User login
Two-stage preeclampsia screening cuts cost, preserves effectiveness
Using maternal characteristics to identify high-risk pregnant women for second-stage preeclampsia screening achieved similar detection rates as screening all pregnant women, based on data from a prospective study of 61,174 singleton pregnancies.
About 90% of preeclampsia cases can be predicted using the “triple test” of mean arterial pressure (MAP), uterine artery pulsatility index (UtA-PI) and serum placental growth factor (PlGF) plus a combination of maternal factors at 11 to 13 weeks’ gestation, wrote Alan Wright, PhD, of the University of Exeter, United Kingdom, and colleagues. The need for detection of preeclampsia is important, as high-risk pregnant women who take aspirin before 16 weeks’ gestation can reduce early preeclampsia by 90% and preterm preeclampsia by 60%, they said.
However, “measurements of serum PlGF and UtA-PI are not part of routine care and would be associated with an additional cost,” Dr. Wright and his colleagues noted in the American Journal of Obstetrics & Gynecology.
In the study, the researchers used a competing risks model to combine MAP, UtA-PI, and PlGF and maternal factors to compare detection rates if the triple test were used for a subset of high-risk women. Most of the women in the study were white.
Overall, Dr. Wright and his colleagues found, if first-stage screening method is maternal factors, then measurements of MAP, UtA-PI, and PlGF can be reserved for 70% of the pregnant population.
When the researchers compared various components of the triple test, they found that, if the first stage of screening included maternal factors along with MAP and UtA-PI, measurement of PlGF could be saved for 30%-40% of pregnant women. Similarly, if first-stage screening included maternal factors, MAP, and PlGF, measurement of UtA-PI can be saved for 20%-30% of the population, they said.
The study findings were limited by several factors, including the homogeneity of the population studied, the researchers noted. “The risk for development of [preeclampsia] is higher in women of black or South Asian racial origin than in white women,” Dr. Wright and his colleagues wrote. “Consequently, in screening in a population of mixed racial origins, for a given risk cut-off, the [detection rate] and [screen positive rate] would be higher in black and South Asian than white women and the overall performance would be dependent on the proportion of the various racial groups within that population.”
However, the results support the effectiveness of using only certain tests paired with maternal factors to identify high-risk patients for further screening.
“Inevitably, ,” the researchers said.
Dr. Wright and his colleagues reported no conflicts of interest. The study was supported in part by the Fetal Medicine Foundation, and the reagents and equipment used for the measurement of serum placental growth factor were provided by PerkinElmer Life and Analytical Sciences.
SOURCE: Wright A et al. Am J Obstet Gynecol. 2018. doi: 10.1016/j.ajog.2018.10.092.
Using maternal characteristics to identify high-risk pregnant women for second-stage preeclampsia screening achieved similar detection rates as screening all pregnant women, based on data from a prospective study of 61,174 singleton pregnancies.
About 90% of preeclampsia cases can be predicted using the “triple test” of mean arterial pressure (MAP), uterine artery pulsatility index (UtA-PI) and serum placental growth factor (PlGF) plus a combination of maternal factors at 11 to 13 weeks’ gestation, wrote Alan Wright, PhD, of the University of Exeter, United Kingdom, and colleagues. The need for detection of preeclampsia is important, as high-risk pregnant women who take aspirin before 16 weeks’ gestation can reduce early preeclampsia by 90% and preterm preeclampsia by 60%, they said.
However, “measurements of serum PlGF and UtA-PI are not part of routine care and would be associated with an additional cost,” Dr. Wright and his colleagues noted in the American Journal of Obstetrics & Gynecology.
In the study, the researchers used a competing risks model to combine MAP, UtA-PI, and PlGF and maternal factors to compare detection rates if the triple test were used for a subset of high-risk women. Most of the women in the study were white.
Overall, Dr. Wright and his colleagues found, if first-stage screening method is maternal factors, then measurements of MAP, UtA-PI, and PlGF can be reserved for 70% of the pregnant population.
When the researchers compared various components of the triple test, they found that, if the first stage of screening included maternal factors along with MAP and UtA-PI, measurement of PlGF could be saved for 30%-40% of pregnant women. Similarly, if first-stage screening included maternal factors, MAP, and PlGF, measurement of UtA-PI can be saved for 20%-30% of the population, they said.
The study findings were limited by several factors, including the homogeneity of the population studied, the researchers noted. “The risk for development of [preeclampsia] is higher in women of black or South Asian racial origin than in white women,” Dr. Wright and his colleagues wrote. “Consequently, in screening in a population of mixed racial origins, for a given risk cut-off, the [detection rate] and [screen positive rate] would be higher in black and South Asian than white women and the overall performance would be dependent on the proportion of the various racial groups within that population.”
However, the results support the effectiveness of using only certain tests paired with maternal factors to identify high-risk patients for further screening.
“Inevitably, ,” the researchers said.
Dr. Wright and his colleagues reported no conflicts of interest. The study was supported in part by the Fetal Medicine Foundation, and the reagents and equipment used for the measurement of serum placental growth factor were provided by PerkinElmer Life and Analytical Sciences.
SOURCE: Wright A et al. Am J Obstet Gynecol. 2018. doi: 10.1016/j.ajog.2018.10.092.
Using maternal characteristics to identify high-risk pregnant women for second-stage preeclampsia screening achieved similar detection rates as screening all pregnant women, based on data from a prospective study of 61,174 singleton pregnancies.
About 90% of preeclampsia cases can be predicted using the “triple test” of mean arterial pressure (MAP), uterine artery pulsatility index (UtA-PI) and serum placental growth factor (PlGF) plus a combination of maternal factors at 11 to 13 weeks’ gestation, wrote Alan Wright, PhD, of the University of Exeter, United Kingdom, and colleagues. The need for detection of preeclampsia is important, as high-risk pregnant women who take aspirin before 16 weeks’ gestation can reduce early preeclampsia by 90% and preterm preeclampsia by 60%, they said.
However, “measurements of serum PlGF and UtA-PI are not part of routine care and would be associated with an additional cost,” Dr. Wright and his colleagues noted in the American Journal of Obstetrics & Gynecology.
In the study, the researchers used a competing risks model to combine MAP, UtA-PI, and PlGF and maternal factors to compare detection rates if the triple test were used for a subset of high-risk women. Most of the women in the study were white.
Overall, Dr. Wright and his colleagues found, if first-stage screening method is maternal factors, then measurements of MAP, UtA-PI, and PlGF can be reserved for 70% of the pregnant population.
When the researchers compared various components of the triple test, they found that, if the first stage of screening included maternal factors along with MAP and UtA-PI, measurement of PlGF could be saved for 30%-40% of pregnant women. Similarly, if first-stage screening included maternal factors, MAP, and PlGF, measurement of UtA-PI can be saved for 20%-30% of the population, they said.
The study findings were limited by several factors, including the homogeneity of the population studied, the researchers noted. “The risk for development of [preeclampsia] is higher in women of black or South Asian racial origin than in white women,” Dr. Wright and his colleagues wrote. “Consequently, in screening in a population of mixed racial origins, for a given risk cut-off, the [detection rate] and [screen positive rate] would be higher in black and South Asian than white women and the overall performance would be dependent on the proportion of the various racial groups within that population.”
However, the results support the effectiveness of using only certain tests paired with maternal factors to identify high-risk patients for further screening.
“Inevitably, ,” the researchers said.
Dr. Wright and his colleagues reported no conflicts of interest. The study was supported in part by the Fetal Medicine Foundation, and the reagents and equipment used for the measurement of serum placental growth factor were provided by PerkinElmer Life and Analytical Sciences.
SOURCE: Wright A et al. Am J Obstet Gynecol. 2018. doi: 10.1016/j.ajog.2018.10.092.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Key clinical point: Reserving two-stage testing for preeclampsia to high-risk subgroups can cut costs without cutting effectiveness.
Major finding: The more costly measurements of MAP, UtA-PI, and PlGF can be reserved for 70% of pregnant women with similar preeclampsia detection rates as testing the entire population.
Study details: The data come from a prospective study of 61,174 singleton pregnancies.
Disclosures: The researchers reported no conflicts of interest. The study was supported in part by the Fetal Medicine Foundation; the reagents and equipment used for the measurement of serum placental growth factor were provided by PerkinElmer Life and Analytical Sciences.
Source: Wright A et al. Am J Obstet Gynecol. 2018. doi: 10.1016/j.ajog.2018.10.092.
CKD, and even dialysis, may not be barriers to pregnancy
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
SAN DIEGO – Nephrologists are often uncomfortable with the idea of advising women with chronic kidney disease (CKD) about pregnancy, a physician told colleagues. They must do better, she said, with sensitivity and insight into once-extreme possibilities like pregnancy during dialysis.
“For many women, having a child is a life goal, and our women with chronic kidney disease are not different,” said Michelle Hladunewich, MD, of Toronto’s Sunnybrook Health Sciences Center. “When we don’t know what we should do, we tend to over-aggressively counsel our women, and that can traumatize them. It’s our role as nephrologists to help them find the safest window to have their pregnancy,” she said at the meeting sponsored by the American Society of Nephrology.
According to Dr. Hladunewich, there are tens of thousands of women of child-bearing age in the United States who have CKD, end-stage renal disease (ESRD), and kidney transplants. However, she said, research presented at Kidney Week 2018 suggested that many nephrologists do not feel confident about counseling patients regarding issues such as pregnancy outcomes in CKD. “We are not that comfortable with it, but we have to become more comfortable,” she said. “We need to be prepared to talk about contraception if they don’t want to have a child or the plan about how to have a child if they do.”
It’s especially important to understand that while women can fear birth defects and the exacerbation of their disease, they may also feel “they’re not fulfilling a societal norm to have a child like everyone else,” she said.
The risks of pregnancy in CKD can affect the mother (via worse kidney function) and/or the fetus (preeclampsia, poor fetal growth, preterm delivery).
In a 2015 study, Italian researchers compared 504 pregnancies in women with CKD to 836 low-risk pregnancies in women without CKD. They found that the risks of adverse outcomes increased in women at higher stages of CKD, compared with those at lower stages: “Renal function matters, and a stepwise increase in the risk of adverse maternal-fetal outcomes is observed from stage 1 to stages 4-5.”
In addition, the researchers noted that their research suggests “the presence of a baseline risk linked to CKD per se” (J Am Soc Nephrol. 2015 Aug; 26[8]:2011-22).
Dr. Hladunewich recommended focusing on “the safest window of opportunity.” Some patients will progress to end-stage renal disease, and an earlier pregnancy during CKD is a better option, she said. As a result, encouraging an earlier pregnancy can be a wise idea.
In some cases, though, a patient may be far into the stages of CKD. Dr. Hladunewich spoke about the case of a 31-year-old patient with a 29-year history of type 1 diabetes mellitus. She’d had one miscarriage, one preterm birth, and one twin pregnancy that was terminated because of safety concerns including rapid loss of kidney function.
The patient saw Dr. Hladunewich when she had a glomerular filtration rate of 25 mL/min, 3.5 g per 24 hour of proteinuria, and hypertension. The patient had a question: “Dr. Michelle, when can I try again?”
Dr. Hladunewich joked that “I had a small stroke.” But then, she said, “I got to the business of pregnancy counseling.”
