User login
Intraoperative Fat Embolism During Core Decompression and Bone Grafting for Osteonecrosis of the Hip: Report of 3 Cases and Literature Review
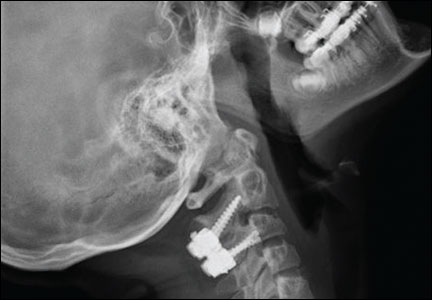
Delayed Presentation of a Cervical Spine Fracture Dislocation With Posterior Ligamentous Disruption in a Gymnast
Trends in Primary and Revision Anterior Cruciate Ligament Reconstruction Among National Basketball Association Team Physicians
A Conversation With AAOS President Frederick M. Azar, MD
For the past 8 years, I have interviewed the president of the American Academy of Orthopaedic Surgeons (AAOS) to better understand the role the Academy plays in our professional lives in general and the contributions of the AAOS president in particular.
At the 2014 AAOS Annual Meeting this past March in New Orleans, Frederick M. Azar, MD, assumed leadership of the AAOS as its 82nd president. He brings a wide range of orthopedic experience to this role. He has been an Academy volunteer for the last 20 years, and is Chief of Staff at the Campbell Clinic as well as Professor of Orthopedic Surgery and Director of the Sports Medicine Fellowship at the University of Tennessee-Campbell Clinic. He is team physician for the NBA (National Basketball Association) Memphis Grizzlies (see Dr. Azar’s article in this issue of AJO, pages 267-271) and team physician for the University of Memphis and Christian Brothers University sports teams.
This year the Board of Directors of the Academy completed a revision of the AAOS Strategic Plan, last updated in 2010, under the leadership of David Teuscher, MD. The plan, dubbed “Vision 20/20,” includes the following essential elements:
◾ AAOS Mission: Serving our profession to provide the highest quality musculoskeletal care.
◾ AAOS Vision: Keeping the world in motion through the prevention and treatment of musculoskeletal conditions.
◾ Core Values: Excellence, Professionalism, Leadership, Collegiality, Lifelong Learning
◾ Strategic Domains: Advocacy, Education, Membership, Organizational Excellence, Quality and Patient Value
Fred explained that a fundamental aspect of this revised Strategic Plan is that the AAOS takes ownership of all aspects of musculoskeletal tear, not simply surgical management. (For further reading, please visit: www.aaos.org/about/strategicplan.asp.)
Dr. Azar views his role as president of the AAOS as a temporary steward furthering the goals of the organization and not as a proponent of a particular personal agenda. To that end, Fred hopes to focus on 2 areas during his tenure as captain of the orthopedic ship of state: education and communication.
Paradigm shifts are occurring in health care with the passage of the Affordable Care Act, access to medical information via the Internet, and changes in practice management with the near-universal implementation of electronic medical records. In an effort to address the educational needs of its members, the AAOS will expand its electronic media platform and develop mobile apps, ebooks, webinars, and webcasts. In addition, the new AAOS headquarters in Rosemont, Illinois, will house a state-of-the-art Orthopaedic Learning Center. These improvements in education will contribute to the Academy’s core value of lifelong learning.
Regarding communication, Dr. Azar believes that it is extremely important that we, orthopedic surgeons, share with our patients just how much orthopedic care contributes to their quality of life, thereby showcasing the great value orthopedic surgeons bring to millions of patients. Finally, communication with regulators and policymakers in Washington, DC, is equally important as is membership support
for the Orthopaedic Political Action Committee.
We are indeed fortunate to have someone of Dr. Azar’s caliber lead our organization. His extensive experience as an administrator, Academy volunteer, educator, and clinician makes him ideally suited to lead the AAOS during these
challenging times in health care. ◾
For the past 8 years, I have interviewed the president of the American Academy of Orthopaedic Surgeons (AAOS) to better understand the role the Academy plays in our professional lives in general and the contributions of the AAOS president in particular.
At the 2014 AAOS Annual Meeting this past March in New Orleans, Frederick M. Azar, MD, assumed leadership of the AAOS as its 82nd president. He brings a wide range of orthopedic experience to this role. He has been an Academy volunteer for the last 20 years, and is Chief of Staff at the Campbell Clinic as well as Professor of Orthopedic Surgery and Director of the Sports Medicine Fellowship at the University of Tennessee-Campbell Clinic. He is team physician for the NBA (National Basketball Association) Memphis Grizzlies (see Dr. Azar’s article in this issue of AJO, pages 267-271) and team physician for the University of Memphis and Christian Brothers University sports teams.
This year the Board of Directors of the Academy completed a revision of the AAOS Strategic Plan, last updated in 2010, under the leadership of David Teuscher, MD. The plan, dubbed “Vision 20/20,” includes the following essential elements:
◾ AAOS Mission: Serving our profession to provide the highest quality musculoskeletal care.
◾ AAOS Vision: Keeping the world in motion through the prevention and treatment of musculoskeletal conditions.
◾ Core Values: Excellence, Professionalism, Leadership, Collegiality, Lifelong Learning
◾ Strategic Domains: Advocacy, Education, Membership, Organizational Excellence, Quality and Patient Value
Fred explained that a fundamental aspect of this revised Strategic Plan is that the AAOS takes ownership of all aspects of musculoskeletal tear, not simply surgical management. (For further reading, please visit: www.aaos.org/about/strategicplan.asp.)
Dr. Azar views his role as president of the AAOS as a temporary steward furthering the goals of the organization and not as a proponent of a particular personal agenda. To that end, Fred hopes to focus on 2 areas during his tenure as captain of the orthopedic ship of state: education and communication.
