User login
May 2024 – ICYMI
Gastroenterology
January 2024
Hirano I, et al; ASCENT WORKING GROUP. Ascending to New Heights for Novel Therapeutics for Eosinophilic Esophagitis. Gastroenterology. 2024 Jan;166(1):1-10. doi: 10.1053/j.gastro.2023.09.004. Epub 2023 Sep 9. PMID: 37690772; PMCID: PMC10872872.
Åkerström JH, et al. Antireflux Surgery Versus Antireflux Medication and Risk of Esophageal Adenocarcinoma in Patients With Barrett’s Esophagus. Gastroenterology. 2024 Jan;166(1):132-138.e3. doi: 10.1053/j.gastro.2023.08.050. Epub 2023 Sep 9. PMID: 37690771.
Barnes EL, et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on the Management of Pouchitis and Inflammatory Pouch Disorders. Gastroenterology. 2024 Jan;166(1):59-85. doi: 10.1053/j.gastro.2023.10.015. PMID: 38128971.
February 2024
Yoo HW, et al. Helicobacter pylori Treatment and Gastric Cancer Risk After Endoscopic Resection of Dysplasia: A Nationwide Cohort Study. Gastroenterology. 2024 Feb;166(2):313-322.e3. doi: 10.1053/j.gastro.2023.10.013. Epub 2023 Oct 18. PMID: 37863270.
Yang J, et al. High Soluble Fiber Promotes Colorectal Tumorigenesis Through Modulating Gut Microbiota and Metabolites in Mice. Gastroenterology. 2024 Feb;166(2):323-337.e7. doi: 10.1053/j.gastro.2023.10.012. Epub 2023 Oct 18. PMID: 37858797.
Young E, et al. Texture and Color Enhancement Imaging Improves Colonic Adenoma Detection: A Multicenter Randomized Controlled Trial. Gastroenterology. 2024 Feb;166(2):338-340.e3. doi: 10.1053/j.gastro.2023.10.008. Epub 2023 Oct 14. PMID: 37839498.
Clinical Gastroenterology and Hepatology
January 2024
Overbeek KA, et al; Dutch Familial Pancreatic Cancer Surveillance Study work group. Intraductal Papillary Mucinous Neoplasms in High-Risk Individuals: Incidence, Growth Rate, and Malignancy Risk. Clin Gastroenterol Hepatol. 2024 Jan;22(1):62-71.e7. doi: 10.1016/j.cgh.2023.03.035. Epub 2023 Apr 7. PMID: 37031711.
Reddy CA, et al. Achalasia is Strongly Associated With Eosinophilic Esophagitis and Other Allergic Disorders. Clin Gastroenterol Hepatol. 2024 Jan;22(1):34-41.e2. doi: 10.1016/j.cgh.2023.06.013. Epub 2023 Jun 28. PMID: 37391057; PMCID: PMC10753026.
Thiruvengadam NR, et al. The Clinical Impact and Cost-Effectiveness of Surveillance of Incidentally Detected Gastric Intestinal Metaplasia: A Microsimulation Analysis. Clin Gastroenterol Hepatol. 2024 Jan;22(1):51-61. doi: 10.1016/j.cgh.2023.05.028. Epub 2023 Jun 9. Erratum in: Clin Gastroenterol Hepatol. 2024 Jan 19;: PMID: 37302442.
February 2024
Goodoory VC, et al. Systematic Review and Meta-analysis: Efficacy of Mesalamine in Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):243-251.e5. doi: 10.1016/j.cgh.2023.02.014. Epub 2023 Feb 27. PMID: 36858143.
Brenner DM, et al. Development and Current State of Digital Therapeutics for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):222-234. doi: 10.1016/j.cgh.2023.09.013. Epub 2023 Sep 22. PMID: 37743035.
Techniques and Innovations in Gastrointestinal Endoscopy
January 2024
Ramirez PR, et al. Gaps and Improvement Opportunities in Post-Colonoscopy Communication. Tech Innov Gastrointest Endosc. 2024 Jan;26(1):90-92. doi: 10.1016/j.tige.2023.10.001. Epub 2023 Oct 22.
Gonzaga ER, et al. Gastric Peroral Endoscopic Myotomy (G-POEM) for the Management of Gastroparesis. Tech Innov Gastrointest Endosc. 2024 Jan; 26(1): 46-55. doi: 10.1016/j.tige.2023.09.002. Epub 2023 Oct 13.
Wang D, et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2024 Jan;26(1): 30-37. doi: 10.1016/j.tige.2023.10.003. Epub 2023 Nov 8.
Gastro Hep Advances
January 2024
Adeniran E, et al. Intense and Sustained Alcohol Consumption Associated With Acute Pancreatitis Warrants Early Intervention. Gastro Hep Advances. 2024 Jan;3(1):61-63. doi: 10.1016/j.gastha.2023.08.017. Epub 2023 Sep 2.
Alkhouri N, et al. A Novel Prescription Digital Therapeutic Option for the Treatment of Metabolic Dysfunction-Associated Steatotic Liver Disease. Gastro Hep Advances. 2024 Jan;3(1): 9-16. doi: 10.1016/j.gastha.2023.08.019. Epub 2023 Oct 1.
Gastroenterology
January 2024
Hirano I, et al; ASCENT WORKING GROUP. Ascending to New Heights for Novel Therapeutics for Eosinophilic Esophagitis. Gastroenterology. 2024 Jan;166(1):1-10. doi: 10.1053/j.gastro.2023.09.004. Epub 2023 Sep 9. PMID: 37690772; PMCID: PMC10872872.
Åkerström JH, et al. Antireflux Surgery Versus Antireflux Medication and Risk of Esophageal Adenocarcinoma in Patients With Barrett’s Esophagus. Gastroenterology. 2024 Jan;166(1):132-138.e3. doi: 10.1053/j.gastro.2023.08.050. Epub 2023 Sep 9. PMID: 37690771.
Barnes EL, et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on the Management of Pouchitis and Inflammatory Pouch Disorders. Gastroenterology. 2024 Jan;166(1):59-85. doi: 10.1053/j.gastro.2023.10.015. PMID: 38128971.
February 2024
Yoo HW, et al. Helicobacter pylori Treatment and Gastric Cancer Risk After Endoscopic Resection of Dysplasia: A Nationwide Cohort Study. Gastroenterology. 2024 Feb;166(2):313-322.e3. doi: 10.1053/j.gastro.2023.10.013. Epub 2023 Oct 18. PMID: 37863270.
Yang J, et al. High Soluble Fiber Promotes Colorectal Tumorigenesis Through Modulating Gut Microbiota and Metabolites in Mice. Gastroenterology. 2024 Feb;166(2):323-337.e7. doi: 10.1053/j.gastro.2023.10.012. Epub 2023 Oct 18. PMID: 37858797.
Young E, et al. Texture and Color Enhancement Imaging Improves Colonic Adenoma Detection: A Multicenter Randomized Controlled Trial. Gastroenterology. 2024 Feb;166(2):338-340.e3. doi: 10.1053/j.gastro.2023.10.008. Epub 2023 Oct 14. PMID: 37839498.
Clinical Gastroenterology and Hepatology
January 2024
Overbeek KA, et al; Dutch Familial Pancreatic Cancer Surveillance Study work group. Intraductal Papillary Mucinous Neoplasms in High-Risk Individuals: Incidence, Growth Rate, and Malignancy Risk. Clin Gastroenterol Hepatol. 2024 Jan;22(1):62-71.e7. doi: 10.1016/j.cgh.2023.03.035. Epub 2023 Apr 7. PMID: 37031711.
Reddy CA, et al. Achalasia is Strongly Associated With Eosinophilic Esophagitis and Other Allergic Disorders. Clin Gastroenterol Hepatol. 2024 Jan;22(1):34-41.e2. doi: 10.1016/j.cgh.2023.06.013. Epub 2023 Jun 28. PMID: 37391057; PMCID: PMC10753026.
Thiruvengadam NR, et al. The Clinical Impact and Cost-Effectiveness of Surveillance of Incidentally Detected Gastric Intestinal Metaplasia: A Microsimulation Analysis. Clin Gastroenterol Hepatol. 2024 Jan;22(1):51-61. doi: 10.1016/j.cgh.2023.05.028. Epub 2023 Jun 9. Erratum in: Clin Gastroenterol Hepatol. 2024 Jan 19;: PMID: 37302442.
February 2024
Goodoory VC, et al. Systematic Review and Meta-analysis: Efficacy of Mesalamine in Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):243-251.e5. doi: 10.1016/j.cgh.2023.02.014. Epub 2023 Feb 27. PMID: 36858143.
Brenner DM, et al. Development and Current State of Digital Therapeutics for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):222-234. doi: 10.1016/j.cgh.2023.09.013. Epub 2023 Sep 22. PMID: 37743035.
Techniques and Innovations in Gastrointestinal Endoscopy
January 2024
Ramirez PR, et al. Gaps and Improvement Opportunities in Post-Colonoscopy Communication. Tech Innov Gastrointest Endosc. 2024 Jan;26(1):90-92. doi: 10.1016/j.tige.2023.10.001. Epub 2023 Oct 22.
Gonzaga ER, et al. Gastric Peroral Endoscopic Myotomy (G-POEM) for the Management of Gastroparesis. Tech Innov Gastrointest Endosc. 2024 Jan; 26(1): 46-55. doi: 10.1016/j.tige.2023.09.002. Epub 2023 Oct 13.
Wang D, et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2024 Jan;26(1): 30-37. doi: 10.1016/j.tige.2023.10.003. Epub 2023 Nov 8.
Gastro Hep Advances
January 2024
Adeniran E, et al. Intense and Sustained Alcohol Consumption Associated With Acute Pancreatitis Warrants Early Intervention. Gastro Hep Advances. 2024 Jan;3(1):61-63. doi: 10.1016/j.gastha.2023.08.017. Epub 2023 Sep 2.
Alkhouri N, et al. A Novel Prescription Digital Therapeutic Option for the Treatment of Metabolic Dysfunction-Associated Steatotic Liver Disease. Gastro Hep Advances. 2024 Jan;3(1): 9-16. doi: 10.1016/j.gastha.2023.08.019. Epub 2023 Oct 1.
Gastroenterology
January 2024
Hirano I, et al; ASCENT WORKING GROUP. Ascending to New Heights for Novel Therapeutics for Eosinophilic Esophagitis. Gastroenterology. 2024 Jan;166(1):1-10. doi: 10.1053/j.gastro.2023.09.004. Epub 2023 Sep 9. PMID: 37690772; PMCID: PMC10872872.
Åkerström JH, et al. Antireflux Surgery Versus Antireflux Medication and Risk of Esophageal Adenocarcinoma in Patients With Barrett’s Esophagus. Gastroenterology. 2024 Jan;166(1):132-138.e3. doi: 10.1053/j.gastro.2023.08.050. Epub 2023 Sep 9. PMID: 37690771.
Barnes EL, et al; AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on the Management of Pouchitis and Inflammatory Pouch Disorders. Gastroenterology. 2024 Jan;166(1):59-85. doi: 10.1053/j.gastro.2023.10.015. PMID: 38128971.
February 2024
Yoo HW, et al. Helicobacter pylori Treatment and Gastric Cancer Risk After Endoscopic Resection of Dysplasia: A Nationwide Cohort Study. Gastroenterology. 2024 Feb;166(2):313-322.e3. doi: 10.1053/j.gastro.2023.10.013. Epub 2023 Oct 18. PMID: 37863270.
Yang J, et al. High Soluble Fiber Promotes Colorectal Tumorigenesis Through Modulating Gut Microbiota and Metabolites in Mice. Gastroenterology. 2024 Feb;166(2):323-337.e7. doi: 10.1053/j.gastro.2023.10.012. Epub 2023 Oct 18. PMID: 37858797.
Young E, et al. Texture and Color Enhancement Imaging Improves Colonic Adenoma Detection: A Multicenter Randomized Controlled Trial. Gastroenterology. 2024 Feb;166(2):338-340.e3. doi: 10.1053/j.gastro.2023.10.008. Epub 2023 Oct 14. PMID: 37839498.
Clinical Gastroenterology and Hepatology
January 2024
Overbeek KA, et al; Dutch Familial Pancreatic Cancer Surveillance Study work group. Intraductal Papillary Mucinous Neoplasms in High-Risk Individuals: Incidence, Growth Rate, and Malignancy Risk. Clin Gastroenterol Hepatol. 2024 Jan;22(1):62-71.e7. doi: 10.1016/j.cgh.2023.03.035. Epub 2023 Apr 7. PMID: 37031711.
Reddy CA, et al. Achalasia is Strongly Associated With Eosinophilic Esophagitis and Other Allergic Disorders. Clin Gastroenterol Hepatol. 2024 Jan;22(1):34-41.e2. doi: 10.1016/j.cgh.2023.06.013. Epub 2023 Jun 28. PMID: 37391057; PMCID: PMC10753026.
Thiruvengadam NR, et al. The Clinical Impact and Cost-Effectiveness of Surveillance of Incidentally Detected Gastric Intestinal Metaplasia: A Microsimulation Analysis. Clin Gastroenterol Hepatol. 2024 Jan;22(1):51-61. doi: 10.1016/j.cgh.2023.05.028. Epub 2023 Jun 9. Erratum in: Clin Gastroenterol Hepatol. 2024 Jan 19;: PMID: 37302442.
February 2024
Goodoory VC, et al. Systematic Review and Meta-analysis: Efficacy of Mesalamine in Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):243-251.e5. doi: 10.1016/j.cgh.2023.02.014. Epub 2023 Feb 27. PMID: 36858143.
Brenner DM, et al. Development and Current State of Digital Therapeutics for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2024 Feb;22(2):222-234. doi: 10.1016/j.cgh.2023.09.013. Epub 2023 Sep 22. PMID: 37743035.
Techniques and Innovations in Gastrointestinal Endoscopy
January 2024
Ramirez PR, et al. Gaps and Improvement Opportunities in Post-Colonoscopy Communication. Tech Innov Gastrointest Endosc. 2024 Jan;26(1):90-92. doi: 10.1016/j.tige.2023.10.001. Epub 2023 Oct 22.
Gonzaga ER, et al. Gastric Peroral Endoscopic Myotomy (G-POEM) for the Management of Gastroparesis. Tech Innov Gastrointest Endosc. 2024 Jan; 26(1): 46-55. doi: 10.1016/j.tige.2023.09.002. Epub 2023 Oct 13.
Wang D, et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2024 Jan;26(1): 30-37. doi: 10.1016/j.tige.2023.10.003. Epub 2023 Nov 8.
Gastro Hep Advances
January 2024
Adeniran E, et al. Intense and Sustained Alcohol Consumption Associated With Acute Pancreatitis Warrants Early Intervention. Gastro Hep Advances. 2024 Jan;3(1):61-63. doi: 10.1016/j.gastha.2023.08.017. Epub 2023 Sep 2.
Alkhouri N, et al. A Novel Prescription Digital Therapeutic Option for the Treatment of Metabolic Dysfunction-Associated Steatotic Liver Disease. Gastro Hep Advances. 2024 Jan;3(1): 9-16. doi: 10.1016/j.gastha.2023.08.019. Epub 2023 Oct 1.
Liquid Biopsy Has Near-Perfect Accuracy for Early Pancreatic Cancer
the most common type of pancreatic cancer.
It is quite encouraging to know we have a blood test that could potentially find this disease early, said Ajay Goel, PhD, a molecular diagnostics specialist at City of Hope in Duarte, California, who presented the findings at the annual meeting of the American Association for Cancer Research (AACR).
Dr. Goel and colleagues developed a signature for pancreatic cancer based on microRNAs identified in the exomes shed from pancreatic cancers and cell-free DNA markers found in the blood of patients with the disease.
Their initial assay tested blood samples for this signature in a training cohort of 252 people in Japan, approximately 60% of whom had pancreatic cancer. The rest were healthy controls. The assay was then tested in validation cohorts of 400 subjects, half with pancreatic cancer and half controls, in China and South Korea.
In both the initial and validation tests, the microRNA assay had an accuracy of about 90% for stage I/II pancreatic cancer, already far better than commercially available assays.
In an additional validation cohort in the United States with 139 patients with pancreatic cancer and 193 controls at six centers across the country, the researchers found that adding carbohydrate antigen 19-9 — a well-known marker of pancreatic cancer — to the assay boosted the test’s accuracy to 97%.
The test performed the same whether the tumor was in the head or tail of the pancreas.
“We are very excited about this data,” said Dr. Goel.
The technology was recently licensed to Pharus Diagnostics for commercial development, which will likely include a prospective screening trial, he told this news organization.
Because pancreatic cancer is fairly uncommon, Dr. Goel did not anticipate the test being used for general screening but rather for screening high-risk patients such as those with newly diagnosed type 2 diabetes, a family history of pancreatic cancer, or predisposing genetic mutations.
“It should be a very inexpensive test; it doesn’t cost us much to do in the lab,” he added.
Study moderator Ryan Corcoran, MD, PhD, a gastrointestinal (GI) oncologist at Massachusetts General Hospital, Boston, saw the potential.
“As a GI oncologist, I know how lethal and hard to treat pancreatic cancer is,” he said. A test that could reliably detect pancreatic cancer early, with an acceptable false-positive rate, would be extremely useful.
“The cure rate is many, many times higher,” if we detect it before it has a chance to spread, he explained.
In the meantime, Dr. Goel said there’s more work to be done.
Almost 4,000 subjects have been enrolled in ongoing validation efforts, and efforts are underway to use the test to screen thousands of banked blood samples from the PLCO, a prospective cancer screening trial in healthy subjects.
The researchers also want to see if the test can distinguish benign pancreatic cysts from ones that turn cancerous.
The idea is to find the earliest possible signs of this disease to see if we can find it not “at the moment of clinical diagnosis, but possibly 6 months, 1 year, 2 years earlier” than with radiologic imaging, Dr. Goel said.
The work was funded by the National Cancer Institute and others. Dr. Goel is a consultant for Pharus Diagnostics and Cellomics. Dr. Corcoran is a consultant for, has grants from, and/or holds stock in numerous companies, including Pfizer, Novartis, Eli Lilly, and Revolution Medicines.
A version of this article appeared on Medscape.com.
the most common type of pancreatic cancer.
It is quite encouraging to know we have a blood test that could potentially find this disease early, said Ajay Goel, PhD, a molecular diagnostics specialist at City of Hope in Duarte, California, who presented the findings at the annual meeting of the American Association for Cancer Research (AACR).
Dr. Goel and colleagues developed a signature for pancreatic cancer based on microRNAs identified in the exomes shed from pancreatic cancers and cell-free DNA markers found in the blood of patients with the disease.
Their initial assay tested blood samples for this signature in a training cohort of 252 people in Japan, approximately 60% of whom had pancreatic cancer. The rest were healthy controls. The assay was then tested in validation cohorts of 400 subjects, half with pancreatic cancer and half controls, in China and South Korea.
In both the initial and validation tests, the microRNA assay had an accuracy of about 90% for stage I/II pancreatic cancer, already far better than commercially available assays.
In an additional validation cohort in the United States with 139 patients with pancreatic cancer and 193 controls at six centers across the country, the researchers found that adding carbohydrate antigen 19-9 — a well-known marker of pancreatic cancer — to the assay boosted the test’s accuracy to 97%.
The test performed the same whether the tumor was in the head or tail of the pancreas.
“We are very excited about this data,” said Dr. Goel.
The technology was recently licensed to Pharus Diagnostics for commercial development, which will likely include a prospective screening trial, he told this news organization.
Because pancreatic cancer is fairly uncommon, Dr. Goel did not anticipate the test being used for general screening but rather for screening high-risk patients such as those with newly diagnosed type 2 diabetes, a family history of pancreatic cancer, or predisposing genetic mutations.
“It should be a very inexpensive test; it doesn’t cost us much to do in the lab,” he added.
Study moderator Ryan Corcoran, MD, PhD, a gastrointestinal (GI) oncologist at Massachusetts General Hospital, Boston, saw the potential.
“As a GI oncologist, I know how lethal and hard to treat pancreatic cancer is,” he said. A test that could reliably detect pancreatic cancer early, with an acceptable false-positive rate, would be extremely useful.
