User login
Trauma surgeons can safely manage many TBI patients
SAN DIEGO – Many patients with traumatic brain injury (TBI) can be safely managed by trauma surgeons or intensive care physicians, if a guideline-based individual protocol is followed. In a recent single-center study using this protocol, charges fell, repeat imaging decreased, and patient outcomes did not suffer when neurosurgery consults were reserved for individuals with more severe brain injuries.
Every year, emergency departments see 2.5 million visits for traumatic brain injuries ranging from concussions to devastating open injuries, and 11% of those seen are hospitalized. Still, only 10% of patients with TBI will require neurosurgical intervention, Dr. Bellal Joseph of the University of Arizona said at the annual meeting of the American Surgical Association.
Finding a way to conserve resources is important, said Dr. Joseph, since the total number of emergency department visits for TBI is increasing, but resources remain constrained: neurosurgeons are in shorter supply than ever. Further, TBI management may not be changed by numerous repeat head CTs, which are costly and can expose patients to significant amounts of radiation.
Dr. Joseph and his coinvestigators at the University of Arizona had previously developed Brain Injury Guidelines (BIG), which would mandate repeat head CTs and neurosurgery consults only for larger intracranial bleeds and displaced skull fractures. The guidelines are used as part of an individualized protocol that includes overall clinical assessment and patient-specific factors, such as anticoagulation status and whether the patient was intoxicated at the time of injury.
After a period of education regarding the guidelines, the University of Arizona’s Level I trauma center – the only one in the state – implemented BIG use in 2012. For the 5-year period from 2009 to 2014 encompassing implementation of the guidelines, investigators followed all patients admitted for TBI and tracked use of hospital resources and patient outcomes during the study period.
A total of 2,184 patients with TBI were included in the study, divided into five cohorts by year of admission, and stratified by severity of brain injury. Patients were included if they were admitted for TBI from the emergency department and the initial head CT found a skull fracture or intracranial hemorrhage. Dr. Bellal and his colleagues collected data regarding the number of neurosurgery consults, repeat head CTs, and patient demographic and injury characteristics. They tracked patient outcomes including in-hospital mortality, any progression on repeat head CT, and patient disposition on discharge.
TBI injuries were classified by Glasgow Coma Scale scoring (13-15 for mild TBI; 9-12 for moderate; and less than 8 for severe).
Over time, the proportion of patients with severe brain injury who received repeat head CTs did not change significantly. However, scans for those with less severe injury declined significantly, with a marked drop in repeat head CTs seen at the time of implementation of the BIG guidelines (P < .001 for mild and P = .012 for moderate brain injuries).
Similarly, 100% of patients with severe TBI received a neurosurgical consult in each year of the study period, but the number of consults declined significantly for those with mild and moderate injuries (P < .001 for both mild and moderate injuries).
Hospital length of stay decreased from a mean 6.2 days to 4.7 at the end of the study period (P = .028), and total hospital costs fell by nearly half, from a total $8.1 million for the 2009-2010 cohort to $4.3 million for the 2013-2014 cohort (P < .001).
Mortality, discharge score on the Glasgow Coma scale, and the proportion of patients discharged to home after their hospital stay did not change significantly over the study period.
Study limitations included potential lack of generalizability to smaller or more rural centers, and the potential for confounding by changes in other institutional factors over the study period. The study did not track long-term neurologic or quality of life outcomes.
Discussant Dr. Karen Brasel of Oregon Health & Science University, Portland, said that the study is the latest in a series of reports in the TBI field that speak to the need to avoid “knee-jerk use of resources based on diagnosis alone.” She cautioned that it is still important to examine individual patient outcomes for the few patients who did not receive a neurosurgery consult but then deteriorated, to better evaluate who is at most risk for poor outcomes.
Still, said Dr. Joseph, a “guideline-based individualized protocol for traumatic brain injury can help reduce the burden on neurological services. Life changes, and so does medicine.”
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Many patients with traumatic brain injury (TBI) can be safely managed by trauma surgeons or intensive care physicians, if a guideline-based individual protocol is followed. In a recent single-center study using this protocol, charges fell, repeat imaging decreased, and patient outcomes did not suffer when neurosurgery consults were reserved for individuals with more severe brain injuries.
Every year, emergency departments see 2.5 million visits for traumatic brain injuries ranging from concussions to devastating open injuries, and 11% of those seen are hospitalized. Still, only 10% of patients with TBI will require neurosurgical intervention, Dr. Bellal Joseph of the University of Arizona said at the annual meeting of the American Surgical Association.
Finding a way to conserve resources is important, said Dr. Joseph, since the total number of emergency department visits for TBI is increasing, but resources remain constrained: neurosurgeons are in shorter supply than ever. Further, TBI management may not be changed by numerous repeat head CTs, which are costly and can expose patients to significant amounts of radiation.
Dr. Joseph and his coinvestigators at the University of Arizona had previously developed Brain Injury Guidelines (BIG), which would mandate repeat head CTs and neurosurgery consults only for larger intracranial bleeds and displaced skull fractures. The guidelines are used as part of an individualized protocol that includes overall clinical assessment and patient-specific factors, such as anticoagulation status and whether the patient was intoxicated at the time of injury.
After a period of education regarding the guidelines, the University of Arizona’s Level I trauma center – the only one in the state – implemented BIG use in 2012. For the 5-year period from 2009 to 2014 encompassing implementation of the guidelines, investigators followed all patients admitted for TBI and tracked use of hospital resources and patient outcomes during the study period.
A total of 2,184 patients with TBI were included in the study, divided into five cohorts by year of admission, and stratified by severity of brain injury. Patients were included if they were admitted for TBI from the emergency department and the initial head CT found a skull fracture or intracranial hemorrhage. Dr. Bellal and his colleagues collected data regarding the number of neurosurgery consults, repeat head CTs, and patient demographic and injury characteristics. They tracked patient outcomes including in-hospital mortality, any progression on repeat head CT, and patient disposition on discharge.
TBI injuries were classified by Glasgow Coma Scale scoring (13-15 for mild TBI; 9-12 for moderate; and less than 8 for severe).
Over time, the proportion of patients with severe brain injury who received repeat head CTs did not change significantly. However, scans for those with less severe injury declined significantly, with a marked drop in repeat head CTs seen at the time of implementation of the BIG guidelines (P < .001 for mild and P = .012 for moderate brain injuries).
Similarly, 100% of patients with severe TBI received a neurosurgical consult in each year of the study period, but the number of consults declined significantly for those with mild and moderate injuries (P < .001 for both mild and moderate injuries).
Hospital length of stay decreased from a mean 6.2 days to 4.7 at the end of the study period (P = .028), and total hospital costs fell by nearly half, from a total $8.1 million for the 2009-2010 cohort to $4.3 million for the 2013-2014 cohort (P < .001).
Mortality, discharge score on the Glasgow Coma scale, and the proportion of patients discharged to home after their hospital stay did not change significantly over the study period.
Study limitations included potential lack of generalizability to smaller or more rural centers, and the potential for confounding by changes in other institutional factors over the study period. The study did not track long-term neurologic or quality of life outcomes.
Discussant Dr. Karen Brasel of Oregon Health & Science University, Portland, said that the study is the latest in a series of reports in the TBI field that speak to the need to avoid “knee-jerk use of resources based on diagnosis alone.” She cautioned that it is still important to examine individual patient outcomes for the few patients who did not receive a neurosurgery consult but then deteriorated, to better evaluate who is at most risk for poor outcomes.
Still, said Dr. Joseph, a “guideline-based individualized protocol for traumatic brain injury can help reduce the burden on neurological services. Life changes, and so does medicine.”
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Many patients with traumatic brain injury (TBI) can be safely managed by trauma surgeons or intensive care physicians, if a guideline-based individual protocol is followed. In a recent single-center study using this protocol, charges fell, repeat imaging decreased, and patient outcomes did not suffer when neurosurgery consults were reserved for individuals with more severe brain injuries.
Every year, emergency departments see 2.5 million visits for traumatic brain injuries ranging from concussions to devastating open injuries, and 11% of those seen are hospitalized. Still, only 10% of patients with TBI will require neurosurgical intervention, Dr. Bellal Joseph of the University of Arizona said at the annual meeting of the American Surgical Association.
Finding a way to conserve resources is important, said Dr. Joseph, since the total number of emergency department visits for TBI is increasing, but resources remain constrained: neurosurgeons are in shorter supply than ever. Further, TBI management may not be changed by numerous repeat head CTs, which are costly and can expose patients to significant amounts of radiation.
Dr. Joseph and his coinvestigators at the University of Arizona had previously developed Brain Injury Guidelines (BIG), which would mandate repeat head CTs and neurosurgery consults only for larger intracranial bleeds and displaced skull fractures. The guidelines are used as part of an individualized protocol that includes overall clinical assessment and patient-specific factors, such as anticoagulation status and whether the patient was intoxicated at the time of injury.
After a period of education regarding the guidelines, the University of Arizona’s Level I trauma center – the only one in the state – implemented BIG use in 2012. For the 5-year period from 2009 to 2014 encompassing implementation of the guidelines, investigators followed all patients admitted for TBI and tracked use of hospital resources and patient outcomes during the study period.
A total of 2,184 patients with TBI were included in the study, divided into five cohorts by year of admission, and stratified by severity of brain injury. Patients were included if they were admitted for TBI from the emergency department and the initial head CT found a skull fracture or intracranial hemorrhage. Dr. Bellal and his colleagues collected data regarding the number of neurosurgery consults, repeat head CTs, and patient demographic and injury characteristics. They tracked patient outcomes including in-hospital mortality, any progression on repeat head CT, and patient disposition on discharge.
TBI injuries were classified by Glasgow Coma Scale scoring (13-15 for mild TBI; 9-12 for moderate; and less than 8 for severe).
Over time, the proportion of patients with severe brain injury who received repeat head CTs did not change significantly. However, scans for those with less severe injury declined significantly, with a marked drop in repeat head CTs seen at the time of implementation of the BIG guidelines (P < .001 for mild and P = .012 for moderate brain injuries).
Similarly, 100% of patients with severe TBI received a neurosurgical consult in each year of the study period, but the number of consults declined significantly for those with mild and moderate injuries (P < .001 for both mild and moderate injuries).
Hospital length of stay decreased from a mean 6.2 days to 4.7 at the end of the study period (P = .028), and total hospital costs fell by nearly half, from a total $8.1 million for the 2009-2010 cohort to $4.3 million for the 2013-2014 cohort (P < .001).
Mortality, discharge score on the Glasgow Coma scale, and the proportion of patients discharged to home after their hospital stay did not change significantly over the study period.
Study limitations included potential lack of generalizability to smaller or more rural centers, and the potential for confounding by changes in other institutional factors over the study period. The study did not track long-term neurologic or quality of life outcomes.
Discussant Dr. Karen Brasel of Oregon Health & Science University, Portland, said that the study is the latest in a series of reports in the TBI field that speak to the need to avoid “knee-jerk use of resources based on diagnosis alone.” She cautioned that it is still important to examine individual patient outcomes for the few patients who did not receive a neurosurgery consult but then deteriorated, to better evaluate who is at most risk for poor outcomes.
Still, said Dr. Joseph, a “guideline-based individualized protocol for traumatic brain injury can help reduce the burden on neurological services. Life changes, and so does medicine.”
The authors reported no conflicts of interest.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Patients with less severe TBIs can be safely managed by intensivists or trauma surgeons.
Major finding: For TBI patients, hospital length of stay decreased from a mean 6.2 days to 4.7 (P = .028), and total hospital costs fell by nearly half, from $8.1 million for the 2009-2010 cohort to $4.3 million for the 2013-2014 cohort (P < .001).
Data source: Prospective single-center 5-year database of all TBI patients with positive imaging findings.
Disclosures: The authors reported no conflicts of interest.
Botox treatments improve urinary incontinence in neurogenic bladder dysfunction
NEW ORLEANS – Regular injections of onabotulinumtoxinA significantly decreased urinary incontinence in patients with neurogenic detrusor bladder overactivity over 4 years of follow-up in 4-year extension study results of a randomized trial.