Paradigm shifts are occurring in health care with the passage of the Affordable Care Act, access to medical information via the Internet, and changes in practice management with the near-universal implementation of electronic medical records. In an effort to address the educational needs of its members, the AAOS will expand its electronic media platform and develop mobile apps, ebooks, webinars, and webcasts. In addition, the new AAOS headquarters in Rosemont, Illinois, will house a state-of-the-art Orthopaedic Learning Center. These improvements in education will contribute to the Academy’s core value of lifelong learning.
Regarding communication, Dr. Azar believes that it is extremely important that we, orthopedic surgeons, share with our patients just how much orthopedic care contributes to their quality of life, thereby showcasing the great value orthopedic surgeons bring to millions of patients. Finally, communication with regulators and policymakers in Washington, DC, is equally important as is membership support
for the Orthopaedic Political Action Committee.
We are indeed fortunate to have someone of Dr. Azar’s caliber lead our organization. His extensive experience as an administrator, Academy volunteer, educator, and clinician makes him ideally suited to lead the AAOS during these
challenging times in health care. ◾
For the past 8 years, I have interviewed the president of the American Academy of Orthopaedic Surgeons (AAOS) to better understand the role the Academy plays in our professional lives in general and the contributions of the AAOS president in particular.
At the 2014 AAOS Annual Meeting this past March in New Orleans, Frederick M. Azar, MD, assumed leadership of the AAOS as its 82nd president. He brings a wide range of orthopedic experience to this role. He has been an Academy volunteer for the last 20 years, and is Chief of Staff at the Campbell Clinic as well as Professor of Orthopedic Surgery and Director of the Sports Medicine Fellowship at the University of Tennessee-Campbell Clinic. He is team physician for the NBA (National Basketball Association) Memphis Grizzlies (see Dr. Azar’s article in this issue of AJO, pages 267-271) and team physician for the University of Memphis and Christian Brothers University sports teams.
This year the Board of Directors of the Academy completed a revision of the AAOS Strategic Plan, last updated in 2010, under the leadership of David Teuscher, MD. The plan, dubbed “Vision 20/20,” includes the following essential elements:
◾ AAOS Mission: Serving our profession to provide the highest quality musculoskeletal care.
◾ AAOS Vision: Keeping the world in motion through the prevention and treatment of musculoskeletal conditions.
◾ Core Values: Excellence, Professionalism, Leadership, Collegiality, Lifelong Learning
◾ Strategic Domains: Advocacy, Education, Membership, Organizational Excellence, Quality and Patient Value
Fred explained that a fundamental aspect of this revised Strategic Plan is that the AAOS takes ownership of all aspects of musculoskeletal tear, not simply surgical management. (For further reading, please visit: www.aaos.org/about/strategicplan.asp.)
Dr. Azar views his role as president of the AAOS as a temporary steward furthering the goals of the organization and not as a proponent of a particular personal agenda. To that end, Fred hopes to focus on 2 areas during his tenure as captain of the orthopedic ship of state: education and communication.
Paradigm shifts are occurring in health care with the passage of the Affordable Care Act, access to medical information via the Internet, and changes in practice management with the near-universal implementation of electronic medical records. In an effort to address the educational needs of its members, the AAOS will expand its electronic media platform and develop mobile apps, ebooks, webinars, and webcasts. In addition, the new AAOS headquarters in Rosemont, Illinois, will house a state-of-the-art Orthopaedic Learning Center. These improvements in education will contribute to the Academy’s core value of lifelong learning.
Regarding communication, Dr. Azar believes that it is extremely important that we, orthopedic surgeons, share with our patients just how much orthopedic care contributes to their quality of life, thereby showcasing the great value orthopedic surgeons bring to millions of patients. Finally, communication with regulators and policymakers in Washington, DC, is equally important as is membership support
for the Orthopaedic Political Action Committee.
We are indeed fortunate to have someone of Dr. Azar’s caliber lead our organization. His extensive experience as an administrator, Academy volunteer, educator, and clinician makes him ideally suited to lead the AAOS during these
challenging times in health care. ◾
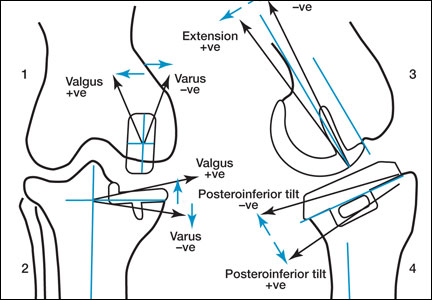
Perioperative Differences in Conventional and Computer-Assisted Surgery in Bilateral Total Knee Arthroplasty
Computer Navigation Systems in Unicompartmental Knee Arthroplasty: A Systematic Review
Activity program staves off mobility disability
A structured physical activity program reduced the rate of major mobility disability among sedentary men and women aged 70-89 years who were at high risk for the condition, in a randomized clinical trial presented at the annual meeting of the American College of Sports Medicine in Orlando and simultaneously published online May 27 in JAMA.
Compared with a sedentary health education intervention, the physical activity program was particularly effective in the large subgroup of participants who had the lowest physical function at baseline, said Dr. Marco Pahor of the department of aging and geriatric research, University of Florida, Gainesville, and his associates in the Lifestyle Interventions and Independence for the Elderly (LIFE) trial.
"These results suggest the potential for structured physical activity as a feasible and effective intervention to reduce the burden of disability among vulnerable older persons, in spite of functional decline in later life," they noted (JAMA 2014 May 27 [doi:10.1001/jama.2014.5616]).
In what they described as the largest and longest lasting randomized trial of physical activity in older persons, Dr. Pahor and his associates assessed 1,635 participants of diverse ethnic/racial backgrounds residing in rural, urban, and suburban communities. These study subjects (mean age, 78.9 years) were followed at geriatric health facilities at eight medical centers across the country.
They were deemed to be at high risk for mobility disability – losing the ability to walk 400 meters within 15 minutes without sitting, leaning, or the assistance of a walker or another person – based on functional limitations determined by the Short Physical Performance Battery (SPPB). This is considered an excellent proxy for impaired mobility in the community, the investigators said, and maintaining such mobility is central to retaining independence and a good quality of life.