“The cure rate is many, many times higher,” if we detect it before it has a chance to spread, he explained.
In the meantime, Dr. Goel said there’s more work to be done.
Almost 4,000 subjects have been enrolled in ongoing validation efforts, and efforts are underway to use the test to screen thousands of banked blood samples from the PLCO, a prospective cancer screening trial in healthy subjects.
The researchers also want to see if the test can distinguish benign pancreatic cysts from ones that turn cancerous.
The idea is to find the earliest possible signs of this disease to see if we can find it not “at the moment of clinical diagnosis, but possibly 6 months, 1 year, 2 years earlier” than with radiologic imaging, Dr. Goel said.
The work was funded by the National Cancer Institute and others. Dr. Goel is a consultant for Pharus Diagnostics and Cellomics. Dr. Corcoran is a consultant for, has grants from, and/or holds stock in numerous companies, including Pfizer, Novartis, Eli Lilly, and Revolution Medicines.
A version of this article appeared on Medscape.com.
the most common type of pancreatic cancer.
It is quite encouraging to know we have a blood test that could potentially find this disease early, said Ajay Goel, PhD, a molecular diagnostics specialist at City of Hope in Duarte, California, who presented the findings at the annual meeting of the American Association for Cancer Research (AACR).
Dr. Goel and colleagues developed a signature for pancreatic cancer based on microRNAs identified in the exomes shed from pancreatic cancers and cell-free DNA markers found in the blood of patients with the disease.
Their initial assay tested blood samples for this signature in a training cohort of 252 people in Japan, approximately 60% of whom had pancreatic cancer. The rest were healthy controls. The assay was then tested in validation cohorts of 400 subjects, half with pancreatic cancer and half controls, in China and South Korea.
In both the initial and validation tests, the microRNA assay had an accuracy of about 90% for stage I/II pancreatic cancer, already far better than commercially available assays.
In an additional validation cohort in the United States with 139 patients with pancreatic cancer and 193 controls at six centers across the country, the researchers found that adding carbohydrate antigen 19-9 — a well-known marker of pancreatic cancer — to the assay boosted the test’s accuracy to 97%.
The test performed the same whether the tumor was in the head or tail of the pancreas.
“We are very excited about this data,” said Dr. Goel.
The technology was recently licensed to Pharus Diagnostics for commercial development, which will likely include a prospective screening trial, he told this news organization.
Because pancreatic cancer is fairly uncommon, Dr. Goel did not anticipate the test being used for general screening but rather for screening high-risk patients such as those with newly diagnosed type 2 diabetes, a family history of pancreatic cancer, or predisposing genetic mutations.
“It should be a very inexpensive test; it doesn’t cost us much to do in the lab,” he added.
Study moderator Ryan Corcoran, MD, PhD, a gastrointestinal (GI) oncologist at Massachusetts General Hospital, Boston, saw the potential.
“As a GI oncologist, I know how lethal and hard to treat pancreatic cancer is,” he said. A test that could reliably detect pancreatic cancer early, with an acceptable false-positive rate, would be extremely useful.
“The cure rate is many, many times higher,” if we detect it before it has a chance to spread, he explained.
In the meantime, Dr. Goel said there’s more work to be done.
Almost 4,000 subjects have been enrolled in ongoing validation efforts, and efforts are underway to use the test to screen thousands of banked blood samples from the PLCO, a prospective cancer screening trial in healthy subjects.
The researchers also want to see if the test can distinguish benign pancreatic cysts from ones that turn cancerous.
The idea is to find the earliest possible signs of this disease to see if we can find it not “at the moment of clinical diagnosis, but possibly 6 months, 1 year, 2 years earlier” than with radiologic imaging, Dr. Goel said.
The work was funded by the National Cancer Institute and others. Dr. Goel is a consultant for Pharus Diagnostics and Cellomics. Dr. Corcoran is a consultant for, has grants from, and/or holds stock in numerous companies, including Pfizer, Novartis, Eli Lilly, and Revolution Medicines.
A version of this article appeared on Medscape.com.
FROM AACR 2024
TRAIL-targeting Therapies Still Hold Promise in Cholangiocarcinoma
primarily due to the adaptive resistance and unexpected immune modulation, according to investigators.
Those prior studies evaluated a combination of immunotherapy and TRAIL agonism, but selective TRAIL antagonism shows greater potential via dual ligand/receptor (TRAIL/TRAIL-R) targeting to block immunosuppression, reported lead author Emilien J. Loeuillard, PhD, of Mayo Clinic, Rochester, Minnesota, and colleagues.
“The TRAIL/TRAIL-R system has garnered considerable interest in cancer biology, especially as a potential anticancer therapy,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. “However, TRAIL-R agonists have had very limited anticancer activity in human beings, challenging this concept of TRAIL as an anticancer agent.”
This may be because they were working in the wrong direction, Dr. Loeuillard and colleagues suggested, citing recent work linking TRAIL with tumor proliferation and invasion, possibly via modification of the tumor immune microenvironment.
Exact mechanisms of modification, however, remain unclear. While TRAIL has been associated with tumor-promoting effects like induction of a promyeloid secretome in adenocarcinoma, it has also been linked with anticancer effects like activation of natural killer cells and cytotoxic T lymphocytes.
“Thus, the potency and hierarchy of TRAIL anticancer vs procancer processes in cancer biology has yet to be defined,” the investigators wrote.
While TRAIL ligation of cognate receptors has been previously investigated and shown to trigger proapoptotic signaling pathways, noncanonical TRAIL-mediated signaling remains largely unexplored, particularly in CCA.
The present study evaluated TRAIL biology in CCA using immunocompetent mouse models.
These experiments showed that noncanonical TRAIL signaling immunosuppresses the tumor microenvironment by increasing quantity and activity of myeloid-derived suppressor cells (MDSCs). Blocking noncanonical TRAIL signaling by selective deletion of TRAIL-R in immune cells had significantly reduced tumor volumes alongside fewer MDSCs, driven by FLICE inhibitory protein (cFLIP)-dependent nuclear factor kappa-B activation (NF-kappa-B) in MDSCs, which has antiapoptotic activity. While MDSCs present one possible target in this chain of immunosuppression, “therapeutic strategies for targeting MDSCs are limited,” the investigators wrote, noting that available myeloid modulators have fallen short in clinical trials.
Instead, cFLIP may be a convincing option, they suggested, as targeting cFLIP can sensitize cancer cells to proapoptotic TRAIL signaling. What’s more, cFLIP appears to protect MDSCs from TRAIL-mediated apoptosis, so taking out this barrier could render MDSCs susceptible to therapy.
“Our studies suggest that switching prosurvival/proliferation TRAIL signaling to canonical proapoptotic TRAIL signaling will promote MDSC apoptosis, which in turn has therapeutic implications for CCA suppression,” the investigators wrote.
Hope therefore remains for targeting TRAIL in patients with CCA, but with selective antagonism instead of agonism, as previously attempted.
“In summary, our findings support the role of selective therapeutic targeting of TRAIL-positive cancer cells in an effort to block TRAIL/TRAIL-R–mediated tumor immunosuppression,” Dr. Loeuillard and colleagues concluded.
This study was funded by the Cholangiocarcinoma Foundation and the Mayo Clinic Eagles 5th District Cancer Telethon Funds for Research Fellowship Program, the CTSA/National Center for Advancing Translational Science, the National Institutes of Health/National Cancer Institute, and others. The investigators disclosed no conflicts of interest.
The dismal response of cholangiocarcinoma to immune checkpoint inhibitors (ICI) is particularly concerning, as it impedes the adoption of combination regimens, now standard in most solid tumors. Strategies modulating selective genes involved in the tumor inflammatory environment and tumor cell viability, including those within the tumor necrosis factor superfamily, parallel the mechanism of action of ICI and present a double-edged sword due to the context-dependent pro- and/or anticancer effects of their canonical and/or phantom roles.
Recent investigations suggest that selectively antagonizing TRAIL via (TRAIL/TRAIL-R) targeting may be more effective than agonism. Dr. Ilyas’ group from Mayo Clinic delved into the potential of TRAIL in cancer biology, particularly in CCA, shedding light on the complexities of TRAIL’s role in cancer, where both procancer and anticancer effects are observed.
Further investigation is warranted to explore how TRAIL/TRAIL-R therapy can be effectively combined with other broad-spectrum and/or targeted therapies to maximize selective toxicity to CCA cells, sparing the nonmalignant tissue, thereby extending the lifespan of CCA patients as well as assessing its preventive potential in predisposed premalignant stages, including cholestasis patients.
Sungjin Ko, DVM, PhD, is assistant professor in the Division of Experimental Pathology at the University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania. He is also a member of the Pittsburgh Liver Research Center. He reported no conflicts of interest.
The dismal response of cholangiocarcinoma to immune checkpoint inhibitors (ICI) is particularly concerning, as it impedes the adoption of combination regimens, now standard in most solid tumors. Strategies modulating selective genes involved in the tumor inflammatory environment and tumor cell viability, including those within the tumor necrosis factor superfamily, parallel the mechanism of action of ICI and present a double-edged sword due to the context-dependent pro- and/or anticancer effects of their canonical and/or phantom roles.
Recent investigations suggest that selectively antagonizing TRAIL via (TRAIL/TRAIL-R) targeting may be more effective than agonism. Dr. Ilyas’ group from Mayo Clinic delved into the potential of TRAIL in cancer biology, particularly in CCA, shedding light on the complexities of TRAIL’s role in cancer, where both procancer and anticancer effects are observed.
Further investigation is warranted to explore how TRAIL/TRAIL-R therapy can be effectively combined with other broad-spectrum and/or targeted therapies to maximize selective toxicity to CCA cells, sparing the nonmalignant tissue, thereby extending the lifespan of CCA patients as well as assessing its preventive potential in predisposed premalignant stages, including cholestasis patients.
Sungjin Ko, DVM, PhD, is assistant professor in the Division of Experimental Pathology at the University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania. He is also a member of the Pittsburgh Liver Research Center. He reported no conflicts of interest.
The dismal response of cholangiocarcinoma to immune checkpoint inhibitors (ICI) is particularly concerning, as it impedes the adoption of combination regimens, now standard in most solid tumors. Strategies modulating selective genes involved in the tumor inflammatory environment and tumor cell viability, including those within the tumor necrosis factor superfamily, parallel the mechanism of action of ICI and present a double-edged sword due to the context-dependent pro- and/or anticancer effects of their canonical and/or phantom roles.
Recent investigations suggest that selectively antagonizing TRAIL via (TRAIL/TRAIL-R) targeting may be more effective than agonism. Dr. Ilyas’ group from Mayo Clinic delved into the potential of TRAIL in cancer biology, particularly in CCA, shedding light on the complexities of TRAIL’s role in cancer, where both procancer and anticancer effects are observed.
Further investigation is warranted to explore how TRAIL/TRAIL-R therapy can be effectively combined with other broad-spectrum and/or targeted therapies to maximize selective toxicity to CCA cells, sparing the nonmalignant tissue, thereby extending the lifespan of CCA patients as well as assessing its preventive potential in predisposed premalignant stages, including cholestasis patients.
Sungjin Ko, DVM, PhD, is assistant professor in the Division of Experimental Pathology at the University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania. He is also a member of the Pittsburgh Liver Research Center. He reported no conflicts of interest.
primarily due to the adaptive resistance and unexpected immune modulation, according to investigators.
Those prior studies evaluated a combination of immunotherapy and TRAIL agonism, but selective TRAIL antagonism shows greater potential via dual ligand/receptor (TRAIL/TRAIL-R) targeting to block immunosuppression, reported lead author Emilien J. Loeuillard, PhD, of Mayo Clinic, Rochester, Minnesota, and colleagues.
“The TRAIL/TRAIL-R system has garnered considerable interest in cancer biology, especially as a potential anticancer therapy,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. “However, TRAIL-R agonists have had very limited anticancer activity in human beings, challenging this concept of TRAIL as an anticancer agent.”
This may be because they were working in the wrong direction, Dr. Loeuillard and colleagues suggested, citing recent work linking TRAIL with tumor proliferation and invasion, possibly via modification of the tumor immune microenvironment.
Exact mechanisms of modification, however, remain unclear. While TRAIL has been associated with tumor-promoting effects like induction of a promyeloid secretome in adenocarcinoma, it has also been linked with anticancer effects like activation of natural killer cells and cytotoxic T lymphocytes.
“Thus, the potency and hierarchy of TRAIL anticancer vs procancer processes in cancer biology has yet to be defined,” the investigators wrote.
While TRAIL ligation of cognate receptors has been previously investigated and shown to trigger proapoptotic signaling pathways, noncanonical TRAIL-mediated signaling remains largely unexplored, particularly in CCA.
The present study evaluated TRAIL biology in CCA using immunocompetent mouse models.
These experiments showed that noncanonical TRAIL signaling immunosuppresses the tumor microenvironment by increasing quantity and activity of myeloid-derived suppressor cells (MDSCs). Blocking noncanonical TRAIL signaling by selective deletion of TRAIL-R in immune cells had significantly reduced tumor volumes alongside fewer MDSCs, driven by FLICE inhibitory protein (cFLIP)-dependent nuclear factor kappa-B activation (NF-kappa-B) in MDSCs, which has antiapoptotic activity. While MDSCs present one possible target in this chain of immunosuppression, “therapeutic strategies for targeting MDSCs are limited,” the investigators wrote, noting that available myeloid modulators have fallen short in clinical trials.
Instead, cFLIP may be a convincing option, they suggested, as targeting cFLIP can sensitize cancer cells to proapoptotic TRAIL signaling. What’s more, cFLIP appears to protect MDSCs from TRAIL-mediated apoptosis, so taking out this barrier could render MDSCs susceptible to therapy.
“Our studies suggest that switching prosurvival/proliferation TRAIL signaling to canonical proapoptotic TRAIL signaling will promote MDSC apoptosis, which in turn has therapeutic implications for CCA suppression,” the investigators wrote.
Hope therefore remains for targeting TRAIL in patients with CCA, but with selective antagonism instead of agonism, as previously attempted.
“In summary, our findings support the role of selective therapeutic targeting of TRAIL-positive cancer cells in an effort to block TRAIL/TRAIL-R–mediated tumor immunosuppression,” Dr. Loeuillard and colleagues concluded.
This study was funded by the Cholangiocarcinoma Foundation and the Mayo Clinic Eagles 5th District Cancer Telethon Funds for Research Fellowship Program, the CTSA/National Center for Advancing Translational Science, the National Institutes of Health/National Cancer Institute, and others. The investigators disclosed no conflicts of interest.
primarily due to the adaptive resistance and unexpected immune modulation, according to investigators.
Those prior studies evaluated a combination of immunotherapy and TRAIL agonism, but selective TRAIL antagonism shows greater potential via dual ligand/receptor (TRAIL/TRAIL-R) targeting to block immunosuppression, reported lead author Emilien J. Loeuillard, PhD, of Mayo Clinic, Rochester, Minnesota, and colleagues.
“The TRAIL/TRAIL-R system has garnered considerable interest in cancer biology, especially as a potential anticancer therapy,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. “However, TRAIL-R agonists have had very limited anticancer activity in human beings, challenging this concept of TRAIL as an anticancer agent.”
This may be because they were working in the wrong direction, Dr. Loeuillard and colleagues suggested, citing recent work linking TRAIL with tumor proliferation and invasion, possibly via modification of the tumor immune microenvironment.
Exact mechanisms of modification, however, remain unclear. While TRAIL has been associated with tumor-promoting effects like induction of a promyeloid secretome in adenocarcinoma, it has also been linked with anticancer effects like activation of natural killer cells and cytotoxic T lymphocytes.
“Thus, the potency and hierarchy of TRAIL anticancer vs procancer processes in cancer biology has yet to be defined,” the investigators wrote.
While TRAIL ligation of cognate receptors has been previously investigated and shown to trigger proapoptotic signaling pathways, noncanonical TRAIL-mediated signaling remains largely unexplored, particularly in CCA.
The present study evaluated TRAIL biology in CCA using immunocompetent mouse models.
These experiments showed that noncanonical TRAIL signaling immunosuppresses the tumor microenvironment by increasing quantity and activity of myeloid-derived suppressor cells (MDSCs). Blocking noncanonical TRAIL signaling by selective deletion of TRAIL-R in immune cells had significantly reduced tumor volumes alongside fewer MDSCs, driven by FLICE inhibitory protein (cFLIP)-dependent nuclear factor kappa-B activation (NF-kappa-B) in MDSCs, which has antiapoptotic activity. While MDSCs present one possible target in this chain of immunosuppression, “therapeutic strategies for targeting MDSCs are limited,” the investigators wrote, noting that available myeloid modulators have fallen short in clinical trials.
Instead, cFLIP may be a convincing option, they suggested, as targeting cFLIP can sensitize cancer cells to proapoptotic TRAIL signaling. What’s more, cFLIP appears to protect MDSCs from TRAIL-mediated apoptosis, so taking out this barrier could render MDSCs susceptible to therapy.
“Our studies suggest that switching prosurvival/proliferation TRAIL signaling to canonical proapoptotic TRAIL signaling will promote MDSC apoptosis, which in turn has therapeutic implications for CCA suppression,” the investigators wrote.
Hope therefore remains for targeting TRAIL in patients with CCA, but with selective antagonism instead of agonism, as previously attempted.
“In summary, our findings support the role of selective therapeutic targeting of TRAIL-positive cancer cells in an effort to block TRAIL/TRAIL-R–mediated tumor immunosuppression,” Dr. Loeuillard and colleagues concluded.
This study was funded by the Cholangiocarcinoma Foundation and the Mayo Clinic Eagles 5th District Cancer Telethon Funds for Research Fellowship Program, the CTSA/National Center for Advancing Translational Science, the National Institutes of Health/National Cancer Institute, and others. The investigators disclosed no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
February 2024 – ICYMI
Gastroenterology
October 2023
El-Salhy M et al. Efficacy of Fecal Microbiota Transplantation for Patients With Irritable Bowel Syndrome at 3 Years After Transplantation. Gastroenterology. 2022 Oct;163(4):982-994.e14. doi: 10.1053/j.gastro.2022.06.020. Epub 2022 Jun 14. PMID: 35709830.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-851. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
Lo CH et al. Association of Proton Pump Inhibitor Use With All-Cause and Cause-Specific Mortality. Gastroenterology. 2022 Oct;163(4):852-861.e2. doi: 10.1053/j.gastro.2022.06.067. Epub 2022 Jul 1. PMID: 35788344; PMCID: PMC9509450.
November 2023
Khoshiwal AM et al. The Tissue Systems Pathology Test Outperforms Pathology Review in Risk Stratifying Patients With Low-Grade Dysplasia. Gastroenterology. 2023 Nov;165(5):1168-1179.e6. doi: 10.1053/j.gastro.2023.07.029. Epub 2023 Aug 30. PMID: 37657759.
Chen YI et al. Endoscopic Ultrasound-Guided Biliary Drainage of First Intent With a Lumen-Apposing Metal Stent vs Endoscopic Retrograde Cholangiopancreatography in Malignant Distal Biliary Obstruction: A Multicenter Randomized Controlled Study (ELEMENT Trial). Gastroenterology. 2023 Nov;165(5):1249-1261.e5. doi: 10.1053/j.gastro.2023.07.024. Epub 2023 Aug 6. PMID: 37549753.
December 2023
Almario CV et al. Prevalence and Burden of Illness of Rome IV Irritable Bowel Syndrome in the United States: Results From a Nationwide Cross-Sectional Study. Gastroenterology. 2023 Dec;165(6):1475-1487. doi: 10.1053/j.gastro.2023.08.010. Epub 2023 Aug 16. PMID: 37595647.
Koopmann BDM et al. The Natural Disease Course of Pancreatic Cyst-Associated Neoplasia, Dysplasia, and Ductal Adenocarcinoma: Results of a Microsimulation Model. Gastroenterology. 2023 Dec;165(6):1522-1532. doi: 10.1053/j.gastro.2023.08.027. Epub 2023 Aug 24. PMID: 37633497.
