User login
Removal from play reduces concussion recovery time in athletes
Sport-related concussion (SRC) recovery time can be reduced if athletes are removed from game participation, according to R.J. Elbin, PhD, of the University of Arkansas, Fayetteville, and his associates.
In the prospective study, 95 athletes sought care for an SRC at a concussion specialty clinic between Sept. 1 and Dec. 1, 2014. The athletes were divided into two groups: those who continued to play after experiencing signs and symptoms of an SRC and those who were immediately removed from play. The played group took longer to recover (44 days) than did the removed group (22 days) (P = .003).
Post hoc analyses revealed that the played group demonstrated significantly worse verbal and visual memory, processing speed, and reaction time, and higher symptoms (all P less than or equal to .001), compared with the removed group at 1-7 days. From 8 to 30 days post injury, the played group demonstrated worse verbal memory (P = .009), visual memory (P less than or equal to .001), processing speed (P = .001), and greater symptoms (P = .001), compared with the removed group.
The study also showed that athletes in the played group were 8.80 times more likely to experience a protracted recovery, compared with athletes in the removed group (21 days or longer) (P less than .001). Athletes participated in a variety of sports including football, soccer, ice hockey, volleyball, field hockey, rugby, basketball, and wrestling.
“This study is the first to show that athletes who continue to play with an SRC experience a longer recovery and more time away from the sport,” researchers concluded. “These findings should be incorporated into SRC education and awareness programs for athletes, coaches, parents, and medical professionals.”
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0910).
Sport-related concussion (SRC) recovery time can be reduced if athletes are removed from game participation, according to R.J. Elbin, PhD, of the University of Arkansas, Fayetteville, and his associates.
In the prospective study, 95 athletes sought care for an SRC at a concussion specialty clinic between Sept. 1 and Dec. 1, 2014. The athletes were divided into two groups: those who continued to play after experiencing signs and symptoms of an SRC and those who were immediately removed from play. The played group took longer to recover (44 days) than did the removed group (22 days) (P = .003).
Post hoc analyses revealed that the played group demonstrated significantly worse verbal and visual memory, processing speed, and reaction time, and higher symptoms (all P less than or equal to .001), compared with the removed group at 1-7 days. From 8 to 30 days post injury, the played group demonstrated worse verbal memory (P = .009), visual memory (P less than or equal to .001), processing speed (P = .001), and greater symptoms (P = .001), compared with the removed group.
The study also showed that athletes in the played group were 8.80 times more likely to experience a protracted recovery, compared with athletes in the removed group (21 days or longer) (P less than .001). Athletes participated in a variety of sports including football, soccer, ice hockey, volleyball, field hockey, rugby, basketball, and wrestling.
“This study is the first to show that athletes who continue to play with an SRC experience a longer recovery and more time away from the sport,” researchers concluded. “These findings should be incorporated into SRC education and awareness programs for athletes, coaches, parents, and medical professionals.”
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0910).
Sport-related concussion (SRC) recovery time can be reduced if athletes are removed from game participation, according to R.J. Elbin, PhD, of the University of Arkansas, Fayetteville, and his associates.
In the prospective study, 95 athletes sought care for an SRC at a concussion specialty clinic between Sept. 1 and Dec. 1, 2014. The athletes were divided into two groups: those who continued to play after experiencing signs and symptoms of an SRC and those who were immediately removed from play. The played group took longer to recover (44 days) than did the removed group (22 days) (P = .003).
Post hoc analyses revealed that the played group demonstrated significantly worse verbal and visual memory, processing speed, and reaction time, and higher symptoms (all P less than or equal to .001), compared with the removed group at 1-7 days. From 8 to 30 days post injury, the played group demonstrated worse verbal memory (P = .009), visual memory (P less than or equal to .001), processing speed (P = .001), and greater symptoms (P = .001), compared with the removed group.
The study also showed that athletes in the played group were 8.80 times more likely to experience a protracted recovery, compared with athletes in the removed group (21 days or longer) (P less than .001). Athletes participated in a variety of sports including football, soccer, ice hockey, volleyball, field hockey, rugby, basketball, and wrestling.
“This study is the first to show that athletes who continue to play with an SRC experience a longer recovery and more time away from the sport,” researchers concluded. “These findings should be incorporated into SRC education and awareness programs for athletes, coaches, parents, and medical professionals.”
Find the full study in Pediatrics (doi: 10.1542/peds.2016-0910).
FROM PEDIATRICS
New and Noteworthy Information—September 2016
Hospitalization of patients with stroke in primary stroke centers, compared with noncertified hospitals, is associated with decreased seven-day and 30-day case fatality, according to a study published online ahead of print July 25 in JAMA Internal Medicine. Among 865,184 elderly patients with stroke (mean age, 78.9; 55.5% female), 53.9% were treated in primary stroke centers. Admission to primary stroke centers was associated with 1.8% lower seven-day and 1.8% lower 30-day case fatality. Fifty-six patients with stroke needed to be treated in primary stroke centers to save one life at 30 days. Overall, receiving treatment in primary stroke centers was associated with a 30-day survival benefit for patients traveling less than 90 minutes, but traveling at least 90 minutes offset any benefit of care in primary stroke centers.
Obesity may increase the risk of neurodegeneration, according to a study published online ahead of print July 27 in Neurobiology of Aging. Participants were a population-based cohort of cognitively healthy adults recruited over a five-year period. In all, 527 subjects with an age range of 20 to 87 were included. Researchers performed a cross-sectional analysis of MRI-based brain structure and found a statistically significant interaction between age and BMI. Cortical reconstruction techniques were used to generate measures of whole brain cerebral white matter volume, cortical thickness, and surface area. Cerebral white matter volume in overweight and obese individuals was associated with a greater degree of atrophy, with maximal effects in middle age corresponding to an estimated increase in brain age of 10 years.
Thymectomy improves clinical outcomes over a three-year period in patients with nonthymomatous myasthenia gravis, according to a study published August 11 in the New England Journal of Medicine. Researchers randomized 126 patients to thymectomy plus alternate-day prednisone or alternate-day prednisone alone. Patients who underwent thymectomy had a lower time-weighted average Quantitative Myasthenia Gravis score over a three-year period than those who received prednisone alone. Patients in the thymectomy group also had a lower average requirement for alternate-day prednisone. Fewer patients in the thymectomy group than in the prednisone-only group required immunosuppression with azathioprine or were hospitalized for exacerbations. The number of patients with treatment-associated complications did not differ significantly between groups. However, patients in the thymectomy group had fewer treatment-associated symptoms related to immunosuppressive medications.
Calcium supplementation may increase the risk of developing dementia in elderly women with cerebrovascular disease, according to a study published online ahead of print August 17 in Neurology. This longitudinal population-based study included 700 women without dementia between ages 70 and 92. At baseline and at five-year follow-up, the women underwent comprehensive neuropsychiatric and somatic examinations. A CT scan also was performed in 447 participants at baseline. Information on the use and dosage of calcium supplements was collected. Women treated with calcium supplements had a higher risk of developing dementia and the subtype of stroke-related dementia. Calcium supplementation was associated with the development of dementia in groups with a history of stroke or presence of white matter lesions, but not in groups without these conditions.
Exposure to bright light during the day may help combat sleep disturbances associated with the evening use of electronic devices emitting blue light, according to a study published online ahead of print June 16 in Sleep Medicine. Following a constant bright light exposure over 6.5 hours, 14 participants read a novel either on a tablet or as a physical book for two hours. Evening concentrations of saliva melatonin were measured repeatedly. Sleepiness was assessed before and after nocturnal sleep. About one week later, experiments were repeated. Participants who had read the novel on a tablet in the first experimental session continued reading the same novel as a physical book, and vice versa. There were no differences in sleep parameters and presleep saliva melatonin levels between the tablet reading and physical book reading conditions.
Treatment immediately after clinically isolated syndrome (CIS) is more beneficial than delayed treatment, according to a study published online ahead of print August 10 in Neurology. Researchers randomized 278 people with CIS to interferon beta-1b or placebo. After two years or a diagnosis of multiple sclerosis (MS), patients receiving placebo could receive treatment. After 11 years, risk of clinically definite MS remained lower in the early-treatment arm, compared with the delayed-treatment arm, with longer time to first relapse and lower overall annualized relapse rate. Twenty-five patients converted to secondary progressive MS. Expanded Disability Status Scale scores remained low and stable, with no difference between treatment arms. The early-treatment group had better Paced Auditory Serial Addition Task-3 total scores. Health resource utilization was low in both groups.
Patients with anemia have increased mortality after stroke, according to a study published online ahead of print August 17 in the Journal of the American Heart Association. Researchers analyzed data from a cohort of 8,013 patients with stroke who were consecutively admitted over 11 years. Anemia was present in 24.5% of the cohort on admission and was associated with increased odds of mortality at most of the time points examined up to one year following stroke. Elevated hemoglobin also was associated with increased mortality. In addition, investigators conducted a systematic review using various databases. When combined with the cohort from the current study, the pooled population had 29,943 patients with stroke. Anemia on admission was associated with an increased risk of mortality in ischemic stroke and hemorrhagic stroke.
Bedside EEG methods may indicate the level of awareness of patients in a vegetative state, according to a study published online ahead of print August 4 in Annals of Neurology. Fourteen patients with severe brain injuries were evaluated with an EEG vibrotactile attention task designed to identify a hierarchy of residual somatosensory and cognitive abilities. Each patient also was assessed with a clinical behavioral scale and two fMRI assessments of covert command following. Six patients produced only sensory responses, with no evidence of cognitive event-related potentials. Furthermore, eight patients demonstrated reliable bottom-up attention-orienting responses. No patient showed evidence of top-down attention. Only patients who followed commands, whether overtly with behavior or covertly with functional neuroimaging, also demonstrated event-related potential evidence of attentional orienting.
The PET tracer [18F]-AV-1451 may help identify the stages of the preclinical and clinical phases of Alzheimer's disease, according to a study published online ahead of print July 25 in JAMA Neurology. In all, 59 participants (64% male; mean age, 74) underwent PET imaging. The [18F]-AV-1451 standardized uptake value ratio (SUVR) in the hippocampus and Alzheimer's disease cortical signature regions distinguished participants with Alzheimer's disease from cognitively normal participants. A SUVR cutoff value of 1.19 from Alzheimer's disease cortical signature regions best distinguished these groups. Amyloid β-positivity was associated with an elevated [18F]-AV-1451 SUVR in Alzheimer's disease cortical signature regions, but not in the hippocampus. Amyloid β-positivity alone was not related to hippocampal volume or Alzheimer's disease signature cortical thickness. An elevated [18F]-AV-1451 SUVR was associated with brain volumetric loss.
Symptom exacerbations after concussion are common among children and may not impede recovery, according to a study published online ahead of print August 1 in JAMA Pediatrics. Eligible participants were between ages 11 and 18 and had sustained a concussion that did not result in an abnormal CT scan or require hospital admission. The mean age of the 63 participants (34.9% girls) was 13.8. Symptom spikes occurred in 31.7% of the sample. An abrupt increase in mental activity from one day to the next increased the risk of a symptom spike. Patients with symptom spikes were initially more symptomatic in the emergency department and throughout the observation period, but did not differ from the group without symptom spikes on cognition or balance 10 days following injury.