Incontinence episodes decreased from an average of four per day to one or less after each treatment, Dr. Eric Rovner said at the annual meeting of the American Urological Association.
Each treatment was effective for about 9 months, and the benefit consistent throughout the 4-year study, said Dr. Rovner of the Medical University of South Carolina, Charleston.
About 90% of patients had at least a 50% reduction in incontinence episodes, and more than half experienced a complete cessation of incontinence.
OnabotulinumtoxinA (Botox) was approved in 2011 as a treatment for neurogenic urinary incontinence. Each treatment consists of 20 injections delivered cystoscopically.
Dr. Rovner reported a post hoc analysis of 227 patients who completed 4 years of treatment – a 1-year placebo-controlled trial, and 3 years of open-label extension with a dosage of 200 units of onabotulinumtoxinA.
Patients were relatively young (mean 45 years); about half were male. Most (53%) had multiple sclerosis. The remainder had a spinal cord injury that affected bladder function. Half were taking an anticholinergic medication, but had not responded to it.
Most patients (71%) were already performing intermittent catheterization. Despite that, they had a mean of four incontinence episodes each day.
Over the entire 4 years, onabotulinumtoxinA was associated with significant and consistent improvements in incontinence, with a mean decrease of up to 3.8 incidents per day each year. Each year, about 90% experienced at least a 50% improvement. About half experienced a complete cessation of incontinence over the period.
Urinary tract infections occurred in 20% of patients in years 1 and 2, and 18% in years 3 and 4, which was not significantly different. Urinary retention was highest in year 1 (12%) and dropped to 2% by years 3 and 4.
In the first year, 39% of those who didn’t need intermittent catheterization at baseline had to begin doing so. By year 2, the de novo catheterization rate was 11%. It was 8% in year 3, and in year 4, there were no new catheterizations.
These changes were not only statistically significant, but clinically important, Dr. Rovner said. On a secondary measure, the Incontinence Quality of Life Questionnaire (I-QOL), patients experienced a mean increase of more than 30 points over each study year. An 11-point change is usually considered clinically meaningful, he said.
“This was making a big difference for these patients.”
Dr. Rovner disclosed relationships with Allergan and a number of other pharmaceutical and medical device companies.
On Twitter @alz_gal
NEW ORLEANS – Regular injections of onabotulinumtoxinA significantly decreased urinary incontinence in patients with neurogenic detrusor bladder overactivity over 4 years of follow-up in 4-year extension study results of a randomized trial.
Incontinence episodes decreased from an average of four per day to one or less after each treatment, Dr. Eric Rovner said at the annual meeting of the American Urological Association.
Each treatment was effective for about 9 months, and the benefit consistent throughout the 4-year study, said Dr. Rovner of the Medical University of South Carolina, Charleston.
About 90% of patients had at least a 50% reduction in incontinence episodes, and more than half experienced a complete cessation of incontinence.
OnabotulinumtoxinA (Botox) was approved in 2011 as a treatment for neurogenic urinary incontinence. Each treatment consists of 20 injections delivered cystoscopically.
Dr. Rovner reported a post hoc analysis of 227 patients who completed 4 years of treatment – a 1-year placebo-controlled trial, and 3 years of open-label extension with a dosage of 200 units of onabotulinumtoxinA.
Patients were relatively young (mean 45 years); about half were male. Most (53%) had multiple sclerosis. The remainder had a spinal cord injury that affected bladder function. Half were taking an anticholinergic medication, but had not responded to it.
Most patients (71%) were already performing intermittent catheterization. Despite that, they had a mean of four incontinence episodes each day.
Over the entire 4 years, onabotulinumtoxinA was associated with significant and consistent improvements in incontinence, with a mean decrease of up to 3.8 incidents per day each year. Each year, about 90% experienced at least a 50% improvement. About half experienced a complete cessation of incontinence over the period.
Urinary tract infections occurred in 20% of patients in years 1 and 2, and 18% in years 3 and 4, which was not significantly different. Urinary retention was highest in year 1 (12%) and dropped to 2% by years 3 and 4.
In the first year, 39% of those who didn’t need intermittent catheterization at baseline had to begin doing so. By year 2, the de novo catheterization rate was 11%. It was 8% in year 3, and in year 4, there were no new catheterizations.
These changes were not only statistically significant, but clinically important, Dr. Rovner said. On a secondary measure, the Incontinence Quality of Life Questionnaire (I-QOL), patients experienced a mean increase of more than 30 points over each study year. An 11-point change is usually considered clinically meaningful, he said.
“This was making a big difference for these patients.”
Dr. Rovner disclosed relationships with Allergan and a number of other pharmaceutical and medical device companies.
On Twitter @alz_gal
NEW ORLEANS – Regular injections of onabotulinumtoxinA significantly decreased urinary incontinence in patients with neurogenic detrusor bladder overactivity over 4 years of follow-up in 4-year extension study results of a randomized trial.
Incontinence episodes decreased from an average of four per day to one or less after each treatment, Dr. Eric Rovner said at the annual meeting of the American Urological Association.
Each treatment was effective for about 9 months, and the benefit consistent throughout the 4-year study, said Dr. Rovner of the Medical University of South Carolina, Charleston.
About 90% of patients had at least a 50% reduction in incontinence episodes, and more than half experienced a complete cessation of incontinence.
OnabotulinumtoxinA (Botox) was approved in 2011 as a treatment for neurogenic urinary incontinence. Each treatment consists of 20 injections delivered cystoscopically.
Dr. Rovner reported a post hoc analysis of 227 patients who completed 4 years of treatment – a 1-year placebo-controlled trial, and 3 years of open-label extension with a dosage of 200 units of onabotulinumtoxinA.
Patients were relatively young (mean 45 years); about half were male. Most (53%) had multiple sclerosis. The remainder had a spinal cord injury that affected bladder function. Half were taking an anticholinergic medication, but had not responded to it.
Most patients (71%) were already performing intermittent catheterization. Despite that, they had a mean of four incontinence episodes each day.
Over the entire 4 years, onabotulinumtoxinA was associated with significant and consistent improvements in incontinence, with a mean decrease of up to 3.8 incidents per day each year. Each year, about 90% experienced at least a 50% improvement. About half experienced a complete cessation of incontinence over the period.
Urinary tract infections occurred in 20% of patients in years 1 and 2, and 18% in years 3 and 4, which was not significantly different. Urinary retention was highest in year 1 (12%) and dropped to 2% by years 3 and 4.
In the first year, 39% of those who didn’t need intermittent catheterization at baseline had to begin doing so. By year 2, the de novo catheterization rate was 11%. It was 8% in year 3, and in year 4, there were no new catheterizations.
These changes were not only statistically significant, but clinically important, Dr. Rovner said. On a secondary measure, the Incontinence Quality of Life Questionnaire (I-QOL), patients experienced a mean increase of more than 30 points over each study year. An 11-point change is usually considered clinically meaningful, he said.
“This was making a big difference for these patients.”
Dr. Rovner disclosed relationships with Allergan and a number of other pharmaceutical and medical device companies.
On Twitter @alz_gal
AT THE AUA ANNUAL MEETING
Key clinical point: OnabotulinumtoxinA injections produced a consistent and significant improvement in urinary incontinence in patients with neurogenic detrusor bladder overactivity.
Major finding: Nearly 90% of patients had at least a 50% improvement in incontinence episodes, and almost half experienced a complete cessation.
Data source: A post hoc analysis of 4-year results from a 1-year, randomized, placebo-controlled trial with 3 years of open-label extension in 227 patients.
Disclosures: Dr. Rovner disclosed relationships with Allergan and a number of other pharmaceutical and medical device companies.
AAN: Scheduled daily DBS effective in small Tourette syndrome study
WASHINGTON – Scheduled administration of bilateral deep brain stimulation of the centromedian thalamus for less than 2 hours a day resulted in a significant reduction in tics in several patients with Tourette syndrome over 2 years in a proof-of-concept study presented at the annual meeting of the American Academy of Neurology.
Of the four patients who completed the 24-month study, three experienced significant improvements, said Justin Rossi, an MD-PhD candidate at the University of Florida in Gainesville.
Instead of using the standard continuous deep brain stimulation (DBS), Mr. Rossi and colleagues at the university's Center for Movement Disorders and Neurorestoration evaluated a scheduled, personalized stimulation approach, with stimulation of the centromedian thalamus (bilaterally) tailored to the times of the day when patients experienced the most sequelae from the tics, such as when they were driving, exercising, or working, and when the intensity of the tics was the greatest.
The rationale for investigating this approach is that instead of using the “classical continuous approach” to DBS, a tailored approach might be effective in these patients, with the potential benefits of increasing battery life (and delaying another surgical procedure to replace the battery) and reducing side effects associated with stimulation, Mr. Rossi said.
Many studies have found that DBS is effective in “select medication-refractory cases of Tourette syndrome,” he noted. “However, in contrast to Parkinson’s disease, essential tremor, and other movement disorders for which DBS has been commonly used as a therapy, Tourette syndrome is a paroxysmal disorder,” and the frequency of tics can vary from patient to patient, with individual patients reporting that the intensity of tics “waxes and wanes throughout the day, often predictably.”
The study enrolled five patients; responses were evaluated with two rating scales, the Yale Global Tic Severity Scale (YGTSS) and the Modified Rush Video-Based Tic Rating Scale (MRTRS). A patient was considered a responder if there was more than a 40% improvement in the YGTSS or MRTRS from the preoperative baseline level, at 24 months, the primary outcome. (One patient was lost to follow-up after 18 months because the center was too far away.) Patients had the opportunity to modify the schedule at each 6-month visit.
At 24 months, the YGTSS total scores improved by 46%, 58%, and 17% and the MRTRS total scores improved by 79%, 81%, and 44% in the three responders. These patients had a mean stimulation time of 1.85 hours a day, ranging from 47 to 186 minutes per day. The one patient who did not meet the primary endpoint – with a 10% response on the YGTSS and a 21% response in the MRTRS – had the greatest amount of stimulation per day (4 hours a day). At 24 months, the responders had statistically significant improvements from baseline in components of the two scales, including the number of phonic tics per minute, motor tic severity, and phonic tic severity, Mr. Rossi said.
This is a proof-of-concept study and the results and conclusions are preliminary, but the results “warrant larger studies,” he concluded.
More research is needed to understand this mechanism on a more physiological level, which is being pursued at his center, he added. The results shed some light on whether the mechanism of DBS in Tourette syndrome is a cumulative effect of stimulation over time or whether DBS has an effect around the time the tics occur, and these results support the latter explanation, Mr. Rossi speculated.
He had no disclosures. The study was sponsored by the National Institutes of Health.
WASHINGTON – Scheduled administration of bilateral deep brain stimulation of the centromedian thalamus for less than 2 hours a day resulted in a significant reduction in tics in several patients with Tourette syndrome over 2 years in a proof-of-concept study presented at the annual meeting of the American Academy of Neurology.
Of the four patients who completed the 24-month study, three experienced significant improvements, said Justin Rossi, an MD-PhD candidate at the University of Florida in Gainesville.
Instead of using the standard continuous deep brain stimulation (DBS), Mr. Rossi and colleagues at the university's Center for Movement Disorders and Neurorestoration evaluated a scheduled, personalized stimulation approach, with stimulation of the centromedian thalamus (bilaterally) tailored to the times of the day when patients experienced the most sequelae from the tics, such as when they were driving, exercising, or working, and when the intensity of the tics was the greatest.
The rationale for investigating this approach is that instead of using the “classical continuous approach” to DBS, a tailored approach might be effective in these patients, with the potential benefits of increasing battery life (and delaying another surgical procedure to replace the battery) and reducing side effects associated with stimulation, Mr. Rossi said.
