User login
Intervention improves antibiotics use in UTIs
A multifaceted intervention significantly changed clinicians’ use of antibiotics to treat urinary tract infections (UTIs) in children, according to data from more than 2,000 cases observed between January 2014 and September 2018.
“Changing clinicians’ antibiotic prescribing practices can be challenging; barriers to change include lack of awareness of new evidence, competing clinical demands, and concern about treatment failure,” wrote Matthew F. Daley, MD, of Kaiser Permanente Colorado, Aurora, and colleagues in Pediatrics.
To promote judicious antibiotic use, the researchers designed an intervention including the development of new local UTI guidelines; a live, case-based educational session; emailed knowledge assessments before and after the session; and a specific UTI order set in the EHR.
The researchers divided the study period into a preintervention period (January 1, 2014, to April 25, 2017) and a postintervention period (April 26, 2017, to September 30, 2018). They collected data on 2,142 incident outpatient UTIs; 1,636 from the preintervention period and 506 from the postintervention period. The patients were younger than 18 years and older than 60 days, and children with complicated urologic or neurologic conditions were excluded.
(P less than .0001). In particular, the use of first-line, narrow spectrum cephalexin increased significantly from 29% during the preintervention period to 53% during the postintervention period (P less than .0001). In addition, use of broad spectrum cefixime decreased from 17% during the preintervention period to 3% during the postintervention period (P less than .0001). These changes in prescribing patterns continued through the end of the study period, the researchers said.
The study was limited by several factors, notably that “the interrupted time-series design prevents us from inferring that the intervention caused the observed change in practice,” the researchers wrote. However, other factors including the immediate change in prescribing patterns after the intervention, multiple time points, large sample size, and consistent UTI case mix support the impact of the intervention, they suggested. Although the results might not translate completely to other settings, “developing a UTI-specific EHR order set is relatively straightforward” and might be applied elsewhere, they noted.
“Despite the limitations inherent in a nonexperimental study design, the methods and interventions developed in the current study may be informative to other learning health systems and other content areas when conducting organization-wide quality improvement initiatives,” they concluded.
The study was supported by unrestricted internal resources from the Colorado Permanente Medical Group. The researchers had no financial conflicts to disclose.
SOURCE: Daley MF et al. Pediatrics. 2020 Mar 3. doi: 10.1542/peds.2019-2503.
A multifaceted intervention significantly changed clinicians’ use of antibiotics to treat urinary tract infections (UTIs) in children, according to data from more than 2,000 cases observed between January 2014 and September 2018.
“Changing clinicians’ antibiotic prescribing practices can be challenging; barriers to change include lack of awareness of new evidence, competing clinical demands, and concern about treatment failure,” wrote Matthew F. Daley, MD, of Kaiser Permanente Colorado, Aurora, and colleagues in Pediatrics.
To promote judicious antibiotic use, the researchers designed an intervention including the development of new local UTI guidelines; a live, case-based educational session; emailed knowledge assessments before and after the session; and a specific UTI order set in the EHR.
The researchers divided the study period into a preintervention period (January 1, 2014, to April 25, 2017) and a postintervention period (April 26, 2017, to September 30, 2018). They collected data on 2,142 incident outpatient UTIs; 1,636 from the preintervention period and 506 from the postintervention period. The patients were younger than 18 years and older than 60 days, and children with complicated urologic or neurologic conditions were excluded.
(P less than .0001). In particular, the use of first-line, narrow spectrum cephalexin increased significantly from 29% during the preintervention period to 53% during the postintervention period (P less than .0001). In addition, use of broad spectrum cefixime decreased from 17% during the preintervention period to 3% during the postintervention period (P less than .0001). These changes in prescribing patterns continued through the end of the study period, the researchers said.
The study was limited by several factors, notably that “the interrupted time-series design prevents us from inferring that the intervention caused the observed change in practice,” the researchers wrote. However, other factors including the immediate change in prescribing patterns after the intervention, multiple time points, large sample size, and consistent UTI case mix support the impact of the intervention, they suggested. Although the results might not translate completely to other settings, “developing a UTI-specific EHR order set is relatively straightforward” and might be applied elsewhere, they noted.
“Despite the limitations inherent in a nonexperimental study design, the methods and interventions developed in the current study may be informative to other learning health systems and other content areas when conducting organization-wide quality improvement initiatives,” they concluded.
The study was supported by unrestricted internal resources from the Colorado Permanente Medical Group. The researchers had no financial conflicts to disclose.
SOURCE: Daley MF et al. Pediatrics. 2020 Mar 3. doi: 10.1542/peds.2019-2503.
A multifaceted intervention significantly changed clinicians’ use of antibiotics to treat urinary tract infections (UTIs) in children, according to data from more than 2,000 cases observed between January 2014 and September 2018.
“Changing clinicians’ antibiotic prescribing practices can be challenging; barriers to change include lack of awareness of new evidence, competing clinical demands, and concern about treatment failure,” wrote Matthew F. Daley, MD, of Kaiser Permanente Colorado, Aurora, and colleagues in Pediatrics.
To promote judicious antibiotic use, the researchers designed an intervention including the development of new local UTI guidelines; a live, case-based educational session; emailed knowledge assessments before and after the session; and a specific UTI order set in the EHR.
The researchers divided the study period into a preintervention period (January 1, 2014, to April 25, 2017) and a postintervention period (April 26, 2017, to September 30, 2018). They collected data on 2,142 incident outpatient UTIs; 1,636 from the preintervention period and 506 from the postintervention period. The patients were younger than 18 years and older than 60 days, and children with complicated urologic or neurologic conditions were excluded.
(P less than .0001). In particular, the use of first-line, narrow spectrum cephalexin increased significantly from 29% during the preintervention period to 53% during the postintervention period (P less than .0001). In addition, use of broad spectrum cefixime decreased from 17% during the preintervention period to 3% during the postintervention period (P less than .0001). These changes in prescribing patterns continued through the end of the study period, the researchers said.
The study was limited by several factors, notably that “the interrupted time-series design prevents us from inferring that the intervention caused the observed change in practice,” the researchers wrote. However, other factors including the immediate change in prescribing patterns after the intervention, multiple time points, large sample size, and consistent UTI case mix support the impact of the intervention, they suggested. Although the results might not translate completely to other settings, “developing a UTI-specific EHR order set is relatively straightforward” and might be applied elsewhere, they noted.
“Despite the limitations inherent in a nonexperimental study design, the methods and interventions developed in the current study may be informative to other learning health systems and other content areas when conducting organization-wide quality improvement initiatives,” they concluded.
The study was supported by unrestricted internal resources from the Colorado Permanente Medical Group. The researchers had no financial conflicts to disclose.
SOURCE: Daley MF et al. Pediatrics. 2020 Mar 3. doi: 10.1542/peds.2019-2503.
FROM PEDIATRICS
Key clinical point: After an educational intervention, approximately 62% of clinicians prescribed first-line antibiotics, up from 43% before the intervention.
Major finding: Cephalexin use increased from 29% before the intervention to 53% after the intervention.
Study details: The data come from a review of 2,142 incident outpatient cases of urinary tract infection in patients aged older than 60 days up to 18 years.
Disclosures: The study was supported by unrestricted internal resources from the Colorado Permanente Medical Group. The researchers had no financial conflicts to disclose.
Source: Daley MF et al. Pediatrics. 2020 Mar 3. doi: 10.1542/peds.2019-2503.
Coronavirus outbreak: Time to prepare
References
- Interim Infection Prevention and Control Recommendations for Patients with Confirmed Coronavirus Disease 2019 (COVID-19) or Persons Under Investigation for COVID-19 in Healthcare Settings. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Updated February 21, 2020. Accessed February 27, 2020.
- Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for 2019 Novel Coronavirus (2019-nCoV). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-home-care.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Preventing the Spread of Coronavirus Disease 2019 (COVID-19) in Homes and Residential Communities. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-prevent-spread.html. Updated February 14, 2020. Accessed February 27, 2020.
- World Health Organization. Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Updated February 26, 2020. Accessed February 27, 2020.
- Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html. Updated February 26, 2020. Accessed February 27, 2020.
ALSO, see last month’s audiocast: “Coronavirus outbreak: Putting it into perspective.”
References
- Interim Infection Prevention and Control Recommendations for Patients with Confirmed Coronavirus Disease 2019 (COVID-19) or Persons Under Investigation for COVID-19 in Healthcare Settings. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Updated February 21, 2020. Accessed February 27, 2020.
- Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for 2019 Novel Coronavirus (2019-nCoV). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-home-care.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Preventing the Spread of Coronavirus Disease 2019 (COVID-19) in Homes and Residential Communities. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-prevent-spread.html. Updated February 14, 2020. Accessed February 27, 2020.
- World Health Organization. Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Updated February 26, 2020. Accessed February 27, 2020.
- Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html. Updated February 26, 2020. Accessed February 27, 2020.
ALSO, see last month’s audiocast: “Coronavirus outbreak: Putting it into perspective.”
References
- Interim Infection Prevention and Control Recommendations for Patients with Confirmed Coronavirus Disease 2019 (COVID-19) or Persons Under Investigation for COVID-19 in Healthcare Settings. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Updated February 21, 2020. Accessed February 27, 2020.
- Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for 2019 Novel Coronavirus (2019-nCoV). Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-home-care.html. Updated February 12, 2020. Accessed February 27, 2020.
