User login
Obstetric trauma rates show long-term decline
Obstetric trauma rates have dropped since 2000 for vaginal deliveries both with and without instrument assistance, but assisted deliveries are still six times more likely to result in injuries, according to the Agency for Healthcare Research and Quality.
In 2014, the trauma rate for unassisted vaginal deliveries was 19 per 1,000, a drop of 51% from the rate of 39 per 1,000 deliveries in 2000. 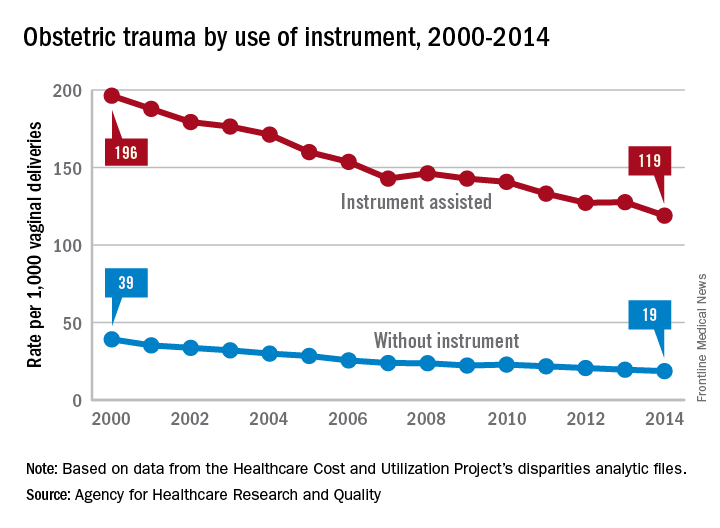
For this analysis, injuries were defined as third- or fourth-degree lacerations of the perineum; rates were adjusted by age using hospitalizations for 2010 as the standard population.
Obstetric trauma rates have dropped since 2000 for vaginal deliveries both with and without instrument assistance, but assisted deliveries are still six times more likely to result in injuries, according to the Agency for Healthcare Research and Quality.
In 2014, the trauma rate for unassisted vaginal deliveries was 19 per 1,000, a drop of 51% from the rate of 39 per 1,000 deliveries in 2000. 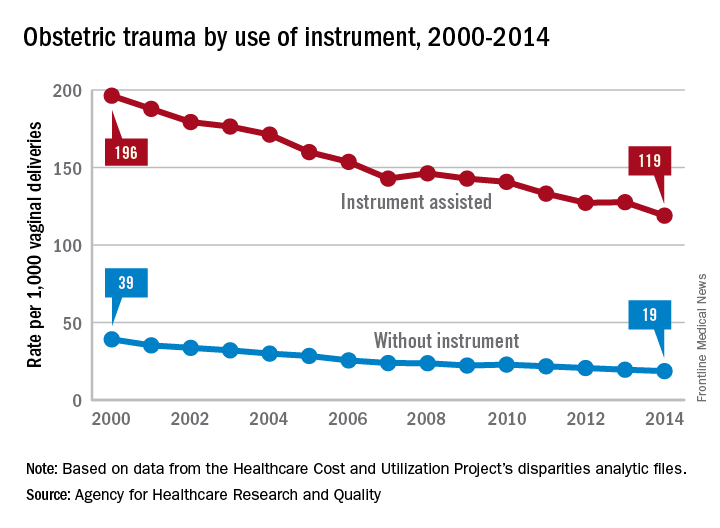
For this analysis, injuries were defined as third- or fourth-degree lacerations of the perineum; rates were adjusted by age using hospitalizations for 2010 as the standard population.
Obstetric trauma rates have dropped since 2000 for vaginal deliveries both with and without instrument assistance, but assisted deliveries are still six times more likely to result in injuries, according to the Agency for Healthcare Research and Quality.
In 2014, the trauma rate for unassisted vaginal deliveries was 19 per 1,000, a drop of 51% from the rate of 39 per 1,000 deliveries in 2000. 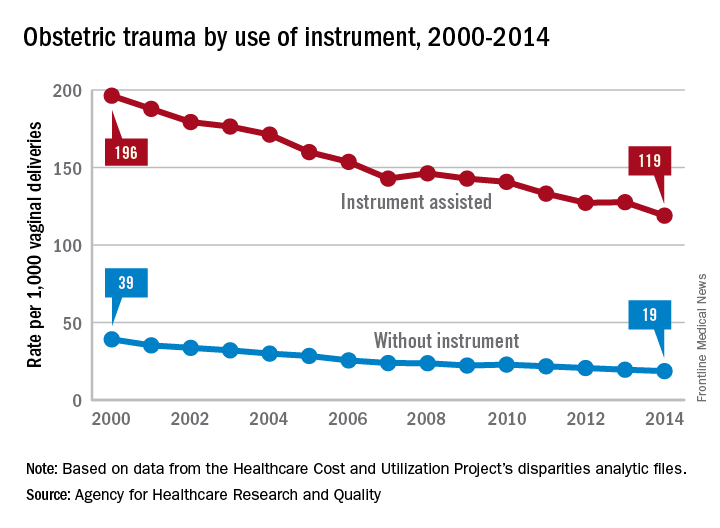
For this analysis, injuries were defined as third- or fourth-degree lacerations of the perineum; rates were adjusted by age using hospitalizations for 2010 as the standard population.
Cerebral palsy rate down in children born very or moderately preterm
, even in children who were born moderately preterm.
The researchers gathered data for cerebral palsy from the medical questionnaire, including information on head control, sitting, standing, walking, and quality of gait; trunk and limb tone; and any abnormal neurologic signs. Development was assessed using the second version of the 24-month Ages and Stages Questionnaire (ASQ), which is completed by parents.
Of 4,199 neonates born between 22 and 34 weeks’ gestation in 2011 enrolled in the EPIPAGE-2 study who lived until a median of 24.2 months corrected age, the rate of cerebral palsy dropped from 7% to 4% in those born between 24-26 and 27-31 weeks’ gestation, reported Véronique Pierrat, MD, PhD, of the Epidemiology and Biostatistics Sorbonne Paris Cité Research Center, INSERM, in Paris, and her associates. At 32-34 weeks’ gestation, the cerebral palsy rate was 1%. Only one child born at 22-23 weeks’ gestation lived beyond the neonatal period. Fewer than 1% of the children overall had severe auditory or visual impairment.
ASQ analysis was considered for 2,506 children, after excluding children with cerebral palsy, deafness or blindness, or severe congenital brain malformations. ASQ scores were below threshold in 50%, 41%, and 36% of children born at 24-26, 27-31, and 32-34 weeks’ gestation, respectively. “The domains most frequently scoring below threshold were communication and personal-social in all gestational age groups. Proportions of children scoring below the threshold in either of these domains decreased with increasing gestational age but still were 18% and 13%, respectively, at 32-34 weeks’ gestation,” the investigators said.
Only 1% or fewer of the children in this cohort had severe gastrointestinal or respiratory disabilities.
In a comparison of 1997 data and this 2011 data after adjustment for baseline characteristics in children born at 22-31 weeks’ gestation, survival increased by a mean 6% , and survival without neuromotor or sensory impairment by 7%; in children born at 24-31 weeks’ gestation, cerebral palsy decreased by a mean 3%. No statistically significant changes were found between the two periods for survival, survival without neuromotor or sensory disabilities, and rates of cerebral palsy in children born at 24 weeks’ gestation, but “noticeable improvements were seen at 25-26 weeks and, to a lesser extent, at 27-31 weeks,” Dr. Pierrat and her associates said. At 32-34 weeks’ gestation, the cerebral palsy rate dropped by 3%, but survival and survival without severe neuromotor or sensory impairment were similar between the two time periods.
In regard to the 2011 data, “the proportion of infants at risk of developmental delay was high, even for those born at 32-34 weeks’ gestation. Our results invite questioning perinatal strategies in France, and in countries with similar recommendations. However, improving outcomes at extremely low gestational age requires a complex change in philosophy of care and close cooperation not only between obstetricians and neonatologists, but also developmental specialists, parent associations, and policy makers,” Dr. Pierrat and her associates concluded.
The investigators said they had no relevant financial disclosures. The study was funded by the French Institute of Public Health Research/Institute of Public Health and several of its partners, the PREMUP Foundation, Fondation de France, and Fondation pour la Recherche Médicale.
, even in children who were born moderately preterm.
The researchers gathered data for cerebral palsy from the medical questionnaire, including information on head control, sitting, standing, walking, and quality of gait; trunk and limb tone; and any abnormal neurologic signs. Development was assessed using the second version of the 24-month Ages and Stages Questionnaire (ASQ), which is completed by parents.
Of 4,199 neonates born between 22 and 34 weeks’ gestation in 2011 enrolled in the EPIPAGE-2 study who lived until a median of 24.2 months corrected age, the rate of cerebral palsy dropped from 7% to 4% in those born between 24-26 and 27-31 weeks’ gestation, reported Véronique Pierrat, MD, PhD, of the Epidemiology and Biostatistics Sorbonne Paris Cité Research Center, INSERM, in Paris, and her associates. At 32-34 weeks’ gestation, the cerebral palsy rate was 1%. Only one child born at 22-23 weeks’ gestation lived beyond the neonatal period. Fewer than 1% of the children overall had severe auditory or visual impairment.
