User login
Runaway youth: Knowing the risk factors and care needs
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
As many as 1 in 20 youth run away from home each year, and you can play a critical role in identifying adolescents at high risk through confidential social histories and discussions, according to a clinical report from the American Academy of Pediatrics.
The academy’s data-rich report, “Runaway Youth: Caring for the Nation’s Largest Segment of Missing Children,” details how unaccompanied youth who run away – either on their own or who are asked to leave home – have high rates of trauma and neglect, mental illness, substance abuse, family dysfunction, and disengagement from school.
Children who identify as lesbian, gay, bisexual, transgender, and questioning or queer (LGBTQ) and youth in protective custody also are at high risk of running away and of becoming homeless – and once away from home, they and other runaways are at high risk for additional trauma, victimization, and violence, including sexual exploitation, according to the report published in Pediatrics.
“There clearly are certain populations at higher risk, and we really need to be aware of and in tune with these risks, and ask about the home and the household in order to try to decrease the risk of these kids getting into dangerous situations,” Thresia B. Gambon, MD, said in an interview. She is coauthor of the report and a pediatrician with the Citrus Health Network in Miami.
Among the AAP’s recommendations for practice is the guidance to conduct a thorough and confidential psychosocial assessment such as the HEEADSSS assessment (home environment, education and employment, eating peer-related activities, drugs, sexuality, suicide/depression, and safety) and to use a validated depression screening tool for adolescents, such as the Patient Health Questionnaire for Adolescents (PHQ-A) and the primary care version of the Beck Depression Inventory (BDI).
Broadly speaking, which involves being aware of trauma and adverse childhood experiences that can affect health,” according to the report. The AAP Trauma Toolbox for Primary Care is mentioned as a resource.
Most surprising to Dr. Gambon in the research and report-writing process were data showing that disengagement from school is a significant risk factor. “This stood out to me,” she said. “If there are school problems [of various types], kids might run away to avoid attending school.”
Tasked with updating the AAP’s 2004 clinical report, “The Pediatrician’s Role in the Prevention of Missing Children,” Dr. Gambon and coauthor, Janna R. Gewirtz O’Brien, MD, decided to look more closely at runaway youth after studying the numbers – some studies estimate that between 5% and 8% of adolescents run away every year. They saw that, “in general, the number of kids who just go missing has actually decreased [with the help of] cell phones,” Dr. Gambon said in an interview.
“The numbers of kids who are actually running away are high,” she said, “and probably we’re underidentifying these in our primary care clinics.”
Because a significant number of runaway youth become homeless, data on the homeless offers a valuable window not only into the health risks of homelessness for teens (substance abuse, pregnancy, STDs,) but also into risk factors for leaving home in the first place, she noted. Research shows, for instance, that about 20%-40% of teenagers who are homeless identify as LGBTQ, compared with 4%-10% of their nonhomeless peers.
When an adolescent at high risk for running away is identified, you should use practice- and community-based resources to address key issues, support psychological and behavioral health needs of the child and family, and ensure safety.
For youth who have run away, you can share information on local resources, as well as the national Runaway Safeline (1-800-RUNAWAY), which provides 24-hour referrals to community resources, including shelter, food banks, social services, and counseling. You also can ask adolescents whether they have sources of support and shelter (safe, supportive adults who might help in a crisis), and discuss safety plans for leaving home that include health care to mitigate risk, such as reliable contraception and access to mental health care.
“The goal with talking about a safety plan isn’t, of course, to encourage a child to run away, but if they feel as if they need to find somewhere else to live or stay, to discuss what resources are available to them to try to keep them as safe as possible when they’re out of their home,” Dr. Gambon said.
Dr. Gambon speaks partly from experience. She works routinely with youth who have run away from foster care homes, youth who have been trafficked, and other runaways. “I always try to talk with them about safety. I try not to put them down for their decisions but to work with them to make better decisions,” she said. “I work closely with a psychologist because a big part of this is getting them to have self-worth. They often feel as if no one cares, and some just want to be heard and to be able to talk about their situations.”
The AAP report notes that, of more than 70,000 contacts made to Runaway Safeline in 2017, 31% were about youth who were contemplating running away, 16% were about youth who had run away, 5% were about youth asked to leave home or prevented from returning, and 9% concerned youth experiencing homelessness. About three-quarters of the calls came from the youth themselves.
Dr. Gambon and Dr. Gewirtz O’Brien, of the department of pediatrics at the University of Minnesota in Minneapolis, worked with the AAP Committee on Psychosocial Aspects of Child and Family Health and the AAP Council on Community Pediatrics in producing the report. There was no external funding for this report and the authors said they had no conflicts of interest.
SOURCE: Gambon TB et al. Pediatrics. 2020 Jan 21. doi: 10.1542/peds.2019-3752.
FROM PEDIATRICS
Adolescent alcohol, opioid misuse linked to risky behaviors
Binge drinking and misuse of opioids led to risky behavior during adolescence, two studies from the journal Pediatrics highlighted. And the binge drinking in high school may predict risky driving behaviors up to 4 years after high school.
Federico E. Vaca, MD, of the developmental neurocognitive driving simulation research center at Yale University, New Haven, Conn., and colleagues examined the associations between risky driving behaviors and binge drinking of 2,785 adolescents in the nationally representative, longitudinal NEXT Generation Health Study. The researchers studied the effects of binge drinking on driving while impaired (DWI), riding with an impaired driver (RWI), blackouts, extreme binge drinking, and risky driving.
The adolescents were studied across seven waves, with Wave 1 beginning in the 2009-2010 school year (10th grade; mean age, 16 years), and data extended up to 4 years after high school. Of all adolescents enrolled, 91% completed Wave 1, 88% completed Wave 2, 86% completed Wave 3 (12th grade), 78% completed Wave 4, 79% completed Wave 5, 84% completed Wave 6, and 83% completed Wave 7 (4 years after leaving high school) of the study.
High school binge drinking predicts later risky behavior
About one-quarter of adolescents reported binge drinking in Waves 1-3, with an incidence of 27% in Wave 1, 24% in Wave 2, and 27% in Wave 3. Adolescents who reported binge drinking in Wave 3 had a higher likelihood of DWI in subsequent waves, with nearly six times higher odds in Wave 5 and more than twice as likely in Wave 7, researchers said. Binge drinking in Wave 3 also was associated with greater than four times higher odds of RWI in Wave 4, and more than two and a half times higher odds of RWI in Wave 7. Among adolescents who reported binge drinking across 3 years in high school, there was a higher likelihood of extreme binge drinking in Wave 7, and higher likelihood of risky driving after graduating.
Impact of parental knowledge of drinking
in some waves. Father monitoring knowledge of drinking in Waves 1-3 lowered the odds of DWI by 30% in Wave 5 and 20% in Wave 6, while also lowering the odds of RWI in Wave 4 and Wave 7 by 20%.
Mother knowledge of drinking in Waves 1-3 was associated with 60% lower odds of DWI in Wave 4, but did not lower odds in any wave for RWI.
Overall, parental support for not drinking lowered odds for DWI by 40% in Waves 4 and 5, and by 30% in Wave 7 while also lowering odds of RWI in Wave 4 by 20%.
The results are consistent with other studies examining risky driving behavior and binge drinking in adolescent populations, but researchers noted that “to an important but limited extent, parental practices while the teenager is in high school may protect against DWI, RWI, and blackouts as adolescents move into early adulthood.”
“Our findings are relevant to prevention programs that seek to incorporate alcohol screening with intentional inquiry about binge drinking. Moreover, our results may be instructive to programs that seek to leverage facets of parental practices to reduce health-risk contexts for youth,” Dr. Vaca and colleagues concluded. “Such prevention activities coupled with strengthening of policies and practices reducing adolescents’ access to alcohol could reduce later major alcohol-related health-risk behaviors and their consequences.”
Opioid misuse and risky behavior
In a second study, Devika Bhatia, MD, of the University of Colorado at Denver, Aurora, and colleagues examined opioid misuse in a nationally-representative sample of 14,765 adolescents from the Centers for Disease Control and Prevention’s 2017 Youth Risk Behavior Surveillance Survey. The researchers measured opioid misuse by categorizing adolescents into groups based on whether they had ever misused prescription opioids and whether they had engaged in risky driving behavior, violent behavior, risky sexual behavior, had a history of substance abuse, or attempted suicide.
Dr. Bhatia and colleagues found 14% of adolescents in the study reported misusing opioids, with an overrepresentation of 17-year-old and 18-year-old participants reporting opioid misuse (P less than .0001). there were no statistically significant difference between those who misused opioids and those who did not in terms of race, ethnicity, or sex.
Those adolescents who reported misusing opioids were 2.8 times more likely to not use a seatbelt; were 2.8 times more likely to have RWI; were 5.8 times more likely to have DWI; or 2.3 times more likely to have texted or emailed while driving. In each of these cases, P was less than .0001.
Adolescents who misused opioids also had significantly increased odds of engaging in risky sexual behaviors such as having sex before 13 years (3.9 times); having sex with four or more partners (4.8 times); using substances before sex (3.6 times); and not using a condom before sex (2.0 times). In each of these cases, P was less than .0001.
Additionally, adolescents in this category were between 5.4 times and 22.3 times more likely to use other substances (P less than .0001 for 10 variables); 4.9 times more likely to have attempted suicide (P less than .0001); or more likely to have engaged in violent behavior such as getting into physical fights (4.0 times), carrying a weapon (3.4 times) or a gun (5.1 times) within the last 30 days. In the four latter cases, P was less than .0001.
“With the ongoing opioid epidemic, pediatricians and child psychiatrists are likely to be more attuned to opioid misuse in their patients,” Dr. Bhatia and colleagues concluded. “If youth are screening positive for opioid misuse, pediatricians, nurses, social workers, child psychiatrists, and other providers assessing adolescents may have a new, broad range of other risky behaviors for which to screen regardless of the direction of the association.”
Substance use screening for treating substance use disorder traditionally has been is provided by a specialist, Jessica A. Kulak, PhD, MPH, said in an interview. “However, integration of care services may help to change societal norms around problematic substance use – both by decreasing stigma associated with substance use, as well as increasing clinicians’ preparedness, knowledge, and confidence in preventing and intervening on adolescents’ substance experimentation and use.” She recommended that clinicians in primary care improve their training by using the Substance Abuse and Mental Health Services Administration’s Screening, Brief Intervention, and Referral to Treatment program, which is available as a free online course.
Confidentiality is important in adolescent health, said Dr. Kulak, who is an assistant professor in the department of health, nutrition, and dietetics at State University of New York at Buffalo. “When discussing sensitive topics, such as binge drinking and opioid misuse, adolescents may fear that these or other risky activities may be disclosed to parents or law enforcement officials. Therefore, adolescent health providers should be aware of local, state, and federal laws pertaining to the confidentiality of minors.”
She added, “adolescents are often susceptible to others’ influences, so having open communication and support from a trusted adult – be it a parent or clinician – may also be protective against risky behaviors.”
The study by Vaca et al. was funded by the National Institutes of Health with support from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration. The study by Bhatia et al. had no external funding. The authors from both studies reported no relevant financial disclosures. Dr. Kulak said she had no financial disclosures or other conflicts of interest.
SOURCE: Vaca FE et al. Pediatrics. 2020; doi: 10.1542/peds.2018-4095. Bhatia D et al. Pediatrics. 2020; doi: 10.1542/peds.2019-2470.
These newly published reports indicate the high prevalence of risky behaviors and their associations – cross-sectionally and longitudinally – with major threats to adolescent health – so asking about alcohol use, opioid misuse, and associated health risks is truly “in the lane” of clinicians, school professionals, and parents who see and care about adolescents.