Clinical Gastroenterology and Hepatology
October 2023
Jung DH et al. Comparison of a Polysaccharide Hemostatic Powder and Conventional Therapy for Peptic Ulcer Bleeding. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2844-2253.e5. doi: 10.1016/j.cgh.2023.02.031. Epub 2023 Mar 10. PMID: 36906081.
Liang PS et al. Blood Test Increases Colorectal Cancer Screening in Persons Who Declined Colonoscopy and Fecal Immunochemical Test: A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2951-2957.e2. doi: 10.1016/j.cgh.2023.03.036. Epub 2023 Apr 8. PMID: 37037262; PMCID: PMC10523873.
November 2023
Li YK et al. Risk of Postcolonoscopy Thromboembolic Events: A Real-World Cohort Study. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3051-3059.e4. doi: 10.1016/j.cgh.2022.09.021. Epub 2022 Sep 24. PMID: 36167228.
Tome J et al. Bile Acid Sequestrants in Microscopic Colitis: Clinical Outcomes and Utility of Bile Acid Testing. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3125-3131.e2. doi: 10.1016/j.cgh.2023.04.031. Epub 2023 May 10. PMID: 37172800.
Berry SK et al. A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3152-3159.e2. doi: 10.1016/j.cgh.2023.06.015. Epub 2023 Jun 28. PMID: 37391055.
December 2023
Kanwal F et al. Risk Stratification Model for Hepatocellular Cancer in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3296-3304.e3. doi: 10.1016/j.cgh.2023.04.019. Epub 2023 Apr 30. PMID: 37390101; PMCID: PMC10661677.
Forss A et al. Patients With Microscopic Colitis Are at Higher Risk of Major Adverse Cardiovascular Events: A Matched Cohort Study. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3356-3364.e9. doi: 10.1016/j.cgh.2023.05.014. Epub 2023 May 26. PMID: 37245713.
Zheng T et al. A Randomized, Controlled Trial of Efficacy and Safety of Cannabidiol in Idiopathic and Diabetic Gastroparesis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3405-3414.e4. doi: 10.1016/j.cgh.2023.07.008. Epub 2023 Jul 22. PMID: 37482172.
Techniques and Innovations in Gastrointestinal Endoscopy
Rengarajan A and Aadam A. Peroral Endoscopic Myotomy (POEM) and Its Use in Esophageal Dysmotility. Tech Innov Gastrointest Endosc. 2023 Dec 16. doi: 10.1016/j.tige.2023.12.004.
Wang D et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2023 Nov 7. doi: 10.1016/j.tige.2023.10.003
Gastro Hep Advances
Gregory MH et al. Short Bowel Syndrome: Transition of Pediatric Patients to Adult Gastroenterology Care. Gastro Hep Advances. 2023 Sep 8. doi: 10.1016/j.gastha.2023.09.006.
Viser AC et al. Inflammatory Bowel Disease Patients in the Ambulatory Setting Commonly Screen Positive for Malnutrition. Gastro Hep Advances. 2023 Nov 16. doi: 10.1016/j.gastha.2023.11.007.
Gastroenterology
October 2023
El-Salhy M et al. Efficacy of Fecal Microbiota Transplantation for Patients With Irritable Bowel Syndrome at 3 Years After Transplantation. Gastroenterology. 2022 Oct;163(4):982-994.e14. doi: 10.1053/j.gastro.2022.06.020. Epub 2022 Jun 14. PMID: 35709830.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-851. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
Lo CH et al. Association of Proton Pump Inhibitor Use With All-Cause and Cause-Specific Mortality. Gastroenterology. 2022 Oct;163(4):852-861.e2. doi: 10.1053/j.gastro.2022.06.067. Epub 2022 Jul 1. PMID: 35788344; PMCID: PMC9509450.
November 2023
Khoshiwal AM et al. The Tissue Systems Pathology Test Outperforms Pathology Review in Risk Stratifying Patients With Low-Grade Dysplasia. Gastroenterology. 2023 Nov;165(5):1168-1179.e6. doi: 10.1053/j.gastro.2023.07.029. Epub 2023 Aug 30. PMID: 37657759.
Chen YI et al. Endoscopic Ultrasound-Guided Biliary Drainage of First Intent With a Lumen-Apposing Metal Stent vs Endoscopic Retrograde Cholangiopancreatography in Malignant Distal Biliary Obstruction: A Multicenter Randomized Controlled Study (ELEMENT Trial). Gastroenterology. 2023 Nov;165(5):1249-1261.e5. doi: 10.1053/j.gastro.2023.07.024. Epub 2023 Aug 6. PMID: 37549753.
December 2023
Almario CV et al. Prevalence and Burden of Illness of Rome IV Irritable Bowel Syndrome in the United States: Results From a Nationwide Cross-Sectional Study. Gastroenterology. 2023 Dec;165(6):1475-1487. doi: 10.1053/j.gastro.2023.08.010. Epub 2023 Aug 16. PMID: 37595647.
Koopmann BDM et al. The Natural Disease Course of Pancreatic Cyst-Associated Neoplasia, Dysplasia, and Ductal Adenocarcinoma: Results of a Microsimulation Model. Gastroenterology. 2023 Dec;165(6):1522-1532. doi: 10.1053/j.gastro.2023.08.027. Epub 2023 Aug 24. PMID: 37633497.
Clinical Gastroenterology and Hepatology
October 2023
Jung DH et al. Comparison of a Polysaccharide Hemostatic Powder and Conventional Therapy for Peptic Ulcer Bleeding. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2844-2253.e5. doi: 10.1016/j.cgh.2023.02.031. Epub 2023 Mar 10. PMID: 36906081.
Liang PS et al. Blood Test Increases Colorectal Cancer Screening in Persons Who Declined Colonoscopy and Fecal Immunochemical Test: A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2951-2957.e2. doi: 10.1016/j.cgh.2023.03.036. Epub 2023 Apr 8. PMID: 37037262; PMCID: PMC10523873.
November 2023
Li YK et al. Risk of Postcolonoscopy Thromboembolic Events: A Real-World Cohort Study. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3051-3059.e4. doi: 10.1016/j.cgh.2022.09.021. Epub 2022 Sep 24. PMID: 36167228.
Tome J et al. Bile Acid Sequestrants in Microscopic Colitis: Clinical Outcomes and Utility of Bile Acid Testing. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3125-3131.e2. doi: 10.1016/j.cgh.2023.04.031. Epub 2023 May 10. PMID: 37172800.
Berry SK et al. A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3152-3159.e2. doi: 10.1016/j.cgh.2023.06.015. Epub 2023 Jun 28. PMID: 37391055.
December 2023
Kanwal F et al. Risk Stratification Model for Hepatocellular Cancer in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3296-3304.e3. doi: 10.1016/j.cgh.2023.04.019. Epub 2023 Apr 30. PMID: 37390101; PMCID: PMC10661677.
Forss A et al. Patients With Microscopic Colitis Are at Higher Risk of Major Adverse Cardiovascular Events: A Matched Cohort Study. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3356-3364.e9. doi: 10.1016/j.cgh.2023.05.014. Epub 2023 May 26. PMID: 37245713.
Zheng T et al. A Randomized, Controlled Trial of Efficacy and Safety of Cannabidiol in Idiopathic and Diabetic Gastroparesis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3405-3414.e4. doi: 10.1016/j.cgh.2023.07.008. Epub 2023 Jul 22. PMID: 37482172.
Techniques and Innovations in Gastrointestinal Endoscopy
Rengarajan A and Aadam A. Peroral Endoscopic Myotomy (POEM) and Its Use in Esophageal Dysmotility. Tech Innov Gastrointest Endosc. 2023 Dec 16. doi: 10.1016/j.tige.2023.12.004.
Wang D et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2023 Nov 7. doi: 10.1016/j.tige.2023.10.003
Gastro Hep Advances
Gregory MH et al. Short Bowel Syndrome: Transition of Pediatric Patients to Adult Gastroenterology Care. Gastro Hep Advances. 2023 Sep 8. doi: 10.1016/j.gastha.2023.09.006.
Viser AC et al. Inflammatory Bowel Disease Patients in the Ambulatory Setting Commonly Screen Positive for Malnutrition. Gastro Hep Advances. 2023 Nov 16. doi: 10.1016/j.gastha.2023.11.007.
Gastroenterology
October 2023
El-Salhy M et al. Efficacy of Fecal Microbiota Transplantation for Patients With Irritable Bowel Syndrome at 3 Years After Transplantation. Gastroenterology. 2022 Oct;163(4):982-994.e14. doi: 10.1053/j.gastro.2022.06.020. Epub 2022 Jun 14. PMID: 35709830.
Bajaj JS and Nagy LE. Natural History of Alcohol-Associated Liver Disease: Understanding the Changing Landscape of Pathophysiology and Patient Care. Gastroenterology. 2022 Oct;163(4):840-851. doi: 10.1053/j.gastro.2022.05.031. Epub 2022 May 19. PMID: 35598629; PMCID: PMC9509416.
Lo CH et al. Association of Proton Pump Inhibitor Use With All-Cause and Cause-Specific Mortality. Gastroenterology. 2022 Oct;163(4):852-861.e2. doi: 10.1053/j.gastro.2022.06.067. Epub 2022 Jul 1. PMID: 35788344; PMCID: PMC9509450.
November 2023
Khoshiwal AM et al. The Tissue Systems Pathology Test Outperforms Pathology Review in Risk Stratifying Patients With Low-Grade Dysplasia. Gastroenterology. 2023 Nov;165(5):1168-1179.e6. doi: 10.1053/j.gastro.2023.07.029. Epub 2023 Aug 30. PMID: 37657759.
Chen YI et al. Endoscopic Ultrasound-Guided Biliary Drainage of First Intent With a Lumen-Apposing Metal Stent vs Endoscopic Retrograde Cholangiopancreatography in Malignant Distal Biliary Obstruction: A Multicenter Randomized Controlled Study (ELEMENT Trial). Gastroenterology. 2023 Nov;165(5):1249-1261.e5. doi: 10.1053/j.gastro.2023.07.024. Epub 2023 Aug 6. PMID: 37549753.
December 2023
Almario CV et al. Prevalence and Burden of Illness of Rome IV Irritable Bowel Syndrome in the United States: Results From a Nationwide Cross-Sectional Study. Gastroenterology. 2023 Dec;165(6):1475-1487. doi: 10.1053/j.gastro.2023.08.010. Epub 2023 Aug 16. PMID: 37595647.
Koopmann BDM et al. The Natural Disease Course of Pancreatic Cyst-Associated Neoplasia, Dysplasia, and Ductal Adenocarcinoma: Results of a Microsimulation Model. Gastroenterology. 2023 Dec;165(6):1522-1532. doi: 10.1053/j.gastro.2023.08.027. Epub 2023 Aug 24. PMID: 37633497.
Clinical Gastroenterology and Hepatology
October 2023
Jung DH et al. Comparison of a Polysaccharide Hemostatic Powder and Conventional Therapy for Peptic Ulcer Bleeding. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2844-2253.e5. doi: 10.1016/j.cgh.2023.02.031. Epub 2023 Mar 10. PMID: 36906081.
Liang PS et al. Blood Test Increases Colorectal Cancer Screening in Persons Who Declined Colonoscopy and Fecal Immunochemical Test: A Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2023 Oct;21(11):2951-2957.e2. doi: 10.1016/j.cgh.2023.03.036. Epub 2023 Apr 8. PMID: 37037262; PMCID: PMC10523873.
November 2023
Li YK et al. Risk of Postcolonoscopy Thromboembolic Events: A Real-World Cohort Study. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3051-3059.e4. doi: 10.1016/j.cgh.2022.09.021. Epub 2022 Sep 24. PMID: 36167228.
Tome J et al. Bile Acid Sequestrants in Microscopic Colitis: Clinical Outcomes and Utility of Bile Acid Testing. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3125-3131.e2. doi: 10.1016/j.cgh.2023.04.031. Epub 2023 May 10. PMID: 37172800.
Berry SK et al. A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome. Clin Gastroenterol Hepatol. 2023 Nov;21(12):3152-3159.e2. doi: 10.1016/j.cgh.2023.06.015. Epub 2023 Jun 28. PMID: 37391055.
December 2023
Kanwal F et al. Risk Stratification Model for Hepatocellular Cancer in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3296-3304.e3. doi: 10.1016/j.cgh.2023.04.019. Epub 2023 Apr 30. PMID: 37390101; PMCID: PMC10661677.
Forss A et al. Patients With Microscopic Colitis Are at Higher Risk of Major Adverse Cardiovascular Events: A Matched Cohort Study. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3356-3364.e9. doi: 10.1016/j.cgh.2023.05.014. Epub 2023 May 26. PMID: 37245713.
Zheng T et al. A Randomized, Controlled Trial of Efficacy and Safety of Cannabidiol in Idiopathic and Diabetic Gastroparesis. Clin Gastroenterol Hepatol. 2023 Dec;21(13):3405-3414.e4. doi: 10.1016/j.cgh.2023.07.008. Epub 2023 Jul 22. PMID: 37482172.
Techniques and Innovations in Gastrointestinal Endoscopy
Rengarajan A and Aadam A. Peroral Endoscopic Myotomy (POEM) and Its Use in Esophageal Dysmotility. Tech Innov Gastrointest Endosc. 2023 Dec 16. doi: 10.1016/j.tige.2023.12.004.
Wang D et al. Sphincterotomy vs Sham Procedure for Pain Relief in Sphincter of Oddi Dysfunction: Systematic Review and Meta-analysis. Tech Innov Gastrointest Endosc. 2023 Nov 7. doi: 10.1016/j.tige.2023.10.003
Gastro Hep Advances
Gregory MH et al. Short Bowel Syndrome: Transition of Pediatric Patients to Adult Gastroenterology Care. Gastro Hep Advances. 2023 Sep 8. doi: 10.1016/j.gastha.2023.09.006.
Viser AC et al. Inflammatory Bowel Disease Patients in the Ambulatory Setting Commonly Screen Positive for Malnutrition. Gastro Hep Advances. 2023 Nov 16. doi: 10.1016/j.gastha.2023.11.007.
What's your diagnosis?
The diagnosis
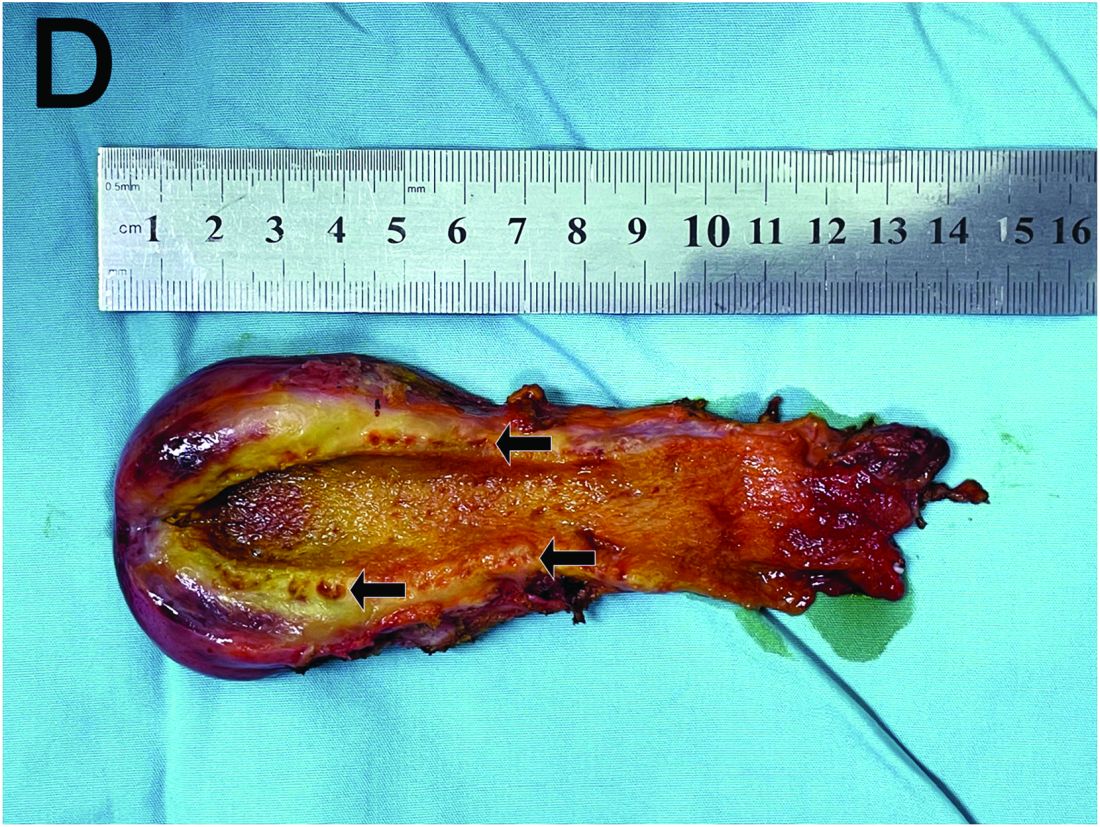
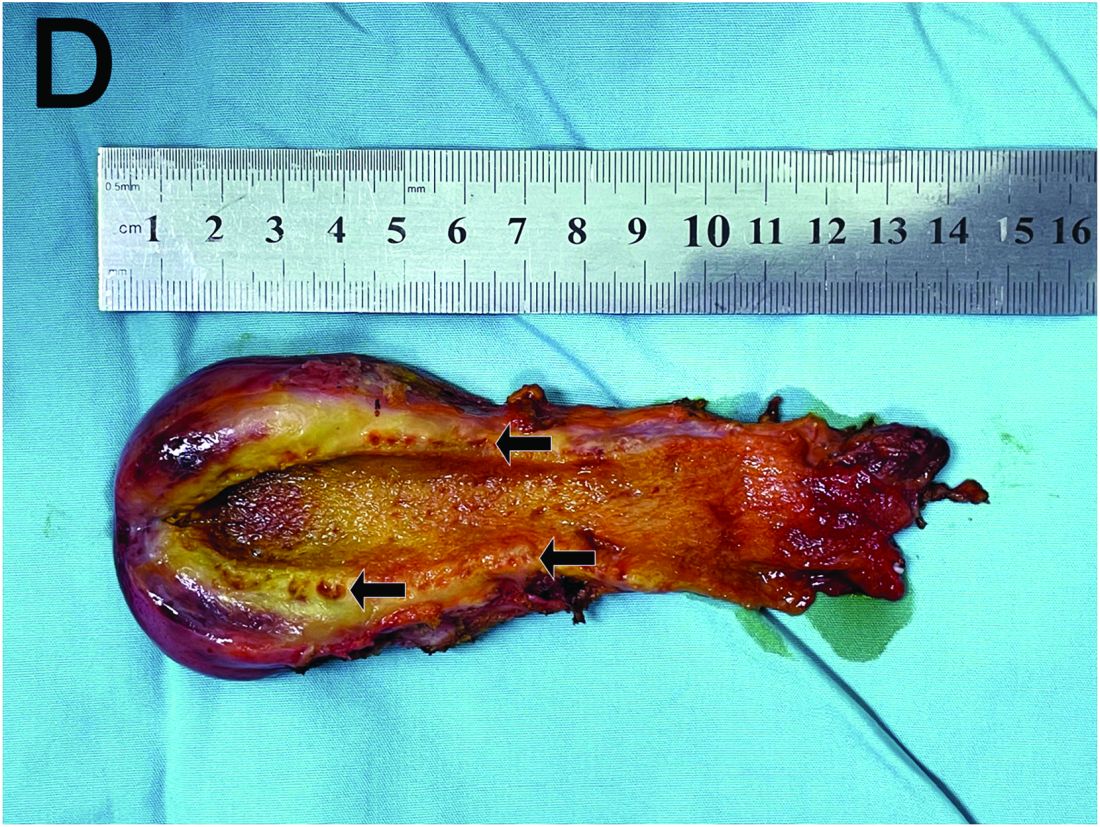
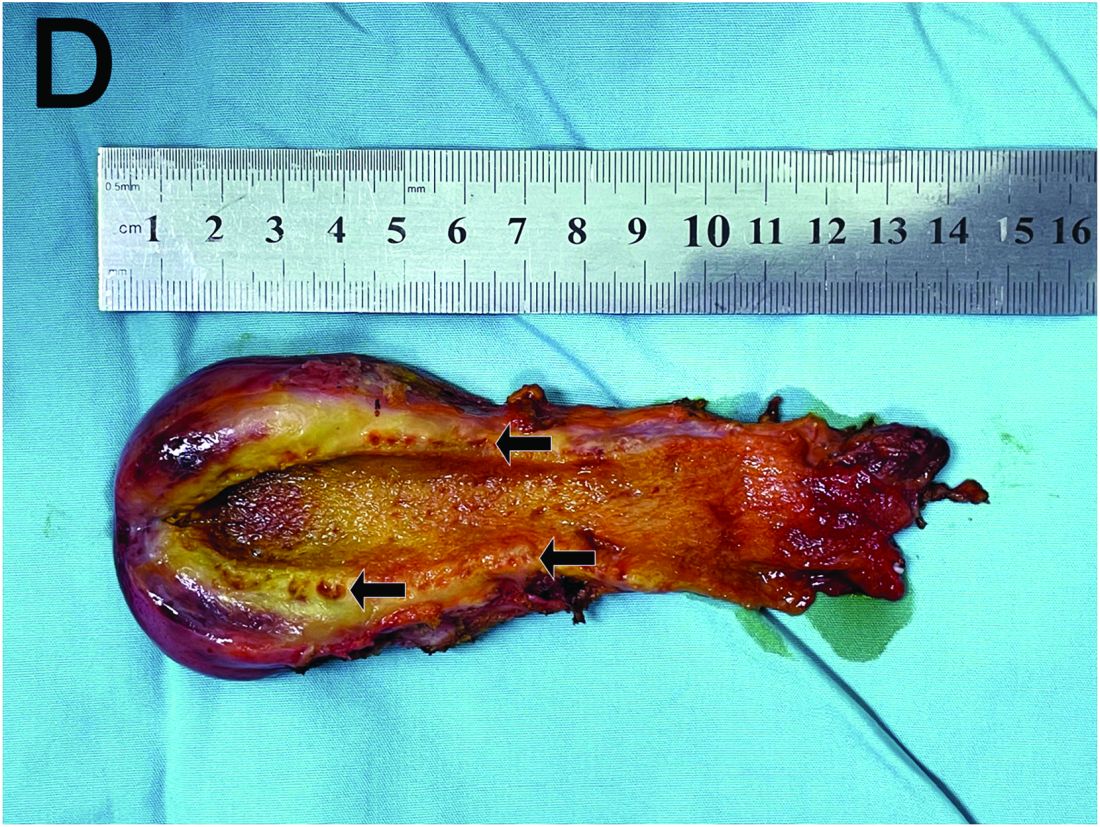
Based on the clinical and imaging findings, a diagnosis of gallbladder adenomyomatosis was made. GA is a benign and usually asymptomatic condition that occurs mainly beyond the age of 50-60 years and is very rare in childhood.1 Symptomatic gallbladder adenomyomatosis indicates cholecystectomy, considering the presence of inflammation or gallbladder stones.2 Therefore, a laparoscopic cholecystectomy was performed on our patient. Rokitansky-Aschoff sinuses were seen in the entire thickened gallbladder wall on gross pathologic examination (Figure D). Histopathologic examination confirmed the diagnosis of GA with cholecystitis. The patient was eventually diagnosed with diffuse GA. She was successfully discharged from the hospital 4 days after surgery, and 3 months of follow-up were uneventful.