Many studies have found that DBS is effective in “select medication-refractory cases of Tourette syndrome,” he noted. “However, in contrast to Parkinson’s disease, essential tremor, and other movement disorders for which DBS has been commonly used as a therapy, Tourette syndrome is a paroxysmal disorder,” and the frequency of tics can vary from patient to patient, with individual patients reporting that the intensity of tics “waxes and wanes throughout the day, often predictably.”
The study enrolled five patients; responses were evaluated with two rating scales, the Yale Global Tic Severity Scale (YGTSS) and the Modified Rush Video-Based Tic Rating Scale (MRTRS). A patient was considered a responder if there was more than a 40% improvement in the YGTSS or MRTRS from the preoperative baseline level, at 24 months, the primary outcome. (One patient was lost to follow-up after 18 months because the center was too far away.) Patients had the opportunity to modify the schedule at each 6-month visit.
At 24 months, the YGTSS total scores improved by 46%, 58%, and 17% and the MRTRS total scores improved by 79%, 81%, and 44% in the three responders. These patients had a mean stimulation time of 1.85 hours a day, ranging from 47 to 186 minutes per day. The one patient who did not meet the primary endpoint – with a 10% response on the YGTSS and a 21% response in the MRTRS – had the greatest amount of stimulation per day (4 hours a day). At 24 months, the responders had statistically significant improvements from baseline in components of the two scales, including the number of phonic tics per minute, motor tic severity, and phonic tic severity, Mr. Rossi said.
This is a proof-of-concept study and the results and conclusions are preliminary, but the results “warrant larger studies,” he concluded.
More research is needed to understand this mechanism on a more physiological level, which is being pursued at his center, he added. The results shed some light on whether the mechanism of DBS in Tourette syndrome is a cumulative effect of stimulation over time or whether DBS has an effect around the time the tics occur, and these results support the latter explanation, Mr. Rossi speculated.
He had no disclosures. The study was sponsored by the National Institutes of Health.
WASHINGTON – Scheduled administration of bilateral deep brain stimulation of the centromedian thalamus for less than 2 hours a day resulted in a significant reduction in tics in several patients with Tourette syndrome over 2 years in a proof-of-concept study presented at the annual meeting of the American Academy of Neurology.
Of the four patients who completed the 24-month study, three experienced significant improvements, said Justin Rossi, an MD-PhD candidate at the University of Florida in Gainesville.
Instead of using the standard continuous deep brain stimulation (DBS), Mr. Rossi and colleagues at the university's Center for Movement Disorders and Neurorestoration evaluated a scheduled, personalized stimulation approach, with stimulation of the centromedian thalamus (bilaterally) tailored to the times of the day when patients experienced the most sequelae from the tics, such as when they were driving, exercising, or working, and when the intensity of the tics was the greatest.
The rationale for investigating this approach is that instead of using the “classical continuous approach” to DBS, a tailored approach might be effective in these patients, with the potential benefits of increasing battery life (and delaying another surgical procedure to replace the battery) and reducing side effects associated with stimulation, Mr. Rossi said.
Many studies have found that DBS is effective in “select medication-refractory cases of Tourette syndrome,” he noted. “However, in contrast to Parkinson’s disease, essential tremor, and other movement disorders for which DBS has been commonly used as a therapy, Tourette syndrome is a paroxysmal disorder,” and the frequency of tics can vary from patient to patient, with individual patients reporting that the intensity of tics “waxes and wanes throughout the day, often predictably.”
The study enrolled five patients; responses were evaluated with two rating scales, the Yale Global Tic Severity Scale (YGTSS) and the Modified Rush Video-Based Tic Rating Scale (MRTRS). A patient was considered a responder if there was more than a 40% improvement in the YGTSS or MRTRS from the preoperative baseline level, at 24 months, the primary outcome. (One patient was lost to follow-up after 18 months because the center was too far away.) Patients had the opportunity to modify the schedule at each 6-month visit.
At 24 months, the YGTSS total scores improved by 46%, 58%, and 17% and the MRTRS total scores improved by 79%, 81%, and 44% in the three responders. These patients had a mean stimulation time of 1.85 hours a day, ranging from 47 to 186 minutes per day. The one patient who did not meet the primary endpoint – with a 10% response on the YGTSS and a 21% response in the MRTRS – had the greatest amount of stimulation per day (4 hours a day). At 24 months, the responders had statistically significant improvements from baseline in components of the two scales, including the number of phonic tics per minute, motor tic severity, and phonic tic severity, Mr. Rossi said.
This is a proof-of-concept study and the results and conclusions are preliminary, but the results “warrant larger studies,” he concluded.
More research is needed to understand this mechanism on a more physiological level, which is being pursued at his center, he added. The results shed some light on whether the mechanism of DBS in Tourette syndrome is a cumulative effect of stimulation over time or whether DBS has an effect around the time the tics occur, and these results support the latter explanation, Mr. Rossi speculated.
He had no disclosures. The study was sponsored by the National Institutes of Health.
AT THE AAN 2015 ANNUAL MEETING
Key clinical point: Promising results of a tailored approach to deep brain stimulation in three patients with Tourette syndrome merits a larger trial.
Major finding: In three of the four patients who completed the study, DBS of the centromedian thalamus for less than 2 hours a day resulted in significant improvements over 24 months.
Data source: A proof-of-concept study in five patients with Tourette syndrome, evaluating DBS of the centromedian thalamus, scheduled for times when tics interfered with activities or were most intense.
Disclosures: The National Institutes of Health sponsored the study. Mr. Rossi had no disclosures.
AAN: Facial nerve stimulator relieves cluster headaches
WASHINGTON – An implantable device that stimulates the sphenopalatine ganglion nerve bundle either reduced or eliminated pain in 68% of more than 5,000 cluster headaches, a 3-year study has determined.
The device, which is approved in Europe, was more effective in attacks of moderate severity, with a 78% rate of pain reduction or elimination, Dr. Jose Miguel Lainez reported at the annual meeting of the American Academy of Neurology.
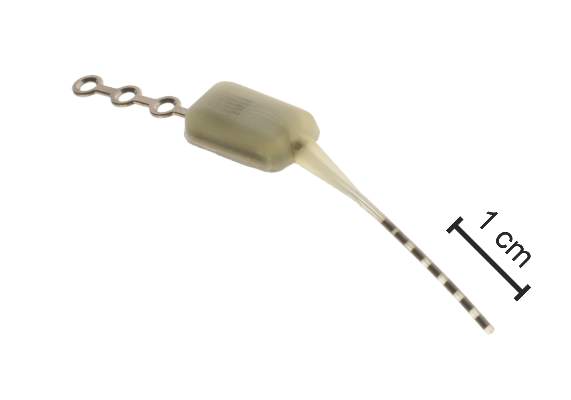
The Pulsante System, manufactured by Autonomic Technologiesof Redwood City, Calif., consists of a neurostimulator about the size of an almond, and a lead with six electrodes. It’s inserted under local anesthetic via a small incision in the upper gum on the side in which the patient experiences symptoms. The electrodes are positioned along the sphenopalatine ganglion (SPG) nerve and the neurostimulator is affixed to the zygomatic process.
A hand-held remote controller placed against the cheek activates the device and controls the intensity of stimulation, which is thought to work by blocking signals to the postganglionic parasympathetic fibers. Those fibers innervate facial structures and the cerebral and meningeal blood vessels and are implicated in the pain and accompanying autonomic symptoms of a cluster headache attack.
Dr. Lainez, professor of neurology at Catholic University of Valencia (Spain), presented 3-year follow-up data from Pathway CH-1, a randomized, sham-controlled trial of 43 patients with cluster headache. Of these, 33 completed the 3-year follow-up period. Of the remaining 10, 1 was lost from observation, 5 violated protocol, 1 had the device implanted incorrectly, and 3 had the device explanted because of incorrect placement or lead migration.
Most of the patients were male. Mean age was 41 years. They had a mean disease duration of 10 years and averaged 17 cluster headaches per week but ranged from 4 to 70 attacks per week. Over the 3 years, 5,130 attacks were treated; the mean stimulation duration for these was 14 minutes with a mean response time of 11 minutes. Therapy was considered effective in 65% (3,354) of these attacks based on a clinically meaningful reduction in pain or pain elimination.
Dr. Lainez did not parse these results. However, in the initial 28-week phase of the Pathway CH-1 study, pain was reduced in 68% of attacks treated with the device and 7% of those treated with the sham control. Pain freedom by 15 minutes was achieved in 34% of attacks with full stimulation, compared with 1.5% of those treated with sham.
In the follow-up study, the device seemed most effective in attacks of moderate severity (78% response rate of pain reduction or elimination). The response rate was 59% in mild attacks and 51% in severe attacks. Most attacks treated with the device (77%) did not involve the use of abortive therapy.
Dr. Lainez did not mention adverse events related to the device. However, in the 28-week study, there were 92, including parasthesias and numbness; facial and tooth pain; and swelling. Others were considered mild and included dry eye, nose bleed, and facial asymmetry.
The device is currently being investigated in a U.S. study. The open-label Pathway-CH2 study aims to recruit 120 patients. For information on Pathway CH-2, contact Anthony Caparso.
The trial was sponsored by Autonomic Technologies Inc. Dr. Lainez had no financial ties with the company.
On Twitter @alz_gal
WASHINGTON – An implantable device that stimulates the sphenopalatine ganglion nerve bundle either reduced or eliminated pain in 68% of more than 5,000 cluster headaches, a 3-year study has determined.
The device, which is approved in Europe, was more effective in attacks of moderate severity, with a 78% rate of pain reduction or elimination, Dr. Jose Miguel Lainez reported at the annual meeting of the American Academy of Neurology.
The Pulsante System, manufactured by Autonomic Technologiesof Redwood City, Calif., consists of a neurostimulator about the size of an almond, and a lead with six electrodes. It’s inserted under local anesthetic via a small incision in the upper gum on the side in which the patient experiences symptoms. The electrodes are positioned along the sphenopalatine ganglion (SPG) nerve and the neurostimulator is affixed to the zygomatic process.
A hand-held remote controller placed against the cheek activates the device and controls the intensity of stimulation, which is thought to work by blocking signals to the postganglionic parasympathetic fibers. Those fibers innervate facial structures and the cerebral and meningeal blood vessels and are implicated in the pain and accompanying autonomic symptoms of a cluster headache attack.
Dr. Lainez, professor of neurology at Catholic University of Valencia (Spain), presented 3-year follow-up data from Pathway CH-1, a randomized, sham-controlled trial of 43 patients with cluster headache. Of these, 33 completed the 3-year follow-up period. Of the remaining 10, 1 was lost from observation, 5 violated protocol, 1 had the device implanted incorrectly, and 3 had the device explanted because of incorrect placement or lead migration.
Most of the patients were male. Mean age was 41 years. They had a mean disease duration of 10 years and averaged 17 cluster headaches per week but ranged from 4 to 70 attacks per week. Over the 3 years, 5,130 attacks were treated; the mean stimulation duration for these was 14 minutes with a mean response time of 11 minutes. Therapy was considered effective in 65% (3,354) of these attacks based on a clinically meaningful reduction in pain or pain elimination.
Dr. Lainez did not parse these results. However, in the initial 28-week phase of the Pathway CH-1 study, pain was reduced in 68% of attacks treated with the device and 7% of those treated with the sham control. Pain freedom by 15 minutes was achieved in 34% of attacks with full stimulation, compared with 1.5% of those treated with sham.
In the follow-up study, the device seemed most effective in attacks of moderate severity (78% response rate of pain reduction or elimination). The response rate was 59% in mild attacks and 51% in severe attacks. Most attacks treated with the device (77%) did not involve the use of abortive therapy.
Dr. Lainez did not mention adverse events related to the device. However, in the 28-week study, there were 92, including parasthesias and numbness; facial and tooth pain; and swelling. Others were considered mild and included dry eye, nose bleed, and facial asymmetry.
The device is currently being investigated in a U.S. study. The open-label Pathway-CH2 study aims to recruit 120 patients. For information on Pathway CH-2, contact Anthony Caparso.
The trial was sponsored by Autonomic Technologies Inc. Dr. Lainez had no financial ties with the company.