At this point, I think it’s incontrovertible that clinicians should screen adolescents to learn about their physical, emotional, and behavioral health. And they should seek opportunities for professional training, skills development, and expansion of their professional networks so they are able to address – individually or collaboratively via referrals – the behavioral and psychosocial health risks of their patients.
The good news is that there is growing awareness of the importance of using validated screening tools to identify patient behavioral health risks – including those pertaining to adolescent and young adult alcohol use and opioid misuse. “Best practice” dictates that screening approaches rely on asking questions using structured tools; intuition and “just winging it” are not effective or reliable for identifying patient behavior. Forward-looking clinics and practices could be asking patients to report about health behaviors in the waiting room (on a computer tablet, for example), or even remotely (using a secure app or data collection tool) in advance of a visit. Asking should be periodic – since behaviors can change fairly rapidly among young people. The benefit is that patient-reported information can be processed in advance to cue clinician follow-up and intervention. And youth tend to share more about their behaviors when they are asked electronically, rather than face to face. Intelligent screens can provide near real-time estimation of risk – to support in-office brief intervention tailored to the risk level of a young person or to trigger follow-up.
These studies indicate that binge alcohol use and misuse of prescription opioids among adolescents are real, pervasive, and deserving of our considered attention. There is no magic bullet. However busy clinicians may have a significant role to play in identifying and addressing these problems.
Elissa Weitzman, ScD, MSc, is an associate professor of pediatrics at Harvard Medical School, Boston, and an associate scientist based in adolescent/young adult medicine and the computational health informatics program at Boston Children’s Hospital. She was asked to comment on the articles by Vaca et al. and Bhatia et al. Dr. Weitzman said she had no relevant financial disclosures.
These newly published reports indicate the high prevalence of risky behaviors and their associations – cross-sectionally and longitudinally – with major threats to adolescent health – so asking about alcohol use, opioid misuse, and associated health risks is truly “in the lane” of clinicians, school professionals, and parents who see and care about adolescents.
At this point, I think it’s incontrovertible that clinicians should screen adolescents to learn about their physical, emotional, and behavioral health. And they should seek opportunities for professional training, skills development, and expansion of their professional networks so they are able to address – individually or collaboratively via referrals – the behavioral and psychosocial health risks of their patients.
The good news is that there is growing awareness of the importance of using validated screening tools to identify patient behavioral health risks – including those pertaining to adolescent and young adult alcohol use and opioid misuse. “Best practice” dictates that screening approaches rely on asking questions using structured tools; intuition and “just winging it” are not effective or reliable for identifying patient behavior. Forward-looking clinics and practices could be asking patients to report about health behaviors in the waiting room (on a computer tablet, for example), or even remotely (using a secure app or data collection tool) in advance of a visit. Asking should be periodic – since behaviors can change fairly rapidly among young people. The benefit is that patient-reported information can be processed in advance to cue clinician follow-up and intervention. And youth tend to share more about their behaviors when they are asked electronically, rather than face to face. Intelligent screens can provide near real-time estimation of risk – to support in-office brief intervention tailored to the risk level of a young person or to trigger follow-up.
These studies indicate that binge alcohol use and misuse of prescription opioids among adolescents are real, pervasive, and deserving of our considered attention. There is no magic bullet. However busy clinicians may have a significant role to play in identifying and addressing these problems.
Elissa Weitzman, ScD, MSc, is an associate professor of pediatrics at Harvard Medical School, Boston, and an associate scientist based in adolescent/young adult medicine and the computational health informatics program at Boston Children’s Hospital. She was asked to comment on the articles by Vaca et al. and Bhatia et al. Dr. Weitzman said she had no relevant financial disclosures.
These newly published reports indicate the high prevalence of risky behaviors and their associations – cross-sectionally and longitudinally – with major threats to adolescent health – so asking about alcohol use, opioid misuse, and associated health risks is truly “in the lane” of clinicians, school professionals, and parents who see and care about adolescents.
At this point, I think it’s incontrovertible that clinicians should screen adolescents to learn about their physical, emotional, and behavioral health. And they should seek opportunities for professional training, skills development, and expansion of their professional networks so they are able to address – individually or collaboratively via referrals – the behavioral and psychosocial health risks of their patients.
The good news is that there is growing awareness of the importance of using validated screening tools to identify patient behavioral health risks – including those pertaining to adolescent and young adult alcohol use and opioid misuse. “Best practice” dictates that screening approaches rely on asking questions using structured tools; intuition and “just winging it” are not effective or reliable for identifying patient behavior. Forward-looking clinics and practices could be asking patients to report about health behaviors in the waiting room (on a computer tablet, for example), or even remotely (using a secure app or data collection tool) in advance of a visit. Asking should be periodic – since behaviors can change fairly rapidly among young people. The benefit is that patient-reported information can be processed in advance to cue clinician follow-up and intervention. And youth tend to share more about their behaviors when they are asked electronically, rather than face to face. Intelligent screens can provide near real-time estimation of risk – to support in-office brief intervention tailored to the risk level of a young person or to trigger follow-up.
These studies indicate that binge alcohol use and misuse of prescription opioids among adolescents are real, pervasive, and deserving of our considered attention. There is no magic bullet. However busy clinicians may have a significant role to play in identifying and addressing these problems.
Elissa Weitzman, ScD, MSc, is an associate professor of pediatrics at Harvard Medical School, Boston, and an associate scientist based in adolescent/young adult medicine and the computational health informatics program at Boston Children’s Hospital. She was asked to comment on the articles by Vaca et al. and Bhatia et al. Dr. Weitzman said she had no relevant financial disclosures.
Binge drinking and misuse of opioids led to risky behavior during adolescence, two studies from the journal Pediatrics highlighted. And the binge drinking in high school may predict risky driving behaviors up to 4 years after high school.
Federico E. Vaca, MD, of the developmental neurocognitive driving simulation research center at Yale University, New Haven, Conn., and colleagues examined the associations between risky driving behaviors and binge drinking of 2,785 adolescents in the nationally representative, longitudinal NEXT Generation Health Study. The researchers studied the effects of binge drinking on driving while impaired (DWI), riding with an impaired driver (RWI), blackouts, extreme binge drinking, and risky driving.
The adolescents were studied across seven waves, with Wave 1 beginning in the 2009-2010 school year (10th grade; mean age, 16 years), and data extended up to 4 years after high school. Of all adolescents enrolled, 91% completed Wave 1, 88% completed Wave 2, 86% completed Wave 3 (12th grade), 78% completed Wave 4, 79% completed Wave 5, 84% completed Wave 6, and 83% completed Wave 7 (4 years after leaving high school) of the study.
High school binge drinking predicts later risky behavior
About one-quarter of adolescents reported binge drinking in Waves 1-3, with an incidence of 27% in Wave 1, 24% in Wave 2, and 27% in Wave 3. Adolescents who reported binge drinking in Wave 3 had a higher likelihood of DWI in subsequent waves, with nearly six times higher odds in Wave 5 and more than twice as likely in Wave 7, researchers said. Binge drinking in Wave 3 also was associated with greater than four times higher odds of RWI in Wave 4, and more than two and a half times higher odds of RWI in Wave 7. Among adolescents who reported binge drinking across 3 years in high school, there was a higher likelihood of extreme binge drinking in Wave 7, and higher likelihood of risky driving after graduating.
Impact of parental knowledge of drinking
in some waves. Father monitoring knowledge of drinking in Waves 1-3 lowered the odds of DWI by 30% in Wave 5 and 20% in Wave 6, while also lowering the odds of RWI in Wave 4 and Wave 7 by 20%.
Mother knowledge of drinking in Waves 1-3 was associated with 60% lower odds of DWI in Wave 4, but did not lower odds in any wave for RWI.
Overall, parental support for not drinking lowered odds for DWI by 40% in Waves 4 and 5, and by 30% in Wave 7 while also lowering odds of RWI in Wave 4 by 20%.
The results are consistent with other studies examining risky driving behavior and binge drinking in adolescent populations, but researchers noted that “to an important but limited extent, parental practices while the teenager is in high school may protect against DWI, RWI, and blackouts as adolescents move into early adulthood.”
“Our findings are relevant to prevention programs that seek to incorporate alcohol screening with intentional inquiry about binge drinking. Moreover, our results may be instructive to programs that seek to leverage facets of parental practices to reduce health-risk contexts for youth,” Dr. Vaca and colleagues concluded. “Such prevention activities coupled with strengthening of policies and practices reducing adolescents’ access to alcohol could reduce later major alcohol-related health-risk behaviors and their consequences.”
Opioid misuse and risky behavior
In a second study, Devika Bhatia, MD, of the University of Colorado at Denver, Aurora, and colleagues examined opioid misuse in a nationally-representative sample of 14,765 adolescents from the Centers for Disease Control and Prevention’s 2017 Youth Risk Behavior Surveillance Survey. The researchers measured opioid misuse by categorizing adolescents into groups based on whether they had ever misused prescription opioids and whether they had engaged in risky driving behavior, violent behavior, risky sexual behavior, had a history of substance abuse, or attempted suicide.
Dr. Bhatia and colleagues found 14% of adolescents in the study reported misusing opioids, with an overrepresentation of 17-year-old and 18-year-old participants reporting opioid misuse (P less than .0001). there were no statistically significant difference between those who misused opioids and those who did not in terms of race, ethnicity, or sex.
Those adolescents who reported misusing opioids were 2.8 times more likely to not use a seatbelt; were 2.8 times more likely to have RWI; were 5.8 times more likely to have DWI; or 2.3 times more likely to have texted or emailed while driving. In each of these cases, P was less than .0001.
Adolescents who misused opioids also had significantly increased odds of engaging in risky sexual behaviors such as having sex before 13 years (3.9 times); having sex with four or more partners (4.8 times); using substances before sex (3.6 times); and not using a condom before sex (2.0 times). In each of these cases, P was less than .0001.
Additionally, adolescents in this category were between 5.4 times and 22.3 times more likely to use other substances (P less than .0001 for 10 variables); 4.9 times more likely to have attempted suicide (P less than .0001); or more likely to have engaged in violent behavior such as getting into physical fights (4.0 times), carrying a weapon (3.4 times) or a gun (5.1 times) within the last 30 days. In the four latter cases, P was less than .0001.
“With the ongoing opioid epidemic, pediatricians and child psychiatrists are likely to be more attuned to opioid misuse in their patients,” Dr. Bhatia and colleagues concluded. “If youth are screening positive for opioid misuse, pediatricians, nurses, social workers, child psychiatrists, and other providers assessing adolescents may have a new, broad range of other risky behaviors for which to screen regardless of the direction of the association.”
Substance use screening for treating substance use disorder traditionally has been is provided by a specialist, Jessica A. Kulak, PhD, MPH, said in an interview. “However, integration of care services may help to change societal norms around problematic substance use – both by decreasing stigma associated with substance use, as well as increasing clinicians’ preparedness, knowledge, and confidence in preventing and intervening on adolescents’ substance experimentation and use.” She recommended that clinicians in primary care improve their training by using the Substance Abuse and Mental Health Services Administration’s Screening, Brief Intervention, and Referral to Treatment program, which is available as a free online course.
Confidentiality is important in adolescent health, said Dr. Kulak, who is an assistant professor in the department of health, nutrition, and dietetics at State University of New York at Buffalo. “When discussing sensitive topics, such as binge drinking and opioid misuse, adolescents may fear that these or other risky activities may be disclosed to parents or law enforcement officials. Therefore, adolescent health providers should be aware of local, state, and federal laws pertaining to the confidentiality of minors.”
She added, “adolescents are often susceptible to others’ influences, so having open communication and support from a trusted adult – be it a parent or clinician – may also be protective against risky behaviors.”
The study by Vaca et al. was funded by the National Institutes of Health with support from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration. The study by Bhatia et al. had no external funding. The authors from both studies reported no relevant financial disclosures. Dr. Kulak said she had no financial disclosures or other conflicts of interest.
SOURCE: Vaca FE et al. Pediatrics. 2020; doi: 10.1542/peds.2018-4095. Bhatia D et al. Pediatrics. 2020; doi: 10.1542/peds.2019-2470.
Binge drinking and misuse of opioids led to risky behavior during adolescence, two studies from the journal Pediatrics highlighted. And the binge drinking in high school may predict risky driving behaviors up to 4 years after high school.
Federico E. Vaca, MD, of the developmental neurocognitive driving simulation research center at Yale University, New Haven, Conn., and colleagues examined the associations between risky driving behaviors and binge drinking of 2,785 adolescents in the nationally representative, longitudinal NEXT Generation Health Study. The researchers studied the effects of binge drinking on driving while impaired (DWI), riding with an impaired driver (RWI), blackouts, extreme binge drinking, and risky driving.
The adolescents were studied across seven waves, with Wave 1 beginning in the 2009-2010 school year (10th grade; mean age, 16 years), and data extended up to 4 years after high school. Of all adolescents enrolled, 91% completed Wave 1, 88% completed Wave 2, 86% completed Wave 3 (12th grade), 78% completed Wave 4, 79% completed Wave 5, 84% completed Wave 6, and 83% completed Wave 7 (4 years after leaving high school) of the study.
High school binge drinking predicts later risky behavior
About one-quarter of adolescents reported binge drinking in Waves 1-3, with an incidence of 27% in Wave 1, 24% in Wave 2, and 27% in Wave 3. Adolescents who reported binge drinking in Wave 3 had a higher likelihood of DWI in subsequent waves, with nearly six times higher odds in Wave 5 and more than twice as likely in Wave 7, researchers said. Binge drinking in Wave 3 also was associated with greater than four times higher odds of RWI in Wave 4, and more than two and a half times higher odds of RWI in Wave 7. Among adolescents who reported binge drinking across 3 years in high school, there was a higher likelihood of extreme binge drinking in Wave 7, and higher likelihood of risky driving after graduating.
Impact of parental knowledge of drinking
in some waves. Father monitoring knowledge of drinking in Waves 1-3 lowered the odds of DWI by 30% in Wave 5 and 20% in Wave 6, while also lowering the odds of RWI in Wave 4 and Wave 7 by 20%.
Mother knowledge of drinking in Waves 1-3 was associated with 60% lower odds of DWI in Wave 4, but did not lower odds in any wave for RWI.
Overall, parental support for not drinking lowered odds for DWI by 40% in Waves 4 and 5, and by 30% in Wave 7 while also lowering odds of RWI in Wave 4 by 20%.
The results are consistent with other studies examining risky driving behavior and binge drinking in adolescent populations, but researchers noted that “to an important but limited extent, parental practices while the teenager is in high school may protect against DWI, RWI, and blackouts as adolescents move into early adulthood.”
“Our findings are relevant to prevention programs that seek to incorporate alcohol screening with intentional inquiry about binge drinking. Moreover, our results may be instructive to programs that seek to leverage facets of parental practices to reduce health-risk contexts for youth,” Dr. Vaca and colleagues concluded. “Such prevention activities coupled with strengthening of policies and practices reducing adolescents’ access to alcohol could reduce later major alcohol-related health-risk behaviors and their consequences.”
Opioid misuse and risky behavior
In a second study, Devika Bhatia, MD, of the University of Colorado at Denver, Aurora, and colleagues examined opioid misuse in a nationally-representative sample of 14,765 adolescents from the Centers for Disease Control and Prevention’s 2017 Youth Risk Behavior Surveillance Survey. The researchers measured opioid misuse by categorizing adolescents into groups based on whether they had ever misused prescription opioids and whether they had engaged in risky driving behavior, violent behavior, risky sexual behavior, had a history of substance abuse, or attempted suicide.
Dr. Bhatia and colleagues found 14% of adolescents in the study reported misusing opioids, with an overrepresentation of 17-year-old and 18-year-old participants reporting opioid misuse (P less than .0001). there were no statistically significant difference between those who misused opioids and those who did not in terms of race, ethnicity, or sex.
Those adolescents who reported misusing opioids were 2.8 times more likely to not use a seatbelt; were 2.8 times more likely to have RWI; were 5.8 times more likely to have DWI; or 2.3 times more likely to have texted or emailed while driving. In each of these cases, P was less than .0001.
Adolescents who misused opioids also had significantly increased odds of engaging in risky sexual behaviors such as having sex before 13 years (3.9 times); having sex with four or more partners (4.8 times); using substances before sex (3.6 times); and not using a condom before sex (2.0 times). In each of these cases, P was less than .0001.
Additionally, adolescents in this category were between 5.4 times and 22.3 times more likely to use other substances (P less than .0001 for 10 variables); 4.9 times more likely to have attempted suicide (P less than .0001); or more likely to have engaged in violent behavior such as getting into physical fights (4.0 times), carrying a weapon (3.4 times) or a gun (5.1 times) within the last 30 days. In the four latter cases, P was less than .0001.
“With the ongoing opioid epidemic, pediatricians and child psychiatrists are likely to be more attuned to opioid misuse in their patients,” Dr. Bhatia and colleagues concluded. “If youth are screening positive for opioid misuse, pediatricians, nurses, social workers, child psychiatrists, and other providers assessing adolescents may have a new, broad range of other risky behaviors for which to screen regardless of the direction of the association.”
Substance use screening for treating substance use disorder traditionally has been is provided by a specialist, Jessica A. Kulak, PhD, MPH, said in an interview. “However, integration of care services may help to change societal norms around problematic substance use – both by decreasing stigma associated with substance use, as well as increasing clinicians’ preparedness, knowledge, and confidence in preventing and intervening on adolescents’ substance experimentation and use.” She recommended that clinicians in primary care improve their training by using the Substance Abuse and Mental Health Services Administration’s Screening, Brief Intervention, and Referral to Treatment program, which is available as a free online course.
Confidentiality is important in adolescent health, said Dr. Kulak, who is an assistant professor in the department of health, nutrition, and dietetics at State University of New York at Buffalo. “When discussing sensitive topics, such as binge drinking and opioid misuse, adolescents may fear that these or other risky activities may be disclosed to parents or law enforcement officials. Therefore, adolescent health providers should be aware of local, state, and federal laws pertaining to the confidentiality of minors.”
She added, “adolescents are often susceptible to others’ influences, so having open communication and support from a trusted adult – be it a parent or clinician – may also be protective against risky behaviors.”
The study by Vaca et al. was funded by the National Institutes of Health with support from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration. The study by Bhatia et al. had no external funding. The authors from both studies reported no relevant financial disclosures. Dr. Kulak said she had no financial disclosures or other conflicts of interest.
SOURCE: Vaca FE et al. Pediatrics. 2020; doi: 10.1542/peds.2018-4095. Bhatia D et al. Pediatrics. 2020; doi: 10.1542/peds.2019-2470.
FROM PEDIATRICS
Adolescents should know risks of tattoos and piercings
NEW ORLEANS – It wasn’t until her teenage daughter wanted to get her belly button pierced that Cora Breuner, MD, became interested in the safety of tattoos and piercings for adolescents.
“You’re a pediatrician,” her daughter said. “Where should I go? Should I get this done?” Although Dr. Breuner didn’t want her daughter to get the piercing, she knew saying “no” wasn’t likely to stop her teenager any more than it would another adolescent, so she looked to the medical literature … and didn’t find much.
“I couldn’t find an article summarizing complication rates or just about the legality of it or other issues around tattooing and piercing,” said Dr. Breuner a professor of pediatrics at Seattle Children’s Hospital and the University of Washington, also in Seattle. So she and the American Academy of Pediatrics’ Committee on Adolescent Health did the work themselves and wrote one.
“I want to make sure that you are talking to your teenagers about this,” she told attendees at the annual meeting of the American Academy of Pediatrics. In her presentation, she focused on knowing the legal age of consent for body modifications and what to watch for in terms of complications.
Tattoos growing in popularity
More than a third (38%) of people aged 18-29 years have at least one tattoo, according to a Pew Research Center report Dr. Breuner cited, and 23% had piercings somewhere on their body besides their ears. In fact, Americans spend about $1.65 billion on tattoos each year.
Most of the people with tattoos (72%), however, had them in places that were covered and not visible, reinforcing the need to ask about them. The popularity of tattoos has been increasing in general, Dr. Breuner noted. In just the 4 years from 2012 to 2016, the prevalence of U.S. adults with at least one tattoo increased 20%.
And people don’t appear to be sorry to have them. According to a Harris Poll that Dr. Breuner cited, 86% of respondents in 2012 did not regret getting their tattoo, and respondents listed a number of feelings they associated with their tattoos: feeling sexy, rebellious, attractive, strong, spiritual, healthier, intelligent, and athletic.
Although the techniques for tattooing have changed over the years since the first documented ones in 4,000 B.C., the basic concept of injecting ink into the dermis hasn’t changed much. By injecting the ink below the epidermis, the ink remains visible for the rest of a person’s life.
The laws for tattoos vary by state, so you need to check the laws where they live. Not much data exist on infections and complaints, but data from the Michigan Department of Health & Human Services suggests the infection rate – at least those infections reported – is low while the rate of illegally operating facilities is a bigger risk. Local health districts in Michigan have received reports of only 18 infections since 2010, but they’ve received 85 reports of illegal operations and 69 reports of social media parties centered on all attendees getting a tattoo.
Risks of tattoos
The biggest concern for adolescents is ensuring they understand the risks of tattoos and piercings and what to look for. One risk for tattoos is hepatitis C. However, the studies on the risk of contracting hepatitis C from tattooing are confounded by the fact that many people getting tattoos also may be engaging in other risky behaviors, such as intravenous drug use or risky sexual behaviors. Still, some research suggests that “commercially acquired tattoos accounted for more than twice as many infections as injection-drug use,” Dr. Breuner said.
Another risk is tattoo-associated bacterial skin infections (Clin Infect Dis. 2019 Aug 30;69[6]:949-55; MMWR Morb Mortal Wkly Rep. 2012 Aug 24;61[33]:653-6).
Risks of body piercing
Although body piercing doesn’t date back quite as far as tattoos – about 700 A.D. – its history remains long. Research suggests the top reason people get body piercings is simply liking the way it looks, as 77% of respondents reported in one study (J Am Osteopath Assoc. 2007 Oct;107[10]:432-8). Other reasons including looking fashionable, catching attention, feeling different, making a personal statement, being daring, fitting in, pressuring from peers, and defying parents.
The most serious potential complication from piercings is gangrene, but the most common is infection. Other possible complications include an allergic reaction to the metal used, a bleeding complication (estimated in 1 of 10), a scar or site reaction (estimated in 1 of 15), or, much less commonly, toxic shock syndrome. In some areas, there’s a risk of nerve damage if the nerve is pierced, such as in the eyebrow or in the bridge of the nose.
Teens particularly should be aware of the average time it takes for a piercing to heal, depending on where they get it. A navel piercing, for example, can take up to 9 months to heal. Others with long healing times include the penis (3-9 months), labia majora (2-4 months), nipple (2-4 months), and scrotum (2-3 months). Other non-ear regions range from 2 to 8 weeks.
Bleeding definitely is a risk for piercings, Dr. Breuner said, especially now that so many teens are piercing body parts besides their ears. “The one I found most disturbing was that of the uvula,” she said. Bleeding risks tend to be low with ear and nose piercings, but the risk increases with the tongue, uvula, navel, nipples, and genitalia.
Another risk of mouth piercings, particularly tongue piercing, is damage to the teeth and gums, Dr. Breuner said. Barbells, the most popular type of mouth piercing, can lead to receding gums and chipped teeth with extended wear, especially because people wearing them have a tendency to frequently bite down on them.
One study found that half the participants who wore a long barbell piercing (1.59 cm or longer) for at least 2 years had lingual recession on their mandibular central incisors (J Periodontol. 2002 Mar;73[3]:289-97). Among those with a tongue piercing of at least 4 years, 47% had tooth chipping on their molars and premolars.
Another study found gingival recession was 11 times more likely among people with tongue piercings than without (J Clin Periodontol. 2010 Aug 1;37(8):712-8). Gingival recession also is a risk with lip piercings, but the risk is greater with tongue piercing, and only tongue piercings have been associated with tooth injuries (Aust Dent J. 2012 Mar;57[1]:71-8; Int J Dent Hyg. 2016 Feb;14[1]:62-73).
Hepatitis C also is a concern with body piercing. According to a systematic review of 12 studies, body piercing was a risk factor for hepatitis C infection in the majority of them (Am J Infect Control. 2001 Aug;29[4]:271-4).
Counseling adolescents on body modifications
You should ask teens about any tattoos or piercings they have at each visit and ask whether they have any plans to get any. Then you can answer questions about them and ensure the teens are aware of risks, particularly viral and bacterial infections and, with piercing, bleeding.
Beyond the medical risks, it’s important for teens to understand that tattoos have the potential to limit their employment in the future, depending on the job and how visible their tattoo is.
Social acceptance of tattoos and piercings have been increasing, but a survey of nearly 2,700 people conducted by Salary.com in 2013 found that 76% of respondents believed tattoos and piercings could reduce a job applicant’s chances of being hired.
If you want to learn more specifically about the safest places in your community for tattoos and piercings, Dr. Breuner recommended going out and visiting the shops. Tattoo artists generally are the most knowledgeable people in the community about the risks of their industry and often welcome local physicians who want to learn and see their equipment, she said.
NEW ORLEANS – It wasn’t until her teenage daughter wanted to get her belly button pierced that Cora Breuner, MD, became interested in the safety of tattoos and piercings for adolescents.
“You’re a pediatrician,” her daughter said. “Where should I go? Should I get this done?” Although Dr. Breuner didn’t want her daughter to get the piercing, she knew saying “no” wasn’t likely to stop her teenager any more than it would another adolescent, so she looked to the medical literature … and didn’t find much.
“I couldn’t find an article summarizing complication rates or just about the legality of it or other issues around tattooing and piercing,” said Dr. Breuner a professor of pediatrics at Seattle Children’s Hospital and the University of Washington, also in Seattle. So she and the American Academy of Pediatrics’ Committee on Adolescent Health did the work themselves and wrote one.
“I want to make sure that you are talking to your teenagers about this,” she told attendees at the annual meeting of the American Academy of Pediatrics. In her presentation, she focused on knowing the legal age of consent for body modifications and what to watch for in terms of complications.
Tattoos growing in popularity
More than a third (38%) of people aged 18-29 years have at least one tattoo, according to a Pew Research Center report Dr. Breuner cited, and 23% had piercings somewhere on their body besides their ears. In fact, Americans spend about $1.65 billion on tattoos each year.
Most of the people with tattoos (72%), however, had them in places that were covered and not visible, reinforcing the need to ask about them. The popularity of tattoos has been increasing in general, Dr. Breuner noted. In just the 4 years from 2012 to 2016, the prevalence of U.S. adults with at least one tattoo increased 20%.
And people don’t appear to be sorry to have them. According to a Harris Poll that Dr. Breuner cited, 86% of respondents in 2012 did not regret getting their tattoo, and respondents listed a number of feelings they associated with their tattoos: feeling sexy, rebellious, attractive, strong, spiritual, healthier, intelligent, and athletic.
Although the techniques for tattooing have changed over the years since the first documented ones in 4,000 B.C., the basic concept of injecting ink into the dermis hasn’t changed much. By injecting the ink below the epidermis, the ink remains visible for the rest of a person’s life.
The laws for tattoos vary by state, so you need to check the laws where they live. Not much data exist on infections and complaints, but data from the Michigan Department of Health & Human Services suggests the infection rate – at least those infections reported – is low while the rate of illegally operating facilities is a bigger risk. Local health districts in Michigan have received reports of only 18 infections since 2010, but they’ve received 85 reports of illegal operations and 69 reports of social media parties centered on all attendees getting a tattoo.
Risks of tattoos
The biggest concern for adolescents is ensuring they understand the risks of tattoos and piercings and what to look for. One risk for tattoos is hepatitis C. However, the studies on the risk of contracting hepatitis C from tattooing are confounded by the fact that many people getting tattoos also may be engaging in other risky behaviors, such as intravenous drug use or risky sexual behaviors. Still, some research suggests that “commercially acquired tattoos accounted for more than twice as many infections as injection-drug use,” Dr. Breuner said.
Another risk is tattoo-associated bacterial skin infections (Clin Infect Dis. 2019 Aug 30;69[6]:949-55; MMWR Morb Mortal Wkly Rep. 2012 Aug 24;61[33]:653-6).
Risks of body piercing
Although body piercing doesn’t date back quite as far as tattoos – about 700 A.D. – its history remains long. Research suggests the top reason people get body piercings is simply liking the way it looks, as 77% of respondents reported in one study (J Am Osteopath Assoc. 2007 Oct;107[10]:432-8). Other reasons including looking fashionable, catching attention, feeling different, making a personal statement, being daring, fitting in, pressuring from peers, and defying parents.
The most serious potential complication from piercings is gangrene, but the most common is infection. Other possible complications include an allergic reaction to the metal used, a bleeding complication (estimated in 1 of 10), a scar or site reaction (estimated in 1 of 15), or, much less commonly, toxic shock syndrome. In some areas, there’s a risk of nerve damage if the nerve is pierced, such as in the eyebrow or in the bridge of the nose.
Teens particularly should be aware of the average time it takes for a piercing to heal, depending on where they get it. A navel piercing, for example, can take up to 9 months to heal. Others with long healing times include the penis (3-9 months), labia majora (2-4 months), nipple (2-4 months), and scrotum (2-3 months). Other non-ear regions range from 2 to 8 weeks.
Bleeding definitely is a risk for piercings, Dr. Breuner said, especially now that so many teens are piercing body parts besides their ears. “The one I found most disturbing was that of the uvula,” she said. Bleeding risks tend to be low with ear and nose piercings, but the risk increases with the tongue, uvula, navel, nipples, and genitalia.
Another risk of mouth piercings, particularly tongue piercing, is damage to the teeth and gums, Dr. Breuner said. Barbells, the most popular type of mouth piercing, can lead to receding gums and chipped teeth with extended wear, especially because people wearing them have a tendency to frequently bite down on them.
One study found that half the participants who wore a long barbell piercing (1.59 cm or longer) for at least 2 years had lingual recession on their mandibular central incisors (J Periodontol. 2002 Mar;73[3]:289-97). Among those with a tongue piercing of at least 4 years, 47% had tooth chipping on their molars and premolars.
Another study found gingival recession was 11 times more likely among people with tongue piercings than without (J Clin Periodontol. 2010 Aug 1;37(8):712-8). Gingival recession also is a risk with lip piercings, but the risk is greater with tongue piercing, and only tongue piercings have been associated with tooth injuries (Aust Dent J. 2012 Mar;57[1]:71-8; Int J Dent Hyg. 2016 Feb;14[1]:62-73).
Hepatitis C also is a concern with body piercing. According to a systematic review of 12 studies, body piercing was a risk factor for hepatitis C infection in the majority of them (Am J Infect Control. 2001 Aug;29[4]:271-4).
Counseling adolescents on body modifications
You should ask teens about any tattoos or piercings they have at each visit and ask whether they have any plans to get any. Then you can answer questions about them and ensure the teens are aware of risks, particularly viral and bacterial infections and, with piercing, bleeding.
Beyond the medical risks, it’s important for teens to understand that tattoos have the potential to limit their employment in the future, depending on the job and how visible their tattoo is.
Social acceptance of tattoos and piercings have been increasing, but a survey of nearly 2,700 people conducted by Salary.com in 2013 found that 76% of respondents believed tattoos and piercings could reduce a job applicant’s chances of being hired.
If you want to learn more specifically about the safest places in your community for tattoos and piercings, Dr. Breuner recommended going out and visiting the shops. Tattoo artists generally are the most knowledgeable people in the community about the risks of their industry and often welcome local physicians who want to learn and see their equipment, she said.
NEW ORLEANS – It wasn’t until her teenage daughter wanted to get her belly button pierced that Cora Breuner, MD, became interested in the safety of tattoos and piercings for adolescents.
“You’re a pediatrician,” her daughter said. “Where should I go? Should I get this done?” Although Dr. Breuner didn’t want her daughter to get the piercing, she knew saying “no” wasn’t likely to stop her teenager any more than it would another adolescent, so she looked to the medical literature … and didn’t find much.
“I couldn’t find an article summarizing complication rates or just about the legality of it or other issues around tattooing and piercing,” said Dr. Breuner a professor of pediatrics at Seattle Children’s Hospital and the University of Washington, also in Seattle. So she and the American Academy of Pediatrics’ Committee on Adolescent Health did the work themselves and wrote one.
“I want to make sure that you are talking to your teenagers about this,” she told attendees at the annual meeting of the American Academy of Pediatrics. In her presentation, she focused on knowing the legal age of consent for body modifications and what to watch for in terms of complications.
Tattoos growing in popularity
More than a third (38%) of people aged 18-29 years have at least one tattoo, according to a Pew Research Center report Dr. Breuner cited, and 23% had piercings somewhere on their body besides their ears. In fact, Americans spend about $1.65 billion on tattoos each year.
Most of the people with tattoos (72%), however, had them in places that were covered and not visible, reinforcing the need to ask about them. The popularity of tattoos has been increasing in general, Dr. Breuner noted. In just the 4 years from 2012 to 2016, the prevalence of U.S. adults with at least one tattoo increased 20%.
And people don’t appear to be sorry to have them. According to a Harris Poll that Dr. Breuner cited, 86% of respondents in 2012 did not regret getting their tattoo, and respondents listed a number of feelings they associated with their tattoos: feeling sexy, rebellious, attractive, strong, spiritual, healthier, intelligent, and athletic.
Although the techniques for tattooing have changed over the years since the first documented ones in 4,000 B.C., the basic concept of injecting ink into the dermis hasn’t changed much. By injecting the ink below the epidermis, the ink remains visible for the rest of a person’s life.
The laws for tattoos vary by state, so you need to check the laws where they live. Not much data exist on infections and complaints, but data from the Michigan Department of Health & Human Services suggests the infection rate – at least those infections reported – is low while the rate of illegally operating facilities is a bigger risk. Local health districts in Michigan have received reports of only 18 infections since 2010, but they’ve received 85 reports of illegal operations and 69 reports of social media parties centered on all attendees getting a tattoo.
Risks of tattoos
The biggest concern for adolescents is ensuring they understand the risks of tattoos and piercings and what to look for. One risk for tattoos is hepatitis C. However, the studies on the risk of contracting hepatitis C from tattooing are confounded by the fact that many people getting tattoos also may be engaging in other risky behaviors, such as intravenous drug use or risky sexual behaviors. Still, some research suggests that “commercially acquired tattoos accounted for more than twice as many infections as injection-drug use,” Dr. Breuner said.
Another risk is tattoo-associated bacterial skin infections (Clin Infect Dis. 2019 Aug 30;69[6]:949-55; MMWR Morb Mortal Wkly Rep. 2012 Aug 24;61[33]:653-6).
Risks of body piercing
Although body piercing doesn’t date back quite as far as tattoos – about 700 A.D. – its history remains long. Research suggests the top reason people get body piercings is simply liking the way it looks, as 77% of respondents reported in one study (J Am Osteopath Assoc. 2007 Oct;107[10]:432-8). Other reasons including looking fashionable, catching attention, feeling different, making a personal statement, being daring, fitting in, pressuring from peers, and defying parents.