She told the woman that her progression to end-stage renal disease was likely inevitable, and “adverse pregnancy outcomes were almost guaranteed.”
The woman responded: “Not now? When?” That, Dr. Hladunewich said, “was when I had my second stroke.”
But there is a possible solution: Pregnancy during dialysis. “Historically, we’ve said absolutely no pregnancy on dialysis,” she said, “but times are changing. We believe aggressive dialysis improves fetal maternal and fetal outcomes.”
Indeed, Dr. Hladunewich led a 2014 study that linked extensive dialysis during pregnancy (compared with less dialysis) to a better likelihood of outcomes such as live birth rate and normal birth weight (JASN May 2014;25[5]:1103-9).
As she noted, “we do offer it as a reproductive option” to patients like the one she mentioned – those who are in ESRD, approaching it, or are nearing the end of their child-bearing years with no transplant in sight. In transplant cases, she said, adequate graft function is linked to good pregnancy outcomes.
Dr. Hladunewich added that it’s important to monitor and adjust treatment of patients during the postpartum period. She said it’s especially important to understand the risks of drugs during breastfeeding. Both dialysis and transplant patients can breastfeed, she said.
Dr. Hladunewich reports no disclosures.
SOURCE: Kidney Week 2018, Abstract FR-OR078.
REPORTING FROM KIDNEY WEEK 2018
Despite declines in prenatal use of alcohol and cigarettes, cannabis use is on the rise
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
Despite general decreases in cigarette and alcohol use among pregnant women during 2002-2016, cannabis use in pregnancy persisted and has actually increased slightly over the past 14 years, reported Arpana Agrawal, PhD, and her associates, of the Washington University, St. Louis.
Dr. Agrawal and her associates analyzed data from the National Survey of Drug Use and Health from 2002-2016 to quantify changes in alcohol, cigarette, and cannabis use among pregnant women aged 18-44 years. Survey-adjusted prevalence estimates of alcohol, cigarette, and cannabis use in 2002 were 10%, 18%, and 3%, respectively, versus corresponding rates in 2016 of 8%, 10%, and 5%, according to their research letter in JAMA Pediatrics.
A sampling of 12,058 women aged 18-25 years (n = 8,170) or 26-44 years (n = 3,888) was taken from a population of more than 436,056 women included in the National Survey database. Fully 3,554 of the women included in the final study group were in their first trimester of pregnancy.
The findings in Dr. Agrawal’s study were similar to another study conducted by Brown et al., although the exact prevalence for cannabis use differed slightly.
In addition to observing a reduction in the use of alcohol and cigarettes, the authors also noted a significant decline in the combined use of alcohol and cigarettes together. For alcohol use specifically, the greatest decrease was seen among women aged 18-25 years. For cigarette smoking in pregnancy, the most significant decreases were seen in white women, those aged 18-25 years, and those who had achieved completion of high school or more advanced studies.
Overall, the effects were modest when sample sizes were stratified by trimester: decreases in cigarette smoking were observed in the first trimester, and more significantly, later in pregnancy. For alcohol, nominal reductions were observed in the second and third trimesters. Cannabis use, on the other hand, increased in the first trimester, but showed no significant increases during the second and third trimesters.
“Greater public awareness regarding the consequences of prenatal cannabis exposure in offspring health is necessary,” Dr. Agrawal and her colleagues wrote.
The authors had no relevant disclosures to report. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
SOURCE: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: Greatest increase in use of cannabis over the 14 years of the study was seen during the first trimester; the increase in use of cannabis in the second and third trimesters was not significant.
Study details: A study of 12,058 pregnant women from 2002-2016.
Disclosures: The authors had no relevant financial disclosures. Funding was provided by grants from the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the National Institute on Alcohol Abuse and Alcoholism.
Source: Agrawal A et al. JAMA Pediatr. 2018 Nov 5. doi: 10.1001/jamapediatrics.2018.3096.
USPSTF advises primary care to screen for unhealthy alcohol use
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
The USPSTF recommendations to screen adults for unhealthy alcohol use acknowledge the serious public health problem it presents, wrote E. Jennifer Edelman, MD, and Jeanette M. Tetrault, MD, in an accompanying editorial.
The recommendations are similar to those issued in 2013 that endorsed screening and brief behavioral interventions for patients with at-risk alcohol use, they said. “Notably, the 2018 recommendations replace alcohol misuse with unhealthy alcohol use and explicitly recommend screening in all pregnant women,” they said.
In clinical practice, most patients with alcohol problems are seen for issues that are consequences of unhealthy alcohol use, such as poorly controlled hypertension, rather than the alcohol use itself, they noted. “Although patients are treated for their immediate problem, they often leave without clear plans to cut back or abstain from alcohol use and thus improve their health.”
Although the recommendations are based on studies showing the effectiveness of brief intervention in primary care, the interventions’ components tend not to be standardized in terms of content, delivery, dose, or duration, the editorialists noted. The terminology used in studies and in clinical practice is inconsistent as well and can cause confusion for doctors and stigma for patients, Dr. Edelman and Dr. Tetrault said.
In addition, they noted that the new USPSTF recommendations don’t incorporate guidance against any alcohol use while taking medications that may interact with it, such as sedating drugs and medications for opioid use disorders.
“Nonetheless, primary care physicians should focus on prevention of alcohol-related harms across the spectrum of alcohol use, including prescribing medications for alcohol use disorder when appropriate,” they noted. “Medications such as naltrexone, acamprosate, and disulfiram can easily be prescribed in primary care and do not require specific training” (JAMA. 2018 Nov 13. doi: 10.1001/jamainternmed.2018.6125).
Dr. Edelman and Dr. Tetrault are affiliated with Yale School of Medicine in New Haven, Conn. They had no financial conflicts to disclose.
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
All adults aged 18 years and older, including pregnant women, should be screened in primary care settings for unhealthy alcohol use and offered behavioral counseling if needed, according to recommendations from the U.S. Preventive Services Task Force.
Adults who meet the criteria for unhealthy alcohol use should be offered brief behavioral counseling interventions, the task force concluded with a B recommendation.
However, the task force also concluded that evidence is insufficient to recommend screening for alcohol use in adolescents aged 12-17 years in primary care settings (an I statement), wrote Susan J. Curry, PhD, of the University of Iowa, Iowa City, and colleagues. The recommendations were published in JAMA as an update of the USPSTF 2013 recommendation on screening for unhealthy alcohol use in primary care settings.
Approximately 88,000 deaths occurred each year in the United States between 2006 and 2010, the task force noted. Those deaths include death by acute causes, such as alcohol-related injuries, and chronic causes, such as alcoholic liver disease. In addition, alcohol use during pregnancy is a major preventable cause of birth defects and developmental disabilities, the task force wrote.
After reviewing the evidence, the USPSTF concluded that brief behavioral counseling offered moderate net benefits for adults 18 years and older, including pregnant women, who met criteria for unhealthy alcohol use.
Unhealthy alcohol used was defined as exceeding the National Institute on Alcohol Abuse and Alcoholism (NIAAA) recommended limits of 4 drinks per day, or 14 drinks per week, for men aged 21-64 years, and 3 drinks per day, or 7 drinks per week, for women aged 21-64 years.
In the evidence review accompanying the recommendations, Elizabeth A. O’Connor, PhD, of Kaiser Permanente in Portland, Ore., and colleagues analyzed data from 113 studies, including 314,466 individuals; 10 studies included adolescents.
In 68 studies including 36,528 individuals, brief counseling was associated with fewer drinks per week, fewer individuals exceeding recommended limits for alcohol consumption, fewer drinkers reporting a heavy drinking episode, and a greater proportion of pregnant women reporting alcohol abstinence after 6-12 months.
None of the studies assessed benefits or harms, but no evidence suggested that the interventions could be harmful.
The USPSTF is supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose.
SOURCES: Curry S et al. JAMA. 2018;320(18):1899-1909; O’Connor E et al. JAMA. 2018;320(18):1910-28.
FROM JAMA
RFM awareness program not effective at preventing stillbirths
Because reduced fetal movement is associated with higher stillbirth risk, asking women to be alert to RFM and report it immediately has emerged as a potential intervention to prevent stillbirth. But a large, randomized trial of one reporting and management protocol showed no reduction in stillbirths, only a rise in C-sections and preterm inductions.
Jane E. Norman, MD, of the University of Edinburgh, and her colleagues published results from a trial in the Lancet, in which 409,175 pregnant women (mean age, 30 years) across 33 hospitals in the United Kingdom and Ireland received either standard care or the experimental RFM care intervention before delivery. Women were seen during an experimental 3-month period, in which all were treated according to the protocol, or the 3-month control period that preceded it. A 2-month washout period occurred between allocations as institutions adapted to the study protocol.
The trial intervention consisted of training clinical staff on the implications and management of RFM, distributing written information on RFM to women at about 20 weeks’ gestation, and a management protocol aimed at quick action following a report of RFM at 24 or more weeks’ gestation. The protocol included cardiotocography within 2 hours of presentation followed by measurement of liquor volume and a growth scan, along with umbilical artery Doppler where available. Delivery was recommended for women at 37 or more weeks’ gestation with estimated fetal weight below the 10th centile, abdominal circumference below the 10th centile, a low liquor volume, an abnormal cardiotocograph, or recurrent RFM.
Incidence of stillbirth at or beyond 24 weeks was 4.40 per 1,000 births during the control period and 4.06 per 1,000 births in the intervention period (adjusted odds ratio, 0.90; 95% confidence interval, 0.75-1.07; P = .23), the researchers found. No differences were seen when stratifying for different gestational ages.
Meanwhile, induction of labor before 39 weeks was more frequent during intervention period at 40% of deliveries, compared with 34% during the control time (P less than .0001), and at term (41% vs. 36%; P = .0015). C-section was higher in the intervention group at 28% versus 26% (P = .0001). Neonatal ICU stays were not more common but were likely to be longer in the intervention period, with stays of 2 days or longer occurring in 6.7% of deliveries versus 6.2% (P =.0001).
The investigators concluded that their protocol, in its current design, was not effective and could not be recommended because of the significant increase in interventions.
Dr. Norman and her colleagues wrote that the findings would “reignite the controversy about the efficacy of RFM awareness to reduce stillbirth and the underlying mechanisms linking RFM and stillbirth.” However, the results do not mean that RFM is a sign of inevitable fetal death or that there is no role for RFM awareness as a stillbirth-prevention strategy. Other large trials testing RFM-based interventions are still underway, they noted.
“Further research to identify better predictive tests for stillbirth [to enable targeting of the only current treatment of earlier delivery] is urgently needed,” the investigators added.
In a related study also published in the Lancet, Lucy K. Smith, PhD, of the University of Leicester (England), and her colleagues reported that the real burden of stillbirth in Europe, while much lower than in the developing world, is still a third higher than reported using the current international cutoff established by the World Health Organization.
Dr. Smith and her colleagues examined national cohort data from 19 European countries between 2004 and 2015 for pregnancy outcomes from 22 completed weeks’ gestation. In 2015, they found more than 9,000 stillbirths occurred among more than 25 million births, and 3,022 of these (32%) occurred between 22 and 28 weeks’ gestation.