ASQ analysis was considered for 2,506 children, after excluding children with cerebral palsy, deafness or blindness, or severe congenital brain malformations. ASQ scores were below threshold in 50%, 41%, and 36% of children born at 24-26, 27-31, and 32-34 weeks’ gestation, respectively. “The domains most frequently scoring below threshold were communication and personal-social in all gestational age groups. Proportions of children scoring below the threshold in either of these domains decreased with increasing gestational age but still were 18% and 13%, respectively, at 32-34 weeks’ gestation,” the investigators said.
Only 1% or fewer of the children in this cohort had severe gastrointestinal or respiratory disabilities.
In a comparison of 1997 data and this 2011 data after adjustment for baseline characteristics in children born at 22-31 weeks’ gestation, survival increased by a mean 6% , and survival without neuromotor or sensory impairment by 7%; in children born at 24-31 weeks’ gestation, cerebral palsy decreased by a mean 3%. No statistically significant changes were found between the two periods for survival, survival without neuromotor or sensory disabilities, and rates of cerebral palsy in children born at 24 weeks’ gestation, but “noticeable improvements were seen at 25-26 weeks and, to a lesser extent, at 27-31 weeks,” Dr. Pierrat and her associates said. At 32-34 weeks’ gestation, the cerebral palsy rate dropped by 3%, but survival and survival without severe neuromotor or sensory impairment were similar between the two time periods.
In regard to the 2011 data, “the proportion of infants at risk of developmental delay was high, even for those born at 32-34 weeks’ gestation. Our results invite questioning perinatal strategies in France, and in countries with similar recommendations. However, improving outcomes at extremely low gestational age requires a complex change in philosophy of care and close cooperation not only between obstetricians and neonatologists, but also developmental specialists, parent associations, and policy makers,” Dr. Pierrat and her associates concluded.
The investigators said they had no relevant financial disclosures. The study was funded by the French Institute of Public Health Research/Institute of Public Health and several of its partners, the PREMUP Foundation, Fondation de France, and Fondation pour la Recherche Médicale.
, even in children who were born moderately preterm.
The researchers gathered data for cerebral palsy from the medical questionnaire, including information on head control, sitting, standing, walking, and quality of gait; trunk and limb tone; and any abnormal neurologic signs. Development was assessed using the second version of the 24-month Ages and Stages Questionnaire (ASQ), which is completed by parents.
Of 4,199 neonates born between 22 and 34 weeks’ gestation in 2011 enrolled in the EPIPAGE-2 study who lived until a median of 24.2 months corrected age, the rate of cerebral palsy dropped from 7% to 4% in those born between 24-26 and 27-31 weeks’ gestation, reported Véronique Pierrat, MD, PhD, of the Epidemiology and Biostatistics Sorbonne Paris Cité Research Center, INSERM, in Paris, and her associates. At 32-34 weeks’ gestation, the cerebral palsy rate was 1%. Only one child born at 22-23 weeks’ gestation lived beyond the neonatal period. Fewer than 1% of the children overall had severe auditory or visual impairment.
ASQ analysis was considered for 2,506 children, after excluding children with cerebral palsy, deafness or blindness, or severe congenital brain malformations. ASQ scores were below threshold in 50%, 41%, and 36% of children born at 24-26, 27-31, and 32-34 weeks’ gestation, respectively. “The domains most frequently scoring below threshold were communication and personal-social in all gestational age groups. Proportions of children scoring below the threshold in either of these domains decreased with increasing gestational age but still were 18% and 13%, respectively, at 32-34 weeks’ gestation,” the investigators said.
Only 1% or fewer of the children in this cohort had severe gastrointestinal or respiratory disabilities.
In a comparison of 1997 data and this 2011 data after adjustment for baseline characteristics in children born at 22-31 weeks’ gestation, survival increased by a mean 6% , and survival without neuromotor or sensory impairment by 7%; in children born at 24-31 weeks’ gestation, cerebral palsy decreased by a mean 3%. No statistically significant changes were found between the two periods for survival, survival without neuromotor or sensory disabilities, and rates of cerebral palsy in children born at 24 weeks’ gestation, but “noticeable improvements were seen at 25-26 weeks and, to a lesser extent, at 27-31 weeks,” Dr. Pierrat and her associates said. At 32-34 weeks’ gestation, the cerebral palsy rate dropped by 3%, but survival and survival without severe neuromotor or sensory impairment were similar between the two time periods.
In regard to the 2011 data, “the proportion of infants at risk of developmental delay was high, even for those born at 32-34 weeks’ gestation. Our results invite questioning perinatal strategies in France, and in countries with similar recommendations. However, improving outcomes at extremely low gestational age requires a complex change in philosophy of care and close cooperation not only between obstetricians and neonatologists, but also developmental specialists, parent associations, and policy makers,” Dr. Pierrat and her associates concluded.
The investigators said they had no relevant financial disclosures. The study was funded by the French Institute of Public Health Research/Institute of Public Health and several of its partners, the PREMUP Foundation, Fondation de France, and Fondation pour la Recherche Médicale.
FROM BMJ
Key clinical point: Cerebral palsy rates are down in children born very and moderately preterm, but the risk of developmental delay remains high.
Major finding: ASQ scores were below threshold in 50%, 41%, and 36% of children born at 24-26, 27-31, and 32-34 weeks’ gestation, respectively.
Data source: A national population study of 4,199 French neonates born between 22 and 34 weeks’ gestation in 2011.
Disclosures: The investigators said they had no relevant financial disclosures. The study was funded by the French Institute of Public Health Research/Institute of Public Health and several of its partners, the PREMUP Foundation, Fondation de France, and Fondation pour la Recherche Médicale.
AMA’s stance on choline, prenatal vitamins could bring ‘staggering’ results
For quite some time now, I’ve been urging my colleagues to follow the science on the powerful impact of choline on the brain.
In May 2017, based on studies using genetically altered mice that show the developmental changes of Down syndrome and Alzheimer’s disease at 6 months, I raised the question of whether prenatal choline could lead to the prevention of Alzheimer’s.
Thanks to the leadership of Niva Lubin-Johnson, MD, now president-elect of the National Medical Association, while a member and immediate past chair of the American Medical Association’s minority affairs section governing council*, the AMA ’s delegates passed a resolution to support an increase in choline in prenatal vitamins.
If the prenatal vitamin companies take the AMA’s resolution to heart and put more choline in their prenatal vitamins or if physicians in the United States pay attention to the AMA’s action and recommend pregnant women ensure they get adequate choline in their diets, the benefit to Americans’ public health could be staggering. Currently, it is known that choline deficiency – usually brought about by fetal alcohol exposure – is a public health problem, and choline deficiency is the leading preventable cause of intellectual disability. Public health efforts aimed at preventing intellectual disabilities from fetal alcohol exposure are designed to warn women about the risks of drinking during pregnancy; while this effort is commendable, it does not solve a very common problem – namely, women’s engaging in social drinking before they realize they are pregnant. (Psychiatric Serv. 2015 66[5]:539-42).
The late Julius B. Richmond, MD, former director of the Institute for Juvenile Research, surgeon general under former President Jimmy Carter, and one of the founders of Head Start under former President Lyndon B. Johnson, used to say that, in order to institutionalize a public policy, you need a solid scientific basis for the policy, a mechanism to actualize the policy, and the “political will” to do so. The AMA’s recommendation has the Institute of Medicine’s science behind it, so putting choline in prenatal vitamins or having physicians recommend that pregnant women get adequate doses of choline should be pretty easy to actualize. The political will to do this extremely important, biotechnical preventive intervention should be a no-brainer.
Should this AMA recommendation gain the traction it deserves, the American people might see a substantial decrease in the prevalence of premature and low-birth-weight infants, intellectual disability, ADHD, speech and language difficulties, epilepsy, heart defects, schizophrenia, Alzheimer’s disease, depression, school failure, juvenile delinquency, violence, and suicide – all of which seem to be tied to choline deficiency.
*This story was updated August 17, 2017.
For quite some time now, I’ve been urging my colleagues to follow the science on the powerful impact of choline on the brain.
In May 2017, based on studies using genetically altered mice that show the developmental changes of Down syndrome and Alzheimer’s disease at 6 months, I raised the question of whether prenatal choline could lead to the prevention of Alzheimer’s.
Thanks to the leadership of Niva Lubin-Johnson, MD, now president-elect of the National Medical Association, while a member and immediate past chair of the American Medical Association’s minority affairs section governing council*, the AMA ’s delegates passed a resolution to support an increase in choline in prenatal vitamins.
If the prenatal vitamin companies take the AMA’s resolution to heart and put more choline in their prenatal vitamins or if physicians in the United States pay attention to the AMA’s action and recommend pregnant women ensure they get adequate choline in their diets, the benefit to Americans’ public health could be staggering. Currently, it is known that choline deficiency – usually brought about by fetal alcohol exposure – is a public health problem, and choline deficiency is the leading preventable cause of intellectual disability. Public health efforts aimed at preventing intellectual disabilities from fetal alcohol exposure are designed to warn women about the risks of drinking during pregnancy; while this effort is commendable, it does not solve a very common problem – namely, women’s engaging in social drinking before they realize they are pregnant. (Psychiatric Serv. 2015 66[5]:539-42).