The FDA has approved the supplemental Biologics License Application from Ipsen Biopharmaceuticals for Dysport (abobotulinumtoxinA) for injection in the treatment of lower limb spasticity in pediatric patients age 2 and older. This approval is based on a phase III pivotal study of 235 pediatric patients ages 2 to 17 with lower limb spasticity because of cerebral palsy causing dynamic equinus foot deformity. Patients treated with Dysport showed statistically significant improvement in ankle plantar flexor muscle tone. Like all botulinum toxin products, Dysport has a boxed warning stating that the effects of the botulinum toxin may spread from the area of injection to other areas of the body, causing symptoms similar to those of botulism. Ipsen Biopharmaceuticals is headquartered in Basking Ridge, New Jersey.
Lower BMI in late life is associated with greater cortical amyloid burden, according to a study published June 18 in the Journal of Alzheimer's Disease. The study entailed cross-sectional analyses that were completed using baseline data from the Harvard Aging Brain Study, which included 280 cognitively normal adults ages 62 to 90. Assessments included medical histories and physical exams, Pittsburgh compound B (PiB) PET amyloid imaging, and APOE4 genotyping. In the primary analysis, greater PiB retention was associated with lower BMI. In the secondary analyses, APOE4 carrier status and normal BMI, as opposed to overweight or obese BMI, were associated with greater PiB retention. The interaction between BMI and APOE4 also was significant. Future studies should seek to clarify the mechanism of this association, said the researchers.
Sleep-disordered breathing (SDB) and sleep-wake disturbances (SWD) increase the risk of stroke in the general population and affect short- and long-term stroke recovery and outcome, according to a literature review published online ahead of print August 3 in Neurology. Several studies have proven SDB to represent an independent risk factor for stroke. Sleep studies in patients with transient ischemic attack or stroke are recommended in view of the high prevalence of SDB, said the researchers. Treatment of obstructive SDB with continuous positive airway pressure is recommended, given the strength of the evidence that supports the treatment's benefit. Oxygen, biphasic positive airway pressure, and adaptive servoventilation may be considered in patients with central SDB, said the researchers. Experimental studies found that SWD may impair neuroplasticity and functional stroke recovery.
—Kimberly Williams
Hospitalization of patients with stroke in primary stroke centers, compared with noncertified hospitals, is associated with decreased seven-day and 30-day case fatality, according to a study published online ahead of print July 25 in JAMA Internal Medicine. Among 865,184 elderly patients with stroke (mean age, 78.9; 55.5% female), 53.9% were treated in primary stroke centers. Admission to primary stroke centers was associated with 1.8% lower seven-day and 1.8% lower 30-day case fatality. Fifty-six patients with stroke needed to be treated in primary stroke centers to save one life at 30 days. Overall, receiving treatment in primary stroke centers was associated with a 30-day survival benefit for patients traveling less than 90 minutes, but traveling at least 90 minutes offset any benefit of care in primary stroke centers.
Obesity may increase the risk of neurodegeneration, according to a study published online ahead of print July 27 in Neurobiology of Aging. Participants were a population-based cohort of cognitively healthy adults recruited over a five-year period. In all, 527 subjects with an age range of 20 to 87 were included. Researchers performed a cross-sectional analysis of MRI-based brain structure and found a statistically significant interaction between age and BMI. Cortical reconstruction techniques were used to generate measures of whole brain cerebral white matter volume, cortical thickness, and surface area. Cerebral white matter volume in overweight and obese individuals was associated with a greater degree of atrophy, with maximal effects in middle age corresponding to an estimated increase in brain age of 10 years.
Thymectomy improves clinical outcomes over a three-year period in patients with nonthymomatous myasthenia gravis, according to a study published August 11 in the New England Journal of Medicine. Researchers randomized 126 patients to thymectomy plus alternate-day prednisone or alternate-day prednisone alone. Patients who underwent thymectomy had a lower time-weighted average Quantitative Myasthenia Gravis score over a three-year period than those who received prednisone alone. Patients in the thymectomy group also had a lower average requirement for alternate-day prednisone. Fewer patients in the thymectomy group than in the prednisone-only group required immunosuppression with azathioprine or were hospitalized for exacerbations. The number of patients with treatment-associated complications did not differ significantly between groups. However, patients in the thymectomy group had fewer treatment-associated symptoms related to immunosuppressive medications.
Calcium supplementation may increase the risk of developing dementia in elderly women with cerebrovascular disease, according to a study published online ahead of print August 17 in Neurology. This longitudinal population-based study included 700 women without dementia between ages 70 and 92. At baseline and at five-year follow-up, the women underwent comprehensive neuropsychiatric and somatic examinations. A CT scan also was performed in 447 participants at baseline. Information on the use and dosage of calcium supplements was collected. Women treated with calcium supplements had a higher risk of developing dementia and the subtype of stroke-related dementia. Calcium supplementation was associated with the development of dementia in groups with a history of stroke or presence of white matter lesions, but not in groups without these conditions.
Exposure to bright light during the day may help combat sleep disturbances associated with the evening use of electronic devices emitting blue light, according to a study published online ahead of print June 16 in Sleep Medicine. Following a constant bright light exposure over 6.5 hours, 14 participants read a novel either on a tablet or as a physical book for two hours. Evening concentrations of saliva melatonin were measured repeatedly. Sleepiness was assessed before and after nocturnal sleep. About one week later, experiments were repeated. Participants who had read the novel on a tablet in the first experimental session continued reading the same novel as a physical book, and vice versa. There were no differences in sleep parameters and presleep saliva melatonin levels between the tablet reading and physical book reading conditions.
Treatment immediately after clinically isolated syndrome (CIS) is more beneficial than delayed treatment, according to a study published online ahead of print August 10 in Neurology. Researchers randomized 278 people with CIS to interferon beta-1b or placebo. After two years or a diagnosis of multiple sclerosis (MS), patients receiving placebo could receive treatment. After 11 years, risk of clinically definite MS remained lower in the early-treatment arm, compared with the delayed-treatment arm, with longer time to first relapse and lower overall annualized relapse rate. Twenty-five patients converted to secondary progressive MS. Expanded Disability Status Scale scores remained low and stable, with no difference between treatment arms. The early-treatment group had better Paced Auditory Serial Addition Task-3 total scores. Health resource utilization was low in both groups.
Patients with anemia have increased mortality after stroke, according to a study published online ahead of print August 17 in the Journal of the American Heart Association. Researchers analyzed data from a cohort of 8,013 patients with stroke who were consecutively admitted over 11 years. Anemia was present in 24.5% of the cohort on admission and was associated with increased odds of mortality at most of the time points examined up to one year following stroke. Elevated hemoglobin also was associated with increased mortality. In addition, investigators conducted a systematic review using various databases. When combined with the cohort from the current study, the pooled population had 29,943 patients with stroke. Anemia on admission was associated with an increased risk of mortality in ischemic stroke and hemorrhagic stroke.
Bedside EEG methods may indicate the level of awareness of patients in a vegetative state, according to a study published online ahead of print August 4 in Annals of Neurology. Fourteen patients with severe brain injuries were evaluated with an EEG vibrotactile attention task designed to identify a hierarchy of residual somatosensory and cognitive abilities. Each patient also was assessed with a clinical behavioral scale and two fMRI assessments of covert command following. Six patients produced only sensory responses, with no evidence of cognitive event-related potentials. Furthermore, eight patients demonstrated reliable bottom-up attention-orienting responses. No patient showed evidence of top-down attention. Only patients who followed commands, whether overtly with behavior or covertly with functional neuroimaging, also demonstrated event-related potential evidence of attentional orienting.
The PET tracer [18F]-AV-1451 may help identify the stages of the preclinical and clinical phases of Alzheimer's disease, according to a study published online ahead of print July 25 in JAMA Neurology. In all, 59 participants (64% male; mean age, 74) underwent PET imaging. The [18F]-AV-1451 standardized uptake value ratio (SUVR) in the hippocampus and Alzheimer's disease cortical signature regions distinguished participants with Alzheimer's disease from cognitively normal participants. A SUVR cutoff value of 1.19 from Alzheimer's disease cortical signature regions best distinguished these groups. Amyloid β-positivity was associated with an elevated [18F]-AV-1451 SUVR in Alzheimer's disease cortical signature regions, but not in the hippocampus. Amyloid β-positivity alone was not related to hippocampal volume or Alzheimer's disease signature cortical thickness. An elevated [18F]-AV-1451 SUVR was associated with brain volumetric loss.
Symptom exacerbations after concussion are common among children and may not impede recovery, according to a study published online ahead of print August 1 in JAMA Pediatrics. Eligible participants were between ages 11 and 18 and had sustained a concussion that did not result in an abnormal CT scan or require hospital admission. The mean age of the 63 participants (34.9% girls) was 13.8. Symptom spikes occurred in 31.7% of the sample. An abrupt increase in mental activity from one day to the next increased the risk of a symptom spike. Patients with symptom spikes were initially more symptomatic in the emergency department and throughout the observation period, but did not differ from the group without symptom spikes on cognition or balance 10 days following injury.
The FDA has approved the supplemental Biologics License Application from Ipsen Biopharmaceuticals for Dysport (abobotulinumtoxinA) for injection in the treatment of lower limb spasticity in pediatric patients age 2 and older. This approval is based on a phase III pivotal study of 235 pediatric patients ages 2 to 17 with lower limb spasticity because of cerebral palsy causing dynamic equinus foot deformity. Patients treated with Dysport showed statistically significant improvement in ankle plantar flexor muscle tone. Like all botulinum toxin products, Dysport has a boxed warning stating that the effects of the botulinum toxin may spread from the area of injection to other areas of the body, causing symptoms similar to those of botulism. Ipsen Biopharmaceuticals is headquartered in Basking Ridge, New Jersey.
Lower BMI in late life is associated with greater cortical amyloid burden, according to a study published June 18 in the Journal of Alzheimer's Disease. The study entailed cross-sectional analyses that were completed using baseline data from the Harvard Aging Brain Study, which included 280 cognitively normal adults ages 62 to 90. Assessments included medical histories and physical exams, Pittsburgh compound B (PiB) PET amyloid imaging, and APOE4 genotyping. In the primary analysis, greater PiB retention was associated with lower BMI. In the secondary analyses, APOE4 carrier status and normal BMI, as opposed to overweight or obese BMI, were associated with greater PiB retention. The interaction between BMI and APOE4 also was significant. Future studies should seek to clarify the mechanism of this association, said the researchers.
Sleep-disordered breathing (SDB) and sleep-wake disturbances (SWD) increase the risk of stroke in the general population and affect short- and long-term stroke recovery and outcome, according to a literature review published online ahead of print August 3 in Neurology. Several studies have proven SDB to represent an independent risk factor for stroke. Sleep studies in patients with transient ischemic attack or stroke are recommended in view of the high prevalence of SDB, said the researchers. Treatment of obstructive SDB with continuous positive airway pressure is recommended, given the strength of the evidence that supports the treatment's benefit. Oxygen, biphasic positive airway pressure, and adaptive servoventilation may be considered in patients with central SDB, said the researchers. Experimental studies found that SWD may impair neuroplasticity and functional stroke recovery.
—Kimberly Williams
Hospitalization of patients with stroke in primary stroke centers, compared with noncertified hospitals, is associated with decreased seven-day and 30-day case fatality, according to a study published online ahead of print July 25 in JAMA Internal Medicine. Among 865,184 elderly patients with stroke (mean age, 78.9; 55.5% female), 53.9% were treated in primary stroke centers. Admission to primary stroke centers was associated with 1.8% lower seven-day and 1.8% lower 30-day case fatality. Fifty-six patients with stroke needed to be treated in primary stroke centers to save one life at 30 days. Overall, receiving treatment in primary stroke centers was associated with a 30-day survival benefit for patients traveling less than 90 minutes, but traveling at least 90 minutes offset any benefit of care in primary stroke centers.