The study participants were randomly assigned to receive either a structured physical activity intervention (818 people) or a health education intervention (817 people) and followed at 6-month intervals for at least 2 years.
The activity intervention involved two visits per week to the medical center, plus home-based activity three-four times per week. The goal was to walk for at least 30 minutes daily at moderate intensity and to perform 10 minutes of lower-extremity strength training with ankle weights, 10 minutes of balance training, and large muscle–group flexibility exercises daily.
The education program involved weekly workshops for 26 weeks, followed by monthly workshops thereafter, in which a health educator spoke about topics related to "successful aging," such as negotiating the health care system, travelling safely, obtaining preventive services and screenings, finding reliable health information, and nutrition. This intervention included 5-10 minutes of seated, gentle, upper-extremity stretching or flexibility exercises at each meeting.
The primary outcome was developing mobility disability – losing the ability to walk 400 meters within 15 minutes at their usual pace, without overexerting and without assistance, at the 2-year follow-up visit. This occurred in 30.1% of the activity group, which was significantly lower than the 35.5% rate in the education group, Dr. Pahor and his associates said.
A subgroup comprising 44.7% of the entire study population had the lowest physical function at baseline, reflected in scores of less than eight on the SPPB. They derived "considerable benefit" from the activity intervention and showed the largest reduction in the rate of impaired mobility, with a hazard ratio of 0.81.
People in the activity group had the same number of hospitalizations as those in the education group, as well as the same mortality. However, the mortality data in this study are considered inconclusive, the researchers said, because there were very few deaths overall.
The LIFE study was supported by the National Institutes of Health, the National Institute on Aging, the National Heart, Lung, and Blood Institute, the Claude D. Pepper Older Americans Independence Centers, the National Center for Research Resources, the Boston Rehabilitation Outcomes Center, the Department of Veterans Affairs, and the Department of Agriculture. Dr. Pahor reported no financial conflicts of interest; his associates reported ties to numerous industry sources.
A structured physical activity program reduced the rate of major mobility disability among sedentary men and women aged 70-89 years who were at high risk for the condition, in a randomized clinical trial presented at the annual meeting of the American College of Sports Medicine in Orlando and simultaneously published online May 27 in JAMA.
Compared with a sedentary health education intervention, the physical activity program was particularly effective in the large subgroup of participants who had the lowest physical function at baseline, said Dr. Marco Pahor of the department of aging and geriatric research, University of Florida, Gainesville, and his associates in the Lifestyle Interventions and Independence for the Elderly (LIFE) trial.
"These results suggest the potential for structured physical activity as a feasible and effective intervention to reduce the burden of disability among vulnerable older persons, in spite of functional decline in later life," they noted (JAMA 2014 May 27 [doi:10.1001/jama.2014.5616]).
In what they described as the largest and longest lasting randomized trial of physical activity in older persons, Dr. Pahor and his associates assessed 1,635 participants of diverse ethnic/racial backgrounds residing in rural, urban, and suburban communities. These study subjects (mean age, 78.9 years) were followed at geriatric health facilities at eight medical centers across the country.
They were deemed to be at high risk for mobility disability – losing the ability to walk 400 meters within 15 minutes without sitting, leaning, or the assistance of a walker or another person – based on functional limitations determined by the Short Physical Performance Battery (SPPB). This is considered an excellent proxy for impaired mobility in the community, the investigators said, and maintaining such mobility is central to retaining independence and a good quality of life.
The study participants were randomly assigned to receive either a structured physical activity intervention (818 people) or a health education intervention (817 people) and followed at 6-month intervals for at least 2 years.
The activity intervention involved two visits per week to the medical center, plus home-based activity three-four times per week. The goal was to walk for at least 30 minutes daily at moderate intensity and to perform 10 minutes of lower-extremity strength training with ankle weights, 10 minutes of balance training, and large muscle–group flexibility exercises daily.
The education program involved weekly workshops for 26 weeks, followed by monthly workshops thereafter, in which a health educator spoke about topics related to "successful aging," such as negotiating the health care system, travelling safely, obtaining preventive services and screenings, finding reliable health information, and nutrition. This intervention included 5-10 minutes of seated, gentle, upper-extremity stretching or flexibility exercises at each meeting.
The primary outcome was developing mobility disability – losing the ability to walk 400 meters within 15 minutes at their usual pace, without overexerting and without assistance, at the 2-year follow-up visit. This occurred in 30.1% of the activity group, which was significantly lower than the 35.5% rate in the education group, Dr. Pahor and his associates said.
A subgroup comprising 44.7% of the entire study population had the lowest physical function at baseline, reflected in scores of less than eight on the SPPB. They derived "considerable benefit" from the activity intervention and showed the largest reduction in the rate of impaired mobility, with a hazard ratio of 0.81.
People in the activity group had the same number of hospitalizations as those in the education group, as well as the same mortality. However, the mortality data in this study are considered inconclusive, the researchers said, because there were very few deaths overall.
The LIFE study was supported by the National Institutes of Health, the National Institute on Aging, the National Heart, Lung, and Blood Institute, the Claude D. Pepper Older Americans Independence Centers, the National Center for Research Resources, the Boston Rehabilitation Outcomes Center, the Department of Veterans Affairs, and the Department of Agriculture. Dr. Pahor reported no financial conflicts of interest; his associates reported ties to numerous industry sources.
A structured physical activity program reduced the rate of major mobility disability among sedentary men and women aged 70-89 years who were at high risk for the condition, in a randomized clinical trial presented at the annual meeting of the American College of Sports Medicine in Orlando and simultaneously published online May 27 in JAMA.
Compared with a sedentary health education intervention, the physical activity program was particularly effective in the large subgroup of participants who had the lowest physical function at baseline, said Dr. Marco Pahor of the department of aging and geriatric research, University of Florida, Gainesville, and his associates in the Lifestyle Interventions and Independence for the Elderly (LIFE) trial.
"These results suggest the potential for structured physical activity as a feasible and effective intervention to reduce the burden of disability among vulnerable older persons, in spite of functional decline in later life," they noted (JAMA 2014 May 27 [doi:10.1001/jama.2014.5616]).