On Twitter @alz_gal
WASHINGTON – An implantable device that stimulates the sphenopalatine ganglion nerve bundle either reduced or eliminated pain in 68% of more than 5,000 cluster headaches, a 3-year study has determined.
The device, which is approved in Europe, was more effective in attacks of moderate severity, with a 78% rate of pain reduction or elimination, Dr. Jose Miguel Lainez reported at the annual meeting of the American Academy of Neurology.
The Pulsante System, manufactured by Autonomic Technologiesof Redwood City, Calif., consists of a neurostimulator about the size of an almond, and a lead with six electrodes. It’s inserted under local anesthetic via a small incision in the upper gum on the side in which the patient experiences symptoms. The electrodes are positioned along the sphenopalatine ganglion (SPG) nerve and the neurostimulator is affixed to the zygomatic process.
A hand-held remote controller placed against the cheek activates the device and controls the intensity of stimulation, which is thought to work by blocking signals to the postganglionic parasympathetic fibers. Those fibers innervate facial structures and the cerebral and meningeal blood vessels and are implicated in the pain and accompanying autonomic symptoms of a cluster headache attack.
Dr. Lainez, professor of neurology at Catholic University of Valencia (Spain), presented 3-year follow-up data from Pathway CH-1, a randomized, sham-controlled trial of 43 patients with cluster headache. Of these, 33 completed the 3-year follow-up period. Of the remaining 10, 1 was lost from observation, 5 violated protocol, 1 had the device implanted incorrectly, and 3 had the device explanted because of incorrect placement or lead migration.
Most of the patients were male. Mean age was 41 years. They had a mean disease duration of 10 years and averaged 17 cluster headaches per week but ranged from 4 to 70 attacks per week. Over the 3 years, 5,130 attacks were treated; the mean stimulation duration for these was 14 minutes with a mean response time of 11 minutes. Therapy was considered effective in 65% (3,354) of these attacks based on a clinically meaningful reduction in pain or pain elimination.
Dr. Lainez did not parse these results. However, in the initial 28-week phase of the Pathway CH-1 study, pain was reduced in 68% of attacks treated with the device and 7% of those treated with the sham control. Pain freedom by 15 minutes was achieved in 34% of attacks with full stimulation, compared with 1.5% of those treated with sham.
In the follow-up study, the device seemed most effective in attacks of moderate severity (78% response rate of pain reduction or elimination). The response rate was 59% in mild attacks and 51% in severe attacks. Most attacks treated with the device (77%) did not involve the use of abortive therapy.
Dr. Lainez did not mention adverse events related to the device. However, in the 28-week study, there were 92, including parasthesias and numbness; facial and tooth pain; and swelling. Others were considered mild and included dry eye, nose bleed, and facial asymmetry.
The device is currently being investigated in a U.S. study. The open-label Pathway-CH2 study aims to recruit 120 patients. For information on Pathway CH-2, contact Anthony Caparso.
The trial was sponsored by Autonomic Technologies Inc. Dr. Lainez had no financial ties with the company.
On Twitter @alz_gal
AT THE AAN 2015 ANNUAL MEETING
Key clinical point: An implantable device that stimulates the sphenopalatine ganglion nerve provided pain relief in cluster headaches.
Major finding: The device reduced or eliminated pain in 68% of more than 5,000 cluster headaches.
Data source: A 3-year follow-up study that examined response in more than 5,000 cluster headaches.
Disclosures: The trial was sponsored by Autonomic Technologies Inc., which makes the Pulsante System. Dr. Lainez had no financial disclosures.
Is brain damage an ‘inevitable consequence or an avoidable risk’ of American football?
More research is needed to better understand and prevent traumatic brain injury such as chronic traumatic encephalopathy in American football players, Chad A. Asplund and Dr. Thomas M. Best wrote in an editorial published March 24 in BMJ.
Currently, chronic traumatic encephalopathy (CTE) can be formally diagnosed only at autopsy.
Though the National Football League denies a relationship between football and CTE, all confirmed cases of the disease in American football players to date were in those with a history of repetitive blows to the head. Athletes who began playing football before 12 years of age show greater cognitive impairment in older age than do those who started later, according to the authors.
“Further work into risk mitigation, paralleled with increased research into the pathophysiology of both concussion and CTE, is needed,” the authors wrote. “For now, it seems that the more we learn about CTE, the more questions are left unanswered – it still remains unclear if brain damage is an inevitable consequence or an avoidable risk of American football.”
Read the full article here: BMJ 2015;349:h1381 (doi:10.1136/bmj.h1381).
More research is needed to better understand and prevent traumatic brain injury such as chronic traumatic encephalopathy in American football players, Chad A. Asplund and Dr. Thomas M. Best wrote in an editorial published March 24 in BMJ.
Currently, chronic traumatic encephalopathy (CTE) can be formally diagnosed only at autopsy.
Though the National Football League denies a relationship between football and CTE, all confirmed cases of the disease in American football players to date were in those with a history of repetitive blows to the head. Athletes who began playing football before 12 years of age show greater cognitive impairment in older age than do those who started later, according to the authors.
“Further work into risk mitigation, paralleled with increased research into the pathophysiology of both concussion and CTE, is needed,” the authors wrote. “For now, it seems that the more we learn about CTE, the more questions are left unanswered – it still remains unclear if brain damage is an inevitable consequence or an avoidable risk of American football.”
Read the full article here: BMJ 2015;349:h1381 (doi:10.1136/bmj.h1381).
More research is needed to better understand and prevent traumatic brain injury such as chronic traumatic encephalopathy in American football players, Chad A. Asplund and Dr. Thomas M. Best wrote in an editorial published March 24 in BMJ.
Currently, chronic traumatic encephalopathy (CTE) can be formally diagnosed only at autopsy.
Though the National Football League denies a relationship between football and CTE, all confirmed cases of the disease in American football players to date were in those with a history of repetitive blows to the head. Athletes who began playing football before 12 years of age show greater cognitive impairment in older age than do those who started later, according to the authors.
“Further work into risk mitigation, paralleled with increased research into the pathophysiology of both concussion and CTE, is needed,” the authors wrote. “For now, it seems that the more we learn about CTE, the more questions are left unanswered – it still remains unclear if brain damage is an inevitable consequence or an avoidable risk of American football.”
Read the full article here: BMJ 2015;349:h1381 (doi:10.1136/bmj.h1381).
Algorithm may predict intracranial pressure swings after TBI
LAKE BUENA VISTA, FLA. – An algorithm might predict whether patients with severe traumatic brain injury are recovering well or need interventions to preempt evolving intracranial hypertension.
“Valid predictive algorithms have the potential to revolutionize the care of patients with traumatic brain injury [TBI] and transform physiologic data from just a pure numeric value buried in a never-ending nursing flow sheet into a useful triage and decision-assist tool,” study author Dr. Brandon Bonds said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
A minimum of 10 hours of continuous data on vital signs (intracranial pressure, heart rate, systolic blood pressure, shock index, and mean arterial pressure) were used to predict intracranial pressure (ICP) values for a retrospective cohort of 132 adults with severe TBI, 97% of which was the result of blunt trauma. Even relatively brief episodes of elevated ICP have been shown to be associated with poor outcomes in TBI patients, while marked elevation of ICP may lead to herniation and death, said Dr. Bonds of the R. Adams Cowley Shock Trauma Center, University of Maryland, Baltimore.
At the trauma center, vital signs are automatically collected every 6 seconds, 24 hours a day, on all TBI patients. This granularity of data was used to map patterns in the patients’ physiology. The approach used a nearest neighbor regression (NNR) method: A model was constructed that predicts future numerical values for an individual based on comparisons to data from historical subjects.
The same mathematical principal is used by a variety of industries to predict likely responses. NetFlix, for example, uses a system similar to the NNR method to predict future television and movie picks based on prior selections, Dr. Bonds explained.
About 20 minutes of continuously collected, automated vital sign data were then used to test the algorithm on a per-patient basis. The algorithm was used to predict future ICP values at 5 minutes to 2 hours from that time. The predictions are made on a rolling basis, with patient data updates every 5 minutes.
The NNR model was good at predicting actual ICP at 5 minutes, with a bias of 0.02 (± 2 standard deviations of 4 mm Hg). As expected, agreement was somewhat lessened at 2 hours (± 2 standard deviations of 10 mm Hg), “but this may still represent a clinically significant value,” Dr. Bonds said.
The next step is a prospective study of the algorithm’s utility.
Dr. Bonds said that NNR research really isn’t all that alien to medicine. Think about the experienced emergency physician who can look out into the wait room and “tell the nurse to bring back [a certain patient] because he didn’t look good,” Dr. Bonds said. Such a physician uses “the minimum amount of data he has and compares that patient to the historic data set of the thousands of patients that he’s seen previously to identify a patient that’s not going to do well. What we’re trying to do with this model is take this subjective skill and turn it into an objective tool.”
In an interview, session comoderator Dr. David A. Hampton, M.Eng., of Oregon Health and Science University in Portland, commented that he could definitely see the NNR method eventually having utility in severe TBI.
Future work will need to address outliers in the data because the standard deviation of 4 mm Hg “is pretty big for ICP swings” and to determine whether multiple libraries of data will need to be created based upon the different types of patients who come in, he said.
The study was funded by the United States Air Force. Dr. Bonds and his coauthors reported no financial disclosures.
LAKE BUENA VISTA, FLA. – An algorithm might predict whether patients with severe traumatic brain injury are recovering well or need interventions to preempt evolving intracranial hypertension.
“Valid predictive algorithms have the potential to revolutionize the care of patients with traumatic brain injury [TBI] and transform physiologic data from just a pure numeric value buried in a never-ending nursing flow sheet into a useful triage and decision-assist tool,” study author Dr. Brandon Bonds said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
A minimum of 10 hours of continuous data on vital signs (intracranial pressure, heart rate, systolic blood pressure, shock index, and mean arterial pressure) were used to predict intracranial pressure (ICP) values for a retrospective cohort of 132 adults with severe TBI, 97% of which was the result of blunt trauma. Even relatively brief episodes of elevated ICP have been shown to be associated with poor outcomes in TBI patients, while marked elevation of ICP may lead to herniation and death, said Dr. Bonds of the R. Adams Cowley Shock Trauma Center, University of Maryland, Baltimore.
At the trauma center, vital signs are automatically collected every 6 seconds, 24 hours a day, on all TBI patients. This granularity of data was used to map patterns in the patients’ physiology. The approach used a nearest neighbor regression (NNR) method: A model was constructed that predicts future numerical values for an individual based on comparisons to data from historical subjects.
The same mathematical principal is used by a variety of industries to predict likely responses. NetFlix, for example, uses a system similar to the NNR method to predict future television and movie picks based on prior selections, Dr. Bonds explained.
About 20 minutes of continuously collected, automated vital sign data were then used to test the algorithm on a per-patient basis. The algorithm was used to predict future ICP values at 5 minutes to 2 hours from that time. The predictions are made on a rolling basis, with patient data updates every 5 minutes.
The NNR model was good at predicting actual ICP at 5 minutes, with a bias of 0.02 (± 2 standard deviations of 4 mm Hg). As expected, agreement was somewhat lessened at 2 hours (± 2 standard deviations of 10 mm Hg), “but this may still represent a clinically significant value,” Dr. Bonds said.
The next step is a prospective study of the algorithm’s utility.
Dr. Bonds said that NNR research really isn’t all that alien to medicine. Think about the experienced emergency physician who can look out into the wait room and “tell the nurse to bring back [a certain patient] because he didn’t look good,” Dr. Bonds said. Such a physician uses “the minimum amount of data he has and compares that patient to the historic data set of the thousands of patients that he’s seen previously to identify a patient that’s not going to do well. What we’re trying to do with this model is take this subjective skill and turn it into an objective tool.”
In an interview, session comoderator Dr. David A. Hampton, M.Eng., of Oregon Health and Science University in Portland, commented that he could definitely see the NNR method eventually having utility in severe TBI.