- Interim Guidance for Preventing the Spread of Coronavirus Disease 2019 (COVID-19) in Homes and Residential Communities. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-prevent-spread.html. Updated February 14, 2020. Accessed February 27, 2020.
- World Health Organization. Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Updated February 26, 2020. Accessed February 27, 2020.
- Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html. Updated February 26, 2020. Accessed February 27, 2020.
ALSO, see last month’s audiocast: “Coronavirus outbreak: Putting it into perspective.”
Washington State grapples with coronavirus outbreak
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
FROM A KING COUNTY, WASH. NEWS BRIEFING
Meta-analysis highlights safety concerns with interleukin inhibition
MAUI, HAWAII – The use of interleukin inhibitors for treatment of rheumatologic diseases doubles a patient’s risk of serious infections, according to a comprehensive systematic review and meta-analysis of 74 randomized, placebo-controlled trials presented by Jawad Bilal, MBBS, at the 2020 Rheumatology Winter Clinical Symposium.
The meta-analysis, which incorporated 29,214 patients with a variety of rheumatic diseases, demonstrated that patients receiving interleukin (IL) inhibitors had a 1.97-fold increased risk of serious infections, a finding accompanied by a high degree of statistical certainty. The number-needed-to-harm was 67 patients treated for a median of 24 weeks in order to generate one additional serious infection.
“That number-needed-to-harm is a significant finding because having a serious infection means by definition you’re getting admitted to the hospital and receiving IV antibiotics,” Dr. Bilal observed in an interview.
The meta-analysis also found that IL inhibition was associated with a 2.35-fold increased risk of opportunistic infections and a 1.52-fold higher risk of developing cancer, both findings with statistical significance (P =.03) but only moderate certainty because fewer of those events were captured in the trials compared to the numbers of serious infections, explained Dr. Bilal of the University of Arizona, Tucson.
For opportunistic infections, the number-needed-to-harm was 250 patients treated with an IL inhibitor for a median of 54 weeks in order to result in one additional opportunistic infection. For cancer, the number-needed-to-harm was 250 for a median of 24 weeks.
Dr. Bilal noted that while the IL inhibitors are drugs of established efficacy in rheumatologic diseases, their safety has not previously undergone anything approaching the comprehensive scrutiny carried out in this meta-analysis. The meta-analysis, which included all published placebo-controlled randomized trials and their extension studies, employed rigorous methodology in accord with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement and the GRADE approach to data analysis. Studies of IL inhibitors in patients with dermatologic and GI diseases were excluded from the meta-analysis.
He offered a caveat regarding the cancer risk findings: “Our analysis showed that the cancer risk is increased, but the results are not conclusive because we only had a few years of data. With cancer, you really need at least 8-10 years of data. So the real-world experience with the interleukin inhibitors in the large registries is what’s going to tell if the cancer risk is really increased or not. In the meantime, we all have to be cautious.”
The number of serious infections collected in the meta-analysis afforded sufficient statistical power for the investigators to break down differential risks based on individual drugs and indications. Among the drugs associated with significantly increased risk of serious infections were anakinra, with an odds ratio of 2.67, compared with placebo; secukinumab with an OR of 2.43; and tocilizumab with an OR or 1.76. Ustekinumab and ixekizumab were associated with 2.57- and 3.89-fold increased risks, respectively, but the number of rheumatology patients treated with those two biologics wasn’t large enough for those findings to achieve statistical significance.
Rheumatoid arthritis patients who received an IL inhibitor rather than placebo had a 1.98-fold increased risk of serious infection, while those with psoriatic arthritis had a 2.21-fold increased risk. Patients treated for SLE had a 6.44-fold increased risk, and those with juvenile idiopathic arthritis had a 5.37-fold higher risk, but the margins for error were such that those results weren’t statistically significant.
“I think this study is going to help clinicians and patients when they’re trying to weigh the risks and benefits of IL inhibitors, especially if they already have risk factors, like a recent history of serious infection or a history of cancer or of opportunistic infection,” Dr. Bilal commented.
A study limitation was that he and his coinvestigators had to lump together the various IL inhibitors in order to gain statistical power, even though the drugs work differently, he noted.
Dr. Bilal reported having no financial conflicts regarding his study, the full details of which have been published (JAMA Netw Open. 2019 Oct 2. doi: 10.1001/jamanetworkopen.2019.13102).
MAUI, HAWAII – The use of interleukin inhibitors for treatment of rheumatologic diseases doubles a patient’s risk of serious infections, according to a comprehensive systematic review and meta-analysis of 74 randomized, placebo-controlled trials presented by Jawad Bilal, MBBS, at the 2020 Rheumatology Winter Clinical Symposium.
The meta-analysis, which incorporated 29,214 patients with a variety of rheumatic diseases, demonstrated that patients receiving interleukin (IL) inhibitors had a 1.97-fold increased risk of serious infections, a finding accompanied by a high degree of statistical certainty. The number-needed-to-harm was 67 patients treated for a median of 24 weeks in order to generate one additional serious infection.
“That number-needed-to-harm is a significant finding because having a serious infection means by definition you’re getting admitted to the hospital and receiving IV antibiotics,” Dr. Bilal observed in an interview.
The meta-analysis also found that IL inhibition was associated with a 2.35-fold increased risk of opportunistic infections and a 1.52-fold higher risk of developing cancer, both findings with statistical significance (P =.03) but only moderate certainty because fewer of those events were captured in the trials compared to the numbers of serious infections, explained Dr. Bilal of the University of Arizona, Tucson.
For opportunistic infections, the number-needed-to-harm was 250 patients treated with an IL inhibitor for a median of 54 weeks in order to result in one additional opportunistic infection. For cancer, the number-needed-to-harm was 250 for a median of 24 weeks.
Dr. Bilal noted that while the IL inhibitors are drugs of established efficacy in rheumatologic diseases, their safety has not previously undergone anything approaching the comprehensive scrutiny carried out in this meta-analysis. The meta-analysis, which included all published placebo-controlled randomized trials and their extension studies, employed rigorous methodology in accord with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement and the GRADE approach to data analysis. Studies of IL inhibitors in patients with dermatologic and GI diseases were excluded from the meta-analysis.
He offered a caveat regarding the cancer risk findings: “Our analysis showed that the cancer risk is increased, but the results are not conclusive because we only had a few years of data. With cancer, you really need at least 8-10 years of data. So the real-world experience with the interleukin inhibitors in the large registries is what’s going to tell if the cancer risk is really increased or not. In the meantime, we all have to be cautious.”
The number of serious infections collected in the meta-analysis afforded sufficient statistical power for the investigators to break down differential risks based on individual drugs and indications. Among the drugs associated with significantly increased risk of serious infections were anakinra, with an odds ratio of 2.67, compared with placebo; secukinumab with an OR of 2.43; and tocilizumab with an OR or 1.76. Ustekinumab and ixekizumab were associated with 2.57- and 3.89-fold increased risks, respectively, but the number of rheumatology patients treated with those two biologics wasn’t large enough for those findings to achieve statistical significance.
Rheumatoid arthritis patients who received an IL inhibitor rather than placebo had a 1.98-fold increased risk of serious infection, while those with psoriatic arthritis had a 2.21-fold increased risk. Patients treated for SLE had a 6.44-fold increased risk, and those with juvenile idiopathic arthritis had a 5.37-fold higher risk, but the margins for error were such that those results weren’t statistically significant.
“I think this study is going to help clinicians and patients when they’re trying to weigh the risks and benefits of IL inhibitors, especially if they already have risk factors, like a recent history of serious infection or a history of cancer or of opportunistic infection,” Dr. Bilal commented.
A study limitation was that he and his coinvestigators had to lump together the various IL inhibitors in order to gain statistical power, even though the drugs work differently, he noted.
Dr. Bilal reported having no financial conflicts regarding his study, the full details of which have been published (JAMA Netw Open. 2019 Oct 2. doi: 10.1001/jamanetworkopen.2019.13102).
MAUI, HAWAII – The use of interleukin inhibitors for treatment of rheumatologic diseases doubles a patient’s risk of serious infections, according to a comprehensive systematic review and meta-analysis of 74 randomized, placebo-controlled trials presented by Jawad Bilal, MBBS, at the 2020 Rheumatology Winter Clinical Symposium.
The meta-analysis, which incorporated 29,214 patients with a variety of rheumatic diseases, demonstrated that patients receiving interleukin (IL) inhibitors had a 1.97-fold increased risk of serious infections, a finding accompanied by a high degree of statistical certainty. The number-needed-to-harm was 67 patients treated for a median of 24 weeks in order to generate one additional serious infection.
“That number-needed-to-harm is a significant finding because having a serious infection means by definition you’re getting admitted to the hospital and receiving IV antibiotics,” Dr. Bilal observed in an interview.
The meta-analysis also found that IL inhibition was associated with a 2.35-fold increased risk of opportunistic infections and a 1.52-fold higher risk of developing cancer, both findings with statistical significance (P =.03) but only moderate certainty because fewer of those events were captured in the trials compared to the numbers of serious infections, explained Dr. Bilal of the University of Arizona, Tucson.
For opportunistic infections, the number-needed-to-harm was 250 patients treated with an IL inhibitor for a median of 54 weeks in order to result in one additional opportunistic infection. For cancer, the number-needed-to-harm was 250 for a median of 24 weeks.