The most serious potential complication from piercings is gangrene, but the most common is infection. Other possible complications include an allergic reaction to the metal used, a bleeding complication (estimated in 1 of 10), a scar or site reaction (estimated in 1 of 15), or, much less commonly, toxic shock syndrome. In some areas, there’s a risk of nerve damage if the nerve is pierced, such as in the eyebrow or in the bridge of the nose.
Teens particularly should be aware of the average time it takes for a piercing to heal, depending on where they get it. A navel piercing, for example, can take up to 9 months to heal. Others with long healing times include the penis (3-9 months), labia majora (2-4 months), nipple (2-4 months), and scrotum (2-3 months). Other non-ear regions range from 2 to 8 weeks.
Bleeding definitely is a risk for piercings, Dr. Breuner said, especially now that so many teens are piercing body parts besides their ears. “The one I found most disturbing was that of the uvula,” she said. Bleeding risks tend to be low with ear and nose piercings, but the risk increases with the tongue, uvula, navel, nipples, and genitalia.
Another risk of mouth piercings, particularly tongue piercing, is damage to the teeth and gums, Dr. Breuner said. Barbells, the most popular type of mouth piercing, can lead to receding gums and chipped teeth with extended wear, especially because people wearing them have a tendency to frequently bite down on them.
One study found that half the participants who wore a long barbell piercing (1.59 cm or longer) for at least 2 years had lingual recession on their mandibular central incisors (J Periodontol. 2002 Mar;73[3]:289-97). Among those with a tongue piercing of at least 4 years, 47% had tooth chipping on their molars and premolars.
Another study found gingival recession was 11 times more likely among people with tongue piercings than without (J Clin Periodontol. 2010 Aug 1;37(8):712-8). Gingival recession also is a risk with lip piercings, but the risk is greater with tongue piercing, and only tongue piercings have been associated with tooth injuries (Aust Dent J. 2012 Mar;57[1]:71-8; Int J Dent Hyg. 2016 Feb;14[1]:62-73).
Hepatitis C also is a concern with body piercing. According to a systematic review of 12 studies, body piercing was a risk factor for hepatitis C infection in the majority of them (Am J Infect Control. 2001 Aug;29[4]:271-4).
Counseling adolescents on body modifications
You should ask teens about any tattoos or piercings they have at each visit and ask whether they have any plans to get any. Then you can answer questions about them and ensure the teens are aware of risks, particularly viral and bacterial infections and, with piercing, bleeding.
Beyond the medical risks, it’s important for teens to understand that tattoos have the potential to limit their employment in the future, depending on the job and how visible their tattoo is.
Social acceptance of tattoos and piercings have been increasing, but a survey of nearly 2,700 people conducted by Salary.com in 2013 found that 76% of respondents believed tattoos and piercings could reduce a job applicant’s chances of being hired.
If you want to learn more specifically about the safest places in your community for tattoos and piercings, Dr. Breuner recommended going out and visiting the shops. Tattoo artists generally are the most knowledgeable people in the community about the risks of their industry and often welcome local physicians who want to learn and see their equipment, she said.
EXPERT ANALYSIS FROM AAP 19
Managing pain in kids during minor procedures: A tricky balance
NEW ORLEANS – Baruch S. Krauss, MD, EdM said at the annual meeting of the American Academy of Pediatrics.
Dr. Krauss, a pediatric emergency physician at Boston Children’s Hospital, shared tips for producing a positive experience when children present for minor procedures such as an intravenous catheter insertion or a laceration repair.
Control the environment
Setting the stage for a positive experience for children and their parents involves decreasing sensory stimuli by minimizing noise and bustle, the number of people in the room, and the reminder cues. “Even if you have trust with the child, there are certain things that could trigger the child to become fearful and anxious,” said Dr. Krauss, who also holds an academic post in the department of pediatrics at Harvard Medical School, Boston. “You want to make sure that medical equipment or a syringe is covered – anything that would remind the child or trigger the child to be more concerned and anxious.”
He recommends careful use of lighting, particularly in children who present with a head laceration or a facial laceration. “You may need to put a light near the wound, but that may be fearful for the child,” said Dr. Krauss, who coauthored a recent article on the topic that contains links to instructional videos (Ann Emerg Med 2019;74[1]:30-5). “Read the cues of the child,” he said. One desensitization technique he uses in such cases is to tell the child a story about the sun. He then goes on to liken the warmth of the exam light to the warmth of the sun.
Limiting the number of clinicians who speak to the child during the procedure also is key. “One person should speak to the child,” he advised. “Otherwise, it creates confusion for the child and it is hard for them to focus their attention. What you really want is to be able to control the child’s attention. You want to be able to capture their attention.”
It’s also important to keep medical equipment out of view. “I can’t tell you how many times I’ve seen consultants come in and a child needs to have a laceration repair, and they’re filling the syringe with lidocaine in front of the child,” Dr. Krauss said. “You want to avoid that. You also want to work outside of the child’s visual field if you can. Positioning is critical. I will try whatever position works for the child and the family.” This may including asking the parent to hold and swaddle an infant during the procedure, or positioning young children in the parent’s lap with their arm secured.
“Two things that upset kids during laceration repair are water dripping into their eyes during irrigation and the suture falling across their face as you’re stitching,” he added. “You want to develop your procedural skills so you can avoid that happening.”
Tailor the approach to the individual child
Some children will want to watch what you’re doing, but normally Dr. Krauss uses towels or blankets to cover the area being worked on. “If the child is part of your practice and you know his temperament and coping style, that makes it a lot easier; you know how to approach him,” he said. “They can trust you but they still can be quite fearful.” Sometimes, the child is relaxed but the parent becomes anxious. That anxiety can be transmitted to child. “If I see that the parents are anxious, I work directly with the child, and not the parent,” he said. “There’s not much I can tell a parent verbally that’s going to change their anxiety or fear level. But, as soon I start moving the child’s emotional state from fear to trust, the parent senses that and they relax, and that gets transmitted back to the child.”
Use age-appropriate language
When treating infants and children, Dr. Krauss often uses “parentese,” a simplified way that parents use to talk to young children. “It’s clearer, simpler, more attention-maintaining, and has longer pauses,” he said. “That can be very comforting to children.” Content and phrasing become important in older children. “You want to avoid the nocebo effect,” he continued. “If you tell a child, ‘This is really going to sting or hurt,’ you’re tipping the scales toward them having that experience.”
In an article about behavioral approaches to anxiety and pain management for pediatric venous access, Lindsey L. Cohen, PhD, devised a list of suggested phrasing to use. For example, instead of saying “You will be fine; there is nothing to worry about,” ask, “What did you do in school today?” as a form of distraction. Instead of saying, “It will feel like a bee sting,” ask, “Tell me how it feels.” And instead of saying, “Don’t cry,” say, “That was hard; I am proud of you” (Pediatrics 2008;122[suppl 3]:S134-9).
In a more recent article, Dr. Krauss and colleagues discussed current concepts of managing pain in children who present to the emergency department (Lancet 2016;387:83-92). Among distracting activities to try with infants and preschoolers are blowing bubbles, the use of a lighted wand, sound, music, or books, they noted. Distracting activities to try with preschoolers and in older children include art activities such as drawing, coloring, and the use of play dough, and computer games.
Clinicians also can ask the child to engage in a developmental task as a form of distraction. Dr. Krauss recalled a 22-month-old boy who presented to the emergency department with a forehead laceration. Mindful that the boy was developing eye-hand coordination and fine motor activity, Dr. Krauss offered him a coloring book that contained a picture of a clown, and instructed him to color the clown’s eyes red while Dr. Krauss tended to the wound. “His attention was completely fixed on that learning task,” he said.
Dr. Krauss reported having no financial disclosures.
NEW ORLEANS – Baruch S. Krauss, MD, EdM said at the annual meeting of the American Academy of Pediatrics.
Dr. Krauss, a pediatric emergency physician at Boston Children’s Hospital, shared tips for producing a positive experience when children present for minor procedures such as an intravenous catheter insertion or a laceration repair.
Control the environment
Setting the stage for a positive experience for children and their parents involves decreasing sensory stimuli by minimizing noise and bustle, the number of people in the room, and the reminder cues. “Even if you have trust with the child, there are certain things that could trigger the child to become fearful and anxious,” said Dr. Krauss, who also holds an academic post in the department of pediatrics at Harvard Medical School, Boston. “You want to make sure that medical equipment or a syringe is covered – anything that would remind the child or trigger the child to be more concerned and anxious.”
He recommends careful use of lighting, particularly in children who present with a head laceration or a facial laceration. “You may need to put a light near the wound, but that may be fearful for the child,” said Dr. Krauss, who coauthored a recent article on the topic that contains links to instructional videos (Ann Emerg Med 2019;74[1]:30-5). “Read the cues of the child,” he said. One desensitization technique he uses in such cases is to tell the child a story about the sun. He then goes on to liken the warmth of the exam light to the warmth of the sun.
Limiting the number of clinicians who speak to the child during the procedure also is key. “One person should speak to the child,” he advised. “Otherwise, it creates confusion for the child and it is hard for them to focus their attention. What you really want is to be able to control the child’s attention. You want to be able to capture their attention.”
It’s also important to keep medical equipment out of view. “I can’t tell you how many times I’ve seen consultants come in and a child needs to have a laceration repair, and they’re filling the syringe with lidocaine in front of the child,” Dr. Krauss said. “You want to avoid that. You also want to work outside of the child’s visual field if you can. Positioning is critical. I will try whatever position works for the child and the family.” This may including asking the parent to hold and swaddle an infant during the procedure, or positioning young children in the parent’s lap with their arm secured.
“Two things that upset kids during laceration repair are water dripping into their eyes during irrigation and the suture falling across their face as you’re stitching,” he added. “You want to develop your procedural skills so you can avoid that happening.”
Tailor the approach to the individual child
Some children will want to watch what you’re doing, but normally Dr. Krauss uses towels or blankets to cover the area being worked on. “If the child is part of your practice and you know his temperament and coping style, that makes it a lot easier; you know how to approach him,” he said. “They can trust you but they still can be quite fearful.” Sometimes, the child is relaxed but the parent becomes anxious. That anxiety can be transmitted to child. “If I see that the parents are anxious, I work directly with the child, and not the parent,” he said. “There’s not much I can tell a parent verbally that’s going to change their anxiety or fear level. But, as soon I start moving the child’s emotional state from fear to trust, the parent senses that and they relax, and that gets transmitted back to the child.”
Use age-appropriate language
When treating infants and children, Dr. Krauss often uses “parentese,” a simplified way that parents use to talk to young children. “It’s clearer, simpler, more attention-maintaining, and has longer pauses,” he said. “That can be very comforting to children.” Content and phrasing become important in older children. “You want to avoid the nocebo effect,” he continued. “If you tell a child, ‘This is really going to sting or hurt,’ you’re tipping the scales toward them having that experience.”
In an article about behavioral approaches to anxiety and pain management for pediatric venous access, Lindsey L. Cohen, PhD, devised a list of suggested phrasing to use. For example, instead of saying “You will be fine; there is nothing to worry about,” ask, “What did you do in school today?” as a form of distraction. Instead of saying, “It will feel like a bee sting,” ask, “Tell me how it feels.” And instead of saying, “Don’t cry,” say, “That was hard; I am proud of you” (Pediatrics 2008;122[suppl 3]:S134-9).
In a more recent article, Dr. Krauss and colleagues discussed current concepts of managing pain in children who present to the emergency department (Lancet 2016;387:83-92). Among distracting activities to try with infants and preschoolers are blowing bubbles, the use of a lighted wand, sound, music, or books, they noted. Distracting activities to try with preschoolers and in older children include art activities such as drawing, coloring, and the use of play dough, and computer games.