Future work will need to address outliers in the data because the standard deviation of 4 mm Hg “is pretty big for ICP swings” and to determine whether multiple libraries of data will need to be created based upon the different types of patients who come in, he said.
The study was funded by the United States Air Force. Dr. Bonds and his coauthors reported no financial disclosures.
LAKE BUENA VISTA, FLA. – An algorithm might predict whether patients with severe traumatic brain injury are recovering well or need interventions to preempt evolving intracranial hypertension.
“Valid predictive algorithms have the potential to revolutionize the care of patients with traumatic brain injury [TBI] and transform physiologic data from just a pure numeric value buried in a never-ending nursing flow sheet into a useful triage and decision-assist tool,” study author Dr. Brandon Bonds said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
A minimum of 10 hours of continuous data on vital signs (intracranial pressure, heart rate, systolic blood pressure, shock index, and mean arterial pressure) were used to predict intracranial pressure (ICP) values for a retrospective cohort of 132 adults with severe TBI, 97% of which was the result of blunt trauma. Even relatively brief episodes of elevated ICP have been shown to be associated with poor outcomes in TBI patients, while marked elevation of ICP may lead to herniation and death, said Dr. Bonds of the R. Adams Cowley Shock Trauma Center, University of Maryland, Baltimore.
At the trauma center, vital signs are automatically collected every 6 seconds, 24 hours a day, on all TBI patients. This granularity of data was used to map patterns in the patients’ physiology. The approach used a nearest neighbor regression (NNR) method: A model was constructed that predicts future numerical values for an individual based on comparisons to data from historical subjects.
The same mathematical principal is used by a variety of industries to predict likely responses. NetFlix, for example, uses a system similar to the NNR method to predict future television and movie picks based on prior selections, Dr. Bonds explained.
About 20 minutes of continuously collected, automated vital sign data were then used to test the algorithm on a per-patient basis. The algorithm was used to predict future ICP values at 5 minutes to 2 hours from that time. The predictions are made on a rolling basis, with patient data updates every 5 minutes.
The NNR model was good at predicting actual ICP at 5 minutes, with a bias of 0.02 (± 2 standard deviations of 4 mm Hg). As expected, agreement was somewhat lessened at 2 hours (± 2 standard deviations of 10 mm Hg), “but this may still represent a clinically significant value,” Dr. Bonds said.
The next step is a prospective study of the algorithm’s utility.
Dr. Bonds said that NNR research really isn’t all that alien to medicine. Think about the experienced emergency physician who can look out into the wait room and “tell the nurse to bring back [a certain patient] because he didn’t look good,” Dr. Bonds said. Such a physician uses “the minimum amount of data he has and compares that patient to the historic data set of the thousands of patients that he’s seen previously to identify a patient that’s not going to do well. What we’re trying to do with this model is take this subjective skill and turn it into an objective tool.”
In an interview, session comoderator Dr. David A. Hampton, M.Eng., of Oregon Health and Science University in Portland, commented that he could definitely see the NNR method eventually having utility in severe TBI.
Future work will need to address outliers in the data because the standard deviation of 4 mm Hg “is pretty big for ICP swings” and to determine whether multiple libraries of data will need to be created based upon the different types of patients who come in, he said.
The study was funded by the United States Air Force. Dr. Bonds and his coauthors reported no financial disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: A short duration of vital sign data might prove useful for forecasting secondary intracranial pressure swings after traumatic brain injury.
Major finding: A model based on data from severe TBI patients predicted fluctuations in ICP at 5 minutes with a standard deviation of 4 mm Hg.
Data source: Retrospective study in 132 patients.
Disclosures: The study was funded by the United States Air Force. Dr. Bonds and his coauthors reported no financial disclosures.
General anesthesia linked to worsened stroke outcomes
NASHVILLE, TENN. – When acute ischemic stroke patients undergo an emergency endovascular procedure is it best done with general anesthesia or nongeneral anesthesia?
A post hoc analysis of data collected by a Dutch randomized, controlled trial of intra-arterial therapy suggested that nongeneral anesthesia was associated with substantially better patient outcomes, and the findings convinced the Dutch investigators who ran the study to stick with nongeneral anesthesia as their default approach.
In MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) (N. Engl. J. Med. 2015;372:11-20), 216 acute ischemic stroke patients underwent intra-arterial treatment following randomization. Among these patients, 79 were treated with general anesthesia and 137 with nongeneral anesthesia. The anesthesia choice was made on a case-by-case basis by each participating interventionalist.
The study’s primary endpoint – 90-day status rated as a good function based on a modified Rankin sale score of 0-2 – occurred in 38% of the intra-arterial patients treated with nongeneral anesthesia, 23% of the intra-arterial patients treated with general anesthesia, and 19% among the control patients who received standard treatment without intra-arterial intervention.
“The effect on outcome that we found with intra-arterial treatment in MR CLEAN was not observed in the subgroup of patients treated with general anesthesia,” said Dr. Olvert A. Berkhemer at the International Stroke Conference. The analysis also showed that patients in the general and nongeneral anesthesia subgroups had similar stroke severity as measured by their National Institutes of Health Stroke Scale score, said Dr. Berkhemer, a researcher at the Academic Medical Center in Amsterdam.
But U.S. stroke specialists who heard the report cautioned that unidentified confounders might explain the results, and they also expressed skepticism that the Dutch observations would deter U.S. interventionalists from continuing to use general anesthesia when they perform endovascular procedures.
“The big concern [about this analysis] is that there may have been some things about the general anesthesia patients that they did not account for. I suspect there is a huge bias, that general anesthesia patients were sicker,” said Dr. Bruce Ovbiagele, professor and chief of neurology at the Medical University of South Carolina in Charleston. “At my institution they have used nongeneral anesthesia, but I have been at other places where they usually use general anesthesia; it is variable,” Dr. Ovbiagele added.
Dr. Berkhemer’s analysis also showed that general anesthesia linked with a delayed start to treatment, but without resulting in a significant difference in time to reperfusion. He noted that “sometimes you cannot do the procedure without general anesthesia,” and in MR CLEAN 6 of the 137 intra-arterial patients who started with nongeneral anesthesia eventually received general anesthesia because of discomfort and pain, Dr. Berkhemer said at the conference, sponsored by the American Heart Association.
He speculated that patients who did not receive general anesthesia did better because they did not undergo acute episodes of reduced blood pressure caused by the hypotensive effect of general anesthesia.
The findings reinforced the approach already used in most of the Dutch centers that participated in MR CLEAN, where nongeneral anesthesia is preferred when possible. “In our center we always use nongeneral anesthesia, we are happy with that and we are not going to change,” said Dr. Diederik W.J. Dippel, lead investigator of MR CLEAN and professor of neurology at Erasmus University Medical Center in Rotterdam, The Netherlands. This prejudice against general anesthesia would make it hard to run a trial in The Netherlands that matched the two anesthesia approaches against each other, Dr. Dippel added.
On Twitter @mitchelzoler
Results from prior analyses had also shown better outcomes of acute ischemic stroke patients undergoing endovascular intervention when they avoided general anesthesia. A notable feature of Dr. Berkhemer’s analysis was that the stroke severity levels were well balanced between the patients who received general anesthesia and those who did not. But many other factors aside from stroke severity can affect whether or not a patient receives general anesthesia.

|
Dr. Larry B. Goldstein |
Although the outcome differences seen in this analysis were striking, many factors could have contributed. Patients received different drugs, patients may have had widely divergent clinical states despite their similar stroke severity, and the people performing the procedures were different. The many variables make it very hard to pinpoint the cause of the different outcomes.
At my institution, Duke, the interventionalists who work on acute ischemic stroke patients almost exclusively use general anesthesia. That’s because of their concern about how patients will act during a very delicate procedure. For example, stroke patients can have an aphasia that makes it hard for them to respond to requests to do something specific during the procedure. I am very skeptical that my colleagues will decide to switch to using no general anesthesia based on the results of this new analysis.
I agree with the Dutch investigators that a randomized, controlled trial of general anesthesia or no general anesthesia would be very hard to perform because individual interventionalists would need to believe there is equipoise between the two anesthesia approaches. Most interventionalists right now probably believe the approach they have always used remains best and so would be unwilling to participate in a randomized controlled trial.
Dr. Larry B. Goldstein is professor of neurology and chief of the stroke center at Duke University in Durham, N.C. He had no relevant disclosures. He made these comments in an interview.
Results from prior analyses had also shown better outcomes of acute ischemic stroke patients undergoing endovascular intervention when they avoided general anesthesia. A notable feature of Dr. Berkhemer’s analysis was that the stroke severity levels were well balanced between the patients who received general anesthesia and those who did not. But many other factors aside from stroke severity can affect whether or not a patient receives general anesthesia.

|
Dr. Larry B. Goldstein |
Although the outcome differences seen in this analysis were striking, many factors could have contributed. Patients received different drugs, patients may have had widely divergent clinical states despite their similar stroke severity, and the people performing the procedures were different. The many variables make it very hard to pinpoint the cause of the different outcomes.
At my institution, Duke, the interventionalists who work on acute ischemic stroke patients almost exclusively use general anesthesia. That’s because of their concern about how patients will act during a very delicate procedure. For example, stroke patients can have an aphasia that makes it hard for them to respond to requests to do something specific during the procedure. I am very skeptical that my colleagues will decide to switch to using no general anesthesia based on the results of this new analysis.
I agree with the Dutch investigators that a randomized, controlled trial of general anesthesia or no general anesthesia would be very hard to perform because individual interventionalists would need to believe there is equipoise between the two anesthesia approaches. Most interventionalists right now probably believe the approach they have always used remains best and so would be unwilling to participate in a randomized controlled trial.
Dr. Larry B. Goldstein is professor of neurology and chief of the stroke center at Duke University in Durham, N.C. He had no relevant disclosures. He made these comments in an interview.
Results from prior analyses had also shown better outcomes of acute ischemic stroke patients undergoing endovascular intervention when they avoided general anesthesia. A notable feature of Dr. Berkhemer’s analysis was that the stroke severity levels were well balanced between the patients who received general anesthesia and those who did not. But many other factors aside from stroke severity can affect whether or not a patient receives general anesthesia.

|
Dr. Larry B. Goldstein |
Although the outcome differences seen in this analysis were striking, many factors could have contributed. Patients received different drugs, patients may have had widely divergent clinical states despite their similar stroke severity, and the people performing the procedures were different. The many variables make it very hard to pinpoint the cause of the different outcomes.
At my institution, Duke, the interventionalists who work on acute ischemic stroke patients almost exclusively use general anesthesia. That’s because of their concern about how patients will act during a very delicate procedure. For example, stroke patients can have an aphasia that makes it hard for them to respond to requests to do something specific during the procedure. I am very skeptical that my colleagues will decide to switch to using no general anesthesia based on the results of this new analysis.
I agree with the Dutch investigators that a randomized, controlled trial of general anesthesia or no general anesthesia would be very hard to perform because individual interventionalists would need to believe there is equipoise between the two anesthesia approaches. Most interventionalists right now probably believe the approach they have always used remains best and so would be unwilling to participate in a randomized controlled trial.
Dr. Larry B. Goldstein is professor of neurology and chief of the stroke center at Duke University in Durham, N.C. He had no relevant disclosures. He made these comments in an interview.
NASHVILLE, TENN. – When acute ischemic stroke patients undergo an emergency endovascular procedure is it best done with general anesthesia or nongeneral anesthesia?
A post hoc analysis of data collected by a Dutch randomized, controlled trial of intra-arterial therapy suggested that nongeneral anesthesia was associated with substantially better patient outcomes, and the findings convinced the Dutch investigators who ran the study to stick with nongeneral anesthesia as their default approach.
In MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) (N. Engl. J. Med. 2015;372:11-20), 216 acute ischemic stroke patients underwent intra-arterial treatment following randomization. Among these patients, 79 were treated with general anesthesia and 137 with nongeneral anesthesia. The anesthesia choice was made on a case-by-case basis by each participating interventionalist.