The late Julius B. Richmond, MD, former director of the Institute for Juvenile Research, surgeon general under former President Jimmy Carter, and one of the founders of Head Start under former President Lyndon B. Johnson, used to say that, in order to institutionalize a public policy, you need a solid scientific basis for the policy, a mechanism to actualize the policy, and the “political will” to do so. The AMA’s recommendation has the Institute of Medicine’s science behind it, so putting choline in prenatal vitamins or having physicians recommend that pregnant women get adequate doses of choline should be pretty easy to actualize. The political will to do this extremely important, biotechnical preventive intervention should be a no-brainer.
Should this AMA recommendation gain the traction it deserves, the American people might see a substantial decrease in the prevalence of premature and low-birth-weight infants, intellectual disability, ADHD, speech and language difficulties, epilepsy, heart defects, schizophrenia, Alzheimer’s disease, depression, school failure, juvenile delinquency, violence, and suicide – all of which seem to be tied to choline deficiency.
*This story was updated August 17, 2017.
For quite some time now, I’ve been urging my colleagues to follow the science on the powerful impact of choline on the brain.
In May 2017, based on studies using genetically altered mice that show the developmental changes of Down syndrome and Alzheimer’s disease at 6 months, I raised the question of whether prenatal choline could lead to the prevention of Alzheimer’s.
Thanks to the leadership of Niva Lubin-Johnson, MD, now president-elect of the National Medical Association, while a member and immediate past chair of the American Medical Association’s minority affairs section governing council*, the AMA ’s delegates passed a resolution to support an increase in choline in prenatal vitamins.
If the prenatal vitamin companies take the AMA’s resolution to heart and put more choline in their prenatal vitamins or if physicians in the United States pay attention to the AMA’s action and recommend pregnant women ensure they get adequate choline in their diets, the benefit to Americans’ public health could be staggering. Currently, it is known that choline deficiency – usually brought about by fetal alcohol exposure – is a public health problem, and choline deficiency is the leading preventable cause of intellectual disability. Public health efforts aimed at preventing intellectual disabilities from fetal alcohol exposure are designed to warn women about the risks of drinking during pregnancy; while this effort is commendable, it does not solve a very common problem – namely, women’s engaging in social drinking before they realize they are pregnant. (Psychiatric Serv. 2015 66[5]:539-42).
The late Julius B. Richmond, MD, former director of the Institute for Juvenile Research, surgeon general under former President Jimmy Carter, and one of the founders of Head Start under former President Lyndon B. Johnson, used to say that, in order to institutionalize a public policy, you need a solid scientific basis for the policy, a mechanism to actualize the policy, and the “political will” to do so. The AMA’s recommendation has the Institute of Medicine’s science behind it, so putting choline in prenatal vitamins or having physicians recommend that pregnant women get adequate doses of choline should be pretty easy to actualize. The political will to do this extremely important, biotechnical preventive intervention should be a no-brainer.
Should this AMA recommendation gain the traction it deserves, the American people might see a substantial decrease in the prevalence of premature and low-birth-weight infants, intellectual disability, ADHD, speech and language difficulties, epilepsy, heart defects, schizophrenia, Alzheimer’s disease, depression, school failure, juvenile delinquency, violence, and suicide – all of which seem to be tied to choline deficiency.
*This story was updated August 17, 2017.
Study advances noninvasive prenatal testing for hemophilia
Digital droplet PCR (ddPCR) was an accurate and noninvasive method to detect mutations leading to hemophilia A and B in maternal plasma DNA in 15 at-risk pregnancies of 8 to 42 weeks’ gestation, researchers reported.
Additionally, the researchers showed for the first time that targeted massively parallel sequencing (MPS) accurately detected the clinically important int22h-related inversion mutations in maternal plasma DNA from pregnant hemophilia carriers from three families with the disorder.
As costs of sequencing continue to fall, larger studies of pregnant carriers of F8 int22h-related inversions can help make MPS “an essential part in noninvasive prenatal testing of hemophilia carriers,” Irena Hudecova, PhD, of Li Ka Shing Institute of Health Sciences, Hong Kong, and her associates wrote (Blood. 2017 Jul 20;130[3]:340-7).
Diagnosing hemophilia during pregnancy helps optimize care and allows mothers to make informed decisions about whether to terminate pregnancies. But for male fetuses, invasive testing has been the only option. In a prior small study, researchers used noninvasive microfluidics PCR to detect sequence variants of F8, which encodes factor VIII, and F9, which encodes Factor IX. The assay uses a chip that can accommodate about 9,000 reaction wells, making noninvasive screening much more feasible and affordable. But technical difficulties had precluded detection of int22h-related inversions, the inversion mutations of intron 22 in F8 on chromosome X that affect about half of individuals with severe hemophilia (Blood. 2011 Mar 31;117[13]:3684-91).
For the current study, the researchers first designed family-specific ddPCR assays to test for relevant maternal sequence variants scattered across the F8 and F9 genes. Tests of 15 male singleton fetuses produced three unclassified samples, but no misclassifications.
“Because of the scalability of ddPCR, the protocol performed reliably even in cases with fetal DNA fraction lower than 10%,” the researchers wrote. “When an unclassified result is encountered, one either performs more digital analyses on the sample to accumulate more data points, or when the sample is consumed, one may resort to an additional blood draw, possibly at a later gestational age with higher fetal DNA fraction.”
Next, the investigators used MPS to create detailed fetal haplotype maps of the 7.6-Md region of F8 where int22h-related inversions occur. This approach yielded an “accurate and robust measurement of maternally inherited fetal haplotypes,” they wrote. “Our data suggest it is feasible to apply targeted MPS to interrogate maternally inherited F8 int22h-related inversions, whereas ddPCR [is] an affordable approach for the identification of F8 and F9 sequence variants in maternal plasma.”
The study was funded by the Research Grants Council of the Hong Kong SAR Government and the Vice Chancellor’s One-Off Discretionary Fund of The Chinese University of Hong Kong. Dr. Hudecova reported having no financial disclosures. Several coauthors disclosed patents for plasma nucleic acid analysis and ties to Sequenom, Illumina, Xcelom, and Cirina.
The use of digital droplet PCR for prenatal diagnosis of hemophilia is a major improvement over current invasive methods, such as chorionic villus sampling, amniocentesis, and cordocentesis.
Knowledge of a hemophilia diagnosis before birth provides an opportunity for early hemostatic intervention before procedures such as circumcision are performed, or to prevent morbidity and mortality by cesarean delivery to reduce the risk of intracranial hemorrhage when the birth of a child with severe hemophilia is anticipated. Prenatal testing is also important to ensure hemostatic support for the mother, for whom it may be necessary to prevent bleeding with perinatal anesthesia and/or postpartum bleeding. These prenatal assays depend on knowledge of the mother’s carrier genotype, which is potentially more accurate than factor levels, which may increase with hormone use or the increasing hormone levels of pregnancy and mask carrier diagnosis.
The development of these assays is timely in view of the ongoing My Life, Our Future (MLOF) genome project in hemophilia and underscores the need for carrier testing and genetic counseling of female members from hemophilia kindreds.
Margaret V. Ragni, MD, is with the University of Pittsburgh Medical Center. She reported having no relevant disclosures. These comments are adapted from an accompanying editorial (Blood. 2017 Jul 20;130[3]:240-1).
The use of digital droplet PCR for prenatal diagnosis of hemophilia is a major improvement over current invasive methods, such as chorionic villus sampling, amniocentesis, and cordocentesis.
Knowledge of a hemophilia diagnosis before birth provides an opportunity for early hemostatic intervention before procedures such as circumcision are performed, or to prevent morbidity and mortality by cesarean delivery to reduce the risk of intracranial hemorrhage when the birth of a child with severe hemophilia is anticipated. Prenatal testing is also important to ensure hemostatic support for the mother, for whom it may be necessary to prevent bleeding with perinatal anesthesia and/or postpartum bleeding. These prenatal assays depend on knowledge of the mother’s carrier genotype, which is potentially more accurate than factor levels, which may increase with hormone use or the increasing hormone levels of pregnancy and mask carrier diagnosis.
The development of these assays is timely in view of the ongoing My Life, Our Future (MLOF) genome project in hemophilia and underscores the need for carrier testing and genetic counseling of female members from hemophilia kindreds.
Margaret V. Ragni, MD, is with the University of Pittsburgh Medical Center. She reported having no relevant disclosures. These comments are adapted from an accompanying editorial (Blood. 2017 Jul 20;130[3]:240-1).
The use of digital droplet PCR for prenatal diagnosis of hemophilia is a major improvement over current invasive methods, such as chorionic villus sampling, amniocentesis, and cordocentesis.
Knowledge of a hemophilia diagnosis before birth provides an opportunity for early hemostatic intervention before procedures such as circumcision are performed, or to prevent morbidity and mortality by cesarean delivery to reduce the risk of intracranial hemorrhage when the birth of a child with severe hemophilia is anticipated. Prenatal testing is also important to ensure hemostatic support for the mother, for whom it may be necessary to prevent bleeding with perinatal anesthesia and/or postpartum bleeding. These prenatal assays depend on knowledge of the mother’s carrier genotype, which is potentially more accurate than factor levels, which may increase with hormone use or the increasing hormone levels of pregnancy and mask carrier diagnosis.
The development of these assays is timely in view of the ongoing My Life, Our Future (MLOF) genome project in hemophilia and underscores the need for carrier testing and genetic counseling of female members from hemophilia kindreds.
Margaret V. Ragni, MD, is with the University of Pittsburgh Medical Center. She reported having no relevant disclosures. These comments are adapted from an accompanying editorial (Blood. 2017 Jul 20;130[3]:240-1).
