User login
With sexually transmitted infections off the charts, California pushes at-home tests
SACRAMENTO, CALIF. – California has become the first state to require health insurance plans to cover at-home tests for sexually transmitted infections such as HIV, chlamydia, and syphilis – which could help quell the STI epidemic that has raged nearly unchecked as public health departments have focused on COVID-19.
The rule, part of a broader law addressing the STI epidemic, took effect Jan. 1 for people with state-regulated private insurance plans and will kick in sometime later for the millions of low-income Californians enrolled in the state’s Medicaid program.
By making it easier and cheaper for Californians to self-administer tests in the privacy of their homes, the provision could bring better disease monitoring to rural and underserved parts of the state, reduce the stigma patients experience when seeking care, and give them more control over their health, say experts on infectious diseases.
“This is the first law of its kind, and I’d say it’s kind of cutting-edge,” said Stephanie Arnold Pang, senior director of policy and government relations for the National Coalition of STD Directors. “We want to bring down every single barrier for someone to get STI testing, and out-of-pocket cost is a huge factor.”
But being first has its downsides. Because the concept of insurance coverage for home STI tests is so new, the state’s Medicaid program, Medi-Cal, could not establish by Jan. 1 the billing codes it needs to start paying for tests. Federal regulators also haven’t approved the tests for home use, which could make labs reluctant to process them. And a state analysis predicts most in-network health care providers won’t start prescribing home tests for at least a year until they adjust their billing and other practices.
Nevertheless, the situation is urgent and requires action, said state Sen. Richard Pan (D-Sacramento), a pediatrician who wrote the law.
“We have children born in California with syphilis,” Dr. Pan said. “You’d think that went away in the Victorian era.”
Even before COVID, sexually transmitted infections hit all-time highs in the United States and California for 6 years in a row, according to 2019 data from the Centers for Disease Control and Prevention. Rates of congenital syphilis, which babies contract from their mothers, illustrate the severity of the STI epidemic: Cases were up 279% from 2015 to 2019 nationally and 232% in California. Of the 445 cases of congenital syphilis in California in 2019, 37 were stillbirths.
The pandemic only worsened the problem because health departments were overwhelmed responding to the COVID emergency, and stay-at-home orders kept people away from clinics.
In surveys of public health programs across the country since May 2020, the National Coalition of STD Directors found that most respondents – up to 78% in one survey – have diverted some of their STI workforces to test and monitor COVID. A report that accompanied the most recent survey found that some STIs were “completely unchecked” because of reductions in clinic hours, diversion of resources, shortages of testing kits and staff burnout.
Some at-home STI tests screen for a single disease but other kits can collect and send samples to check for a variety of infections. Depending on the test, patients collect a drop of blood with a lancet, or swab their mouth, vagina, anus, or penis.
Some tests require patients to send samples to a lab for analysis, while some oral HIV tests give results at home in a few minutes.
Ivan Beas, a 25-year-old graduate student at University of California, Los Angeles, was getting tested frequently as part of a 2-year research study. When clinics closed during the pandemic, researchers sent him a home kit.
The kit, which tests for HIV, hepatitis C, herpes, syphilis, chlamydia, gonorrhea, and trichomoniasis, was packaged discreetly and came with easy instructions. It took Mr. Beas about 10 minutes to prick his finger, swab his mouth and send the samples to the lab.
Mr. Beas wanted to continue screening himself every few months after the study ended, he said, but the kit he used retails for $289, which is out of reach for him.
The last time he went to a clinic in person, “I spent 2 hours waiting to even be seen by a doctor because of how busy they are,” he said. Until Medi-Cal begins covering home tests, he said, he will have to find time to get tested for free at a Planned Parenthood clinic.
“If insurance were to cover it, I’d definitely do it more,” he said.
Under California’s new law, plans regulated by the state must cover home STI tests when ordered by a health care provider.
Privately insured Californians can take advantage of the coverage immediately. How much they will owe out-of-pocket for the tests – if anything – depends on the type of plan they have, whether their provider is in-network, and whether they fall into a category the federal government has designated for free screening.
Medi-Cal patients almost never face out-of-pocket expenses, but they will have to wait for coverage because the Department of Health Care Services, which administers Medi-Cal, is working with the American Medical Association and the federal government to create billing codes. The reimbursement rates for those codes will then need federal approval.
The state doesn’t know how long that process will take, according to department spokesperson Anthony Cava.
The rule does not apply to the millions of Californians whose job-based health insurance plans are regulated by the federal government.
Other states and organizations have experimented with at-home STI tests. The public health departments in Alabama and the District of Columbia send free kits to residents who request them, but neither jurisdiction requires insurance coverage for them. The National Coalition of STD Directors is sending free kits to people through health departments in Philadelphia; Iowa; Virginia; Indiana; Puerto Rico; and Navajo County, Arizona. The list of recipients is expected to grow this month.
Iwantthekit.org, a project of Johns Hopkins University, has been sending free kits to Maryland residents since 2004, and to Alaskans since 2011. The program is funded by grants and works with local health departments.
Charlotte Gaydos, cofounder of the project, said that requests for test kits during the pandemic nearly tripled – and that she would expand to every state if she could bill insurance the way the California law mandates.
The tests fall into a murky regulatory area. While they have been approved by the Food and Drug Administration, none have been cleared for use at home. Patients are supposed to collect their own samples within the walls of a health facility, and some labs may not analyze samples collected at home.
Public health officials cited other potential challenges: Patients may not have the same access to counseling, treatment, or referrals to other services such as food banks that they would receive at clinics. And although patients are supposed to self-report the results of their tests to public health authorities, some people won’t follow through.
Vlad Carrillo, 31, experienced such trade-offs recently. Mr. Carrillo used to get tested at a San Francisco clinic, where they could get counseling and other services. But Carrillo lost their apartment during the pandemic and moved about 7 hours away to Bishop, the only incorporated city in rural Inyo County.
“Being away from the city, it took me a whole year to find a way to get tested,” Carrillo said.
Carrillo eventually got the kit through the mail, avoiding the stigma of going to the clinic in Bishop, which is “more focused on straight stuff,” like preventing pregnancy. Without the test, Carrillo couldn’t get PrEP, a medication to prevent HIV.
“Going without it for so long was really hard on me,” Carrillo said.
This story was produced by Kaiser Health News (KHN), which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO, CALIF. – California has become the first state to require health insurance plans to cover at-home tests for sexually transmitted infections such as HIV, chlamydia, and syphilis – which could help quell the STI epidemic that has raged nearly unchecked as public health departments have focused on COVID-19.
The rule, part of a broader law addressing the STI epidemic, took effect Jan. 1 for people with state-regulated private insurance plans and will kick in sometime later for the millions of low-income Californians enrolled in the state’s Medicaid program.
By making it easier and cheaper for Californians to self-administer tests in the privacy of their homes, the provision could bring better disease monitoring to rural and underserved parts of the state, reduce the stigma patients experience when seeking care, and give them more control over their health, say experts on infectious diseases.
“This is the first law of its kind, and I’d say it’s kind of cutting-edge,” said Stephanie Arnold Pang, senior director of policy and government relations for the National Coalition of STD Directors. “We want to bring down every single barrier for someone to get STI testing, and out-of-pocket cost is a huge factor.”
But being first has its downsides. Because the concept of insurance coverage for home STI tests is so new, the state’s Medicaid program, Medi-Cal, could not establish by Jan. 1 the billing codes it needs to start paying for tests. Federal regulators also haven’t approved the tests for home use, which could make labs reluctant to process them. And a state analysis predicts most in-network health care providers won’t start prescribing home tests for at least a year until they adjust their billing and other practices.
Nevertheless, the situation is urgent and requires action, said state Sen. Richard Pan (D-Sacramento), a pediatrician who wrote the law.
“We have children born in California with syphilis,” Dr. Pan said. “You’d think that went away in the Victorian era.”
Even before COVID, sexually transmitted infections hit all-time highs in the United States and California for 6 years in a row, according to 2019 data from the Centers for Disease Control and Prevention. Rates of congenital syphilis, which babies contract from their mothers, illustrate the severity of the STI epidemic: Cases were up 279% from 2015 to 2019 nationally and 232% in California. Of the 445 cases of congenital syphilis in California in 2019, 37 were stillbirths.
The pandemic only worsened the problem because health departments were overwhelmed responding to the COVID emergency, and stay-at-home orders kept people away from clinics.
In surveys of public health programs across the country since May 2020, the National Coalition of STD Directors found that most respondents – up to 78% in one survey – have diverted some of their STI workforces to test and monitor COVID. A report that accompanied the most recent survey found that some STIs were “completely unchecked” because of reductions in clinic hours, diversion of resources, shortages of testing kits and staff burnout.
Some at-home STI tests screen for a single disease but other kits can collect and send samples to check for a variety of infections. Depending on the test, patients collect a drop of blood with a lancet, or swab their mouth, vagina, anus, or penis.
Some tests require patients to send samples to a lab for analysis, while some oral HIV tests give results at home in a few minutes.
Ivan Beas, a 25-year-old graduate student at University of California, Los Angeles, was getting tested frequently as part of a 2-year research study. When clinics closed during the pandemic, researchers sent him a home kit.
The kit, which tests for HIV, hepatitis C, herpes, syphilis, chlamydia, gonorrhea, and trichomoniasis, was packaged discreetly and came with easy instructions. It took Mr. Beas about 10 minutes to prick his finger, swab his mouth and send the samples to the lab.
Mr. Beas wanted to continue screening himself every few months after the study ended, he said, but the kit he used retails for $289, which is out of reach for him.
The last time he went to a clinic in person, “I spent 2 hours waiting to even be seen by a doctor because of how busy they are,” he said. Until Medi-Cal begins covering home tests, he said, he will have to find time to get tested for free at a Planned Parenthood clinic.
“If insurance were to cover it, I’d definitely do it more,” he said.
Under California’s new law, plans regulated by the state must cover home STI tests when ordered by a health care provider.
Privately insured Californians can take advantage of the coverage immediately. How much they will owe out-of-pocket for the tests – if anything – depends on the type of plan they have, whether their provider is in-network, and whether they fall into a category the federal government has designated for free screening.
Medi-Cal patients almost never face out-of-pocket expenses, but they will have to wait for coverage because the Department of Health Care Services, which administers Medi-Cal, is working with the American Medical Association and the federal government to create billing codes. The reimbursement rates for those codes will then need federal approval.
The state doesn’t know how long that process will take, according to department spokesperson Anthony Cava.
The rule does not apply to the millions of Californians whose job-based health insurance plans are regulated by the federal government.
Other states and organizations have experimented with at-home STI tests. The public health departments in Alabama and the District of Columbia send free kits to residents who request them, but neither jurisdiction requires insurance coverage for them. The National Coalition of STD Directors is sending free kits to people through health departments in Philadelphia; Iowa; Virginia; Indiana; Puerto Rico; and Navajo County, Arizona. The list of recipients is expected to grow this month.
Iwantthekit.org, a project of Johns Hopkins University, has been sending free kits to Maryland residents since 2004, and to Alaskans since 2011. The program is funded by grants and works with local health departments.
Charlotte Gaydos, cofounder of the project, said that requests for test kits during the pandemic nearly tripled – and that she would expand to every state if she could bill insurance the way the California law mandates.
The tests fall into a murky regulatory area. While they have been approved by the Food and Drug Administration, none have been cleared for use at home. Patients are supposed to collect their own samples within the walls of a health facility, and some labs may not analyze samples collected at home.
Public health officials cited other potential challenges: Patients may not have the same access to counseling, treatment, or referrals to other services such as food banks that they would receive at clinics. And although patients are supposed to self-report the results of their tests to public health authorities, some people won’t follow through.
Vlad Carrillo, 31, experienced such trade-offs recently. Mr. Carrillo used to get tested at a San Francisco clinic, where they could get counseling and other services. But Carrillo lost their apartment during the pandemic and moved about 7 hours away to Bishop, the only incorporated city in rural Inyo County.
“Being away from the city, it took me a whole year to find a way to get tested,” Carrillo said.
Carrillo eventually got the kit through the mail, avoiding the stigma of going to the clinic in Bishop, which is “more focused on straight stuff,” like preventing pregnancy. Without the test, Carrillo couldn’t get PrEP, a medication to prevent HIV.
“Going without it for so long was really hard on me,” Carrillo said.
This story was produced by Kaiser Health News (KHN), which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
SACRAMENTO, CALIF. – California has become the first state to require health insurance plans to cover at-home tests for sexually transmitted infections such as HIV, chlamydia, and syphilis – which could help quell the STI epidemic that has raged nearly unchecked as public health departments have focused on COVID-19.
The rule, part of a broader law addressing the STI epidemic, took effect Jan. 1 for people with state-regulated private insurance plans and will kick in sometime later for the millions of low-income Californians enrolled in the state’s Medicaid program.