The study’s primary endpoint – 90-day status rated as a good function based on a modified Rankin sale score of 0-2 – occurred in 38% of the intra-arterial patients treated with nongeneral anesthesia, 23% of the intra-arterial patients treated with general anesthesia, and 19% among the control patients who received standard treatment without intra-arterial intervention.
“The effect on outcome that we found with intra-arterial treatment in MR CLEAN was not observed in the subgroup of patients treated with general anesthesia,” said Dr. Olvert A. Berkhemer at the International Stroke Conference. The analysis also showed that patients in the general and nongeneral anesthesia subgroups had similar stroke severity as measured by their National Institutes of Health Stroke Scale score, said Dr. Berkhemer, a researcher at the Academic Medical Center in Amsterdam.
But U.S. stroke specialists who heard the report cautioned that unidentified confounders might explain the results, and they also expressed skepticism that the Dutch observations would deter U.S. interventionalists from continuing to use general anesthesia when they perform endovascular procedures.
“The big concern [about this analysis] is that there may have been some things about the general anesthesia patients that they did not account for. I suspect there is a huge bias, that general anesthesia patients were sicker,” said Dr. Bruce Ovbiagele, professor and chief of neurology at the Medical University of South Carolina in Charleston. “At my institution they have used nongeneral anesthesia, but I have been at other places where they usually use general anesthesia; it is variable,” Dr. Ovbiagele added.
Dr. Berkhemer’s analysis also showed that general anesthesia linked with a delayed start to treatment, but without resulting in a significant difference in time to reperfusion. He noted that “sometimes you cannot do the procedure without general anesthesia,” and in MR CLEAN 6 of the 137 intra-arterial patients who started with nongeneral anesthesia eventually received general anesthesia because of discomfort and pain, Dr. Berkhemer said at the conference, sponsored by the American Heart Association.
He speculated that patients who did not receive general anesthesia did better because they did not undergo acute episodes of reduced blood pressure caused by the hypotensive effect of general anesthesia.
The findings reinforced the approach already used in most of the Dutch centers that participated in MR CLEAN, where nongeneral anesthesia is preferred when possible. “In our center we always use nongeneral anesthesia, we are happy with that and we are not going to change,” said Dr. Diederik W.J. Dippel, lead investigator of MR CLEAN and professor of neurology at Erasmus University Medical Center in Rotterdam, The Netherlands. This prejudice against general anesthesia would make it hard to run a trial in The Netherlands that matched the two anesthesia approaches against each other, Dr. Dippel added.
On Twitter @mitchelzoler
NASHVILLE, TENN. – When acute ischemic stroke patients undergo an emergency endovascular procedure is it best done with general anesthesia or nongeneral anesthesia?
A post hoc analysis of data collected by a Dutch randomized, controlled trial of intra-arterial therapy suggested that nongeneral anesthesia was associated with substantially better patient outcomes, and the findings convinced the Dutch investigators who ran the study to stick with nongeneral anesthesia as their default approach.
In MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) (N. Engl. J. Med. 2015;372:11-20), 216 acute ischemic stroke patients underwent intra-arterial treatment following randomization. Among these patients, 79 were treated with general anesthesia and 137 with nongeneral anesthesia. The anesthesia choice was made on a case-by-case basis by each participating interventionalist.
The study’s primary endpoint – 90-day status rated as a good function based on a modified Rankin sale score of 0-2 – occurred in 38% of the intra-arterial patients treated with nongeneral anesthesia, 23% of the intra-arterial patients treated with general anesthesia, and 19% among the control patients who received standard treatment without intra-arterial intervention.
“The effect on outcome that we found with intra-arterial treatment in MR CLEAN was not observed in the subgroup of patients treated with general anesthesia,” said Dr. Olvert A. Berkhemer at the International Stroke Conference. The analysis also showed that patients in the general and nongeneral anesthesia subgroups had similar stroke severity as measured by their National Institutes of Health Stroke Scale score, said Dr. Berkhemer, a researcher at the Academic Medical Center in Amsterdam.
But U.S. stroke specialists who heard the report cautioned that unidentified confounders might explain the results, and they also expressed skepticism that the Dutch observations would deter U.S. interventionalists from continuing to use general anesthesia when they perform endovascular procedures.
“The big concern [about this analysis] is that there may have been some things about the general anesthesia patients that they did not account for. I suspect there is a huge bias, that general anesthesia patients were sicker,” said Dr. Bruce Ovbiagele, professor and chief of neurology at the Medical University of South Carolina in Charleston. “At my institution they have used nongeneral anesthesia, but I have been at other places where they usually use general anesthesia; it is variable,” Dr. Ovbiagele added.
Dr. Berkhemer’s analysis also showed that general anesthesia linked with a delayed start to treatment, but without resulting in a significant difference in time to reperfusion. He noted that “sometimes you cannot do the procedure without general anesthesia,” and in MR CLEAN 6 of the 137 intra-arterial patients who started with nongeneral anesthesia eventually received general anesthesia because of discomfort and pain, Dr. Berkhemer said at the conference, sponsored by the American Heart Association.
He speculated that patients who did not receive general anesthesia did better because they did not undergo acute episodes of reduced blood pressure caused by the hypotensive effect of general anesthesia.
The findings reinforced the approach already used in most of the Dutch centers that participated in MR CLEAN, where nongeneral anesthesia is preferred when possible. “In our center we always use nongeneral anesthesia, we are happy with that and we are not going to change,” said Dr. Diederik W.J. Dippel, lead investigator of MR CLEAN and professor of neurology at Erasmus University Medical Center in Rotterdam, The Netherlands. This prejudice against general anesthesia would make it hard to run a trial in The Netherlands that matched the two anesthesia approaches against each other, Dr. Dippel added.
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: Post hoc analysis of acute ischemic stroke patients treated intra-arterially suggests that avoiding general anesthesia produces better long-term outcomes.
Major finding: After 90 days, 38% of patients treated without general anesthesia and 23% of those who received general anesthesia had good outcomes.
Data source: Analysis of 216 patients in the Dutch MR CLEAN trial who underwent treatment for acute ischemic stroke.
Disclosures: Dr. Berkhemer, Dr. Dippel, and Dr. Ovbiagele had no disclosures.
Giant intracranial aneurysm treatment confers some long-term survival benefit
NASHVILLE, TENN. – The 10-year outcome for most giant intracranial aneurysms is rather dismal even if the lesions are initially successfully treated, according to findings from the International Study of Unruptured Intracranial Aneurysms.
Most patients lived through the first 2 years after diagnosis, but by 10 years, 37% of treated patients had died. Untreated patients had significantly higher mortality at 57%, Dr. James C. Torner said at the International Stroke Conference, which was sponsored by the American Heart Association.
“Compared to small aneurysms, the risk of all-cause mortality for these giant aneurysms is seven times greater in the first year, and the risk of hemorrhage or procedure-related death is 15 times higher. The risk does decrease over time, but it’s still elevated. It’s twice as high for death from hemorrhage and six times more likely from death due to rupture or a procedure by 10 years.”
Dr. Torner of the University of Iowa, Iowa City, presented 10-year outcomes from the International Study of Unruptured Intracranial Aneurysms (ISUIA), which followed 4,059 patients, of whom 187 had a giant unruptured intracranial aneurysm.
The mean lesion size was about 30 mm, but ranged from 25 to 63 mm. A third involved the internal carotid, and another third were cavernous. The remainder were either vestibular, posterior communicating, anterior cerebral, or middle cerebral.
Most were irregular; about 40% were a single sac. Daughter sacs were present in the rest. The volume ranged from 1,100 to 38,000 mm3, with about 10% having a volume of greater than 20,000 mm3.
Most of the patients were women (91%). Age was not related to occurrence; patients ranged from 25 to 82 years. There were some common risk factors, including smoking (in 70%), a family history of aneurysm (in 10%), a family history of coronary artery disease (in up to 45%, depending on patient age), hypertension (in up to 40%), and vascular headache. Patients aged 50 years or older were most likely to present with vascular headache (75%).
The baseline score on the modified Rankin Scale (mRS) was 1 in about 93% of the group. But 80% presented with some symptoms, including cranial nerve deficit (47%; commonly in cranial nerves III and IV), mass effect (16%), headache (44%), orbital pain (21%), and partial vision loss (25%).
Surgery was performed in 39% and endovascular treatment in 27%; the rest of the patients were initially untreated, although 3% later received endovascular treatment and 5% underwent surgical treatment during the follow-up period.
By 10 years, many of the lesions had ruptured. Posterior aneurysms were most likely to rupture (53%), while cavernous aneurysms were least likely to rupture (5%). About a third of the posterior communicating and 36% of the anterior lesions were unruptured.
The risk of rupture increased over the first 5 years, rising from almost 0% in year 1 to 20% by year 5. “Hemorrhage risk is huge over the first 5 years, even with the cavernous aneurysms – even they can rupture,” Dr. Torner said. “In those with smaller aneurysms, the risk of rupture may be high in the first 2 years, but then it subsides somewhat.”
Among the 59% of the overall group who survived, the mRS score remained excellent (1 or 2) by 10 years. Of the remainder who died, 23% died of a cranial or subarachnoid hemorrhage, and 11% of a cerebral infarct. Coronary disease, respiratory disease, and cancer were the other causes.
Treated patients generally fared better than untreated, although mortality varied significantly by lesion location. For anterior lesions, the death rate was 25% in untreated patients , 32% for surgical patients, and 19% in endovascular patients. Death rates for those with posterior communicating lesions were 90% for untreated and 50% for surgically treated patients; all of those with endovascular treatment died. For those with posterior lesions, death rates approached 100% for all groups.
Dr. Torner cautioned that because the study outcomes were collected during the 1990s, most treated patients underwent only coiling or clipping; better outcomes may be seen with more advanced therapies.
He said he had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
NASHVILLE, TENN. – The 10-year outcome for most giant intracranial aneurysms is rather dismal even if the lesions are initially successfully treated, according to findings from the International Study of Unruptured Intracranial Aneurysms.
Most patients lived through the first 2 years after diagnosis, but by 10 years, 37% of treated patients had died. Untreated patients had significantly higher mortality at 57%, Dr. James C. Torner said at the International Stroke Conference, which was sponsored by the American Heart Association.
“Compared to small aneurysms, the risk of all-cause mortality for these giant aneurysms is seven times greater in the first year, and the risk of hemorrhage or procedure-related death is 15 times higher. The risk does decrease over time, but it’s still elevated. It’s twice as high for death from hemorrhage and six times more likely from death due to rupture or a procedure by 10 years.”
Dr. Torner of the University of Iowa, Iowa City, presented 10-year outcomes from the International Study of Unruptured Intracranial Aneurysms (ISUIA), which followed 4,059 patients, of whom 187 had a giant unruptured intracranial aneurysm.
The mean lesion size was about 30 mm, but ranged from 25 to 63 mm. A third involved the internal carotid, and another third were cavernous. The remainder were either vestibular, posterior communicating, anterior cerebral, or middle cerebral.
Most were irregular; about 40% were a single sac. Daughter sacs were present in the rest. The volume ranged from 1,100 to 38,000 mm3, with about 10% having a volume of greater than 20,000 mm3.
Most of the patients were women (91%). Age was not related to occurrence; patients ranged from 25 to 82 years. There were some common risk factors, including smoking (in 70%), a family history of aneurysm (in 10%), a family history of coronary artery disease (in up to 45%, depending on patient age), hypertension (in up to 40%), and vascular headache. Patients aged 50 years or older were most likely to present with vascular headache (75%).
The baseline score on the modified Rankin Scale (mRS) was 1 in about 93% of the group. But 80% presented with some symptoms, including cranial nerve deficit (47%; commonly in cranial nerves III and IV), mass effect (16%), headache (44%), orbital pain (21%), and partial vision loss (25%).
Surgery was performed in 39% and endovascular treatment in 27%; the rest of the patients were initially untreated, although 3% later received endovascular treatment and 5% underwent surgical treatment during the follow-up period.
