patients had risk factors for bacteremia, namely advanced cirrhosis and allogeneic hematopoietic stem cell transplantation and they also received oral antibiotics around the time of the fecal microbiota transplantation.
“Despite the infectious complications reported here, the benefits of FMT should be balanced with the associated risks when considering treatment options for patients with recurrent or refractory C. difficile infection,” the authors wrote. “Ongoing assessment of the risks and benefit of FMT research is needed, as are continuing efforts to improve donor screening to limit transmission of microorganisms that could lead to adverse infectious events.”
The American Gastroenterological Association FMT National Registry is a critical effort to track short- and long-term patient outcomes and potential risks associated with FMT. The registry's goal is to track 4,000 patients for 10 years. If you perform FMT, please contribute to this important initiative. Learn more at www.gastro.org/FMTRegistry.
The study was supported by a grant from the American College of Gastroenterology. Three authors declared personal fees and grants from the medical sector outside the submitted work, and two were attached to a diagnostics company involved in the study.
SOURCE: DeFilipp Z et al. N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMoa1910437.
* This story was updated on Oct. 31, 2019.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Two cases of bacteremia – one fatal – have been linked to a fecal microbiota transplant.
Major finding: Two patients developed bacteremia after receiving a fecal microbiota transplant from the same donor.
Study details: Case studies.
Disclosures: The study was supported by a grant from the American College of Gastroenterology. Three authors declared personal fees and grants from the medical sector outside the submitted work, and two authors were attached to a diagnostics company involved in the study.
Source: DeFillip Z et al. N Engl J Med. 2019 Oct 30. doi: 10.1056/NEJMoa1910437.