References
Eroglu N et al. Diffuse adenomyomatosis of the gallbladder in a child. J Pediatr Hematol Oncol. 2016;38:e307-9.
Bonatti M. et al. Gallbladder adenomyomatosis: imaging findings, tricks and pitfalls. Insights Imaging. 2017;8:243-53.
Hammad AY et al. A literature review of radiological findings to guide the diagnosis of gallbladder adenomyomatosis. HPB (Oxford). 2016;18:129-35.
The diagnosis
Based on the clinical and imaging findings, a diagnosis of gallbladder adenomyomatosis was made. GA is a benign and usually asymptomatic condition that occurs mainly beyond the age of 50-60 years and is very rare in childhood.1 Symptomatic gallbladder adenomyomatosis indicates cholecystectomy, considering the presence of inflammation or gallbladder stones.2 Therefore, a laparoscopic cholecystectomy was performed on our patient. Rokitansky-Aschoff sinuses were seen in the entire thickened gallbladder wall on gross pathologic examination (Figure D). Histopathologic examination confirmed the diagnosis of GA with cholecystitis. The patient was eventually diagnosed with diffuse GA. She was successfully discharged from the hospital 4 days after surgery, and 3 months of follow-up were uneventful.
References
Eroglu N et al. Diffuse adenomyomatosis of the gallbladder in a child. J Pediatr Hematol Oncol. 2016;38:e307-9.
Bonatti M. et al. Gallbladder adenomyomatosis: imaging findings, tricks and pitfalls. Insights Imaging. 2017;8:243-53.
Hammad AY et al. A literature review of radiological findings to guide the diagnosis of gallbladder adenomyomatosis. HPB (Oxford). 2016;18:129-35.
The diagnosis
Based on the clinical and imaging findings, a diagnosis of gallbladder adenomyomatosis was made. GA is a benign and usually asymptomatic condition that occurs mainly beyond the age of 50-60 years and is very rare in childhood.1 Symptomatic gallbladder adenomyomatosis indicates cholecystectomy, considering the presence of inflammation or gallbladder stones.2 Therefore, a laparoscopic cholecystectomy was performed on our patient. Rokitansky-Aschoff sinuses were seen in the entire thickened gallbladder wall on gross pathologic examination (Figure D). Histopathologic examination confirmed the diagnosis of GA with cholecystitis. The patient was eventually diagnosed with diffuse GA. She was successfully discharged from the hospital 4 days after surgery, and 3 months of follow-up were uneventful.
References
Eroglu N et al. Diffuse adenomyomatosis of the gallbladder in a child. J Pediatr Hematol Oncol. 2016;38:e307-9.
Bonatti M. et al. Gallbladder adenomyomatosis: imaging findings, tricks and pitfalls. Insights Imaging. 2017;8:243-53.
Hammad AY et al. A literature review of radiological findings to guide the diagnosis of gallbladder adenomyomatosis. HPB (Oxford). 2016;18:129-35.
A 15-year-old girl presented with an 18-month history of intermittent right upper quadrant pain that appeared after meals and was relieved after rest. She denied any nausea, vomiting, chills, diarrhea, or constipation. The patient reported no trauma. At admission, physical examination showed tenderness in the right upper abdomen without rebound or guarding. Murphy's sign was also present. The laboratory tests were unremarkable.
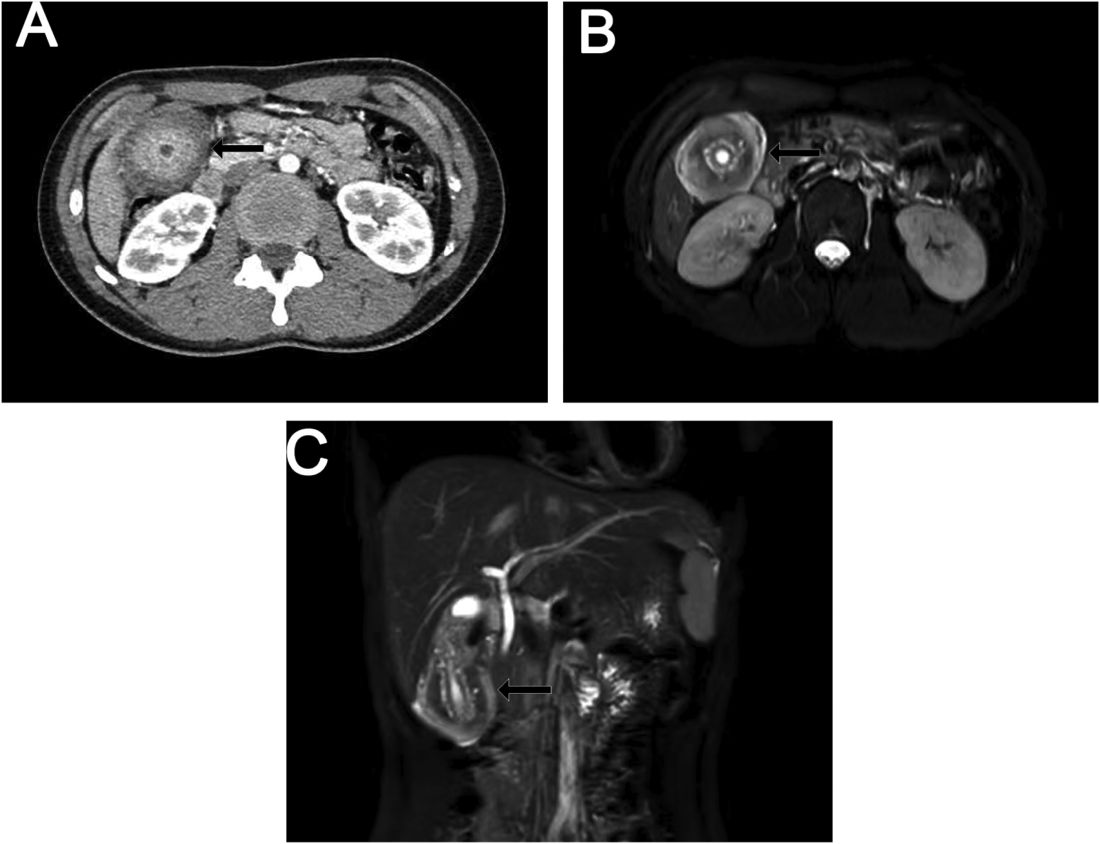
Ultrasound examination indicated gallbladder wall thickening. Furthermore, a contrast-enhanced computed tomographic scan showed marked gallbladder wall thickening with an annular unenhanced proliferative muscularis layer surrounding enhanced proliferative mucosal epithelium (Figure A), and magnetic resonance imaging showed multiple cyst-like spaces in the gallbladder wall (Figures B and C).
What is the diagnosis, and how should it be managed?
Previously published in Gastroenterology
Misdiagnosis, mismatch still common in pancreatic cystic neoplasms
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
AT DDW 2023
PDAC surveillance in high-risk cases improves outcomes
shows a new study published in Gastroenterology.
While other studies have shown potential benefit in screening high-risk individuals, “a concern is that in absence of sufficiently large control groups with unscreened controls,” the outcomes may be influenced by lead-time bias. The current study is the first to address that important limitation.
The study, which was led by Derk C.F. Klatte, MD, of the department of gastroenterology and hepatology at Leiden University Medical Center, the Netherlands, included 43,762 patients from the Netherlands Cancer Registry who were diagnosed with PDAC between January 2000 and December 2020. Using a 1:5 ratio, researchers matched 31 patients who were diagnosed in the pancreatic cancer surveillance cohort against 155 patients in the non-surveillance group.
“We show that surveillance for PDAC in high-risk individuals results in significant earlier detection, increased resectability, and improved survival as compared with average-risk individuals diagnosed with PDAC not under surveillance. This reaffirms that pancreatic surveillance for certain in high-risk individuals is beneficial and could have a meaningful impact on disease course,” the authors wrote.
PDAC has the worst outcomes all cancers and is on pace to become the second-leading cause of cancer-related mortality. By the time a tumor is detected, it is usually unresectable or has developed distant metastases. In principle, early detection could improve outcomes, but there is no test that is adequate for population-wide screening. Surveillance must therefore concentrate on individuals deemed to be at heightened risk. Prospective studies have shown a benefit of pancreatic cancer screening in patients who are at high-risk. Such studies may be misleading, however, due to the potential for lead-time bias. This can occur when a condition is detected at an earlier time than it would have been identified based on clinical signs, as usually occurs in nonscreened populations, and this asymptomatic lag time between diagnosis and initial symptoms does not get incorporated into a survival analysis. The result can be an artificially longer survival time following diagnosis in the screened population.
Guidelines from the International Cancer of the Pancreas Screening (CAPS) consortium, the American Society for Gastrointestinal Endoscopy, and American Society of Clinical Oncology recommend surveillance in high-risk cases.
In this study, researchers conducted a propensity score matched cohort analysis of patients from the general population with primary PDAC who were diagnosed outside of a screening program, with carriers of a germline CDKN2A/p16 mutation who were diagnosed after surveillance.
The surveillance group received a stage 1 diagnosis in 38.7% of cases, versus 5.8% of those outside of surveillance (odds ratio [OR], 0.09; 95% confidence interval [CI], 0.04-0.19). Surgical resection occurred in 71.0% of surveillance patients, versus 18.7% of non-surveillance patients (OR, 10.62; 95% CI, 4.56-26.63), and stage 4 diagnoses were much more common in the nonsurveillance population (61.3% versus 9.7%). Among the patients who did not undergo surveillance, 61.3% were diagnosed with stage 4 disease compared with 9.7% of those in the surveillance group.
The 5-year survival rate (unadjusted for lead-time) in the surveillance group was 32.4% and 4.3% in the nonsurveillance group. The median overall survival was 26.8 months in the surveillance group compared with 5.2 months in the nonsurveillance group, (hazard ratio, 0.22; 95% CI, 0.14-0.36). The mortality rate per 100 person-years was 114.5 (95% CI, 96.2–135.3) in nonsurveillance patients and 21.9 (95% CI, 13.4–33.8) in surveillance patients.
Despite the apparent benefit of screening, there is room for improvement. “Although the outcomes presented here are encouraging and endorse our earlier findings, a significant proportion of surveillance patients (61%) still had poor outcomes because of diagnosis in a late stage (T2–4N0M0 and nodal or distant metastatic PDAC), with a 5-year survival of 16%,” the authors wrote.
The study received no funding and the authors declared no conflicts.
shows a new study published in Gastroenterology.
While other studies have shown potential benefit in screening high-risk individuals, “a concern is that in absence of sufficiently large control groups with unscreened controls,” the outcomes may be influenced by lead-time bias. The current study is the first to address that important limitation.
The study, which was led by Derk C.F. Klatte, MD, of the department of gastroenterology and hepatology at Leiden University Medical Center, the Netherlands, included 43,762 patients from the Netherlands Cancer Registry who were diagnosed with PDAC between January 2000 and December 2020. Using a 1:5 ratio, researchers matched 31 patients who were diagnosed in the pancreatic cancer surveillance cohort against 155 patients in the non-surveillance group.
“We show that surveillance for PDAC in high-risk individuals results in significant earlier detection, increased resectability, and improved survival as compared with average-risk individuals diagnosed with PDAC not under surveillance. This reaffirms that pancreatic surveillance for certain in high-risk individuals is beneficial and could have a meaningful impact on disease course,” the authors wrote.
PDAC has the worst outcomes all cancers and is on pace to become the second-leading cause of cancer-related mortality. By the time a tumor is detected, it is usually unresectable or has developed distant metastases. In principle, early detection could improve outcomes, but there is no test that is adequate for population-wide screening. Surveillance must therefore concentrate on individuals deemed to be at heightened risk. Prospective studies have shown a benefit of pancreatic cancer screening in patients who are at high-risk. Such studies may be misleading, however, due to the potential for lead-time bias. This can occur when a condition is detected at an earlier time than it would have been identified based on clinical signs, as usually occurs in nonscreened populations, and this asymptomatic lag time between diagnosis and initial symptoms does not get incorporated into a survival analysis. The result can be an artificially longer survival time following diagnosis in the screened population.
Guidelines from the International Cancer of the Pancreas Screening (CAPS) consortium, the American Society for Gastrointestinal Endoscopy, and American Society of Clinical Oncology recommend surveillance in high-risk cases.
In this study, researchers conducted a propensity score matched cohort analysis of patients from the general population with primary PDAC who were diagnosed outside of a screening program, with carriers of a germline CDKN2A/p16 mutation who were diagnosed after surveillance.
The surveillance group received a stage 1 diagnosis in 38.7% of cases, versus 5.8% of those outside of surveillance (odds ratio [OR], 0.09; 95% confidence interval [CI], 0.04-0.19). Surgical resection occurred in 71.0% of surveillance patients, versus 18.7% of non-surveillance patients (OR, 10.62; 95% CI, 4.56-26.63), and stage 4 diagnoses were much more common in the nonsurveillance population (61.3% versus 9.7%). Among the patients who did not undergo surveillance, 61.3% were diagnosed with stage 4 disease compared with 9.7% of those in the surveillance group.
The 5-year survival rate (unadjusted for lead-time) in the surveillance group was 32.4% and 4.3% in the nonsurveillance group. The median overall survival was 26.8 months in the surveillance group compared with 5.2 months in the nonsurveillance group, (hazard ratio, 0.22; 95% CI, 0.14-0.36). The mortality rate per 100 person-years was 114.5 (95% CI, 96.2–135.3) in nonsurveillance patients and 21.9 (95% CI, 13.4–33.8) in surveillance patients.
Despite the apparent benefit of screening, there is room for improvement. “Although the outcomes presented here are encouraging and endorse our earlier findings, a significant proportion of surveillance patients (61%) still had poor outcomes because of diagnosis in a late stage (T2–4N0M0 and nodal or distant metastatic PDAC), with a 5-year survival of 16%,” the authors wrote.
The study received no funding and the authors declared no conflicts.
shows a new study published in Gastroenterology.
While other studies have shown potential benefit in screening high-risk individuals, “a concern is that in absence of sufficiently large control groups with unscreened controls,” the outcomes may be influenced by lead-time bias. The current study is the first to address that important limitation.
The study, which was led by Derk C.F. Klatte, MD, of the department of gastroenterology and hepatology at Leiden University Medical Center, the Netherlands, included 43,762 patients from the Netherlands Cancer Registry who were diagnosed with PDAC between January 2000 and December 2020. Using a 1:5 ratio, researchers matched 31 patients who were diagnosed in the pancreatic cancer surveillance cohort against 155 patients in the non-surveillance group.
“We show that surveillance for PDAC in high-risk individuals results in significant earlier detection, increased resectability, and improved survival as compared with average-risk individuals diagnosed with PDAC not under surveillance. This reaffirms that pancreatic surveillance for certain in high-risk individuals is beneficial and could have a meaningful impact on disease course,” the authors wrote.
PDAC has the worst outcomes all cancers and is on pace to become the second-leading cause of cancer-related mortality. By the time a tumor is detected, it is usually unresectable or has developed distant metastases. In principle, early detection could improve outcomes, but there is no test that is adequate for population-wide screening. Surveillance must therefore concentrate on individuals deemed to be at heightened risk. Prospective studies have shown a benefit of pancreatic cancer screening in patients who are at high-risk. Such studies may be misleading, however, due to the potential for lead-time bias. This can occur when a condition is detected at an earlier time than it would have been identified based on clinical signs, as usually occurs in nonscreened populations, and this asymptomatic lag time between diagnosis and initial symptoms does not get incorporated into a survival analysis. The result can be an artificially longer survival time following diagnosis in the screened population.
Guidelines from the International Cancer of the Pancreas Screening (CAPS) consortium, the American Society for Gastrointestinal Endoscopy, and American Society of Clinical Oncology recommend surveillance in high-risk cases.
In this study, researchers conducted a propensity score matched cohort analysis of patients from the general population with primary PDAC who were diagnosed outside of a screening program, with carriers of a germline CDKN2A/p16 mutation who were diagnosed after surveillance.
The surveillance group received a stage 1 diagnosis in 38.7% of cases, versus 5.8% of those outside of surveillance (odds ratio [OR], 0.09; 95% confidence interval [CI], 0.04-0.19). Surgical resection occurred in 71.0% of surveillance patients, versus 18.7% of non-surveillance patients (OR, 10.62; 95% CI, 4.56-26.63), and stage 4 diagnoses were much more common in the nonsurveillance population (61.3% versus 9.7%). Among the patients who did not undergo surveillance, 61.3% were diagnosed with stage 4 disease compared with 9.7% of those in the surveillance group.