By 10 years, many of the lesions had ruptured. Posterior aneurysms were most likely to rupture (53%), while cavernous aneurysms were least likely to rupture (5%). About a third of the posterior communicating and 36% of the anterior lesions were unruptured.
The risk of rupture increased over the first 5 years, rising from almost 0% in year 1 to 20% by year 5. “Hemorrhage risk is huge over the first 5 years, even with the cavernous aneurysms – even they can rupture,” Dr. Torner said. “In those with smaller aneurysms, the risk of rupture may be high in the first 2 years, but then it subsides somewhat.”
Among the 59% of the overall group who survived, the mRS score remained excellent (1 or 2) by 10 years. Of the remainder who died, 23% died of a cranial or subarachnoid hemorrhage, and 11% of a cerebral infarct. Coronary disease, respiratory disease, and cancer were the other causes.
Treated patients generally fared better than untreated, although mortality varied significantly by lesion location. For anterior lesions, the death rate was 25% in untreated patients , 32% for surgical patients, and 19% in endovascular patients. Death rates for those with posterior communicating lesions were 90% for untreated and 50% for surgically treated patients; all of those with endovascular treatment died. For those with posterior lesions, death rates approached 100% for all groups.
Dr. Torner cautioned that because the study outcomes were collected during the 1990s, most treated patients underwent only coiling or clipping; better outcomes may be seen with more advanced therapies.
He said he had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
NASHVILLE, TENN. – The 10-year outcome for most giant intracranial aneurysms is rather dismal even if the lesions are initially successfully treated, according to findings from the International Study of Unruptured Intracranial Aneurysms.
Most patients lived through the first 2 years after diagnosis, but by 10 years, 37% of treated patients had died. Untreated patients had significantly higher mortality at 57%, Dr. James C. Torner said at the International Stroke Conference, which was sponsored by the American Heart Association.
“Compared to small aneurysms, the risk of all-cause mortality for these giant aneurysms is seven times greater in the first year, and the risk of hemorrhage or procedure-related death is 15 times higher. The risk does decrease over time, but it’s still elevated. It’s twice as high for death from hemorrhage and six times more likely from death due to rupture or a procedure by 10 years.”
Dr. Torner of the University of Iowa, Iowa City, presented 10-year outcomes from the International Study of Unruptured Intracranial Aneurysms (ISUIA), which followed 4,059 patients, of whom 187 had a giant unruptured intracranial aneurysm.
The mean lesion size was about 30 mm, but ranged from 25 to 63 mm. A third involved the internal carotid, and another third were cavernous. The remainder were either vestibular, posterior communicating, anterior cerebral, or middle cerebral.
Most were irregular; about 40% were a single sac. Daughter sacs were present in the rest. The volume ranged from 1,100 to 38,000 mm3, with about 10% having a volume of greater than 20,000 mm3.
Most of the patients were women (91%). Age was not related to occurrence; patients ranged from 25 to 82 years. There were some common risk factors, including smoking (in 70%), a family history of aneurysm (in 10%), a family history of coronary artery disease (in up to 45%, depending on patient age), hypertension (in up to 40%), and vascular headache. Patients aged 50 years or older were most likely to present with vascular headache (75%).
The baseline score on the modified Rankin Scale (mRS) was 1 in about 93% of the group. But 80% presented with some symptoms, including cranial nerve deficit (47%; commonly in cranial nerves III and IV), mass effect (16%), headache (44%), orbital pain (21%), and partial vision loss (25%).
Surgery was performed in 39% and endovascular treatment in 27%; the rest of the patients were initially untreated, although 3% later received endovascular treatment and 5% underwent surgical treatment during the follow-up period.
By 10 years, many of the lesions had ruptured. Posterior aneurysms were most likely to rupture (53%), while cavernous aneurysms were least likely to rupture (5%). About a third of the posterior communicating and 36% of the anterior lesions were unruptured.
The risk of rupture increased over the first 5 years, rising from almost 0% in year 1 to 20% by year 5. “Hemorrhage risk is huge over the first 5 years, even with the cavernous aneurysms – even they can rupture,” Dr. Torner said. “In those with smaller aneurysms, the risk of rupture may be high in the first 2 years, but then it subsides somewhat.”
Among the 59% of the overall group who survived, the mRS score remained excellent (1 or 2) by 10 years. Of the remainder who died, 23% died of a cranial or subarachnoid hemorrhage, and 11% of a cerebral infarct. Coronary disease, respiratory disease, and cancer were the other causes.
Treated patients generally fared better than untreated, although mortality varied significantly by lesion location. For anterior lesions, the death rate was 25% in untreated patients , 32% for surgical patients, and 19% in endovascular patients. Death rates for those with posterior communicating lesions were 90% for untreated and 50% for surgically treated patients; all of those with endovascular treatment died. For those with posterior lesions, death rates approached 100% for all groups.
Dr. Torner cautioned that because the study outcomes were collected during the 1990s, most treated patients underwent only coiling or clipping; better outcomes may be seen with more advanced therapies.
He said he had no relevant financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: Giant intracranial aneurysms have a generally poor 10-year outcome, although treated patients fare better than untreated.
Major finding: By 10 years, the death rate was 37% among the treated patients and 57% among the untreated.
Data source: The retrospective analysis comprised 187 patients with aneurysms greater than 25 mm.
Disclosures: Dr. Torner said he had no relevant financial disclosures.
VIDEO: Many stroke patients may miss out on clot-retrieval options
NASHVILLE, TENN. – A 1 million–patient analysis of the Get With the Guidelines database found striking improvements in outcomes after ischemic stroke.
Despite the proven benefits of new-generation clot-retrieval devices, however, only about 2% of such stroke patients undergo endovascular therapy.
In a video interview at the International Stroke Conference, Dr. Bijoy Menon of the department of clinical neurosciences at the University of Calgary (Alta.), who presented the findings at the conference, discussed this apparent clinical paradox.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Menon’s study echoes findings of the landmark Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke (ESCAPE) trial, which found dramatically improved stroke outcomes after endovascular therapy.
But the benefits of such treatment should never outweigh the need for thoroughly screening patients and carefully considering their recovery prospects, Dr. Michael Hill, professor of neurology at the University of Calgary and primary investigator on the ESCAPE study, cautioned in another video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
NASHVILLE, TENN. – A 1 million–patient analysis of the Get With the Guidelines database found striking improvements in outcomes after ischemic stroke.
Despite the proven benefits of new-generation clot-retrieval devices, however, only about 2% of such stroke patients undergo endovascular therapy.
In a video interview at the International Stroke Conference, Dr. Bijoy Menon of the department of clinical neurosciences at the University of Calgary (Alta.), who presented the findings at the conference, discussed this apparent clinical paradox.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Menon’s study echoes findings of the landmark Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke (ESCAPE) trial, which found dramatically improved stroke outcomes after endovascular therapy.
But the benefits of such treatment should never outweigh the need for thoroughly screening patients and carefully considering their recovery prospects, Dr. Michael Hill, professor of neurology at the University of Calgary and primary investigator on the ESCAPE study, cautioned in another video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
NASHVILLE, TENN. – A 1 million–patient analysis of the Get With the Guidelines database found striking improvements in outcomes after ischemic stroke.
Despite the proven benefits of new-generation clot-retrieval devices, however, only about 2% of such stroke patients undergo endovascular therapy.
In a video interview at the International Stroke Conference, Dr. Bijoy Menon of the department of clinical neurosciences at the University of Calgary (Alta.), who presented the findings at the conference, discussed this apparent clinical paradox.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Menon’s study echoes findings of the landmark Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke (ESCAPE) trial, which found dramatically improved stroke outcomes after endovascular therapy.
But the benefits of such treatment should never outweigh the need for thoroughly screening patients and carefully considering their recovery prospects, Dr. Michael Hill, professor of neurology at the University of Calgary and primary investigator on the ESCAPE study, cautioned in another video interview at the meeting.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Regionalized trauma care trims 30-day mortality
LAKE BUENA VISTA, FLA. – Regionalized trauma care significantly reduces long-term mortality and maintains similar functional outcomes in patients with severe traumatic brain injury, a study showed.
Regionalization of trauma care is a health care strategy that attempts to improve outcomes for trauma patients by setting up a tiered, integrated system that aims to match the injured patient with the appropriate health care facility in a timely fashion. The Northern Ohio Trauma System (NOTS) was created in 2010 to manage trauma patients using the regionalization model.
In this study of outcomes in NOTS patients, longer-term follow-up of 3,496 severe traumatic brain injury (TBI) admissions showed 30-day mortality fell from 21% to 16% after regionalization (24% relative reduction; P value < .0001) and 6-month mortality declined from 24% to 20% (17% relative reduction; P = .004).
Multivariable logistic regression only strengthened the effect of regionalization on the primary outcome, lead study author Dr. Michael Kelly said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
The odds ratio for 30-day mortality was 0.74, representing a 26% relative mortality reduction, and 0.82 for 6-month mortality, representing an 18% relative reduction.
At last year’s EAST meeting, Dr. Kelly and his colleagues reported that hospital mortality declined from 19% (262/1,359 patients) to 14% (302/2,137) in patients with severe TBI after the creation of the NOTS in 2010.
Despite bucking the current trend of rising mortality in hospitalized TBI patients, particularly those with severe brain injuries, their previous results were criticized by some as incomplete because hospital mortality was used without functional status measures or long-term mortality, he said.
To bridge the knowledge gap, the investigators identified all TBI patients older than 14 years with a Head Abbreviated Injury Scale (AIS) ≥ 3 from 2008 to 2012 in the NOTS database and matched them to the Ohio death index and the regional TBI rehabilitation database. Overall Functional Independence Measure (FIM) scores and FIM score gains were compared in 414 patients who were discharged to the regional TBI rehabilitation unit.
As a general rule of thumb, an overall FIM score of 60 is equivalent to 4 hours of personal care assistance in a nursing facility–type setting, a score of 80 equals 2 hours of personalized care in a nursing facility, more than 80 means the patient is able to receive family care at home, and ≥ 100 means minimal burdens in personal care, said Dr. Kelly of the MetroHealth Medical Center, Cleveland, and Cleveland Clinic.
A gain of 22 points is considered a minimal clinically important difference (MCID) for the overall FIM score. The MCID is 17 points for a FIM motor subscale gain, 3 for a FIM cognitive subscale gain, and has not been established for the FIM social subscale.
Overall FIM scores were similar before and after regionalization of trauma care (RT) at admission (54 vs. 48; P = .2) and at discharge (92 vs. 89; P = .1), he said.
FIM scores were similar in both groups at admission and discharge on the cognitive and social subscale domains, but were significantly lower post RT on the motor subscale at admission (38 vs. 31; P = .02) and discharge (68 vs. 65; P = .03). These differences were not clinically significant, according to Dr. Kelly and senior study author Dr. Jeffrey Claridge, NOTS medical director.
Pre- and post-RT patients had similar overall FIM score gains (37 vs. 36; P = .6), motor subscale gains (both groups 29), and social subscale gains (both groups 1). FIM cognitive subscale gains were significantly lower post RT (6 vs. 5; P = .01), but this difference was also not clinically significant.
Notably, discharges to regional TBI rehabilitation increased from 9% before RT to 14% after RT, Dr. Kelly said. The percentage of patients who were discharged to a skilled nurse facility or long-term care facility remained stable at about 30%, as did the percentage discharged home at about 40%.
“Regionalization improves long-term survival and maintains similar functional outcomes for patients with severe traumatic brain injury,” he concluded.
Discussant Dr. Jeffrey Coughenour of the University of Missouri Health System in Columbia said it appears regionalization is working, but added, “While we are saving more lives, what kind of lives are we saving? A question that has ever increasing implications for patients and payers evaluating the care we provide.”
He praised the investigators for using the FIM scale rather than the Glasgow Outcome Scale to try and answer this question, but said more information is needed on whether FIM scores improved in more challenging patients such as those with an AIS score of 4 or 5 or those entering rehabilitation after discharge to a skilled nursing or long-term care facility.