By making it easier and cheaper for Californians to self-administer tests in the privacy of their homes, the provision could bring better disease monitoring to rural and underserved parts of the state, reduce the stigma patients experience when seeking care, and give them more control over their health, say experts on infectious diseases.
“This is the first law of its kind, and I’d say it’s kind of cutting-edge,” said Stephanie Arnold Pang, senior director of policy and government relations for the National Coalition of STD Directors. “We want to bring down every single barrier for someone to get STI testing, and out-of-pocket cost is a huge factor.”
But being first has its downsides. Because the concept of insurance coverage for home STI tests is so new, the state’s Medicaid program, Medi-Cal, could not establish by Jan. 1 the billing codes it needs to start paying for tests. Federal regulators also haven’t approved the tests for home use, which could make labs reluctant to process them. And a state analysis predicts most in-network health care providers won’t start prescribing home tests for at least a year until they adjust their billing and other practices.
Nevertheless, the situation is urgent and requires action, said state Sen. Richard Pan (D-Sacramento), a pediatrician who wrote the law.
“We have children born in California with syphilis,” Dr. Pan said. “You’d think that went away in the Victorian era.”
Even before COVID, sexually transmitted infections hit all-time highs in the United States and California for 6 years in a row, according to 2019 data from the Centers for Disease Control and Prevention. Rates of congenital syphilis, which babies contract from their mothers, illustrate the severity of the STI epidemic: Cases were up 279% from 2015 to 2019 nationally and 232% in California. Of the 445 cases of congenital syphilis in California in 2019, 37 were stillbirths.
The pandemic only worsened the problem because health departments were overwhelmed responding to the COVID emergency, and stay-at-home orders kept people away from clinics.
In surveys of public health programs across the country since May 2020, the National Coalition of STD Directors found that most respondents – up to 78% in one survey – have diverted some of their STI workforces to test and monitor COVID. A report that accompanied the most recent survey found that some STIs were “completely unchecked” because of reductions in clinic hours, diversion of resources, shortages of testing kits and staff burnout.
Some at-home STI tests screen for a single disease but other kits can collect and send samples to check for a variety of infections. Depending on the test, patients collect a drop of blood with a lancet, or swab their mouth, vagina, anus, or penis.
Some tests require patients to send samples to a lab for analysis, while some oral HIV tests give results at home in a few minutes.
Ivan Beas, a 25-year-old graduate student at University of California, Los Angeles, was getting tested frequently as part of a 2-year research study. When clinics closed during the pandemic, researchers sent him a home kit.
The kit, which tests for HIV, hepatitis C, herpes, syphilis, chlamydia, gonorrhea, and trichomoniasis, was packaged discreetly and came with easy instructions. It took Mr. Beas about 10 minutes to prick his finger, swab his mouth and send the samples to the lab.
Mr. Beas wanted to continue screening himself every few months after the study ended, he said, but the kit he used retails for $289, which is out of reach for him.
The last time he went to a clinic in person, “I spent 2 hours waiting to even be seen by a doctor because of how busy they are,” he said. Until Medi-Cal begins covering home tests, he said, he will have to find time to get tested for free at a Planned Parenthood clinic.
“If insurance were to cover it, I’d definitely do it more,” he said.
Under California’s new law, plans regulated by the state must cover home STI tests when ordered by a health care provider.
Privately insured Californians can take advantage of the coverage immediately. How much they will owe out-of-pocket for the tests – if anything – depends on the type of plan they have, whether their provider is in-network, and whether they fall into a category the federal government has designated for free screening.
Medi-Cal patients almost never face out-of-pocket expenses, but they will have to wait for coverage because the Department of Health Care Services, which administers Medi-Cal, is working with the American Medical Association and the federal government to create billing codes. The reimbursement rates for those codes will then need federal approval.
The state doesn’t know how long that process will take, according to department spokesperson Anthony Cava.
The rule does not apply to the millions of Californians whose job-based health insurance plans are regulated by the federal government.
Other states and organizations have experimented with at-home STI tests. The public health departments in Alabama and the District of Columbia send free kits to residents who request them, but neither jurisdiction requires insurance coverage for them. The National Coalition of STD Directors is sending free kits to people through health departments in Philadelphia; Iowa; Virginia; Indiana; Puerto Rico; and Navajo County, Arizona. The list of recipients is expected to grow this month.
Iwantthekit.org, a project of Johns Hopkins University, has been sending free kits to Maryland residents since 2004, and to Alaskans since 2011. The program is funded by grants and works with local health departments.
Charlotte Gaydos, cofounder of the project, said that requests for test kits during the pandemic nearly tripled – and that she would expand to every state if she could bill insurance the way the California law mandates.
The tests fall into a murky regulatory area. While they have been approved by the Food and Drug Administration, none have been cleared for use at home. Patients are supposed to collect their own samples within the walls of a health facility, and some labs may not analyze samples collected at home.
Public health officials cited other potential challenges: Patients may not have the same access to counseling, treatment, or referrals to other services such as food banks that they would receive at clinics. And although patients are supposed to self-report the results of their tests to public health authorities, some people won’t follow through.
Vlad Carrillo, 31, experienced such trade-offs recently. Mr. Carrillo used to get tested at a San Francisco clinic, where they could get counseling and other services. But Carrillo lost their apartment during the pandemic and moved about 7 hours away to Bishop, the only incorporated city in rural Inyo County.
“Being away from the city, it took me a whole year to find a way to get tested,” Carrillo said.
Carrillo eventually got the kit through the mail, avoiding the stigma of going to the clinic in Bishop, which is “more focused on straight stuff,” like preventing pregnancy. Without the test, Carrillo couldn’t get PrEP, a medication to prevent HIV.
“Going without it for so long was really hard on me,” Carrillo said.
This story was produced by Kaiser Health News (KHN), which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KHN is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Fossilized blood proteins from child illness may cause chalky teeth
FROM FRONTIERS IN PHYSIOLOGY
Researchers have identified a potential cause of molar hypomineralization (MH), or “chalky teeth,” an underrecognized condition affecting one in five children worldwide. The discovery could lead to preventive medical therapies to reduce dental caries and extractions, they said.
According to a team led by biochemist Michael J. Hubbard, BDS, PhD, professor in the department of medicine, dentistry, and health sciences at the University of Melbourne, the “groundbreaking” research found that the failure of enamel to adequately harden is associated with exposure to serum albumin while teeth are developing. The blood protein “poisons” the growth of mineral crystals rather than injure the cells that deposit enamel, they reported.
The investigators, including researchers from Chile, said their findings hold promise for better clinical management of MH and open a new door into research on the broader pathogenesis and causes of the condition.
“We hope this breakthrough will eventually lead to medical prevention of MH, prompting global health benefits including major reductions in childhood tooth decay,” they wrote in an article published online Dec. 21 in Frontiers in Physiology.
More than cosmetic
Chalky teeth, characterized by discolored enamel spots, are not merely a cosmetic problem. The condition can lead to severe toothache, painful eating, tooth decay, and even abscesses and extractions. Although its triggers have eluded dental research for a century, Dr. Hubbard’s group said fossilized blood proteins such as albumin in the tooth appear to be at least one cause.
Biochemical evidence indicates that serum albumin surrounding developing teeth is normally excluded from enamel, Dr. Hubbard said in an interview. “Given that albumin binds strongly to hydroxyapatite-based mineral and blocks its growth, we infer that the epithelial barrier – the enamel-forming cells termed ameloblasts and normally responsible for excluding albumin – must break down in places in response to medical triggers.”
This breach enables localized infiltration of albumin, which then blocks further hardening of soft, immature enamel, leading to residual spots or patches of chalky enamel once the tooth eventually erupts into the mouth. “In other words, we infer that chalky enamel spots coincide with localized breaches of an epithelial barrier that are triggered by yet-to-be determined systemic insults,” he said.
Joseph Brofsky, DMD, section head of pediatric dentistry at North Shore LIJ Cohen Children’s Medical Center of New York, in Queens, agreed that that the definitive cause of MH has evaded identification for a hundred years. However, he expressed skepticism about the fossilized blood protein hypothesis.
“That’s a long shot. It’s a possibility, and I’m not ruling it out, but we’re not 100% sure,” said Dr. Brofsky, who was not involved in the research.
In his experience, MH is somewhat less prevalent in the United States, affecting about 1 in 10 children here, which is about half the global rate. “But it’s a problem, and we wish it would go away, but before we know beyond a reasonable doubt what causes this condition, it’s going to be hard to stop it.”
Most cases of MH involve hypomineralization of the 6-year molars, the first adult molars to erupt, but the process starts at birth. “For 6-year molars, normal hardening of dental enamel takes place from the early postnatal period through infancy,” Dr. Hubbard said.
The 2-year and 12-year molars are affected about half as frequently as their 6-year counterparts, “so this extends the medical-risk window out to early school days, and slightly back to the perinatal period for the 12-year and 2-year molars, respectively,” he said.
A critical question is which childhood illnesses are most likely to set the stage for MH, he added. “Forty-plus years of epidemiology have failed to nail a specific cause or causal association. But given the high prevalence of MH – 20% in otherwise healthy kids – naturally we suspect some common illnesses are the culprits,” he said. “But which diseases, which medications, and which combinations?”
Dr. Hubbard’s advice to pediatricians is to be alert to MH: “If you’re inspecting a child’s throat, then why not look at their back teeth, too – particularly when they’re getting their new molars at 2, 6, and 12 years?”
The study was supported by the Melbourne Research Unit for Facial Disorders Department of Pharmacology & Therapeutics, Department of Paediatrics, and Faculty of Medicine, Dentistry, and Health Sciences at the University of Melbourne. The authors and Dr. Brofsky have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN PHYSIOLOGY
Researchers have identified a potential cause of molar hypomineralization (MH), or “chalky teeth,” an underrecognized condition affecting one in five children worldwide. The discovery could lead to preventive medical therapies to reduce dental caries and extractions, they said.
According to a team led by biochemist Michael J. Hubbard, BDS, PhD, professor in the department of medicine, dentistry, and health sciences at the University of Melbourne, the “groundbreaking” research found that the failure of enamel to adequately harden is associated with exposure to serum albumin while teeth are developing. The blood protein “poisons” the growth of mineral crystals rather than injure the cells that deposit enamel, they reported.
The investigators, including researchers from Chile, said their findings hold promise for better clinical management of MH and open a new door into research on the broader pathogenesis and causes of the condition.
“We hope this breakthrough will eventually lead to medical prevention of MH, prompting global health benefits including major reductions in childhood tooth decay,” they wrote in an article published online Dec. 21 in Frontiers in Physiology.
More than cosmetic
Chalky teeth, characterized by discolored enamel spots, are not merely a cosmetic problem. The condition can lead to severe toothache, painful eating, tooth decay, and even abscesses and extractions. Although its triggers have eluded dental research for a century, Dr. Hubbard’s group said fossilized blood proteins such as albumin in the tooth appear to be at least one cause.
Biochemical evidence indicates that serum albumin surrounding developing teeth is normally excluded from enamel, Dr. Hubbard said in an interview. “Given that albumin binds strongly to hydroxyapatite-based mineral and blocks its growth, we infer that the epithelial barrier – the enamel-forming cells termed ameloblasts and normally responsible for excluding albumin – must break down in places in response to medical triggers.”
This breach enables localized infiltration of albumin, which then blocks further hardening of soft, immature enamel, leading to residual spots or patches of chalky enamel once the tooth eventually erupts into the mouth. “In other words, we infer that chalky enamel spots coincide with localized breaches of an epithelial barrier that are triggered by yet-to-be determined systemic insults,” he said.
Joseph Brofsky, DMD, section head of pediatric dentistry at North Shore LIJ Cohen Children’s Medical Center of New York, in Queens, agreed that that the definitive cause of MH has evaded identification for a hundred years. However, he expressed skepticism about the fossilized blood protein hypothesis.
“That’s a long shot. It’s a possibility, and I’m not ruling it out, but we’re not 100% sure,” said Dr. Brofsky, who was not involved in the research.
In his experience, MH is somewhat less prevalent in the United States, affecting about 1 in 10 children here, which is about half the global rate. “But it’s a problem, and we wish it would go away, but before we know beyond a reasonable doubt what causes this condition, it’s going to be hard to stop it.”
Most cases of MH involve hypomineralization of the 6-year molars, the first adult molars to erupt, but the process starts at birth. “For 6-year molars, normal hardening of dental enamel takes place from the early postnatal period through infancy,” Dr. Hubbard said.
The 2-year and 12-year molars are affected about half as frequently as their 6-year counterparts, “so this extends the medical-risk window out to early school days, and slightly back to the perinatal period for the 12-year and 2-year molars, respectively,” he said.
A critical question is which childhood illnesses are most likely to set the stage for MH, he added. “Forty-plus years of epidemiology have failed to nail a specific cause or causal association. But given the high prevalence of MH – 20% in otherwise healthy kids – naturally we suspect some common illnesses are the culprits,” he said. “But which diseases, which medications, and which combinations?”
Dr. Hubbard’s advice to pediatricians is to be alert to MH: “If you’re inspecting a child’s throat, then why not look at their back teeth, too – particularly when they’re getting their new molars at 2, 6, and 12 years?”
The study was supported by the Melbourne Research Unit for Facial Disorders Department of Pharmacology & Therapeutics, Department of Paediatrics, and Faculty of Medicine, Dentistry, and Health Sciences at the University of Melbourne. The authors and Dr. Brofsky have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN PHYSIOLOGY
Researchers have identified a potential cause of molar hypomineralization (MH), or “chalky teeth,” an underrecognized condition affecting one in five children worldwide. The discovery could lead to preventive medical therapies to reduce dental caries and extractions, they said.
According to a team led by biochemist Michael J. Hubbard, BDS, PhD, professor in the department of medicine, dentistry, and health sciences at the University of Melbourne, the “groundbreaking” research found that the failure of enamel to adequately harden is associated with exposure to serum albumin while teeth are developing. The blood protein “poisons” the growth of mineral crystals rather than injure the cells that deposit enamel, they reported.
The investigators, including researchers from Chile, said their findings hold promise for better clinical management of MH and open a new door into research on the broader pathogenesis and causes of the condition.
“We hope this breakthrough will eventually lead to medical prevention of MH, prompting global health benefits including major reductions in childhood tooth decay,” they wrote in an article published online Dec. 21 in Frontiers in Physiology.
More than cosmetic
Chalky teeth, characterized by discolored enamel spots, are not merely a cosmetic problem. The condition can lead to severe toothache, painful eating, tooth decay, and even abscesses and extractions. Although its triggers have eluded dental research for a century, Dr. Hubbard’s group said fossilized blood proteins such as albumin in the tooth appear to be at least one cause.
Biochemical evidence indicates that serum albumin surrounding developing teeth is normally excluded from enamel, Dr. Hubbard said in an interview. “Given that albumin binds strongly to hydroxyapatite-based mineral and blocks its growth, we infer that the epithelial barrier – the enamel-forming cells termed ameloblasts and normally responsible for excluding albumin – must break down in places in response to medical triggers.”
This breach enables localized infiltration of albumin, which then blocks further hardening of soft, immature enamel, leading to residual spots or patches of chalky enamel once the tooth eventually erupts into the mouth. “In other words, we infer that chalky enamel spots coincide with localized breaches of an epithelial barrier that are triggered by yet-to-be determined systemic insults,” he said.
Joseph Brofsky, DMD, section head of pediatric dentistry at North Shore LIJ Cohen Children’s Medical Center of New York, in Queens, agreed that that the definitive cause of MH has evaded identification for a hundred years. However, he expressed skepticism about the fossilized blood protein hypothesis.
“That’s a long shot. It’s a possibility, and I’m not ruling it out, but we’re not 100% sure,” said Dr. Brofsky, who was not involved in the research.
In his experience, MH is somewhat less prevalent in the United States, affecting about 1 in 10 children here, which is about half the global rate. “But it’s a problem, and we wish it would go away, but before we know beyond a reasonable doubt what causes this condition, it’s going to be hard to stop it.”
Most cases of MH involve hypomineralization of the 6-year molars, the first adult molars to erupt, but the process starts at birth. “For 6-year molars, normal hardening of dental enamel takes place from the early postnatal period through infancy,” Dr. Hubbard said.
The 2-year and 12-year molars are affected about half as frequently as their 6-year counterparts, “so this extends the medical-risk window out to early school days, and slightly back to the perinatal period for the 12-year and 2-year molars, respectively,” he said.
A critical question is which childhood illnesses are most likely to set the stage for MH, he added. “Forty-plus years of epidemiology have failed to nail a specific cause or causal association. But given the high prevalence of MH – 20% in otherwise healthy kids – naturally we suspect some common illnesses are the culprits,” he said. “But which diseases, which medications, and which combinations?”
Dr. Hubbard’s advice to pediatricians is to be alert to MH: “If you’re inspecting a child’s throat, then why not look at their back teeth, too – particularly when they’re getting their new molars at 2, 6, and 12 years?”
The study was supported by the Melbourne Research Unit for Facial Disorders Department of Pharmacology & Therapeutics, Department of Paediatrics, and Faculty of Medicine, Dentistry, and Health Sciences at the University of Melbourne. The authors and Dr. Brofsky have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
First ‘flurona’ cases reported in the U.S.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
Pneumonia in infancy predicts respiratory problems in early childhood
Preschoolers who experienced community-acquired pneumonia in infancy were significantly more likely than were those with no history of pneumonia to develop chronic respiratory disorders, based on data from approximately 7,000 individuals.
“Lower respiratory tract infections (LRTI) during the first years of life cause injury to the rapidly developing lung at its most critical stage,” wrote Rotem Lapidot, MD, of Boston University, and colleagues. Previous research has linked pneumonia with subsequent chronic cough, bronchitis, and recurrent pneumonia in children, but data are needed to assess the impact of early community-acquired pneumonia (CAP) on respiratory health in otherwise healthy infants, the researchers said.
In a retrospective matched cohort study published in Respiratory Medicine , the researchers identified 1,343 infants who had CAP in the first 2 years of life, and 6,715 controls, using a large electronic health records dataset (Optum EHR dataset) for the period from Jan. 2011 through June 2018.
The primary outcomes were the development of any chronic respiratory disorders, reactive airway disease, and CAP hospitalizations between ages 2 and 5 years. Infants in the CAP group were otherwise healthy; those with congenital or other conditions that might predispose them to pneumonia were excluded. Baseline characteristics were similar between the CAP patients and controls.
Future risk
Overall, the rates per 100 patient-years for any chronic respiratory disorder were 11.6 for CAP patients versus 4.9 for controls (relative risk, 2.4). Rates for reactive airway disease and CAP hospitalization were 6.1 versus 1.9 per 100 patient-years (RR, 3.2) and 1.0 versus 0.2 per 100 patient-years (RR, 6.3) for the CAP patients and controls, respectively.
The distribution of CAP etiology of CAP in infants at the first hospitalization was 20% bacterial, 27% viral, and 53% unspecified. The relative rates of later respiratory illness were similar across etiologies of the initial hospitalization for CAP, which support the association between infant CAP and later respiratory disease, the researchers said.
Nearly all (97%) of the CAP patients had only one qualifying hospitalization for CAP before 2 years of age, and the mean age at the first hospitalization was 8.9 months. “Rates and relative rates of any chronic respiratory disorder, and our composite for reactive airway disease, increased with age at which the initial CAP hospitalization occurred,” and were highest for children hospitalized at close to 2 years of age, the researchers noted.
Persistent inflammation?
“Our findings add to the evolving hypothesis that persistent inflammation following pneumonia creates an increased risk for subsequent respiratory disease and exacerbations of underlying disease,” the researchers wrote.
The study findings were limited by several factors, including the potential for misclassification of some infants with and without underlying conditions, reliance on discharge information for etiology, and possible lack of generalizability to other populations, the researchers noted.
However, the results indicate an increased risk for respiratory illness in early childhood among infants with CAP, and support the need for greater attention to CAP prevention and for strategies to reduce inflammation after pneumonia, they said. “Further study is needed to confirm the long-term consequences of infant CAP and the underlying mechanisms that lead to such long-term sequelae,” they concluded.
Dr. Lapidot and several coauthors disclosed ties with Pfizer, the study sponsor.
A version of this article first appeared on Medscape.com.
Preschoolers who experienced community-acquired pneumonia in infancy were significantly more likely than were those with no history of pneumonia to develop chronic respiratory disorders, based on data from approximately 7,000 individuals.
“Lower respiratory tract infections (LRTI) during the first years of life cause injury to the rapidly developing lung at its most critical stage,” wrote Rotem Lapidot, MD, of Boston University, and colleagues. Previous research has linked pneumonia with subsequent chronic cough, bronchitis, and recurrent pneumonia in children, but data are needed to assess the impact of early community-acquired pneumonia (CAP) on respiratory health in otherwise healthy infants, the researchers said.
In a retrospective matched cohort study published in Respiratory Medicine , the researchers identified 1,343 infants who had CAP in the first 2 years of life, and 6,715 controls, using a large electronic health records dataset (Optum EHR dataset) for the period from Jan. 2011 through June 2018.
The primary outcomes were the development of any chronic respiratory disorders, reactive airway disease, and CAP hospitalizations between ages 2 and 5 years. Infants in the CAP group were otherwise healthy; those with congenital or other conditions that might predispose them to pneumonia were excluded. Baseline characteristics were similar between the CAP patients and controls.
Future risk
Overall, the rates per 100 patient-years for any chronic respiratory disorder were 11.6 for CAP patients versus 4.9 for controls (relative risk, 2.4). Rates for reactive airway disease and CAP hospitalization were 6.1 versus 1.9 per 100 patient-years (RR, 3.2) and 1.0 versus 0.2 per 100 patient-years (RR, 6.3) for the CAP patients and controls, respectively.
The distribution of CAP etiology of CAP in infants at the first hospitalization was 20% bacterial, 27% viral, and 53% unspecified. The relative rates of later respiratory illness were similar across etiologies of the initial hospitalization for CAP, which support the association between infant CAP and later respiratory disease, the researchers said.
Nearly all (97%) of the CAP patients had only one qualifying hospitalization for CAP before 2 years of age, and the mean age at the first hospitalization was 8.9 months. “Rates and relative rates of any chronic respiratory disorder, and our composite for reactive airway disease, increased with age at which the initial CAP hospitalization occurred,” and were highest for children hospitalized at close to 2 years of age, the researchers noted.
Persistent inflammation?
“Our findings add to the evolving hypothesis that persistent inflammation following pneumonia creates an increased risk for subsequent respiratory disease and exacerbations of underlying disease,” the researchers wrote.
The study findings were limited by several factors, including the potential for misclassification of some infants with and without underlying conditions, reliance on discharge information for etiology, and possible lack of generalizability to other populations, the researchers noted.
However, the results indicate an increased risk for respiratory illness in early childhood among infants with CAP, and support the need for greater attention to CAP prevention and for strategies to reduce inflammation after pneumonia, they said. “Further study is needed to confirm the long-term consequences of infant CAP and the underlying mechanisms that lead to such long-term sequelae,” they concluded.
Dr. Lapidot and several coauthors disclosed ties with Pfizer, the study sponsor.
A version of this article first appeared on Medscape.com.
Preschoolers who experienced community-acquired pneumonia in infancy were significantly more likely than were those with no history of pneumonia to develop chronic respiratory disorders, based on data from approximately 7,000 individuals.
“Lower respiratory tract infections (LRTI) during the first years of life cause injury to the rapidly developing lung at its most critical stage,” wrote Rotem Lapidot, MD, of Boston University, and colleagues. Previous research has linked pneumonia with subsequent chronic cough, bronchitis, and recurrent pneumonia in children, but data are needed to assess the impact of early community-acquired pneumonia (CAP) on respiratory health in otherwise healthy infants, the researchers said.
In a retrospective matched cohort study published in Respiratory Medicine , the researchers identified 1,343 infants who had CAP in the first 2 years of life, and 6,715 controls, using a large electronic health records dataset (Optum EHR dataset) for the period from Jan. 2011 through June 2018.
The primary outcomes were the development of any chronic respiratory disorders, reactive airway disease, and CAP hospitalizations between ages 2 and 5 years. Infants in the CAP group were otherwise healthy; those with congenital or other conditions that might predispose them to pneumonia were excluded. Baseline characteristics were similar between the CAP patients and controls.
Future risk
Overall, the rates per 100 patient-years for any chronic respiratory disorder were 11.6 for CAP patients versus 4.9 for controls (relative risk, 2.4). Rates for reactive airway disease and CAP hospitalization were 6.1 versus 1.9 per 100 patient-years (RR, 3.2) and 1.0 versus 0.2 per 100 patient-years (RR, 6.3) for the CAP patients and controls, respectively.
The distribution of CAP etiology of CAP in infants at the first hospitalization was 20% bacterial, 27% viral, and 53% unspecified. The relative rates of later respiratory illness were similar across etiologies of the initial hospitalization for CAP, which support the association between infant CAP and later respiratory disease, the researchers said.
Nearly all (97%) of the CAP patients had only one qualifying hospitalization for CAP before 2 years of age, and the mean age at the first hospitalization was 8.9 months. “Rates and relative rates of any chronic respiratory disorder, and our composite for reactive airway disease, increased with age at which the initial CAP hospitalization occurred,” and were highest for children hospitalized at close to 2 years of age, the researchers noted.
Persistent inflammation?
“Our findings add to the evolving hypothesis that persistent inflammation following pneumonia creates an increased risk for subsequent respiratory disease and exacerbations of underlying disease,” the researchers wrote.
The study findings were limited by several factors, including the potential for misclassification of some infants with and without underlying conditions, reliance on discharge information for etiology, and possible lack of generalizability to other populations, the researchers noted.
However, the results indicate an increased risk for respiratory illness in early childhood among infants with CAP, and support the need for greater attention to CAP prevention and for strategies to reduce inflammation after pneumonia, they said. “Further study is needed to confirm the long-term consequences of infant CAP and the underlying mechanisms that lead to such long-term sequelae,” they concluded.
Dr. Lapidot and several coauthors disclosed ties with Pfizer, the study sponsor.
A version of this article first appeared on Medscape.com.
FROM RESPIRATORY MEDICINE
HIV+ patients get good outcomes after kidney or liver transplant
in new research that represents some of the longest follow-up on these patients to date.
The findings further support the inclusion of people with HIV in transplant resource allocation, say the researchers.
“Overall, the excellent outcomes following liver and kidney transplant recipients in HIV-infected recipients justify the utilization of a scarce resource,” senior author Peter G. Stock, MD, PhD, surgical director of the Kidney and Pancreas Transplant Program and surgical director of the Pediatric Renal Transplant Program at the University of California, San Francisco (UCSF), said in an interview.
“Many centers still view HIV as a strict contraindication [for transplantation]. This data shows it is not,” he emphasized.
The study, published in JAMA Surgery, involved HIV-positive patients who received kidney or liver transplants between 2000 and 2019 at UCSF, which has unique access to some of the longest-term data on those outcomes.
“UCSF was the first U.S. center to do transplants routinely in people with HIV, and based on the large volume of transplants that are performed, we were able to use propensity matching to address the comparison of HIV-positive and negative liver and kidney transplant recipients at a single center,” Dr. Stock explained.
“To the best of our knowledge, there are no long-term reports [greater than 10 years] on [transplant] outcomes in the HIV-positive population.”
Commenting on the study, David Klassen, MD, chief medical officer of the United Network for Organ Sharing (UNOS), noted that the findings “confirm previous research done at UCSF and reported in the New England Journal of Medicine” in 2010. “It extends the previous findings.”
“The take-home message is that these HIV-positive patients can be successfully transplanted with expected good outcomes and will derive substantial benefit from transplantation,” Dr. Klassen said.
Kidney transplant patient survival lower, graft survival similar
For the kidney transplant analysis, 119 HIV-positive recipients were propensity matched with 655 recipients who were HIV-negative, with the patients’ mean age about 52 and approximately 70% male.
At 15-years post-transplant, patient survival was 53.6% among the HIV-positive patients versus 79.6% for HIV-negative (P = .03).
Graft survival among the kidney transplant patients was proportionally higher among HIV-positive patients after 15 years (75% vs. 57%); however, the difference was not statistically significant (P = .77).
First author Arya Zarinsefat, MD, of the Department of Surgery at UCSF, speculated that the lower long-term patient survival among HIV-positive kidney transplant recipients may reflect known cardiovascular risks among those patients.
“We postulated that part of this may be due to the fact that HIV-positive patients certainly have additional comorbidities, specifically cardiovascular” ones, he told this news organization.
“When looking at the survival curve, survival was nearly identical at 5 years and only started to diverge at 10 years post-transplant,” he noted.
A further evaluation of patients with HIV who were co-infected with hepatitis C (HCV) showed that those with HIV-HCV co-infection prior to the center’s introduction of anti-HCV direct-acting antiviral (DAA) medications in 2014 had the lowest survival rate of all subgroups, at 57.1% at 5 years post-transplant (P = .045 vs. those treated after 2014).
Liver transplant patient survival similar
In terms of liver transplant outcomes, among 83 HIV-positive recipients who were propensity-matched with 468 HIV-negative recipients, the mean age was about 53 and about 66% were male.
The patient survival rates at 15 years were not significantly different between the groups, at 70% for HIV-positive and 75.7% for HIV-negative, (P = .12).
Similar to the kidney transplant recipients, the worst survival among all liver transplant subgroups was among HIV-HCV co-infected patients prior to access to HCV direct-acting antivirals in 2014, with a 5-year survival of 59.5% (P = .04).
“Since the advent of HCV direct-acting antivirals, liver transplant outcomes in HCV mono-infected patients are comparable to HCV/HIV co-infected recipients,” Dr. Stock said.
Acute rejection rates higher with HIV-positivity versus national averages
The rates of acute rejection at 1 year in the kidney and liver transplant, HIV-positive groups – at about 20% and 30%, respectively – were, however, higher than national average incidence rates of about 10% at 1 year.
Long-term data on those patients showed the acute rejection affected graft survival outcomes with kidney transplant recipients: HIV-positive kidney transplant recipients who had at least one episode of acute rejection had a graft survival of just 52.8% at 15 years post-transplant, compared with 91.8% among recipients without acute rejection.
Such differences were not observed among HIV-positive liver transplant recipients.
The authors note that the increased risk of acute rejection in HIV-positive kidney transplant patients is consistent with previous studies, with causes that may be multifactorial.
Top theories include drug interactions with protease inhibitors, resulting in some centers transitioning HIV-infected patients from those regimens to integrase-based regimens prior to transplant.
“The management and prevention of acute rejection in HIV-positive kidney transplant [patients] will therefore continue to be a key component in the care of these patients,” the authors note in their study.
The study was supported in part by the National Institutes of Health. The study authors and Dr. Klassen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in new research that represents some of the longest follow-up on these patients to date.
The findings further support the inclusion of people with HIV in transplant resource allocation, say the researchers.
“Overall, the excellent outcomes following liver and kidney transplant recipients in HIV-infected recipients justify the utilization of a scarce resource,” senior author Peter G. Stock, MD, PhD, surgical director of the Kidney and Pancreas Transplant Program and surgical director of the Pediatric Renal Transplant Program at the University of California, San Francisco (UCSF), said in an interview.
“Many centers still view HIV as a strict contraindication [for transplantation]. This data shows it is not,” he emphasized.
The study, published in JAMA Surgery, involved HIV-positive patients who received kidney or liver transplants between 2000 and 2019 at UCSF, which has unique access to some of the longest-term data on those outcomes.
“UCSF was the first U.S. center to do transplants routinely in people with HIV, and based on the large volume of transplants that are performed, we were able to use propensity matching to address the comparison of HIV-positive and negative liver and kidney transplant recipients at a single center,” Dr. Stock explained.
“To the best of our knowledge, there are no long-term reports [greater than 10 years] on [transplant] outcomes in the HIV-positive population.”
Commenting on the study, David Klassen, MD, chief medical officer of the United Network for Organ Sharing (UNOS), noted that the findings “confirm previous research done at UCSF and reported in the New England Journal of Medicine” in 2010. “It extends the previous findings.”
“The take-home message is that these HIV-positive patients can be successfully transplanted with expected good outcomes and will derive substantial benefit from transplantation,” Dr. Klassen said.
Kidney transplant patient survival lower, graft survival similar
For the kidney transplant analysis, 119 HIV-positive recipients were propensity matched with 655 recipients who were HIV-negative, with the patients’ mean age about 52 and approximately 70% male.
At 15-years post-transplant, patient survival was 53.6% among the HIV-positive patients versus 79.6% for HIV-negative (P = .03).
Graft survival among the kidney transplant patients was proportionally higher among HIV-positive patients after 15 years (75% vs. 57%); however, the difference was not statistically significant (P = .77).
First author Arya Zarinsefat, MD, of the Department of Surgery at UCSF, speculated that the lower long-term patient survival among HIV-positive kidney transplant recipients may reflect known cardiovascular risks among those patients.
“We postulated that part of this may be due to the fact that HIV-positive patients certainly have additional comorbidities, specifically cardiovascular” ones, he told this news organization.
“When looking at the survival curve, survival was nearly identical at 5 years and only started to diverge at 10 years post-transplant,” he noted.
A further evaluation of patients with HIV who were co-infected with hepatitis C (HCV) showed that those with HIV-HCV co-infection prior to the center’s introduction of anti-HCV direct-acting antiviral (DAA) medications in 2014 had the lowest survival rate of all subgroups, at 57.1% at 5 years post-transplant (P = .045 vs. those treated after 2014).
Liver transplant patient survival similar
In terms of liver transplant outcomes, among 83 HIV-positive recipients who were propensity-matched with 468 HIV-negative recipients, the mean age was about 53 and about 66% were male.
The patient survival rates at 15 years were not significantly different between the groups, at 70% for HIV-positive and 75.7% for HIV-negative, (P = .12).
Similar to the kidney transplant recipients, the worst survival among all liver transplant subgroups was among HIV-HCV co-infected patients prior to access to HCV direct-acting antivirals in 2014, with a 5-year survival of 59.5% (P = .04).
“Since the advent of HCV direct-acting antivirals, liver transplant outcomes in HCV mono-infected patients are comparable to HCV/HIV co-infected recipients,” Dr. Stock said.
Acute rejection rates higher with HIV-positivity versus national averages
The rates of acute rejection at 1 year in the kidney and liver transplant, HIV-positive groups – at about 20% and 30%, respectively – were, however, higher than national average incidence rates of about 10% at 1 year.
Long-term data on those patients showed the acute rejection affected graft survival outcomes with kidney transplant recipients: HIV-positive kidney transplant recipients who had at least one episode of acute rejection had a graft survival of just 52.8% at 15 years post-transplant, compared with 91.8% among recipients without acute rejection.
Such differences were not observed among HIV-positive liver transplant recipients.
The authors note that the increased risk of acute rejection in HIV-positive kidney transplant patients is consistent with previous studies, with causes that may be multifactorial.
Top theories include drug interactions with protease inhibitors, resulting in some centers transitioning HIV-infected patients from those regimens to integrase-based regimens prior to transplant.
“The management and prevention of acute rejection in HIV-positive kidney transplant [patients] will therefore continue to be a key component in the care of these patients,” the authors note in their study.
The study was supported in part by the National Institutes of Health. The study authors and Dr. Klassen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in new research that represents some of the longest follow-up on these patients to date.
The findings further support the inclusion of people with HIV in transplant resource allocation, say the researchers.
“Overall, the excellent outcomes following liver and kidney transplant recipients in HIV-infected recipients justify the utilization of a scarce resource,” senior author Peter G. Stock, MD, PhD, surgical director of the Kidney and Pancreas Transplant Program and surgical director of the Pediatric Renal Transplant Program at the University of California, San Francisco (UCSF), said in an interview.
“Many centers still view HIV as a strict contraindication [for transplantation]. This data shows it is not,” he emphasized.
The study, published in JAMA Surgery, involved HIV-positive patients who received kidney or liver transplants between 2000 and 2019 at UCSF, which has unique access to some of the longest-term data on those outcomes.
“UCSF was the first U.S. center to do transplants routinely in people with HIV, and based on the large volume of transplants that are performed, we were able to use propensity matching to address the comparison of HIV-positive and negative liver and kidney transplant recipients at a single center,” Dr. Stock explained.
“To the best of our knowledge, there are no long-term reports [greater than 10 years] on [transplant] outcomes in the HIV-positive population.”
Commenting on the study, David Klassen, MD, chief medical officer of the United Network for Organ Sharing (UNOS), noted that the findings “confirm previous research done at UCSF and reported in the New England Journal of Medicine” in 2010. “It extends the previous findings.”
“The take-home message is that these HIV-positive patients can be successfully transplanted with expected good outcomes and will derive substantial benefit from transplantation,” Dr. Klassen said.
Kidney transplant patient survival lower, graft survival similar
For the kidney transplant analysis, 119 HIV-positive recipients were propensity matched with 655 recipients who were HIV-negative, with the patients’ mean age about 52 and approximately 70% male.
At 15-years post-transplant, patient survival was 53.6% among the HIV-positive patients versus 79.6% for HIV-negative (P = .03).
Graft survival among the kidney transplant patients was proportionally higher among HIV-positive patients after 15 years (75% vs. 57%); however, the difference was not statistically significant (P = .77).
First author Arya Zarinsefat, MD, of the Department of Surgery at UCSF, speculated that the lower long-term patient survival among HIV-positive kidney transplant recipients may reflect known cardiovascular risks among those patients.
“We postulated that part of this may be due to the fact that HIV-positive patients certainly have additional comorbidities, specifically cardiovascular” ones, he told this news organization.
“When looking at the survival curve, survival was nearly identical at 5 years and only started to diverge at 10 years post-transplant,” he noted.
A further evaluation of patients with HIV who were co-infected with hepatitis C (HCV) showed that those with HIV-HCV co-infection prior to the center’s introduction of anti-HCV direct-acting antiviral (DAA) medications in 2014 had the lowest survival rate of all subgroups, at 57.1% at 5 years post-transplant (P = .045 vs. those treated after 2014).
Liver transplant patient survival similar
In terms of liver transplant outcomes, among 83 HIV-positive recipients who were propensity-matched with 468 HIV-negative recipients, the mean age was about 53 and about 66% were male.
The patient survival rates at 15 years were not significantly different between the groups, at 70% for HIV-positive and 75.7% for HIV-negative, (P = .12).
Similar to the kidney transplant recipients, the worst survival among all liver transplant subgroups was among HIV-HCV co-infected patients prior to access to HCV direct-acting antivirals in 2014, with a 5-year survival of 59.5% (P = .04).
“Since the advent of HCV direct-acting antivirals, liver transplant outcomes in HCV mono-infected patients are comparable to HCV/HIV co-infected recipients,” Dr. Stock said.
Acute rejection rates higher with HIV-positivity versus national averages
The rates of acute rejection at 1 year in the kidney and liver transplant, HIV-positive groups – at about 20% and 30%, respectively – were, however, higher than national average incidence rates of about 10% at 1 year.
Long-term data on those patients showed the acute rejection affected graft survival outcomes with kidney transplant recipients: HIV-positive kidney transplant recipients who had at least one episode of acute rejection had a graft survival of just 52.8% at 15 years post-transplant, compared with 91.8% among recipients without acute rejection.
Such differences were not observed among HIV-positive liver transplant recipients.
The authors note that the increased risk of acute rejection in HIV-positive kidney transplant patients is consistent with previous studies, with causes that may be multifactorial.
Top theories include drug interactions with protease inhibitors, resulting in some centers transitioning HIV-infected patients from those regimens to integrase-based regimens prior to transplant.
“The management and prevention of acute rejection in HIV-positive kidney transplant [patients] will therefore continue to be a key component in the care of these patients,” the authors note in their study.
The study was supported in part by the National Institutes of Health. The study authors and Dr. Klassen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Could the Omicron surge hasten the transition from pandemic to endemic?
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
As Omicron surges, hospital beds fill, but ICUs less affected
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
Freshwater aquarium provides source for melioidosis infection
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Herpes Zoster Following a Nucleoside-Modified Messenger RNA COVID-19 Vaccine
Since the end of 2019, COVID-19 infection caused by SARS-CoV-2 has spread in a worldwide pandemic. The first cutaneous manifestations possibly linked to COVID-19 were reported in spring 2020.1 Herpes zoster (HZ) was suspected as a predictive cutaneous manifestation of COVID-19 with a debated prognostic significance.2 The end of 2020 was marked with the beginning of vaccination against COVID-19, and safety studies reported few side effects after vaccination with nucleoside-modified messenger RNA (mRNA) COVID-19 vaccines.3 Real-life use of vaccines could lead to the occurrence of potential side effects (or fortuitous medical events) that were not observed in these studies. We report a series of 5 cases of HZ occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine extracted from a declarative cohort of cutaneous reactions in our vaccination center.
Case Series
We identified 2 men and 3 women (Table) who experienced HZ after vaccination with a nucleoside-modified mRNA COVID-19 vaccine (Comirnaty, Pfizer-BioNTech). Patients fulfilled French governmental criteria for vaccination at the time of the report—older than 75 years or a health care professional—and they were vaccinated at the vaccination center of a French university hospital. The median age of the patients was 56 years (interquartile range [IQR], 51–82 years). One patient was diagnosed with COVID-19 in February 2020. A medical history of HZ was found in 1 patient. No medical history of immunosuppression was noted. Herpes zoster was observed on the same side of the body as the vaccination site in 4 patients. The median delay before the onset of symptoms was 6 days (IQR, 1–15 days) after injection. The median duration of the symptoms was 13 days (IQR, 11.5–16.5 days). Clinical signs of HZ were mild with few vesicles in 4 patients, and we observed a notably long delay between the onset of pain and the eruption of vesicles in 2 cases (4 and 10 days, respectively). The clinical diagnosis of HZ was confirmed by a dermatologist for all patients (Figures 1 and 2). Polymerase chain reaction assays for the detection of the varicella-zoster virus were performed in 2 cases and were positive. A complete blood cell count was performed in 1 patient, and we observed isolated lymphopenia (500/mm3 [reference range, 1000–4000/mm3]). Herpes zoster occurred after the first dose of vaccine in 4 patients and after the second dose for 1 patient. Three patients were treated with antiviral therapy (acyclovir) for 7 days. Three patients recovered from symptoms within 2 weeks and 2 patients within 1 week.
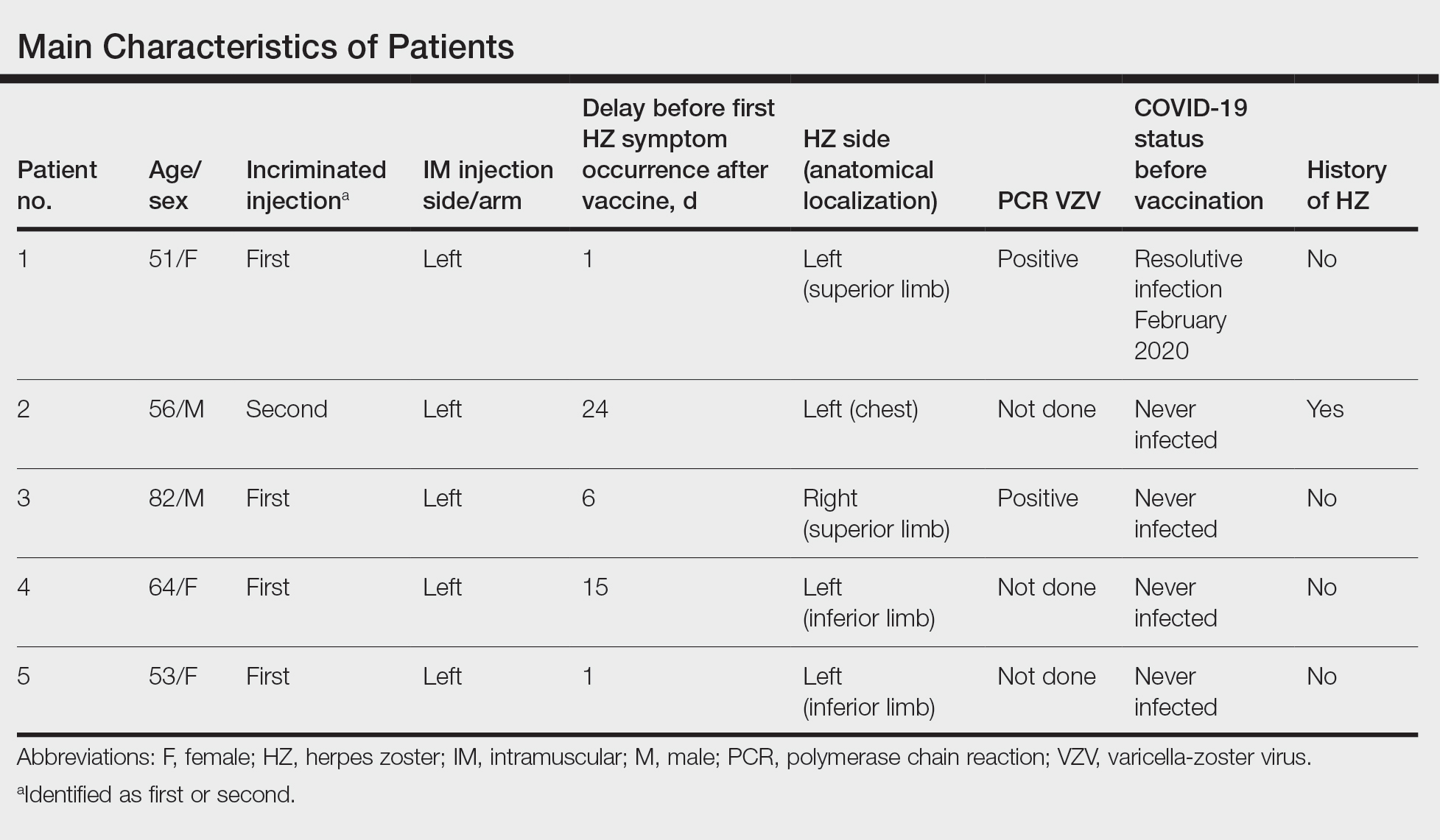
Comment
We report a series of HZ cases occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine. We did not observe complicated HZ, and most of the time, HZ lesions were located on the same side of the body as the vaccine injection. One case of HZ after COVID-19 vaccination was reported by Bostan and Yalici-Armagan,4 but it followed injection with an inactivated vaccine, which is different from our series. Herpes zoster remains rarely reported, mainly following mRNA COVID-19 vaccination.5

Cases of HZ after vaccination have been reported after the live attenuated zoster or yellow fever vaccines, but HZ should not appear as a concomitant effect after any type of vaccines.6,7 Kawai et al8 reported that the incidence rate of HZ ranged from 3 to 5 cases per 1000 person-years in North America, Europe, and Asia-Pacific. The risk for recurrence of HZ ranged from 1% to 6% depending on the type of study design, age distribution of studied populations, and definition.8 In another retrospective database analysis in Israel, the incidence density rate of HZ was 3.46 cases per 1000 person-years in the total population and 12.8 cases per 1000 person-years in immunocompromised patients, therefore the immunocompromised status is important to consider.9

In our declarative cohort of skin eruptions before vaccination, we recorded 11 cases of HZ among 148 skin eruptions (7.43%) at the time of the study, but the design of the study did not allow us to estimate the exact incidence of HZ in the global COVID-19–vaccinated population because our study was not based on a systematic and prospective analysis of all vaccinated patients. The comparison between the prevalence of HZ in the COVID-19–vaccinated population and the nonvaccinated population is difficult owing to the lack of data about HZ in the nonvaccinated population at the time of our analysis. Furthermore, we did not include all vaccinated patients in a prospective follow-up. We highlight the importance of medical history of patients that differed between vaccinated patients (at the time of our analysis) and the global population due to French governmental access criteria to vaccination. The link to prior SARS-CoV-2 infection was uncertain because a medical history of COVID-19 was found in only 1 patient. Only 1 patient had a history of HZ, which is not a contraindication of COVID-19 vaccination.
Postinjection pains are frequent with COVID-19 vaccines, but clinical signs such as extension of pain, burning sensation, and eruption of vesicles should lead the physician to consider the diagnosis of HZ, regardless of the delay between the injection and the symptoms. Indeed, the onset of symptoms could be late, and the clinical presentation initially may be mistaken for an injection-site reaction, which is a frequent known side effect of vaccines. These new cases do not prove causality between COVID-19 vaccination and HZ. Varicella-zoster virus remains latent in dorsal-root or ganglia after primary infection, and HZ caused by reactivation of varicella-zoster virus may occur spontaneously or be triggered. In our series, we did not observe medical history of immunosuppression, and no other known risk factors of HZ (eg, radiation therapy, physical trauma, fever after vaccination) were recorded. The pathophysiologic mechanism remains elusive, but local vaccine-induced immunomodulation or an inflammatory state may be involved.
Conclusion
Our case series highlights that clinicians must remain vigilant to diagnose HZ early to prevent potential complications, such as postherpetic neuralgia. Also, vaccination should not be contraindicated in patients with medical history of HZ; the occurrence of HZ does not justify avoiding the second injection of the vaccine due to the benefit of vaccination.
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:E212-E213.
- Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther. 2020;33:e13666.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383:2603-2615.
- Bostan E, Yalici-Armagan B. Herpes zoster following inactivated COVID-19 vaccine: a coexistence or coincidence? J Cosmet Dermatol. 2021;20:1566-1567.
- Desai HD, Sharma K, Shah A, et al. Can SARS-CoV-2 vaccine increase the risk of reactivation of varicella zoster? a systematic review. J Cosmet Dermatol. 2021;20:3350-3361.
- Fahlbusch M, Wesselmann U, Lehmann P. Herpes zoster after varicella-zoster vaccination [in German]. Hautarzt. 2013;64:107-109.
- Bayas JM, González-Alvarez R, Guinovart C. Herpes zoster after yellow fever vaccination. J Travel Med. 2007;14:65-66.
- Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;10;4:E004833.
- Weitzman D, Shavit O, Stein M, et al. A population based study of the epidemiology of herpes zoster and its complications. J Infect. 2013;67:463-469.
Since the end of 2019, COVID-19 infection caused by SARS-CoV-2 has spread in a worldwide pandemic. The first cutaneous manifestations possibly linked to COVID-19 were reported in spring 2020.1 Herpes zoster (HZ) was suspected as a predictive cutaneous manifestation of COVID-19 with a debated prognostic significance.2 The end of 2020 was marked with the beginning of vaccination against COVID-19, and safety studies reported few side effects after vaccination with nucleoside-modified messenger RNA (mRNA) COVID-19 vaccines.3 Real-life use of vaccines could lead to the occurrence of potential side effects (or fortuitous medical events) that were not observed in these studies. We report a series of 5 cases of HZ occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine extracted from a declarative cohort of cutaneous reactions in our vaccination center.
Case Series
We identified 2 men and 3 women (Table) who experienced HZ after vaccination with a nucleoside-modified mRNA COVID-19 vaccine (Comirnaty, Pfizer-BioNTech). Patients fulfilled French governmental criteria for vaccination at the time of the report—older than 75 years or a health care professional—and they were vaccinated at the vaccination center of a French university hospital. The median age of the patients was 56 years (interquartile range [IQR], 51–82 years). One patient was diagnosed with COVID-19 in February 2020. A medical history of HZ was found in 1 patient. No medical history of immunosuppression was noted. Herpes zoster was observed on the same side of the body as the vaccination site in 4 patients. The median delay before the onset of symptoms was 6 days (IQR, 1–15 days) after injection. The median duration of the symptoms was 13 days (IQR, 11.5–16.5 days). Clinical signs of HZ were mild with few vesicles in 4 patients, and we observed a notably long delay between the onset of pain and the eruption of vesicles in 2 cases (4 and 10 days, respectively). The clinical diagnosis of HZ was confirmed by a dermatologist for all patients (Figures 1 and 2). Polymerase chain reaction assays for the detection of the varicella-zoster virus were performed in 2 cases and were positive. A complete blood cell count was performed in 1 patient, and we observed isolated lymphopenia (500/mm3 [reference range, 1000–4000/mm3]). Herpes zoster occurred after the first dose of vaccine in 4 patients and after the second dose for 1 patient. Three patients were treated with antiviral therapy (acyclovir) for 7 days. Three patients recovered from symptoms within 2 weeks and 2 patients within 1 week.
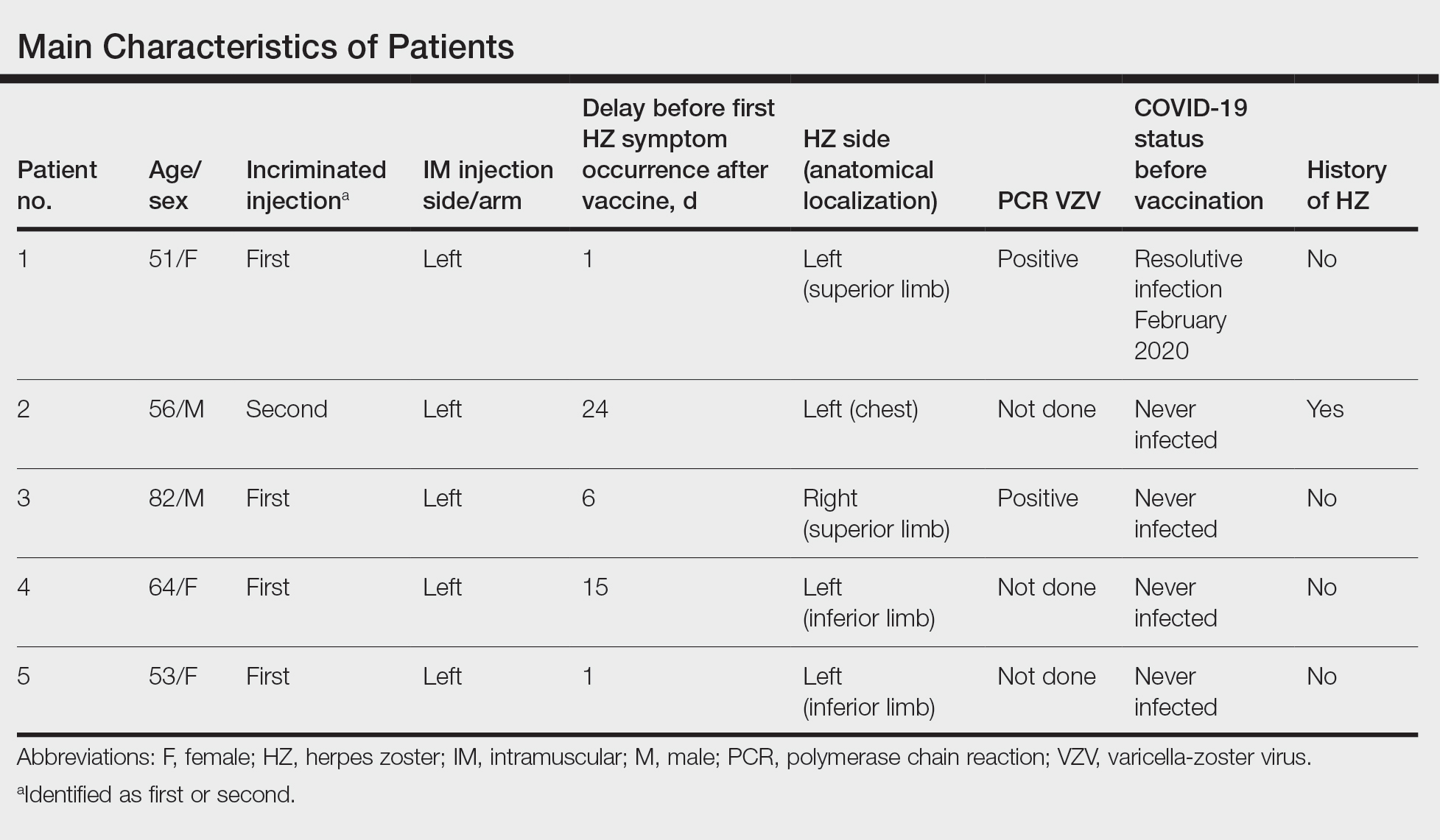
Comment
We report a series of HZ cases occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine. We did not observe complicated HZ, and most of the time, HZ lesions were located on the same side of the body as the vaccine injection. One case of HZ after COVID-19 vaccination was reported by Bostan and Yalici-Armagan,4 but it followed injection with an inactivated vaccine, which is different from our series. Herpes zoster remains rarely reported, mainly following mRNA COVID-19 vaccination.5

Cases of HZ after vaccination have been reported after the live attenuated zoster or yellow fever vaccines, but HZ should not appear as a concomitant effect after any type of vaccines.6,7 Kawai et al8 reported that the incidence rate of HZ ranged from 3 to 5 cases per 1000 person-years in North America, Europe, and Asia-Pacific. The risk for recurrence of HZ ranged from 1% to 6% depending on the type of study design, age distribution of studied populations, and definition.8 In another retrospective database analysis in Israel, the incidence density rate of HZ was 3.46 cases per 1000 person-years in the total population and 12.8 cases per 1000 person-years in immunocompromised patients, therefore the immunocompromised status is important to consider.9

In our declarative cohort of skin eruptions before vaccination, we recorded 11 cases of HZ among 148 skin eruptions (7.43%) at the time of the study, but the design of the study did not allow us to estimate the exact incidence of HZ in the global COVID-19–vaccinated population because our study was not based on a systematic and prospective analysis of all vaccinated patients. The comparison between the prevalence of HZ in the COVID-19–vaccinated population and the nonvaccinated population is difficult owing to the lack of data about HZ in the nonvaccinated population at the time of our analysis. Furthermore, we did not include all vaccinated patients in a prospective follow-up. We highlight the importance of medical history of patients that differed between vaccinated patients (at the time of our analysis) and the global population due to French governmental access criteria to vaccination. The link to prior SARS-CoV-2 infection was uncertain because a medical history of COVID-19 was found in only 1 patient. Only 1 patient had a history of HZ, which is not a contraindication of COVID-19 vaccination.
Postinjection pains are frequent with COVID-19 vaccines, but clinical signs such as extension of pain, burning sensation, and eruption of vesicles should lead the physician to consider the diagnosis of HZ, regardless of the delay between the injection and the symptoms. Indeed, the onset of symptoms could be late, and the clinical presentation initially may be mistaken for an injection-site reaction, which is a frequent known side effect of vaccines. These new cases do not prove causality between COVID-19 vaccination and HZ. Varicella-zoster virus remains latent in dorsal-root or ganglia after primary infection, and HZ caused by reactivation of varicella-zoster virus may occur spontaneously or be triggered. In our series, we did not observe medical history of immunosuppression, and no other known risk factors of HZ (eg, radiation therapy, physical trauma, fever after vaccination) were recorded. The pathophysiologic mechanism remains elusive, but local vaccine-induced immunomodulation or an inflammatory state may be involved.
Conclusion
Our case series highlights that clinicians must remain vigilant to diagnose HZ early to prevent potential complications, such as postherpetic neuralgia. Also, vaccination should not be contraindicated in patients with medical history of HZ; the occurrence of HZ does not justify avoiding the second injection of the vaccine due to the benefit of vaccination.
Since the end of 2019, COVID-19 infection caused by SARS-CoV-2 has spread in a worldwide pandemic. The first cutaneous manifestations possibly linked to COVID-19 were reported in spring 2020.1 Herpes zoster (HZ) was suspected as a predictive cutaneous manifestation of COVID-19 with a debated prognostic significance.2 The end of 2020 was marked with the beginning of vaccination against COVID-19, and safety studies reported few side effects after vaccination with nucleoside-modified messenger RNA (mRNA) COVID-19 vaccines.3 Real-life use of vaccines could lead to the occurrence of potential side effects (or fortuitous medical events) that were not observed in these studies. We report a series of 5 cases of HZ occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine extracted from a declarative cohort of cutaneous reactions in our vaccination center.
Case Series
We identified 2 men and 3 women (Table) who experienced HZ after vaccination with a nucleoside-modified mRNA COVID-19 vaccine (Comirnaty, Pfizer-BioNTech). Patients fulfilled French governmental criteria for vaccination at the time of the report—older than 75 years or a health care professional—and they were vaccinated at the vaccination center of a French university hospital. The median age of the patients was 56 years (interquartile range [IQR], 51–82 years). One patient was diagnosed with COVID-19 in February 2020. A medical history of HZ was found in 1 patient. No medical history of immunosuppression was noted. Herpes zoster was observed on the same side of the body as the vaccination site in 4 patients. The median delay before the onset of symptoms was 6 days (IQR, 1–15 days) after injection. The median duration of the symptoms was 13 days (IQR, 11.5–16.5 days). Clinical signs of HZ were mild with few vesicles in 4 patients, and we observed a notably long delay between the onset of pain and the eruption of vesicles in 2 cases (4 and 10 days, respectively). The clinical diagnosis of HZ was confirmed by a dermatologist for all patients (Figures 1 and 2). Polymerase chain reaction assays for the detection of the varicella-zoster virus were performed in 2 cases and were positive. A complete blood cell count was performed in 1 patient, and we observed isolated lymphopenia (500/mm3 [reference range, 1000–4000/mm3]). Herpes zoster occurred after the first dose of vaccine in 4 patients and after the second dose for 1 patient. Three patients were treated with antiviral therapy (acyclovir) for 7 days. Three patients recovered from symptoms within 2 weeks and 2 patients within 1 week.
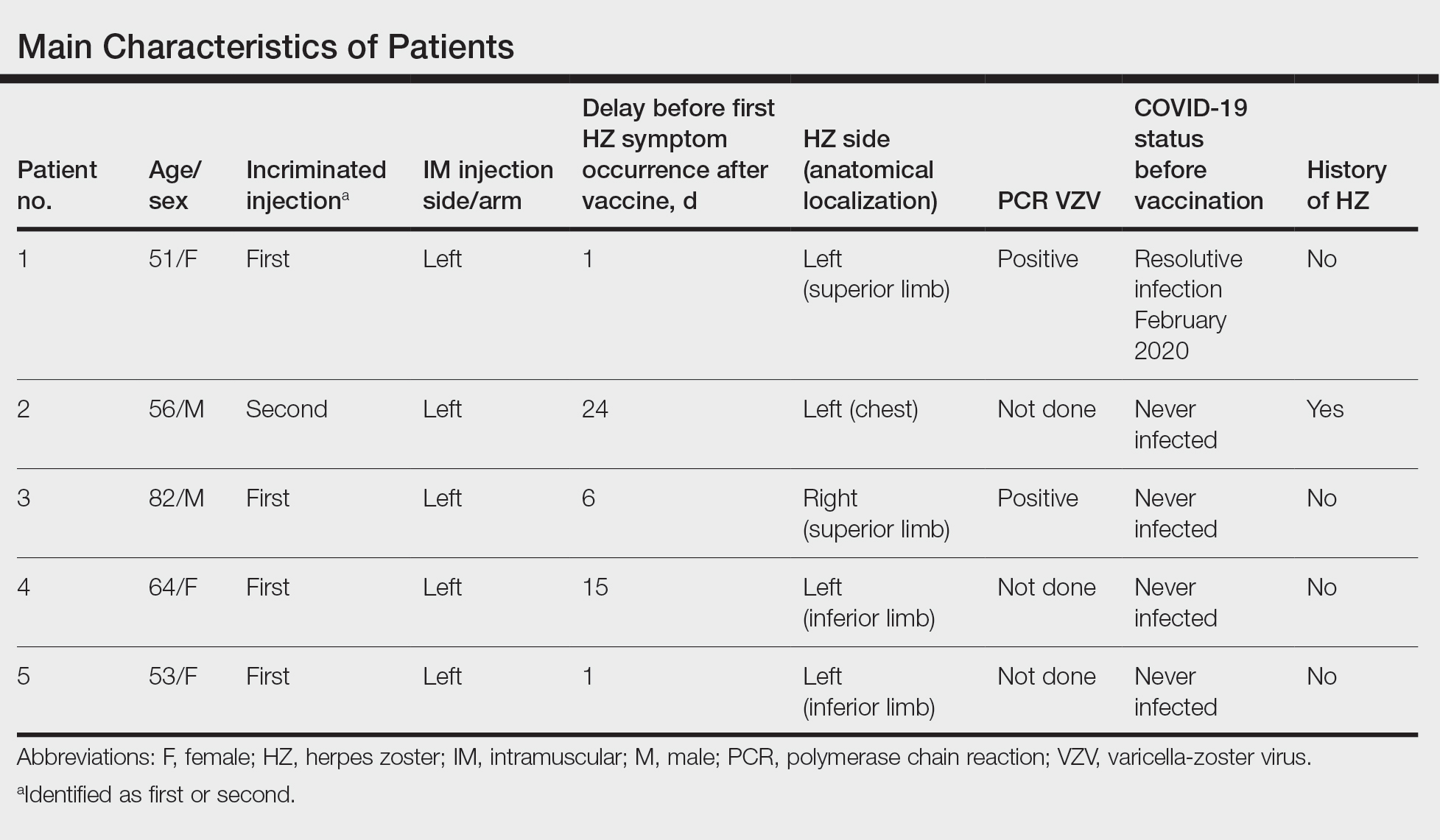
Comment
We report a series of HZ cases occurring after vaccination with a nucleoside-modified mRNA COVID-19 vaccine. We did not observe complicated HZ, and most of the time, HZ lesions were located on the same side of the body as the vaccine injection. One case of HZ after COVID-19 vaccination was reported by Bostan and Yalici-Armagan,4 but it followed injection with an inactivated vaccine, which is different from our series. Herpes zoster remains rarely reported, mainly following mRNA COVID-19 vaccination.5

Cases of HZ after vaccination have been reported after the live attenuated zoster or yellow fever vaccines, but HZ should not appear as a concomitant effect after any type of vaccines.6,7 Kawai et al8 reported that the incidence rate of HZ ranged from 3 to 5 cases per 1000 person-years in North America, Europe, and Asia-Pacific. The risk for recurrence of HZ ranged from 1% to 6% depending on the type of study design, age distribution of studied populations, and definition.8 In another retrospective database analysis in Israel, the incidence density rate of HZ was 3.46 cases per 1000 person-years in the total population and 12.8 cases per 1000 person-years in immunocompromised patients, therefore the immunocompromised status is important to consider.9

In our declarative cohort of skin eruptions before vaccination, we recorded 11 cases of HZ among 148 skin eruptions (7.43%) at the time of the study, but the design of the study did not allow us to estimate the exact incidence of HZ in the global COVID-19–vaccinated population because our study was not based on a systematic and prospective analysis of all vaccinated patients. The comparison between the prevalence of HZ in the COVID-19–vaccinated population and the nonvaccinated population is difficult owing to the lack of data about HZ in the nonvaccinated population at the time of our analysis. Furthermore, we did not include all vaccinated patients in a prospective follow-up. We highlight the importance of medical history of patients that differed between vaccinated patients (at the time of our analysis) and the global population due to French governmental access criteria to vaccination. The link to prior SARS-CoV-2 infection was uncertain because a medical history of COVID-19 was found in only 1 patient. Only 1 patient had a history of HZ, which is not a contraindication of COVID-19 vaccination.
Postinjection pains are frequent with COVID-19 vaccines, but clinical signs such as extension of pain, burning sensation, and eruption of vesicles should lead the physician to consider the diagnosis of HZ, regardless of the delay between the injection and the symptoms. Indeed, the onset of symptoms could be late, and the clinical presentation initially may be mistaken for an injection-site reaction, which is a frequent known side effect of vaccines. These new cases do not prove causality between COVID-19 vaccination and HZ. Varicella-zoster virus remains latent in dorsal-root or ganglia after primary infection, and HZ caused by reactivation of varicella-zoster virus may occur spontaneously or be triggered. In our series, we did not observe medical history of immunosuppression, and no other known risk factors of HZ (eg, radiation therapy, physical trauma, fever after vaccination) were recorded. The pathophysiologic mechanism remains elusive, but local vaccine-induced immunomodulation or an inflammatory state may be involved.
Conclusion
Our case series highlights that clinicians must remain vigilant to diagnose HZ early to prevent potential complications, such as postherpetic neuralgia. Also, vaccination should not be contraindicated in patients with medical history of HZ; the occurrence of HZ does not justify avoiding the second injection of the vaccine due to the benefit of vaccination.
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:E212-E213.
- Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther. 2020;33:e13666.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383:2603-2615.
- Bostan E, Yalici-Armagan B. Herpes zoster following inactivated COVID-19 vaccine: a coexistence or coincidence? J Cosmet Dermatol. 2021;20:1566-1567.
- Desai HD, Sharma K, Shah A, et al. Can SARS-CoV-2 vaccine increase the risk of reactivation of varicella zoster? a systematic review. J Cosmet Dermatol. 2021;20:3350-3361.
- Fahlbusch M, Wesselmann U, Lehmann P. Herpes zoster after varicella-zoster vaccination [in German]. Hautarzt. 2013;64:107-109.
- Bayas JM, González-Alvarez R, Guinovart C. Herpes zoster after yellow fever vaccination. J Travel Med. 2007;14:65-66.
- Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;10;4:E004833.
- Weitzman D, Shavit O, Stein M, et al. A population based study of the epidemiology of herpes zoster and its complications. J Infect. 2013;67:463-469.
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:E212-E213.
- Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther. 2020;33:e13666.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. 2020;383:2603-2615.
- Bostan E, Yalici-Armagan B. Herpes zoster following inactivated COVID-19 vaccine: a coexistence or coincidence? J Cosmet Dermatol. 2021;20:1566-1567.
- Desai HD, Sharma K, Shah A, et al. Can SARS-CoV-2 vaccine increase the risk of reactivation of varicella zoster? a systematic review. J Cosmet Dermatol. 2021;20:3350-3361.
- Fahlbusch M, Wesselmann U, Lehmann P. Herpes zoster after varicella-zoster vaccination [in German]. Hautarzt. 2013;64:107-109.
- Bayas JM, González-Alvarez R, Guinovart C. Herpes zoster after yellow fever vaccination. J Travel Med. 2007;14:65-66.
- Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;10;4:E004833.
- Weitzman D, Shavit O, Stein M, et al. A population based study of the epidemiology of herpes zoster and its complications. J Infect. 2013;67:463-469.
Practice Points
- Herpes zoster (HZ) has been reported following COVID-19 vaccination.
- Postinjection pain is common with COVID-19 vaccination, but clinical signs such as extension of pain, burning sensation, and eruption of vesicles should lead the physician to consider the diagnosis of HZ, regardless of the delay in onset between the injection and the symptoms.
- When indicated, the second vaccine dose should not be avoided in patients who are diagnosed with HZ.
Children and COVID: New cases, admissions are higher than ever
Weekly COVID-19 cases in children passed 300,000 for the first time since the pandemic started, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The rate of new COVID-related hospital admissions also reached a new high of 0.74 per 100,000 children as of Dec. 31. The highest rate seen before the current Omicron-fueled surge was 0.47 per 100,000 in early September, data from the Centers for Disease Control and Prevention show.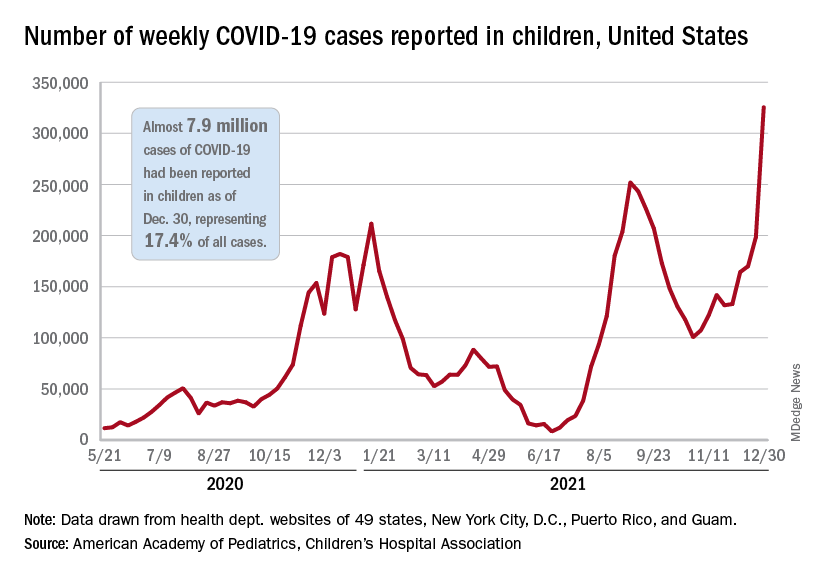
and exceeding the previous week’s count by almost 64%, the AAP and CHA said in their weekly COVID report.
New cases were up in all four regions of the United States, with the Northeast adding the most newly infected children while setting a new high for the fifth consecutive week. The South was just behind for the week but still well off the record it reached in September, the Midwest was third but recorded its busiest week ever, and the West was fourth and nowhere near its previous high, the AAP/CHA report indicated.
The total number of child cases since the pandemic began is almost 7.9 million, they said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. That figure represents 17.4% of all cases reported in the United States, and the cumulative rate of COVID infection is up to almost 10,500 per 100,000 children, meaning that 1 in 10 children have been infected.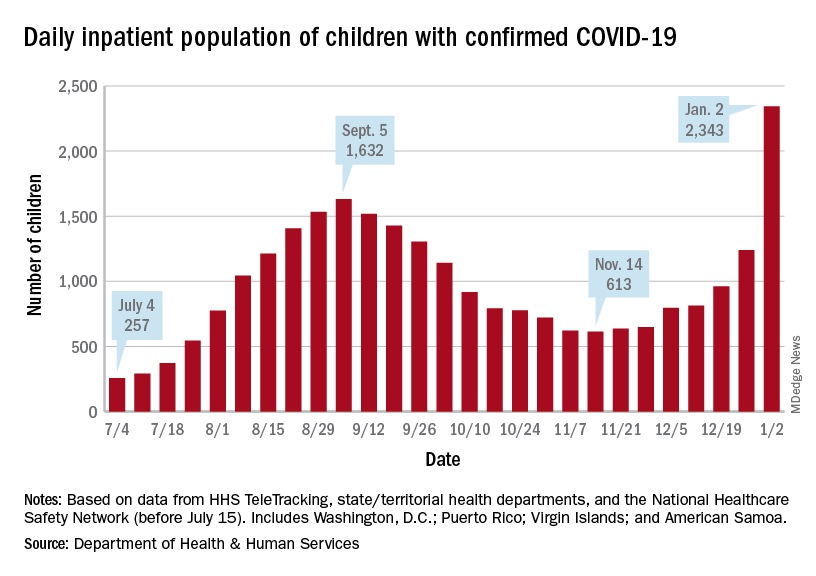
Children are still less likely to be hospitalized than adults, but the gap appears to be closing. On Jan. 2 there were 2,343 children and 87,690 adults in the hospital with confirmed COVID, a ratio of 37 adults for each child, but on Sept. 5, at the height of the previous surge, the ratio of hospitalized adults (93,647) to children (1,632) was 57:1, according to data from the Department of Health & Human Services.
New admissions show a similar pattern: The 0.74 admissions per 100,000 children recorded on Dec. 31 was lower than, for example, adults aged 30-39 years (2.7 per 100,000) or 50-59 years (4.25 per 100,000), but on Sept. 5 the corresponding figures were 0.46 (children), 2.74 (ages 30-39), and 5.03 (aged 50-59), based on the HHS data.
A look at vaccinations
The vaccination response to Omicron, however, has been more subdued and somewhat inconsistent. Vaccine initiation, not surprisingly, was down among eligible children for the week of Dec. 23-29. Before that, both the 5- to 11-year-olds and 12- to 15-year-olds were down for the second week of December and then up a bit (5.6% and 14.3%, respectively) during the third week, while the 16- to 17-year-olds, increased initiation by 63.2%, CDC’s COVID Data Tracker shows.
Less than a quarter (23.5%) of children aged 5-11 received at least one dose of the vaccine in the first 2 months of their eligibility, and only 14.7% are fully vaccinated. Among the older children, coverage looks like this: at least one dose for 61.2% of 12- to 15-year-olds and 67.4% of 16- to 17-year-olds and full vaccination for 51.3% and 57.6%, respectively, the CDC said.
At the state level, Massachusetts and Hawaii have the highest rates for children aged 12-17 years, with 86% having received a least one dose, and Vermont is highest for children aged 5-11 at 56%. The lowest rates can be found in Wyoming (38%) for 12- to 17-year-olds and in Mississippi (6%) for 5- to 11-year-olds, the AAP said in a separate report.
Weekly COVID-19 cases in children passed 300,000 for the first time since the pandemic started, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The rate of new COVID-related hospital admissions also reached a new high of 0.74 per 100,000 children as of Dec. 31. The highest rate seen before the current Omicron-fueled surge was 0.47 per 100,000 in early September, data from the Centers for Disease Control and Prevention show.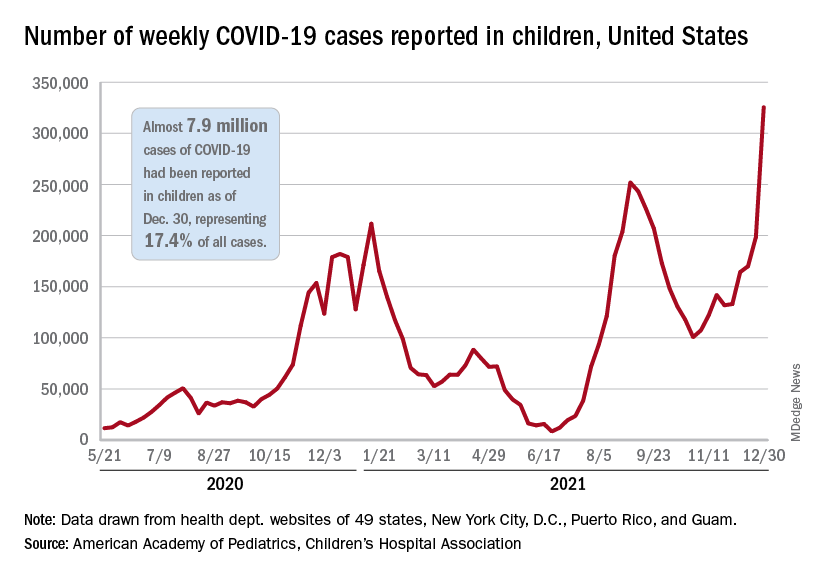
and exceeding the previous week’s count by almost 64%, the AAP and CHA said in their weekly COVID report.
New cases were up in all four regions of the United States, with the Northeast adding the most newly infected children while setting a new high for the fifth consecutive week. The South was just behind for the week but still well off the record it reached in September, the Midwest was third but recorded its busiest week ever, and the West was fourth and nowhere near its previous high, the AAP/CHA report indicated.
The total number of child cases since the pandemic began is almost 7.9 million, they said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. That figure represents 17.4% of all cases reported in the United States, and the cumulative rate of COVID infection is up to almost 10,500 per 100,000 children, meaning that 1 in 10 children have been infected.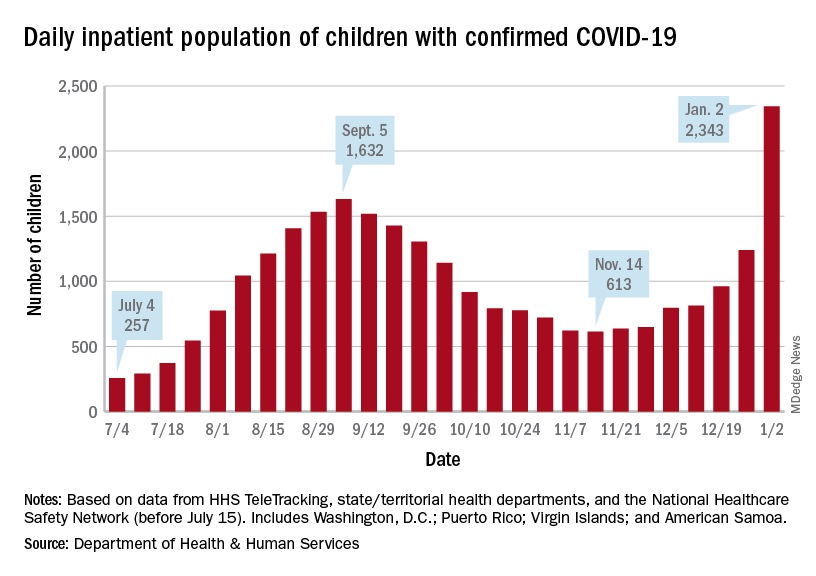
Children are still less likely to be hospitalized than adults, but the gap appears to be closing. On Jan. 2 there were 2,343 children and 87,690 adults in the hospital with confirmed COVID, a ratio of 37 adults for each child, but on Sept. 5, at the height of the previous surge, the ratio of hospitalized adults (93,647) to children (1,632) was 57:1, according to data from the Department of Health & Human Services.
New admissions show a similar pattern: The 0.74 admissions per 100,000 children recorded on Dec. 31 was lower than, for example, adults aged 30-39 years (2.7 per 100,000) or 50-59 years (4.25 per 100,000), but on Sept. 5 the corresponding figures were 0.46 (children), 2.74 (ages 30-39), and 5.03 (aged 50-59), based on the HHS data.
A look at vaccinations
The vaccination response to Omicron, however, has been more subdued and somewhat inconsistent. Vaccine initiation, not surprisingly, was down among eligible children for the week of Dec. 23-29. Before that, both the 5- to 11-year-olds and 12- to 15-year-olds were down for the second week of December and then up a bit (5.6% and 14.3%, respectively) during the third week, while the 16- to 17-year-olds, increased initiation by 63.2%, CDC’s COVID Data Tracker shows.
Less than a quarter (23.5%) of children aged 5-11 received at least one dose of the vaccine in the first 2 months of their eligibility, and only 14.7% are fully vaccinated. Among the older children, coverage looks like this: at least one dose for 61.2% of 12- to 15-year-olds and 67.4% of 16- to 17-year-olds and full vaccination for 51.3% and 57.6%, respectively, the CDC said.
At the state level, Massachusetts and Hawaii have the highest rates for children aged 12-17 years, with 86% having received a least one dose, and Vermont is highest for children aged 5-11 at 56%. The lowest rates can be found in Wyoming (38%) for 12- to 17-year-olds and in Mississippi (6%) for 5- to 11-year-olds, the AAP said in a separate report.
Weekly COVID-19 cases in children passed 300,000 for the first time since the pandemic started, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The rate of new COVID-related hospital admissions also reached a new high of 0.74 per 100,000 children as of Dec. 31. The highest rate seen before the current Omicron-fueled surge was 0.47 per 100,000 in early September, data from the Centers for Disease Control and Prevention show.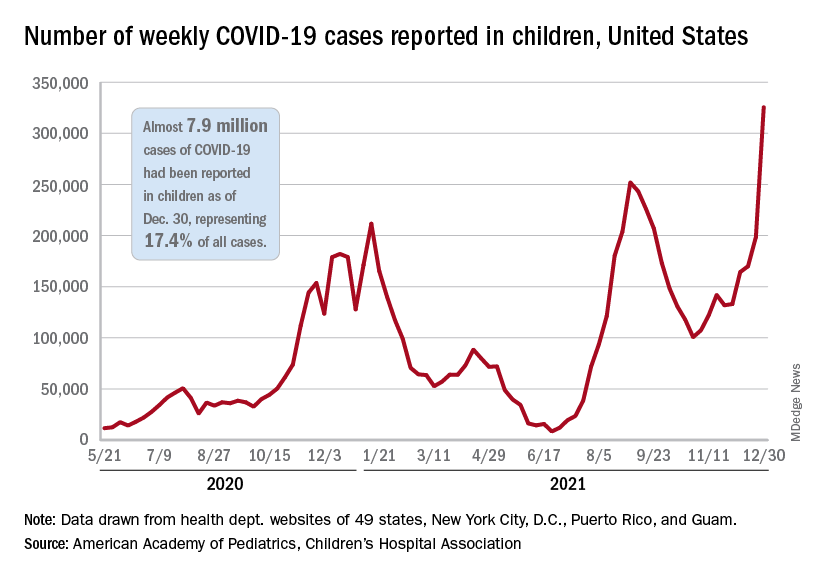
and exceeding the previous week’s count by almost 64%, the AAP and CHA said in their weekly COVID report.
New cases were up in all four regions of the United States, with the Northeast adding the most newly infected children while setting a new high for the fifth consecutive week. The South was just behind for the week but still well off the record it reached in September, the Midwest was third but recorded its busiest week ever, and the West was fourth and nowhere near its previous high, the AAP/CHA report indicated.
The total number of child cases since the pandemic began is almost 7.9 million, they said based on data collected from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. That figure represents 17.4% of all cases reported in the United States, and the cumulative rate of COVID infection is up to almost 10,500 per 100,000 children, meaning that 1 in 10 children have been infected.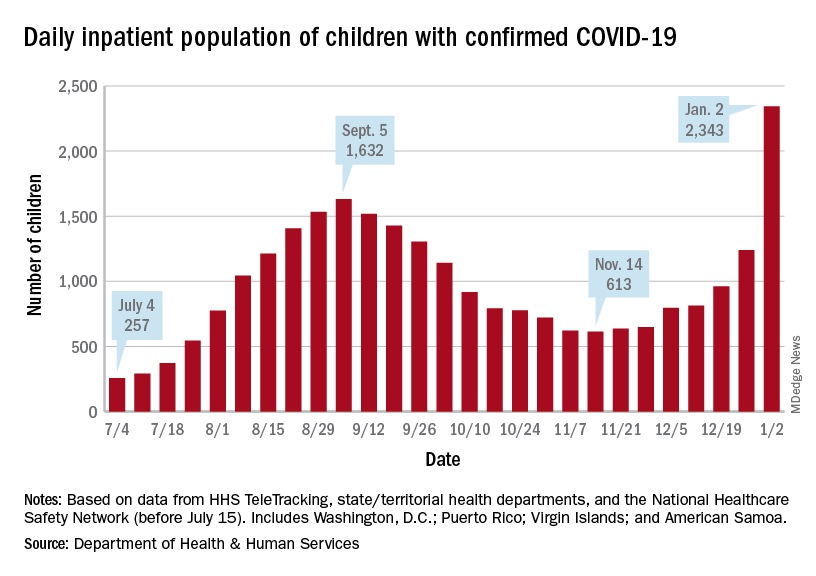
Children are still less likely to be hospitalized than adults, but the gap appears to be closing. On Jan. 2 there were 2,343 children and 87,690 adults in the hospital with confirmed COVID, a ratio of 37 adults for each child, but on Sept. 5, at the height of the previous surge, the ratio of hospitalized adults (93,647) to children (1,632) was 57:1, according to data from the Department of Health & Human Services.
New admissions show a similar pattern: The 0.74 admissions per 100,000 children recorded on Dec. 31 was lower than, for example, adults aged 30-39 years (2.7 per 100,000) or 50-59 years (4.25 per 100,000), but on Sept. 5 the corresponding figures were 0.46 (children), 2.74 (ages 30-39), and 5.03 (aged 50-59), based on the HHS data.
A look at vaccinations
The vaccination response to Omicron, however, has been more subdued and somewhat inconsistent. Vaccine initiation, not surprisingly, was down among eligible children for the week of Dec. 23-29. Before that, both the 5- to 11-year-olds and 12- to 15-year-olds were down for the second week of December and then up a bit (5.6% and 14.3%, respectively) during the third week, while the 16- to 17-year-olds, increased initiation by 63.2%, CDC’s COVID Data Tracker shows.
Less than a quarter (23.5%) of children aged 5-11 received at least one dose of the vaccine in the first 2 months of their eligibility, and only 14.7% are fully vaccinated. Among the older children, coverage looks like this: at least one dose for 61.2% of 12- to 15-year-olds and 67.4% of 16- to 17-year-olds and full vaccination for 51.3% and 57.6%, respectively, the CDC said.
At the state level, Massachusetts and Hawaii have the highest rates for children aged 12-17 years, with 86% having received a least one dose, and Vermont is highest for children aged 5-11 at 56%. The lowest rates can be found in Wyoming (38%) for 12- to 17-year-olds and in Mississippi (6%) for 5- to 11-year-olds, the AAP said in a separate report.