Clinicians also can ask the child to engage in a developmental task as a form of distraction. Dr. Krauss recalled a 22-month-old boy who presented to the emergency department with a forehead laceration. Mindful that the boy was developing eye-hand coordination and fine motor activity, Dr. Krauss offered him a coloring book that contained a picture of a clown, and instructed him to color the clown’s eyes red while Dr. Krauss tended to the wound. “His attention was completely fixed on that learning task,” he said.
Dr. Krauss reported having no financial disclosures.
NEW ORLEANS – Baruch S. Krauss, MD, EdM said at the annual meeting of the American Academy of Pediatrics.
Dr. Krauss, a pediatric emergency physician at Boston Children’s Hospital, shared tips for producing a positive experience when children present for minor procedures such as an intravenous catheter insertion or a laceration repair.
Control the environment
Setting the stage for a positive experience for children and their parents involves decreasing sensory stimuli by minimizing noise and bustle, the number of people in the room, and the reminder cues. “Even if you have trust with the child, there are certain things that could trigger the child to become fearful and anxious,” said Dr. Krauss, who also holds an academic post in the department of pediatrics at Harvard Medical School, Boston. “You want to make sure that medical equipment or a syringe is covered – anything that would remind the child or trigger the child to be more concerned and anxious.”
He recommends careful use of lighting, particularly in children who present with a head laceration or a facial laceration. “You may need to put a light near the wound, but that may be fearful for the child,” said Dr. Krauss, who coauthored a recent article on the topic that contains links to instructional videos (Ann Emerg Med 2019;74[1]:30-5). “Read the cues of the child,” he said. One desensitization technique he uses in such cases is to tell the child a story about the sun. He then goes on to liken the warmth of the exam light to the warmth of the sun.
Limiting the number of clinicians who speak to the child during the procedure also is key. “One person should speak to the child,” he advised. “Otherwise, it creates confusion for the child and it is hard for them to focus their attention. What you really want is to be able to control the child’s attention. You want to be able to capture their attention.”
It’s also important to keep medical equipment out of view. “I can’t tell you how many times I’ve seen consultants come in and a child needs to have a laceration repair, and they’re filling the syringe with lidocaine in front of the child,” Dr. Krauss said. “You want to avoid that. You also want to work outside of the child’s visual field if you can. Positioning is critical. I will try whatever position works for the child and the family.” This may including asking the parent to hold and swaddle an infant during the procedure, or positioning young children in the parent’s lap with their arm secured.
“Two things that upset kids during laceration repair are water dripping into their eyes during irrigation and the suture falling across their face as you’re stitching,” he added. “You want to develop your procedural skills so you can avoid that happening.”
Tailor the approach to the individual child
Some children will want to watch what you’re doing, but normally Dr. Krauss uses towels or blankets to cover the area being worked on. “If the child is part of your practice and you know his temperament and coping style, that makes it a lot easier; you know how to approach him,” he said. “They can trust you but they still can be quite fearful.” Sometimes, the child is relaxed but the parent becomes anxious. That anxiety can be transmitted to child. “If I see that the parents are anxious, I work directly with the child, and not the parent,” he said. “There’s not much I can tell a parent verbally that’s going to change their anxiety or fear level. But, as soon I start moving the child’s emotional state from fear to trust, the parent senses that and they relax, and that gets transmitted back to the child.”
Use age-appropriate language
When treating infants and children, Dr. Krauss often uses “parentese,” a simplified way that parents use to talk to young children. “It’s clearer, simpler, more attention-maintaining, and has longer pauses,” he said. “That can be very comforting to children.” Content and phrasing become important in older children. “You want to avoid the nocebo effect,” he continued. “If you tell a child, ‘This is really going to sting or hurt,’ you’re tipping the scales toward them having that experience.”
In an article about behavioral approaches to anxiety and pain management for pediatric venous access, Lindsey L. Cohen, PhD, devised a list of suggested phrasing to use. For example, instead of saying “You will be fine; there is nothing to worry about,” ask, “What did you do in school today?” as a form of distraction. Instead of saying, “It will feel like a bee sting,” ask, “Tell me how it feels.” And instead of saying, “Don’t cry,” say, “That was hard; I am proud of you” (Pediatrics 2008;122[suppl 3]:S134-9).
In a more recent article, Dr. Krauss and colleagues discussed current concepts of managing pain in children who present to the emergency department (Lancet 2016;387:83-92). Among distracting activities to try with infants and preschoolers are blowing bubbles, the use of a lighted wand, sound, music, or books, they noted. Distracting activities to try with preschoolers and in older children include art activities such as drawing, coloring, and the use of play dough, and computer games.
Clinicians also can ask the child to engage in a developmental task as a form of distraction. Dr. Krauss recalled a 22-month-old boy who presented to the emergency department with a forehead laceration. Mindful that the boy was developing eye-hand coordination and fine motor activity, Dr. Krauss offered him a coloring book that contained a picture of a clown, and instructed him to color the clown’s eyes red while Dr. Krauss tended to the wound. “His attention was completely fixed on that learning task,” he said.
Dr. Krauss reported having no financial disclosures.
EXPERT ANALYSIS AT AAP 19
Inexperience is the main cause of unsafe driving among teens
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
NEW ORLEANS – Teens need to drive for a wide range of reasons, from going to and from school or work to overall mobility, but driving still is the most dangerous thing teenagers do, according to Brian Johnston, MD, MPH, professor of pediatrics at the University of Washington in Seattle.
Motor vehicle traffic accidents continue to be the leading cause of death of adolescents aged 15-19 years, according to 2017 data from the National Center for Health Statistics at the Centers for the Disease Control and Prevention.
“Inexperience drives the statistics we see,” Dr. Johnston said at the annual meeting of the American Academy of Pediatrics. “There is a steep learning curve among drivers of all ages, and crash rates are highest during the first few months after teens begin driving without supervision.”
Although the risk of accidents is higher than average for any new driver, it’s disproportionately higher for younger teens, compared with other ages: 16-year-old novice drivers have a higher accident risk than that of 17-year-olds, whose risk is similar to that of 18- and 19-year-old novices.
How long drivers have been licensed has a far bigger impact on crash risk, Dr. Johnston said (Traffic Inj. Prev. 2009 Jun;10[3]:209-19).
But the risk of an accident also increases with each additional passenger a teen driver has, particularly for younger and male drivers (Traffic Inj Prev. 2013;14[3]:283-92). More passengers likely means more distraction, and distraction, driving too fast for road conditions, and not scanning the roadway are the three most common errors – together accounting for about half of all teen drivers’ crashes.
Risk factors for accidents
Speed is a contributing factor in just over a third (36%) of teens’ fatal crashes. Adolescents drive faster and keep shorter following distances than adults do. But as with adults, wearing seat belts substantially reduces the risk of death in accidents.
Nationally, 90% of drivers use seat belts, with higher rates in states with primary enforcement (92%) than those in states with secondary enforcement (83%).
But barely more than half (54%) of U.S. high school students say they “always” wear a seat belt, and just under half of teens (47%) who died in crashes in 2017 weren’t wearing one. As seen in adults, teens are more likely to buckle up, by 12%, in states with primary seat belt laws.
Distraction during driving can be visual, manual, or cognitive – and handheld electronic devices such as smartphones cause all three distraction types. Cell phones nearly double the proportion of teen drivers who die in crashes, from 7% to 13%.
But if teens can keep their eyes on the roadway at all times, even the risks posed by cellphones drop considerably.
“The best evidence shows that secondary tasks only degrade driving performance when they require drivers to look away from the road,” Dr. Johnston said. Looking away for 2 seconds or longer increases crash risk more than fivefold.
Two other risk factors for teen car accidents are drowsiness and nighttime driving. Sleepiness can play a role in crashes at any time of day, and Dr. Johnston noted that some research has associated later high school start times with reduced crash risk.
Teens aged 16-19 years are about four times more likely to have a car accident at night than during the day per each mile driven, the pediatrician noted. Many licensing laws restrict teen driving starting at 11 p.m. or later, but about 50%-60% of their crashes occur between 9 and 11 p.m.
One reason for the increased risk is less experience driving in more difficult conditions, but teens also are more likely to have teen passengers, to be driving excessively fast, or to be under the influence of alcohol at night.
Adolescents’ crash risk is higher than that of adults for any level of blood alcohol content. Self-reported driving after drinking dropped by almost half – from 10% to 5.5% – from 2013 to 2017, but alcohol still is implicated in a substantial number of fatal teen crashes.
As drunk driving has declined, however, driving while under the influence of marijuana has been increasing. According to the National Highway Traffic Safety Administration, case control studies show drivers with tetrahydrocannabinol (THC) in their blood have a 25% increased risk of accidents – but the excess risk associated with THC vanishes when researchers control for age, sex, and concurrent use of alcohol. Not enough research exists to determine what the crash risk would be for adolescent drivers using THC alone.
A less-recognized risk factor for car accidents in teen drivers is ADHD, which increases a teen’s risk of crashing by 36%, particularly in the first month after getting a license, Dr. Johnston said.
ADHD medication appears to mitigate the danger, according to data: Crash risk was 40% lower in adult drivers with ADHD during months they filled their stimulant prescriptions. But one study found only 12% of teens with ADHD filled their prescriptions the month they got their license, and adolescents may not take their medications or still have them in their system on weekends or at night.
Teens recovering from concussion also may have an increased risk. Some evidence suggests driving impairment continues even when other symptoms have resolved, but not enough data exist to determine appropriate criteria for clearing teens to begin driving again.
Interventions to improve teens’ driving safety
Most teens take a basic driver education course before getting their licenses, but no evidence shows that it reduces risk of citations, crashes, or injury. In fact, “skid control training and other kinds of advanced skill training seem to increase crash risk, particularly among young males,” Dr. Johnston said.
What helps teens most is, ironically, more driving.
“If I say inexperience is the single most important risk factor for dying in a crash as a teen, driving experience is the intervention,” he said. More time spent driving – “with supervision in particular, and under diverse conditions,” Dr. Johnston said – increases the repertoire of skills and abilities.
Parents should be encouraged to ride along as their teens drive under diverse road conditions: different roads, different times of the day, and different weather conditions, for example. Parents can narrate their own driving, pointing out hazards and times when they slow down for increased caution, Dr. Johnston said. It might feel “awkward and unnatural,” but “some of the things you as a driver notice all the time are novel to teen drivers.”
Parents can influence road safety for teens in terms of their own behavior and in selecting a safer vehicle. A strong correlation exists between parental texting while driving when children are younger and what they do as teen drivers, for example.
Safer vehicles are bigger, heavier cars with electronic stability control, which reduces risk of death about as much as wearing seat belts. Parents should avoid vehicles with high horsepower and look for cars with the best safety ratings they can afford, Dr. Johnston said.
Several special features in newer cars can help reduce crash risk, such as blind spot detection, automatic breaking, collision avoidance systems, lane departure warning systems, and driver drowsiness detection. Parents may worry that relying on this technology could reduce teens’ learning, but it actually can compensate for skill deficits as they are becoming more skilled drivers.
Parents can look into feedback programs such as smartphone apps or other in-car units that allow parents to see data on teens’ speed, unsafe driving, “near-misses,” and similar driving behaviors. Research has shown that unsafe driving in newly licensed teens dropped by 66% over 4 months of using one of these feedback programs, compared with teens who didn’t use it.
Dr. Johnston also discussed the idea of prelicensure medical exams, similar to physicals that are required before playing sports. These already exist for commercial licenses in most states, but no data exist on whether it’s effective for teens. The goal would be to promote a discussion between parents and their teens about driving: reviewing medications the teen is taking and whether they affect driving; discussing safety of different vehicles; and assessing the teens’ risks, including any cognitive or other medical conditions that could affect driving safety. Even if such a “driving physical” is not currently required, pediatricians can do their own version of one with families.