Obesity may increase the risk of neurodegeneration, according to a study published online ahead of print July 27 in Neurobiology of Aging. Participants were a population-based cohort of cognitively healthy adults recruited over a five-year period. In all, 527 subjects with an age range of 20 to 87 were included. Researchers performed a cross-sectional analysis of MRI-based brain structure and found a statistically significant interaction between age and BMI. Cortical reconstruction techniques were used to generate measures of whole brain cerebral white matter volume, cortical thickness, and surface area. Cerebral white matter volume in overweight and obese individuals was associated with a greater degree of atrophy, with maximal effects in middle age corresponding to an estimated increase in brain age of 10 years.
Thymectomy improves clinical outcomes over a three-year period in patients with nonthymomatous myasthenia gravis, according to a study published August 11 in the New England Journal of Medicine. Researchers randomized 126 patients to thymectomy plus alternate-day prednisone or alternate-day prednisone alone. Patients who underwent thymectomy had a lower time-weighted average Quantitative Myasthenia Gravis score over a three-year period than those who received prednisone alone. Patients in the thymectomy group also had a lower average requirement for alternate-day prednisone. Fewer patients in the thymectomy group than in the prednisone-only group required immunosuppression with azathioprine or were hospitalized for exacerbations. The number of patients with treatment-associated complications did not differ significantly between groups. However, patients in the thymectomy group had fewer treatment-associated symptoms related to immunosuppressive medications.
Calcium supplementation may increase the risk of developing dementia in elderly women with cerebrovascular disease, according to a study published online ahead of print August 17 in Neurology. This longitudinal population-based study included 700 women without dementia between ages 70 and 92. At baseline and at five-year follow-up, the women underwent comprehensive neuropsychiatric and somatic examinations. A CT scan also was performed in 447 participants at baseline. Information on the use and dosage of calcium supplements was collected. Women treated with calcium supplements had a higher risk of developing dementia and the subtype of stroke-related dementia. Calcium supplementation was associated with the development of dementia in groups with a history of stroke or presence of white matter lesions, but not in groups without these conditions.
Exposure to bright light during the day may help combat sleep disturbances associated with the evening use of electronic devices emitting blue light, according to a study published online ahead of print June 16 in Sleep Medicine. Following a constant bright light exposure over 6.5 hours, 14 participants read a novel either on a tablet or as a physical book for two hours. Evening concentrations of saliva melatonin were measured repeatedly. Sleepiness was assessed before and after nocturnal sleep. About one week later, experiments were repeated. Participants who had read the novel on a tablet in the first experimental session continued reading the same novel as a physical book, and vice versa. There were no differences in sleep parameters and presleep saliva melatonin levels between the tablet reading and physical book reading conditions.
Treatment immediately after clinically isolated syndrome (CIS) is more beneficial than delayed treatment, according to a study published online ahead of print August 10 in Neurology. Researchers randomized 278 people with CIS to interferon beta-1b or placebo. After two years or a diagnosis of multiple sclerosis (MS), patients receiving placebo could receive treatment. After 11 years, risk of clinically definite MS remained lower in the early-treatment arm, compared with the delayed-treatment arm, with longer time to first relapse and lower overall annualized relapse rate. Twenty-five patients converted to secondary progressive MS. Expanded Disability Status Scale scores remained low and stable, with no difference between treatment arms. The early-treatment group had better Paced Auditory Serial Addition Task-3 total scores. Health resource utilization was low in both groups.
Patients with anemia have increased mortality after stroke, according to a study published online ahead of print August 17 in the Journal of the American Heart Association. Researchers analyzed data from a cohort of 8,013 patients with stroke who were consecutively admitted over 11 years. Anemia was present in 24.5% of the cohort on admission and was associated with increased odds of mortality at most of the time points examined up to one year following stroke. Elevated hemoglobin also was associated with increased mortality. In addition, investigators conducted a systematic review using various databases. When combined with the cohort from the current study, the pooled population had 29,943 patients with stroke. Anemia on admission was associated with an increased risk of mortality in ischemic stroke and hemorrhagic stroke.
Bedside EEG methods may indicate the level of awareness of patients in a vegetative state, according to a study published online ahead of print August 4 in Annals of Neurology. Fourteen patients with severe brain injuries were evaluated with an EEG vibrotactile attention task designed to identify a hierarchy of residual somatosensory and cognitive abilities. Each patient also was assessed with a clinical behavioral scale and two fMRI assessments of covert command following. Six patients produced only sensory responses, with no evidence of cognitive event-related potentials. Furthermore, eight patients demonstrated reliable bottom-up attention-orienting responses. No patient showed evidence of top-down attention. Only patients who followed commands, whether overtly with behavior or covertly with functional neuroimaging, also demonstrated event-related potential evidence of attentional orienting.
The PET tracer [18F]-AV-1451 may help identify the stages of the preclinical and clinical phases of Alzheimer's disease, according to a study published online ahead of print July 25 in JAMA Neurology. In all, 59 participants (64% male; mean age, 74) underwent PET imaging. The [18F]-AV-1451 standardized uptake value ratio (SUVR) in the hippocampus and Alzheimer's disease cortical signature regions distinguished participants with Alzheimer's disease from cognitively normal participants. A SUVR cutoff value of 1.19 from Alzheimer's disease cortical signature regions best distinguished these groups. Amyloid β-positivity was associated with an elevated [18F]-AV-1451 SUVR in Alzheimer's disease cortical signature regions, but not in the hippocampus. Amyloid β-positivity alone was not related to hippocampal volume or Alzheimer's disease signature cortical thickness. An elevated [18F]-AV-1451 SUVR was associated with brain volumetric loss.
Symptom exacerbations after concussion are common among children and may not impede recovery, according to a study published online ahead of print August 1 in JAMA Pediatrics. Eligible participants were between ages 11 and 18 and had sustained a concussion that did not result in an abnormal CT scan or require hospital admission. The mean age of the 63 participants (34.9% girls) was 13.8. Symptom spikes occurred in 31.7% of the sample. An abrupt increase in mental activity from one day to the next increased the risk of a symptom spike. Patients with symptom spikes were initially more symptomatic in the emergency department and throughout the observation period, but did not differ from the group without symptom spikes on cognition or balance 10 days following injury.
The FDA has approved the supplemental Biologics License Application from Ipsen Biopharmaceuticals for Dysport (abobotulinumtoxinA) for injection in the treatment of lower limb spasticity in pediatric patients age 2 and older. This approval is based on a phase III pivotal study of 235 pediatric patients ages 2 to 17 with lower limb spasticity because of cerebral palsy causing dynamic equinus foot deformity. Patients treated with Dysport showed statistically significant improvement in ankle plantar flexor muscle tone. Like all botulinum toxin products, Dysport has a boxed warning stating that the effects of the botulinum toxin may spread from the area of injection to other areas of the body, causing symptoms similar to those of botulism. Ipsen Biopharmaceuticals is headquartered in Basking Ridge, New Jersey.
Lower BMI in late life is associated with greater cortical amyloid burden, according to a study published June 18 in the Journal of Alzheimer's Disease. The study entailed cross-sectional analyses that were completed using baseline data from the Harvard Aging Brain Study, which included 280 cognitively normal adults ages 62 to 90. Assessments included medical histories and physical exams, Pittsburgh compound B (PiB) PET amyloid imaging, and APOE4 genotyping. In the primary analysis, greater PiB retention was associated with lower BMI. In the secondary analyses, APOE4 carrier status and normal BMI, as opposed to overweight or obese BMI, were associated with greater PiB retention. The interaction between BMI and APOE4 also was significant. Future studies should seek to clarify the mechanism of this association, said the researchers.
Sleep-disordered breathing (SDB) and sleep-wake disturbances (SWD) increase the risk of stroke in the general population and affect short- and long-term stroke recovery and outcome, according to a literature review published online ahead of print August 3 in Neurology. Several studies have proven SDB to represent an independent risk factor for stroke. Sleep studies in patients with transient ischemic attack or stroke are recommended in view of the high prevalence of SDB, said the researchers. Treatment of obstructive SDB with continuous positive airway pressure is recommended, given the strength of the evidence that supports the treatment's benefit. Oxygen, biphasic positive airway pressure, and adaptive servoventilation may be considered in patients with central SDB, said the researchers. Experimental studies found that SWD may impair neuroplasticity and functional stroke recovery.
—Kimberly Williams
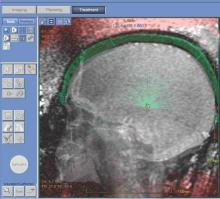
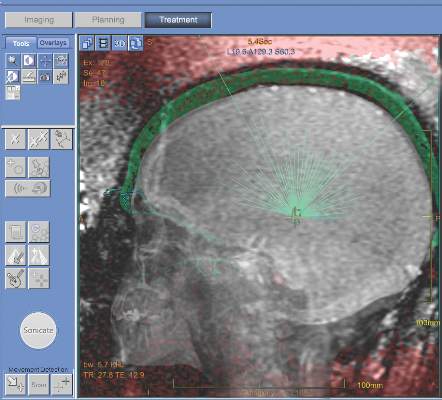
MRI-guided thalamotomy significantly reduces hand tremors
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The severity of hand tremors in patients with essential tremor can be significantly reduced via use of MRI-guided focused ultrasound thalamotomy.
Major finding: Greater improvement was observed in the ultrasound thalamotomy cohort than in the control (sham treatment) cohort: 18.1 to 9.6 hand tremor score vs. 16.0 to 15.8, respectively.
Data source: A double-blind, randomized, sham-controlled cohort study of 76 patients with moderate-to-severe essential tremor.
Disclosures: Study supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Some coauthors reported potentially relevant disclosures.
ATV injuries: where risk taking and medical helplessness collide
I. Hate. ATVs.
The modern world is full of potentially dangerous things that we regulate – sometimes by the knowledge of the person giving it (medication) or by age (tobacco, alcohol, cars). Or sometimes we simply ban something altogether (illicit drugs).
After years of neurology practice, I’ve learned to hate ATVs. Outside of firearms, I don’t think I’ve seen any gadget that has such a devastating effect on young lives.
My first medical encounter with one was 20-some years ago during my neurosurgery rotation. It was a man in his mid-20s. He was young, muscular, and clearly in excellent condition. And here he was, flaccid below the neck, and permanently on a ventilator.
I sat at the nurses station for a long time, looking at him and thinking about how a young life can go so horribly wrong so quickly. He hadn’t been drunk at the time. He’d simply had a wreck, the cause of which I never found out. After a few days, he was shipped off to a long-term ventilator facility, and I never saw him again.
Cars are dangerous, too, but are bigger and have gadgets to try to improve safety. ATVs are exposed, with only minimal, if any, protection for their riders. Their use is most typically by the young, meaning a disproportionate number of serious injuries will affect those at the beginning of adulthood.
Sadly, banning ATVs won’t stop injuries. There will always be people who do risky things in the name of being daring and having fun.
What’s changed is that 100 years ago they’d likely have died of their injuries soon afterward. Today they’ll probably survive, debilitated long term because of medical advancements.
These are the situations where I feel helpless. There are all kinds of horrible diseases we handle that have no known cause or cure. That’s one kind of helpless. But the ones with easily avoidable risk factors (ATVs, illegal drugs, tobacco) that occur are just plain frustrating for us and tragic for the patients and families.