In what they described as the largest and longest lasting randomized trial of physical activity in older persons, Dr. Pahor and his associates assessed 1,635 participants of diverse ethnic/racial backgrounds residing in rural, urban, and suburban communities. These study subjects (mean age, 78.9 years) were followed at geriatric health facilities at eight medical centers across the country.
They were deemed to be at high risk for mobility disability – losing the ability to walk 400 meters within 15 minutes without sitting, leaning, or the assistance of a walker or another person – based on functional limitations determined by the Short Physical Performance Battery (SPPB). This is considered an excellent proxy for impaired mobility in the community, the investigators said, and maintaining such mobility is central to retaining independence and a good quality of life.
The study participants were randomly assigned to receive either a structured physical activity intervention (818 people) or a health education intervention (817 people) and followed at 6-month intervals for at least 2 years.
The activity intervention involved two visits per week to the medical center, plus home-based activity three-four times per week. The goal was to walk for at least 30 minutes daily at moderate intensity and to perform 10 minutes of lower-extremity strength training with ankle weights, 10 minutes of balance training, and large muscle–group flexibility exercises daily.
The education program involved weekly workshops for 26 weeks, followed by monthly workshops thereafter, in which a health educator spoke about topics related to "successful aging," such as negotiating the health care system, travelling safely, obtaining preventive services and screenings, finding reliable health information, and nutrition. This intervention included 5-10 minutes of seated, gentle, upper-extremity stretching or flexibility exercises at each meeting.
The primary outcome was developing mobility disability – losing the ability to walk 400 meters within 15 minutes at their usual pace, without overexerting and without assistance, at the 2-year follow-up visit. This occurred in 30.1% of the activity group, which was significantly lower than the 35.5% rate in the education group, Dr. Pahor and his associates said.
A subgroup comprising 44.7% of the entire study population had the lowest physical function at baseline, reflected in scores of less than eight on the SPPB. They derived "considerable benefit" from the activity intervention and showed the largest reduction in the rate of impaired mobility, with a hazard ratio of 0.81.
People in the activity group had the same number of hospitalizations as those in the education group, as well as the same mortality. However, the mortality data in this study are considered inconclusive, the researchers said, because there were very few deaths overall.
The LIFE study was supported by the National Institutes of Health, the National Institute on Aging, the National Heart, Lung, and Blood Institute, the Claude D. Pepper Older Americans Independence Centers, the National Center for Research Resources, the Boston Rehabilitation Outcomes Center, the Department of Veterans Affairs, and the Department of Agriculture. Dr. Pahor reported no financial conflicts of interest; his associates reported ties to numerous industry sources.
FROM THE ACSM ANNUAL MEETING
Major finding: After 2 years, the primary outcome was developing mobility disability – losing the ability to walk 400 meters within 15 minutes at the usual pace, without overexertion and without assistance. It occurred in 30.1% of the activity group, which was significantly lower than the 35.5% rate in the education group.
Data source: A multicenter, single-blind, randomized trial involving 1,635 sedentary men and women aged 70-89 years at high risk for mobility disability, who participated in either a structured physical activity program or a sedentary health education program and were followed for a mean of 2.6 years.
Disclosures: The LIFE study was supported by the National Institutes of Health, the National Institute on Aging, the National Heart, Lung, and Blood Institute, the Claude D. Pepper Older Americans Independence Centers, the National Center for Research Resources, the Boston Rehabilitation Outcomes Center, the Department of Veterans Affairs, and the Department of Agriculture. Dr. Pahor reported no financial conflicts of interest; his associates reported ties to numerous industry sources.
Tapping office IT boosts orthopedic patient–reported outcomes
PARIS – Combining e-mail and office-based technology garnered patient-reported outcomes from more than 90% of patients receiving orthopedic care, in an analysis of 18,073 physician-patient encounters.
"Integrating [patient-reported outcomes] measurement into orthopedic standard of care without interrupting clinical practice is possible and currently in use," Xiang Zhou, Ph.D., reported at the World Congress on Osteoarthritis.
Patient-reported outcomes, or PROs, have taken center stage in recent years as a way to measure the safety and effectiveness of total joint arthroplasty, with respect to both technical and patient satisfaction.
New York University Langone Medical Center implemented an IT system in May 2012 for all nine adult orthopedic reconstructive surgeons at its Center for Musculoskeletal Care. Patients with e-mail addresses on file were sent a link to a PRO questionnaire, individualized to their clinical needs, 3 days before their appointment. A reminder e-mail was sent the day before their visit if the questionnaire was not completed. Tablets were also distributed in the waiting room for patients who did not complete via e-mail. Real-time and previous PRO scores were available in the electronic health record for physicians to review during the examination.
PRO records were captured for 83% of 8,864 patients seen in 20 months. Of those, 72% had multiple, longitudinal PRO scores recorded, according to Dr. Zhou, a research scientist in NYU Langone’s orthopedic surgery department.
Of the 18,073 physician-patient encounters, 71% included a completed PRO score. Monthly completion rates ranged from a high of 91% to a low of 56%.
"Reaching more than a 90% PRO collection rate is possible with the support of participating physicians," he noted.
Patients under age 65 had a significantly higher overall PRO completion rate than did older patients (76% vs. 65%; P less than .001), as did males vs. females (73% vs. 70%; P less than .001), Dr. Zhou reported at the meeting, sponsored by the Osteoarthritis Research Society International.
In all, 55% of patients who provided an e-mail address completed their PRO questionnaires via e-mail. In that subset, no significant differences were seen by age (55% both groups; P = .996) or gender (56% male vs. 55% female; P = .752).
PRO scores are now included in the electronic health record and routinely captured and used by physicians.
"Routine real-time and longitudinal PRO reports are a valuable tool to stimulate patient-physician communication and inform treatment decisions," the authors concluded in the poster presentation.
Dr. Zhou reported having no financial disclosures.
