User login
Phase 2 data: Inotuzumab, approved in adults with B-ALL, shows promise in kids, too
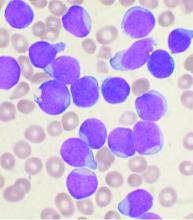
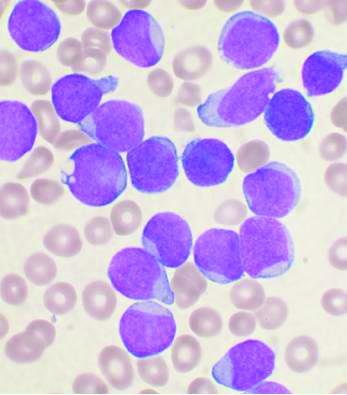
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
REPORTING FROM ASH 2019
FDA: Cell phones still look safe
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
according to a review by the Food and Drug Administration.
The FDA reviewed the published literature from 2008 to 2018 and concluded that the data don’t support any quantifiable adverse health risks from RFR. However, the evidence is not without limitations.
The FDA’s evaluation included evidence from in vivo animal studies from Jan. 1, 2008, to Aug. 1, 2018, and epidemiologic studies in humans from Jan. 1, 2008, to May 8, 2018. Both kinds of evidence had limitations, but neither produced strong indications of any causal risks from cell phone use.
The FDA noted that in vivo animal studies are limited by variability of methods and RFR exposure, which make comparisons of results difficult. These studies are also impacted by the indirect effects of temperature increases (the only currently established biological effect of RFR) and stress experienced by the animals, which make teasing out the direct effects of RFR difficult.
The FDA noted that strong epidemiologic studies can provide more relevant and accurate information than in vivo studies, but epidemiologic studies are not without limitations. For example, most have participants track and self-report their cell phone use. There’s also no way to directly track certain factors of RFR exposure, such as frequency, duration, or intensity.
Even with those caveats in mind, the FDA wrote that, “based on the studies that are described in detail in this report, there is insufficient evidence to support a causal association between RFR exposure and tumorigenesis. There is a lack of clear dose-response relationship, a lack of consistent findings or specificity, and a lack of biological mechanistic plausibility.”
The full review is available on the FDA website.
Survival for older AML patients better with HSCT from unrelated donors
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
FROM HAEMATOLOGICA
Global project reveals cancer’s genomic playbook
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
FROM NATURE
Novel mutations contribute to progression of venetoclax-treated CLL
Newly discovered gene mutations in the progression of venetoclax-treated relapsed chronic lymphocytic leukemia (CLL) may improve understanding of clinical resistance mechanisms underlying the disease, according to recent research.
“We investigated patients with progressive CLL on venetoclax harboring subclonal BCL2 Gly101Val mutations for the presence of additional acquired BCL2 resistance mutations,” wrote Piers Blombery, MBBS, of the University of Melbourne in Victoria, Australia, and his colleagues in Blood.
Among 67 patients with relapsed disease treated with the BCL2 inhibitor venetoclax, the researchers identified a total of 11 patients with co-occurring BCL2 Gly101Val mutations. Each patient was enrolled in an early phase clinical trial at an institution in Australia.
With respect to testing methods, next-generation sequencing (NGS) and hybridization-based target enrichment technologies were used to detect novel acquired mutations in the BCL2 coding region.
Among those harboring the Gly101Val mutation, additional BCL2 mutations were identified in 10 patients (91%), with a median of three mutations detected per patient (range, 1-7). Previously undescribed mutations included an in-frame insertion mutation (Arg107_Arg110dup), and other substitutions (Asp103/Val156) in the BCL2 gene.
“As with the Gly101Val, these observations support the specificity of these mutations for the context of venetoclax resistance,” they wrote.
The investigators further explained that the BCL2 Asp103Glu mutation could have particular significance in the context of venetoclax sensitivity because of selective targeting of the BCL2 gene.
In comparison to wild-type aspartic acid, the BCL2 Asp103Glu substitution was linked to an approximate 20-fold reduction in affinity for venetoclax, they reported.
“[Our findings] consolidate the paradigm emerging across hematological malignancies of multiple independent molecular mechanisms underpinning an ‘oligoclonal’ pattern of clinical relapse on targeted therapies,” they concluded.
Further studies are needed to fully characterize the relationship between acquired BCL2 mutations and venetoclax resistance.