In the land of the free, freedom to endanger your own life and health are pretty deeply entrenched. The best we can do is present people with the facts and let them make informed decisions about risky behaviors (sadly, the young often believe they’re immortal). If we ban ATVs, we still won’t stop people from making bad decisions on motorcycles or in cars, or with firearms or illegal drugs.
Like so much in medicine, there are no easy answers, and there likely never will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I. Hate. ATVs.
The modern world is full of potentially dangerous things that we regulate – sometimes by the knowledge of the person giving it (medication) or by age (tobacco, alcohol, cars). Or sometimes we simply ban something altogether (illicit drugs).
After years of neurology practice, I’ve learned to hate ATVs. Outside of firearms, I don’t think I’ve seen any gadget that has such a devastating effect on young lives.
My first medical encounter with one was 20-some years ago during my neurosurgery rotation. It was a man in his mid-20s. He was young, muscular, and clearly in excellent condition. And here he was, flaccid below the neck, and permanently on a ventilator.
I sat at the nurses station for a long time, looking at him and thinking about how a young life can go so horribly wrong so quickly. He hadn’t been drunk at the time. He’d simply had a wreck, the cause of which I never found out. After a few days, he was shipped off to a long-term ventilator facility, and I never saw him again.
Cars are dangerous, too, but are bigger and have gadgets to try to improve safety. ATVs are exposed, with only minimal, if any, protection for their riders. Their use is most typically by the young, meaning a disproportionate number of serious injuries will affect those at the beginning of adulthood.
Sadly, banning ATVs won’t stop injuries. There will always be people who do risky things in the name of being daring and having fun.
What’s changed is that 100 years ago they’d likely have died of their injuries soon afterward. Today they’ll probably survive, debilitated long term because of medical advancements.
These are the situations where I feel helpless. There are all kinds of horrible diseases we handle that have no known cause or cure. That’s one kind of helpless. But the ones with easily avoidable risk factors (ATVs, illegal drugs, tobacco) that occur are just plain frustrating for us and tragic for the patients and families.
In the land of the free, freedom to endanger your own life and health are pretty deeply entrenched. The best we can do is present people with the facts and let them make informed decisions about risky behaviors (sadly, the young often believe they’re immortal). If we ban ATVs, we still won’t stop people from making bad decisions on motorcycles or in cars, or with firearms or illegal drugs.
Like so much in medicine, there are no easy answers, and there likely never will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I. Hate. ATVs.
The modern world is full of potentially dangerous things that we regulate – sometimes by the knowledge of the person giving it (medication) or by age (tobacco, alcohol, cars). Or sometimes we simply ban something altogether (illicit drugs).
After years of neurology practice, I’ve learned to hate ATVs. Outside of firearms, I don’t think I’ve seen any gadget that has such a devastating effect on young lives.
My first medical encounter with one was 20-some years ago during my neurosurgery rotation. It was a man in his mid-20s. He was young, muscular, and clearly in excellent condition. And here he was, flaccid below the neck, and permanently on a ventilator.
I sat at the nurses station for a long time, looking at him and thinking about how a young life can go so horribly wrong so quickly. He hadn’t been drunk at the time. He’d simply had a wreck, the cause of which I never found out. After a few days, he was shipped off to a long-term ventilator facility, and I never saw him again.
Cars are dangerous, too, but are bigger and have gadgets to try to improve safety. ATVs are exposed, with only minimal, if any, protection for their riders. Their use is most typically by the young, meaning a disproportionate number of serious injuries will affect those at the beginning of adulthood.
Sadly, banning ATVs won’t stop injuries. There will always be people who do risky things in the name of being daring and having fun.
What’s changed is that 100 years ago they’d likely have died of their injuries soon afterward. Today they’ll probably survive, debilitated long term because of medical advancements.
These are the situations where I feel helpless. There are all kinds of horrible diseases we handle that have no known cause or cure. That’s one kind of helpless. But the ones with easily avoidable risk factors (ATVs, illegal drugs, tobacco) that occur are just plain frustrating for us and tragic for the patients and families.
In the land of the free, freedom to endanger your own life and health are pretty deeply entrenched. The best we can do is present people with the facts and let them make informed decisions about risky behaviors (sadly, the young often believe they’re immortal). If we ban ATVs, we still won’t stop people from making bad decisions on motorcycles or in cars, or with firearms or illegal drugs.
Like so much in medicine, there are no easy answers, and there likely never will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Focused-ultrasound device approved to treat essential tremor
A device that uses transcranial focused ultrasound to destroy the MRI-identified pathologic area of the thalamus in essential tremor patients became the first of its kind to receive Food and Drug Administration approval for use in patients whose condition has been refractory to medications such as beta-blockers or anticonvulsant drugs.
In patients who have undergone evaluation by CT and MRI to determine their suitability for the procedure, the Exablate Neuro device delivers focused ultrasound at incrementally higher energies until patients achieve a reduction of tremor. Patients are awake and responsive during the entire treatment.
“As with other treatments for essential tremor, this new device is not a cure but could help patients enjoy a better quality of life,” said Carlos Peña, PhD, director of the division of neurological and physical medicine devices in the FDA’s Center for Devices and Radiological Health, in the agency’s announcement of the approval. The device “could help them to avoid more extensive surgical treatments,” such as thalamotomy or a deep brain stimulation device, Dr. Peña said.
The clinical data used to support the approval included a double-blind, controlled trial of 76 patients with essential tremor who had not responded to medication therapy.
The 56 patients who were randomly selected to receive the Exablate Neuro treatment showed nearly a 50% improvement in their tremors and motor function 3 months after treatment, compared with their baseline score. The 20 patients who received a sham control treatment had no improvement, and some experienced a slight worsening after the sham procedure before they crossed over into the treatment group at the 3-month time point.
At 12 months post procedure, the treatment group retained a 40% improvement in those scores, compared with baseline.
Adverse events reported by patients treated with the device were similar to those reported by patients who have undergone thalamotomy. Events included numbness/tingling of the fingers, headache, imbalance/unsteadiness, loss of control of body movements (ataxia), or gait disturbance.
Other side effects identified as possibly related to treatment with MR-guided focused ultrasound treatments include tissue damage in an area other than the treatment area, hemorrhage in the treated area requiring emergency treatment, skin burns with ulceration of the skin, skin retraction, and scar formation and blood clots.
InSightec manufacturers the Exablate Neuro device.
A device that uses transcranial focused ultrasound to destroy the MRI-identified pathologic area of the thalamus in essential tremor patients became the first of its kind to receive Food and Drug Administration approval for use in patients whose condition has been refractory to medications such as beta-blockers or anticonvulsant drugs.
In patients who have undergone evaluation by CT and MRI to determine their suitability for the procedure, the Exablate Neuro device delivers focused ultrasound at incrementally higher energies until patients achieve a reduction of tremor. Patients are awake and responsive during the entire treatment.
“As with other treatments for essential tremor, this new device is not a cure but could help patients enjoy a better quality of life,” said Carlos Peña, PhD, director of the division of neurological and physical medicine devices in the FDA’s Center for Devices and Radiological Health, in the agency’s announcement of the approval. The device “could help them to avoid more extensive surgical treatments,” such as thalamotomy or a deep brain stimulation device, Dr. Peña said.
The clinical data used to support the approval included a double-blind, controlled trial of 76 patients with essential tremor who had not responded to medication therapy.
The 56 patients who were randomly selected to receive the Exablate Neuro treatment showed nearly a 50% improvement in their tremors and motor function 3 months after treatment, compared with their baseline score. The 20 patients who received a sham control treatment had no improvement, and some experienced a slight worsening after the sham procedure before they crossed over into the treatment group at the 3-month time point.
At 12 months post procedure, the treatment group retained a 40% improvement in those scores, compared with baseline.
Adverse events reported by patients treated with the device were similar to those reported by patients who have undergone thalamotomy. Events included numbness/tingling of the fingers, headache, imbalance/unsteadiness, loss of control of body movements (ataxia), or gait disturbance.
Other side effects identified as possibly related to treatment with MR-guided focused ultrasound treatments include tissue damage in an area other than the treatment area, hemorrhage in the treated area requiring emergency treatment, skin burns with ulceration of the skin, skin retraction, and scar formation and blood clots.
InSightec manufacturers the Exablate Neuro device.
A device that uses transcranial focused ultrasound to destroy the MRI-identified pathologic area of the thalamus in essential tremor patients became the first of its kind to receive Food and Drug Administration approval for use in patients whose condition has been refractory to medications such as beta-blockers or anticonvulsant drugs.
In patients who have undergone evaluation by CT and MRI to determine their suitability for the procedure, the Exablate Neuro device delivers focused ultrasound at incrementally higher energies until patients achieve a reduction of tremor. Patients are awake and responsive during the entire treatment.
“As with other treatments for essential tremor, this new device is not a cure but could help patients enjoy a better quality of life,” said Carlos Peña, PhD, director of the division of neurological and physical medicine devices in the FDA’s Center for Devices and Radiological Health, in the agency’s announcement of the approval. The device “could help them to avoid more extensive surgical treatments,” such as thalamotomy or a deep brain stimulation device, Dr. Peña said.
The clinical data used to support the approval included a double-blind, controlled trial of 76 patients with essential tremor who had not responded to medication therapy.
The 56 patients who were randomly selected to receive the Exablate Neuro treatment showed nearly a 50% improvement in their tremors and motor function 3 months after treatment, compared with their baseline score. The 20 patients who received a sham control treatment had no improvement, and some experienced a slight worsening after the sham procedure before they crossed over into the treatment group at the 3-month time point.
At 12 months post procedure, the treatment group retained a 40% improvement in those scores, compared with baseline.
Adverse events reported by patients treated with the device were similar to those reported by patients who have undergone thalamotomy. Events included numbness/tingling of the fingers, headache, imbalance/unsteadiness, loss of control of body movements (ataxia), or gait disturbance.
Other side effects identified as possibly related to treatment with MR-guided focused ultrasound treatments include tissue damage in an area other than the treatment area, hemorrhage in the treated area requiring emergency treatment, skin burns with ulceration of the skin, skin retraction, and scar formation and blood clots.
InSightec manufacturers the Exablate Neuro device.
Improving our crystal ball: prognostication in neuroscience ICUs
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
Baseline King-Devick concussion score skewed by English proficiency issues
VANCOUVER – In a study at New York University, it took 27 healthy, native English–speaking volunteers 42.8 seconds to complete the King-Devick concussion screening test, which is about average for nonconcussed subjects.
However, it took 27 other volunteers with English as a second language 54.4 seconds (P = .001). Had the test been given on the sidelines instead of in a laboratory, the extra 12 seconds might easily have been mistaken as a sign of serious concussion because concussions generally add about 5 seconds to the King-Devick score.
“A prolongation of 12 seconds in non-native English speakers has real clinical implications,” said lead investigator Katharine Dempsey, a medical student and member of the eye movement research team in the department of neurology at New York University.
King-Devick (KD) is an increasingly popular sideline screening tool used widely in professional sports. Subjects are timed on how long it takes to read out loud and in English three sets of 40 numbers, with each set progressively more difficult to read. It’s administered by flashcards or, as in the study, by computer screen.
All of the non-native speakers at NYU were largely proficient in English, but their native languages – 18 in total, most often Spanish or Chinese – were often dominant, meaning they were used at home and to work out mental arithmetic. Some subjects did not use Roman numerals or right-to-left reading in their native tongues.