Dr. Johnston had no disclosures.
Football for the young
A few weeks ago I was at a Friday-night football game, but not to watch the game. I’ve been there and done that too many times when I used to be the team physician. I was there to listen to my granddaughter drumming in the pep band. And there was a lot of drumming because her high school’s team is having a hot year and outscoring opponents by three and four touchdowns every week.
At half time, the field was swarmed by 45-50 early grade schoolers looking like bobblehead dolls in their oversize helmets and surprisingly professional-appearing miniature football outfits. Under the lights, on the local college’s turf field, they were in football heaven. The pep band got into it and there was more drumming as the few kids who had a clue what football was about were scampering over and around their teammates and opponents who were roughhousing with each other, rolling around on the turf having a grand time, blissfully unimpressed by such trivial concepts as the line of scrimmage or the difference between blocking and tackling or even offense and defense.
Despite all the alarming articles both lay and professional that you and I see, this was an evening on which no one seemed particularly concerned about sports-related concussions. This is class B football in Maine, not a state well known as an incubator of Division I college football players. While there were a few scrawny kids with some speed,
Watching 4- and 5-year-olds in their football uniforms seemed to me to be a rather harmless exercise and certainly a more positive investment in their time on a Friday night than sitting on the couch with an electronic device clutched in their little hands. A recent report in JAMA Pediatrics suggests that my lack of concern has some validity (“Consensus statement on sports-related concussions in youth sports using a modified delphi approach.” JAMA Pediatr. 2019 Nov 11. doi: 10.1001/jamapediatrics.2019.4006). Eleven experts in sports-related injuries were surveyed with multiple rounds of questionnaires. Their anonymous responses were aggregated and shared with the group after each round until a consensus could be arrived on for each of seven broad questions about sports-related concussions. It is a paper worth reading and like most good literature surveys determined that in many situations more study needs to be done.
Among the many findings that impressed me was the group’s failure to find an “association between repetitive head impact exposure in youth and long-term neurocognitive outcomes.” In addition, “there is little evidence that age at first exposure repetitive head impacts in sports is independently associated with neurodegenerative changes.” The experts also could find “no evidence that growth or development affect the risk of sports-related concussions.”
The problem with youth football is that it is the portal that can lead to college and professional football, in which large bodies are allowed to collide after accelerating at speeds we mortals only can achieve behind the wheel of our motor vehicles. Rules to minimize those collisions do exist, but lax enforcement has failed to prevent their cumulative damage.
Whether the culture of big-time football is going to change to a point at which a conscientious parent could encourage his or her child to play after adolescence remains to be seen. However, the evidence seems to suggest that allowing young children to bang themselves around imitating the big guys seems to be reasonably safe. At least as safe as what kids used to do to each other before we adults invented television and video games.
When my son was 3 or 4 years old, he played on a hockey team he thought was called the Toronto Make-Believes (Maple Leafs). Maybe we should be telling parents it’s safe for their children to play make-believe contact sports. The challenge comes after those kids reach puberty and want to start playing the real thing.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I was at a Friday-night football game, but not to watch the game. I’ve been there and done that too many times when I used to be the team physician. I was there to listen to my granddaughter drumming in the pep band. And there was a lot of drumming because her high school’s team is having a hot year and outscoring opponents by three and four touchdowns every week.
At half time, the field was swarmed by 45-50 early grade schoolers looking like bobblehead dolls in their oversize helmets and surprisingly professional-appearing miniature football outfits. Under the lights, on the local college’s turf field, they were in football heaven. The pep band got into it and there was more drumming as the few kids who had a clue what football was about were scampering over and around their teammates and opponents who were roughhousing with each other, rolling around on the turf having a grand time, blissfully unimpressed by such trivial concepts as the line of scrimmage or the difference between blocking and tackling or even offense and defense.
Despite all the alarming articles both lay and professional that you and I see, this was an evening on which no one seemed particularly concerned about sports-related concussions. This is class B football in Maine, not a state well known as an incubator of Division I college football players. While there were a few scrawny kids with some speed,
Watching 4- and 5-year-olds in their football uniforms seemed to me to be a rather harmless exercise and certainly a more positive investment in their time on a Friday night than sitting on the couch with an electronic device clutched in their little hands. A recent report in JAMA Pediatrics suggests that my lack of concern has some validity (“Consensus statement on sports-related concussions in youth sports using a modified delphi approach.” JAMA Pediatr. 2019 Nov 11. doi: 10.1001/jamapediatrics.2019.4006). Eleven experts in sports-related injuries were surveyed with multiple rounds of questionnaires. Their anonymous responses were aggregated and shared with the group after each round until a consensus could be arrived on for each of seven broad questions about sports-related concussions. It is a paper worth reading and like most good literature surveys determined that in many situations more study needs to be done.
Among the many findings that impressed me was the group’s failure to find an “association between repetitive head impact exposure in youth and long-term neurocognitive outcomes.” In addition, “there is little evidence that age at first exposure repetitive head impacts in sports is independently associated with neurodegenerative changes.” The experts also could find “no evidence that growth or development affect the risk of sports-related concussions.”
The problem with youth football is that it is the portal that can lead to college and professional football, in which large bodies are allowed to collide after accelerating at speeds we mortals only can achieve behind the wheel of our motor vehicles. Rules to minimize those collisions do exist, but lax enforcement has failed to prevent their cumulative damage.
Whether the culture of big-time football is going to change to a point at which a conscientious parent could encourage his or her child to play after adolescence remains to be seen. However, the evidence seems to suggest that allowing young children to bang themselves around imitating the big guys seems to be reasonably safe. At least as safe as what kids used to do to each other before we adults invented television and video games.
When my son was 3 or 4 years old, he played on a hockey team he thought was called the Toronto Make-Believes (Maple Leafs). Maybe we should be telling parents it’s safe for their children to play make-believe contact sports. The challenge comes after those kids reach puberty and want to start playing the real thing.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I was at a Friday-night football game, but not to watch the game. I’ve been there and done that too many times when I used to be the team physician. I was there to listen to my granddaughter drumming in the pep band. And there was a lot of drumming because her high school’s team is having a hot year and outscoring opponents by three and four touchdowns every week.
At half time, the field was swarmed by 45-50 early grade schoolers looking like bobblehead dolls in their oversize helmets and surprisingly professional-appearing miniature football outfits. Under the lights, on the local college’s turf field, they were in football heaven. The pep band got into it and there was more drumming as the few kids who had a clue what football was about were scampering over and around their teammates and opponents who were roughhousing with each other, rolling around on the turf having a grand time, blissfully unimpressed by such trivial concepts as the line of scrimmage or the difference between blocking and tackling or even offense and defense.
Despite all the alarming articles both lay and professional that you and I see, this was an evening on which no one seemed particularly concerned about sports-related concussions. This is class B football in Maine, not a state well known as an incubator of Division I college football players. While there were a few scrawny kids with some speed,
Watching 4- and 5-year-olds in their football uniforms seemed to me to be a rather harmless exercise and certainly a more positive investment in their time on a Friday night than sitting on the couch with an electronic device clutched in their little hands. A recent report in JAMA Pediatrics suggests that my lack of concern has some validity (“Consensus statement on sports-related concussions in youth sports using a modified delphi approach.” JAMA Pediatr. 2019 Nov 11. doi: 10.1001/jamapediatrics.2019.4006). Eleven experts in sports-related injuries were surveyed with multiple rounds of questionnaires. Their anonymous responses were aggregated and shared with the group after each round until a consensus could be arrived on for each of seven broad questions about sports-related concussions. It is a paper worth reading and like most good literature surveys determined that in many situations more study needs to be done.
Among the many findings that impressed me was the group’s failure to find an “association between repetitive head impact exposure in youth and long-term neurocognitive outcomes.” In addition, “there is little evidence that age at first exposure repetitive head impacts in sports is independently associated with neurodegenerative changes.” The experts also could find “no evidence that growth or development affect the risk of sports-related concussions.”
The problem with youth football is that it is the portal that can lead to college and professional football, in which large bodies are allowed to collide after accelerating at speeds we mortals only can achieve behind the wheel of our motor vehicles. Rules to minimize those collisions do exist, but lax enforcement has failed to prevent their cumulative damage.
Whether the culture of big-time football is going to change to a point at which a conscientious parent could encourage his or her child to play after adolescence remains to be seen. However, the evidence seems to suggest that allowing young children to bang themselves around imitating the big guys seems to be reasonably safe. At least as safe as what kids used to do to each other before we adults invented television and video games.
When my son was 3 or 4 years old, he played on a hockey team he thought was called the Toronto Make-Believes (Maple Leafs). Maybe we should be telling parents it’s safe for their children to play make-believe contact sports. The challenge comes after those kids reach puberty and want to start playing the real thing.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Urban or rural, children’s gun-related injuries equally deadly
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
AT AAP 2019
Suicide deaths rising in children aged 10-19 years
according to the National Center for Health Statistics.
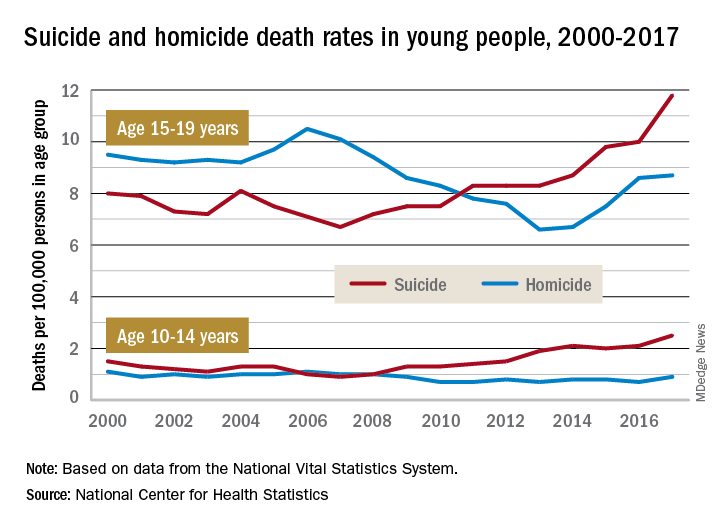
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.
according to the National Center for Health Statistics.
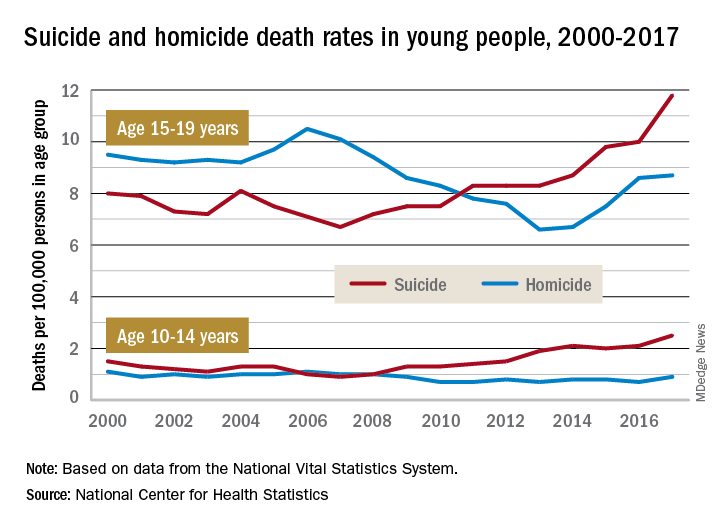
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.
according to the National Center for Health Statistics.