The study was funded by the Snowdome Foundation, Vision Super and the Wilson Centre for Lymphoma Genomics, the Leukemia and Lymphoma Society, the National Health and Medical Research Council of Australia, and other grant funding sources provided to the study authors. The authors reported financial affiliations with AbbVie, Genentech, and the Walter and Eliza Hall Institute.
Newly discovered gene mutations in the progression of venetoclax-treated relapsed chronic lymphocytic leukemia (CLL) may improve understanding of clinical resistance mechanisms underlying the disease, according to recent research.
“We investigated patients with progressive CLL on venetoclax harboring subclonal BCL2 Gly101Val mutations for the presence of additional acquired BCL2 resistance mutations,” wrote Piers Blombery, MBBS, of the University of Melbourne in Victoria, Australia, and his colleagues in Blood.
Among 67 patients with relapsed disease treated with the BCL2 inhibitor venetoclax, the researchers identified a total of 11 patients with co-occurring BCL2 Gly101Val mutations. Each patient was enrolled in an early phase clinical trial at an institution in Australia.
With respect to testing methods, next-generation sequencing (NGS) and hybridization-based target enrichment technologies were used to detect novel acquired mutations in the BCL2 coding region.
Among those harboring the Gly101Val mutation, additional BCL2 mutations were identified in 10 patients (91%), with a median of three mutations detected per patient (range, 1-7). Previously undescribed mutations included an in-frame insertion mutation (Arg107_Arg110dup), and other substitutions (Asp103/Val156) in the BCL2 gene.
“As with the Gly101Val, these observations support the specificity of these mutations for the context of venetoclax resistance,” they wrote.
The investigators further explained that the BCL2 Asp103Glu mutation could have particular significance in the context of venetoclax sensitivity because of selective targeting of the BCL2 gene.
In comparison to wild-type aspartic acid, the BCL2 Asp103Glu substitution was linked to an approximate 20-fold reduction in affinity for venetoclax, they reported.
“[Our findings] consolidate the paradigm emerging across hematological malignancies of multiple independent molecular mechanisms underpinning an ‘oligoclonal’ pattern of clinical relapse on targeted therapies,” they concluded.
Further studies are needed to fully characterize the relationship between acquired BCL2 mutations and venetoclax resistance.
The study was funded by the Snowdome Foundation, Vision Super and the Wilson Centre for Lymphoma Genomics, the Leukemia and Lymphoma Society, the National Health and Medical Research Council of Australia, and other grant funding sources provided to the study authors. The authors reported financial affiliations with AbbVie, Genentech, and the Walter and Eliza Hall Institute.
Newly discovered gene mutations in the progression of venetoclax-treated relapsed chronic lymphocytic leukemia (CLL) may improve understanding of clinical resistance mechanisms underlying the disease, according to recent research.
“We investigated patients with progressive CLL on venetoclax harboring subclonal BCL2 Gly101Val mutations for the presence of additional acquired BCL2 resistance mutations,” wrote Piers Blombery, MBBS, of the University of Melbourne in Victoria, Australia, and his colleagues in Blood.
Among 67 patients with relapsed disease treated with the BCL2 inhibitor venetoclax, the researchers identified a total of 11 patients with co-occurring BCL2 Gly101Val mutations. Each patient was enrolled in an early phase clinical trial at an institution in Australia.
With respect to testing methods, next-generation sequencing (NGS) and hybridization-based target enrichment technologies were used to detect novel acquired mutations in the BCL2 coding region.
Among those harboring the Gly101Val mutation, additional BCL2 mutations were identified in 10 patients (91%), with a median of three mutations detected per patient (range, 1-7). Previously undescribed mutations included an in-frame insertion mutation (Arg107_Arg110dup), and other substitutions (Asp103/Val156) in the BCL2 gene.
“As with the Gly101Val, these observations support the specificity of these mutations for the context of venetoclax resistance,” they wrote.
The investigators further explained that the BCL2 Asp103Glu mutation could have particular significance in the context of venetoclax sensitivity because of selective targeting of the BCL2 gene.
In comparison to wild-type aspartic acid, the BCL2 Asp103Glu substitution was linked to an approximate 20-fold reduction in affinity for venetoclax, they reported.
“[Our findings] consolidate the paradigm emerging across hematological malignancies of multiple independent molecular mechanisms underpinning an ‘oligoclonal’ pattern of clinical relapse on targeted therapies,” they concluded.
Further studies are needed to fully characterize the relationship between acquired BCL2 mutations and venetoclax resistance.