KD instructions recommend testing subjects against their own preseason baseline scores; the NYU findings emphasize how important that is when subjects aren’t native English speakers. The investigators are concerned that when baseline scores are unavailable, non-native English speakers will be scored against reference ranges for native speakers.
“There’s incredible utility in using a sideline concussion screening test, but we definitely have to get out the message that the best practice is to take an athlete’s own preseason baseline. We have to be incredibly cautious when comparing test times of non-native English speakers to a normative database for native speakers,” Ms. Dempsey said at the annual meeting of the American Academy of Neurology.
The participants were in their early 30s, on average, and had no histories of concussion. The majority were women, and most were NYU employees or their friends.
The team also tracked eye movements during testing. Non-native speakers had more quick eye movement (149 vs. 135; P = .03), but also fixated longer on numbers before initiating eye movement (345.4 milliseconds vs. 288.0; P = .007). Lag time correlated with native language dominance and suggests longer processing time.
The next step is to test how well patients do with KD testing in their native language, Ms. Dempsey said.
Ms. Dempsey had no disclosures.
VANCOUVER – In a study at New York University, it took 27 healthy, native English–speaking volunteers 42.8 seconds to complete the King-Devick concussion screening test, which is about average for nonconcussed subjects.
However, it took 27 other volunteers with English as a second language 54.4 seconds (P = .001). Had the test been given on the sidelines instead of in a laboratory, the extra 12 seconds might easily have been mistaken as a sign of serious concussion because concussions generally add about 5 seconds to the King-Devick score.
“A prolongation of 12 seconds in non-native English speakers has real clinical implications,” said lead investigator Katharine Dempsey, a medical student and member of the eye movement research team in the department of neurology at New York University.
King-Devick (KD) is an increasingly popular sideline screening tool used widely in professional sports. Subjects are timed on how long it takes to read out loud and in English three sets of 40 numbers, with each set progressively more difficult to read. It’s administered by flashcards or, as in the study, by computer screen.
All of the non-native speakers at NYU were largely proficient in English, but their native languages – 18 in total, most often Spanish or Chinese – were often dominant, meaning they were used at home and to work out mental arithmetic. Some subjects did not use Roman numerals or right-to-left reading in their native tongues.
KD instructions recommend testing subjects against their own preseason baseline scores; the NYU findings emphasize how important that is when subjects aren’t native English speakers. The investigators are concerned that when baseline scores are unavailable, non-native English speakers will be scored against reference ranges for native speakers.
“There’s incredible utility in using a sideline concussion screening test, but we definitely have to get out the message that the best practice is to take an athlete’s own preseason baseline. We have to be incredibly cautious when comparing test times of non-native English speakers to a normative database for native speakers,” Ms. Dempsey said at the annual meeting of the American Academy of Neurology.
The participants were in their early 30s, on average, and had no histories of concussion. The majority were women, and most were NYU employees or their friends.
The team also tracked eye movements during testing. Non-native speakers had more quick eye movement (149 vs. 135; P = .03), but also fixated longer on numbers before initiating eye movement (345.4 milliseconds vs. 288.0; P = .007). Lag time correlated with native language dominance and suggests longer processing time.
The next step is to test how well patients do with KD testing in their native language, Ms. Dempsey said.
Ms. Dempsey had no disclosures.
VANCOUVER – In a study at New York University, it took 27 healthy, native English–speaking volunteers 42.8 seconds to complete the King-Devick concussion screening test, which is about average for nonconcussed subjects.
However, it took 27 other volunteers with English as a second language 54.4 seconds (P = .001). Had the test been given on the sidelines instead of in a laboratory, the extra 12 seconds might easily have been mistaken as a sign of serious concussion because concussions generally add about 5 seconds to the King-Devick score.
“A prolongation of 12 seconds in non-native English speakers has real clinical implications,” said lead investigator Katharine Dempsey, a medical student and member of the eye movement research team in the department of neurology at New York University.
King-Devick (KD) is an increasingly popular sideline screening tool used widely in professional sports. Subjects are timed on how long it takes to read out loud and in English three sets of 40 numbers, with each set progressively more difficult to read. It’s administered by flashcards or, as in the study, by computer screen.
All of the non-native speakers at NYU were largely proficient in English, but their native languages – 18 in total, most often Spanish or Chinese – were often dominant, meaning they were used at home and to work out mental arithmetic. Some subjects did not use Roman numerals or right-to-left reading in their native tongues.
KD instructions recommend testing subjects against their own preseason baseline scores; the NYU findings emphasize how important that is when subjects aren’t native English speakers. The investigators are concerned that when baseline scores are unavailable, non-native English speakers will be scored against reference ranges for native speakers.
“There’s incredible utility in using a sideline concussion screening test, but we definitely have to get out the message that the best practice is to take an athlete’s own preseason baseline. We have to be incredibly cautious when comparing test times of non-native English speakers to a normative database for native speakers,” Ms. Dempsey said at the annual meeting of the American Academy of Neurology.
The participants were in their early 30s, on average, and had no histories of concussion. The majority were women, and most were NYU employees or their friends.
The team also tracked eye movements during testing. Non-native speakers had more quick eye movement (149 vs. 135; P = .03), but also fixated longer on numbers before initiating eye movement (345.4 milliseconds vs. 288.0; P = .007). Lag time correlated with native language dominance and suggests longer processing time.
The next step is to test how well patients do with KD testing in their native language, Ms. Dempsey said.
Ms. Dempsey had no disclosures.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: King-Devick instructions recommend testing subjects against their own preseason baseline scores; the NYU findings emphasize how important that is when subjects aren’t native English speakers.
Major finding: It took 27 healthy, native English–speaking volunteers 42.8 seconds to complete the King-Devick concussion screening test, but 27 other volunteers with English as a second language 54.4 seconds (P = .001).
Data source: Prospective screening of 54 healthy volunteers.
Disclosures: The presenter had no disclosures.
Doppler ultrasound headset performs well at spotting sports-related concussion
VANCOUVER – A new transcranial Doppler platform that analyzes subtle changes in the cerebral blood flow waveform performed well in detecting sports-related concussion in a cohort study of 238 Los Angeles high school athletes.
The investigational headset device was able to differentiate between those with and without a recent concussion 83% of the time, investigators reported at the annual meeting of the American Academy of Neurology. In contrast, traditional transcranial Doppler analysis detected a recent concussion only 50%-60% of the time.
“Over the last few years, there has been growing evidence that cerebral hemodynamics are altered following sports-related concussion,” senior author Robert Hamilton, Ph.D., cofounder and chief science officer of Neural Analytics in Los Angeles, commented in a session and interview.
Most studies in this area have used MRI or traditional transcranial Doppler analysis, he said. However, the former is costly, time consuming, and not portable, and the latter has not proven very accurate.
As traditional Doppler analysis disregards the majority of waveform data, Dr. Hamilton and his colleagues developed an advanced platform that uses machine learning to analyze the entire shape of the cerebral blood flow velocity waveform through quantitative cerebral hemodynamics.
They compared the advanced analysis with traditional analysis among 69 high school athletes in contact sports who had sustained a concussion an average of 6 days earlier and a control group of 169 unaffected age-matched high school athletes from contact and noncontact sports.
Both groups had bilateral monitoring of blood flow in the middle cerebral artery with transcranial Doppler while they followed a standard cerebrovascular reactivity protocol that included rest and breath holding.
Results showed that for differentiating between athletes who did and did not have concussion, the advanced analysis had an area under the receiver operating characteristic curve of 83%. (Sensitivity was 72%, specificity was 82%, and overall accuracy was 80%.)
In comparison, the area under the curve was substantially lower for the traditional analysis measures: It was 55% for mean velocity (100% sensitivity, 0% specificity, 76% accuracy), 52% for the pulsatility index (86% sensitivity, 23% specificity, 61% accuracy), and 60% for the cerebrovascular reactivity index (51% sensitivity, 68% specificity, 64% accuracy).
“Unfortunately, concussion diagnostics and management today are basically subjective,” Dr. Hamilton commented. The advanced analysis may therefore improve the situation by providing objective evidence of blood flow dysfunction after injury.
The new analysis platform “is easy to use and portable, and [testing] can be done very quickly, within 5 minutes,” he noted. “The nice thing is it can be done on the sideline, in the emergency room, or in a doctor’s office.”
The investigators will next use the advanced analysis to track recovery of blood flow regulation after sports-related concussion and will compare its performance with that of additional modalities, such as MRI, according to Dr. Hamilton. Furthermore, they are testing it in various other populations: adolescents, college athletes, and members of the military.
“Ultimately, blood flow dysfunction is also important in a wide variety of conditions, such as stroke and dementia,” he pointed out. “So those are conditions that we are looking at to study this year and moving forward in the future.”
The research was supported by the National Institutes of Health and the National Science Foundation.
VANCOUVER – A new transcranial Doppler platform that analyzes subtle changes in the cerebral blood flow waveform performed well in detecting sports-related concussion in a cohort study of 238 Los Angeles high school athletes.
The investigational headset device was able to differentiate between those with and without a recent concussion 83% of the time, investigators reported at the annual meeting of the American Academy of Neurology. In contrast, traditional transcranial Doppler analysis detected a recent concussion only 50%-60% of the time.
“Over the last few years, there has been growing evidence that cerebral hemodynamics are altered following sports-related concussion,” senior author Robert Hamilton, Ph.D., cofounder and chief science officer of Neural Analytics in Los Angeles, commented in a session and interview.
Most studies in this area have used MRI or traditional transcranial Doppler analysis, he said. However, the former is costly, time consuming, and not portable, and the latter has not proven very accurate.
As traditional Doppler analysis disregards the majority of waveform data, Dr. Hamilton and his colleagues developed an advanced platform that uses machine learning to analyze the entire shape of the cerebral blood flow velocity waveform through quantitative cerebral hemodynamics.
They compared the advanced analysis with traditional analysis among 69 high school athletes in contact sports who had sustained a concussion an average of 6 days earlier and a control group of 169 unaffected age-matched high school athletes from contact and noncontact sports.
Both groups had bilateral monitoring of blood flow in the middle cerebral artery with transcranial Doppler while they followed a standard cerebrovascular reactivity protocol that included rest and breath holding.
Results showed that for differentiating between athletes who did and did not have concussion, the advanced analysis had an area under the receiver operating characteristic curve of 83%. (Sensitivity was 72%, specificity was 82%, and overall accuracy was 80%.)
In comparison, the area under the curve was substantially lower for the traditional analysis measures: It was 55% for mean velocity (100% sensitivity, 0% specificity, 76% accuracy), 52% for the pulsatility index (86% sensitivity, 23% specificity, 61% accuracy), and 60% for the cerebrovascular reactivity index (51% sensitivity, 68% specificity, 64% accuracy).
“Unfortunately, concussion diagnostics and management today are basically subjective,” Dr. Hamilton commented. The advanced analysis may therefore improve the situation by providing objective evidence of blood flow dysfunction after injury.
The new analysis platform “is easy to use and portable, and [testing] can be done very quickly, within 5 minutes,” he noted. “The nice thing is it can be done on the sideline, in the emergency room, or in a doctor’s office.”
The investigators will next use the advanced analysis to track recovery of blood flow regulation after sports-related concussion and will compare its performance with that of additional modalities, such as MRI, according to Dr. Hamilton. Furthermore, they are testing it in various other populations: adolescents, college athletes, and members of the military.
“Ultimately, blood flow dysfunction is also important in a wide variety of conditions, such as stroke and dementia,” he pointed out. “So those are conditions that we are looking at to study this year and moving forward in the future.”
The research was supported by the National Institutes of Health and the National Science Foundation.