Data were not broken down for these more challenging subsets, Dr. Kelly said. The question of quality of life post regionalization was asked after the first study and that functional status was shown to be maintained in TBI patients in the follow-up study.
“Since no major changes in the hospital-based care or rehabilitation care of these TBI patients occurred, we weren’t surprised to see that functional outcomes did not improve,” he said in an interview. “The regionalization protocols were designed primarily to improve survival.”
During a discussion of the results, audience members questioned whether the investigators could be certain the results could be attributed to regionalization and not improvements in treatment of concurrent injuries or improvements in TBI treatment already underway at the time of policy change.
For the most part, these patients had isolated TBIs and no major changes in personnel or TBI care occurred during the study period, Dr. Kelly said.
Under NOTS, region-wide initiatives included use of the Centers for Disease Control and Prevention guidelines for field triage, a transfer line and transfer protocols, and a research database shared between two large hospital systems comprising the level I MetroHealth Medical Center trauma center, two level II trauma centers, and 12 nontrauma hospitals.
Dr. Kelly, his coauthors, and Dr. Coughenour reported no financial disclosures.
LAKE BUENA VISTA, FLA. – Regionalized trauma care significantly reduces long-term mortality and maintains similar functional outcomes in patients with severe traumatic brain injury, a study showed.
Regionalization of trauma care is a health care strategy that attempts to improve outcomes for trauma patients by setting up a tiered, integrated system that aims to match the injured patient with the appropriate health care facility in a timely fashion. The Northern Ohio Trauma System (NOTS) was created in 2010 to manage trauma patients using the regionalization model.
In this study of outcomes in NOTS patients, longer-term follow-up of 3,496 severe traumatic brain injury (TBI) admissions showed 30-day mortality fell from 21% to 16% after regionalization (24% relative reduction; P value < .0001) and 6-month mortality declined from 24% to 20% (17% relative reduction; P = .004).
Multivariable logistic regression only strengthened the effect of regionalization on the primary outcome, lead study author Dr. Michael Kelly said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
The odds ratio for 30-day mortality was 0.74, representing a 26% relative mortality reduction, and 0.82 for 6-month mortality, representing an 18% relative reduction.
At last year’s EAST meeting, Dr. Kelly and his colleagues reported that hospital mortality declined from 19% (262/1,359 patients) to 14% (302/2,137) in patients with severe TBI after the creation of the NOTS in 2010.
Despite bucking the current trend of rising mortality in hospitalized TBI patients, particularly those with severe brain injuries, their previous results were criticized by some as incomplete because hospital mortality was used without functional status measures or long-term mortality, he said.
To bridge the knowledge gap, the investigators identified all TBI patients older than 14 years with a Head Abbreviated Injury Scale (AIS) ≥ 3 from 2008 to 2012 in the NOTS database and matched them to the Ohio death index and the regional TBI rehabilitation database. Overall Functional Independence Measure (FIM) scores and FIM score gains were compared in 414 patients who were discharged to the regional TBI rehabilitation unit.
As a general rule of thumb, an overall FIM score of 60 is equivalent to 4 hours of personal care assistance in a nursing facility–type setting, a score of 80 equals 2 hours of personalized care in a nursing facility, more than 80 means the patient is able to receive family care at home, and ≥ 100 means minimal burdens in personal care, said Dr. Kelly of the MetroHealth Medical Center, Cleveland, and Cleveland Clinic.
A gain of 22 points is considered a minimal clinically important difference (MCID) for the overall FIM score. The MCID is 17 points for a FIM motor subscale gain, 3 for a FIM cognitive subscale gain, and has not been established for the FIM social subscale.
Overall FIM scores were similar before and after regionalization of trauma care (RT) at admission (54 vs. 48; P = .2) and at discharge (92 vs. 89; P = .1), he said.
FIM scores were similar in both groups at admission and discharge on the cognitive and social subscale domains, but were significantly lower post RT on the motor subscale at admission (38 vs. 31; P = .02) and discharge (68 vs. 65; P = .03). These differences were not clinically significant, according to Dr. Kelly and senior study author Dr. Jeffrey Claridge, NOTS medical director.
Pre- and post-RT patients had similar overall FIM score gains (37 vs. 36; P = .6), motor subscale gains (both groups 29), and social subscale gains (both groups 1). FIM cognitive subscale gains were significantly lower post RT (6 vs. 5; P = .01), but this difference was also not clinically significant.
Notably, discharges to regional TBI rehabilitation increased from 9% before RT to 14% after RT, Dr. Kelly said. The percentage of patients who were discharged to a skilled nurse facility or long-term care facility remained stable at about 30%, as did the percentage discharged home at about 40%.
“Regionalization improves long-term survival and maintains similar functional outcomes for patients with severe traumatic brain injury,” he concluded.
Discussant Dr. Jeffrey Coughenour of the University of Missouri Health System in Columbia said it appears regionalization is working, but added, “While we are saving more lives, what kind of lives are we saving? A question that has ever increasing implications for patients and payers evaluating the care we provide.”
He praised the investigators for using the FIM scale rather than the Glasgow Outcome Scale to try and answer this question, but said more information is needed on whether FIM scores improved in more challenging patients such as those with an AIS score of 4 or 5 or those entering rehabilitation after discharge to a skilled nursing or long-term care facility.
Data were not broken down for these more challenging subsets, Dr. Kelly said. The question of quality of life post regionalization was asked after the first study and that functional status was shown to be maintained in TBI patients in the follow-up study.
“Since no major changes in the hospital-based care or rehabilitation care of these TBI patients occurred, we weren’t surprised to see that functional outcomes did not improve,” he said in an interview. “The regionalization protocols were designed primarily to improve survival.”
During a discussion of the results, audience members questioned whether the investigators could be certain the results could be attributed to regionalization and not improvements in treatment of concurrent injuries or improvements in TBI treatment already underway at the time of policy change.
For the most part, these patients had isolated TBIs and no major changes in personnel or TBI care occurred during the study period, Dr. Kelly said.
Under NOTS, region-wide initiatives included use of the Centers for Disease Control and Prevention guidelines for field triage, a transfer line and transfer protocols, and a research database shared between two large hospital systems comprising the level I MetroHealth Medical Center trauma center, two level II trauma centers, and 12 nontrauma hospitals.
Dr. Kelly, his coauthors, and Dr. Coughenour reported no financial disclosures.
LAKE BUENA VISTA, FLA. – Regionalized trauma care significantly reduces long-term mortality and maintains similar functional outcomes in patients with severe traumatic brain injury, a study showed.
Regionalization of trauma care is a health care strategy that attempts to improve outcomes for trauma patients by setting up a tiered, integrated system that aims to match the injured patient with the appropriate health care facility in a timely fashion. The Northern Ohio Trauma System (NOTS) was created in 2010 to manage trauma patients using the regionalization model.
In this study of outcomes in NOTS patients, longer-term follow-up of 3,496 severe traumatic brain injury (TBI) admissions showed 30-day mortality fell from 21% to 16% after regionalization (24% relative reduction; P value < .0001) and 6-month mortality declined from 24% to 20% (17% relative reduction; P = .004).
Multivariable logistic regression only strengthened the effect of regionalization on the primary outcome, lead study author Dr. Michael Kelly said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
The odds ratio for 30-day mortality was 0.74, representing a 26% relative mortality reduction, and 0.82 for 6-month mortality, representing an 18% relative reduction.
At last year’s EAST meeting, Dr. Kelly and his colleagues reported that hospital mortality declined from 19% (262/1,359 patients) to 14% (302/2,137) in patients with severe TBI after the creation of the NOTS in 2010.
Despite bucking the current trend of rising mortality in hospitalized TBI patients, particularly those with severe brain injuries, their previous results were criticized by some as incomplete because hospital mortality was used without functional status measures or long-term mortality, he said.
To bridge the knowledge gap, the investigators identified all TBI patients older than 14 years with a Head Abbreviated Injury Scale (AIS) ≥ 3 from 2008 to 2012 in the NOTS database and matched them to the Ohio death index and the regional TBI rehabilitation database. Overall Functional Independence Measure (FIM) scores and FIM score gains were compared in 414 patients who were discharged to the regional TBI rehabilitation unit.
As a general rule of thumb, an overall FIM score of 60 is equivalent to 4 hours of personal care assistance in a nursing facility–type setting, a score of 80 equals 2 hours of personalized care in a nursing facility, more than 80 means the patient is able to receive family care at home, and ≥ 100 means minimal burdens in personal care, said Dr. Kelly of the MetroHealth Medical Center, Cleveland, and Cleveland Clinic.
A gain of 22 points is considered a minimal clinically important difference (MCID) for the overall FIM score. The MCID is 17 points for a FIM motor subscale gain, 3 for a FIM cognitive subscale gain, and has not been established for the FIM social subscale.
Overall FIM scores were similar before and after regionalization of trauma care (RT) at admission (54 vs. 48; P = .2) and at discharge (92 vs. 89; P = .1), he said.
FIM scores were similar in both groups at admission and discharge on the cognitive and social subscale domains, but were significantly lower post RT on the motor subscale at admission (38 vs. 31; P = .02) and discharge (68 vs. 65; P = .03). These differences were not clinically significant, according to Dr. Kelly and senior study author Dr. Jeffrey Claridge, NOTS medical director.
Pre- and post-RT patients had similar overall FIM score gains (37 vs. 36; P = .6), motor subscale gains (both groups 29), and social subscale gains (both groups 1). FIM cognitive subscale gains were significantly lower post RT (6 vs. 5; P = .01), but this difference was also not clinically significant.
Notably, discharges to regional TBI rehabilitation increased from 9% before RT to 14% after RT, Dr. Kelly said. The percentage of patients who were discharged to a skilled nurse facility or long-term care facility remained stable at about 30%, as did the percentage discharged home at about 40%.
“Regionalization improves long-term survival and maintains similar functional outcomes for patients with severe traumatic brain injury,” he concluded.
Discussant Dr. Jeffrey Coughenour of the University of Missouri Health System in Columbia said it appears regionalization is working, but added, “While we are saving more lives, what kind of lives are we saving? A question that has ever increasing implications for patients and payers evaluating the care we provide.”
He praised the investigators for using the FIM scale rather than the Glasgow Outcome Scale to try and answer this question, but said more information is needed on whether FIM scores improved in more challenging patients such as those with an AIS score of 4 or 5 or those entering rehabilitation after discharge to a skilled nursing or long-term care facility.
Data were not broken down for these more challenging subsets, Dr. Kelly said. The question of quality of life post regionalization was asked after the first study and that functional status was shown to be maintained in TBI patients in the follow-up study.
“Since no major changes in the hospital-based care or rehabilitation care of these TBI patients occurred, we weren’t surprised to see that functional outcomes did not improve,” he said in an interview. “The regionalization protocols were designed primarily to improve survival.”
During a discussion of the results, audience members questioned whether the investigators could be certain the results could be attributed to regionalization and not improvements in treatment of concurrent injuries or improvements in TBI treatment already underway at the time of policy change.
For the most part, these patients had isolated TBIs and no major changes in personnel or TBI care occurred during the study period, Dr. Kelly said.
Under NOTS, region-wide initiatives included use of the Centers for Disease Control and Prevention guidelines for field triage, a transfer line and transfer protocols, and a research database shared between two large hospital systems comprising the level I MetroHealth Medical Center trauma center, two level II trauma centers, and 12 nontrauma hospitals.
Dr. Kelly, his coauthors, and Dr. Coughenour reported no financial disclosures.
AT THE EAST SCIENTIFIC ASSEMBLY
Key clinical point: Regionalized trauma care reduces long-term mortality and maintains functional outcomes in patients with severe TBI.
Major finding: RT reduced 30-day mortality from 21% to 16% (P < .0001) and 6-month mortality from 24% to 20% (P = .004).
Data source: Analysis of 3,496 patients with severe TBI.
Disclosures: Dr. Kelly, his coauthors, and Dr. Coughenour reported no financial disclosures.