Digital droplet PCR (ddPCR) was an accurate and noninvasive method to detect mutations leading to hemophilia A and B in maternal plasma DNA in 15 at-risk pregnancies of 8 to 42 weeks’ gestation, researchers reported.
Additionally, the researchers showed for the first time that targeted massively parallel sequencing (MPS) accurately detected the clinically important int22h-related inversion mutations in maternal plasma DNA from pregnant hemophilia carriers from three families with the disorder.
As costs of sequencing continue to fall, larger studies of pregnant carriers of F8 int22h-related inversions can help make MPS “an essential part in noninvasive prenatal testing of hemophilia carriers,” Irena Hudecova, PhD, of Li Ka Shing Institute of Health Sciences, Hong Kong, and her associates wrote (Blood. 2017 Jul 20;130[3]:340-7).
Diagnosing hemophilia during pregnancy helps optimize care and allows mothers to make informed decisions about whether to terminate pregnancies. But for male fetuses, invasive testing has been the only option. In a prior small study, researchers used noninvasive microfluidics PCR to detect sequence variants of F8, which encodes factor VIII, and F9, which encodes Factor IX. The assay uses a chip that can accommodate about 9,000 reaction wells, making noninvasive screening much more feasible and affordable. But technical difficulties had precluded detection of int22h-related inversions, the inversion mutations of intron 22 in F8 on chromosome X that affect about half of individuals with severe hemophilia (Blood. 2011 Mar 31;117[13]:3684-91).
For the current study, the researchers first designed family-specific ddPCR assays to test for relevant maternal sequence variants scattered across the F8 and F9 genes. Tests of 15 male singleton fetuses produced three unclassified samples, but no misclassifications.
“Because of the scalability of ddPCR, the protocol performed reliably even in cases with fetal DNA fraction lower than 10%,” the researchers wrote. “When an unclassified result is encountered, one either performs more digital analyses on the sample to accumulate more data points, or when the sample is consumed, one may resort to an additional blood draw, possibly at a later gestational age with higher fetal DNA fraction.”
Next, the investigators used MPS to create detailed fetal haplotype maps of the 7.6-Md region of F8 where int22h-related inversions occur. This approach yielded an “accurate and robust measurement of maternally inherited fetal haplotypes,” they wrote. “Our data suggest it is feasible to apply targeted MPS to interrogate maternally inherited F8 int22h-related inversions, whereas ddPCR [is] an affordable approach for the identification of F8 and F9 sequence variants in maternal plasma.”
The study was funded by the Research Grants Council of the Hong Kong SAR Government and the Vice Chancellor’s One-Off Discretionary Fund of The Chinese University of Hong Kong. Dr. Hudecova reported having no financial disclosures. Several coauthors disclosed patents for plasma nucleic acid analysis and ties to Sequenom, Illumina, Xcelom, and Cirina.
Digital droplet PCR (ddPCR) was an accurate and noninvasive method to detect mutations leading to hemophilia A and B in maternal plasma DNA in 15 at-risk pregnancies of 8 to 42 weeks’ gestation, researchers reported.
Additionally, the researchers showed for the first time that targeted massively parallel sequencing (MPS) accurately detected the clinically important int22h-related inversion mutations in maternal plasma DNA from pregnant hemophilia carriers from three families with the disorder.
As costs of sequencing continue to fall, larger studies of pregnant carriers of F8 int22h-related inversions can help make MPS “an essential part in noninvasive prenatal testing of hemophilia carriers,” Irena Hudecova, PhD, of Li Ka Shing Institute of Health Sciences, Hong Kong, and her associates wrote (Blood. 2017 Jul 20;130[3]:340-7).
Diagnosing hemophilia during pregnancy helps optimize care and allows mothers to make informed decisions about whether to terminate pregnancies. But for male fetuses, invasive testing has been the only option. In a prior small study, researchers used noninvasive microfluidics PCR to detect sequence variants of F8, which encodes factor VIII, and F9, which encodes Factor IX. The assay uses a chip that can accommodate about 9,000 reaction wells, making noninvasive screening much more feasible and affordable. But technical difficulties had precluded detection of int22h-related inversions, the inversion mutations of intron 22 in F8 on chromosome X that affect about half of individuals with severe hemophilia (Blood. 2011 Mar 31;117[13]:3684-91).
For the current study, the researchers first designed family-specific ddPCR assays to test for relevant maternal sequence variants scattered across the F8 and F9 genes. Tests of 15 male singleton fetuses produced three unclassified samples, but no misclassifications.
“Because of the scalability of ddPCR, the protocol performed reliably even in cases with fetal DNA fraction lower than 10%,” the researchers wrote. “When an unclassified result is encountered, one either performs more digital analyses on the sample to accumulate more data points, or when the sample is consumed, one may resort to an additional blood draw, possibly at a later gestational age with higher fetal DNA fraction.”
Next, the investigators used MPS to create detailed fetal haplotype maps of the 7.6-Md region of F8 where int22h-related inversions occur. This approach yielded an “accurate and robust measurement of maternally inherited fetal haplotypes,” they wrote. “Our data suggest it is feasible to apply targeted MPS to interrogate maternally inherited F8 int22h-related inversions, whereas ddPCR [is] an affordable approach for the identification of F8 and F9 sequence variants in maternal plasma.”
The study was funded by the Research Grants Council of the Hong Kong SAR Government and the Vice Chancellor’s One-Off Discretionary Fund of The Chinese University of Hong Kong. Dr. Hudecova reported having no financial disclosures. Several coauthors disclosed patents for plasma nucleic acid analysis and ties to Sequenom, Illumina, Xcelom, and Cirina.
FROM BLOOD
Key clinical point:
Major finding: Digital droplet PCR (ddPCR) detected relevant F8 and F9 gene mutations. Targeted massively parallel sequencing (MPS) determined fetal inheritance of F8 int22h-related inversions, which up to half of individuals with severe hemophilia carry.
Data source: ddPCR of 15 singleton male fetuses from at-risk mothers and MPS of the maternal plasma of pregnant carriers from three hemophilia families.
Disclosures: The study was funded by the Research Grants Council of the Hong Kong SAR Government and the Vice Chancellor’s One-Off Discretionary Fund of The Chinese University of Hong Kong. Dr. Hudecova reported having no financial disclosures. Some of the coauthors disclosed patents for plasma nucleic acid analysis and ties to Sequenom, Illumina, Xcelom, and Cirina.
VIDEO: How to catch postpartum necrotizing fasciitis in time
PARK CITY, UTAH – , and it’s easy to misdiagnose at first.
There’s no pus, and the skin can look mostly normal with just a little swelling. The tipoff is pain that seems out of proportion to the clinical signs.
David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, Seattle, knows the infection well. In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, he shared his insights on how physicians can recognize and treat postpartum necrotizing fasciitis in time to limit the damage.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PARK CITY, UTAH – , and it’s easy to misdiagnose at first.
There’s no pus, and the skin can look mostly normal with just a little swelling. The tipoff is pain that seems out of proportion to the clinical signs.
David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, Seattle, knows the infection well. In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, he shared his insights on how physicians can recognize and treat postpartum necrotizing fasciitis in time to limit the damage.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PARK CITY, UTAH – , and it’s easy to misdiagnose at first.
There’s no pus, and the skin can look mostly normal with just a little swelling. The tipoff is pain that seems out of proportion to the clinical signs.
David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, Seattle, knows the infection well. In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, he shared his insights on how physicians can recognize and treat postpartum necrotizing fasciitis in time to limit the damage.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT IDSOG
VIDEO: When to turn to surgery in postpartum uterine infection
PARK CITY, UTAH – When postpartum infections don’t respond to antibiotics, doctors and surgeons need to move fast; surgery – often hysterectomy – is the only thing that will save the woman’s life.
The problem is that with today’s antibiotics, doctors may have never encountered the situation, and sometimes continue to treat with antibiotics until it’s too late.
In Seattle, physicians turn to David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, for advice on when it’s time to give up on antibiotics and go to the OR. It’s a difficult decision, especially when patients are young.
In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Dr. Eschenbach shared what he’s learned from decades of experience in dealing with one of the most devastating postpartum complications.
PARK CITY, UTAH – When postpartum infections don’t respond to antibiotics, doctors and surgeons need to move fast; surgery – often hysterectomy – is the only thing that will save the woman’s life.
The problem is that with today’s antibiotics, doctors may have never encountered the situation, and sometimes continue to treat with antibiotics until it’s too late.
In Seattle, physicians turn to David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, for advice on when it’s time to give up on antibiotics and go to the OR. It’s a difficult decision, especially when patients are young.
In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Dr. Eschenbach shared what he’s learned from decades of experience in dealing with one of the most devastating postpartum complications.
PARK CITY, UTAH – When postpartum infections don’t respond to antibiotics, doctors and surgeons need to move fast; surgery – often hysterectomy – is the only thing that will save the woman’s life.
The problem is that with today’s antibiotics, doctors may have never encountered the situation, and sometimes continue to treat with antibiotics until it’s too late.
In Seattle, physicians turn to David Eschenbach, MD, chair of the department of obstetrics and gynecology at the University of Washington, for advice on when it’s time to give up on antibiotics and go to the OR. It’s a difficult decision, especially when patients are young.
In an interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Dr. Eschenbach shared what he’s learned from decades of experience in dealing with one of the most devastating postpartum complications.