VANCOUVER – A new transcranial Doppler platform that analyzes subtle changes in the cerebral blood flow waveform performed well in detecting sports-related concussion in a cohort study of 238 Los Angeles high school athletes.
The investigational headset device was able to differentiate between those with and without a recent concussion 83% of the time, investigators reported at the annual meeting of the American Academy of Neurology. In contrast, traditional transcranial Doppler analysis detected a recent concussion only 50%-60% of the time.
“Over the last few years, there has been growing evidence that cerebral hemodynamics are altered following sports-related concussion,” senior author Robert Hamilton, Ph.D., cofounder and chief science officer of Neural Analytics in Los Angeles, commented in a session and interview.
Most studies in this area have used MRI or traditional transcranial Doppler analysis, he said. However, the former is costly, time consuming, and not portable, and the latter has not proven very accurate.
As traditional Doppler analysis disregards the majority of waveform data, Dr. Hamilton and his colleagues developed an advanced platform that uses machine learning to analyze the entire shape of the cerebral blood flow velocity waveform through quantitative cerebral hemodynamics.
They compared the advanced analysis with traditional analysis among 69 high school athletes in contact sports who had sustained a concussion an average of 6 days earlier and a control group of 169 unaffected age-matched high school athletes from contact and noncontact sports.
Both groups had bilateral monitoring of blood flow in the middle cerebral artery with transcranial Doppler while they followed a standard cerebrovascular reactivity protocol that included rest and breath holding.
Results showed that for differentiating between athletes who did and did not have concussion, the advanced analysis had an area under the receiver operating characteristic curve of 83%. (Sensitivity was 72%, specificity was 82%, and overall accuracy was 80%.)
In comparison, the area under the curve was substantially lower for the traditional analysis measures: It was 55% for mean velocity (100% sensitivity, 0% specificity, 76% accuracy), 52% for the pulsatility index (86% sensitivity, 23% specificity, 61% accuracy), and 60% for the cerebrovascular reactivity index (51% sensitivity, 68% specificity, 64% accuracy).
“Unfortunately, concussion diagnostics and management today are basically subjective,” Dr. Hamilton commented. The advanced analysis may therefore improve the situation by providing objective evidence of blood flow dysfunction after injury.
The new analysis platform “is easy to use and portable, and [testing] can be done very quickly, within 5 minutes,” he noted. “The nice thing is it can be done on the sideline, in the emergency room, or in a doctor’s office.”
The investigators will next use the advanced analysis to track recovery of blood flow regulation after sports-related concussion and will compare its performance with that of additional modalities, such as MRI, according to Dr. Hamilton. Furthermore, they are testing it in various other populations: adolescents, college athletes, and members of the military.
“Ultimately, blood flow dysfunction is also important in a wide variety of conditions, such as stroke and dementia,” he pointed out. “So those are conditions that we are looking at to study this year and moving forward in the future.”
The research was supported by the National Institutes of Health and the National Science Foundation.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: Advanced transcranial Doppler analysis may improve identification of athletes with concussion at the point of care.
Major finding: For differentiating between athletes who did and did not have concussion, the advanced analysis had an area under the receiver operating characteristic curve of 83%.
Data source: A cohort study of 69 concussed and 169 nonconcussed high school athletes.
Disclosures: Dr. Hamilton disclosed that he is a cofounder and chief science officer of Neural Analytics. The study was supported by the National Institutes of Health and the National Science Foundation.
Scans show high prevalence of TBI among symptomatic retired NFL players
VANCOUVER – Many retired National Football League (NFL) players seeking care for neurocognitive symptoms have MRI evidence of traumatic brain injury, according to the largest study of this issue among living players.
Data reported at the annual meeting of the American Academy of Neurology show that 43% of a cohort of 40 symptomatic NFL retirees had abnormal results on diffusion tensor MRI and 30% had evidence of traumatic axonal injury on conventional MRI.
The likelihood of abnormal diffusion tensor MRI results was correlated, albeit weakly, with the length of the player’s NFL career, but not with the number of concussions sustained.
“It appears that subconcussive hits – that is, the cumulative effects and longer playing careers – place retired alumni at risk for abnormal diffusion tensor MRI,” commented lead author Dr. Francis X. Conidi, director of the Florida Center for Headache & Sports Neurology in Palm Beach and team neurologist for the Florida Panthers of the National Hockey League.
“This could be a possible link to chronic traumatic encephalopathy, as consensus is you need to have repetitive head trauma,” he proposed. “Or this could be a separate entity whereby, in NFL players, the symptoms we are seeing are actually related to the traumatic brain injury itself and [in a subset] with some genetic predisposition, they will go on to have progressive neurological decline.”
Although the cohort was quite young, only 39 years old on average, some had likely played football since youth, and that has implications for prevention, Dr. Conidi added in an interview. “One thing we need to consider is limiting the amount of contact that these people receive on a cumulative basis, starting when they are young and starting in practice, because that’s where most of the contact occurs,” he recommended.
“It is important to note that diffusion tensor imaging is not a routine part of a brain MRI study,” session moderator Dr. José E. Cavazos, professor of neurology and assistant dean at the University of Texas Health Science Center in San Antonio, said in comments provided by email. “The significant correlation between duration of years played and abnormalities in diffusion tensor imaging is of concern given the popularity of the sport.”
“The next step is to replicate the findings, but more importantly, it is to find surrogate markers for early detection for these abnormalities, aiming to intervene (sideline) those players at greater risk for developing cognitive deficits or other impairments,” he added.
In the study, the retired players had a battery of neuropsychological and imaging examinations and tests over a period of 2 days. They were classified as having abnormal diffusion tensor MRI results if they had fractional anisotropy (FA) values at least 2.5 standard deviations below those of age-matched peers in a normative database for specific regions of interest in the brain.
The players ranged in age from 27 to 56 years. On average, they had played 7 years in the NFL and sustained eight concussions during that time. Most had retired in the past 5 years.
Results showed that, overall, 43% had abnormal diffusion tensor MRI results, Dr. Conidi reported. Prevalence, however, varied according to player position: It was highest for defensive linemen (64%) and wide receivers (60%); intermediate for running backs (43%), defensive backs (33%), and offensive linemen (29%); and lowest for quarterbacks (0%) and linebackers (0%).
The number of years played was significantly correlated with abnormal results (P = .049), but the number of concussions was not.
In other findings, sizable proportions of the players had significant abnormalities in attention and concentration (43%), executive function (54%), learning and memory (46%), spatial and perceptual function (24%), and language (5%).
“These guys have played these positions probably since they were young. This isn’t just NFL. We don’t make any claims that professional football caused this,” Dr. Conidi emphasized.
As for future research, the investigators plan to undertake PET scanning to assess clinical and laboratory evidence of Alzheimer’s disease, study sleep pathology, and look for tau protein (a marker for chronic traumatic encephalopathy) in cerebrospinal fluid. Additionally, they will assess treatment outcomes.
The study is not without limitations, Dr. Conidi acknowledged. “With every study that has ever been done on these guys, it is a skewed population: They are coming to us and they are looking to be evaluated,” he elaborated. “The other issue is we don’t have a normative comparison database for the neuropsychological testing.”
Dr. Conidi disclosed that he is a consultant for the NFL, NHL, USTA, PGA, and NCAA and that he receives research support from the Seeing Stars Foundation.
VANCOUVER – Many retired National Football League (NFL) players seeking care for neurocognitive symptoms have MRI evidence of traumatic brain injury, according to the largest study of this issue among living players.
Data reported at the annual meeting of the American Academy of Neurology show that 43% of a cohort of 40 symptomatic NFL retirees had abnormal results on diffusion tensor MRI and 30% had evidence of traumatic axonal injury on conventional MRI.
The likelihood of abnormal diffusion tensor MRI results was correlated, albeit weakly, with the length of the player’s NFL career, but not with the number of concussions sustained.
“It appears that subconcussive hits – that is, the cumulative effects and longer playing careers – place retired alumni at risk for abnormal diffusion tensor MRI,” commented lead author Dr. Francis X. Conidi, director of the Florida Center for Headache & Sports Neurology in Palm Beach and team neurologist for the Florida Panthers of the National Hockey League.
“This could be a possible link to chronic traumatic encephalopathy, as consensus is you need to have repetitive head trauma,” he proposed. “Or this could be a separate entity whereby, in NFL players, the symptoms we are seeing are actually related to the traumatic brain injury itself and [in a subset] with some genetic predisposition, they will go on to have progressive neurological decline.”
Although the cohort was quite young, only 39 years old on average, some had likely played football since youth, and that has implications for prevention, Dr. Conidi added in an interview. “One thing we need to consider is limiting the amount of contact that these people receive on a cumulative basis, starting when they are young and starting in practice, because that’s where most of the contact occurs,” he recommended.
“It is important to note that diffusion tensor imaging is not a routine part of a brain MRI study,” session moderator Dr. José E. Cavazos, professor of neurology and assistant dean at the University of Texas Health Science Center in San Antonio, said in comments provided by email. “The significant correlation between duration of years played and abnormalities in diffusion tensor imaging is of concern given the popularity of the sport.”
“The next step is to replicate the findings, but more importantly, it is to find surrogate markers for early detection for these abnormalities, aiming to intervene (sideline) those players at greater risk for developing cognitive deficits or other impairments,” he added.
In the study, the retired players had a battery of neuropsychological and imaging examinations and tests over a period of 2 days. They were classified as having abnormal diffusion tensor MRI results if they had fractional anisotropy (FA) values at least 2.5 standard deviations below those of age-matched peers in a normative database for specific regions of interest in the brain.
The players ranged in age from 27 to 56 years. On average, they had played 7 years in the NFL and sustained eight concussions during that time. Most had retired in the past 5 years.
Results showed that, overall, 43% had abnormal diffusion tensor MRI results, Dr. Conidi reported. Prevalence, however, varied according to player position: It was highest for defensive linemen (64%) and wide receivers (60%); intermediate for running backs (43%), defensive backs (33%), and offensive linemen (29%); and lowest for quarterbacks (0%) and linebackers (0%).
The number of years played was significantly correlated with abnormal results (P = .049), but the number of concussions was not.
In other findings, sizable proportions of the players had significant abnormalities in attention and concentration (43%), executive function (54%), learning and memory (46%), spatial and perceptual function (24%), and language (5%).
“These guys have played these positions probably since they were young. This isn’t just NFL. We don’t make any claims that professional football caused this,” Dr. Conidi emphasized.
As for future research, the investigators plan to undertake PET scanning to assess clinical and laboratory evidence of Alzheimer’s disease, study sleep pathology, and look for tau protein (a marker for chronic traumatic encephalopathy) in cerebrospinal fluid. Additionally, they will assess treatment outcomes.
The study is not without limitations, Dr. Conidi acknowledged. “With every study that has ever been done on these guys, it is a skewed population: They are coming to us and they are looking to be evaluated,” he elaborated. “The other issue is we don’t have a normative comparison database for the neuropsychological testing.”
Dr. Conidi disclosed that he is a consultant for the NFL, NHL, USTA, PGA, and NCAA and that he receives research support from the Seeing Stars Foundation.
VANCOUVER – Many retired National Football League (NFL) players seeking care for neurocognitive symptoms have MRI evidence of traumatic brain injury, according to the largest study of this issue among living players.
Data reported at the annual meeting of the American Academy of Neurology show that 43% of a cohort of 40 symptomatic NFL retirees had abnormal results on diffusion tensor MRI and 30% had evidence of traumatic axonal injury on conventional MRI.