PARIS – Combining e-mail and office-based technology garnered patient-reported outcomes from more than 90% of patients receiving orthopedic care, in an analysis of 18,073 physician-patient encounters.
"Integrating [patient-reported outcomes] measurement into orthopedic standard of care without interrupting clinical practice is possible and currently in use," Xiang Zhou, Ph.D., reported at the World Congress on Osteoarthritis.
Patient-reported outcomes, or PROs, have taken center stage in recent years as a way to measure the safety and effectiveness of total joint arthroplasty, with respect to both technical and patient satisfaction.
New York University Langone Medical Center implemented an IT system in May 2012 for all nine adult orthopedic reconstructive surgeons at its Center for Musculoskeletal Care. Patients with e-mail addresses on file were sent a link to a PRO questionnaire, individualized to their clinical needs, 3 days before their appointment. A reminder e-mail was sent the day before their visit if the questionnaire was not completed. Tablets were also distributed in the waiting room for patients who did not complete via e-mail. Real-time and previous PRO scores were available in the electronic health record for physicians to review during the examination.
PRO records were captured for 83% of 8,864 patients seen in 20 months. Of those, 72% had multiple, longitudinal PRO scores recorded, according to Dr. Zhou, a research scientist in NYU Langone’s orthopedic surgery department.
Of the 18,073 physician-patient encounters, 71% included a completed PRO score. Monthly completion rates ranged from a high of 91% to a low of 56%.
"Reaching more than a 90% PRO collection rate is possible with the support of participating physicians," he noted.
Patients under age 65 had a significantly higher overall PRO completion rate than did older patients (76% vs. 65%; P less than .001), as did males vs. females (73% vs. 70%; P less than .001), Dr. Zhou reported at the meeting, sponsored by the Osteoarthritis Research Society International.
In all, 55% of patients who provided an e-mail address completed their PRO questionnaires via e-mail. In that subset, no significant differences were seen by age (55% both groups; P = .996) or gender (56% male vs. 55% female; P = .752).
PRO scores are now included in the electronic health record and routinely captured and used by physicians.
"Routine real-time and longitudinal PRO reports are a valuable tool to stimulate patient-physician communication and inform treatment decisions," the authors concluded in the poster presentation.
Dr. Zhou reported having no financial disclosures.
PARIS – Combining e-mail and office-based technology garnered patient-reported outcomes from more than 90% of patients receiving orthopedic care, in an analysis of 18,073 physician-patient encounters.
"Integrating [patient-reported outcomes] measurement into orthopedic standard of care without interrupting clinical practice is possible and currently in use," Xiang Zhou, Ph.D., reported at the World Congress on Osteoarthritis.
Patient-reported outcomes, or PROs, have taken center stage in recent years as a way to measure the safety and effectiveness of total joint arthroplasty, with respect to both technical and patient satisfaction.
New York University Langone Medical Center implemented an IT system in May 2012 for all nine adult orthopedic reconstructive surgeons at its Center for Musculoskeletal Care. Patients with e-mail addresses on file were sent a link to a PRO questionnaire, individualized to their clinical needs, 3 days before their appointment. A reminder e-mail was sent the day before their visit if the questionnaire was not completed. Tablets were also distributed in the waiting room for patients who did not complete via e-mail. Real-time and previous PRO scores were available in the electronic health record for physicians to review during the examination.
PRO records were captured for 83% of 8,864 patients seen in 20 months. Of those, 72% had multiple, longitudinal PRO scores recorded, according to Dr. Zhou, a research scientist in NYU Langone’s orthopedic surgery department.
Of the 18,073 physician-patient encounters, 71% included a completed PRO score. Monthly completion rates ranged from a high of 91% to a low of 56%.
"Reaching more than a 90% PRO collection rate is possible with the support of participating physicians," he noted.
Patients under age 65 had a significantly higher overall PRO completion rate than did older patients (76% vs. 65%; P less than .001), as did males vs. females (73% vs. 70%; P less than .001), Dr. Zhou reported at the meeting, sponsored by the Osteoarthritis Research Society International.
In all, 55% of patients who provided an e-mail address completed their PRO questionnaires via e-mail. In that subset, no significant differences were seen by age (55% both groups; P = .996) or gender (56% male vs. 55% female; P = .752).
PRO scores are now included in the electronic health record and routinely captured and used by physicians.
"Routine real-time and longitudinal PRO reports are a valuable tool to stimulate patient-physician communication and inform treatment decisions," the authors concluded in the poster presentation.
Dr. Zhou reported having no financial disclosures.
AT OARSI 2014
Major finding: Monthly completion rates of patient-reported outcomes questionnaires ranged from a high of 91% to a low of 56%.
Data source: An analysis of 18,073 orthopedic physician-patient encounters.
Disclosures: Dr. Zhou reported having no financial disclosures.
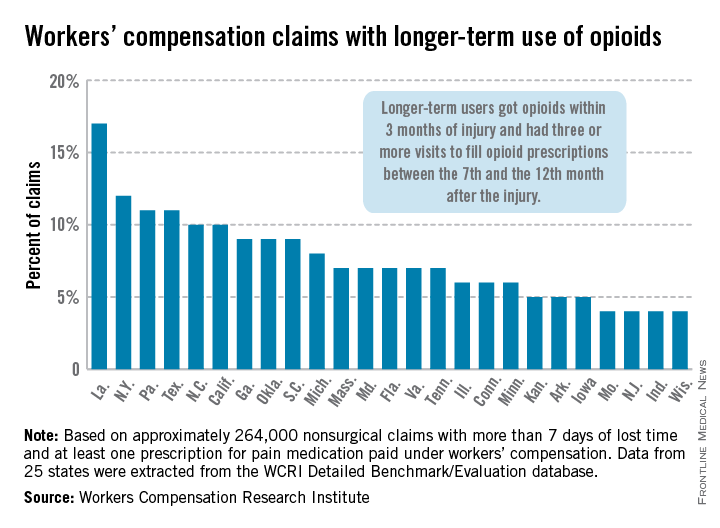
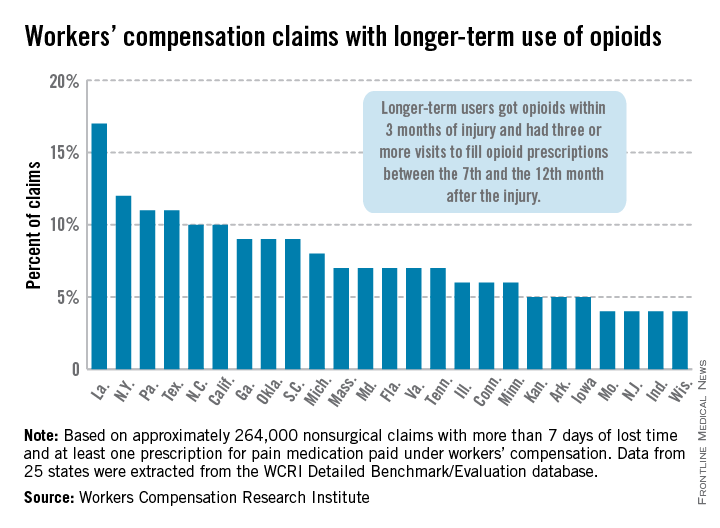
Longer-term opioid use in workers’ comp cases highest in Louisiana
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
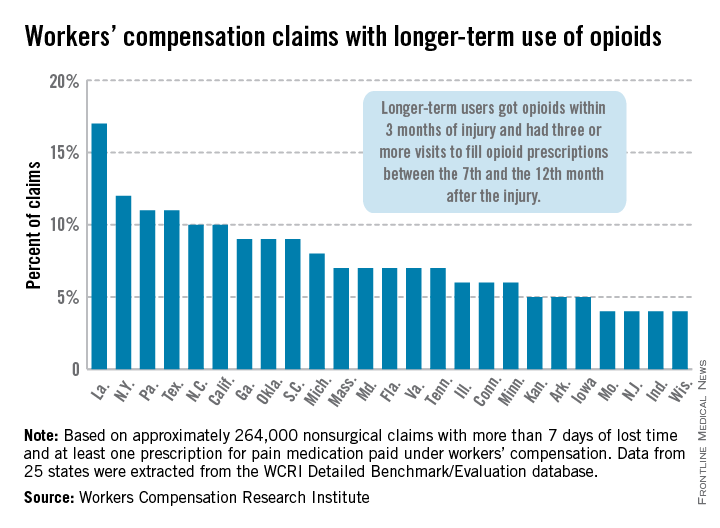
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
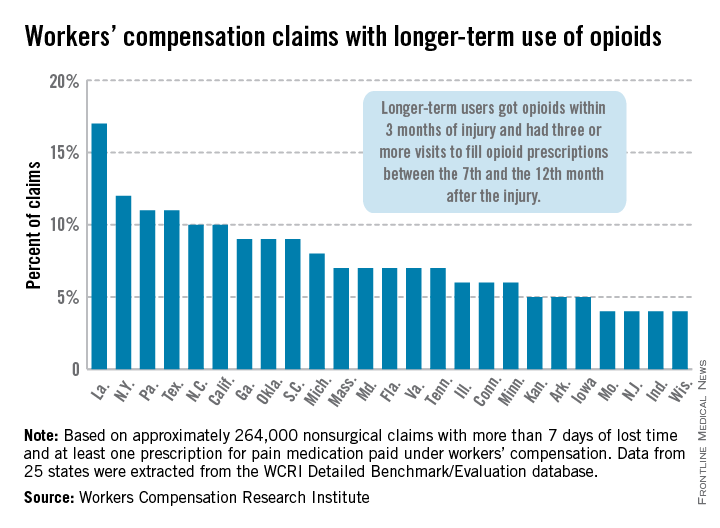
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
Recent knee injuries spark rapid cascade to joint failure
PARIS – Recent knee injuries are strongly associated with accelerated knee osteoarthritis, according to an analysis from the prospective, multicenter Osteoarthritis Initiative.
"Certain injuries may initiate or coincide with an accelerated cascade towards joint failure in as little as 12 months," Jeffrey Driban, Ph.D., said at the World Congress on Osteoarthritis. "In fact, 76% of individuals with an injury and accelerated knee osteoarthritis experienced their injury in the 12 months prior to the study outcome."
The study defined accelerated knee OA as progression from a Kellgren-Lawrence grade 0 or 1 on baseline bilateral radiographs to end-stage KL grade 3 or 4 within 48 months.
Although knee OA typically has been a slowly progressive disorder, 5%-17% of patients now experience accelerated forms of OA.
"If we can better characterize this phenomenon and its potential risk factors, we can provide more insights into the nature of progression in hopes of identifying an at-risk subset," said Dr. Driban of the division of rheumatology at Tufts Medical Center, Boston.
The study by Dr. Driban and his colleagues was published in Arthritis Care & Research (2014 April 29 [doi:10.1002/acr.22359]).
A total of 1,930 participants in the Osteoarthritis Initiative, all with a KL grade of 0 or 1 on baseline bilateral radiographs, were asked at baseline and at each annual visit whether they had ever been "injured enough to limit ability to walk for at least 2 days."
On follow-up, 1,325 had no knee OA, 54 had accelerated knee OA, and 187 had typical knee OA, defined as at least one knee increased in radiographic scoring within 48 months (excluding accelerated OA).
After exclusion of 12 patients with missing data, 30% of the accelerated OA group, 28% in the typical OA group, and 35% in the no OA group had a history of knee injury before baseline. A new knee injury was reported by 32%, 13%, and 11%, respectively, with data missing from 59 persons.
In univariate analyses, participants with accelerated knee OA were significantly older than were those with typical OA or no OA (61.8 years vs. 58 years vs. 59.2 years; P = .023) and had a greater body mass index (28.9 kg/m2 vs. 27.9 kg/m2 vs. 27.1 kg/m2; P = .002), Dr. Driban said.
In multinomial logistic regression analyses that adjusted for age, sex, BMI, presence of static knee malalignment, and systolic blood pressure, there was no association between prior knee injury and accelerated OA (odds ratio, 0.84) or typical OA (OR, 0.76).
However, when the investigators looked further, participants with accelerated OA were almost 3.5 times more likely to report a recent knee injury during the observation period (OR, 3.37; 95% confidence interval, 1.82-6.25) than were those with typical OA (OR, 0.99) or no OA (reference), he said.
Moreover, if a participant experienced a knee injury 1 year before the study outcome, the risk of accelerated OA increased ninefold (OR, 9.22; CI, 4.50-18.90) versus threefold for typical OA (OR, 3.04; CI, 1.66-5.58).
Despite the focus on injuries leading to accelerated OA, the analyses can’t rule out that accelerated OA may also cause an injury or that there could be a "vicious cycle," in which an injury can cause accelerated OA, associated with joint space loss, increased symptoms, and increased risk for subsequent injury, Dr. Driban said.
This line of thought helps explain why prior injury was not associated with accelerated knee OA, but recent injury was. As patients were free of radiographic OA at baseline, those with a history of a prior injury that could cause accelerated knee OA would already have been eliminated from the study, he explained in an interview.
Secondly, if accelerated knee OA can increase the risk of injury, knee injuries from years ago would not be related to accelerated knee OA because the disorder did not exist at the time of the injury.
Finally, there also could be a recall bias, as patients often have a hard time recalling injuries that may have happened years ago.
Despite the limitations of self-reported injuries and insufficient data regarding the type, severity, status of the meniscus, mechanism, or subsequent treatment of the knee injury, the findings represent an important "starting point" in understanding the association between injuries and accelerated osteoarthritis, Dr. Driban said.
"We need to monitor older adults who report an injury, as this may initiate accelerated OA or indicate an individual experiencing accelerated OA, and we need to determine which injuries may be related to accelerated osteoarthritis," he said at the meeting, sponsored by the Osteoarthritis Research Society International.
During the discussion following the formal presentation, Dr. David Felson, professor of medicine and epidemiology at Boston University, said, "I think what you are saying is exactly right," but suggested that the investigators exclude patients with spontaneous osteonecrosis of the knee and osteochondritis dissecans, as both conditions are more common than anticipated and can drive very rapid development of OA. Conversely, inclusion of patients with osteophyte-only knee OA would increase the number likely identified with accelerated OA, he said.
Dr. Driban reported no conflicting interests.
PARIS – Recent knee injuries are strongly associated with accelerated knee osteoarthritis, according to an analysis from the prospective, multicenter Osteoarthritis Initiative.
"Certain injuries may initiate or coincide with an accelerated cascade towards joint failure in as little as 12 months," Jeffrey Driban, Ph.D., said at the World Congress on Osteoarthritis. "In fact, 76% of individuals with an injury and accelerated knee osteoarthritis experienced their injury in the 12 months prior to the study outcome."
The study defined accelerated knee OA as progression from a Kellgren-Lawrence grade 0 or 1 on baseline bilateral radiographs to end-stage KL grade 3 or 4 within 48 months.
Although knee OA typically has been a slowly progressive disorder, 5%-17% of patients now experience accelerated forms of OA.
"If we can better characterize this phenomenon and its potential risk factors, we can provide more insights into the nature of progression in hopes of identifying an at-risk subset," said Dr. Driban of the division of rheumatology at Tufts Medical Center, Boston.
The study by Dr. Driban and his colleagues was published in Arthritis Care & Research (2014 April 29 [doi:10.1002/acr.22359]).
A total of 1,930 participants in the Osteoarthritis Initiative, all with a KL grade of 0 or 1 on baseline bilateral radiographs, were asked at baseline and at each annual visit whether they had ever been "injured enough to limit ability to walk for at least 2 days."
On follow-up, 1,325 had no knee OA, 54 had accelerated knee OA, and 187 had typical knee OA, defined as at least one knee increased in radiographic scoring within 48 months (excluding accelerated OA).
After exclusion of 12 patients with missing data, 30% of the accelerated OA group, 28% in the typical OA group, and 35% in the no OA group had a history of knee injury before baseline. A new knee injury was reported by 32%, 13%, and 11%, respectively, with data missing from 59 persons.
In univariate analyses, participants with accelerated knee OA were significantly older than were those with typical OA or no OA (61.8 years vs. 58 years vs. 59.2 years; P = .023) and had a greater body mass index (28.9 kg/m2 vs. 27.9 kg/m2 vs. 27.1 kg/m2; P = .002), Dr. Driban said.
In multinomial logistic regression analyses that adjusted for age, sex, BMI, presence of static knee malalignment, and systolic blood pressure, there was no association between prior knee injury and accelerated OA (odds ratio, 0.84) or typical OA (OR, 0.76).
However, when the investigators looked further, participants with accelerated OA were almost 3.5 times more likely to report a recent knee injury during the observation period (OR, 3.37; 95% confidence interval, 1.82-6.25) than were those with typical OA (OR, 0.99) or no OA (reference), he said.
Moreover, if a participant experienced a knee injury 1 year before the study outcome, the risk of accelerated OA increased ninefold (OR, 9.22; CI, 4.50-18.90) versus threefold for typical OA (OR, 3.04; CI, 1.66-5.58).
Despite the focus on injuries leading to accelerated OA, the analyses can’t rule out that accelerated OA may also cause an injury or that there could be a "vicious cycle," in which an injury can cause accelerated OA, associated with joint space loss, increased symptoms, and increased risk for subsequent injury, Dr. Driban said.
This line of thought helps explain why prior injury was not associated with accelerated knee OA, but recent injury was. As patients were free of radiographic OA at baseline, those with a history of a prior injury that could cause accelerated knee OA would already have been eliminated from the study, he explained in an interview.
Secondly, if accelerated knee OA can increase the risk of injury, knee injuries from years ago would not be related to accelerated knee OA because the disorder did not exist at the time of the injury.
Finally, there also could be a recall bias, as patients often have a hard time recalling injuries that may have happened years ago.
Despite the limitations of self-reported injuries and insufficient data regarding the type, severity, status of the meniscus, mechanism, or subsequent treatment of the knee injury, the findings represent an important "starting point" in understanding the association between injuries and accelerated osteoarthritis, Dr. Driban said.
"We need to monitor older adults who report an injury, as this may initiate accelerated OA or indicate an individual experiencing accelerated OA, and we need to determine which injuries may be related to accelerated osteoarthritis," he said at the meeting, sponsored by the Osteoarthritis Research Society International.
During the discussion following the formal presentation, Dr. David Felson, professor of medicine and epidemiology at Boston University, said, "I think what you are saying is exactly right," but suggested that the investigators exclude patients with spontaneous osteonecrosis of the knee and osteochondritis dissecans, as both conditions are more common than anticipated and can drive very rapid development of OA. Conversely, inclusion of patients with osteophyte-only knee OA would increase the number likely identified with accelerated OA, he said.
Dr. Driban reported no conflicting interests.
PARIS – Recent knee injuries are strongly associated with accelerated knee osteoarthritis, according to an analysis from the prospective, multicenter Osteoarthritis Initiative.
"Certain injuries may initiate or coincide with an accelerated cascade towards joint failure in as little as 12 months," Jeffrey Driban, Ph.D., said at the World Congress on Osteoarthritis. "In fact, 76% of individuals with an injury and accelerated knee osteoarthritis experienced their injury in the 12 months prior to the study outcome."
The study defined accelerated knee OA as progression from a Kellgren-Lawrence grade 0 or 1 on baseline bilateral radiographs to end-stage KL grade 3 or 4 within 48 months.
Although knee OA typically has been a slowly progressive disorder, 5%-17% of patients now experience accelerated forms of OA.
"If we can better characterize this phenomenon and its potential risk factors, we can provide more insights into the nature of progression in hopes of identifying an at-risk subset," said Dr. Driban of the division of rheumatology at Tufts Medical Center, Boston.
The study by Dr. Driban and his colleagues was published in Arthritis Care & Research (2014 April 29 [doi:10.1002/acr.22359]).
A total of 1,930 participants in the Osteoarthritis Initiative, all with a KL grade of 0 or 1 on baseline bilateral radiographs, were asked at baseline and at each annual visit whether they had ever been "injured enough to limit ability to walk for at least 2 days."
On follow-up, 1,325 had no knee OA, 54 had accelerated knee OA, and 187 had typical knee OA, defined as at least one knee increased in radiographic scoring within 48 months (excluding accelerated OA).
After exclusion of 12 patients with missing data, 30% of the accelerated OA group, 28% in the typical OA group, and 35% in the no OA group had a history of knee injury before baseline. A new knee injury was reported by 32%, 13%, and 11%, respectively, with data missing from 59 persons.
In univariate analyses, participants with accelerated knee OA were significantly older than were those with typical OA or no OA (61.8 years vs. 58 years vs. 59.2 years; P = .023) and had a greater body mass index (28.9 kg/m2 vs. 27.9 kg/m2 vs. 27.1 kg/m2; P = .002), Dr. Driban said.
In multinomial logistic regression analyses that adjusted for age, sex, BMI, presence of static knee malalignment, and systolic blood pressure, there was no association between prior knee injury and accelerated OA (odds ratio, 0.84) or typical OA (OR, 0.76).
However, when the investigators looked further, participants with accelerated OA were almost 3.5 times more likely to report a recent knee injury during the observation period (OR, 3.37; 95% confidence interval, 1.82-6.25) than were those with typical OA (OR, 0.99) or no OA (reference), he said.
Moreover, if a participant experienced a knee injury 1 year before the study outcome, the risk of accelerated OA increased ninefold (OR, 9.22; CI, 4.50-18.90) versus threefold for typical OA (OR, 3.04; CI, 1.66-5.58).
Despite the focus on injuries leading to accelerated OA, the analyses can’t rule out that accelerated OA may also cause an injury or that there could be a "vicious cycle," in which an injury can cause accelerated OA, associated with joint space loss, increased symptoms, and increased risk for subsequent injury, Dr. Driban said.
This line of thought helps explain why prior injury was not associated with accelerated knee OA, but recent injury was. As patients were free of radiographic OA at baseline, those with a history of a prior injury that could cause accelerated knee OA would already have been eliminated from the study, he explained in an interview.
Secondly, if accelerated knee OA can increase the risk of injury, knee injuries from years ago would not be related to accelerated knee OA because the disorder did not exist at the time of the injury.
Finally, there also could be a recall bias, as patients often have a hard time recalling injuries that may have happened years ago.
Despite the limitations of self-reported injuries and insufficient data regarding the type, severity, status of the meniscus, mechanism, or subsequent treatment of the knee injury, the findings represent an important "starting point" in understanding the association between injuries and accelerated osteoarthritis, Dr. Driban said.
"We need to monitor older adults who report an injury, as this may initiate accelerated OA or indicate an individual experiencing accelerated OA, and we need to determine which injuries may be related to accelerated osteoarthritis," he said at the meeting, sponsored by the Osteoarthritis Research Society International.
During the discussion following the formal presentation, Dr. David Felson, professor of medicine and epidemiology at Boston University, said, "I think what you are saying is exactly right," but suggested that the investigators exclude patients with spontaneous osteonecrosis of the knee and osteochondritis dissecans, as both conditions are more common than anticipated and can drive very rapid development of OA. Conversely, inclusion of patients with osteophyte-only knee OA would increase the number likely identified with accelerated OA, he said.
Dr. Driban reported no conflicting interests.
AT OARSI 2014
Key clinical point: Older adults who report a knee injury should be monitored for accelerated knee OA.
Major finding: Knee injury within 1 year of the study outcome increased the odds of accelerated OA ninefold (OR, 9.22; CI, 4.50-18.90).
Data source: Person-based analyses of 1,930 participants in the Osteoarthritis Initiative.
Disclosures: Dr. Driban reported no conflicting interests.