AT IDSOG
Folic acid fortification prevents millions of cases of anemia
DENVER – Mandatory food fortification with folic acid not only prevents neural tube defects, it also prevents an estimated 10 million cases of folate-deficiency anemia annually in the United States, James L. Mills, MD, reported at the annual meeting of the Teratology Society.
“We should have people be thinking about the fact that we’re preventing millions of cases of folate-deficiency anemia, not just thousands of cases of neural tube defects. That point does not seem to have reached the public health community. We need to correct the erroneous assumption that a small group are the only ones benefiting by exposing the entire population to folic acid,” said Dr. Mills, senior investigator at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md.
Extrapolating from the nationally representative survey to the full U.S. population, Dr. Mills estimated that translates to roughly 10 million cases of folate-deficiency anemia prevented per year as a result of the mandatory fortification of grain introduced in 1998. That represents an enormous financial savings in avoided costs of diagnosis and treatment of this disorder.
The Food Fortification Initiative reports that 86 countries have embraced mandatory food fortification of wheat, maize, and/or rice. More than two dozen reports from around the world describe 40%-60% reductions in neural tube defect rates as a consequence. However, some of the world’s most populous nations are not on board. These include China, India, Russia, and the entire European Union.
Among the arguments raised by opponents of mandatory food fortification is the notion that it exposes the entire population to folic acid while benefiting only a small group of individuals who are spared having a neural tube defect. But the findings regarding prevention of folate-deficiency anemia demonstrate that argument is incorrect, Dr. Mills said.
Increased risks of asthma, cancer, and twinning as a consequence of mandatory food fortification have been proposed but are not supported by evidence. The only well-established adverse event is masking of vitamin B12 deficiency by correction of the anemia. But most reported cases have occurred after exposure to folic acid in milligram per day amounts, whereas the average U.S. exposure in women of childbearing age is just 163 mcg per day, less than half the recommended daily intake for that group. Also, no increase in cases of newly diagnosed vitamin B12 deficiency without anemia occurred in the U.S. after mandatory fortification was introduced, according to Dr. Mills.
Audience member Godfrey P. Oakley Jr., MD, noted that there is randomized trial evidence to indicate that folic acid supplementation has another important benefit: primary prevention of stroke in hypertensive adults. He cited the randomized, double-blind China Stroke Primary Prevention Trial, in which almost 21,000 hypertensive Chinese adults without a history of myocardial infarction or stroke were randomized to a single-pill combination of 10 mg of enalapril and 0.8 mg of folic acid daily or to a tablet containing 10 mg of enalapril alone.
During a median 4.5 years of follow-up, the enalapril/folic acid group had a 24% reduction in the risk of ischemic stroke and a 20% reduction in the composite of cardiovascular death, MI, and stroke (JAMA. 2015 Apr 7;313[13]:1325-35).
This is a potential game-changing finding which cries out for a confirmatory trial, he said. “There’s a lot going for that paper. I don’t know of a research agenda item that’s more important than trying to find out the relationship between folic acid fortification and stroke. I wish somebody would put some money into it,” said Dr. Oakley, research professor of epidemiology at Emory University in Atlanta.
Dr. Mills responded that he has reservations about the quality of the Chinese study, particularly in light of a Chinese government analysis that concluded that 80% of Chinese clinical trials were fraudulent (BMJ. 2016 Oct 5;355:i5396).
“That makes me want to see more data from a source I have a little bit more confidence in,” he added.
Another possible benefit of folic acid supplementation worthy of investigation is its theoretic potential for cancer prevention. “Folic acid provides one-carbon atoms for DNA repair,” Dr. Mills noted.
Dr. Mills reported having no relevant financial disclosures.
DENVER – Mandatory food fortification with folic acid not only prevents neural tube defects, it also prevents an estimated 10 million cases of folate-deficiency anemia annually in the United States, James L. Mills, MD, reported at the annual meeting of the Teratology Society.
“We should have people be thinking about the fact that we’re preventing millions of cases of folate-deficiency anemia, not just thousands of cases of neural tube defects. That point does not seem to have reached the public health community. We need to correct the erroneous assumption that a small group are the only ones benefiting by exposing the entire population to folic acid,” said Dr. Mills, senior investigator at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md.
Extrapolating from the nationally representative survey to the full U.S. population, Dr. Mills estimated that translates to roughly 10 million cases of folate-deficiency anemia prevented per year as a result of the mandatory fortification of grain introduced in 1998. That represents an enormous financial savings in avoided costs of diagnosis and treatment of this disorder.
The Food Fortification Initiative reports that 86 countries have embraced mandatory food fortification of wheat, maize, and/or rice. More than two dozen reports from around the world describe 40%-60% reductions in neural tube defect rates as a consequence. However, some of the world’s most populous nations are not on board. These include China, India, Russia, and the entire European Union.
Among the arguments raised by opponents of mandatory food fortification is the notion that it exposes the entire population to folic acid while benefiting only a small group of individuals who are spared having a neural tube defect. But the findings regarding prevention of folate-deficiency anemia demonstrate that argument is incorrect, Dr. Mills said.
Increased risks of asthma, cancer, and twinning as a consequence of mandatory food fortification have been proposed but are not supported by evidence. The only well-established adverse event is masking of vitamin B12 deficiency by correction of the anemia. But most reported cases have occurred after exposure to folic acid in milligram per day amounts, whereas the average U.S. exposure in women of childbearing age is just 163 mcg per day, less than half the recommended daily intake for that group. Also, no increase in cases of newly diagnosed vitamin B12 deficiency without anemia occurred in the U.S. after mandatory fortification was introduced, according to Dr. Mills.
Audience member Godfrey P. Oakley Jr., MD, noted that there is randomized trial evidence to indicate that folic acid supplementation has another important benefit: primary prevention of stroke in hypertensive adults. He cited the randomized, double-blind China Stroke Primary Prevention Trial, in which almost 21,000 hypertensive Chinese adults without a history of myocardial infarction or stroke were randomized to a single-pill combination of 10 mg of enalapril and 0.8 mg of folic acid daily or to a tablet containing 10 mg of enalapril alone.
During a median 4.5 years of follow-up, the enalapril/folic acid group had a 24% reduction in the risk of ischemic stroke and a 20% reduction in the composite of cardiovascular death, MI, and stroke (JAMA. 2015 Apr 7;313[13]:1325-35).
This is a potential game-changing finding which cries out for a confirmatory trial, he said. “There’s a lot going for that paper. I don’t know of a research agenda item that’s more important than trying to find out the relationship between folic acid fortification and stroke. I wish somebody would put some money into it,” said Dr. Oakley, research professor of epidemiology at Emory University in Atlanta.
Dr. Mills responded that he has reservations about the quality of the Chinese study, particularly in light of a Chinese government analysis that concluded that 80% of Chinese clinical trials were fraudulent (BMJ. 2016 Oct 5;355:i5396).
“That makes me want to see more data from a source I have a little bit more confidence in,” he added.
Another possible benefit of folic acid supplementation worthy of investigation is its theoretic potential for cancer prevention. “Folic acid provides one-carbon atoms for DNA repair,” Dr. Mills noted.
Dr. Mills reported having no relevant financial disclosures.
DENVER – Mandatory food fortification with folic acid not only prevents neural tube defects, it also prevents an estimated 10 million cases of folate-deficiency anemia annually in the United States, James L. Mills, MD, reported at the annual meeting of the Teratology Society.
“We should have people be thinking about the fact that we’re preventing millions of cases of folate-deficiency anemia, not just thousands of cases of neural tube defects. That point does not seem to have reached the public health community. We need to correct the erroneous assumption that a small group are the only ones benefiting by exposing the entire population to folic acid,” said Dr. Mills, senior investigator at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md.
Extrapolating from the nationally representative survey to the full U.S. population, Dr. Mills estimated that translates to roughly 10 million cases of folate-deficiency anemia prevented per year as a result of the mandatory fortification of grain introduced in 1998. That represents an enormous financial savings in avoided costs of diagnosis and treatment of this disorder.
The Food Fortification Initiative reports that 86 countries have embraced mandatory food fortification of wheat, maize, and/or rice. More than two dozen reports from around the world describe 40%-60% reductions in neural tube defect rates as a consequence. However, some of the world’s most populous nations are not on board. These include China, India, Russia, and the entire European Union.
Among the arguments raised by opponents of mandatory food fortification is the notion that it exposes the entire population to folic acid while benefiting only a small group of individuals who are spared having a neural tube defect. But the findings regarding prevention of folate-deficiency anemia demonstrate that argument is incorrect, Dr. Mills said.
Increased risks of asthma, cancer, and twinning as a consequence of mandatory food fortification have been proposed but are not supported by evidence. The only well-established adverse event is masking of vitamin B12 deficiency by correction of the anemia. But most reported cases have occurred after exposure to folic acid in milligram per day amounts, whereas the average U.S. exposure in women of childbearing age is just 163 mcg per day, less than half the recommended daily intake for that group. Also, no increase in cases of newly diagnosed vitamin B12 deficiency without anemia occurred in the U.S. after mandatory fortification was introduced, according to Dr. Mills.