The likelihood of abnormal diffusion tensor MRI results was correlated, albeit weakly, with the length of the player’s NFL career, but not with the number of concussions sustained.
“It appears that subconcussive hits – that is, the cumulative effects and longer playing careers – place retired alumni at risk for abnormal diffusion tensor MRI,” commented lead author Dr. Francis X. Conidi, director of the Florida Center for Headache & Sports Neurology in Palm Beach and team neurologist for the Florida Panthers of the National Hockey League.
“This could be a possible link to chronic traumatic encephalopathy, as consensus is you need to have repetitive head trauma,” he proposed. “Or this could be a separate entity whereby, in NFL players, the symptoms we are seeing are actually related to the traumatic brain injury itself and [in a subset] with some genetic predisposition, they will go on to have progressive neurological decline.”
Although the cohort was quite young, only 39 years old on average, some had likely played football since youth, and that has implications for prevention, Dr. Conidi added in an interview. “One thing we need to consider is limiting the amount of contact that these people receive on a cumulative basis, starting when they are young and starting in practice, because that’s where most of the contact occurs,” he recommended.
“It is important to note that diffusion tensor imaging is not a routine part of a brain MRI study,” session moderator Dr. José E. Cavazos, professor of neurology and assistant dean at the University of Texas Health Science Center in San Antonio, said in comments provided by email. “The significant correlation between duration of years played and abnormalities in diffusion tensor imaging is of concern given the popularity of the sport.”
“The next step is to replicate the findings, but more importantly, it is to find surrogate markers for early detection for these abnormalities, aiming to intervene (sideline) those players at greater risk for developing cognitive deficits or other impairments,” he added.
In the study, the retired players had a battery of neuropsychological and imaging examinations and tests over a period of 2 days. They were classified as having abnormal diffusion tensor MRI results if they had fractional anisotropy (FA) values at least 2.5 standard deviations below those of age-matched peers in a normative database for specific regions of interest in the brain.
The players ranged in age from 27 to 56 years. On average, they had played 7 years in the NFL and sustained eight concussions during that time. Most had retired in the past 5 years.
Results showed that, overall, 43% had abnormal diffusion tensor MRI results, Dr. Conidi reported. Prevalence, however, varied according to player position: It was highest for defensive linemen (64%) and wide receivers (60%); intermediate for running backs (43%), defensive backs (33%), and offensive linemen (29%); and lowest for quarterbacks (0%) and linebackers (0%).
The number of years played was significantly correlated with abnormal results (P = .049), but the number of concussions was not.
In other findings, sizable proportions of the players had significant abnormalities in attention and concentration (43%), executive function (54%), learning and memory (46%), spatial and perceptual function (24%), and language (5%).
“These guys have played these positions probably since they were young. This isn’t just NFL. We don’t make any claims that professional football caused this,” Dr. Conidi emphasized.
As for future research, the investigators plan to undertake PET scanning to assess clinical and laboratory evidence of Alzheimer’s disease, study sleep pathology, and look for tau protein (a marker for chronic traumatic encephalopathy) in cerebrospinal fluid. Additionally, they will assess treatment outcomes.
The study is not without limitations, Dr. Conidi acknowledged. “With every study that has ever been done on these guys, it is a skewed population: They are coming to us and they are looking to be evaluated,” he elaborated. “The other issue is we don’t have a normative comparison database for the neuropsychological testing.”
Dr. Conidi disclosed that he is a consultant for the NFL, NHL, USTA, PGA, and NCAA and that he receives research support from the Seeing Stars Foundation.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: MRI findings suggest that traumatic brain injury is prevalent among symptomatic retired NFL players.
Major finding: Overall, 43% of the players had abnormal diffusion tensor MRI results and 30% had evidence of traumatic axonal injury on conventional MRI.
Data source: A prospective cohort study of 40 retired NFL players who sought care for neurocognitive symptoms.
Disclosures: Dr. Conidi disclosed that he is a consultant for the NFL, NHL, USTA, PGA, and NCAA and that he receives research support from the Seeing Stars Foundation.
Benefit of lumbar fusion for spinal stenosis found to be small to nonexistent
The benefit of adding lumbar fusion surgery to decompression surgery for spinal stenosis was nonexistent in one large clinical trial and very modest in another, according to separate reports published online April 13 in the New England Journal of Medicine.
Both studies indicated that, given the considerable cost and the potential complications associated with lumbar fusion, it may not be worthwhile to add it to decompression surgery for spinal stenosis. “The goal of surgery in lumbar spinal stenosis is to improve walking distance and to relieve pain by decompression of the nerve roots. The addition of instrumented fusion – ‘just to be sure’ – for the treatment of the most frequent forms of lumbar spinal stenosis does not create any added value for patients and might be regarded as an overcautious and unnecessary treatment,” Dr. Wilco C. Peul and Dr. Wouter A. Moojen said in an editorial accompanying the two reports.
Surgical decompression of spinal stenosis using laminectomy is increasingly being supplemented with lumbar fusion, which is thought to firm up spinal instability and minimize the risk of future deformity. In the United States, approximately half of patients who have surgery for spinal stenosis undergo fusion procedures. Of those who also show degenerative spondylolisthesis on preoperative imaging studies, 96% undergo fusion procedures because many spine surgeons see this as a sign of instability and a mandatory indication for fusion. However, the evidence supporting the use of fusion plus decompression, as opposed to decompression alone, is weak, according to the investigators who conducted the Swedish Spinal Stenosis Study. The other study in the New England Journal of Medicine, the Spinal Laminectomy Versus Instrumented Pedicle Screw (SLIP) trial, was conducted in the United States.
Both of those clinical trials were performed to shed further light on the issue.
In the Swedish Spinal Stenosis Study, the investigators assessed outcomes in 247 patients aged 50-80 years who were treated at seven Swedish hospitals over the course of 6 years. This open-label, superiority trial randomly assigned 124 patients to decompression surgery alone and 123 to decompression plus fusion. The primary outcome measure was score on the Oswestry Disability Index (ODI), which measures disability and quality of life in patients with low-back pain, 2 years after surgery. The ODI scale runs from 0 to 100, with higher scores indicating more severe disability, said Dr. Peter Försth of the department of surgical sciences at Uppsala (Sweden) University and the Stockholm Spine Center and his associates.
At 2 years, there was no significant difference between the two study groups; the decompression-only group had a mean ODI score of 24, and the fusion group had a mean score of 27. The ODI scores in both groups had improved from baseline to a similar degree: by 17 points with decompression alone and by 15 points with fusion. In addition, fusion surgery was not superior to decompression alone regardless of whether patients had any degree of spondylolisthesis and regardless of whether they had severe spondylolisthesis involving a vertebral slip of 7.4 mm or more, the investigators reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1513721).The two study groups also showed no significant differences in secondary outcome measures, including performance on the 6-minute walk test and subjective patient assessment of improvement in walking ability. Moreover, these results persisted in the 144 patients who were assessed at 5-year follow-up.
In contrast, decompression alone was associated with fewer complications than decompression plus fusion. Postoperative wound infection developed in only 4% of the decompression-only group, compared with 10% of the fusion group. Although this study wasn’t adequately powered to draw firm conclusions regarding complications, a previous analysis of registry data reported that adding fusion surgery to decompression surgery doubles the risk of severe adverse events in older patients, Dr. Försth and his associates said.
Decompression alone also was markedly less expensive than fusion surgery. Mean direct costs were $6,800 higher for fusion than for decompression alone, because of the additional operating time needed, the extended hospital stay, and the cost of the implant.
In the SLIP trial, the researchers compared outcomes in 66 patients aged 50-80 years who all had spinal stenosis with grade 1 degenerative spondylolisthesis. The participants were randomly assigned to undergo decompression alone (35 patients) or decompression plus fusion (31 patients) at five U.S. medical centers, said Dr. Zoher Ghogawala of the Alan and Jacqueline B. Stuart Spine Research Center in the department of neurosurgery at Lahey Hospital and Medical Center, Burlington, Mass., and his associates.
The primary outcome measure was the physical-component summary score on the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) 2 years after surgery. This scale also runs from 0 to 100, but higher scores indicate better physical health. Five points was prespecified as the minimal clinically important difference on the SF-36.
At 2 years, patients in the fusion group showed a small but significant advantage of 5.7 points on the SF-36, with a mean score of 15.2, compared with patients in the decompression-only group (mean score, 9.5). However, the ODI scores, a secondary outcome measure in this study, were not significantly different between the two study groups, Dr. Ghogawala and his associates reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1508788).Surgical complications, blood loss, and length of stay all were significantly greater with fusion than with decompression alone.
Dr. Försth’s study was supported by Uppsala University, Uppsala County Council, the Stockholm Spine Center, and Johnson & Johnson. Two of his associates reported ties to Medtronic and Quantify Research. Dr. Ghogawala’s study was supported by the Jean and David Wallace Foundation, the Greenwich Lumbar Stenosis SLIP Study Fund. His associates reported ties to numerous industry sources.
Both of these studies clearly demonstrated that for most patients, stenosis surgery should be limited to decompression when no overt instability is present. Dr. Ghogawala and his colleagues correctly concluded that the modest difference in SF-36 score in favor of fusion doesn’t justify that procedure’s higher cost and complication rate.
Fusion surgery is no longer best practice and should be restricted to patients who have proven spinal instability; vertebral destruction caused by trauma, tumors, infections, or spinal deformities; or possibly neuroforamen stenosis with compressed exiting nerves due to postsurgical disk collapse.
Dr. Wilco C. Peul is at Leiden (the Netherlands) University Medical Center and at Medical Center Haaglanden, the Hague. Dr. Wouter A. Moojen is at Medical Center Haaglanden. Dr. Peul reported receiving grants from ZonMW, Paradigm Spine, Medtronic, Eurospine Foundation, and CVZ. Dr. Moojen reported having no relevant financial disclosures. Dr. Peul and Dr. Moojen made these remarks in an editorial accompanying the reports on the Swedish Spinal Stenosis Study and the Spinal Laminectomy Versus Instrumented Pedicle Screw trial (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMe1600955).
Both of these studies clearly demonstrated that for most patients, stenosis surgery should be limited to decompression when no overt instability is present. Dr. Ghogawala and his colleagues correctly concluded that the modest difference in SF-36 score in favor of fusion doesn’t justify that procedure’s higher cost and complication rate.
Fusion surgery is no longer best practice and should be restricted to patients who have proven spinal instability; vertebral destruction caused by trauma, tumors, infections, or spinal deformities; or possibly neuroforamen stenosis with compressed exiting nerves due to postsurgical disk collapse.
Dr. Wilco C. Peul is at Leiden (the Netherlands) University Medical Center and at Medical Center Haaglanden, the Hague. Dr. Wouter A. Moojen is at Medical Center Haaglanden. Dr. Peul reported receiving grants from ZonMW, Paradigm Spine, Medtronic, Eurospine Foundation, and CVZ. Dr. Moojen reported having no relevant financial disclosures. Dr. Peul and Dr. Moojen made these remarks in an editorial accompanying the reports on the Swedish Spinal Stenosis Study and the Spinal Laminectomy Versus Instrumented Pedicle Screw trial (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMe1600955).
Both of these studies clearly demonstrated that for most patients, stenosis surgery should be limited to decompression when no overt instability is present. Dr. Ghogawala and his colleagues correctly concluded that the modest difference in SF-36 score in favor of fusion doesn’t justify that procedure’s higher cost and complication rate.
Fusion surgery is no longer best practice and should be restricted to patients who have proven spinal instability; vertebral destruction caused by trauma, tumors, infections, or spinal deformities; or possibly neuroforamen stenosis with compressed exiting nerves due to postsurgical disk collapse.
Dr. Wilco C. Peul is at Leiden (the Netherlands) University Medical Center and at Medical Center Haaglanden, the Hague. Dr. Wouter A. Moojen is at Medical Center Haaglanden. Dr. Peul reported receiving grants from ZonMW, Paradigm Spine, Medtronic, Eurospine Foundation, and CVZ. Dr. Moojen reported having no relevant financial disclosures. Dr. Peul and Dr. Moojen made these remarks in an editorial accompanying the reports on the Swedish Spinal Stenosis Study and the Spinal Laminectomy Versus Instrumented Pedicle Screw trial (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMe1600955).
The benefit of adding lumbar fusion surgery to decompression surgery for spinal stenosis was nonexistent in one large clinical trial and very modest in another, according to separate reports published online April 13 in the New England Journal of Medicine.
Both studies indicated that, given the considerable cost and the potential complications associated with lumbar fusion, it may not be worthwhile to add it to decompression surgery for spinal stenosis. “The goal of surgery in lumbar spinal stenosis is to improve walking distance and to relieve pain by decompression of the nerve roots. The addition of instrumented fusion – ‘just to be sure’ – for the treatment of the most frequent forms of lumbar spinal stenosis does not create any added value for patients and might be regarded as an overcautious and unnecessary treatment,” Dr. Wilco C. Peul and Dr. Wouter A. Moojen said in an editorial accompanying the two reports.
Surgical decompression of spinal stenosis using laminectomy is increasingly being supplemented with lumbar fusion, which is thought to firm up spinal instability and minimize the risk of future deformity. In the United States, approximately half of patients who have surgery for spinal stenosis undergo fusion procedures. Of those who also show degenerative spondylolisthesis on preoperative imaging studies, 96% undergo fusion procedures because many spine surgeons see this as a sign of instability and a mandatory indication for fusion. However, the evidence supporting the use of fusion plus decompression, as opposed to decompression alone, is weak, according to the investigators who conducted the Swedish Spinal Stenosis Study. The other study in the New England Journal of Medicine, the Spinal Laminectomy Versus Instrumented Pedicle Screw (SLIP) trial, was conducted in the United States.
Both of those clinical trials were performed to shed further light on the issue.
In the Swedish Spinal Stenosis Study, the investigators assessed outcomes in 247 patients aged 50-80 years who were treated at seven Swedish hospitals over the course of 6 years. This open-label, superiority trial randomly assigned 124 patients to decompression surgery alone and 123 to decompression plus fusion. The primary outcome measure was score on the Oswestry Disability Index (ODI), which measures disability and quality of life in patients with low-back pain, 2 years after surgery. The ODI scale runs from 0 to 100, with higher scores indicating more severe disability, said Dr. Peter Försth of the department of surgical sciences at Uppsala (Sweden) University and the Stockholm Spine Center and his associates.
At 2 years, there was no significant difference between the two study groups; the decompression-only group had a mean ODI score of 24, and the fusion group had a mean score of 27. The ODI scores in both groups had improved from baseline to a similar degree: by 17 points with decompression alone and by 15 points with fusion. In addition, fusion surgery was not superior to decompression alone regardless of whether patients had any degree of spondylolisthesis and regardless of whether they had severe spondylolisthesis involving a vertebral slip of 7.4 mm or more, the investigators reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1513721).The two study groups also showed no significant differences in secondary outcome measures, including performance on the 6-minute walk test and subjective patient assessment of improvement in walking ability. Moreover, these results persisted in the 144 patients who were assessed at 5-year follow-up.
In contrast, decompression alone was associated with fewer complications than decompression plus fusion. Postoperative wound infection developed in only 4% of the decompression-only group, compared with 10% of the fusion group. Although this study wasn’t adequately powered to draw firm conclusions regarding complications, a previous analysis of registry data reported that adding fusion surgery to decompression surgery doubles the risk of severe adverse events in older patients, Dr. Försth and his associates said.
Decompression alone also was markedly less expensive than fusion surgery. Mean direct costs were $6,800 higher for fusion than for decompression alone, because of the additional operating time needed, the extended hospital stay, and the cost of the implant.
In the SLIP trial, the researchers compared outcomes in 66 patients aged 50-80 years who all had spinal stenosis with grade 1 degenerative spondylolisthesis. The participants were randomly assigned to undergo decompression alone (35 patients) or decompression plus fusion (31 patients) at five U.S. medical centers, said Dr. Zoher Ghogawala of the Alan and Jacqueline B. Stuart Spine Research Center in the department of neurosurgery at Lahey Hospital and Medical Center, Burlington, Mass., and his associates.
The primary outcome measure was the physical-component summary score on the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) 2 years after surgery. This scale also runs from 0 to 100, but higher scores indicate better physical health. Five points was prespecified as the minimal clinically important difference on the SF-36.
At 2 years, patients in the fusion group showed a small but significant advantage of 5.7 points on the SF-36, with a mean score of 15.2, compared with patients in the decompression-only group (mean score, 9.5). However, the ODI scores, a secondary outcome measure in this study, were not significantly different between the two study groups, Dr. Ghogawala and his associates reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1508788).Surgical complications, blood loss, and length of stay all were significantly greater with fusion than with decompression alone.
Dr. Försth’s study was supported by Uppsala University, Uppsala County Council, the Stockholm Spine Center, and Johnson & Johnson. Two of his associates reported ties to Medtronic and Quantify Research. Dr. Ghogawala’s study was supported by the Jean and David Wallace Foundation, the Greenwich Lumbar Stenosis SLIP Study Fund. His associates reported ties to numerous industry sources.
The benefit of adding lumbar fusion surgery to decompression surgery for spinal stenosis was nonexistent in one large clinical trial and very modest in another, according to separate reports published online April 13 in the New England Journal of Medicine.
Both studies indicated that, given the considerable cost and the potential complications associated with lumbar fusion, it may not be worthwhile to add it to decompression surgery for spinal stenosis. “The goal of surgery in lumbar spinal stenosis is to improve walking distance and to relieve pain by decompression of the nerve roots. The addition of instrumented fusion – ‘just to be sure’ – for the treatment of the most frequent forms of lumbar spinal stenosis does not create any added value for patients and might be regarded as an overcautious and unnecessary treatment,” Dr. Wilco C. Peul and Dr. Wouter A. Moojen said in an editorial accompanying the two reports.
Surgical decompression of spinal stenosis using laminectomy is increasingly being supplemented with lumbar fusion, which is thought to firm up spinal instability and minimize the risk of future deformity. In the United States, approximately half of patients who have surgery for spinal stenosis undergo fusion procedures. Of those who also show degenerative spondylolisthesis on preoperative imaging studies, 96% undergo fusion procedures because many spine surgeons see this as a sign of instability and a mandatory indication for fusion. However, the evidence supporting the use of fusion plus decompression, as opposed to decompression alone, is weak, according to the investigators who conducted the Swedish Spinal Stenosis Study. The other study in the New England Journal of Medicine, the Spinal Laminectomy Versus Instrumented Pedicle Screw (SLIP) trial, was conducted in the United States.
Both of those clinical trials were performed to shed further light on the issue.
In the Swedish Spinal Stenosis Study, the investigators assessed outcomes in 247 patients aged 50-80 years who were treated at seven Swedish hospitals over the course of 6 years. This open-label, superiority trial randomly assigned 124 patients to decompression surgery alone and 123 to decompression plus fusion. The primary outcome measure was score on the Oswestry Disability Index (ODI), which measures disability and quality of life in patients with low-back pain, 2 years after surgery. The ODI scale runs from 0 to 100, with higher scores indicating more severe disability, said Dr. Peter Försth of the department of surgical sciences at Uppsala (Sweden) University and the Stockholm Spine Center and his associates.
At 2 years, there was no significant difference between the two study groups; the decompression-only group had a mean ODI score of 24, and the fusion group had a mean score of 27. The ODI scores in both groups had improved from baseline to a similar degree: by 17 points with decompression alone and by 15 points with fusion. In addition, fusion surgery was not superior to decompression alone regardless of whether patients had any degree of spondylolisthesis and regardless of whether they had severe spondylolisthesis involving a vertebral slip of 7.4 mm or more, the investigators reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1513721).The two study groups also showed no significant differences in secondary outcome measures, including performance on the 6-minute walk test and subjective patient assessment of improvement in walking ability. Moreover, these results persisted in the 144 patients who were assessed at 5-year follow-up.
In contrast, decompression alone was associated with fewer complications than decompression plus fusion. Postoperative wound infection developed in only 4% of the decompression-only group, compared with 10% of the fusion group. Although this study wasn’t adequately powered to draw firm conclusions regarding complications, a previous analysis of registry data reported that adding fusion surgery to decompression surgery doubles the risk of severe adverse events in older patients, Dr. Försth and his associates said.
Decompression alone also was markedly less expensive than fusion surgery. Mean direct costs were $6,800 higher for fusion than for decompression alone, because of the additional operating time needed, the extended hospital stay, and the cost of the implant.
In the SLIP trial, the researchers compared outcomes in 66 patients aged 50-80 years who all had spinal stenosis with grade 1 degenerative spondylolisthesis. The participants were randomly assigned to undergo decompression alone (35 patients) or decompression plus fusion (31 patients) at five U.S. medical centers, said Dr. Zoher Ghogawala of the Alan and Jacqueline B. Stuart Spine Research Center in the department of neurosurgery at Lahey Hospital and Medical Center, Burlington, Mass., and his associates.
The primary outcome measure was the physical-component summary score on the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) 2 years after surgery. This scale also runs from 0 to 100, but higher scores indicate better physical health. Five points was prespecified as the minimal clinically important difference on the SF-36.
At 2 years, patients in the fusion group showed a small but significant advantage of 5.7 points on the SF-36, with a mean score of 15.2, compared with patients in the decompression-only group (mean score, 9.5). However, the ODI scores, a secondary outcome measure in this study, were not significantly different between the two study groups, Dr. Ghogawala and his associates reported (N Engl J Med. 2016 April 13. doi: 10.1056/NEJMoa1508788).Surgical complications, blood loss, and length of stay all were significantly greater with fusion than with decompression alone.
Dr. Försth’s study was supported by Uppsala University, Uppsala County Council, the Stockholm Spine Center, and Johnson & Johnson. Two of his associates reported ties to Medtronic and Quantify Research. Dr. Ghogawala’s study was supported by the Jean and David Wallace Foundation, the Greenwich Lumbar Stenosis SLIP Study Fund. His associates reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The benefit of adding lumbar fusion surgery to decompression surgery for spinal stenosis was nonexistent in one large trial and very modest in another.
Major finding: At 2 years in the Swedish Spinal Stenosis Study, there was no significant difference between the two study groups; the decompression-only group had a mean Oswestry Disability Index score of 24, and the fusion group had a mean score of 27.
Data source: Two multicenter, randomized trials involving 247 patients and 66 patients, comparing decompression surgery alone with decompression plus fusion.
Disclosures: Dr. Försth’s study was supported by Uppsala University, Uppsala County Council, Stockholm Spine Center, and Johnson & Johnson. Two of his associates reported ties to Medtronic and Quantify Research. Dr. Ghogawala’s study was supported by the Jean and David Wallace Foundation, the Greenwich Lumbar Stenosis SLIP Study Fund. His associates reported ties to numerous industry sources.