The 5-year survival rate (unadjusted for lead-time) in the surveillance group was 32.4% and 4.3% in the nonsurveillance group. The median overall survival was 26.8 months in the surveillance group compared with 5.2 months in the nonsurveillance group, (hazard ratio, 0.22; 95% CI, 0.14-0.36). The mortality rate per 100 person-years was 114.5 (95% CI, 96.2–135.3) in nonsurveillance patients and 21.9 (95% CI, 13.4–33.8) in surveillance patients.
Despite the apparent benefit of screening, there is room for improvement. “Although the outcomes presented here are encouraging and endorse our earlier findings, a significant proportion of surveillance patients (61%) still had poor outcomes because of diagnosis in a late stage (T2–4N0M0 and nodal or distant metastatic PDAC), with a 5-year survival of 16%,” the authors wrote.
The study received no funding and the authors declared no conflicts.
FROM GASTROENTEROLOGY
Joint symposium addresses exocrine pancreatic insufficiency
Based on discussions during PancreasFest 2021, , according to a recent report in Gastro Hep Advances
Due to its complex and individualized nature, EPI requires multidisciplinary approaches to therapy, as well as better pancreas function tests and biomarkers for diagnosis and treatment, wrote researchers who were led by David C. Whitcomb, MD, PhD, AGAF, emeritus professor of medicine in the division of gastroenterology, hepatology and nutrition at the University of Pittsburgh.
“This condition remains challenging even to define, and serious limitations in diagnostic testing and therapeutic options lead to clinical confusion and frequently less than optimal patient management,” the authors wrote.
EPI is clinically defined as inadequate delivery of pancreatic digestive enzymes to meet nutritional needs, which is typically based on a physician’s assessment of a patient’s maldigestion. However, there’s not a universally accepted definition or a precise threshold of reduced pancreatic digestive enzymes that indicates “pancreatic insufficiency” in an individual patient.
Current guidelines also don’t clearly outline the role of pancreatic function tests, the effects of different metabolic needs and nutrition intake, the timing of pancreatic enzyme replacement therapy (PERT), or the best practices for monitoring or titrating multiple therapies.
In response, Dr. Whitcomb and colleagues proposed a new mechanistic definition of EPI, including the disorder’s physiologic effects and impact on health. First, they said, EPI is a disorder caused by failure of the pancreas to deliver a minimum or threshold level of specific pancreatic digestive enzymes to the intestine in concert with ingested nutrients, followed by enzymatic digestion of individual meals over time to meet certain nutritional and metabolic needs. In addition, the disorder is characterized by variable deficiencies in micronutrients and macronutrients, especially essential fats and fat-soluble vitamins, as well as gastrointestinal symptoms of nutrient maldigestion.
The threshold for EPI should consider the nutritional needs of the patient, dietary intake, residual exocrine pancreas function, and the absorptive capacity of the intestine based on anatomy, mucosal function, motility, inflammation, the microbiome, and physiological adaptation, the authors wrote.
Due to challenges in diagnosing EPI and its common chronic symptoms such as abdominal pain, bloating, and diarrhea, several conditions may mimic EPI, be present concomitantly with EPI, or hinder PERT response. These include celiac disease, small intestinal bacterial overgrowth, disaccharidase deficiencies, inflammatory bowel disease (IBD), bile acid diarrhea, giardiasis, diabetes mellitus, and functional conditions such as irritable bowel syndrome. These conditions should be considered to address underlying pathology and PERT diagnostic challenges.
Although there is consensus that exocrine pancreatic function testing (PFT) is important to diagnosis EPI, no optimal test exists, and pancreatic function is only one aspect of digestion and absorption that should be considered. PFT may be needed to make an objective EPI diagnosis related to acute pancreatitis, pancreatic cancer, pancreatic resection, gastric resection, cystic fibrosis, or IBD. Direct or indirect PFTs may be used, which typically differs by center.
“The medical community still awaits a clinically useful pancreas function test that is easy to perform, well tolerated by patients, and allows personalized dosing of PERT,” the authors wrote.
After diagnosis, a general assessment should include information about symptoms, nutritional status, medications, diet, and lifestyle. This information can be used for a multifaceted treatment approach, with a focus on lifestyle changes, concomitant disease treatment, optimized diet, dietary supplements, and PERT administration.
PERT remains a mainstay of EPI treatment and has shown improvements in steatorrhea, postprandial bloating and pain, nutrition, and unexplained weight loss. The Food and Drug Administration has approved several formulations in different strengths. The typical starting dose is based on age and weight, which is derived from guidelines for EPI treatment in patients with cystic fibrosis. However, the recommendations don’t consider many of the variables discussed above and simply provide an estimate for the average subject with severe EPI, so the dose should be titrated as needed based on age, weight, symptoms, and the holistic management plan.
For optimal results, regular follow-up is necessary to monitor compliance and treatment response. A reduction in symptoms can serve as a reliable indicator of effective EPI management, particularly weight stabilization, improved steatorrhea and diarrhea, and reduced postprandial bloating, pain, and flatulence. Physicians may provide patients with tracking tools to record their PERT compliance, symptom frequency, and lifestyle changes.
For patients with persistent concerns, PERT can be increased as needed. Although many PERT formulations are enteric coated, a proton pump inhibitor or H2 receptor agonist may improve their effectiveness. If EPI symptoms persist despite increased doses, other causes of malabsorption should be considered, such as the concomitant conditions mentioned above.
“As EPI escalates, a lower fat diet may become necessary to alleviate distressing gastrointestinal symptoms,” the authors wrote. “A close working relationship between the treating provider and the [registered dietician] is crucial so that barriers to optimum nutrient assimilation can be identified, communicated, and overcome. Frequent monitoring of the nutritional state with therapy is also imperative.”
PancreasFest 2021 received no specific funding for this event. The authors declared grant support, adviser roles, and speaking honoraria from several pharmaceutical and medical device companies and health care foundations, including the National Pancreas Foundation.
Recognition of recent advances and unaddressed gaps can clarify key issues around exocrine pancreatic insufficiency (EPI).
The loss of pancreatic digestive enzymes and bicarbonate is caused by exocrine pancreatic and proximal small intestine disease. EPI’s clinical impact has been expanded by reports that 30% of subjects can develop EPI after a bout of acute pancreatitis. Diagnosing and treating EPI challenges clinicians and investigators.
The contribution on EPI by Whitcomb and colleagues provides state-of-the-art content relating to diagnosing EPI, assessing its metabolic impact, enzyme replacement, nutritional considerations, and how to assess the effectiveness of therapy.
Though the diagnosis and treatment of EPI have been examined for over 50 years, a consensus for either is still needed. Assessment of EPI with luminal tube tests and endoscopic collections of pancreatic secretion are the most accurate, but they are invasive, limited in availability, and time-consuming. Indirect assays of intestinal activities of pancreatic enzymes by the hydrolysis of substrates or stool excretion are frequently used to diagnose EPI. However, they need to be more insensitive and specific to meet clinical and investigative needs.
Indeed, all tests of exocrine secretion are surrogates of unclear value for the critical endpoint of EPI, its nutritional impact. An unmet need is the development of nutritional standards for assessing EPI and measures for the adequacy of pancreatic enzyme replacement therapy. In this context, a patient’s diet, and other factors, such as the intestinal microbiome, can affect pancreatic digestive enzyme activity and must be considered in designing the best EPI treatments. The summary concludes with a thoughtful and valuable road map for moving forward.
Fred Sanford Gorelick, MD, is the Henry J. and Joan W. Binder Professor of Medicine (Digestive Diseases) and of Cell Biology for Yale School of Medicine, New Haven, Conn. He also serves as director of the Yale School of Medicine NIH T32-funded research track in gastroenterology; and as deputy director of Yale School of Medicine MD-PhD program.
Potential conflicts: Dr. Gorelick serves as chair of NIH NIDDK DSMB for Stent vs. Indomethacin for Preventing Post-ERCP Pancreatitis (SVI) study. He also holds grants for research on mechanisms of acute pancreatitis from the U.S. Department of Veterans Affairs and the Department of Defense.
Recognition of recent advances and unaddressed gaps can clarify key issues around exocrine pancreatic insufficiency (EPI).
The loss of pancreatic digestive enzymes and bicarbonate is caused by exocrine pancreatic and proximal small intestine disease. EPI’s clinical impact has been expanded by reports that 30% of subjects can develop EPI after a bout of acute pancreatitis. Diagnosing and treating EPI challenges clinicians and investigators.
The contribution on EPI by Whitcomb and colleagues provides state-of-the-art content relating to diagnosing EPI, assessing its metabolic impact, enzyme replacement, nutritional considerations, and how to assess the effectiveness of therapy.
Though the diagnosis and treatment of EPI have been examined for over 50 years, a consensus for either is still needed. Assessment of EPI with luminal tube tests and endoscopic collections of pancreatic secretion are the most accurate, but they are invasive, limited in availability, and time-consuming. Indirect assays of intestinal activities of pancreatic enzymes by the hydrolysis of substrates or stool excretion are frequently used to diagnose EPI. However, they need to be more insensitive and specific to meet clinical and investigative needs.
Indeed, all tests of exocrine secretion are surrogates of unclear value for the critical endpoint of EPI, its nutritional impact. An unmet need is the development of nutritional standards for assessing EPI and measures for the adequacy of pancreatic enzyme replacement therapy. In this context, a patient’s diet, and other factors, such as the intestinal microbiome, can affect pancreatic digestive enzyme activity and must be considered in designing the best EPI treatments. The summary concludes with a thoughtful and valuable road map for moving forward.
Fred Sanford Gorelick, MD, is the Henry J. and Joan W. Binder Professor of Medicine (Digestive Diseases) and of Cell Biology for Yale School of Medicine, New Haven, Conn. He also serves as director of the Yale School of Medicine NIH T32-funded research track in gastroenterology; and as deputy director of Yale School of Medicine MD-PhD program.
Potential conflicts: Dr. Gorelick serves as chair of NIH NIDDK DSMB for Stent vs. Indomethacin for Preventing Post-ERCP Pancreatitis (SVI) study. He also holds grants for research on mechanisms of acute pancreatitis from the U.S. Department of Veterans Affairs and the Department of Defense.
Recognition of recent advances and unaddressed gaps can clarify key issues around exocrine pancreatic insufficiency (EPI).
The loss of pancreatic digestive enzymes and bicarbonate is caused by exocrine pancreatic and proximal small intestine disease. EPI’s clinical impact has been expanded by reports that 30% of subjects can develop EPI after a bout of acute pancreatitis. Diagnosing and treating EPI challenges clinicians and investigators.
The contribution on EPI by Whitcomb and colleagues provides state-of-the-art content relating to diagnosing EPI, assessing its metabolic impact, enzyme replacement, nutritional considerations, and how to assess the effectiveness of therapy.
Though the diagnosis and treatment of EPI have been examined for over 50 years, a consensus for either is still needed. Assessment of EPI with luminal tube tests and endoscopic collections of pancreatic secretion are the most accurate, but they are invasive, limited in availability, and time-consuming. Indirect assays of intestinal activities of pancreatic enzymes by the hydrolysis of substrates or stool excretion are frequently used to diagnose EPI. However, they need to be more insensitive and specific to meet clinical and investigative needs.
Indeed, all tests of exocrine secretion are surrogates of unclear value for the critical endpoint of EPI, its nutritional impact. An unmet need is the development of nutritional standards for assessing EPI and measures for the adequacy of pancreatic enzyme replacement therapy. In this context, a patient’s diet, and other factors, such as the intestinal microbiome, can affect pancreatic digestive enzyme activity and must be considered in designing the best EPI treatments. The summary concludes with a thoughtful and valuable road map for moving forward.
Fred Sanford Gorelick, MD, is the Henry J. and Joan W. Binder Professor of Medicine (Digestive Diseases) and of Cell Biology for Yale School of Medicine, New Haven, Conn. He also serves as director of the Yale School of Medicine NIH T32-funded research track in gastroenterology; and as deputy director of Yale School of Medicine MD-PhD program.
Potential conflicts: Dr. Gorelick serves as chair of NIH NIDDK DSMB for Stent vs. Indomethacin for Preventing Post-ERCP Pancreatitis (SVI) study. He also holds grants for research on mechanisms of acute pancreatitis from the U.S. Department of Veterans Affairs and the Department of Defense.
Based on discussions during PancreasFest 2021, , according to a recent report in Gastro Hep Advances
Due to its complex and individualized nature, EPI requires multidisciplinary approaches to therapy, as well as better pancreas function tests and biomarkers for diagnosis and treatment, wrote researchers who were led by David C. Whitcomb, MD, PhD, AGAF, emeritus professor of medicine in the division of gastroenterology, hepatology and nutrition at the University of Pittsburgh.
“This condition remains challenging even to define, and serious limitations in diagnostic testing and therapeutic options lead to clinical confusion and frequently less than optimal patient management,” the authors wrote.
EPI is clinically defined as inadequate delivery of pancreatic digestive enzymes to meet nutritional needs, which is typically based on a physician’s assessment of a patient’s maldigestion. However, there’s not a universally accepted definition or a precise threshold of reduced pancreatic digestive enzymes that indicates “pancreatic insufficiency” in an individual patient.
Current guidelines also don’t clearly outline the role of pancreatic function tests, the effects of different metabolic needs and nutrition intake, the timing of pancreatic enzyme replacement therapy (PERT), or the best practices for monitoring or titrating multiple therapies.
In response, Dr. Whitcomb and colleagues proposed a new mechanistic definition of EPI, including the disorder’s physiologic effects and impact on health. First, they said, EPI is a disorder caused by failure of the pancreas to deliver a minimum or threshold level of specific pancreatic digestive enzymes to the intestine in concert with ingested nutrients, followed by enzymatic digestion of individual meals over time to meet certain nutritional and metabolic needs. In addition, the disorder is characterized by variable deficiencies in micronutrients and macronutrients, especially essential fats and fat-soluble vitamins, as well as gastrointestinal symptoms of nutrient maldigestion.
The threshold for EPI should consider the nutritional needs of the patient, dietary intake, residual exocrine pancreas function, and the absorptive capacity of the intestine based on anatomy, mucosal function, motility, inflammation, the microbiome, and physiological adaptation, the authors wrote.
Due to challenges in diagnosing EPI and its common chronic symptoms such as abdominal pain, bloating, and diarrhea, several conditions may mimic EPI, be present concomitantly with EPI, or hinder PERT response. These include celiac disease, small intestinal bacterial overgrowth, disaccharidase deficiencies, inflammatory bowel disease (IBD), bile acid diarrhea, giardiasis, diabetes mellitus, and functional conditions such as irritable bowel syndrome. These conditions should be considered to address underlying pathology and PERT diagnostic challenges.
Although there is consensus that exocrine pancreatic function testing (PFT) is important to diagnosis EPI, no optimal test exists, and pancreatic function is only one aspect of digestion and absorption that should be considered. PFT may be needed to make an objective EPI diagnosis related to acute pancreatitis, pancreatic cancer, pancreatic resection, gastric resection, cystic fibrosis, or IBD. Direct or indirect PFTs may be used, which typically differs by center.
“The medical community still awaits a clinically useful pancreas function test that is easy to perform, well tolerated by patients, and allows personalized dosing of PERT,” the authors wrote.
After diagnosis, a general assessment should include information about symptoms, nutritional status, medications, diet, and lifestyle. This information can be used for a multifaceted treatment approach, with a focus on lifestyle changes, concomitant disease treatment, optimized diet, dietary supplements, and PERT administration.
PERT remains a mainstay of EPI treatment and has shown improvements in steatorrhea, postprandial bloating and pain, nutrition, and unexplained weight loss. The Food and Drug Administration has approved several formulations in different strengths. The typical starting dose is based on age and weight, which is derived from guidelines for EPI treatment in patients with cystic fibrosis. However, the recommendations don’t consider many of the variables discussed above and simply provide an estimate for the average subject with severe EPI, so the dose should be titrated as needed based on age, weight, symptoms, and the holistic management plan.
For optimal results, regular follow-up is necessary to monitor compliance and treatment response. A reduction in symptoms can serve as a reliable indicator of effective EPI management, particularly weight stabilization, improved steatorrhea and diarrhea, and reduced postprandial bloating, pain, and flatulence. Physicians may provide patients with tracking tools to record their PERT compliance, symptom frequency, and lifestyle changes.
For patients with persistent concerns, PERT can be increased as needed. Although many PERT formulations are enteric coated, a proton pump inhibitor or H2 receptor agonist may improve their effectiveness. If EPI symptoms persist despite increased doses, other causes of malabsorption should be considered, such as the concomitant conditions mentioned above.
“As EPI escalates, a lower fat diet may become necessary to alleviate distressing gastrointestinal symptoms,” the authors wrote. “A close working relationship between the treating provider and the [registered dietician] is crucial so that barriers to optimum nutrient assimilation can be identified, communicated, and overcome. Frequent monitoring of the nutritional state with therapy is also imperative.”
PancreasFest 2021 received no specific funding for this event. The authors declared grant support, adviser roles, and speaking honoraria from several pharmaceutical and medical device companies and health care foundations, including the National Pancreas Foundation.
Based on discussions during PancreasFest 2021, , according to a recent report in Gastro Hep Advances
Due to its complex and individualized nature, EPI requires multidisciplinary approaches to therapy, as well as better pancreas function tests and biomarkers for diagnosis and treatment, wrote researchers who were led by David C. Whitcomb, MD, PhD, AGAF, emeritus professor of medicine in the division of gastroenterology, hepatology and nutrition at the University of Pittsburgh.
“This condition remains challenging even to define, and serious limitations in diagnostic testing and therapeutic options lead to clinical confusion and frequently less than optimal patient management,” the authors wrote.
EPI is clinically defined as inadequate delivery of pancreatic digestive enzymes to meet nutritional needs, which is typically based on a physician’s assessment of a patient’s maldigestion. However, there’s not a universally accepted definition or a precise threshold of reduced pancreatic digestive enzymes that indicates “pancreatic insufficiency” in an individual patient.
Current guidelines also don’t clearly outline the role of pancreatic function tests, the effects of different metabolic needs and nutrition intake, the timing of pancreatic enzyme replacement therapy (PERT), or the best practices for monitoring or titrating multiple therapies.
In response, Dr. Whitcomb and colleagues proposed a new mechanistic definition of EPI, including the disorder’s physiologic effects and impact on health. First, they said, EPI is a disorder caused by failure of the pancreas to deliver a minimum or threshold level of specific pancreatic digestive enzymes to the intestine in concert with ingested nutrients, followed by enzymatic digestion of individual meals over time to meet certain nutritional and metabolic needs. In addition, the disorder is characterized by variable deficiencies in micronutrients and macronutrients, especially essential fats and fat-soluble vitamins, as well as gastrointestinal symptoms of nutrient maldigestion.
The threshold for EPI should consider the nutritional needs of the patient, dietary intake, residual exocrine pancreas function, and the absorptive capacity of the intestine based on anatomy, mucosal function, motility, inflammation, the microbiome, and physiological adaptation, the authors wrote.
Due to challenges in diagnosing EPI and its common chronic symptoms such as abdominal pain, bloating, and diarrhea, several conditions may mimic EPI, be present concomitantly with EPI, or hinder PERT response. These include celiac disease, small intestinal bacterial overgrowth, disaccharidase deficiencies, inflammatory bowel disease (IBD), bile acid diarrhea, giardiasis, diabetes mellitus, and functional conditions such as irritable bowel syndrome. These conditions should be considered to address underlying pathology and PERT diagnostic challenges.
Although there is consensus that exocrine pancreatic function testing (PFT) is important to diagnosis EPI, no optimal test exists, and pancreatic function is only one aspect of digestion and absorption that should be considered. PFT may be needed to make an objective EPI diagnosis related to acute pancreatitis, pancreatic cancer, pancreatic resection, gastric resection, cystic fibrosis, or IBD. Direct or indirect PFTs may be used, which typically differs by center.
“The medical community still awaits a clinically useful pancreas function test that is easy to perform, well tolerated by patients, and allows personalized dosing of PERT,” the authors wrote.
After diagnosis, a general assessment should include information about symptoms, nutritional status, medications, diet, and lifestyle. This information can be used for a multifaceted treatment approach, with a focus on lifestyle changes, concomitant disease treatment, optimized diet, dietary supplements, and PERT administration.