Dr. Bilal noted that while the IL inhibitors are drugs of established efficacy in rheumatologic diseases, their safety has not previously undergone anything approaching the comprehensive scrutiny carried out in this meta-analysis. The meta-analysis, which included all published placebo-controlled randomized trials and their extension studies, employed rigorous methodology in accord with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement and the GRADE approach to data analysis. Studies of IL inhibitors in patients with dermatologic and GI diseases were excluded from the meta-analysis.
He offered a caveat regarding the cancer risk findings: “Our analysis showed that the cancer risk is increased, but the results are not conclusive because we only had a few years of data. With cancer, you really need at least 8-10 years of data. So the real-world experience with the interleukin inhibitors in the large registries is what’s going to tell if the cancer risk is really increased or not. In the meantime, we all have to be cautious.”
The number of serious infections collected in the meta-analysis afforded sufficient statistical power for the investigators to break down differential risks based on individual drugs and indications. Among the drugs associated with significantly increased risk of serious infections were anakinra, with an odds ratio of 2.67, compared with placebo; secukinumab with an OR of 2.43; and tocilizumab with an OR or 1.76. Ustekinumab and ixekizumab were associated with 2.57- and 3.89-fold increased risks, respectively, but the number of rheumatology patients treated with those two biologics wasn’t large enough for those findings to achieve statistical significance.
Rheumatoid arthritis patients who received an IL inhibitor rather than placebo had a 1.98-fold increased risk of serious infection, while those with psoriatic arthritis had a 2.21-fold increased risk. Patients treated for SLE had a 6.44-fold increased risk, and those with juvenile idiopathic arthritis had a 5.37-fold higher risk, but the margins for error were such that those results weren’t statistically significant.
“I think this study is going to help clinicians and patients when they’re trying to weigh the risks and benefits of IL inhibitors, especially if they already have risk factors, like a recent history of serious infection or a history of cancer or of opportunistic infection,” Dr. Bilal commented.
A study limitation was that he and his coinvestigators had to lump together the various IL inhibitors in order to gain statistical power, even though the drugs work differently, he noted.
Dr. Bilal reported having no financial conflicts regarding his study, the full details of which have been published (JAMA Netw Open. 2019 Oct 2. doi: 10.1001/jamanetworkopen.2019.13102).
REPORTING FROM RWCS 2020
Screen all adults for hepatitis C, says USPSTF
Adults aged 18-79 years should be screened for hepatitis C virus infection, according to an updated grade B recommendation from the U.S. Preventive Services Task Force.
Cases of acute hepatitis C virus (HCV) infection have spiked in the last decade, in part because of increased use of injection drugs and in part because of better surveillance, Douglas K. Owens, MD, of Stanford (Calif.) University, and colleagues wrote in the recommendation statement published in JAMA.
The recommendation applies to all asymptomatic adults aged 18-79 years without known liver disease, and expands on the 2013 recommendation to screen adults born between 1945 and 1965. The grade B designation means that the task force concluded with moderate certainty that HCV screening for adults aged 18-79 years had “substantial net benefit.”
The recommendations are based on an evidence report including 8 randomized, controlled trials, 48 other treatment studies, and 33 cohort studies published through February 2019 for a total of 179,230 individuals.
The screening is a one-time procedure for most adults, according to the task force, but clinicians should periodically screen individuals at increased risk, such as those with a past or current history of injection drug use. In addition, clinicians should consider screening individuals at increased risk who are above or below the recommended age range.
Although the task force identified no direct evidence on the benefit of screening for HCV infection in asymptomatic adults, a notable finding was that the newer direct-acting antiviral (DAA) regimens are sufficiently effective to support the expanded screening recommendation, they said. However, clinicians should inform patients that screening is voluntary and conducted only with the patient’s knowledge. Clinicians should educate patients about hepatitis C and give them an opportunity to ask questions and to make a decision about screening, according to the task force.
In the evidence report, a total of 49 studies including 10,181 individuals showed DAA treatment associated with pooled sustained virologic response rates greater than 95% across all virus genotypes, and a short-term serious adverse event rate of 1.9%. In addition, sustained virologic response following an antiviral therapy was associated with a reduction in risk of all-cause mortality (pooled hazard ratio 0.40) and of hepatocellular carcinoma (pooled HR 0.29) compared with cases of no sustained virologic response.
The evidence report findings were limited by several factors, including the relatively small number of randomized trials involving current DAA treatments, limited data on baseline symptoms, limited data on adolescents, and limited evidence on potential long-term harms of DAA therapy, noted Richard Chou, MD, of Oregon Health & Science University, Portland, and colleagues. However, new pooled evidence “indicates that SVR rates with currently recommended all-oral DAA regimens are substantially higher (more than 95%) than with interferon-based therapies evaluated in the prior review (68%-78%),” they said.
Several editorials were published concurrently with the recommendation.
In an editorial published in JAMA, Camilla S. Graham, MD, of Harvard Medical School, Boston, and Stacey Trooskin, MD, of the University of Pennsylvania, Philadelphia, wrote that the new recommendation reflects changes in hepatitis C virus management.
“With the approvals of sofosbuvir and simeprevir in 2013, patients with hepatitis C, a chronic viral illness associated with the deaths of more U.S. patients than the next 60 reportable infectious diseases combined, including HIV and tuberculosis, could expect a greater than 90% rate of achieving sustained virologic response (SVR, defined as undetectable HCV levels 12 weeks or longer after treatment completion, which is consistent with virologic cure of HCV infection) following 12 weeks of treatment,” they said.
These medications are effective but expensive; however, the combination of the availability of generic medications and the ongoing opioid epidemic in the United States are important contributors to the expanded recommendations, which “are welcome,” and may help meeting WHO 2030 targets for reducing new HCV infections, they said.
Dr. Graham disclosed personal fees from UpToDate. Dr. Trooskin disclosed grants from Gilead Sciences and personal fees from Merck, AbbVie, and Gilead Sciences.
In an editorial published in JAMA Internal Medicine, Jennifer C. Price, MD, and Danielle Brandman, MD, both of the University of California, San Francisco, wrote that “the advancements in HCV diagnosis and treatment have been extraordinary,” but that the new recommendation does not go far enough. “Implementation of HCV screening and linkage to treatment requires large-scale coordinated efforts, innovation, and resources. For example, point-of-care HCV RNA testing would enable scale-up of HCV screening and confirmatory testing among individuals at greatest risk of HCV infection,” they said. “Additionally, barriers remain between diagnosis and treatment, such as access to a health care provider who can treat HCV and authorization to receive affordable DAAs,” they noted. “Although the USPSTF HCV screening recommendation is a step forward for controlling HCV infection in the U.S., it will take a coordinated and funded effort to ensure that the anticipated benefits are realized,” they concluded.
Dr. Price disclosed research funding from Gilead Sciences and Merck. Dr. Brandman disclosed research funding from Gilead Sciences, Pfizer, Conatus, Allergan, and Grifols, as well as personal fees from Alnylam.
In an editorial published in JAMA Network Open, Eli S. Rosenberg, PhD, of the University at Albany (N.Y.) School of Public Health, and Joshua A. Barocas, MD, of Boston University, emphasized the need to change the stigma surrounding HCV infection in the United States.
“Given the changing epidemiology of HCV infection, new public health priorities, advancements in treatment, and unmet diagnostic needs, it is wise to periodically reevaluate screening recommendations to ensure that they are maximally addressing these areas and patients’ individual needs,” they said. “The Affordable Care Act requires private insurers and Medicaid to cover preventive services recommended by the USPSTF with a grade of A or B with no cost sharing (i.e., no deductible or copayment),” they noted. Although the new recommendation for one-time screening will likely identify more cases, improve outcomes, and reduce deaths, the editorialists cautioned that “one-time screening should not be interpreted like catch-up vaccinations, whereby we immunize someone at any age for hepatitis B virus, for example, and they are then immunized for the remainder of their life,” and that reassessments are needed, especially for younger adults.
In addition, they emphasized the need to reduce the stigma surrounding HCV and allow for recommendations based on risk, rather than age. “We have forced the USPSTF to adopt age-based screening recommendations because we, as a society, have created a culture in which we have stigmatized these behaviors and we, as practitioners, have proven to be inadequate at eliciting HCV risk behaviors,” they said. “Our responsibility as a society and practice community is to address structural and individual factors that limit our ability to most precisely address the needs of our patients and truly move toward HCV elimination,” they concluded.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The task force researchers had no financial conflicts to disclose.
SOURCES: Owens DK et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2020.1123; Chou R et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.20788; Graham CS, Trooskin S. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.22313; Price JC and Brandman D. JAMA Intern Med. 2020 Mar 2. doi: 10.1001/jamainternmed.2019.7334; Rosenberg ES, Barocas JA. JAMA Network Open. 2020 Mar 2. doi: 10.1001/jamanetworkopen.2020.0538.
Adults aged 18-79 years should be screened for hepatitis C virus infection, according to an updated grade B recommendation from the U.S. Preventive Services Task Force.
Cases of acute hepatitis C virus (HCV) infection have spiked in the last decade, in part because of increased use of injection drugs and in part because of better surveillance, Douglas K. Owens, MD, of Stanford (Calif.) University, and colleagues wrote in the recommendation statement published in JAMA.
The recommendation applies to all asymptomatic adults aged 18-79 years without known liver disease, and expands on the 2013 recommendation to screen adults born between 1945 and 1965. The grade B designation means that the task force concluded with moderate certainty that HCV screening for adults aged 18-79 years had “substantial net benefit.”