The WHO officially defines stillbirth as any baby born without life at 28 weeks or beyond, although it recommends that countries collect data on fetal death from 22 weeks. However, discrepancies between and even within countries in reporting laws and their implementation “inhibit reliable international comparisons” at those earlier gestational ages, Dr. Smith and her colleagues wrote.
The researchers, pooling data from the 19 countries, found that the stillbirth rate at 24-28 weeks’ gestation declined from 0.97 per 1,000 births (95% CI, 0.80-1.14) to 0.70 per 1,000 births (95% CI, 0.57-0.82) between 2004 and 2015, a reduction of 25% (risk ratio; 0.75; 95% CI, 0.65-0.85).
“The decrease of 25% in stillbirths at 24 weeks to less than 28 weeks is very similar to that seen globally for stillbirths of 28 weeks of gestation [25.5% worldwide and 24.5% in developed regions] and above for a similar time period of 2000-2015, suggesting consistent improvements over time in the reduction of stillbirths from 24 completed weeks of gestation,” the researchers wrote in their analysis.
Data from France, Spain, and Cyprus was not included in the analysis as these countries did not collect fetal death reports for the gestational periods in the study. Also, for a few countries in the study, late terminations of pregnancy could not be distinguished from spontaneous fetal death.
“The consistency in reporting of births over time at 24 weeks to less than 28 weeks of gestation and the similarity of reduction in the rate of stillbirth over time to births at 28 completed weeks of gestation and above suggest that stillbirths at 24 weeks to less than 28 weeks of gestation can be routinely included in rates of stillbirth for international comparisons from now on,” at least in high-income countries, the investigators wrote.
The study by Norman et al. was funded by the Scottish government, Tommy’s Health Center, and Sands, a U.K. stillbirth charity. The article presents research funded in part by the National Institute for Health Research. Several investigators, including the lead author, reported financial support from these entities. One author reported salary from National Health Service Lothian. All other authors reported no relevant financial disclosures. The study by Smith et al. was funded by the European Union and National Institute for Health Research. Dr. Smith received funding from a National Institute for Health Research Career Development Fellowship. All other authors reported no financial conflicts of interest.
SOURCES: Norman JE et al. Lancet. 2018;392:1629-38; Smith LK et al. Lancet. 2018;392:1639-46.
The well-conducted, randomized trial by Norman et al. enrolled over 400,000 women at 33 trials to see if reduced fetal movement reporting would significantly reduce stillbirths. It did not, but it did increase C-sections, Kate F. Walker, PhD, and Jim G. Thornton wrote in an invited commentary.
“Repeated episodes of reduced fetal movement can be so stressful to the mother that some doctors are persuaded to induce, even if further tests are normal. There also are anecdotes of women feigning reduced fetal movements to attain an ultrasound scan or induction of labor. The prevalence of women falsifying RFM is important because, although induction of birth at full term is unlikely to seriously harm the mother or the baby, preterm induction has risks,” they wrote.
“Failure of health care providers to respond to reported changes to fetal movement is probably impossible. However, discouraging campaigns that promote awareness preterm, improving induction guidelines, and not inducing delivery in response to perception of altered movement alone would seem to be sensible first steps,” Dr. Walker and Mr. Thornton concluded.
Dr. Walker and Mr. Thornton are with the division of child health, obstetrics, and gynecology at the University of Nottingham (England). They reported no financial interests related to their commentary (Lancet. 2018 Nov 3. doi: 10.1016/S0140-6736[18]31720-3).
The well-conducted, randomized trial by Norman et al. enrolled over 400,000 women at 33 trials to see if reduced fetal movement reporting would significantly reduce stillbirths. It did not, but it did increase C-sections, Kate F. Walker, PhD, and Jim G. Thornton wrote in an invited commentary.
“Repeated episodes of reduced fetal movement can be so stressful to the mother that some doctors are persuaded to induce, even if further tests are normal. There also are anecdotes of women feigning reduced fetal movements to attain an ultrasound scan or induction of labor. The prevalence of women falsifying RFM is important because, although induction of birth at full term is unlikely to seriously harm the mother or the baby, preterm induction has risks,” they wrote.
“Failure of health care providers to respond to reported changes to fetal movement is probably impossible. However, discouraging campaigns that promote awareness preterm, improving induction guidelines, and not inducing delivery in response to perception of altered movement alone would seem to be sensible first steps,” Dr. Walker and Mr. Thornton concluded.
Dr. Walker and Mr. Thornton are with the division of child health, obstetrics, and gynecology at the University of Nottingham (England). They reported no financial interests related to their commentary (Lancet. 2018 Nov 3. doi: 10.1016/S0140-6736[18]31720-3).
The well-conducted, randomized trial by Norman et al. enrolled over 400,000 women at 33 trials to see if reduced fetal movement reporting would significantly reduce stillbirths. It did not, but it did increase C-sections, Kate F. Walker, PhD, and Jim G. Thornton wrote in an invited commentary.
“Repeated episodes of reduced fetal movement can be so stressful to the mother that some doctors are persuaded to induce, even if further tests are normal. There also are anecdotes of women feigning reduced fetal movements to attain an ultrasound scan or induction of labor. The prevalence of women falsifying RFM is important because, although induction of birth at full term is unlikely to seriously harm the mother or the baby, preterm induction has risks,” they wrote.
“Failure of health care providers to respond to reported changes to fetal movement is probably impossible. However, discouraging campaigns that promote awareness preterm, improving induction guidelines, and not inducing delivery in response to perception of altered movement alone would seem to be sensible first steps,” Dr. Walker and Mr. Thornton concluded.
Dr. Walker and Mr. Thornton are with the division of child health, obstetrics, and gynecology at the University of Nottingham (England). They reported no financial interests related to their commentary (Lancet. 2018 Nov 3. doi: 10.1016/S0140-6736[18]31720-3).
Because reduced fetal movement is associated with higher stillbirth risk, asking women to be alert to RFM and report it immediately has emerged as a potential intervention to prevent stillbirth. But a large, randomized trial of one reporting and management protocol showed no reduction in stillbirths, only a rise in C-sections and preterm inductions.
Jane E. Norman, MD, of the University of Edinburgh, and her colleagues published results from a trial in the Lancet, in which 409,175 pregnant women (mean age, 30 years) across 33 hospitals in the United Kingdom and Ireland received either standard care or the experimental RFM care intervention before delivery. Women were seen during an experimental 3-month period, in which all were treated according to the protocol, or the 3-month control period that preceded it. A 2-month washout period occurred between allocations as institutions adapted to the study protocol.
The trial intervention consisted of training clinical staff on the implications and management of RFM, distributing written information on RFM to women at about 20 weeks’ gestation, and a management protocol aimed at quick action following a report of RFM at 24 or more weeks’ gestation. The protocol included cardiotocography within 2 hours of presentation followed by measurement of liquor volume and a growth scan, along with umbilical artery Doppler where available. Delivery was recommended for women at 37 or more weeks’ gestation with estimated fetal weight below the 10th centile, abdominal circumference below the 10th centile, a low liquor volume, an abnormal cardiotocograph, or recurrent RFM.
Incidence of stillbirth at or beyond 24 weeks was 4.40 per 1,000 births during the control period and 4.06 per 1,000 births in the intervention period (adjusted odds ratio, 0.90; 95% confidence interval, 0.75-1.07; P = .23), the researchers found. No differences were seen when stratifying for different gestational ages.
Meanwhile, induction of labor before 39 weeks was more frequent during intervention period at 40% of deliveries, compared with 34% during the control time (P less than .0001), and at term (41% vs. 36%; P = .0015). C-section was higher in the intervention group at 28% versus 26% (P = .0001). Neonatal ICU stays were not more common but were likely to be longer in the intervention period, with stays of 2 days or longer occurring in 6.7% of deliveries versus 6.2% (P =.0001).
The investigators concluded that their protocol, in its current design, was not effective and could not be recommended because of the significant increase in interventions.
Dr. Norman and her colleagues wrote that the findings would “reignite the controversy about the efficacy of RFM awareness to reduce stillbirth and the underlying mechanisms linking RFM and stillbirth.” However, the results do not mean that RFM is a sign of inevitable fetal death or that there is no role for RFM awareness as a stillbirth-prevention strategy. Other large trials testing RFM-based interventions are still underway, they noted.
“Further research to identify better predictive tests for stillbirth [to enable targeting of the only current treatment of earlier delivery] is urgently needed,” the investigators added.
In a related study also published in the Lancet, Lucy K. Smith, PhD, of the University of Leicester (England), and her colleagues reported that the real burden of stillbirth in Europe, while much lower than in the developing world, is still a third higher than reported using the current international cutoff established by the World Health Organization.
Dr. Smith and her colleagues examined national cohort data from 19 European countries between 2004 and 2015 for pregnancy outcomes from 22 completed weeks’ gestation. In 2015, they found more than 9,000 stillbirths occurred among more than 25 million births, and 3,022 of these (32%) occurred between 22 and 28 weeks’ gestation.
The WHO officially defines stillbirth as any baby born without life at 28 weeks or beyond, although it recommends that countries collect data on fetal death from 22 weeks. However, discrepancies between and even within countries in reporting laws and their implementation “inhibit reliable international comparisons” at those earlier gestational ages, Dr. Smith and her colleagues wrote.
The researchers, pooling data from the 19 countries, found that the stillbirth rate at 24-28 weeks’ gestation declined from 0.97 per 1,000 births (95% CI, 0.80-1.14) to 0.70 per 1,000 births (95% CI, 0.57-0.82) between 2004 and 2015, a reduction of 25% (risk ratio; 0.75; 95% CI, 0.65-0.85).
“The decrease of 25% in stillbirths at 24 weeks to less than 28 weeks is very similar to that seen globally for stillbirths of 28 weeks of gestation [25.5% worldwide and 24.5% in developed regions] and above for a similar time period of 2000-2015, suggesting consistent improvements over time in the reduction of stillbirths from 24 completed weeks of gestation,” the researchers wrote in their analysis.
Data from France, Spain, and Cyprus was not included in the analysis as these countries did not collect fetal death reports for the gestational periods in the study. Also, for a few countries in the study, late terminations of pregnancy could not be distinguished from spontaneous fetal death.
“The consistency in reporting of births over time at 24 weeks to less than 28 weeks of gestation and the similarity of reduction in the rate of stillbirth over time to births at 28 completed weeks of gestation and above suggest that stillbirths at 24 weeks to less than 28 weeks of gestation can be routinely included in rates of stillbirth for international comparisons from now on,” at least in high-income countries, the investigators wrote.
The study by Norman et al. was funded by the Scottish government, Tommy’s Health Center, and Sands, a U.K. stillbirth charity. The article presents research funded in part by the National Institute for Health Research. Several investigators, including the lead author, reported financial support from these entities. One author reported salary from National Health Service Lothian. All other authors reported no relevant financial disclosures. The study by Smith et al. was funded by the European Union and National Institute for Health Research. Dr. Smith received funding from a National Institute for Health Research Career Development Fellowship. All other authors reported no financial conflicts of interest.
SOURCES: Norman JE et al. Lancet. 2018;392:1629-38; Smith LK et al. Lancet. 2018;392:1639-46.
Because reduced fetal movement is associated with higher stillbirth risk, asking women to be alert to RFM and report it immediately has emerged as a potential intervention to prevent stillbirth. But a large, randomized trial of one reporting and management protocol showed no reduction in stillbirths, only a rise in C-sections and preterm inductions.
Jane E. Norman, MD, of the University of Edinburgh, and her colleagues published results from a trial in the Lancet, in which 409,175 pregnant women (mean age, 30 years) across 33 hospitals in the United Kingdom and Ireland received either standard care or the experimental RFM care intervention before delivery. Women were seen during an experimental 3-month period, in which all were treated according to the protocol, or the 3-month control period that preceded it. A 2-month washout period occurred between allocations as institutions adapted to the study protocol.
The trial intervention consisted of training clinical staff on the implications and management of RFM, distributing written information on RFM to women at about 20 weeks’ gestation, and a management protocol aimed at quick action following a report of RFM at 24 or more weeks’ gestation. The protocol included cardiotocography within 2 hours of presentation followed by measurement of liquor volume and a growth scan, along with umbilical artery Doppler where available. Delivery was recommended for women at 37 or more weeks’ gestation with estimated fetal weight below the 10th centile, abdominal circumference below the 10th centile, a low liquor volume, an abnormal cardiotocograph, or recurrent RFM.
Incidence of stillbirth at or beyond 24 weeks was 4.40 per 1,000 births during the control period and 4.06 per 1,000 births in the intervention period (adjusted odds ratio, 0.90; 95% confidence interval, 0.75-1.07; P = .23), the researchers found. No differences were seen when stratifying for different gestational ages.
Meanwhile, induction of labor before 39 weeks was more frequent during intervention period at 40% of deliveries, compared with 34% during the control time (P less than .0001), and at term (41% vs. 36%; P = .0015). C-section was higher in the intervention group at 28% versus 26% (P = .0001). Neonatal ICU stays were not more common but were likely to be longer in the intervention period, with stays of 2 days or longer occurring in 6.7% of deliveries versus 6.2% (P =.0001).
The investigators concluded that their protocol, in its current design, was not effective and could not be recommended because of the significant increase in interventions.
Dr. Norman and her colleagues wrote that the findings would “reignite the controversy about the efficacy of RFM awareness to reduce stillbirth and the underlying mechanisms linking RFM and stillbirth.” However, the results do not mean that RFM is a sign of inevitable fetal death or that there is no role for RFM awareness as a stillbirth-prevention strategy. Other large trials testing RFM-based interventions are still underway, they noted.
“Further research to identify better predictive tests for stillbirth [to enable targeting of the only current treatment of earlier delivery] is urgently needed,” the investigators added.
In a related study also published in the Lancet, Lucy K. Smith, PhD, of the University of Leicester (England), and her colleagues reported that the real burden of stillbirth in Europe, while much lower than in the developing world, is still a third higher than reported using the current international cutoff established by the World Health Organization.
Dr. Smith and her colleagues examined national cohort data from 19 European countries between 2004 and 2015 for pregnancy outcomes from 22 completed weeks’ gestation. In 2015, they found more than 9,000 stillbirths occurred among more than 25 million births, and 3,022 of these (32%) occurred between 22 and 28 weeks’ gestation.
The WHO officially defines stillbirth as any baby born without life at 28 weeks or beyond, although it recommends that countries collect data on fetal death from 22 weeks. However, discrepancies between and even within countries in reporting laws and their implementation “inhibit reliable international comparisons” at those earlier gestational ages, Dr. Smith and her colleagues wrote.
The researchers, pooling data from the 19 countries, found that the stillbirth rate at 24-28 weeks’ gestation declined from 0.97 per 1,000 births (95% CI, 0.80-1.14) to 0.70 per 1,000 births (95% CI, 0.57-0.82) between 2004 and 2015, a reduction of 25% (risk ratio; 0.75; 95% CI, 0.65-0.85).
“The decrease of 25% in stillbirths at 24 weeks to less than 28 weeks is very similar to that seen globally for stillbirths of 28 weeks of gestation [25.5% worldwide and 24.5% in developed regions] and above for a similar time period of 2000-2015, suggesting consistent improvements over time in the reduction of stillbirths from 24 completed weeks of gestation,” the researchers wrote in their analysis.
Data from France, Spain, and Cyprus was not included in the analysis as these countries did not collect fetal death reports for the gestational periods in the study. Also, for a few countries in the study, late terminations of pregnancy could not be distinguished from spontaneous fetal death.
“The consistency in reporting of births over time at 24 weeks to less than 28 weeks of gestation and the similarity of reduction in the rate of stillbirth over time to births at 28 completed weeks of gestation and above suggest that stillbirths at 24 weeks to less than 28 weeks of gestation can be routinely included in rates of stillbirth for international comparisons from now on,” at least in high-income countries, the investigators wrote.
The study by Norman et al. was funded by the Scottish government, Tommy’s Health Center, and Sands, a U.K. stillbirth charity. The article presents research funded in part by the National Institute for Health Research. Several investigators, including the lead author, reported financial support from these entities. One author reported salary from National Health Service Lothian. All other authors reported no relevant financial disclosures. The study by Smith et al. was funded by the European Union and National Institute for Health Research. Dr. Smith received funding from a National Institute for Health Research Career Development Fellowship. All other authors reported no financial conflicts of interest.
SOURCES: Norman JE et al. Lancet. 2018;392:1629-38; Smith LK et al. Lancet. 2018;392:1639-46.
FROM THE LANCET
Key clinical point:
Major finding: Incidence of stillbirth at 24 weeks’ gestation or later was 4.06 per 1,000 in the intervention group and 4.40 per 1,000 with standard care (adjusted odds ratio, 0.90; 95% confidence interval, 0.75-1.07; P = .23).
Study details: Data from more than 400,000 pregnancies across 33 hospitals in the United Kingdom and Ireland; women were seen during a 3-month period of standard care or a 3-month intervention period.
Disclosures: The study by Norman et al. was funded by the Scottish government, Tommy’s Health Center, and Sands, a U.K. stillbirth charity. The article presents research funded in part by the National Institute for Health Research. Several investigators, including the lead author, reported financial support from these entities. One author reported salary from National Health Service Lothian. All other authors reported no relevant financial disclosures. The study by Smith et al. was funded by the European Union and National Institute for Health Research. Dr. Smith received funding from a National Institute for Health Research Career Development Fellowship. All other authors reported no financial conflicts of interest.
Sources: Norman JE et al. Lancet. 2018;392:1629-38; Smith LK et al. Lancet. 2018;392:1639-46.
Antimigraine agents in pregnancy and lactation
Migraine is a common neurovascular disorder with episodic attacks of throbbing headache, nausea/vomiting, photophobia, and phonophobia. Migraine symptoms will lessen in up to 70% of pregnant women, usually during the second and third trimesters, but will worsen in 4%-8%, and new-onset migraine may account for as many as 16% of all cases of the disorder in pregnancy.
Prevention of migraines
A 2002 review by Goadsby PJ et al. (N Engl J Med. 2002 Jan 24;346[4]:257-70) identified 11 drugs or drug classes for the prevention of migraine attacks. Four agents that are available in the United States were thought to have proven efficacy or were well accepted: metoprolol, propranolol, amitriptyline, and valproate. Valproate should not be used during pregnancy because it is a known teratogen and can cause other fetal problems throughout gestation. Metoprolol, a cardioselective beta-blocker, is a risk for intrauterine growth restriction (IUGR) in the second/third trimesters.
Three other agents are not available in the United States: flunarizine (an agent with calcium channel blocking activity) and two serotonin antagonists, pizotifen and methysergide (a semisynthetic ergot alkaloid). Based on the drug class, flunarizine probably is compatible with pregnancy. Ergot alkaloids, including methysergide, are contraindicated in pregnancy.
Verapamil (Calan, Isoptin) and the selective serotonin reuptake inhibitors (SSRIs) were widely used, but the reviewers concluded that there was poor evidence of benefit.
Use of the SSRI antidepressants in the third trimester may cause newborn toxicity.
Only amitriptyline, verapamil, and low-dose propranolol (30-40 mg/day) have sufficient data to classify as compatible throughout pregnancy, but higher doses of propranolol may cause IUGR and other fetal/neonatal toxicity.
Two agents, gabapentin (Neurontin) and topiramate (Topamax), were considered promising agents for migraine prophylaxis. However, topiramate is best avoided in pregnancy. There are inadequate human data to assess the risk of gabapentin and topiramate, therefore both agents should be avoided in the first trimester.
Breastfeeding: Prevention therapy
Based on their potential for harm, topiramate and valproate should not be used during breastfeeding. All of the other drugs probably are compatible with breastfeeding, but the nursing infant should be monitored for adverse effects common in nonpregnant adults.
Acute treatment of migraines
There are 11 single-agent drugs that are indicated for the acute treatment of migraine.
Almotriptan (Axert) is available as an oral tablet. There are no human pregnancy data and the animal data suggest low risk. However, there is a possible risk of preterm birth.
Dihydroergotamine (Migranal, D.H.E. 45) is available for injection and nasal spray. It is contraindicated, especially near term (it has oxytocic properties), and the animal data suggest risk of IUGR.
Eletriptan (Relpax) is an oral tablet. There are no human data and the animal data suggest low risk. There is a possible risk of preterm birth.
Ergotamine (Ergomar), an oral tablet, is contraindicated in pregnancy and breastfeeding (see above and below).
Methysergide (Sansert) is contraindicated but is not available in United States.
Frovatriptan (Frova) has no human pregnancy data. The animal data suggests low risk but there is the possibility of preterm birth.
There are 93 cases in pregnancy for naratriptan (Amerge) but none during breastfeeding. The drug did not cause major defects in animals but did produce dose-related embryo and fetal development toxicity. In addition, the data did suggest a possible increase in preterm births.
For the rizatriptan (Maxalt, Maxalt-MLT) tablet, animal data suggest low risk. There was exposure to the drug in more than 81 human pregnancy cases. Although there was no evidence of birth defects, the data raised the concern of preterm birth.
There is no evidence that sumatriptan (Alsuma, Imitrex, Imitrex Statdose, Sumavel DosePro, Zecuity) is a human teratogen but there is a possible increase in preterm birth. The drug was teratogenic in one animal species. This agent is available as a tablet and for injection.
There is no human pregnancy data for zolmitriptan (Zomig; Zomig-ZMT) but, as with all triptans, there is a possible risk of preterm birth. The animal data suggest low risk. It is available as an oral tablet.
There are three multiagent products that can be used to treat migraines. There are no published human pregnancy data for these combination products. The combination oral drug sumatriptan and naproxen (Treximet) is best avoided in pregnancy because first trimester exposure to the NSAID naproxen may cause embryo-fetal harm (structural anomalies and abortion) or close to term (premature closure of the ductus arteriosus) and other newborn toxicities.
Caffeine and ergotamine (Cafergot, Migergot) tablets should be considered contraindicated in pregnancy and breastfeeding. Although small, infrequent doses of this product do not appear to be fetotoxic or teratogenic, idiosyncratic responses may occur with ergotamine that endanger the fetus.
The third product, acetaminophen, dichloralphenazone, and isometheptene (Epidrin, LarkaDrin, Migragesic IDA) is an over-the-counter tablet. It does not appear to be related to embryo-fetal harm, but its effectiveness is unknown.
Breastfeeding: Acute treatment
Consistent with their relatively low molecular weights, all of the acute treatment agents most likely are excreted into breast milk. With the exception of the two ergotamine products, both of which should be considered contraindicated, all of the other agents probably are compatible during breastfeeding.
Summary
Migraine headaches are common but can be prevented and/or treated safely in pregnancy and when nursing. In addition to the review mentioned above, three other reviews are well worth reading: Becker WJ. Continuum (Minneap Minn). 2015 Aug;21(4 Headache):953-72; Becker WJ. Headache. 2015 Jun;55(6):778-93; Hutchinson S et al. Headache. 2013 Apr;53(4):614-27.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Migraine is a common neurovascular disorder with episodic attacks of throbbing headache, nausea/vomiting, photophobia, and phonophobia. Migraine symptoms will lessen in up to 70% of pregnant women, usually during the second and third trimesters, but will worsen in 4%-8%, and new-onset migraine may account for as many as 16% of all cases of the disorder in pregnancy.
Prevention of migraines
A 2002 review by Goadsby PJ et al. (N Engl J Med. 2002 Jan 24;346[4]:257-70) identified 11 drugs or drug classes for the prevention of migraine attacks. Four agents that are available in the United States were thought to have proven efficacy or were well accepted: metoprolol, propranolol, amitriptyline, and valproate. Valproate should not be used during pregnancy because it is a known teratogen and can cause other fetal problems throughout gestation. Metoprolol, a cardioselective beta-blocker, is a risk for intrauterine growth restriction (IUGR) in the second/third trimesters.
Three other agents are not available in the United States: flunarizine (an agent with calcium channel blocking activity) and two serotonin antagonists, pizotifen and methysergide (a semisynthetic ergot alkaloid). Based on the drug class, flunarizine probably is compatible with pregnancy. Ergot alkaloids, including methysergide, are contraindicated in pregnancy.
Verapamil (Calan, Isoptin) and the selective serotonin reuptake inhibitors (SSRIs) were widely used, but the reviewers concluded that there was poor evidence of benefit.
Use of the SSRI antidepressants in the third trimester may cause newborn toxicity.
Only amitriptyline, verapamil, and low-dose propranolol (30-40 mg/day) have sufficient data to classify as compatible throughout pregnancy, but higher doses of propranolol may cause IUGR and other fetal/neonatal toxicity.
Two agents, gabapentin (Neurontin) and topiramate (Topamax), were considered promising agents for migraine prophylaxis. However, topiramate is best avoided in pregnancy. There are inadequate human data to assess the risk of gabapentin and topiramate, therefore both agents should be avoided in the first trimester.
Breastfeeding: Prevention therapy
Based on their potential for harm, topiramate and valproate should not be used during breastfeeding. All of the other drugs probably are compatible with breastfeeding, but the nursing infant should be monitored for adverse effects common in nonpregnant adults.
Acute treatment of migraines
There are 11 single-agent drugs that are indicated for the acute treatment of migraine.
Almotriptan (Axert) is available as an oral tablet. There are no human pregnancy data and the animal data suggest low risk. However, there is a possible risk of preterm birth.
Dihydroergotamine (Migranal, D.H.E. 45) is available for injection and nasal spray. It is contraindicated, especially near term (it has oxytocic properties), and the animal data suggest risk of IUGR.
Eletriptan (Relpax) is an oral tablet. There are no human data and the animal data suggest low risk. There is a possible risk of preterm birth.
Ergotamine (Ergomar), an oral tablet, is contraindicated in pregnancy and breastfeeding (see above and below).
Methysergide (Sansert) is contraindicated but is not available in United States.
Frovatriptan (Frova) has no human pregnancy data. The animal data suggests low risk but there is the possibility of preterm birth.
There are 93 cases in pregnancy for naratriptan (Amerge) but none during breastfeeding. The drug did not cause major defects in animals but did produce dose-related embryo and fetal development toxicity. In addition, the data did suggest a possible increase in preterm births.
For the rizatriptan (Maxalt, Maxalt-MLT) tablet, animal data suggest low risk. There was exposure to the drug in more than 81 human pregnancy cases. Although there was no evidence of birth defects, the data raised the concern of preterm birth.
There is no evidence that sumatriptan (Alsuma, Imitrex, Imitrex Statdose, Sumavel DosePro, Zecuity) is a human teratogen but there is a possible increase in preterm birth. The drug was teratogenic in one animal species. This agent is available as a tablet and for injection.
There is no human pregnancy data for zolmitriptan (Zomig; Zomig-ZMT) but, as with all triptans, there is a possible risk of preterm birth. The animal data suggest low risk. It is available as an oral tablet.
There are three multiagent products that can be used to treat migraines. There are no published human pregnancy data for these combination products. The combination oral drug sumatriptan and naproxen (Treximet) is best avoided in pregnancy because first trimester exposure to the NSAID naproxen may cause embryo-fetal harm (structural anomalies and abortion) or close to term (premature closure of the ductus arteriosus) and other newborn toxicities.
Caffeine and ergotamine (Cafergot, Migergot) tablets should be considered contraindicated in pregnancy and breastfeeding. Although small, infrequent doses of this product do not appear to be fetotoxic or teratogenic, idiosyncratic responses may occur with ergotamine that endanger the fetus.
The third product, acetaminophen, dichloralphenazone, and isometheptene (Epidrin, LarkaDrin, Migragesic IDA) is an over-the-counter tablet. It does not appear to be related to embryo-fetal harm, but its effectiveness is unknown.
Breastfeeding: Acute treatment
Consistent with their relatively low molecular weights, all of the acute treatment agents most likely are excreted into breast milk. With the exception of the two ergotamine products, both of which should be considered contraindicated, all of the other agents probably are compatible during breastfeeding.
Summary
Migraine headaches are common but can be prevented and/or treated safely in pregnancy and when nursing. In addition to the review mentioned above, three other reviews are well worth reading: Becker WJ. Continuum (Minneap Minn). 2015 Aug;21(4 Headache):953-72; Becker WJ. Headache. 2015 Jun;55(6):778-93; Hutchinson S et al. Headache. 2013 Apr;53(4):614-27.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Migraine is a common neurovascular disorder with episodic attacks of throbbing headache, nausea/vomiting, photophobia, and phonophobia. Migraine symptoms will lessen in up to 70% of pregnant women, usually during the second and third trimesters, but will worsen in 4%-8%, and new-onset migraine may account for as many as 16% of all cases of the disorder in pregnancy.
Prevention of migraines
A 2002 review by Goadsby PJ et al. (N Engl J Med. 2002 Jan 24;346[4]:257-70) identified 11 drugs or drug classes for the prevention of migraine attacks. Four agents that are available in the United States were thought to have proven efficacy or were well accepted: metoprolol, propranolol, amitriptyline, and valproate. Valproate should not be used during pregnancy because it is a known teratogen and can cause other fetal problems throughout gestation. Metoprolol, a cardioselective beta-blocker, is a risk for intrauterine growth restriction (IUGR) in the second/third trimesters.
Three other agents are not available in the United States: flunarizine (an agent with calcium channel blocking activity) and two serotonin antagonists, pizotifen and methysergide (a semisynthetic ergot alkaloid). Based on the drug class, flunarizine probably is compatible with pregnancy. Ergot alkaloids, including methysergide, are contraindicated in pregnancy.
Verapamil (Calan, Isoptin) and the selective serotonin reuptake inhibitors (SSRIs) were widely used, but the reviewers concluded that there was poor evidence of benefit.
Use of the SSRI antidepressants in the third trimester may cause newborn toxicity.
Only amitriptyline, verapamil, and low-dose propranolol (30-40 mg/day) have sufficient data to classify as compatible throughout pregnancy, but higher doses of propranolol may cause IUGR and other fetal/neonatal toxicity.
Two agents, gabapentin (Neurontin) and topiramate (Topamax), were considered promising agents for migraine prophylaxis. However, topiramate is best avoided in pregnancy. There are inadequate human data to assess the risk of gabapentin and topiramate, therefore both agents should be avoided in the first trimester.
Breastfeeding: Prevention therapy
Based on their potential for harm, topiramate and valproate should not be used during breastfeeding. All of the other drugs probably are compatible with breastfeeding, but the nursing infant should be monitored for adverse effects common in nonpregnant adults.
Acute treatment of migraines
There are 11 single-agent drugs that are indicated for the acute treatment of migraine.
Almotriptan (Axert) is available as an oral tablet. There are no human pregnancy data and the animal data suggest low risk. However, there is a possible risk of preterm birth.
Dihydroergotamine (Migranal, D.H.E. 45) is available for injection and nasal spray. It is contraindicated, especially near term (it has oxytocic properties), and the animal data suggest risk of IUGR.
Eletriptan (Relpax) is an oral tablet. There are no human data and the animal data suggest low risk. There is a possible risk of preterm birth.
Ergotamine (Ergomar), an oral tablet, is contraindicated in pregnancy and breastfeeding (see above and below).
Methysergide (Sansert) is contraindicated but is not available in United States.
Frovatriptan (Frova) has no human pregnancy data. The animal data suggests low risk but there is the possibility of preterm birth.
There are 93 cases in pregnancy for naratriptan (Amerge) but none during breastfeeding. The drug did not cause major defects in animals but did produce dose-related embryo and fetal development toxicity. In addition, the data did suggest a possible increase in preterm births.
For the rizatriptan (Maxalt, Maxalt-MLT) tablet, animal data suggest low risk. There was exposure to the drug in more than 81 human pregnancy cases. Although there was no evidence of birth defects, the data raised the concern of preterm birth.
There is no evidence that sumatriptan (Alsuma, Imitrex, Imitrex Statdose, Sumavel DosePro, Zecuity) is a human teratogen but there is a possible increase in preterm birth. The drug was teratogenic in one animal species. This agent is available as a tablet and for injection.
There is no human pregnancy data for zolmitriptan (Zomig; Zomig-ZMT) but, as with all triptans, there is a possible risk of preterm birth. The animal data suggest low risk. It is available as an oral tablet.
There are three multiagent products that can be used to treat migraines. There are no published human pregnancy data for these combination products. The combination oral drug sumatriptan and naproxen (Treximet) is best avoided in pregnancy because first trimester exposure to the NSAID naproxen may cause embryo-fetal harm (structural anomalies and abortion) or close to term (premature closure of the ductus arteriosus) and other newborn toxicities.
Caffeine and ergotamine (Cafergot, Migergot) tablets should be considered contraindicated in pregnancy and breastfeeding. Although small, infrequent doses of this product do not appear to be fetotoxic or teratogenic, idiosyncratic responses may occur with ergotamine that endanger the fetus.
The third product, acetaminophen, dichloralphenazone, and isometheptene (Epidrin, LarkaDrin, Migragesic IDA) is an over-the-counter tablet. It does not appear to be related to embryo-fetal harm, but its effectiveness is unknown.
Breastfeeding: Acute treatment
Consistent with their relatively low molecular weights, all of the acute treatment agents most likely are excreted into breast milk. With the exception of the two ergotamine products, both of which should be considered contraindicated, all of the other agents probably are compatible during breastfeeding.
Summary
Migraine headaches are common but can be prevented and/or treated safely in pregnancy and when nursing. In addition to the review mentioned above, three other reviews are well worth reading: Becker WJ. Continuum (Minneap Minn). 2015 Aug;21(4 Headache):953-72; Becker WJ. Headache. 2015 Jun;55(6):778-93; Hutchinson S et al. Headache. 2013 Apr;53(4):614-27.
Mr. Briggs is a clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Needle aspiration comes first for most breast abscesses
BOSTON – When surgeon Wendy R. Greene, MD, FACS, director of acute and critical care surgery at Emory University, Atlanta, asked a room of about 300 general surgeons at the annual clinical congress of the American College of Surgeons how many use needle aspiration first for breast abscesses, and how many use a scalpel, it was about a 50-50 split.
This divided response is why Dr. Greene addressed in her presentation the right approach to the problem of breast abscesses. In short, “for run-of-the-mill abscesses less than 5 cm, don’t get out the scalpel; get out the needle first,” she said.
New mothers over age 30 years are most at risk, especially if they are past 40 weeks’ gestation.
There certainly are indications for the scalpel first. If the skin overlaying the abscess is dead, shiny, sloughing off, or leaking pus, or if the abscess is larger than 5 cm on ultrasound, a small stab incision is in order, and it should be made at the maximum point of fluctuation, after numbing the surrounding tissue. Put a wipe in place to catch the pus, debride as necessary, and “irrigate, irrigate, irrigate,” Dr. Greene said.
She uses suction to make sure all the pus is out, then injects a lidocaine into the cavity for pain control and lets it rest a few minutes before another round of suction.
Septic, deteriorating patients, and the immunocompromised, need a larger incision and drainage, with IV antibiotics in the hospital, but even in those cases, “avoid placing percutaneous drains; there’s rarely a role for them in modern management of breast abscesses.” Women will have poorer results and poorer cosmesis, Dr. Greene said.
Aggressive drainage isn’t necessary most of the time, and it can destroy healthy tissue and leave new mothers with breastfeeding problems and milk fistulas. There’s also a risk for scarring, deformity, and loss of the ability to lactate.
An 18-21 gauge needle with local anesthetic is usually enough. The lesion should be obvious on ultrasound, and it’s useful to guide the needle and ensure the cavity collapses on aspiration.
Dr. Greene said it also is important to culture milk in new mothers, and culture her infant’s nose and mouth, because cracked skin on the breast can let germs from nursing into the milk ducts.
Women are sent home after aspiration with antibiotics for 7-10 days, ones that are safe for nursing infants. They might be back with another abscess in a few weeks, so it’s important to be patient and ready for ongoing treatment.
The ultimate worry with recurrent cases is that a breast mass is blocking a milk duct, so mammography is often in order for repeat patients, especially with a family history of breast cancer. Wait until the acute infection has died down; a mammograph can be too painful otherwise, Dr. Greene said.
In the meantime, let infants nurse. They “are a great way to help drain the breast,” she said.
Dr. Greene had no relevant disclosures.
BOSTON – When surgeon Wendy R. Greene, MD, FACS, director of acute and critical care surgery at Emory University, Atlanta, asked a room of about 300 general surgeons at the annual clinical congress of the American College of Surgeons how many use needle aspiration first for breast abscesses, and how many use a scalpel, it was about a 50-50 split.
This divided response is why Dr. Greene addressed in her presentation the right approach to the problem of breast abscesses. In short, “for run-of-the-mill abscesses less than 5 cm, don’t get out the scalpel; get out the needle first,” she said.
New mothers over age 30 years are most at risk, especially if they are past 40 weeks’ gestation.
There certainly are indications for the scalpel first. If the skin overlaying the abscess is dead, shiny, sloughing off, or leaking pus, or if the abscess is larger than 5 cm on ultrasound, a small stab incision is in order, and it should be made at the maximum point of fluctuation, after numbing the surrounding tissue. Put a wipe in place to catch the pus, debride as necessary, and “irrigate, irrigate, irrigate,” Dr. Greene said.
She uses suction to make sure all the pus is out, then injects a lidocaine into the cavity for pain control and lets it rest a few minutes before another round of suction.
Septic, deteriorating patients, and the immunocompromised, need a larger incision and drainage, with IV antibiotics in the hospital, but even in those cases, “avoid placing percutaneous drains; there’s rarely a role for them in modern management of breast abscesses.” Women will have poorer results and poorer cosmesis, Dr. Greene said.
Aggressive drainage isn’t necessary most of the time, and it can destroy healthy tissue and leave new mothers with breastfeeding problems and milk fistulas. There’s also a risk for scarring, deformity, and loss of the ability to lactate.
An 18-21 gauge needle with local anesthetic is usually enough. The lesion should be obvious on ultrasound, and it’s useful to guide the needle and ensure the cavity collapses on aspiration.
Dr. Greene said it also is important to culture milk in new mothers, and culture her infant’s nose and mouth, because cracked skin on the breast can let germs from nursing into the milk ducts.
Women are sent home after aspiration with antibiotics for 7-10 days, ones that are safe for nursing infants. They might be back with another abscess in a few weeks, so it’s important to be patient and ready for ongoing treatment.
The ultimate worry with recurrent cases is that a breast mass is blocking a milk duct, so mammography is often in order for repeat patients, especially with a family history of breast cancer. Wait until the acute infection has died down; a mammograph can be too painful otherwise, Dr. Greene said.
In the meantime, let infants nurse. They “are a great way to help drain the breast,” she said.
Dr. Greene had no relevant disclosures.
BOSTON – When surgeon Wendy R. Greene, MD, FACS, director of acute and critical care surgery at Emory University, Atlanta, asked a room of about 300 general surgeons at the annual clinical congress of the American College of Surgeons how many use needle aspiration first for breast abscesses, and how many use a scalpel, it was about a 50-50 split.
This divided response is why Dr. Greene addressed in her presentation the right approach to the problem of breast abscesses. In short, “for run-of-the-mill abscesses less than 5 cm, don’t get out the scalpel; get out the needle first,” she said.
New mothers over age 30 years are most at risk, especially if they are past 40 weeks’ gestation.
There certainly are indications for the scalpel first. If the skin overlaying the abscess is dead, shiny, sloughing off, or leaking pus, or if the abscess is larger than 5 cm on ultrasound, a small stab incision is in order, and it should be made at the maximum point of fluctuation, after numbing the surrounding tissue. Put a wipe in place to catch the pus, debride as necessary, and “irrigate, irrigate, irrigate,” Dr. Greene said.
She uses suction to make sure all the pus is out, then injects a lidocaine into the cavity for pain control and lets it rest a few minutes before another round of suction.
Septic, deteriorating patients, and the immunocompromised, need a larger incision and drainage, with IV antibiotics in the hospital, but even in those cases, “avoid placing percutaneous drains; there’s rarely a role for them in modern management of breast abscesses.” Women will have poorer results and poorer cosmesis, Dr. Greene said.
Aggressive drainage isn’t necessary most of the time, and it can destroy healthy tissue and leave new mothers with breastfeeding problems and milk fistulas. There’s also a risk for scarring, deformity, and loss of the ability to lactate.
An 18-21 gauge needle with local anesthetic is usually enough. The lesion should be obvious on ultrasound, and it’s useful to guide the needle and ensure the cavity collapses on aspiration.
Dr. Greene said it also is important to culture milk in new mothers, and culture her infant’s nose and mouth, because cracked skin on the breast can let germs from nursing into the milk ducts.
Women are sent home after aspiration with antibiotics for 7-10 days, ones that are safe for nursing infants. They might be back with another abscess in a few weeks, so it’s important to be patient and ready for ongoing treatment.
The ultimate worry with recurrent cases is that a breast mass is blocking a milk duct, so mammography is often in order for repeat patients, especially with a family history of breast cancer. Wait until the acute infection has died down; a mammograph can be too painful otherwise, Dr. Greene said.
In the meantime, let infants nurse. They “are a great way to help drain the breast,” she said.
Dr. Greene had no relevant disclosures.
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
FDA panels back brexanolone infusion for postpartum depression
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
Hospitals could reduce maternal mortality with four achievable steps
rate in the United States, according to a new perspective from leading obstetricians published in the New England Journal of Medicine.
The authors, including Kimberlee McKay, MD, president of the American College of Obstetricians and Gynecologists (ACOG), also call for collaboration with family physicians to increase access to obstetric care in rural areas.
The president of the American Academy of Family Physicians (AAFP), John S. Cullen, MD, in a separate statement, welcomed the opportunity for collaboration in addressing the maternal mortality crisis. However, some distance still lies between the finer points of how the two organizations see family physicians helping curb the crisis.
“Women in the United States are more likely to die from childbirth- or pregnancy-related causes than women in any other high-income country, and black women die at a rate three to four times that of white women,” noted Susan Mann, MD, along with her coauthors of the obstetric perspective, calling increasing maternal mortality a “tragedy.”
In an interview, Dr. Cullen concurred, calling the current situation “unconscionable.” One of the primary reasons he sought AAFP leadership, he said, was to bring experiences learned during his 25 years of obstetric practice in rural Alaska to bear on the current crisis.
A set of maternal care bundles created by the Alliance for Innovation on Maternal Health (AIM) provides the framework for the first action recommended by Dr. Mann and her coauthors. The AIM bundles focus on protocols that improve readiness, recognition, response, and reporting in maternal care. The protocols are institution specific. For example, the authors noted, antihypertensive medications should be readily available around the clock, because not all facilities will have a pharmacist in-house at all times, and hypertensive emergencies are among the gravest obstetric complications.
“Although management may vary from institution to institution, each unit can be required to demonstrate readiness to deal with emergencies 24/7,” said Dr. Mann, a physician in private practice in Boston, and her coauthors.
The second recommended action revolves around multidisciplinary staff meetings to perform individual assessments for each woman’s obstetric risk factors. These huddles should include assessing hemorrhage risk by using the California Maternal Quality Care Collaborative guidelines, and briefings with the full care team to “develop shared understandings of the patient and the procedure” before elective or nonurgent cesarean deliveries, said Dr. Mann and her colleagues. Patients should be informed of any safety concerns, and caregivers should use shared decision-making moving forward.
“Approximately 50% of U.S. hospitals provide care for three or fewer deliveries per day, but the need to identify women at risk is equally important for these small obstetrics services,” Dr. Mann and her coauthors noted.
Third, simulation of obstetric emergencies lets all members of the team understand the speed at which decisions must be made and actions taken when minutes, or even seconds, count. Dr. Mann and her coauthors pointed out that logistics problems come out during a well-run simulation, giving such examples as a lag in receiving blood products or a poorly placed hemorrhage cart.
Drawing an analogy to the extensive time pilots spend in flight simulators, Dr. Mann and her coauthors noted that “because severe maternity-related events are rare and often unpredictable, and because members of the care team may not know each other, it is important to train for low-probability but high-risk events.”
Using the Maternal Health Compact will help ensure that lower-resource hospitals have a relationship in place with a facility that can provide a higher level of maternal care when needed, they said.