The study was funded by the Snowdome Foundation, Vision Super and the Wilson Centre for Lymphoma Genomics, the Leukemia and Lymphoma Society, the National Health and Medical Research Council of Australia, and other grant funding sources provided to the study authors. The authors reported financial affiliations with AbbVie, Genentech, and the Walter and Eliza Hall Institute.
FROM BLOOD
Ofatumumab works safely for elderly patients with CLL, comorbidities
For elderly patients with chronic lymphocytic leukemia (CLL) and comorbidities, the anti-CD20 monoclonal antibody ofatumumab may be a safe and effective treatment option, according to a recent phase 2 trial.
Among 32 patients with a median age of 73 years, the overall response rate was 72%, and no grade 4 adverse events occurred, reported lead author Candida Vitale, MD, PhD, of the University of Torino (Italy) and colleagues.
These findings help fill in a knowledge gap created by clinical trial exclusions, which currently make treatment planning “a significant challenge,” the investigators wrote in Journal of Geriatric Oncology.
The study, which was conducted at MD Anderson Cancer Center in Houston, enrolled 34 treatment-naive patients with CLL who were 65 years or older. All patients had an Eastern Cooperative Oncology Group performance status of 2 or 3, or a Charlson comorbidity index of at least 2. Patients with other serious medical conditions and/or primary malignancies were eligible, given that they were not already receiving anticancer therapy.
More than half of the patients (53%) had advanced-stage disease and almost one-third (29%) had at least one other primary cancer diagnosis. Many patients also had high-risk disease characteristics, including a complex karyotype involving three or more chromosomal abnormalities (15%), and/or unmutated immunoglobulin heavy chain variable region (IGHV, 59%).
Among 32 patients eligible for efficacy analysis, the overall response rate was 72%, of which 53% were partial and 19% were complete. Six percent (6%) of patients achieved minimal residual disease negativity. The benefits of ofatumumab extended to patients with high-risk disease characteristics, including unmutated IGHV (65% response rate) and/or a complex karyotype (60% response rate).
Ofatumumab also demonstrated a favorable safety profile, according to the investigators.
With all 34 patients evaluable for safety data, 19 (56%) experienced a grade 1 or 2 infusion-related reaction, and 1 (3%) experienced a grade 3 infusion-related reaction. Twenty-one grade 2 infections were reported, and one grade 3 infection occurred. Other grade 3 treatment-related adverse events included gastrointestinal disturbances, pulmonary embolism, allergic reaction, and hyperglycemia, each of which occurred in one patient. No grade 4 adverse events, or grade 2 or higher hematologic toxicities occurred.
“Our findings show that older patients with poor performance status and comorbidities can safely undergo treatment with ofatumumab,” the investigators concluded. “[The results] also support the possibility of enrolling these patients in clinical trials, so that a larger number of patients will be included and their characteristics will more closely mirror those of typical patients seen in the community.”
The study was funded by Novartis, which markets the antibody. The investigators reported additional relationships with AbbVie, Roche, Celgene, and others.
SOURCE: Vitale et al. J Geriatr Oncol. 2019 Apr 18. doi: 10.1016/j.jgo.2019.04.002.
For elderly patients with chronic lymphocytic leukemia (CLL) and comorbidities, the anti-CD20 monoclonal antibody ofatumumab may be a safe and effective treatment option, according to a recent phase 2 trial.
Among 32 patients with a median age of 73 years, the overall response rate was 72%, and no grade 4 adverse events occurred, reported lead author Candida Vitale, MD, PhD, of the University of Torino (Italy) and colleagues.
These findings help fill in a knowledge gap created by clinical trial exclusions, which currently make treatment planning “a significant challenge,” the investigators wrote in Journal of Geriatric Oncology.
The study, which was conducted at MD Anderson Cancer Center in Houston, enrolled 34 treatment-naive patients with CLL who were 65 years or older. All patients had an Eastern Cooperative Oncology Group performance status of 2 or 3, or a Charlson comorbidity index of at least 2. Patients with other serious medical conditions and/or primary malignancies were eligible, given that they were not already receiving anticancer therapy.
More than half of the patients (53%) had advanced-stage disease and almost one-third (29%) had at least one other primary cancer diagnosis. Many patients also had high-risk disease characteristics, including a complex karyotype involving three or more chromosomal abnormalities (15%), and/or unmutated immunoglobulin heavy chain variable region (IGHV, 59%).
Among 32 patients eligible for efficacy analysis, the overall response rate was 72%, of which 53% were partial and 19% were complete. Six percent (6%) of patients achieved minimal residual disease negativity. The benefits of ofatumumab extended to patients with high-risk disease characteristics, including unmutated IGHV (65% response rate) and/or a complex karyotype (60% response rate).