The recommendations are based on an evidence report including 8 randomized, controlled trials, 48 other treatment studies, and 33 cohort studies published through February 2019 for a total of 179,230 individuals.
The screening is a one-time procedure for most adults, according to the task force, but clinicians should periodically screen individuals at increased risk, such as those with a past or current history of injection drug use. In addition, clinicians should consider screening individuals at increased risk who are above or below the recommended age range.
Although the task force identified no direct evidence on the benefit of screening for HCV infection in asymptomatic adults, a notable finding was that the newer direct-acting antiviral (DAA) regimens are sufficiently effective to support the expanded screening recommendation, they said. However, clinicians should inform patients that screening is voluntary and conducted only with the patient’s knowledge. Clinicians should educate patients about hepatitis C and give them an opportunity to ask questions and to make a decision about screening, according to the task force.
In the evidence report, a total of 49 studies including 10,181 individuals showed DAA treatment associated with pooled sustained virologic response rates greater than 95% across all virus genotypes, and a short-term serious adverse event rate of 1.9%. In addition, sustained virologic response following an antiviral therapy was associated with a reduction in risk of all-cause mortality (pooled hazard ratio 0.40) and of hepatocellular carcinoma (pooled HR 0.29) compared with cases of no sustained virologic response.
The evidence report findings were limited by several factors, including the relatively small number of randomized trials involving current DAA treatments, limited data on baseline symptoms, limited data on adolescents, and limited evidence on potential long-term harms of DAA therapy, noted Richard Chou, MD, of Oregon Health & Science University, Portland, and colleagues. However, new pooled evidence “indicates that SVR rates with currently recommended all-oral DAA regimens are substantially higher (more than 95%) than with interferon-based therapies evaluated in the prior review (68%-78%),” they said.
Several editorials were published concurrently with the recommendation.
In an editorial published in JAMA, Camilla S. Graham, MD, of Harvard Medical School, Boston, and Stacey Trooskin, MD, of the University of Pennsylvania, Philadelphia, wrote that the new recommendation reflects changes in hepatitis C virus management.
“With the approvals of sofosbuvir and simeprevir in 2013, patients with hepatitis C, a chronic viral illness associated with the deaths of more U.S. patients than the next 60 reportable infectious diseases combined, including HIV and tuberculosis, could expect a greater than 90% rate of achieving sustained virologic response (SVR, defined as undetectable HCV levels 12 weeks or longer after treatment completion, which is consistent with virologic cure of HCV infection) following 12 weeks of treatment,” they said.
These medications are effective but expensive; however, the combination of the availability of generic medications and the ongoing opioid epidemic in the United States are important contributors to the expanded recommendations, which “are welcome,” and may help meeting WHO 2030 targets for reducing new HCV infections, they said.
Dr. Graham disclosed personal fees from UpToDate. Dr. Trooskin disclosed grants from Gilead Sciences and personal fees from Merck, AbbVie, and Gilead Sciences.
In an editorial published in JAMA Internal Medicine, Jennifer C. Price, MD, and Danielle Brandman, MD, both of the University of California, San Francisco, wrote that “the advancements in HCV diagnosis and treatment have been extraordinary,” but that the new recommendation does not go far enough. “Implementation of HCV screening and linkage to treatment requires large-scale coordinated efforts, innovation, and resources. For example, point-of-care HCV RNA testing would enable scale-up of HCV screening and confirmatory testing among individuals at greatest risk of HCV infection,” they said. “Additionally, barriers remain between diagnosis and treatment, such as access to a health care provider who can treat HCV and authorization to receive affordable DAAs,” they noted. “Although the USPSTF HCV screening recommendation is a step forward for controlling HCV infection in the U.S., it will take a coordinated and funded effort to ensure that the anticipated benefits are realized,” they concluded.
Dr. Price disclosed research funding from Gilead Sciences and Merck. Dr. Brandman disclosed research funding from Gilead Sciences, Pfizer, Conatus, Allergan, and Grifols, as well as personal fees from Alnylam.
In an editorial published in JAMA Network Open, Eli S. Rosenberg, PhD, of the University at Albany (N.Y.) School of Public Health, and Joshua A. Barocas, MD, of Boston University, emphasized the need to change the stigma surrounding HCV infection in the United States.
“Given the changing epidemiology of HCV infection, new public health priorities, advancements in treatment, and unmet diagnostic needs, it is wise to periodically reevaluate screening recommendations to ensure that they are maximally addressing these areas and patients’ individual needs,” they said. “The Affordable Care Act requires private insurers and Medicaid to cover preventive services recommended by the USPSTF with a grade of A or B with no cost sharing (i.e., no deductible or copayment),” they noted. Although the new recommendation for one-time screening will likely identify more cases, improve outcomes, and reduce deaths, the editorialists cautioned that “one-time screening should not be interpreted like catch-up vaccinations, whereby we immunize someone at any age for hepatitis B virus, for example, and they are then immunized for the remainder of their life,” and that reassessments are needed, especially for younger adults.
In addition, they emphasized the need to reduce the stigma surrounding HCV and allow for recommendations based on risk, rather than age. “We have forced the USPSTF to adopt age-based screening recommendations because we, as a society, have created a culture in which we have stigmatized these behaviors and we, as practitioners, have proven to be inadequate at eliciting HCV risk behaviors,” they said. “Our responsibility as a society and practice community is to address structural and individual factors that limit our ability to most precisely address the needs of our patients and truly move toward HCV elimination,” they concluded.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The task force researchers had no financial conflicts to disclose.
SOURCES: Owens DK et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2020.1123; Chou R et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.20788; Graham CS, Trooskin S. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.22313; Price JC and Brandman D. JAMA Intern Med. 2020 Mar 2. doi: 10.1001/jamainternmed.2019.7334; Rosenberg ES, Barocas JA. JAMA Network Open. 2020 Mar 2. doi: 10.1001/jamanetworkopen.2020.0538.
Adults aged 18-79 years should be screened for hepatitis C virus infection, according to an updated grade B recommendation from the U.S. Preventive Services Task Force.
Cases of acute hepatitis C virus (HCV) infection have spiked in the last decade, in part because of increased use of injection drugs and in part because of better surveillance, Douglas K. Owens, MD, of Stanford (Calif.) University, and colleagues wrote in the recommendation statement published in JAMA.
The recommendation applies to all asymptomatic adults aged 18-79 years without known liver disease, and expands on the 2013 recommendation to screen adults born between 1945 and 1965. The grade B designation means that the task force concluded with moderate certainty that HCV screening for adults aged 18-79 years had “substantial net benefit.”
The recommendations are based on an evidence report including 8 randomized, controlled trials, 48 other treatment studies, and 33 cohort studies published through February 2019 for a total of 179,230 individuals.
The screening is a one-time procedure for most adults, according to the task force, but clinicians should periodically screen individuals at increased risk, such as those with a past or current history of injection drug use. In addition, clinicians should consider screening individuals at increased risk who are above or below the recommended age range.
Although the task force identified no direct evidence on the benefit of screening for HCV infection in asymptomatic adults, a notable finding was that the newer direct-acting antiviral (DAA) regimens are sufficiently effective to support the expanded screening recommendation, they said. However, clinicians should inform patients that screening is voluntary and conducted only with the patient’s knowledge. Clinicians should educate patients about hepatitis C and give them an opportunity to ask questions and to make a decision about screening, according to the task force.
In the evidence report, a total of 49 studies including 10,181 individuals showed DAA treatment associated with pooled sustained virologic response rates greater than 95% across all virus genotypes, and a short-term serious adverse event rate of 1.9%. In addition, sustained virologic response following an antiviral therapy was associated with a reduction in risk of all-cause mortality (pooled hazard ratio 0.40) and of hepatocellular carcinoma (pooled HR 0.29) compared with cases of no sustained virologic response.
The evidence report findings were limited by several factors, including the relatively small number of randomized trials involving current DAA treatments, limited data on baseline symptoms, limited data on adolescents, and limited evidence on potential long-term harms of DAA therapy, noted Richard Chou, MD, of Oregon Health & Science University, Portland, and colleagues. However, new pooled evidence “indicates that SVR rates with currently recommended all-oral DAA regimens are substantially higher (more than 95%) than with interferon-based therapies evaluated in the prior review (68%-78%),” they said.
Several editorials were published concurrently with the recommendation.
In an editorial published in JAMA, Camilla S. Graham, MD, of Harvard Medical School, Boston, and Stacey Trooskin, MD, of the University of Pennsylvania, Philadelphia, wrote that the new recommendation reflects changes in hepatitis C virus management.
“With the approvals of sofosbuvir and simeprevir in 2013, patients with hepatitis C, a chronic viral illness associated with the deaths of more U.S. patients than the next 60 reportable infectious diseases combined, including HIV and tuberculosis, could expect a greater than 90% rate of achieving sustained virologic response (SVR, defined as undetectable HCV levels 12 weeks or longer after treatment completion, which is consistent with virologic cure of HCV infection) following 12 weeks of treatment,” they said.
These medications are effective but expensive; however, the combination of the availability of generic medications and the ongoing opioid epidemic in the United States are important contributors to the expanded recommendations, which “are welcome,” and may help meeting WHO 2030 targets for reducing new HCV infections, they said.