This fourth action means that there’s a connection that “can be activated by lower-resource hospitals to get immediate consultation in the event of an unexpected obstetrical emergency whose care demands exceed their resources,” said Dr. Mann and her coauthors. When transport is necessary, it too can be facilitated if a compact is already in place.
The final, broader, recommendation from the obstetricians is that ACOG and AAFP collaborate “on an additional year of comprehensive training for family medicine physicians who are considering practicing obstetrics in rural areas.” The fourth year of training for these family physicians could help address widespread shortages of obstetricians and midwives in rural communities, Dr. Mann and her coauthors wrote. They observed that “pregnant women who live in rural areas may need to travel hundreds of miles to obtain routine prenatal care or consultation with an obstetrical specialist.”
Dr. Cullen, whose practice is in Valdez, Alaska, said he happily reciprocates the desire for collaboration. In his inaugural blog post after assuming the AAFP presidency in October, 2018, he extended warm thanks to his obstetrician and perinatologist colleagues. “The relationship between family physicians and obstetricians is vital in rural communities like mine. The training I received has saved lives and prevented catastrophe,” he wrote.
At the same time, Dr. Cullen said that he believes family physicians are the best hope for quality obstetrical care in rural communities. Dr. Cullen’s own training, he said, was structured to involve significant obstetric experience with obstetrician mentorship. “A 3-year residency left me very comfortable with fairly sophisticated obstetric management at graduation,” he added.
In his practice, Dr. Cullen said, a family physician hired a decade ago after a 3-year residency came with excellent obstetric skills, which have been further honed during the succeeding years of rural practice. During a 3-year residency, “family physicians receive training and demonstrate the skills and competencies required to deliver high-quality maternity care in any community, including those in rural settings,” he said in his statement.
“The bigger issue is really the closure of obstetric units in rural hospitals,” said Dr. Cullen. He pointed out that although obstetric services may have left a community, that rural hospital will still have miscarrying patients with hemorrhage, patients in preterm labor, and other obstetric emergencies arriving at the doorstep. These and other instances often “represent true emergencies without possibility of transfer, requiring immediate and effective response,” he wrote.
“We would encourage the authors to ensure an equal focus on improving care at all levels and in all hospitals, as well as relying on transfer as appropriate,” Dr. Cullen said in his statement.
Such mutual support can be bolstered by new technology, wrote Dr. Mann and her coauthors, because “telehealth and collaborations and consultation with clinics and regional hospitals can help increase the availability of maternity care in the United States.”
For Dr. Cullen also, the way forward is together. In his blog, he wrote: “As family physicians, we can only deliver obstetrical care to our patients with the cooperation of obstetricians and perinatologists. Conversely, obstetricians can only improve maternal and infant mortality rates, especially in rural areas, with the help of family physicians.”
SOURCE: Mann S et al. N Engl J Med 2018;379:1689-91.
rate in the United States, according to a new perspective from leading obstetricians published in the New England Journal of Medicine.
The authors, including Kimberlee McKay, MD, president of the American College of Obstetricians and Gynecologists (ACOG), also call for collaboration with family physicians to increase access to obstetric care in rural areas.
The president of the American Academy of Family Physicians (AAFP), John S. Cullen, MD, in a separate statement, welcomed the opportunity for collaboration in addressing the maternal mortality crisis. However, some distance still lies between the finer points of how the two organizations see family physicians helping curb the crisis.
“Women in the United States are more likely to die from childbirth- or pregnancy-related causes than women in any other high-income country, and black women die at a rate three to four times that of white women,” noted Susan Mann, MD, along with her coauthors of the obstetric perspective, calling increasing maternal mortality a “tragedy.”
In an interview, Dr. Cullen concurred, calling the current situation “unconscionable.” One of the primary reasons he sought AAFP leadership, he said, was to bring experiences learned during his 25 years of obstetric practice in rural Alaska to bear on the current crisis.
A set of maternal care bundles created by the Alliance for Innovation on Maternal Health (AIM) provides the framework for the first action recommended by Dr. Mann and her coauthors. The AIM bundles focus on protocols that improve readiness, recognition, response, and reporting in maternal care. The protocols are institution specific. For example, the authors noted, antihypertensive medications should be readily available around the clock, because not all facilities will have a pharmacist in-house at all times, and hypertensive emergencies are among the gravest obstetric complications.
“Although management may vary from institution to institution, each unit can be required to demonstrate readiness to deal with emergencies 24/7,” said Dr. Mann, a physician in private practice in Boston, and her coauthors.
The second recommended action revolves around multidisciplinary staff meetings to perform individual assessments for each woman’s obstetric risk factors. These huddles should include assessing hemorrhage risk by using the California Maternal Quality Care Collaborative guidelines, and briefings with the full care team to “develop shared understandings of the patient and the procedure” before elective or nonurgent cesarean deliveries, said Dr. Mann and her colleagues. Patients should be informed of any safety concerns, and caregivers should use shared decision-making moving forward.
“Approximately 50% of U.S. hospitals provide care for three or fewer deliveries per day, but the need to identify women at risk is equally important for these small obstetrics services,” Dr. Mann and her coauthors noted.
Third, simulation of obstetric emergencies lets all members of the team understand the speed at which decisions must be made and actions taken when minutes, or even seconds, count. Dr. Mann and her coauthors pointed out that logistics problems come out during a well-run simulation, giving such examples as a lag in receiving blood products or a poorly placed hemorrhage cart.
Drawing an analogy to the extensive time pilots spend in flight simulators, Dr. Mann and her coauthors noted that “because severe maternity-related events are rare and often unpredictable, and because members of the care team may not know each other, it is important to train for low-probability but high-risk events.”
Using the Maternal Health Compact will help ensure that lower-resource hospitals have a relationship in place with a facility that can provide a higher level of maternal care when needed, they said.
This fourth action means that there’s a connection that “can be activated by lower-resource hospitals to get immediate consultation in the event of an unexpected obstetrical emergency whose care demands exceed their resources,” said Dr. Mann and her coauthors. When transport is necessary, it too can be facilitated if a compact is already in place.
The final, broader, recommendation from the obstetricians is that ACOG and AAFP collaborate “on an additional year of comprehensive training for family medicine physicians who are considering practicing obstetrics in rural areas.” The fourth year of training for these family physicians could help address widespread shortages of obstetricians and midwives in rural communities, Dr. Mann and her coauthors wrote. They observed that “pregnant women who live in rural areas may need to travel hundreds of miles to obtain routine prenatal care or consultation with an obstetrical specialist.”
Dr. Cullen, whose practice is in Valdez, Alaska, said he happily reciprocates the desire for collaboration. In his inaugural blog post after assuming the AAFP presidency in October, 2018, he extended warm thanks to his obstetrician and perinatologist colleagues. “The relationship between family physicians and obstetricians is vital in rural communities like mine. The training I received has saved lives and prevented catastrophe,” he wrote.
At the same time, Dr. Cullen said that he believes family physicians are the best hope for quality obstetrical care in rural communities. Dr. Cullen’s own training, he said, was structured to involve significant obstetric experience with obstetrician mentorship. “A 3-year residency left me very comfortable with fairly sophisticated obstetric management at graduation,” he added.
In his practice, Dr. Cullen said, a family physician hired a decade ago after a 3-year residency came with excellent obstetric skills, which have been further honed during the succeeding years of rural practice. During a 3-year residency, “family physicians receive training and demonstrate the skills and competencies required to deliver high-quality maternity care in any community, including those in rural settings,” he said in his statement.
“The bigger issue is really the closure of obstetric units in rural hospitals,” said Dr. Cullen. He pointed out that although obstetric services may have left a community, that rural hospital will still have miscarrying patients with hemorrhage, patients in preterm labor, and other obstetric emergencies arriving at the doorstep. These and other instances often “represent true emergencies without possibility of transfer, requiring immediate and effective response,” he wrote.
“We would encourage the authors to ensure an equal focus on improving care at all levels and in all hospitals, as well as relying on transfer as appropriate,” Dr. Cullen said in his statement.
Such mutual support can be bolstered by new technology, wrote Dr. Mann and her coauthors, because “telehealth and collaborations and consultation with clinics and regional hospitals can help increase the availability of maternity care in the United States.”
For Dr. Cullen also, the way forward is together. In his blog, he wrote: “As family physicians, we can only deliver obstetrical care to our patients with the cooperation of obstetricians and perinatologists. Conversely, obstetricians can only improve maternal and infant mortality rates, especially in rural areas, with the help of family physicians.”
SOURCE: Mann S et al. N Engl J Med 2018;379:1689-91.
rate in the United States, according to a new perspective from leading obstetricians published in the New England Journal of Medicine.
The authors, including Kimberlee McKay, MD, president of the American College of Obstetricians and Gynecologists (ACOG), also call for collaboration with family physicians to increase access to obstetric care in rural areas.
The president of the American Academy of Family Physicians (AAFP), John S. Cullen, MD, in a separate statement, welcomed the opportunity for collaboration in addressing the maternal mortality crisis. However, some distance still lies between the finer points of how the two organizations see family physicians helping curb the crisis.
“Women in the United States are more likely to die from childbirth- or pregnancy-related causes than women in any other high-income country, and black women die at a rate three to four times that of white women,” noted Susan Mann, MD, along with her coauthors of the obstetric perspective, calling increasing maternal mortality a “tragedy.”
In an interview, Dr. Cullen concurred, calling the current situation “unconscionable.” One of the primary reasons he sought AAFP leadership, he said, was to bring experiences learned during his 25 years of obstetric practice in rural Alaska to bear on the current crisis.
A set of maternal care bundles created by the Alliance for Innovation on Maternal Health (AIM) provides the framework for the first action recommended by Dr. Mann and her coauthors. The AIM bundles focus on protocols that improve readiness, recognition, response, and reporting in maternal care. The protocols are institution specific. For example, the authors noted, antihypertensive medications should be readily available around the clock, because not all facilities will have a pharmacist in-house at all times, and hypertensive emergencies are among the gravest obstetric complications.
“Although management may vary from institution to institution, each unit can be required to demonstrate readiness to deal with emergencies 24/7,” said Dr. Mann, a physician in private practice in Boston, and her coauthors.
The second recommended action revolves around multidisciplinary staff meetings to perform individual assessments for each woman’s obstetric risk factors. These huddles should include assessing hemorrhage risk by using the California Maternal Quality Care Collaborative guidelines, and briefings with the full care team to “develop shared understandings of the patient and the procedure” before elective or nonurgent cesarean deliveries, said Dr. Mann and her colleagues. Patients should be informed of any safety concerns, and caregivers should use shared decision-making moving forward.
“Approximately 50% of U.S. hospitals provide care for three or fewer deliveries per day, but the need to identify women at risk is equally important for these small obstetrics services,” Dr. Mann and her coauthors noted.
Third, simulation of obstetric emergencies lets all members of the team understand the speed at which decisions must be made and actions taken when minutes, or even seconds, count. Dr. Mann and her coauthors pointed out that logistics problems come out during a well-run simulation, giving such examples as a lag in receiving blood products or a poorly placed hemorrhage cart.
Drawing an analogy to the extensive time pilots spend in flight simulators, Dr. Mann and her coauthors noted that “because severe maternity-related events are rare and often unpredictable, and because members of the care team may not know each other, it is important to train for low-probability but high-risk events.”
Using the Maternal Health Compact will help ensure that lower-resource hospitals have a relationship in place with a facility that can provide a higher level of maternal care when needed, they said.
This fourth action means that there’s a connection that “can be activated by lower-resource hospitals to get immediate consultation in the event of an unexpected obstetrical emergency whose care demands exceed their resources,” said Dr. Mann and her coauthors. When transport is necessary, it too can be facilitated if a compact is already in place.
The final, broader, recommendation from the obstetricians is that ACOG and AAFP collaborate “on an additional year of comprehensive training for family medicine physicians who are considering practicing obstetrics in rural areas.” The fourth year of training for these family physicians could help address widespread shortages of obstetricians and midwives in rural communities, Dr. Mann and her coauthors wrote. They observed that “pregnant women who live in rural areas may need to travel hundreds of miles to obtain routine prenatal care or consultation with an obstetrical specialist.”
Dr. Cullen, whose practice is in Valdez, Alaska, said he happily reciprocates the desire for collaboration. In his inaugural blog post after assuming the AAFP presidency in October, 2018, he extended warm thanks to his obstetrician and perinatologist colleagues. “The relationship between family physicians and obstetricians is vital in rural communities like mine. The training I received has saved lives and prevented catastrophe,” he wrote.
At the same time, Dr. Cullen said that he believes family physicians are the best hope for quality obstetrical care in rural communities. Dr. Cullen’s own training, he said, was structured to involve significant obstetric experience with obstetrician mentorship. “A 3-year residency left me very comfortable with fairly sophisticated obstetric management at graduation,” he added.
In his practice, Dr. Cullen said, a family physician hired a decade ago after a 3-year residency came with excellent obstetric skills, which have been further honed during the succeeding years of rural practice. During a 3-year residency, “family physicians receive training and demonstrate the skills and competencies required to deliver high-quality maternity care in any community, including those in rural settings,” he said in his statement.
“The bigger issue is really the closure of obstetric units in rural hospitals,” said Dr. Cullen. He pointed out that although obstetric services may have left a community, that rural hospital will still have miscarrying patients with hemorrhage, patients in preterm labor, and other obstetric emergencies arriving at the doorstep. These and other instances often “represent true emergencies without possibility of transfer, requiring immediate and effective response,” he wrote.
“We would encourage the authors to ensure an equal focus on improving care at all levels and in all hospitals, as well as relying on transfer as appropriate,” Dr. Cullen said in his statement.
Such mutual support can be bolstered by new technology, wrote Dr. Mann and her coauthors, because “telehealth and collaborations and consultation with clinics and regional hospitals can help increase the availability of maternity care in the United States.”
For Dr. Cullen also, the way forward is together. In his blog, he wrote: “As family physicians, we can only deliver obstetrical care to our patients with the cooperation of obstetricians and perinatologists. Conversely, obstetricians can only improve maternal and infant mortality rates, especially in rural areas, with the help of family physicians.”
SOURCE: Mann S et al. N Engl J Med 2018;379:1689-91.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Medical calculator apps allow point of care, rapid decision-making
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
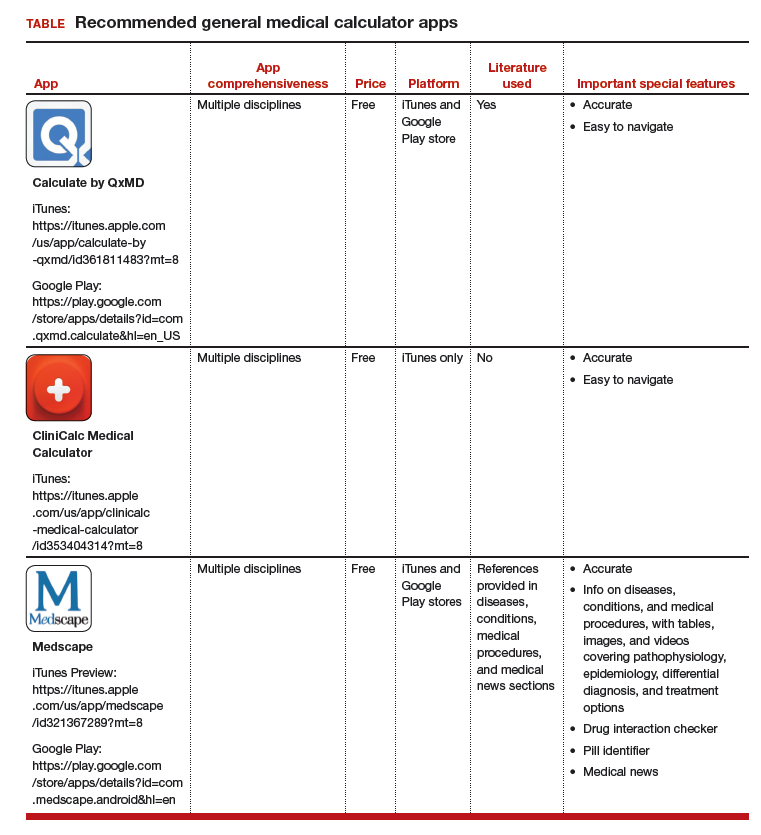
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
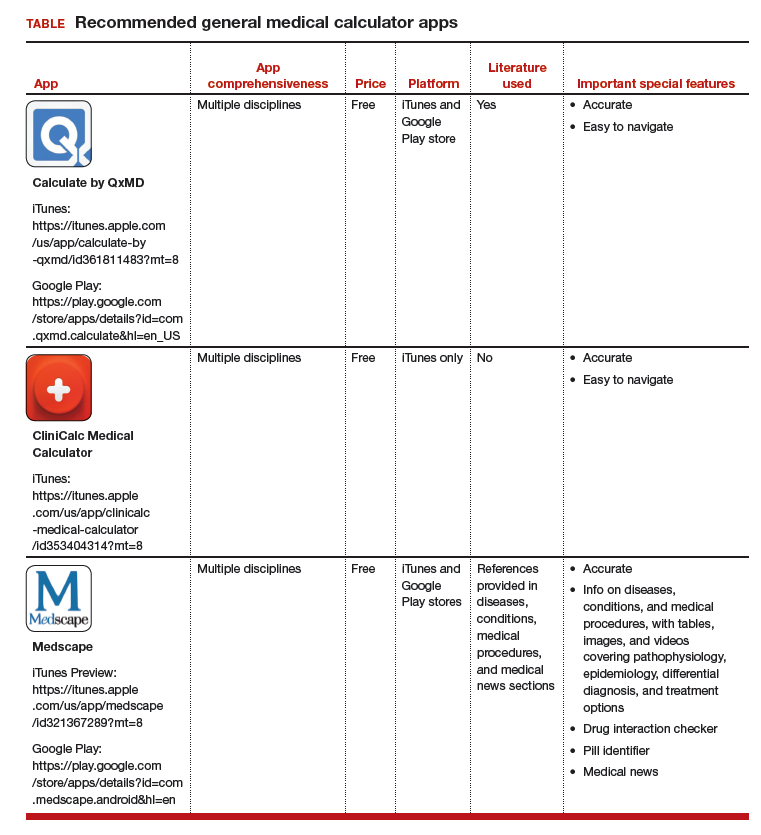
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The most useful applications (apps) for health care professionals and students? Medical calculator apps (along with drug reference and disease diagnosis apps), according to surveys of clinicians and students.1,2 The utility of calculator apps to these groups is not surprising; calculator apps fall in the category of clinical decision-making apps, which also includes decision support systems, clinical treatment guidelines, disease diagnosis aids, differential diagnosis aids, laboratory test ordering, laboratory test interpretation, and medical exams.3 Calculator apps obviously save time as most health care providers have not memorized the many medical formulas and do not have computational speed. I have previously discussed other, more ObGyn-specific calculators, such as due date calculators.4,5 In this App Review column, however, I would like to highlight 3 general calculator apps: Calculate by QxMD, CliniCalc Medical Calculator, and Medscape. Researchers found all 3 apps 100% accurate and contained the most functions desired by internists.6 The apps are available at no cost and include many unique calculators. My colleagues and I actually used Calculate by QxMD to verify calculations in a previous study.7
A clinical example for how to apply calculators in practice is as follows: A multiparous patient at term has undergone an unscheduled cesarean delivery for arrest of dilation and intra-amniotic infection. You need to decide if the patient requires anti‑coagulants for deep venous thrombosis (DVT) prophylaxis and her necessary daily dose for gentamicin for postpartum infection prophylaxis. You can use Medscape’s body mass index (BMI) calculator to find out that this patient’s BMI is 45 kg/m2 and that DVT prophylaxis is in fact indicated. You also can use QxMD’s ideal body weight calculator to get the patient’s weight and determine the appropriate daily dose for gentamicin.
The TABLE provides more information on the apps, with its inclusions based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).7
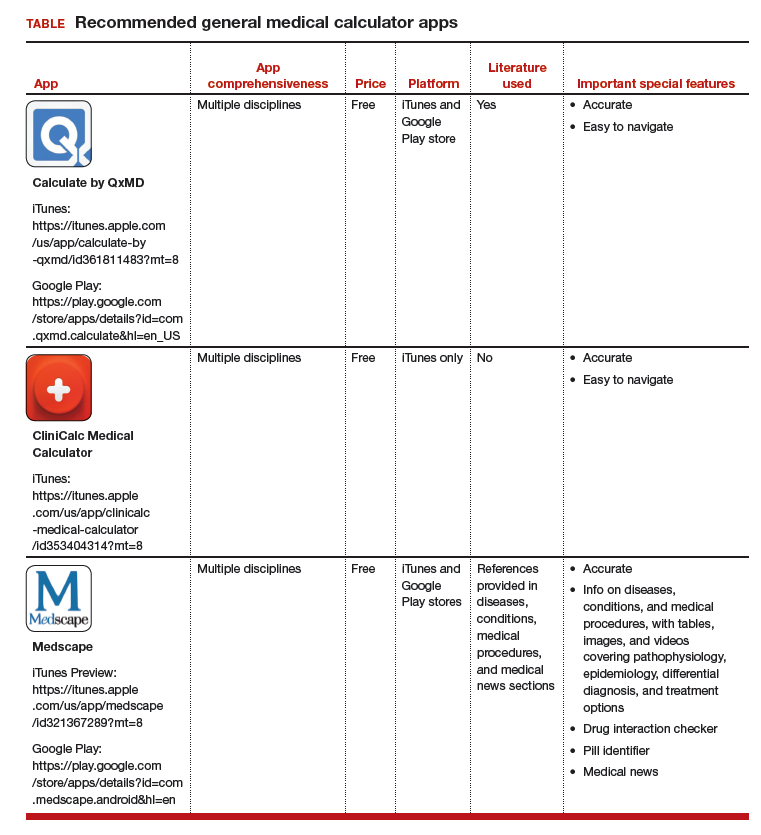
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
1. Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67.
2. Payne KB, Wharrad H, Watts K. Smartphone and medical related App use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
3. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356-364.
4. Chen KT. Three good apps for calculating the date of delivery. OBG Manag. 2017;29:45-46.
5. Chen KT. ACOG app and applets: tools to augment your practice. OBG Manag. 2018;30:41-42.
6. Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
7. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.