Audience member Godfrey P. Oakley Jr., MD, noted that there is randomized trial evidence to indicate that folic acid supplementation has another important benefit: primary prevention of stroke in hypertensive adults. He cited the randomized, double-blind China Stroke Primary Prevention Trial, in which almost 21,000 hypertensive Chinese adults without a history of myocardial infarction or stroke were randomized to a single-pill combination of 10 mg of enalapril and 0.8 mg of folic acid daily or to a tablet containing 10 mg of enalapril alone.
During a median 4.5 years of follow-up, the enalapril/folic acid group had a 24% reduction in the risk of ischemic stroke and a 20% reduction in the composite of cardiovascular death, MI, and stroke (JAMA. 2015 Apr 7;313[13]:1325-35).
This is a potential game-changing finding which cries out for a confirmatory trial, he said. “There’s a lot going for that paper. I don’t know of a research agenda item that’s more important than trying to find out the relationship between folic acid fortification and stroke. I wish somebody would put some money into it,” said Dr. Oakley, research professor of epidemiology at Emory University in Atlanta.
Dr. Mills responded that he has reservations about the quality of the Chinese study, particularly in light of a Chinese government analysis that concluded that 80% of Chinese clinical trials were fraudulent (BMJ. 2016 Oct 5;355:i5396).
“That makes me want to see more data from a source I have a little bit more confidence in,” he added.
Another possible benefit of folic acid supplementation worthy of investigation is its theoretic potential for cancer prevention. “Folic acid provides one-carbon atoms for DNA repair,” Dr. Mills noted.
Dr. Mills reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM TERATOLOGY SOCIETY 2017
Can low-dose aspirin reduce the risk of spontaneous preterm birth?
Antiplatelet agents (mainly low-dose aspirin) have been shown to reduce the risk of preeclampsia in women at risk for the condition. The American College of Obstetricians and Gynecologists currently supports consideration of the use of low-dose aspirin (81 mg/day), initiated between 12 and 28 weeks of gestation, for the prevention of preeclampsia in women at high risk.1
Can antiplatelet agents also reduce the risk of preterm birth? It is a reasonable question, postulate van Vliet and colleagues2: Women with a history of preeclampsia also have an increased risk of spontaneous preterm birth (SPB), and vice versa. Uteroplacental ischemia is present in cases of preeclampsia, and research is showing that uteroplacental ischemia also plays a role in the etiology of spontaneous preterm labor.3,4
Details of the study
To investigate their research question, van Vliet and colleagues performed an additional analysis of the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis. The original meta-analysis involved the data of 32,217 women at risk for preeclampsia who were randomly assigned to low-dose aspirin-dipyridamole or placebo (no treatment); the study revealed a moderate risk reduction for preeclampsia as well as a significant reduction in preterm birth at less than 34 weeks of gestation in women treated with antiplatelets.2
In the additional analysis, for women with an SPB who began antiplatelet treatment before 20 weeks of gestation, the researchers assessed the time between 20 weeks and spontaneous preterm delivery, iatrogenic preterm delivery, and any preterm delivery. Overall, 9.7% of women (n = 2,670) had an SPB before 37 weeks of gestation, 2.8% (n = 773) had an SPB before 34 weeks of gestation, and 0.5% (n = 151) had an SPB before 28 weeks of gestation. Antiplatelet agents were associated with a significant reduction in the risk of SPB before 37 weeks (relative risk [RR], 0.93; 95% confidence interval [CI], 0.86–0.996) and before 34 weeks (RR, 0.86; 95% CI, 0.76–0.99). The RR of having an SPB at less than 37 weeks of gestation was 0.83 for women with a previous pregnancy and 0.98 for women in their first pregnancy.2
Bottom line
Antiplatelet use resulted in a 7% reduction in SPB risk in women at risk for preeclampsia. Antiplatelet use resulted in a 14% reduction in moderate to very preterm birth risk (<34 weeks’ gestation).
The authors advise that their study “provides clinicians with the best available evidence to counsel women regarding who might benefit from” antiplatelet use during pregnancy and suggest that antiplatelet use may be a promising intervention for women at high risk for SPB, especially in high-risk women with a previous pregnancy.2
Caveats
The researchers found no difference among those receiving and not receiving antiplatelets in the incidence of antepartum hemorrhage (RR, 1.02; 95% CI, 0.90–1.15), placental abruption (RR, 1.13; 95% CI, 0.87–1.48), or neonatal bleeding (RR, 0.93; 95% CI, 0.80–1.09). The incidence of postpartum hemorrhage (PPH) was again found to be borderline significant (RR, 1.06; 95% CI, 1.00–1.13), but it was more frequent. The authors caution that the SPB reduction that they found in their study (as well as the reduced risk for preeclampsia with low-dose aspirin use) be balanced against the potential higher risk for PPH.2
- The American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Updated July 11, 2016. Accessed August 14, 2017.
- van Vliet EO, Askie LA, Mol BW, Oudijk MA. Antiplatelet agents and the prevention of spontaneous preterm birth. Obstet Gynecol. 2017;129(2):327–336.
- Arias F, Rodriquez L, Rayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am J Obstet Gynecol. 1993;168(2):585–591.
- Kelly R, Holzman C, Senagore P, et al. Placental vascular pathology findings and pathways of preterm delivery. Am J Epidemiol. 2009;170(2):148–158.
Antiplatelet agents (mainly low-dose aspirin) have been shown to reduce the risk of preeclampsia in women at risk for the condition. The American College of Obstetricians and Gynecologists currently supports consideration of the use of low-dose aspirin (81 mg/day), initiated between 12 and 28 weeks of gestation, for the prevention of preeclampsia in women at high risk.1
Can antiplatelet agents also reduce the risk of preterm birth? It is a reasonable question, postulate van Vliet and colleagues2: Women with a history of preeclampsia also have an increased risk of spontaneous preterm birth (SPB), and vice versa. Uteroplacental ischemia is present in cases of preeclampsia, and research is showing that uteroplacental ischemia also plays a role in the etiology of spontaneous preterm labor.3,4
Details of the study
To investigate their research question, van Vliet and colleagues performed an additional analysis of the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis. The original meta-analysis involved the data of 32,217 women at risk for preeclampsia who were randomly assigned to low-dose aspirin-dipyridamole or placebo (no treatment); the study revealed a moderate risk reduction for preeclampsia as well as a significant reduction in preterm birth at less than 34 weeks of gestation in women treated with antiplatelets.2
In the additional analysis, for women with an SPB who began antiplatelet treatment before 20 weeks of gestation, the researchers assessed the time between 20 weeks and spontaneous preterm delivery, iatrogenic preterm delivery, and any preterm delivery. Overall, 9.7% of women (n = 2,670) had an SPB before 37 weeks of gestation, 2.8% (n = 773) had an SPB before 34 weeks of gestation, and 0.5% (n = 151) had an SPB before 28 weeks of gestation. Antiplatelet agents were associated with a significant reduction in the risk of SPB before 37 weeks (relative risk [RR], 0.93; 95% confidence interval [CI], 0.86–0.996) and before 34 weeks (RR, 0.86; 95% CI, 0.76–0.99). The RR of having an SPB at less than 37 weeks of gestation was 0.83 for women with a previous pregnancy and 0.98 for women in their first pregnancy.2
Bottom line
Antiplatelet use resulted in a 7% reduction in SPB risk in women at risk for preeclampsia. Antiplatelet use resulted in a 14% reduction in moderate to very preterm birth risk (<34 weeks’ gestation).
The authors advise that their study “provides clinicians with the best available evidence to counsel women regarding who might benefit from” antiplatelet use during pregnancy and suggest that antiplatelet use may be a promising intervention for women at high risk for SPB, especially in high-risk women with a previous pregnancy.2
Caveats
The researchers found no difference among those receiving and not receiving antiplatelets in the incidence of antepartum hemorrhage (RR, 1.02; 95% CI, 0.90–1.15), placental abruption (RR, 1.13; 95% CI, 0.87–1.48), or neonatal bleeding (RR, 0.93; 95% CI, 0.80–1.09). The incidence of postpartum hemorrhage (PPH) was again found to be borderline significant (RR, 1.06; 95% CI, 1.00–1.13), but it was more frequent. The authors caution that the SPB reduction that they found in their study (as well as the reduced risk for preeclampsia with low-dose aspirin use) be balanced against the potential higher risk for PPH.2
Antiplatelet agents (mainly low-dose aspirin) have been shown to reduce the risk of preeclampsia in women at risk for the condition. The American College of Obstetricians and Gynecologists currently supports consideration of the use of low-dose aspirin (81 mg/day), initiated between 12 and 28 weeks of gestation, for the prevention of preeclampsia in women at high risk.1
Can antiplatelet agents also reduce the risk of preterm birth? It is a reasonable question, postulate van Vliet and colleagues2: Women with a history of preeclampsia also have an increased risk of spontaneous preterm birth (SPB), and vice versa. Uteroplacental ischemia is present in cases of preeclampsia, and research is showing that uteroplacental ischemia also plays a role in the etiology of spontaneous preterm labor.3,4
Details of the study
To investigate their research question, van Vliet and colleagues performed an additional analysis of the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis. The original meta-analysis involved the data of 32,217 women at risk for preeclampsia who were randomly assigned to low-dose aspirin-dipyridamole or placebo (no treatment); the study revealed a moderate risk reduction for preeclampsia as well as a significant reduction in preterm birth at less than 34 weeks of gestation in women treated with antiplatelets.2
In the additional analysis, for women with an SPB who began antiplatelet treatment before 20 weeks of gestation, the researchers assessed the time between 20 weeks and spontaneous preterm delivery, iatrogenic preterm delivery, and any preterm delivery. Overall, 9.7% of women (n = 2,670) had an SPB before 37 weeks of gestation, 2.8% (n = 773) had an SPB before 34 weeks of gestation, and 0.5% (n = 151) had an SPB before 28 weeks of gestation. Antiplatelet agents were associated with a significant reduction in the risk of SPB before 37 weeks (relative risk [RR], 0.93; 95% confidence interval [CI], 0.86–0.996) and before 34 weeks (RR, 0.86; 95% CI, 0.76–0.99). The RR of having an SPB at less than 37 weeks of gestation was 0.83 for women with a previous pregnancy and 0.98 for women in their first pregnancy.2
Bottom line
Antiplatelet use resulted in a 7% reduction in SPB risk in women at risk for preeclampsia. Antiplatelet use resulted in a 14% reduction in moderate to very preterm birth risk (<34 weeks’ gestation).