PERT remains a mainstay of EPI treatment and has shown improvements in steatorrhea, postprandial bloating and pain, nutrition, and unexplained weight loss. The Food and Drug Administration has approved several formulations in different strengths. The typical starting dose is based on age and weight, which is derived from guidelines for EPI treatment in patients with cystic fibrosis. However, the recommendations don’t consider many of the variables discussed above and simply provide an estimate for the average subject with severe EPI, so the dose should be titrated as needed based on age, weight, symptoms, and the holistic management plan.
For optimal results, regular follow-up is necessary to monitor compliance and treatment response. A reduction in symptoms can serve as a reliable indicator of effective EPI management, particularly weight stabilization, improved steatorrhea and diarrhea, and reduced postprandial bloating, pain, and flatulence. Physicians may provide patients with tracking tools to record their PERT compliance, symptom frequency, and lifestyle changes.
For patients with persistent concerns, PERT can be increased as needed. Although many PERT formulations are enteric coated, a proton pump inhibitor or H2 receptor agonist may improve their effectiveness. If EPI symptoms persist despite increased doses, other causes of malabsorption should be considered, such as the concomitant conditions mentioned above.
“As EPI escalates, a lower fat diet may become necessary to alleviate distressing gastrointestinal symptoms,” the authors wrote. “A close working relationship between the treating provider and the [registered dietician] is crucial so that barriers to optimum nutrient assimilation can be identified, communicated, and overcome. Frequent monitoring of the nutritional state with therapy is also imperative.”
PancreasFest 2021 received no specific funding for this event. The authors declared grant support, adviser roles, and speaking honoraria from several pharmaceutical and medical device companies and health care foundations, including the National Pancreas Foundation.
FROM GASTRO HEP ADVANCES
Pancreas cysts – What’s the best approach?
Dear colleagues,
Pancreas cysts have become almost ubiquitous in this era of high-resolution cross-sectional imaging. They are a common GI consult with patients and providers worried about the potential risk of malignant transformation. Despite significant research over the past few decades, predicting the natural history of these cysts, especially the side-branch intraductal papillary mucinous neoplasms (IPMNs), remains difficult. There have been a variety of expert recommendations and guidelines, but heterogeneity exists in management especially regarding timing of endoscopic ultrasound, imaging surveillance, and cessation of surveillance. Some centers will present these cysts at multidisciplinary conferences, while others will follow general or local algorithms. In this issue of Perspectives, Dr. Lauren G. Khanna, assistant professor of medicine at NYU Langone Health, New York, and Dr. Santhi Vege, professor of medicine at the Mayo Clinic, Rochester, Minn., present updated and differing approaches to managing these cysts. Which side of the debate are you on? We welcome your thoughts, questions and input– share with us on Twitter @AGA_GIHN
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Continuing pancreas cyst surveillance indefinitely is reasonable
BY LAUREN G. KHANNA, MD, MS
Pancreas cysts remain a clinical challenge. The true incidence of pancreas cysts is unknown, but from MRI and autopsy series, may be up to 50%. Patients presenting with a pancreas cyst often have significant anxiety about their risk of pancreas cancer. We as a medical community initially did too; but over the past few decades as we have gathered more data, we have become more comfortable observing many pancreas cysts. Yet our recommendations for how, how often, and for how long to evaluate pancreas cysts are still very much under debate; there are multiple guidelines with discordant recommendations. In this article, I will discuss my approach to patients with a pancreas cyst.
At the first evaluation, I review available imaging to see if there are characteristic features to determine the type of pancreas cyst: IPMN (including main duct, branch duct, or mixed type), serous cystic neoplasm (SCA), mucinous cystic neoplasm (MCN), solid pseudopapillary neoplasm (SPN), cystic neuroendocrine tumor (NET), or pseudocyst. I also review symptoms, including abdominal pain, weight loss, history of pancreatitis, and onset of diabetes, and check hemoglobin A1c and Ca19-9. I often recommend magnetic resonance cholangiopancreatography (MRCP) if it has not already been obtained and is feasible (that is, if a patient does not have severe claustrophobia or a medical device incompatible with MRI). If a patient is not a candidate for treatment should a pancreatic malignancy be identified, because of age, comorbidities, or preference, I recommend no further evaluation.
Where cyst type remains unclear despite MRCP, and for cysts over 2 cm, I recommend endoscopic ultrasound (EUS) for fluid sampling to assist in determining cyst type and to rule out any other high-risk features. In accordance with international guidelines, if a patient has any concerning imaging features, including main pancreatic duct dilation >5 mm, solid component or mural nodule, or thickened or enhancing duct walls, regardless of cyst size, I recommend EUS to assess for and biopsy any solid component and to sample cyst fluid to examine for dysplasia. Given the lower sensitivity of CT for high-risk features, if MRCP is not feasible, for cysts 1-2 cm, I recommend EUS for better evaluation.
If a cyst is determined to be a cystic NET; main duct or mixed-type IPMN; MCN; or SPN; or a branch duct IPMN with mural nodule, high-grade dysplasia, or adenocarcinoma, and the patient is a surgical candidate, I refer the patient for surgical evaluation. If a cyst is determined to be an SCA, the malignant potential is minimal, and patients do not require follow-up. Patients with a pseudocyst are managed according to their clinical scenario.
Many patients have a proven or suspected branch duct IPMN, an indeterminate cyst, or multiple cysts. Cyst management during surveillance is then determined by the size of the largest cyst and stability of the cyst(s). Of note, patients with an IPMN also have been shown to have an elevated risk of concurrent pancreas adenocarcinoma, which I believe is one of the strongest arguments for heightened surveillance of the entire pancreas in pancreas cyst patients. EUS in particular can identify small or subtle lesions that are not detected by cross-sectional imaging.
If a patient has no prior imaging, in accordance with international and European guidelines, I recommend the first surveillance MRCP at a 6-month interval for cysts <2 cm, which may offer the opportunity to identify rapidly progressing cysts. If a patient has previous imaging available demonstrating stability, I recommend surveillance on an annual basis for cysts <2 cm. For patients with a cyst >2 cm, as above, I recommend EUS, and if there are no concerning features on imaging or EUS, I then recommend annual surveillance.
While the patient is under surveillance, if there is more than minimal cyst growth, a change in cyst appearance, or development of any imaging high-risk feature, pancreatitis, new onset or worsening diabetes, or elevation of Ca19-9, I recommend EUS for further evaluation and consideration of surgery based on EUS findings. If an asymptomatic cyst <2 cm remains stable for 5 years, I offer patients the option to extend imaging to every 2 years, if they are comfortable. In my experience, though, many patients prefer to continue annual imaging. The American Gastroenterological Association guidelines promote stopping surveillance after 5 years of stability, however there are studies demonstrating development of malignancy in cysts that were initially stable over the first 5 years of surveillance. Therefore, I discuss with patients that it is reasonable to continue cyst surveillance indefinitely, until they would no longer be interested in pursuing treatment of any kind if a malignant lesion were to be identified.
There are two special groups of pancreas cyst patients who warrant specific attention. Patients who are at elevated risk of pancreas adenocarcinoma because of an associated genetic mutation or a family history of pancreatic cancer already may be undergoing annual pancreas cancer screening with either MRCP, EUS, or alternating MRCP and EUS. When these high-risk patients also have pancreas cysts, I utilize whichever strategy would image their pancreas most frequently and do not extend beyond 1-year intervals. Another special group is patients who have undergone partial pancreatectomy for IPMN. As discussed above, given the elevated risk of concurrent pancreas adenocarcinoma in IPMN patients, I recommend indefinite continued surveillance of the remaining pancreas parenchyma in these patients.
Given the prevalence of pancreas cysts, it certainly would be convenient if guidelines were straightforward enough for primary care physicians to manage pancreas cyst surveillance, as they do for breast cancer screening. However, the complexities of pancreas cysts necessitate the expertise of gastroenterologists and pancreas surgeons, and a multidisciplinary team approach is best where possible.
Dr. Khanna is chief, advanced endoscopy, Tisch Hospital; director, NYU Advanced Endoscopy Fellowship; assistant professor of medicine, NYU Langone Health. Email: [email protected]. There are no relevant conflicts to disclose.
References
Tanaka M et al. Pancreatology. 2017 Sep-Oct;17(5):738-75.
Sahora K et al. Eur J Surg Oncol. 2016 Feb;42(2):197-204.
Del Chiaro M et al. Gut. 2018 May;67(5):789-804
Vege SS et al. Gastroenterology. 2015 Apr;148(4):819-22
Petrone MC et al. Clin Transl Gastroenterol. 2018 Jun 13;9(6):158
Pancreas cysts: More is not necessarily better!
BY SANTHI SWAROOP VEGE, MD
Pancreas cysts (PC) are very common, incidental findings on cross-sectional imaging, performed for non–pancreas-related symptoms. The important issues in management of patients with PC in my practice are the prevalence, natural history, frequency of occurrence of high-grade dysplasia (HGD) and/or pancreatic cancer (PDAC), concerning clinical symptoms and imaging findings, indications for EUS and fine-needle aspiration cytology, ideal method and frequency of surveillance, indications for surgery (up front and during follow-up), follow-up after surgery, stopping surveillance, costs, and unintentional harms of management. Good population-based evidence regarding many of the issues described above does not exist, and all information is from selected clinic, radiology, EUS, and surgical cohorts (very important when trying to assess the publications). Cohort studies should start with all PC undergoing surveillance and assess various outcomes, rather than looking backward from EUS or surgical cohorts.
The 2015 American Gastroenterological Association guidelines on asymptomatic neoplastic pancreas cysts, which I coauthored, recommend, consistent with principles of High Value Care (minimal unintentional harms and cost effectiveness), that two of three high-risk features (mural nodule, cyst size greater than 3 cm, and dilated pancreatic duct) be present for EUS-guided fine-needle aspiration (EUS-FNA). By the same token, they advise surgery for those with two of three high-risk features and or concerning features on EUS and cytology. Finally, they suggest stopping surveillance at 5 years if there are no significant changes. Rigorous GRADE methodology along with systematic review of all relevant questions (rather than cohorts of 500 or fewer patients) formed the basis of the guidelines. Those meta-analyses showed that risk of PDAC in mural nodules, cyst size >3 cm, and dilated pancreatic duct, while elevated, still is very low in absolute terms. Less than 20% of resections for highly selected, high-risk cysts showed PDAC. The guidelines were met with a lot of resistance from several societies and physician groups. The recommendations for stopping surveillance after 5 years and no surveillance for absent or low-grade dysplasia after surgery are hotly contested, and these areas need larger, long-term studies.
The whole area of cyst fluid molecular markers that would suggest mucinous type (KRAS and GNAS mutations) and, more importantly, the presence or imminent development of PDAC (next-generation sequencing or NGS) is an exciting field. One sincerely hopes that there will be a breakthrough in this area to achieve the holy grail. Cost effectiveness studies demonstrate the futility of existing guidelines and favor a less intensive approach. Guidelines are only a general framework, and management of individual patients in the clinic is entirely at the discretion of the treating physician. One should make every attempt to detect advanced lesions in PC, but such effort should not subject a large majority of patients to unintentional harms by overtreatment and add further to the burgeoning health care costs in the country.
PC are extremely common (10% of all abdominal imaging), increase with age, are seen in as many as 40%-50% of MRI examinations for nonpancreatic indications, and most (>50%) are IPMNs. Most of the debate centers around the concerns of PDAC and/or HGD associated with mucinous cysts (MCN, IPMN, side-branch, main duct, or mixed).
The various guidelines by multiple societies differ in some aspects, such as in selection of patients based on clinical, laboratory, and imaging findings for up-front surgery or surveillance, the frequency of surveillance based on the size of the cyst and the presence of other concerning cyst features (usually with MRCP), the indications for EUS (both initial and subsequent), importance of the magnitude of growth (most IPMNs slowly grow over a period of time), indications for surgery during surveillance and postsurgery surveillance, and the decision to stop surveillance at some point in time. The literature is replete with small case series reporting a proportion of cancers detected and often ignoring the harms of surgery. Incidence of and mortality caused by PDAC are very low (about 1% for both) in a large national cohort of VA pancreatic cyst patients with long-term follow-up and other studies.
Marcov modeling suggests that none of the guidelines would lead to cost-effective care with low mortality because of overtreatment of low-risk lesions, and a specificity of 67% or more for PDAC/HGB is required. AGA guidelines came close to it but with low sensitivity. Monte Carlo modeling suggests that less intensive strategies, compared with more intensive, result in a similar number of deaths at a much lower cost. While molecular markers in PC fluid are reported to increase the specificity of PDAC/HGD to greater than 70%, it should be observed that such validation was done in a small percentage of patients who had both those markers and resection.
The costs of expensive procedures like EUS, MRI, and surgery, the 3% complication rate with EUS-FNA (primarily acute pancreatitis), and the 1% mortality and approximately 20%-30% morbidity with surgery (bleeding, infection, fistula) and postpancreatectomy diabetes of approximately 30% in the long run need special attention.
In conclusion, one could say pancreas cysts are extremely frequent, most of the neoplastic cysts are mucinous (IPMN and MCN) and slowly growing over time without an associated cancer, and the greatest need at this time is to identify the small proportion of such cysts with PDAC and/or HGD. Until such time, judicious selection of patients for surveillance and reasonable intervals of such surveillance with selective use of EUS will help identify patients requiring resection. In our enthusiasm to detect every possible pancreatic cancer, we should not ignore the unintentional outcomes of surgery to a large majority of patients who would never develop PDAC and the astronomical costs associated with such practice.
Dr. Vege is professor of medicine at the Mayo Clinic. He reported having no conflicts of interest regarding this article.
References
Vege SS et al. Gastroenterology. 2015;148:819-22.
Lobo JM et al. Surgery. 2020;168:601-9.
Lennon AM and Vege SS. Clin Gastroenterol Hepatol. 2022;20:1663-7.
Harris RP. Ann Intern Med. 2015;162:787-9.
Dear colleagues,
Pancreas cysts have become almost ubiquitous in this era of high-resolution cross-sectional imaging. They are a common GI consult with patients and providers worried about the potential risk of malignant transformation. Despite significant research over the past few decades, predicting the natural history of these cysts, especially the side-branch intraductal papillary mucinous neoplasms (IPMNs), remains difficult. There have been a variety of expert recommendations and guidelines, but heterogeneity exists in management especially regarding timing of endoscopic ultrasound, imaging surveillance, and cessation of surveillance. Some centers will present these cysts at multidisciplinary conferences, while others will follow general or local algorithms. In this issue of Perspectives, Dr. Lauren G. Khanna, assistant professor of medicine at NYU Langone Health, New York, and Dr. Santhi Vege, professor of medicine at the Mayo Clinic, Rochester, Minn., present updated and differing approaches to managing these cysts. Which side of the debate are you on? We welcome your thoughts, questions and input– share with us on Twitter @AGA_GIHN
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Continuing pancreas cyst surveillance indefinitely is reasonable
BY LAUREN G. KHANNA, MD, MS
Pancreas cysts remain a clinical challenge. The true incidence of pancreas cysts is unknown, but from MRI and autopsy series, may be up to 50%. Patients presenting with a pancreas cyst often have significant anxiety about their risk of pancreas cancer. We as a medical community initially did too; but over the past few decades as we have gathered more data, we have become more comfortable observing many pancreas cysts. Yet our recommendations for how, how often, and for how long to evaluate pancreas cysts are still very much under debate; there are multiple guidelines with discordant recommendations. In this article, I will discuss my approach to patients with a pancreas cyst.
At the first evaluation, I review available imaging to see if there are characteristic features to determine the type of pancreas cyst: IPMN (including main duct, branch duct, or mixed type), serous cystic neoplasm (SCA), mucinous cystic neoplasm (MCN), solid pseudopapillary neoplasm (SPN), cystic neuroendocrine tumor (NET), or pseudocyst. I also review symptoms, including abdominal pain, weight loss, history of pancreatitis, and onset of diabetes, and check hemoglobin A1c and Ca19-9. I often recommend magnetic resonance cholangiopancreatography (MRCP) if it has not already been obtained and is feasible (that is, if a patient does not have severe claustrophobia or a medical device incompatible with MRI). If a patient is not a candidate for treatment should a pancreatic malignancy be identified, because of age, comorbidities, or preference, I recommend no further evaluation.
Where cyst type remains unclear despite MRCP, and for cysts over 2 cm, I recommend endoscopic ultrasound (EUS) for fluid sampling to assist in determining cyst type and to rule out any other high-risk features. In accordance with international guidelines, if a patient has any concerning imaging features, including main pancreatic duct dilation >5 mm, solid component or mural nodule, or thickened or enhancing duct walls, regardless of cyst size, I recommend EUS to assess for and biopsy any solid component and to sample cyst fluid to examine for dysplasia. Given the lower sensitivity of CT for high-risk features, if MRCP is not feasible, for cysts 1-2 cm, I recommend EUS for better evaluation.
If a cyst is determined to be a cystic NET; main duct or mixed-type IPMN; MCN; or SPN; or a branch duct IPMN with mural nodule, high-grade dysplasia, or adenocarcinoma, and the patient is a surgical candidate, I refer the patient for surgical evaluation. If a cyst is determined to be an SCA, the malignant potential is minimal, and patients do not require follow-up. Patients with a pseudocyst are managed according to their clinical scenario.
Many patients have a proven or suspected branch duct IPMN, an indeterminate cyst, or multiple cysts. Cyst management during surveillance is then determined by the size of the largest cyst and stability of the cyst(s). Of note, patients with an IPMN also have been shown to have an elevated risk of concurrent pancreas adenocarcinoma, which I believe is one of the strongest arguments for heightened surveillance of the entire pancreas in pancreas cyst patients. EUS in particular can identify small or subtle lesions that are not detected by cross-sectional imaging.
If a patient has no prior imaging, in accordance with international and European guidelines, I recommend the first surveillance MRCP at a 6-month interval for cysts <2 cm, which may offer the opportunity to identify rapidly progressing cysts. If a patient has previous imaging available demonstrating stability, I recommend surveillance on an annual basis for cysts <2 cm. For patients with a cyst >2 cm, as above, I recommend EUS, and if there are no concerning features on imaging or EUS, I then recommend annual surveillance.
While the patient is under surveillance, if there is more than minimal cyst growth, a change in cyst appearance, or development of any imaging high-risk feature, pancreatitis, new onset or worsening diabetes, or elevation of Ca19-9, I recommend EUS for further evaluation and consideration of surgery based on EUS findings. If an asymptomatic cyst <2 cm remains stable for 5 years, I offer patients the option to extend imaging to every 2 years, if they are comfortable. In my experience, though, many patients prefer to continue annual imaging. The American Gastroenterological Association guidelines promote stopping surveillance after 5 years of stability, however there are studies demonstrating development of malignancy in cysts that were initially stable over the first 5 years of surveillance. Therefore, I discuss with patients that it is reasonable to continue cyst surveillance indefinitely, until they would no longer be interested in pursuing treatment of any kind if a malignant lesion were to be identified.
There are two special groups of pancreas cyst patients who warrant specific attention. Patients who are at elevated risk of pancreas adenocarcinoma because of an associated genetic mutation or a family history of pancreatic cancer already may be undergoing annual pancreas cancer screening with either MRCP, EUS, or alternating MRCP and EUS. When these high-risk patients also have pancreas cysts, I utilize whichever strategy would image their pancreas most frequently and do not extend beyond 1-year intervals. Another special group is patients who have undergone partial pancreatectomy for IPMN. As discussed above, given the elevated risk of concurrent pancreas adenocarcinoma in IPMN patients, I recommend indefinite continued surveillance of the remaining pancreas parenchyma in these patients.
Given the prevalence of pancreas cysts, it certainly would be convenient if guidelines were straightforward enough for primary care physicians to manage pancreas cyst surveillance, as they do for breast cancer screening. However, the complexities of pancreas cysts necessitate the expertise of gastroenterologists and pancreas surgeons, and a multidisciplinary team approach is best where possible.
Dr. Khanna is chief, advanced endoscopy, Tisch Hospital; director, NYU Advanced Endoscopy Fellowship; assistant professor of medicine, NYU Langone Health. Email: [email protected]. There are no relevant conflicts to disclose.