Dr. Graham disclosed personal fees from UpToDate. Dr. Trooskin disclosed grants from Gilead Sciences and personal fees from Merck, AbbVie, and Gilead Sciences.
In an editorial published in JAMA Internal Medicine, Jennifer C. Price, MD, and Danielle Brandman, MD, both of the University of California, San Francisco, wrote that “the advancements in HCV diagnosis and treatment have been extraordinary,” but that the new recommendation does not go far enough. “Implementation of HCV screening and linkage to treatment requires large-scale coordinated efforts, innovation, and resources. For example, point-of-care HCV RNA testing would enable scale-up of HCV screening and confirmatory testing among individuals at greatest risk of HCV infection,” they said. “Additionally, barriers remain between diagnosis and treatment, such as access to a health care provider who can treat HCV and authorization to receive affordable DAAs,” they noted. “Although the USPSTF HCV screening recommendation is a step forward for controlling HCV infection in the U.S., it will take a coordinated and funded effort to ensure that the anticipated benefits are realized,” they concluded.
Dr. Price disclosed research funding from Gilead Sciences and Merck. Dr. Brandman disclosed research funding from Gilead Sciences, Pfizer, Conatus, Allergan, and Grifols, as well as personal fees from Alnylam.
In an editorial published in JAMA Network Open, Eli S. Rosenberg, PhD, of the University at Albany (N.Y.) School of Public Health, and Joshua A. Barocas, MD, of Boston University, emphasized the need to change the stigma surrounding HCV infection in the United States.
“Given the changing epidemiology of HCV infection, new public health priorities, advancements in treatment, and unmet diagnostic needs, it is wise to periodically reevaluate screening recommendations to ensure that they are maximally addressing these areas and patients’ individual needs,” they said. “The Affordable Care Act requires private insurers and Medicaid to cover preventive services recommended by the USPSTF with a grade of A or B with no cost sharing (i.e., no deductible or copayment),” they noted. Although the new recommendation for one-time screening will likely identify more cases, improve outcomes, and reduce deaths, the editorialists cautioned that “one-time screening should not be interpreted like catch-up vaccinations, whereby we immunize someone at any age for hepatitis B virus, for example, and they are then immunized for the remainder of their life,” and that reassessments are needed, especially for younger adults.
In addition, they emphasized the need to reduce the stigma surrounding HCV and allow for recommendations based on risk, rather than age. “We have forced the USPSTF to adopt age-based screening recommendations because we, as a society, have created a culture in which we have stigmatized these behaviors and we, as practitioners, have proven to be inadequate at eliciting HCV risk behaviors,” they said. “Our responsibility as a society and practice community is to address structural and individual factors that limit our ability to most precisely address the needs of our patients and truly move toward HCV elimination,” they concluded.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The task force researchers had no financial conflicts to disclose.
SOURCES: Owens DK et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2020.1123; Chou R et al. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.20788; Graham CS, Trooskin S. JAMA. 2020 Mar 2. doi: 10.1001/jama.2019.22313; Price JC and Brandman D. JAMA Intern Med. 2020 Mar 2. doi: 10.1001/jamainternmed.2019.7334; Rosenberg ES, Barocas JA. JAMA Network Open. 2020 Mar 2. doi: 10.1001/jamanetworkopen.2020.0538.
FROM JAMA
Expert: Eliminating HCV ‘sounds ambitious, but I think it’s possible’
LAS VEGAS – Between 2010 and 2017, the proportion of newly diagnosed cases of acute hepatitis C virus infection rose threefold, driven largely by the concomitant opioid epidemic.
That makes efforts to screen, diagnose, and cure high-risk populations more important than ever, Stevan A. Gonzalez, MD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
About 70% of HCV cases are related to injection drug use,” said Dr. Gonzalez, medical director of liver transplantation at the Baylor Simmons Transplant Institute at the Baylor Scott & White All Saints Medical Center in Fort Worth, Tex. “This is affecting whites as much as blacks and Hispanics, females as much as males, and in nonurban areas as much as in urban areas.”
Data from the Centers for Disease Control and Prevention and the Substance Abuse and Mental Health Services Administration indicate that during 2004-2014, the number of acute HCV cases among those aged 18-29 years increased 400%, and the use of injection opioids rose 600%.
At the same time, the number of HCV cases among those aged 30-39 years increased 325%, and the use of injection opioids rose 83%.
“We’re starting to see a pattern overlapping between HCV exposure and opioid injection,” Dr. Gonzalez said. Other high-risk populations include homeless and incarcerated individuals.
More than 70 million people worldwide have chronic HCV infection, Dr. Gonzalez noted, with possibly as many as 5 million cases in the United States. It remains the nation’s most common blood-borne infection.
Chronic disease develops in up to 85% of people who are exposed, infection is asymptomatic, and HCV remains one of the leading indications for liver transplantation and causes of liver cancer.
From a geographic standpoint, the prevalence of HCV in young adults is eclipsing that of Baby Boomers in several states in the Appalachian region and in Northeast, which have long been trouble spots for opioid use disorder (Gastroenterol. 2018 May;154[6]:1850-1).
Surprising exposure risk
The primary risk of transmission is through contaminated blood and the exposure through needles.
“It really doesn’t matter whether it’s a needle that has a small amount of dead space where a little bit of blood can remain or needles that have a larger amount of blood,” Dr. Gonzalez said.
“I’ve had patients who come to me and say, ‘I can’t believe I have HCV. It’s impossible. I always use my own needles. They’re always brand new; I’ve never shared with anybody,’” he continued.
“This is where education and awareness is so critical, because it’s not just the needles,” Dr. Gonzalez explained. “HCV can survive on inanimate objects. For example, on a tabletop surface or a water container, HCV can remain viable up to 3 weeks. In a syringe, 2 months. For that reason, HCV can also be transmitted through crack pipes and nasal drug use, where the prevalence can be up to 35%.”
The duration of a person’s HCV infection drives the transmission.
“That’s important to think about, because people who have chronic hepatitis C are infectious until they’re treated,” Dr. Gonzalez said. “If they don’t know that they have hepatitis C, they continue to transmit the virus to others.”
One study found that half of people living with HCV are unaware of their infection (PLoS One. 2014 Jul 2;9[7]:e101554). According to Dr. Gonzalez, forthcoming guidelines from the U.S. Preventive Services Task Force are expected to recommend a one-time screening for HCV infection in all adults aged 18-79 years, a Grade B recommendation. “That’s a big deal,” he said. (The draft recommendations are available here.)
HCV infection disproportionately affects individuals in correctional institutions. In fact, an estimated one in three inmates in the United States has chronic HCV.
“This is sort of a forgotten population with a lot of substance use and mental illness,” Dr. Gonzalez said. “Injection drug use in that setting is the most common risk factor: It’s about 60% in terms of the risk of transmission within correctional settings. HCV-associated liver disease has now surpassed HIV as a cause of death within correctional settings.”
Weighing treatment options
The most common oral regimens for chronic HCV include sofosbuvir/ledipasvir, sofosbuvir/velpatasvir, and glecaprevir/pibrentasvir. They achieve cure in 93%-100% of cases.
“HCV can be cured; it can be eradicated from the body long term,” Dr. Gonzalez said. “The choice of regimen, treatment duration, and use of ribavirin depends on the presence/absence of cirrhosis, prior treatment experience, and the genotype.”
All six forms of the HCV genotype can be treated with oral medication, he added, and methadone, bupropion, and naloxone are safe to use during therapy.
Reinfection following HCV treatment occurs infrequently. Dr. Gonzalez cited a randomized, controlled trial presented as an abstract at the 2018 annual meeting of the American Association for the Study of Liver Diseases. That study’s researchers found that – among 199 patients on opioid-replacement therapy who were receiving direct-acting antiviral therapy, in whom greater than 50% were actively using drugs – the rate of reinfection at 3 years was 1.8 reinfections/100 person-years.
“That’s lower than people expect,” Dr. Gonzalez said.
How to boost screening
Electronic health record systems can be used as an important tool to increase HCV screening in health care settings.
In 2017, researchers published an analysis of three randomized trials carried out at three separate primary care settings to improve screening for HCV: repeated mailings, an EHR best practice alert (BPA), and patient solicitation (Hepatology 2017 Jan;65[1]:44-53). They evaluated HCV antibody testing, diagnosis, and costs for each of the interventions, compared with standard-of-care testing.
The investigators found that the BPA intervention had the lowest incremental cost per completed test – $24 with fixed start-up costs, including technical design and development of the BPA system; $3 without fixed start-up costs. The BPA intervention also had the lowest incremental cost per new case identified.
Other efforts to expand access to screening and treatment are underway.
In 2019, Louisiana health officials negotiated a one-time fee for unlimited access for 5 years to sofosbuvir/velpatasvir (Epclusa) to treat the estimated 30,000 patients on Louisiana Medicaid and in that state’s department of corrections who have HCV.
“The goal is 90% cure; the burden is on the state health department to screen, diagnose, and dispense medication,” Dr. Gonzalez said.
Also in 2019, the state of Washington used an open bidding process to negotiate access to glecaprevir/pibrentasvir (Mavyret) for the state’s Medicaid population who have HCV.
“Those states are setting the pace,” Dr. Gonzalez said. “They are showing examples of how we can start implementing a process to treat these vulnerable populations.”
Meanwhile, the World Health Organization set a goal of eliminating viral hepatitis as a major public health threat by 2030.
“That sounds ambitious, but I think it’s possible,” Dr. Gonzalez said. “It’s important to address these high-risk populations: the incarcerated, people who use drugs, and the homeless, because those are the groups that have a high prevalence of HCV – mainly through injection drug use.
“If we don’t address that population, and we only target the general population, we’re going to have a continual source of transmission,” Dr. Gonzalez warned. “In that case, we would never be able to achieve elimination.”
Dr. Gonzalez disclosed that he is a member of the speakers bureau for AbbVie and Salix.
LAS VEGAS – Between 2010 and 2017, the proportion of newly diagnosed cases of acute hepatitis C virus infection rose threefold, driven largely by the concomitant opioid epidemic.
That makes efforts to screen, diagnose, and cure high-risk populations more important than ever, Stevan A. Gonzalez, MD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
About 70% of HCV cases are related to injection drug use,” said Dr. Gonzalez, medical director of liver transplantation at the Baylor Simmons Transplant Institute at the Baylor Scott & White All Saints Medical Center in Fort Worth, Tex. “This is affecting whites as much as blacks and Hispanics, females as much as males, and in nonurban areas as much as in urban areas.”
Data from the Centers for Disease Control and Prevention and the Substance Abuse and Mental Health Services Administration indicate that during 2004-2014, the number of acute HCV cases among those aged 18-29 years increased 400%, and the use of injection opioids rose 600%.
At the same time, the number of HCV cases among those aged 30-39 years increased 325%, and the use of injection opioids rose 83%.
“We’re starting to see a pattern overlapping between HCV exposure and opioid injection,” Dr. Gonzalez said. Other high-risk populations include homeless and incarcerated individuals.
More than 70 million people worldwide have chronic HCV infection, Dr. Gonzalez noted, with possibly as many as 5 million cases in the United States. It remains the nation’s most common blood-borne infection.
Chronic disease develops in up to 85% of people who are exposed, infection is asymptomatic, and HCV remains one of the leading indications for liver transplantation and causes of liver cancer.
From a geographic standpoint, the prevalence of HCV in young adults is eclipsing that of Baby Boomers in several states in the Appalachian region and in Northeast, which have long been trouble spots for opioid use disorder (Gastroenterol. 2018 May;154[6]:1850-1).
Surprising exposure risk
The primary risk of transmission is through contaminated blood and the exposure through needles.
“It really doesn’t matter whether it’s a needle that has a small amount of dead space where a little bit of blood can remain or needles that have a larger amount of blood,” Dr. Gonzalez said.
“I’ve had patients who come to me and say, ‘I can’t believe I have HCV. It’s impossible. I always use my own needles. They’re always brand new; I’ve never shared with anybody,’” he continued.
“This is where education and awareness is so critical, because it’s not just the needles,” Dr. Gonzalez explained. “HCV can survive on inanimate objects. For example, on a tabletop surface or a water container, HCV can remain viable up to 3 weeks. In a syringe, 2 months. For that reason, HCV can also be transmitted through crack pipes and nasal drug use, where the prevalence can be up to 35%.”
The duration of a person’s HCV infection drives the transmission.
“That’s important to think about, because people who have chronic hepatitis C are infectious until they’re treated,” Dr. Gonzalez said. “If they don’t know that they have hepatitis C, they continue to transmit the virus to others.”
One study found that half of people living with HCV are unaware of their infection (PLoS One. 2014 Jul 2;9[7]:e101554). According to Dr. Gonzalez, forthcoming guidelines from the U.S. Preventive Services Task Force are expected to recommend a one-time screening for HCV infection in all adults aged 18-79 years, a Grade B recommendation. “That’s a big deal,” he said. (The draft recommendations are available here.)
HCV infection disproportionately affects individuals in correctional institutions. In fact, an estimated one in three inmates in the United States has chronic HCV.
“This is sort of a forgotten population with a lot of substance use and mental illness,” Dr. Gonzalez said. “Injection drug use in that setting is the most common risk factor: It’s about 60% in terms of the risk of transmission within correctional settings. HCV-associated liver disease has now surpassed HIV as a cause of death within correctional settings.”
Weighing treatment options
The most common oral regimens for chronic HCV include sofosbuvir/ledipasvir, sofosbuvir/velpatasvir, and glecaprevir/pibrentasvir. They achieve cure in 93%-100% of cases.
“HCV can be cured; it can be eradicated from the body long term,” Dr. Gonzalez said. “The choice of regimen, treatment duration, and use of ribavirin depends on the presence/absence of cirrhosis, prior treatment experience, and the genotype.”
All six forms of the HCV genotype can be treated with oral medication, he added, and methadone, bupropion, and naloxone are safe to use during therapy.
Reinfection following HCV treatment occurs infrequently. Dr. Gonzalez cited a randomized, controlled trial presented as an abstract at the 2018 annual meeting of the American Association for the Study of Liver Diseases. That study’s researchers found that – among 199 patients on opioid-replacement therapy who were receiving direct-acting antiviral therapy, in whom greater than 50% were actively using drugs – the rate of reinfection at 3 years was 1.8 reinfections/100 person-years.
“That’s lower than people expect,” Dr. Gonzalez said.
How to boost screening
Electronic health record systems can be used as an important tool to increase HCV screening in health care settings.
In 2017, researchers published an analysis of three randomized trials carried out at three separate primary care settings to improve screening for HCV: repeated mailings, an EHR best practice alert (BPA), and patient solicitation (Hepatology 2017 Jan;65[1]:44-53). They evaluated HCV antibody testing, diagnosis, and costs for each of the interventions, compared with standard-of-care testing.
The investigators found that the BPA intervention had the lowest incremental cost per completed test – $24 with fixed start-up costs, including technical design and development of the BPA system; $3 without fixed start-up costs. The BPA intervention also had the lowest incremental cost per new case identified.
Other efforts to expand access to screening and treatment are underway.
In 2019, Louisiana health officials negotiated a one-time fee for unlimited access for 5 years to sofosbuvir/velpatasvir (Epclusa) to treat the estimated 30,000 patients on Louisiana Medicaid and in that state’s department of corrections who have HCV.
“The goal is 90% cure; the burden is on the state health department to screen, diagnose, and dispense medication,” Dr. Gonzalez said.
Also in 2019, the state of Washington used an open bidding process to negotiate access to glecaprevir/pibrentasvir (Mavyret) for the state’s Medicaid population who have HCV.
“Those states are setting the pace,” Dr. Gonzalez said. “They are showing examples of how we can start implementing a process to treat these vulnerable populations.”
Meanwhile, the World Health Organization set a goal of eliminating viral hepatitis as a major public health threat by 2030.
“That sounds ambitious, but I think it’s possible,” Dr. Gonzalez said. “It’s important to address these high-risk populations: the incarcerated, people who use drugs, and the homeless, because those are the groups that have a high prevalence of HCV – mainly through injection drug use.
“If we don’t address that population, and we only target the general population, we’re going to have a continual source of transmission,” Dr. Gonzalez warned. “In that case, we would never be able to achieve elimination.”
Dr. Gonzalez disclosed that he is a member of the speakers bureau for AbbVie and Salix.
LAS VEGAS – Between 2010 and 2017, the proportion of newly diagnosed cases of acute hepatitis C virus infection rose threefold, driven largely by the concomitant opioid epidemic.
That makes efforts to screen, diagnose, and cure high-risk populations more important than ever, Stevan A. Gonzalez, MD, said at an annual psychopharmacology update held by the Nevada Psychiatric Association.
About 70% of HCV cases are related to injection drug use,” said Dr. Gonzalez, medical director of liver transplantation at the Baylor Simmons Transplant Institute at the Baylor Scott & White All Saints Medical Center in Fort Worth, Tex. “This is affecting whites as much as blacks and Hispanics, females as much as males, and in nonurban areas as much as in urban areas.”
Data from the Centers for Disease Control and Prevention and the Substance Abuse and Mental Health Services Administration indicate that during 2004-2014, the number of acute HCV cases among those aged 18-29 years increased 400%, and the use of injection opioids rose 600%.
At the same time, the number of HCV cases among those aged 30-39 years increased 325%, and the use of injection opioids rose 83%.
“We’re starting to see a pattern overlapping between HCV exposure and opioid injection,” Dr. Gonzalez said. Other high-risk populations include homeless and incarcerated individuals.
More than 70 million people worldwide have chronic HCV infection, Dr. Gonzalez noted, with possibly as many as 5 million cases in the United States. It remains the nation’s most common blood-borne infection.
Chronic disease develops in up to 85% of people who are exposed, infection is asymptomatic, and HCV remains one of the leading indications for liver transplantation and causes of liver cancer.
From a geographic standpoint, the prevalence of HCV in young adults is eclipsing that of Baby Boomers in several states in the Appalachian region and in Northeast, which have long been trouble spots for opioid use disorder (Gastroenterol. 2018 May;154[6]:1850-1).
Surprising exposure risk
The primary risk of transmission is through contaminated blood and the exposure through needles.
“It really doesn’t matter whether it’s a needle that has a small amount of dead space where a little bit of blood can remain or needles that have a larger amount of blood,” Dr. Gonzalez said.
“I’ve had patients who come to me and say, ‘I can’t believe I have HCV. It’s impossible. I always use my own needles. They’re always brand new; I’ve never shared with anybody,’” he continued.
“This is where education and awareness is so critical, because it’s not just the needles,” Dr. Gonzalez explained. “HCV can survive on inanimate objects. For example, on a tabletop surface or a water container, HCV can remain viable up to 3 weeks. In a syringe, 2 months. For that reason, HCV can also be transmitted through crack pipes and nasal drug use, where the prevalence can be up to 35%.”
The duration of a person’s HCV infection drives the transmission.
“That’s important to think about, because people who have chronic hepatitis C are infectious until they’re treated,” Dr. Gonzalez said. “If they don’t know that they have hepatitis C, they continue to transmit the virus to others.”
One study found that half of people living with HCV are unaware of their infection (PLoS One. 2014 Jul 2;9[7]:e101554). According to Dr. Gonzalez, forthcoming guidelines from the U.S. Preventive Services Task Force are expected to recommend a one-time screening for HCV infection in all adults aged 18-79 years, a Grade B recommendation. “That’s a big deal,” he said. (The draft recommendations are available here.)
HCV infection disproportionately affects individuals in correctional institutions. In fact, an estimated one in three inmates in the United States has chronic HCV.
“This is sort of a forgotten population with a lot of substance use and mental illness,” Dr. Gonzalez said. “Injection drug use in that setting is the most common risk factor: It’s about 60% in terms of the risk of transmission within correctional settings. HCV-associated liver disease has now surpassed HIV as a cause of death within correctional settings.”
Weighing treatment options
The most common oral regimens for chronic HCV include sofosbuvir/ledipasvir, sofosbuvir/velpatasvir, and glecaprevir/pibrentasvir. They achieve cure in 93%-100% of cases.
“HCV can be cured; it can be eradicated from the body long term,” Dr. Gonzalez said. “The choice of regimen, treatment duration, and use of ribavirin depends on the presence/absence of cirrhosis, prior treatment experience, and the genotype.”
All six forms of the HCV genotype can be treated with oral medication, he added, and methadone, bupropion, and naloxone are safe to use during therapy.
Reinfection following HCV treatment occurs infrequently. Dr. Gonzalez cited a randomized, controlled trial presented as an abstract at the 2018 annual meeting of the American Association for the Study of Liver Diseases. That study’s researchers found that – among 199 patients on opioid-replacement therapy who were receiving direct-acting antiviral therapy, in whom greater than 50% were actively using drugs – the rate of reinfection at 3 years was 1.8 reinfections/100 person-years.
“That’s lower than people expect,” Dr. Gonzalez said.
How to boost screening
Electronic health record systems can be used as an important tool to increase HCV screening in health care settings.
In 2017, researchers published an analysis of three randomized trials carried out at three separate primary care settings to improve screening for HCV: repeated mailings, an EHR best practice alert (BPA), and patient solicitation (Hepatology 2017 Jan;65[1]:44-53). They evaluated HCV antibody testing, diagnosis, and costs for each of the interventions, compared with standard-of-care testing.
The investigators found that the BPA intervention had the lowest incremental cost per completed test – $24 with fixed start-up costs, including technical design and development of the BPA system; $3 without fixed start-up costs. The BPA intervention also had the lowest incremental cost per new case identified.
Other efforts to expand access to screening and treatment are underway.
In 2019, Louisiana health officials negotiated a one-time fee for unlimited access for 5 years to sofosbuvir/velpatasvir (Epclusa) to treat the estimated 30,000 patients on Louisiana Medicaid and in that state’s department of corrections who have HCV.
“The goal is 90% cure; the burden is on the state health department to screen, diagnose, and dispense medication,” Dr. Gonzalez said.
Also in 2019, the state of Washington used an open bidding process to negotiate access to glecaprevir/pibrentasvir (Mavyret) for the state’s Medicaid population who have HCV.
“Those states are setting the pace,” Dr. Gonzalez said. “They are showing examples of how we can start implementing a process to treat these vulnerable populations.”
Meanwhile, the World Health Organization set a goal of eliminating viral hepatitis as a major public health threat by 2030.
“That sounds ambitious, but I think it’s possible,” Dr. Gonzalez said. “It’s important to address these high-risk populations: the incarcerated, people who use drugs, and the homeless, because those are the groups that have a high prevalence of HCV – mainly through injection drug use.
“If we don’t address that population, and we only target the general population, we’re going to have a continual source of transmission,” Dr. Gonzalez warned. “In that case, we would never be able to achieve elimination.”
Dr. Gonzalez disclosed that he is a member of the speakers bureau for AbbVie and Salix.
REPORTING FROM NPA 2020
Antibiotic resistance rises among pneumococcus strains in kids
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Dr. Kaur and colleagues report their analysis of pneumococcal resistance among nasopharyngeal and middle ear isolates (90% nasopharyngeal and 10% middle ear) collected between 2008 and 2016. They demonstrate the dominant role that nonvaccine serotypes play in carriage and acute otitis media (AOM) in children, and by extension potentially the entire spectrum of pneumococcal disease in the 13-valent pneumococcal conjugate vaccine (PCV13) era. Nonsusceptibility to beta-lactams was reported for one-third of isolates with the increase in the most recent reported years (2013-2016).
What are the implications for treatment of pneumococcal infections? For AOM, amoxicillin minimum inhibitory concentrations (MIC) were all less than 4 mcg/mL, which is the pharmacodynamic breakpoint for high-dose (90 mg/kg per day) AOM regimens; these data support continued use of high-dose amoxicillin for children with AOM that requires antimicrobial treatment. Resistance to macrolides (erythromycin and likely azithromycin) occurred in approximately one-third of isolates; however, in contrast to beta-lactams (amoxicillin), higher macrolide doses do not overcome resistance. Thus macrolide use for AOM appears limited to those with beta-lactam allergy and no better alternative drug, i.e., expect failure in one-third of AOM patients if macrolides are used. For ceftriaxone, no 2013-2016 isolate had a MIC over 0.5 mcg/mL, implying that ceftriaxone remains appropriate first-line therapy for serious pneumococcal disease and effective for pneumococcal AOM when oral drugs have failed or are not an option because of repeated emesis. Interestingly, trimethoprim/sulfamethoxazole (T/S) had lower resistance rates against the nonvaccine “bad boy” serogroup 35 (8%-15%), compared with cephalosporins (32%-57%). Perhaps we are back to the future and T/S will again have a role against pneumococcal AOM. Of note, no isolate was resistant to levofloxacin or linezolid. Linezolid or macrolide use alone must be considered with the caveat that nontypeable Haemophilus influenzae now likely surpasses pneumococcus as an AOM pathogen, and neither drug class is active against nontypeable H. influenzae.
What are the implications for prevention? This is one of many studies in the post-PCV era reporting serotype replacement with nonvaccine serotypes. But most prior studies reported reduced overall disease burden; in other words, the absolute number of pneumococcal infections was reduced, but residual AOM nonvaccine types dominated as the etiology. The current study, however, suggests that the overall number of AOM episodes may not be less because increases in AOM caused by nonvaccine serotypes may be offsetting declines in AOM caused by vaccine serotypes. This concept contrasts to multiple large epidemiologic studies demonstrating a decline in overall incidence of AOM office visits/episodes and several Israeli studies reporting a decline in pneumococcal AOM in children who warrant tympanocentesis. These new data are food for thought, but antibiotic resistance can vary regionally, so confirmation based on data from other regions seems warranted.
Next-generation vaccines will need to consider which serotypes are prevalent in pneumococcal disease, including AOM, as we continue into the PCV13 era. However, serotypes causing invasive pneumococcal disease and pneumonia would be higher priorities than AOM. Indeed, several candidate PCV vaccines are currently in clinical trials adding up to seven serotypes, including most of the newly emerging invasive disease serotypes. One downside to the newer PCVs is lack of serogroup 35, a prominent culprit in AOM resistance in the current report.
Stephen I. Pelton, MD, is professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. Christopher J. Harrison, MD, is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital–Kansas City, Mo. Dr. Pelton has received honorarium from Merck Vaccines, Pfizer, and Sanofi for participation in advisory board meeting on pneumococcal vaccine and/or membership on the Data and Safety Monitoring Board. Boston Medical Center has received investigator-initiated research grants from Merck Vaccines and Pfizer.
Children’s Mercy Hospital – Kansas City Boston Medical Center has received funding from GlaxoSmithKline, Merck, and Pfizer for research vaccine studies, and from Pfizer and Merck for investigator-initiated research grants for in vitro pneumococcal investigations on which Dr. Harrison is an investigator.
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
Antibiotic resistance in strains of Streptococcus pneumoniae has been rising since 2013 because of changing susceptibility profiles, based on data from 1,201 isolates collected from 448 children in primary care settings.
“New strains expressing capsular serotypes not included in the 13-valent pneumococcal conjugate vaccine are emerging to cause disease, and strains that acquire antibiotic resistance are increasing in frequency due to their survival of the fittest advantage,” wrote Ravinder Kaur, PhD, of Rochester (N.Y.) General Hospital Research Institute, and colleagues.
Similar Darwinian principles occurred after the introduction of PCV-7, the study authors added.
In a prospective cohort study published in Clinical Infectious Diseases, the researchers reviewed 1,201 isolates collected from the nasopharynx during healthy periods, and from the nasopharynx and middle ear fluid (MEF) during episodes of acute otitis media, in children aged 6-36 months who were seen in primary care settings.
The isolates were collected during 2006-2016 to reflect the pre- and post-PCV13 era. Children received PCV-7 from 2006 until April 2010, and received PCV-13 after April 2010.
Overall, the number of acute otitis media (AOM) cases caused by S. pneumoniae was not significantly different between the PCV-7 and PCV-13 eras, nor was the frequency of pneumococci identified in the nasopharynx during healthy visits and visits at the start of an AOM infection.
The researchers examined susceptibility using minimum inhibitory concentrations (MIC). During healthy visits, the MIC50 of isolated pneumococci was low (no greater than 0.06 mcg/mL) for all four beta-lactam drugs tested. And it didn’t change significantly over the study years.
In contrast, among the nasopharyngeal and MEF isolates during AOM, the MIC50 to penicillin, amoxicillin, ceftriaxone, and meropenem during 2013-2016 rose significantly, the investigators said.
A change in antibiotic susceptibility within a subtype also contributed to the development of PCV-13 resistance.
The study authors identified three serotypes that affected the changes in susceptibility in their study population. Serotypes 35B and 35F increased their beta-lactam resistance during 2013-2016, and serotype 11A had a higher MIC to quinolones and became more prevalent during 2013-2016. Those three serotypes accounted for most of the change in antibiotic susceptibility, the researchers said.
In addition, “the frequency of strains resistant to penicillin and amoxicillin decreased with the introduction of PCV-13, but rebounded to levels similar to those before PCV-13 introduction by 2015-2016,” the investigators noted.
The study findings were limited by several factors, including the homogeneous study population and potential lack of generalizability to other settings. In addition, the researchers did not study antibiotic consumption or antibiotic treatment failure, and they could not account for potential AOM cases that may have been treated in settings other than primary care.
However, the investigators said the results support the need for additional studies and attention to the development of the next generation of PCVs, the PCV-15 and PCV-20. Both include serotypes 22F and 33F, but neither includes 35B or 35F. The PCV-20 also includes 11A and 15B.
The study was supported in part by the National Institutes of Health and Sanofi Pasteur. Some isolates collected during the 2010-2013 time period were part of a study supported by Pfizer. The researchers had no relevant financial conflicts to disclose.
SOURCE: Kaur R et al. Clin Inf Dis. 2020 Feb 18. doi: 10.1093/cid/ciaa157.
FROM CLINICAL INFECTIOUS DISEASES
U.S. reports first death from COVID-19, possible outbreak at long-term care facility
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
CDC revises COVID-19 test kits, broadens ‘person under investigation’ definition
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
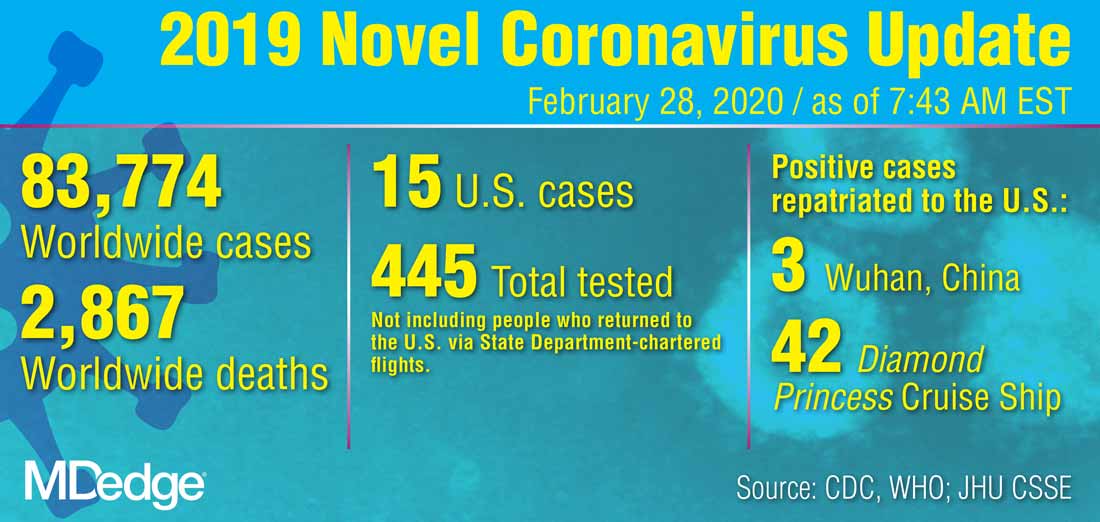
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
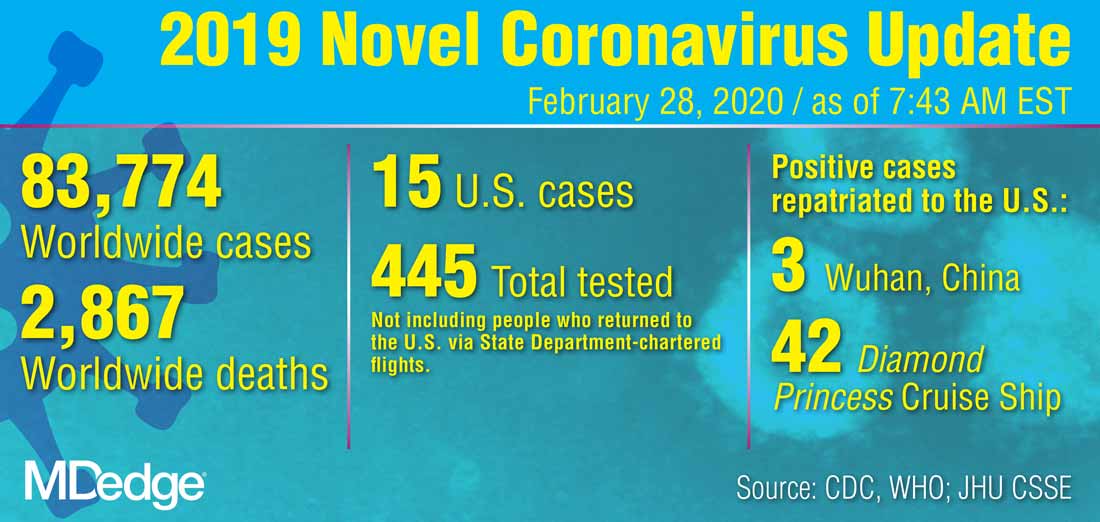
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
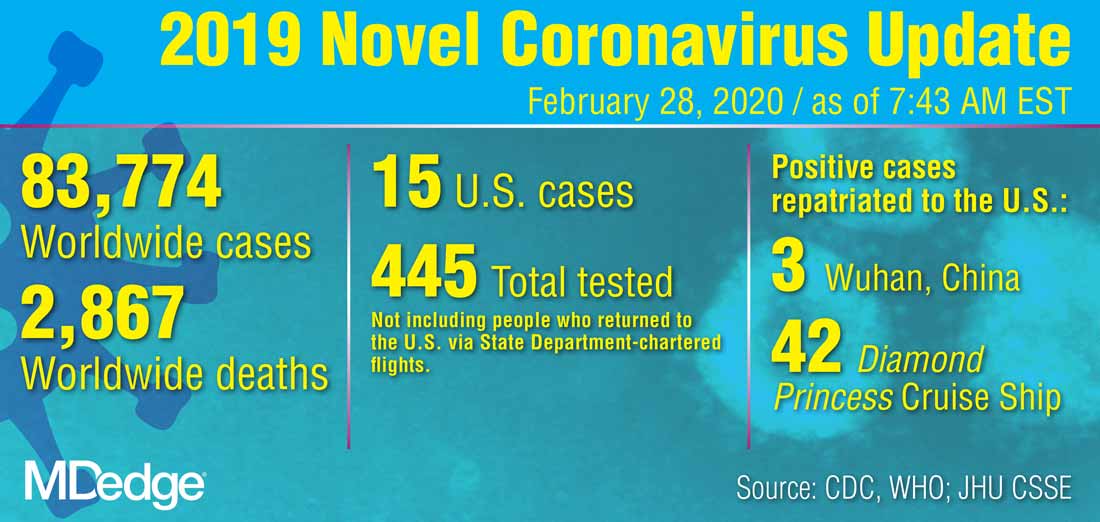
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
REPORTING FROM A CDC BRIEFING
Children bearing the brunt of declining flu activity
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”
National flu activity decreased for the second consecutive week, but pediatric mortality is heading in the opposite direction, according to the Centers for Disease Control and Prevention.
Influenza-like illness (ILI) represented 5.5% of all visits to outpatient health care providers during the week ending Feb. 22, compared with 6.1% the previous week, the CDC’s influenza division reported Feb. 28. The ILI visit rate had reached 6.6% in early February after dropping to 5.0% in mid-January, following a rise to a season-high 7.1% in the last week of December.
Another measure of ILI activity, the percentage of laboratory specimens testing positive, also declined for the second week in a row. The rate was 26.4% for the week ending Feb. 22, which is down from the season high of 30.3% reached 2 weeks before, the influenza division said.
ILI-related deaths among children, however, are not dropping. The total for 2019-2020 is now up to 125, and that “number is higher for the same time period than in every season since reporting began in 2004-05, except for the 2009 pandemic,” the CDC noted.
Hospitalization rates, which have been fairly typical in the general population, also are elevated for young adults and school-aged children, the agency said, and “rates among children 0-4 years old are now the highest CDC has on record at this point in the season, surpassing rates reported during the second wave of the 2009 H1N1 pandemic.”