The authors advise that their study “provides clinicians with the best available evidence to counsel women regarding who might benefit from” antiplatelet use during pregnancy and suggest that antiplatelet use may be a promising intervention for women at high risk for SPB, especially in high-risk women with a previous pregnancy.2
Caveats
The researchers found no difference among those receiving and not receiving antiplatelets in the incidence of antepartum hemorrhage (RR, 1.02; 95% CI, 0.90–1.15), placental abruption (RR, 1.13; 95% CI, 0.87–1.48), or neonatal bleeding (RR, 0.93; 95% CI, 0.80–1.09). The incidence of postpartum hemorrhage (PPH) was again found to be borderline significant (RR, 1.06; 95% CI, 1.00–1.13), but it was more frequent. The authors caution that the SPB reduction that they found in their study (as well as the reduced risk for preeclampsia with low-dose aspirin use) be balanced against the potential higher risk for PPH.2
- The American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Updated July 11, 2016. Accessed August 14, 2017.
- van Vliet EO, Askie LA, Mol BW, Oudijk MA. Antiplatelet agents and the prevention of spontaneous preterm birth. Obstet Gynecol. 2017;129(2):327–336.
- Arias F, Rodriquez L, Rayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am J Obstet Gynecol. 1993;168(2):585–591.
- Kelly R, Holzman C, Senagore P, et al. Placental vascular pathology findings and pathways of preterm delivery. Am J Epidemiol. 2009;170(2):148–158.
- The American College of Obstetricians and Gynecologists. Practice advisory on low-dose aspirin and prevention of preeclampsia: updated recommendations. https://www.acog.org/About-ACOG/News-Room/Practice-Advisories/Practice-Advisory-Low-Dose-Aspirin-and-Prevention-of-Preeclampsia-Updated-Recommendations. Updated July 11, 2016. Accessed August 14, 2017.
- van Vliet EO, Askie LA, Mol BW, Oudijk MA. Antiplatelet agents and the prevention of spontaneous preterm birth. Obstet Gynecol. 2017;129(2):327–336.
- Arias F, Rodriquez L, Rayne SC, Kraus FT. Maternal placental vasculopathy and infection: two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am J Obstet Gynecol. 1993;168(2):585–591.
- Kelly R, Holzman C, Senagore P, et al. Placental vascular pathology findings and pathways of preterm delivery. Am J Epidemiol. 2009;170(2):148–158.
VIDEO: How to prevent, manage perinatal HIV infection
PARK CITY, UTAH – Despite notable progress in recent years, . Early recognition and treatment of HIV infection in pregnancy, prophylaxis for at-risk women, and retention of infected women in postpartum HIV care remain important goals, but they aren’t always met.
In a wide-ranging interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Gweneth Lazenby, MD, associate professor of obstetrics and gynecology at the Medical University of South Carolina, Charleston, explained what to do to improve the situation. Among the many pearls she shared: One HIV test isn’t enough for at-risk women.
PARK CITY, UTAH – Despite notable progress in recent years, . Early recognition and treatment of HIV infection in pregnancy, prophylaxis for at-risk women, and retention of infected women in postpartum HIV care remain important goals, but they aren’t always met.
In a wide-ranging interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Gweneth Lazenby, MD, associate professor of obstetrics and gynecology at the Medical University of South Carolina, Charleston, explained what to do to improve the situation. Among the many pearls she shared: One HIV test isn’t enough for at-risk women.
PARK CITY, UTAH – Despite notable progress in recent years, . Early recognition and treatment of HIV infection in pregnancy, prophylaxis for at-risk women, and retention of infected women in postpartum HIV care remain important goals, but they aren’t always met.
In a wide-ranging interview at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Gweneth Lazenby, MD, associate professor of obstetrics and gynecology at the Medical University of South Carolina, Charleston, explained what to do to improve the situation. Among the many pearls she shared: One HIV test isn’t enough for at-risk women.
AT IDSOG
Treating women with opioid use disorders poses unique challenges
The opioid epidemic in the United States is reaching a boiling point, with President Trump calling it a “national emergency” and instructing his administration to use all appropriate authority to respond. Experts say that women are disproportionately affected and require unique treatment approaches.
The rate of prescription opioid–related overdoses increased by 471% among women in 2015, compared with an increase of 218% among men. Heroin deaths among women have risen at more than twice the rate among men, according to a report from the Office of Women’s Health (OWH), part of the U.S. Department of Health & Human Services.
The OWH report, released in July, paints a different picture of addiction for women than for men. Women are more likely to experience chronic pain and turn to prescription opioids for longer periods of time and in higher doses. But women also become dependent at smaller doses and in a shorter period of time. Add to this the fact that psychological and emotional distress are risk factors for opioid abuse among women, but not among men, according to the report.
ACOG guidance
In August, the American College of Obstetricians and Gynecologists (ACOG) updated its recommendations for treatments and best practices related to opioid use among pregnant women (Obstet Gynecol. 2017;130:e81-94).
The committee opinion, developed with the American Society of Addiction Medicine, focuses on tearing down stereotypes about women with substance use disorders that could cause patients to slip through the cracks. ACOG recommended universal screening as a part of regular obstetric care, starting with the first prenatal visit.
While screening can involve laboratory testing, the recommendations focus more on creating a comfortable environment for pregnant women to share substance use history and to have a frank conversation about what treatment options are available.
“The document highlights the use of a verbal screening tool which enables the obstetric provider to have a direct conversation with the patient about their answers,” Maria Mascola, MD, an ob.gyn. at the Marshfield (Wis.) Clinic and lead author of the ACOG committee opinion, said in an interview. “It talks about substance use and then provides an opportunity to understand what substances and how much, why these substances might be bad, why this behavior should be changed, and how obstetricians can try to help the person make those changes.”
ACOG continues to recommend medication-assisted treatment (MAT) – typically with methadone or buprenorphine – as the most effective pathway for pregnant women to deal with substance use disorders. However, in cases in which the patient does not accept treatment with an opioid agonist or the treatment is unavailable, medically supervised withdrawal can be considered. ACOG cautions that relapse rates are high (from 59% to more than 90%) and that withdrawal often involves inpatient care and intensive outpatient follow-up. But recent evidence suggests medically supervised withdrawal is not associated with fetal death or preterm delivery.
“There have been some studies looking at smaller groups that have shown pregnant women going through medically supervised withdrawals and there have been some data from those studies that indicate women may be able to successfully go through this withdrawal without harm to the baby,” Dr. Mascola said. “The information we have on medically supervised withdrawal is a small amount of data, and we definitely need more before this is a primary approach.”
Access to care
Regardless of the treatment approach, the larger issue may be accessibility of care. Just 20% of adults with an opioid use disorder get the treatment and care they need each year, according to the OWH, with access and cost cited as the primary barriers to care. This problem is likely worse in rural areas.
“Rural health care is tougher. There is less access; that is an absolute truth, and it’s a burden then for those women to travel long distances to get the care they need,” Dr. Mascola said. “I think ob.gyns. should advocate for more attention in those areas where patients are underserved.”
One potential solution is for ob.gyns. to become certified in providing buprenorphine, which would allow physicians in rural areas to dispense these approved pharmacotherapies to patients who would otherwise be unable to have the proper treatment and follow-up necessary to prevent relapse, Dr. Mascola said.
There is already some federal funding available for this approach. In 2016, the Health Resources and Services Administration awarded $94 million to health centers across the country to expand substance use services, specifically increasing screening for substance use disorders, improving access to medication-assisted treatment, and training clinicians. Similarly, the Substance Abuse and Mental Health Services Administration recently announced it will allocate an additional $485 million to states through the State Targeted Response to the Opioid Crisis Grants to fund medication-assisted treatment and other services.
Unique challenges
Treating women with opioid use disorder isn’t just about identifying the best treatment approach. Social factors appear to play a larger role among women.
“Another difference with women over men is the prevalence of sexual trauma, as well as being in unhealthy relationships where the women are more likely to be enticed into leaving treatment,” she added.
Trauma among women with substance abuse disorders is prevalent, with 55%-99% of women reporting experiencing some form of trauma, compared with 36%-51% of the general population, according to the OWH report.
Beyond exploratory research, there needs to be a major shift in the public perception of opioid substance use, which currently does not approach the disorder as a chronic disease, according to Dr. Jones.
“The treatment process cannot just involve a detoxification program and then send patients off because that will commonly just end in relapse.” Dr. Jones said. “We need to approach substance use disorders with a recovery-oriented system of care in order to create a true safety net they can rely on.”