References
Tanaka M et al. Pancreatology. 2017 Sep-Oct;17(5):738-75.
Sahora K et al. Eur J Surg Oncol. 2016 Feb;42(2):197-204.
Del Chiaro M et al. Gut. 2018 May;67(5):789-804
Vege SS et al. Gastroenterology. 2015 Apr;148(4):819-22
Petrone MC et al. Clin Transl Gastroenterol. 2018 Jun 13;9(6):158
Pancreas cysts: More is not necessarily better!
BY SANTHI SWAROOP VEGE, MD
Pancreas cysts (PC) are very common, incidental findings on cross-sectional imaging, performed for non–pancreas-related symptoms. The important issues in management of patients with PC in my practice are the prevalence, natural history, frequency of occurrence of high-grade dysplasia (HGD) and/or pancreatic cancer (PDAC), concerning clinical symptoms and imaging findings, indications for EUS and fine-needle aspiration cytology, ideal method and frequency of surveillance, indications for surgery (up front and during follow-up), follow-up after surgery, stopping surveillance, costs, and unintentional harms of management. Good population-based evidence regarding many of the issues described above does not exist, and all information is from selected clinic, radiology, EUS, and surgical cohorts (very important when trying to assess the publications). Cohort studies should start with all PC undergoing surveillance and assess various outcomes, rather than looking backward from EUS or surgical cohorts.
The 2015 American Gastroenterological Association guidelines on asymptomatic neoplastic pancreas cysts, which I coauthored, recommend, consistent with principles of High Value Care (minimal unintentional harms and cost effectiveness), that two of three high-risk features (mural nodule, cyst size greater than 3 cm, and dilated pancreatic duct) be present for EUS-guided fine-needle aspiration (EUS-FNA). By the same token, they advise surgery for those with two of three high-risk features and or concerning features on EUS and cytology. Finally, they suggest stopping surveillance at 5 years if there are no significant changes. Rigorous GRADE methodology along with systematic review of all relevant questions (rather than cohorts of 500 or fewer patients) formed the basis of the guidelines. Those meta-analyses showed that risk of PDAC in mural nodules, cyst size >3 cm, and dilated pancreatic duct, while elevated, still is very low in absolute terms. Less than 20% of resections for highly selected, high-risk cysts showed PDAC. The guidelines were met with a lot of resistance from several societies and physician groups. The recommendations for stopping surveillance after 5 years and no surveillance for absent or low-grade dysplasia after surgery are hotly contested, and these areas need larger, long-term studies.
The whole area of cyst fluid molecular markers that would suggest mucinous type (KRAS and GNAS mutations) and, more importantly, the presence or imminent development of PDAC (next-generation sequencing or NGS) is an exciting field. One sincerely hopes that there will be a breakthrough in this area to achieve the holy grail. Cost effectiveness studies demonstrate the futility of existing guidelines and favor a less intensive approach. Guidelines are only a general framework, and management of individual patients in the clinic is entirely at the discretion of the treating physician. One should make every attempt to detect advanced lesions in PC, but such effort should not subject a large majority of patients to unintentional harms by overtreatment and add further to the burgeoning health care costs in the country.
PC are extremely common (10% of all abdominal imaging), increase with age, are seen in as many as 40%-50% of MRI examinations for nonpancreatic indications, and most (>50%) are IPMNs. Most of the debate centers around the concerns of PDAC and/or HGD associated with mucinous cysts (MCN, IPMN, side-branch, main duct, or mixed).
The various guidelines by multiple societies differ in some aspects, such as in selection of patients based on clinical, laboratory, and imaging findings for up-front surgery or surveillance, the frequency of surveillance based on the size of the cyst and the presence of other concerning cyst features (usually with MRCP), the indications for EUS (both initial and subsequent), importance of the magnitude of growth (most IPMNs slowly grow over a period of time), indications for surgery during surveillance and postsurgery surveillance, and the decision to stop surveillance at some point in time. The literature is replete with small case series reporting a proportion of cancers detected and often ignoring the harms of surgery. Incidence of and mortality caused by PDAC are very low (about 1% for both) in a large national cohort of VA pancreatic cyst patients with long-term follow-up and other studies.
Marcov modeling suggests that none of the guidelines would lead to cost-effective care with low mortality because of overtreatment of low-risk lesions, and a specificity of 67% or more for PDAC/HGB is required. AGA guidelines came close to it but with low sensitivity. Monte Carlo modeling suggests that less intensive strategies, compared with more intensive, result in a similar number of deaths at a much lower cost. While molecular markers in PC fluid are reported to increase the specificity of PDAC/HGD to greater than 70%, it should be observed that such validation was done in a small percentage of patients who had both those markers and resection.
The costs of expensive procedures like EUS, MRI, and surgery, the 3% complication rate with EUS-FNA (primarily acute pancreatitis), and the 1% mortality and approximately 20%-30% morbidity with surgery (bleeding, infection, fistula) and postpancreatectomy diabetes of approximately 30% in the long run need special attention.
In conclusion, one could say pancreas cysts are extremely frequent, most of the neoplastic cysts are mucinous (IPMN and MCN) and slowly growing over time without an associated cancer, and the greatest need at this time is to identify the small proportion of such cysts with PDAC and/or HGD. Until such time, judicious selection of patients for surveillance and reasonable intervals of such surveillance with selective use of EUS will help identify patients requiring resection. In our enthusiasm to detect every possible pancreatic cancer, we should not ignore the unintentional outcomes of surgery to a large majority of patients who would never develop PDAC and the astronomical costs associated with such practice.
Dr. Vege is professor of medicine at the Mayo Clinic. He reported having no conflicts of interest regarding this article.
References
Vege SS et al. Gastroenterology. 2015;148:819-22.
Lobo JM et al. Surgery. 2020;168:601-9.
Lennon AM and Vege SS. Clin Gastroenterol Hepatol. 2022;20:1663-7.
Harris RP. Ann Intern Med. 2015;162:787-9.
Dear colleagues,
Pancreas cysts have become almost ubiquitous in this era of high-resolution cross-sectional imaging. They are a common GI consult with patients and providers worried about the potential risk of malignant transformation. Despite significant research over the past few decades, predicting the natural history of these cysts, especially the side-branch intraductal papillary mucinous neoplasms (IPMNs), remains difficult. There have been a variety of expert recommendations and guidelines, but heterogeneity exists in management especially regarding timing of endoscopic ultrasound, imaging surveillance, and cessation of surveillance. Some centers will present these cysts at multidisciplinary conferences, while others will follow general or local algorithms. In this issue of Perspectives, Dr. Lauren G. Khanna, assistant professor of medicine at NYU Langone Health, New York, and Dr. Santhi Vege, professor of medicine at the Mayo Clinic, Rochester, Minn., present updated and differing approaches to managing these cysts. Which side of the debate are you on? We welcome your thoughts, questions and input– share with us on Twitter @AGA_GIHN
Gyanprakash A. Ketwaroo, MD, MSc, is associate professor of medicine, Yale University, New Haven, Conn., and chief of endoscopy at West Haven (Conn.) VA Medical Center. He is an associate editor for GI & Hepatology News.
Continuing pancreas cyst surveillance indefinitely is reasonable
BY LAUREN G. KHANNA, MD, MS
Pancreas cysts remain a clinical challenge. The true incidence of pancreas cysts is unknown, but from MRI and autopsy series, may be up to 50%. Patients presenting with a pancreas cyst often have significant anxiety about their risk of pancreas cancer. We as a medical community initially did too; but over the past few decades as we have gathered more data, we have become more comfortable observing many pancreas cysts. Yet our recommendations for how, how often, and for how long to evaluate pancreas cysts are still very much under debate; there are multiple guidelines with discordant recommendations. In this article, I will discuss my approach to patients with a pancreas cyst.
At the first evaluation, I review available imaging to see if there are characteristic features to determine the type of pancreas cyst: IPMN (including main duct, branch duct, or mixed type), serous cystic neoplasm (SCA), mucinous cystic neoplasm (MCN), solid pseudopapillary neoplasm (SPN), cystic neuroendocrine tumor (NET), or pseudocyst. I also review symptoms, including abdominal pain, weight loss, history of pancreatitis, and onset of diabetes, and check hemoglobin A1c and Ca19-9. I often recommend magnetic resonance cholangiopancreatography (MRCP) if it has not already been obtained and is feasible (that is, if a patient does not have severe claustrophobia or a medical device incompatible with MRI). If a patient is not a candidate for treatment should a pancreatic malignancy be identified, because of age, comorbidities, or preference, I recommend no further evaluation.
Where cyst type remains unclear despite MRCP, and for cysts over 2 cm, I recommend endoscopic ultrasound (EUS) for fluid sampling to assist in determining cyst type and to rule out any other high-risk features. In accordance with international guidelines, if a patient has any concerning imaging features, including main pancreatic duct dilation >5 mm, solid component or mural nodule, or thickened or enhancing duct walls, regardless of cyst size, I recommend EUS to assess for and biopsy any solid component and to sample cyst fluid to examine for dysplasia. Given the lower sensitivity of CT for high-risk features, if MRCP is not feasible, for cysts 1-2 cm, I recommend EUS for better evaluation.
If a cyst is determined to be a cystic NET; main duct or mixed-type IPMN; MCN; or SPN; or a branch duct IPMN with mural nodule, high-grade dysplasia, or adenocarcinoma, and the patient is a surgical candidate, I refer the patient for surgical evaluation. If a cyst is determined to be an SCA, the malignant potential is minimal, and patients do not require follow-up. Patients with a pseudocyst are managed according to their clinical scenario.
Many patients have a proven or suspected branch duct IPMN, an indeterminate cyst, or multiple cysts. Cyst management during surveillance is then determined by the size of the largest cyst and stability of the cyst(s). Of note, patients with an IPMN also have been shown to have an elevated risk of concurrent pancreas adenocarcinoma, which I believe is one of the strongest arguments for heightened surveillance of the entire pancreas in pancreas cyst patients. EUS in particular can identify small or subtle lesions that are not detected by cross-sectional imaging.
If a patient has no prior imaging, in accordance with international and European guidelines, I recommend the first surveillance MRCP at a 6-month interval for cysts <2 cm, which may offer the opportunity to identify rapidly progressing cysts. If a patient has previous imaging available demonstrating stability, I recommend surveillance on an annual basis for cysts <2 cm. For patients with a cyst >2 cm, as above, I recommend EUS, and if there are no concerning features on imaging or EUS, I then recommend annual surveillance.
While the patient is under surveillance, if there is more than minimal cyst growth, a change in cyst appearance, or development of any imaging high-risk feature, pancreatitis, new onset or worsening diabetes, or elevation of Ca19-9, I recommend EUS for further evaluation and consideration of surgery based on EUS findings. If an asymptomatic cyst <2 cm remains stable for 5 years, I offer patients the option to extend imaging to every 2 years, if they are comfortable. In my experience, though, many patients prefer to continue annual imaging. The American Gastroenterological Association guidelines promote stopping surveillance after 5 years of stability, however there are studies demonstrating development of malignancy in cysts that were initially stable over the first 5 years of surveillance. Therefore, I discuss with patients that it is reasonable to continue cyst surveillance indefinitely, until they would no longer be interested in pursuing treatment of any kind if a malignant lesion were to be identified.
There are two special groups of pancreas cyst patients who warrant specific attention. Patients who are at elevated risk of pancreas adenocarcinoma because of an associated genetic mutation or a family history of pancreatic cancer already may be undergoing annual pancreas cancer screening with either MRCP, EUS, or alternating MRCP and EUS. When these high-risk patients also have pancreas cysts, I utilize whichever strategy would image their pancreas most frequently and do not extend beyond 1-year intervals. Another special group is patients who have undergone partial pancreatectomy for IPMN. As discussed above, given the elevated risk of concurrent pancreas adenocarcinoma in IPMN patients, I recommend indefinite continued surveillance of the remaining pancreas parenchyma in these patients.
Given the prevalence of pancreas cysts, it certainly would be convenient if guidelines were straightforward enough for primary care physicians to manage pancreas cyst surveillance, as they do for breast cancer screening. However, the complexities of pancreas cysts necessitate the expertise of gastroenterologists and pancreas surgeons, and a multidisciplinary team approach is best where possible.
Dr. Khanna is chief, advanced endoscopy, Tisch Hospital; director, NYU Advanced Endoscopy Fellowship; assistant professor of medicine, NYU Langone Health. Email: [email protected]. There are no relevant conflicts to disclose.
References
Tanaka M et al. Pancreatology. 2017 Sep-Oct;17(5):738-75.
Sahora K et al. Eur J Surg Oncol. 2016 Feb;42(2):197-204.
Del Chiaro M et al. Gut. 2018 May;67(5):789-804
Vege SS et al. Gastroenterology. 2015 Apr;148(4):819-22
Petrone MC et al. Clin Transl Gastroenterol. 2018 Jun 13;9(6):158
Pancreas cysts: More is not necessarily better!
BY SANTHI SWAROOP VEGE, MD
Pancreas cysts (PC) are very common, incidental findings on cross-sectional imaging, performed for non–pancreas-related symptoms. The important issues in management of patients with PC in my practice are the prevalence, natural history, frequency of occurrence of high-grade dysplasia (HGD) and/or pancreatic cancer (PDAC), concerning clinical symptoms and imaging findings, indications for EUS and fine-needle aspiration cytology, ideal method and frequency of surveillance, indications for surgery (up front and during follow-up), follow-up after surgery, stopping surveillance, costs, and unintentional harms of management. Good population-based evidence regarding many of the issues described above does not exist, and all information is from selected clinic, radiology, EUS, and surgical cohorts (very important when trying to assess the publications). Cohort studies should start with all PC undergoing surveillance and assess various outcomes, rather than looking backward from EUS or surgical cohorts.
The 2015 American Gastroenterological Association guidelines on asymptomatic neoplastic pancreas cysts, which I coauthored, recommend, consistent with principles of High Value Care (minimal unintentional harms and cost effectiveness), that two of three high-risk features (mural nodule, cyst size greater than 3 cm, and dilated pancreatic duct) be present for EUS-guided fine-needle aspiration (EUS-FNA). By the same token, they advise surgery for those with two of three high-risk features and or concerning features on EUS and cytology. Finally, they suggest stopping surveillance at 5 years if there are no significant changes. Rigorous GRADE methodology along with systematic review of all relevant questions (rather than cohorts of 500 or fewer patients) formed the basis of the guidelines. Those meta-analyses showed that risk of PDAC in mural nodules, cyst size >3 cm, and dilated pancreatic duct, while elevated, still is very low in absolute terms. Less than 20% of resections for highly selected, high-risk cysts showed PDAC. The guidelines were met with a lot of resistance from several societies and physician groups. The recommendations for stopping surveillance after 5 years and no surveillance for absent or low-grade dysplasia after surgery are hotly contested, and these areas need larger, long-term studies.
The whole area of cyst fluid molecular markers that would suggest mucinous type (KRAS and GNAS mutations) and, more importantly, the presence or imminent development of PDAC (next-generation sequencing or NGS) is an exciting field. One sincerely hopes that there will be a breakthrough in this area to achieve the holy grail. Cost effectiveness studies demonstrate the futility of existing guidelines and favor a less intensive approach. Guidelines are only a general framework, and management of individual patients in the clinic is entirely at the discretion of the treating physician. One should make every attempt to detect advanced lesions in PC, but such effort should not subject a large majority of patients to unintentional harms by overtreatment and add further to the burgeoning health care costs in the country.
PC are extremely common (10% of all abdominal imaging), increase with age, are seen in as many as 40%-50% of MRI examinations for nonpancreatic indications, and most (>50%) are IPMNs. Most of the debate centers around the concerns of PDAC and/or HGD associated with mucinous cysts (MCN, IPMN, side-branch, main duct, or mixed).
The various guidelines by multiple societies differ in some aspects, such as in selection of patients based on clinical, laboratory, and imaging findings for up-front surgery or surveillance, the frequency of surveillance based on the size of the cyst and the presence of other concerning cyst features (usually with MRCP), the indications for EUS (both initial and subsequent), importance of the magnitude of growth (most IPMNs slowly grow over a period of time), indications for surgery during surveillance and postsurgery surveillance, and the decision to stop surveillance at some point in time. The literature is replete with small case series reporting a proportion of cancers detected and often ignoring the harms of surgery. Incidence of and mortality caused by PDAC are very low (about 1% for both) in a large national cohort of VA pancreatic cyst patients with long-term follow-up and other studies.
Marcov modeling suggests that none of the guidelines would lead to cost-effective care with low mortality because of overtreatment of low-risk lesions, and a specificity of 67% or more for PDAC/HGB is required. AGA guidelines came close to it but with low sensitivity. Monte Carlo modeling suggests that less intensive strategies, compared with more intensive, result in a similar number of deaths at a much lower cost. While molecular markers in PC fluid are reported to increase the specificity of PDAC/HGD to greater than 70%, it should be observed that such validation was done in a small percentage of patients who had both those markers and resection.
The costs of expensive procedures like EUS, MRI, and surgery, the 3% complication rate with EUS-FNA (primarily acute pancreatitis), and the 1% mortality and approximately 20%-30% morbidity with surgery (bleeding, infection, fistula) and postpancreatectomy diabetes of approximately 30% in the long run need special attention.
In conclusion, one could say pancreas cysts are extremely frequent, most of the neoplastic cysts are mucinous (IPMN and MCN) and slowly growing over time without an associated cancer, and the greatest need at this time is to identify the small proportion of such cysts with PDAC and/or HGD. Until such time, judicious selection of patients for surveillance and reasonable intervals of such surveillance with selective use of EUS will help identify patients requiring resection. In our enthusiasm to detect every possible pancreatic cancer, we should not ignore the unintentional outcomes of surgery to a large majority of patients who would never develop PDAC and the astronomical costs associated with such practice.
Dr. Vege is professor of medicine at the Mayo Clinic. He reported having no conflicts of interest regarding this article.
References
Vege SS et al. Gastroenterology. 2015;148:819-22.
Lobo JM et al. Surgery. 2020;168:601-9.
Lennon AM and Vege SS. Clin Gastroenterol Hepatol. 2022;20:1663-7.
Harris RP. Ann Intern Med. 2015;162:787-9.
New clinical guideline for biliary strictures issued
The recommendations provide guidance on the care of patients with extrahepatic and perihilar strictures, with a focus on diagnosis and drainage. Although some of the principles may apply to intrahepatic strictures, the guideline doesn’t specifically address them. The new guideline is considered separate from the 2015 ACG guideline related to primary sclerosing cholangitis.
“The appropriate diagnosis and management of biliary strictures is still a big clinical challenge and has important implications in endoscopic, surgical, and oncological decision-making,” co-author Jennifer Maranki, MD, a professor of medicine and director of endoscopy at Penn State Hershey Medical Center, said in an interview.
“We wanted to provide the best possible guidance to gastroenterologists based on the available body of literature, with key shifts in diagnosis and management based on currently available modalities and tools,” she said.
The guideline was published in the March issue of the American Journal of Gastroenterology.
The recommendations were developed by a diverse group of authors from across the United States in recognition of the potential influence of commercial and intellectual conflicts of interest. The panel used a systematic process that involved structured literature searches by librarians and independent appraisal of the quality of evidence by dedicated methodologists, the authors write.
Overall, the team outlined 11 recommendations and 12 key concepts. A strong recommendation was made when the benefits of the test or intervention clearly outweighed the potential disadvantages. A conditional recommendation was made when some uncertainty remained about the balance of benefits and harms. Key concepts address important clinical questions that lack adequate evidence to inform recommendations. They are based on indirect evidence and expert opinion.
Epidemiology and diagnosis
The burden of biliary strictures is difficult to estimate, owing to the lack of a specific administrative code. The estimated cost of caring for biliary disease in the United States is about $16.9 billion annually, although this figure includes costs associated with gallbladder disease, choledocholithiasis, and other (nonobstructive) biliary disorders, the authors write.
Among the 57,000 new cases of pancreatic cancer each year, at least 60% will cause obstructive jaundice, resulting in about 34,000 annual cases of malignant extrahepatic biliary stricture, the team notes. In addition, about 3,000 cases of malignant perihilar stricture are expected in the United States each year. Patients may also seek care for benign strictures associated with chronic pancreatitis, primary sclerosing cholangitis, autoimmune disease, and post-cholecystectomy injury.