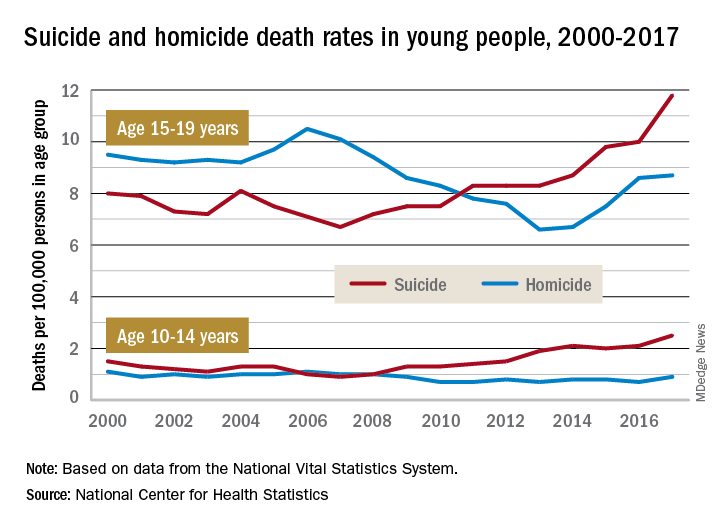
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.
Research on pediatric firearms deaths is underfunded
new research has found.
For the period 2008-2017, an average of $88 million per year was granted to study motor vehicle crashes, the leading cause of death in this age group. Cancer, the third leading cause of mortality, received on average $335 million per year. However, research into mortality from firearms, the second leading cause of death in this age group, received $12 million total during the entire research period across a total of 32 research grants.
This translates to $26,136 in research funding per death for the 33,577 deaths of children and adolescents in motor vehicle crashes from 2008-2017, $195,508 per death from cancer (17,111 deaths recorded), and just $597 per death from firearm injury (20,719 deaths recorded).
Pediatric firearm injury prevention “is substantially underfunded in relation to the magnitude of the public health problem,” Rebecca Cunningham, MD, from the University of Michigan, Ann Arbor, and colleagues wrote in the October 2019 issue of Health Affairs.
“According to our analysis, federal funding for this leading cause of pediatric mortality is 3.3 percent of what would be needed for it to be commensurate with the funding for other common causes of pediatric death,” the authors continued.
Dr. Cunningham and colleagues said that the “lack of an evidence base for firearm safety prevention has likely contributed to the lack of progress on, and recent increase in, firearm deaths among children and adolescents since 2013.”
They did note that there was an increase in federal research funding following the shooting in Newtown, Conn., with an increase from $136,224 in 2012 to $4.5 million in 2017, but it clearly is not enough.
“Our analysis, using other major diseases and the country’s history of federal funding as a guide, demonstrates that approximately $37 million per year over the next decade is needed to realize a reduction in pediatric firearm mortality that is comparable to that observed for other pediatric causes of death,” the authors state.
The group also suggests the development of a group similar to the National Highway Traffic Safety Administration that is focused specifically on firearm safety that could “begin to address the large gaps in foundational epidemiological and multidisciplinary behavioral research that the nation needs. It could have a transformational impact on the reduction of firearm injuries among children and adolescents parallel to what has been seen for other major causes of pediatric death in the U.S.”
SOURCE: Cunningham R et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00476.
new research has found.
For the period 2008-2017, an average of $88 million per year was granted to study motor vehicle crashes, the leading cause of death in this age group. Cancer, the third leading cause of mortality, received on average $335 million per year. However, research into mortality from firearms, the second leading cause of death in this age group, received $12 million total during the entire research period across a total of 32 research grants.
This translates to $26,136 in research funding per death for the 33,577 deaths of children and adolescents in motor vehicle crashes from 2008-2017, $195,508 per death from cancer (17,111 deaths recorded), and just $597 per death from firearm injury (20,719 deaths recorded).
Pediatric firearm injury prevention “is substantially underfunded in relation to the magnitude of the public health problem,” Rebecca Cunningham, MD, from the University of Michigan, Ann Arbor, and colleagues wrote in the October 2019 issue of Health Affairs.
“According to our analysis, federal funding for this leading cause of pediatric mortality is 3.3 percent of what would be needed for it to be commensurate with the funding for other common causes of pediatric death,” the authors continued.
Dr. Cunningham and colleagues said that the “lack of an evidence base for firearm safety prevention has likely contributed to the lack of progress on, and recent increase in, firearm deaths among children and adolescents since 2013.”
They did note that there was an increase in federal research funding following the shooting in Newtown, Conn., with an increase from $136,224 in 2012 to $4.5 million in 2017, but it clearly is not enough.
“Our analysis, using other major diseases and the country’s history of federal funding as a guide, demonstrates that approximately $37 million per year over the next decade is needed to realize a reduction in pediatric firearm mortality that is comparable to that observed for other pediatric causes of death,” the authors state.
The group also suggests the development of a group similar to the National Highway Traffic Safety Administration that is focused specifically on firearm safety that could “begin to address the large gaps in foundational epidemiological and multidisciplinary behavioral research that the nation needs. It could have a transformational impact on the reduction of firearm injuries among children and adolescents parallel to what has been seen for other major causes of pediatric death in the U.S.”
SOURCE: Cunningham R et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00476.
new research has found.
For the period 2008-2017, an average of $88 million per year was granted to study motor vehicle crashes, the leading cause of death in this age group. Cancer, the third leading cause of mortality, received on average $335 million per year. However, research into mortality from firearms, the second leading cause of death in this age group, received $12 million total during the entire research period across a total of 32 research grants.
This translates to $26,136 in research funding per death for the 33,577 deaths of children and adolescents in motor vehicle crashes from 2008-2017, $195,508 per death from cancer (17,111 deaths recorded), and just $597 per death from firearm injury (20,719 deaths recorded).
Pediatric firearm injury prevention “is substantially underfunded in relation to the magnitude of the public health problem,” Rebecca Cunningham, MD, from the University of Michigan, Ann Arbor, and colleagues wrote in the October 2019 issue of Health Affairs.
“According to our analysis, federal funding for this leading cause of pediatric mortality is 3.3 percent of what would be needed for it to be commensurate with the funding for other common causes of pediatric death,” the authors continued.
Dr. Cunningham and colleagues said that the “lack of an evidence base for firearm safety prevention has likely contributed to the lack of progress on, and recent increase in, firearm deaths among children and adolescents since 2013.”
They did note that there was an increase in federal research funding following the shooting in Newtown, Conn., with an increase from $136,224 in 2012 to $4.5 million in 2017, but it clearly is not enough.
“Our analysis, using other major diseases and the country’s history of federal funding as a guide, demonstrates that approximately $37 million per year over the next decade is needed to realize a reduction in pediatric firearm mortality that is comparable to that observed for other pediatric causes of death,” the authors state.
The group also suggests the development of a group similar to the National Highway Traffic Safety Administration that is focused specifically on firearm safety that could “begin to address the large gaps in foundational epidemiological and multidisciplinary behavioral research that the nation needs. It could have a transformational impact on the reduction of firearm injuries among children and adolescents parallel to what has been seen for other major causes of pediatric death in the U.S.”
SOURCE: Cunningham R et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00476.
FROM HEALTH AFFAIRS
Firearm-related deaths show recent increase
After years of relative stability, firearm-related mortality in the United States rose sharply starting in 2015, according to analysis of a national mortality database.

U.S. firearm mortality was 10.4 per 100,000 person-years during 1999-2014, with the high in that period occurring in 2012 and dropping each of the next 2 years – compared with 11.8 per 100,000 during 2015-2017, an increase of 13.8%, Jason E. Goldstick, PhD, and associates wrote Oct. 8 in Health Affairs.
The majority of the 612,310 firearm deaths over the entire study period were suicides, with the proportion rising slightly from 58.6% in 1999-2014 to 60.0% in 2015-2017. Homicides made up 38.5% of deaths in 1999-2014 and 37.9% in 2015-2017, while the combined share of unintentional and undetermined deaths dropped from 2.9% to 2.1%, the investigators reported.
Dr. Goldstick of the University of Michigan, Ann Arbor, said in a separate written statement.
The geographic broadness can be seen when the change in mortality from 1999-2014 to 2015-2017 was calculated for each locale: 29 states had an increase of more than 20% and only 3 states (California, New York, and Rhode Island) and the District of Columbia had a decrease of at least 12.5%, they said. The data came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research tool.
The different trends among states and subpopulations make it difficult to offer policy-based interventions. “The epidemiology of firearm violence is complex and varies based on the mechanism of death, demographic group under study, and regionally specific culture, making a one-size-fits-all solution inappropriate,” Dr. Goldstick and associates wrote.
The study was funded mainly by a grant from the National Institute of Child Health and Human Development. The investigators did not provide any information on conflicts of interest.
SOURCE: Goldstick JE et al. Health Aff. 2019;38(10):1646-52.
After years of relative stability, firearm-related mortality in the United States rose sharply starting in 2015, according to analysis of a national mortality database.

U.S. firearm mortality was 10.4 per 100,000 person-years during 1999-2014, with the high in that period occurring in 2012 and dropping each of the next 2 years – compared with 11.8 per 100,000 during 2015-2017, an increase of 13.8%, Jason E. Goldstick, PhD, and associates wrote Oct. 8 in Health Affairs.
The majority of the 612,310 firearm deaths over the entire study period were suicides, with the proportion rising slightly from 58.6% in 1999-2014 to 60.0% in 2015-2017. Homicides made up 38.5% of deaths in 1999-2014 and 37.9% in 2015-2017, while the combined share of unintentional and undetermined deaths dropped from 2.9% to 2.1%, the investigators reported.
Dr. Goldstick of the University of Michigan, Ann Arbor, said in a separate written statement.
The geographic broadness can be seen when the change in mortality from 1999-2014 to 2015-2017 was calculated for each locale: 29 states had an increase of more than 20% and only 3 states (California, New York, and Rhode Island) and the District of Columbia had a decrease of at least 12.5%, they said. The data came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research tool.
The different trends among states and subpopulations make it difficult to offer policy-based interventions. “The epidemiology of firearm violence is complex and varies based on the mechanism of death, demographic group under study, and regionally specific culture, making a one-size-fits-all solution inappropriate,” Dr. Goldstick and associates wrote.
The study was funded mainly by a grant from the National Institute of Child Health and Human Development. The investigators did not provide any information on conflicts of interest.
SOURCE: Goldstick JE et al. Health Aff. 2019;38(10):1646-52.
After years of relative stability, firearm-related mortality in the United States rose sharply starting in 2015, according to analysis of a national mortality database.

U.S. firearm mortality was 10.4 per 100,000 person-years during 1999-2014, with the high in that period occurring in 2012 and dropping each of the next 2 years – compared with 11.8 per 100,000 during 2015-2017, an increase of 13.8%, Jason E. Goldstick, PhD, and associates wrote Oct. 8 in Health Affairs.
The majority of the 612,310 firearm deaths over the entire study period were suicides, with the proportion rising slightly from 58.6% in 1999-2014 to 60.0% in 2015-2017. Homicides made up 38.5% of deaths in 1999-2014 and 37.9% in 2015-2017, while the combined share of unintentional and undetermined deaths dropped from 2.9% to 2.1%, the investigators reported.
Dr. Goldstick of the University of Michigan, Ann Arbor, said in a separate written statement.
The geographic broadness can be seen when the change in mortality from 1999-2014 to 2015-2017 was calculated for each locale: 29 states had an increase of more than 20% and only 3 states (California, New York, and Rhode Island) and the District of Columbia had a decrease of at least 12.5%, they said. The data came from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research tool.
The different trends among states and subpopulations make it difficult to offer policy-based interventions. “The epidemiology of firearm violence is complex and varies based on the mechanism of death, demographic group under study, and regionally specific culture, making a one-size-fits-all solution inappropriate,” Dr. Goldstick and associates wrote.
The study was funded mainly by a grant from the National Institute of Child Health and Human Development. The investigators did not provide any information on conflicts of interest.
SOURCE: Goldstick JE et al. Health Aff. 2019;38(10):1646-52.
FROM HEALTH AFFAIRS