[email protected]
On Twitter @eaztweets
The opioid epidemic in the United States is reaching a boiling point, with President Trump calling it a “national emergency” and instructing his administration to use all appropriate authority to respond. Experts say that women are disproportionately affected and require unique treatment approaches.
The rate of prescription opioid–related overdoses increased by 471% among women in 2015, compared with an increase of 218% among men. Heroin deaths among women have risen at more than twice the rate among men, according to a report from the Office of Women’s Health (OWH), part of the U.S. Department of Health & Human Services.
The OWH report, released in July, paints a different picture of addiction for women than for men. Women are more likely to experience chronic pain and turn to prescription opioids for longer periods of time and in higher doses. But women also become dependent at smaller doses and in a shorter period of time. Add to this the fact that psychological and emotional distress are risk factors for opioid abuse among women, but not among men, according to the report.
ACOG guidance
In August, the American College of Obstetricians and Gynecologists (ACOG) updated its recommendations for treatments and best practices related to opioid use among pregnant women (Obstet Gynecol. 2017;130:e81-94).
The committee opinion, developed with the American Society of Addiction Medicine, focuses on tearing down stereotypes about women with substance use disorders that could cause patients to slip through the cracks. ACOG recommended universal screening as a part of regular obstetric care, starting with the first prenatal visit.
While screening can involve laboratory testing, the recommendations focus more on creating a comfortable environment for pregnant women to share substance use history and to have a frank conversation about what treatment options are available.
“The document highlights the use of a verbal screening tool which enables the obstetric provider to have a direct conversation with the patient about their answers,” Maria Mascola, MD, an ob.gyn. at the Marshfield (Wis.) Clinic and lead author of the ACOG committee opinion, said in an interview. “It talks about substance use and then provides an opportunity to understand what substances and how much, why these substances might be bad, why this behavior should be changed, and how obstetricians can try to help the person make those changes.”
ACOG continues to recommend medication-assisted treatment (MAT) – typically with methadone or buprenorphine – as the most effective pathway for pregnant women to deal with substance use disorders. However, in cases in which the patient does not accept treatment with an opioid agonist or the treatment is unavailable, medically supervised withdrawal can be considered. ACOG cautions that relapse rates are high (from 59% to more than 90%) and that withdrawal often involves inpatient care and intensive outpatient follow-up. But recent evidence suggests medically supervised withdrawal is not associated with fetal death or preterm delivery.
“There have been some studies looking at smaller groups that have shown pregnant women going through medically supervised withdrawals and there have been some data from those studies that indicate women may be able to successfully go through this withdrawal without harm to the baby,” Dr. Mascola said. “The information we have on medically supervised withdrawal is a small amount of data, and we definitely need more before this is a primary approach.”
Access to care
Regardless of the treatment approach, the larger issue may be accessibility of care. Just 20% of adults with an opioid use disorder get the treatment and care they need each year, according to the OWH, with access and cost cited as the primary barriers to care. This problem is likely worse in rural areas.
“Rural health care is tougher. There is less access; that is an absolute truth, and it’s a burden then for those women to travel long distances to get the care they need,” Dr. Mascola said. “I think ob.gyns. should advocate for more attention in those areas where patients are underserved.”
One potential solution is for ob.gyns. to become certified in providing buprenorphine, which would allow physicians in rural areas to dispense these approved pharmacotherapies to patients who would otherwise be unable to have the proper treatment and follow-up necessary to prevent relapse, Dr. Mascola said.
There is already some federal funding available for this approach. In 2016, the Health Resources and Services Administration awarded $94 million to health centers across the country to expand substance use services, specifically increasing screening for substance use disorders, improving access to medication-assisted treatment, and training clinicians. Similarly, the Substance Abuse and Mental Health Services Administration recently announced it will allocate an additional $485 million to states through the State Targeted Response to the Opioid Crisis Grants to fund medication-assisted treatment and other services.
Unique challenges
Treating women with opioid use disorder isn’t just about identifying the best treatment approach. Social factors appear to play a larger role among women.
“Another difference with women over men is the prevalence of sexual trauma, as well as being in unhealthy relationships where the women are more likely to be enticed into leaving treatment,” she added.
Trauma among women with substance abuse disorders is prevalent, with 55%-99% of women reporting experiencing some form of trauma, compared with 36%-51% of the general population, according to the OWH report.
Beyond exploratory research, there needs to be a major shift in the public perception of opioid substance use, which currently does not approach the disorder as a chronic disease, according to Dr. Jones.
“The treatment process cannot just involve a detoxification program and then send patients off because that will commonly just end in relapse.” Dr. Jones said. “We need to approach substance use disorders with a recovery-oriented system of care in order to create a true safety net they can rely on.”
[email protected]
On Twitter @eaztweets
The opioid epidemic in the United States is reaching a boiling point, with President Trump calling it a “national emergency” and instructing his administration to use all appropriate authority to respond. Experts say that women are disproportionately affected and require unique treatment approaches.
The rate of prescription opioid–related overdoses increased by 471% among women in 2015, compared with an increase of 218% among men. Heroin deaths among women have risen at more than twice the rate among men, according to a report from the Office of Women’s Health (OWH), part of the U.S. Department of Health & Human Services.
The OWH report, released in July, paints a different picture of addiction for women than for men. Women are more likely to experience chronic pain and turn to prescription opioids for longer periods of time and in higher doses. But women also become dependent at smaller doses and in a shorter period of time. Add to this the fact that psychological and emotional distress are risk factors for opioid abuse among women, but not among men, according to the report.
ACOG guidance
In August, the American College of Obstetricians and Gynecologists (ACOG) updated its recommendations for treatments and best practices related to opioid use among pregnant women (Obstet Gynecol. 2017;130:e81-94).
The committee opinion, developed with the American Society of Addiction Medicine, focuses on tearing down stereotypes about women with substance use disorders that could cause patients to slip through the cracks. ACOG recommended universal screening as a part of regular obstetric care, starting with the first prenatal visit.
While screening can involve laboratory testing, the recommendations focus more on creating a comfortable environment for pregnant women to share substance use history and to have a frank conversation about what treatment options are available.
“The document highlights the use of a verbal screening tool which enables the obstetric provider to have a direct conversation with the patient about their answers,” Maria Mascola, MD, an ob.gyn. at the Marshfield (Wis.) Clinic and lead author of the ACOG committee opinion, said in an interview. “It talks about substance use and then provides an opportunity to understand what substances and how much, why these substances might be bad, why this behavior should be changed, and how obstetricians can try to help the person make those changes.”
ACOG continues to recommend medication-assisted treatment (MAT) – typically with methadone or buprenorphine – as the most effective pathway for pregnant women to deal with substance use disorders. However, in cases in which the patient does not accept treatment with an opioid agonist or the treatment is unavailable, medically supervised withdrawal can be considered. ACOG cautions that relapse rates are high (from 59% to more than 90%) and that withdrawal often involves inpatient care and intensive outpatient follow-up. But recent evidence suggests medically supervised withdrawal is not associated with fetal death or preterm delivery.
“There have been some studies looking at smaller groups that have shown pregnant women going through medically supervised withdrawals and there have been some data from those studies that indicate women may be able to successfully go through this withdrawal without harm to the baby,” Dr. Mascola said. “The information we have on medically supervised withdrawal is a small amount of data, and we definitely need more before this is a primary approach.”
Access to care
Regardless of the treatment approach, the larger issue may be accessibility of care. Just 20% of adults with an opioid use disorder get the treatment and care they need each year, according to the OWH, with access and cost cited as the primary barriers to care. This problem is likely worse in rural areas.
“Rural health care is tougher. There is less access; that is an absolute truth, and it’s a burden then for those women to travel long distances to get the care they need,” Dr. Mascola said. “I think ob.gyns. should advocate for more attention in those areas where patients are underserved.”
One potential solution is for ob.gyns. to become certified in providing buprenorphine, which would allow physicians in rural areas to dispense these approved pharmacotherapies to patients who would otherwise be unable to have the proper treatment and follow-up necessary to prevent relapse, Dr. Mascola said.
There is already some federal funding available for this approach. In 2016, the Health Resources and Services Administration awarded $94 million to health centers across the country to expand substance use services, specifically increasing screening for substance use disorders, improving access to medication-assisted treatment, and training clinicians. Similarly, the Substance Abuse and Mental Health Services Administration recently announced it will allocate an additional $485 million to states through the State Targeted Response to the Opioid Crisis Grants to fund medication-assisted treatment and other services.
Unique challenges
Treating women with opioid use disorder isn’t just about identifying the best treatment approach. Social factors appear to play a larger role among women.
“Another difference with women over men is the prevalence of sexual trauma, as well as being in unhealthy relationships where the women are more likely to be enticed into leaving treatment,” she added.
Trauma among women with substance abuse disorders is prevalent, with 55%-99% of women reporting experiencing some form of trauma, compared with 36%-51% of the general population, according to the OWH report.
Beyond exploratory research, there needs to be a major shift in the public perception of opioid substance use, which currently does not approach the disorder as a chronic disease, according to Dr. Jones.
“The treatment process cannot just involve a detoxification program and then send patients off because that will commonly just end in relapse.” Dr. Jones said. “We need to approach substance use disorders with a recovery-oriented system of care in order to create a true safety net they can rely on.”
[email protected]
On Twitter @eaztweets