Under the first key concept, the authors note that biliary strictures in adults are more likely to be malignant than benign, except in certain well-defined scenarios. This underscores the importance of having a high index of clinical suspicion during evaluation, they add.
In general, a definitive tissue diagnosis is necessary to guide oncologic and endoscopic care for most strictures that aren’t surgically resectable at the time of presentation. For patients with extrahepatic biliary stricture due to an apparent or suspected pancreatic mass, endoscopic ultrasound (EUS) with fine-needle sampling (aspiration or biopsy) is recommended over endoscopic retrograde cholangiopancreatography (ERCP) as the preferred method of evaluation for malignancy.
For patients with suspected malignant perihilar stricture, multimodality sampling is recommended over brush cytology alone at the time of the index ERCP.
Guidance on drainage
For management, the principal objective is to restore the physiologic flow of bile into the duodenum. Although there is wide variability in the difficulty and risk of drainage, depending on location and complexity, perihilar strictures are generally more challenging and are riskier to drain than extrahepatic strictures. The goals should be to alleviate symptoms, reduce serum bilirubin to a level such that chemotherapy can be safely administered, and optimize surgical outcomes.
For benign extrahepatic biliary strictures, ERCP is the preferred modality for durable treatment. Fully covered self-expanding metallic stent (SEMS) placement is recommended over multiple plastic stents to reduce the number of procedures required for long-term treatment.
For extrahepatic strictures due to resectable pancreatic cancer or cholangiocarcinoma, the authors recommend against routine preoperative biliary drainage. However, drainage is warranted for some patients, including those with acute cholangitis, severe pruritus, very high serum bilirubin levels, those undergoing neoadjuvant therapy, and those for whom surgery is delayed.
For malignant extrahepatic strictures that are unresectable or borderline resectable, SEMS placement is recommended over plastic stents. The evidence is insufficient to recommend for or against uncovered SEMS versus fully covered SEMS.
For perihilar strictures due to suspected malignancy, the evidence is insufficient to recommend for or against ERCP versus percutaneous transhepatic biliary drainage. In addition, for malignant perihilar strictures, the evidence is insufficient to recommend for or against plastic stents versus uncovered SEMS.
For perihilar strictures due to cholangiocarcinoma in cases in which resection or transplantation is not possible, adjuvant endobiliary ablation plus plastic stent placement is recommended over plastic stent placement alone.
Overall, for patients with a biliary stricture for which ERCP is indicated but is unsuccessful or impossible, EUS-guided biliary access and drainage is recommended over PTBD, because it is associated with fewer adverse events. However, these interventional EUS procedures should be performed by an endoscopist with substantial experience.
“The workup of biliary strictures is challenging, invasive, and costly, requiring multiple diagnostic tools with highly variable yields,” co-author Victoria Gomez, MD, associate professor of medicine and director of bariatric endoscopy at Mayo Clinic, Jacksonville, Fla., said in an interview.
“Providers caring for these patients must be up to date with the most current evidence so that they can make the safest and most well-informed decisions for their patients,” she said. “These include considerations such as limiting the use of anesthesia, using tests that will result in the highest diagnostic yield, and providing effective therapies to decompress biliary obstruction.”
Future questions
Additional research is needed in several areas to strengthen recommendations and advance the field, the study authors write.
“Biliary strictures without an associated mass are a diagnostic challenge, and there are exciting opportunities to understand how new technologies, such as artificial intelligence, can be used to improve our assessment,” co-author Anna Tavakkoli, MD, assistant professor of internal medicine in digestive and liver diseases at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
“Also, we highlighted several controversies in the drainage of perihilar strictures, including whether to use ERCP versus percutaneous drainage, whether metallic or plastic stents are better, and what the optimal stent placement should be,” she said. “Future multicenter studies are needed to address these key controversies.”
Although fully covered SEMS placement remains effective for benign biliary strictures, multiple plastic stents may be a better alternative in some cases. Such cases include those in which the stricture is close to the hilum, those in which the gallbladder is intact and in which crossing the cystic duct orifice cannot be avoided, those in which a fully covered SEMS has previously migrated or was not well tolerated, and those in which stricture has recurred after removal of a fully covered SEMS.
‘Comprehensive list’
“Overall, the authors have done a commendable job putting together a comprehensive list of recommendations that will invariably alter the practice of many therapeutic endoscopists for the diagnosis and management of biliary strictures,” Matthew Fasullo, DO, an advanced endoscopy and gastroenterology fellow at New York University Medical Center, told this news organization.
Dr. Fasullo, who wasn’t involved with the guideline, has published on advances in pathophysiology, diagnosis, and treatment for post-transplant biliary complications.
“The fact that ... cholangioscopy-directed biopsies after an initial negative evaluation via ERCP reveal malignancy in 54% of cases underscores the need for best practice guidelines and supports advancements in diagnostics to confidently rule in or out cancer,” he said.
“The movement toward multimodality sampling at the time of initial evaluation with a combination of brushing, fluoroscopy-directed biopsies, cholangioscopy-directed biopsies, and fluorescence in situ hybridization should become universally adopted in those with an ambiguous diagnosis,” he added. “As technology continues to improve, next-generation sequencing will prove to be an invaluable adjunct to the current pathological evaluation.”
The authors received no financial support for the guideline. One author has a consultant role for Takeda Pharmaceuticals and is an advisory board member role for Advarra. The other authors and Dr. Fasullo have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The recommendations provide guidance on the care of patients with extrahepatic and perihilar strictures, with a focus on diagnosis and drainage. Although some of the principles may apply to intrahepatic strictures, the guideline doesn’t specifically address them. The new guideline is considered separate from the 2015 ACG guideline related to primary sclerosing cholangitis.
“The appropriate diagnosis and management of biliary strictures is still a big clinical challenge and has important implications in endoscopic, surgical, and oncological decision-making,” co-author Jennifer Maranki, MD, a professor of medicine and director of endoscopy at Penn State Hershey Medical Center, said in an interview.
“We wanted to provide the best possible guidance to gastroenterologists based on the available body of literature, with key shifts in diagnosis and management based on currently available modalities and tools,” she said.
The guideline was published in the March issue of the American Journal of Gastroenterology.
The recommendations were developed by a diverse group of authors from across the United States in recognition of the potential influence of commercial and intellectual conflicts of interest. The panel used a systematic process that involved structured literature searches by librarians and independent appraisal of the quality of evidence by dedicated methodologists, the authors write.
Overall, the team outlined 11 recommendations and 12 key concepts. A strong recommendation was made when the benefits of the test or intervention clearly outweighed the potential disadvantages. A conditional recommendation was made when some uncertainty remained about the balance of benefits and harms. Key concepts address important clinical questions that lack adequate evidence to inform recommendations. They are based on indirect evidence and expert opinion.
Epidemiology and diagnosis
The burden of biliary strictures is difficult to estimate, owing to the lack of a specific administrative code. The estimated cost of caring for biliary disease in the United States is about $16.9 billion annually, although this figure includes costs associated with gallbladder disease, choledocholithiasis, and other (nonobstructive) biliary disorders, the authors write.
Among the 57,000 new cases of pancreatic cancer each year, at least 60% will cause obstructive jaundice, resulting in about 34,000 annual cases of malignant extrahepatic biliary stricture, the team notes. In addition, about 3,000 cases of malignant perihilar stricture are expected in the United States each year. Patients may also seek care for benign strictures associated with chronic pancreatitis, primary sclerosing cholangitis, autoimmune disease, and post-cholecystectomy injury.
Under the first key concept, the authors note that biliary strictures in adults are more likely to be malignant than benign, except in certain well-defined scenarios. This underscores the importance of having a high index of clinical suspicion during evaluation, they add.
In general, a definitive tissue diagnosis is necessary to guide oncologic and endoscopic care for most strictures that aren’t surgically resectable at the time of presentation. For patients with extrahepatic biliary stricture due to an apparent or suspected pancreatic mass, endoscopic ultrasound (EUS) with fine-needle sampling (aspiration or biopsy) is recommended over endoscopic retrograde cholangiopancreatography (ERCP) as the preferred method of evaluation for malignancy.
For patients with suspected malignant perihilar stricture, multimodality sampling is recommended over brush cytology alone at the time of the index ERCP.
Guidance on drainage
For management, the principal objective is to restore the physiologic flow of bile into the duodenum. Although there is wide variability in the difficulty and risk of drainage, depending on location and complexity, perihilar strictures are generally more challenging and are riskier to drain than extrahepatic strictures. The goals should be to alleviate symptoms, reduce serum bilirubin to a level such that chemotherapy can be safely administered, and optimize surgical outcomes.
For benign extrahepatic biliary strictures, ERCP is the preferred modality for durable treatment. Fully covered self-expanding metallic stent (SEMS) placement is recommended over multiple plastic stents to reduce the number of procedures required for long-term treatment.
For extrahepatic strictures due to resectable pancreatic cancer or cholangiocarcinoma, the authors recommend against routine preoperative biliary drainage. However, drainage is warranted for some patients, including those with acute cholangitis, severe pruritus, very high serum bilirubin levels, those undergoing neoadjuvant therapy, and those for whom surgery is delayed.
For malignant extrahepatic strictures that are unresectable or borderline resectable, SEMS placement is recommended over plastic stents. The evidence is insufficient to recommend for or against uncovered SEMS versus fully covered SEMS.
For perihilar strictures due to suspected malignancy, the evidence is insufficient to recommend for or against ERCP versus percutaneous transhepatic biliary drainage. In addition, for malignant perihilar strictures, the evidence is insufficient to recommend for or against plastic stents versus uncovered SEMS.
For perihilar strictures due to cholangiocarcinoma in cases in which resection or transplantation is not possible, adjuvant endobiliary ablation plus plastic stent placement is recommended over plastic stent placement alone.
Overall, for patients with a biliary stricture for which ERCP is indicated but is unsuccessful or impossible, EUS-guided biliary access and drainage is recommended over PTBD, because it is associated with fewer adverse events. However, these interventional EUS procedures should be performed by an endoscopist with substantial experience.
“The workup of biliary strictures is challenging, invasive, and costly, requiring multiple diagnostic tools with highly variable yields,” co-author Victoria Gomez, MD, associate professor of medicine and director of bariatric endoscopy at Mayo Clinic, Jacksonville, Fla., said in an interview.
“Providers caring for these patients must be up to date with the most current evidence so that they can make the safest and most well-informed decisions for their patients,” she said. “These include considerations such as limiting the use of anesthesia, using tests that will result in the highest diagnostic yield, and providing effective therapies to decompress biliary obstruction.”
Future questions
Additional research is needed in several areas to strengthen recommendations and advance the field, the study authors write.
“Biliary strictures without an associated mass are a diagnostic challenge, and there are exciting opportunities to understand how new technologies, such as artificial intelligence, can be used to improve our assessment,” co-author Anna Tavakkoli, MD, assistant professor of internal medicine in digestive and liver diseases at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
“Also, we highlighted several controversies in the drainage of perihilar strictures, including whether to use ERCP versus percutaneous drainage, whether metallic or plastic stents are better, and what the optimal stent placement should be,” she said. “Future multicenter studies are needed to address these key controversies.”
Although fully covered SEMS placement remains effective for benign biliary strictures, multiple plastic stents may be a better alternative in some cases. Such cases include those in which the stricture is close to the hilum, those in which the gallbladder is intact and in which crossing the cystic duct orifice cannot be avoided, those in which a fully covered SEMS has previously migrated or was not well tolerated, and those in which stricture has recurred after removal of a fully covered SEMS.
‘Comprehensive list’
“Overall, the authors have done a commendable job putting together a comprehensive list of recommendations that will invariably alter the practice of many therapeutic endoscopists for the diagnosis and management of biliary strictures,” Matthew Fasullo, DO, an advanced endoscopy and gastroenterology fellow at New York University Medical Center, told this news organization.
Dr. Fasullo, who wasn’t involved with the guideline, has published on advances in pathophysiology, diagnosis, and treatment for post-transplant biliary complications.
“The fact that ... cholangioscopy-directed biopsies after an initial negative evaluation via ERCP reveal malignancy in 54% of cases underscores the need for best practice guidelines and supports advancements in diagnostics to confidently rule in or out cancer,” he said.
“The movement toward multimodality sampling at the time of initial evaluation with a combination of brushing, fluoroscopy-directed biopsies, cholangioscopy-directed biopsies, and fluorescence in situ hybridization should become universally adopted in those with an ambiguous diagnosis,” he added. “As technology continues to improve, next-generation sequencing will prove to be an invaluable adjunct to the current pathological evaluation.”
The authors received no financial support for the guideline. One author has a consultant role for Takeda Pharmaceuticals and is an advisory board member role for Advarra. The other authors and Dr. Fasullo have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The recommendations provide guidance on the care of patients with extrahepatic and perihilar strictures, with a focus on diagnosis and drainage. Although some of the principles may apply to intrahepatic strictures, the guideline doesn’t specifically address them. The new guideline is considered separate from the 2015 ACG guideline related to primary sclerosing cholangitis.
“The appropriate diagnosis and management of biliary strictures is still a big clinical challenge and has important implications in endoscopic, surgical, and oncological decision-making,” co-author Jennifer Maranki, MD, a professor of medicine and director of endoscopy at Penn State Hershey Medical Center, said in an interview.
“We wanted to provide the best possible guidance to gastroenterologists based on the available body of literature, with key shifts in diagnosis and management based on currently available modalities and tools,” she said.
The guideline was published in the March issue of the American Journal of Gastroenterology.
The recommendations were developed by a diverse group of authors from across the United States in recognition of the potential influence of commercial and intellectual conflicts of interest. The panel used a systematic process that involved structured literature searches by librarians and independent appraisal of the quality of evidence by dedicated methodologists, the authors write.
Overall, the team outlined 11 recommendations and 12 key concepts. A strong recommendation was made when the benefits of the test or intervention clearly outweighed the potential disadvantages. A conditional recommendation was made when some uncertainty remained about the balance of benefits and harms. Key concepts address important clinical questions that lack adequate evidence to inform recommendations. They are based on indirect evidence and expert opinion.
Epidemiology and diagnosis
The burden of biliary strictures is difficult to estimate, owing to the lack of a specific administrative code. The estimated cost of caring for biliary disease in the United States is about $16.9 billion annually, although this figure includes costs associated with gallbladder disease, choledocholithiasis, and other (nonobstructive) biliary disorders, the authors write.
Among the 57,000 new cases of pancreatic cancer each year, at least 60% will cause obstructive jaundice, resulting in about 34,000 annual cases of malignant extrahepatic biliary stricture, the team notes. In addition, about 3,000 cases of malignant perihilar stricture are expected in the United States each year. Patients may also seek care for benign strictures associated with chronic pancreatitis, primary sclerosing cholangitis, autoimmune disease, and post-cholecystectomy injury.
Under the first key concept, the authors note that biliary strictures in adults are more likely to be malignant than benign, except in certain well-defined scenarios. This underscores the importance of having a high index of clinical suspicion during evaluation, they add.
In general, a definitive tissue diagnosis is necessary to guide oncologic and endoscopic care for most strictures that aren’t surgically resectable at the time of presentation. For patients with extrahepatic biliary stricture due to an apparent or suspected pancreatic mass, endoscopic ultrasound (EUS) with fine-needle sampling (aspiration or biopsy) is recommended over endoscopic retrograde cholangiopancreatography (ERCP) as the preferred method of evaluation for malignancy.
For patients with suspected malignant perihilar stricture, multimodality sampling is recommended over brush cytology alone at the time of the index ERCP.
Guidance on drainage
For management, the principal objective is to restore the physiologic flow of bile into the duodenum. Although there is wide variability in the difficulty and risk of drainage, depending on location and complexity, perihilar strictures are generally more challenging and are riskier to drain than extrahepatic strictures. The goals should be to alleviate symptoms, reduce serum bilirubin to a level such that chemotherapy can be safely administered, and optimize surgical outcomes.
For benign extrahepatic biliary strictures, ERCP is the preferred modality for durable treatment. Fully covered self-expanding metallic stent (SEMS) placement is recommended over multiple plastic stents to reduce the number of procedures required for long-term treatment.
For extrahepatic strictures due to resectable pancreatic cancer or cholangiocarcinoma, the authors recommend against routine preoperative biliary drainage. However, drainage is warranted for some patients, including those with acute cholangitis, severe pruritus, very high serum bilirubin levels, those undergoing neoadjuvant therapy, and those for whom surgery is delayed.
For malignant extrahepatic strictures that are unresectable or borderline resectable, SEMS placement is recommended over plastic stents. The evidence is insufficient to recommend for or against uncovered SEMS versus fully covered SEMS.
For perihilar strictures due to suspected malignancy, the evidence is insufficient to recommend for or against ERCP versus percutaneous transhepatic biliary drainage. In addition, for malignant perihilar strictures, the evidence is insufficient to recommend for or against plastic stents versus uncovered SEMS.
For perihilar strictures due to cholangiocarcinoma in cases in which resection or transplantation is not possible, adjuvant endobiliary ablation plus plastic stent placement is recommended over plastic stent placement alone.
Overall, for patients with a biliary stricture for which ERCP is indicated but is unsuccessful or impossible, EUS-guided biliary access and drainage is recommended over PTBD, because it is associated with fewer adverse events. However, these interventional EUS procedures should be performed by an endoscopist with substantial experience.
“The workup of biliary strictures is challenging, invasive, and costly, requiring multiple diagnostic tools with highly variable yields,” co-author Victoria Gomez, MD, associate professor of medicine and director of bariatric endoscopy at Mayo Clinic, Jacksonville, Fla., said in an interview.
“Providers caring for these patients must be up to date with the most current evidence so that they can make the safest and most well-informed decisions for their patients,” she said. “These include considerations such as limiting the use of anesthesia, using tests that will result in the highest diagnostic yield, and providing effective therapies to decompress biliary obstruction.”
Future questions
Additional research is needed in several areas to strengthen recommendations and advance the field, the study authors write.
“Biliary strictures without an associated mass are a diagnostic challenge, and there are exciting opportunities to understand how new technologies, such as artificial intelligence, can be used to improve our assessment,” co-author Anna Tavakkoli, MD, assistant professor of internal medicine in digestive and liver diseases at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
“Also, we highlighted several controversies in the drainage of perihilar strictures, including whether to use ERCP versus percutaneous drainage, whether metallic or plastic stents are better, and what the optimal stent placement should be,” she said. “Future multicenter studies are needed to address these key controversies.”
Although fully covered SEMS placement remains effective for benign biliary strictures, multiple plastic stents may be a better alternative in some cases. Such cases include those in which the stricture is close to the hilum, those in which the gallbladder is intact and in which crossing the cystic duct orifice cannot be avoided, those in which a fully covered SEMS has previously migrated or was not well tolerated, and those in which stricture has recurred after removal of a fully covered SEMS.
‘Comprehensive list’
“Overall, the authors have done a commendable job putting together a comprehensive list of recommendations that will invariably alter the practice of many therapeutic endoscopists for the diagnosis and management of biliary strictures,” Matthew Fasullo, DO, an advanced endoscopy and gastroenterology fellow at New York University Medical Center, told this news organization.
Dr. Fasullo, who wasn’t involved with the guideline, has published on advances in pathophysiology, diagnosis, and treatment for post-transplant biliary complications.
“The fact that ... cholangioscopy-directed biopsies after an initial negative evaluation via ERCP reveal malignancy in 54% of cases underscores the need for best practice guidelines and supports advancements in diagnostics to confidently rule in or out cancer,” he said.
“The movement toward multimodality sampling at the time of initial evaluation with a combination of brushing, fluoroscopy-directed biopsies, cholangioscopy-directed biopsies, and fluorescence in situ hybridization should become universally adopted in those with an ambiguous diagnosis,” he added. “As technology continues to improve, next-generation sequencing will prove to be an invaluable adjunct to the current pathological evaluation.”
The authors received no financial support for the guideline. One author has a consultant role for Takeda Pharmaceuticals and is an advisory board member role for Advarra. The other authors and Dr. Fasullo have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY