User login
New Classifications and Emerging Treatments in Brain Cancer
- Sokolov AV et al. Pharmacol Rev. 2021;73(4):1-32. doi:10.1124/pharmrev.121.000317
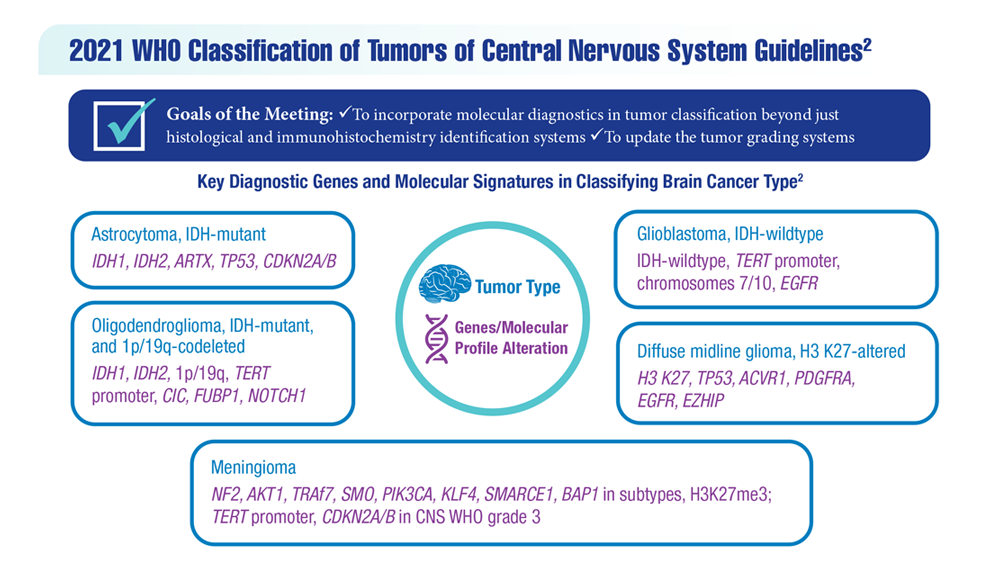
- Louis DN et al. Neuro Oncol. 2021;23(8):1231-1251. doi:10.1093/neuonc/noab106
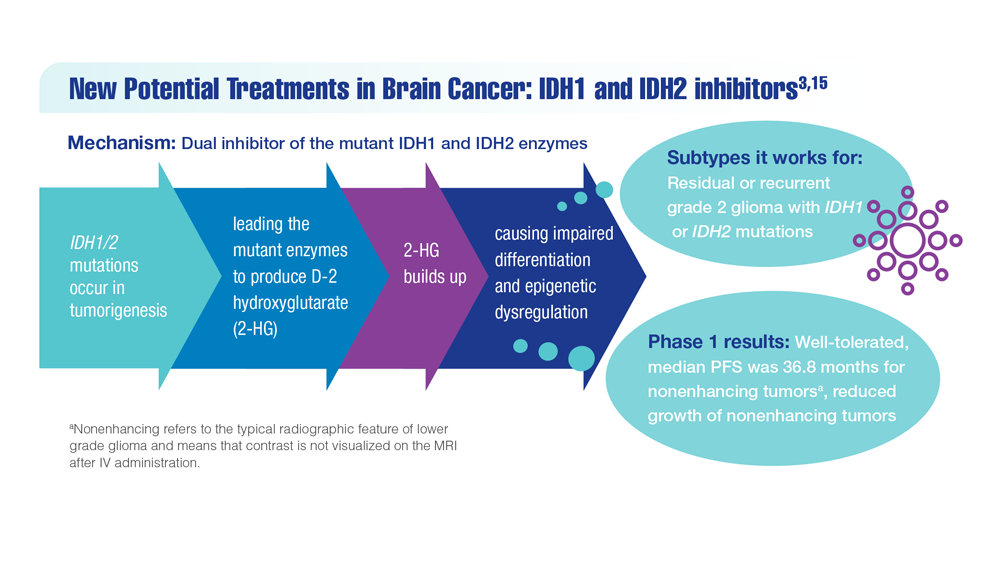
- Mellinghoff IK et al. Clin Cancer Res. 2021;27(16):4491-4499. doi:10.1158/1078-0432.CCR-21-0611
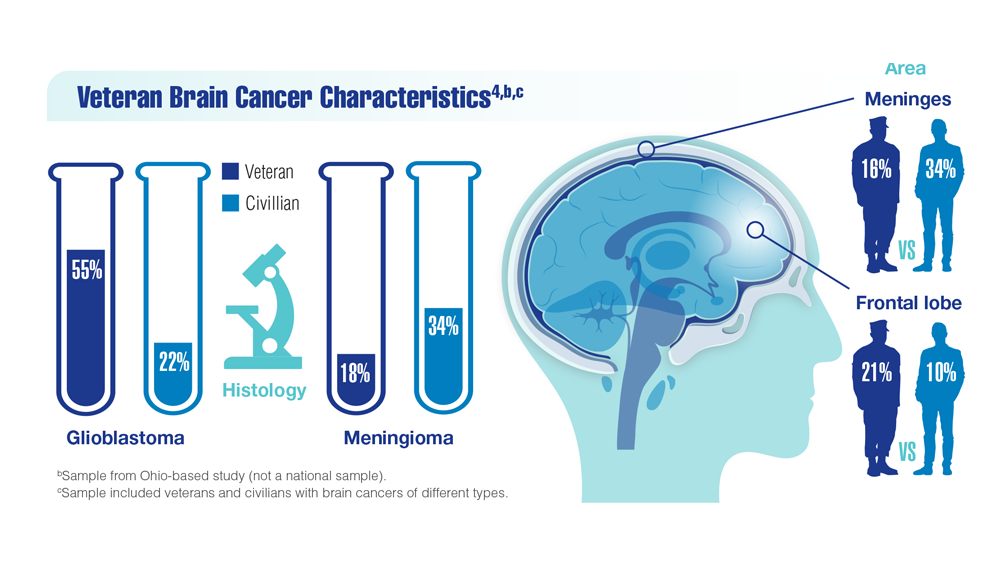
- Woo C et al. JCO Clin Cancer Inform. 2021;5:985-994. doi:10.1200/CCI.21.00052
- Study of vorasidenib (AG-881) in participants with residual or recurrent grade 2 glioma with an IDH1 or IDH2 mutation (INDIGO). ClinicalTrials.gov. Updated May 17, 2022. Accessed December 8, 2022. https://clinicaltrials.gov/ct2/show/NCT04164901
- Servier's pivotal phase 3 indigo trial investigating vorasidenib in IDH-mutant low-grade glioma meets primary endpoint of progression-free survival (PFS) and key secondary endpoint of time to next intervention (TTNI) (no date) Servier US. March 14, 2023. Accessed March 20, 2023. https://www.servier.us/serviers-pivotal-phase-3-indigo-trial-meets-primary-endpoint
- Nehra M et al. J Control Release. 2021;338:224-243. doi:10.1016/j.jconrel.2021.08.027
- Hersh AM et al. Cancers (Basel). 2022;14(19):4920. doi:10.3390/cancers14194920
- Shoaf ML, Desjardins A. Neurotherapeutics. 2022;19(6):1818-1831. doi:10.1007/s13311-022-01256-1
- Bagley SJ, O’Rourke DM. Pharmacol Ther. 2020;205:107419. doi:10.1016/j.pharmthera.2019.107419
- Batich KA et al. Clin Cancer Res. 2020;26(20):5297-5303. doi:10.1158/1078-0432.CCR-20-1082
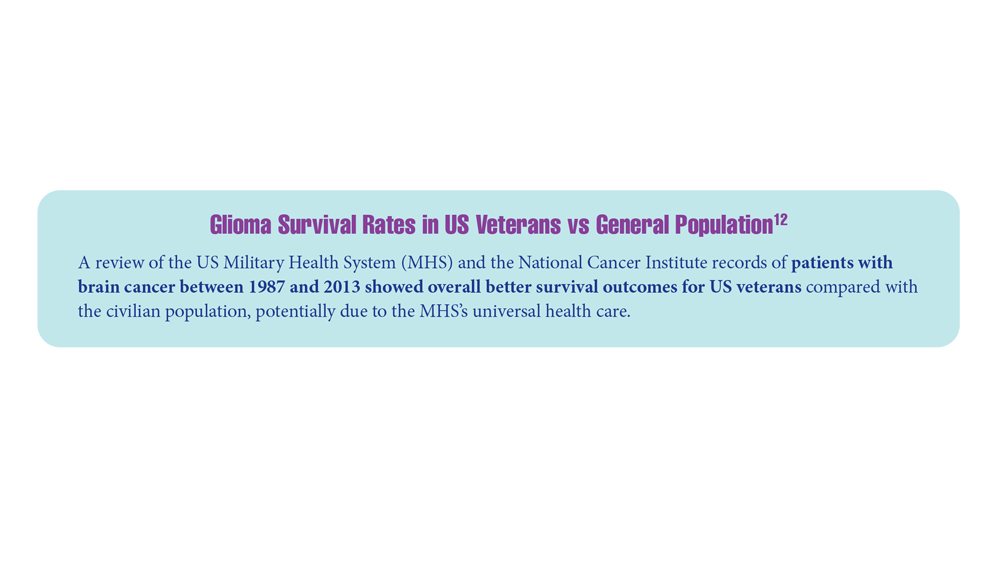
- Lin J et al. Cancer. 2020;126(13):3053-3060. doi:10.1002/cncr.32884
- Barth SK et al. Cancer Epidemiol. 2017;50(pt A):22-29. doi:10.1016/j.canep.2017.07.012
- VA and partners hope APOLLO program will be leap forward for precision oncology. US Department of Veteran Affairs. May 1, 2019. Accessed December 8, 2022. https://www.research.va.gov/currents/0519-VA-and-partners-hope-APOLLO-program-will-be-leap-forward-for-precision-oncology.cfm
- Konteatis Z et al. ACS Med Chem Lett. 2020;11(2):101-107. doi:10.1021/acsmedchemlett.9b00509
- Sokolov AV et al. Pharmacol Rev. 2021;73(4):1-32. doi:10.1124/pharmrev.121.000317
- Louis DN et al. Neuro Oncol. 2021;23(8):1231-1251. doi:10.1093/neuonc/noab106
- Mellinghoff IK et al. Clin Cancer Res. 2021;27(16):4491-4499. doi:10.1158/1078-0432.CCR-21-0611
- Woo C et al. JCO Clin Cancer Inform. 2021;5:985-994. doi:10.1200/CCI.21.00052
- Study of vorasidenib (AG-881) in participants with residual or recurrent grade 2 glioma with an IDH1 or IDH2 mutation (INDIGO). ClinicalTrials.gov. Updated May 17, 2022. Accessed December 8, 2022. https://clinicaltrials.gov/ct2/show/NCT04164901
- Servier's pivotal phase 3 indigo trial investigating vorasidenib in IDH-mutant low-grade glioma meets primary endpoint of progression-free survival (PFS) and key secondary endpoint of time to next intervention (TTNI) (no date) Servier US. March 14, 2023. Accessed March 20, 2023. https://www.servier.us/serviers-pivotal-phase-3-indigo-trial-meets-primary-endpoint
- Nehra M et al. J Control Release. 2021;338:224-243. doi:10.1016/j.jconrel.2021.08.027
- Hersh AM et al. Cancers (Basel). 2022;14(19):4920. doi:10.3390/cancers14194920
- Shoaf ML, Desjardins A. Neurotherapeutics. 2022;19(6):1818-1831. doi:10.1007/s13311-022-01256-1
- Bagley SJ, O’Rourke DM. Pharmacol Ther. 2020;205:107419. doi:10.1016/j.pharmthera.2019.107419
- Batich KA et al. Clin Cancer Res. 2020;26(20):5297-5303. doi:10.1158/1078-0432.CCR-20-1082
- Lin J et al. Cancer. 2020;126(13):3053-3060. doi:10.1002/cncr.32884
- Barth SK et al. Cancer Epidemiol. 2017;50(pt A):22-29. doi:10.1016/j.canep.2017.07.012
- VA and partners hope APOLLO program will be leap forward for precision oncology. US Department of Veteran Affairs. May 1, 2019. Accessed December 8, 2022. https://www.research.va.gov/currents/0519-VA-and-partners-hope-APOLLO-program-will-be-leap-forward-for-precision-oncology.cfm
- Konteatis Z et al. ACS Med Chem Lett. 2020;11(2):101-107. doi:10.1021/acsmedchemlett.9b00509
- Sokolov AV et al. Pharmacol Rev. 2021;73(4):1-32. doi:10.1124/pharmrev.121.000317
- Louis DN et al. Neuro Oncol. 2021;23(8):1231-1251. doi:10.1093/neuonc/noab106
- Mellinghoff IK et al. Clin Cancer Res. 2021;27(16):4491-4499. doi:10.1158/1078-0432.CCR-21-0611
- Woo C et al. JCO Clin Cancer Inform. 2021;5:985-994. doi:10.1200/CCI.21.00052
- Study of vorasidenib (AG-881) in participants with residual or recurrent grade 2 glioma with an IDH1 or IDH2 mutation (INDIGO). ClinicalTrials.gov. Updated May 17, 2022. Accessed December 8, 2022. https://clinicaltrials.gov/ct2/show/NCT04164901
- Servier's pivotal phase 3 indigo trial investigating vorasidenib in IDH-mutant low-grade glioma meets primary endpoint of progression-free survival (PFS) and key secondary endpoint of time to next intervention (TTNI) (no date) Servier US. March 14, 2023. Accessed March 20, 2023. https://www.servier.us/serviers-pivotal-phase-3-indigo-trial-meets-primary-endpoint
- Nehra M et al. J Control Release. 2021;338:224-243. doi:10.1016/j.jconrel.2021.08.027
- Hersh AM et al. Cancers (Basel). 2022;14(19):4920. doi:10.3390/cancers14194920
- Shoaf ML, Desjardins A. Neurotherapeutics. 2022;19(6):1818-1831. doi:10.1007/s13311-022-01256-1
- Bagley SJ, O’Rourke DM. Pharmacol Ther. 2020;205:107419. doi:10.1016/j.pharmthera.2019.107419
- Batich KA et al. Clin Cancer Res. 2020;26(20):5297-5303. doi:10.1158/1078-0432.CCR-20-1082
- Lin J et al. Cancer. 2020;126(13):3053-3060. doi:10.1002/cncr.32884
- Barth SK et al. Cancer Epidemiol. 2017;50(pt A):22-29. doi:10.1016/j.canep.2017.07.012
- VA and partners hope APOLLO program will be leap forward for precision oncology. US Department of Veteran Affairs. May 1, 2019. Accessed December 8, 2022. https://www.research.va.gov/currents/0519-VA-and-partners-hope-APOLLO-program-will-be-leap-forward-for-precision-oncology.cfm
- Konteatis Z et al. ACS Med Chem Lett. 2020;11(2):101-107. doi:10.1021/acsmedchemlett.9b00509
Medical cannabis does not reduce use of prescription meds
TOPLINE:
, according to a new study published in Annals of Internal Medicine.
METHODOLOGY:
- Cannabis advocates suggest that legal medical cannabis can be a partial solution to the opioid overdose crisis in the United States, which claimed more than 80,000 lives in 2021.
- Current research on how legalized cannabis reduces dependence on prescription pain medication is inconclusive.
- Researchers examined insurance data for the period 2010-2022 from 583,820 adults with chronic noncancer pain.
- They drew from 12 states in which medical cannabis is legal and from 17 in which it is not legal to create a hypothetical randomized trial. The control group simulated prescription rates where medical cannabis was not available.
- Authors evaluated prescription rates for opioids, nonopioid painkillers, and pain interventions, such as physical therapy.
TAKEAWAY:
In a given month during the first 3 years after legalization, for states with medical cannabis, the investigators found the following:
- There was an average decrease of 1.07 percentage points in the proportion of patients who received any opioid prescription, compared to a 1.12 percentage point decrease in the control group.
- There was an average increase of 1.14 percentage points in the proportion of patients who received any nonopioid prescription painkiller, compared to a 1.19 percentage point increase in the control group.
- There was a 0.17 percentage point decrease in the proportion of patients who received any pain procedure, compared to a 0.001 percentage point decrease in the control group.
IN PRACTICE:
“This study did not identify important effects of medical cannabis laws on receipt of opioid or nonopioid pain treatment among patients with chronic noncancer pain,” according to the researchers.
SOURCE:
The study was led by Emma E. McGinty, PhD, of Weill Cornell Medicine, New York, and was funded by the National Institute on Drug Abuse.
LIMITATIONS:
The investigators used a simulated, hypothetical control group that was based on untestable assumptions. They also drew data solely from insured individuals, so the study does not necessarily represent uninsured populations.
DISCLOSURES:
Dr. McGinty reports receiving a grant from NIDA. Her coauthors reported receiving support from NIDA and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a new study published in Annals of Internal Medicine.
METHODOLOGY:
- Cannabis advocates suggest that legal medical cannabis can be a partial solution to the opioid overdose crisis in the United States, which claimed more than 80,000 lives in 2021.
- Current research on how legalized cannabis reduces dependence on prescription pain medication is inconclusive.
- Researchers examined insurance data for the period 2010-2022 from 583,820 adults with chronic noncancer pain.
- They drew from 12 states in which medical cannabis is legal and from 17 in which it is not legal to create a hypothetical randomized trial. The control group simulated prescription rates where medical cannabis was not available.
- Authors evaluated prescription rates for opioids, nonopioid painkillers, and pain interventions, such as physical therapy.
TAKEAWAY:
In a given month during the first 3 years after legalization, for states with medical cannabis, the investigators found the following:
- There was an average decrease of 1.07 percentage points in the proportion of patients who received any opioid prescription, compared to a 1.12 percentage point decrease in the control group.
- There was an average increase of 1.14 percentage points in the proportion of patients who received any nonopioid prescription painkiller, compared to a 1.19 percentage point increase in the control group.
- There was a 0.17 percentage point decrease in the proportion of patients who received any pain procedure, compared to a 0.001 percentage point decrease in the control group.
IN PRACTICE:
“This study did not identify important effects of medical cannabis laws on receipt of opioid or nonopioid pain treatment among patients with chronic noncancer pain,” according to the researchers.
SOURCE:
The study was led by Emma E. McGinty, PhD, of Weill Cornell Medicine, New York, and was funded by the National Institute on Drug Abuse.
LIMITATIONS:
The investigators used a simulated, hypothetical control group that was based on untestable assumptions. They also drew data solely from insured individuals, so the study does not necessarily represent uninsured populations.
DISCLOSURES:
Dr. McGinty reports receiving a grant from NIDA. Her coauthors reported receiving support from NIDA and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a new study published in Annals of Internal Medicine.
METHODOLOGY:
- Cannabis advocates suggest that legal medical cannabis can be a partial solution to the opioid overdose crisis in the United States, which claimed more than 80,000 lives in 2021.
- Current research on how legalized cannabis reduces dependence on prescription pain medication is inconclusive.
- Researchers examined insurance data for the period 2010-2022 from 583,820 adults with chronic noncancer pain.
- They drew from 12 states in which medical cannabis is legal and from 17 in which it is not legal to create a hypothetical randomized trial. The control group simulated prescription rates where medical cannabis was not available.
- Authors evaluated prescription rates for opioids, nonopioid painkillers, and pain interventions, such as physical therapy.
TAKEAWAY:
In a given month during the first 3 years after legalization, for states with medical cannabis, the investigators found the following:
- There was an average decrease of 1.07 percentage points in the proportion of patients who received any opioid prescription, compared to a 1.12 percentage point decrease in the control group.
- There was an average increase of 1.14 percentage points in the proportion of patients who received any nonopioid prescription painkiller, compared to a 1.19 percentage point increase in the control group.
- There was a 0.17 percentage point decrease in the proportion of patients who received any pain procedure, compared to a 0.001 percentage point decrease in the control group.
IN PRACTICE:
“This study did not identify important effects of medical cannabis laws on receipt of opioid or nonopioid pain treatment among patients with chronic noncancer pain,” according to the researchers.
SOURCE:
The study was led by Emma E. McGinty, PhD, of Weill Cornell Medicine, New York, and was funded by the National Institute on Drug Abuse.
LIMITATIONS:
The investigators used a simulated, hypothetical control group that was based on untestable assumptions. They also drew data solely from insured individuals, so the study does not necessarily represent uninsured populations.
DISCLOSURES:
Dr. McGinty reports receiving a grant from NIDA. Her coauthors reported receiving support from NIDA and the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Lean muscle mass protective against Alzheimer’s?
Investigators analyzed data on more than 450,000 participants in the UK Biobank as well as two independent samples of more than 320,000 individuals with and without AD, and more than 260,000 individuals participating in a separate genes and intelligence study.
They estimated lean muscle and fat tissue in the arms and legs and found, in adjusted analyses, over 500 genetic variants associated with lean mass.
On average, higher genetically lean mass was associated with a “modest but statistically robust” reduction in AD risk and with superior performance on cognitive tasks.
“Using human genetic data, we found evidence for a protective effect of lean mass on risk of Alzheimer’s disease,” study investigators Iyas Daghlas, MD, a resident in the department of neurology, University of California, San Francisco, said in an interview.
Although “clinical intervention studies are needed to confirm this effect, this study supports current recommendations to maintain a healthy lifestyle to prevent dementia,” he said.
The study was published online in BMJ Medicine.
Naturally randomized research
Several measures of body composition have been investigated for their potential association with AD. Lean mass – a “proxy for muscle mass, defined as the difference between total mass and fat mass” – has been shown to be reduced in patients with AD compared with controls, the researchers noted.
“Previous research studies have tested the relationship of body mass index with Alzheimer’s disease and did not find evidence for a causal effect,” Dr. Daghlas said. “We wondered whether BMI was an insufficiently granular measure and hypothesized that disaggregating body mass into lean mass and fat mass could reveal novel associations with disease.”
Most studies have used case-control designs, which might be biased by “residual confounding or reverse causality.” Naturally randomized data “may be used as an alternative to conventional observational studies to investigate causal relations between risk factors and diseases,” the researchers wrote.
In particular, the Mendelian randomization (MR) paradigm randomly allocates germline genetic variants and uses them as proxies for a specific risk factor.
MR “is a technique that permits researchers to investigate cause-and-effect relationships using human genetic data,” Dr. Daghlas explained. “In effect, we’re studying the results of a naturally randomized experiment whereby some individuals are genetically allocated to carry more lean mass.”
The current study used MR to investigate the effect of genetically proxied lean mass on the risk of AD and the “related phenotype” of cognitive performance.
Genetic proxy
As genetic proxies for lean mass, the researchers chose single nucleotide polymorphisms (genetic variants) that were associated, in a genome-wide association study (GWAS), with appendicular lean mass.
Appendicular lean mass “more accurately reflects the effects of lean mass than whole body lean mass, which includes smooth and cardiac muscle,” the authors explained.
This GWAS used phenotypic and genetic data from 450,243 participants in the UK Biobank cohort (mean age 57 years). All participants were of European ancestry.
The researchers adjusted for age, sex, and genetic ancestry. They measured appendicular lean mass using bioimpedance – an electric current that flows at different rates through the body, depending on its composition.
In addition to the UK Biobank participants, the researchers drew on an independent sample of 21,982 people with AD; a control group of 41,944 people without AD; a replication sample of 7,329 people with and 252,879 people without AD to validate the findings; and 269,867 people taking part in a genome-wide study of cognitive performance.
The researchers identified 584 variants that met criteria for use as genetic proxies for lean mass. None were located within the APOE gene region. In the aggregate, these variants explained 10.3% of the variance in appendicular lean mass.
Each standard deviation increase in genetically proxied lean mass was associated with a 12% reduction in AD risk (odds ratio [OR], 0.88; 95% confidence interval [CI], 0.82-0.95; P < .001). This finding was replicated in the independent consortium (OR, 0.91; 95% CI, 0.83-0.99; P = .02).
The findings remained “consistent” in sensitivity analyses.
A modifiable risk factor?
Higher appendicular lean mass was associated with higher levels of cognitive performance, with each SD increase in lean mass associated with an SD increase in cognitive performance (OR, 0.09; 95% CI, 0.06-0.11; P = .001).
“Adjusting for potential mediation through performance did not reduce the association between appendicular lean mass and risk of AD,” the authors wrote.
They obtained similar results using genetically proxied trunk and whole-body lean mass, after adjusting for fat mass.
The authors noted several limitations. The bioimpedance measures “only predict, but do not directly measure, lean mass.” Moreover, the approach didn’t examine whether a “critical window of risk factor timing” exists, during which lean mass might play a role in influencing AD risk and after which “interventions would no longer be effective.” Nor could the study determine whether increasing lean mass could reverse AD pathology in patients with preclinical disease or mild cognitive impairment.
Nevertheless, the findings suggest “that lean mass might be a possible modifiable protective factor for Alzheimer’s disease,” the authors wrote. “The mechanisms underlying this finding, as well as the clinical and public health implications, warrant further investigation.”
Novel strategies
In a comment, Iva Miljkovic, MD, PhD, associate professor, department of epidemiology, University of Pittsburgh, said the investigators used “very rigorous methodology.”
The finding suggesting that lean mass is associated with better cognitive function is “important, as cognitive impairment can become stable rather than progress to a pathological state; and, in some cases, can even be reversed.”
In those cases, “identifying the underlying cause – e.g., low lean mass – can significantly improve cognitive function,” said Dr. Miljkovic, senior author of a study showing muscle fat as a risk factor for cognitive decline.
More research will enable us to “expand our understanding” of the mechanisms involved and determine whether interventions aimed at preventing muscle loss and/or increasing muscle fat may have a beneficial effect on cognitive function,” she said. “This might lead to novel strategies to prevent AD.”
Dr. Daghlas is supported by the British Heart Foundation Centre of Research Excellence at Imperial College, London, and is employed part-time by Novo Nordisk. Dr. Miljkovic reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data on more than 450,000 participants in the UK Biobank as well as two independent samples of more than 320,000 individuals with and without AD, and more than 260,000 individuals participating in a separate genes and intelligence study.
They estimated lean muscle and fat tissue in the arms and legs and found, in adjusted analyses, over 500 genetic variants associated with lean mass.
On average, higher genetically lean mass was associated with a “modest but statistically robust” reduction in AD risk and with superior performance on cognitive tasks.
“Using human genetic data, we found evidence for a protective effect of lean mass on risk of Alzheimer’s disease,” study investigators Iyas Daghlas, MD, a resident in the department of neurology, University of California, San Francisco, said in an interview.
Although “clinical intervention studies are needed to confirm this effect, this study supports current recommendations to maintain a healthy lifestyle to prevent dementia,” he said.
The study was published online in BMJ Medicine.
Naturally randomized research
Several measures of body composition have been investigated for their potential association with AD. Lean mass – a “proxy for muscle mass, defined as the difference between total mass and fat mass” – has been shown to be reduced in patients with AD compared with controls, the researchers noted.
“Previous research studies have tested the relationship of body mass index with Alzheimer’s disease and did not find evidence for a causal effect,” Dr. Daghlas said. “We wondered whether BMI was an insufficiently granular measure and hypothesized that disaggregating body mass into lean mass and fat mass could reveal novel associations with disease.”
Most studies have used case-control designs, which might be biased by “residual confounding or reverse causality.” Naturally randomized data “may be used as an alternative to conventional observational studies to investigate causal relations between risk factors and diseases,” the researchers wrote.
In particular, the Mendelian randomization (MR) paradigm randomly allocates germline genetic variants and uses them as proxies for a specific risk factor.
MR “is a technique that permits researchers to investigate cause-and-effect relationships using human genetic data,” Dr. Daghlas explained. “In effect, we’re studying the results of a naturally randomized experiment whereby some individuals are genetically allocated to carry more lean mass.”
The current study used MR to investigate the effect of genetically proxied lean mass on the risk of AD and the “related phenotype” of cognitive performance.
Genetic proxy
As genetic proxies for lean mass, the researchers chose single nucleotide polymorphisms (genetic variants) that were associated, in a genome-wide association study (GWAS), with appendicular lean mass.
Appendicular lean mass “more accurately reflects the effects of lean mass than whole body lean mass, which includes smooth and cardiac muscle,” the authors explained.
This GWAS used phenotypic and genetic data from 450,243 participants in the UK Biobank cohort (mean age 57 years). All participants were of European ancestry.
The researchers adjusted for age, sex, and genetic ancestry. They measured appendicular lean mass using bioimpedance – an electric current that flows at different rates through the body, depending on its composition.
In addition to the UK Biobank participants, the researchers drew on an independent sample of 21,982 people with AD; a control group of 41,944 people without AD; a replication sample of 7,329 people with and 252,879 people without AD to validate the findings; and 269,867 people taking part in a genome-wide study of cognitive performance.
The researchers identified 584 variants that met criteria for use as genetic proxies for lean mass. None were located within the APOE gene region. In the aggregate, these variants explained 10.3% of the variance in appendicular lean mass.
Each standard deviation increase in genetically proxied lean mass was associated with a 12% reduction in AD risk (odds ratio [OR], 0.88; 95% confidence interval [CI], 0.82-0.95; P < .001). This finding was replicated in the independent consortium (OR, 0.91; 95% CI, 0.83-0.99; P = .02).
The findings remained “consistent” in sensitivity analyses.
A modifiable risk factor?
Higher appendicular lean mass was associated with higher levels of cognitive performance, with each SD increase in lean mass associated with an SD increase in cognitive performance (OR, 0.09; 95% CI, 0.06-0.11; P = .001).
“Adjusting for potential mediation through performance did not reduce the association between appendicular lean mass and risk of AD,” the authors wrote.
They obtained similar results using genetically proxied trunk and whole-body lean mass, after adjusting for fat mass.
The authors noted several limitations. The bioimpedance measures “only predict, but do not directly measure, lean mass.” Moreover, the approach didn’t examine whether a “critical window of risk factor timing” exists, during which lean mass might play a role in influencing AD risk and after which “interventions would no longer be effective.” Nor could the study determine whether increasing lean mass could reverse AD pathology in patients with preclinical disease or mild cognitive impairment.
Nevertheless, the findings suggest “that lean mass might be a possible modifiable protective factor for Alzheimer’s disease,” the authors wrote. “The mechanisms underlying this finding, as well as the clinical and public health implications, warrant further investigation.”
Novel strategies
In a comment, Iva Miljkovic, MD, PhD, associate professor, department of epidemiology, University of Pittsburgh, said the investigators used “very rigorous methodology.”
The finding suggesting that lean mass is associated with better cognitive function is “important, as cognitive impairment can become stable rather than progress to a pathological state; and, in some cases, can even be reversed.”
In those cases, “identifying the underlying cause – e.g., low lean mass – can significantly improve cognitive function,” said Dr. Miljkovic, senior author of a study showing muscle fat as a risk factor for cognitive decline.
More research will enable us to “expand our understanding” of the mechanisms involved and determine whether interventions aimed at preventing muscle loss and/or increasing muscle fat may have a beneficial effect on cognitive function,” she said. “This might lead to novel strategies to prevent AD.”
Dr. Daghlas is supported by the British Heart Foundation Centre of Research Excellence at Imperial College, London, and is employed part-time by Novo Nordisk. Dr. Miljkovic reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data on more than 450,000 participants in the UK Biobank as well as two independent samples of more than 320,000 individuals with and without AD, and more than 260,000 individuals participating in a separate genes and intelligence study.
They estimated lean muscle and fat tissue in the arms and legs and found, in adjusted analyses, over 500 genetic variants associated with lean mass.
On average, higher genetically lean mass was associated with a “modest but statistically robust” reduction in AD risk and with superior performance on cognitive tasks.
“Using human genetic data, we found evidence for a protective effect of lean mass on risk of Alzheimer’s disease,” study investigators Iyas Daghlas, MD, a resident in the department of neurology, University of California, San Francisco, said in an interview.
Although “clinical intervention studies are needed to confirm this effect, this study supports current recommendations to maintain a healthy lifestyle to prevent dementia,” he said.
The study was published online in BMJ Medicine.
Naturally randomized research
Several measures of body composition have been investigated for their potential association with AD. Lean mass – a “proxy for muscle mass, defined as the difference between total mass and fat mass” – has been shown to be reduced in patients with AD compared with controls, the researchers noted.
“Previous research studies have tested the relationship of body mass index with Alzheimer’s disease and did not find evidence for a causal effect,” Dr. Daghlas said. “We wondered whether BMI was an insufficiently granular measure and hypothesized that disaggregating body mass into lean mass and fat mass could reveal novel associations with disease.”
Most studies have used case-control designs, which might be biased by “residual confounding or reverse causality.” Naturally randomized data “may be used as an alternative to conventional observational studies to investigate causal relations between risk factors and diseases,” the researchers wrote.
In particular, the Mendelian randomization (MR) paradigm randomly allocates germline genetic variants and uses them as proxies for a specific risk factor.
MR “is a technique that permits researchers to investigate cause-and-effect relationships using human genetic data,” Dr. Daghlas explained. “In effect, we’re studying the results of a naturally randomized experiment whereby some individuals are genetically allocated to carry more lean mass.”
The current study used MR to investigate the effect of genetically proxied lean mass on the risk of AD and the “related phenotype” of cognitive performance.
Genetic proxy
As genetic proxies for lean mass, the researchers chose single nucleotide polymorphisms (genetic variants) that were associated, in a genome-wide association study (GWAS), with appendicular lean mass.
Appendicular lean mass “more accurately reflects the effects of lean mass than whole body lean mass, which includes smooth and cardiac muscle,” the authors explained.
This GWAS used phenotypic and genetic data from 450,243 participants in the UK Biobank cohort (mean age 57 years). All participants were of European ancestry.
The researchers adjusted for age, sex, and genetic ancestry. They measured appendicular lean mass using bioimpedance – an electric current that flows at different rates through the body, depending on its composition.
In addition to the UK Biobank participants, the researchers drew on an independent sample of 21,982 people with AD; a control group of 41,944 people without AD; a replication sample of 7,329 people with and 252,879 people without AD to validate the findings; and 269,867 people taking part in a genome-wide study of cognitive performance.
The researchers identified 584 variants that met criteria for use as genetic proxies for lean mass. None were located within the APOE gene region. In the aggregate, these variants explained 10.3% of the variance in appendicular lean mass.
Each standard deviation increase in genetically proxied lean mass was associated with a 12% reduction in AD risk (odds ratio [OR], 0.88; 95% confidence interval [CI], 0.82-0.95; P < .001). This finding was replicated in the independent consortium (OR, 0.91; 95% CI, 0.83-0.99; P = .02).
The findings remained “consistent” in sensitivity analyses.
A modifiable risk factor?
Higher appendicular lean mass was associated with higher levels of cognitive performance, with each SD increase in lean mass associated with an SD increase in cognitive performance (OR, 0.09; 95% CI, 0.06-0.11; P = .001).
“Adjusting for potential mediation through performance did not reduce the association between appendicular lean mass and risk of AD,” the authors wrote.
They obtained similar results using genetically proxied trunk and whole-body lean mass, after adjusting for fat mass.
The authors noted several limitations. The bioimpedance measures “only predict, but do not directly measure, lean mass.” Moreover, the approach didn’t examine whether a “critical window of risk factor timing” exists, during which lean mass might play a role in influencing AD risk and after which “interventions would no longer be effective.” Nor could the study determine whether increasing lean mass could reverse AD pathology in patients with preclinical disease or mild cognitive impairment.
Nevertheless, the findings suggest “that lean mass might be a possible modifiable protective factor for Alzheimer’s disease,” the authors wrote. “The mechanisms underlying this finding, as well as the clinical and public health implications, warrant further investigation.”
Novel strategies
In a comment, Iva Miljkovic, MD, PhD, associate professor, department of epidemiology, University of Pittsburgh, said the investigators used “very rigorous methodology.”
The finding suggesting that lean mass is associated with better cognitive function is “important, as cognitive impairment can become stable rather than progress to a pathological state; and, in some cases, can even be reversed.”
In those cases, “identifying the underlying cause – e.g., low lean mass – can significantly improve cognitive function,” said Dr. Miljkovic, senior author of a study showing muscle fat as a risk factor for cognitive decline.
More research will enable us to “expand our understanding” of the mechanisms involved and determine whether interventions aimed at preventing muscle loss and/or increasing muscle fat may have a beneficial effect on cognitive function,” she said. “This might lead to novel strategies to prevent AD.”
Dr. Daghlas is supported by the British Heart Foundation Centre of Research Excellence at Imperial College, London, and is employed part-time by Novo Nordisk. Dr. Miljkovic reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BMJ MEDICINE
Discontinuing Disease-Modifying Therapies in Nonactive Secondary Progressive MS:Review of the Evidence
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
AI model interprets EEGs with near-perfect accuracy
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
An automated artificial intelligence (AI) model trained to read electroencephalograms (EEGs) in patients with suspected epilepsy is just as accurate as trained neurologists, new data suggest.
Known as SCORE-AI, the technology distinguishes between abnormal and normal EEG recordings and classifies irregular recordings into specific categories crucial for patient decision-making.
“SCORE-AI can be used in place of experts in underprivileged areas, where expertise is missing, or to help physicians to preselect or prescore recordings in areas where the workload is high – we can all benefit from AI,” study investigator Sándor Beniczky, MD, PhD, said in a JAMA Neurology podcast.
Dr. Beniczky is professor of clinical neurophysiology at Aarhus University in Denmark.
The findings were published online in JAMA Neurology.
Gaining a foothold
Increasingly, AI is gaining a foothold in medicine by credibly addressing patient queries and aiding radiologists.
To bring AI to EEG interpretation, the researchers developed and validated an AI model that was able to assess routine, clinical EEGs in patients with suspected epilepsy.
Beyond using AI to distinguish abnormal from normal EEG recordings, the researchers wanted to train the new system to classify abnormal recordings into the major categories that are most relevant for clinical decision-making in patients who may have epilepsy. The categories included epileptiform-focal, epileptiform-generalized, nonepileptiform-focal, and nonepileptiform-diffuse abnormalities.
The researchers trained the learning model using Standardized Computer-based Organized Reporting of EEG (SCORE) software.
In the development phase, the model was trained using more than 30,490 anonymized and highly annotated EEG recordings from 14,100 men (median age, 25 years) from a single center. The recordings had an average duration of 31 minutes and were interpreted by 17 neurologists using standardized criteria. If an EEG recording was abnormal, the physicians had to specify which abnormal features were present.
SCORE-AI then performed an analysis of the recordings based on input from the experts.
To validate the findings, investigators used two independent test datasets. The first dataset consisted of 100 representative routine EEGs from 61 men (median age, 26 years), evaluated by 11 neurologists from different centers.
The consensus of these evaluations served as the reference standard. The second dataset comprised nearly 10,000 EEGs from a single center (5,170 men; median age, 35 years), independently assessed by 14 neurologists.
Near-perfect accuracy
When compared with the experts, SCORE-AI had near-perfect accuracy with an area under the receiver operating characteristic (AUROC) curve for differentiating normal from abnormal EEG recordings of 0.95.
SCORE-AI also performed well at identifying generalized epileptiform abnormalities (AUROC, 0.96), focal epileptiform abnormalities (AUROC, 0.91), focal nonepileptiform abnormalities (AUROC, 0.89), and diffuse nonepileptiform abnormalities (AUROC, 0.93).
In addition, SCORE-AI had excellent agreement with clinicians – and sometimes agreed with individual experts more than the experts agreed with one another.
When Dr. Beniczky and team tested SCORE-AI against three previously published AI models, SCORE-AI demonstrated greater specificity than those models (90% vs. 3%-63%) but was not as sensitive (86.7%) as two of the models (96.7% and 100%).
One of the study’s limitations was the fact that SCORE-AI was developed and validated on routine EEGs that excluded neonates and critically ill patients.
In the future, Dr. Beniczky said on the podcast, the team would like to train SCORE-AI to read EEGs with more granularity, and eventually use only one single channel to record EEGs. At present, SCORE-AI is being integrated with Natus Neuro, a widely used EEG equipment system, the investigators note.
In an accompanying editorial, Jonathan Kleen, MD, PhD, and Elan Guterman, MD, said, “The overall approach taken ... in developing and validating SCORE-AI sets a standard for this work going forward.”
Dr. Kleen and Dr. Guterman note that the technological gains brought about by SCORE-AI technology “could offer an exciting prospect to improve EEG availability and clinical care for the 50 million people with epilepsy worldwide.”
A version of this article originally appeared on Medscape.com.
New data on traumatic brain injury show it’s chronic, evolving
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
FDA clears new biomarker assays for early Alzheimer’s detection
The Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys total-tau CSF assays (tTau) (used as a tTau/Abeta42 ratio) are for use in adults ages 55 and older being evaluated for AD.
They join the Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys phospho-tau (181P) CSF (pTau181) assays (used as a pTau181/Abeta42 ratio) that received FDA 510(k) clearance in 2022.
“An early and accurate diagnosis can help patients, caregivers and physicians determine a path forward, and the Elecsys CSF assays support diagnosis at early disease stages, when treatment is most effective,” Brad Moore, president and CEO of Roche Diagnostics North America, said in a statement.
Appropriate use recommendations for new and emerging AD drugs call for confirmation of amyloid pathology. Currently, the only FDA-cleared methods to confirm amyloid pathology are CSF tests and PET scans.
“The Elecsys AD CSF assays are concordant with amyloid PET scan imaging and have the potential to provide a more affordable and accessible routine option to confirm the presence of amyloid pathology in the brain,” Roche said.
“They also offer detection of both amyloid and tau biomarkers from one draw, with no radiation and potential to detect Alzheimer’s pathology in early stages of disease,” the company added.
The previously approved Elecsys pTau181/Abeta42 ratio is currently available and the newly approved Elecsys tTau/Abeta42 ratio will be available in the fourth quarter of 2023.
A version of this article first appeared on Medscape.com.
The Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys total-tau CSF assays (tTau) (used as a tTau/Abeta42 ratio) are for use in adults ages 55 and older being evaluated for AD.
They join the Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys phospho-tau (181P) CSF (pTau181) assays (used as a pTau181/Abeta42 ratio) that received FDA 510(k) clearance in 2022.
“An early and accurate diagnosis can help patients, caregivers and physicians determine a path forward, and the Elecsys CSF assays support diagnosis at early disease stages, when treatment is most effective,” Brad Moore, president and CEO of Roche Diagnostics North America, said in a statement.
Appropriate use recommendations for new and emerging AD drugs call for confirmation of amyloid pathology. Currently, the only FDA-cleared methods to confirm amyloid pathology are CSF tests and PET scans.
“The Elecsys AD CSF assays are concordant with amyloid PET scan imaging and have the potential to provide a more affordable and accessible routine option to confirm the presence of amyloid pathology in the brain,” Roche said.
“They also offer detection of both amyloid and tau biomarkers from one draw, with no radiation and potential to detect Alzheimer’s pathology in early stages of disease,” the company added.
The previously approved Elecsys pTau181/Abeta42 ratio is currently available and the newly approved Elecsys tTau/Abeta42 ratio will be available in the fourth quarter of 2023.
A version of this article first appeared on Medscape.com.
The Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys total-tau CSF assays (tTau) (used as a tTau/Abeta42 ratio) are for use in adults ages 55 and older being evaluated for AD.
They join the Elecsys beta-amyloid (1-42) CSF II (Abeta42) and Elecsys phospho-tau (181P) CSF (pTau181) assays (used as a pTau181/Abeta42 ratio) that received FDA 510(k) clearance in 2022.
“An early and accurate diagnosis can help patients, caregivers and physicians determine a path forward, and the Elecsys CSF assays support diagnosis at early disease stages, when treatment is most effective,” Brad Moore, president and CEO of Roche Diagnostics North America, said in a statement.
Appropriate use recommendations for new and emerging AD drugs call for confirmation of amyloid pathology. Currently, the only FDA-cleared methods to confirm amyloid pathology are CSF tests and PET scans.
“The Elecsys AD CSF assays are concordant with amyloid PET scan imaging and have the potential to provide a more affordable and accessible routine option to confirm the presence of amyloid pathology in the brain,” Roche said.
“They also offer detection of both amyloid and tau biomarkers from one draw, with no radiation and potential to detect Alzheimer’s pathology in early stages of disease,” the company added.
The previously approved Elecsys pTau181/Abeta42 ratio is currently available and the newly approved Elecsys tTau/Abeta42 ratio will be available in the fourth quarter of 2023.
A version of this article first appeared on Medscape.com.
No link between heartburn meds and dementia
A new study provides reassurance about the safety of long-term proton pump inhibitor (PPIs) and histamine-2 receptor antagonist (H2RA) use in older adults, finding no increased risk for dementia or cognitive changes.
It was published online in Gastroenterology.
The post hoc observational study was led by Raaj Mehta, MD, PhD, with Massachusetts General Hospital and Harvard Medical School in Boston.
The researchers analyzed results from the Aspirin in Reducing Events in the Elderly clinical trial. The randomized trial of aspirin included 18,934 adults aged 65 and older from the United States and Australia. Patients’ use of PPI and H2RA was tracked, along with dementia incidence and cognitive changes.
The results showed that there was no link to new dementia diagnoses in patients who used PPIs (25%) and H2RA (2%) at baseline, versus those who did not use either heartburn medication.
Limitations of prior studies are referenced, including the potential for residual confounding and underestimation of PPI and H2RA use, the lack of data on medication dose and duration, and the absence of apo E4 allele status.
The study was funded by grants from the National Institute on Aging, the National Cancer Institute, and other institutions. Dr. Mehta has disclosed no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
A new study provides reassurance about the safety of long-term proton pump inhibitor (PPIs) and histamine-2 receptor antagonist (H2RA) use in older adults, finding no increased risk for dementia or cognitive changes.
It was published online in Gastroenterology.
The post hoc observational study was led by Raaj Mehta, MD, PhD, with Massachusetts General Hospital and Harvard Medical School in Boston.
The researchers analyzed results from the Aspirin in Reducing Events in the Elderly clinical trial. The randomized trial of aspirin included 18,934 adults aged 65 and older from the United States and Australia. Patients’ use of PPI and H2RA was tracked, along with dementia incidence and cognitive changes.
The results showed that there was no link to new dementia diagnoses in patients who used PPIs (25%) and H2RA (2%) at baseline, versus those who did not use either heartburn medication.
Limitations of prior studies are referenced, including the potential for residual confounding and underestimation of PPI and H2RA use, the lack of data on medication dose and duration, and the absence of apo E4 allele status.
The study was funded by grants from the National Institute on Aging, the National Cancer Institute, and other institutions. Dr. Mehta has disclosed no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
A new study provides reassurance about the safety of long-term proton pump inhibitor (PPIs) and histamine-2 receptor antagonist (H2RA) use in older adults, finding no increased risk for dementia or cognitive changes.
It was published online in Gastroenterology.
The post hoc observational study was led by Raaj Mehta, MD, PhD, with Massachusetts General Hospital and Harvard Medical School in Boston.
The researchers analyzed results from the Aspirin in Reducing Events in the Elderly clinical trial. The randomized trial of aspirin included 18,934 adults aged 65 and older from the United States and Australia. Patients’ use of PPI and H2RA was tracked, along with dementia incidence and cognitive changes.
The results showed that there was no link to new dementia diagnoses in patients who used PPIs (25%) and H2RA (2%) at baseline, versus those who did not use either heartburn medication.
Limitations of prior studies are referenced, including the potential for residual confounding and underestimation of PPI and H2RA use, the lack of data on medication dose and duration, and the absence of apo E4 allele status.
The study was funded by grants from the National Institute on Aging, the National Cancer Institute, and other institutions. Dr. Mehta has disclosed no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
FROM GASTROENTEROLOGY
Women with atrial fibrillation more likely to develop dementia
New data suggest a significantly stronger link in women compared with men between atrial fibrillation (AF) and mild cognitive impairment (MCI) and dementia.
“Our findings imply that women with AF may be at higher risk for MCI and dementia with potentially more rapid disease progression from normal cognition to MCI or dementia than women without AF or men with and without AF,” wrote authors of a new study led by Kathryn A. Wood, PhD, RN, Neil Hodgson Woodruff School of Nursing at Emory University in Atlanta.
The findings were published online in Alzheimer’s & Dementia.
Researchers used the National Alzheimer’s Coordinating Center data with 43,630 patients and analyzed sex differences between men and women with AF and their performance on neuropsychological tests and cognitive disease progression.
Higher odds of dementia, MCI in women
According to the paper, AF is associated with higher odds of dementia (odds ratio [OR], 3.00; 95% confidence interval [CI], 1.22-7.37) in women and MCI in women (OR, 3.43; 95% CI, 1.55-7.55) compared with men.
Women with AF and normal cognition at baseline had a higher risk of disease progression (hazard ratio [HR], 1.26; 95% CI, 1.06-1.50) from normal to MCI and from MCI to vascular dementia (HR, 3.27; 95% CI, 1.89-5.65) than that of men with AF or men and women without AF.
AF is a major public health problem linked with stroke and heart failure, and is an independent risk factor of increased mortality. It is associated with higher risk of cognitive impairment and dementia independent of stroke history.
Cognitive screening for AF patients
The authors wrote that cognitive screening, especially in women, should be part of yearly cardiology visits for patients with AF to help identify early those at highest risk for cognitive disease.
T. Jared Bunch, MD, professor of medicine in the division of cardiovascular medicine at University of Utah in Salt Lake City, said in an interview, “We have learned that how we treat atrial fibrillation can influence risk.”
First, he said, outcomes, including brain health, are better when rhythm control approaches are used within the first year of diagnosis.
“Restoring a normal heart rhythm improves brain perfusion and cognitive function. Next, aggressive rhythm control – such as catheter ablation – is associated with much lower long-term risks of dementia in the [patients]. Finally, early and effective use of anticoagulation in patients with atrial fibrillation lowers risk of stroke, dementia, and cognitive decline.”
Several factors unknown
Dr. Bunch said there are some unknowns in the study, such as how long patients were in atrial fibrillation.
He said one way to address the inequities is to refer women earlier as women are often referred later in disease to specialty care, which can have consequences.
He said it is not known how many people underwent early and effective rhythm control.
“Women also are less likely to receive catheter ablation, a cardioversion, or be placed on antiarrhythmic drugs,” said Dr. Bunch, who was not part of the study. “These also represent potential opportunities to improve outcomes by treating the rhythm in a similar and aggressive manner in both men and women.”
Also unknown is how many people were on effective oral anticoagulation, Dr. Bunch noted.
The study importantly highlights a significant problem surrounding the care of women with AF, he said, but there are strategies to improve outcomes.
In addition to earlier screening and referral for women, providers should recognize that men and women may present differently with different AF symptoms. He added that physicians should offer catheter ablation, the most effective treatment, equally to men and women who are candidates.
In all people, he said, it’s important “to start anticoagulation very early in the disease to lower the risk of micro- and macrothrombotic events that lead to poor brain health and function.”
The study authors and Dr. Bunch declared no relevant financial relationships.
New data suggest a significantly stronger link in women compared with men between atrial fibrillation (AF) and mild cognitive impairment (MCI) and dementia.
“Our findings imply that women with AF may be at higher risk for MCI and dementia with potentially more rapid disease progression from normal cognition to MCI or dementia than women without AF or men with and without AF,” wrote authors of a new study led by Kathryn A. Wood, PhD, RN, Neil Hodgson Woodruff School of Nursing at Emory University in Atlanta.
The findings were published online in Alzheimer’s & Dementia.
Researchers used the National Alzheimer’s Coordinating Center data with 43,630 patients and analyzed sex differences between men and women with AF and their performance on neuropsychological tests and cognitive disease progression.
Higher odds of dementia, MCI in women
According to the paper, AF is associated with higher odds of dementia (odds ratio [OR], 3.00; 95% confidence interval [CI], 1.22-7.37) in women and MCI in women (OR, 3.43; 95% CI, 1.55-7.55) compared with men.
Women with AF and normal cognition at baseline had a higher risk of disease progression (hazard ratio [HR], 1.26; 95% CI, 1.06-1.50) from normal to MCI and from MCI to vascular dementia (HR, 3.27; 95% CI, 1.89-5.65) than that of men with AF or men and women without AF.
AF is a major public health problem linked with stroke and heart failure, and is an independent risk factor of increased mortality. It is associated with higher risk of cognitive impairment and dementia independent of stroke history.
Cognitive screening for AF patients
The authors wrote that cognitive screening, especially in women, should be part of yearly cardiology visits for patients with AF to help identify early those at highest risk for cognitive disease.
T. Jared Bunch, MD, professor of medicine in the division of cardiovascular medicine at University of Utah in Salt Lake City, said in an interview, “We have learned that how we treat atrial fibrillation can influence risk.”
First, he said, outcomes, including brain health, are better when rhythm control approaches are used within the first year of diagnosis.
“Restoring a normal heart rhythm improves brain perfusion and cognitive function. Next, aggressive rhythm control – such as catheter ablation – is associated with much lower long-term risks of dementia in the [patients]. Finally, early and effective use of anticoagulation in patients with atrial fibrillation lowers risk of stroke, dementia, and cognitive decline.”
Several factors unknown
Dr. Bunch said there are some unknowns in the study, such as how long patients were in atrial fibrillation.
He said one way to address the inequities is to refer women earlier as women are often referred later in disease to specialty care, which can have consequences.
He said it is not known how many people underwent early and effective rhythm control.
“Women also are less likely to receive catheter ablation, a cardioversion, or be placed on antiarrhythmic drugs,” said Dr. Bunch, who was not part of the study. “These also represent potential opportunities to improve outcomes by treating the rhythm in a similar and aggressive manner in both men and women.”
Also unknown is how many people were on effective oral anticoagulation, Dr. Bunch noted.
The study importantly highlights a significant problem surrounding the care of women with AF, he said, but there are strategies to improve outcomes.
In addition to earlier screening and referral for women, providers should recognize that men and women may present differently with different AF symptoms. He added that physicians should offer catheter ablation, the most effective treatment, equally to men and women who are candidates.
In all people, he said, it’s important “to start anticoagulation very early in the disease to lower the risk of micro- and macrothrombotic events that lead to poor brain health and function.”
The study authors and Dr. Bunch declared no relevant financial relationships.
New data suggest a significantly stronger link in women compared with men between atrial fibrillation (AF) and mild cognitive impairment (MCI) and dementia.
“Our findings imply that women with AF may be at higher risk for MCI and dementia with potentially more rapid disease progression from normal cognition to MCI or dementia than women without AF or men with and without AF,” wrote authors of a new study led by Kathryn A. Wood, PhD, RN, Neil Hodgson Woodruff School of Nursing at Emory University in Atlanta.
The findings were published online in Alzheimer’s & Dementia.
Researchers used the National Alzheimer’s Coordinating Center data with 43,630 patients and analyzed sex differences between men and women with AF and their performance on neuropsychological tests and cognitive disease progression.
Higher odds of dementia, MCI in women
According to the paper, AF is associated with higher odds of dementia (odds ratio [OR], 3.00; 95% confidence interval [CI], 1.22-7.37) in women and MCI in women (OR, 3.43; 95% CI, 1.55-7.55) compared with men.
Women with AF and normal cognition at baseline had a higher risk of disease progression (hazard ratio [HR], 1.26; 95% CI, 1.06-1.50) from normal to MCI and from MCI to vascular dementia (HR, 3.27; 95% CI, 1.89-5.65) than that of men with AF or men and women without AF.
AF is a major public health problem linked with stroke and heart failure, and is an independent risk factor of increased mortality. It is associated with higher risk of cognitive impairment and dementia independent of stroke history.
Cognitive screening for AF patients
The authors wrote that cognitive screening, especially in women, should be part of yearly cardiology visits for patients with AF to help identify early those at highest risk for cognitive disease.
T. Jared Bunch, MD, professor of medicine in the division of cardiovascular medicine at University of Utah in Salt Lake City, said in an interview, “We have learned that how we treat atrial fibrillation can influence risk.”
First, he said, outcomes, including brain health, are better when rhythm control approaches are used within the first year of diagnosis.
“Restoring a normal heart rhythm improves brain perfusion and cognitive function. Next, aggressive rhythm control – such as catheter ablation – is associated with much lower long-term risks of dementia in the [patients]. Finally, early and effective use of anticoagulation in patients with atrial fibrillation lowers risk of stroke, dementia, and cognitive decline.”
Several factors unknown
Dr. Bunch said there are some unknowns in the study, such as how long patients were in atrial fibrillation.
He said one way to address the inequities is to refer women earlier as women are often referred later in disease to specialty care, which can have consequences.
He said it is not known how many people underwent early and effective rhythm control.
“Women also are less likely to receive catheter ablation, a cardioversion, or be placed on antiarrhythmic drugs,” said Dr. Bunch, who was not part of the study. “These also represent potential opportunities to improve outcomes by treating the rhythm in a similar and aggressive manner in both men and women.”
Also unknown is how many people were on effective oral anticoagulation, Dr. Bunch noted.
The study importantly highlights a significant problem surrounding the care of women with AF, he said, but there are strategies to improve outcomes.
In addition to earlier screening and referral for women, providers should recognize that men and women may present differently with different AF symptoms. He added that physicians should offer catheter ablation, the most effective treatment, equally to men and women who are candidates.
In all people, he said, it’s important “to start anticoagulation very early in the disease to lower the risk of micro- and macrothrombotic events that lead to poor brain health and function.”
The study authors and Dr. Bunch declared no relevant financial relationships.
FROM ALZHEIMER’S & DEMENTIA
Migraine device expands treatment possibilities
AUSTIN, TEX – Migraine treatment and prevention is challenging in any population, but some present even more difficulties. Pregnant women and pediatric patients are two such groups where physicians and patients may be hesitant to use drugs.
Neuromodulation devices are proven alternatives to medical interventions, and the remote electrical neuromodulation device Nerivio (Theranica) was cleared by the Food and Drug Administration for acute treatment of migraine patients aged 12 and over in 2021. In March 2023, the agency expanded the clearance to include prevention of migration in adolescents aged 12 and over as well as adults.
Two studies presented at the annual meeting of the American Headache Society showed The latter study yielded similar findings to adults and was used by FDA in its decision to expand the device’s indication in adolescents in 2023, according to Teshamae Monteith, MD, who presented the study at a poster session.
The device, worn on the arm, allows the user to modulate the intensity of the stimulation so that it activates nociceptive pain receptors, but not in a painful way. “Each [patient] raises the intensity until it feels strong, yet comfortable, and when that happens, they activate the nociceptive receptors and the arm sends a signal all the way back up to the brainstem, where the pain control area is. Activating it causes the release of neurotransmitters that inhibit pain. That inhibition is a global pain inhibition mechanism, which causes inhibition of the migraine pain, and also the symptoms associated with migraine like photophobia and vomiting,” said Alit Stark-Inbar, PhD, who presented the study of treatment of pregnant women during a poster session.
Declining treatment days over time in adolescents
Dr. Monteith’s team studied high-frequency remote electrical neuromodulation device use in adolescents who had migraine on 10 days or more per month. They also required at least three treatment days in months 2 and 3 to control for the possibility that patients might stop using the device because they couldn’t afford it or for some reason other than efficacy or because their migraines went away.
The study included 83 adolescents aged 12-17 (mean, 15.9 years, 89% female). In the first month of use, the mean number of migraine treatment days was 12.6, which dropped to 9.0 in month 2 (P < .001), and 7.4 in month 3 (P < .001 from month 2). At 2 hours after treatment, 61.9% had pain relief, 24.5% had freedom from pain, 67.4% had functional disability relief, and 41.3% had functional disability freedom.
“It parallels the findings of the randomized, sham-controlled study in adults. The safety profile was excellent with just one person complaining of minor discomfort of the arm that resolved after treatment. The combination of the exceedingly safe profile and the likelihood of efficacy based on using monthly migraine treatment days as a proxy, the FDA decided to clear this for an adolescent indication,” said Dr. Monteith, associate professor of clinical neurology and chief of the headache division at the University of Miami.
The device design is convenient, according to Dr. Monteith. “The arm is just an easy place to stimulate. It’s a wearable device, and it’s 45 minutes [of treatment] and it’s app controlled. You know adolescents like their technology. They can track their symptoms here, and there’s some biobehavioral power to this because they can do biobehavioral exercises in addition to receiving the simulation,” she said.
The fact that the device is discrete is also an advantage for adolescents in school. “You have to go to the nurse to get your medication versus a device, you can just put it on, it’s easy, no one sees it, and no one’s making fun of you,” said Dr. Monteith.
Advantages for adolescents
The device offers a useful alternative to medication, according to Alan M. Rapoport, MD, who was asked for comment on the adolescent study. “I’d rather not give medication and certainly not preventive medication to an adolescent,” he said. He noted that over-the-counter acute care migraine medications such as aspirin or acetaminophen and combination medications with caffeine, as well as prescription medications such as triptans, “all have possible side effects, and when used to an increased extent can even cause medication overuse headache, increasing the severity and frequency of headache and migraine days per month,” Dr. Rapoport said. Using an effective device with almost no side effects is preferable to any of these acute care medications, especially if there are several headaches a month,” he said. Some newer medications that block calcitonin gene-related peptide might be quite effective when they are approved for adolescents, and should have few adverse events, he added.
In the past, Dr. Rapoport has favored biofeedback training for acute and especially preventive treatment of migraine in adolescents. “[Remote electrical neuromodulation] seems to do just as well, children enjoy it, and it’s easier for a patient to do at home,” said Dr. Rapoport.
Biofeedback training is usually taught to patients by a PhD psychologist. Once the patients have been on the biofeedback equipment and learn the techniques, they can practice on their own at home without equipment. “This new device treatment using Nerivio for acute care and prevention of migraine in adults and children 12 and older, where they can easily apply the device in almost any situation, whether they are at home or possibly even in school or out and about, looks very promising,” said Dr. Rapoport. It is quite effective and has almost no adverse events, which is what you really want, especially for adolescents,” he said.
Also asked to comment on the study of remote electrical neuromodulation use in adolescents, Abraham Avi Ashkenazi, MD, director of the Headache Clinic at Shaare Zedek Medical Center in Jerusalem, who attended the session, was enthusiastic, and said he has begun using it in his own practice. “It shows that remote electrical neuromodulation can not only be effective for the acute migraine attack, but also has a potential preventive effect on future migraine attacks. [This] actually makes sense, because we know that the more migraine attacks a person has, the more likely they are to progress to a more chronic form of the disease,” he said in an interview.
Asked what distinguishes REN from other neuromodulation therapies such as vagus nerve stimulation or transcranial magnetic stimulation (TMS), Dr. Ashkenazi said: “It’s just a different way of modulating the brain system via a different mechanism. In both ways, though, the advantage is that there are literally no adverse effects, as opposed to drug treatment.”
An alternative during pregnancy
Adolescents aren’t the only population where there is reluctance to use medication. Physicians have been prescribing the device for pregnant women, who are reluctant to take medication due to concerns effects on the fetus. However, pregnant women were not included in the pivotal studies. “They expect it to be safe. This study was done in order to validate that assumption. We reached out to women who either used the device during pregnancy or women from the same database who started it using afterwards, but did not use it during the pregnancy,” said Dr. Stark-Inbar, vice president of medical information at Theranica.
The study included 140 women, 59 in the remote electrical neuromodulation device group and 81 controls. The primary endpoint was gestational age, which was 38 weeks and 5 days in the remote electrical neuromodulation device group and 39 weeks among controls (P = .150). There were no significant between-group differences with respect to newborn birth weight, miscarriage rate, preterm birth rate, birth defect rate, developmental milestone rate, or emergency department visit rate.
Dr. Monteith and Dr. Ashkenazi have no relevant financial disclosures. Dr. Rapoport advises AbbVie, Biohaven, Cala Health, Dr. Reddy’s, Pfizer, Satsuma, Teva Pharmaceutical Industries, and Theranica. He is on the speakers bureau of AbbVie, Dr. Reddy’s, Impel, Pfizer and Teva Pharmaceutical Industries. Dr. Rapoport is the editor-in-chief of Neurology Reviews and on the editorial board of CNS Drugs.
AUSTIN, TEX – Migraine treatment and prevention is challenging in any population, but some present even more difficulties. Pregnant women and pediatric patients are two such groups where physicians and patients may be hesitant to use drugs.
Neuromodulation devices are proven alternatives to medical interventions, and the remote electrical neuromodulation device Nerivio (Theranica) was cleared by the Food and Drug Administration for acute treatment of migraine patients aged 12 and over in 2021. In March 2023, the agency expanded the clearance to include prevention of migration in adolescents aged 12 and over as well as adults.
Two studies presented at the annual meeting of the American Headache Society showed The latter study yielded similar findings to adults and was used by FDA in its decision to expand the device’s indication in adolescents in 2023, according to Teshamae Monteith, MD, who presented the study at a poster session.
The device, worn on the arm, allows the user to modulate the intensity of the stimulation so that it activates nociceptive pain receptors, but not in a painful way. “Each [patient] raises the intensity until it feels strong, yet comfortable, and when that happens, they activate the nociceptive receptors and the arm sends a signal all the way back up to the brainstem, where the pain control area is. Activating it causes the release of neurotransmitters that inhibit pain. That inhibition is a global pain inhibition mechanism, which causes inhibition of the migraine pain, and also the symptoms associated with migraine like photophobia and vomiting,” said Alit Stark-Inbar, PhD, who presented the study of treatment of pregnant women during a poster session.
Declining treatment days over time in adolescents
Dr. Monteith’s team studied high-frequency remote electrical neuromodulation device use in adolescents who had migraine on 10 days or more per month. They also required at least three treatment days in months 2 and 3 to control for the possibility that patients might stop using the device because they couldn’t afford it or for some reason other than efficacy or because their migraines went away.
The study included 83 adolescents aged 12-17 (mean, 15.9 years, 89% female). In the first month of use, the mean number of migraine treatment days was 12.6, which dropped to 9.0 in month 2 (P < .001), and 7.4 in month 3 (P < .001 from month 2). At 2 hours after treatment, 61.9% had pain relief, 24.5% had freedom from pain, 67.4% had functional disability relief, and 41.3% had functional disability freedom.
“It parallels the findings of the randomized, sham-controlled study in adults. The safety profile was excellent with just one person complaining of minor discomfort of the arm that resolved after treatment. The combination of the exceedingly safe profile and the likelihood of efficacy based on using monthly migraine treatment days as a proxy, the FDA decided to clear this for an adolescent indication,” said Dr. Monteith, associate professor of clinical neurology and chief of the headache division at the University of Miami.
The device design is convenient, according to Dr. Monteith. “The arm is just an easy place to stimulate. It’s a wearable device, and it’s 45 minutes [of treatment] and it’s app controlled. You know adolescents like their technology. They can track their symptoms here, and there’s some biobehavioral power to this because they can do biobehavioral exercises in addition to receiving the simulation,” she said.
The fact that the device is discrete is also an advantage for adolescents in school. “You have to go to the nurse to get your medication versus a device, you can just put it on, it’s easy, no one sees it, and no one’s making fun of you,” said Dr. Monteith.
Advantages for adolescents
The device offers a useful alternative to medication, according to Alan M. Rapoport, MD, who was asked for comment on the adolescent study. “I’d rather not give medication and certainly not preventive medication to an adolescent,” he said. He noted that over-the-counter acute care migraine medications such as aspirin or acetaminophen and combination medications with caffeine, as well as prescription medications such as triptans, “all have possible side effects, and when used to an increased extent can even cause medication overuse headache, increasing the severity and frequency of headache and migraine days per month,” Dr. Rapoport said. Using an effective device with almost no side effects is preferable to any of these acute care medications, especially if there are several headaches a month,” he said. Some newer medications that block calcitonin gene-related peptide might be quite effective when they are approved for adolescents, and should have few adverse events, he added.
In the past, Dr. Rapoport has favored biofeedback training for acute and especially preventive treatment of migraine in adolescents. “[Remote electrical neuromodulation] seems to do just as well, children enjoy it, and it’s easier for a patient to do at home,” said Dr. Rapoport.
Biofeedback training is usually taught to patients by a PhD psychologist. Once the patients have been on the biofeedback equipment and learn the techniques, they can practice on their own at home without equipment. “This new device treatment using Nerivio for acute care and prevention of migraine in adults and children 12 and older, where they can easily apply the device in almost any situation, whether they are at home or possibly even in school or out and about, looks very promising,” said Dr. Rapoport. It is quite effective and has almost no adverse events, which is what you really want, especially for adolescents,” he said.
Also asked to comment on the study of remote electrical neuromodulation use in adolescents, Abraham Avi Ashkenazi, MD, director of the Headache Clinic at Shaare Zedek Medical Center in Jerusalem, who attended the session, was enthusiastic, and said he has begun using it in his own practice. “It shows that remote electrical neuromodulation can not only be effective for the acute migraine attack, but also has a potential preventive effect on future migraine attacks. [This] actually makes sense, because we know that the more migraine attacks a person has, the more likely they are to progress to a more chronic form of the disease,” he said in an interview.
Asked what distinguishes REN from other neuromodulation therapies such as vagus nerve stimulation or transcranial magnetic stimulation (TMS), Dr. Ashkenazi said: “It’s just a different way of modulating the brain system via a different mechanism. In both ways, though, the advantage is that there are literally no adverse effects, as opposed to drug treatment.”
An alternative during pregnancy
Adolescents aren’t the only population where there is reluctance to use medication. Physicians have been prescribing the device for pregnant women, who are reluctant to take medication due to concerns effects on the fetus. However, pregnant women were not included in the pivotal studies. “They expect it to be safe. This study was done in order to validate that assumption. We reached out to women who either used the device during pregnancy or women from the same database who started it using afterwards, but did not use it during the pregnancy,” said Dr. Stark-Inbar, vice president of medical information at Theranica.
The study included 140 women, 59 in the remote electrical neuromodulation device group and 81 controls. The primary endpoint was gestational age, which was 38 weeks and 5 days in the remote electrical neuromodulation device group and 39 weeks among controls (P = .150). There were no significant between-group differences with respect to newborn birth weight, miscarriage rate, preterm birth rate, birth defect rate, developmental milestone rate, or emergency department visit rate.
Dr. Monteith and Dr. Ashkenazi have no relevant financial disclosures. Dr. Rapoport advises AbbVie, Biohaven, Cala Health, Dr. Reddy’s, Pfizer, Satsuma, Teva Pharmaceutical Industries, and Theranica. He is on the speakers bureau of AbbVie, Dr. Reddy’s, Impel, Pfizer and Teva Pharmaceutical Industries. Dr. Rapoport is the editor-in-chief of Neurology Reviews and on the editorial board of CNS Drugs.
AUSTIN, TEX – Migraine treatment and prevention is challenging in any population, but some present even more difficulties. Pregnant women and pediatric patients are two such groups where physicians and patients may be hesitant to use drugs.
Neuromodulation devices are proven alternatives to medical interventions, and the remote electrical neuromodulation device Nerivio (Theranica) was cleared by the Food and Drug Administration for acute treatment of migraine patients aged 12 and over in 2021. In March 2023, the agency expanded the clearance to include prevention of migration in adolescents aged 12 and over as well as adults.
Two studies presented at the annual meeting of the American Headache Society showed The latter study yielded similar findings to adults and was used by FDA in its decision to expand the device’s indication in adolescents in 2023, according to Teshamae Monteith, MD, who presented the study at a poster session.
The device, worn on the arm, allows the user to modulate the intensity of the stimulation so that it activates nociceptive pain receptors, but not in a painful way. “Each [patient] raises the intensity until it feels strong, yet comfortable, and when that happens, they activate the nociceptive receptors and the arm sends a signal all the way back up to the brainstem, where the pain control area is. Activating it causes the release of neurotransmitters that inhibit pain. That inhibition is a global pain inhibition mechanism, which causes inhibition of the migraine pain, and also the symptoms associated with migraine like photophobia and vomiting,” said Alit Stark-Inbar, PhD, who presented the study of treatment of pregnant women during a poster session.
Declining treatment days over time in adolescents
Dr. Monteith’s team studied high-frequency remote electrical neuromodulation device use in adolescents who had migraine on 10 days or more per month. They also required at least three treatment days in months 2 and 3 to control for the possibility that patients might stop using the device because they couldn’t afford it or for some reason other than efficacy or because their migraines went away.
The study included 83 adolescents aged 12-17 (mean, 15.9 years, 89% female). In the first month of use, the mean number of migraine treatment days was 12.6, which dropped to 9.0 in month 2 (P < .001), and 7.4 in month 3 (P < .001 from month 2). At 2 hours after treatment, 61.9% had pain relief, 24.5% had freedom from pain, 67.4% had functional disability relief, and 41.3% had functional disability freedom.
“It parallels the findings of the randomized, sham-controlled study in adults. The safety profile was excellent with just one person complaining of minor discomfort of the arm that resolved after treatment. The combination of the exceedingly safe profile and the likelihood of efficacy based on using monthly migraine treatment days as a proxy, the FDA decided to clear this for an adolescent indication,” said Dr. Monteith, associate professor of clinical neurology and chief of the headache division at the University of Miami.
The device design is convenient, according to Dr. Monteith. “The arm is just an easy place to stimulate. It’s a wearable device, and it’s 45 minutes [of treatment] and it’s app controlled. You know adolescents like their technology. They can track their symptoms here, and there’s some biobehavioral power to this because they can do biobehavioral exercises in addition to receiving the simulation,” she said.
The fact that the device is discrete is also an advantage for adolescents in school. “You have to go to the nurse to get your medication versus a device, you can just put it on, it’s easy, no one sees it, and no one’s making fun of you,” said Dr. Monteith.
Advantages for adolescents
The device offers a useful alternative to medication, according to Alan M. Rapoport, MD, who was asked for comment on the adolescent study. “I’d rather not give medication and certainly not preventive medication to an adolescent,” he said. He noted that over-the-counter acute care migraine medications such as aspirin or acetaminophen and combination medications with caffeine, as well as prescription medications such as triptans, “all have possible side effects, and when used to an increased extent can even cause medication overuse headache, increasing the severity and frequency of headache and migraine days per month,” Dr. Rapoport said. Using an effective device with almost no side effects is preferable to any of these acute care medications, especially if there are several headaches a month,” he said. Some newer medications that block calcitonin gene-related peptide might be quite effective when they are approved for adolescents, and should have few adverse events, he added.
In the past, Dr. Rapoport has favored biofeedback training for acute and especially preventive treatment of migraine in adolescents. “[Remote electrical neuromodulation] seems to do just as well, children enjoy it, and it’s easier for a patient to do at home,” said Dr. Rapoport.
Biofeedback training is usually taught to patients by a PhD psychologist. Once the patients have been on the biofeedback equipment and learn the techniques, they can practice on their own at home without equipment. “This new device treatment using Nerivio for acute care and prevention of migraine in adults and children 12 and older, where they can easily apply the device in almost any situation, whether they are at home or possibly even in school or out and about, looks very promising,” said Dr. Rapoport. It is quite effective and has almost no adverse events, which is what you really want, especially for adolescents,” he said.
Also asked to comment on the study of remote electrical neuromodulation use in adolescents, Abraham Avi Ashkenazi, MD, director of the Headache Clinic at Shaare Zedek Medical Center in Jerusalem, who attended the session, was enthusiastic, and said he has begun using it in his own practice. “It shows that remote electrical neuromodulation can not only be effective for the acute migraine attack, but also has a potential preventive effect on future migraine attacks. [This] actually makes sense, because we know that the more migraine attacks a person has, the more likely they are to progress to a more chronic form of the disease,” he said in an interview.
Asked what distinguishes REN from other neuromodulation therapies such as vagus nerve stimulation or transcranial magnetic stimulation (TMS), Dr. Ashkenazi said: “It’s just a different way of modulating the brain system via a different mechanism. In both ways, though, the advantage is that there are literally no adverse effects, as opposed to drug treatment.”
An alternative during pregnancy
Adolescents aren’t the only population where there is reluctance to use medication. Physicians have been prescribing the device for pregnant women, who are reluctant to take medication due to concerns effects on the fetus. However, pregnant women were not included in the pivotal studies. “They expect it to be safe. This study was done in order to validate that assumption. We reached out to women who either used the device during pregnancy or women from the same database who started it using afterwards, but did not use it during the pregnancy,” said Dr. Stark-Inbar, vice president of medical information at Theranica.
The study included 140 women, 59 in the remote electrical neuromodulation device group and 81 controls. The primary endpoint was gestational age, which was 38 weeks and 5 days in the remote electrical neuromodulation device group and 39 weeks among controls (P = .150). There were no significant between-group differences with respect to newborn birth weight, miscarriage rate, preterm birth rate, birth defect rate, developmental milestone rate, or emergency department visit rate.
Dr. Monteith and Dr. Ashkenazi have no relevant financial disclosures. Dr. Rapoport advises AbbVie, Biohaven, Cala Health, Dr. Reddy’s, Pfizer, Satsuma, Teva Pharmaceutical Industries, and Theranica. He is on the speakers bureau of AbbVie, Dr. Reddy’s, Impel, Pfizer and Teva Pharmaceutical Industries. Dr. Rapoport is the editor-in-chief of Neurology Reviews and on the editorial board of CNS Drugs.
AT AHS 2023