Ofatumumab also demonstrated a favorable safety profile, according to the investigators.
With all 34 patients evaluable for safety data, 19 (56%) experienced a grade 1 or 2 infusion-related reaction, and 1 (3%) experienced a grade 3 infusion-related reaction. Twenty-one grade 2 infections were reported, and one grade 3 infection occurred. Other grade 3 treatment-related adverse events included gastrointestinal disturbances, pulmonary embolism, allergic reaction, and hyperglycemia, each of which occurred in one patient. No grade 4 adverse events, or grade 2 or higher hematologic toxicities occurred.
“Our findings show that older patients with poor performance status and comorbidities can safely undergo treatment with ofatumumab,” the investigators concluded. “[The results] also support the possibility of enrolling these patients in clinical trials, so that a larger number of patients will be included and their characteristics will more closely mirror those of typical patients seen in the community.”
The study was funded by Novartis, which markets the antibody. The investigators reported additional relationships with AbbVie, Roche, Celgene, and others.
SOURCE: Vitale et al. J Geriatr Oncol. 2019 Apr 18. doi: 10.1016/j.jgo.2019.04.002.
For elderly patients with chronic lymphocytic leukemia (CLL) and comorbidities, the anti-CD20 monoclonal antibody ofatumumab may be a safe and effective treatment option, according to a recent phase 2 trial.
Among 32 patients with a median age of 73 years, the overall response rate was 72%, and no grade 4 adverse events occurred, reported lead author Candida Vitale, MD, PhD, of the University of Torino (Italy) and colleagues.
These findings help fill in a knowledge gap created by clinical trial exclusions, which currently make treatment planning “a significant challenge,” the investigators wrote in Journal of Geriatric Oncology.
The study, which was conducted at MD Anderson Cancer Center in Houston, enrolled 34 treatment-naive patients with CLL who were 65 years or older. All patients had an Eastern Cooperative Oncology Group performance status of 2 or 3, or a Charlson comorbidity index of at least 2. Patients with other serious medical conditions and/or primary malignancies were eligible, given that they were not already receiving anticancer therapy.
More than half of the patients (53%) had advanced-stage disease and almost one-third (29%) had at least one other primary cancer diagnosis. Many patients also had high-risk disease characteristics, including a complex karyotype involving three or more chromosomal abnormalities (15%), and/or unmutated immunoglobulin heavy chain variable region (IGHV, 59%).
Among 32 patients eligible for efficacy analysis, the overall response rate was 72%, of which 53% were partial and 19% were complete. Six percent (6%) of patients achieved minimal residual disease negativity. The benefits of ofatumumab extended to patients with high-risk disease characteristics, including unmutated IGHV (65% response rate) and/or a complex karyotype (60% response rate).
Ofatumumab also demonstrated a favorable safety profile, according to the investigators.
With all 34 patients evaluable for safety data, 19 (56%) experienced a grade 1 or 2 infusion-related reaction, and 1 (3%) experienced a grade 3 infusion-related reaction. Twenty-one grade 2 infections were reported, and one grade 3 infection occurred. Other grade 3 treatment-related adverse events included gastrointestinal disturbances, pulmonary embolism, allergic reaction, and hyperglycemia, each of which occurred in one patient. No grade 4 adverse events, or grade 2 or higher hematologic toxicities occurred.
“Our findings show that older patients with poor performance status and comorbidities can safely undergo treatment with ofatumumab,” the investigators concluded. “[The results] also support the possibility of enrolling these patients in clinical trials, so that a larger number of patients will be included and their characteristics will more closely mirror those of typical patients seen in the community.”
The study was funded by Novartis, which markets the antibody. The investigators reported additional relationships with AbbVie, Roche, Celgene, and others.
SOURCE: Vitale et al. J Geriatr Oncol. 2019 Apr 18. doi: 10.1016/j.jgo.2019.04.002.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
CAR T-cell therapy may worsen mental health in some patients
Chimeric antigen receptor (CAR) T-cell therapy is generally associated with good long-term neuropsychiatric status, based on a recent patient-reported outcomes study.
But almost one out of five patients may have notably worse cognitive and psychiatric outcomes within 1-5 years of therapy, reported Julia Ruark, MD, of the University of Washington, Seattle, and colleagues. According to Dr. Ruark and associates, this latter finding suggests that CAR T-cell therapy may negatively impact mental health in a subset of patients.
These findings provide clinical insight into a minimally researched patient population.
“At this time, only limited data are available regarding the long-term effects of CAR T-cell therapy,” the investigators wrote in Biology of Blood and Marrow Transplantation. “Thus, it is important to evaluate the late neuropsychiatric effects of CAR T and evaluate their effect on survivors’ quality of life.”
The study involved 40 patients with relapsed or refractory chronic lymphocytic leukemia, non-Hodgkin lymphoma, or acute lymphoblastic leukemia. Before undergoing CAR T-cell therapy, patients underwent standardized mental health screening with validated instruments such as the 7-item Generalized Anxiety Disorder scale. At least 1 year after CAR T-cell therapy, patients completed a questionnaire consisting of the Patient-Reported Outcomes Measurement Information System (PROMIS) Scale v1.2 Global Health and the PROMIS-29 Profile v2.1, and 30 additional questions, 4 of which evaluated cognitive function. These data were converted to T scores for comparative purposes.
Patients who underwent CAR T-cell therapy had statistically similar T scores to the general population mean, suggesting comparable overall neuropsychiatric status. However, a closer look at the data showed that almost one out of five patients who underwent CAR T-cell therapy had global mental health scores that were at least 1 standard deviation lower than the mean for the general population and patients with cancer.
Almost half of the patients (47.5%) who underwent CAR T-cell therapy reported at least one clinically meaningful negative neuropsychiatric outcome. Specifically, 20% reported cognitive difficulties and depression or anxiety, 17.5% reported cognitive difficulties without depression or anxiety, and 10% reported depression or anxiety without cognitive difficulties. One-quarter (25%) of patients reported taking a medication for depression, 20% reported use of anxiolytics, and 15% reported use of sleep medications. Multivariate analysis revealed an association between younger age and depression (P = .01), anxiety (P = .001), and worse long-term global mental health (P = .02). Cognitive difficulties were significantly more common among patients with worse physical and/or mental health.
“[A] subset of patients may experience psychiatric symptoms or cognitive impairment [which may be related to CAR T-cell therapy or other treatments patients have been exposed to], and it is important to identify those patients to assist with intervention strategies,” the investigators concluded.The study was funded by the National Institutes of Health, Life Science Discovery Fund, Juno Therapeutics/Celgene, and others. The investigators reported additional relationships with Nektar Therapeutics, Allogene Therapeutics, T-CURX, and others.
SOURCE: Ruark J et al. Biol Blood Marrow Transplant. 2019 Oct 9. doi: 10.1016/j.bbmt.2019.09.037.
Chimeric antigen receptor (CAR) T-cell therapy is generally associated with good long-term neuropsychiatric status, based on a recent patient-reported outcomes study.
But almost one out of five patients may have notably worse cognitive and psychiatric outcomes within 1-5 years of therapy, reported Julia Ruark, MD, of the University of Washington, Seattle, and colleagues. According to Dr. Ruark and associates, this latter finding suggests that CAR T-cell therapy may negatively impact mental health in a subset of patients.
These findings provide clinical insight into a minimally researched patient population.
“At this time, only limited data are available regarding the long-term effects of CAR T-cell therapy,” the investigators wrote in Biology of Blood and Marrow Transplantation. “Thus, it is important to evaluate the late neuropsychiatric effects of CAR T and evaluate their effect on survivors’ quality of life.”
The study involved 40 patients with relapsed or refractory chronic lymphocytic leukemia, non-Hodgkin lymphoma, or acute lymphoblastic leukemia. Before undergoing CAR T-cell therapy, patients underwent standardized mental health screening with validated instruments such as the 7-item Generalized Anxiety Disorder scale. At least 1 year after CAR T-cell therapy, patients completed a questionnaire consisting of the Patient-Reported Outcomes Measurement Information System (PROMIS) Scale v1.2 Global Health and the PROMIS-29 Profile v2.1, and 30 additional questions, 4 of which evaluated cognitive function. These data were converted to T scores for comparative purposes.
Patients who underwent CAR T-cell therapy had statistically similar T scores to the general population mean, suggesting comparable overall neuropsychiatric status. However, a closer look at the data showed that almost one out of five patients who underwent CAR T-cell therapy had global mental health scores that were at least 1 standard deviation lower than the mean for the general population and patients with cancer.
Almost half of the patients (47.5%) who underwent CAR T-cell therapy reported at least one clinically meaningful negative neuropsychiatric outcome. Specifically, 20% reported cognitive difficulties and depression or anxiety, 17.5% reported cognitive difficulties without depression or anxiety, and 10% reported depression or anxiety without cognitive difficulties. One-quarter (25%) of patients reported taking a medication for depression, 20% reported use of anxiolytics, and 15% reported use of sleep medications. Multivariate analysis revealed an association between younger age and depression (P = .01), anxiety (P = .001), and worse long-term global mental health (P = .02). Cognitive difficulties were significantly more common among patients with worse physical and/or mental health.
“[A] subset of patients may experience psychiatric symptoms or cognitive impairment [which may be related to CAR T-cell therapy or other treatments patients have been exposed to], and it is important to identify those patients to assist with intervention strategies,” the investigators concluded.The study was funded by the National Institutes of Health, Life Science Discovery Fund, Juno Therapeutics/Celgene, and others. The investigators reported additional relationships with Nektar Therapeutics, Allogene Therapeutics, T-CURX, and others.
SOURCE: Ruark J et al. Biol Blood Marrow Transplant. 2019 Oct 9. doi: 10.1016/j.bbmt.2019.09.037.
Chimeric antigen receptor (CAR) T-cell therapy is generally associated with good long-term neuropsychiatric status, based on a recent patient-reported outcomes study.
But almost one out of five patients may have notably worse cognitive and psychiatric outcomes within 1-5 years of therapy, reported Julia Ruark, MD, of the University of Washington, Seattle, and colleagues. According to Dr. Ruark and associates, this latter finding suggests that CAR T-cell therapy may negatively impact mental health in a subset of patients.
These findings provide clinical insight into a minimally researched patient population.
“At this time, only limited data are available regarding the long-term effects of CAR T-cell therapy,” the investigators wrote in Biology of Blood and Marrow Transplantation. “Thus, it is important to evaluate the late neuropsychiatric effects of CAR T and evaluate their effect on survivors’ quality of life.”
The study involved 40 patients with relapsed or refractory chronic lymphocytic leukemia, non-Hodgkin lymphoma, or acute lymphoblastic leukemia. Before undergoing CAR T-cell therapy, patients underwent standardized mental health screening with validated instruments such as the 7-item Generalized Anxiety Disorder scale. At least 1 year after CAR T-cell therapy, patients completed a questionnaire consisting of the Patient-Reported Outcomes Measurement Information System (PROMIS) Scale v1.2 Global Health and the PROMIS-29 Profile v2.1, and 30 additional questions, 4 of which evaluated cognitive function. These data were converted to T scores for comparative purposes.
Patients who underwent CAR T-cell therapy had statistically similar T scores to the general population mean, suggesting comparable overall neuropsychiatric status. However, a closer look at the data showed that almost one out of five patients who underwent CAR T-cell therapy had global mental health scores that were at least 1 standard deviation lower than the mean for the general population and patients with cancer.
Almost half of the patients (47.5%) who underwent CAR T-cell therapy reported at least one clinically meaningful negative neuropsychiatric outcome. Specifically, 20% reported cognitive difficulties and depression or anxiety, 17.5% reported cognitive difficulties without depression or anxiety, and 10% reported depression or anxiety without cognitive difficulties. One-quarter (25%) of patients reported taking a medication for depression, 20% reported use of anxiolytics, and 15% reported use of sleep medications. Multivariate analysis revealed an association between younger age and depression (P = .01), anxiety (P = .001), and worse long-term global mental health (P = .02). Cognitive difficulties were significantly more common among patients with worse physical and/or mental health.
“[A] subset of patients may experience psychiatric symptoms or cognitive impairment [which may be related to CAR T-cell therapy or other treatments patients have been exposed to], and it is important to identify those patients to assist with intervention strategies,” the investigators concluded.The study was funded by the National Institutes of Health, Life Science Discovery Fund, Juno Therapeutics/Celgene, and others. The investigators reported additional relationships with Nektar Therapeutics, Allogene Therapeutics, T-CURX, and others.
SOURCE: Ruark J et al. Biol Blood Marrow Transplant. 2019 Oct 9. doi: 10.1016/j.bbmt.2019.09.037.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
UKALL14: Rituximab improves EFS in B-ALL, but four doses not enough
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
REPORTING FROM ASH 2019
Promising early efficacy of venetoclax/navitoclax in r/r acute lymphoblastic leukemia
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
REPORTING FROM ASH 2019
Chemo-free induction-consolidation protocol for Ph+ ALL improved survival
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
REPORTING FROM ASH 2019